3
www.thevillagenews.co.za
22 April 2020
I think I may have COVID-19 – now what? Writer Hedda Mittner
T
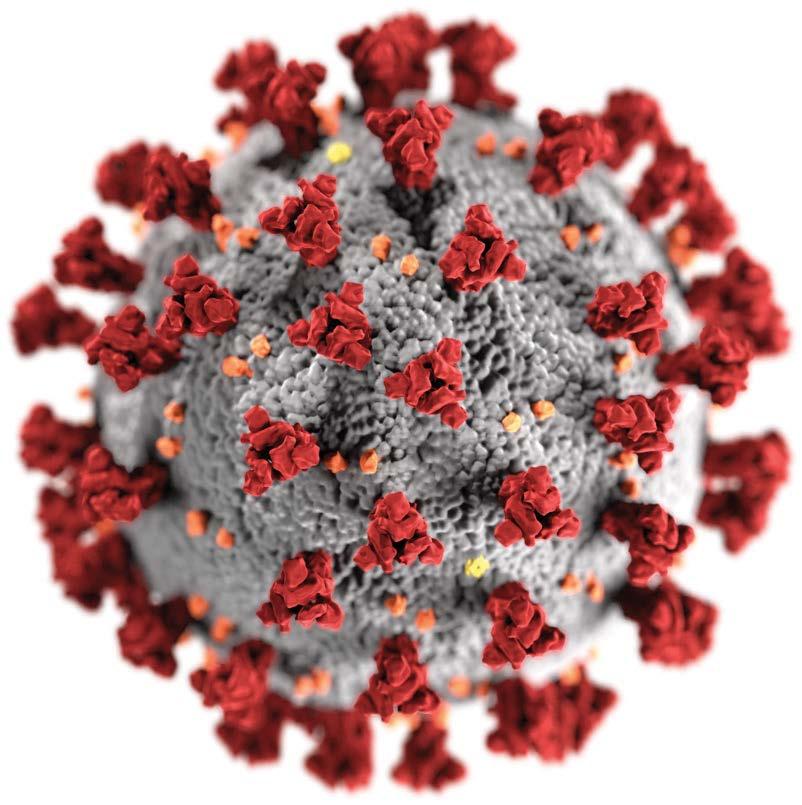
he public has been inundated with information on how to protect themselves during this global pandemic to prevent becoming infected by the Coronavirus, and spreading it to others. Understandably, this has created stress and anxiety, but it is important to remember that, if you adhere to the health safety protocols, the chances of contracting COVID-19, the disease caused by the novel Coronavirus, SARS-CoV-2, are relatively small. While it’s easy to become fixated on the devastating scenes being played out in the ICUs of hospitals in Europe, the UK and US, we should also remind ourselves that the overwhelming majority of people who are infected with Coronavirus experience an asymptomatic or mild disease which can be treated at home. Unfortunately this encouraging fact is also the reason why COVID-19 is so contagious and widespread. The latest research studies, using blood tests to look for antibodies, are showing that the number of undetected cases of COVID-19 are much higher than the confirmed cases. This means that more people have been infected by the virus while showing none or only very mild symptoms, and may be contributing to the spread of the disease without knowing it. What are my chances of getting sick? With winter approaching, many people will be contracting the “normal flu” and you might at first be unsure what your symptoms mean – is it just a cold, a bout of seasonal flu, or the dreaded Coronavirus? While a cold is called exactly that because patients generally don’t develop a fever, there are some similarities between COVID-19 and the seasonal flu, both of which are viral respiratory infections that spread from person to person. Flu viruses have been with us for a long time and there are basically two types – Influenza A (with several subtypes) and Influenza B. As its name implies, the novel Coronavirus is a new virus that has spread exponentially, which is why researchers and scientists have not had time to develop treatments and vaccines for the disease. But it is not all bad news. Although COVID-19 spreads faster than ordinary flu and has a higher chance of developing into a critical
infection and death, about 80% of those infected will be able to recover on their own. According to the World Health Organisation (WHO), around 15% of recorded COVID-19 cases are severe, and 5% are critical. These patients may require hospitalisation and often the administration of oxygen or mechanical ventilation. There is no definitive mortality rate for COVID-19 at this time, mainly due to the variation in factors such as age and location, but the range is estimated to be between 0.25 and 3%. This is still higher than the mortality rate of Influenza, which is estimated to be around 0.1%. As grim as these statistics are, the chances are still overwhelmingly in your favour of being one of the mild or asymptomatic cases, especially if you are under 65, if you are reasonably fit and healthy and not obese, if your immune system is not suppressed, if you are not a smoker and don’t have underlying medical conditions such as heart or lung disease, diabetes, asthma, or liver or renal disease. It also helps to be a woman, as statistics indicate that men are almost twice as likely to die from COVID-19.
usually more abrupt and you are likely to suffer body aches and pains, fatigue, fever and chills, in addition to a variation of cold-like symptoms. These flu symptoms do overlap with those of COVID-19 in its early stage, but there are small differences to look out for. With flu, the symptoms set in rapidly but usually remain mild and are resolved within about a week. The incubation period for COVID-19 is 2 – 14 days and symptoms set in more gradually and may be difficult to distinguish at first. Like a cold, the infection starts in the upper part of the respiratory system and the point where you should start paying attention is when it moves lower down, into the chest. This may only happen a week or more after the initial symptoms started. The most common symptoms to look out for are a persistent cough, fever (a temperature above 37.8°C), shortness of breath and difficulty breathing. If you are experiencing any of these symptoms, you should contact your GP, the nearest clinic or hospital in order to be tested for COVID-19.
