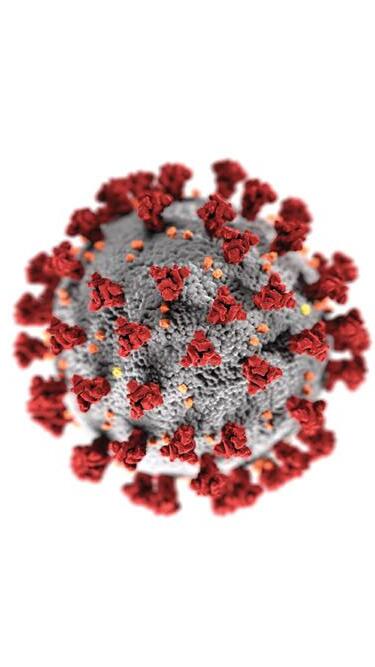
Ophthalmology & the Coronavirus SPECIAL FOCUS COVID-19 CATARACT & REFRACTIVE | CORNEA | RETINA | GLAUCOMA PAEDIATRIC OPHTHALMOLOGY May 2020 | Vol 25 Issue 5



YOUR NAVIGATING PARTNER IN CATARACT AND CORNEA www.ziemergroup.com The FEMTO LDV Z8 and the GALILEI are CE marked and FDA cleared. For some countries, availability may be restricted due to regulatory requirements. Please contact Ziemer for details.
Publisher
Carol Fitzpatrick
Executive Editor
Colin Kerr
Editors
Sean Henahan
Paul McGinn
Managing Editor
Caroline Brick
Content Editor
Aidan Hanratty
Senior Designer

Lara Fitzgibbon
Designer
Ria Pollock
Circulation Manager
Angela Morrissey
Contributing Editors

Howard Larkin
Dermot McGrath
Roibeard Ó hÉineacháin
Contributors
Maryalicia Post
Leigh Spielberg
Gearóid Tuohy
Priscilla Lynch
Soosan Jacob
Colour and Print
W&G Baird Printers
Advertising Sales
Amy Bartlett
ESCRS





Tel: 353 1 209 1100
email: amy.bartlett@escrs.org
Published by the European Society of Cataract and Refractive Surgeons, Temple House, Temple Road, Blackrock, Co Dublin, Ireland. No part of this publication may be reproduced without the permission of the managing editor.
Letters to the editor and other unsolicited contributions are assumed intended for this publication and are subject to editorial review and acceptance.

ESCRS EuroTimes is not responsible for statements made by any contributor. These contributions are presented for review and comment and not as a statement on the standard of care. Although all advertising material is expected to conform to ethical medical standards, acceptance does not imply endorsement by ESCRS EuroTimes. ISSN 1393-8983
P.46 EUROTIMES | MAY 2020 CONTENTS A EUROPEAN OUTLOOK ON THE WORLD OF OPHTHALMOLOGY www.eurotimes.org REGULARS 40 Outlook on Industry 42 Travel 43 Books 44 Industry News 46 Random Thoughts 47 Calendar SPECIAL FOCUS COVID-19 04 How the global pandemic has affected ophthalmology 06 UK doctors must rely on teamwork 08 The long-lasting impact of the virus 09 Dutch colleagues working together to save lives 10 A nightmare situation in Spain 12 Ups and downs in Germany 14 Looking to the future in France 15 Belgian doctors tackle the virus 16 The calm before the storm 17 Inside Ophthalmology: Waiting on the sidelines CATARACT & REFRACTIVE 18 New questions raised about the use of intracameral antibiotics 19 Using toric IOLs to reduce corneal astigmatism 20 Use of AI and smart lenses edges ever closer 21 The challenge of abnormal corneas 22 Corneal and refractive parameters used to avoid LASIK surprises 23 What impact does surgery have on the environment 24 Apps show benefits for IOL alignment 25 JCRS highlights CORNEA 26 Wavefront-guided transepithelial PTK for correcting irregularities 28 New handheld device useful for ocular surface quantification 29 Using OCT to diagnose early disease in computer users 30 Prompt treatment essential for corneal ulcers RETINA 32 Robot-assisted vitreoretinal surgery assessed 33 Measuring macular pigment can determine health 35 Perspectives and cautions on using AI GLAUCOMA 37 Treating patients with low IOP 38 Is there any benefit to using SMILE in young patients? P.17
As certified by ABC, the EuroTimes average net circulation for the 10 issues distributed between February and December 2019 was 47,863
MEDICAL EDITORS
New normal
The ESCRS will give the ophthalmology community every support


Dear Colleagues, I write this editorial on Easter Saturday, a beautiful day in the south of the Netherlands where normally the roads would be filled with bikers and hikers because of the long weekend. However, recreational traffic is forbidden and we have landed in a silent, Kafkaesque atmosphere that permits us time to reflect on these worrying and unique times for the medical community and all those on the front lines of battling the COVID-19 threat. It is our job to protect our loved ones, our colleagues and our patients. As a sign of hope and light in this period of Easter, in the last few days we welcome some positivity as there is a slight “flattening of the curve” visible in various European countries.
The ESCRS is committed to giving the ophthalmology community every support in the coming days, weeks and months. To encourage and facilitate communication, we have established an ESCRS COVID-19 website. www.eurotimes.org will publish weekly updates on how the virus is affecting ophthalmologists in their daily practices and how they can keep themselves and their patients safe. We will be reporting from your colleagues, their hospitals, their governments, the ophthalmology industry and the European Commission. We have created an online resource centre with protocols, guidelines and informational material from many countries across Europe. We will be updating the website as more material becomes available to us.
We do not intend any communications from ESCRS to either validate nor conflict with any local regulations or guidance. Please be aware that any information offered here in our magazine or on our website is not an endorsement by ESCRS of any procedures or activities.
The ESCRS annual Congress is scheduled to open on October 3rd 2020 in Amsterdam. We have no knowledge of what the situation will be at that time. We will keep you updated in the magazine and through all ESCRS communication channels.
INTERNATIONAL EDITORIAL BOARD






Noel Alpins (Australia), Bekir Aslan (Turkey), Roberto Bellucci (Italy), Hiroko Bissen-Miyajima (Japan), John Chang (China), Béatrice Cochener-Lamard (France), Oliver Findl (Austria), Nino Hirnschall (Austria), Soosan Jacob (India), Vikentia Katsanevaki (Greece), Daniel Kook (Germany), Boris Malyugin (Russia), Marguerite McDonald (USA), Cyres Mehta (India), Sorcha Ní Dhubhghaill (Ireland)
Rudy Nuijts (The Netherlands), Leigh Spielberg (The Netherlands), Sathish Srinivasan (UK), Robert Stegmann (South Africa), Ulf Stenevi (Sweden), Marie-José Tassignon (Belgium), Manfred Tetz (Germany), Carlo Enrico Traverso (Italy)
However, my dream still is that we will gather together in Amsterdam, and as Europeans and friends from all over the world have a moment to socialise and discuss what we have experienced, share our emotions and look forward to what our governments currently call “the new normal”.
The good wishes of the ESCRS Trustees, Council of Management and Executive are with you and your families to stay safe and well.
EDITORIAL 2
Emanuel Rosen Chief Medical Editor
José Güell
EUROTIMES | MAY 2020
Thomas Kohnen Paul Rosen
The ESCRS is committed to giving the ophthalmology community every support in the coming days, weeks and months
A WORD FROM RUDY MMA NUIJTS MD, PHD GUEST EDITORIAL
Rosen Chief José Güell
Rudy MMA Nuijts
Thomas Kohnen
Rudy MMA Nuijts President European Society of Cataract and Refractive Surgeons
Paul Rosen
THE BENZ ICE MANDREL
The Benz Ice Mandrel is the cold answer to your hydrophobic lens manufacturing problems

Just add water!
Precision Molded Optics
HF-1.2 | HF-2 | F156
What comes next after COVID-19
Ophthalmologists are facing their greatest ever challenge. EuroTimes
Executive Editor
Colin Kerr
looks at what the future may hold
At the time of writing this article all routine clinical activity, outpatient clinics and surgery has stopped for most ophthalmologists. Some patients may receive treatment for emergency vitreoretinal surgery, intravitreal injections for macular degeneration and trauma cases, but as the number of patients requiring treatment for illnesses caused by COVID-19 increases, this will change.
Since the outbreak of the virus in Europe, EuroTimes has run a series of articles on
eurotimes.org detailing the experiences of individual ophthalmologists in some of the countries worst hit by the virus.
In this issue of EuroTimes , key opinion leaders in European ophthalmology offer some hope for the future. This article summarises some of the key points they have raised.
ARTIFICIAL INTELLIGENCE
When ophthalmologists return to normality, or as close to normality as possible, they will need extra resources and support to help them adjust to the
new model of post-COVID healthcare. Artificial Intelligence solutions and supports will become increasingly important in the weeks, months and years ahead. That does not mean that ophthalmologists will become obsolete, as Professor Béatrice Cochener-Lamard pointed out in EuroTimes . ( EuroTimes Sept 2019: Vol 24; Issue 9; pp 4-7).
Prof Cochener-Lamard suggested that it should be up to doctors to define the mission to be fulfilled by AI. “That mission should be to assist in diagnosis and to ensure remote expertise with proposals
EUROTIMES | MAY 2020 SPECIAL FOCUS: COVID-19 4
for aetiology or decision-making. It is also important that we have guidelines, which will depend on the ethical rules and regulations of individual countries. No one stops progress; it is up to us doctors to do everything to support and control it,” she said.
HARMONISING HEALTHCARE POLICIES
As the President of the ESCRS, Professor Rudy MMA Nuijts, has pointed out, one thing that we have learned from the current crisis is that EU member states are not harmonised in their healthcare policies.

“Hopefully this crisis will provoke a paradigm shift for the future and lead to the level of solidarity and co-operation that we now already see on a micro level in our hospitals,” says Prof Nuijts.
HOMEWORKING
Physical distancing is one of the key strategies in preventing the spread of the virus. This has forced some ophthalmologists and their staff to work from home. While the majority of ophthalmologists, practice nurses and administrative staff will return to work, some may decide that home-working is a more effective way of carrying out their daily functions. If remote contact with patients, including teleconferencing, is introduced, this may become a model for some practices in the future.
LEADERSHIP
One of the key messages from recent months has been the importance of leadership and teamwork. Ophthalmologists have had to multi-task and take on roles that they would not previously have taken on in the past. While some doctors will be content to revert to their former roles in the future, others will be expected to take up leadership positions and to introduce new ideas and new ways of approaching ophthalmology.
The ESCRS Practice Management And Development Programme at the 38th Congress of the ESCRS in Amsterdam, The Netherlands, will include a special module on leadership.
“This period of great uncertainty will, I hope, lead to the opportunity and stimulus for innovation,” said Paul Rosen, Consultant Ophthalmic Surgeon at the Oxford Eye Hospital and Chairman of the Trustees of ESCRS and a former President of ESCRS. “Out of this adversity and tragedy we have to create opportunity, opportunity for people to excel, to show leadership, to innovate and to demonstrate what we can do for our fellow mankind.”
PATIENT FLOW
With elective procedures being cancelled, ophthalmologists will face long waiting
lists both in public and private practice, as they try to deal with the backlog caused by cancelled appointments. In some cases, patients will have formally contacted their ophthalmologist to inform him or her that they will not be presenting for treatment. A bigger problem is dealing with those patients who had underlying conditions but who decided not to contact their ophthalmologist in the knowledge that COVID-19 was swamping the healthcare system. This means that eye surgeons, who have been working around the clock in some cases on medical emergencies arising from COVID-19, may be overwhelmed by the pressure of dealing with the post COVID overflow. This will require significant investment in ophthalmology from national governments once hospitals and clinics reopen.
PUBLIC AND PRIVATE MIX AFTER COVID-19 OUTBREAK
Ophthalmology will return after COVID-19 but health administrators are likely to demand more co-operation between public and private clinics in the future. Ophthalmologists in both public and private practice may also need to recruit extra staff to deal with increased demand. “When clinics return to full opening, we will have to catch up with everything that has been delayed; cataract surgeries, vitrectomies and so on. We are already making plans for doing extra clinics and weekend surgery when this happens, though of course staff will need time off after the crisis so a lot of preparation will be needed,” says Carroll Webers MD, PhD, head of the University Eye Clinic Maastricht in The Netherlands.
RESEARCH
Research has effectively been suspended in most countries as the treatment of COVID-19 cases takes priority. This situation cannot continue effectively and steps will have to be taken not only to deal with the backlog of research cases suspended since the outbreak of COVID19, but ophthalmologists will also need to develop new research projects which will help them to deal with other viruses and other health emergencies in the future. In the meantime, the Journal of Cataract and Refractive Surgery is continuing to publish new research papers.
TRAINING
While formal training is on hold, young ophthalmologists will need support after COVID to allow them to resume their studies and take their exams.
Bruce Allan, consultant ophthalmic surgeons at Moorfields, UK offers some words of encouragement: “I am telling the trainees what I always have – you never stop learning, and while everything is on hold academically, there are plenty of really good resources online. Now is actually a very good time to put the hard yards in for the professional exams (when they come back).”
WHAT LIES AHEAD?
Finally, although there may be very difficult and very sad months ahead, the pervading message from the ophthalmologists that EuroTimes has interviewed is one of optimism. Sorcha Ní Dhubhghaill, Anterior Segment Ophthalmic Surgeon at the Netherlands Institute for Innovative Ocular Surgery (NIIOS) and Antwerp University Hospital says:
“As this tragedy unfolds, I have found a source of optimism and strength in the way this is bringing people together. My hope is that you too will find such pockets of strength, hope, and resilience, that will allow us to weather this storm together.”
SPECIAL FOCUS: COVID-19 5 EUROTIMES | MAY 2020
Hopefully this crisis will provoke a paradigm shift for the future and lead to the level of solidarity and co-operation that we now already see on a micro level in our hospitals
Rudy MMA Nuijts MD, PhD
COVID-19 success will rely on teamwork
Paul Rosen FRCS FRCOphth stresses the need for adaptability and the adoption of new working practices. Aidan Hanratty reports
How is this situation affecting ophthalmology in the UK? The UK Government has adopted a policy aimed at slowing the spread of the virus to protect the NHS and allow them to cope with those who are severely affected by the infection.
All routine clinical activity, outpatient clinics and surgery, has stopped. Certain things will continue for the moment, for example, emergency vitreoretinal surgery, and intravitreal injections for macular degeneration, but I suspect the latter may come to halt if the health service is overwhelmed.
It is extremely important to try and see the opportunities in this otherwise terrible situation. This includes people showing their leadership skills, working at the limits of their comfort zone and stretching their personal and clinical skills.
We have to look at our clinical practices and care pathways and challenge what has become established and adapt them for the current situation. For example do we need to see patients as frequently as we do, do we need to see them face to face or even at all? We have had to start telephone consultations, which you may think is not possible in ophthalmology, but you can gain a lot of information from talking to the patient – we are going back to the basics of taking a history from the patient.
In these very difficult circumstances, everyone is having to make significant compromises and at the moment we can’t deliver the perfect, ideal care that we have all previously aspired to.
The effects of COVID-19 will last many months, the NHS has taken over a number of Private Hospitals initially for three months with an option to extend; the suspension of routine activity has no end date proposed.
People are now working from home as much as possible to avoid coming into the hospital and risk transmitting or catching COVID-19. When the storm hits, ophthalmologists will, in addition to their own work, have to support those on the frontlines, in Intensive Care Units (ICU), respiratory wards and accident and emergency departments. We’ve been
asked what medical skills we have, which, if you’re a senior ophthalmologist, general medicine was a long time ago. The trainees who have done general medicine more recently, have already been drafted into supporting the physicians and ICU and we will be running the eye department on a skeleton staff. If the situation deteriorates, senior ophthalmologists will have to participate in acute medical services
Ophthalmologists are at increased risk because of the close proximity to patients during clinical examination and we are now using PPF3 masks for level 2 protection.
What sort of measures have you been taking in terms social distancing and keeping a distance from staff? It is quite difficult to maintain social distancing in the workplace, with staff and patients, in part due to the confines of the physical space in eye departments. We’re all wearing face masks in the clinics, with the level of protection dependent on the type of activity/intervention eg intravitreal injections, lasers, surgery.
We will need to address the requirement for people to re-skill their clinical, and in particular surgical skills after a period of three-to-six months without operating.
Success in dealing with COVID-19 will depend on great teamwork – every member, from the most senior surgeon to the newest administrator has a vitally important role to play. Without the support of the ‘troops’ on the ground we will not achieve success.
What is the situation with research and training? We have been told that we can’t submit new research proposals to the ethics committees or recruit or follow-up research patients. All our research nurses have been redeployed to the 16 COVID-related research projects that have just started in Oxford.
Routine training is no longer possible and all the Royal Colleges have cancelled the National Exams at least until September. It is important to emphasise that out of this disaster one can create opportunities and experiences which will be of lifelong value. Having to work in different circumstances, scenarios, and
situations at the edge of your “comfort zone” makes you evaluate your clinical practice and attitudes, and makes you take decisions that will challenge you. Therefore formal training is on hold, but there is still learning and training to be had in abundance.
What are your concerns about the impact on patients who might not be able to get in for appointments? In the Oxford Eye Hospital, we have triaged our clinics with all routine appointments deferred for four to six months. Urgent conditions are being seen, bearing in mind the risk to the patient, other patients, the general public and our staff. We have modified our post-op regime to reduce follow-up visits after surgery. The biggest problems are firstly the great unknown – we don’t know how long this is going to go on, and secondly if you’re cancelling thousands of appointments, there is the risk of losing patients completely, known as “lost to follow up”, resulting in permanent visual loss.
How do you see the future of ophthalmology in the UK after this? Very busy. Once everything has settled down, which may be a long time, there’s going to be a huge backlog, which will need to be managed. Patients are going to have to make significant compromises, for example needing cataract surgery. The way services are delivered may be very different with more use of Artificial Intelligence (AI) for consultations, as a part of imaging for virtual clinics and remote consultations. This period of great uncertainty will, I hope, lead to the opportunity and stimulus for innovation.
Out of this adversity and tragedy we have to create opportunity, opportunity for people to excel, to show leadership, to innovate and to demonstrate what we can do for our fellow mankind.
Finally, a key to success in dealing with this terrible situation is communication; between individuals, within specialties, within Eye Hospitals, within Nations and between colleagues across the world. I would like to congratulate the ESCRS team for their major contribution to this key element.
SPECIAL FOCUS: COVID-19 6 EUROTIMES | MAY 2020
Trifocal IOLs
When expectations and outcomes align
Premium trifocal IOL solutions for all your patients
• Advanced 16 diffractive step optic reduces light loss to only 11%:
- Improved contrast sensitivity
- Clinically-proven less photic phenomena

- Improved quality of night vision
• Smallest fully preloaded injector system*
The most complete family of trifocal IOLs in the industry
Speak to your Rayner representative today rayner.com/trifocal
Supplementary:
Support the best visual outcomes with...

