


Agenda 1 Contents Floor Plan of Conference Rooms ....................................................................................... 2 Daily Program Schedule ...................................................................................................... 5 Opening Remarks ................................................................................................................. 7 Board of Directors ................................................................................................................. 9 Moderator & Speaker.......................................................................................................... 10 Sponsors 13 Agenda ................................................................................................................................. 14 Abstract PL:Plenary Lecture (1-4) ................................................................................................. 39 DAROC-TADE:DAROC – TADE Joint Symposium .................................................... 43 MTP-E:Meet the Professor-Endocrine 1 & Endocrine 2................................................. 49 MTP-D:Meet the Professor-Diabetes .............................................................................. 52 SE:Symposium-Endocrine (1-9) ...................................................................................... 54 SD:Symposium-Diabetes (1-9) ........................................................................................ 88 OE:Oral Presentation-Endocrine(1-6) 117 OD: O ral P resentation-Diabetes (1-6) 126 AR:2023 Outstanding Research Award 135 AP:2023 Outstanding Paper Award(1-4) .................................................................... 137 PE:Poster Presentation-Endocrine(1-23 ) ...................................................................... 145 PD:Poster Presentation- Diabetes(1-24) ..................................................................... 179 BP:Brief Research Proposal of Pharmaceutical Company (1-5) .............................. 218

2 Annual Meeting of the Endocrine Society and the Diabetes Association of the R.O.C. (Taiwan) The45 th March
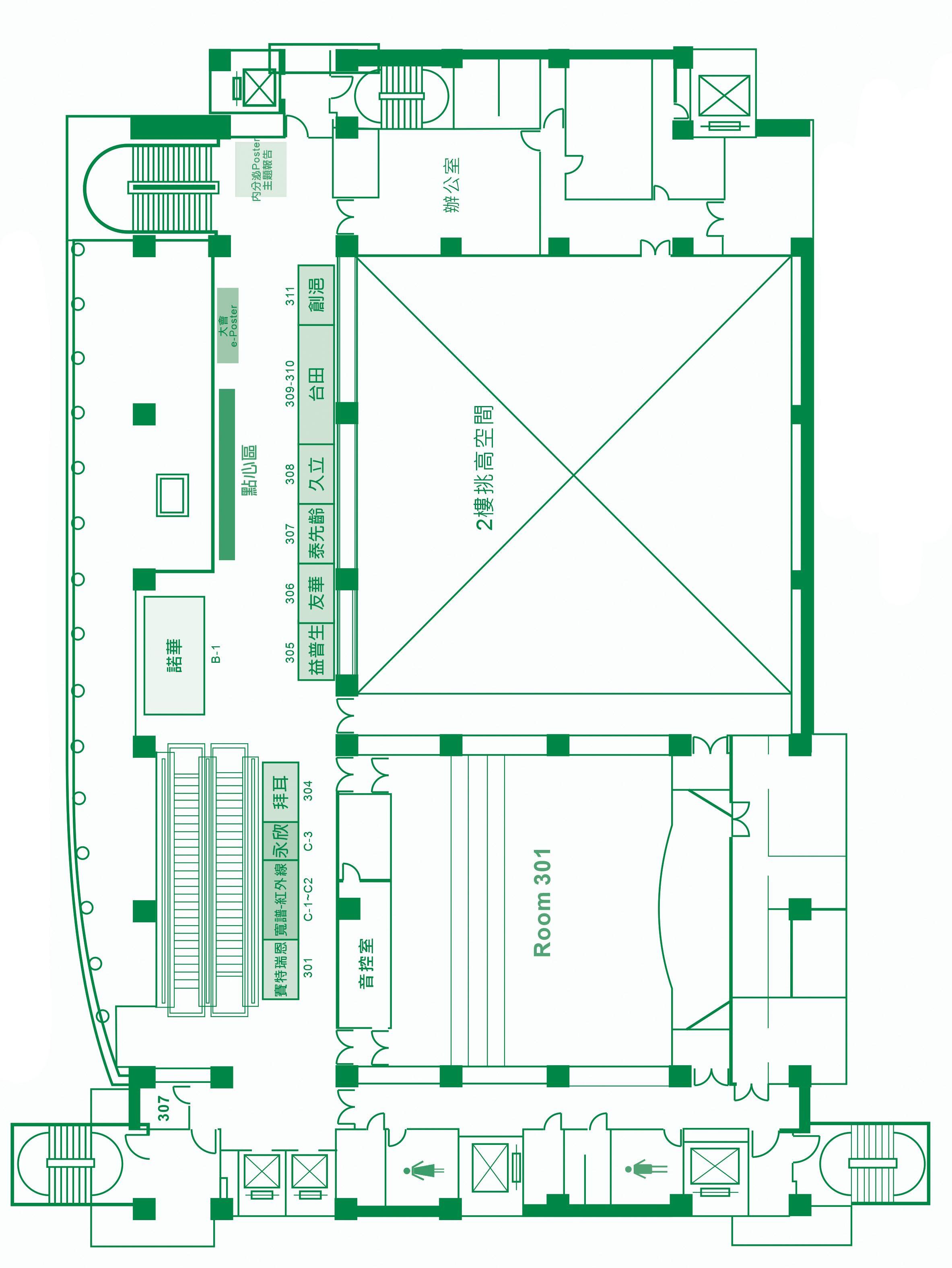
2024 臺大國際會議中心二樓平面圖
23-24,
Floor Plan of Conference Rooms
3
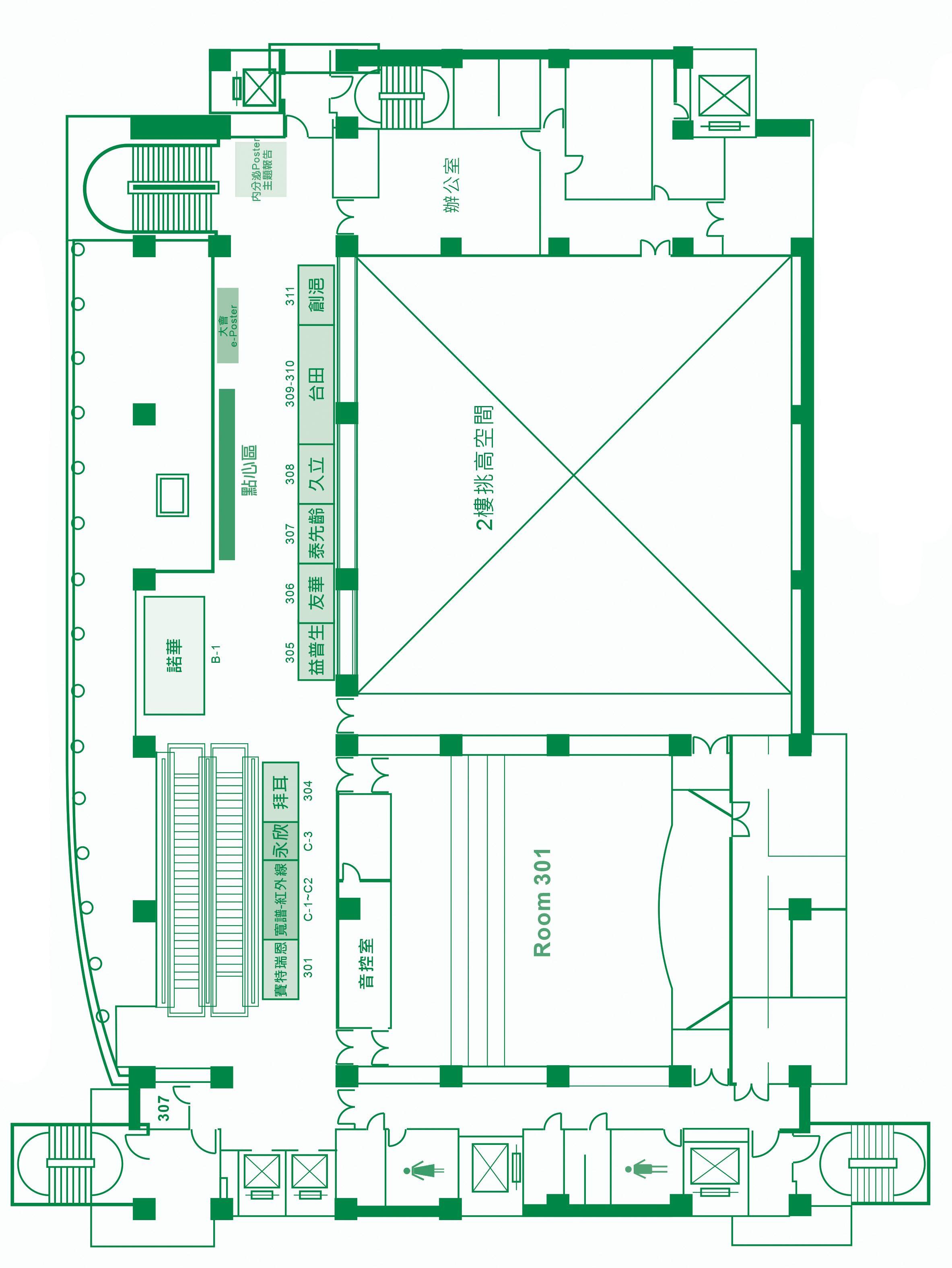
臺大國際會議中心三樓平面圖

4 Annual Meeting of the Endocrine Society and the Diabetes Association of the R.O.C. (Taiwan) The45 th March
2024 臺大國際會議中心四樓平面圖
23-24,
08:00-12:00
12:00-13:00
社團法人中華民國內分泌暨糖尿病學會 第 15 屆第 3 次會員大會暨學術研討會
日期:民國 113 年 3 月 23-24 日/地點:臺大醫院國際會議中心
節目表
March 23, 2024 (Saturday)
DAROC-TADE (Room 201)
DAROC-TADE Joint Symposium 主持人:歐弘毅、許惠恒、黃建寧、王治元、劉鳳炫、蔡世澤、陳榮福 演講者:吳昭軍、曾耀賢、沈峰志、簡國龍、劉秀珍、歐陽鍾美
13:10-13:20 Opening (Room 201)
13:20-14:05
14:05-14:50
PL1 Plenary Lecture-1 (Endocrine) (Room 201) Re-Defining Primary Aldosteronism 主持人:劉鳳炫 演講者:Anand Vaidya
PL2 Plenary Lecture-2 (DM) (Room 201) Expanding Incretin Universe: from Basic Biology to Clinical Translation 主持人:黃建寧 演講者:Daniel J. Drucker
14:50-15:20 Break (e-Poster -3&4F Walkway)
PE:陳瑜忻、李宇璇、林冠宇、黃峻偉 PD:沈宜靜、沈峰志、蘇聖強、曾耀賢
15:20-17:00
17:00-18:00
晚宴場佈
SD-1
Precision Medicine in Diabetes
糖尿病的精準 醫療
主持人:許惠恒 葉振聲
林慶齡 演講者: Jianfeng Xu 楊偉勛 王俊興
MTP-D
Driving Safety in People Living with Diabetes 糖尿病病人的 駕駛安全議題
主持人:陳榮福 朱志勳 王治元 演講者:沈宜靜 林時逸
SE-1
Precision Medicine in Obesity-from bench to clinic
肥胖精準醫療
主持人:簡銘男 盧介祥
許惠恒
演講者:謝博軒 張以承 吳忠擇
MTP-E1
Diagnosing and Treating Primary Aldosteronism
主持人:吳允升 演講者: Anand Vaidya
SE-2
Endocrine and New Technology
內分泌與科技 - 智慧醫療
主持人:王舒儀 陳沛隆
曾耀賢
演講者:陳維健 連加恩 鄧居義
MTP-E2
Evolving Concepts of Low-density Lipoprotein: from structure to function 主持人:葉森洲 演講者:陳珠璜
SD-2
Diabetes, Eye Complication 糖尿病併發症 : 眼睛
主持人:黃建寧 楊純宜
陳清助 演講者:王元聖 李美月 楊宜瑱
SE-3
Endocrine and Exercise 內分泌與運動
主持人:黃兆山 蔡克嵩 李亭儀 演講者:方姿蓉 韓德生 馬文雅
OE
Oral PresentationEndocrine
SD-3 Young Research Symposium
國科會跨領 域學門對談
主持人:李弘元 洪乙仁
歐弘毅 查岱龍 演講者:蔡文瑄 吳泓璁 林俊良
OD
Oral PresentationDiabetes
主持人:呂介華 陳思達 姜和均
18:00-21:00 Welcome Dinner (Room 201)
主持人:張恬君 陳清助 范綱志
5
Daily Program Schedule
Room 201 Room 301 Room 401 Room 402AB Room 402CD Room 202 Room 203 Room 205 Room 403 600 人 220 人 220 人 200 人 200 人 80 人 80 人 80 人 60 人
LS1 諾和 諾德 LS2 阿斯特 捷利康 LS3 諾華 LS4 拜耳 LS5 亞培 ( 糖尿病照護 ) LS6 台田 LS7 友華 LS8 羅氏 醫療
08:00-09:40
SD-4
Obesity
Management: from clinical trials to clinical practice 肥胖治療 主持人:楊偉勛
何橈通
胡啟民 演講者:廖國盟
沈峰志
杜思德
09:40-10:00
10:00-10:45
10:45-12:20
12:20-12:30
SE-4
ESROC and KES Joint Symposium 台灣與韓國內 分泌學會交流
主持人:劉鳳炫 Yoon-Sok Chung 演講者:林嘉鴻 Jeonghoon Ha 郭俸志 Man-Ho Choi
March 24, 2024 (Sunday)
SD-5
Advancements in Diabetes Tech 糖尿病照護新 科技運用的新 發展
主持人:黃建寧
朱志勳 莊立民 演講者:王治元
曾耀賢 Stephan Bakker
SD-6
Young-Onset
Type 2 Diabetes 年輕型的第二 型糖尿病
主持人:蔡世澤 葉振聲
演講者:
Elaine Chow 張恬君
SE-5
Image of Pituitary Gland -expert opinion 從腦下垂體影 像學談起
主持人:陳涵栩 張慶忠 郭萬祐 演講者:林慶齡
李丞騏 游鎧蔚
SE-6
Thyroid Cytology 甲狀腺細胞學
主持人:施翔蓉 郭錦松 周振凱 演講者:陳瑜忻 詹一秀 劉之怡
Break (e-Poster – 3/4 F Walkway)
PL3 Plenary Lecture-3 (Endocrine) (Room 201)
New Form of Hypophysitis: A Journey for the Discovery of Novel Diseases 主持人:王治元 演講者:Yutaka Takahashi
General Assembly 會員大會 (Room 201)
Group Picture 會員大合照
12:30-13:30 LS9 葛蘭素史克 LS10 諾和諾德
13:35-14:20
LS11 華廣 LS12 新穎 LS13 安進 LS14 禮來 百靈佳 LS15 裕利 LS16 禮來
PL4 Plenary Lecture-4 (DM) (Room 201)
The Double Jeopardy between Diabetes and Dementia 主持人:許惠恒 演講者:陳榮福
14:20-14:40 Break (Poster Stand -3 Floor Walkway)
14:40-16:20
SE-7 Neuroendocrine Tumor 神經內分泌瘤 主持人:曾芬郁
林宏達
張宏猷 演講者:蔡慧珍
林亮羽
施翔蓉
SD-7
Emerging Diabetes Therapy: bringing back the beta cell 以貝他細胞為 標靶的糖尿病 治療新趨勢 主持人:何橈通 林慶齡 李建興 演講者:林嘉鴻
沈家寧 莊峻鍠
SE-8
Early Career Forum
早期生涯規劃 講座
主持人:邱偉益
陳榮福
劉鳳炫
演講者:蔡克嵩
王佩文
陳沛隆
SE-9
How to Initiate Research-from clinic to bench 基礎研究的濫 觴
主持人:胡啟民
歐弘毅
演講者:陳珠璜
康宏佑
SD-8 Diabetes, Foot Complications
糖尿病足部併 發症
SD-9 Clinical Practice Guideline for Diabetes in Pregnancy 2023 孕期糖尿病 臨床照護指引
主持人:黃禹堯
張恬君
演講者:林詠翔
李建智
16:20-16:30 Closing
主持人:許志成 黃建霈 李淳權
演講者:李弘元
郭俊亨
陳思潔
6 Annual Meeting of the Endocrine Society and the Diabetes Association of the R.O.C. (Taiwan) The45 th March 23-24, 2024
Room 201Room 301Room 401 Room 402AB Room 402CD Room 202 Room 203 Room 205 Room 403 600 人 220 人 220 人 200 人 200 人 80 人 80 人 80 人 60 人
理事長致詞
中華民國內分泌暨糖尿病學會 113 年度年會,3 月 23 日至 24 日於台大醫院國際會 議中心舉行,內分泌學會邀請美國 Anand Vaidya 教授及日本 Yutaka Takahashi 教授蒞台 擔任 Plenary Lecture 的來賓,Vaidya 教授專精於腎上腺領域,他是哈佛醫學院的副教 授也是 Brigham and Women’s Hospital 的腎上腺疾病中心主任,他常常至各國演講原發
性醛酮症的診治,高橋 裕教授是日本神戶大學醫學博士,目前任職奈良國立醫科大學, 是糖尿病內分泌內科學講座教授,他要講述發現抗 PIT-1 下垂體炎的歷史。今年的幾場 內分泌論壇 Symposium 皆由秘書長、副秘書長與各委員會主委商討籌劃,計有 SE-1 肥 胖精準醫療、SE-2 內分泌與科技智慧醫療、SE-3 內分泌與運動、SE-4 韓國內分泌學會 聯合會議、SE-5 從腦下垂體影像學談起、SE-6 甲狀腺細胞學、SE-7 神經內分泌瘤、 SE-8 早期生涯規劃講座、SE-9 基礎研究的濫觴等九場節目,以及兩場與教授晤談,內 容多元又多彩,相信會是很豐盛的學術饗宴。同時糖尿病學會也呈現滿堂學術節目, 今年總計有 64 篇的會員論文投稿,安排成口頭論文報告與兩會首創的電子版壁報展示, 與藥界同仁安排的 Lunch Symposium 等也都是精彩萬分,相信所有與會的會員朋友們 都能夠在這場學術大會中找尋亮點而收穫滿滿。
在週日的會員大會上,我們也要頒發今年度的各項獎項,傑出研究獎由張以承教 授獲得,以及四位優秀論文獎得主,分別是周振凱醫師、林冠宇醫師、顏福順醫師、 吳至行醫師獲得,恭喜他們。
感謝今年負責場地佈置及節目規劃的秘書處,謹此感謝所有主持人及演講者、糖 尿病及內分泌學會兩會的秘書長、副秘書長、全體秘書、所有的贊助廠商,更謝謝所 有會員對學會的支持,有您們的熱心參予與持續鼓勵才是我們走下去的原動力,讓我 們一起同心協力,為台灣的內分泌暨新陳代謝醫療而努力。
謹祝 大家身體健康、萬事如意。 社團法人中華民國內分泌學會
7
理事長 2024
年 3 月 23 日
理事長致詞
各位會員平安:
於此春暖花開,龍年展現欣欣向榮之際,非常感謝大家在百忙之中能夠撥冗參與學 會的年度盛會。
近年來,台灣在慢性病照護方面展現了產官學三方面的通力合作,尤其在智慧照護 的發展上,目前也受到世界各國的矚目。政府各單位在許多場合均極力倡議,期待能利 用智慧照護來提升慢性病管理及其危險因數的預防與介入,希冀透過 IT 資源整合,提供
個人化預防保健資訊,並結合新科技智慧型載具的發展,讓民眾獲得更完整的照護服務。
在醫療端,我們也必須與時俱進,思考如何應用並連結各醫療院所的智慧醫療平臺,提 供醫療人員與病人的溝通管道,除了可獲得快速傳遞的訊息外,最重要的是,要能建立 完善的機制,兼顧醫療診治流程效率,從而提升整體照護品質。
學會成立了多個委員會及糖尿病各工作小組,定期開會討論國內外有關糖尿病的最 新科技、知識與研究報告,並定期修訂指引。今年,我們預計向所有會員發放「2023 孕 期糖尿病年鑑」及「2023 孕期糖尿病臨床照護指引」,除了瞭解台灣的照護現況外,也 整理了國內外有關孕期糖尿病的照護新知,提供會員參考與臨床應用,這也是學會持續 進步的動力。
今年的年會節目安排特別邀請了國內外優秀的講者。其中 Plenary Lecture 方面有 Prof. Daniel J. Drucker 主講「Expanding incretin universe: from basic biology to clinical translation」, 以及陳榮福教授主講「糖尿病及失智症的雙向影響」。另外,Meet professor 場次,邀請 了林時逸主任、沈宜靜醫師主講近年來國內外備受重視的「糖尿病病人的駕駛安全」等 相關議題。其他課程則包括糖尿病足部併發症、肥胖治療、視網膜病變、新科技運用的新 發展、孕期糖尿病臨床照護、年輕型第 2 型糖尿病、以β細胞為標靶的糖尿病治療新趨勢、 精準醫療、以及 Young research symposium 等。受邀的專家學者們在糖尿病領域上皆俱專研 成就,各議題的選定也都經由秘書處精心規畫,歡迎各位會員們前往聆聽交流學習。
最後,誠摯感謝所有理監事與會員們的共同努力參與,衷心祝福各位會員們身體健 康,事業順利!期待並預祝年會順利圓滿成功!
社團法人中華民國糖尿病學會
8 Annual Meeting of the Endocrine Society and the Diabetes Association of the R.O.C. (Taiwan) The45 th March
2024 Opening
23-24,
Remarks
理事長 2024 年
日
3 月 23
Board of Directors
(依照姓氏筆劃排序)
The Endocrine Society of the Republic of China (Taiwan)
President
Executive Director
Director
Executive Supervisor
Supervisor
Secretary General
Deputy Secretary General
劉鳳炫 Feng Hsuan Liu
王治元 Chih-Yuan Wang
蔡克嵩 Keh-Sung Tsai
王舒儀 Shu-Yi Wang
李亭儀 Annie Lee
施翔蓉 Shyang-Rong Shih
陳思達 Szu-Tah Chen
歐弘毅 Horng-Yih Ou
曾芬郁 Fen-Yu Tseng
林宏達 Hong-Da Lin
張宏猷 Hung-Yu Chang
陳維健 Wai-Kin Chan
李宇璇 Yu-Hsuan Li
姜和均 He-Jiun Jiang
黃峻偉 Jin-Wei Huang
陳涵栩 Harn-Shen Chen
簡銘男 Ming-Nan Chien
呂介華 Chieh-Hua Lu
周振凱 Chen-Kai Chou
陳沛隆 Pei-Lung Chen
黃兆山 Jawl-Shan Hwang
盧介祥 Chieh-Hsiang Lu
張慶忠 Ching-Chung Chang
郭錦松 Chin-Sung Kuo
林冠宇 Kuan-Yu Lin
陳思綺 Szu-Chi Chen
陳瑜忻 Yu-Hsin Chen
The Diabetes Association of the Republic of China (Taiwan)
President
Executive Director
Director
Executive Supervisor
Supervisor
Secretary General
Deputy Secretary General
黃建寧 Chien-Ning Huang
陳榮福 Jung-Fu Chen
杜思德 Shih Te Tu
李弘元 Hung-Yuan Li
曾慶孝 Chin-Hsiao Tseng
楊偉勛 Wei-Shiung Yang
洪乙仁 Yi-Jen Hung
林嘉鴻 Chia-Hung Lin
許惠恒 Wayne Huey-Herng Sheu
莊立民 Lee-Ming Chuang
何橈通 Low-Tone Ho
楊宜瑱 Yi-Sun Yang
沈宜靜 Yi - Jing Sheen
范綱志 Kang-Chih Fan
曾耀賢 Yao-Hsien Tseng
胡啟民 Chii-Min Hwu
蔡世澤 Shih-Tzer Tsai
陳清助 Ching-Chu Chen
林慶齡 Ching-Ling Lin
李建興 Chien-Hsing Lee
張恬君 Tien-Jyun Chang
朱志勳 Chih-Hsun Chu
楊純宜 Chun-Yi Yang
葉振聲 Tjin-Shing Jap
沈峰志 Feng-Chih Shen
蘇聖強 Sheng-Chiang Su
9
主持人、演講者列表 ( 外賓 )
外賓 單位
Anand Vaidya , MD, MMSc
Chu-Huang (Mendel) Chen, MD PhD
Director, Center for Adrenal Disorders, Brigham and Women's Hospital
Associate Professor of Medicine, Harvard Medical School Division of Endocrinology, Diabetes, and Hypertension Director, e-Learning Initiative, New England Journal of Medicine (NEJM)/ Department of Medicine, BWH
Director, Vascular and Medicinal Research, Molecular Cardiology, The Texas Heart Institute
Daniel J. Drucker, MD Senior Scientist, Lunenfeld-Tanenbaum Research Institute, Mt. Sinai Hospital Professor of Medicine, University of Toronto
Elaine Chow, BSc, MBChB, MRCP (UK), MSc Clinical Research, PhD
Jeonghoon Ha, MD, PhD
Clinical Associate Professor, Deputy Medical Director, Phase 1 Clinical Trial Centre, Department of Medicine and Therapeutics, Prince of Wales Hospital, The Chinese University of Hong Kong, Hong Kong SAR
Assistant Professor, Division of Endocrinology and Metabolism, Department of Internal Medicine, Seoul St. Mary's Hospital, College of Medicine, The Catholic University of Korea, Seoul, Republic of Korea
Jianfeng Xu, MD, DrPH Vice President and Director, Program for Personalized Cancer Care Endowed Chair of Cancer Genomic Research NorthShore University HealthSystem Research Professor, University of Chicago Pritzker School of Medicine
Man-Ho Choi, PhD Professor, Center for Advanced Biomolecular Recognition, Korea Institute of Science and Technology, Seoul, Korea
Stephan J.L. Bakker, M.D., Ph.D.
Yoon-Sok (Martin) Chung, MD, PhD
Professor of Internal Medicine, Department of Internal Medicine, University Medical Center Groningen, Groningen, The Netherlands Program Leader Groningen Research Institute for Organ Transplantation Head of the PREVEND epidemiological study laboratory
President, Board of Directors, Korean Endocrine Society
Professor, Department of Endocrinology and Metabolism, Ajou University School of Medicine, Suwon, Korea
Ajou Institute on Aging, Ajou University Medical Center
Yutaka Takahashi, MD, PhD Professor, Department of Diabetes and Endocrinology, Nara Medical University, Japan ( 依照 First name 字母順序 )
10 Annual Meeting of the Endocrine Society and the Diabetes Association of the R.O.C. (Taiwan) The45 th March 23-24, 2024
主持人、演講者列表 ( 國內 )
方姿蓉 高雄醫學大學附設中和紀念醫院內科部內分泌暨新陳代謝科
王子源 中國醫藥大學附設醫院內分泌新陳代謝科
王元聖 新光吳火獅紀念醫院眼科部
王佩文 高雄長庚醫院暨長庚大學醫學院
王治元 臺大醫院內科部代謝內分泌科
王俊興 臺中榮民總醫院內科部內分泌新陳代謝科
王舒儀 彰化基督教醫院內分泌新陳代謝科
朱志勳 高雄榮民總醫院內分泌暨新陳代謝科
何橈通 臺北榮民總醫院
吳允升 臺大醫院內科部
吳忠擇 臺北醫學大學衛生福利部雙和醫院新陳代謝科
吳泓璁 成大醫院內科部
呂介華 三軍總醫院內分泌及新陳代謝科
呂金盈 臺大醫院檢驗醫學部 / 臺大醫院內科部代謝內分泌科
李弘元 臺大醫院內科部代謝內分泌科
李丞騏 林口長庚醫院腦腫瘤神經外科
李宇璇 臺中榮民總醫院內分泌新陳代謝科
李亭儀 臺北市立萬芳醫院內分泌新陳代謝科
李建智 中國醫藥大學附設醫院
李建興 松山班廷建興診所
李美月 高雄醫學大學附設醫院
李淳權 馬偕醫院內分泌暨新陳代謝科
杜思德 彰化基督教醫院內分泌新陳代謝科
沈宜靜 臺中榮民總醫院新陳代謝科
沈家寧 中央研究院基因體研究中心
沈峰志 高雄長庚紀念醫院內分泌暨新陳代謝科
周振凱 高雄長庚紀念醫院內分泌暨新陳代謝科
林宏達 臺北榮民總醫院
林志弘 臺大醫院內科部代謝內分泌科
林亮羽 臺北榮民總醫院內分泌新陳代謝科
林俊良 嘉義長庚紀念醫院 內科教授
林冠宇 暖新診所
林時逸 臺中榮民總醫院內分泌暨新陳代謝科
林詠翔 嘉義長庚醫院內分泌新陳代謝科
林嘉鴻 林口長庚醫院內科部新陳代謝科 / 長庚大學醫學院
林慶齡 國泰綜合醫院內科
邱偉益 臺大醫院內科部代謝內分泌科
姜和均 義大大昌醫院新陳代謝科
施翔蓉 臺大醫學系內科 / 臺大醫院代謝內分泌科
查岱龍 國防醫學院暨三軍總醫院外科
洪乙仁 三軍總醫院內分泌新陳代謝科
胡啟民 臺北榮民總醫院內分泌新陳代謝科 / 陽明交通大學醫學系
范綱志 臺大醫院新竹臺大分院代謝內分泌科
馬文雅 新店耕莘醫院內分泌科
康宏佑 長庚大學臨床醫學研究所
張以承 臺大醫院代謝內分泌科主治醫師暨減重與代謝手術中心 / 臺大醫 學院基因體暨蛋白體醫學研究所 / 中研院生醫所
張宏猷 林口長庚紀念醫院內分泌暨新陳代謝科
張恬君 臺大醫院內科部代謝內分泌科
張慶忠 中國醫藥大學附設醫院內科部
莊立民 臺大醫院內科部代謝內分泌科
莊峻鍠 林口長庚醫院內分泌暨新陳代謝科
許志成 國衛院高齡醫學暨健康福祉研究中心 許惠恒 國家衛生研究院
連加恩 宏碁智醫 Acer Medical 董事長暨執行長
郭俊亨 輔仁大學附設醫院內分泌新陳代謝科
郭俸志 三軍總醫院內分泌暨新陳代謝科暨代謝症候群防治中心 郭萬祐 臺北榮民總醫院放射線部 / 陽明交通大學醫學院
郭錦松 臺北榮民總醫院內分泌暨新陳代謝科
郭耀仁 高雄市立大同醫院
陳沛隆 臺大醫院內科部新陳代謝科暨基因醫學部 / 臺灣大學基因體暨蛋 白體醫學研究所
陳思達 土城醫院內分泌暨新陳代謝科
陳思潔 好心肝門診中心新陳代謝內分泌科
陳涵栩 臺北榮民總醫院新陳代謝科 / 國立陽明交通大學內科教授
陳清助 中國醫藥大學附設醫院內分泌新陳代謝科
陳瑜忻 國泰醫院內分泌新陳代謝科
陳榮福 高雄長庚紀念醫院內分泌暨新陳代謝科
陳維健 林口長庚醫院內分泌暨新陳代謝科
曾芬郁 臺大醫院新竹臺大分院代謝內分泌科
曾耀賢 童綜合醫院新陳代謝科
游鎧蔚 臺北榮民總醫院放射線部
黃兆山 林口長庚紀念醫院內分泌暨新陳代謝科 黃建寧 中山醫學大學
黃建霈 馬偕紀念醫院婦產部
黃禹堯 林口長庚醫院內分泌暨新陳代謝科
黃峻偉 禾馨醫療
楊宜瑱 中山醫學大學附設醫院內分泌暨新陳代謝科
楊純宜 奇美醫院內分泌新陳代謝科
楊偉勛 臺大醫學院臨床醫學研究所 / 臺大醫院醫學研究部 / 臺大醫院內 科部代謝內分泌科
葉振聲 為恭紀念醫院新陳代謝科
葉森洲 林口長庚醫院
詹一秀 臺大醫院檢驗醫學部
廖國盟 臺北市立聯合醫院忠孝院區內分泌新陳代謝科
劉之怡 汐止國泰綜合醫院病理科
劉秀珍 臺中榮總糖尿病健康促進機構
劉鳳炫 林口長庚紀念醫院內分泌暨新陳代謝科
歐弘毅 成大醫院內分泌暨新陳代謝科 / 成功大學醫學院
歐陽鍾美 臺大醫院新竹台大分院營養室
蔡文瑄 臺北馬偕醫院
蔡世澤 振興醫院營養治療科暨新陳代謝科
蔡克嵩 臺大醫院內科部及遠東診所
蔡尚峰 臺中榮民總醫院腎臟科
蔡慧珍 國家衛生研究院癌症研究所
鄧居義 智抗糖慧康生活執行長
鄭畬方 彰化基督教醫院內分泌新陳代謝科
盧介祥 高雄基督教醫院
蕭璧容 義大大昌醫院新陳代謝科
謝博軒 國防醫學院醫學科學研究所
韓德生 臺大醫學院臨床教授 / 臺大醫院北護分院醫療部
簡國龍 臺大公共衛生學院流行病學與預防醫學研究所
簡銘男 臺北馬偕紀念醫院內分泌新陳代謝科
蘇聖強 三軍總醫院內分泌暨新陳代謝科
( 依照姓氏筆畫順序 )
11 Moderator & Speaker
The Endocrine Society and the Diabetes Association of the R.O.C (Taiwan) Would Like to Recongnize the Following for Their Support of the 45th Annual Meeting
(依照贊助項目和中文筆畫排序)
臺灣阿斯特捷利康股份有限公司 ( 白金級 )
台灣諾和諾德藥品股份有限公司 ( 金級 )
台灣諾華股份有限公司 ( 金級 )
美商亞培股份有限公司台灣分公司 ( 金級 )
台灣禮來股份有限公司 ( 銀級 )
荷商葛蘭素史克藥廠股份有限公司台灣分公司 ( 銀級 )
新穎生醫股份有限公司 ( 銀級 )
台灣田邊製藥股份有限公司 ( 銅級 )
ASTRAZENECA TAIWAN LIMITED
NOVO NORDISK PHARMA (TAIWAN) LTD.
NOVARTIS (TAIWAN) CO., LTD.
ABBOTT LABORATORIES SERVICES LLC TAIWAN BRANCH (U.S.A.)
ELI LILLY AND COMPANY TAIWAN
HOLLAND GLAXOSMITHKLINE PHARMACEUTICAL CO., LTD. TAIWAN BRANCH
BIO PREVENTIVE MEDICINE CORP.
TAIWAN TANABE SEIYAKU CO., LTD.
力大圖書有限公司 THE LEADER BOOK COMPANY LTD.
久立藥品有限公司 GOLEAD BIOPHARM INC.
友霖生技醫藥股份有限公司
台灣安進藥品有限公司
台灣百靈佳殷格翰股份有限公司
台灣拜耳股份有限公司
台灣賽特瑞恩有限公司
台灣羅氏醫療診斷設備股份有限公司
永欣儀器有限公司
法商益普生股份有限公司台灣分公司
科懋生物科技股份有限公司
泰先齡有限公司
創浥有限公司
華廣生技股份有限公司
暉致醫藥股分有限公司
ORIENT PHARMA CO., LTD.
AMEGAN TAIWAN LIMITED
BOEHRINGER INGELHEIM TAIWAN LTD.
BAYER TAIWAN COMPANY LTD.
CELLTRION HEALTHCARE TAIWAN LTD.
ROCHE DIAGNOSTICS LTD., TAIWAN
EVERLIGHT INSTRUMENT CO., LTD.
IPSEN PHARMA TAIWAN BRANCH
EXCELSIOR BIOPHARMA INC.
TAI SCHERING CO., LTD.
TRONMED CO., LTD.
BIONIME CORPORATION
VIATRIS PHARMACEUTICAL COMPANY LIMITED
裕利股份有限公司 ZUELLIG PHARMA TAIWAN
寬譜醫學科技股份有限公司
衛采製藥股份有限公司
賽諾菲股份有限公司
醫影股份有限公司
WS FAR IR MEDICAL TECHNOLOGY CO., LTD.)
EISAI TAIWAN INC.
SANOFI TAIWAN CO.,LTD
MEDICAL IMAGING CORP.