The overwhelming majority of people who are infected experience an asymptomatic or mild disease which can be treated at home
What are the differences between flu and COVID-19? So, if you do start to feel sick, the last thing you want to do is panic and immediately start catastrophizing about the possible outcome. First make sure that you are not just suffering from a cold or seasonal flu (which you may have contracted anyway, pandemic or no pandemic). We all know what it feels like: sneezing, sore throat, runny or stuffy nose, headache. As long as you don’t have a fever or a severe cough, it’s probably the common cold. If in doubt, contact your GP or pharmacist for advice and try to keep calm while giving your body a chance to recover. What you do have to do, however, is to self-isolate immediately in order to protect your loved ones and your community until you have a definite diagnosis. People who have the flu will typically experience symptoms within 1 – 4 days. The onset is
What if I test positive? Do not put off having the test because of fear or denial. You should also not feel stigmatised or ashamed, as contracting COVID-19 does not necessarily mean that you’ve done anything wrong, or that you’ve somehow managed to bring this on yourself. With any disease as contagious and insidious as COVID-19, you may never know for sure how, where or when you were exposed to the virus. If you have tested positive, you will be interviewed by a contact tracer and asked to provide a list of your movements and those you had come into contact with over the 14 days prior to the development of your first symptoms. Unless you have developed complications such as pneumonia or have serious underlying health conditions, you will probably be advised by the medical facility where your test was conducted to self-isolate and manage your symptoms at home. Treating COVID-19 at home There is currently no cure for COVID-19 and the aim of treatment is to manage and reduce symptoms until you have recovered. As with other viruses such as colds and flu, taking it easy and looking after yourself are crucial to your recovery. So what should you
do to feel better? • Drink plenty of fluids. Drink enough water so that your urine is a pale, clear colour. Avoid alcohol as this will make you more dehydrated. • Get enough rest and avoid any strenuous activity whilst you are unwell. • Eat nutritious meals that include fresh fruit and vegetables, nuts, legumes, fish and poultry. • Use over-the-counter medicines to treat some of your symptoms. To relieve pain and fever, it is recommended that you use a painkiller like paracetamol rather than anti-inflammatory drugs such as aspirin, ibuprofen and naproxen. (However, if you have been prescribed an NSAID to treat a health condition, you should continue to take it until you are told not to by your doctor.) Your GP or pharmacist will be able to advise you on other medications used to treat colds and flu, such as cough syrup or throat lozenges, which could also alleviate symptoms. • Do not take any antibiotics you may have lying around at home to treat COVID-19. As it is a viral disease, antibiotics will have no effect. (You should in any case never take antibiotics which haven't been prescribed for a certain condition by a medical practitioner.) • Although there is no ‘miracle cure’ for COVID-19, there are proven herbal remedies that have strong anti-inflammatory properties and are also high in antioxidants, such as ginger and turmeric. Add them to freshly-squeezed orange juice or make a soothing hot drink with water, lemon, honey, ginger and a pinch of turmeric. • Supplements that may help to support your immune system include Vitamin C, Vitamin D, Vitamin B-complex, Zinc, Selenium, Echinacea, Elderberry and Licorice. But be careful not to suddenly overload your system with large doses of supplements or start experimenting with new herbal remedies without checking with your doctor or pharmacist, as some may have properties that could be potentially harmful. • Monitor your symptoms and your temperature. Stay in touch with your doctor and report any deterioration in your condition. If your symptoms are worsening and you have difficulty breathing or are experiencing persistent pain or pressure in the chest, contact your doctor or local healthcare provider. How to get tested for COVID-19 – See P7 How to self-isolate at home – See P9 Sources: cdc.gov; patient.info; medicalnewstoday.com; healthline.com; news24.com
GET CASH BACK AND FREE MEMBER BENEFITS If you as the policy premium payer are claim-free for five consecutive years, you’ll get your fifth year’s premiums back in CASH*.
MEMBER BENEFITS* In the event of retrenchment, the policy premium payer receives a six-month premium holiday
PLUS FREE funeral benefits* provided by AVBOB Funeral Service
You get ALL this on top of your full policy pay-out – it’s all 100% FREE* to AVBOB members.
Contact AVBOB Hermanus on 028 312 1156. *Terms and conditions apply. Free funeral benefits only apply if AVBOB Funeral Service conducts the funeral. AVBOB is an authorised financial services provider. AVBOB is a level 2 B-BBEE contributor. FSP 20656. www.AVBOB.co.za Google Play and the Google Play logo are trademarks of Google LLC.
AVB-VIL-191127
A FREE basic funeral valued at R11 000, which includes the funeral arrangements, a specified coffin and hearse A R2 500 immediate cash payment for initial expenses FREE transport of the deceased within the borders of South Africa