An eye drop family designed specifically to support visual outcomes and patient satisfaction before and after surgery. rayner.com/aeon

A free mobile and web-based digital platform that collects powerful Patient Reported Outcomes (PROs) over three years. rayner.com/raypro




and
are proprietary marks of Rayner.
Intraocular Lenses Limited, 10 Dominion Way, Worthing, West Sussex, BN14 8AQ. Registered in England: 615539. EC-2019-122 12/19
*RayOne Trifocal, RayOne Trifocal Toric ©2020 Rayner. Sulcoflex, RayOne,
AEON
RayPRO
Rayner
Long-lasting impact of COVID-19
Ophthalmology has come to a standstill in northern Italy, with operating theatres being used as intensive care units. Cheryl Guttman Krader reports
The outbreak of COVID-19 in Europe began in northern Italy where Roberto Bellucci MD, practises in the city of Verona. The first cases in Italy were reported in mid-February, and as the number began to rise quickly, the government soon imposed a lockdown that brought ophthalmology care to a standstill.
“Ophthalmology in hospital settings in northern Italy is completely locked down as all hospital departments were converted to the care of COVID-19 patients. The lockdown is affecting both private and public hospitals, and the very operating theatres in these facilities are being used as intensive care units to save the life of the most seriously ill virus patients,” said Dr Bellucci.
Ophthalmology trainees in Italy, who include Dr Bellucci’s son, are now working as general practitioners taking care of infected patients.
“Teaching is suspended, and we do not know when it will begin again,” Dr Bellucci said, adding that the entire year 2020 may be lost for ophthalmology training.

Patients with ophthalmic emergencies or who require a small invasive procedure, such as for removal of a corneal foreign body, can still be seen in hospital emergency departments. Fear of contracting the coronavirus infection, however, keeps patients from coming, Dr Bellucci observed.
Ophthalmologists in private practice are seeing patients for emergencies and relying on each other to provide the necessary service.
“We continue to phone colleagues until
we find someone who can schedule a surgical appointment. The opening may require that the patient travel to another city, and with such limited availability, a wait time of at least one week is common for a patient needing repair of a retinal detachment,” Dr Bellucci said.
To protect themselves and patients, practices are following proper disinfection methods, using personal protection equipment, and following a strict scheduling limit. Despite those precautions, patients are staying away.
“We allow just one patient per waiting room per hour in our clinic,” Dr Bellucci said.
“The request for appointments, however, has been very low. In total, we see just 10-to-12 patients a week.”
FUTURE IMPACT
The inability to provide care could have devastating consequences for some patients, Dr Bellucci said.
In particular, he expressed concern about the prognosis for patients who had been receiving intravitreal injections to control exudative age-related macular degeneration.
“This treatment, which was 100% public, is no longer available to patients,” Dr Bellucci said.
“Depending on how long the lack of access continues, some patients will probably suffer permanent damage and loss of vision.”
Dr Bellucci said he is also worried about how the ophthalmology workforce will be able to address the need for services once the crisis is over.
“Each public facility has cancelled
thousands of appointments for visits, intravitreal therapy and cataract surgery. We do not know how we will meet this accumulating demand considering that the wait time for future appointments was already extending for months,” he explained.
“We can expect that our dedicated doctors and nurses will step up as much as they can to take care of this situation. There is a limit to what can be done, however, and we cannot ask our providers to double their work hours for months to come.”
Research was already suffering in Italy because of the country’s incredible bureaucracy, and Dr Bellucci said he expects nothing will change in that regard after the crisis is over.
Ophthalmology practice itself, however, may be changed forever.
“Nothing will be as it was,” Dr Bellucci predicted.
“Because of COVID-19, we will see practices restructuring their waiting rooms to avoid crowding, and we will probably see requirements issued by government authority. Maintaining proper distancing between patients will translate into a decrease in the number of patients we will be able to see,” he said.
SPECIAL FOCUS: COVID-19 8 EUROTIMES | MAY 2020
Each public facility has cancelled thousands of appointments for visits, intravitreal therapy and cataract surgery
Roberto Bellucci MD
Ophthalmology in hospital settings in northern Italy is completely locked down as all hospital departments were converted to the care of COVID-19 patients
Roberto Bellucci MD
Professional solidarity in The Netherlands
What is the current situation in The Netherlands? I live in Rotterdam and while schools and universities have been closed, we are not in lockdown mode as has been applied in Italy and France. People are still allowed to freely circulate and most of the shops are still open. However, restaurants, cinemas and theatres have closed and all public gatherings cancelled.
Most people are adhering to the guidelines in terms of social distance to try to contain the spread of the virus. However, there have been reports of people crowding in parks and on beaches.
What about your hospital? Are you still continuing to operate on patients? No, we stopped surgery in the O.R. under anaesthesia to try to reduce the demands on key staff and reduce the pressure on the intensive care units. We did complete some cataract surgeries before we took the decision to stop to protect ourselves and our patients. It simply didn’t feel safe to continue operating under the current circumstances so it was decided that it was better not to take the risk. Even with protection, there is the issue of proximity and we are obliged to administer drops in the eye and then at the end of surgery to remove the drapes, which increases the risk of exposure.
What about for emergency cases such as retinal detachments? Are they still being treated? We are continuing to treat emergency cases. In our outpatient department there are now only emergency cases or those that we know that we have to see and which can’t be postponed. We have streamlined our schedules and scaled down all our activity enormously. We have taken several measures to ensure everything runs smoothly.
There are 12 ophthalmologists in our department, five residents in training and two residents who are not in training yet. We also have four optometrists. Normally, one ophthalmologist serves as the supervisor of the outpatient department and one resident-in-training does the emergency clinic. The others are doing general clinics, specialised clinics or surgery.
But now, to spread the flow of patients, we have two residents doing the emergency cases to ensure greater space between each patient and reduce the risk of contamination. The supervisor focuses on keeping the entire operation running smoothly. We then have one ophthalmologist for triage who receives calls from non-ophthalmologist specialists in hospital and from general practitioners in the area and also patients who call the hospital. Our triage specialist then decides what course of action is most appropriate for each individual case and whether urgent intervention is required.
What about patients who require intravitreal injections? We are still doing intravitreal injections where absolutely necessary but with a lot of precautions. We use several waiting areas for the patients and use controlled circuits to keep contact to a minimum. The retinal doctors carefully examine each patient’s charts in advance and decide if it is safe or not to postpone the injection. But monocular patients and those deemed at high risk of visual loss are still being treated.
Have there been clear guidelines from the national authorities in terms of what measures to take in terms of treating patients during the COVID-19 epidemic? Up until now, it has been up to the individual hospitals the measures that they take. But there is a lot of dialogue with the Dutch Ophthalmological Society, which is starting to coordinate the national response.
I am working in the Amphia Hospital in Breda, which along with Uden, Tilburg, and ‘s-Hertogenbosch is one of the areas with the highest concentration of coronavirus cases. The hospitals in these three areas have been hardest hit by the crisis. Other areas in the north of the country are less affected for the moment.
However, the situation is evolving rapidly and the situation is changing almost hour by hour and we have to adapt to deal with new developments. We are working closely with other medical centres in the northern part of The Netherlands to organise transfers of surgical cases that can no longer be performed in our hospital in Breda.
This crisis looks like it will last weeks and probably months. Is The Netherlands equipped to deal with this epidemic over the longer term and how will it affect ophthalmic care going forward? I think the Amphia Hospital is doing a really good job at the moment in terms of its outbreak management and forward planning for what potentially lies ahead. They are scaling up a bit earlier than other hospitals, and have been transferring patients, including some COVID-19 patients to other centres in The Netherlands to reduce the pressure.
Every department in our hospital has been asked to assign onequarter of their doctors to go and help in the hospital to deal directly with COVID-19 patients. I am currently on standby to resume work as a general doctor and help with treating the expected upsurge in patients over the coming days and weeks, not in intensive care units but in the general clinic to help my colleagues.
I am having to rapidly brush up on both basic and emergency medicine in order to be able to do this effectively. Professional solidarity is very important at times of crisis like these. We are all in this together and I have been impressed by the level of dedication of my Dutch colleagues who are working together to tackle this epidemic and save as many lives as possible.
Nic Reus MD, PhD, spoke with EuroTimes contributing editor Dermot McGrath on the response to the COVID-19 pandemic in his country
SPECIAL FOCUS: COVID-19 9 EUROTIMES | MAY 2020
A Nightmare Situation
José L. Güell MD, PhD, spoke with EuroTimes editor Sean Henahan, about
the coronavirus situation in Spain
Spain is now in the middle of severe coronavirus outbreak. The virus can be found in all regions of the country, particularly in Madrid and Barcelona. One-fifth of the 50 million population is over the age of 65 and thus at increased risk of COVID-19.
José L. Güell MD, PhD, is associate professor of Ophthalmology at Barcelona’s Autònoma University, as well as being Director of the Cornea and Anterior Segment Unit at IMO Barcelona. He is also Past President of the European Society of Cataract and Refractive Surgery.

First of all, how are you doing? I’m fine, we’re at home, observing the nationwide shutdown. The situation is a nightmare. I am only visiting the clinic for emergency cases.
First the suggestion was for us to treat only emergency cases, but now this is mandatory. Any private clinics in Catalonia are only handling emergencies. Ophthalmologists in private clinics from today are going to start covering emergencies within the national health system. The public system is so busy dealing with corona patients that they are not able to deal with specialty requirements. Many ophthalmologists within the public hospital system are being asked to fill other positions beyond ophthalmology. All private
clinics with beds are now being used for corona cases by the national system.
What is the situation with testing? Until recently the level of testing has been quite low, and tests were only available for those who were sick. Things are changing every 24 hours. We now have sufficient testing for senior care facilities, and for anybody sick or not sick who is working in healthcare. Within the near future we hope to have enough tests for everyone. It is a similar situation to what happened in Italy, is happening in France and will happen in the UK and other places.
We are using the PCR (polymerase chain reaction) tests, but this is a complex test, requiring special facilities to evaluate results. I would like to see broader availability for other testing methods that are cheap and offer quick results, then follow-up with the PCR in positive cases.

It is easy to speak in retrospect, but it does seem that the government response was slow. But everybody was slow. Some in the healthcare system had been calling for preparation for the pandemic a while ago, but not all were calling for hard measures early on.
What is the situation with personal protection equipment? This is a critical issue, and should have been better planned. The situation has been bad for
Sophi Experience #sophifamily
the last four or five days. There is a significant lack of materials. I expect this situation to improve soon as efforts are now under way to make up the shortages. We need equipment for face protection, gloves and respirators for the OR. The situation varies regionally, with Madrid being the worst. I think we have enough equipment for today, the problem is the next few days.
How is the public support for healthcare workers in Spain? Every night at 8 pm, recently, everywhere, in small villages and large cities, there is a kind of public thank you. People stand on their balconies and clap together for healthcare workers returning from work. I hope they will include in their gratitude an appreciation not only for the healthcare workers, not just nurses and doctors, but all of the other people who are working in hospitals – the orderlies, the cleaning people, the maintenance and food service workers. They are taking equal amounts of risk.
What is your advice to colleagues in other areas? Ophthalmologists are among the most at-risk specialties because we work close with patients. Take all necessary precautions to protect yourself when treating patients, but also at home.
SPECIAL FOCUS: COVID-19 10 EUROTIMES | MAY 2020 www.sophi.info
«What really differentiates Sophi is the attention to detail which makes the surgery even more pleasant for the surgeon, the staff and above all the patient.»
Ches Heredia MD Philippines
Faros™ MAKING THE DIFFERENCE WITH LEADING INNOVATION

Precision and efficiency in eye surgery
The Faros surgical platform enables cataract, vitrectomy and glaucoma surgery of the highest level while constantly remaining comfortable and intuitively operable. The reliable flow control makes the surgeon’s work even easier and safer than before. In addition, the Faros impresses with versatility, innovative technologies, exceptional functionality and ease of use.
→ Available as an anterior platform or as a combined anterior/posterior platform
→ Cutting-edge dual-pump system with flow and vacuum control with its unique SPEEP Mode™
→ Proven easyPhaco® technology
→ Continuous Flow Cutter for traction-free vitreous body removal
Make the difference – with the new Faros: www.oertli-instruments.com

EYE SURGERY. SWISS MADE.
Not available for sales in the US NEW
A lot of ups and downs
Thomas Kohnen MD, PhD, FEBO
spoke with EuroTimes editor Sean Henahan, giving us an update on the coronavirus situation in Germany
First of all, how are you doing? I’m fine, but there are lot of ups and downs. We have prepared as much as we can. Germany is basically shut down, nobody should go out of the house. German guidelines now say you can’t have more than two people together. We have stopped short of the last step, where everyone is forced to stay home and not go anywhere. From our perspective, most of the German people understand this, but not everyone, which is a problem. The police can’t do, it is the responsibility of every citizen of Germany.
What is your day-to-day situation now and how have things changed in recent days? We have a very special situation, I am at a University clinic in the middle of Frankfurt. We have seen a big change in the last two weeks as we prepare for the COVID patients, those who have to be in intensive care. We as ophthalmologists don’t have much to do with this effort at the moment. We have cancelled all of our elective surgeries. We have gone from seeing 50-60 cases a day in our clinic to seeing only emergency cases. This includes retinal detachments, perforated globes, cases that need treatment because of pain. We are still doing some cases requiring intravitreal injections. At this point we are conserving our resources such as masks for emergencies. We also want to keep the older people at home. However, some of these older patients made decisions on their own that they do want to be treated to preserve vision.
We do also see emergency cases in the ambulatory clinic. We have to titrate care in the ambulatory clinic. We find out why they came in, and a senior ophthalmologist decides if they need immediate care, or can go home. For example even if a patient comes in with really bad dry eye we would send him home with some drops and ask him to come back when the circumstances allow this.
The current situation also requires logistical changes for my staff. Some have to stay home, or take over hours. It is very difficult just to keep everything running.
When you do have an emergency, what is the protocol? We have a protocol for COVID and non-COVID patients. We take the temperature and ask questions. If we don’t have signs, we treat them.
If it is a COVID patient with the recognised signs, we would not treat him in the eye clinic, we would transfer directly to our COVID clinic. This is where we have the emergency cases, as well as those under treatment. We have not had an emergency eye COVID case so far.
Are ophthalmologists being asked to work in clinical areas beyond their specialty skills? Not yet, but I have already prepared some steps for this. As physicians when the time comes we will do whatever we can.
Do you have enough personal protection equipment? At the moment we do. We had a donation from a company of 800 FFP3 masks. Looking ahead, this will be a big logistical problem.
Germany is said to have a relatively low COVID 19 mortality rate, of 0.4% compared with 5%-6% elsewhere.
We have had around 200 deaths as of 26 March. To date we have had less than 10 COVID patients in the ICU at the
University clinic, and no deaths. Yesterday we have started in Frankfurt to help our French colleagues from Strasbourg and took some IC patients from them. This has also been done in some other cities in Germany. The mortality in our country is dependent on the number tested, so it is a grey zone
You are at one of the busiest teaching hospitals in Germany. What is the impact of the crisis on training the next generation of ophthalmologists? We have had to cancel conferences including the AAD, an annual teaching meeting in March in Düsseldorf with 7,000 attendees. We try to do the best for our residents. They know there is a problem. We are not allowed to do teaching, as we have been preparing for COVID. The residents are not complaining. In our system, in contrast to the US, most residents are doing less surgery in the beginning of their education and are doing more in the clinic. We can do other things, learning by studying texts and watching videos. Once we are past the peak of the crisis we will come up with ideas and may even be able to improve on what we were doing before.
Your department is noted for research. What has been the effect of the crisis on ongoing research? This is a problem. We want to keep patients in the trials under way, but some of them don’t come in, but we do what we can. We prepare but can not really start any new trials at the moment. But because we have more time, there is the opportunity to catch up on the documentation side of research.
Do you have any COVID research underway? Yes, just this month in the ophthalmology department we have started some research. We are working with virologists and those in intensive care. People are so busy preparing for the catastrophe that they have little time to think about this. Once we are over this we can start. Now we might collect some samples and store them for later. We are also working with Prof Rudy Nuijts (President of the ESCRS) in the Netherlands to do some multinational projects.
You are also the editor of JCRS. What is status of the journal? The journal is ongoing. My secretary works from home and we continue to review and edit manuscripts online. We have a system working with our ESCRS and ASCRS offices to keep the flow of manuscripts going. Indeed, we have a little more time to do what we need to do because of what is going on. It is running very smoothly.
What are your thoughts for colleagues in other areas? This is a very tough time. Everybody is afraid, I’m afraid as well, for my family, for my peers, for everybody around me. We will get through it. Many things will change and we will see things differently. We need to stay positive, do our jobs and keep going. We will need to find ways to come back. I hope that laboratories all over the world will soon develop treatments and vaccines.
Let’s hope we can all get together in Amsterdam in October for the ESCRS Congress and in Las Vegas for the AAO. My hope is that we can all restart ophthalmology, doing research, sharing our friendships together, and bringing this field forward.
SPECIAL FOCUS: COVID-19 12
EUROTIMES | MAY 2020
Research Education Innovation
ESCRS’s vision is to educate and help our peers excel in our field. Together, we are driving the field of ophthalmology forward.