12 Annual Meeting of the Endocrine Society and the Diabetes Association of the R.O.C. (Taiwan) The45 th March 23-24, 2024 Sponsors
社團法人中華民國內分泌暨糖尿病學會 第 15 屆第 3 次會員大會暨學術研討會
日期:民國 113 年 3 月 23-24 日/地點:臺大醫院國際會議中心
March 23, 2024
【Room 201】
Time
PL1: Plenary Lecture 1 (Endocrine)
13:20-13:25 OPENING Feng-Hsuan Liu ( 劉鳳炫 )
PL-1 13:25-14:05 RE-DEFINING PRIMARY ALDOSTERONISM
March 23, 2024
【Room 201】
Time
Anand Vaidya Feng-Hsuan Liu ( 劉鳳炫 )
PL2: Plenary Lecture 2 (Diabetes)
14:05-14:10 OPENING
PL-2 14:10-14:50 EXPANDING INCRETIN UNIVERSE: FROM BASIC BIOLOGY TO CLINICAL TRANSLATION ( 預錄 )
March 24, 2024
【Room 201】
Time
Chien-Ning
Huang ( 黃建寧 )
Daniel J. Drucker Chien-Ning Huang ( 黃建寧 )
PL3: Plenary Lecture 3 (Endocrine)
10:00-10:05 OPENING
PL-3 10:05-10:45 NOVEL FORM OF HYPOPHYSITIS: A JOURNEY FOR THE DISCOVERY OF NOVEL DISEASES
Chih-Yuan Wang ( 王治元 )
Yutaka Takahashi Chih-Yuan Wang ( 王治元 )
Agenda 13
Topic Speaker Moderator
Topic Speaker Moderator
Topic Speaker Moderator
March 24, 2024
【Room 201】
Time
PL4: Plenary Lecture 4 (Diabetes)
13:35-13:40 OPENING
PL-4
13:40-14:20 THE DOUBLE JEOPARDY BETWEEN DIABETES AND DEMENTIA
March 23, 2024
【Room 201】
TADE-1
Jung-Fu Chen ( 陳榮福 )
Moderator
Wayne Huey-Herng Sheu ( 許惠恒 )
Wayne Huey-Herng Sheu ( 許惠恒 )
DAROC-TADE: Joint Symposium
08:20-08:30 OPENING REMARKS
08:30-09:00 代謝症候群國內防治政策與實施 現況
TADE-2 09:00-09:30 QUASI-EXPERIMENTAL EVALUATION OF A NATIONWIDE DIABETES PREVENTION PROGRAMME
TADE-3 09:30-10:00 IMPACT OF LIFESTYLE CHANGES ON METABOLIC SYNDROME: IMPLICATIONS FROM THE PERSPECTIVE OF THE DIABETES PREVENTION PROGRAM (DPP)
TADE-4 10:00-10:40 EFFECT OF LIFESTYLE CHANGE ON THE RISK OF METABOLIC SYNDROME AND DIABETES: VIEWPOINT FROM TAIWAN HEALTH DATA
10:40-10:50 BREAK
Chao-Chun Wu ( 吳昭軍 )
Yao-Hsien Tseng ( 曾耀賢 )
Feng-Chih Shen ( 沈峰志 )
Moderator
Horng-Yih Ou ( 歐弘毅 )
Horng-Yih Ou ( 歐弘毅 )
Wayne HueyHerng Sheu ( 許惠恒 )
Chien-Ning Huang ( 黃建寧 )
Kuo-Liong Chien ( 簡國龍 )
Chih-Yuan Wang ( 王治元 )
14 Annual Meeting of the Endocrine Society and the Diabetes Association of the R.O.C. (Taiwan) The45 th March 23-24, 2024
Topic Speaker
Topic Speaker
Time
TADE-5 10:50-11:15 A NURSE’S PERSPECTIVE ON THE IMPACT OF LIFESTYLE CHANGES ON METABOLIC SYNDROME
TADE-6 11:15-11:40 EFFECT OF LIFESTYLE CHANGES ON METABOLIC SYNDROME FROM DIETITIAN’S POINT OF VIEW
11:40-12:00 PANEL DISCUSSION
12:00-12:05 CLOSING REMARKS
March 23, 2024
Sheu-Chen Liu ( 劉秀珍 )
Chung-Mei Ouyang ( 歐陽鐘美 )
Feng-Hsuan Liu ( 劉鳳炫 )
Shih-Tzer Tsai ( 蔡世澤 )
Jung-Fu Chen ( 陳榮福 )
Jung-Fu Chen ( 陳榮福 )
【Room 401】 MTP-E1: Meet the Professor - Endocrine 1
MTP-E1 17:00-18:00 DIAGNOSING AND TREATING PRIMARY ALDOSTERONISM
March 23, 2024
【Room 402AB】
Anand Vaidya Vin-Cent Wu ( 吳允升 )
MTP-E2: Meet the Professor - Endocrine 2
MTP-E2 17:00-18:00 EVOLVING CONCEPTS OF LOWDENSITY LIPOPROTEIN: FROM STRUCTURE TO FUNCTION
Chu-Huang (Mendel) Chen ( 陳珠璜 )
San-Jou Yeh ( 葉森洲 )
March 23, 2024
【Room 301】
MTP-D: Meet the Professor - Diabetes Driving Safety in People Living with Diabetes 糖尿病病人的駕駛安全議題
MTP-D 17:00-17:05 OPENING
Jung-Fu Chen ( 陳榮福 )
Agenda 15
Time Topic Speaker Moderator
Time Topic Speaker Moderator
Time Topic Speaker Moderator
17:05-17:30 DRIVING SAFETY IN PEOPLE LIVING WITH DIABETES
17:30-17:55 DRIVING SAFETY IN OLDER PATIENTS WITH DIABETES
17:55-18:00 PANEL DISCUSSION
March 23, 2024
【Room 401】
Time
Yi-Jing Sheen ( 沈宜靜 )
Shih-Yi Lin ( 林時逸 )
Chih-Hsun Chu ( 朱志勳 )
Chih-Yuan Wang ( 王治元 )
Jung-Fu Chen ( 陳榮福 )
SE1: Symposium-Endocrine 1 Precision Medicine in Obesity-from bench to clinic
15:20-15:25 OPENING REMARK
SE1-1 15:25-15:55 THE INVOLVEMENT OF DIETINDUCED THERMOGENESIS IN OBESITY DEVELOPMENT- THE ROLE OF BROWN ADIPOSE TISSUE
SE1-2 15:55-16:25 PRECLINICAL DEVELOPMENT FOR OBESITY
SE1-3 16:25-16:55 CROSSTALK BETWEEN ADIPOSE TISSUE, MUSCLE, AND APOPTOSIS OF β CELLS IN OBESITY AND TYPE 2 DIABETES
Po-Shiuan Hsieh ( 謝博軒 )
Yi-Cheng Chang ( 張以承 )
Chung-Ze Wu ( 吳忠擇 )
16:55-17:00 PANEL DISCUSSION All
March 23, 2024
【Room 402AB】
Time
Ming-Nan Chien ( 簡銘男 )
Chieh-Hsiang Lu ( 盧介祥 )
Wayne HueyHerng Sheu ( 許惠恒 )
SE2: Symposium-Endocrine 2 Endocrine and New Technology
15:20-15:25 OPENING REMARK
16 Annual Meeting of the Endocrine Society and the Diabetes Association of the R.O.C. (Taiwan) The45 th March 23-24, 2024
肥胖精準醫療
Topic Speaker Moderator
內分泌與科技 - 智慧醫療
Topic Speaker Moderator
SE2-1 15:25-15:55 ENDOCRINOLOGISTS´ EXPERIENCES IN RESEARCHING AND DEVELOPING ARTIFICIAL INTELLIGENCE FOR THYROID ULTRASOUND IMAGING
Wai-Kin Chan ( 陳維健 )
SE2-2 15:55-16:25 ACER MEDICAL: FROM INNOVATION TO IMPLEMENTATION Allen (Chia En) Lien ( 連加恩 )
SE2-3 16:25-16:55 HEALTH2SYNC AND ITS VISION OF THE FUTURE IN DIGITAL DIABETES CARE
16:55-17:00 PANEL DISCUSSION
March 23, 2024 【Room 202】
Chu-Yie Deng ( 鄧居義 )
Shu-Yi Wang ( 王舒儀 )
Pei-Lung Chen ( 陳沛隆 )
Yao-Hsien Tseng ( 曾耀賢 )
All
SE3: Endocrine Symposium 3
15:20-15:25 OPENING REMARK
SE3-1 15:25-15:55 THE IMPACT OF EXERCISE ON THE ENDOCRINE SYSTEM
SE3-2 15:55-16:25 EFFECT OF PHYSICAL ACTIVITY ON MUSCULOSKELETAL SYSTEM
SE3-3 16:25-16:55 ENDOCRINE ADAPTATION IN ATHLETES AND RELATIVE ENERGY DEFICIENCY SYNDROME (RED-S)
16:55-17:00 PANEL DISCUSSION
Tzu-Jung Fang ( 方姿蓉 )
Der-Sheng Han ( 韓德生 )
Wen Ya Ma ( 馬文雅 )
All
Jawl-Shan Hwang ( 黃兆山 )
Keh-Sung Tsai ( 蔡克嵩 )
Annie Lee ( 李亭儀 )
Agenda 17
Topic Speaker Moderator
Endocrine and Exercise 內分泌與運動 Time
March 24, 2024
【Room 301】
Time
SE4: Symposium-Endocrine 4 ESROC and KES Joint Symposium
08:00-08:05 OPENING REMARK
SE4-1 08:05-08:30 THE PREDICTION OF INCRETIN EFFECT THROUGH THE DIFFERENTIALLY METHYLATED REGION (DMR) IN GENOMIC DNA
SE4-2 08:30-08:55 EFFECTS OF ANTIDIABETIC MEDICATION ON BONE HEALTH IN TYPE 2 DIABETES
SE4-3 08:55-09:20 CONNECT THE EXPLORATION OF REGIONAL ADIPOCYTE BIOLOGY TO CLINICAL SIGNIFICANCE -MY POINT OF VIEW AS AN ENDOCRINOLOGIST AND PHYSICIAN SCIENTIST
SE4-4 09:20-09:45 EXPLORING STEROIDOGENESIS FOR CHARACTERIZATION OF ADRENAL DISORDERS
Chia-Hung Lin ( 林嘉鴻 ) (ESROC)
Feng-Hsuan Liu ( 劉鳳炫 ) (ESROC)
Jeonghoon Ha (KES) Yoon-Sok Chung (KES)
Feng-Chih Kuo ( 郭俸志 ) (ESROC)
Feng-Hsuan Liu ( 劉鳳炫 ) (ESROC)
Man-Ho Choi (KES) Yoon-Sok Chung (KES)
09:45-09:50 PANEL DISCUSSION All
March 24, 2024
【Room 402CD】
SE5: Symposium-Endocrine 5 Image of Pituitary Gland-expert opinion
Time Topic
08:00-08:05 OPENING REMARK
18 Annual Meeting of the Endocrine Society and the Diabetes Association of the R.O.C. (Taiwan) The45 th March 23-24, 2024
台灣與韓國內分泌學會交流
Topic Speaker Moderator
從腦下垂體影像學談起
Speaker
Moderator
SE5-1 08:05-08:35 DEAL WITH PITUITARY DISORDER
SE5-2 08:35-09:05 INTERACTION BETWEEN PITUITARY TUMOR IMAGING AND NEUROSURGEON
SE5-3 09:05-09:35 CURRENT APPLICATION OF ARTIFICIAL INTELLIGENCE IN PITUITARY GLAND AND ITS FUTURE: EXPERIENCE OF TAIPEI VETERANS GENERAL HOSPITAL
09:35-09:40 PANEL DISCUSSION
March 24, 2024 【Room 202】
Ching-Ling Lin ( 林慶齡 )
Cheng-Chi Lee ( 李丞騏 )
Kai-Wei Yu ( 游鎧蔚 )
All
Harn-Shen Chen ( 陳涵栩 )
Ching-Chung Chang ( 張慶忠 )
Wan Yuo Guo ( 郭萬祐 )
SE6: Symposium-Endocrine 6 Thyroid Cytology 甲狀腺細胞學 Time
08:00-08:05 OPENING REMARK
SE6-1 08:05-08:35 BENIGN NON THYROID CYTOMORPHOLOGY NOTED IN THYROID ASPIRATION
SE6-2 08:35-09:05 CYTOMORPHOLOGY FOR METASTATIC TUMORS OF THE THYROID
SE6-3 09:05-09:35 THE 2023 BETHESDA SYSTEM FOR REPORTING THYROID CYTOPATHOLOGY
09:35-09:40 PANEL DISCUSSION
Yu-Hsin Chen ( 陳瑜忻 )
I-Shiow Jan ( 詹一秀 )
Chih-Yi Liu ( 劉之怡 )
Shyang-Rong Shih ( 施翔蓉 )
Chin-Sung Kuo ( 郭錦松 )
Chen-Kai Chou ( 周振凱 )
All
Agenda 19
Topic Speaker Moderator
March 24, 2024
【Room 201】
SE7: Symposium-Endocrine 7 Neuroendocrine Tumor
神經內分泌瘤
Time Topic Speaker Moderator
14:40-14:45 OPENING REMARK
SE7-1 14:45-15:15 ADVANCES IN SYSTEMIC TREATMENT OF NEUROENDOCRINE TUMORS
SE7-2 15:15-15:45 UPDATE OF FUNCTIONING PANCREATIC NEUROENDOCRINE TUMOR
Hui-Jen Tsai ( 蔡慧珍 )
Liang-Yu Lin ( 林亮羽 )
SE7-3 15:45-16:15 CLINICAL SIGNIFICANCE OF MEN1 GENE Shyang-Rong Shih ( 施翔蓉 )
16:15-16:20 PANEL DISCUSSION All
March 24, 2024
【Room 401】
Fen-Yu Tseng ( 曾芬郁 )
Hong-Da Lin ( 林宏達 )
Hung-Yu Chang ( 張宏猷 )
SE8: Symposium-Endocrine 8 Early Career Forum
14:40-14:45 OPENING REMARK
SE8-1 14:45-15:15 OSTEOPOROSIS IS AN IMPORTANT ENDOCRINE DISORDER FOR ENDOCRINOLOGISTS
SE8-2 15:15-15:45 CHALLENGES FACED BY EARLY CAREER RESEARCHERS
Keh-Sung Tsai ( 蔡克嵩 ) Wei-Yih Chiu ( 邱偉益 )
Pei-Wen Wang ( 王佩文 )
Jung-Fu Chen ( 陳榮福 )
20 Annual Meeting of the Endocrine Society and the Diabetes Association of the R.O.C. (Taiwan) The45 th March 23-24, 2024
早期生涯規劃講座
Topic Speaker
Time
Moderator
SE8-3 15:45-16:15 CHOOSE WHAT YOU LOVE, AND LOVE WHAT YOU CHOOSE
Pei-Lung Chen ( 陳沛隆 )
16:15-16:20 PANEL DISCUSSION All
March 24, 2024
【Room 402AB】
Time
Feng-Hsuan Liu ( 劉鳳炫 )
SE9: Symposium-Endocrine 9
How to Initiate Research -from clinic to bench 基礎研究的濫觴
14:40-14:45 OPENING REMARK
SE9-1 14:45-15:25 ROLES OF ELECTRONEGATIVE LIPOPROTEINS IN CARDIOVASCULAR DISEASES: FROM CLINIC TO BENCH
SE9-2 15:25-16:05 NAVIGATING ANDROGENRELATED DISEASES: UNRAVELING ANDROGEN RECEPTOR MECHANISMS FROM BEDSIDE TO BENCH AND BACK AGAIN
Chu-Huang (Mendel) Chen ( 陳珠璜 )
Chii-Min Hwu ( 胡啟民 )
Hong-Yo Kang ( 康宏佑 ) Horng-Yih Ou ( 歐弘毅 )
16:05-16:20 PANEL DISCUSSION All
March 23, 2024
【Room 301】
SD1: Symposium-Diabetes 1
Precision Medicine in Diabetes 糖尿病的精準醫療
Time Topic Speaker Moderator
15:20-15:25 OPENING REMARK Wayne
Huey-Herng Sheu ( 許惠恒 )
Agenda 21
Topic Speaker Moderator
SD1-1 15:25-15:55 USING POLYGENIC RISK SCORES TO DIFFERENTIATE T1D AND T2D IN PATIENTS WITH ATYPICAL PHENOTYPES OF DIABETES( 預錄 )
Jianfeng Xu Wayne
Huey-Herng Sheu ( 許惠恒 )
SD1-2 15:55-16:25 PRECISION MEDICINE IN T2D Wei-Shiung Yang ( 楊偉勛 )
SD1-3 16:25-16:55 GAPS AND OPPORTUNITIES FOR THE CLINICAL TRANSLATION OF PRECISION DIABETES MEDICINE
Jun-Sing Wang ( 王俊興 )
Tjin-Shing Jap ( 葉振聲 )
Ching-Ling Lin ( 林慶齡 )
16:55-17:00 PANEL DISCUSSION All Ching-Ling Lin ( 林慶齡 )
March 23, 2024 【Room 402CD】
Time
SD2: Symposium-Diabetes 2
Diabetes, Eye Complication
Topic
15:20-15:25 OPENING
SD2-1 15:25-15:55 DIABETIC RETINOPATHY AND DIABETIC MACULAR EDEMA: THE OPHTHALMOLOGIST POINT OF VIEW
SD2-2 15:55-16:25 DIABETES RETINOPATHY AND DME: THE DIABETOLOGIST POINT OF VIEW
Speaker
Yuan-Shen Wang ( 王元聖 )
Mei-Yueh Lee ( 李美月 )
Moderator
Chien-Ning Huang ( 黃建寧 )
Chien-Ning Huang ( 黃建寧 )
Chun-Yi Yang ( 楊純宜 )
22 Annual Meeting of the Endocrine Society and the Diabetes Association of the R.O.C. (Taiwan) The45 th March 23-24, 2024
糖尿病併發症:眼睛
SD2-3 16:25-16:55 WORSENING OF DIABETES RETINOPATHY WITH RAPID IMPROVEMENT IN SYSTEMIC GLUCOSE CONTROL
Yi-Sun Yang ( 楊宜瑱 )
Ching-Chu Chen ( 陳清助 )
16:55-17:00 PANEL DISCUSSION All Ching-Chu Chen ( 陳清助 )
March 23, 2024 【Room 203】
SD3: Symposium-Diabetes 3
Young Research Symposium
15:20-15:25 OPENING
SD3-1 15:25-15:55 ANTIOSTEOPOROSIS MEDICATIONS AND CARDIOVASCULAR DISEASE: A POPULATION-BASED NATIONWIDE NESTED CASE–CONTROL STUDY
SD3-2 15:55-16:25 CROSS-TALK BETWEEN ADIPOSE TISSUE AND LIVER
SD3-3 16:25-16:55 ORCHESTRATING EPIGENETIC-BASED PRECISION MEDICINE FOR DIABETIC KIDNEY DISEASE: NEW PROSPECTIVE FROM CHIAYI
16:55-17:00 PANEL DISCUSSION
Wen-Hsuan Tsai ( 蔡文瑄 )
Hung-Yuan Li ( 李弘元 )
Yi-Jen Hung ( 洪乙仁 )
Hung-Tsung Wu ( 吳泓璁 )
Chun-Liang Lin ( 林俊良 )
Horng-Yih Ou ( 歐弘毅 )
Tai-Lung Cha ( 查岱龍 )
All Hung-Yuan Li ( 李弘元 )
Agenda 23
國科會跨領域學門對談 Time Topic Speaker Moderator
March 24, 2024
【Room 201】
SD4: Symposium-Diabetes 4
Obesity Management: from clinical trials to clinical practice 肥胖治療
Time Topic Speaker Moderator
08:00-08:05 OPENING
SD4-1 08:05-08:35 CRITICAL APPRAISAL OF CLINICAL STUDIES: AN OVERVIEW OF RECENT OBESITY TRIALS DESIGNS
SD4-2 08:35-09:05 MEDICATIONS TO TREAT OBESITY: WHAT ARE THE EFFICACY AND SAFETY RESULTS OF RECENT OBESITY TRIALS
SD4-3 09:05-09:35 MEDICATIONS TO TREAT OBESITY: CLINICAL PRACTICE AND LOOK FORWARD TO THE FUTURE
09:35-09:40 PANEL DISCUSSION
March 24, 2024
【Room 401】
Time
Wei-Shiung Yang ( 楊偉勛 )
Kuo-Meng Liao ( 廖國盟 ) Wei-Shiung Yang ( 楊偉勛 )
Feng-Chih Shen ( 沈峰志 )
Low-Tone Ho ( 何橈通 )
Shih-Te Tu ( 杜思德 ) Chii-Min Hwu ( 胡啟民 )
All Chii-Min Hwu ( 胡啟民 )
SD5: Symposium-Diabetes 5
Advancements in Diabetes Tech
08:00-08:05 OPENING REMARK
Chien-Ning Huang ( 黃建寧 )
24 Annual Meeting of the Endocrine Society and the Diabetes Association of the R.O.C. (Taiwan) The45 th March 23-24, 2024
糖尿病照護新科技運用的新發展
Topic
Speaker Moderator
SD5-1 08:05-08:35 AI-AIDS FOR INSULIN DOSING IN TYPE 2 DIABETES
SD5-2 08:35-09:05 APPLICATIONS OF CHATGPT IN DIABETES CARE: POTENTIAL, CHALLENGES, AND PROSPECTS
SD5-3 09:05-09:35 NOVEL BIOMARKERS IN DIABETES AND ASSOCIATED COMPLICATIONS
Chih-Yuan Wang ( 王治元 )
Yao-Hsien Tseng ( 曾耀賢 )
Chien-Ning Huang ( 黃建寧 )
Chih-Hsun Chu ( 朱志勳 )
Stephan Bakker Lee-Ming Chuang ( 莊立民 )
09:35-09:40 PANEL DISCUSSION All Lee-Ming Chuang ( 莊立民 )
March 24, 2024 【Room 402AB】
SD6: Symposium-Diabetes 6
Young-Onset Type 2 Diabetes
08:00-08:05 OPENING
SD6-1 08:05-08:40 OVERCOMING CHALLENGES IN EARLY DETECTION AND INTERVENTION IN YOUNGONSET TYPE 2 DIABETES( 預錄 )
08:40-08:50 Q/A(Live)
SD6-2 08:50-09:20 LATEST GLUCOSE MONITORING AND GLUCOSE LOWERING AGENTS FOR CHILDREN AND ADOLESCENTS WITH TYPE 2 DIABETES
09:20-09:30 Q/A AND CLOSING
Shih-Tzer Tsai ( 蔡世澤 )
Elaine Chow Shih-Tzer Tsai ( 蔡世澤 )
Tien-Jyun Chang ( 張恬君 )
Tjin-Shing Jap ( 葉振聲 )
Tjin-Shing Jap ( 葉振聲 )
Agenda 25
Time Topic Speaker Moderator
年輕型的第二型糖尿病
March 24, 2024
【Room 301】
Time
SD7: Symposium-Diabetes 7
Emerging Diabetes Therapy: bringing back the beta cell 以貝他細胞為標靶的糖尿病治療新趨勢
Topic Speaker Moderator
14:40-14:55 OPENING Low-Tone Ho ( 何橈通 )
SD7-1 14:55-15:20 IMMUNE THERAPY IN TYPE 1 DIABETES
SD7-2 15:20-15:50 REVERSING PANCREATIC BETA CELL DEDIFFERENTIATION IN THE TREATMENT OF TYPE 2 DIABETES
SD7-3 15:50-16:15 BETA CELL REPLACEMENT THERAPY FOR DIABETES
16:15-16:20 PANEL DISCUSSION
March 24, 2024
【Room 402CD】
Chia-Hung Lin ( 林嘉鴻 ) Low-Tone Ho ( 何橈通 )
Chia-Ning Shen ( 沈家寧 )
Jyuhn-Huarng Juang ( 莊峻鍠 )
Ching-Ling Lin ( 林慶齡 )
Chien-Hsing Lee ( 李建興 )
Chien-Hsing Lee ( 李建興 )
SD8: Symposium-Diabetes 8
Diabetes, Foot Complications 糖尿病足部併發症
Time Topic Speaker Moderator
14:40-14:45 OPENING
SD8-1 14:45-15:30 DIABETES-RELATED FOOT DISEASE – GUIDELINE AND CONSENSUS UPDATE
Yung-Hsiang Lin ( 林詠翔 )
Yu-Yao Huang ( 黃禹堯 )
Yu-Yao Huang ( 黃禹堯 )
26 Annual Meeting of the Endocrine Society and the Diabetes Association of the R.O.C. (Taiwan) The45 th March 23-24, 2024
SD8-2 15:30-16:15 WOUND CARE IN DIABETIC FOOT
Jian-Jr Lee ( 李建智 )
Tien-Jyun Chang ( 張恬君 )
16:15-16:20 PANEL DISCUSSION All Tien-Jyun Chang ( 張恬君 )
March 24, 2024
【Room 202】
SD9: Symposium-Diabetes 9
Clinical Practice Guideline for Diabetes in Pregnancy 2023 孕期糖尿病臨床照護指引 Time
14:40-14:45 OPENING
SD9-1 14:45-15:15 EPIDEMIOLOGY OF DIABETES IN PREGNANCY IN TAIWAN
SD9-2 15:15-15:45 DAROC CLINICAL PRACTICE GUIDELINE FOR DIABETES IN PREGNANCY – PRECONCEPTION AND PERINATAL CARE FOR PREGNANT WOMEN WITH DIABETES
SD9-3 15:45-16:15 DIAGNOSIS, MANAGEMENT, AND POSTPARTUM FOLLOWUP OF GESTATIONAL DIABETES MELLITUS
Hung-Yuan Li ( 李弘元 )
Chun-Heng Kuo ( 郭俊亨 )
Chih-Cheng Hsu ( 許志成 )
Chih-Cheng Hsu ( 許志成 )
Jian-Pei Huang ( 黃建霈 )
Szu-Chieh Chen ( 陳思潔 )
Chun-Chuan Lee ( 李淳權 )
16:15-16:20 PANEL DISCUSSION All Chun-Chuan Lee ( 李淳權 )
Agenda 27
Topic Speaker
Moderator
March 23-24, 2024
LS: Lunch Symposium
March 23 (Sat)
12:00-13:00
March 24 (Sun)
12:30-13:30
March 23, 2024
Topic
LS1 諾和 諾德 EXPECT MORE FROM GLP-1: THE FUTURE OF HYPERGLYCEMIA TREATMENT
LS2 阿斯特 捷利康
A COMPREHENSIVE APPROACH TO PREVENT COMORBIDITIES AND COORDINATED TREATMENT FOR T2DM MANAGEMENT
LS3 諾華 PRECISION MEDICINE: BRAF MUTATIONS IN THYROID CANCER
LS4 拜耳 (1)NEW PILLAR TO ESTABLISH STANDARD OF CARE FOR CKD IN T2D: NON-STEROIDAL MRAS (FINERENONE)
SpeakerModerator
Kuo-Meng Liao ( 廖國盟 )
Shu-Yi Wang ( 王舒儀 )
Jin-Ying Lu ( 呂金盈 )
Shih-Tzer Tsai ( 蔡世澤 )
Chih-Yuan Wang ( 王治元 )
Pi-Jung Hsiao ( 蕭璧容 )
Chih-Hsun Chu ( 朱志勳 ) Chien-Ning Huang ( 黃建寧 ) (2)FIRSTHAND EXPERIENCE OF KERENDIA (FINERENONE)
LS5 亞培 ( 糖尿病 照護 ) CGM 數據的生成到臨床判讀: 利用 CGM 改變不同糖尿病患的生活方式
LS6 台田 MANAGEMENT OF DIABESITY: CURRENT CONCEPT & FUTURE PERSPECTIVES
LS7 友華 WHY SHOULD WE CONSIDER PITAVASTATIN /EZETIMIBE FIXEDDOSE COMB INATION FOR DYSLIPIDEMIA MANAGEMENT?
Shang-Feng Tsai ( 蔡尚峰 )
Chia-Hung Lin ( 林嘉鴻 )
Feng-Hsuan Liu ( 劉鳳炫 )
Shih Te Tu ( 杜思德 )
Hung-Yu Chang ( 張宏猷 )
Jung-Fu Chen ( 陳榮福 )
Chii-Min Hwu ( 胡啟民 )
28 Annual Meeting of the Endocrine Society and the Diabetes Association of the R.O.C. (Taiwan) The45 th March 23-24, 2024
Room Room 201 Room 301 Room 401 Room 402AB Room 202 Room 203 Room 205 Room 403 容納人數 600 人 220 人 220 人 200 人 80 人 80 人 80 人 60 人
LS1 諾和諾德 LS2 阿斯特 捷利康 LS3 諾華 LS4 拜耳 LS5 亞培 ( 糖尿病 照護 ) LS6 台田 LS7 友華 LS8 羅氏 醫療
LS9 葛蘭素 史克 LS10 諾和 諾德 LS11 華廣 LS12 新穎 LS13 安進 LS14 禮來 百靈佳 LS15 裕利 LS16 禮來
LS8 羅氏 醫療 (1)HEART FAILURE RISK MANAGEMENT IN DIABETES
(2) 羅氏甲狀腺檢測介紹
March 24, 2024 Topic
William (Roche)
Chandra (Roche)
SpeakerModerator
LS09 葛蘭素 史克 深入瞭解糖尿病患者帶狀疱疹的預防策略 Tzu-Yuan Wang ( 王子源 )
LS10 諾和 諾德
CUTTING-EDGE INSULIN TREATMENT STRATEGIES FOR DIABETES MANAGEMENT Yu-Fang Cheng ( 鄭畬方 )
LS11 華廣 I NTERNET OF THINGS BASED CONTINUOUS GLUCOSE MONITORING
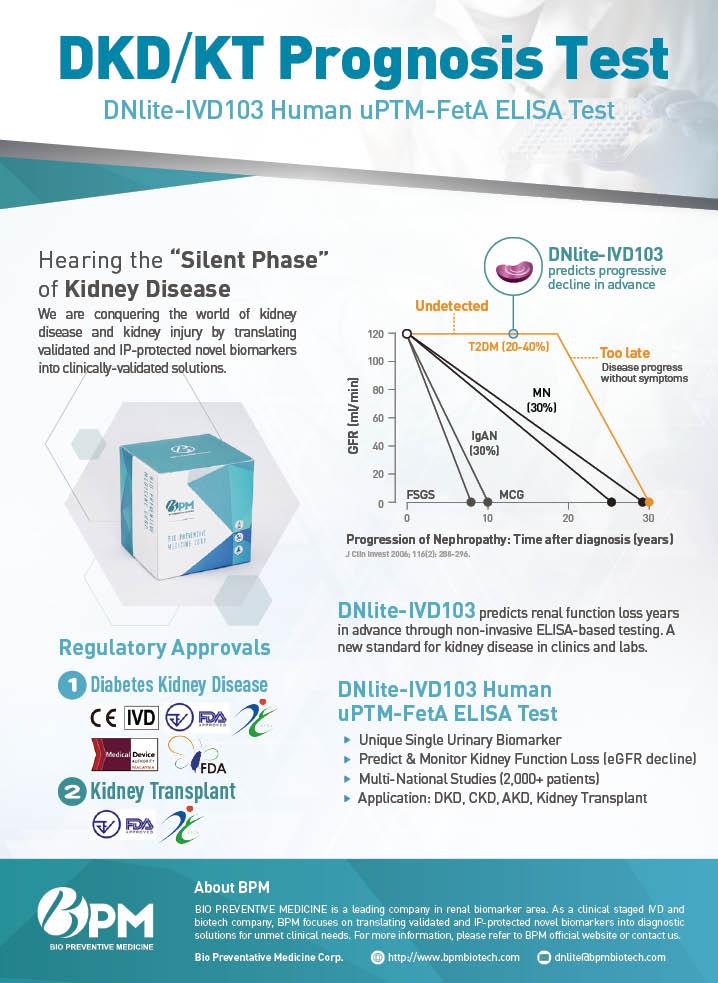
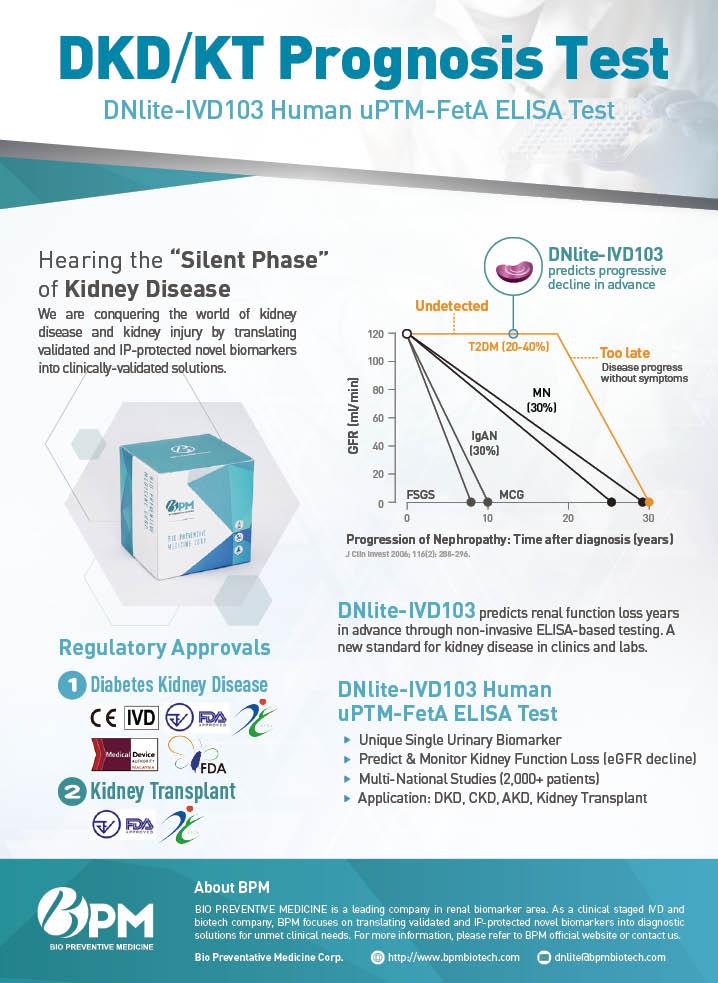
LS12 新穎 (1)URINARY PTM-FETA PREDICTS PROGRESSIVE EGFR DECLINE IN T2D - A NTUH COHORT STUDY
(2)PROGRESSIVE EGFR DECLINE IN TYPE 2 DIABETES IN THE DUTCH DIALECT COHORT: FOCUS ON URINARY PTM-FETA
LS13 安進 THE SILENT DISEASE: LONGTERM TREATMENT AND LATEST DEVELOPMENTS OF OSTEOPOROSIS!
LS14 禮來 百靈佳 JARDIANCE MAKES PROTECTION YOUR SUPER-POWER FROM PROTECTING KIDNEY, HEART AND METABOLIC DISEASES
LS15 裕利 TIMING OF INTENSIFICATION OF GLUCOSE-LOWERING THERAPY IN PATIENTS WITH TYPE 2 DIABETES: WHEN TO SELECT, WHAT TO EXPECT?
LS16 禮來 HOW CAN INCRETIN PHYSIOLOGY REVOLUTIONIZE T2D TREATMENT ?
Po-Tsun Tu ( 杜柏村 )
Ching-Chu Chen ( 陳清助 )
Shih-Te Tu ( 杜思德 )
Ming-Chia Hsieh ( 謝明家 )
Lee-Ming Chuang ( 莊立民 ) Chien-Ning Huang ( 黃建寧 )
Stephan Bakker
Keh-Sung Tsai ( 蔡克嵩 )
Chih-Yuan Wang ( 王治元 )
Feng-Chih Kuo ( 郭俸志 ) Jung-Fu Chen ( 陳榮福 )
Chih-Hung Lin ( 林志弘 ) Wei-Shiung Yang ( 楊偉勛 )
Kuo-Meng Liao ( 廖國盟 )
Yi-Sun Yang ( 楊宜瑱 )
Agenda 29
March 23, 2024
Room 202】
Time
OE: Oral Presentation-Endocrine
Topic
OE1 17:00-17:10 THYROGLOBULIN IN WASHOUT FLUID OF LYMPH NODE ASPIRATION: AS A METHOD TO DETECT CERVICAL LYMPH NODE METASTASIS FROM PAPILLARY THYROID CANCER: CASE REPORTS AND LITERATURE REVIEW
OE2 17:10-17:20 CHANGES IN THYROID FUNCTION DURING PREGNANCY: A PROSPECTIVE OBSERVATIONAL STUDY TO DETERMINE TRIMESTER SPECIFIC REFERENCE INTERVALS
OE3 17:20-17:30 A CASE OF BILATERAL ADRENAL ADENOMA WITH PRIMARY ALDOSTERONISM AND CUSHING SYNDROME
OE4 17:30-17:40 EXTENDED REAL-WORLD OBSERVATION OF PATIENTS TREATED WITH SORAFENIB FOR RADIOACTIVE IODINE-REFRACTORY DIFFERENTIATED THYROID CARCINOMA AND IMPACT OF LENVATINIB SALVAGE TREATMENT: EXPERIENCE FROM CHANG GUNG MEMORIAL HOSPITAL, LINKOU
OE5 17:40-17:50 INVESTIGATION OF DIETARY EFFECTS ON BODY COMPOSITION AND SKELETAL MUSCLE PERFORMANCE IN ANIMAL MODEL OF SARCOPENIC OBESITY
OE6 17:50-18:00 THERAPEUTIC INHIBITION OF ATR IN DIFFERENTIATED THYROID CANCER
Speaker
Ping-Chen Kuo ( 郭柄辰 )
Li-Hsin Pan ( 潘立昕 )
Moderator
Yun-Kai Yeh ( 葉雲凱 )
Chieh-Hua Lu ( 呂介華 )
Miaw-Jene Liou ( 劉妙真 )
Szu-Tah Chen ( 陳思達 )
Chia-Luen Huang ( 黃嘉崙 )
Shu-Fu Lin ( 林樹福 )
He-Jiun Jiang ( 姜和均 )
30 Annual Meeting of the Endocrine Society and the Diabetes Association of the R.O.C. (Taiwan) The45 th March 23-24, 2024
【
March 23 2024
【Room 203】
Time
OD: Oral Presentation-Diabetes
Topic
OD-1 17:00-17:10 A COST-EFFECTIVENSS ANALYSIS OF FIRST-LINE COMBINATION USE OF LINAGLIPTIN (TRAJENTA ®) AND METFORMIN IN PATIENTS WITH TYPE 2 DIABETES MELLITUS IN TAIWAN
OD-2 17:10-17:20 LIRAGLUTIDE REDUCES HEPATOCYTE LIPID ACCUMULATION AND RELATED DAMAGE BY INHIBITING EPITHELIALMESENCHYMAL TRANSITION
OD-3 17:20-17:30 RELATIONSHIP BETWEEN HABITUAL LATE CHRONOTYPE GENE AND METABOLIC SYNDROME: ONESAMPLE AND TWO-SAMPLE MENDELIAN RANDOMIZATION
OD-4 17:30-17:40 DIFFERENCES IN HEALTH-RELATED QUALITY OF LIFE BETWEEN PATIENTS WITH YOUNG-ONSET TYPE 2 DIABETES MELLITUS AND PATIENTS WITH TYPE 1 DIABETES MELLITUS: RESULTS FROM THE TAIWAN DIABETES REGISTRY
OD-5 17:40-17:50 DIABETIC PERIPHERAL NEUROPATHY IS A MAJOR DETERMINANT OF 10YEAR ATHEROSCLEROTIC CARDIOVASCULAR DISEASE RISKS IN PATIENTS WITH TYPE 2 DIABETES MELLITUS
OD-6 17:50-18:00 CORRELATION WITH FIB-4 AND CHRONIC KIDNEY DISEASE IN PATIENTS WITH DM - A RETROSPECTIVE COHORT STUDY
Speaker Moderator
HuangTz (Anita) Ou ( 歐凰姿 )
ChunCheng Liao ( 廖俊正 )
Chun-Yi Lee ( 李君儀 )
Tien-Jyun Chang ( 張恬君 )
HsuanWei Lin ( 林軒維 )
Ching-Chu Chen ( 陳清助 )
Tsung-Hui Wu ( 吳崇暉 ) Kang-Chih Fan ( 范綱志 )
Ya-Chen Yang ( 楊亞宸 )
Agenda 31
March 23-24, 2024
【3/4 F Walkway】 AR: 2023 Outstanding Research Award
Topic
AR-1 A COMMON EAST-ASIAN ALDH2 MUTATION CAUSES METABOLIC DISORDERS AND THE THERAPEUTIC EFFECT OF ALDH2 ACTIVATORS
March 23-24, 2024
【3/4 F Walkway】
Topic
內分泌暨糖尿病學會優秀論文獎
AP-1 CLINICAL IMPACT OF ANDROGEN RECEPTORSUPRESSING MIR-146B EXPRESSION IN PAPILLARY THYROID CARCINOMA
AP-2 TRAITS OF PATIENTS WITH PITUITARY TUMORS IN MULTIPLE ENDOCRINE NEOPLASIA TYPE 1 AND COMPARING DIFFERENT MUTATION STATUS
諾和諾德優秀論文獎
AP-3 THE RISK OF SEVERE HYPOGLYCEMIA AND MORTALITY IN PATIENTS WITH TYPE 2 DIABETES AND DISCHARGED WITH ACUTE LIVER INJURY
AP-4 COMPARISONS BETWEEN DIFFERENT ANTIOSTEOPOROSIS MEDICATIONS ON POSTFRACTURE MORTALITY: A POPULATION-BASED STUDY
Author
Yi-Cheng Chang ( 張以承 )
Author
Chen-Kai Chou ( 周振凱 )
Kuan Yu Lin ( 林冠宇 )
Fu-Shun Yen ( 顏福順 )
Chih-Hsing Wu ( 吳至行 )
32 Annual Meeting of the Endocrine Society and the Diabetes Association of the R.O.C. (Taiwan) The45 th March 23-24, 2024
傑出研究獎
AP:
優秀論文獎
2023 Outstanding Paper Award
March 23-24, 2024 【3F Walkway】
PE: Poster Presentation- Endocrine
Reviewers: Yu-Hsin Chen、Yu-Hsuan Li、Kuan Yu Lin、Jin-Wei Huang ( 陳瑜忻、李宇璇、林冠宇、黃峻偉 )
Scoring time: 14:50-15:20, March 23(Sat)
Topic
PE01 TRADITIONAL CHINESE MEDICINE THERAPY ASSOCIATED WITH LOWER RISK OF FRACTURE, HOSPITALIZATION AND DEATH IN PATIENTS WITH LOWER EXTREMITY INJURIES COMBINED WITH OSTEOPOROSIS
PE02 HYPOTHALAMIC LANGERHANS CELL HISTIOCYTOSIS PRESENTING WITH CENTRAL DIABETES INSIPIDUS, RHABDOMYOLYSIS, AND ENDOCRINOPATHY IN A 36-YEAR-OLD WOMAN
PE03 DELAYED SURGICAL INTERVENTION IN AN ELDERLY PATIENT WITH PERSISTENT HEMATOMA AFTER THYROID FINE-NEEDLE ASPIRATION: A CASE REPORT
PE04 A 34-YEAR-OLD WOMAN WITH SEVERE HYPONATREMIA AND SECONDARY ADRENAL INSUFFICIENCY DUE TO PARTIALLY EMPTY SELLA SYNDROME A CASE REPORT
PE05 RESISTANCE TO THYROID HORMOINE COEXISTING WITH PROLATINOMA---A CASE REPORT
PE06 PHEOCHROMOCYTOMA WITH PAPILLARY THYROID CARCINOMA: A CASE REPORT
PE07 RISK FACTORS FOR MORTALITY IN PATIENTS WITH POORLY DIFFERENTIATED THYROID CANCER
PE08 MEDICAL MANAGEMENT OF ECTOPIC CUSHING SYNDROME: CASE REPORT
Author
Hong-Han Lin ( 林宏翰 )
Yu-Shiuan Liang ( 梁友瑄 )
Meng-Jie Tsai ( 蔡孟潔 )
Yun-Ju Pan ( 潘韻如 )
Wan-Yi Lu ( 呂宛頤 )
Hao-Ting Chuang ( 莊皓廷 )
Chih-Wei Hsu ( 徐智威 )
Yi-Fu Lin ( 林以茀 )
Agenda 33
Topic
PE09 CRIBRIFORM-MORULAR VARIANT OF PAPILLARY THYROID CARCINOMA AND FAP : A CASE REPORT
PE10 CARBIMAZOLE INDUCED CHOLESTATIC HEPATITIS IN GRAVES´DISEASE: CASE REPORT AND REVIEW LITERATURE
PE11 DETERMINATION OF IODINE AND SELENIUM CONCENTRATION IN EDIBLE AND MEDICINAL CHINESE HERBS USING INDUCTIVELY COUPLED PLASMA MASS SPECTROMETRY
PE12 A CASE OF BILATERAL ADRENAL LYMPHOMA WITH PRESENTATION OF ADRENAL INSUFFICIENCY
PE13 PROGNOSIS OF YOUNG PATIENTS WITH PAPILLARY THYROID CANCER
PE14 PRIMARY HYPERPARATHYROIDISM PRESENTING WITH SEVERE HYPERCALCEMIA: TWO CASE REPORTS
PE15 THYROID ARTERY EMBOLIZATION FOR THE TREATMENT OF HYPERTHYROIDISM AND THYROID NODULES: A CASE REVIEW IN A SINGLE HOSPITAL
PE16 NORMOTENSIVE ADRENAL INCIDENTALOMA AS THE INITIAL PRESENTATION OF CONNSHING' SYNDROME
PE17 A CASE OF LUNG ADENOCARCINOMA PRESENT WITH SECONDARY ADRENAL INSUFFICIENCY AND PRIMARY HYPOTHYROIDISM DUE TO PEMBROLIZUMAB
PE18 OUTCOMES IN CHILDREN AND ADOLESCENTS WITH FOLLICULAR THYROID CANCER
PE19 CASE REPORT: A CASE HAD HYPERTHYROIDISM COMBINE CEREBRAL VENOUS THROMBOSIS
Author
Chih-Wei Hsu ( 徐智威 )
Myo Myo Aye ( 王寶妹 )
Chao-Jung Chang ( 張召融 )
Wan-Yin Cheng ( 鄭菀韻 )
Yu-Ling Lu ( 呂毓苓 )
Yu-Ping Hsieh ( 謝育平 )
Chia-Yu Chang ( 張嘉裕 )
Jau-Fong Hunag ( 黃兆逢 )
Yu-Ching Huang ( 黃郁青 )
Chia-Jung Hsu ( 許嘉容 )
Ying-Yu Tseng ( 曾盈瑜 )
34 Annual Meeting of the Endocrine Society and the Diabetes Association of the R.O.C. (Taiwan) The45 th March 23-24, 2024
Topic
PE20 ANALYSIS OF RISK FACTORS FOR HIGH-RISK LYMPH NODE METASTASIS IN PAPILLARY THYROID MICROCARCINOMA
PE21 A HASHIMOTO'S ENCEPHALOPATHY PATIENT PRESENTING WITH ACUTE ONSET OF NEUROCOGNITIVE BEHAVIORAL DISORDER: A CASE REPORT
PE22 A RARE CASE OF MALIGNANT HYPERCALCEMIA THAT WAS CAUSED BY ECTPOIC HYPERPARATHYROIDISM
PE23 COMBINED TRADITIONAL CHINESE MEDICINE TREATMENT IN PATIENTS WITH HYPERTHYROIDISM ASSOCIATED WITH LOWER RISK OF FRACTURE, HOSPITALIZATION RATE AND MORTALITY, A NATIONAL-WIDE POPULATION-BASED STUDY
March 23-24, 2024
3F Walkway】
Author
Yi-Hsiang Chiu ( 邱奕翔 )
Yi-Ting Chiu ( 邱依婷 )
Yi-Ching Tsai ( 蔡依靜 )
Chieh-Hua Lu ( 呂介華 )
PD: Poster Presentation-Diabetes
Reviewers: Yi-Jing Sheen, Feng-Chih Shen, Sheng-Chiang Su, Yao-Hsien Tseng ( 沈宜靜、沈峰志、蘇聖強、曾耀賢 )
Scoring time: 14:50-15:20, March 23(Sat)
Topic
PD01 THE GLUCOTYPES AMONG PATIENTS WITH TYPE 2 DIABETES IN DIALYSIS
PD02 A CASE OF MATERNALLY INHERITED DIABETES AND DEAFNESS WITH MITOCHONDRIAL A3243G MUTATION IN THE MT-TL1 GENE
PD03 METABOLIC SYNDROME Z SCORE (METS-Z) RISK ASSESSMENT IN ASSOCIATION WITH DIABETES
PD04 A CASE REPORT OF SEVERE HYPOGLYCEMIA DUE TO METASTATIC LUNG SARCOMA
Author
Yu-Yun Chou ( 周鈺芸 )
Fu-Shun Ko ( 柯富翔 )
Paul Wei-Che Hsu ( 徐唯哲 )
Jui-Hsiang Li ( 李瑞祥 )
Agenda 35
【
Topic
PD05 CURRENT STATUS OF TREATMENT FOR DIABETES MELLITUS IN PREGNANCY IN A REGINAL HOSPOITAL
PD06 HEMOLYTIC ANEMIA DUE TO GLUCOSE-6-PHOSPHATE DEHYDROGENASE DEFICIENCY IN A NEWLY DIAGNOSED TYPE 2 DIABETES.
PD07 THE IMPACT OF PAY-FOR-PERFORMANCE PROGRAMS ON HOSPITALIZATION RISKS IN PATIENTS WITH TYPE 1 DIABETES
PD08 A CASE OF EPISODES OF HYPOGLYCEMIA IN NONDIABETIC ADULTS, SUSPECTED NON-ISLET CELL TUMOR RELATED
PD09 FIBROSIS-4 INDEX IS LINK TO THE RISK OF CARDIOVASCULAR DISEASE IN PATIENTS WITH TYPE 2 DIABETES MELLITUS AND HEPATITIS C INFECTION
PD10 SERUM AMYLOID A TAKING VITAMIN A ENHANCES INSULIN RESISTANCE IN ADIPOSE TISSUE THROUGH TLR4 SIGNALING
PD11 DIABETIC KETOACIDOSIS INDUCED BY SODIUMGLUCOSE TRANSPORTER 2 INHIBITOR IN A PATIENT WITH IMMUNE CHECKPOINT INHIBITOR-TRIGGERED TYPE 1 DIABETES: A CASE REPORT.
PD12 A PATIENT WITH MALIGNANT INSULINOMA AND MULTIPLE LIVER METASTASES: SYMPTOM IMPROVEMENT AFTER TREATMENT. - A CASE REPORT.
PD13 THE BENEFICIAL EFFECTS OF BEE POLLEN SUPPLEMENT ON METABOLIC SYNDROME COMPONENTS AND INFLAMMATION MARKERS: A TWOYEAR OBSERVATIONAL STUDY IN A HEALTHY COHORT
PD14 RELATIONSHIP BETWEEN GROWTH DIFFERENTIATION FACTOR-15 AND MUSCLE STRENGTH IN TYPE 2 DIABETES PATIENTS
Author
Jui-Hsiang Li ( 李瑞祥 )
Hung-Chun Chen ( 陳泓均 )
Fu-Shun Ko ( 柯富翔 )
Jui-Hsiang Sung ( 宋瑞祥 )
Guan-Yu Su ( 蘇冠伃 )
Pi-Chen Lin ( 林碧珍 )
Li-Na Ma ( 馬儷娜 )
Yun-Chi Lee ( 李蘊琪 )
Jia-Pei Wu ( 吳佳培 )
Wan-Yin Cheng ( 鄭菀韻 )
36 Annual Meeting of the Endocrine Society and the Diabetes Association of the R.O.C. (Taiwan) The45 th March 23-24, 2024
Topic
PD15 CORRELATION OF BRAIN-DERIVED NEUROTROPHIC FACTOR AS A PREDICTOR FOR PERIPHERAL NEUROPATHY IN PATIENTS WITH TYPE 2 DIABETES
PD16 METFORMIN AND THE RISKS OF CELLULITIS, FOOT INFECTIONS, AND AMPUTATION IN PATIENTS WITH TYPE 2 DIABETES
Author
Jui-Hsiang Sung ( 宋瑞祥 )
Yun-Kai Yeh ( 葉雲凱 )
PD17 THE IMPACT OF HEMODIALYSIS ON DIABETES MELLITUS Li-Yu Kao ( 高立宇 )
PD18 SARCOPENIA AND SEVERE SARCOPENIA IN ELDERLY WITH AND WITHOUT DIABETES: A COMMUNITY-BASED STUDY
Wei-Fu Huang ( 黃偉輔 )
PD19 PANCREATIC INSULINOMA: A CASE REPORT Chun-Yuan Huang ( 黃俊淵 )
PD20 DYSBIOSIS OF GUT MICROBIOTA IN PATIENTS WITH TYPE 2 DIABETES MELLITUS
PD21 VITAMIN E SUPPLEMENT PROVIDES BENEFICIAL EFFECTS ON METABOLIC SYNDROME COMPONENTS IN HEALTHY POPULATION
PD22 WHOLE TRANSCRIPTOME ANALYSIS REVEALS THAT SODIUM-GLUCOSE CO-TRANSPORTER 2 INHIBITOR MIGHT MODULATE AUTOPHAGY AND INFLAMMATORY PROPERTIES OF PERIPHERAL BLOOD MONONUCLEAR CELLS IN PATIENTS WITH TYPE 2 DIABETES.
PD23 GLP-1 RA THERAPY TO ATTENUATE THE RISK OF OSTEOARTHRITIS AND TOTAL KNEE REPLACEMENT IN TYPE 2 DIABETES MELLITUS, A NATIONAL-WIDE POPULATION-BASED COHORT STUDY
Ching-Chu Chen ( 陳清助 )
Chai-Chun Chen ( 陳茝君 )
Hsuan-Yu Fan ( 范軒瑜 )
Chih-Ping Lin ( 林治平 )
Agenda 37
PD24 ASSOCIATION WITH LOWERING FRACTURE, INPATIENT AND MORTALITY RISK IN PATIENTS OF DIABETES WITH OSTEOPOROSIS COMBINED TRADITIONAL CHINESE MEDICINE THERAPY
March 23-24, 2024 【3/4 F Walkway
An-Che Cheng ( 鄭安哲 )
BP: Brief Research Proposal of Pharmaceutical Company
BP-1 COMPARING THE REAL-WORLD EFFECTS OF ONCEWEEKLY GLP-1 RAS AND DPP-4IS ON ISCHEMIC STROKE AND MYOCARDIAL INFARCTION IN INDIVIDUALS WITH T2D AND ASCVD
BP-2 BENEFIT OF DUAL THERAPY WITH GLP-1 RA AND SGLT2I ON CARDIOVASCULAR OUTCOMES IN TYPE 2 DIABETES
BP-3 BENEFIT OF DUAL THERAPY WITH GLP-1 RA AND SGLT2I ON RENAL OUTCOMES IN TYPE 2 DIABETES
BP-4 LONGER TIME SPENT IN GLYCEMIC CONTROL AFTER INITIATING TIRZEPATIDE VS COMPARATORS: EXPLORATORY ANALYSIS OF SURPASS 1-5 TRIAL
BP-5 “SURPASS(ING)” AN ERA OF BASAL-BOLUS INSULIN THERAPY: TIRZEPATIDE VS INSULIN LISPRO TID ADDED-ON TO POORLY CONTROLLED BASAL INSULINTREATED TYPE 2 DIABETES!
Novo Nordisk
Novo Nordisk
Novo Nordisk
Eli Lilly
Eli Lilly
38 Annual Meeting of the Endocrine Society and the Diabetes Association of the R.O.C. (Taiwan) The45 th March 23-24, 2024
Topic Author
】
Topic Pharmaceutical Company
RE-DEFINING PRIMARY ALDOSTERONISM
ANAND VAIDYA, MD, MMSC
CenterforAdrenalDisorders,BrighamandWomen’sHospital,HarvardMedicalSchool,Boston,USA
There has been a revolution in our understanding of primary aldosteronism. We have recently learned that primary aldosteronism is a highly prevalent syndrome that is caused by heterogeneous adrenal morphologies, largely attributable to pathogenic somatic mutations. Primary aldosteronism contributes to cardiovascular, metabolic, and kidney disease. When recognized early, primary aldosteronism can be adequately treated with widely available mineralocorticoid receptor antagonists and/or surgical adrenalectomy to mitigate these adverse outcomes. Unfortunately, primary aldosteronism is rarely diagnosed, or adequately treated, mainly because of a lack of awareness and education. Most clinicians still operate using an outdated understanding of primary aldosteronism, wherein they rely on overly complex, arbitrarily derived, and unvalidated diagnostic processes that often delay diagnosis, or worse, result in erroneous exclusion of the diagnosis. In this plenary talk, the speaker will review the pathogenesis and pathophysiology of primary aldosteronism, the shortcomings of current diagnostic recommendations, and propose simplified and pragmatic approaches to maximize the detection, or empiric treatment, of primary aldosteronism.
Abstract 39 PL-1
EXPANDING INCRETIN UNIVERSE: FROM BASIC BIOLOGY TO CLINICAL TRANSLATION
DANIEL J. DRUCKER
Lunenfeld-TanenbaumResearchInstitute,Mt.SinaiHospital&UniversityofToronto,Canada
Enthusiasm for gut-derived therapies stems from a precise understanding of the physiological and pharmacological roles of gut hormones in control of normal and disordered energy homeostasis, coupled with extensive clinical validation. Interrogation of gut hormone action encompasses studies of hormone synthesis and secretion, clearance and degradation, receptor signaling and PK-PD relationships, receptor desensitization, communication with the CNS, and evaluation of the utility of preclinical models. Improved understanding of enteroendocrine science has yielded multiple gut-derived therapies for treatment of diabetes and more recently, obesity. The pleiotropic actions and striking efficacy of the GLP-1R agonists, has validated the enteroendocrine system and peptide hormone-based therapies as viable targets and platforms for development of improved next generation therapies for treatment of energy homeostasis. This lecture will discuss evidence based medicine linking the use of GLP-1-based medicines to improved cardiometabolic outcomes in people with type 2 diabetes and obesity. The future of GLP-1-based medicine will be highlighting, presaging the opportunity to extend disease indications while greatly enhancing the efficacy of current medical pharmacotherapy for type 2 diabetes. Next generation GLP-1-based medicines promise to deliver substantial improvements in glucose control, and greater weight loss, associated with major health benefits spanning multiple outcomes relevant to people living with type 2 diabetes, obesity, and cardiometabolic disorders.
Annual Meeting of the Endocrine Society and the Diabetes Association of the R.O.C. (Taiwan) The45 th 40 March 23-24, 2024 PL-2
NEW FORM OF HYPOPHYSITIS: A JOURNEY FOR THE DISCOVERY OF NOVEL DISEASES
YUTAKA TAKAHASHI M.D., PH.D.
DepartmentDiabetesandEndocrinology,NaraMedicalUniversity,Japan
This story began in 2003, we encountered a patient exhibiting acquired specific defect in GH, PRL, and TSH. The case was obviously “outlier” and we have been trying to clarify the pathophysiology of this condition. Subsequently, we have elucidated that this disease was caused by autoimmunity against pituitary specific transcription factor PIT-1, proposed a new clinical entity, and named as “anti-PIT-1 hypophysitis” (formerly “anti-PIT-1 antibody syndrome”.
Furthermore, we clarified that anti-PIT-1 hypophysitis was caused by the ectopic expression of PIT-1 in the complicated tumour, evoking autoimmunity against PIT-1-expressing cells in the pituitary. In this condition, the cytotoxic T cells that specifically react with PIT-1 epitopes attacked somatotrophs, lactotrophs and thyrotrophs. Recently, we have succeeded the disease modeling using co-culture system of patient’s iPS cells-derived pituitary and cytotoxic T cells.
Subsequently, we found a component of immune checkpoint inhibitor-related hypophysitis and isolated ACTH deficiency was caused by the similar mechanisms; therefore, we proposed a new clinical entity, paraneoplastic autoimmune hypophysitis that includes antiPIT-1 hypophysitis and, a component of immune checkpoint inhibitor-related hypophysitis and isolated ACTH deficiency, defined as hypophysitis caused by autoimmunity against specific anterior pituitary cells, associated with neoplasm.
The underlying mechanism involves the ectopic expression of pituitary antigen in the tumour, evoking autoimmunity against anterior pituitary cells. Its discovery has led to the classification of hypophysitis being revised based on pathophysiology and aetiology
Moreover, the concept of paraneoplastic autoimmune hypophysitis highlights several insights not only for physician scientists, but also for physicians. In this plenary lecture, I talk about the story of discovery of anti-PIT-1 hypophysitis, developing the concept of paraneoplastic autoimmune hypophysitis, corresponding lessons, and new approaches of onco-immune endocrinology over 20 years of the series of research.
Abstract 41 PL-3
THE DOUBLE JEOPARDY BETWEEN DIABETES AND DEMENTIA
糖尿病及失智症的雙向影響
JUNG-FU CHEN
陳榮福
DivisionofEndocrinologyandMetabolism,DepartmentofInternalMedicine,KaohsiungChangGungMemorial Hospital,Kaohsiung,Taiwan.
高雄長庚醫院內分泌暨新陳代謝科
Type 2 diabetes mellitus (T2DM) is a well-known worldwide epidemic that is increasing as the years progress. Many complications arise from T2DM, such as coronary vascular disease, kidney and eye damage, and quite significantly, dementia. Type 2 diabetes has been consistently associated with an increased risk of dementia, including Alzheimer’s disease and vascular dementia, mild cognitive impairment. It is speculated that dementia stems from the fact that the brain is susceptible to hyperglycemic conditions, which are promoted by insulin resistance of target cells in the central nervous system. This directly affects cognitive processes and memory, which correlates to decreased temporal and front lobes volume. The risk of diabetic complications can be minimized with therapeutic interventions such as oralantidiabetic (OAD) agents and insulin. Thiazolidinediones may be the most beneficial drug class for reducing the risk of dementia in T2DM patients. Future research should focus on whether early intervention with specific classes of OADs can not only improve glycemic control, but also prevent the build-up of damaged brain tissue and help to reduce the risk and incidence of dementia in patients with T2DM.