French Surgeons believe in the future
Béatrice
Cochener-Lamard
MD, PhD, told EuroTimes how the COVID-19 crisis is affecting ophthalmology in France

What does the lockdown mean for ophthalmologists in their daily practices?
The situation has led all specialties to massive deprogramming of surgeries and consultations, keeping open only a channel for medical and surgical emergencies. This reduction in usual activity was initiated before the lockdown, in the interest of citizens’ attitude aimed at limiting circulation of the population and therefore of the virus.
The medical community is showing an enormous mobilisation and a great surge of solidarity, and caregivers are offering their services in areas other than their specialties. For example, ophthalmologists are involved in the telephone regulation of emergencies and in screening centres.
Not all regions in France are affected to the same extent by the virus, but the examples from Italy put all hospitals in battle order, ready to deploy the capacity to care for the sick, support saturated areas, and prepare for the fight against this virtual enemy. As in many countries, the first fight is to ensure the protection of exposed individuals, starting with healthcare personnel. We are also alerting people to ensure that they have sufficient supplies of masks and alcohol-based solutions.
What is the future of French ophthalmology after COVID-19?
If in this unprecedented war, the sense of fraternity and commitment, which has characterised France through many battles, is expressed through touching support initiatives (such as a heartfelt
tribute honouring hospital teams paid by citizens on the balconies of major cities each evening), it is certain that the country, like the rest of the world, is anxious to advance towards the unknown in terms of the weapons to be deployed, the appropriate strategy to adopt and the time it will take to achieve the eradication that everyone dreams of.
What everyone fears above all is having to reintegrate the effect of the deprogrammed activity into the already busy agendas. This concern is especially high in ophthalmology where the average waiting time for an appointment is at least six months. As seen in previous world wars, we fear that confined patients with conditions such as glaucoma, diabetes, maculopathies and amblyopia will have abandoned self-care so that they develop irreducible pathologies.
If the crisis lasts several months, it is likely that some practices will be economically threatened and have difficulty retaining their staff, including secretaries, nurses, and orthoptists, which many doctors in private practice had to send home.
On the other hand, we dare to imagine that the positive lesson of this tragic period will be that the population gains a better civic sense and develops more responsible behaviour with regard to the rules of hygiene and respect for others.
We are all aware that we are writing a sad page in the history of mankind. It is certain that French ophthalmology will be happy to go back to work and will redouble its energy to make up as best it can for the time lost and the delayed care.
What is the future for research and training? Of course, there is currently no question of initiating a clinical trial or enrolling patients into ongoing trials. Every effort is being made, however, to monitor existing study participants.
We want to believe in the future and continue to design the research work.
Everyone is invited to use spare time not dedicated to the hospital to work on analysing clinical data collected before the crisis, writing about the state of the art and analysing the literature.
Regarding education, from primary school to university, and therefore a fortiori for medical students, residents, and fellows, courses are being maintained online and sometimes in small groups for the hospital team while respecting the necessary hygiene barriers. Currently, defence dates for examinations, theses and certification have been postponed until after May. They will happen.
What are you telling your trainees?
We do not need to tell them that they are going through a unique period in history, because spontaneously, they are generous and offer their energy and time. We can be proud of our young ophthalmologists. They will surely represent a particular generation having been enriched by this human tragedy from which they will emerge grown.
Our trainees are aware that the coming months may not be devoted solely to learning their specialty and that they will be mobilised on other fronts. They are staying the course by dividing their time between emergency management, supporting activities around COVID-19 and deepening their basic knowledge. Depending on the duration of the crisis, the Ministry of Education may discuss offering trainees an additional six months of conventional training in ophthalmology. We hope we do not have to use it!
In case of ophthalmic emergencies, where can patients be treated?
Emergency lines are being maintained by hospitals and several clinics.
SPECIAL FOCUS: COVID-19 14 EUROTIMES | MAY 2020
The medical community is showing an enormous mobilisation and a great surge of solidarity , and caregivers are offering their services in areas other than their specialties
Béatrice Cochener-Lamard MD, PhD
Tackling COVID-19

Marie-José Tassignon still believes an adequate battle against COVID-19 will save lives in her native Belgium. Aidan Hanratty reports
Marie-José Tassignon’s department at the University Hospital of Antwerp (UZA) started to decrease the number of contacts with patients. New patients and basic cases were cancelled, while the hospital director called for the cancellation of as much elective surgery as possible. Postoperative controls were done by phone, thereby reducing hospital footfall.
A few colleagues became COVID-19 positive, but all recovered very well.
The only cataract procedures now being carried out are for paediatric patients.

“If we don’t operate on them, they lose vision and they lose potential for social integration later,” she said. “Babies and children don’t seem to be a target for the COVID19 virus.
Her hospital has a daily update at 5pm: “The medical director gives indications
of what should be done, and the hospital website gives you alerts when something has been decided.” These are crucial for ophthalmology as they are dealing specifically with the conjunctiva and tear film and examination occurs at short distance to the patient.
Directions need to be implemented and this requires strong leadership, improvisation and optimal communication. “Some colleagues turn out to be very talented in creating a positive atmosphere and avoiding chaos. They deserve special thanks.”
Prof Tassignon’s take-home message is simple. “Take it seriously. Pay attention to clean everything you look, at and which may be a source of contamination. Clean it with alcohol before starting your consultation. Have a second critical look around of what may be a potential source to spread the virus and clean it again with alcohol. Wear a mask and gloves and
protect your eyes with special shields.”
Another key message is that if you must check a patient’s intraocular pressure, use your hands (with gloves) and no air puffs, as the puff may cause the spreading of tear drops.
By March 23, no more than three doctors were present at once at the outpatient clinic.
“The good news is that we know there will be an end of this pandemic. Although, we must be prepared that there may be a second peak after this, so be aware that recovering your normal working rhythm will take time.”
This pandemic will be memorable but solidarity has never been so high, believes Prof Tassignon, with ophthalmologists volunteering to help in non-ophthalmology wards. They are the real heroes, she said. “You cannot put the clock back, but we have to believe that when following the rules, we shall overcome,” she said.

SPECIAL FOCUS: COVID-19
15 EUROTIMES | MAY 2020
10 Year Limited Warranty
The excellent optics and the superior mechanics make a Haag-Streit slit lamp one of the best investments you can ever make for your practice.
www.haag-streit.com HAAG-STREIT SLIT LAMP
Calm before the storm
Oliver Findl MD, PhD, Chief of the Department of Ophthalmology at Vienna Hanusch Hospital, Austria, spoke with Dermot McGrath on measures taken to deal with COVID-19

What is the current situation in Austria?
All schools and universities are closed, as are cafes and restaurants, theatres, shops and so forth. Only supermarkets and essential services such as banks and post offices remain open. The request to limit social contact seems to have been respected by the vast majority of the population. It is quite strict, as needs to be the case to contain the virus, and you need to have a valid reason to be outside and can only do so in the company of your immediate family members living in the same household. The police will intervene if they see groups gathering in public places and fines are in place for any breach of the regulations concerning confinement and social distancing. The duration of the confinement measures was supposed to last for at least four weeks in total, but that could change depending how the situation evolves.
What about your hospital and the health services in general? What measures have been put in place to deal with the epidemic? At the moment there are still relatively few cases of COVID-19 in Austria, at least compared to countries such as Italy, Spain and France. Our hospital has set up two separate triage stations: one for personnel and one for patients. Everyone who comes to the hospital answers a series of questions relating to possible COVID-19 infection and has their temperature taken. It is only once they have passed screening that they are allowed on to the hospital premises.
In terms of ophthalmic care, all elective surgery has been cancelled and we only see patients in the outpatient setting who require emergency treatment such as retinal detachment, trauma and so forth. We have stepped up protective measures in our clinics, all of which have now been fitted with plexiglass shields on the slit lamp. There is greater use of masks as
well but there is still some debate about the utility of using them in all situations. We try to keep at least two metres’ distance between personnel and not to stay in the same room with a colleague for more than 15 minutes at a time. This is a precaution in case one of the personnel turns out to be infected with COVID19. If we keep those rules then the personnel who have been in contact with the infected staff member are defined as category 3 risk and not category 1 and 2. Personnel who fall into the latter categories 1 and 2 need to go into quarantine for two weeks, whereas the measures are less stringent for category 3 and allows the hospital to maintain staff levels high at a time when they are needed most.
We have split up into three teams, two of which work from home offices at any given time while the other team is in the hospital. Each team has a set number of doctors, nurses, orthoptic staff and secretaries and we rotate shifts to ensure that there is rolling coverage at all times
What about patients who require intravitreal injections? We have considerably reduced the volume from around 60 patients a day before the coronavirus crisis to around 25 a day in the current circumstances. We have gone through the patient records and are seeing those who require treatment the most. We are not seeing the patients in our hospital here in Vienna but are using a centre off site where our staff go to administer the injections. The idea is to protect the hospital here as much as possible.
How are resident ophthalmologists being managed during the crisis? Training has been severely restricted of course given the exceptional circumstances that the entire medical profession is facing. But the residents who are working from home have been given work packages with particular assignments that they
can complete during this period, whether it is writing up studies for peer-review publications or other work. They have also been asked to research COVID-19 and become familiar with this particular family of viruses. The next step will probably be to have them refresh their knowledge of emergency and intensive care treatment in case they are called into action at a future point.
Is Austria ready to deal with this epidemic? At our department we have written a Standard Operating Procedure (SOP) document now for COVID-19 for everyone in our department and have made it available for everyone to have access. The IT department in our hospital has also worked hard to enable everyone to access their work emails from their home offices and to facilitate communication. So that all helps us to prepare for what is coming and it all went smoothly and efficiently.
We have all the structures and teams in place to tackle this crisis and are on a war footing. It is a little bit surreal as everything is ready but there are very few patients for the moment. It is the calm before the storm. There are not yet so many COVID19 positive patients in Austria and very few currently need hospitalisation. But as we have seen elsewhere, this can change very quickly and we need to be ready for every eventuality.
SPECIAL FOCUS: COVID-19 16 EUROTIMES | MAY 2020
Oliver Findl MD, PhD
We have all the structures and teams in place to tackle this crisis and are on a war footing
Oliver Findl MD, PhD
Waiting on the Sidelines
If there’s one thing I didn’t anticipate about the coronavirus outbreak, it’s how useless it makes me feel.
I love being an ophthalmologist. I wouldn’t want to change that. But at a time like this, it’s hard not to feel that if only I had opted for a different specialty, I could have contributed more.
While Belgium hasn’t seen numbers anywhere close of those of Italy, Spain or France, our numbers are going upward, and the rate of change is accelerating. Nobody has any doubt that we are on the cusp of a coronavirus wave. The only question is what the size of that wave will be. Will it gradually swell into an onslaught that will prove hard — but hopefully not impossible — to deal with?
Or will it be a tidal wave, which will wreak havoc on healthcare infrastructure and workers alike?
Antwerp University Hospital (UZA) — my home away from home — is one of the COVID19 reference hospitals in Belgium. For the last few weeks, we’ve been getting ready for the wave to hit. Shoring up defences, re-purposing infrastructure, equipment and staff alike. The atmosphere is that of a veritable war room, except that the war hasn’t really started yet.
I do not mean to tell people what they should be doing. I only want to share my own experiences in this strangest of times about what things look like from the ophthalmology department:

- All elective procedures are cancelled
- All non-urgent clinic appointments are cancelled
- Consultations are handled via telephone or email where possible
I have been using WhatsApp to see my keratitis patients where I can. The point is to keep them away from the hospital.
I’ve volunteered for a team to transport known positive patients to ensure we do everything to limit exposure. Ensuring that the protective equipment is sufficient. I am hoping by doing so I can protect the more “useful” doctors and nurses and keep them on the front line. If it is needed, I will be trained to do more practical interventions.
Every day we get updates from our medical director, Guy
Hans. Meetings are forbidden, so they are in the form of video conference calls. These updates are direct and frank. I may learn about problems that I was unaware of before. But I also learn about what we’re doing to tackle them, and what I can do to help. This in turn, goes a long way to alleviate my sense that I can’t do much. My own head of Department, Carina Koppen, is checking in with everyone and leading from the front.
We’re in this together. I’m still nervous, but I’m not afraid. I might be a mere foot-soldier marching to the drum beaten by someone else. But I stand shoulder to shoulder with my colleagues, saying ‘bring it on’.
At the moment there are still very few colleagues in the team who have fallen ill; perhaps because our exposure to patients is typically rather low. So as a team we are ready to be placed where we are needed. Some of our residents are being retrained to work in the emergency department, others are learning to intubate. Like reservists, waiting on the sidelines to be deployed where the need is direst.
The sense of solidarity extends beyond the walls of the hospital. When a large government order of face masks fell through at the last minute, several companies donated their stocks of filter masks and one of the product development schools is using their 3D printers to design and make new masks for the infected patients. A call has also been send out for the community to make reusable fabric masks so that the stocks can be reserved for patient contact and procedures.
I’m sure all of you can all share similar stories. Better ones too. For me, as this tragedy unfolds, I have found a source of optimism and strength in the way this is bringing people together.
My hope is that you too will find such pockets of strength, hope, and resilience, that will allow us to weather this storm together.
Sorcha Ní Dhubhghaill MB PhD MRCSI(Ophth) FEBO is an Anterior Segment Ophthalmic Surgeon at the Netherlands Institute for Innovative Ocular Surgery (NIIOS) and Antwerp University Hospital


Belgian ophthalmologists are ready and waiting to tackle the COVID-19 pandemic in any way they can. Sorcha Ní Dhubhghaill reports
SPECIAL FOCUS: COVID-19 17 EUROTIMES | MAY 2020
Illustration by Eoin Coveney
Intracameral antibiotics debate
Modern surgery raises new questions regarding the use of intracameral antibiotics. Roibeard Ó hÉineacháin reports
In this age of modern cataract surgery with improved surgery and sterile techniques, is the use of intracameral antibiotics still necessary to reduce the incidence of endophthalmitis? That was the question addressed in a debate held at the 37th Congress of the ESCRS in Paris, France.
Arguing in favour of intracameral antibiotics was one of the early proponents of the practice, Prof Anders Behndig MD, PhD, Umeå University Hospital, Umeå, Sweden.
“I have been a cataract surgeon since 1993. I’ve used intracameral antibiotics in every single case since 1999 and I wouldn’t dare to do anything else,” Prof Behndig said.
He pointed out that in the 15 years since the publication of the ESCRS endophthalmitis prophylaxis study, decreased rates of postoperative endophthalmitis (POE) have accompanied the adoption of intracameral antibiotics by ophthalmic surgery practices around the world.
He noted that Swedish cataract surgeons had already adopted intracameral cefuroxime because the Swedish National Cataract Register (NCR) – which has registered endophthalmitis after cataract surgery (POE) since 1998 – showed that intraocular antibiotics such as cefuroxime, moxifloxacin and ampicillin can significantly reduce the POE rate.
The reports from the Swedish NCR were the inspiration behind the ESCRS endophthalmitis study, he noted. The prospective randomised controlled trial involved 16,603 cataract patients who underwent cataract surgery at 24 centres throughout Europe from September 2003 to January 2006. It showed that the POE rate among patients randomised to receive intracameral cefuroxime was only 0.03%
in those who also received levofloxacin drops, and only 0.05% in those who received placebo drops. That compared to POE rates of 0.17% and 0.25% in the same respective groups who did not receive the intracameral antibiotic.
Since that time, the near universal adoption of intracameral antibiotics in France has coincided with a reduction in the incidence of POE from 0.145% in 2005 to 0.044% in 2014 (Creuzot-Garcher C, et al, Ophthalmology. 2016;123:1414-20). In a very recent study from India, a review of 2,062,643 cataract surgeries showed that the rate of POE was only 0.02% in patients that received intracameral moxifloxacin compared to 0.07% in those who did not receive it (A Haripriya et al, J Cataract Refract Surg. 2019 Jul 29. [Epub ahead of print]).
“Intracameral antibiotics have been used in many millions of cataract procedures and they reduce endophthalmitis rates by three- to sevenfold in different studies and side-effects are extremely rare,” Dr Behndig added.
THE FEAR FACTOR
Prof Antoine Brézin MD, Université Paris Descartes, Paris, France, maintained that intraocular antibiotics should not be mandatory in cataract surgeries, as in France where there is now an official recommendation in favour of the prophylaxis approach.
“Doubtless the incidence of endophthalmitis after cataract surgery has gone down dramatically over the past 15 years, but is it really due to the use of intracameral antibiotics? I think we have been brainwashed to believe it is cefuroxime, but I think there are a number of other factors to consider,” he said.
He argued that although the ESCRS study showed that intracameral cefuroxime reduced the rates of POE, it also confirmed that surgical complications were a major risk factor for POE. Other studies have shown rates of POE after cataract surgery without intracameral antibiotics as low as those achieved with them in the ESCRS study. He cited a Japanese study that showed that among 63,244 cataract patients the rate of POE was only 0.025%, even though only 11.8% received intracameral antibiotics (T Inoue et al; Jpn J Ophthalmol 2018; 62:24-30).
Other surgical factors may therefore may play a more important role in preventing the complication. He noted, for example, in the ESCRS study the risk of the POE was more greatly elevated by the use of clear corneal incisions instead of scleral tunnel incisions than it was by the absence of intracameral antibiotics (5.8-fold vs 4.9fold), Dr Brézin said.
Prof Brézin added that the studies cited in support of the ESCRS study are almost all based on before-and-after comparisons, which overlook the many advances in cataract surgery that may have also contributed to the reduction of the complication. Such advances include smaller incisions that are less prone to leakage, shorter surgical times and fewer complications like posterior capsule rupture. Other factors include improved surgical theatre air filtration and preloaded IOL cartridges.
He noted that a study prospectively comparing the outcome of cataract surgery with and without intracameral antibiotics in 15,000 cataract patients showed that the prophylaxis did not significantly reduce the incidence of POE (0.108% vs 0.15%, p=0.57) (Sharma et al, J Cataract Refract Surg 2015;41:393-399).
“In 2019, do I inject because of the science? No, I inject because of the official recommendation. I inject because of the fear factor, because, like everyone else, I’m afraid of lawyers. But if we could turn the page back, I think I would no longer do so,” Prof Brézin concluded.
Anders Behndig: anders.behndig@umu.se
Antoine Brézin: antoine.brezin@aphp.fr
CATARACT & REFRACTIVE 18 EUROTIMES | MAY 2020
I have been a cataract surgeon since 1993. I’ve used intracameral antibiotics in every single case since 1999 and I wouldn’t dare to do anything else
Anders Behndig MD, PhD
Eliminating astigmatic defocus
Treating low corneal astigmatism brings benefits. Cheryl Guttman Krader reports
Toric IOLs are not merely suitable for eyes with low corneal astigmatism (0.5 to 0.75 D). Rather they are an indispensable tool for optimising refractive outcomes, visual performance and patient satisfaction after cataract surgery. And considering the relative predictability and risks associated with incisional techniques for treating astigmatism, toric IOLs are a far superior option, said Graham Barrett MD, at the 37th ESCRS Congress in Paris, France.
Dr Barrett told attendees that he performs a toric calculation targeting 0D residual astigmatism in all cataract surgery patients. An analysis evaluating outcomes using that approach showed that in a series of 290 eyes, 85% presented with ≥0.5D keratometric cylinder and 81% underwent toric IOL implantation. Postoperatively, 90% of eyes had ≤0.5D residual astigmatism, only 1.4% of eyes had 1.0D residual astigmatism and no eye had >1.0D.
“Astigmatic defocus is just as bad as spherical defocus. There is no benefit for leaving anyone with residual astigmatism,” said Dr Barrett, Professor, Lions Eye Institute, Perth, Australia.
PARAMETERS FOR PREDICTABLE OUTCOMES
Obtaining accurate measurements is the first step to success when correcting low levels of astigmatism. Dr Barrett recommended measuring keratometry (K) with at least two devices – a biometer and topographer or tomographer –and ideally a third instrument such as a second biometer, autokeratomter or even a manual keratometer, for a third measurement. Likely the values will differ, but when put into the current Barrett Toric Calculator, an integrated K value is generated using vector analysis. The integrated K, which represents the mean if two data points are input and the median for three, is then used for the toric IOL calculation.
“The integrated K is significantly more accurate than a value from a single device, and its use enhances surgeon workflow because it eliminates time spent cogitating over which K value to use,” Dr Barrett said.

For the toric IOL calculation, Dr Barrett’s calculator uses a theoretical model to predict posterior cornea astigmatism or accepts a measured value. His calculator also incorporates an algorithm accounting for IOL tilt.
Incisions are another critical consideration. Dr Barrett said they should be made small (≤2.4mm) and consistently on the same axis. Regarding surgically induced astigmatism, he said the centroid value, not the mean, should be used in the toric IOL calculation.
Although an alignment error will result in increased residual astigmatism, the lower the toric power, the less the effect. To optimise alignment accuracy, Dr Barrett said he uses both a free app that he developed (toriCAM) as a manual marking aid and an intraoperative image guidance system.
“Using both methods helps because each checks the other,” he said.


Keep the Light On
with OCULUS Perimeters
OCULUS Easyfield ® C: A complete perimeter with no dark room required
The OCULUS Easyfield ® C provides quick screening and glaucoma threshold exams without the need of a dark room.
Its small footprint and full functionality make it a flexible alternative also for confined spaces.

CATARACT & REFRACTIVE
us!
Follow
www.oculus.de
Eurotimes Easyfield Image - Keep the lights on 93x266 e 4c 03.20 v2.indd 1 31.03.2020 13:51:02 19 EUROTIMES | MAY 2020
Astigmatic defocus is just as bad as spherical defocus
Graham Barrett MD
AI and smart lenses
Smart lenses, microelectronics and AI edge closer to the clinic. Dermot McGrath reports
Rapid advances in biomedical engineering, artificial intelligence and miniaturised electronics are bringing the prospect of smart lenses ever closer as potential solutions for various ophthalmic disorders and potential applications for the management of presbyopia, according to Dimitri T Azar MD, MBA.
“There have been concerted efforts in recent years to bring microelectronics, sensors and smart lenses from the lab into ophthalmic clinical and preclinical testing,” he told delegates attending a symposium of artificial intelligence at the 37th Congress of the ESCRS in Paris, France.
Dr Azar, Senior Director of Ophthalmic Innovations at Verily Life Sciences, gave an overview of the future of microelectronics in ophthalmology, broad progress made to date and the challenges in bringing microelectronics, diagnostics and smart lenses to the ophthalmic market.
“The future involves engineering novel solutions to address the considerable technical challenges of building wireless sensing capabilities in and on the eye. Future smart lenses are likely to incorporate sensors, miniaturised low power electronics and data analytics in devices that are as small as 600 microns in diameter, which is quite a feat of engineering,” he said.
Dr Azar said that artificial intelligence allied to the hardware miniaturisation revolution of recent years would have a profound impact on all domains of life, including medicine and ophthalmology.
“We are in the new era of technological pervasiveness with AI and nanofabrication, which will inevitably change the way we practise medicine and
ophthalmology. We have experienced three revolutions in medicine since the Flexner Report, a book-length study of medical education in the United States and Canada, published in 1910: molecular biology in the 1950s with the discovery of DNA; genomics in the 1980s with all the biologics that we currently use in ophthalmology and medicine; and more recently, the convergence of AI with the hardware miniaturisation revolution in the 2000s,” he said.
UNMET NEEDS
These advances will allow ophthalmologists to address unmet needs in cataract and ophthalmic disease management, noted Dr Azar.
“AI can really help us with screening in order to identify which patient should be referred to the sub-specialist for management and will help with workload reduction for better efficiency with limited healthcare resources. Algorithms can be run on PCs or smartphones; we will see improved sensitivity and specificity of at-risk patient detection and promotion of personalised cataract surgery and personalised disease management,” he said.
Diagnostic imaging is currently the highest and most efficient application of AI-based analyses and will likely further expand as imaging modalities become more advanced and multi-modal, said Dr Azar.
“We are also looking at applications beyond diagnostics to AI-based discovery. AI should improve IOL power calculations,” said Dr Azar, with effective lens position (ELP) representing the biggest potential source of error. “Research led by Dr Jose De La Cruz at the University of Illinois is showing how data about the lens, cornea, anterior
chamber depth and angle anatomy can be collected during laser cataract surgery in order to calculate the postoperative ELP,” he said.
“It requires knowledge of axial length, central K, A constant and postoperative refraction. There is great scope for AI to capture these important predictors as well as other preoperative characteristics in order to improve outcomes but we need better data sets to be able to do this properly. We especially need data sets with accurate refractive error calculations in patients having good postoperative Snellen acuity,” he said.
Published reports have also shown the potential of AI to predict refractive errors with a relatively high degree of accuracy just from analysis of fundus images, said Dr Azar.

“The images were derived from the UK Biobank and AREDS data set. Looking at some of these fundus images, one could perhaps distinguish a high myope from a high hyperope. However, these deep learning programmes can do the job much better than humans in predicting refractive errors,” he said.
COMPLEX FUTURE TECHNOLOGIES
Dr Azar referred to experimental and theoretical data in the public domain regarding ophthalmic microelectronics, such as electronic autofocus lenses, and explained that these future technologies are much more complex than today’s IOLs. “For implantable lenses, the lens would be ideally positioned in the bag or elsewhere in the eye. The first step is to determine the afferent pathway and estimate the distance at which the patient is looking. AI and feedback loops are potentially incorporated to change the power of the lens,” he said.
“All of this would require miniaturisation, tiny batteries, antennae and computer chips placed inside ophthalmic devices,” he said.
Setting the optimal cut-off point for the add power of the smart lens is one of the key decisions to be made by the designers, said Dr Azar.
“One could potentially set the lens for progressive add corrections for near distance at +2D, +3D or +3.5D. There are trade-offs for every one of these decisions,” he said.
EUROTIMES | MAY 2020 CATARACT & REFRACTIVE 20
Dimitri T Azar MD, MBA
There have been concerted efforts in recent years to bring microelectronics, sensors and smart lenses from the lab into ophthalmic clinical and preclinical testing
Dimitri T Azar MD, MBA
The challenge of abnormal corneas
An abnormal cornea may fool the chosen IOL power calculation formula, thus careful consideration to what formula is best in these eyes, as well as using all possible useful data, is essential, Thomas Olsen MD, Denmark, told delegates attending the 37th Congress of the ESCRS in Paris, France.

Dr Olsen, the creator of the Olsen formula and software using the C-constant approach for the prediction of the IOL position, discussed the challenges of IOL calculations in the pathological cornea during the ESCRS/EuCornea Symposium: Cataract Surgery in Eyes with Diseased Corneas.
Since the advent of the original theoretical IOL power calculation formulas in the late 1960s there have been significant advances, Dr Olsen pointed out, referencing the development of improved thin lens formulas, improved biometry, estimated lens plane (ELP) and ray tracing methodology, leading to the newer statistical or hybrid fourthgeneration formulas.
However, Dr Olsen warned that pathological corneas can “fool” even the best formulas and be very challenging to choose the correct lens position.
Some IOL formulas assume a normal eye model for the K-reading for the estimation of the ELP (Barrett II, Hill-RBF, etc), while others do not depend on the K-reading for the estimation of the ELP (Olsen, Haigis, etc).
Dr Olsen focused on cases of post-LASIK cornea, keratoconus, megalocornea to highlight his points.
He quoted a post-LASIK study of 74 eyes with previous Rx correction ranging from -6D to -14D. All cases were measured pre-op with Lenstar biometry and Pentacam Scheimpflug photography.


PREDICTION ERROR
Comparing the prediction error with four different calculation methods, the Olsen formula, using ray tracing to calculate lens power and the concept of the C-constant to predict implant location, had the best result (60.8% with a prediction error within 0.5D), with the poorest result from the Haigis formula (37.8%).
Dr Olsen also discussed a keratoconus case where ray tracing of Pentacam data was used in the calculation, and IOL implantation was performed as a staged procedure; postop unaided visual acuity was 20/40, while in a megalocornea case the prediction of the IOL position was calculated using the C-constant and there was also good visual results.
Concluding, Dr Olsen said there is still no perfect IOL power calculation formula for all eyes and better methods to obtain the true corneal power and to predict the best lens position are still needed, as are formulas that use all the information that can now be obtained from patients.
 Thomas Olsen: tolsenmail@gmail.com
Thomas Olsen: tolsenmail@gmail.com
CATARACT & REFRACTIVE
Even the best IOL calculations can be ‘fooled’ by the pathological cornea. Priscilla Lynch reports
21 EUROTIMES | MAY 2020
Thomas Olsen MD
CALL FOR ENTRIES
JOHN HENAHAN PRIZE 2020
Young ophthalmologists are invited to write an 800-word essay on
“Will Clinicians Be Replaced By A Robot To Perform Cataract Surgery?”
The prize is a travel bursary worth €1,000 to attend the 38th Congress of the ESCRS in Amsterdam,The Netherlands
CLOSING DATE
FRIDAY 29 MAY 2020
Entries to be sent to: henprize@eurotimes.org
For further information visit: www.escrs.org
Vector Planning for astigmatism
Managing astigmatism to avoid LASIK surprises.
Dermot McGrath reports
Incorporating Vector Planning in which both corneal and refractive parameters are used in creating an ablation treatment plan could help to avoid debilitating visual symptoms after LASIK and other refractive surgery procedures, according to Prof Noel Alpins FRANZCO, FRCOphth, FACS.
“Treatment based solely on refractive parameters can result in excess corneal astigmatism, causing any one or more of symptoms of glare, starbursts, haloes and reduced contrast sensitivity (known as GASH),” Dr Alpins told delegates attending the 37th Congress of the ESCRS in Paris.
Dr Alpins presented a case study of a 34-year-old man who presented to his practice after undergoing bilateral LASIK with another surgeon in 2016. He had been treated with the latest generation Schwind Amaris 1050 laser. He reported symptoms of glare, ghosting, starbursts and haloes with a loss of contrast sensitivity. Preoperatively, the patient had myopic astigmatism with a BCVA of 20/20 in each eye with regular topography and no such pre-existing symptoms.
Postoperatively, his UCVA was 20/20 in each eye with no refractive error, but he could drive at night only by shining his cell phone flashlight in his eyes to reduce the pupil size and mitigate the effect of his GASH symptoms. He had more than 1.00D of corneal astigmatism remaining in each eye postoperatively because he had undergone LASIK treatment based on traditional 100% refractive parameters.
“While he had 20/20 vision in each eye he would definitely be classed as a 20/20 unhappy patient. The preoperative ocular residual astigmatism (ORA) was 0.99D in the right eye and 1.24D in the left eye. The key point is that he had a high ORA, which is quite a common finding of up to 46% of eyes in some studies and which puts the patient at risk for GASH,” he said.
Treating such a patient by using 100% refractive parameters, as is done in around 95% of LASIK cases around the world, the surgeon can calculate ahead of time how much astigmatism will remain on the cornea afterwards, said Dr Alpins.
“Had he been my patient, I would have treated him with Vector Planning, which means we are treating somewhere between the refractive cylinder and the corneal astigmatism by taking an optimised view of it. The treatment breakdown is around 60% by refractive and 40% by corneal parameters, essentially generating a balance between the refractive cylinder and the corneal astigmatism and thereby reducing the risk of GASH,” he said.
Dr Alpins said that refractive surgeons could avoid similar surprises in their own LASIK surgeries by using the free Vector Planning and ORA calculator tools at www.ISRS.org
CATARACT & REFRACTIVE
22 EUROTIMES | MAY 2020
While he had 20/20 vision in each eye he would definitely be classed as a 20/20 unhappy patient
Noel Alpins FRANZCO, FRCOphth, FACS
Congress of the ESCRS in Paris, France.
“Technology can be evaluated with different views,” said Dr Mura, Centro de la Visión, Clínica Las Condes, Santiago, Chile.
Spotlight on:
Toric IOLs and Presbyopia

Glaucoma
Ocular Surface Disease
Corneal Therapeutics


























“The word disposable does not mean that the object will disappear. It has to go somewhere else. Therefore, the use of new disposable technology must be associated with a recycling strategy, and that is our responsibility. We and the industry forum.escrs.org

CATARACT & REFRACTIVE
A library of symposia, interviews, video discussions, supplements, articles and presentations
NEW CONTENT 23 EUROTIMES | MAY 2020
Juan José Mura MD, MHA
ALIGNMENT techniques compared
Mobile app-based guidance compares favourably with digital axis marking system. Cheryl
 Guttman Krader reports
Guttman Krader reports
Amobile app digital reference marker offers cataract surgeons an inexpensive, consistent, and reproducible way to enhance outcomes of toric IOL surgery, reported Rahil Chaudhary MD, at the 37th Congress of the ESCRS in Paris, France.
Dr Chaudhary and colleagues from Eye7 Chaudhary Eye Centre, New Delhi, India, investigated the performance of Toraxis (iOS/ App Store), a mobile app designed to help guide intraoperative toric IOL alignment, by comparing its accuracy with that of a digital axis marking system (Verion, Alcon) and the use of a manual horizontal bubble marker.
“Smartphone apps are being increasingly used by healthcare professionals, and ophthalmological toric IOL axis marking apps are easily available for download,” said Dr Chaudhary.

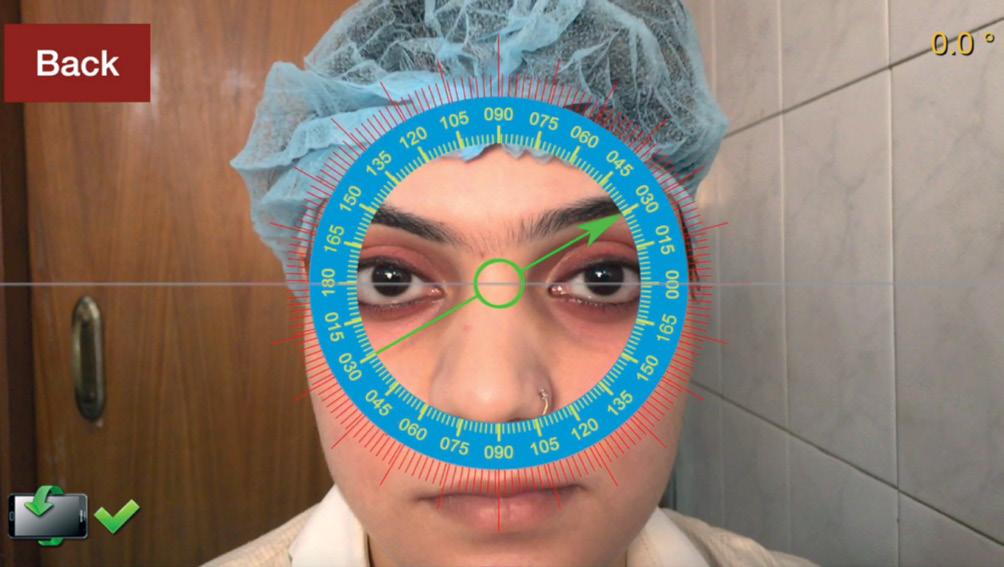
“The purpose of our study was to assess the accuracy of one particular reference marking app. Although we found that it was not as good as the digital marking system, the results of the mobile app were consistent with the results of the digital marking system and associated with less variability than the manual bubble marker.”
The app investigated in this study is a non-contact approach that does not involve ink markings. It takes a high-definition image of the eye from which the user identifies an anatomical

landmark, such as a prominent blood vessel. The app establishes the angle coordinates of the landmark as a reference for determining the axis of astigmatism that is then identified intraoperatively using a Mendez ring or a surgical microscopeintegrated overlay.
The study assessing the accuracy of the mobile app included 50 eyes. All three systems for guiding toric IOL alignment were used in all cases. All marks were made by a single surgeon, and the data of the mobile app marker and digital axis marker were collected by the same surgeon.
Assuming that the digital axis marker represented the most accurate technique, it was used as the “gold standard” reference for analysing the accuracy of the mobile app and manual marking system. Compared with the axis of alignment identified with the digital axis marker, mean (± standard deviation) variability was 1.8±1.1 degrees for the mobile app and 3.2±1.8 degrees for the manual bubble marker (P<.0001).
Based on the study findings, Dr Chaudhary suggested the mobile app is something that surgeons could consider using for confirmation of reference marks that are manually placed preoperatively.
Rahil Chaudhary: rahilchaudhary@gmail.com
EUROTIMES | MAY 2020 CATARACT & REFRACTIVE 24
ESCRS Practice Management and Development Innovation Award Submission Deadline: Friday 24 July 2020 For further details email: innovation@escrs.org Grow Your Practice Through Innovation Win a €1,500 Bursary Practice Management & Development ESCRS
Screenshots from the Toraxis digital marking app for alignment of toric intraocular lenses
Courtesy of Rahil Chaudhary MD
THOMAS KOHNEN European Editor of JCRS


JCRS HIGHLIGHTS








VOL: 46 ISSUE: 3 MONTH: MARCH 2020


NEW SOURCE OF DLK IDENTIFIED
Toxic anterior segment syndrome (TASS) and diffuse lamellar keratitis (DLK) have been attributed to many factors, including surgical technique, instruments and intraocular and extraocular solutions used during surgery. A recent study suggests that autoclave reservoir biofilm may also play a role.
US researchers evaluated 147 eyes that developed DLK following laser in situ keratomileusis (LASIK) over a five-year period. A cluster developed in spite of efforts to changes surgical and operating room protocols. The cluster persisted until an older STATIM 2000 autoclave was replaced with a new STATIM autoclave and a reservoir sterilisation and surveillance protocol implemented. When the retired autoclave reservoir chamber wall was cultured for microbial contamination, Pseudomonas aeruginosa and the Burkholderia cepacia were found. The authors suggest that stringent reservoir cleaning and maintenance may significantly reduce this risk by preventing and removing these biofilms. The article includes a reservoir sterilisation protocol for ophthalmic surgical centres to consider. AL Soreneson et al., “Diffuse lamellar keratitis associated with tabletop autoclave biofilms”, Vol. 46, #3, 340-349.
PSEUDOPHAKIC CME
The combination of intraoperative phenylephrine 1%/ketorolac 0.3% solution with perioperative bromfenac may limit the occurrence of clinically significant pseudophakic cystoid macular oedema after cataract surgery without the drawbacks of topical corticosteroids, a cohort review suggests. Investigators reviewed 824 patient records, analysing 504 eyes treated in this way. Only two of these eyes developed cystoid macular oedema, a rate of 0.4%. The researchers note that this rate is below the historical rates derived from a literature review of CME development with the use of steroids, alone or in combination with NSAIDs. The researchers believe the combination of intraoperatively delivered phenylephrine 1%/ketorolac 0.3% intraocular solution and perioperative topical bromfenac offers an effective alternative to topical corticosteroids and to combinations of corticosteroids and NSAIDs for limiting the occurrence of clinically significant pseudophakic CME. K Walter et al. “Rate of pseudophakic cystoid macular edema using intraoperative and topical nonsteroidal antiinflammatory drugs alone without steroids”, 46(3):350-354.





INTRACAMERAL MOXIFLOXACIN DOSES
A contralateral eye study showed that a 500mg dose of moxifloxacin given as an intracameral bolus after phacoemulsification is associated with no difference in central corneal endothelial cell loss when compared with a 250mg dose. The higher dose may have a greater bactericidal effect and may be more effective against certain bacteria. The authors also cite extensive clinical data from hospital groups to support this conclusion. D Chang et al., “Comparative corneal endothelial cell toxicity of differing intracameral moxifloxacin doses after phacoemulsification”, Vol. 46, #3 355-359.

JCRS is the official journal of ESCRS and ASCRS CATARACT & REFRACTIVE 25
EUROTIMES | MAY 2020
Therapeutic PTK
Wavefront-guided transepithelial PTK effective for stromal irregularities. Dermot McGrath reports
Corneal wavefrontguided transepithelial phototherapeutic keratectomy (TPTK) offers surgeons a safe and effective means to correct anterior stromal irregularities and achieve visual rehabilitation in eyes that have suffered loss of vision after a corneal event, according to a study presented at the 37th Congress of the ESCRS in Paris, France.
“We think wavefront-guided TPTK is a nice and elegant procedure for visual rehabilitation in cases of anterior stromal irregularities, including anterior stromal scars, or irregularities after refractive surgery such as LASIK and SMILE, or post-radial keratotomy,” said Michiel Luger MD.