Annual Meeting of the Endocrine Society and the Diabetes Association of the R.O.C. (Taiwan) The45 th 42 March 23-24, 2024 PL-4
DAROC-TADE-2
QUASI-EXPERIMENTAL EVALUATION OF A NATIONWIDE DIABETES PREVENTION PROGRAMME
英國全國性糖尿病預防計劃的準實驗評估
YAO-HSIEN TSENG
曾耀賢
DivisionofEndocrinologyandMetabolism,TaichungMetroHarborHospital
童綜合醫院新陳代謝科
National Health Service Diabetes Prevention Program (NHS DPP) in the UK was designed to mitigate the risk of type 2 diabetes through a structured behavior change program. It used a quasi-experimental study design to assess the impact of the NHS DPP on health outcomes such as HbA1c, body mass index, weight, and serum lipid levels. Data for the analysis was drawn from a substantial cohort of general practice records within the Clinical Practice Research Datalink (CPRD) Aurum and NHS England Hospital Episode Statistics
Admitted Patient Care (HES APC) databases.
The study utilized a regression discontinuity approach, where the eligibility threshold for the NHS DPP played a pivotal role in determining the impact of referrals to intensive lifestyle counseling on health outcomes. This approach effectively captures the causal effect of the NHS DPP by comparing patients just above and below the HbA1c eligibility threshold, thus mimicking a randomized controlled trial.
A difference-in-differences analysis was also employed to leverage the phased national roll-out of the NHS DPP across three waves, with the control group being the practices from wave 3, which had not yet implemented the program. This method accounts for both the timing of the treatment and the changes in health outcomes observed at different time points across the waves.
Furthermore, instrumental variable estimation was used to address potential endogeneity issues by using regional variation in NHS DPP coverage as an instrumental variable for actual program referral. This method helps in providing more reliable estimates of the treatment effect on health outcomes, particularly HbA1c concentrations.
The study's findings indicated that referral to the NHS DPP resulted in significant health
Abstract 43
benefits, including reductions in HbA1c, BMI, and weight. These results were robust across various analytical adjustments, such as accounting for the prescription of relevant medications and controlling for baseline characteristics.
Despite the positive outcomes, the study also noted the challenges in achieving a significant impact on diabetes complications, emergency hospitalizations for major adverse cardiac events (MACE), and mortality rates. Moreover, the increase in the diagnosis of type 2 diabetes at the eligibility threshold suggests the need for cautious interpretation, considering the potential for over-diagnosis due to increased screening efforts.
The study's methodology was rigorous, with several robustness checks and subgroup analyses conducted to validate the findings. These included negative outcome controls and stratified regression discontinuity analyses for primary and secondary outcomes. The study also accounted for variations in the implementation of the NHS DPP and controlled for several confounding factors.
Overall, the study provides strong evidence supporting the effectiveness of the NHS DPP in improving glycemic control and reducing the risk of type 2 diabetes. It underscores the value of large-scale preventive health programs and contributes significantly to the understanding of how such programs can be effectively implemented within a national health system. The NHS DPP serves as a model for other countries aiming to establish similar preventive health interventions, highlighting the importance of targeted, evidence-based approaches to public health challenges.
Annual Meeting of the Endocrine Society and the Diabetes Association of the R.O.C. (Taiwan) The45 th 44 March 23-24, 2024
DAROC-TADE-3
IMPACT OF LIFESTYLE CHANGES ON METABOLIC SYNDROME: IMPLICATIONS FROM THE PERSPECTIVE OF THE DIABETES
PREVENTION PROGRAM (DPP)
談生活型態改變對代謝症候的影響
FENG-CHIH SHEN
沈峰志
DivisionofEndocrinologyandMetabolism,DepartmentofInternalMedicine,KaohsiungChangGungMemorial Hospital,Kaohsiung,Taiwan.
高雄長庚醫院內分泌暨新陳代謝科
The National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) has enhanced the Diabetes Prevention Program (DPP) to create more accessible and cost-effective variants for the large population at risk of type 2 diabetes in the United States. The DPP aimed to assess whether its Lifestyle Change Program or metformin could delay or prevent type 2 diabetes. Results after three years showed a 58% reduction in diabetes development among participants of the Lifestyle Change Program compared to a placebo, with even greater efficacy (71%) in those aged 60 and above. Metformin also reduced diabetes risk by 31%, particularly effective in women with a history of gestational diabetes, younger adults (25-44 years), and individuals with a BMI of 35 or higher.
The DPP's success led to the Diabetes Prevention Program Outcomes Study (DPPOS), which continued to track the same participants. At the 10-year mark, the Lifestyle Change Program showed a 34% reduction in diabetes development, with a 49% reduction in participants over 60. Those continuing metformin had an 18% reduction. Both groups exhibited improved cardiovascular risk factors, with the Lifestyle Change Program achieving this with fewer medications. At 15 years, the delay in diabetes development was 27% for the Lifestyle Change Program and 18% for metformin users. About 55-56% of participants in both groups developed diabetes, compared to 62% in the placebo group. Notably, women from the Lifestyle Change Program had fewer small blood vessel complications.
Abstract 45
DAROC-TADE-4
EFFECT OF LIFESTYLE CHANGE ON THE RISK OF METABOLIC SYNDROME AND DIABETES: VIEWPOINT FROM TAIWAN HEALTH DATA
從台灣資料庫看生活型態改變對代謝症候群及糖尿病的影響
KUO-LIONG
CHIEN
簡國龍
InstituteofEpidemiologyandPreventiveMedicine,CollegeofPublicHealth,NationalTaiwanUniversity DepartmentofInternalMedicine,NationalTaiwanUniversity,Taipei,Taiwan
台大公共衛生學院流行病學與預防醫學研究所、台大醫院內科部
Metabolic syndrome and diabetes are a great disease burden globally: the World Health Organization 25x25 Global Action Plan for the Prevention and Control of Noncommunicable Disease has set up the voluntary goal to keep diabetes and obesity prevalence stable. To achieve the goal, primary prevention strategy for health promotion through various lifestyle change, such as improving physical activity, reducing risky dietary habits, controlling body weight, smoking quitting and appropriate alcohol drinking, has been advocated for controlling noncommunicable diseases.
Up to now, evidence from lifestyle change on reducing metabolic syndrome risk has been from randomized controlled clinical trial and large-scale population study, including Diabetes Prevention Programs in different countries, such as USA and UK. However, the effects of lifestyle change may be affected by cultural and ethnic backgrounds. In addition, some novel approaches, such as Mendelian Randomization using genomic information as instrumental variables, have been applied in primary prevention causation study. Moreover, the data from the Taiwanese official document, such as the 2019 Diabetes Atlas, did not provide the lifestyle change data.
Therefore, I would like to present some studies from the health dataset in Taiwan, including health insurance data and open available data, to provide the evidence for lifestyle change and the effect on metabolic syndrome and diabetes control.
Annual Meeting of the Endocrine Society and the Diabetes Association of the R.O.C. (Taiwan) The45 th 46 March 23-24, 2024
DAROC-TADE-5
A NURSE’S PERSPECTIVE ON THE IMPACT OF LIFESTYLE CHANGES ON METABOLIC SYNDROME
從護理師端看生活型態改變對代謝症候群的影響
HSEU-CHEN
LIU
劉秀珍
CaseManagementOFDiabetesHealthPromotionCenterofTaichungVeteransGeneralHospitalTaichung VeteransGeneralHospital
The role of the nurse is to provide educational guidance on the impact of lifestyle changes on metabolic syndrome - manage the condition - promote healthy life - support mental health - and play an important and indispensable role in communication and coordination.
The rise of smart lifestyle AI prediction tools help us enter a new era of health management. Traditional medicine mainly focuses on disease treatment. Modern people have different lifestyles. High-pressure work environments, busy life rhythms, and poor eating habits have become the causes of modern diseases. There are six pillars to improve your lifestyle: 1. Effective nutrition 2. Physical activity 3. Good sleep 4. Stress manage According to the "Survey on Health Behavior of Chinese People Over 35 Years Old", 80% of people think that their physical condition is not bad. After the DKABio health risk analysis model of Junhong Data, a subsidiary of Qisda, locates the health status of the respondents, 70% of men and 50% of women are only " "Feel good about yourself", which shows that the public's awareness of illness is seriously insufficient. Through the power of AI data, it will be possible to stimulate awareness of illness, and then actively manage health and say no to unhealthy lifestyles!
Based on the literature and lifestyle adjustment content, whether it is based on case questions or researchers' self-defined diabetes-related topics, they all emphasize stimulating case awakening, open communication, joint participation and utilization, finding resources and application, and providing necessary information to promote health. Behavior and wellbeing to improve health, advance deployment, and active control to jointly improve people's health and quality of life.ment 5. Positive social interaction 6. Avoiding the use of hazardous substances.
Abstract 47
DAROC-TADE-6
EFFECT OF LIFESTYLE CHANGES ON METABOLIC SYNDROME FROM DIETITIAN‘S POINT OF VIEW
從營養師端看生活型態改變對代謝症候群的影響
CHUNG-MEI OUYANG
歐陽鍾美
DepartmentofDietetics,NationalTaiwanUniversityHospitalHsin-ChuBranch,HsinchuCounty,Taiwan 臺大醫院新竹台大分院營養室
Metabolic syndrome (Mets) is a cluster of obesity-related cardiovascular risk factors including abdominal obesity, atherogenic dyslipidemia, high blood pressure and impaired glucose tolerance. It is highly prevalent and strongly associated with an increased risk of developing diabetes. Studies have shown that lifestyle modification has improved all components of Mets, and reduces the incidence of diabetes and cardiovascular disease. Lifestyle modifications, especially dietary habits, are the main therapeutic strategy for the treatment and management of metabolic syndrome. Excess energy intake and western dietary pattern may influence the development of metabolic syndrome. By contrast, both Mediterranean diet (Med-diet) and Dietary Approaches to Stop Hypertension (DASH) diet, with or without calorie restriction, have positive effects. For the prevention and management of Mets, it is recommended to increase the daily intake of fiber-rich and low-glycemic-index foods and the consumption of fish and dairy products, especially yogurt and nuts. It is also advisable to consume a large variety of unprocessed cereals, legumes, and fruit. Moreover, individual motivation leading to improved lifestyle adherence is a key factor in achieving reduction in metabolic syndrome components. These elements can be enhanced via frequent encounters with the health care system. Use of technologies such as mobile and Internet-based communication can increase the effectiveness of lifestyle change in metabolic syndrome, but should not replace personal contact as the cornerstone of therapy.
Annual Meeting of the Endocrine Society and the Diabetes Association of the R.O.C. (Taiwan) The45 th 48 March 23-24, 2024
DIAGNOSING AND TREATING PRIMARY ALDOSTERONISM
ANAND VAIDYA, MD MMSC
CenterforAdrenalDisorders,BrighamandWomen’sHospital,HarvardMedicalSchool,Boston,USA
This meet-the-professor session will build on the plenary talk by the same speaker. Using a case-based approach, the speaker will highlight pragmatic approaches to the diagnosis and treatment of primary aldosteronism. Topics of discussion will include the variability of aldosterone production, the interpretation of diagnostic testing, the value and pitfalls of conducting aldosterone suppression testing, and biomarkers to optimize the treatment of primary aldosteronism.
Abstract 49 MTP-E1
EVOLVING CONCEPTS OF LOW-DENSITY LIPOPROTEIN: FROM STRUCTURE TO FUNCTION
CHU-HUANG (MENDEL) CHEN, MD PHD
陳珠璜
The Texas Heart Institute
Lipid metabolism orchestrates a delicate balance in cellular functions, energy homeostasis, and cardiovascular health, employing dynamic carriers such as lipoproteins. Among these, low-density lipoprotein (LDL) assumes a pivotal role in lipid transport and is closely intertwined with cardiovascular disease.
Widely recognized as “bad cholesterol,” LDL stands as a linchpin in lipid transport, its elevated levels intricately linked to heightened cardiovascular risks. Recent research has broadened our comprehension of LDL beyond its role as a mere cholesterol carrier, unveiling its versatile and multifaceted functions.
Despite aggressive lipid-lowering treatments, residual cardiovascular risk persists, driven by non-lipid factors like hypertension, diabetes, smoking, and lifestyle choices. Moreover, lipid-lowering therapies may not directly address plaque stability. Atherosclerosis proves a complex process with varying impacts on distinct vascular beds, and multifactorial etiologies can influence treatment efficacy.
In this lecture, I will summarize the evolving understanding of LDL, emphasizing both its structural intricacies and dynamic functional roles. Going beyond its role as a cholesterol transporter, LDL’s involvement in various physiological and pathological processes challenges conventional perspectives. The presentation delves into historical viewpoints, emerging research, and clinical implications, providing insights into the transforming landscape of LDL—from a simple lipid carrier to a molecular entity with profound implications for human health.
A brief historical review reveals that efforts in the early 20th century to isolate and identify lipoproteins paved the way for the distinct identification of LDL, marking a significant milestone in further investigations. Notably, Russian scientist Nikolay N.
Annual Meeting of the Endocrine Society and the Diabetes Association of the R.O.C. (Taiwan) The45 th 50 March 23-24, 2024 MTP-E2
Anichkov (1885–1964), often spelled Anitschkow in German literature, emerges as one of the foremost contributors to the discovery of LDL. His pioneering research on lipoproteins and substantial contributions to early lipid metabolism studies played a pivotal role in advancing our understanding of this crucial component. In the mid-20th century, the formulation of the cholesterol transport hypothesis by researchers such as Gofman and Lindgren provided a theoretical framework linking elevated LDL levels to increased cardiovascular risk. A pivotal moment in LDL research occurred in the 1970s with the development of the Friedewald equation, which facilitated practical estimation of LDL cholesterol levels and standardized assessments in clinical settings.
The groundbreaking work of Brown and Goldstein in the 1980s elucidated the receptormediated endocytosis of LDL, offering a molecular understanding of cellular cholesterol acquisition and establishing connections between LDL metabolism and cellular processes. Advances in genetic research, including the discovery of familial hypercholesterolemia, underscored genetic factors influencing LDL metabolism, emphasizing the importance of personalized approaches. Recent research has revealed diverse functions of LDL, challenging traditional views and highlighting its involvement in various physiological and pathological processes.
In summary, LDL is a complex particle essential to life, but it can also pose health risks when it undergoes inappropriate modifications. As science and technology advance, our understanding of LDL continues to evolve. Our team is committed to further exploring the mysteries surrounding this ancient lipid entity.
Abstract 51
DRIVING SAFETY IN PEOPLE LIVING WITH DIABETES
糖尿病友行車安全
YI-JING SHEEN
沈宜靜
DepartmentRadiationOncology,Lo-TungPohaiHospital,YilanCounty,Taiwan
臺中榮民總醫院新陳代謝科
The interplay between diabetes management and driving safety represents a critical concern for individuals living with diabetes, healthcare providers, and public safety officials. This lecture aims to elucidate the impact of diabetes on driving capabilities, emphasizing the importance of blood glucose control, complications screening, early identification of hypoglycemic events, and the implementation of strategies to mitigate risks associated with driving. Diabetes can significantly affect an individual's ability to drive safely due to the potential for hypoglycemic episodes, which may impair cognitive function, reaction times, and visual perception. The lecture will discuss the physiological and psychological effects of diabetes that can influence driving skills, including hypoglycemia unawareness, a condition that diminishes the ability to recognize early signs of low blood glucose levels. We will explore evidence-based guidelines for managing diabetes in the context of driving, including the role of glucose monitoring strategy and insulin management strategies to maintain optimal blood glucose levels. The importance of regular medical evaluations and the development of individualized health plans that consider the unique challenges faced by drivers with diabetes will also be highlighted. By integrating clinical insights with practical advice, this lecture aims to foster a comprehensive understanding of the challenges and solutions associated with driving safety in people living with diabetes. The goal is to empower individuals with diabetes to maintain their independence and safety on the road while ensuring the well-being of the wider community.
Annual Meeting of the Endocrine Society and the Diabetes Association of the R.O.C. (Taiwan) The45 th 52 March 23-24, 2024
MTP-D1
DRIVING SAFETY IN OLDER PATIENTS WITH DIABETES
老年糖尿病人駕駛安全
SHIH-YI LIN
林時逸
CenterforGeriatricsandGerontology, TaichungVeteransGeneralHospital,Taichung,Taiwan
臺中榮民總醫院高齡醫學中心
With the aging population, the number of older drivers is rapidly increasing. By 2025, it is projected that 20% of the Taiwan population will be aged 65 or older, meaning that one in every five drivers is expected to be over 65 years old. As older individuals lead increasingly active lifestyles, they are expected to rely more on vehicles, travel longer distances, and retain their driver’s licenses for longer periods compared to previous generations. Diabetes can affect driving performance because chronic complications can impair sensory or motor functions (such as retinopathy, neuropathy, amputation, vascular diseases), and temporary cognitive impairment or loss of consciousness due to hypoglycemia induced by anti-hyperglycemic medications. Additionally, other medical conditions related to diabetes, such as sleep apnea, may also negatively impact driving performance. Undetected hypoglycemia is the most relevant driving risk for diabetic drivers. Data on the effects of hyperglycemia on driving are limited and may depend on how hyperglycemia is defined. The higher accident rate among older adults may be attributed to age-related medical conditions. Many studies indicate that these diseases lead to poorer driving performance on road and simulator assessments compared to the general elderly population. Complications of diabetes in older individuals may exacerbate their condition, necessitating additional preventive measures. Besides, example, older diabetic individuals may experience visual impairment, mild cognitive impairment, early dementia, and other neurodegenerative diseases, or they may have suffered strokes. All of these conditions produce symptoms that affect the skills required for safe driving. Given these findings, special consideration may be needed for elderly individuals with diabetes when it comes to driving. Encouraging safe driving among diabetic patients is likely most important, whereby healthcare professionals treating diabetes provide education on the potential risks of diabetes-related driving and patient treatment plans and interventions that are tailored for them. Finally, given impact of traffic accident with death and injury from road trauma, developed guidelines are needed to be made and facilitated in clinical practice.
Abstract 53
MTP-D2
THE INVOLVEMENT OF DIET-INDUCED THERMOGENESIS IN OBESITY DEVELOPMENT- THE ROLE OF BROWN ADIPOSE TISSUE
飲食誘發產熱作用與肥胖發展之關係 - 棕色脂肪組織所扮演的角色
PO-SHIUAN HSIEH
謝博軒
GraduateInstituteofMedicalSciences,NationalDefenseMedicalCenter,Taipei,Taiwan
國防醫學院醫學科學研究所
Brown adipose tissue (BAT) has been considered a vital organ in response to nonshivering adaptive thermogenesis, which could be activated during cold exposure through the sympathetic nervous system (SNS) or under postprandial conditions contributing to dietinduced thermogenesis (DIT). Humans prefer to live within their thermal comfort or neutral zone with minimal energy expenditure created by wearing clothing, making shelters, or using an air conditioner to regulate their ambient temperature; thereby, DIT would become an important mechanism to counter-regulate energy intake and lipid accumulation. In addition, there has been a long interest in the intriguing possibility that a defect in DIT predisposes one to obesity and other metabolic diseases. Due to the recent advances in methodology to evaluate the functional activity of BAT and DIT, this lecture will focus on the role and regulatory mechanism of BAT biology in DIT in health and obesity condition.
Annual Meeting of the Endocrine Society and the Diabetes Association of the R.O.C. (Taiwan) The45 th 54 March 23-24, 2024
SE1-1
SE1-2
PRECLINICAL DEVELOPMENT FOR OBESITY
臨床前減重藥物研發
YI-CHENG CHANG
張以承
DepartmentofMetabolismandEndocrinology,NationalTaiwanUniversityHospital,Taiwan;GraduateInstitute ofMedicalGenomicsandProteomics,NationalTaiwanUniversity,Taiwan;InstituteofBiomedicalSciences, AcademiaSinica,Taiwan
臺大醫院內分泌新陳代謝科;臺大醫學院基因體暨蛋白體醫學研究所,中央研究院生物醫學科學研究所
ALDH2 (acetaldehyde dehydrogenase 2, mitochondrial) is the key metabolizing enzyme of acetaldehyde and other toxic aldehydes, such as 4-hydroxynonenal. A missense Glu504Lys mutation of the ALDH2 gene is prevalent in 560 million East Asians, resulting in reduced ALDH2 enzymatic activity. We find that Aldh2 knock-in mice mimicking human Glu504Lys mutation were prone to develop diet-induced obesity, glucose intolerance, insulin resistance, and fatty liver due to reduced adaptive thermogenesis and energy expenditure. AD-9308, a water-soluble, potent, and highly selective ALDH2 activator ameliorates diet-induced obesity and fatty liver, and improves glucose homeostasis in both Aldh2 wild-type and knock-in mice. These results highlight the potential of reducing toxic aldehyde levels by activating ALDH2 for treating obesity.
Peroxisome proliferator-activated receptor γ (PPARγ) is a master transcriptional regulator of systemic insulin sensitivity and energy balance. The anti-diabetic drug thiazolidinediones (TZDs) are potent synthetic PPARγ ligands with undesirable side effects, including obesity, fluid retention, and osteoporosis. 15-keto-PGE2 is an endogenous PPARγ ligand metabolized by prostaglandin reductase 2 (PTGR2). Here, we confirmed that 15-keto-PGE2 binds and activates PPARγ via covalent binding. In patients with type 2 diabetes and obese mice, serum 15-keto-PGE2 levels were decreased. Administration of 15-keto-PGE2 improves glucose homeostasis and prevented diet-induced obesity in mice. Either genetic inhibition of PTGR2 or PTGR2 inhibitor BPRPT0425 protected mice from diet-induced obesity, insulin resistance, and hepatic steatosis without fluid retention and osteoporosis. These data indicate inhibition of PTGR2 is a new therapeutic approach to treat diabetes and obesity through increasing
Abstract 55
endogenous PPARγ ligands without side effects of synthetic PPARγ ligands TZDs.
We also identified a glucose polymer can effectively absorb intestinal fat and reduce dietinduced obesity by approximately ~10% in high-fat high-sucrose diet-induced obese rats. This fat sequestrant can complement the shortcomings of current incretin-based therapy.
Annual Meeting of the Endocrine Society and the Diabetes Association of the R.O.C. (Taiwan) The45 th 56 March 23-24, 2024
CROSSTALK BETWEEN ADIPOSE TISSUE, MUSCLE, AND APOPTOSIS OF β CELLS IN OBESITY AND TYPE 2 DIABETES
脂肪組織、肌肉與 β 細胞凋亡於肥胖和第二型糖尿病之串聯
CHUNG-ZE
WU
吳忠擇
DivisionofEndocrinologyandMetabolism,DepartmentofInternalMedicine,SchoolofMedicine,Collegeof Medicine,TaipeiMedicalUniversity
臺北醫學大學醫學院醫學系新陳代謝與內分泌科
The rising prevalence of obesity and type 2 diabetes mellitus has become increasingly prominent in recent decades. This increase is closely linked to the accumulation of excess body fat, which triggers systemic inflammation and thrombosis, consequently leading to cardiovascular diseases and associated comorbidities. It is important to recognize that white adipose tissue is not merely a storage site for fat but also functions as an endocrine organ. During white adipose tissue dysfunction, adipocytes release various adipokines, some of which have been shown to play roles in the apoptosis and regeneration of β cells. However, it is crucial to understand that not all adipose tissues contribute negatively. Particularly noteworthy is brown adipose tissue, which is actively involved in thermogenesis and energy expenditure. Moreover, there exists a possibility for the conversion of white adipose tissue into brown adipose tissue. One study highlighted that 66g of brown adipose tissue has the potential to burn approximately 4 Kg of white adipose tissue. Therefore, increasing the mass of brown adipose tissue emerges as a promising strategy for weight reduction and the prevention of type 2 diabetes in the future.
In addition to these findings, the importance of exercise cannot be emphasized. Physical exercise offers numerous benefits, including weight reduction, enhanced fitness, and improved cardiorespiratory capacity, and plays a significant role in the prevention and management of obesity and type 2 diabetes. Additionally, exercise also offers protective benefits against senile dementia. The cyclical process of muscle contraction and relaxation during exercise stimulates myocytes to release various myokines. The cycle of muscle contraction and relaxation during
Abstract 57
SE1-3
exercise stimulates myocytes to release various myokines. Research has indicated that some of these myokines are associated with the apoptosis and regeneration of β cells. Among these myokines, irisin has garnered considerable attention. Irisin, which is cleaved from FNDC5 in myocytes, is secreted into the circulation during physical activity. It is believed to facilitate the conversion of white adipose tissue into brown adipose tissue. Furthermore, numerous studies have also indicated that irisin contributes to the apoptosis and regeneration of β cells.
Understanding the complex interactions between adipose tissue, myokines, and their role in metabolic disorders is essential for developing effective strategies for the prevention and management of obesity and type 2 diabetes. The transformation of white to brown adipose tissue and the secretion of beneficial myokines through exercise are promising areas for further research.
Annual Meeting of the Endocrine Society and the Diabetes Association of the R.O.C. (Taiwan) The45 th 58 March 23-24, 2024
SE2-1
ENDOCRINOLOGISTS' EXPERIENCES IN RESEARCHING AND DEVELOPING ARTIFICIAL INTELLIGENCE FOR THYROID ULTRASOUND IMAGING
內分泌醫師在人工智慧應用於甲狀腺超音波影像的研發經驗
WAI-KIN CHAN
陳維健
DivisionofEndocrinologyandMetabolism,ChangGungMemorialHospital,Taoyuan,Taiwan 林口長庚紀念醫院內分泌暨新陳代謝科
Artificial intelligence (AI) is a key technology in the on-going personalization and development of precision medicine. Deep learning algorithms are increasingly being used to facilitate the detection and diagnosis of tumors. In the future of endocrinology, clinicians would be able to diagnose thyroid cancer more easily by combining ultrasound with AI. Several AI models have been developed worldwide for clinical applications. As clinical physicians, we have a deeper understanding of the current unmet needs and areas where AI can assist in our daily work. Challenges such as data collection and image labelling are often encountered in the development of ultrasound imaging. In this presentation, I will share insights into the development process of AI, as well as future trends and discoveries.
Abstract 59
SE2-2
ACER MEDICAL: FROM INNOVATION TO IMPLEMENTATION
宏碁智醫:從創新到落地
ALLEN (CHIA EN) LIEN
連加恩
Acer Medical
宏碁智醫股份有限公司
Acer Medical, a subsidiary of Acer, leverages artificial intelligence, extensive clinical datasets, and software development capabilities in its operations. Acer Medical remains committed to make AI work for the core needs of humanity by applying AI in healthcare, such as precision medicine, preventive medicine and public health. The company has successfully introduced four medical equipment products, with three of them representing AI image interpretation solutions. Achieving regulatory approvals from both Taiwanese and international regulatory authorities, Acer Medical adheres to the ISO 13485 quality system, meeting rigorous global standards.
Aligned with the prevailing global trend in artificial intelligence, Acer Medical's flagship product, VeriSee DR, is an AI-assisted diagnostic software designed for diabetic retinopathy (DR) within the field of ophthalmology. This innovative solution identifies high-risk DR patients through its core AI model, which has been meticulously trained using images annotated by retina specialists. The software's efficacy has been validated through a pivotal clinical trial against stringent clinical reference standards. Employing advanced AI deep learning techniques, VeriSee DR yields diagnostic results comparable to those of professional ophthalmologists, boasting a screening accuracy of 93% on referral recommendations.
Acer Medical remains committed to ongoing collaborative research with its partners, dedicated to ensuring that intelligent and human-centric medical care remains accessible on a global scale.
Annual Meeting of the Endocrine Society and the Diabetes Association of the R.O.C. (Taiwan) The45 th 60 March 23-24, 2024
SE2-3
HEALTH2SYNC AND ITS VISION OF THE FUTURE IN DIGITAL DIABETES CARE
從智抗糖經驗,展望數位糖尿病照護未來
ED (CHU-YIE) DENG
鄧居義
Co-Found&CEO,Health2Sync
共同創辦人暨執行長
Health2Sync provides a comprehensive disease-management platform starting with diabetes and started branching out to CKD and CVD. Its products combine mobile, cloud, and data analytics, enabling patients to obtain personalized care and allowing healthcare providers (HCPs) and families to care for patients in real-time.
Health2Sync was founded in Taiwan in 2013 and started by providing a simple digital utility to patients and HCPs. In August 2023, it was recognized by the National Development Council and a panel of judges as one of the 13 NextBig startups in Taiwan. Over the years, as it earned the trust of patients and HCPs, the company started to develop and provide features and analytics and became an integral part of the patient journey in battling diabetes. It now has over 110 employees and its digital service spans across Taiwan, Japan, United States, Egypt, Kingdom of Saudi Arabia, Korea, Singapore, and Australia.
With the largest network of clinics and hospitals it digital deployed, Health2Sync has become Asia’s leading solution that delivers an effective and scalable solution for diabetes management. In Asia alone, there are over 600 HCPs that utilize Health2sync’s web-based solution. In November 2023, Health2Snc received TFDA approval of what is Taiwan’s first digital therapeutic, an App based solution prescribed by doctors aiming to assist insulin using patients achieve glucose control in the shortest timeframe while minimizing the risk of hypoglycemia. As of March 2024, Health2Sync has over 1.3 million registered users worldwide. Its strategic partners include Abbott, Novonordisk, and Sanofi, just to name a few. The company continues to leverage latest technology innovation in delivering access, knowledge and scalability with the goal of improving patient outcomes and reducing healthcare burden.
Abstract 61
THE IMPACT OF EXERCISE ON THE ENDOCRINE SYSTEM
運動對內分泌的影響
TZU-JUNG FANG
方姿蓉
1SchoolofMedicine,CollegeofMedicine,KaohsiungMedicalUniversity,Taiwan; 2DivisionofEndocrinology andMetabolism,DepartmentofInternalMedicine,KaohsiungMedicalUniversityHospital,Taiwan; 3Division of GeriatricsandGerontology,DepartmentofInternalMedicine,KaohsiungMedicalUniversityHospital,Taiwan 1 高雄醫學大學醫學院醫學系;2 高雄醫學大學附設中和紀念醫院內科部內分泌暨新陳代謝科;3 高雄醫 學大學附設中和紀念醫院內科部老年醫學科
We will talk about how exercise influences hormone levels, the effects of hormone abuse in sports, and the complex interactions between physical activity and the endocrine system. Physical activity and exercise play a crucial role in modulating the synthesis and secretion of hormones such as growth hormone, ghrelin, testosterone, cortisol, and thyroid hormones. The effects of physical activity on these hormones can vary depending on the type, intensity, and duration of the activity, as well as individual factors like fitness level and nutritional status. A combination of factors including exercise intensity, fitness level, nutritional status, time of day, hydration, age, gender, environmental conditions, and psychological factors can influence how the endocrine system responds to exercise. Understanding these factors is crucial for optimizing the hormonal benefits of physical activity and promoting overall health and performance. Hormone abuse in sports can have detrimental effects on long-term health, affecting cardiovascular health, endocrine function, liver function, reproductive health, mental well-being, musculoskeletal integrity, and metabolic balance. It is essential to raise awareness about the risks associated with hormone abuse and promote safe and ethical practices in sports to safeguard the health and well-being of athletes.
Annual Meeting of the Endocrine Society and the Diabetes Association of the R.O.C. (Taiwan) The45 th 62 March 23-24, 2024
SE3-1
EFFECT OF PHYSICAL ACTIVITY ON MUSCULOSKELETAL SYSTEM
運動對於肌肉骨骼系統之效益
DER-SHENG HAN
韓德生
DepartmentofPhysicalMedicineandRehabilitation,NationalTaiwanUniversityHospitalBeihuBranch,Taipei, Taiwan
臺大醫院北護分院復健科
Many studies describe exercise programs for the treatment and prevention of sarcopenia, osteoporosis and their complications. The characteristics and principles upon which exercise studies are based for increasing muscle mass and improving BMD. Multiple component training focused on resistance training are recommended for sarcopenia; progressive resistance training, weight-bearing impact training, and functional balance training are suggested for osteoporosis. This speech summarizes evidence on the preventive and therapeutic effect of exercise on the musculoskeletal system.
Abstract 63
SE3-2
ENDOCRINE ADAPTATION IN ATHLETES AND RELATIVE ENERGY DEFICIENCY SYNDROME (RED-S)
運動員的內分泌適應和相對能量缺乏症候群
WEN-YA MA
馬文雅
Divisionofendocrinologyandmetabolism,InternalMedicine,CardinalTienHospital,NewTaipeiCity 天主教耕莘醫院新店總院內分泌科
Exercise represents a stress paradigm in which many regulatory endocrine systems are involved to achieve homeostasis. The HPA axis response to resistance exercise depends on the intensity and volume of the exercise. The hypothalamic-pituitary-gonadal (HPG) axis is essential for adequate responses to exercise and training both acutely and chronically. Both testosterone and estrogen play leading roles in neuromuscular adaptation to exercise in males and females. These endocrine adaptive responses may be either beneficial or harmful in case they exceed a certain threshold.
Relative Energy Deficiency in Sport (REDs) was first introduced in 2014 by the International Olympic Committee’s expert writing panel, identifying a syndrome of deleterious health and performance outcomes experienced by female and male athletes exposed to low energy availability (LEA; inadequate energy intake in relation to exercise energy expenditure). An imbalance caused by low energy availability due to a restrictive diet, eating disorders or long periods of energy expenditure leads to multisystemic deregulation favoring the essential functions of the body. This phenomenon, described as the female athlete triad, occurs in a considerable percentage of high-performance athletes, with harmful consequences for their future.
The objective is to promote the acquisition of more consolidated knowledge on an undervalued theme, enabling the acquisition of preventive strategies, early diagnosis and/or appropriate treatment.
Annual Meeting of the Endocrine Society and the Diabetes Association of the R.O.C. (Taiwan) The45 th 64 March 23-24, 2024
SE3-3
THE PREDICTION OF INCRETIN EFFECT THROUGH THE DIFFERENTIALLY METHYLATED REGION (DMR) IN GENOMIC DNA
透過基因組 DNA 差異甲基化區域 (DMR) 預測腸泌素反應
CHIA-HUNG LIN
林嘉鴻
DepartmentRadiationOncology,Lo-TungPohaiHospital,YilanCounty,Taiwan
林口長庚醫院內科部新陳代謝科,長庚大學醫學院
In patients with poorly controlled type 2 diabetes, incretin therapies are clinically used and treated with other hypoglycemic agents. Incretin is known to be associated with blood glucose control. But the clinical effect is not the same for every patient. Further studies have found that differentially methylated regions (DMRs) in the promoter of VTRNA2-1 gene play a role in glucose control and clinical response of incretin therapy in patients with type 2 diabetes.
In the genome-wide methylation analysis, a hypomethylation state (< 40%) over the VTRNA2-1 promoter region is closely linked to GLP-1 analogue non-responsiveness. VTRNA2-1 is an RNA polymerase III-transcribed, noncoding RNA that is 101 bp in size. The VTRNA2-1 has been shown to be modulated by its promoter methylation and could be induced by TGF-β1. It can bind to Dicer to inhibit miRNA maturation and subsequently suppress the miRNA pathway in other therapeutic drug resistance study. The clinical application of screening DMRs near VTRNA2-1 may be able to identify the patients who would be non-responsiveness to GLP-1 analogues before starting treatment. This would be helpful to avoid the ineffective use of this expensive drug in the current era of precision therapy for patients with T2DM.
Abstract 65
SE4-1
EFFECTS OF ANTIDIABETIC MEDICATION ON BONE HEALTH IN TYPE 2 DIABETES
JEONGHOON HA, M.D., PH.D.
SeoulStMary’sHospital,TheCatholicUniversityofKorea
Osteoporosis, a systemic skeletal disease marked by reduced bone mass and the deterioration of bone microarchitecture, leads to increased bone fragility and a higher risk of fractures. Its prevalence is on the rise worldwide, partly due to the aging population, resulting in significant socioeconomic impacts. There is a well-established link between diabetes and osteoporosis. Type 1 diabetes, in particular, acts as a significant secondary cause, leading to lower bone mass and higher fracture rates than those found in the healthy population. Interestingly, individuals with Type 2 diabetes mellitus (T2DM) often present with normal or even increased bone mineral density (BMD) at the lumbar spine and hip. However, they face a greater risk of fragility fractures, a risk compounded by factors such as the duration of diabetes, the presence of diabetes-related complications, specific antidiabetic medications, and a higher frequency of falls.
The impact of antidiabetic medications on fracture risk varies. For example, peroxisome proliferator-activated receptor γ agonists are known to increase fracture risk, while sodiumglucose cotransporter 2 inhibitors (SGLT2i) like canagliflozin may decrease BMD and heighten fracture risk. This is not the case with dapagliflozin or empagliflozin, which seem not to negatively influence bone density or fracture rates. Conversely, metformin and sulfonylureas exhibit a neutral impact on bone health, and incretin-based treatments might actually benefit it.
Research to date has primarily focused on the effects of single drugs or their comparison to a placebo. Yet, in practical clinical settings, it’s common to employ combinations of antidiabetic agents with diverse mechanisms to manage blood glucose levels, revealing a research gap in the effects of combined antidiabetic therapies, such as gemigliptin and empagliflozin, on bone metabolism. This presentation aims to outline the effects of various diabetes medication regimens on bone metabolism, addressing a critical area of need in understanding the complex interplay between diabetes management and bone health.
Annual Meeting of the Endocrine Society and the Diabetes Association of the R.O.C. (Taiwan) The45 th 66 March 23-24, 2024 SE4-2
SE4-3
CONNECT THE EXPLORATION OF REGIONAL ADIPOCYTE
BIOLOGY TO CLINICAL SIGNIFICANCE: MY POINT OF VIEW AS AN ENDOCRINOLOGIST AND PHYSICIAN SCIENTIST
探索局部脂肪細胞生物學功能並與臨床運用進行連結:我作為內
分泌學家和醫師科學家的觀點
FENG-CHIH KUO
郭俸志
DivisionofEndocrinologyandMetabolism,DepartmentofInternalMedicine,Tri-ServiceGeneralHospital, Taipei,Taiwan.
三軍總醫院內科部內分泌暨新陳代謝科
Human body fat distribution has been well-recognized as an import surrogate for assessing cardio-metabolic risks. Central fat accumulation represents an insulin-resistant and inflammatory phenotype that considerably raises the risk of diabetes, cardiovascular diseases, and cancers. However, the mechanisms governing human body fat distribution and regional adipocyte biology are still poorly understood. My research during Ph.D. degree has pointed out HOTAIR as a long non-coding RNA possesses important epigenetic regulation on regional adipocyte development and biology. Our recent work further identifies HOTAIR can conduct abdominal specific anti-adipogenesis through remodelling global methylation and transcription. Besides, we also identified infrapatellar fat pad (IFP) as an unique fat depot possessing differential HOTAIR expression and IFP-derived dedifferentiated fat cells could serve as superior cell material for cartilage differentiation and adipogenesis. Via utilizing Dual-energy X-ray absorptiometry, bioelectric impedance analysis, grip strength, skinfold measurements with collection of blood samples, we are currently aiming to build up an inhouse system merging clinical work and laboratory experiments. Till now, we have generated some intriguing data to support the clinical utilization of skinfold measurements for evaluating the cardiovascular and osteoporotic risks in diabetic patients.
Abstract 67
EXPLORING STEROIDOGENESIS FOR CHARACTERIZATION OF ADRENAL DISORDERS
MAN-HO CHOI, PHD
CenterforAdvancedBiomolecularRecognition,KoreaInstituteofScienceandTechnology,Seoul,Republicof Korea
The adrenal glands play a key role in the endocrine system and are responsible for producing steroid hormones that regulate various endocrine processes in the body. Exploring steroidogenesis is crucial for understanding the normal functioning of the adrenal glands and, especially, diagnosing adrenal diseases.
The conventional diagnosis of adrenal diseases, such as adrenal incidentalomas and congenital adrenal hyperplasia (CAH), typically involves a laborious workup and may face limitations in distinguishing between subtypes. Specific subtypes of adrenal tumors and CAH can exhibit distinctive characteristics through abnormal enzyme functions responsible for altered steroidogenesis. Therefore, our studies aimed to discriminate adrenal tumors and various hydroxylase deficiencies (OHDs) in CAH from a single blood sample using liquid chromatography-mass spectrometry with or without the integration of machine learning algorithms.
Variations in serum levels of adrenal steroids were noted among various adrenal tumors, encompassing adrenal Cushing’s syndrome, non-functioning adrenal adenoma, and primary aldosteronism, when compared to one another. Remarkably elevated serum levels of individual steroids and metabolic ratios, indicative of enzymatic activities associated with impaired steroidogenic enzymes, were observed in the CAH subtypes of 21-OHD, 17α-OHD, and 11β-OHD. Despite the limited number of patients in both the 17α-OHD and 11β-OHD groups, these methodologies are poised to enhance the precision of diagnosing different CAH subtypes.
The metabolic signatures of steroid in adrenal disorders with proposed individual steroids and their metabolic ratios hold significant value for the comprehensive assessment of various adrenal disorders in clinical practice, all within a single run. Here are a few examples why exploring steroidogenesis is important and the knowledges is essential for maintaining hormonal balance and overall health in individuals with adrenal disorders.
Annual Meeting of the Endocrine Society and the Diabetes Association of the R.O.C. (Taiwan) The45 th 68 March 23-24, 2024 SE4-4
SE5-1
DEAL WITH PITUITARY DISORDER
內分泌人如何看腦垂體疾病
CHING-LING LIN
林慶齡
Divisionof EndocrinologyandMetabolism,CathayGeneralHospital,Taipei,Taiwan
國泰醫院內分泌新陳代謝科
大綱:
1)天方夜譚
2)非戰之罪
3)先畫靶再射箭
4)大衛對巨人
5)善用老二哲學
6)基隆東岸事件
7)地表板塊遷移
8)莫作諸葛亮
Abstract 69
INTERACTION BETWEEN PITUITARY TUMOR IMAGING AND NEUROSURGEON
腦下垂體腫瘤影像與神外醫師的對話
CHENG-CHI LEE
李丞騏
BrainTumorDivision,DepartmentofNeurosurgery,ChangGungMemorialHospitalatLinkou 林口長庚醫院腦腫瘤神經外科
Surgical intervention remains primary treatment choice in most pituitary adenomas, especially non-functioning adenomas exerting mass effect and functioning adenomas, except prolactinoma. Magnetic resonance imaging (MRI) is the most suitable diagnostic tool. Preoperative careful radiographic interpretation in tumor characteristics and invasion status is the most crucial step in achieving grossly total resection and avoiding complications.
Tumor size or diameter was most used to describe the mass effect on surrounding structures, however it lacks precise evaluation because of 2-dimensional measurement compared with volumetric method. Furthermore, more scientific volumetric measurement method is especially useful when lesions are irregularly shaped or when treatment is determined exclusively based on the tumor volume.
Knosp grading and Hardy classification are the most adapted system to evaluate tumor invasion status. Higher grade invasion status impedes complete surgical resection and endocrinologic outcome. Careful appreciation of neurovascular structures during removing tumor pieces is the key to promising neurologic and endocrinologic outcomes. Besides, by applying quantitative T2-weighted MRI analyses may provide a potential marker for response to somatostatin analogs in newly diagnosed GH-secreting pituitary adenomas.
In conclusion, careful radiographic evaluation not only provide thorough understanding of tumor characteristics during operation but also treatment responses in some functioning tumors. As a result, improve treatment outcomes of patients with pituitary adenomas.
Annual Meeting of the Endocrine Society and the Diabetes Association of the R.O.C. (Taiwan) The45 th 70 March 23-24, 2024
SE5-2
SE5-3
CURRENT APPLICATION OF ARTIFICIAL INTELLIGENCE IN PITUITARY GLAND AND ITS FUTURE: EXPERIENCE OF TAIPEI
VETERANS GENERAL HOSPITAL
未來可以靠人工智慧嗎 ?
KAI-WEI YU
游鎧蔚
DepartmentRadiology,TaipeiVeteransGeneralHospital,Taiwan
臺北榮民總醫院放射線部
The pituitary gland plays a crucial role in the neuroendocrine system, overseeing various physiological functions. In recent years, the rapid development of artificial intelligence (AI) technology has provided new opportunities for neuroscience and medical research. This talk will mainly focus on update of current status in the field of pituitary AI and the perspective from a radiologist.
AI has demonstrated outstanding potential in the assisting diagnosis and treatment of pituitary gland diseases. Using machine learning algorithms, it is possible to more accurately analyze imaging, anatomy, and clinical data, improving the efficiency of early detection and personalized treatment of pituitary gland diseases. However, developing AI required massive needs of annotation, anatomical identification was also complicated surrounding pituitary region. There are even more obstacles in generalized pituitary AI into clinical application due to heterogeneity of data base and higher standard of patient privacy.
Research related to the pituitary gland has made significant progress with the push of artificial intelligence, offering new perspectives and possibilities for our understanding of the neuroendocrine system and the treatment of associated diseases. In the future, with the continuous evolution of AI technology, it is believed that innovative applications will be further deepen but needs cross-institution cooperation.
Abstract 71
BENIGN NON-THYROID CYTOMORPHOLOGY NOTED IN THYROID ASPIRATION
YU-HSIN CHEN
陳瑜忻
國泰醫院內分泌新陳代謝科
Divisionof EndocrinologyandMetabolism,CathayGeneralHospital,Taipei,Taiwan
Fine needle aspiration cytology is important for diagnosing thyroid nodule. There are some non-thyroid finding either benign or malignancy noted by cytology. In this section, we will discussion cases of the benign non-thyroid cytomorphology finding including ciliated bronchial mucosal cells, esophageal diverticulum, intrathyroid parathyroid adenoma. Besides intrathyroid findings, hypoglossal duct cyst and bronchial cleft cyst were 2 benign finding out of thyroid gloand discovered by neck ultrasound.
Annual Meeting of the Endocrine Society and the Diabetes Association of the R.O.C. (Taiwan) The45 th 72 March 23-24, 2024
SE6-1
CYTOMORPHOLOGY FOR METASTATIC TUMORS OF THE THYROID
甲狀腺轉移性腫瘤的細胞形態學
I-SHIOW JAN
詹一秀
DepartmentofLaboratoryMedicine,NationalTaiwanUniversityHospital,Taipei,Taiwan
臺大醫院檢驗醫學部
Fine needle aspiration (FNA) cytology of the thyroid is a reliable diagnostic tool for the evaluation of patients with thyroid nodules. It is for the detection of primary thyroid neoplasm, but uncommon metastatic malignancy to the thyroid is important to recognize in the daily cytological practice. The frequency of metastatic tumors to the thyroid varies between 2.7% and 4.0%. The most common metastatic tumors to the thyroid are cancers of the lung, breast, colon, and kidney. Clinical history and radiologic correlation are very helpful in distinction from a primary thyroid neoplasm. The cytomorphology of metastatic tumors to the thyroid by FNA of the thyroid will be presented.
Abstract 73
SE6-2
THE 2023 BETHESDA SYSTEM FOR REPORTING THYROID CYTOPATHOLOGY
2023 BETHESDA 甲狀腺細胞病理報告系統介紹
CHIH-YI LIU
劉之怡
DivisionofPathology,SijhihCathayGeneralHospital,NewTaipeiCity,Taiwan
汐止國泰綜合醫院病理科
The 2023 Bethesda System for Reporting Thyroid Cytopathology (TBSRTC) is an updated, standardized system for categorizing thyroid fine needle aspirations, building on its previous editions since 2010. The third edition introduces several key updates, most notably the assignment of a single name for each of the six diagnostic categories: nondiagnostic, benign, atypia of undetermined significance, follicular neoplasm, suspicious for malignancy, and malignant. Each category now comes with an updated average risk of malignancy (ROM), refined from data since the second edition. The system has simplified the subcategorization of atypia of undetermined significance into two subgroups based on ROM and molecular profiling. New additions include a discussion on pediatric thyroid disease, updated nomenclature to align with the 2022 World Health Organization Classification of Thyroid Neoplasms, and two new chapters addressing molecular and ancillary testing in thyroid cytopathology, and clinical perspectives and imaging findings in thyroid disease . These enhancements aim to provide more accurate diagnostics and clearer communication between cytopathologists and clinicians.
Annual Meeting of the Endocrine Society and the Diabetes Association of the R.O.C. (Taiwan) The45 th 74 March 23-24, 2024 SE6-3
ADVANCES IN SYSTEMIC TREATMENT OF NEUROENDOCRINE TUMORS
神經內分泌瘤之治療進展
HUI-JEN TSAI
蔡慧珍
NationalInstituteofCancerResearch,NationalHealthResearchInstitutes
國家衛生研究院 / 癌症研究所
Neuroendocrine tumors (NETs) are heterogenous tumors with different grade and of different primary sites. The most common sites of NETs include gastroentero-pancreas (GEP) and lung. Early-stage NETs can usually be cured by surgical resection. However, advanced NETs have relatively poor survival. The treatment for advanced NETs is still an unmet medical needs. Somatostatin analogues (SSA), everolimus (mTOR inhibitor), and sunitinib have been shown to improve the survival and quality of life of functional or advanced GEPNET patients by phase II/III trials in the recent decades. Everolimus has also been shown to improve the survival of lung NETs by phase III clinical trial. Other target agents, such as surufatinib, lenvatinib, axitinib, pazopanib, and cabozantinib have also been shown their efficacy in advanced GEP-NETs in phase II or III clinical trials. Cabozantinib has been shown to prolong the progression free survival of GEP-NET patients who failed one line of targeted agents than placebo control by randomized phase III study published in 2023. In addition to single agent use, combinational treatment is also a treatment option. The efficacy of everolimus combined with SSA has also evaluated in clinical trials. Combination of target agent with chemotherapeutic agent may also be a treatment option. Exploration of other novel targeted agents or combinations is still ongoing not only to prolong the survival but also maintain the quality of life of advanced NET patients.