“It is important, however, that the PTK phase of the treatment matches or exceeds the depth of the epithelial masking so as to get into healthy stroma, and that the residual stromal bed thickness is respected,” he added.
The cornea typically heals after anterior damage by regrowing and filling the gap with epithelium noted Dr Luger, Medical Director, Bergman Refractive Surgery, Naarden, the Netherlands.

“It creates an epithelium mask for the underlying irregularity but often leaves the patient with distorted vision. For these cases, we assess the patient, measure the corneal wavefront, pachymetry and epithelial thickness pattern and obtain the
we calculate the ablation profile to erase the irregularity, correct the wavefront error and end up with healthy stromal tissue and improved vision,” he said.
Dr Luger presented a series of case studies to highlight the viability of the method. The first case was a young male patient with a corneal ulcer in his left eye after SMILE®.
“He had severe haloes and glare and other visual symptoms. The stromal tissue overlying the ulcer was completely melted away and filled with epithelium. The corneal wavefront preoperatively showed higher order aberrations, so we treated him with transepithelial PRK with the addition of sufficient PTK to end up with a clear and healthy stroma. After three months he had improved visual acuity and he was very happy with the big improvement in side-effects,” he said.
Dr Luger’s second case was a postradial keratotomy female patient who had presented for cataract surgery.
“When we examined her, she had a very
high refractive cylinder and a lot of coma and spherical aberration on the wavefront and irregular topography. We thought it was a better idea in this instance to treat the cornea first and then see if we had to do the cataract surgery as well. After transepithelial wavefront-guided PRK she ended up with very functional uncorrected vision with very low myopia and a big improvement in her corneal aberrations. Her vision was that good that she postponed the cataract surgery,” he said.
Dr Luger’s final case study was a patient with irregular astigmatism postSMILE with an over-correction in his left eye and high levels of coma and spherical aberration. After treatment of transepithelial wavefront-guided PRK including PTK he ended up with a good visual outcome and an almost total reduction of corneal aberrations.
Dr Luger reported a total of three cases showing very satisfactory outcomes, and continues to refine the technique to further increase the success of this approach.
EUROTIMES | MAY 2020
26 CORNEA RUSSIAN LANGUAGE EDITION NOW ONLINE Visit: www.eurotimesrussia.org
We think wavefront-guided TPTK is a nice and elegant procedure for visual rehabilitation in cases of anterior stromal irregularities...
Michiel Luger MD



www.eucornea.org RAI Amsterdam, The Netherlands 11th EuCornea Congress AMSTERDAM 2 – 3 October 2020
European Union Web-Based Registry
The aim of the project is to build a common assessment methodology and establish an EU web-based registry and network for academics, health professionals and authorities to assess and verify the safety quality and efficacy of corneal transplantation.
Ocular surface evaluation
Anew low-cost interferometry platform called Lacrydiag (Quantel) allows the quick, objective and non-invasive analysis of tear film and meibomian glands for the diagnosis of dry eye and can help monitor the efficacy of dry eye disease treatment, said Béatrice Cochener-Lamard MD, PhD, at the 37th Congress of the ESCRS.
The Lacrydiag device provides assessment of tear film properties using interferometry ergonomic hand held device it has two removable magnetic cones, one for meniscus interferometry and the other for non-invasive break-up time (NIBUT). It also has a yellow filter that allows evaluation of the integrity of the ocular surface, said Dr Cochener-Lamard, University Hospital of Brest – CHU Morvan, Brest, France.
In a validation study involving 100 patients from the general population with a mean age of 55 years (range 44-71 years), Prof Cochener-Lamard and her associates performed a range of measurements with the Lacrydiag device, including measurement of NIBUT, height of lacrimal meniscus, thickness of the tear film and meibography. They compared the automated analysis was with the clinical examination including break-up time (BUT) measurement, SPEED life questionnaire and Oxford score.

the ECCTR Registry
Join Track
your Surgical Results
www.ecctr.org
ECCTR is a project funded by the ESCRS with initial support from the EU
They found a moderate correlation between the Lacrydiag meiboscale values and those of conventional meibography (r=0.595). They found that there was no correlation between the TBUT and NIBUT, with a mean variation of 2.35 seconds. Prof Cochener-Lamard pointed out that thresholds have not yet been set for the device.
She noted that 30 of the patients were treated with the Eyelight (Topcon) device for meibomian gland disease, a photobiomodulation technology that uses an LED matrix at a specific wavelength to stimulate a healing response in the inner eyelid tissues. The inclusion criteria were grade 1 to 3 on the Lacrydiag meiboscale. The patients underwent two-to-four treatment sessions.
SIGNIFICANT IMPROVEMENT
At one month’s follow-up was there significant improvement in mean BUT, and there was also a significant improvement in the Oxford score. However, tear meniscus height and NIBUT measured with the Lacrydiag device did not change. On the other hand, meibography with the device showed a significant improvement.
Regarding patient satisfaction, patients’ scores improved on the OSDI and SPEED quality of life questionnaire. Functional symptoms decreased in 73%. The main sideeffect was erythema of facial skin, which disappeared after a couple of hours. However, there were two cases of herpetic keratitis, which occurred in the stroma in one patient with previous ocular herpes and in the epithelium of another patient without previous ocular herpes. Both cases resolved following antiviral therapy.
Béatrice Cochener-Lamard: beatrice.cochener@ophtalmologie-chu29.fr
Hand-held device provides quantification of OSD parameters. Roibeard Ó hÉineacháin reports
EUROTIMES | MAY 2020 CORNEA 28
Béatrice Cochener-Lamard MD, PhD
computer users
SD OCT can reveal signs of dry eye in patients with prolonged computer use. Roibeard Ó hÉineacháin reports
Patients who use computers for long periods of time show a correlated pattern of corneal pachymetry and epithelial thickness, high speed spectraldomain OCT scans show. This observation allows for early detection of minor pathologic changes, according to the findings of a study presented by Argyrios Tzamalis MD at the 37th Congress of the ESCRS.
“Prolonged computer use may be correlated with reduced tear break-up time (TBUT) and produce ocular surface symptoms affecting the patients’ quality of life. Epithelial thickness measurements are found to be associated with some ocular symptoms but not directly to the signs of dry eye disease,” said Dr Tzamalis, Aristotle University of Thessaloniki, Thessaloniki, Greece.
The prospective, cross-sectional study involved 67 patients who reported using computer and mobile phone screens more than eight hours per day. Dr Tzamalis and his team performed three consecutive measurements with the AngioVue OCTA Imaging System (Optovue) in each of the patients’ eyes, to assess the measurement’s repeatability and evaluate correlations between epithelial thickness and tear film quality.
The patients in the study had a mean age of 44.5 years and used computers for a mean 9.2 hours daily. All patients completed the Ocular Surface Disease Index (OSDI) questionnaire and also underwent TBUT testing and Schirmer testing. Patients with prior refractive surgery, contact lens use or other ocular pathology were excluded from the analysis.
Dr Tzamalis noted that the mean central corneal pachymetry as measured with the device was 528.4µm and mean central epithelial thickness was 52.9µm, with no statistically significant differences between the patients’ right and left eyes (p>0.05).
He added that the intraclass correlation coefficient (ICC) was found to be excellent for both central corneal pachymetry (ICC=0.99) and epithelial thickness (ICC=0.98) measurements. However, the ICCs of other regions were slightly lower, although they did not differ significantly from the central part (p>0.05).
Epithelial thickness was strongly correlated with total corneal thickness in every quadrant (p<0.01).
He noted that central epithelial thickness correlated significantly with reported difficulty while watching TV (r=-0.303, p=0.01) and irritation in windy weather conditions (r=-0.394, p=0.01). However, there was no significant association between corneal epithelial thickness and TBUT, Schirmer test, BCVA or total OSDI score (p>0.05).
In addition, the OSDI score correlated significantly to the reported number of hours spent in front of computer screens (p-0.007) and TBUT(p=0.02) but not with Schirmer testing. The most commonly reported symptoms were light sensitivity, pain and discomfort in windy conditions, Dr Tzamalis said.
Argyrios Tzamalis: argyriostzamalis@yahoo.com
• ESCRS Study Portals (PREMED, Endophthalmitis)
• Landmark Journal Articles
• Case Studies
• EBO – ESCRS Examination
• ESCRS Media Player
• ESCRS On Demand
• ESCRS iLearn
• Cataract Tutorial Group and more...
with our new
of online resources
education.escrs.org
when
are.
OCT in
Continue your education all year
range
Visit
Ready
you
EUROTIMES | MAY 2020 CORNEA 29
Epithelial thickness measurements are found to be associated with some ocular symptoms...
Argyrios Tzamalis MD
Prompt treatment ESSENTIAL

Old and established treatments best for corneal ulcers.
Priscilla Lynch reports
Corneal ulcers require prompt treatment to avoid further complications and longestablished techniques still provide the best options for ophthalmic surgeons today, the 37th Congress of the ESCRS in Paris, France, was told by a leading expert in the area.
Marc Muraine MD, PhD, France, discussed the various surgical approaches for treating corneal ulcers, giving practical advice and outlining his personal experiences, during a dedicated session on non-healing corneal ulcers at the Congress.
“As we know, corneal ulcers require prompt treatment as there is a high risk of perforation and, in addition, the corneal ulcer could result in sight-threatening complications due to neovascularisation and infection risk.
“So when dealing with a severe nonhealing corneal ulcer that has perforated the strategy is to cover it as soon as possible. Using glue is the easiest technique, as it doesn’t involve going to the operating room, amniotic membrane transplantation is the most popular technique, and conjunctival flap is the most efficient technique,” he said.
Sometimes it will be necessary to perform tectonic grafts, and sometimes to combine them with a conjunctival flap and tarsoraphia for more difficult ulcers, Dr Muraine added.
the various surgical approaches for those attending the session. He noted that glue is most suitable in perforations of <1mm, adding that fibrin glue is more expensive than cyanoacrylate glue. Describing the use of amniotic membrane transplantation, Dr Muraine said it is the “gold standard in the management of deep corneal ulcers”, and in treating corneal pre-perforation or perforation <2mm. Most often, amniotic membrane transplantation has to be performed using a multilayer technique, he explained. Dr Muraine then briefly described tectonic keratoplasty saying it is a useful new trepanation technique for penetrating keratoplasty in cases of large corneal perforation.
To compare the success rates of the various procedures, Dr Muraine quoted a 2006 study he contributed to of 56 eyes treated for a non-traumatic corneal perforation between 1997 and 2004. Mean patient age was 69 years (range, 16-95 years) and the mean follow-up was 20.5
peripheral ulcerative keratitis (PUK) in 21%, infectious keratitis in 15% and dry eye in the remaining 13% of cases.
As a first procedure, cyanoacrylate glue was used in 24% of cases (50% anatomic success), multilayer amniotic membrane transplantation in 39% of cases (100% anatomic success), conjunctival flap in 10%, and tectonic keratoplasty in 27% of cases.
Dr Muraine also discussed the latest technique, corneal neurotisation, ‘a novel solution to neurotrophic keratopathy’. He described the direct approach involving re-innervation of the anaesthetic cornea using the contralateral supraorbital and supratrochlear branches, but said it is currently suitable for very few patients.
Speaking to Eurotimes Dr Muraine summarised his thoughts on treating corneal ulcers: “The surgical techniques to deal with corneal ulcers are well known, and are long established and are very good. They include the glue, amniotic membrane, and conjunctival flap and tectonic graft
CORNEA 30 VISIT OUR WEBSITE FOR INDIAN DOCTORS www.eurotimesindia.org INDIA
...when dealing with a severe non-healing corneal ulcer that has perforated the strategy is to cover it as soon as possible
Marc Muraine MD, PhD

ASCRS is your trusted source for innovative education, philanthropy and advocacy –for every stage of your career. Join today: ASCRS.org
Robot-assisted surgery
Robot-assisted vitreoretinal surgery – slower but safer? Dermot McGrath reports
Robot-assisted vitreoretinal surgery may hold significant advantages especially for novice surgeons both during training and the early phases of their careers, by improving precision and limiting tissue damage compared to manual surgery, according to a study presented at the 19th EURETINA Congress in Paris.
“Our study suggests that at the cost of additional time, robot-assisted vitreoretinal surgery is more precise for both experienced and novice surgeons, and is associated with less tissue damage for novice surgeons,” said Mads Forslund Jacobsen MD.


“In the future it will be interesting to look at the learning curves for robotassisted surgery and the impact on patient outcomes in human trials in order to fully shed light on this subject and see if it truly merits a place in everyday clinical application,” he added.
Dr Forslund Jacobsen, Department of Ophthalmology, Rigshospitalet-Glostrup, Copenhagen, Denmark, noted that the very mention of robots triggers certain reflex images in people’s imaginations.
“In science fiction humans have always had an expectation that robots would be part of our future, and the same goes for vitreoretinal surgery. Robotic approaches to VR surgery have long heralded a new age of unprecedented dexterity and precision. However, the discussion on robot-assisted VR surgery is often based on subjective assessment alone. We need hardcore quantifiable data on the possible benefits,” he said.
Therefore, the Copenhagen-based group consisting of Ann Sofia Skou Thomsen MD, PhD, Lars Konge MD, PhD, Prof Morten la Cour MD, DMSc, and Mads Forslund Jacobsen MD, PhD-fellow, decided to use their background in research in simulation based surgical education to conduct this study and generate the needed data.
The randomised controlled crossover study included 10 experienced vitreoretinal
surgeons and 10 novice ophthalmic surgeons who were randomised to start with either manual or robotassisted surgery using the Preceyes robotic system. The surgery was assessed using a virtual-reality based surgical simulator (Eyesi) as a safe and standardised platform, with participants performing ILM peeling, ERM peeling and bimanual manoeuvrability tasks.
The automated metrics of performance supplied by the Eyesi simulator were used as outcome measures and included time with instruments inserted (seconds), instrument movement (mm) and tissue treatment (mm2).

In terms of results, both novices and vitreoretinal surgeons were significantly
slower when using robot-assisted surgery as compared to manual surgery. However, the movement outcomes showed that both novices and vitreoretinal surgeons were significantly more precise when performing tasks with less movement of instruments. Novice surgeons were also found to have significantly less tissue damage when using robot-assisted surgery compared to manual surgery, whereas there was no statistically significant difference for experienced VR surgeons.
Mads Forslund Jacobsen: mads.forslund.jacobsen@regionh.dk
EUROTIMES | MAY 2020
RETINA 32
In the future it will be interesting to look at the learning curves for robotassisted surgery and the impact on patient outcomes in human trials...
Mads Forslund Jacobsen MD
The Preceyes Surgical System: A tele-operated robotically assistive device dedicated to vitreoretinal surgery
The experimental robot-assisted surgery setup. (A) EyeSi Simulator controls display. (B) EyeSi Simulator phantom head. (C) Robot instrument manipulator. (D) Robot motion controller. (E) Robot controls display of Preceyes BV
Images
courtesy
Macular pigment measurement
Objective technique provides valuable tool in macular health assessment. Roibeard Ó hÉineacháin reports

Macular pigment optical volume (MPOV) measurements obtained with the dual-wavelength autofluorescence technique can provide a standardised means of assessing the nutritional health of the macula and the brain, according to a study conducted by Prof John M. Nolan PhD and his associates at the Nutrition Research Centre Ireland, School of Health Science, Waterford Institute of Technology, Waterford, Ireland.
“This research is another step in the validation of this highly repeatable imagebased technique to measure the full amount of macular pigment in the living person and this should represent a new standard,” Prof Nolan told EuroTimes in an interview.
He noted that a standardised method of measuring and recording macular pigment levels will allow clearer interpretation of the impact of higher and lower concentrations of the pigments on visual quality. It should also eventually allow the establishment of a normative database so that treatment effects can be closely monitored in both a research and clinical setting.
The study, published in the December 2019 issue of the Journal Translational Vision Science & Technology, involved 393 participants who ranged in age from 21 to 88 years, with a mean age of 55.5 years. None of those included had a critical medical condition or a previous history of oral carotenoid supplementation. However, 37% had a medical diagnosis of AMD or a neurocognitive disorder.
All participants underwent examination with the Heidelberg Engineering SPECTRALIS with the investigational Macular Pigment Optical Volume (MPOV) Module to measure macular pigment optical volume (MPOV) and macular pigment optical density (MPOD) at four foveal eccentricities (0.23°, 0.51°, 0.98°, 1.76° [7° as reference point]). The researchers also evaluated serum concentrations and dietary intake of the macular pigments lutein and zeaxanthin.
The investigation showed that the participants’ mean MPOV was 5,094 and ranged from 527 to 10,652. MPOV was inversely correlated with body mass index (p=0.002) and positively correlated with education (p=0.014) and serum concentrations of lutein and zeaxanthin (p<0.001 and p<0.001, respectively). However there were no significant correlations between MPOV and the clinical and demographic variables, including medical diagnosis, dietary intake, smoking status and sex.
The SPECTRALIS MPOV Module uses confocal scanning laser ophthalmoscopy with blue (486nm) and green (518nm) laser diodes for auto fluorescent excitation. Because macular pigment is yellow, it absorbs blue light four times more strongly than it absorbs green light. Therefore, where macular pigment is present the blue lightexcited autofluorescence will be lower than that of green light-excited AF at the same location. The MPOV value is a measure of MP density as well as its distribution within the macula, providing
a measurement of the total MP across all eccentricities.
Dr Nolan noted macular pigments act as a blue filter, protecting the photoreceptors from harmful blue rays, reducing chromatic aberration and scattered blue light, in turn reducing glare and enhancing contrast sensitivity. Macular pigments also have antioxidant and anti-inflammatory properties. Macular pigments also tend to be lower in patients with age-related macular degeneration. Furthermore, in the AREDS2 trial and other studies, formulas containing lutein and zeaxanthin were 10% more effective in slowing the progression of intermediate dry AMD as the original betacarotene formulation, he said.
In addition, post-mortem studies have shown that the amount of macular pigment in the macula is highly correlated with the amount of macular pigment in the brain. Research has also shown that people with higher concentrations of the carotenoids in their macula had better cognitive abilities, whereas those with Alzheimer’s disease tended to have highly deficient concentrations.
Some studies have documented improvements in quality of life in patients with cognitive disorders who received carotenoid supplementation. A major study is now under way to determine the validity of these promising findings.
“If you expect that having an antiinflammatory agent with antioxidant propertiesis good for brain health then one could see macular pigment levels as a biomarker for brain nutrition,” Prof Nolan added.
John Nolan: john@ivr.ie
EUROTIMES | MAY 2020
RETINA 33
This research is another step in the validation of this highly repeatable imagebased technique to measure the full amount of macular pigment in the living person
Prof John M. Nolan PhD
...macular pigments act as a blue filter, protecting the photoreceptors from harmful blue rays...
Prof John M. Nolan PhD
Prof John M. Nolan PhD
1–4 October 2020
RAI Amsterdam, The Netherlands

For all the latest updates surrounding the Congress & SARs-CoV-2, please visit the website
www.euretina.org
Euretina Congress Amsterdam th
Big data moves research forward
What’s the big deal with big data?
Leigh Spielberg MD reports
What is big data? Why am I interested in big data? And why should you be interested in it?” were the three big questions that Adnan Tufail MD, Moorfields Eye Hospital, London, United Kingdom, sought to answer during his presentation at the 19th EURETINA Congress in Paris, France.
Entitled “Big Data for Retina: Perspectives and Cautions”, Dr Tufail presented to delegates during a session on novelties in retina & technology.
Big data refers to extremely large data sets that can be analysed computationally to reveal patterns, trends and associations. Dr Tufail’s interest in big data originated with the discrepancies that he had noticed in anti-VEGF treatments between clinical trial results and real-world outcomes, he said.

“When we started treating with ranibizumab, we expected visual gains of 10 letters like those reported in the ANCHOR trial and eight letters in the VIEW trial. But were these realistic expectations?” he wondered.
So, Dr Tufail started investigating large data sets drawn from electronic medical records (EMRs). “Ironically, large data sets may help with precision medicine, meaning: what can an individual patient expect from a certain treatment?” said Dr Tufail.
“Within two months, we had generated a database of more than 11,000 eyes. Our initial aims were to provide real-world outcome data, provide benchmarks for therapy, long-term outcomes of therapy and especially to create predictive models to guide future studies.”
Useful conclusions have since been drawn from analyses of big data for other diseases. Diabetic retinopathy progression can be predicted more accurately based on the baseline retinopathy and clinical features at presentation. A history of intravitreal injections is a significant predictor of posterior capsular rupture during cataract surgery. Large datasets have been used to develop AI algorithms that can accurately distinguish agerelated macular degeneration from normal eyes on OCT. The time course of developing anti-VEGF-requiring diabetic macular oedema in relation to time since cataract surgery can now also be calculated.
“EMRs will eventually capture all patient episodes, giving us the potential to monitor all patients on new therapies. I expect this to allow for more detailed post-marketing surveillance, because n = all and there is thus less selection bias.
Integration with general hospital EMR data will be the future of phase IV trials,” said Dr Tufail.
The next step is integrating machine learning, that can then be applied to large datasets of AMD and diabetic retinopathy images too large for human grading, he predicted.
*Average net circulation for the 10 issues circulated between 1 February 2019 to 31 December 2019. See www.abc.org.uk Results from the EuroTimes Readership Study 2017 NUMBER 1! 47,863 * Reach of readers are satisfied or very satisfied with EuroTimes 83 %
EUROTIMES | MAY 2020 RETINA 35
Ironically, large data sets may help with precision medicine, meaning: what can an individual patient expect from a certain treatment?
Adnan Tufail MD
Exceptional Clinical Education is One Click Away! Visit ASCRS.ORG Today!
ASCRS.ORG is now a dynamic web portal featuring an all-new design, enhanced features and delivering an exceptional user experience.

The new web portal features one-touch video playback, seamless navigation across all ASCRS online platforms, and coming soon flexible payment options including stored credit information, recurring monthly payment option and more!

Visit ASCRS.org Today!
Explore hundreds of surgical videos, presentations, webinars, and more by type, topic or meeting date
Find the latest and most relevant anterior segment surgery techniques and trends by keyword, type topic
Track your current CME credit status through real-time access to your CME transcript and CME certificates
Coming soon: Membership renewal option for either one annual fee or monthly payments!
ASCRS.org – your 24/7 one-stop resource for anterior segment surgical online education.
Low IOP, but glaucoma progressing?
Consider patient needs, adherence and other possible diagnoses. Howard Larkin reports
The patient’s intraocular pressure (IOP) is seemingly low, but glaucoma continues to progress. What can be done? Karl Mercieca MD, PGCME, FRCOpth, FEBOS-GL, consultant ophthalmologist and glaucoma surgeon at Manchester Royal Eye Hospital, Manchester, UK, outlined several steps at the ESCRS Glaucoma Day 2019 in Paris, France.
VISUAL DISABILITY THRESHOLD
First, put the problem in perspective, and that requires specific patient information, Mr Mercieca said.
“We are dealing with patients, not eyes. We are not dealing with pressure, we are dealing with a person who needs a certain quality of life.”
Therefore, the goal of treatment should not be to reach an arbitrary IOP, but to prevent disabling visual loss over a patient’s expected lifespan. For example, an aggressive but potentially risky treatment such as trabeculectomy may be appropriate to achieve a very low IOP for a 54-year-old patient with pseudoexfoliation who is progressing significantly at an IOP of 15mmHg, but not for an 84-year-old with similar functional loss due to primary open-angle disease progressing more slowly at 20mmHg, Mr Mercieca suggested.
Referencing European Glaucoma Society (EGS) 014 guidelines, Mr Mercieca discussed several factors to consider in setting a target IOP for glaucoma treatment.
Early glaucomatous damage, short life expectancy, high
untreated IOP, few additional risk factors and slow progression all gravitate toward a higher IOP target.
Conversely, advanced glaucomatous damage, longer life expectancy, low untreated IOP, additional risk factors such as family history of glaucoma and pseudoexfoliation, and fast progression suggest a lower IOP target.
The rate of progression is critical, Mr Mercieca said. While the median speed of loss is about -0.1dB/year, about 3% of patients progress more than -1.5dB/year (Saunders LJ et al. IOVS 2014;55:102-109). For a patient diagnosed at a 65% visual field index progressing at 5% annually, lowering IOP from 20mmHg to 16mmHg could mean just five years before reaching the visual disability threshold, compared with 26 years if 12mmHg is achieved.
However, it’s important to make sure progression is actually occurring, Mr Mercieca emphasised.
“You don’t want to condemn the patient to an invasive procedure with the possibity of hypotony if the progression isn’t real.”
Additional testing, such as day phasing to detect IOP fluctuations, and ensuring patients are adhering to medication treatment, can help confirm possible reasons for progression. Non-IOP medical factors such as cerebrospinal fluid pressure factors, variable ocular blood flow, brain lesions, 24-hour blood pressure variation and the influence of vitamin B12, folate levels and drugs should also be investigated and treated as indicated, Mr Mercieca said.
Karl Mercieca: doctormercieca@yahoo.com
EUROTIMES | MAY 2020
GLAUCOMA 37 Watch the latest video content from ESCRS and EuroTimes, FREE on the ESCRS Player Advanced Instructional Courses Eye Contact Interviews Video of the Month Video Journal of Cataract, Refractive & Glaucoma Surgery Young Ophthalmologists Videos: “My Early Surgeries” Online Museum player.escrs.org
Paediatric SMILE?
SMILE effective for select cases of paediatric myopic anisometropia. Dermot McGrath reports
Small-incision lenticule extraction (SMILE®) is a safe and viable treatment option for select cases of children with ametropic and anisometropic amblyopia, according to Soosan Jacob MS, FRCS.
“These young patients can undergo refractive surgery if they are spectacle or contact lens intolerant for any reason. SMILE offers particular advantages in paediatric populations – it is safe, there are no flap complications to worry about and no haze or regression as in surface ablation treatments,” she told delegates attending the 37th Congress of the ESCRS in Paris.
Although considered controversial by some ophthalmologists, refractive surgery should not be ruled out completely in paediatric patients if strict selection criteria are adhered to and there are no other acceptable alternatives, noted Dr Jacob, Director and Chief at Dr Agarwal’s Refractive and Cornea Foundation, Chennai, India.
“Refractive surgery may be appropriate in bilateral high refractive error or unilateral severe anisometropia with amblyopia in children who cannot wear glasses or contact lenses. The majority of children with ametropia do well with glasses or contact lenses but a small minority do not. Refractive surgery can give them visual improvement, as well as social and psychological benefits that should not be underestimated,” she said.
Refractive surgery is particularly challenging in young patients, said Dr Jacob.
“We are dealing with an eye that is still growing and with changing refractive status. The preoperative assessment, the surgery itself, and postoperative assessment, are all more difficult in paediatric patients,” she said.
The advantages of refractive surgery in indicated children include a reduced chance for amblyopia, a better chance of binocularity, full-time correction of refractive error, and the outcome is not dependent on compliance, she said. It also avoids difficulties, challenges and risks associated with contact lens wear, she said.

“It is a safe procedure with the use of corneal suction and an immobile cap. There is less risk of flap rubbing, displacement,
epithelial ingrowth or striae, and also less chance of general anaesthesia gases affecting the machine settings and outcomes. There is no need to shift between machines, there is less dry eye and better biomechanics,” she said.
Drawbacks of SMILE include the fact that it cannot currently be used to treat hyperopia or higher-order aberrations, said Dr Jacob.
To date, she said that she has successfully treated seven paediatric patients with a mean age of 10 years, all of whom were suffering from anisometropic amblyopia.
She advised, however, that rigorous follow-up for residual refractive error and occlusion therapy is required after surgery for these young patients.
Soosan Jacob: dr_soosanj@hotmail.com

EUROTIMES | MAY 2020
PAEDIATRIC OPHTHALMOLOGY 38
more at https://elearning.escrs.org
Keep learning. Whenever, wherever.
Learn
Soosan Jacob MS, FRCS
5th World Congress of Paediatric
Ophthalmology and Strabismus
2–4 October 2020 | RAI Amsterdam, The Netherlands
Keynotes
Friday 2 October 2020
David Mackey AUSTRALIA
Non-Strabismus Keynote Lecture
Genes and Environment: Towards Personalised Prevention of Myopia in Children
Saturday 3 October 2020
Burton Kushner USA
Strabismus Keynote Lecture


Forty-Five Years of Studying Intermittent Exotro pia — What Have I Learned
Sunday 4 October 2020
Marie-José Tassignon BELGIUM

Kanski Medal Lecture
A Thing of Beauty is a Joy Forever
Registration Open
Membership to WSPOS is available for FREE online
WCPOS V | 2020
www.wspos.org
All in the family
German company celebrates 125 years of innovation. Aidan Hanratty reports

Oculus has always been a family business. Originally established in 1895 by Alois Mager, it was originally called the A. Mager Specialist Factory for Ophthalmological Instruments [A. Mager Spezialfabrik Ophthalmologischer Instrumente]. Early products included a universal trial frame, an ophthalmoscope, a Javal ophthalmometer and a Förster arc perimeter.
Mager’s son Wilhelm joined the company in 1922, and acted as managing director from 1924 until 1956. In that time the company name changed to Oculus (1932) and the firm moved from Berlin to the “optic town” of Wetzlar (1947). It was at this time that graduate engineer Kurt Kirchhübel joined the company as additional managing director, a role he held until 1986.
Kurt’s son Rainer joined the company in 1979 and became a member of the board two years later. Today he is co-director with his own son, Christian, while his wife Rita is Marketing Director.

Just as the key personnel can trace a long lineage, so do some of the key components of the business. Trial frames have been a key part of the company since the beginning. The current standard, the UB 6, is composed of 166 parts, all of which are crafted and assembled by hand on site in Wetzlar.
These frames “keep the company going”, according to Christian. Providing a highquality product at a reasonable price point is a core competency for Oculus, especially when another one of those core aims is the durability of its machines. “What I want to put in the foreground is the sustainability of the devices,” said Rita.
“You will not find a used Pentacam on the entire market, it has been on the market since
2002. We have been serving our customers with software updates and extensions for decades.”
Similarly, the concept of static perimetry goes back to the company’s work with the University Eye Clinic in Tübingen in 1958, resulting in the creation of the “Tübinger Hand-Perimeter”.
“This static perimetry is the basic requirement that we have in all automatic
40
EUROTIMES | MAY 2020 OUTLOOK ON INDUSTRY
Kerstin Kirchhübel, Christian Kirchhübel, Rainer Kirchhübel, Rita Kirchhübel and Matthias Kirchhübel
Oculus headquarters in Wetzlar
Images courtesy of OCULUS
perimeters today,” said Rainer. “Not only in our devices but all automatic perimeters that are offered in the world – they all work with static perimetry. The device here was a highly complex, scientific device – you almost had to be trained in Tübingen to operate it.”
On the company’s 100th anniversary in 1995 they launched the Twinfield device, offering static and kinetic perimetry as both manual and automatic options. They now offer four devices for visual field tests, for a range of markets.
That’s not to say that everything is refined and updated. In 1985 the company developed the SDI/BIOM (stereoscopic diagonal inverter and binocular indirect ophthalmomicroscope) for wide-angle vitreoretinal surgery. The BIOM is now on its fifth generation, with automatic and manual inversion as well as accompanying customisable sterilisation packs.
In 2019 it introduced the Myopia Master, an all-in-one device for performing refraction, axial length measurement and keratometry. The device creates reports for each patient, as well as taking into account risk factors such as family history and lifestyle.

Oculus has also collaborated with the Brien Holden Vision Institute in Australia (BHVI), incorporating its algorithms for tracking and estimating refractive error into the device. Available to opticians, optometrists and ophthalmologists, this device may prove key in the management of myopia in the face of a global epidemic.
Sustainability is a key factor for Oculus, and that’s evident on all levels of operations in their factory in Wetzlar, where EuroTimes attended a press day to mark the company’s 125th anniversary. The company runs an apprenticeship programme, taking teenagers into their workshops and training them in all aspects of engineering. They learn to make and build things, operate machinery and so on. A small display showed items made by apprentices, including race cars, a foosball table, a chess set and a hammer. As Christian says, if apprentices don’t understand the most basic principles of how things are made, they won’t understand the bigger picture.
The company has trained 74 industrial mechanics in the past 20 years. These are now working across the board in preparation, assembly and service, as industrial mechanics and electronic technicians.
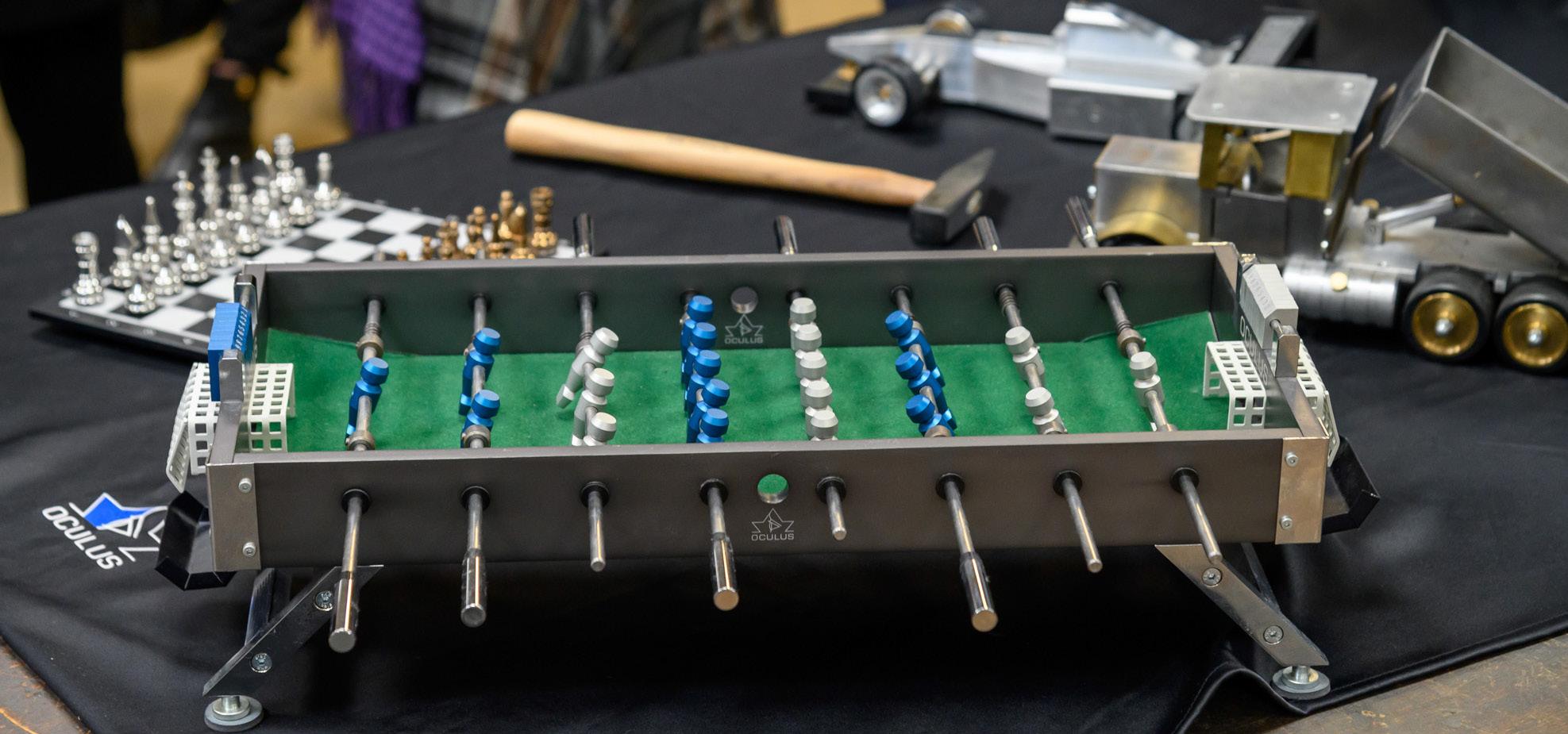
“We have a total of 400 employees here today, that’s a quarter of the employees who are trained here,” says Rainer. “If you then look at the fact that another 100 of the 400 have been in the house for more than 25 years – that’s a long bond. We have a relatively low turnover, we are actually very proud that once someone has decided to work here, they will stay here.”