Abstract 75
SE7-1
UPDATE OF FUNCTIONING PANCREATIC NEUROENDOCRINE TUMOR
功能性胰臟神經內分泌腫瘤之最新進展
LIANG-YU LIN
林亮羽
DivisionofEndocrinologyandMetabolism,TaipeiVeteransGeneralHospital,Taipei,Taiwan
臺北榮民總醫院內分泌新陳代謝科
Pancreatic neuroendocrine tumors (pNETs) are a rare group of neoplasms that arise from multipotent stem cells in the pancreatic ductal epithelium. Although they comprise only 2% to 4% of pancreatic cancers, several data showed the incidence is increased in the past 30 years. Most pNETs are nonfunctioning, but they can secrete various hormones resulting in unique clinical syndromes and may be undetected for years without obvious signs or symptoms. Insulin, gastrin and glucagon are three common hormones secreted from pNETs. Complicated screening tests for functioning pNETs are major challenges for endocrinologists. pNETs are often advanced at the time of diagnosis and is a progressive disease. Outcomes in patients with locally inoperable or metastatic pNETs are poor, survival is also associated with tumor grade. Diagnosing pNETs requires the systematic approach. History taking and physical examination are essential and biochemical markers are useful. Imaging studies, CT scan, MRI, PET scan and somatostatin‐receptor scintigraphy (Octreoscan) can be used. Arterial stimulation venous sampling for insulin and gastrin is a helpful invasive tool for functional localization of pNETs. Somatostatin receptor analogues showed symptomatic, biochemical and disease control. Targeted agents such as everolimus and sunitinib also showed benefit for advanced pancreatic NETs. Other treatments including peptide receptor radionuclide therapy (PRRT), hepatic regional therapy for liver metastases (arterial embolization, chemoembolization), or ablative therapy can be used. Chemotherapy, such as streptozotocin, 5‐fluorouracil, doxorubicin, dacarbazine, etoposide, cisplatin, temozolomide, capecitabine is another option for the treatment of pNETs. In addition, hormone control of malignant pNETs should be considered for patient’s quality of life and mortality. In conclusion, pNETs are no longer rare disease. Clinicians must be aware of the diverse manifestations of this disease, as the key step
Annual Meeting of the Endocrine Society and the Diabetes Association of the R.O.C. (Taiwan) The45 th 76 March 23-24, 2024 SE7-2
to management of these tumors is to first suspect the diagnosis. The management of patients with a functioning Pan-NET syndrome is complex due to its heterogeneous presentation and multisystem involvement. Consequently, work-up and treatment of a (suspected) functioning syndrome should preferably be performed in a multidisciplinary setting and discussed in expert tumor boards.
Abstract 77
CLINICAL SIGNIFICANCE OF MEN1 GENE
MEN1 基因的臨床意義
SHYANG-RONG
SHIH
施翔蓉
NationalTaiwanUniversityCollegeofMedicine,DepartmentofInternalMedicine;NationalTaiwanUniversity Hospital,DepartmentofEndocrinologyandMetabolism
臺灣大學醫學系內科;臺大醫院代謝內分泌科
Characteristics of the pituitary tumors (PITs) in multiple endocrine neoplasia type 1 (MEN1) have changed after screening program suggested by new guidelines. Comparisons of the patients with different MEN1 mutation status has not been comprehensively analyzed. To assess characteristics of patients with MEN1 and PITs and to compare the characteristics between different MEN1 mutation status, we reviewed the medical records of MEN1 patients in National Taiwan University Hospital in 2010-2023 to analyze. We finally included 42 MEN1 patients. Among them, PITs were diagnosed in 24 patients. The PITs of three patients were invasive and managed with transsphenoid surgery. During follow-up, only one PIT enlarged. Median ages at MEN1 diagnosis were older in patients with PITs when compared to those without PITs (p=0.044). MEN1 mutations were identified in 57.1% of patients who received genetic study. Five novel mutations were found. Among MEN1 patients with PITs, more organs in MEN1 diagnostic criteria (hyperparathyroidism, PITs and gastro-intestinalpancreatic neuroendocrine neoplasia (GEP-NEN)) were affected in patients with MEN1 mutation (mutation+/PIT+ group) than in patients without MEN1 mutation (mutation-/PIT+ group) (p=0.005). The most common GEP-NEN was insulin-secreting in mutation-/PIT+ group, and was non-functional in mutation+/PIT+ group. The incidence of adrenal tumor was higher in mutation+/PIT+ group than in the mutation-/PIT+ group (p=0.011). Median age at initial manifestation of MEN1 was younger in mutation-/PIT+ group than in mutation+/PIT+ group (p=0.049). This is the first study comparing the characteristics of patients with MEN1 and PITs harboring different mutation status. Patients with MEN1 mutation tended to have more organ involvement and might be feasible to receive more intensive follow-up.
Annual Meeting of the Endocrine Society and the Diabetes Association of the R.O.C. (Taiwan) The45 th 78 March 23-24, 2024
SE7-3
SE8-1
OSTEOPOROSIS IS AN IMPORTANT ENDOCRINE DISORDER FOR ENDOCRINOLOGISTS
內分泌科醫師在代謝性骨病 / 骨鬆症的重要性
KEH SUNG TSAI
蔡克嵩
DepartmentofInternalMedicineandEndocrinology,NationalTaiwanUniversityHospitalandFarEastern Polyclinic,Taipei
臺大醫院內科與遠東聯合診所
Taiwanese showed the highest osteoporotic fracture rate in Asia. The incidents are still increasing because of the rapid increase of the elderly population. This trend was foreseen by my late tutors in the university hospital. Thus I had the opportunity to study osteoporosis at the Mayo Clinic for 2 years with Prof. Riggs 1981 to 1983. In these years I attended and saw the growth of ASBMR, which is still the main academic society of metabolic bone diseases and osteoporosis of the world. ASBMR separated from the Endocrine Society in 1977, just like ADA did in 1940, implying that these societies are all part of the endocrinology family.
Metabolic bone diseases are the results of dysfunction of bone cells. While osteoporosis is the most common metabolic bone disease, it is the result of hyper-function of osteoclasts and/or hypo-function of the osteoblasts. This is a situation just like the hyperthyroidism and hypercorticoidism that we see in every day clinical practice. We as endocrinologists are able to handle them easily. On the other hand, metabolic bone diseases often are caused by other primary endocrine disorders such as hyperparathyroidism, hyperthyroidism or hypercorticoid syndromes, that need an endocrinologist to do screening work-up for secondary causes.
In the past 25 years, the National Health Insurance Program has provided a reliable clinical database. Based on this, physicians and surgeons in Taiwan have published many important articles in the famous bone journals with high Impact Factor scores. This advantage will persist for many more years to come.
In clinical business sense, the setting up of an osteoporosis clinic is relatively simple. The medical education programs are available, The case management teams are readily available
Abstract 79
because it can be the same team for the DM patients. Furthermore, DXA BMD measurement will be provide free of charge for the elderlies in some cities of Taiwan . The reimbursement will be more comprehensive soon, to cover Colle’s fracture and humoral fractures. The changes will increase the patient flow to the practicing endocrinologists.
Endocrinologists are quite busy in Taiwan, seeing mostly patients with DM or thyroid disorders. DM, thyroid, parathyroid, adrenal, gonadal disorders are all interesting and worth a life long devotion to study and practice. The fact is that in the elderlies, osteoporosis is a far more common disease than DM and thyroid disorders. Osteoporosis fractures can be fatal, and its management protocols are mature and solid. After all, osteoporosis and other related metabolic bone diseases need the participation and devotion of the young Endocrinologists in Taiwan.
Annual Meeting of the Endocrine Society and the Diabetes Association of the R.O.C. (Taiwan) The45 th 80 March 23-24, 2024
CHALLENGES FACED BY EARLY CAREER RESEARCHERS
年輕學者生涯規劃面臨的挑戰
PEI-WEN WANG
王佩文
KaohsiungChangGungMemorialHospital,ChangGungUniversityCollegeofMedicineKaohsiung,Taiwan 高雄長庚醫院暨長庚大學醫學院
Personal factors affecting career paths include the desire for meaningful work, career satisfaction, work-life balance, spending time with family, working in a preferred location, and finances.
To thrive in a medical center, younger doctors need to be an academic physician. Early-career researchers (ECR) need a navigator and mentor to provide guidance about the relevance and context of their research, and affinity groups to organize social and professional development events together. Furthermore, they need to establish collaborations between basic scientists and clinical researchers to facilitate translational research projects. Researchers frequently define ‘success’ by traditional metrics including the number of papers produced, journal impact factors, total citations, and amount of funding obtained. These metrics highlight the reality of ‘publish or perish’. When institutions look to recruit and promote individuals, they look at CVs, and there is tremendous pressure to fill up ones CV with publications. Often, the publications that come forward are rushed and do not always move the field forward or really help advance patient care.
We encourage ECR to practice independent scrutiny of clinical material that surrounds them and to find questions that should be asked. ECR may be encouraged to “think out of the box” and start from important but overlooked aspects of research and open the door to new areas. Each new generation of researchers face unique challenges in comparison with more senior colleagues. The pace of change appears to have accelerated, and the breadth of research areas has expanded significantly and become more multidisciplinary. ECR need to connect with leaders or mentors outside of their home institutions and attend and present in congress meetings to gain a broader international impact.
Abstract 81
SE8-2
Every individual’s career path, circumstances and goals are unique. Key concepts can be applied to help ECR navigate their career. We suggest networking and making friends, taking opportunities that arise, setting goals, investing time wisely, building resilience, and not being afraid to ask questions. ECR are the future of science and medicine. To support them is to advance our field.
Annual Meeting of the Endocrine Society and the Diabetes Association of the R.O.C. (Taiwan) The45 th 82 March 23-24, 2024
CHOOSE WHAT YOU LOVE, AND LOVE WHAT YOU CHOOSE
擇你所愛愛你所擇
PEI-LUNG CHEN
陳沛隆
DivisionofEndocrinologyandMetabolism,DepartmentofInternalMedicine,DepartmentofMedicalGenetics, NationalTaiwanUniversityHospital,Taiwan,GraduateInstituteofMedicalGenomicsandProteomics,National TaiwanUniversity,Taiwan
臺大醫院內科部新陳代謝科,臺大醫院基因醫學部,臺灣大學基因體暨蛋白體醫學研究所
Being a medical professional in the field of endocrinology and metabolism, it is with great appreciation that I acknowledge the rich resources, unique capabilities, and growthoriented mindset our profession provides. Throughout various stages of our careers, we are presented with a spectrum of choices. There is no single best choice. Each individual’s selection is influenced by their own set of priorities, which may include personal wellbeing, familial commitments, clinical responsibilities, teaching, research, and more.
In my upcoming presentation, I intend to narrate the trajectory of my professional life over the past 25 years. A significant portion of this discourse will be devoted to my investigative forays into research possibilities, my sojourn overseas for doctoral studies, the deliberations involved in choosing my area of research, and ultimately, establishing a conducive environment that integrates clinical practice, education, and scholarly inquiry. Furthermore, I will take the opportunity to express my profound thanks to the numerous mentors and collaborators who have been instrumental in my journey. It is of paramount importance to recognize what we really love. It is a blessing to continue to love what we choose.
Abstract 83 SE8-3
ROLES OF ELECTRONEGATIVE LIPOPROTEINS IN CARDIOVASCULAR DISEASES: FROM CLINIC TO BENCH
CHU-HUANG (MENDEL) CHEN, MD PHD
The Texas Heart Institute
Given that aggressive lipid-lowing, with a focus on reducing plasma low-density lipoprotein cholesterol (LDL-C) concentrations, does not eradicate atherosclerotic cardiovascular disease (ASCVD), an old question revolving around the identification of “culprit atherogenic LDL entities” remains a hot topic in lipid research and medical practice. Among the candidates, small-dense LDL (sdLDL) and lipoprotein (a) [Lp(a)] have received significant attention. With extensive clinical observations, sdLDL appears to be closely associated with increased ASCVD risks and incidences. However, there is a lack of cell and animal evidence to underscore the mechanics. While Lp(a) is positively correlated with ASCVD and complications, its plasma concentration is mostly determined by genetic predisposition and does not fluctuate with disease occurrence and progression. Therefore, its value for prognostic stratification is limited.
Using anion-exchange chromatography, we have divided LDL into five subclasses, L1 to L5, based on their surface electrical characteristics, with L5 being the most electronegative. Compared with artificially oxidized LDL (oxLDL), L5 is not oxidized in vivo, and its oxidative value is as low as the least electronegative and health-beneficial subclass, L1. However, L5 is as toxic as oxLDL to endothelial cells (ECs) and other vascular cells.
We have further divided LDL into 7 subclasses according to their density ranges, LDL1 to LDL7, and discovered that L5 exists in all the density-defined subclasses, from the most buoyant LDL1 to the small-dense LDL7. Furthermore, careful examination by transmission electron microscope (TEM) revealed that L5 has a diameter similar to that of L1.
Lp(a) is a normal LDL attached to a molecule of apolipoprotein (a) [apo(a)], which, owing to its structural resemblance to plasminogen and tissue plasminogen activator, competes with plasminogen for receptor binding, leading to reduced fibrinolysis. Thorough chemical delineation demonstrates that L5 is also attached to an apo(a) molecule, which may partially explain L5’s prominent thrombogenic effects. However, unlike Lp(a), the LDL in L5 contains
Annual Meeting of the Endocrine Society and the Diabetes Association of the R.O.C. (Taiwan) The45 th 84 March 23-24, 2024 SE9-1
numerous structural changes uncharacteristic of a normal LDL. These changes include the association of apoE, apoCII/III, apoA1 with glycosylation and other posttranslational modifications of these proteins, as well as rich contents of triglycerides (TG) and cholesterol esters. The unique chemical composition of L5 contributes to its electronegativity and atherogenicity.
Because of its electronegativity, L5 is not recognized by the normal LDL receptor (LDLR) but is instead internalized through lectin-like oxidized LDL receptor 1 (LOX-1), which has a strong affinity for a variety of electronegative ligands. In summary, L5 is a TGand apoCIII-rich, apo(a)-containing LDL, distinct from sdLDL, Lp(a), or artificially prepared oxLDL. In a series of publications in well-respected journals, we have demonstrated the atherogenic and thrombogenic properties of L5 both in vitro and in vivo.
Abstract 85
NAVIGATING ANDROGEN-RELATED DISEASES: UNRAVELING ANDROGEN RECEPTOR MECHANISMS FROM BEDSIDE TO BENCH AND BACK AGAIN
雄性激素相關疾病的領航研究-從往返臨床和實驗室之間來闡明 雄性激素受體作用機制
HONG-YO KANG
康宏佑
GraduateInstituteofClinicalMedicalSciences,ChangGungUniversityCollegeofMedicine;Divisionof EndocrinologyandMetabolism,DepartmentofInternalMedicine,KaohsiungChangGungMemorialHospital CenterforHormoneandReproductiveMedicineResearch,DepartmentofObstetricsandGynecology, KaohsiungChangGungMemorialHospital,ChangGungUniversity,CollegeofMedicine,Kaohsiung
長庚大學臨床醫學研究所;高雄長庚紀念醫院內分泌暨新陳代謝科;高雄長庚紀念醫院婦產部荷爾蒙 暨生殖醫學研究中心
Androgens, primarily testosterone and 5α-dihydrotestosterone, exert diverse effects on numerous target organs. Their biological actions are mediated by a ligand-dependent nuclear transcription factor known as the androgen receptor (AR). As a member of the steroid hormone receptor family, the AR plays crucial roles throughout development, aging, and malignant transformation.
Our research interest delves into the landscape of androgen-related diseases, focusing specifically on unraveling the mechanisms of androgen/AR-mediated gene regulatory pathways. Aberrant AR function, resulting from mutations or altered expression levels, has been implicated in the progression of androgen/AR -mediated diseases. Despite intensive research activity in this area, numerous intriguing questions persist regarding the fundamental mechanisms of androgen/AR signaling pathways in androgen-related diseases, such as Spinal and Bulbar Muscular Atrophy (SBMA) and Androgen Insensitivity Syndrome (AIS).
Bridging the gap between clinical observations and bench research, our investigation navigates the complex journey from bedside insights to bench discoveries and back again. Through a comprehensive exploration of androgen/AR actions, we aim to enhance our understanding of the molecular mechanisms underlying androgen-related diseases. Our
Annual Meeting of the Endocrine Society and the Diabetes Association of the R.O.C. (Taiwan) The45 th 86 March 23-24, 2024
SE9-2
translational research encompasses both clinical perspectives and cutting-edge scientific analysis, providing a holistic approach to address the challenges posed by these diseases. This two-way investigation not only sheds light on the fundamental mechanisms of androgen/AR but also explores potential therapeutic implications, paving the way for advancements in both clinical practice and scientific research.
Abstract 87
USING POLYGENIC RISK SCORES TO DIFFERENTIATE T1D AND T2D IN PATIENTS WITH ATYPICAL PHENOTYPES OF DIABETES
JIANFENG XU, MD, DR.PH
PersonalizedMedicine,NorthShoreUniversityHealthSystem(EndeavorHealth),Illinois,U.S.;Universityof ChicagoPritzkerSchoolofMedicine,Illinois,U.S
Diabetes is a complex condition encompassing various types, including Type 1 diabetes (T1D), Type 2 diabetes (T2D), and others. Despite distinct etiologies and clinical presentations for T1D and T2D, accurately classifying diabetes poses challenges in clinical settings, as a large proportion of adult diabetes patients exhibit atypical and overlapping features of both types. Recent advances of genetic studies of diabetes may offer an opportunity to improve the characterization of atypical diabetes patients for appropriate therapy, such as insulin, oral hypoglycemic medications, and lifestyle management
This presentation will delve into the evaluation of two existing polygenic risk scores for diabetes, namely PGST1D and PGST2D, assessing their efficacy in predicting the risk associated with these diabetes types. Furthermore, the discussion will highlight the performance of PGST1D and PGST2D in distinguishing between T1D and T2D among patients exhibiting typical and atypical phenotypes of these conditions. A noteworthy addition to this discussion is the introduction of GenProb-T1D, a novel genetic probability measurement for T1D that integrates both PGST1D and PGST2D. This probability metric was developed based on a study involving 41,787 diabetes patients in the UK Biobank (Billings LK, et al, 2023, PMID: 37560999) and subsequently validated in 3,363 diabetes patients from the Genomic Health Initiative (GHI) cohort at NorthShore.
Lastly, the early implementation experience of PGST1D and PGST2D, as well as GenProb-T1D in a clinical setting at NorthShore will be discussed. This includes the development of a clinical-grade genetic test that is offered by a CLIA-certified commercial testing laboratory, and its integration into the Electronic Health Record (EHR) for seamless test ordering by physicians, comprehensive reporting, and the development of individualized care pathways.
Annual Meeting of the Endocrine Society and the Diabetes Association of the R.O.C. (Taiwan) The45 th 88 March 23-24, 2024 SD1-1
SD1-2
PRECISION MEDICINE IN T2D
第二型糖尿病之精準醫療
WEI-SHIUNG YANG
楊偉勛
GraduateInstituteofClinicalMedicine,CollegeofMedicine,NationalTaiwanUniversity,Taipei,TAIWAN
臺大醫學院臨床醫學研究所
An overview of precision medicine, and precision medicine of diabetes will be first given. After setting the tone, the genomic data of T2D from Taiwan Biobank will be presented in the context precision prevention, diagnosis, treatment, and prognosis. At the end, the existing gaps and future opportunity of precision diabetes medicine will be discussed from both local and global perspectives.
Abstract 89
GAPS AND OPPORTUNITIES FOR CLINICAL TRANSLATION OF PRECISION DIABETES MEDICINE
精準醫學運用於糖尿病臨床治療的不足之處與契機
JUN-SING WANG
王俊興
DivisionofEndocrinologyandMetabolism,TaichungVeteransGeneralHospital,Taichung,Taiwan 臺中榮民總醫院內分泌新陳代謝科
Diabetes is a severe chronic metabolic disorder, which causes many complications including micro- and macro-vascular diseases. These complications have similar risk factors and pathophysiological pathways, with diverse clinical manifestations. Moreover, patients may have different responses to established treatments for diabetes and its complications. Heterogeneous responses to treatment and residual risks among patients with diabetes and its chronic complications remain unsolved issues.
Genetic factors play a role in the variations of clinical presentations and responses to treatment. Explore potential associations between clinical phenotypes and genotypes, and functional mechanisms of diabetic complications related genes may be helpful to implement precision medicine for diabetes management. With the advances in molecular genetics, scientists are able to undertake comprehensive explorations for disease pathogenesis, therapies, and risk models. In this talk, I will briefly review on this topic.
Annual Meeting of the Endocrine Society and the Diabetes Association of the R.O.C. (Taiwan) The45 th 90 March 23-24, 2024
SD1-3
SD2-1
DIABETIC RETINOPATHY AND DIABETIC MACULAR EDEMA: THE OPHTHALMOLOGIST POINT OF VIEW
從眼科醫師的觀點來探討糖尿病視網膜病變及糖尿病黃斑水腫
YUAN-SHEN WANG
王元聖
DepartmentofOphthalmology,ShinKongWuHo-SuMemorialHospital,Taipei,Taiwan 新光吳火獅紀念醫院眼科部
Diabetic macular edema (DME) is the most common cause of vision loss in patients with diabetic retinopathy with an increasing prevalence tied to the global epidemic in type 2 diabetes mellitus. Its pathophysiology starts with decreased retinal oxygen tension that manifests as retinal capillary hyperpermeability and increased intravascular pressure mediated by vascular endothelial growth factor (VEGF) upregulation and retinal vascular autoregulation, respectively. Spectral domain optical coherence tomography (SD-OCT) is the cornerstone of clinical assessment of DME. The foundation of treatment is metabolic control of hyperglycemia and blood pressure. Specific ophthalmic treatments include intravitreal anti-VEGF drug injections, intravitreal corticosteroid injections, focal laser photocoagulation, and vitrectomy, but a substantial fraction of eyes respond incompletely to all of these modalities resulting in visual loss and disordered retinal structure and vasculature visible on SD-OCT and OCT angiography. Efforts to close the gap between the results of interventions within randomized clinical trials and in real-world contexts, and to reduce the cost of care increasingly occupy innovation in the social organization of ophthalmic care of DME. Pharmacologic research is exploring other biochemical pathways involved in retinal vascular homeostasis that may provide new points of intervention effective in those cases unresponsive to current treatments.
Abstract 91
DIABETES RETINOPATHY AND DME: THE DIABETOLOGIST POINT OF VIEW
從糖尿病治療醫師看糖尿病黃斑部病變與糖尿病引起之黃斑部水腫
MEI-YUEH LEE
李美月
DivisionofEndocrinologyandMetabolism,DepartmentofInternalMedicine,KaohsiungMedicalUniversity Hospital
高雄醫學大學附設中和紀念醫院內分泌新陳代謝內科
Diabetes mellitus (DM) is a growing healthcare concern; in Taiwan, almost 2.5 million individuals have DM, and 200 thousand new onset DM were diagnosed in one year. Diabetesrelated complications including cardiovascular disease, kidney disease, neuropathy, blindness, and lower-extremity amputation. In blindness case Diabetic retinopathy (DR) and diabetic macular edema (DME) are the 2 most common ophthalmic complications of DM.
As the incidence of diabetes increases, the prevalence of visual impairment will continue to rise. DR incidence has increased, especially in the DR forms that cause a loss of sight. It’s approved that any DR increased selectively in some age groups, surprisingly, in the 41–50 and 51–60 age.
There are correlations in glycemic control and DME. Glycaemic control can affect the treatment outcome of best corrected visual acuity (BCVA) in the management of DME and the response was found to be better in patients with good glycaemic control. HbA1c level has a significant correlation with central macular thickness (CMT) in diabetic patients, the lower HbA1c the lower CMT. It indicates intensive glycemic control for good visual with DME patient with anti-VEGF treatment.
Intraocular pharmacotherapy with anti-VEGF agents is now the standard of DME care. Before 2023/02/01 the payment from NHI for anti-VEGF treatment had 8 agents for one eye with HbA1c<10%. It’s expand from 8 to 14 agents with more strictly HbA1c<8% level for secondly payment from NHI. There should be more DME patient in anti-VEGF treatment that keep HbA1c<8%. Not only for NHI payment but also for the benefits for intensive glycemic control.
Annual Meeting of the Endocrine Society and the Diabetes Association of the R.O.C. (Taiwan) The45 th 92 March 23-24, 2024
SD2-2
WORSENING OF DIABETIC RETINOPATHY WITH RAPID IMPROVEMENT IN SYSTEMIC GLUCOSE CONTROL
YI-SUN YANG
楊宜瑱
DivisionofEndocrinologyandMetabolism,DepartmentofInternalMedicine,ChungShanMedicalUniversity Hospital,Taichung,Taiwan
中山醫學大學附設醫院內分泌暨新陳代謝科
Worsening of diabetic retinopathy with rapid improvement in systemic glucose control is a phenomenon known as “rapid worsening of diabetic retinopathy” or “accelerated diabetic retinopathy progression.” It’s a paradoxical response observed in some diabetic patients when their blood glucose levels are brought under tight control, especially after a period of poor control. In diabetic retinopathy, abnormal blood vessels form due to chronic hypoxia (oxygen deprivation) in the retina. Rapid improvement in blood glucose levels can lead to sudden changes in retinal blood flow, which may exacerbate retinal ischemia and worsen existing damage. Rapid changes in blood glucose levels may trigger an inflammatory response in the retina, leading to increased vascular permeability and leakage, exacerbating retinopathy. Rapid normalization of blood glucose levels may lead to a sudden increase in retinal blood flow, causing reperfusion injury and further damage to the already compromised retinal vessels. Rapid normalization of blood glucose levels may lead to the release of vascular endothelial growth factor and other growth factors, promoting the proliferation of abnormal blood vessels in the retina. Because of this phenomenon, it’s recommended that diabetic patients undergo regular eye examinations, especially after initiating intensive glucose control therapy. Ophthalmologists and endocrinologists often collaborate to manage such cases, balancing the benefits of tight glucose control with the risks of exacerbating retinopathy. In some cases, additional treatments such as anti-VEGF injections or laser therapy may be necessary to manage worsening retinopathy. Overall, while tight glucose control is crucial in managing diabetes and preventing complications in the long term, the potential for rapid worsening of retinopathy underscores the importance of careful monitoring and individualized treatment approaches for diabetic patient.
Abstract 93
SD2-3
SD3-1
ANTIOSTEOPOROSIS MEDICATIONS AND CARDIOVASCULAR DISEASE: A POPULATION-BASED NATIONWIDE NESTED CASE–CONTROL STUDY
骨質疏鬆藥物使病患產生心血管疾病的風險 : 全人口巢式病例對照
研究
WEN-HSUAN TSAI
蔡文瑄
DivisionofEndocrinologyandMetabolism,DepartmentofInternalMedicine,MackayMemorialHospital, Taipei,Taiwan
臺北馬偕醫院內分泌暨新陳代謝科
Purpose: Patients with osteoporosis are at an increased risk of cardiovascular disease (CVD). Several antiosteoporosis medications have been demonstrated with the benefit of preventing osteoporosis. Our aim is to assess the CVD risks associated with antiosteoporosis medications using the National Health Insurance Research Database in Taiwan between 2000 and 2016.
Methods: Among 41,102 patients of 40+ years old with newly diagnosed osteoporosis, 69.1% (N = 28,387) of patients were included in the user cohort of antiosteoporosis medicines, of whom 13, 472 developed CVD by the end of 2016, while 14,915 did not. Using the nested case-control analysis in the user cohort (88.0% women and 77.4% elderly), we applied conditional logistic regression to estimate odds ratios (ORs) of eight types of CVD for the users of denosumab, bisphosphonate, teriparatide, and hormone replacement therapy (HRT).
Results: The adjusted ORs of overall CVDs were 0.13 (95% CI: 0.12-0.15) for denosumab users, 0.52 (95% CI: 0.45-0.61) for teriparatide users, and 0.80 (95% CI: 0.760.85) for bisphosphonate users. The HRT users were at higher odds of coronary artery and peripheral artery diseases, heart failure, pulmonary embolism, and deep vein thrombosis.
Conclusions: Denosumab, teriparatide, and bisphosphonate may have more protective effects against CVD than hormone therapy. Physicians may take subsequent cardiovascular risks into account when choosing an adequate antiosteoporosis medication for patients with osteoporosis.
Annual Meeting of the Endocrine Society and the Diabetes Association of the R.O.C. (Taiwan) The45 th 94 March 23-24, 2024
SD3-2
CROSS-TALK BETWEEN ADIPOSE TISSUE AND LIVER
脂肪組織與肝臟的對話
HUNG-TSUNG WU
吳泓璁
DepartmentInternalMedicine,SchoolofMedicine,CollegeofMedicine,NationalChengKungUniversity, Tainan,Taiwan
國立成功大學醫學院醫學系內科學科
In view of the challenges posed by the ageing population, diabetes becomes one of the important public health issues worldwide. Although numerous studies explored possible factors related to diabetes, the detail mechanisms in the development of the disease still need further studies to investigate, especially the crosstalk between the tissues that participate in the regulation of glucose homeostasis. In recent years, we found a novel hepakine, hapassocin that might play a pathophysiological role in insulin resistance.
The serum concentrations of hepassocin were significantly increased in subjects with non-alcoholic fatty liver disease or diabetes. To investigate the causal relationship between increased hepassocin levels and the metabolic diseases, high fat diet-induced fatty liver and insulin resistance animal model was used. We found that overexpression of hepassocin increased lipid accumulation and insulin resistance in the liver through an ERK1/2-dependent pathway. On the other hand, specific deletion of hepassocin in the liver ameliorated the fatty liver and insulin resistance in a high fat diet mice model. In addition, hepassocin induced adipogenesis through an ERK1/2-C/EBPβ-dependent pathway in 3T3-L1 adipocytes. Furthermore, we found that unsaturated fatty acids increased the expression of hepassocin through a STAT3-dependent pathway.
Taken together, overnutrition might increase the expression of hepassocin in the liver, and the increased circulating hepassocin levels mediated the crosstalk among liver and other blood glucose-regulating tissues, and further induced systemic insulin resistance in adipose tissue and muscle.
Abstract 95
SD3-3
ORCHESTRATING EPIGENETIC-BASED PRECISION MEDICINE FOR DIABETIC KIDNEY DISEASE: NEW PROSPECTIVE FROM CHIAYI
編排表觀遺傳學的糖尿病腎病精準醫學:嘉義新展望
CHUN-LIANG LIN
林俊良
DepartmentofNephrology,ChangGungMemorialHospital,Chiayi,Taiwan
嘉義長庚腎臟內科
Diabetic Kidney Disease (DKD) is one of leading cause of end-stage renal disease that becomes a tremendous healthcare burden in Taiwan. Dysfunction of mesangial cells and podocytes in renal glomerular micro-compartments contribute to DKD. Compared with conventional mechanisms of diabetic nephropathy, the Dickkopf-1(DKK1)/Wnt/ β-catenin signaling pathway is virgin land in this field. By searching the PubMed at that time (2006), there is no research group in the world studies on molecular mechanism of DKK1/Wnt/GSK3β/β-catenin signaling pathways that mediated diabetic nephropathy. In 10th Anniversary of Chang-Gung Memorial Hospital, Chiayi, international symposium on DKD, we are clearly have demonstrated that embryonic stem cell signaling in DKD are important cellular events underlying diabetes-mediated renal injury. Although the new era of KDCRT in DKD research has made great progress in the first 10 years (2002-2011), the studies related the underlying mechanisms in DKD are still ongoing within last 10 years (2012-2022). KDCRT are trying to put much effort to establish and understand this molecular frame-signaling model in DKD. Furthermore, in 20th Anniversary of Chang-Gung Memorial Hospital, Chiayi, on Precision medicine in the Kidneys, we would like to demonstrate that miR-29a and HDAC4 is an important regulator in the maintenance of podocyte ultra-structure integrity and renal homeostasis. This study highlights an emerging view of an epigenetic mechanism underlying nephrin acetylation in podocytes and suggests that the addition of the miR-29a function is beneficial for improving diabetic podocytopathy. Our hypothesis in this paper was selected to be the cover page of this top journal “JASN” which recognized the importance of our theory. Furthermore, we would have also demonstrated that targeting the KDM6A-KLF10
Annual Meeting of the Endocrine Society and the Diabetes Association of the R.O.C. (Taiwan) The45 th 96 March 23-24, 2024
feedback loop may be beneficial to attenuate diabetes-induced kidney injury which is publish in top journal EMBO Molecular medicine. In this talk, our group KDCRT would orchestrate Epigenetic-Based Precision Medicine for Diabetic Kidney Disease from Chiayi CGMH prospective, and provide precision platform of epigenetic against diabetic kidney disease and exciting new venues for improving renal outcome by retarding the progression of DKD, which are regarded as the therapeutic hope in the future.
Abstract 97
CRITICAL APPRAISAL OF CLINICAL STUDIES: AN OVERVIEW OF RECENT OBESITY TRIALS DESIGNS
從研究設計上嚴格評讀肥胖藥物的臨床試驗
KUO MENG LIAO
廖國盟
DepartmentofEndocrinologyandMetabolism,TaipeiCityHospital,Zongxiaobranch 臺北市立醫院忠孝院區內分泌新陳代謝科
"Recently, numerous clinical trials of incretin-based anti-obesity drugs have been published in prominent journals or presented at the ADA, showcasing remarkable effects on body weight loss and blood sugar reduction. However, despite these promising outcomes, a critical appraisal of these trials, particularly concerning study design, is necessary. So, in this lecture, we aim to elucidate some concepts that are frequently misunderstood yet crucial, by utilizing recently published outcome trials. These trials include Semaglutide in both injected and oral forms, GLP-1/GIP duo-agonist, GLP-1/GIP/Glucagon tri-agonist, GLP-1/Amylin duo-agonist, and oral non-peptide GLP-1 agonist as examples. The concepts we'll explore encompass:
1. Distinguishing between Obesity trials and Diabetic trials
2. Understanding the differences between Phase 2 and Phase 3 trials
3. Comparing Intention-to-Treat vs. On-Treat analysis
4. Clarifying Primary, Secondary, and other Pre-specified endpoints
5. Examining Subgroup analysis and testing for heterogeneity
6. Evaluating study duration
Moreover, we will provide an overview of obesity trial design, which includes four basic design schemes, essential for validating new anti-obesity drugs."
Annual Meeting of the Endocrine Society and the Diabetes Association of the R.O.C. (Taiwan) The45 th 98 March 23-24, 2024
SD4-1
SD4-2
MEDICATIONS TO TREAT OBESITY: WHAT ARE THE EFFICACY AND SAFETY RESULTS OF RECENT OBESITY TRIALS
從近期肥胖相關臨床研究來看治療肥胖症藥物的療效以及安全性
FENG-CHIH SHEN
沈峰志
DivisionofEndocrinologyandMetabolism,DepartmentofInternalMedicine,KaohsiungChangGungMemorial Hospital,Kaohsiung,Taiwan
高雄長庚醫院內分泌暨新陳代謝科
By 2025, it's estimated that 2.7 billion individuals will face overweight issues, with nearly 1 billion grappling with obesity. This escalating issue is not just a health crisis but a complex chronic condition affecting emotional, physical, and social well-being. Obesity intertwines with numerous medical complications, making it a multifaceted and progressive public health challenge. Addressing this requires prompt, personalized, and sustained weight loss strategies. Effective management often involves a blend of lifestyle changes, medication, and in some cases, surgical procedures. Even modest reductions in weight can yield substantial health benefits.
Before prescribing any anti-obesity drugs, it's crucial to evaluate their effectiveness, safety, and affordability for the patient. Continuous monitoring and follow-up are essential for achieving lasting weight loss. Traditional anti-obesity medications have been limited by modest weight reduction and various side effects. However, the recent endorsement of GLP-1 RA (such as semaglutide) and GLP1-GIP 1 agonists (like tirzepatide) has marked a significant advancement. These drugs, which suppress appetite and enhance satiety, have been comparable to gastric bypass surgery in terms of weight loss efficacy and are generally well-received.
These medications are advised for individuals who are obese or overweight with related health issues. Nevertheless, their routine and sustained use face challenges such as high costs, safety concerns, understanding of their appropriate use, the need for healthcare provider training, societal stigma, and insurance limitations. Despite these hurdles, the notable weight loss benefits have surged demand, occasionally outstripping supply, especially in certain countries. This trend has sparked concerns about potential misuse, diverting these drugs away from those who need them for diabetes or obesity treatment
Abstract 99
SD4-3
MEDICATIONS TO TREAT OBESITY: CLINICAL PRACTICE AND LOOK FORWARD TO THE FUTURE
肥胖症治療藥物臨床實務及未來趨勢
SHIH TE TU
杜思德
Departmentofinternalmedicine,divisionofEndocrineandMetabolism,ChanghuaChristianhospital,Changhua County,Taiwan
彰化基督教醫院內分泌新陳代謝科
1. 糖尿病年輕化趨勢及相關併發症
(1)糖尿病年輕化已是趨勢,去年台灣 20-59 歲就醫的糖尿病人口高達八十三點五萬 人,其中大部分皆有肥胖的共病,而他們的就醫醫從性較差,相關併發症發生也 較快
(2)根據 2023 AACE 針對代謝症候群同時有體重過重及肥胖的族群首選藥物是腸泌素
2. 如何介入代謝症候群管理及治療糖胖症的管理及策略
(1)體重管理
● 簡介目前新型減重藥物的進展
(2)連續血糖監測
● 如何使用工具強化病人飲食行為改善的動機
3. 體重門診設立和肥胖症溝通 / 治療遵從性技巧
(1)肥胖是慢性病
(2)行為介入長期維持減重成效是困難的
(3)持續回診追蹤對於長期體重維持相當重要
(4)自費藥品溝通
(5)減重效益可能比苦口婆心的衛教好
Annual Meeting of the Endocrine Society and the Diabetes Association of the R.O.C. (Taiwan) The45 th 100 March 23-24, 2024
AI-AIDS FOR INSULIN DOSING IN TYPE 2 DIABETES
CHIH-YUAN WANG
王治元
DivisionofEndocrinologyandMetabolism,DepartmentofInternalMedicine,NationalTaiwanUniversity Hospital,CollegeofMedicine,NationalTaiwanUniversity
臺大醫院內科部代謝內分泌科,臺灣大學醫學院
We should finally highlight the benefits of AI-aids in the near future, including improved glycemic control, reduced risk of hypoglycemia, and enhanced quality of life for patients. It would also cover the design and outcomes of clinical trials that assess the efficacy and safety of AI-driven insulin dosing systems. Furthermore, we would discuss the potential of these technologies to transform diabetes care by enabling more precise, efficient, and patientcentered treatment approaches. Key components of artificial intelligence would encompass the technological foundations of AI aids, their application in clinical settings, patient engagement strategies, and the implications for future diabetes management practices. It would also address the regulatory, ethical, and privacy concerns associated with the deployment of AI in healthcare, emphasizing the importance of interdisciplinary collaboration in advancing the field of digital health for diabetes care. By synthesizing insights from the presentation, the abstract would articulate the significance of AI-aids in bridging the gap between traditional diabetes management methods and the evolving digital health landscape, showcasing their role in fostering innovation, optimizing treatment outcomes, and supporting the holistic wellbeing of individuals with type 2 diabetes.
Abstract 101
SD5-1
APPLICATIONS OF CHATGPT IN DIABETES CARE: POTENTIAL, CHALLENGES, AND PROSPECTS
CHATGPT 在糖尿病照護中的應用:潛力、挑戰與展望
YAO-HSIEN TSENG
曾耀賢
DivisionofEndocrinologyandMetabolism,TaichungMetroHarborHospital 童綜合醫院新陳代謝科
Abstract
The integration of artificial intelligence (AI) in healthcare, spanning from technical aspects such as algorithms and neural networks to practical applications including patient engagement, data privacy, ethics, and personalized medical care, forms a crucial foundation for leveraging AI to enhance and innovate medical paradigms. I will explore the role of ChatGPT in diabetes care, showcasing its capacity to improve patient interactions and provide personalized medical advice. ChatGPT, a language prediction model, has demonstrated its potential in offering real-time assistance and information to patients and healthcare professionals, thereby broadening the scope of diabetes care and its application possibilities.
Significant advancements in generative conversational AI, such as ChatGPT 4.0, have introduced innovative features that enhance its applicability and effectiveness in diabetes care. These include plugin integration for enriched user interaction, advanced data analysis for improved data interpretation, including glucose readings and continuous glucose monitoring (CGM) charts, and the inclusion of Bing search functionality for real-time information retrieval. GPT-4 vision, a potent computer vision technology, recognizes and understands content within images and videos, offering extensive potential applications in diabetes management.
ChatGPT's diverse applications in healthcare extend to patient interactions, appointment scheduling, medication reminders, medical data analysis, mental health support, medical training, research assistance, and telemedicine support. These applications demonstrate ChatGPT's ability to automate and enhance various aspects of diabetes care, from patient education to managing dietary plans and medication adherence.
Annual Meeting of the Endocrine Society and the Diabetes Association of the R.O.C. (Taiwan) The45 th 102 March 23-24, 2024 SD5-2
Despite the promising prospects of ChatGPT in diabetes care, challenges such as data privacy, the accuracy of provided information, system reliability, and ethical considerations remain. The journey towards integrating ChatGPT into diabetes care involves balancing technological reliance with maintaining professional medical advice and ensuring continuous support despite technical limitations.
Looking ahead, predictive healthcare represents a promising field where generative AI can forecast blood sugar fluctuations and potential health risks, paving the way for a more proactive and predictive healthcare approach. However, discussions on AI-driven care highlight the ethical considerations necessitating a careful and principled approach to exploring the ethical dimensions of using ChatGPT in diabetes care.
Abstract 103
.
NOVEL BIOMARKERS IN DIABETES AND ASSOCIATED COMPLICATIONS
STEPHAN J.L. BAKKER M.D., PH.D.
InternalMedicine,DepartmentofInternalMedicine,UniversityMedicalCenterGroningen,Groningen,The Netherlands;GroningenResearchInstituteforOrganTransplantation;ThePREVENDepidemiologicalstudy laboratory
It is estimated that worldwide more than 500 million people are currently living with diabetes and that this number will rise to more than 750 million by 2045. Many patients suffering from diabetes develop associated complications. These encompass traditional microand macrovascular complications, including neuropathy, nephropathy, retinopathy, coronary artery disease, heart failure, stroke and peripheral vascular disease, and newly recognized complications, including cognitive decline, functional disability, affective disorders, obstructive sleep apnoea and liver disease. Together with the enormous health burden caused by diabetes and these complications, it also comes with an enormous financial burden on health care systems worldwide. Often complications are already present to a certain extent at the diagnosis of diabetes, with high variation in expression and progression between the different complications to clinically overt disease. Complications are preferably halted or reversed, by personalized, guided interventions that already exist or can be developed. Such a strategy requires development and implementation of existing, but particularly also of novel biomarkers, preferably specific to each of the compliations, to allow for early assessment of increased risk for development of the specific complications, and halting or reversal thereof. Many existing biomarkers only allow for detection of already relatively advanced complications. So, there is a great need for novel biomarkers that can detect increased risk for complications in earlier phases. Since end-stage renal disease, heart failure and myocardial infarction are the three traditional complications with the highest health and financial burdens, the fields of these complications may be most eligible to introduction of novel biomarkers.
Annual Meeting of the Endocrine Society and the Diabetes Association of the R.O.C. (Taiwan) The45 th 104 March 23-24, 2024 SD5-3
OVERCOMING CHALLENGES IN EARLY DETECTION AND INTERVENTION IN YOUNGONSET TYPE 2 DIABETES
ELAINE CHOW BSC, MBCHB, MRCP (UK), MSC CLINICAL RESEARCH, PHD
Phase1ClinicalTrialCentre,DepartmentofMedicineandTherapeutics,PrinceofWalesHospital,TheChinese UniversityofHongKong,HongKongSAR
Overcoming challenges in early detection and intervention in Young-Onset type 2 diabetes
One in five patients with diabetes are diagnosed below the age of 40 in Asia. This epidemic of young-onset diabetes is driven by changes in lifestyles, obesity against a genetic predisposition towards poorer beta cell function. Patients with young adults onset diabetes have more rapid decline in beta cell function, are more likely to require insulin compared with those with late onset diabetes. However, what is most challenging is identifying and encouraging early intervention for this group. Patients in their 30-40s are facing competing demands with family, career and reproductive choices. Denial and diabetes distress are more prevalent, as well as mental health disorders. Despite high use of multiple newer glucoselowering drugs, many patients do not reach treatment targets partially secondary to suboptimal treatment adherence. We will share our insights from recent clinical and research experience in Hong Kong and explore alternative models to engage these patients for better care.
Abstract 105 SD6-1
LATEST GLUCOSE MONITORING AND GLUCOSE LOWERING AGENTS FOR CHILDREN AND ADOLESCENTS WITH TYPE 2 DIABETES
第 2 型糖尿病兒童和青少年的血糖監測與降血糖藥物之最新進展
TIEN-JYUN CHANG
張恬君
DivisionofEndocrinologyandMetabolism,DepartmentofInternalMedicine,NationalTaiwanUniversity Hospital;DepartmentofInternalMedicine,NationalTaiwanUniversitySchoolofMedicine
臺大醫院內科部內分泌新陳代謝科;國立臺灣大學醫學院醫學系內科
The worldwide prevalence and annual incidence of type 2 diabetes mellitus (T2DM) in children and adolescents is increasing, and T2DM in this age group is a more aggressive disease and is associated with higher risk of severe long term and potentially life threatening complications (cardiovascular and renal diseases) compared with older adults with T2DM. According to the data from National Health Insurance Claim data (2014-2019), the incidence and prevalence of type 2 diabetes between 6 and 19 y/o is 2.12/10,000 and 9.26/10,000, respectively. Furthermore, the loss of β-cells observed in adolescents with T2DM is three to four times faster compared to adults. Therefore, we need a specific guideline for childhood and adolescence with type 2 diabetes.
Based on the updated 2023 NICE guidance, it is recommended to refer children and young people with suspected or diagnosed T2DM to a multidisciplinary pediatric diabetes team to ensure appropriate diagnosis, investigation, and treatment, including a continuing program of education on how diet, physical activity, and reducing body weight can improve glycemic control, how and when to SMBG, how metformin can help and its possible adverse effects, DM related complications and how to prevent it. Diabetes education should consider personal preference, emotional well being, age and maturity, culture consideration, existing knowledge, current and future social circumstances, life goals. It is important for considering social and cultural preference when providing dietary advice to children and young people with type 2 diabetes. At each clinic visit, the followings should be measured: (1) BH, BW, BMI, and plot on an appropriate growth chart (2) Check for normal growth or significant
Annual Meeting of the Endocrine Society and the Diabetes Association of the R.O.C. (Taiwan) The45 th 106 March 23-24, 2024 SD6-2
changes in weight because these may reflect changes in blood glucose levels. Capillary blood glucose monitoring is now recommended for all children and young people with T2DM, and CGM for people treated with insulin. Specialists should consider offering liraglutide or dulaglutide, or alternatively empagliflozin, in combination with metformin and/or insulin to lower blood glucose. However, duraglutide, liraglutide, and empagliflozin have not been approved by Taiwan Food and Drug Administration.
Abstract 107
SD7-1
IMMUNE THERAPY IN TYPE 1 DIABETES
第 1 型糖尿病的免疫療法
CHIA-HUNG LIN
林嘉鴻
DivisionofEndocrinologyandMetabolism,DepartmentofInternalMedicine,ChangGungMemorialHospital, Linkou,TaoyuanCity,Taiwan;DepartmentofChineseMedicine,CollegeofMedicine,ChangGungUniversity, TaoyuanCity,Taiwan
林口長庚醫院內科部新陳代謝科,長庚大學醫學院
Type 1 diabetes (T1D) is an autoimmune disease characterized by the destruction of insulin-producing beta cells. Current treatments focus on insulin replacement therapy, but do not address the underlying immune dysfunction. Immune therapy aims to modulate the immune response to preserve beta cell function and potentially halt disease progression. Approaches include antigen-specific therapies like oral insulin and monoclonal antibodies targeting immune cells. Despite promising results in early trials, challenges such as treatment variability, side effects, and heterogeneity of T1D hinder progress.
Novel approaches hold promise for personalized treatment. Cell-based therapies using regulatory T cells and mesenchymal stem cells aim to restore immune balance. Biologic agents targeting immune checkpoints offer precision immunotherapy options. Gene editing technologies like CRISPR/Cas9 may enable targeted immune cell modification.
In conclusion, immune therapy represents a promising avenue for T1D treatment. Understanding the immunopathogenesis and identifying biomarkers are crucial for personalized therapy development. Overcoming challenges such as treatment variability and side effects is essential. Future research should focus on optimizing immune therapy efficacy and safety for individuals with T1D.
Annual Meeting of the Endocrine Society and the Diabetes Association of the R.O.C. (Taiwan) The45 th 108 March 23-24, 2024
SD7-2
REPROGRAMMING APPROACHES FOR DEVELOPING BETA CELL REPLACEMENT THERAPIES FOR DIABETES
應用細胞重新編程策略來開發糖尿病的胰島細胞移植治療
CHIA-NING SHEN
沈家寧
GenomicsResearchCenter,AcademiaSinica,Taipei,Taiwan
中央研究院基因體研究中心
Although the isolation of insulin in 1921 has transformed diabetes from a terminal disease to a treatable illness, there is still lack of a disease-modifying therapy that can combat the autoimmune-mediated attack of beta cells or precisely control blood glucose level in patients with type 1 diabetes (T1D) as data obtained from large population studies have consistently supported the notion that tight glycemic control can effectively reduce the development of diabetes complication and conferred mortality and morbidity benefits. Beta cell replacement therapy is believed to be able to improve glycemic control. However, the shortage of beta cell sources limits the potential use of beta cell replacement therapy T1D patients. To provide alternative resources for beta cells to meet current and future needs, the possibility of producing beta-cells from autologous resources would be a key challenge. The explosion of interest in autologous cell reprogramming has been fueled by their potential as an alternative source of beta cells. The approach closest to clinical implementation is the replacement of beta cells derived from human induced pluripotent stem cells (iPSC-derived beta cells), which are currently under investigation in a clinical trial to assess their safety and initial efficacy in humans. The other two most pursued strategies are beta- cell replacement through conversion of alpha-cells or acinar cells.Our recent work demonstrated co-administration of Pdx1, Ngn3, and PDGFR efficiently reprogrammed hepatocytes of autoimmune non-obese diabetic (NOD) mice to glucose-responsive beta-like cells. Autologous transplantation of hepatocyte-derived beta-like cells to diabetic NOD mice significantly improved hyperglycemic status without needs of tolerogenic treatments. Here, my talk will provide an overview of progress made toward β cell replacement and regeneration and discuss promises and challenges for clinical implementation of these strategies.
Abstract 109
BETA CELL REPLACEMENT THERAPY FOR DIABETES
以貝他細胞移植治療糖尿病
JYUHN-HUARNG
JUANG
莊峻鍠
DivisionofEndocrinologyandMetabolism,DepartmentofInternalMedicine,ChangGungMemorialHospital 長庚紀念醫院內分泌暨新陳代謝科
Current approaches to insulin replacement in type 1 diabetes are unable to achieve optimal levels of glycemic control without substantial risk of hypoglycemia and substantial burden of self-management. Advances in biology and technology present beta cell replacement and automated insulin delivery as two alternative approaches.
Whole-organ pancreas and islet transplantations are performed in a highly selected group of patients with diabetes mellitus, primarily those with type 1 diabetes mellitus, complicated by recurrent severe hypoglycaemia or renal failure requiring kidney transplantation. Clinical accessibility to pancreases or islets, and patient characteristics and therapeutic goals, may dictate choice of procedure. Pancreas transplantation is most often performed simultaneous with a kidney transplant, but patients with particularly labile type 1 diabetes may be considered for a pancreas transplant alone. While highly successful at restoring insulin independence, pancreas transplants carry the significant risks of major surgery and immunosuppression. Islet transplantation is a relatively minor procedure, usually performed for labile type 1 diabetes with severe hypoglycaemia. It is highly successful at resolving hypoglycaemia, but more than one pancreas donor may be required for insulin independence. Access to transplantation is limited by the number of deceased donors and the necessity of immunosuppression.
The number of deceased donors of pancreases or islets is only sufficient to treat a small fraction of this population. Ultimately, in order for beta cell replacement therapy to truly provide a ‘cure’, new and renewable sources of islets (or beta cells) are needed. Current work has focused on two potential future sources for islets: xenogeneic islets and stem cell-derived islets. Clinical trials of potentially unlimited supply of porcine islets and stem cell-derived beta cells are showing promise.
Annual Meeting of the Endocrine Society and the Diabetes Association of the R.O.C. (Taiwan) The45 th 110 March 23-24, 2024
SD7-3
SD8-1
DIABETES-RELATED FOOT DISEASE – GUIDELINE AND CONSENSUS UPDATE
糖尿病足治療指引及共識最新進展
YUNG-HSIANG LIN
林詠翔
Departmentofendocrineandmetabolism,ChangGungMemorialHospital,ChiayiBranch
嘉義長庚醫院新陳代謝科
Diabetes-associated foot diseases pose a significant worldwide challenge, impacting both patients and healthcare systems. Since 1999, the International Working Group on the Diabetic Foot (IWGDF) has been developing evidence-based guidance for the prevention and treatment of such conditions. In 2023, the IWGDF updated all its guidelines, drawing on comprehensive literature reviews and contributions from multidisciplinary experts globally. A new guideline was also introduced to address acute Charcot neuro-osteoarthropathy.
For individuals with diabetes, the guidelines advise tailoring foot screening frequency to each person's risk level for developing foot ulcers. To facilitate communication between healthcare professionals, the guidelines recommend the SINBAD (Site, Ischemia, Neuropathy, Bacterial infection, Area, and Depth) classification system, or the WIfI (Wound, Ischemia, foot Infection) system as an alternative, when necessary equipment and expertise are available.
The guidelines extensively discuss the diagnosis of soft tissue and bone infections, as well as the surgical and medical management of diabetic foot infections. They suggest considering bypass surgery using a single segment saphenous vein over endovascular therapy for diabetic individuals with peripheral artery disease, foot ulcers, or gangrene, when appropriate. The guidelines also recommend using a non-removable knee-high offloading device as the primary method for treating neuropathic plantar forefoot or midfoot ulcers in diabetic patients. For wound care, the guidelines offer conditional recommendations for various treatments, including sucrose octasulfate dressings, negative pressure wound therapy for post-surgical wounds, placental-derived products, autologous leukocyte/platelet/fibrin patches, topical oxygen therapy, and hyperbaric oxygen therapy.
In summary, these updated guidelines serve as a comprehensive resource for healthcare providers to help mitigate the global impact of diabetes-related foot complications.
Abstract 111
WOUND CARE IN DIABETIC FOOT
糖尿病足之傷口照護
JIAN-JR LEE
李建智
DepartmentofPlasticandReconstructiveSurgery,ChinaMedicalUniversityHospital,Taichung,Taiwan 中國醫藥大學附設醫院整形外科
The differentiation between diabetic foot ulcers and general abrasions or trauma lies primarily in the pathophysiological effects of diabetes mellitus, notably hyperglycemia, on the body. High blood sugar levels contribute to nerve damage (neuropathy), leading to numbness, vascular blockages, decreased bactericidal capability of leukocytes, and reduced deformability of erythrocytes. These complications make diabetic patients' feet particularly susceptible to wounds, which, without prompt and effective management, often result in amputations. The complexity of diabetic foot conditions, categorized as chronic, difficult-to-heal, and progressively deteriorating diseases, significantly impacts patients' health and quality of life. Integrated care involving a multidisciplinary team is crucial for the management of diabetes and chronic ulcerative wounds. A professional diagnosis and appropriate staging are essential initial steps, followed by tailored treatments including debridement, reconstructive surgery, selection of suitable dressings, hyperbaric oxygen therapy, and addressing underlying chronic diseases to promote wound healing. Through an integrated wound care treatment approach and the collaboration of hospital, community, and long-term care systems, patients can regain health and improve their quality of life.
Annual Meeting of the Endocrine Society and the Diabetes Association of the R.O.C. (Taiwan) The45 th 112 March 23-24, 2024
SD8-2
EPIDEMIOLOGY OF DIABETES IN PREGNANCY IN TAIWAN
孕期糖尿病流行病學
HUNG-YUAN LI
李弘元
DivisionofEndocrinologyandMetabolism,DepartmentofInternalMedicine,NationalTaiwanUniversity Hospital,Taipei,Taiwan.
臺大醫院代謝內分泌科
Diabetes in pregnancy includes preexisting diabetes mellitus, newly diagnosed diabetes mellitus during early pregnancy, and gestational diabetes mellitus. Diabetes in pregnancy is associated with increased risk of various complications during pregnancy, in perinatal period, and after delivery. In 2023, an atlas collecting and analyzing data of diabetes in pregnancy in Taiwan has been published by the Diabetes Association of R.O.C. and the Taiwanese Association of Diabetes Educators. It shows that the complications during pregnancy and perinatal period remained significantly higher in pregnant women with preexisting diabetes mellitus, and newly diagnosed diabetes mellitus, compared with pregnant women without diabetes. In women with gestational diabetes mellitus, the incidence for most of the perinatal complications were similar to that in pregnant women without diabetes, except for the incidence of delivering newborn with macrosomia. In addition, the percentage of pregnant women with advanced maternal age increases significantly. In this talk, I will review these data and discuss what can be done to further improve clinical care for women with diabetes in pregnancy in Taiwan.
Abstract 113
SD9-1
DAROC CLINICAL PRACTICE GUIDELINE FOR DIABETES IN PREGNANCY – PRECONCEPTION AND PERINATAL CARE FOR PREGNANT WOMEN WITH DIABETES
孕期糖尿病臨床照護指引 - 糖尿病婦女的孕前及周產期照護
CHUN-HENG KUO
郭俊亨
DivisionofEndocrine&Metabolism,FuJenCatholicUniversityHospital,NewTaipeiCity,Taiwan,ROC 輔大醫院代謝內分泌科
By definition, diabetes in pregnancy can be classified as preexisting diabetes mellitus, newly diagnosed diabetes mellitus or gestational diabetes mellitus (GDM). Women with the first two diagnoses account for less than 2% of pregnant population. Pregnant women with diabetes and their offspring have increased risks of adverse perinatal outcomes, including primary cesarean section, preeclampsia, congenital anomalies, macrosomia, neonatal jaundice, neonatal hypoglycemia, and birth trauma. Since uncontrolled hyperglycemia in the early stages of pregnancy can cause congenital anomalies, all women with preexisting diabetes mellitus who plan for pregnancy should receive preconception counseling. Screening for undiagnosed diabetes mellitus is also recommended for women planning pregnancy or pregnant women at the first prenatal visit if they have risk factors for diabetes. Initiation of treatment soon after diagnosis is crucial as it can reduce adverse perinatal outcomes. All pregnant women with diabetes are recommended to receive nutrition and exercise counseling…
In my section of this updated guideline symposium, I will introduce preconception and perinatal care for women with preexisting diabetes mellitus or newly diagnosed diabetes mellitus. The content will encompass epidemiology, diagnostic criteria, adverse perinatal outcomes, preconception counseling and care, glycemic monitoring and goals, pharmacological treatment, delivery and nursing, and postpartum follow-up.
Annual Meeting of the Endocrine Society and the Diabetes Association of the R.O.C. (Taiwan) The45 th 114 March 23-24, 2024
SD9-2
DIAGNOSIS, MANAGEMENT, AND POSTPARTUM FOLLOW-UP OF GESTATIONAL DIABETES MELLITUS
妊娠糖尿病的診斷治療與產後追蹤
SZU-CHIEH
CHEN
陳思潔
GoodLiverClinicandGoodLiverHealthManagementCenter,Taipei,Taiwan;GestationalDiabetesMellitus IntegratedClinic,NationalTaiwanUniversityHospital,Taipei,Taiwan
好心肝門診中心暨好心肝健康管理中心;國立臺灣大學醫學院附設醫院妊娠糖尿病整合門診
Diabetes mellitus in pregnancy encompasses several conditions, including women who have known diabetes before becoming pregnant, those who are newly diagnosed with diabetes during pregnancy, and gestational diabetes mellitus (GDM). For women without preexisting diabetes, GDM is diagnosed through an oral glucose tolerance test (OGTT) conducted between gestational weeks 24 and 28 if they meet diagnostic criteria.
If only pregnant women at high risk for GDM are screened, it is possible that 30% to 50% of women with GDM will not be diagnosed. Therefore, routine screening is currently recommended. Using one-step method (referring to the 75g OGTT) to diagnose GDM, despite resulting in a higher diagnostic rate, enables earlier intervention and is associated with a lower rate of primary cesarean section and improved fetal outcomes, making it a more cost-effective approach.
Interventions for GDM can be divided into non-pharmacological and pharmacological managements. Non-pharmacological management involves lifestyle adjustments, including personalized dietary and exercise recommendations. Medical nutrition therapy (MNT) provides guidance on appropriate weight gain during pregnancy, daily calorie intake, proportions of macronutrients, and daily micronutrient intake, aiming to balance maternal blood sugar control and fetal growth needs. During pregnancy, it's important to be aware of any contraindications to exercise. Pregnant women without contraindications are advised to continue exercising throughout pregnancy. The healthcare team can provide guidance on suitable types of exercise, intensity, frequency, and duration, as well as considerations for exercising during pregnancy, to help pregnant women find manageable exercise. In Taiwan,
Abstract 115
SD9-3
approximately 90% of pregnant women with GDM can achieve good blood sugar control through lifestyle modifications.
When lifestyle adjustments fail to achieve desired glucose control, insulin is the preferred option for pharmacological treatment. Oral hypoglycemic agents such as metformin and glyburide pass through the placenta and are associated with adverse maternal and fetal outcomes during pregnancy. Moreover, there is a lack of long-term safety reports. Therefore, they are not recommended as first-line treatment options and are only suggested as alternatives to insulin.
During pregnancy, monitoring of fasting and postprandial blood glucose levels is recommended as the primary monitoring target. Glycated hemoglobin (HbA1c) is influenced by physiological anemia during pregnancy and its own half-life, making it unable to reflect real blood glucose status. Glycated albumin (GA) currently lacks rigorous randomized controlled trials comparing different targets for neonatal outcomes. Continuous glucose monitoring (CGM) use and target recommendations in GDM still lack evidence-based guidance.
The first postpartum follow-up is recommended to be conducted between 4 to 12 weeks after delivery, with a 75g OGTT, measuring fasting and two-hour postprandial blood glucose levels. Subsequent management or follow-up recommendations are provided based on the results. Women previously diagnosed with GDM have a higher risk of developing type 2 diabetes later in life compared to pregnant women without GDM. Therefore, it is advised that all women with GDM continue monitoring their blood glucose levels to detect prediabetes or type 2 diabetes mellitus early.
Annual Meeting of the Endocrine Society and the Diabetes Association of the R.O.C. (Taiwan) The45 th 116 March 23-24, 2024
THYROGLOBULIN IN WASHOUT FLUID OF LYMPH NODE
ASPIRATION:
AS A METHOD TO DETECT CERVICAL LYMPH NODE METASTASIS FROM PAPILLARY THYROID CANCER: CASE REPORTS AND LITERATURE REVIEW
PING-CHEN KUO, WEN-CHIEH CHEN, CHEN-KAI CHOU
DivisionofEndocrinologyandMetabolism,DepartmentofInternalMedicine,KaohsiungChangGungMemorial Hospital,Taiwan
INTRODUCTION: Thyroglobulin (Tg) is produced in thyroid cells for the synthesis of thyroxine.. In the monitoring of recurrent thyroid cancer, the regular assessment of serum Tg is employed. The utilization of washout Tg obtained through fine-needle aspiration (FNA) is helpful in identifying cervical lymph node metastases. There is no consensus on specific cutoff values for now. Herein we demonstrated two cases of thyroid papillary carcinoma (PTC) who presented with suspicious neck nodules and levated FNA washout Tg levels. This discovery prompted further surgical intervention, with pathological confirmed lymph node metastasis
CASE REPORTS: A 53-year-old woman with a history of PTC was discovered to have new hypoechoic nodules in the right level VI area. FNA cytology confirmed malignant metastasis to the neck lymph nodes. At the same time, washout Tg revealed a level of 804 ng/ mL, whereas the serum Tg level was 0.3 ng/mL. Another case present a 39-year-old woman with confirmed malignant metastasis to the neck lymph nodes. Simultaneously, Tg testing revealed a level of 535 ng/mL, while the serum Tg level was 42.8 ng/mL. Additionally, Her anti-Tg Antibodies was positive.
DISCUSSION: Our cases demonstrated the effectiveness of washout Tg in diagnosing lymph node malignancy, even in the presence of low serum Tg or positive anti-Tg antibodies. We have conducted a literature review to determine the optimal cutoff value of washout Tg. We also assessed the potential influence of other pertinent variables, including Tg antibodies, TSH levels, and the presence of the thyroid gland, on washout Tg values. We also collected data from 35 patients diagnosed with PTC neck lymph node metastasis in single medical center to establish a reference for determining the washout Tg cutoff value for clinical experts.
Abstract 117
OE-1
CHANGES IN THYROID FUNCTION DURING PREGNANCY: A PROSPECTIVE OBSERVATIONAL STUDY TO DETERMINE TRIMESTER
SPECIFIC REFERENCE INTERVALS
1LI-HSIN PAN, 2,3,4CHANG-CHING YEH, 5,6,7,8CHEN-CHANG CHEN-CHANG, 5,9CHII-MIN HWU, 5,9HARN-SHEN CHEN, 9,10FAN-FEN WANG
1DivisionofEndocrinologyandMetabolism,DepartmentofMedicine,TaipeiCityHospitalZhongxingBranch, Taipei,Taiwan;
2InstituteofClinicalMedicine,NationalYangMingChiaoTungUniversity,Taipei,Taiwan;
3DepartmentofObstetrics&Gynecology,TaipeiVeteransGeneralHospital,Taipei,Taiwan;
4DepartmentofObstetricsandGynecology,FacultyofMedicine,SchoolofMedicine,NationalYangMingChiao TungUniversity,Taipei,Taiwan;
5FacultyofMedicine,SchoolofMedicine,NationalYangMingChiaoTungUniversity,Taipei,Taiwan;
6InstituteofPublicHealth,SchoolofMedicine,NationalYangMingChiaoTungUniversity,Taipei,Taiwan; 7InstituteofEnvironmental&OccupationalHealthSciences,SchoolofMedicine,NationalYangMingChiao TungUniversity,Taipei,Taiwan;
8DepartmentofClinicalToxicology&OccupationalMedicine,TaipeiVeteransGeneralHospital,Taipei,Taiwan;
9DivisionofEndocrinologyandMetabolism,DepartmentofMedicine,TaipeiVeteransGeneralHospital,Taipei, Taiwan; 10DivisionofEndocrinologyandMetabolism,DepartmentofMedicine,TaipeiCityHospitalYangming Branch,Taipei,Taiwan
Background: Thyroid function test (TFT) reference ranges vary across ethnicities and pregnancy trimesters, underscoring the importance of utilizing population-based reference intervals for accurate thyroid disorder diagnosis.
Methods: We designed a prospective study to establish trimester-specific reference ranges for TFTs in Taiwan. From March 2019 to March 2023, 209 pregnant women in their first trimester at Taipei Veterans General Hospital were enrolled. Anti-thyroid antibodies and TFTs were assessed in each trimester. The trimester-specific TFTs reference ranges were determined based on the 2.5th and 97.5th percentiles of the women (n=123) who did not have thyroid disorder, tested negative on all thyroid autoantibodies, and had complete follow-up through all three trimesters.
Results: The mean age of the cohort was 33.9 years, with 61.0% experiencing their first pregnancy. The median value and trimester-specific reference ranges for TFTs in the first, second and third trimester were: Thyroid-stimulating hormone (TSH) (1.00 [0.007-3.08], 1.46 [0.33-4.55], 1.52 [0.29-4.64] μIU/mL), free T4 (1.29 [0.96-2.44], 0.97 [0.74-1.24], 0.94
Annual Meeting of the Endocrine Society and the Diabetes Association of the R.O.C. (Taiwan) The45 th 118 March 23-24, 2024 OE-2
[0.72-1.18] ng/dL), total T4 (9.9 [6.4-17.2], 9.4 [6.5-13.2], 9.4 [6.7-12.7] μg/dL), free T3 (3.0 [2.2-5.1], 2.5 [1.9-3.2], 2.4 [1.8-2.9] pg/mL), and total T3 (135 [89-214], 141 [92-203], 140 [85-194] ng/dL), respectively. Notably, TSH increased significantly between the first and second trimesters, while free T4 and free T3 gradually decreased throughout pregnancy. The percentage of patients with positive thyroid antibodies in the first, second and third trimester were 7.2%, 3.3%, and 2.9% for anti-thyroid-peroxidase antibody (aTPO) and 7.2%, 6.7%, and 5.7% for anti-thyroglobulin antibody (aTG), respectively. For those whose thyroid antibodies were persistently positive (n= 13 for aTPO, n= 7 for aTG) through pregnancy, significant decrease in aTPO levels between the first and second trimesters was observed (first, second and third trimester levels for aTPO: 1036.9 ± 1323.1 IU/mL, 749.6 ± 760.3 IU/mL, and 691.1 ± 791.9 IU/mL; aTG: 516.1 ± 534.9 IU/mL, 292.2 ± 290.2 IU/mL, and 213.1 ± 209.4 IU/mL, respectively).
Conclusions: Our study represents the first comprehensive investigation of ethnicitybased and trimester-specific reference intervals for TFTs in Taiwan.
Abstract 119
A CASE OF BILATERAL ADRENAL ADENOMA WITH PRIMARY ALDOSTERONISM AND CUSHING SYNDROME
1YUN-KAI YEH , 1FU-SHUN KO, 1JUI-HSIANG SUNG, 1WAN-YIN CHENG, 1,2CHII-MIN HWU
1SectionofEndocrinologyandMetabolism,DepartmentofMedicine,TaipeiVeteransGeneralHospital,Taipei, Taiwan;
2FacultyofMedicine,NationalYangMingChiaoTungUniversitySchoolofMedicine,Taipei,Taiwan.
Background: While primary aldosteronism with concurrent cortisol secretion is not uncommon, the occurrence of bilateral adrenocortical adenomas, each secreting cortisol and aldosterone, respectively, has been rarely reported.
Methods: We reported a case with bilateral adrenal adenoma with concurrent cortisol and aldosterone secretion in different side.
Results: A 55-year-old man with a history of hypertension, hyperlipidemia, and sleep apnea reported poor control of blood pressure (BP) over the past six months. A computer tomography scan revealed bilateral adrenal adenoma, raising suspicion of primary aldosteronism (PA). He was admitted for a PA survey, during which confirmation tests, including the Captopril suppression test (CST) and saline infusion suppression test (SIT), both yielded negative results for PA. However, a 1mg overnight dexamethasone suppression test (DST) indicated unsuppressible cortisol secretion, prompting suspicion of autonomous cortisol secretion. Despite the absence of typical Cushingoid features, an outpatient department (OPD) follow-up was recommended.
Due to persistently elevated BP, he was readmitted for a PA survey one year later. Repeat CST and SIT were conducted, with the CST this time showing a positive result for PA. Diurnal cortisol revealed ACTH-independent hypercortisolism, and a 1mg DST indicated an unsuppressible outcome. Adrenal venous sampling was performed, indicating right lateralization before ACTH stimulation, but with higher cortisol levels on the left side. Following a multidisciplinary meeting, a diagnosis of bilateral adrenal adenoma with concurrent cortisol and aldosterone secretion was established. Furthermore, the left adrenal adenoma predominantly secreted cortisol, while the right adrenal adenoma predominantly
Annual Meeting of the Endocrine Society and the Diabetes Association of the R.O.C. (Taiwan) The45 th 120 March 23-24, 2024 OE-3
secreted aldosterone.
Conclusions: Adrenal venous sampling is crucial for diagnosing bilateral functional adrenocortical adenoma. The accurate interpretation of laboratory findings is especially vital in these patients, and a multidisciplinary discussion should be conducted to ensure comprehensive understanding
Abstract 121
EXTENDED REAL-WORLD OBSERVATION OF PATIENTS TREATED WITH SORAFENIB FOR RADIOACTIVE IODINE-REFRACTORY DIFFERENTIATED THYROID CARCINOMA AND IMPACT OF LENVATINIB SALVAGE TREATMENT: EXPERIENCE FROM CHANG GUNG MEMORIAL HOSPITAL, LINKOU
1MIAW-JENE LIOU, 1YI-WEN CHEN, 2YU-CHAO WANG, 3WEN-HWEI CHAN,
4CHUN HSUEH
1DivisionofEndocrinologyandMetabolism,DepartmentofInternalMedicine,ChangGungMemorialHospital, ChangGungUniversity,Taiwan,
2DepartmentofGeneralSurgery,ChangGungMemorialHospital,Taiwan
3DepartmentofImagingdiagnosisandtreatmentdepartmentChangGungMemorialHospital
4DepartmentofPathology,ChangGungMemorialHospital,Taiwan
Background: Treatment for patients with radioactive iodine (RAI)-refractory differentiated thyroid carcinoma (DTC) is challenging. Since 2017, two tyrosine kinase inhibitors (sorafenib and subsequently lenvatinib) have been approved and reimbursed in Taiwan and showed benefits for progression-free survival with tolerable adverse events.
Methods: This is an extension study of a retrospective cohort study of real-world experience in treating 67 patients with progressive RAI-refractory DTC with sorafenib. The primary endpoint was overall survival (OS). The efficacy of lenvatinib as salvage therapy after disease progression on first-line sorafenib was evaluated by comparing outcomes in 16 (23.9%) patients who were treated with lenvatinib with 51 (76.1%) patients who were not and therefore served as a no salvage treatment group.
Results: The median OS of all 67 patients treated with sorafenib was 41.5 months, and the median progression-free survival was 28 months. About half of these patients continue to treatment with sorafenib. Younger Age (HR: 1.046 [CI:1.004,1.089] p:0.0309 ) and renal metastasis (HR: 5.349 [CI 1.376, 20.791], p=0.0155*) at initial have impact on survival. Early treatment with sorafenib (less than 6 months by Time from RAR-TKI) might be associated with OS (53.2 mos v.s not reached) and PFS (28 mos v.s not reached) . Lenvatinib salvage treatment significantly improved OS in patients receiving it compared with those who did not (HR =0.352 [CI 0.160, 0.77 ], p= 0.0095*). The median OS from the time of disease
Annual Meeting of the Endocrine Society and the Diabetes Association of the R.O.C. (Taiwan) The45 th 122 March 23-24, 2024 OE-4
progression after first-line sorafenib treatment was 5.3 months in no salvage treatment group, whereas it was not reached in the sorafenib treatment only group ( 64.7%).
Conclusions: Age and renal metastasis have impact on survival. Early treatment with sorafenib, probable smaller tumor burden was associated with survival benefits of first-line sorafenib treatment in patients with progressive RAI-refractory DTC. Lenvatinib salvage therapy was effective in improving OS in patients with disease progression after first-line sorafenib.
Abstract 123
INVESTIGATION OF DIETARY EFFECTS ON BODY COMPOSITION AND SKELETAL MUSCLE PERFORMANCE IN ANIMAL MODEL OF SARCOPENIC OBESITY
1CHIA-LUEN HUANG, 1YI-JEN HUNG, 1CHIEN-HSING LEE, 1CHENG-CHIANG SU, 1FENG-CHIH KUO, 1CHIEH-HUA LU, 2FU-HUANG LIN, 1PENG-FEI LI, 1LI-RU HO, 1YICHENG LIU
1DivisionofEndocrinologyandMetabolism,DepartmentofInternalMedicine,Tri-ServiceGeneralHospital, NationalDefenseMedicalCenter,Taipei,Taiwan; 2SchoolofPublicHealth,NationalDefenseMedicalCenter,Taipei,Taiwan
Purpose: Obesity is associated with the development and progression of sarcopenia. Increasing evidence suggests that obesity plays an important role in certain patients with obesity. Therefore, we investigate the dietary effects of exercise performances in skeletal muscles and effects on body composition.
Method: We investigated dietary effects on body composition and skeletal muscle performance in sarcopenic obesity mice model. Two animal groups, divided as young and old mice, are fed a high fat diet or normal diet for 4 months. We perform the exercise performance tests by the grip test, maximum speed test and endurance in animal model; we also arrange body composition to investigate the effect on different diet pattern.
Result: The mice demonstrated increasing fat composition in high fat diet (HFD) groups than those in normal diet (ND) groups in each young and old mice. In the grip strength test, HFD might reduce the muscle power with grip strength but increasing grip strength in the young mice fed with HFD. Age is the most impact factor on grip strength, indicated to poor muscle power and performance. Endurance by rota-rod test. Age might reduce endurance and HFD is the most impact factor on endurance. Maximum speed by rota-rod test. Age might reduce maximum speed and HFD is the most impact factor on maximum speed.
Conclusion: Dietary pattern is one of the effective factors on the performances of exercise and body composition, also indicated to the dietary effect on skeletal muscle health and performances.
Annual Meeting of the Endocrine Society and the Diabetes Association of the R.O.C. (Taiwan) The45 th 124 March 23-24, 2024 OE-5
THERAPEUTIC INHIBITION OF ATR IN DIFFERENTIATED THYROID CANCER
1SHU-FU LIN, 1YI-YIN LEE, 1MING-HSIEN WU, 2YU-LING LU, 3CHUN-NAN YEH,
4
WEI-YI CHEN, 5TING-CHAO CHOU, 6RICHARD WONG
1DepartmentofInternalMedicine,NewTaipeiMunicipalTuChengHospital(builtandoperatedbyChangGung MedicalFoundation),NewTaipeiCity,Taiwan;
2DepartmentofInternalMedicine,ChangGungMemorialHospital,Taoyuan,Taiwan;
3DepartmentofSurgery,ChangGungMemorialHospital,Taoyuan,Taiwan; 4InstituteofBiochemistryandMolecularBiology,NationalYangMingChiaoTungUniversity,Taipei,Taiwan;
5PDScience,Inc.,599MillRun,Paramus,NJ,USA; 6DepartmentofSurgery,MemorialSloanKetteringCancerCenter,NewYork,NY,USA
Background: Ataxia telangiectasia and Rad3-related protein (ATR) is a critical component of the DNA damage response and a potential target in the treatment of cancers. An ATR inhibitor, BAY 1895344, was evaluated for its use in differentiated thyroid cancer (DTC) therapy.
Methods: Cytotoxicity was measured using LDH assay. Cell cycle was assessed with flow cytometry and immunofluorescence microscopy. Caspase-3 activity and apoptosis were assessed with fluorometric assay and flow cytometry. Combination treatment was evaluated. Mice bearing flank DTC were treated with BAY 1895344 and multi-kinase inhibitors.
Results: BAY 1895344 inhibited cell viability in four DTC cell lines (TPC1, K1, FTC133, and FTC-238) in a dose-dependent manner. BAY 1895344 treatment arrested DTC cells in the G2/M phase, increased caspase-3 activity, and caused apoptosis. BAY 1895344 in combination with either sorafenib or lenvatinib showed mainly synergistic effects in four DTC cell lines. The combination of BAY 1895344 with dabrafenib plus trametinib revealed synergistic effects in K1 cells that harbor BRAFV600E. BAY 1895344 monotherapy retarded the growth of K1 and FTC-133 tumors in xenograft models. The combinations of BAY 1895344 plus lenvatinib and BAY 1895344 with dabrafenib plus trametinib were more effective than any single therapy in a K1 xenograft model. No appreciable toxicity appeared in animals treated with either a single therapy or a combination treatment.
Conclusions: Our findings provide the rationale for the development of clinical trials of BAY 1895344 in the treatment of DTC.
Abstract 125 OE-6
A COST-EFFECTIVENSS ANALYSIS OF FIRST-LINE COMBINATION USE OF LINAGLIPTIN (TRAJENTA®) AND METFORMIN IN PATIENTS WITH TYPE 2 DIABETES MELLITUS IN TAIWAN
1,2HUANG-TZ OU, 3,4CHIH-YUAN WANG
1InstituteofClinicalPharmacyandPharmaceuticalSciences,CollegeofMedicine,NationalChengKung University,Tainan,Taiwan;
2DepartmentofPharmacy,CollegeofMedicine,NationalChengKungUniversity,Tainan,Taiwan; 3DivisionofEndocrinologyandMetabolism,DepartmentofInternalMedicine,NationalTaiwanUniversity Hospital,Taipei,Taiwan,;
4DepartmentofInternalMedicine,NationalTaiwanUniversityCollegeofMedicine,Taipei,Taiwan
Background: Clinical studies suggest that early combination treatment of dipeptidyl peptidase 4 inhibitors and metformin in patients with newly diagnosed type 2 diabetes mellitus (T2DM) provides more durable long-term benefits than standard treatment with metformin alone. This study aimed to evaluate the long-term cost-effectiveness of first-line combination of linagliptin (Trajenta®) and metformin in treatment-naïve T2DM patients in Taiwan.
Method: The IQVIA CORE Diabetes Model (CDM) was used to compare the lifetime quality-adjusted life-years (QALYs) and direct healthcare costs of patients who received linagliptin (Trajenta®) and metformin combination or the current standard of care, metformin alone, as the first-line treatment. Treatment-naïve patients with inadequately controlled HbA1c of 8.5% were included in the study. The model was simulated from the perspective of Taiwan’s National Health Insurance Administration with a life-time horizon of 40 years. Duration of each treatment line was set based on the results from a clinical trial - VERIFY. The other parameters of the CDM were derived from published literatures with Taiwanese or Asian populations, local government publications, and clinical experts’ insights in Taiwan to optimize the CDM model.
Results: The early combination of linagliptin (Trajenta®) and metformin dominates metformin monotherapy, with an incremental QALY of 0.086 years and a cost saving with NT$ 15,257, leading to an incremental cost-effectiveness ratio of NT$ -177,202 per QALY gained. Although the combination arm had higher treatment costs (NT$ 10,410), the costs were offset by less incidence rates of complications such as cardiovascular diseases (e.g.,
Annual Meeting of the Endocrine Society and the Diabetes Association of the R.O.C. (Taiwan) The45 th 126 March 23-24, 2024 OD-1
reduced the risk of stroke), renal, and neuropathy due to the improved HbA1c values.
Conclusion: First-line combination of linagliptin (Trajenta®) and metformin is a costeffective treatment option, compared with metformin alone, among treatment-naïve T2DM patients, thereby supporting its rational use in Taiwan’s clinical setting.
Abstract 127
LIRAGLUTIDE REDUCES HEPATOCYTE LIPID ACCUMULATION AND RELATED DAMAGE BY INHIBITING EPITHELIAL-MESENCHYMAL TRANSITION
1,2,3CHUN-CHENG LIAO, 4CHIH-LI LIN, 5SING-HUA TSOU
1DepartmentofFamilyMedicine,TaichungArmedForcesGeneralHospital,Taichung,Taiwan;
2SchoolofMedicine,NationalDefenseMedicalCenter,Taipei,Taiwan;
3DepartmentofMedicalEducationandResearch,TaichungArmedForcesGeneralHospital,Taichung,Taiwan;
4InstituteofMedicine,ChungShanMedicalUniversity,Taichung,Taiwan;
5DepartmentofMedicalResearch,ChungShanMedicalUniversityHospital,Taichung,Taiwan
The prevalence of metabolic dysfunction-associated fatty liver disease (MASLD) has progressively risen in recent years. This syndrome might potentially result in an elevated susceptibility to serious liver disease, including non-alcoholic steatohepatitis (NASH), liver fibrosis, cirrhosis, and liver cancer. The primary etiology of MASLD is the pathological buildup of lipids inside hepatocytes. It results in heightened oxidative stress, triggers inflammatory reactions, and thus stimulates the accumulation of extracellular matrix (ECM) leading to fibrosis. Studies have demonstrated that many pathways may be implicated in these processes, with epithelial-mesenchymal transition (EMT) emerging as a pivotal factor in facilitating fibrosis. Hence, the suppression of EMT and its associated signaling pathways is regarded as a promising therapeutic approach. Nevertheless, there are currently no medications specifically formulated for this objective. The current investigation revealed that Liraglutide, a signaling molecule belonging to glucagon-like peptide-1 (GLP-1), can impede epithelial-mesenchymal transition (EMT) by activating 5’-AMP-activated protein kinase (AMPK). Consequently, the TGFβ/Smad signaling pathway can be inhibited, leading to a decrease in hepatic lipid deposition. This scenario has the potential to decrease the likelihood of the progression of MASLD into NASH. Based on these findings, we hypothesize that enhancing GLP-1 signaling can decrease the excessive buildup of lipids and the deposition of extracellular matrix, thereby reducing the severity of liver fibrosis by inhibiting EMT. This mechanism may explain how GLP-1 signaling contributes to the development of MASLD.
Annual Meeting of the Endocrine Society and the Diabetes Association of the R.O.C. (Taiwan) The45 th 128 March 23-24, 2024 OD-2
RELATIONSHIP BETWEEN HABITUAL LATE CHRONOTYPE GENE AND METABOLIC SYNDROME: ONE-SAMPLE AND TWO-SAMPLE MENDELIAN RANDOMIZATION
1CHUN-YI LEE, 2REN-HUA CHUNG, 2YONG-SHENG CHUANG, 1WAYNE H-H SHEU
1InstituteofMolecularandGenomicMedicine,NationalHealthResearchInstitutes,Miaoli,Taiwan; 2InstituteofPopulationHealthSciences,NationalHealthResearchInstitutes,Miaoli,Taiwan
Background:
Chronotype, also known as circadian preference, which stands for one’s tendency to have earlier or later bedtimes, has been shown to be genetically determined. Although sleep duration carries potential influences on metabolic syndrome, little is known regarding the relationship between chronotype and metabolic syndrome, especially in East Asians. This study aimed to explore the causal relationship between late chronotype and metabolic syndrome based on Mendelian randomization (MR) analysis using data from the Taiwan Biobank (TWB) and validated in two cohorts from Europeans (the UK Biobank (UKB) and the Meta-Analyses of Glucose and Insulin-Related Traits Consortium (MAGIC)).
Methods:
This study included 43,554 subjects from TWB as the discovery cohort, and 263,656 subjects from UKB as the replication cohort. Late chronotype or late circadian preference was defined as preference for having a bedtime after midnight in TWB, and self-reported more an ‘evening’ than ‘morning’ person or an ‘evening’ person in UKB. The relationship between late chronotype and metabolic syndrome and its factors were evaluated using TWB data, and then confirmed using UKB data. We constructed the polygenic risk score (PRS) of late chronotype and examine its associations with metabolic syndrome using TWB. Then, the causality between late chronotype and metabolic syndrome were assessed by one sample MR analysis using TWB and validated using two sample MR with cohorts from UKB and MAGIC. Finally, mediation analysis were used to explore the relationships among late chronotype PRS, late chronotype and metabolic syndrome.
Results:
We found that late chronotype were significantly associated with metabolic syndrome, as
Abstract 129
OD-3
well as central obesity, hyperglycemia, hypertriglyceridemia, and dyslipidemia separately (all p <0.05). Similar findings were found between late chronotype PRS and metabolic syndrome and its components. One sample MR analysis demonstrated that late chronotype was associated with metabolic syndrome, central obesity, hyperglycemia, hypertriglyceridemia, and dyslipidemia (all p <0.05). Two sample MR verified that late chronotype was associated with metabolic syndrome, waist circumference, systolic blood pressure, and high-density lipoprotein cholesterol (all p <0.001) in Europeans. Finally, mediation analysis revealed that late chronotype PRS imposed no direct effects but through late chronotype on metabolic syndrome and its components.
Conclusions:
Late chronotype might be associated with metabolic syndrome in both Taiwan and European populations. MR studies confirmed that genetic associated late chronotype is a potentially causal risk factor for metabolic syndrome. However, mediation analysis found that the association between late chronotype PRS and metabolic syndrome occurred only through late chronotype.
Annual Meeting of the Endocrine Society and the Diabetes Association of the R.O.C. (Taiwan) The45 th 130 March 23-24, 2024
DIFFERENCES IN HEALTH-RELATED QUALITY OF LIFE BETWEEN PATIENTS WITH YOUNG-ONSET TYPE 2 DIABETES MELLITUS AND PATIENTS WITH TYPE 1 DIABETES MELLITUS: RESULTS FROM THE TAIWAN DIABETES REGISTRY
1,2HSUAN-WEI LIN, 3,4CHII-MIN HWU, 2,5,6CHEN-CHANG YANG, 3,7,8WAYNE HUEY-HERNG SHEU
1DivisionofEndocrinologyandMetabolism,DepartmentofInternalMedicine,Min-ShengGeneralHospital, Taoyuan,Taiwan;
2InstituteofPublicHealth,SchoolofMedicine,NationalYangMingChiaoTungUniversity,Taipei,Taiwan;
3DivisionofEndocrinologyandMetabolism,DepartmentofMedicine,TaipeiVeteransGeneralHospital,Taipei, Taiwan;
4SchoolofMedicine,NationalYangMingChiaoTungUniversity,Taipei,Taiwan;
5InstituteofEnvironmentalandOccupationalHealthSciences,CollegeofMedicine,NationalYangMingChiao TungUniversity,Taipei,Taiwan;
6DepartmentofOccupationalMedicineandClinicalToxicology,TaipeiVeteransGeneralHospital,Taipei, Taiwan;
7InstituteofMolecularandGenomicMedicine,NationalHealthResearchInstitutes,Miaoli,Taiwan; 8DivisionofEndocrinologyandMetabolism,DepartmentofInternalMedicine,TaichungVeteransGeneral Hospital,Taichung,Taiwan.
Background: Young onset type 2 diabetes mellitus (YOD), defined as age at diagnosis less than 40 years, is becoming increasingly prevalent. Compared to patients with type 1 diabetes mellitus (T1D), patients with YOD develop microvascular complications earlier and have a higher mortality rate. However, little is known about the impact of YOD on healthrelated quality of life (HRQoL).
Methods: We analyzed 839 adult patients with T1D and 603 adult patients with YOD enrolled in the Taiwan Diabetes Registry (TDR) between October 2015 and August 2018. HRQoL was assessed with the EuroQol EQ-5D instrument, which consists of a five-dimension health profile and a visual analog scale (VAS). The health profile was converted to a single index value using the Taiwanese time-tradeoff tariff and then subtracted from one to produce a disutility score. Multiple linear regression and a two-part model were used to estimate the impact of YOD on the VAS and the disutility score compared to T1D, respectively. In addition, associations between the VAS and 15 diabetes specific HRQoL issues were examined.
Abstract 131
OD-4
Results: Mean EQ-5D VAS was lower in YOD patients compared with T1D patients, while the difference in disutility score was not statistically significant; the unadjusted effect on the VAS was -4.05 (95% confidence interval [CI] (-5.64,-2.47), p <0.0001) and on the disutility score was 8.3% (95% CI (-9.2%,29%), p = 0.37). After controlling for demographic and lifestyle factors, comorbidities, and diabetes goal attainment, the adjusted effect on the VAS was -2.65 (95% CI (-4.92, -0.38), p = 0.022). In terms of diabetes specific HRQoL issues, fewer YOD patients were concerned about the risk of hypoglycemia compared to T1D patients (29.97% vs. 56.07%, p <0.0001) but higher levels of concern were associated with lower VAS, whereas no such association was observed in T1D patients (p for interaction = 0.0089). Although a similar proportion of patients with YOD and T1D were bothered by dietary control (38.61% vs. 34.16%, p = 0.079), higher levels of distress were associated with lower VAS in YOD patients compared with T1D patients (p-interaction = 0.084).
Conclusions: YOD may have a direct impact on subjective HRQoL in addition to the indirect effects of diabetes-related complications. Further study is needed to address the differences in the impact of diabetes-specific issues on HRQoL between patients with YOD and those with T1D.
Annual Meeting of the Endocrine Society and the Diabetes Association of the R.O.C. (Taiwan) The45 th 132 March 23-24, 2024
DIABETIC PERIPHERAL NEUROPATHY IS A MAJOR DETERMINANT OF 10-YEAR ATHEROSCLEROTIC CARDIOVASCULAR DISEASE RISKS IN PATIENTS WITH TYPE 2 DIABETES MELLITUS
1,4TSUNG-HUI WU, 1GUAN-YU SU, 2PEI-CHUAN LEE, 1YUN-KAI YEH, 1MENG-HAN CHIANG, 3SHIOW-CHWEN TSAI, 1,4CHII-MIN HWU
1SectionofEndocrinologyandMetabolism,DepartmentofMedicine,TaipeiVeteransGeneralHospital,Taipei, Taiwan;
2DivisionofEndocrinologyandMetabolism,DepartmentofInternalMedicine,DalinTzuChiHospital,Buddhist TzuChiMedicalFoundation,Chiayi,Taiwan;
3InstituteofSportsScience,UniversityofTaipei,Taipei,Taiwan;
4FacultyofMedicine,NationalYangMingChiaoTungUniversitySchoolofMedicine,Taipei,Taiwan
Background: The aim of this study was to evaluate the relative impact of diabetic peripheral neuropathy and clinical variables on 10-year atherosclerotic cardiovascular disease (ASCVD) risk estimates in patients with type 2 diabetes mellitus.
Methods: A total of 306 patients with type 2 diabetes were enrolled. The assessment for diabetic peripheral neuropathy was performed using Michigan Neuropathy Screening Instrument Physical Examination (MNSI-PE). Ten-year ASCVD risk was assessed using Pooled Cohort Equations. We utilized univariate and multivariate logistic regression analyses to analyze the variables associated with 10-year ASCVD risk estimates. Stepwise multiple regression analysis was subsequently used to evaluate the effects of clinical variables on MNSI-PE score.
Results: Participants with MNSI-PE score ≥2.5 had higher 10-year ASCVD risk estimates than those with MNSI-PE score <2.5 (31.4 (26.9-36.7) vs. 23.4 (21.1-25.9), P = 0.0030). The MNSI-PE score was significantly associated with logarithmic transformation of 10-year ASCVD risk estimates in the multivariate regression analysis (OR = 2.68, 95% CI = 0.082-5.28, P = 0.043). HbA1c, age, estimated glomerular filtration rate, waist circumference, and smoking status independently explained the variance of MNSI-PE score in stepwise multiple regression.
Conclusions: Our data demonstrated that diabetic peripheral neuropathy is an important determinant of 10-year atherosclerotic cardiovascular disease risks in patients with type 2 diabetes mellitus.
Abstract 133
OD-5
CORRELATION WITH FIB-4 AND CHRONIC KIDNEY DISEASE IN PATIENTS WITH DM - A RETROSPECTIVE COHORT STUDY
YA-CHEN YANG, YUNG-NIEN CHEN, JUNG-FU CHEN, CHEN-KAI CHOU
DivisionofMetabolism,DepartmentofInternalMedicine,KaohsiungChangGungMemorialHospitaland ChangGungUniversityCollegeofMedicine,Kaohsiung,Taiwan.
Background: Fibrosis-4 (FIB-4) index is an inexpensive, non-invasive but reliable markers to detect non-alcoholic fatty liver disease (NAFLD). Besides, FIB-4 index is also a predictor of prevalence and incidence of CKD, CVD, metabolic disease. We aim to evaluate the prevalence of and severity of renal function impairment and proteinuria in patients with DM and high FIB-4 score.
Methods: This retrospective cohort study on Chang Gung Research Database included adults with Diabetes Mellitus barcode and complete FIB-4 score. A cutoff value of FIB-4 over 2.67 indicates advance liver fibrosis. Logistic regression models evaluated the associations of elevated FIB-4 with HbA1c status, CKD and severity of proteinuria.
Results: This cohort analyzed 1181 patients without exclusion criteria, 756 patients with lower FIB-4 level and 325 patients with high FIB-4 level. Of 1181 patients, UACR data were available for 640. Method for quantitative evaluation of proteinuria is measurement of urine albumin-to-creatinine ratio. Logistic regression analysis models identified significantly associations of high FIB-4 score with lower HbA1c(95% CI, 0.519-0.891), higher CKD incidence(95% CI, 1.188-2.035). Subgroup analysis identified high FIB-4 level did not correlate with proteinuria.
Conclusions: This study demonstrate that high FIB-4 score is associated with high risk of CKD but limit evidence of association with proteinuria and blood sugar control in diabetes patients.
Annual Meeting of the Endocrine Society and the Diabetes Association of the R.O.C. (Taiwan) The45 th 134 March 23-24, 2024 OD-6
TOPIC: A COMMON EAST-ASIAN ALDH2 MUTATION CAUSES
METABOLIC DISORDERS AND THE THERAPEUTIC EFFECT OF ALDH2 ACTIVATORS
東亞地區常見的 ALDH2 基因突變導致代謝異常及 ALDH2 活化劑 的治療效果
1,2,3YI-CHENG CHANG, 2HSIAO-LIN LEE, 4WENJIN YANG, 1,2MENG-LUN HSIEH,CAICIN LIU1, 1TUNG-YUAN LEE, 1,2JING-YONG HUANG, 1,2JIUN-YI NONG, 3FU-AN LI , 5HSIAO-LI CHUANG, 1ZHI-ZHONG DING, 1WEI-LUN SU, 1LI-YUN CHUEH , 6YI-TING TSAI, 7CHE-HONG CHEN, 7DARIAMOCHLY-ROSEN & 2,8,9LEE-MING CHUANG
1GraduateInstituteofMedicalGenomicsandProteomics,NationalTaiwanUniversity,Taipei,Taiwan.;
2DepartmentofInternalMedicine,NationalTaiwanUniversityHospital,Taipei,Taiwan.;
3InstituteofBiomedicalSciences,AcademiaSinica,Taipei,Taiwan.; 4ForeseePharmaceuticals,Co.Ltd,Taipei,Taiwan.;
5NationalLaboratoryAnimalCenter,Taipei,Taiwan.;
6LaboratoryAnimalCenter,CollegeofMedicine,NationalTaiwanUniversity,Taipei,Taiwan.;
7DepartmentofChemicalandSystemsBiology,StanfordUniversitySchoolofMedicine,Stanford,CA,USA.;
8GraduateInstituteofMolecularMedicine,NationalTaiwanUniversity,Taipei,Taiwan.; 9Graduate Institute of ClinicalMedicine,NationalTaiwanUniversity,Taipei,Taiwan.
Purpose
Obesity and type 2 diabetes have reached pandemic proportion. ALDH2 (acetaldehyde dehydrogenase 2, mitochondrial) is the key metabolizing enzyme of acetaldehyde and other toxic aldehydes, such as 4-hydroxynonenal. A missense Glu504Lys mutation of the ALDH2 gene is prevalent in 560 million East Asians, resulting in reduced ALDH2 enzymatic activity. Here, we examined the metabolic phenotype of this missense mutation in mice and tested the effect of ALDH2 activators.