The Pentacam, which was introduced to the market in 2002, is now the flagship device in the Oculus arsenal. A rotating Scheimpflug camera system for anterior segment analysis, it measures topography
and elevation of the anterior and posterior corneal surface as well as corneal thickness. Further to the original device, there is also the Pentacam HR, offering high-resolution imaging, and the Pentacam AXL, with integrated axial length measurement for IOL calculations. Furthermore, in 2019 the company introduced the Pentcam AXL Wave, offering wavefront aberrometry along with Scheimpflug tomography, optical biometry, refraction and retroillumination.
As well as selling these devices, Oculus makes sure to inform its customers how to use them. The company runs an academy with domestic and international symposia on a regular basis. “This year we trained 1,636 opticians and ophthalmologists with the academy,” said Rainer. “And this is not just advertising for Oculus products, I think you take something away with you where you see a completely different area of application.”
“It is increasingly the case that the device itself has become so complex by now,” adds Christian.” “Many people buy a device and find that they only use it so much and could actually do so much more.” The academy therefore shows the full scope of possibility with each device.
On a lighter note, the company is proud to have on its walls the largest eye test in
the world. Along with the completion of the company’s new logistics centre in 2015, they placed on the outer walls a vision test that can be seen from a viewing platform 1.5km away.
“We had [former world number one table tennis player] Timo Boll here with us as a guest of honour; he tried the test first –he passed the test quite well. We then tested internally with him here too, I think he managed a visual acuity of 1.6 or 2.0, which is why he can play table tennis quite well,” said Rainer.
From small beginnings to world records, it’s clear this family business is in good shape for looking to its next milestone.
41
EUROTIMES | MAY 2020 OUTLOOK ON INDUSTRY
The Pentacam AXL
Examples of designs produced by apprentice engineers
Matthias Kirchhübel leads a tour of the facility
AMSTERDAM
3 TO KNOW...
DON’T DO THINGS BY HALVES IN AMSTERDAM
My first day in Amsterdam I asked the concierge to book me a taxi for an appointment at ‘half six’ that evening and showed him the dinner address. He said “it’s not far… 5.15 should be fine”. We caught my mistake before he made the booking. In the Netherlands, half six means half way before the hour of six, not a half hour after six as it does to me. To add to the confusion, some hotels and restaurants, used to English visitors, use the phrase in the ‘English’ sense. When speaking of time, the Dutch use the 12-hour clock but without AM and PM. Phrases like in the morning, in the afternoon or in the evening clarify the time frame. In writing, both the 12-hour and the 24-hour clock are used.
DEBIT OVER CREDIT, WHILE CASH IS KING
You may find credit cards less commonly accepted in Amsterdam than in other European countries. Many restaurants and shops in the city don’t accept them at all. Some establishments add a 5% charge for card payment. Visa and Mastercard are the most widely accepted but you will need a four-digit Personal Identity Number, so check you have one before you travel. Debit cards are widely used; smaller shops may prefer cash and you can top up your supply at ATMs with your debit card. Taxis accept debit, Visa and Mastercards, but if you would prefer to pay in cash be sure to have some smaller denomination bills with you.
CITY CARD HELPS YOU TRAVEL AND SEE THE CITY WITHOUT DELAY OR FUSS
Buy an I amsterdam City Card online before you arrive. Armed with this, you can hop on buses, trams, ferries and metros – even a one-hour canal cruise and a one-day bike rental – without stopping to buy tickets. You can also enter almost over 70 museums without delay or fuss – even the booked out Van Gogh Museum (you need to make a time-slot reservation though, which you can do up to two months in advance.) The I amsterdam City Card come in five time frames, from 24 hours at €65 to 120 hours at €130. Visit iamsterdam.com
Smart shopping
Sustainable fashion and timeless etchings.
Maryalicia Post reports
This is the year of the ‘buy it diet’, the year the penny dropped in the fashion industry. The rate of consumption of fast fashion is being widely viewed as unsustainable. For the story behind the story, stop off in Amsterdam’s extraordinary exhibition space, Fashion for Good: “The world’s first interactive museum for sustainable fashion.”
Installed across three floors of an imposing Rokin Square building, Fashion for Good is not only fact-filled, it’s funfilled; this lively, multi-faceted presentation borrows techniques from gaming to involve you in the action. Along the way you discover that subjects such as non-toxic fabric dye and textile recycling are much more interesting than you might have imagined There’s an on-site store featuring eco-friendly apparel, while in the museum’s Studio you can custom-design your own cotton polyester tee shirt as you’re walked through the eight steps involved in the process. The experience itself is designed to change the way you shop.

Having honed your sustainability sensibility, Amsterdam’s shops offer a chance to exercise it. Here are four shops to try: Nukuhiva. Sustainable fashion, accessories and shoes for men and women. Trendy urban brands include People Tree, Alchemist, HoodLamb and Nudie Jeans, Haarlemmerstraat 36, 1013 ES Amsterdam; Het Faire Oosten features local products and Fair Trade options in gifts, fashion, homeware and food, Oostpoort, Waldenlaan 208, 1093 NH Amsterdam; Charlie & Mary, a shop celebrating ‘true fashion’, where brands have been chosen for their use of organic cotton, hemp and recycled materials plus a range of sustainable jewellery using recycled silver and gold. Gerard Doustraat 84, 1072 VW Amsterdam; O My Bag products, which
include weekend bags, passport cases, iPad covers and clutches, provide small communities in India with a sustainable livelihood; the leather used is tanned using no chemical products. Ceintuurbaan 117-H, 1072 EZ Amsterdam.
On a random stroll in Amsterdam one Sunday afternoon, I came upon the Art Market on the Spui, where I was intrigued by the elegant engravings of Wim Van Der Meij. They are evocative, original, easily transportable and reasonably priced – in fact, the ideal souvenir of a visit to the Netherlands as well as a striking addition to any room decor. Delegates to the 38th ESCRS Congress in Amsterdam can expect to find Mr Van Der Meij at his stand in the Spui Art Market on Sunday 4 October from 11.00-18.00. Otherwise, contact the artist directly to arrange a visit to his studio in Zutphen, a picturesque 1,700-year-old village about an hour and a half by train or car from Amsterdam.
For an overview of Mr Van Der Meij’s work, including sizes and prices, have a look at his website, where you’ll also find his contact details : www.wimvandermeij.nl.
 Etching by Wim Van Der Meij
Etching by Wim Van Der Meij
EXPLORING AMSTERDAM 42 EUROTIMES | MAY 2020
Fashion for Good, “the world’s first interactive museum for sustainable fashion”
LEIGH SPIELBERG MD Books Editor
BOOK Reviews
PUBLICATION
OCULOPLASTIC SURGERY: THIRD EDITION
EDITORS
BRIAN LEATHERBARROW

PUBLISHED BY THIEME
Refresher course and reference work in one
Oculoplastic surgery is a remarkably broad subspecialty with a wide range of pathologies and approaches, from the simple blepharoplasty to the repair of complex traumatic cases.
Oculoplastic Surgery: Third Edition (Thieme), by Brian Leatherbarrow, succeeds in bringing it all together. Texts this size are usually collaborations, with each chapter being written by one or more contributors, but this book is a solo work, and the 700page text reflects the author’s “more than 25 years of experience and multidisciplinary collaboration in treating patients with a wide spectrum of oculoplastic, orbital and lacrimal conditions”.

It is comprehensive. Section I outlines the “Basic Principles,” both surgical and anatomical. It serves as both a refresher course and a reference work, delving into details such as the correct selection of suture needles and the refinement of suture techniques.
Section II devotes 250 pages to eyelid surgery, from upper and lower eyelid entropion through thyroid-related eyelid retraction and facial palsy to the use of autologous grafts in ophthalmic plastic surgery. The crucial points of many procedures are illustrated with high-quality surgical photographs and, where necessary, detailed artwork by Philip Ferguson Jones, a highly skilled medical illustrator.
Cosmetic surgery is the topic covered in Section III, starting with “The Evaluation and Management of the Cosmetic Patient”, and then detailing blepharoplasty, complications of blepharoplasty and the management of brow ptosis. This section is likely to be of greatest interest to those ophthalmologists who have incorporated basic cosmetic eyelid procedures into their practice.
Section IV, “Orbital Surgery”, literally moves deeper, opening with a review of orbital disorders and then a chapter devoted to surgical approaches to the orbit. Thyroid eye disease also gets its own chapter. Sections V, VI and VI are devoted to Lacrimal Surgery, Socket Surgery and Trauma, respectively.
This book, which includes access to an eBook on MedOne, Thieme’s online platform, is appropriate for oculoplastic fellows, plastic surgery fellows with a particular interest in the upper face, ambitious residents and ophthalmologists who perform extraocular surgery at any degree of complexity, from simple to spectacular.
NOTHING LEFT OUT OF THIS COMPREHENSIVE TEXT
The Practical Handbook for Small-Gauge Vitrectomy: A Step-By-Step Introduction to Surgical Techniques (Springer), is currently in its second edition. Written by Ulrich Spandau and Heinrich Heimann, this 365-page handbook serves as a comprehensive reference text for the (aspiring) vitreoretinal surgeon.
PUBLICATION
CLINICAL PATHWAYS IN NEURO-OPHTHALMOLOGY
EDITORS
STACY SMITH, ANDREW LEE, PAUL BRAZIS
PUBLISHED BY THIEME
DIDACTIC TEXT LAYS SOLID FOUNDATION
I love focused, didactic ophthalmology texts in which each clearly defined symptom, sign or specific diagnosis is tackled separately and on its own accord.
Clinical Pathways in Neuro-Ophthalmology: An Evidence-Based Approach (Thieme), edited by Drs Smith, Lee and Brazis, intends to “lay a solid foundation” by approaching problems systematically. Simplicity is the goal. Incorporating my personal favourite tool, the flow-chart, common problems like transient vision loss, visual field defects and diplopia are handled with as much care as rarer and more difficult entities like supranuclear disorders of gaze and optic disc oedema with a macular star and neuroretinitis.
The text is most appropriate for ophthalmology residents, especially those preparing for a neuro-ophthalmology rotation or exam, as well as general ophthalmologists looking to refresh their knowledge.
PUBLICATION
ADVANCES IN VISION RESEARCH VOL II
EDITORS
GYAN PRAKESH AND TAKESHI IWATA
PUBLISHED BY SPRINGER
THE CURRENT STATE OF RESEARCH AND INSIGHT
Advances in Vision Research, Volume II (Springer) covers “Genetic Eye Research in Asia and the Pacific”. Edited by Gyan Prakesh and Takeshi Iwata, this text, part of the “Essentials in Ophthalmology” series, is a resource on the current state of research and insight into a historically under-investigated population that also happens to be the largest in the world.


PUBLICATION
SMALL-GAUGE VITRECTOMY EDITORS
ULRICH SPANDAU AND HEINRICH HEIMANN
PUBLISHED BY SPRINGER
EUROTIMES |
Covering everything from equipment recommendations to all the major procedures in vitreoretinal surgery, such as macular peeling, submacular haemorrhage, suprachoroidal haemorrhage, intraocular tumour biopsies and intraocular foreign bodies, nothing seems to have been left out.
High-quality surgical photographs and informative illustrations help the reader, particularly young surgeons, visualise what is being discussed. This is especially useful for the chapter on difficult proliferative diabetic retinopathy.
This book is appropriate for ambitious ophthalmology residents preparing for their vitreoretinal surgery rotation, vitreoretinal fellows and young VR surgeons.
Examples of topics covered are “Stargardt Disease in Asian Populations”, “Genomic Approaches to Eye Diseases: An Asian Perspective” and “Myopia Genes in Asians.”
This book is intended for researchers, epidemiologists with interest in genetic disease and ophthalmologists with a particular focus on genetic eye disease who also see a significant number of patients of Asian or Pacific origin.
If you have a book you would like to have reviewed please send it to: EuroTimes, Temple House, Temple Road, Blackrock, Co Dublin, Ireland
BOOK REVIEWS 43
MONTH YEAR
EUROTIMES | MAY 2020 PUBLICATION PRACTICAL HANDBOOK FOR SMALL-GAUGE VITRECTOMY EDITORS ULRICH SPANDAU AND HEINRICH HEIMANN PUBLISHED BY SPRINGER
Join Track
the EUREQUO Platform your Surgical Results
Convenient Web-Based Registry
Cataract, Refractive and Patient Reported Outcomes in One Platform
The patient-reported outcome is linked to clinical data in EUREQUO. This enables better knowledge of indications for surgery and o ers a tool for clinical improvement work based on the patients’ outcome.
Glaucoma screening

Allergan, Sightsavers and the International Agency for the Prevention of Blindness (IAPB) has announced the launch of a joint initiative – ‘Keep Sight India’ – a community-based glaucoma screening programme to prevent glaucoma-related vision loss in Ganjam District, Odisha. The programme provides training for healthcare professionals to screen at-risk populations, ensure early and accurate diagnosis and provide appropriate treatment and long-term care to make a positive impact on people with glaucoma at all levels of comprehensive eye care.
Sightsavers India CEO RN Mohanty said: “We are excited to be partnering with Allergan, an organisation with a long legacy in eye care.
“India will play a crucial role in meeting WHO’s targets for eye health”, said Joanna Conlon, Director of Development and Communications, IAPB. “Keep Sight will work with Indian partners to support and extend India’s successes around eye health and glaucoma,” she said. www.allergan.com
VIVEO CORNEAL MICROSCOPE
Heidelberg Engineering has announced the reintroduction of its HRT3 Rostock Cornea Module (RCM) to offer in vivo corneal confocal microscopy in its anterior segment product portfolio.
“The relaunch of the HRT3 RCM is exciting as this unique imaging device aids the ophthalmologist in the diagnosis of corneal diseases by allowing imaging at a cellular level,” said says Dr Jaya Chidambaram BSc (Hons), MBBS, MRCOphth, PhD, Senior Lecturer, University of Manchester, United Kingdom.
www.heidelberg engineering.com/ int/company
INNOVATION AND STRATEGY
Julius Müller-Albinus has joined Geuder AG as Head of Innovation Management and Strategy.
Mr Müller-Albinus will be responsible for establishing sustainable innovation processes, realising management projects that will foster innovation and expanding strategic partnerships.
“Julius Müller-Albinus has profound market, product and user knowledge in the field of ophthalmic surgery and he will support us with comprehensive expertise in actively positioning the company and expanding our market position”, said Geuder AG CEO Volker Geuder. www.geuder.de
INDUSTRY NEWS 44
EUREQUO is free of charge for all ESCRS members www.eurequo.org
INDUSTRY NEWS
EUROTIMES | MAY 2020
COVID-19 INTERACTIVE PLATFORM

The ESCRS is committed to giving the ophthalmology community every support in the coming weeks and months. To encourage and facilitate communication, we have established an ESCRS COVID-19 Interactive Platform.
We want to hear from you with stories, suggestions or ideas, national recommendations and guidelines. Please send all your items to covid19@escrs.org or use wetransfer.com for larger fi les
Drawing a line
With governments across the globe introducing measures to stop the spread of the coronavirus, many people are finding themselves working from home for the first time. While this may seem like a dream – no commute! No need to look your best! – it comes with its own challenges.
The lines between work and rest can quickly become blurred, with no clear start or end to the day. With that in mind, it’s important to establish a routine.

Maybe this could be done by having a daily call with a boss or colleague. Maybe it’s taking lunch at the same time and stepping outside for a while (where safe and where possible).
Be sure to communicate with your management about when your “off” time starts, so you’re not fielding calls when your day is over or eating into your dinner time with unexpected emails.
What all this also means, sadly, is that you may have to say to your children that they can’t sit on your lap or play with you until your “very important work” is finished!
Conversely, if you do end up working outside of your regular hours, it’s important to let your kids enjoy some of that time you’re spending at home, be it horsing around on the floor or drawing and colouring in at the table.
Of course, as I write this many ophthalmologists are in a kind of interbellum period, having cancelled elective surgery and waiting to be drafted on to the frontlines in the fight against the coronavirus pandemic. Some will be stuck at home longer than usual, waiting to show up to work as part of a skeletal team in their institutions.
In these times it’s important to keep occupied, hard as it is with a looming catastrophe taking up space in your mind and on the headlines. That can be done by reading, exercise, video games or even baking. Across the world people are escaping into books (be they pandemic related, like Emily St John Mandel’s Station Eleven or The Old Drift by Namwali Serpell, or something completely unrelated like Hilary Mantel’s Wolf Hall conclusion The Mirror & the Light or Household Gods and Other Narrative
Offences, free stories from Tade Thompson);
There are many online resources for people who can’t get out to run or go to the gym. These include the wildly popular Yoga With Adriene, as well as Joe Wicks’s channel, which includes a daily “PE lesson” for kids and adults alike.
The Nintendo Switch console is increasing in demand, with many retailers selling out and prices on third-party sites rising accordingly. For those already in possession of the device, the island life simulator game Animal Crossing is becoming a major hit. Finally, some people are getting back to basics and baking their own bread.
There are many benefits to baking, beyond having something delicious to eat as an end product. Key among them is the practising of mindfulness. Speaking to HuffPost, associate professor of psychological and brain sciences at Boston University, Donna Pincus said: “Baking actually requires a lot of full attention. You have to measure, focus physically on rolling out dough. If you’re focusing on smell and taste, on being present with what you’re creating, that act of mindfulness in that present moment can also have a result in stress reduction.”
According to Pincus, this activity and focus will mean “you’re not spending time ruminating over your thoughts, we know that rumination leads to depression and sad thoughts”. Focusing on your bread may be a simple but effective way to keep your mind off the global pandemic for even a few hours.
Strange is it may sound, it’s important to carve out some “me” time. If you’re used to having a routine including an hour or two on the train and a walk around at lunchtime, it can be overwhelming losing that time for yourself. Sit down, take a breath, be by yourself. Just don’t think about yourself.
Keeping with the theme of looking after yourself, you may consider seeing a therapist. Many are now operating via video platforms such as Zoom, so you can talk to someone without leaving your home. If you’re already seeing someone, see if they can accommodate you in this way.
It probably won’t be an easy time and there’s no telling how long it will last. It’s up to you what you do with it. Stay safe and be well.
46
Working and staying at home can be challenging. Aidan Hanratty reports
EUROTIMES | MAY 2020 RANDOM THOUGHTS
Due to the COVID-19 virus, a number of meetings have been cancelled or rescheduled. The information in this calendar is correct at the time of going to print; please check the meeting website or email the conference organisers to confirm all meeting dates.
MAY
VIRTUAL CONGRESS ASCRS
16 – 17 May
Boston, USA
https://annualmeeting.ascrs.org/
EyeAdvance 2020
29 – 31 May
Mumbai, India
SEPTEMBER
50th Cambridge Ophthalmological Symposium 2020 (COS 2020)
2 – 4 September
Cambridge, UK
https://www.cambridgesymposium.org/
32nd Meeting of the Club Jules Gonin 2020
↙ TO BE CONFIRMED
The following meetings have been postponed, dates to be confirmed:
European Paediatric Ophthalmological Society 2020 (EPOS 2020)
Copenhagen, Denmark
https://epos2020.dk/
20th EVRS Meeting 2020
Verona, Italy
http://www.evrs.eu
https://www.eyeadvance.org/
JUNE
VIRTUAL CONGRESS
World Ophthalmology Congress (WOC)
26 – 29 June
Cape Town, South Africa
http://woc2020.icoph.org
JULY
ASRS 2020
24 – 28 July
Seattle, USA
www.asrs.org
AUGUST
NEW DATE
34th Asia Pacific Academy of Opthamology Congress 2020 (APAO 2020)
5 – 9 August
Xiamen, China
http://2020.apaophth.org/
5th Asia Pacific Glaucoma Congress 2020 (APGC 2020)
14 – 16 August
Kuala Lumpur, Malaysia https://apgc2020.org/
2 – 5 September
Dubrovnik , Croatia

https://www.clubjulesgonin.com/ member/index.asp
5th International Glaucoma Symposium
4 – 5 September
Mainz, Germany
https://glaucoma-mainz.de/
SEPTEMBER
NEW DATE
SFO 2020 Congress
4 – 7 September
Paris, France
https://www.sfo.asso.fr/
Ophthalmic Anesthesia Society 34th Annual Scientific Meeting 2020 (OAS 2020)
11 – 13 September
Chicago, USA
https://eyeanesthesia.org/page-1271154
49th European Contact Lens and Ocular Surface Congress (ECLSO)
18 – 19 September
Paris, France
https://www.eclso.eu/
CALENDAR 47 EUROTIMES | MAY 2020
The 32nd Meeting of the Club Jules Gonin 2020 will be held in Dubrovnik, Croatia
OCTOBER
20th Euretina Congress
1 – 4 October
Amsterdam, The Netherlands
www.euretina.org
11th EuCornea Congress
2 – 3 October
Amsterdam, The Netherlands
www.eucornea.org
WCPOS V
5th World Congress of Paediatric Ophthalmology and Strabismus
2 – 4 October
Amsterdam, The Netherlands
www.wspos.org
38th Congress of the ESCRS
3 – 7 October
Amsterdam, The Netherlands

www.escrs.org
NOVEMBER
AAO Annual
Meeting 2020
14 – 17 November
Las Vegas, USA
www.aao.org
100th SOI National Congress
25 – 28 November
Rome, Italy
https://www.congressisoi.com
NEW DATE
XXI International Congress of the Brazilian Society of Ophthalmology
26–28 November
Rio de Janeiro, Brazil
https://sistemacenacon.com.br/site/ sbo2020/mensagem
DECEMBER
NEW DATE
14th EGS Congress
14 - 16 December
Brussels, Belgium
https://www.eugs.org/eng/ default.asp
2021
MARCH
NEW DATE
6th San Raffaele OCT Forum
5 – 6 March
Milan, Italy
https://www.octforum2020.eu/
JUNE
NEW DATE
AECOS 2021 European Symposium
3 – 6 June Florence, Italy https://aecosurgery.org/ 2021-european-symposium/
JULY
NEW
AECOS 2021 Summer Symposium
15 – 18 July Utah, USA https://aecosurgery.org/ 2020-summer-symposium/
ESCRS Membership
JULY
NEW DATE
33rd Asia-Pacific Association of Cataract & Refractive Surgeon Annual Meeting (APACRS)
29 – 31 July
Suntec City, Singapore
https://apacrs-snec2020.org/
• Reduced Registration Fees for ESCRS Congresses