Method
Aldh2 knock-in mice mimicking human Glu504Lys mutation were examined for metabolic phenotypes and the effect of a new-generation ALDH2 activator AD-9308, a watersoluble, potent, and highly selective ALDH2 activator was tested.
Results
We find that Aldh2 knock-in mice mimicking human Glu504Lys mutation were
Abstract 135
AR-1
prone to develop diet-induced obesity, glucose intolerance, insulin resistance, and fatty liver due to reduced adaptive thermogenesis and energy expenditure. We find reduced activity of ALDH2 of the brown adipose tissue from the Aldh2 homozygous knock-in mice. Proteomic analyses of the brown adipose tissue from the male Aldh2 knock-in mice identifies increased 4-hydroxynonenal adducted proteins involved in mitochondrial fatty acid oxidation and electron transport chain, leading to markedly decreased fatty acid oxidation rate and mitochondrial respiration of brown adipose tissue, which is essential for adaptive thermogenesis and energy expenditure. AD-9308 treatment ameliorates diet-induced obesity and fatty liver, and improves glucose homeostasis in both Aldh2 wild-type and knock-in mice in a dose-dependent manner.
Conclusion
Our data highlight the therapeutic potential of reducing toxic aldehyde levels by activating ALDH2 for metabolic diseases.
Annual Meeting of the Endocrine Society and the Diabetes Association of the R.O.C. (Taiwan) The45 th 136 March 23-24, 2024
CLINICAL IMPACT OF ANDROGEN RECEPTOR-SUPRESSING MIR146B EXPRESSION IN PAPILLARY THYROID CARCINOMA
甲狀腺乳突癌中雄性賀爾蒙接受體異常表現與高癌症風險和甲狀 腺外侵犯相關
1CHEN-KAI CHOU, 2SHUN-YU CHI, 3YI-YUNG HUNG, 4YI-CHIEN YANG, 5HUNGCHUN FU, 1JIA-HE WANG, 1CHUEH-CHEN CHEN AND 6HONG-YO KANG
1DivisionofEndocrinologyandMetabolism,DepartmentofInternalMedicine,KaohsiungChangGung MemorialHospital,ChangGungUniversityCollegeofMedicine,Kaohsiung,Taiwan;
2DepartmentofSurgery,KaohsiungChangGungMemorialHospital,ChangGungUniversityCollegeof Medicine,Kaohsiung,Taiwan;
3DepartmentofPsychiatry,KaohsiungChangGungMemorialHospital,andChangGungUniversityCollegeof Medicine,Kaohsiung,Taiwan;
4DepartmentofDermatology,KaohsiungChangGungMemorialHospitalandChangGungUniversityCollege ofMedicine,Kaohsiung,Taiwan;
5DepartmentofObstetricsandGynecology,KaohsiungChangGungMemorialHospitalandChangGung UniversityCollegeofMedicine,Kaohsiung,Taiwan;
6GraduateInstituteofClinicalMedicalSciences,ChangGungUniversityCollegeofMedicine,TaoyuanCity
Purpose
Papillary thyroid carcinoma (PTC) is the most common thyroid malignancy. Dysregulated expression of miR-146b and androgen receptor (AR) has been shown to play critical roles in tumorigenesis in PTC. However, the mechanistic and clinical association between AR and miR-146b is not fully understood. The purpose was to investigate miR-146b as the potential AR target miRNA and its involvement in advanced tumor characteristics of PTC.
Method
Expression of AR and miR-146b were assessed in frozen and formalin-fixed paraffinembedded (FFPE) tissue samples from PTC and adjacent normal thyroid specimens by quantitative real-time polymerase chain reaction, and their correlation was examined. Human thyroid cancer cell lines BCPAP and TPC-1 were used to evaluate the effect of AR on miR146b signaling. Chromatin immunoprecipitation (ChIP) assays were performed to determine whether AR binds to the miR-146b promoter region.
Result
Pearson correlation analysis confirmed significant inverse correlation between miR-
Abstract 137 AP-1
146b and AR expression. Over-expressing AR BCPAP and TPC-1 cells showed relatively lower miR-146b expression. ChIP assay revealed that AR might bind to the androgen receptor element (ARE) located on the promoter region of miRNA-146b gene and overexpression of AR suppresses miR-146b-mediated tumor aggressiveness. The low-AR/high miR-146b PTC patient group was associated with advanced tumor characteristics, including higher tumor stage, lymph node metastasis and worse treatment response..
Conclusion
To sum up, miR-146b is a molecular target of AR transcriptional repression, therefore, AR suppresses miR-146b expression to reduce PTC tumor aggressiveness.
Annual Meeting of the Endocrine Society and the Diabetes Association of the R.O.C. (Taiwan) The45 th 138 March 23-24, 2024
TRAITS OF PATIENTS WITH PITUITARY TUMORS IN MULTIPLE ENDOCRINE NEOPLASIA TYPE 1 AND COMPARING DIFFERENT MUTATION STATUS
腦下垂體腫瘤於多發性內分泌腫瘤第一型患者的特徵及不同基因 變異型之比較
1KUAN-YU LIN, 2YU-TING KUO, 3,4MEI-FANG CHENG, 5,6,7PEI-LUNG CHEN, 2HSIU-PO WANG, 2,8TSU-YAO CHENG, 5CHIA-HSUIN CHANG, 9HSIANG-FONG KAO, 10SHIH-HUNG YANG, 5HUNG-YUAN LI, 11CHIA-HUNG LIN, 6YUH-TSYR CHOU, 6AN-KO CHUNG, 5WAN-CHEN WU, 5JIN-YING LU, 5,12CHIH-YUAN WANG, 1WEN-HUI HSIH, 1CHEN-YU WEN, 12,13WEI-SHIUNG YANG, AND 5,12,14SHYANG-RONG SHIH.
1DivisionofEndocrinologyandMetabolism,DepartmentofInternalMedicine,NationalTaiwanUniversity Hospital,YunlinBranch,DouliuCity,Taiwan;
2DivisionofGastroenterologyandHepatology,DepartmentofInternalMedicine,NationalTaiwanUniversity Hospital,Taipei,Taiwan;
3DepartmentofNuclearMedicine,NationalTaiwanUniversityHospital,Taipei,Taiwan;
4InstituteofEnvironmentalandOccupationalHealthSciences,NationalTaiwanUniversity,Taipei,Taiwan;
5DivisionofEndocrinologyandMetabolism,DepartmentofInternalMedicine,NationalTaiwanUniversity Hospital,Taipei,Taiwan;
6GraduateInstituteofMedicalGenomicsandProteomics,NationalTaiwanUniversityCollegeofMedicine, Taipei,Taiwan;
7DepartmentofMedicalGenetics,NationalTaiwanUniversityHospital,Taipei,Taiwan;
8DepartmentofLaboratoryMedicine,NationalTaiwanUniversityCancerCenter,Taipei,Taiwan;
9DepartmentofMedicalOncology,NationalTaiwanUniversityCancerCenter,Taipei,Taiwan;
10DivisionofNeurosurgery,DepartmentofSurgery,NationalTaiwanUniversityHospital,Taipei,Taiwan;
11DivisionofEndocrinologyandMetabolism,DepartmentofInternalMedicine,NationalTaiwanUniversity Hospital,Hsin-ChuBranch,Hsin-Chu,Taiwan;
12DepartmentofInternalMedicine,NationalTaiwanUniversityCollegeofMedicine,Taipei,Taiwan;
13GraduateInstituteofClinicalMedicine,NationalTaiwanUniversityCollegeofMedicine,Taipei,Taiwan;
14CenterofAnti-AgingandHealthConsultation,NationalTaiwanUniversityHospital,Taipei,Taiwan
Purpose
To assess characteristics of patients with MEN1 with and without PITs, and compare among different MEN1 mutations. Method
Data of patients with MEN1 in a tertiary referral center from 2010 to 2023 were retrospectively analyzed.
Abstract 139 AP-2
Result
Forty-two patients with MEN1 were included. Twenty-four patients had PITs, 3 of which were invasive and managed with transsphenoidal surgery. One PIT enlarged during followup. Patients with PITs had a higher median age at MEN1 diagnosis than those without PITs. MEN1 mutations were identified in 57.1% of patients, including 5 novel mutations. In patients with PITs, those with MEN1 mutations (mutation+/PIT+ group) had more additional MEN1associated tumors than those without (mutation−/PIT+ group). The mutation+/PIT+ group had a higher incidence of adrenal tumors and a lower median age at initial manifestation of MEN1 than the mutation−/PIT+ group. The most common neuroendocrine neoplasm was nonfunctional in the mutation+/PIT+ group and insulin-secreting in the mutation−/PIT+ group.
Conclusion
This is the first study comparing characteristics of patients with MEN1 with and without PITs harboring different mutations. Patients without MEN1 mutations tended to have less organ involvement and it might be reasonable for them to receive less intensive follow-up.
Annual Meeting of the Endocrine Society and the Diabetes Association of the R.O.C. (Taiwan) The45 th 140 March 23-24, 2024
THE RISK OF SEVERE HYPOGLYCEMIA AND MORTALITY IN PATIENTS WITH TYPE 2 DIABETES AND DISCHARGED WITH ACUTE LIVER INJURY
2 型糖尿病人因急性肝損傷出院其嚴重低血糖及死亡的風險
1FU-SHUN YEN, 2,3MING-CHIH HOU, 4CHUN-WEI PAN, 5JIA-SIN LIU, 5,6,7,8CHIH-CHENG HSU, 2,9CHII-MIN HWU
1Dr.Yen’sClinic,Taoyuan,Taiwan;
2InstituteofClinicalMedicine,SchoolofMedicine,NationalYang-MingChiaoTungUniversity,Departmentof Medicine,NationalYang-MingUniversitySchoolofMedicine,Taipei,Taiwan;
3DivisionofGastroenterologyandHepatology,DepartmentofMedicine,TaipeiVeteransGeneralHospital, Taipei,Taiwan;
4DepartmentofMedicine,CookCountyHospital,Chicago,Illinois, USA.;
5InstituteofPopulationHealthSciences,NationalHealthResearchInstitutes,35KeyanRoad,Zhunan,Miaoli County,Taiwan;
6DepartmentofHealthServicesAdministration,ChinaMedicalUniversity,Taichung,Taiwan;
7DepartmentofFamilyMedicine,Min-ShengGeneralHospital,Taoyuan,Taiwan;
8NationalCenterforGeriatricsandWelfareResearch,NationalHealthResearchInstitutes, Miaoli,Taiwan;
9SectionofEndocrinologyandMetabolism,DepartmentofMedicine,TaipeiVeteransGeneralHospital,Section ofEndocrinologyandMetabolism,DepartmentofMedicine,TaipeiVeteransGeneralHospital,Taipei,Taiwan.
Purpose
To compare the risks of severe hypoglycemia and mortality between patients with type 2 diabetes (T2D) and discharged with and without acute liver injury.
Method
From January 1, 2000, to December 31, 2010, we identified patients with T2D and hospitalization for acute liver injury and hospitalization for other causes from the National Health Insurance Research Database of Taiwan. Multivariable-adjusted Cox proportional hazards models were used to compare the risks of severe hypoglycemia and mortality between the study and control groups.
Result
The incidence rates and adjusted hazard ratios (aHRs) for severe hypoglycemia within 90 days and 365 days after discharge were 12.28 and 5.59 per 1000 person-years [aHR 1.92 (1.30-2.85)] and 7.35 and 2.9 per 1000 person-years [aHR 1.98 (1.52-2.58)] for patients discharged with and without acute liver injury, respectively. The incidence rates and aHRs for
Abstract 141 AP-3
mortality within 90 days and 365 days after discharge were 82.4 and 27.54 per 1000 personyears [aHR 1.73 (1.46-2.05)] and 36.8 and 9.3 per 1000 person-years [aHR1.94 (1.69-2.24)] for patients discharged with and without acute liver injury, respectively. The subgroup analysis of hypoglycemia risk in patients discharged with acute liver injury revealed no significant interaction in risk factors of age, chronic kidney disease, and medications, except for sex difference has significant interaction.
Conclusion
This cohort study demonstrated that patients with T2D and discharged with acute liver injury showed significantly higher risks of severe hypoglycemia and mortality within 90 days and 365 days after discharge than patients discharged with other causes.
Annual Meeting of the Endocrine Society and the Diabetes Association of the R.O.C. (Taiwan) The45 th 142 March 23-24, 2024
COMPARISONS BETWEEN DIFFERENT ANTI-OSTEOPOROSIS
MEDICATIONS ON POSTFRACTURE
MORTALITY: A POPULATIONBASED STUDY
比較不同骨質疏鬆症藥物對骨折後死亡率的影響:以全人口為基 礎的研究
1,2,3CHIH-HSING
WU, 2,4CHIA-CHUN LI, 5YU-HSUAN HSU, 6FU-WEN LIANG, 2YIN-FAN CHANG, 7JAWL-SHAN HWANG
1InstituteofGerontology,CollegeofMedicine,NationalChengKungUniversity,Taiwan;
2DepartmentofFamilyMedicine,CollegeofMedicine,NationalChengKungUniversity,Taiwan;
3DepartmentofFamilyMedicine,NationalChengKungUniversityHospital,CollegeofMedicine,National ChengKungUniversity,Taiwan;
4InstituteofAlliedHealthSciences,CollegeofMedicine,NationalChengKungUniversity,Taiwan;
5InstituteofClinicalPharmacyandPharmaceuticalSciences,CollegeofMedicine,NationalChengKung University,Taiwan;
6DepartmentofPublicHealth,CollegeofHealthSciences,KaohsiungMedicalUniversity,Taiwan;
7DivisionofEndocrinologyandMetabolism,DepartmentofInternalMedicine,ChangGungMemorialHospital, ChangGungUniversity,Taiwan
Purpose
Osteoporosis is becoming a global epidemic in aging societies. Anti-osteoporotic medications can prevent fractures, and their pleiotropic effect on mortality is interesting but not well compared among each other. To provide real-world evidence on the pleiotropic effect of different anti-osteoporotic medications on all-cause mortality, stratified by fracture site, sex, and age.
Method
This longitudinal population-based postfracture cohort study, included mega-data from subjects ≥40 years of age with osteoporotic fracture who used anti-osteoporotic medications as recorded in Taiwan's National Health Insurance Research Database from 2009 to 2017 and followed until 2018. A multivariate Cox proportional hazards model with immortal time bias was used to assess the relationship between fracture sites and mortality stratified by antiosteoporosis medication.
Result
Abstract 143 AP-4
A total of 46 729 subjects with an average age of 74.45 years (80.0% female) and a mean follow-up period of 4.73 years were enrolled. In the total fracture group, compared with raloxifene and bazedoxifene, we found that alendronate/risedronate (hazard ratio [HR] 0.83; 95% CI, 0.79-0.88), denosumab (HR 0.86; 95% CI, 0.81-0.91), and zoledronic acid (HR 0.78; 95% CI, 0.73-0.84) resulted in significantly lower mortality. Similar trends were observed in the hip, vertebral, or nonhip/nonvertebral fracture groups. Subjects receiving long-acting zoledronic acid showed the lowest mortality in the subanalysis according to sex or age over 65 years.
Conclusion
This real-world mega-data study suggests that the usage of osteoporotic medication, especially a long-acting regimen, may lower postfracture mortality.
Annual Meeting of the Endocrine Society and the Diabetes Association of the R.O.C. (Taiwan) The45 th 144 March 23-24, 2024
TRADITIONAL
CHINESE MEDICINE THERAPY ASSOCIATED WITH LOWER RISK OF FRACTURE, HOSPITALIZATION AND DEATH IN PATIENTS WITH LOWER EXTREMITY INJURIES COMBINED WITH OSTEOPOROSIS
1HONG-HAN LIN, 2,3CHI-HSIANG CHUNG, 4CHIEN-JUNG LIN, 1SHENG-CHIANG SU, 1FENG-CHIH KUO, 1PENG-FEI LI, 1CHIA-LUEN HUANG, 1LI-JU HO, 1,5CHIEH-HUA LU, 2,5WU-CHIEN CHIEN
1DivisionofEndocrinologyandMetabolism,Tri-ServiceGeneralHospital,NationalDefenseMedicalCenter, Taipei,Taiwan.;
2SchoolofPublicHealth,NationalDefenseMedicalCenter,Taipei,Taiwan.;
3TaiwaneseInjuryPreventionandSafetyPromotionAssociation,Taipei,Taiwan.;
4DepartmentofChineseMedicine,Tri-ServiceGeneralHospital,Taipei,Taiwan.; 5DepartmentofMedicalResearch,NationalDefenseMedicalCenter,Taipei,Taiwan.
Background:
Studies have confirmed that the health hazards of patients with lower limb injuries combined with osteoporosis are more obvious. This study is mainly based on the Taiwan National Health Insurance Database (TNHID), and through big data analysis, it shows that the combined treatment of traditional Chinese medicine (TCM) is helpful to the health of patients with lower limb injuries combined with osteoporosis.
Methods:
A total of 9,989 combined TCM-treated patients and 19,978 2:1 sex-, age-, and indexyear-matched controls who did not receive TCM treatment were selected from the TNHID. Cox proportional hazards analyzes were performed to compare fracture surgery, inpatient, and all-cause mortality during a mean follow-up period of 17 years.
Results:
A total of 5,406/8,601/2,564 enrolled-subjects (14.11%/25.46%/5.53%) had fracture surgery/inpatient/all-cause mortality, including 1,409/2,543/552 in the combined TCM group (14.11%/25.46%/5.53%) and 3,997/6,058/2,012 in the control group (20.01%/30.32%/10.07%). Cox proportional hazard regression analysis showed a lower rate of fracture surgery, inpatient and all-cause mortality for subjects in the combined TCM group
Abstract 145
PE-1
(adjusted HR=0.723; 95% CI=0.604-0.810, P<0.001; adjusted HR=0.803; 95% CI=0.7120.950, P = 0.001; adjusted HR=0.842; 95% CI=0.731-0.953, P = 0.007, respectively). After ten years of follow-up, the cumulative incidence of fracture surgery in patients combining TCM treatment seems to be half of that without combining TCM treatment those are shown in Kaplan-Meier analysis with statistically significant (log rank, P<0.001, P<0.001 and P = 0.010, respectively).
Conclusions:
This study hopes to provide clinicians with the option of combined TCM treatment for patients of lower limbs injuries combined with osteoporosis, so that such patients will be associate with a lower risk of fracture surgery, inpatient or all-cause mortality.
Annual Meeting of the Endocrine Society and the Diabetes Association of the R.O.C. (Taiwan) The45 th 146 March 23-24, 2024
HYPOTHALAMIC LANGERHANS CELL HISTIOCYTOSIS PRESENTING WITH CENTRAL DIABETES INSIPIDUS, RHABDOMYOLYSIS, AND ENDOCRINOPATHY IN A 36-YEAR-OLD WOMAN
1YU-SHIUAN LIANG, 2TSE-YING HUANG
1DepartmentofInternalMedicine,NationalTaiwanUniversityHospital,CollegeofMedicine,NationalTaiwan University,Taipei,Taiwan.;
2DepartmentofInternalMedicine,NationalTaiwanUniversityHospitalHsin-ChuBranch,Taiwan.
This 36-year-old woman presented with altered mental status and lower extremities weakness for 10 days. This time, she experienced worsening weakness in the lower limbs, decreased appetite, intermittent vomiting, and visual hallucinations. Her medical history included a previous cholecystectomy and 1 year-long treatment for secondary amenorrhea. Physical examination showed proximal muscle weakness, dry mucosa, and hypoactive bowel sounds. Laboratory tests showed severe hypernatremia, rhabdomyolysis, elevated liver enzymes, acute kidney injury and hypokalemia. A desmopressin test confirmed a diagnosis of central diabetes insipidus. The presence of severe dehydration, which is atypical for diabetes insipidus, led to the suspicion of hypodipsia. The simultaneous presentation of central diabetes insipidus and hypodipsia raised the possibility of hypothalamic dysfunction. Then Brain MRI was performed and revealed a hypothalamic mass. A subsequent brain biopsy confirmed Langerhans cell histiocytosis. Pituitary function and stimulation tests were performed. The final diagnosis was hypothalamic Langerhans cell histiocytosis, with central diabetes insipidus, hypodipsia, hypopituitarism and hyperprolactinemia. The patient received 2 cycles of cladribine and cytarabine and is currently under hormone replacement therapy.
Abstract 147 PE-2
DELAYED SURGICAL INTERVENTION IN AN ELDERLY PATIENT WITH PERSISTENT HEMATOMA AFTER THYROID FINE-NEEDLE ASPIRATION:
A
CASE REPORT
1MENG-JIE TSAI, 1YU-CHENG LIANG, 1,2HORNG-YIH OU
1DivisionofEndocrinologyandMetabolism,DepartmentofInternalMedicine,NationalChengKungUniversity Hospital,CollegeofMedicine,NationalChengKungUniversity,Tainan,Taiwan.; 2DepartmentofInternalMedicine,SchoolofMedicine,CollegeofMedicine,NationalChengKungUniversity, Tainan,Taiwan.
Background
Fine-needle aspiration is a valuable and minimally invasive technique for diagnosing thyroid cancer, yet, albeit uncommon, it carries potential risks that may result in lifethreatening complications.
Patient Findings
An 85-year-old woman experienced the development of a large cervical hematoma and subsequent respiratory failure following thyroid fine-needle aspiration. Due to her advanced age, conservative treatment was initially pursued. However, after a two-week observation period revealed no interval regression of the hematoma, attempts at catheter drainage proved unsuccessful. Consequently, surgical removal of the hematoma was performed. During the procedure, severe local adhesions were discovered, leading to esophageal injury. Subsequently, the patient was extubated and discharged.
Discussion
This case stands as the oldest documented instance in current literature of a patient surviving post-thyroid hematoma, enduring the lengthiest period before surgical intervention. Our review of literature on surviving cases of thyroid fine-needle aspiration complicated by cervical hematoma indicates that the majority of patients underwent hematoma removal either immediately or within two days of its formation, with no instances of catheter drainage. However, in this case, postponed surgical intervention and catheter drainage offered no discernible benefits.
Conclusions
Surgical intervention is warranted in cases where the airway is compromised, and
Annual Meeting of the Endocrine Society and the Diabetes Association of the R.O.C. (Taiwan) The45 th 148 March 23-24, 2024 PE-3
early intervention is particularly advisable, especially when the likelihood of spontaneous hematoma resolution is low.
Abstract 149
A 34-YEAR-OLD WOMAN WITH SEVERE HYPONATREMIA AND SECONDARY ADRENAL INSUFFICIENCY DUE TO PARTIALLY EMPTY SELLA SYNDROME—A CASE REPORT
1YUN-JU PAN, 1SHU-TIN YEH, 2JU-YEH YANG
1DivisionofEndocrinologyandMetabolism,DepartmentofInternalMedicine,FarEasternMemorialHospital, Taiwan;
2DepartmentofNephrology,FarEasternMemorialHospital,Taiwan
Background: Hyponatremia is a common electrolyte abnormality which can be caused by multiple conditions. Thorough investigation and precise treatment can avoid severe complication. Adrenal insufficiency is one of etiology of hyponatremia, which can mimic as SIADH, which is the major cause of euvolemic hyponatremia. Empty Sella syndrome, a condition which pituitary gland was flattened or shrunk, can also cause secondary adrenal insufficiency. Here we discuss a case of an Asian women presenting with severe hyponatremia and secondary adrenal insufficiency due to partial empty Sella syndrome.
Case report: A 34-year-old Asian female presented with dizziness, poor appetite, general weakness and low-grade fever for 1 week. Physical examination revealed no suspicious finding. Laboratory tests reported severe hyponatremia (sodium 103 mmol/L), low cortisol levels (cortisol: 9.10 µg/dL (9.52-26.21µg/dL)) and corresponding low adrenocorticotropic hormone (ACTH: 10.37 pg/mL (9.60-49.70 pg/mL)), which were suggestive of secondary adrenal insufficiency. Meanwhile her other hormonal axes remained normal. Brain magnetic resonance imaging without and with contrast demonstrated a partial empty Sella appearance. The patient symptoms of dizziness, low grade fever and hyponatremia prompt resolved after hydrocortisone supplement and was discharged under well condition after 10 days hospitalization. During outpatient department, she was maintained on oral cortisone acetate 25mg in the morning and 12.5mg in the afternoon. She continued to be well and plasma sodium level continued to be within normal range.
Conclusion: We reported a case of initially severe hyponatremia and finale diagnosis of partially empty Sella syndrome resulting in secondary adrenal insufficiency. We demonstrate that partial empty Sella syndrome can manifest with severe hyponatremia as a result of
Annual Meeting of the Endocrine Society and the Diabetes Association of the R.O.C. (Taiwan) The45 th 150 March 23-24, 2024 PE-4
secondary adrenal insufficiency. We also highlight that precise replacement of cortisone results in complete resolution of symptoms and hyponatremia.
Abstract 151
RESISTANCE TO THYROID HORMOINE COEXISTING WITH PROLATINOMA---A CASE REPORT
1WAN-YI LU, 1,2LIANG-YU LIN
1DivisionofEndocrinologyandMetabolism,DepartmentofMedicine,TaipeiVeteransGeneralHospital,Taipei, Taiwan;
2FacultyofMedicine,SchoolofMedicine,NationalYangMingChiaoTungUniversity,Taipei,Taiwan
Background:
Disorders of thyroid function with hyperthyroxinemia with non-suppressed thyroidstimulating hormone (TSH) levels should differentiate between resistance to thyroid hormone (RTH) and TSH-secreting pituitary adenoma (TSHoma). Biochemical tests should be repeated to exclude interference of assay. Family and drug history were essential. Laboratory screenings, dynamic tests, radiological and genetic studies should be conducted.
Methods:
We reported a case of hyperthyroxinemia with non-suppressed TSH levels with a rare THRB gene mutation by whole exome sequencing.
Results:
A 33-year-old woman with history of hyperprolactinemia with left pituitary microadenoma presented with intermittent headache, irregular menstrual cycle and palpitation under cabergoline treatment for 2 years. The patient’s laboratory analysis revealed persistent elevations in free thyroxine (FT4) with unsuppressed TSH levels with different assays. The patient received TRH stimulation test showing normal response to TRH, which favors RTH. Repeated sella MRI unveiled a nodule about 4.5 mm at left pituitary gland, microadenoma is considered. Genetic analysis using next-generation sequencing method resulted THRB gene mutation (NM_001354712.2:c.997G>A, NP_001341641.1:p.Glu333Lys) which is likely pathogenic.
Conclusions:
The possibility of pituitary tumor with RTH occurs concurrently in patients presenting hyperthyroxinemia with non-suppressed TSH levels so this makes differential diagnosis challenging. Thus, extensive investigation and further genetic analysis are critical to determine the diagnosis.
Annual Meeting of the Endocrine Society and the Diabetes Association of the R.O.C. (Taiwan) The45 th 152 March 23-24, 2024 PE-5
PHEOCHROMOCYTOMA WITH PAPILLARY THYROID CARCINOMA:
A CASE REPORT
1HAO-TING CHUANG, 2CHUNG-HSIN TSAI, 2SHIH-PING CHENG, 1MING-NAN CHIEN, 1WEN-HSUAN TSAI
1DivisionofEndocrinologyandMetabolism,DepartmentofInternalMedicine,MackayMemorialHospital, Taiwan;
2DepartmentofGeneralSurgery,MackayMemorialHospital,Taiwan
Pheochromocytomas are rare catecholamine-producing tumors of chromaffin cells of the adrenal medulla. 10–25% can be associated with genetic familial syndromes, such as multiple endocrine neoplasia type 2 (MEN 2), type 1 neurofibromatosis, and Von-HippelLandau disease, particularly in younger individuals. We present a case involving a 23-yearold male patient with a left adrenal incidentaloma. Biochemical analysis revealed normal 24hour urine cortisol with suppressible overnight dexamethasone suppression test (ONDST), elevated 24-hour urine norepinephrine, and normal serum aldosterone levels. A diagnosis of pheochromocytoma was established, leading to the subsequent performance of an adrenalectomy. As part of the comprehensive evaluation for multiple endocrine neoplasia, a thyroid ultrasound was conducted. Following a right thyroid lobectomy, papillary carcinoma was confirmed. Gene testing yielded a negative result for the specific gene mutation. The rare coexistence of pheochromocytoma and papillary thyroid carcinoma has been reported in literature, with some case reports indicating distinct genetic variants. The nature of the association, whether coincidental or rooted in an underlying genetic predisposition, remains unknown.
Abstract 153 PE-6
RISK FACTORS FOR MORTALITY IN PATIENTS WITH POORLY DIFFERENTIATED THYROID CANCER
1CHIH-WEI HSU, 1YU-LING LU, 1CHIA-JUNG HSU, 2SHU-FU LIN
1DivisionofEndocrinologyandMetabolism,DepartmentofInternalMedicine,ChangGungMemorialHospital, ChangGungUniversity,Taiwan;
2DepartmentofInternalMedicine,NewTaipeiMunicipalTuChengHospital,NewTaipeiCity,Taiwan
Purpose
Poorly differentiated thyroid cancer (PDTC) is uncommon, accounting for < 5% of thyroid cancers. PDTC is more aggressive than differentiated thyroid cancer with 66% of five-year disease specific survival. The aim of this study was to investigate the risk factors associated with mortality in PDTC patients.
Methods
Patients with PDTC were assessed using a prospectively maintained database of thyroid cancer registered at a medical center in Taiwan between 1985 and 2021.
Results
A total of 49 patients with a mean follow-up of 8.8 years were included in this study. Univariate analysis revealed older age, distant metastasis and less than total thyroidec-tomy were significantly associated with increased risk of mortality. Multivariate anal-ysis showed only distant metastasis was correlated with higher risk of death. Further analysis revealed older patients had increased risk to have metastatic PDTC.
Conclusions
Distant metastasis is associated with mortality in patients with PDTC. Older patients had increased risk to have metastatic PDTC.
Annual Meeting of the Endocrine Society and the Diabetes Association of the R.O.C. (Taiwan) The45 th 154 March 23-24, 2024 PE-7
MEDICAL MANAGEMENT OF ECTOPIC CUSHING SYNDROME:
CASE REPORT
YI-FU LIN, WAN-CHEN WU, SHYANG-RONG SHIH, CHIH-YUAN WANG
DivisionofEndocrinologyandMetabolism,DepartmentofInternalMedicine,NationalTaiwanUniversity Hospital,NationalTaiwanUniversity,Taiwan
Background: Ectopic Cushing Syndrome (ECS) accounts for 6% of Cushing syndrome cases. Tumors producing adrenocorticotropic hormone (ACTH) are rarely identified as the root cause. The prevailing treatment approach is the surgical removal of the primary lesion causing ECS. In situations where surgery is impractical, medical methods are considered to manage hypercortisolism.
Case Presentation: A 51-year-old male was diagnosed with stage IIIB small cell carcinoma, displaying characteristics of a Cushingoid appearance. Laboratory assessments, imaging, and biopsy confirmed ectopic Cushing syndrome due to an ACTH-secreting lung tumor. After the initial chemotherapy, the patient suffered septic shock and acute respiratory distress syndrome, necessitating transfer to the intensive care unit (ICU). In the ICU, hypercortisolism was treated with continuous etomidate infusion, which was later switched to metyrapone in the general ward. The treatment results indicated that etomidate infusion was more effective in controlling hypercortisolism and its related complications compared to metyrapone. A follow-up CT scan showed a notable reduction in the size of the lung tumor. Nevertheless, high ACTH levels and adrenal gland enlargement continued, leading to the consideration of bilateral adrenalectomy after completing chemoradiotherapy.
Conclusion: This case showcases ECS where surgery was not an option. The continuous infusion of etomidate proved to be more effective than intermittent metyrapone in managing hypercortisolism. The decision to consider bilateral adrenalectomy as a final measure reflects the complexities in managing the primary lung cancer’s prognosis, potential surgical risks, and the financial implications of ongoing medical management for hypercortisolism.
Abstract 155
PE-8
CRIBRIFORM-MORULAR VARIANT OF PAPILLARY THYROID CARCINOMA AND FAP : A CASE REPORT
1CHIH-WEI HSU, 1CHENG-WEI LIN, 2CHUN-YI TSAI, 3YU-HSIU CHEN, HSIN-YI CHEN, 1FENG-HSUAN LIU
1DivisionofEndocrinologyandMetabolism,DepartmentofInternalMedicine,ChangGungMemorialHospital, ChangGungUniversity,Taiwan.;
2DivisionofofGeneralSurgery,,ChangGungMemorialHospitalatLinkou,Taoyuan,Taiwan.; 3DepartmentofPathology,ChangGungMemorialHospitalatLinkou,Taoyuan,Taiwan.
Background: Familial adenomatous polyposis (FAP) is an autosomal dominantly inherited intestinal polyposis syndrome, occurring in approximately 1 in 8300 births and representing about 1% of all colorectal cancers. This syndrome manifests various extraintestinal complications, with thyroid carcinoma occurring in 1–2% of affected individuals. The cribriform morular variant (CMV) is a rare histological subtype of papillary thyroid carcinoma (PTC) associated with FAP. This report details a case of FAP presenting with the cribriform-morular variant of papillary thyroid carcinoma (CMV-PTC).
Case presentation: A 26-year-old female with hereditary colorectal polyps syndrome sought screening at the surgical clinic. Concurrently, she reported a prolonged history of daily diarrhea with bloody stool twice a week. Annual colonoscopies since 2015 revealed a progressive increase in polyp numbers, with the latest biopsy confirming tubular adenomas. Following laparoscopic total colectomy and ileorectal anastomosis, the patient experienced intermittent abdominal cramping pain post-discharge. Abdominal CT revealed a sizable intra-abdominal tumor suspected to be of mesenteric origin. Incidentally discovered were right thyroid nodules, leading to a subsequent total thyroidectomy that unveiled CMV PTC. Histologically, the tumor displayed a prominent cribriform growth pattern, interspersed cell clusters forming morules, and characteristic papillary structures—defining features of this subtype.
Conclusion: Recognition of the infrequent but notable occurrence of CMV PTC in patients with underlying FAP underscores the importance of thyroid screening for early intervention and improved outcomes.
Annual Meeting of the Endocrine Society and the Diabetes Association of the R.O.C. (Taiwan) The45 th 156 March 23-24, 2024 PE-9
CARBIMAZOLE INDUCED CHOLESTATIC HEPATITIS IN GRAVES’
DISEASE: CASE REPORT AND REVIEW LITERATURE
1BAO-MEI WANG, 2,3TON-HO YANG, 1WEN-YA MA, 4LE-YU TSAI
1DivisionofEndocrinologyandMetabolism,DepartmentofInternalMedicine,CardinalTienHospital,New TaipeiCity,Taiwan.
2SchoolofMedicine,FuJenCatholicUniversity,NewTaipeiCity,Taiwan.
3DivisionofGastroenterologyandHepatology,DepartmentofInternalMedicine,CardinalTienHospital,New TaipeiCity,Taiwan.
4DivisionofEndocrinologyandMetabolism,DepartmentofInternalMedicine,YongHeCardinalTienHospital, NewTaipeiCity,Taiwan
Background: Carbimazole Induced Cholestatic Hepatitis in Graves’ disease
Methods: The typical clinical and biochemical findings in a patient with carbimazole induced cholestatic hepatitis in Graves’ disease .
Results: Rare presentation of carbimazole induced cholestatic hepatitis in Graves’ disease.
Conclusions: In this rare case report, carbimazole caused severe but reversible cholestatic jaundice. It is a diagnosis of exclusion. Autoimmune based liver dysfunction, viral hepatitis and other iatrogenic cause of liver injury should be differentiated. The first action when occurs is to discontinue carbimazole. It may spontaneously relieve or improve after using systemic steroids.
Abstract 157
PE-10
DETERMINATION OF IODINE AND SELENIUM CONCENTRATION IN EDIBLE AND MEDICINAL CHINESE HERBS USING INDUCTIVELY COUPLED PLASMA MASS SPECTROMETRY
1CHAO-JUNG CHANG, 2FAN-FEN WANG, 3CHEN-CHANG YANG, 4YI-FANG LIU, 3YI-LIN LIU, 5CHUN-JUI HUANG
1InstituteofFoodSafetyandHealthRiskAssessment,NationalYangMingChiaoTungUniversity,Taipei, Taiwan;
2DivisionofEndocrinologyandMetabolism,DepartmentofInternalMedicine,YangmingBranch,TaipeiCity Hospital,Taipei,Taiwan;
3DepartmentofOccupationalMedicineandClinicalToxicology,TaipeiVeteransGeneralHospital,Taipei, Taiwan;
4DepartmentofNutritionalScience,FuJenCatholicUniversity;
5DivisionofEndocrinologyandMetabolism,DepartmentofInternalMedicine,TaipeiVeteransGeneralHospital, Taipei,Taiwan
Background: Iodine and selenium are essential trace elements required to maintain stable thyroid hormone secretion. Edible and medicinal Chinese herbs are commonly incorporated into various applications including decoctions, herbal teas and health supplements. However, there are no reports on the concentrations of iodine and selenium in these herbs.
Methods: Based on the 37 items listed by Taiwan’s Ministry of Health and Welfare as “medicinal herbs suitable for simultaneous use in food”, 111 samples of herbs were analyzed. The iodine and selenium concentrations were measured using inductively coupled plasma mass spectrometry.
Results: The top three herbs for iodine content were seaweed, kelp and lotus leaf, with iodine levels of 85.36 μg/g (range: 60.0-105.8 μg/g), 5.11 μg/g (3.6-6.8 μg/g) and 1.52 μg/g (1.2-1.8 μg/ g), respectively. According to the Chinese Pharmacopoeia and Taiwan Herbal Pharmacopoeia, the suggested dosages of the above items are 6-12 g, 3-12 g and 3-12 g per serving, respectively. The iodine contributions of these suggested dosages to the recommended daily iodine intake of 150 μg per day are 341-683%, 10-41% and 3-12%, respectively. The top three for selenium content were fennel fruit, purslane herb and fresh ginger, with selenium levels of 0.12 μg/g (0.08-0.16 μg/g), 0.07 μg/g (0.04-0.1 μg/g), and 0.06 μg/g (0.03-0.1 μg/g), respectively.
Conclusions: Iodine and selenium were detectable in most of the analyzed items. Given
Annual Meeting of the Endocrine Society and the Diabetes Association of the R.O.C. (Taiwan) The45 th 158 March 23-24, 2024 PE-11
the increasing use of health supplements and decoctions which may contain medicinal herbs, we suggest that the iodine and selenium contents be reported on the food labels.
Abstract 159
A CASE OF BILATERAL ADRENAL LYMPHOMA WITH PRESENTATION OF ADRENAL INSUFFICIENCY
WAN-YIN CHENG, FU-SHUN KO, JUI-HSIANG SUNG, YUN-KAI YEH, CHII-MIN HWU
DivisionofEndocrinologyandMetabolism,DepartmentofMedicine,TaipeiVeteransGeneralHospital.
Background: Adrenal incidentalomas affect approximately 2% of the population, and can be classified as either non-functional or functional which have excessive production of adrenal hormones. Notably, pheochromocytoma should be excluded and larger-sized incidentalomas may pose an increased risk of malignancy. Herein, we present a rare case of a bilateral adrenal incidentaloma which was ultimately identified as adrenal lymphoma.
Methods: We reported a case of bilateral adrenal incidentaloma exceeding 4cm in size, presenting with clinical symptoms of low blood pressure, leading to a diagnosis of adrenal insufficiency. The patient was subsequently diagnosed with adrenal diffuse large B cell lymphoma.
Results: A 67 year-old male with medical history of type 2 diabetes mellitus, hypertension, hyperlipidemia, presented with low blood pressure and cold-intolerance in recent two months. He had visited another hospital one week ago and an abdominal CT scan disclosed bilateral adrenal tumors, measuring 4.8x 3.6cm on the left, and 4.0x 2.8cm on the right tumor, with a differential diagnosis including pheochromocytoma, lymphoma, metastatic lesion and adrenocortical carcinoma. Blood laboratory findings was notable for white blood cell of 4180 /uL with 8% of immature cells, bicytopenia with hemoglobulin 9.5 g/dL , platelet 77,000 /uL . Hormonal evaluation for adrenal incidentaloma disclosed aldosterone, PRA (renin activity), DHEA-S levels were within normal limit. Blood and 24-hour urine catecholamine levels were within normal limit. Morning 8am cortisol was 10.8 ug/dL, ACTH was 59.1 pg/ mL with diurnal variation, and 24-hour urine cortisol was less than three times of upper normal limit. Dynamic function tests with high dose ACTH stimulation test reported adrenal insufficiency. While clonidine suppression test yielded suppressible results that was less likely pheochromocytoma. Hematological consultation for bicytopenia led to a bone marrow biopsy, which reported erythroid hyperplasia. Considering the size of the adrenal tumors, which were larger than 4cm, the patient underwent robotic-assisted left adrenalectomy. Pathology
Annual Meeting of the Endocrine Society and the Diabetes Association of the R.O.C. (Taiwan) The45 th 160 March 23-24, 2024 PE-12
of left adrenal gland reported diffuse large B cell lymphoma. Whole body PET-CT identified multiple uptake over nodal group above diaphragm, right adrenal, bone marrow, suggesting Ann Arbor stage 4 disease of lymphoma. The patient subsequently received dose-adjusted R-EPOCH chemotherapy regimen, along with prophylaxis CNS intrathecal chemotherapy for the treatment of bilateral adrenal diffuse large B cell lymphoma.
Conclusions : This case highlights the significance of including lymphoma in the differential diagnoses for adrenal incidentaloma, especially when accompanied by concurrent hematologic abnormalities. Adrenal lymphomas, though uncommon, often exhibit bilateral adrenal involvement and can manifest with adrenal insufficiency in approximately 70% of cases. Imaging modalities with MRI and PET play a crucial role in identifying these lesions. Adrenalectomy has no benefit for treatment, and despite the implementation of chemotherapy, the overall survival rate remains poor.
Abstract 161
PROGNOSIS OF YOUNG PATIENTS WITH PAPILLARY THYROID CANCER
1,2YU-LING LU, 1,2SHU-FU LIN
1Endocrinology&MetabolismDivision,DepartmentofInternalMedicine,ChangGungMemorialHospital, LinkouMainBranch,TaoyuanCity,Taiwan, 2DepartmentofInternalMedicine,NewTaipeiMunicipalTuChengHospital,NewTaipeiCity,Taiwan
Background:
Papillary thyroid cancer (PTC) in young patients is rare. This study aimed to evaluate outcomes in young patients with PTC.
Methods:
Patients aged <20 years with PTC were analyzed using a thyroid cancer registry dataset at Chang Gung Memorial Hospital between December 1, 1976, and March 2, 2023.
Results:
A total of 109 patients were included in this study. The median age was 17.7 years (IQR, 5.8-19.9), including 20 males (18.3%) and 89 females (81.7%). Seven patients (6.4%) had distant metastasis at diagnosis, including lung (n=6) and bone (n=1). Most patients (88.1%) underwent total thyroidectomy, followed by subtotal thyroidectomy (7.3%), and lobectomy (4.6%). Thirty-four patients (31.2%) had histologically proven lymph node metastasis. Most patients (90.8%) received radioiodine therapy, with a median dose of 107.5 mCi [IQR, 29.61030]. Recurrence appeared in 13 patients (11.9%) during a median follow-up of 11.9 years [IQR, 1.1-37]. The median time to develop recurrence was 5.8 years [IQR, 0.9-17.4]. The sites of recurrence were the thyroid bed (n = 1) and cervical lymph nodes (n = 12). All 109 patients were alive during follow-up.
Conclusions:
Young patients with PTC had excellent survival, even in those patients with metastatic disease at diagnosis.
Annual Meeting of the Endocrine Society and the Diabetes Association of the R.O.C. (Taiwan) The45 th 162 March 23-24, 2024 PE-13
PE-14
PRIMARY HYPERPARATHYROIDISM PRESENTING WITH SEVERE HYPERCALCEMIA: TWO CASE REPORTS
YU-PING HSIEH, CHUN-YUAN HUANG, PO-YIN LAI, SHANG-HSIEN WU, HAN-SHENG LU, WEI-FU HUANG, MEI-CHEN YEH, CHEWN-YI YANG, HAO-CHANG HUNG
DivisionofEndocrinologyandMetabolism,DepartmentofInternalMedicine,ChimeiMedicalCenter
Case 1
This is a case of a 78-year-old man with a medical history that includes hypertension, type 2 diabetes mellitus, dyslipidemia, and gastric ulcer, all of which are under treatment. During a routine follow-up at the gastrointestinal (GI) outpatient department (OPD), his renal function deteriorated (serum creatinine: 1.75 mg/dL, baseline serum creatinine around 0.90 mg/dL). As a result, he was referred to our nephrology OPD. At that time, he experienced general malaise and had a poor appetite for several days. Laboratory tests revealed severe hypercalcemia (serum calcium: 15.2 mg/dL), hypophosphatemia (serum phosphorus: 2.3 mg/dL) and hypomagnesemia (serum magnesium: 1.2 mg/dL), prompting his referral to the emergency department. Treatment for hypercalcemia included intravenous hydration, calcitonin, and furosemide. Further investigation for hypercalcemia revealed an elevated intact parathyroid hormone level (iPTH: 351.9 pg/mL). Urine calcium-creatinine ratio was 0.15. Tumor markers such as CEA, CA 15-3, and SCC Ag were all within normal range. Additionally, 25-OH vitamin D level was measured at 21.0 ng/mL. Thyroid ultrasound showed an 8.0 x 5.7 x 5.3 mm well-defined isoechoic nodule in the right thyroid lobe. Parathyroid scan indicated the probable presence of a parathyroid adenoma in the left lower portion near the thyroid bed. Bone densitometry was arranged to rule out osteoporosis, and it showed normal bone density. Consequently, a consultation with a general surgeon was sought for surgical evaluation. The patient underwent right thyroid subtotal lobectomy and left lower parathyroidectomy. Pathological examination confirmed a right thyroid adenoma and the removal of left parathyroid gland. After surgery, his iPTH level normalized (iPTH: 27.8 pg/ mL), and hypercalcemia resolved. The patient was discharged in stable condition and advised to follow up at the outpatient department.
Abstract 163
Case 2
This is a case of 57-year-old man with a medical history of hypertension and left renal pelvis stone, status post ureterorenoscopic stone manipulation in 2018. He presented to our emergency department with symptoms of general malaise and poor appetite for several days. Laboratory tests indicated impaired renal function (serum creatinine: 3.82 mg/dL, baseline serum creatinine around 1.20 mg/dL), severe hypercalcemia (serum calcium: 18.3 mg/dL), hypophosphatemia (serum phosphorus: 1.6 mg/dL) and hypomagnesemia (serum magnesium: 1.7 mg/dL). Fractional excretion of calcium (FECa) was 0.017. Treatment for hypercalcemia included intravenous hydration and calcitonin. Further investigation for hypercalcemia revealed elevated iPTH levels (743.1 pg/mL), while the 25-OH vitamin D level measured at 24.0 ng/mL. Thyroid ultrasound identified a 2.3 x 2.1 x 3.2 cm cystic mass located in the right thyroid or parathyroid region, and spongiform nodules in bilateral thyroid lobes, up to 1.5cm. Parathyroid scan suggested possible parathyroid hyperplasia in bilateral lower portions near the thyroid bed. Bone densitometry showed osteoporosis, with the lowest T-score recorded at -2.9. A consultation with a general surgeon was sought for surgical evaluation. Subsequently, the patient underwent a right upper parathyroidectomy. The operative record indicated the presence of a 2.0 x 2.0 x 3.5 cm cystic lesion containing clear fluid. Pathological examination confirmed the diagnosis of a parathyroid adenoma. Post-surgery, his iPTH level normalized (iPTH: 9.4 pg/mL), and hypercalcemia resolved. The patient was discharged in stable condition with instructions to follow up at the outpatient department.
Discussion
Primary hyperparathyroidism (PHPT) typically manifests with hypercalcemia and an unsuppressed or elevated PTH level. Serum levels of 25-hydroxy-vitamin D are usually normal or low-normal due to the effect of PTH on increasing the conversion of this metabolite to 1,25-dihydroxy-vitamin D. These laboratory findings were consistent in our patients. PHPT commonly leads to renal and skeletal complications, such as renal function impairment, nephrolithiasis, and osteoporosis. PHPT is not casually associated with peptic ulcer disease, however, in multiple endocrine neoplasia type 1 syndrome (MEN1), patients may exhibit parathyroid tumor and gastrinoma. In the first case, gastric ulcer occurred in 2023 when PHPT was diagnosed. During another hospitalization, an abdominal computed tomography scan revealed a 0.5 cm hypervascular lesion in the pancreatic head, suspicion of a neuroendocrine tumor. Further investigations for MEN1 should be considered, such as laboratory tests including chromogranin A, gastrin level, or an endoscopic ultrasonography-guided biopsy.
Annual Meeting of the Endocrine Society and the Diabetes Association of the R.O.C. (Taiwan) The45 th 164 March 23-24, 2024
Moreover, in the first case, the patient had previously presented with normocalcemia, and the FECa was greater than 0.01, making familial hypocalciuric hypercalcemia less likely. Urine calcium was not assessed in the second case.
According to guidelines from the Fifth International Workshop, surgery remains the definitive treatment for hyperparathyroidism. All patients undergoing pre-operative imaging should have biochemically proven PHPT. The primary role of imaging is to assess the presence or absence of a solitary adenoma. Ultrasonography and parathyroid scan (technetium-99m sestamibi) are common first-line modality. However, no universally accepted algorithm exists for pre-operative localization. In our second case, although the largest lesion detected by ultrasound was situated in the right upper region of the thyroid, the parathyroid scan indicated potential parathyroid hyperplasia in bilateral lower portions. The decision to remove the right upper parathyroid was made based on intra-operative findings following bilateral thyroid exposure. These two cases presented typical features and complications of PHPT, and also highlighting the efficacy of parathyroidectomy as standard treatment.
Abstract 165
THYROID ARTERY EMBOLIZATION FOR THE TREATMENT OF HYPERTHYROIDISM AND THYROID NODULES: A CASE REVIEW IN A SINGLE HOSPITAL
1CHIA-YU CHANG, 1YUNG-HSIANG LIN, 2CHIEN-WEI CHEN
1DivisionofEndocrinologyandMetabolism,DepartmentofInternalMedicine,ChangGungMemorialHospital ChiayiBranch,Taiwan;
2DepartmentofDiagnosticRadiology,ChangGungMemorialHospitalChiayiBranch,Taiwan
Background:
Thyroid artery embolization (TAE) is a novel method used to alleviate thyrotoxicosis and reduce the size of thyroid goiter. TAE has been initiated as a treatment for thyrotoxicosis and goiter since 2022 in our hospital. We aim to evaluate the effectiveness and safety of TAE for patients with Graves’ disease and large symptomatic benign thyroid nodules based on our clinical experience.
Methods:
The included patients with compressive or cosmetic symptoms were unwilling to receive surgery. The indications for TAE are as follows: Case No 1~3 are Graves’ disease with diffuse goiter. Case No 4~5 are subclinical hyperthyroidism with diffuse goiter. Case No 6~8 are single large benign nodular goiter.
Results:
In five out of eight cases, bilateral thyroid embolization was performed. The right thyroid lobe exhibited a minimum volume reduction ratio (VRR) of 40.59%, with a maximum VRR of 65.41% three months post TAE. Similarly, the left thyroid lobe showed substantial changes, ranging from a minimum VRR of 15.31% to a maximum of 66.07% after the same duration. Additionally, three cases involving a single large thyroid nodule showed separative VRR at the 1-month follow-up as 4.21%, 28.07%, and 35.12%, with VRR of 80.21% after 3 months. Notably, no complications were observed during or after the procedure.
Conclusions:
This is a preliminary report of the efficacy and safety of TAE in a single hospital. Further case enrollment and longer observation period is warranted for a more comprehensive statistical analysis.
Annual Meeting of the Endocrine Society and the Diabetes Association of the R.O.C. (Taiwan) The45 th 166 March 23-24, 2024 PE-15
PE-16
NORMOTENSIVE ADRENAL INCIDENTALOMA AS THE INITIAL PRESENTATION OF CONNSHING’ SYNDROME
JAU-FONG HUNAG, FANG-RONG LE, TZU-YUAN WANG, CHING-CHU CHEN, CHWEN-TZUEI CHANG
DivisionofEndocrinologyandMetabolism,DepartmentofMedicine,ChinaMedicalUniversityHospital
Background:
Primary aldosteronism(PA) is the most common cause of endocrine hypertension(HTN) with prevalence estimates ranging from 5% to 15% in the general population. PA was first described by Conn in 1955. The classic features of PA are HTN, hypokalemia and metabolic alkalosis, but only a minority of patients without HTN. Plasma aldosterone to renin ratio (ARR) is the standard screening test. An ARR > 30 ng/dL per ng/mL/h when the PRA <1 ng/ mL/hour with plasma aldosterone concentration (PAC) ≥ 15 ng/dL has been shown to be high sensitive and specific for the diagnosis of PA. However, several studies indicate that some patients with PA have plasma aldosterone less than 15 ng/dL. Connshing syndrome named by W. Arlt et al. in 2017 is characterized by mixed over production of aldosterone and cortisol from adrenal adenoma. Here, we report a rare case of Connshing’ syndrome presenting as normotensive adrenal incidentaloma and the PAC is less than 15 ng/dl.
Case Report
A 53-year-old female staff with a history of chronic hepatitis B was transferred to our out patient department (OPD) due to the incidentally discovered a 1.0 cm left adrenal mass by the abdominal magnetic resonance Imaging (MRI). Diagnostic workup of adrenal incidentaloma was performed. 1 mg overnight dexamethasone suppression test was cortisol 6.03 μg/ dL. Plasma renin activity (PRA) was less than 0.07 ng/ mL/ hr with aldosterone 8.59 ng/dL. The 24 hours urine catecholamine was all within normal limit . Subclinical Cushing’ syndrome(SCS),but not PA was diagnosed because the aldosterone was less than 15 ng/ dL. Regular follow-up was suggested due to no clinical features of CS. Two years later, she suffered from newly diagnosed HTN and increasing body weight. She went back to our OPD for further evaluation. Repeat 1 mg overnight dexamethasone suppression test showed the cortisol level 3.68 μg/ dL. PRA, aldosterone was 0.19 ng/mL/hr and 9.73 ng/dL respectively.
Abstract 167
Connshing’ syndrome was highly suspected. I-131 NP-59 SPECT/CT scintigraphy was arranged and revealed moderate uptake in left adrenal gland.
Laparoscopic left adrenalectomy was performed with hydrocortisol 100 mg intravenous drip before operation for prevention of postoperative adrenal insufficiency. The pathologic report was adrenal cortical adenoma. 9 days after operation, the cortisol level was 10.28 μg/ dL and ACTH 15.9 pg/mL. 46 days after operation, Her HTN turned to normal without antihypertensive drugs and there was apparent weight loss.
78 days after operation, the cortisol level was 10.28 μg/ dL, ACTH 15.9 pg/mL, PRA 0.61 ng/mL/hour and aldosterone 7.78 ng/dL. Physiologic steroid dosage was prescribed. The patient’s condition was stable and regularly followed up at OPD.
Conclusions:
The correct diagnosis of patients with Connshing’s syndrome presenting normotensive adrenal incidentaloma is challenging for physician. The aldosterone level may be less than 15 ng/dL in primary aldosterone. NP-59 SPECT/CT is useful diagnostic tool for Connshing’ syndrome due to unilateral adrenal adenoma. Postoperative operative adrenal insufficiency may be delayed in Connshing’s syndrome with subclinical CS.
Annual Meeting of the Endocrine Society and the Diabetes Association of the R.O.C. (Taiwan) The45 th 168 March 23-24, 2024
A CASE OF LUNG ADENOCARCINOMA PRESENT WITH SECONDARY ADRENAL INSUFFICIENCY AND PRIMARY HYPOTHYROIDISM DUE TO PEMBROLIZUMAB
YU-CHING HUANG, CHING-CHU CHEN, JUEI-YU TSENG, YING YU TSENG, YI-TING CHIU, YUN CHI LEE, YI CHING TSAI
DivisionofEndocrinologyandMetabolism,DepartmentofMedicine,ChinaMedicalUniversity Hospital,Taichung,Taiwan
BACKGROUND: Pembrolizumab is an immune-checkpoint inhibitor, a highly selective anti-programmed death-1(PD-1) humanized monoclonal antibody which is approved for various malignancies, including non-small cell lung cancer, melanoma, cervical cancer, and Hodgkin lymphoma. It is now considered to be a main component of cancer therapy. However, it was associated with variety of adverse effects including pneumonitis, hepatitis as well as endocrinology systems such as hypothyroidism and adrenal insufficiency .
CASE REPORT: The patient is a 68-year-old male with a past medical history of lung adenocarcinoma with bilateral adrenal gland metastasis which was treatment with pembrolizumab, present with bilateral leg weakness for 3 days. Lab data reveal hypotonic hyponatremia latter attributed to secondary adrenal insufficiency and primary hypothyroidism secondary to pembrolizumab usage. After hydrocortisone and levothyroxine replacement. His serum sodium levels return to normal range.
CONCLUSIONS: Pembrolizumab associated irAE symptoms can be vague and unspecified. Thus, physicians should maintain a high index of suspicions when patient undergo immune check point inhibitors therapy.
Abstract 169
PE-17
OUTCOMES IN CHILDREN AND ADOLESCENTS WITH FOLLICULAR THYROID CANCER
1CHIA-JUNG HSU, 2SHU-FU LIN
1DivisionofEndocrinologyandMetabolism,DepartmentofInternalMedicine,ChangGungMemorialHospital, TaoyuanCity,Taiwan;
2DivisionofEndocrinologyandMetabolism,DepartmentofInternalMedicine,NewTaipeiCityTucheng Hospital,NewTaipeiCity,Taiwan
Background
To evaluate the characteristics, treatments, and prognosis in children and adolescents with follicular thyroid cancer (FTC).
Methods
Patients with follicular thyroid cancer aged < 20 years registered in Chang Gung Memorial Hospital thyroid cancer dataset between January 1979 and December 2021 were analyzed in this study. These data were compared to adults with FTC.
Results
Twenty-six children and adolescents with FTC were identified in this dataset, including 6 males and 20 females, with a median age at 17 years old (IQR, 13-18). One patient (3.8%) had lymph node metastasis and no distant metastasis were identified at diagnosis. Therefore, all patients had stage I disease according to the 8th edition of the AJCC staging system. Regarding surgery, most patients (42.3%) underwent total thyroidectomy, followed by lobectomy (7.7%). The majority of patients (92.3%) received radioactive iodine therapy with the median dose of 90 mCi (IQR, 60-140). One patient (3.8%) developed distant metastasis and all patients (100%) were alive during the median follow-up of 14.3 years (IQR, 5.6-24.5). As compared to adult patients, young patients received more conservative surgeries and had lower risk to develop distant metastasis.
Conclusions
The prognosis of children and adolescents with FTC is favorable, with low risk of distant metastasis and mortality.
Annual Meeting of the Endocrine Society and the Diabetes Association of the R.O.C. (Taiwan) The45 th 170 March 23-24, 2024 PE-18
PE-19
CASE REPORT: A CASE HAD HYPERTHYROIDISM COMBINE CEREBRAL VENOUS THROMBOSIS
1YING-YU TSENG, 2SHENG-TA TSAI, 1CHING-CHU CHEN
1DivisionofEndocrinologyandMetabolism,DepartmentofInternalMedicine,ChinaMedicalUniversity Hospital,Taiwan;
2DepartmentofNeurology,ChinaMedicalUniversityHospital,Taiwan
Introduction:
Cerebral venous thrombosis is an uncommon disease. There were some case reports discussion cerebral venous thrombosis connected with thyrotoxicosis. We plan to discuss one young female with uncontrol hyperthyroidism with cerebral venous thrombosis.
Case report
This is a 28 year old female with history of irregular control hyperthyroidism came with severe headache and dizziness for 1 weeks, came to our hospital for help and found cerebral venous thrombosis and hyperthyroidism. We had done thrombosis survey, She did not had atrial fibrillation. We had check coagulation PT,APTT, protein C and S and rule out other autoimmune disease case. We had control hyperthyroidism and use rivaroxaban treatment and thrombectomy, after treatment her clinical condition improve.
Discussion
Cerebral venous thrombosis is rare disease . It may appearance like acute stroke with dizziness or vertigo. It appearant on young and children, particular in young female. Hyperthyroidism has been associated with thrombocytopenia, coagulation factor abnormalities, and decreased fibrinolytic and plasminogen activities. Hyperthyroidism increases the risk of atrial fibrillation, and it also cause increase veinous thrombosis. But in our case, the patient did not had atrial fibrillation. Some special case repot show Graves’ Disease connected with Antiphospholipid Syndrome. May suspected connected with high fibrinogen, FIX, VWF, antithrombin (AT)- III), and PAI-1 in hyperthyroidism patient
Abstract 171
ANALYSIS OF RISK FACTORS FOR HIGH-RISK LYMPH NODE METASTASIS IN PAPILLARY THYROID MICROCARCINOMA
YI-HSIANG CHIU, SHU-TING WU, CHEN-KAI CHOU
DivisionofEndocrinologyandMetabolism,DepartmentofInternalMedicine,KaohsiungChangGungMemorial Hospital,Taiwan
Background:
Papillary thyroid microcarcinoma (PTMC) usually has an indolent course compared with other differentiated thyroid cancer (DTC). Despite having small tumor size, patients with PTMC have a relatively high incidence of lymph node metastasis. Previous studies reported some worse prognostic factors, such as the presence of high-volume lymph node metastases and extranodal extension leading to a higher recurrence rate. This study aimed to examine clinicopathologic factors and outcomes of high-risk lymph node metastasis in PTMC.
Methods:
We retrospectively reviewed 909 patients with PTMC alone who received thyroidectomy between January 2013 to December 2021 in Kaohsiung Chang Gung Memorial Hospital, Taiwan. A total of 88 patients with lymph node metastasis were enrolled for further analysis. High-risk lymph node metastasis (hr-LNM) is defined as high-volume lymph node metastasis (number > 5) and/or extranodal extension. Patients were grouped according to the presence or absence of hr-LNM. The clinicopathological factors associated with high-risk lymph node metastasis were analyzed.
Results:
A total of 88 cases with lymph node metastasis in the setting of PTMC were identified from the initial 909 patients, showing a prevalence rate of 9.7 % at our center. A total of 24 patients (27.2%) fulfill the definition of high-risk lymph node metastasis. Patients with hrLNM had a mean age at diagnosis was 47.0 ± 12.7 years, and the majority were female (15 females, 62.5%). The mean tumor size was 0.60 ± 0.27 cm. A significantly higher proportion of extrathyroidal extension (54.2% vs. 17.2%, p=0.001), multifocality (70.8% vs. 42.2%, p=0.017), and lateral lymph node metastasis (50.0% vs. 14.1%, p<0.001) were observed in the hr-LNM group. Patients with hr-LNM had higher proportion (23 cases, 95.8%) receiving
Annual Meeting of the Endocrine Society and the Diabetes Association of the R.O.C. (Taiwan) The45 th 172 March 23-24, 2024 PE-20
radioactive iodine therapy (23 cases, 95.8%). After a median follow-up period of 3.94 ± 2.38 years, patients with hr-LNM a less excellent treatment response rate (18 cases, 75%) and higher recurrence rate (2 cases, 8.3%).
Conclusions:
Extrathyroidal extension, multifocality, and lateral lymph node metastasis were associated with high-risk lymph node metastasis in PTMC. Patients with these characteristics had a higher recurrence rate. Therefore, cautious follow-up is necessary.
Abstract 173
A HASHIMOTO’S ENCEPHALOPATHY PATIENT PRESENTING WITH ACUTE ONSET OF NEUROCOGNITIVE BEHAVIORAL DISORDER: A CASE REPORT
1YEN-HSIN CHEN, 2YI-TING CHIU, 2YI-CHING TSAI, 2CHING-CHU CHEN, 2CHWEN-TZUEI CHANG, 2RONG-HSING CHEN, 2TZU-YUAN WANG, 2YUN-CHI LEE
1ChinaMedicalUniversity,CollegeofMedicine,Taichung,Taiwan; 2DivisionofEndocrinologyandMetabolism,DepartmentofInternalMedicine,ChinaMedicalUniversity Hospital,Taichung,Taiwan
This 36-year-old male, previously diagnosed with Graves’ disease and Graves’ orbitopathy, presented with acute onset of altered consciousness, characterized by lying still with eyes open but non-responsive. He was initially admitted to the emergency department. Laboratory tests showed primary hypothyroidism (TSH: 34.125 uIU/mL, Free T4: 1000 IU/ mL, TSH receptor antibody >40 IU/L, Thyroid-Stimulating Immunoglobulin >40.0 IU/L) and insignificant findings on other autoimmune panel tests.
Based on clinical, laboratory, and imaging findings, Hashimoto’s encephalopathy was suspected. The patient received a high-dose intravenous regimen of methylprednisolone 500 mg daily for 3 days, resulting in a rapid improvement in consciousness disturbance. However, symptoms recurred when the dose was tapered to 20-30 mg per day. Consequently, a maintenance dose of 40 mg per day of intravenous methylprednisolone was administered, followed by oral prednisolone 50 mg per day. The patient remained asymptomatic for 1 month and was maintained in a euthyroid state through thyroxine treatment for Hashimoto’s thyroiditis, along with a reduced oral prednisolone dose of 20 mg per day. There have been no neuropsychiatric alterations, and the patient has resumed his normal daily activities.
Annual Meeting of the Endocrine Society and the Diabetes Association of the R.O.C. (Taiwan) The45 th 174 March 23-24, 2024 PE-21
A RARE CASE OF MALIGNANT HYPERCALCEMIA THAT WAS CAUSED BY ECTPOIC HYPERPARATHYROIDISM
YI-CHING
TSAI, CHING-CHU CHEN,
CHWEN-TZUEI CHANG, RONG-HSHING CHEN, TZU-YUAN WANG, YING-YU TSENG, YI-TING CHIU, YUN-CHI LEE
DivisionofEndocrinologyandMetabolism,DepartmentofMedicine,ChinaMedicalUniversityHospital, Taichung,Taiwan
Background:
Malignant hypercalcemia is usually caused by excessive secretion of PTHrP from cancer cells and we could detected suppressed PTH level. There were only rare cases that reported some cancer cells secreted iPTH instead and resulted in malignant hypercalcemia.
Case:
This 53 years old female with a history of uterine myoma presented to emergency department due to epigastric pain radited to left flank and general discomfort for 1 month. The patient had nausea, poor appetie and constipation. She also reported vaginal spotting for 1 year. Laboratory test revealed acute pancreatitis (lipase: 429 U/L), acute kidney injury (Cr: 4.49 mg/dL, BUN: 89 mg/dL), hypercalcemia (Ca: 13.4 mg/dL) with elevated iPTH level (iPTH: 462.6 pg/mL) was noted. Abdominal CT without contrast revealed infiltration in peripancreatic region. There were enlargement of uterus and paraaortic lymphadenopathy noted. The patient was given aggressive hydration and NPO but the calcium level kept elevating. Her epigastric pain gradually improved but she still had poor appetite and complained of right lower quadrant abdominal dull pain. For hyperparathyroidism survey, thyroid echo and parathyroid scan disclosed no visible parathyroid lesion. Neck and chest CT with 3-D reconstruction didn’t dectected ectpic parathyroid lesion either. Ectopic secretion of iPTH was suspected. In addition, due to refractory hypercalcemia, we give her biphosphonate infusion once per week. Initially, it worked to control calcium level. But the following weeks, there was limited effect. Cancer work-up was done. Tumor marker (CEA: 195.43 ng/mL, CA125: 179.7 U/mL) showed elevation. PET scan showed heterogenous and intensely increased FDG uptake in uterus, uterine cervical region, paraaortic region, bilateral common iliac region and left supraclavicular region. She received dilatation and currettage for endometrium biopsy
Abstract 175 PE-22
and the pathology showed adenocarcinoma. She also received echo-guided biopsy for left neck mass and the pathology showed poorly differentiated carcinoma, metastatic. Endometrial cancer with paraaortic lymph node and left neck metastasis was diagnosed. She started paclitaxel, carboplatin for endometrial cancer treatment. However, there was no improvement of hypercalcemia. Another chemotherapy regimen with cisplatin and fluorouracil targeting poorly differentiated carcinoma was administered. Calcium level and iPTH level gradually decreased.
Discussion: There are some characteristics of cancer related ectpoic hyperparathyroidism. First, there was no dectable parathyroid lesion. Second, the iPTH level may be very high. In this case, endometrial cancer resulted in paraneoplastic syndrome with ectopic hyperparathyroidism and hypercalcemia.
Annual Meeting of the Endocrine Society and the Diabetes Association of the R.O.C. (Taiwan) The45 th 176 March 23-24, 2024
COMBINED TRADITIONAL CHINESE MEDICINE TREATMENT IN PATIENTS
WITH HYPERTHYROIDISM ASSOCIATED WITH LOWER RISK OF FRACTURE, HOSPITALIZATION RATE AND MORTALITY, A NATIONAL-WIDE POPULATION-BASED
STUDY
1,2CHIEH-HUA LU, 3,4CHI-HSIANG CHUNG, 5CHIEN-JUNG LIN, 1SHENG-CHIANG SU, 1FENG-CHIH KUO, 1PENG-FEI LI, 1CHIA-LUEN HUANG, 1LI-JU HO, 1JHIH-SYUAN LIU, 1CHIEN-HSING LEE, 1CHANG-HSUN HSIEH, 1YI-JEN
HUNG, 2,3WU-CHIEN CHIEN
1DivisionofEndocrinologyandMetabolism,DepartmentofInternalMedicine,Tri-ServiceGeneralHospital, SchoolofMedicine,NationalDefenseMedicalCenter,Taipei,Taiwan, 2DepartmentofMedicalResearch,Tri-ServiceGeneralHospital,NationalDefenseMedicalCenter,Taipei, Taiwan, 3SchoolofPublicHealth,NationalDefenseMedicalCenter,Taipei,Taiwan, 4TaiwaneseInjuryPreventionandSafetyPromotionAssociation,Taipei,Taiwan, 5DepartmentofChineseMedicine,Tri-ServiceGeneralHospital,NationalDefenseMedicalCenter,Taipei, Taiwan
Background: Previous studies have confirmed that hyperthyroidism is one of the common causes of secondary osteoporosis and can aggravate the disease severity in patients with osteoporosis. This study is mainly based on the Taiwan National Health Insurance Database (TNHID) and through big data analysis shows that combining traditional Chinese medicine (TCM) treatment can help the health of patients with hyperthyroidism and osteoporosis.
Methods: There were 4980 patients who received TCM treatment and 19920 controls who did not receive TCM treatment selected from TNHID in a 4:1 ratio of gender, age, and index year. Cox proportional hazards analyzes were performed to compare fracture, inpatient, and all-cause mortality over an average follow-up period of 15 years.
Results: A total of 4745/5823/3487 enrolled subjects (19.06%/23.39%/14.00%) suffered fractures/hospitalization/all-cause death which TCM group was 901/752/511 (15.10%/19.82%/ 10.26%); control group was 3993/4836/2976 (20.05%/24.28%/14.94%). Cox proportional hazards regression analysis showed that subjects in the TCM group had lower fractures, hospital mortality and all-cause mortality (adjusted HR=0.549; 95% CI=0.386-0.656, P<0.001; adjusted HR=0.599; 95 % CI=0.467-0.689, P < 0.001; adjusted HR=0.674; 95% CI=0.561-0.764, P < 0.001. Kaplan-Meier analysis showed that the cumulative risk of
Abstract 177
PE-23
fracture, hospitalization and death were lower in TCM group with significant differences (all log-rank P < 0.001).
Conclusion: The analysis of this study shows that patients with hyperthyroidism and osteoporosis combined with TCM treatment are associated with a lower risk of fractures, hospitalization, or all-cause death, providing clinicians with a treatment option.
Annual Meeting of the Endocrine Society and the Diabetes Association of the R.O.C. (Taiwan) The45 th 178 March 23-24, 2024
THE GLUCOTYPES AMONG PATIENTS WITH TYPE 2 DIABETES IN DIALYSIS
1YU-YUN CHOU, 1,2FENG-HSUAN LIU
1DivisionofEndocrinologyandMetabolism,DepartmentofInternalMedicine,ChangGungMemorialHospital, Linkou,Taoyuan,Taiwan.
2CollegeofMedicine,ChangGungUniversity,Taoyuan,Taiwan.
Background:
HbA1c limitations in diabetes and chronic kidney disease prompt the use of continuous glucose monitoring (CGM). We aim to evaluate glycotypes in patients with type 2 diabetes (T2D) and end-stage renal disease (ESRD) undergoing dialysis and those without ESRD through CGM.
Methods:
Patients with T2D and CKD or dialysis received CGM (Medtronic iPro®2 Professional or Guardian™ Connect) were recruited. Glucotypes were established by measuring ambulatory glucose profile (AGP) index. The various day-to-day change in dialysis and non-dialysis periods were compared. The primary outcome was time-in-range (TIR). The secondary outcomes included hypoglycemia and glucose variability.
Results:
A total of 31 participants with 16 non-dialysis and 15 dialysis subjects were enrolled. The baseline characteristics were similar between the two groups. The dialysis group exhibited significantly higher coefficient of variation (30.89±8.54 vs. 34.13±9.11%, P=0.039) and mean amplitude of glycemic excursions (MAGE) (5.94±2.04 vs. 7.62±2.29 mg/dl, P=0.046) than non-dialysis. No significant difference in glycemic variability was noted between hemodialysis (HD) and non-HD days. In the dialysis group, patients with peritoneal dialysis (PD) had higher glycemic mean index (GMI) (9.25±0.21 vs. 7.69±0.94%, P=0.045), continuous overlapping net glycemic action (CONGA) (13.66±2.43 vs. 9.29±2.21, P=0.027), J-Index (112.82±18.14 vs. 58.26±23.20, P=0.010), high blood glucose index (HBGI) (27.10±6.22 vs. 13.74±6.96, P=0.028), Glycemic Risk Assessment in Diabetes Equation (GRADE) (19.19±4.83 vs. 9.48±5.21, P=0.033), and M-value (49.33±17.32 vs. 18.27±12.36, P=0.009) than HD.
Abstract 179
PD-1
Conclusions:
Patients on dialysis show significantly elevated glycemic variability compared to those without dialysis. No significant variability differences were found between HD and non-HD days in patients with ESRD. Patients with PD exhibit higher glycemic variability and blood glucose levels compared to HD.
Annual Meeting of the Endocrine Society and the Diabetes Association of the R.O.C. (Taiwan) The45 th 180 March 23-24, 2024
A CASE OF MATERNALLY INHERITED DIABETES AND DEAFNESS WITH MITOCHONDRIAL A3243G MUTATION IN THE MT-TL1 GENE
1FU-SHUN KO, 1YUN-KAI YEH, 1JUI-HSIANG SUNG, 1WAN-YIN CHENG, 1,2CHII-MIN HWU
1SectionofEndocrinologyandMetabolism,DepartmentofMedicine,TaipeiVeteransGeneralHospital,Taipei, Taiwan; 2FacultyofMedicine,NationalYangMingChiaoTungUniversitySchoolofMedicine,Taipei,Taiwan.
Background:
Diabetes mellitus is a common disease with many types of clinical expression. Mutations in mitochondrial DNA (mtDNA) lead to the development of several disease and diabetes mellitus, particularly. Of these people with diabetes carrying the mitochondrial DNA mutation, symptoms of sensorineural hearing loss are common.
Methods:
We present a case with Maternally Inherited Diabetes and Deafness with mitochondrial 3243A>G mutation in the MT-TL1(Mitochondrially Encoded TRNA-Leu (UUA/G) 1) gene.
Results:
Case: A 46-year-old male with underlying disease with Diabetes Mellitus for 20 years was admitted to our hospital due to blood sugar fluctuation and easily fatigue in recent two months. After admission, insulin therapy adjustment was prescribed. During admission, we also arranged thorough survey for Diabetes mellitus type clarification due to maternaldominant family history. Genetic test for mutations in mitochondrial DNA was arranged and mitochondrial 3243A>G(m.3243A > G) mutation in the MT-TL1(Mitochondrially Encoded TRNA-Leu (UUA/G) 1) gene was reported. Level of blood sugar was acceptable for discharge and he was discharged with out-patient department follow-up.
Conclusions:
Maternally inherited diabetes with deafness is rare diabetes caused by mutations in mitochondrial DNA (mtDNA). Most of cases are associated with m.3243A > G mutation. Maternally inherited diabetes with deafness should be considered if strong family history with diabetes and symptoms of deafness without trauma related noted.
Abstract 181
PD-2
METABOLIC SYNDROME Z SCORE (METS-Z) RISK ASSESSMENT IN ASSOCIATION WITH DIABETES
PAUL WEI-CHE HSU, WAYNE HUEY-HERNG SHEU
InstituteofMolecularandGenomicMedicine,NationalHealthResearchInstitutes,Miaoli,Taiwan
Background:
Metabolic Syndrome (MetS) is traditionally diagnosed based on the presence of at least three out of five key indicators: blood glucose, triglycerides (TG), high-density lipoprotein (HDL), waist circumference, and blood pressure. However, this approach does not account for variations in gender and age, potentially leading to diagnostic biases.
Methods:
This study introduces a novel scoring system, MetS-Z, which assigns different weights to these five indicators based on individual gender and age. We analyzed baseline data from n=189,132 participants in the Taiwan Biobank, categorizing them by gender and into four age groups (20-39, 40-54, 55-64, 65+ years). Confirmatory factor analysis (CFA) was used to determine the relative importance of each indicator across different age and gender groups. This study evaluated the differences of MetS-Z scores between DM and nonDM at baseline. We also evaluated the changes of MetS-Z scores from baseline to development of new DM (n=1,984 out of n=46,458) over an average period of 4.49 ± 1.27 years for men and 4.44 ± 1.27 years for women.
Results:
Waist circumference emerged as the most crucial indicator for MetS-Z scores, with its significance increasing with age. The contribution of TG to MetS-Z scores decreased with age in men but increased in women. Utilizing logistic regression models demonstrated a progressive increase in DM likelihood with higher MetS-Z scores, with MetS-Z score 4.52 was linked to a 50% probability of having DM, while a MetS-Z score 6.76 indicated an over 80% probability of having DM. Overall, per unit increase in MetS-Z scores was associated with a 1.85-folds increases in the probability of having DM. In the following up dataset, higher MetS-Z scores at baseline were associated with higher chances of developing new DM, both for men (1.25, p value = 1.4e-132) and women (1.65, p-value = 1.6e-229).
Annual Meeting of the Endocrine Society and the Diabetes Association of the R.O.C. (Taiwan) The45 th 182 March 23-24, 2024 PD-3
Conclusions:
The MetS-Z scoring system offers a more nuanced risk assessment for metabolic syndrome, considering the critical factors of age and gender. This approach could be pivotal in precisely targeting individuals prone to develop DM and related metabolic disorders in the Taiwanese population.
Abstract 183
A CASE REPORT OF SEVERE HYPOGLYCEMIA DUE TO METASTATIC LUNG SARCOMA
JUI-HSIANG LI, SU-HUEY LO
DivisionofEndocrinologyandMetabolism,DepartmentofInternalMedicine,Tao-YuanGeneralHospital
A 68-year-old female was diagnosed with a left lung solitary fibrous tumor and underwent surgical resection in 2011. In January 2020, she had local tumor recurrence and underwent left radical pleurodectomy and tumor resection with hyperthermic intraperitoneal chemotherapy. She then received radiotherapy and chemotherapy. She also started on the targeted therapy agent with votrient.
In November 2023, she experienced an episode of acute loss of consciousness at night preceded by one month of cold sweating. Lab tests showed hypoglycemia with a blood glucose level of 5 mg/dL, along with a normal CRP of 0.1 mg/L, WBC count of 8,600/ μL. She was given intravenous glucose with subsequent regain of consciousness. Recurrent hypoglycemia with levels as low as 22 and 56 mg/dL was noted when intravenous fluids were discontinued. Further workup showed free T4 0.72 ng/dL, TSH 1.768 μIU/mL, ACTH 41.2 pg/mL, cortisol 9.7 μg/dL, C-peptide 0.24 ng/mL, insulin 10. First-line treatment is surgical resection, but chemotherapy and radiation may reduce tumor size and improve hypoglycemia to a lesser degree. If these measures fail, glucocorticoids or recombinant growth hormone can be used to increase gluconeogenesis and counter regulatory hormone levels.
In conclusion, recurrent hypoglycemia, especially with decreased consciousness, should prompt workup for IGF-2 secreting extra-pancreatic tumors in patients with known sarcomas.
Annual Meeting of the Endocrine Society and the Diabetes Association of the R.O.C. (Taiwan) The45 th 184 March 23-24, 2024 PD-4
CURRENT STATUS OF TREATMENT FOR DIABETES MELLITUS IN PREGNANCY IN A REGINAL HOSPOITAL
JUI-HSIANG LI, SU-HUEY LO, XIUWEN CHEN, XUE-MEI. LO
DivisionofEndocrinologyandMetabolism,DepartmentofInternalMedicineTao-YuanGeneralHospital
The number of pregnant women with Diabetes Mellitus in Pregnancy continues to increase. Good blood glucose control during pregnancy can reduce the incidence of complications, which is crucial for both pregnant women and fetuses. Our hospital has established a special GDM clinic, consisting of the Department of Obstetrics and Gynecology in our hospital and 9 surrounding gynecology clinics, to provide joint care. An analysis was conducted on patients from January 1, 2020 to December 31, 2021. A total of 154 patients had gestational diabetes(GDM), while 13 had preexisting diabetes mellitus (PDM). For blood glucose control methods, 144 (93.5%) GDM patients had dietary control, 6 (3.9%) used insulin therapy, 3 (1.9%) took oral medications, and 1 (0.6%) used basal insulin plus oral medications. Among PDM patients, 11 (84.6%) used insulin therapy, none took oral medications, 1 (7.7%) used basal insulin plus oral medications, and 1 (7.7%) had dietary control. Regarding family history, 74 (48.1%) GDM patients had a family history of diabetes, 72 (46.8%) had no family history, and 8 (5.2%) had an unknown family history. Among PDM patients, 6 (46.2%) had a family history while 7 (53.8%) did not. A chi-squared test was used for statistical analysis. According to the data, there was no significant statistical difference in terms of family history between the two groups (P>0.05). For prognosis, an oral glucose tolerance test with 75 g glucose was performed 4-12 weeks postpartum. It showed that 6 (3.9%) were diagnosed with diabetes, 11 (7.1%) had impaired fasting tolerance, 11 (7.1%) had impaired glucose tolerance, 45 (29.2%) had normal results, and 82 (53.2%) did not return for reexamination. Regarding GDM fetus outcomes, 136 (88.3%) were full-term births, 14 (9.1%) were premature births, and 4 (2.6%) were post-term births (over 40 weeks). Among PDM patients, 9 (69.2%) had full-term births while 4 (30.8%) delivered prematurely. A chi-squared test was used to compare differences between the two groups. According to the data, the GDM group had a higher proportion of full-term births (88.3% vs 69.2%), while the PDM group had a higher rate of premature births (30.8% vs 9.1%) (P=0.046). For delivery methods in GDM
Abstract 185 PD-5
patients, 106 (68.8%) had vaginal delivery and 28 (18.2%) had C-sections, while 23 (14.9%) only had one prenatal visit without returning for follow-ups. Among PDM patients, 7 (53.8%) had vaginal delivery and 6 (46.2%) had C-sections. For fetal birth weight, 14 (9.1%) GDM babies were underweight, 138 (89.6%) were normal weight, and 2 (1.3%) were overweight. In the PDM group, 12 (92.3%) were normal weight and 1 (7.7%) was overweight. To compare differences in low birthweight and overweight between the two groups, a chi-squared test was used. There was a significant difference in the data (P<0.05), indicating GDM mothers were more likely to deliver underweight infants, while PDM mothers tended to deliver heavier babies. However, due to the small sample size, a larger sample is needed for further verification.
The above results show that GDM patients had poorer follow-up visit compliance, possibly due to referring gynecologists not strongly requiring follow-ups and patients neglecting the importance of blood glucose management. The limited sample analysis also showed the PDM group had a higher premature birth rate, while GDM mothers were more likely to deliver underweight infants and PDM mothers tended to have heavier babies. Tightly controlling blood glucose levels in GDM and PDM patients to FPG <95mg/dl, 1hr PG <140, 2hr PG <120, HbA1c <6.0%, and glycoalbumin between 11.5-15.7% can help reduce complications in both mothers and infants.
Annual Meeting of the Endocrine Society and the Diabetes Association of the R.O.C. (Taiwan) The45 th 186 March 23-24, 2024
HEMOLYTIC ANEMIA DUE TO GLUCOSE-6-PHOSPHATE
DEHYDROGENASE DEFICIENCY IN A NEWLY DIAGNOSED TYPE 2 DIABETES.
1HUNG-CHUN CHEN, 2CHENG-EN TSAI, 3FENG-MING TIEN, 4*YING-CHUEN LAI
1DivisionofEndocrinologyandMetabolism,DepartmentofInternalMedicine,TaiwanUniversityHospital, Taiwan;
2DepartmentofInternalMedicine,TaiwanUniversityHospital,Taiwan;
3DivisionofDivisionofHematologyandOncology,DepartmentofInternalMedicine,TaiwanUniversity Hospital,Taiwan;
4DivisionofEndocrinologyandMetabolism,DepartmentofInternalMedicine,TaiwanUniversityHospital, Taiwan
Background: Severe hemolytic anemia is a serious complication in patients with glucose-6-phosphate dehydrogenase (G6PD) deficiency and can be triggered by a first hyperglycemic episode or induced by oral antidiabetics.
Case Report: A 47-year-old man with no significant medical history was admitted due to a near syncope episode. Laboratory tests revealed an extremely high blood sugar level of 798 mg/dl and other indicators suggesting hyperosmolar hyperglycemic state (HHS). The HbA1c level was 15.8%. Treatment with an intravenous insulin pump was initiated, followed by a transition to insulin glargine, metformin, repaglinide, and acarbose after HHS resolution. However, four days post-admission, a spiking fever was noted. Further laboratory tests showed indirect hyperbilirubinemia, anemia, and low haptoglobin levels, suggesting hemolytic anemia. The direct antiglobulin (Coombs) test was negative for anti-IgG and anti-C3. Blood smear examination indicated possible spherocytosis, but the eosin-5′-maleimide (EMA) assay for spherocytosis was negative, suggesting hereditary spherocytosis was unlikely. Markers for paroxysmal nocturnal hemoglobinuria (PNH) showed no evidence of PNH. G6PD levels were found to be very low (<1.0 U/gHb), indicating a G6PD deficiency. Oral antidiabetics were discontinued, and the patient was managed with subcutaneous insulin for glycemic control. His hemoglobin levels stabilized after one week.
Conclusion: For patients newly diagnosed with type 2 diabetes and presenting with hyperglycemia, measuring the G6PD level is recommended to avoid hemolytic anemia.
Abstract 187 PD-6
THE IMPACT OF PAY-FOR-PERFORMANCE PROGRAMS ON HOSPITALIZATION RISKS IN PATIENTS WITH TYPE 1 DIABETES
1 F U-SHUN KO , 1 YUN-KAI YEH, 2,3 HENG-JUN LIN, 2,3 YING-HSIU SHIH, 4,5,6,7CHIH-CHENG HSU, 1JUI-HSIANG SUNG, 1WAN-YIN CHENG, 1,8CHII-MIN HWU, 9FU-SHUN YEN
1SectionofEndocrinologyandMetabolism,DepartmentofMedicine,TaipeiVeteransGeneralHospital,Taipei, Taiwan;
2ManagementOfficeforHealthData,ChinaMedicalUniversityHospital,Taichung,Taiwan;
3CollegeofMedicine,ChinaMedicalUniversity,Taichung,Taiwan;
4InstituteofPopulationHealthSciences,NationalHealthResearchInstitutes,MiaoliCounty,Taiwan;
5DepartmentofHealthServicesAdministration,ChinaMedicalUniversity,Taichung,Taiwan;
6DepartmentofFamilyMedicine,Min-ShengGeneralHospital,Taoyuan,Taiwan;
7NationalCenterforGeriatricsandWelfareResearch,NationalHealthResearchInstitutes,,MiaoliCounty, Taiwan;
8FacultyofMedicine,NationalYangMingChiaoTungUniversitySchoolofMedicine,Taipei,Taiwan.;
9Dr. Yen’sClinic,Taoyuan,Taiwan
Background:
Individuals with type 1 diabetes (T1D) often experience a longer duration of diabetes, exposing them to a higher risk of diabetes-related complications. We conducted this research to investigate the Pay-for-Performance Programs (P4P) on hospitalization rates in patients with T1D.
Methods:
Using propensity score matching, we recruited 625 pairs of Type 1 Diabetes (T1D) patients with and without Pay-for-Performance (P4P) care from the National Health Insurance Research Database of Taiwan between January 1, 2006, and December 31, 2018. The study employed a multivariable Cox regression model to compare the risks of hospitalization for various reasons in T1D patients with and without P4P care
Results
T1D patients with P4P care had significantly lower risks of all-cause hospitalization (aHR 0.63, 95%CI 0.54-0.73), hospitalization for glycemic control or metabolic disorders (aHR 0.66, 95%CI 0.57-0.77), infectious diseases (aHR 0.5, 95%CI 0. 4-0.63), pneumonia (aHR 0.55, 65%CI 0.42-0.73), diseases of the circulatory system (aHR 0.64, 95%CI 0.53-0.76), diseases of the respiratory system (aHR 0.57, 95%CI 0.46-0.71) and mental health (aHR 0.5,
Annual Meeting of the Endocrine Society and the Diabetes Association of the R.O.C. (Taiwan) The45 th 188 March 23-24, 2024 PD-7
95%CI 0.33-0.76) than those without P4P care. No significant differences were observed in the risk of hospitalization for hyperglycemic crisis, severe hypoglycemia, or injury between T1D patients with and without P4P care.
Conclusions:
This nationwide cohort study showed that T1D patients with P4P care had significantly lower risks of hospitalizations, particularly for conditions related to glycemic control or metabolic disorders, infectious diseases, pneumonia, diseases of the circulatory system, diseases of the respiratory system, and mental health. P4P may be helpful in reducing the risk of hospitalization for patients with type 1 diabetes.
Abstract 189
A CASE OF EPISODES OF HYPOGLYCEMIA IN NON-DIABETIC ADULTS, SUSPECTED NON-ISLET CELL TUMOR RELATED
JUI-HSIANG SUNG, WAN-YIN CHENG, FU-SHUN KO, YUN-KAI YEH, CHII-MIN HWU
SectionofEndocrinologyandMetabolism,DepartmentofMedicine,TaipeiVeteransGeneralHospital,Taipei, Taiwan
Background:
Hypoglycemia poses a significant challenge in the glycemic management of diabetic patients undergoing insulin therapies and other anti-diabetic treatments, as persistent and severe episodes may carry the potential risk of fatality. However, this clinical issue is relatively uncommon among individuals without diabetes mellitus. Maintaining an optimal plasma glucose concentration is paramount for survival, leading to the development of physiological and behavioral mechanisms aimed at preventing or promptly correcting hypoglycemia. The differential diagnosis of hypoglycemia in non-diabetic patients encompasses various factors such as alcoholism, critical illnesses like hepatic, renal, or cardiac failure, sepsis, inanition, deficiencies in cortisol, glucagon, or epinephrine, non-islet cell tumors, insulinomas, noninsulinoma pancreatogenous hypoglycemia, and the presence of antibodies to insulin or insulin receptors. We present a 56-year-old man who has experienced multiple episodes of hypoglycemia characterized by sweating over the past two months. The suspicion is raised that these episodes may be related to a non-islet cell tumor.
Methods:
We present a 56-year-old man with multiple episodes of hypoglycemia presenting as sweating in recent 2 months, which is suspected non-islet cell tumor related.
Results:
A 56-year-old man was admitted to our hospital due to multiple episodes of hypoglycemia, manifested by sweating, over the past two months. His medical history included a malignant solitary fibrous tumor, ranging from 8 to 12 cm in size, located in the retrovesical space. He underwent repeated excisions in 2001, 2007, and 2009 due to tumor recurrence. Following the third surgery in 2011, a pelvic CT revealed a lobulated mass measuring 12 x 9.4 x 8.2 cm in the left portion of the pelvis, presumed to be a recurrent tumor.
Annual Meeting of the Endocrine Society and the Diabetes Association of the R.O.C. (Taiwan) The45 th 190 March 23-24, 2024 PD-8
This mass was larger than the one observed in 2009, leading to the initiation of Dacarbazine and Avastin treatment on August 21, 2011. In January 2012, the patient experienced episodes of sweating and palpitations at midnight, without reporting hunger or conscious loss. Selfmonitoring of blood sugar at home revealed hypoglycemia, prompting his visit to our hospital for further evaluation and management. The patient denied a history of diabetes mellitus, hypertension, thyroid disease, or other systemic illnesses, with no reported family history contributing to his current condition.
Several investigations were conducted in our ward, revealing low serum glucose, low serum IGF-1, and low C-peptide levels during hypoglycemic episodes. Thyroid function and morning cortisol were within the normal range. Based on his clinical presentation and the results of various examinations, a non-Islet Cell Tumor was suspected.
Conclusions:
Non-islet cell tumor-induced hypoglycemia is a rare paraneoplastic phenomenon that should be considered when evaluating non-diabetic patients experiencing unexplained hypoglycemic episodes, particularly if a large tumor is detected by CT or MRI. In such cases, it is advisable to check the IGF-II and IGF-1 ratio if feasible.
Abstract 191
FIBROSIS-4 INDEX IS LINK TO THE RISK OF CARDIOVASCULAR DISEASE IN PATIENTS WITH TYPE 2 DIABETES MELLITUS AND HEPATITIS C INFECTION
1GUAN-YU SU, 2PEI-CHUAN LEE, 1,3TSUNG-HUI WU, 3,4CHEN-TA CHI, 3,4,5YI-HSIANG HUANG, 1,3CHII-MIN HWU
1DivisionofEndocrinologyandMetabolism,DepartmentofMedicine,TaipeiVeteransGeneralHospital,Taipei, Taiwan;
2DivisionofEndocrinologyandMetabolism,BuddhistTzuChiMedicalFoundationDalinTzuChiHospital, Chiayi,Taiwan;
3DepartmentofInternalMedicine,SchoolofMedicine,CollegeofMedicine,NationalYangMingChiaoTung University,Taipei,Taiwan;
4DivisionofGastroenterologyandHepatology,DepartmentofMedicine,TaipeiVeteransGeneralHospital, Taipei,Taiwan;
5InstituteofClinicalMedicine,NationalYangMingChiaoTungUniversity,Taipei,Taiwan
Background:
The fibrosis-4 index has demonstrated its ability to independently predict major adverse cardiovascular events in individuals with nonalcoholic fatty liver disease. This study aims to investigate whether the fibrosis-4 index maintains an independent correlation with the risk of cardiovascular disease in patients diagnosed with both type 2 diabetes mellitus and hepatitis C infection.
Method:
We enrolled 104 patients diagnosed with both type 2 diabetes mellitus and hepatitis C infection in Taipei Veterans General Hospital from March 2022 to May 2023. Those who are younger than 18 year-old were excluded in this study. Each participant underwent comprehensive history taking and blood sample collection to determine fibrosis-4 index. The atherosclerotic cardiovascular disease (ASCVD) risk estimator was used to assess 10-year ASCVD risk.
Results:
The participants were categorized into three groups based on the tertiles of the fibrosis-4 index and significant differences were observed among these groups.
The high-tertile group exhibited an older age compared to the mid-tertile and low-tertile
Annual Meeting of the Endocrine Society and the Diabetes Association of the R.O.C. (Taiwan) The45 th 192 March 23-24, 2024 PD-9
groups (70.4 ± 5.2, 68.3 ± 6.3, and 62.4 ± 6.3, respectively, P < 0.001). Additionally, the estimated glomerular filtration rate (eGFR) was lower in the high-tertile group in comparison with the mid-tertile and low-tertile groups (72 ± 25, 84 ± 29, and 84 ± 29, respectively, P = 0.016). Furthermore, the high-tertile group demonstrated the highest 10-year ASCVD risk (30.6 ± 17.7, 29.8 ± 15.1, and 18.6 ± 11.5 in the high-tertile, mid-tertile, and low-tertile groups, respectively, P = 0.004) in this study. Though stepwise multiple regression analysis, with logarithmic transformation of the 10-year ASCVD risk, both eGFR and Log(fibrosis-4 index) emerged as independent variables correlated with the 10-year ASCVD risk (P=0.001 and P=0.040, respectively).
Conclusions:
Our findings suggest the fibrosis-4 index not only serves as a marker for assessing liver fibrosis but also as a potential predictor for evaluating cardiovascular risk in individuals with type 2 diabetes mellitus and hepatitis C infection.
Abstract 193
SERUM AMYLOID A TAKING VITAMIN A ENHANCES INSULIN
RESISTANCE IN ADIPOSE TISSUE THROUGH TLR4 SIGNALING
1PI-CHEN LIN, 2GUAN-MING KE, 3CHAO-HUNG CHEN
1DivisionofEndocrinologyandMetabolism,KaohsiungMedicalUniversityHospital,KaohsiungMedical University,Kaohsiung,Taiwan;
2GraduateInstituteofAnimalVaccineTechnology,CollegeofVeterinaryMedicine,NationalPingtungUniversity ofScienceandTechnology,Pingtung,Taiwan;
3GeneralResearchServiceCenter,NationalPingtungUniversityofScienceandTechnology,Pingtung,Taiwan
Background:
In clinic, serum amyloid A (SAA) are elevated in chronic inflammatory conditions including obesity and type 2 diabetes. Based on poor solubility in aqueous solutions, SAA is considered as apolipoprotein and presents aggregation and deposition in circulation. Clinic studies shows that SAA positively associates with Homeostasis model assessment-insulin resistance index (HOMR-IR). Therefore, SAA is seen as an aggressive factor of inflammation in chronic diseases, especially diabetes. However, pathological mechanism of SAA has not been understood.
Methods:
In animal study, regular β-carotene diet (4.5 μg/g chow deit) or high β-carotene diet (5 μg/g chow deit)-feed db/db mice were transduced with adeno-associated virus (AAV)carried plasmid of SAA combined with or without TAK-242 (TLR4 inhibitor) through vein injection for 4 weeks. . At end point, db/db mice were been sacrificed, and then blood were collected for detecting SAA, retinol, retinol binding protein 4 (RBP4), insulin, blood glucose, and calculated HOMR-IR; and adipose tissue were collected for analyzing SAA, and TLR signaling. Non-Denaturing Gel Electrophoresis was used to detect retinol binding to SAA and RBP4 of blood.