• Subscription to Journal of Cataract & Refractive Surgery
• Access to ESCRS Grants, Bursaries and Research Awards

Access to:
• ESCRS iLearn
Online CME accredited interactive courses
• ESCRS On Demand
Online library of presentations from ESCRS Congresses

• EUREQUO
European Registry of Quality Outcomes for Cataract and Refractive Surgery
• ECCTR
European Cornea and Cell Transplantation Registry
Join today.
CALENDAR 48
5 year membership for trainees
FREE
www.escrs.org
EUROTIMES | MAY 2020
The 38th Congress of the ESCRS, 20th Euretina Congress, 11th EuCornea Congress and 5th World Congress of Paediatric Ophthalmology and Strabismus will be held in Amsterdam, The Netherlands
Main Symposia
Dealing with the Traumatized Cornea
Cataract Surgery in Patients with AMD
20/20 in 2020: The Lens
20/20 in 2020: The Cornea
The Next Decade of Cataract Surgery
What to Do When the Unexpected Happens
Ridley Medal Lecture
David Chang USA
Five Compelling Lessons from the Greatest Team of Cataract Surgeons
www.escrs.org
38th Congress 3-7 October, R AI Amsterdam Amsterdam 2020
ADVANCED CONTROL CENTER, AT YOUR FINGERTIPS

The CENTURION® Vision System1 with ACTIVE SENTRY® Handpiece safeguards every outcome with smooth phaco performance:*
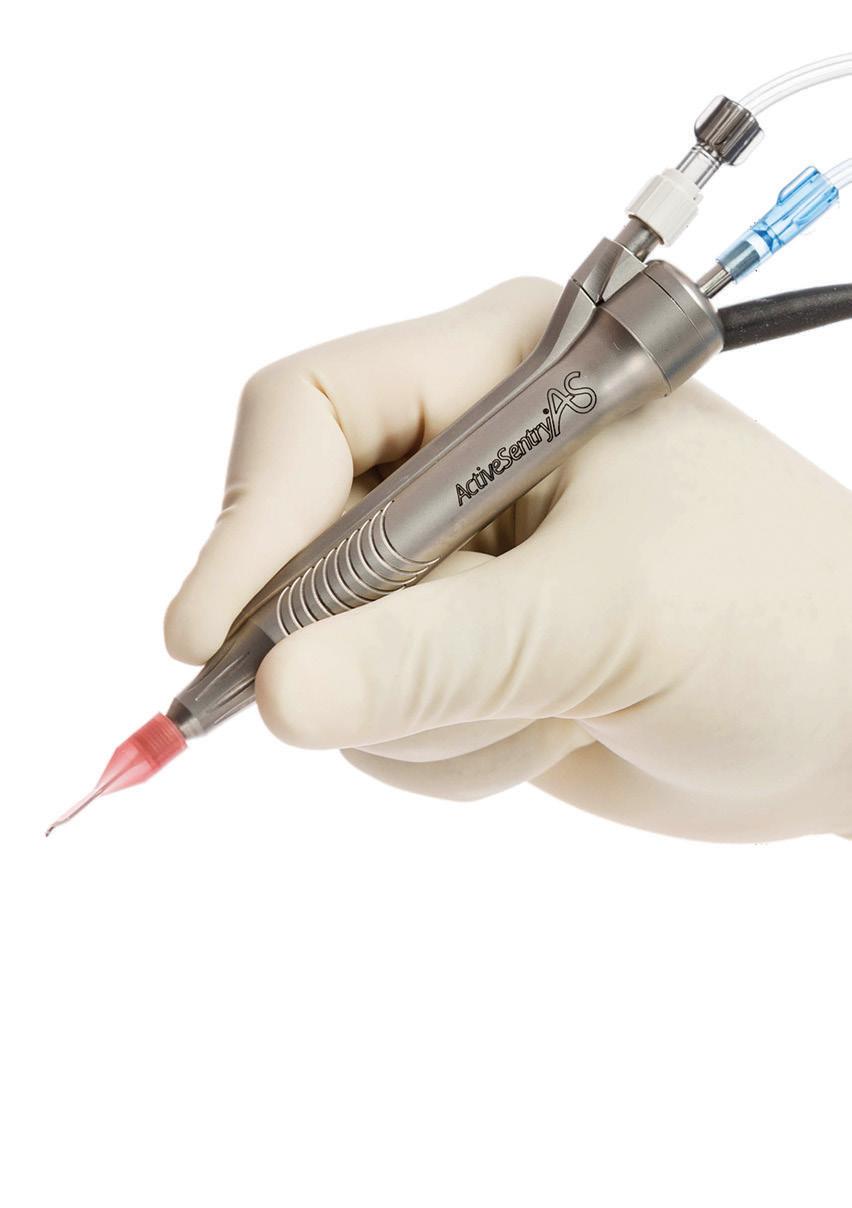
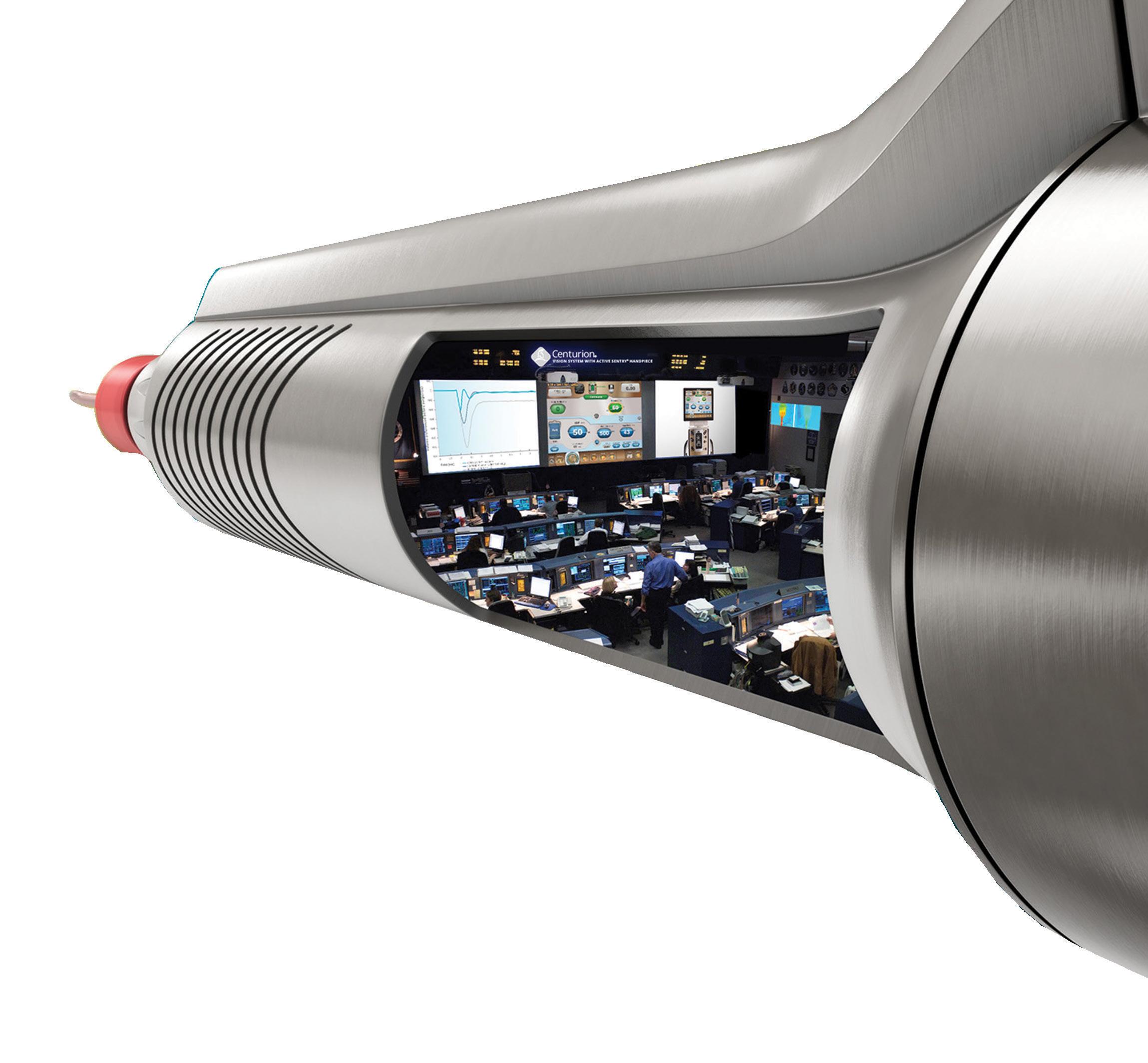
• Reduces surge by detecting pressure and triggering precise adjustments to ensure consistency
• Maintains target IOP – regardless of PEL – with Active Fluidics™ Technology 3-6
• Maintains stability across a variety of vacuum levels 4,5,7
• Reduces phaco procedure times, as well as fluid use8,9
• Protects eye from heat injury
8,10,11
• INTREPID ® Hybrid Tip helps reduce the risk of capsular tears and improves safety in the OR 12,13
Refer to the Directions for Use and Operator’s Manual for a complete listing of indications, warnings, cautions and notes. * Compared to previous generations of Alcon phaco systems.
1. Centurion® Vision System Operating Manual. 2.Active Sentry ® pressure sensing handpiece directions for use. 3.Alcon data on file, Ref. 02559, 03.05.2017. 4. Thorne A. et al. Phacoemulsifier occlusion break surge volume reduction. J Cataract Refract Surg 2018; 44:1491–1496. 5. Nicoli CM, Dimalanta R, Miller K. Experimental anterior chamber maintenance in active versus passive phacoemulsification fluidics systems. J Cataract Refract Surg. 2016;42(1):157-162. 6. Boukhny M, Sorensen G, Gordon R. A novel phacoemulsification system utilizing feedback based IOP target control. ASCRS-ASOA Symposium and Congress; April 25-29, 2014; Boston, MA. 7. Aravena et al. Aqueous volume loss associated with occlusion break surge in phacoemulsifiers from 4 different manufacturers. J Cataract Refract Surg. 2018; 44:884–888. 8. Khokhar S, Aron N, Sen S, Pillay G, Agarwal E. Effect of balanced phacoemulsification tip on the outcomes of torsional phacoemulsification using an active-fluidics system. J Cataract Refract Surg. 2017;43(1):22-28. 9. Solomon et al. Clinical study using a new phacoemulsification system with surgical intraocular pressure control. J Cataract Refract Surg. 2016; 42:542–549. 10. Zacharías J. Laboratory assessment of thermal characteristics of three phacoemulsification tip designs operated using torsional ultrasound. Clinical Ophthalmology 2016:10 1095–1101. 11. Zacharías J. Comparative thermal characterization of phacoemulsification probes operated in elliptical, torsional and longitudinal ultrasound modalities. ASCRS-ASOA Symposium and Congress; April 25-29, 2014; Boston, MA. 12. Shumway C et al. Evaluation of the capsular safety of a new hybrid phacoemulsification tip in a cadaver eye model. J Cataract Refract Surg. 2019; 45:1660–1664. 13. Centurion® FMS pack directions for use.
© 2020 Alcon Inc 03/20 EMEA-CAT-2000001 Centurion® VISION SYSTEM WITH ACTIVE SENTR Y® HANDPIECE Contact your Alcon representative to learn more about bringing a new level of safety and efficiency to your procedures.















































 Thomas Olsen: tolsenmail@gmail.com
Thomas Olsen: tolsenmail@gmail.com
























 Guttman Krader reports
Guttman Krader reports
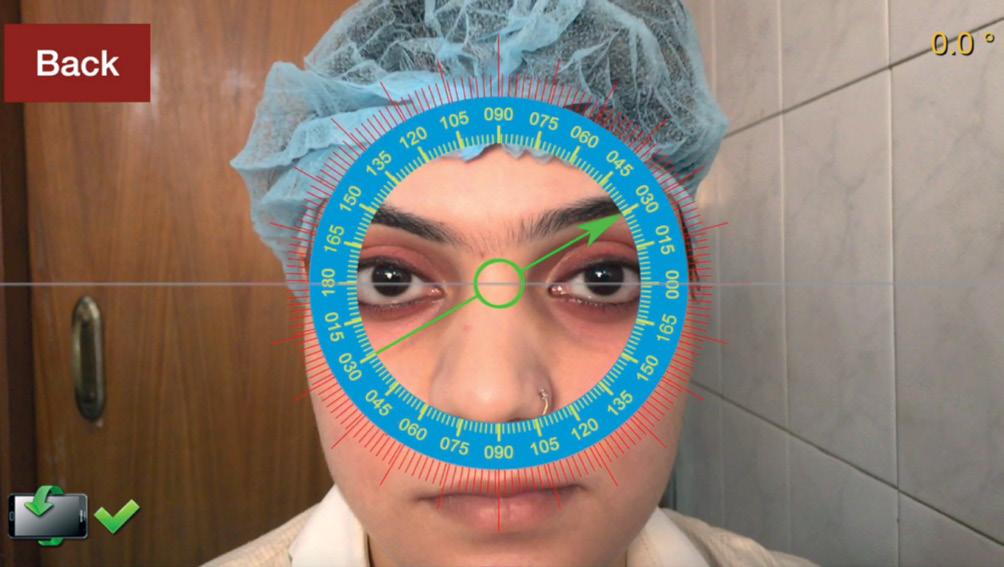







































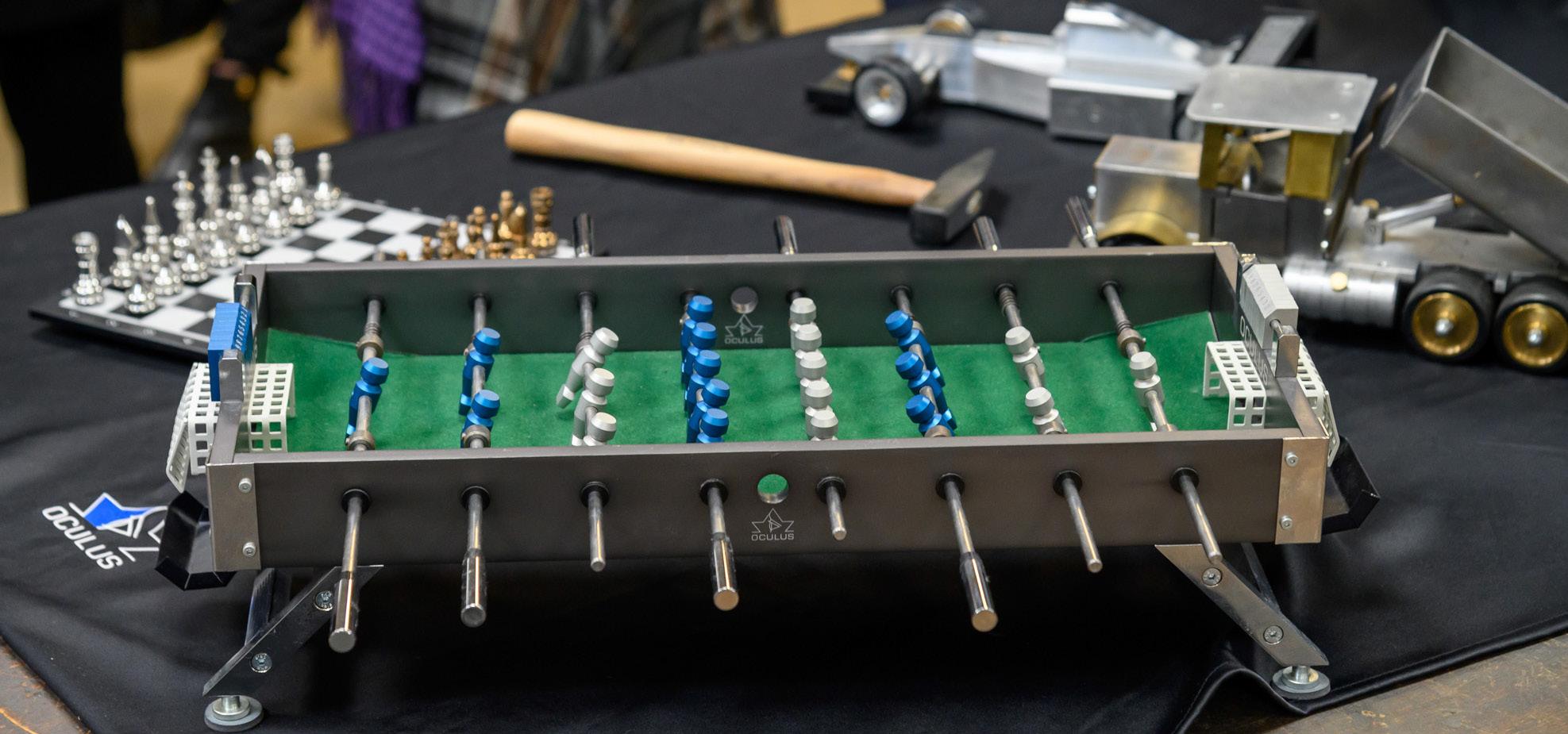


 Etching by Wim Van Der Meij
Etching by Wim Van Der Meij