Results:
This study found that retinol to SAA, and HOMR-IR significantly increased in AAVSAA-transduced mice under regular β-carotene diet and high β-carotene diet. Moreover, under AAV-SAA-transduction, HOMR-IR in high β-carotene diet mice is higher than regular β-carotene diet mice. In adipose tissues, TLR4 signaling (IKK and NF-kB) expression
Annual Meeting of the Endocrine Society and the Diabetes Association of the R.O.C. (Taiwan) The45 th 194 March 23-24, 2024 PD-10
increased, but insulin signaling (IRS, PI3K, and Akt) reduced in AAV-SAA-transduced mice under regular β-carotene diet and high β-carotene diet. Similarly, above effects in high β-carotene diet mice were significantly higher than regular β-carotene diet mice. However, TAK-242 injection could reduce above conditions in vivo
Conclusions:
Above results concluded that retinol-binding to SAA induced the special activation of TLR4 signaling in diabetic adipose for enhancing insulin resistance.
Abstract 195
DIABETIC KETOACIDOSIS INDUCED BY SODIUM-GLUCOSE
TRANSPORTER 2 INHIBITOR IN A PATIENT WITH IMMUNE CHECKPOINT
INHIBITOR-TRIGGERED
TYPE 1 DIABETES: A CASE REPORT
LI-NA MA, DONG-HWA TSAI, SHI-DOU LIN
DivisionofEndocrinologyandMetabolism,DepartmentofInternalMedicine,ChanghuaChristianHospital, Changhua,Taiwan
Type 1 diabetes is a rare complication of immune checkpoint inhibitors (ICIs) and may be misdiagnosed as type 2 diabetes, leading to inappropriate treatment and unnecessary complications.
We reported a women diagnosed with immune checkpoint inhibitor-triggered type 1 diabetes. She developed diabetic ketoacidosis after sodium-glucose transporter 2 inhibitor usage.
The 66-year-old woman who developed type 1 diabetes after receiving pembrolizumab, an ICI, for invasive ureteral mid-urethelial carcinoma. Treatment with a sodium-glucose transporter 2 inhibitor induced diabetic ketoacidosis. Biochemical examination revealed extremely low fasting C-peptide levels, indicating extremely low insulin secretion. Subsequent glucagon stimulation tests showed no significant change in C-peptide concentration in the blood after glucagon injection. The patient’s blood sugar levels gradually stabilized after intensive insulin therapy.
This case reminds clinical physicians to remain highly vigilant for endocrine-related adverse reactions that may occur in patients receiving ICI treatment. When symptoms such as hyperglycemia occur, the possibility of type 1 diabetes should be considered so that early diagnosis and timely correct treatment can be given.
Annual Meeting of the Endocrine Society and the Diabetes Association of the R.O.C. (Taiwan) The45 th 196 March 23-24, 2024 PD-11
A PATIENT WITH MALIGNANT INSULINOMA AND MULTIPLE LIVER METASTASES: SYMPTOM IMPROVEMENT AFTER TREATMENT. - A CASE REPORT.
YUN CHI LEE, YI TING CHIU, YI CHING TSAI, CHING CHU CHEN
DivisionofEndocrinologyandMetabolism,DepartmentofMedicine,ChinaMedicalUniversityHospital
A 66-year-old male with hypertension experienced general weakness for at least 3 months.
According to the patient and his family, he suffered from general weakness for at least 3 months, accompanied by peculiar behavior, incoherent speech, and an unsteady gait upon waking up in the morning. Symptoms worsened with muscle weakness, and he was even unable to stand up. One day, the patient was found with a confused mental state, so he was taken to the emergency department, where hypoglycemia (30mg/dL) was diagnosed. Therefore, the patient was referred to us for the hypoglycemia survey.
During admission, the patient underwent a 72-hour fasting test. When hypoglycemia occurred, his blood glucose level was 35 mg/dL, C-peptide level was 11.7 ng/mL, and insulin level was 7.58 uIU/mL. He had normal liver function, normal thyroid function, and his cortisol level was within the normal range. Chromogranin A level was 135576.0 ng/mL (normal range: <101.9). The 24-hour urine 5-HIAA level was 64.34 mg/24hrs (normal range: 2-8). Insulinoma was highly suspected. Abdominal sonography showed bilateral multiple liver tumors, favoring metastatic tumors. Pre- and post-contrast enhanced abdominal and pelvic computed tomography revealed a mass in the pancreatic body and tail region with encasement of the splenic artery and splenic vein, and multiple masses in both hepatic lobes. A liver echoguided biopsy was arranged, and pathology reported a metastatic grade 1 neuroendocrine tumor. The mitotic figure is scanty (less than 1/10 HPF). Immunohistochemical study shows cytokeratin (+), Hep-par1 (-), CD56 (+), synaptophysin (+), and Ki-67 (2%).
Under the impression of a pancreatic body to tail neuroendocrine tumor with multiple liver metastases, NET Grade 1, Octreotide 0.2mg subcutaneous injection Q12H was given for 9 days. Afterwards, Lanreotide 120 mg every month and Sunitinib 12.5 mg/cap 3 caps every day were prescribed. Up to now, treatment has been ongoing for three months and continues. No hypoglycemia has occurred in the recent 2 months.
Abstract 197
PD-12
THE BENEFICIAL EFFECTS OF BEE POLLEN SUPPLEMENT ON METABOLIC SYNDROME COMPONENTS AND INFLAMMATION MARKERS: A TWO-YEAR OBSERVATIONAL STUDY IN A HEALTHY COHORT
JIA-PEI WU, CHAI-CHUN CHEN, JIUNN-DIANN LIN, CHIH-TSUENG HE, ANNE CHANG, CHUNG-ZE WU
DivisionofEndocrinologyandMetabolism,DepartmentofInternalMedicine,ShuangHoHospital,Taipei MedicalUniversity,Taiwan
Background: Bee pollen, known for its diverse range of health-promoting compounds such as polyphenols, flavonoids, phytosterols, and essential fatty acids, has the potential to be used as a therapeutic treatment for metabolic syndrome These components may enhance insulin sensitivity, improve inflammation, and regulate lipid profiles. However, there is a lack of extensive clinical research on the long-term effects of bee pollen. This study aims to evaluate the influence of bee pollen supplements on clinical parameters over a two-year period in a routine health examination.
Methods: Participants undergoing annual health examinations at a medical center were selected and categorized according to their usage of bee pollen supplements. We collected various physical and metabolic syndrome components, including body mass index (BMI), blood pressure, lipid profiles, blood counts, and C-reactive protein (CRP). The participants were matched on their age and gender and then reassessed after a period of two years. They were then divided into groups of c continuous, discontinued, and non-supplement for subsequent analysis.
Results: The study included 701 adults, among whom 15 consistently used bee pollen supplements. Additionally, there was a control group consisting of 30 persons without bee pollen supplements for comparison. Initial findings indicated that the supplement group had lower body weight, BMI, fasting plasma glucose, systolic blood pressure, and white blood cell counts. Although CRP levels were lower in the bee pollen group compared to the control group, the difference was not statistically significant. At the end of the follow-up, participants were reclassified into supplement and control groups. Both continuous and discontinued
Annual Meeting of the Endocrine Society and the Diabetes Association of the R.O.C. (Taiwan) The45 th 198 March 23-24, 2024 PD-13
groups displayed lower BMI, fasting plasma glucose, and CRP levels compared to the control group. The discontinued group also showed reduced white blood cell counts and fasting plasma glucose compared to control group.
Conclusions: Individuals with bee pollen supplements showed a decreased risk of obesity and hyperglycemia, enhanced control of blood pressure, and ameliorated inflammation. Significantly, those who ceased the supplement of bee pollen still had positive effects in terms of improving inflammation and fasting glucose levels.
Abstract 199
RELATIONSHIP BETWEEN GROWTH DIFFERENTIATION FACTOR-15 AND MUSCLE STRENGTH IN TYPE 2 DIABETES PATIENTS
1WAN-YIN CHENG, 1TSUNG-HUI WU, 1GUAN-YU SU, 1MENG-HAN CHIANG, 2SHIOW-CHWEN TSAI, 1CHII-MIN HWU
1DivisionofEndocrinologyandMetabolism,DepartmentofMedicine,TaipeiVeteransGeneralHospital.;
2 Chair ofInstituteofSportsSciencesUniversityofTaipei,Taipei,Taiwan
Background: Middle-aged and elderly patients with type 2 diabetes mellitus (T2DM) have worse mobility than non-diabetes, characterized by slower walking speed and poor physical performance. The peptide hormone growth/differentiation factor-15 (GDF-15) acts on the central nervous system, reduces dietary intake, and changes the autonomic tone, which may in turn affect muscle strength and physical performance. GDF-15 plasma concentrations are 1-2 folds higher in patients with T2DM than the controls. The effects of GDF-15 on skeletal muscle and physical performance need to be examined in individuals with T2DM due to their exposure to highers level of GDF-15 milieu.
Methods: We recruited 145 patients with T2DM for the present study, grouping them into three categories based on tertiles of baseline plasma GDF-15 levels. We successfully followed up with 143 patients over 12 months to assess the effects of GDF-15 on relative muscle strength and physical performance.
Results: At both baseline and follow-up, there were no significant differences in relative muscle strength among the three groups. While there were initial between-group effects in the Short Physical Performance Battery summary score and the timed up-and-go test, these differences disappeared after adjusting for age, sex, and baseline body mass index (BMI).
Baseline plasma GDF-15 levels showed a significant correlation with parameters of physical performance at both baseline and follow-up. However, this correlation was no longer observed after adjustments for age, sex, and baseline BMI.
Conclusions: This longitudinal study demonstrates that baseline plasma GDF-15 levels are not associated with indicators of relative muscle strength and physical performance. The contributions of circulating GDF-15 to muscle strength and physical performance appear to be neutral in patients with T2DM.
Annual Meeting of the Endocrine Society and the Diabetes Association of the R.O.C. (Taiwan) The45 th 200 March 23-24, 2024 PD-14
CORRELATION OF BRAIN-DERIVED NEUROTROPHIC FACTOR AS A PREDICTOR FOR PERIPHERAL NEUROPATHY IN PATIENTS WITH TYPE 2 DIABETES
1JUI-HSIANG SUNG, 1TSUNG-HUI WU, 1GUAN-YU SU, 1MENG-HAN CHIANG, 2SHIOW-CHWEN TSAI, 1CHII-MIN HWU
1DivisionofEndocrinologyandMetabolism,DepartmentofMedicine,TaipeiVeteransGeneralHospital,Taipei, Taiwan;
2InstituteofSportsSciences,UniversityofTaipei
Background:
Diabetic peripheral neuropathy (DPN) is the most prevalent chronic complications of diabetes, leading to great morbidity and impaired quality of life in patients. The precise mechanisms underlying DPN much remain enigmatic. A prevailing view suggests that deficiency in neurotrophins is a risk marker for DPN since a number of neurotrophic factors are impaired or altered in the progression of DPN. Among the neurotrophins, brain-derived neurotrophic factor (BDNF) appears to be a special character and becomes the target of the present study because it is crucial in modulating the maintenance and growth of neurons and affects synaptic efficiency and plasticity.
Methods:
To explore the assocaition between circulating BDNF and the marker of DPN, namely, the Michigan neuropathy screening score (MNSI-PE) in patients with type 2 diabetes
Results:
The patients were divided into three groups by tertiles of serum free BDNF. The three groups were comparable in the MNSI-PE score (P =0.95). The results of multivariate linear regression analyses showed that serum free BDNF was not an important covariate for the MNSI-PE score (P = 0.32). Stepwise multiple regression analyses were subsequently used to further observe the effects of clinical parameters on MNSI-PE scores. Duration of diabetes was entered into the model at the first step (P < 0.0001) and predicted about 11% of the variance of MNSI-PE scores. Fasting PG was entered into the model at the second step, eGFR the third step, WC the forth step, and age the fifth step. These additional variables explained
Abstract 201
PD-15
15 % more of the variance (Table 3). Serum BDNF was excluded from the model.
Conclusions:
In the present study, we demonstrated that there were no association between serum BDNF and MNSI-PE score in patients with type 2 diabetes. Serum BDNF levels may not be useful as a biomarker of DPN outcome.
Annual Meeting of the Endocrine Society and the Diabetes Association of the R.O.C. (Taiwan) The45 th 202 March 23-24, 2024
METFORMIN AND THE RISKS OF CELLULITIS, FOOT INFECTIONS, AND AMPUTATION IN PATIENTS WITH TYPE 2 DIABETES
1YUN-KAI YEH, 2,3,4JAMES CHENG-CHUNG WEI, 5,6KAI-CHIEH HU, 5,6TENG-SHUN YU,
7,8,9,10
CHIH-CHENG HSU, 1,11CHII-MIN HWU, 12FU-SHUN YEN
1SectionofEndocrinologyandMetabolism,DepartmentofMedicine,TaipeiVeteransGeneralHospital,Taipei, Taiwan;
2DepartmentofAllergy,Immunology&Rheumatology,ChungShanMedicalUniversityHospital,Taichung, Taiwan;
3InstituteofMedicine,ChungShanMedicalUniversity,Taichung,Taiwan;
4GraduateInstituteofIntegratedMedicine,ChinaMedicalUniversity,Taichung,Taiwan;
5ManagementofficeforHealthData,ChinaMedicalUniversityHospital,Taichung,Taiwan;
6CollegeofMedicine,ChinaMedicalUniversity,Taichung,Taiwan;
7InstituteofPopulationHealthSciences,NationalHealthResearchInstitutes,MiaoliCounty,Taiwan;
8DepartmentofHealthServicesAdministration,ChinaMedicalUniversity,Taichung,Taiwan; 9DepartmentofFamilyMedicine,Min-ShengGeneralHospital,Taoyuan,Taiwan;
10NationalCenterforGeriatricsandWelfareResearch,NationalHealthResearchInstitutes,MiaoliCounty, Taiwan;
11FacultyofMedicine,NationalYang-MingChiaoTungUniversitySchoolofMedicine,Taipei,Taiwan; 12Dr.Yen’sClinic,Taoyuan,Taiwan
Background: Patients with diabetes tend to have cellulitis, foot infections, and amputation. We conducted this research to compare the risks of cellulitis, foot infections, and amputation between metformin no-use and use in persons with type 2 diabetes.
Methods: Using propensity score matching, we identified 23234 pairs of metformin nonusers and users from the National Health Insurance Research Database of Taiwan, since January 1, 2000, to December 31, 2017. Cox proportional hazards models were adopted to examine the risks of incident cellulitis, recurrent cellulitis, foot infections, and amputation between metformin use and no-use.
Results: The mean follow-up period of metformin use and no-use was 6.31 (3.93) and 5.54 (3.97) years, respectively. Compared with metformin no-use, the adjusted hazard ratio and 95% confidence interval for metformin use in cellulitis development, recurrent cellulitis, foot infections, and amputation were 1.08 (1.04-1.12), 1.33 (1.14-1.55), 1.91 (1.75-2.09), and 1.88 (1.35-2.62), respectively. The longer cumulative duration of metformin usage had association with higher risks of these outcomes than metformin no-use.
Abstract 203 PD-16
Conclusions: This population-based cohort study revealed that metformin use had association with significantly higher risks of incident cellulitis, recurrent cellulitis, foot infections, and amputation than metformin no-use in patients with type 2 diabetes.
Annual Meeting of the Endocrine Society and the Diabetes Association of the R.O.C. (Taiwan) The45 th 204 March 23-24, 2024
THE IMPACT OF HEMODIALYSIS ON DIABETES MELLITUS
LI-YU KAO, TING-WEI LEE, TING-I LEE
DivisionofEndocrinologyandMetabolism,DepartmentofInternalMedicine,WanfangHospital,Taipei,Taiwan
Background:
Highlights the prevalence of chronic kidney disease (CKD) and end-stage renal disease (ESRD) in Taiwan, particularly in diabetes mellitus (DM) patients. Emphasizes the serious complications associated with hypoglycemia in DM patients undergoing regular hemodialysis. Introduces the concept of continuous glucose monitoring (CGM) as a tool for assessing glycemic variability.
Methods:
Describes the study’s participants, involving 9 DM patients undergoing maintenance hemodialysis, and the use of CGM for 5-7 days. Outlines the statistical analysis, including the calculation of mean blood glucose levels and the use of sample entropy to quantify glucose level fluctuations.
Discusses the comparison of postprandial CGM data before and after hemodialysis with age- and sex-matched non-dialysis patients.
Results:
Presents the general characteristics of the 9 hemodialysis patients with DM. Shows a progressive decrease in blood glucose levels during hemodialysis, reaching a nadir during the 1-2 hour intra-dialysis period. Indicates a potential impact of hemodialysis on postprandial glycemic variability, with lower postprandial glucose levels and reduced variability on hemodialysis days compared to non-hemodialysis days.
Conclusion:
Discusses the common occurrence of hypoglycemia in ESRD patients, emphasizing its association with diabetes mellitus. Compares the study’s findings with existing literature on CGM in dialysis, interpreting the results in the context of glucose control during and after hemodialysis. Explores the influence of hemodialysis timing on postprandial glucose levels and variability, relating it to previous studies.
Abstract 205
PD-17
SARCOPENIA AND SEVERE SARCOPENIA IN ELDERLY WITH AND WITHOUT DIABETES: A COMMUNITY-BASED STUDY
1,5WEI-FU HUANG, 2CHIA-CHUN LI, 2CHIN-SUNG CHANG, 4LYH-JYH HAO, 1CHWEN-YI YANG, 3HORNG-YIH OU
1DivisionofEndocrinologyandMetabolism,DepartmentofInternalMedicine,ChiMeiMedicalCenter,Tainan, Taiwan;
2DepartmentofFamilyMedicine,NationalChengKungUniversityHospital,CollegeofMedicine,National ChengKungUniversity,Tainan,Taiwan;
3DepartmentofInternalMedicine,NationalChengKungUniversityHospital,CollegeofMedicine,National ChengKungUniversity,Tainan,Taiwan;
4DivisionofEndocrinologyandMetabolism,DepartmentofInternalMedicine,KaohsiungVeteranGeneral Hospital,TainanBranch,Tainan,Taiwan;
5InstituteofGerontology,CollegeofMedicine,NationalChengKungUniversity,Tainan,Taiwan
Background: Whether the diabetes mellitus (DM) is associated with the risk of sarcopenia is an emerging issue. This study examines the prevalence and associated risk factors of sarcopenia in elderly individuals with and without diabetes living in a rural community, addressing a critical gap in geriatric health studies.
Methods: Through the comprehensive whole-community sampling methods, a total of 549 participants (285 men, 264 women) aged over 65 were randomly selected and thoroughly examined (response rate = 50%) in 2012 from the Tianliao District, southern Taiwan. The study utilized cross-sectional data, including detailed health questionnaires, anthropometric assessments, and biochemical tests. The waist circumference (WC) was measured (Gulick II, WI, USA; to the nearest mm) midway between the lateral lower rib margin and the superior anterior iliac crest at the end of a gentle expiration phase. A single frequency 8-electrode bioelectrical impedance analysis (BIA) device (BC-418; Tanita, Tokyo, Japan) was used to measure body composition, which had been validated to measure the skeletal muscle mass (SMM).Sarcopenia and severe sarcopenia were defined according to the 2019 update consensus of the Asia Working Group for Sarcopenia (AWGS). Participants were categorized into the DM group based on either medical history, blood HbA1c levels (≥6.5%), or fasting glucose (≥126 mg/dl), while others as the non-DM group.
Results: Of the 549 study participants, 66 (12.0%) were classified as having sarcopenia/
Annual Meeting of the Endocrine Society and the Diabetes Association of the R.O.C. (Taiwan) The45 th 206 March 23-24, 2024 PD-18
severe sarcopenia, including 11 with diabetes and 55 without diabetes. The prevalence of sarcopenia/ severe sarcopenia was comparable in the elderly non-diabetic population (55/420 = 13.1%) compared to the diabetic group (11/129 = 8.5%). Multiple logistic regression models indicated a clear association of sarcopenia/ severe sarcopenia with age (odds ratio [OR] 1.12, 95% confidence interval [CI] 1.06-1.19), female gender (OR 52.84, 95% CI 16.65167.72), body fat percentage (OR 0.90, 95% CI 0.86-0.95), and Min Nutritional Assessment score (<24) (OR 2.52, 95% CI 1.23-5.17). There is a trend of sarcopenia/severe sarcopenia (OR 3.07, 95% CI 0.48-19.75) along with the poor glycemic control (HbA1C < 5.7%, ≥5.7%<7%, ≥7%- <9%, ≥9%).
Conclusions: Approximately one-tenth of community-dwelling older adults in southern Taiwan, either with or without diabetes, faced the threat of sarcopenia/severe sarcopenia. Adequate nutrition and effective glycemic control emerged as crucial factors in reducing the risk of sarcopenia/ severe sarcopenia in the elderly. These findings have implications for geriatric health management and preventive strategies, particularly in rural settings.
Abstract 207
PANCREATIC INSULINOMA: A CASE REPORT
CHUN-YUAN HUANG, YU-PING HSIEH, PO-YIN LAI, SHANG-HSIEN WU, HAN-SHENG LU, MEI-CHEN YEH, CHEWN-YI YANG, HAO-CHANG HUNG
DivisionofEndocrinologyandMetabolism,DepartmentofInternalMedicine,ChiMeiMedicalCenter,Taiwan
This report presents the case of a previously healthy 42-year-old man, manifesting altered mental status and hypoglycemia during a work meeting. Emergency assessment revealed a blood glucose level of 46 mg/dL, promptly alleviated by glucose administration. The patient reported similar symptoms—cold sweating, blurred vision—following exercise the day before
Prompted by the patient’s altered mental status, a comprehensive diagnostic approach was adopted, including a 72-hour fasting test revealing hyperinsulinemic hypoglycemia. Imaging studies, comprising enhanced pancreas CT and magnetic resonance cholangiopancreatography, precisely localized a 2.2 cm neuroendocrine tumor at the pancreas head. Serum and urine markers remained within normal limits. The patient subsequently underwent laparoscopic excision of the tumor..
Pathological examination confirmed a grade 1 neuroendocrine tumor without lymph node involvement. Immunohistochemical stains were positive for chromogranin A and synaptophysin. Importantly, post-surgery, the patient remained free of hypoglycemic episodes. This case underscores the intricacies involved in the diagnosis and management of insulinoma. The 72-hour fasting test remains the gold standard for diagnosis. Surgical enucleation is the preferred treatment for the majority of insulinomas, with exceptions made for cases of extensive or malignant tumors. In instances where surgery is impractical or declined by patients, alternative treatments such as somatostatin analogs, alcohol ablation, radiofrequency ablation, or embolization have been explored. A multidisciplinary approach is imperative for the effective management of insulinoma.
Annual Meeting of the Endocrine Society and the Diabetes Association of the R.O.C. (Taiwan) The45 th 208 March 23-24, 2024 PD-19
DYSBIOSIS OF GUT MICROBIOTA IN PATIENTS WITH TYPE 2 DIABETES MELLITUS
1CHING-CHU
CHEN, 2YI-YAO HSU, 2ZI-LUN LAI, 2,3PO-REN HSUEH
1DivisionofEndocrinologyandMetabolism,DepartmentofMedicine,ChinaMedicalUniversityHospital, Taichung,Taiwan;
2DepartmentofLaboratoryMedicine,ChinaMedicalUniversityHospital,Taichung,Taiwan;
3DivisionofInfectiousDiseases,DepartmentofMedicine,ChinaMedicalUniversityHospital,Taichung,Taiwan
Background: Dysbiosis of gut microbiota has been reported to be associated with many metabolic diseases. In this study, we aimed to evaluate the differences of fecal gut microbiota composition between patients with type 2 diabetes mellitus (T2DM) and non-DM controls.
Methods: A total of 30 patients (17 males, mean age 58.1 yrs) with T2DM and 30 age, sex matched non-DM controls (17 males, mean age 58.6 yrs) were enrolled in this study. Fecal samples were collected in three tubes and stored at -20˚C before analysis. The full length 16S ribosomal RNA analysis using quantitative polymerase chain reaction was used to characterized the gut microbiota.
Results: Both the evenness and Shannon index of α diversity (within sample diversity) was significantly lower in T2DM group (Evenness, p=0.000572; Shannon index, p=0.046).
The beta diversity (Bray-Curtis dissimilarity) was also significantly different between T2DM group and control group (p=0.001). The species of Fusicatenibacter saccharivorans, Bifidobacterium longum, Ruminococcus bicirculans, Collinsella aerofaciens, Anaerostipes hadrus, and genera of Fusicatenibacter saccharivorans were significantly lower in patients with T2DM, while the species of Escherichia coli, Bacteroides caccae, and Bacteroides sp. were significantly higher in patients with T2DM.
Conclusions: Patients with T2DM showed a gut microbial dysbiosis. The causal relationship between T2DM and gut microbial dysbiosis needs further investigation.
Abstract 209
PD-20
VITAMIN E SUPPLEMENT PROVIDES BENEFICIAL EFFECTS ON METABOLIC SYNDROME COMPONENTS IN HEALTHY POPULATION
1,2CHAI-CHUN CHEN, 3,4DEE PEI, 1,2JIUNN DIANN LIN, 1,2CHIH-TSUENG HE, 1,2ANNIE CHANG, 1,2CHUNG-ZE WU
1SchoolofMedicine,DepartmentofInternalMedicine,TaipeiMedicalUniversity
2DivisionofEndocrinologyandMetabolism,DepartmentofInternalMedicine,ShuangHoHospital,Taipei MedicalUniversity,Taipei,Taiwan
3SchoolofMedicine,FuJenCatholicUniversity
4DivisionofEndocrinologyandMetabolism,DepartmentofInternalMedicine,FuJenCatholicUniversity Hospital,NewTaipeiCity,Taiwan
Background: Vitamin E, an essential nutrient, is recognized for its diverse benefits, including of antioxidative, anti-inflammatory, anti-obesity, and antihyperglycemic properties. However, the existing research on the effects of vitamin E is limited and produces inconclusive findings. The objective of our study was to examine the changes in metabolic syndrome components over a two-year period in individuals, specifically comparing individuals with and without vitamin E supplements.
Methods: A retrospective observational cohort study utilized a health examination database. The study enrolled 214 healthy individuals. Based on responses to a questionnaire, these subjects were divided into two groups: with and without vitamin E supplements. Data on the components of metabolic syndrome were gathered at two-year intervals. We analyzed the changes in metabolic syndrome components over a two-year period, comparing age- and sexmatched individuals across both groups.
Results: This study enrolled 214 healthy participants. Following sex and age matching, subjects with vitamin E supplements displayed lower body mass index, fasting plasma glucose, uric acid, body fat, and higher levels of high-density lipoprotein cholesterol. After two years, 52 participants continued with the vitamin E supplementation. This group, compared to subjects without vitamin E supplement, showed reductions in body mass index, weight, systolic and diastolic blood pressure, fasting plasma glucose, uric acid, triglycerides, waist circumference, body fat, and maintained higher high-density lipoprotein cholesterol levels.
Annual Meeting of the Endocrine Society and the Diabetes Association of the R.O.C. (Taiwan) The45 th 210 March 23-24, 2024 PD-21
Conclusions: Individuals with vitamin E supplements showed a reduced risk of developing obesity, hyperglycemia, hypertension, and dyslipidemia. The beneficial impacts of vitamin E administration were consistently maintained during a duration of two years.
Abstract 211
WHOLE TRANSCRIPTOME ANALYSIS REVEALS THAT SODIUMGLUCOSE CO-TRANSPORTER 2 INHIBITOR MIGHT MODULATE AUTOPHAGY AND INFLAMMATORY PROPERTIES OF PERIPHERAL BLOOD MONONUCLEAR CELLS IN PATIENTS WITH TYPE 2 DIABETES.
1FAN HSUAN-YU, 2LEE CHIEN-HSING, 2KUO FENG-CHIH
1DepartmentandGraduateInstituteofBiochemistry,NationalDefenseMedicalCenter,Taipei,Taiwan; 2DivisionofEndocrinologyandMetabolism,DepartmentofInternalMedicine,Tri-ServiceGeneralHospital, NationalDefenseMedicalCenter,Taipei,Taiwan.
Background: Sodium-glucose co-transporter 2 Inhibitor (SGLT2i) was widely prescribed for glycemic control in patients with type 2 diabetes due to its protective effects on cardiovascular diseases and nephropathy. However, whether SGLT2i could modulate the cellular function of peripheral blood mononuclear cells (PBMCs) in patients with type 2 diabetes is still largely unknown.
Methods: PBMCs were collected from patients with type 2 diabetes (n =3) before and after receiving three months SGLT2i therapy for performing total RNA-sequencing with functional exploration using Ingenuity Pathway Analysis (IPA). Hyperglycemia-mediated changes of transcriptomic landscape on human monocytes were also evaluated using in vitro cellular model (THP-1 cell line). Then, we integrated these two datasets of RNA-sequencing to pinpoint the most likely functional pathways in PBMCs that were modulated by SGLT2i administration.
Results: Our data disclosed total 217 differentially expressed genes (DEGs) (105 down-regulated and 112 up-regulated) were identified in PBMCs after SGLT2i treatment. IPA analysis further revealed top 3 canonical pathways that were significantly altered including “PPAR Signaling”, “Toll-like Receptor Signaling” and “Granulocyte Adhesion and Diapedesis”. In the human monocyte cell lines, we found total 1188 DEGs (573 downregulated and 615 up-regulated) were induced by hyperglycemia with functionally enriched on “Oxidative Phosphorylation”, “EIF2 Signaling” and “Mitochondrial Dysfunction”. Then, we performed integrative analysis and unveiled that total 26 DEGs (12 down-regulated and 14
Annual Meeting of the Endocrine Society and the Diabetes Association of the R.O.C. (Taiwan) The45 th 212 March 23-24, 2024 PD-22
up-regulated in PBMCs after SGLT2i therapy) were concurrently changed in these two RNAsequencing datasets, which were further functionally enriched for “Autophagy”, “IL-17A Signaling in Gastric Cells” and “TNFR2 Signaling”.
Conclusions: Our results suggest SGLT2i might possess functional roles to modulate autophagy and inflammatory properties of PBMCs in patients with type 2 diabetes. Further in vitro experiments are still required to confirm our observations.
Abstract 213
GLP-1 RA THERAPY TO ATTENUATE THE RISK OF OSTEOARTHRITIS AND TOTAL KNEE REPLACEMENT IN TYPE 2 DIABETES MELLITUS, A NATIONAL-WIDE POPULATION-BASED COHORT STUDY
1,2
CHIH-PING LIN, 3,4CHI-HSIANG CHUNG, 2CHIEH-HUA LU, 2SHENG-CHIANG SU, 2FENG-CHIH KUO, 2PENG-FEI LI, 2CHIA-LUEN HUANG, 2LI-JU HO, 5LAN-YUEN GUO, 3,6WU-CHIEN CHIEN
1DivisionofEndocrinologyandMetabolism,DepartmentofInternalMedicine,ZuoyingArmedForcesGeneral Hospital;
2DivisionofEndocrinologyandMetabolism,DepartmentofInternalMedicine,Tri-ServiceGeneralHospital, SchoolofMedicine,NationalDefenseMedicalCenter,Taipei,Taiwan;
3SchoolofPublicHealth,NationalDefenseMedicalCenter,Taipei,Taiwan;
4TaiwaneseInjuryPreventionandSafetyPromotionAssociation,Taipei,Taiwan;
5DepartmentofSportsMedicine,CollegeofMedicine,KaohsiungMedicalUniversity,Kaohsiung,Taiwan;
6DepartmentofMedicalResearch,Tri-ServiceGeneralHospital,NationalDefenseMedicalCenter,Taipei, Taiwan
Backgrounds:
Type 2 diabetes mellitus (T2DM) has been identified as an independent risk factor for knee osteoarthritis (KOA). This study is mainly based on the Taiwan National Health Insurance Database (TNHID), and through big data analysis, it shows that glucagon-like peptide-1 receptor agonists (GLP-1RA) treatment is helpful to T2DM had lower risk KOA or total knee replacement (TKR).
Methods:
There were 35,762 patients with T2DM were included. We divided these patients into 988 patients with T2DM without KOA and 372 patients with T2DM with KOA and received GLP-1RA treatment and those who did not receive GLP-1RA treatment and were matched with sex, age and inclusion date by 1:1 propensity score which included in the control group. Cox proportional hazards analyzes were performed to compare KOA risk and TKR rate during a mean follow-up period of 5 years.
Results:
There were 1976/744 patients with T2DM without/with KOA who received and did not receive GLP-1RA treatment, including 1052/322 males (53.24/43.28 %) and 924/422 females
Annual Meeting of the Endocrine Society and the Diabetes Association of the R.O.C. (Taiwan) The45 th 214 March 23-24, 2024 PD-23
(46.76/56.72 %). At the end of follow-up, there were 46/39 (4.66/10.48 %) patients with T2DM without/with KOA who received GLP-1RA treatment had KOA/TKR were lower than those without GLP-1RA treatment 87/70 (8.81/18.82 %). Cox proportional hazard regression analysis showed a lower rate of KOA/TKR for patient with GLP-1RA treatment (adjusted HR=0.852; 95 CI=0.784-0.930, P<0.001 / adjusted HR=0.913; 95 CI=0.885-0.977, P=0.015, respectively). Kaplan-Meier analysis showed that the cumulative risk of KOA/TKR in patient with/without GLP-1RA was significantly different (log rank, P<0.001 / P<0.001, respectively).
Conclusions:
This study hopes to provide clinicians with the option of GLP-1RA treatment for patients with T2DM with or without KOA, so that such patients will be associate with a lower risk of KOA or TKR rate.
Abstract 215
ASSOCIATION WITH LOWERING FRACTURE, INPATIENT AND MORTALITY RISK IN PATIENTS OF DIABETES WITH OSTEOPOROSIS COMBINED TRADITIONAL CHINESE MEDICINE THERAPY
1AN-CHE CHENG, 2,3CHI-HSIANG CHUNG, 4CHIEN-JUNG LIN, 1,5CHIEH-HUA LU, 2,5WU-CHIEN CHIEN
1DivisionofEndocrinologyandMetabolism,DepartmentofInternalMedicine,Tri-ServiceGeneralHospital, SchoolofMedicine,NationalDefenseMedicalCenter,Taipei,Taiwan;
2SchoolofPublicHealth,NationalDefenseMedicalCenter,Taipei,Taiwan;
3TaiwaneseInjuryPreventionandSafetyPromotionAssociation,Taipei,Taiwan;
4DepartmentofChineseMedicine,Tri-ServiceGeneralHospital,NationalDefenseMedicalCenter,Taipei, Taiwan;
5DepartmentofMedicalResearch,Tri-ServiceGeneralHospital,NationalDefenseMedicalCenter,Taipei, Taiwan
Background: Studies have confirmed that osteoporosis has been considered as one of the complications of diabetes, and the health hazards to patients are more obvious. This study is mainly based on the Taiwan National Health Insurance Database (TNHID). Through the analysis of TNHID, it is shown that the combined treatment of traditional Chinese medicine (TCM) medicine in patients of diabetes with osteoporosis (T2DOP) with lower related risks.
Methods: According to the study design, 3131 patients selected from TNHID who received TCM treatment were matched by 1-fold propensity score according to gender, age, and inclusion date as the control group. Cox proportional hazards analyzes were performed to compare fracture surgery, hospitalization, and all-cause mortality during a mean follow-up from 2000 to 2015.
Results: A total of 1050/1459/708 subjects (16.77%/23.3%/11.31%) had fracture surgery/ inpatient/all-cause mortality of which 433/624/318 (13.83%/19.93%) were in the TCM group /10.16%) and 617/835/390 (19.71%/26.67%/12.46%) in the control group. Cox proportional hazards regression analysis showed that subjects in the TCM group had lower rates of fracture surgery, inpatient and all-cause mortality (adjusted HR=0.479; 95% CI = 0.234-0.609, P<0.001; adjusted HR=0.571; 95% CI = 0.343-0.762, P<0.001; adjusted HR=0.723; 95% CI = 0.494-0.937, P=0.017). Kaplan-Meier analysis showed that the cumulative risk of fracture surgery, inpatient and all-cause mortality was significantly different between the case and
Annual Meeting of the Endocrine Society and the Diabetes Association of the R.O.C. (Taiwan) The45 th 216 March 23-24, 2024 PD-24
control groups (all log-rank p<0.001).
Conclusion: This study provides longitudinal evidence through a cohort study of the value of integrated TCM for T2DOP. More research is needed to fully understand the clinical significance of these results.
Abstract 217
COMPARING THE REAL-WORLD EFFECTS OF ONCE-WEEKLY GLP1 RAS AND DPP-4IS ON ISCHEMIC STROKE AND MYOCARDIAL INFARCTION IN INDIVIDUALS WITH T2D AND ASCVD
1XI TAN, 1YUANJIE LIANG, 1JIGAR R. RAJPURA, 1LARISA YEDIGAROVA, 1JOSH NOONE, 1LIN XIE, 2ADAM DE HAVENON, 3Y-C CHEN
1NovoNordiskInc.,Plainsboro,NJ,USA, 2DepartmentofNeurology,YaleUniversity,NewHaven,CT,USA, 3Novo Nordisk Taiwan.
Background: Despite guidelines advocating for their use, there is limited realworld evidence comparing the effects of once-weekly (OW) glucagon-like peptide-1 receptor agonists (GLP-1 RAs) and dipeptidyl peptidase 4 inhibitors (DPP-4is) on the risk of cardiovascular events in individuals with type 2 diabetes (T2D) and atherosclerotic cardiovascular disease (ASCVD).
Methods: This retrospective cohort study compared the time to incidence of ischemic stroke, myocardial infarction (MI), and 2-point major adverse cardiovascular events (MACE; ischemic stroke or MI) while on treatment in new adult users of OW GLP-1 RAs and DPP4is who had T2D and ASCVD using data from the Optum Clinformatics® Data Mart (20172021). Patients were followed until drug discontinuation, enrollment end, or an event. Inverse probability of treatment weighting was used to balance baseline characteristics, and survival analyses were conducted to compare risks during exposure, defined as continuous use of either drug.
Results: We found that users of OW GLP-1 RAs (weighted N=25,287) had significantly lower risks of ischemic stroke (HR=0.74 [95% CI, 0.63, 0.87]), MI (0.78 [0.67, 0.92]), and 2-point MACE (0.76 [0.68, 0.86]) compared with users of DPP-4is (weighted N=39,684; all P <0.01).
Conclusion: This study suggests that OW GLP-1 RAs reduce the risk of MI and stroke relative to DPP-4is in individuals with T2D and ASCVD.
Annual Meeting of the Endocrine Society and the Diabetes Association of the R.O.C. (Taiwan) The45 th 218 March 23-24, 2024 BP-1
BENEFIT OF DUAL THERAPY WITH GLP-1 RA AND SGLT2I ON CARDIOVASCULAR OUTCOMES IN TYPE 2 DIABETES
1BOCHRA
3,4
ZAREINI, 2THOMAS GERDS, 1KATHRINE KOLD SØRENSEN,
KIM K. B. CLEMMENSEN, 3KAJSA KVIST, 3JENS-PETER DAVID, 1CHRISTIAN TORP-PEDERSEN, 5Y-C CHEN
1DepartmentofCardiology,CopenhagenUniversityHospital–NorthZealandHospital,Hillerød,Denmark.
2SectionofBiostatistics,UniversityofCopenhagen,Copenhagen,Denmark. 3NovoNordiskA/S,Søborg,Denmark.
4StenoDiabetesCenterCopenhagen,Herlev,Denmark. 5Novo Nordisk Taiwan.
Background: Evidence on the cardiovascular benefit of dual glucagon like peptide-1 receptor agonist (GLP-1 RA) and sodium-glucose co-transporter-2 inhibitor (SGLT2i) therapy is lacking.
Aim: To compare the benefit of dual GLP-1 RA and SGLT2i therapy to other dual type 2 diabetes therapies with respect to heart failure and major cardiovascular adverse events (MACE).
Methods: From 2010-2021 patients from the Danish nationwide registries were followed from start of dual second-line type 2 diabetes treatment. Primary outcome was heart failure, and secondary outcomes were MACE and all-cause death. The estimated risk following 1 of 4 dual therapy combinations was determined using a longitudinal causal inference framework assuming all patients followed one dual therapy for 5 years.
Results: A total of 87,201 persons were included (GLP-1 RA and SGLT2i: 14,831, GLP1 RA and DPP4/SU/TZD: 20,417, SGLT2i and DPP4/SU/TZD: 22,803, dual DPP4/SU/TZD: 29,150). The 5-year risk ratio (95% CI) of dual GLP-1 RA and SGLT2i therapy compared to reference (dual DPP4/SU/TZD) for heart failure was: 0.93 (0.87;1.00), for MACE: 0.91 (0.87;0.95) and for all cause death: 0.78 (0.74;0.82), see Figure.
Conclusion: Dual therapy with GLP-1 RA and SGLT2i showed a benefit on heart failure compared to other dual therapies. Dual therapy with GLP-1 RA and SGLT2i showed a benefit on MACE and all-cause death compared to the reference treatment.
Abstract 219
BP-2
BENEFIT OF DUAL THERAPY WITH GLP-1 RA AND SGLT2I ON RENAL OUTCOMES IN TYPE 2 DIABETES
1BOCHRA ZAREINI, 2THOMAS GERDS, 1KATHRINE KOLD SØRENSEN, 3,4KIM K. B. CLEMMENSEN, 3KAJSA KVIST, 3JENS-PETER DAVID, 1CHRISTIAN TORP-PEDERSEN, 5Y-C CHEN
1DepartmentofCardiology,CopenhagenUniversityHospital–NorthZealandHospital,Hillerød,Denmark.
2SectionofBiostatistics,UniversityofCopenhagen,Copenhagen,Denmark. 3NovoNordiskA/S,Søborg,Denmark.
4StenoDiabetesCenterCopenhagen,Herlev,Denmark. 5Novo Nordisk Taiwan.
Background: There is increased use of dual glucagon like peptide-1 receptor agonist (GLP-1 RA) and sodium-glucose co-transporter-2 inhibitor (SGLT2i) therapy, but real-world evidence on the renal benefit is lacking.
Aim: To compare the dual use of GLP-1 RA and SGLT2i to other dual second-line type 2 diabetes therapies with respect to renal outcomes.
Methods: From 2010-2021 patients from the Danish nationwide registries were followed from start of dual second-line type 2 diabetes treatment. Outcomes were chronic renal disease, end-stage renal disease and >50% eGFR decrease from baseline. The estimated risk following 1 of 4 dual therapy combinations was determined using a longitudinal causal inference framework assuming all patients followed one dual therapy for 5 years.
Results: In total 87,201 persons were included (GLP-1 RA and SGLT2i: 14,831, GLP1 RA and DPP4/SU/TZD: 20,417, SGLT2i and DPP4/SU/TZD: 22,803, dual DPP4/SU/TZD: 29,150). The 5-year risk ratio (95%CI) of dual GLP-1 RA and SGLT2i therapy compared to reference (dual DPP4/SU/TZD) for chronic renal disease: 1.03 (0.97;1.08), end-stage renal disease: 0.12 (0.09;0.15) and >50% decrease in eGFR: 0.52 (0.45;0.59).
Conclusion: Dual therapy with GLP-1 RA and SGLT2i compared to other dual therapies results in greater risk reduction of end-stage renal disease and eGFR decline, while dual SGLT2i and DPP4/SU/TZD showed greater risk reduction of chronic renal disease.
Annual Meeting of the Endocrine Society and the Diabetes Association of the R.O.C. (Taiwan) The45 th 220 March 23-24, 2024 BP-3
LONGER TIME SPENT IN GLYCEMIC CONTROL AFTER INITIATING TIRZEPATIDE VS COMPARATORS: EXPLORATORY ANALYSIS OF SURPASS 1-5 TRIAL
1JULIO ROSENSTOCK, 2W TIMOTHY GARVEY, 3RACHEL L BATTERHAM, 4MINZHI LIU, 5BRANDON K BERGMAN, 5ANDREA HEMMINGWAY, 5VIVIAN THUYANH THIEU, 6JUSTINE CHUNG
1VelocityClinicalResearchatMedicalCity,Dallas,TX,USA;
2UABDiabetesResearchCenter,TheUniversityofAlabamaatBirmingham,Birmingham,AL,USA;
3CentreforObesityResearch,UniversityCollegeLondon;BariatricCentreforWeightManagementand MetabolicSurgery;UniversityCollegeLondonHospitalsNHSTrust;NationalInstituteforHealthResearch, UCLHBiomedicalResearchCentre,London,UK; 4Tigermed-BDMInc.,Somerset,NJ,USA;
5EliLillyandCompany,Indianapolis,IN,USA; 6EliLillyandCompany,Taipei,Taiwan
Purpose: Conventional trials in people with T2D typically report HbA1c at study end as the primary outcome. In SURPASS 1-5 trials, 81-97% of adults with T2D treated with the GIP/GLP-1 receptor agonist tirzepatide (TZP) (5, 10, or 15 mg) achieved an HbA1c <7.0% at the primary endpoint. Here we report the time spent in glycemic control throughout the duration of each trial.
Method: Participants were randomized to TZP (5, 10, or 15 mg) or comparator (placebo in SURPASS 1 and 5, semaglutide 1 mg in SURPASS 2, insulin degludec in SURPASS 3, and insulin glargine in SURPASS 4), with primary treatment durations of 40 or 52 weeks (wks). Continuous time spent with HbA1c <7.0% was descriptively analysed in all patients on treatment without rescue medication, with missing data imputed, in this post-hoc analysis.
Result: Participants on TZP 5, 10, or 15 mg spent longer time with HbA1c <7.0% than comparators. In studies of 40 wks duration, median time spent with HbA1c <7.0% was 32 wks for all TZP doses, 28 wks for semaglutide 1 mg, and 0 wks for placebo. In studies of 52 wks, this was up to 44 wks for TZP, 32 wks for insulin degludec, and 12 wks for insulin glargine. Time spent with HbA1c <7.0% was generally similar across all TZP doses in each study.
Conclusion: TZP allowed greater continuous time spent with HbA1c <7.0% vs placebo, semaglutide 1 mg, and basal insulins.
Abstract 221
BP-4
Previously submitted to the American Diabetes Association - 83rd Annual Scientific Sessions (ADA 2023)
the Endocrine Society
the Diabetes Association of the R.O.C.
The45 th 222
Annual Meeting of
and
(Taiwan)
March 23-24, 2024
“SURPASS(ING)” AN ERA OF BASAL-BOLUS INSULIN THERAPY: TIRZEPATIDE VS INSULIN LISPRO TID ADDED-ON TO POORLY CONTROLLED BASAL INSULIN-TREATED TYPE 2 DIABETES!
1JULIO
ROSENSTOCK, 2JUAN P. FRÍAS, 3HELENA RODBARD, 4SANTIAGO TOFÉ, 5EMMALEE SEARS, 5RUTH HUH, 5LAURA FERNÁNDEZ LANDÓ, 5HIREN PATEL, 6JUSTINE CHUNG
1VelocityClinicalResearchatMedicalCity,Dallas,TX,USA;
2VelocityClinicalResearch,LosAngeles,CA,USA;
3EndocrineandMetabolicConsultants,Rockville,MD,USA; 4DepartmentofEndocrinologyandNutrition,UniversityHospitalSonEspases,PalmadeMallorca,Spain;
5EliLillyandCompany,Indianapolis,IN,USA; 6EliLillyandCompany,Taipei,Taiwan
Purpose: Tirzepatide (TZP) is a once weekly GIP and GLP-1 receptor agonist for the treatment of type 2 diabetes (T2D). Efficacy and safety of once weekly TZP vs insulin lispro (iLispro) was assessed in people with T2D with inadequately controlled glycemic control on insulin glargine (iGlar) with or without metformin.
Method: In this 52-wk open-label, multicenter, Phase 3b study, 1428 patients with T2D (mean baseline [BL] age 59 y; T2D duration 14 y; HbA1C 8.8%; BMI 33 kg/m2; insulin glargine (iGlar) dose 46 IU/day) were randomized (1:1:1:3) to TZP (5, 10, 15 mg) or insulin lispro (iLispro) TID, as an add-on to iGlar ± metformin. Insulin doses were titrated to a target fasting and pre-prandial glucose of 100-125 mg/dL. Primary efficacy measure was change in HbA1C from BL for TZP (pooled) vs iLispro at 52 wk. Secondary measures were change from BL in fasting serum glucose and body weight (BW), and proportion of patients at HbA1C and BW loss goals (TZP pooled and each dose vs iLispro).
Result: At 52 wk, TZP (pooled) was superior vs iLispro in change from BL in HbA1C, achieving a mean HbA1C of 6.5% vs 7.6%, with substantially less in insulin use (iGlar: 13 IU/day vs 42 IU/day [iLispro 62 IU/day]) and BW loss of 10 kg vs gain of 4 kg, respectively. Rate of Level 2 and 3 hypoglycemia was 10-fold higher with iLispro. The most common adverse events with TZP were nausea, diarrhea, and vomiting of mild to moderate severity.
Conclusion: In conclusion, TZP demonstrated clinically meaningful and superior
Abstract 223 BP-5
glycemic and BW control vs iLispro associated with substantially less hypoglycemia and insulin use.
Previously submitted to the American Diabetes Association - 83rd Annual Scientific Sessions (ADA 2023)
Annual
of the Endocrine Society and the Diabetes Association of the R.O.C. (Taiwan) The45 th 224 March
Meeting
23-24, 2024