





Independent medical education supported by Alcon and Zeiss.







Independent medical education supported by Alcon and Zeiss.
BY BRUCE ALLAN, MD, FRCS
Modern cataract surgery is increasingly considered as a refractive procedure. As a result, meticulous preoperative evaluation, precise surgical planning, and optimization of postoperative outcomes are emphasized more now than ever before. One way to streamline workflows, optimize results, and enhance the patient experience is to integrate advanced technologies in a digital operating room (OR) setting.
Conversations about a digital OR often focus on isolated technologies. The most important aspect of a digital OR, however, is software integration. A digital OR therefore should refer to a cohesive system where imaging tools, surgical planning software, intraoperative guidance and visualization technology, safety checks, and outcomes reporting form a seamless, virtuous circle. This vision is achievable if the systems utilized can communicate and work in harmony.
The 2023 ESCRS Clinical Trends Survey, with more than 3,000 respondents, highlights critical insights into the adoption of digital tools in ophthalmic surgery. Although 68% of delegates reported they do not currently use digital visualization technology during cataract surgery, 40% of them said they plan to in the near future. The other 28% indicated that they do not plan on integrating digital visualization technology. Not surprisingly, those with higher surgical volume are ahead in leveraging digital systems (Figure 1), possibly because they are more likely to have the resources to invest in IT infrastructure. The challenge is to make such innovations accessible across all practice settings.
DOR usage by Annual Cataract Surgery Volume
What do you believe to be the main advantages of working in a digital operating room (DOR)? (Select all that apply.)
systems to reduce the physical strain (i.e., pain and soreness) of conventional microscopes, an issue that 79% of surgeons report dealing with, whether occasionally (41%), very rarely (28%), or almost always (10%). Other advantages of a digital OR are improved surgical outcomes, optics and safety, and shortened procedure time (Figure 2).
The most important aspect of a digital OR is software integration.
The two main advantages cited for working in a digital OR were improved efficiency and workflow (52%) as well as ergonomic benefits (47%). The latter underscores the importance of heads-up displays and advanced visualization
Cost is the primary barrier to more widespread adoption for most (75%) respondents, followed by space limitations (21%). Two other concerns are access to the technology (18%) and difficulty integrating the technologies with a current OR setup (17%). Many systems lock users into proprietary ecosystems, limiting flexibility. However, to advance digital OR integration, industry-wide collaboration is needed. Surgeons must advocate for systems that communicate effectively and are financially accessible.
Sharing and discussing challenges and unaddressed needs can help drive necessary changes to make the digital OR a reality for everyone. Close collaboration between industry and surgeons will shift the dial and bring the future of integrated ophthalmic surgery within reach.


Bruce Allan, MD, FRCS Consultant Ophthalmic Surgeon, Moorfields Private Eye Hospital, London
bruce.allan@ucl.ac.uk
FINANCIAL DISCLOSURE:
Professor Allan derives income from cataract surgery in private and NHS practice. He supervises research in digital health funded by the Frost Trust, University College London, ESCRS, and the NIHR BRC in Ophthalmology at Moorfields Eye Hospital and the UCL Institute of Ophthalmology
BY KAREN GLANDORF, MD, FEBO
Cataract surgery is one of the most common surgical interventions worldwide.1 More than 92% of individuals aged 80 and above undergo the procedure.2 As the world’s population continues to age, with an estimated 1.5 billion people over the age of 65 by 2050,3 the demand for cataract surgery is projected to soar. Managing the growing demand while maintaining surgical precision and efficiency is one of the biggest need facing ophthalmologists today.
The path toward streamlining the cataract patient’s journey while meeting their expectations and optimizing outcomes is a complex process. From patient counseling and precise preoperative measurements to IOL selection, power calculation, as well as alignment and implantation of an IOL, every phase of cataract surgery carries risks for errors (Figure 1). Thankfully, advancements in digital technology are transforming every step of the journey, making workflows more efficient, accurate, and patient-centered.
faster than a conventional non-digital workflow. They found digital preoperative assessments were completed 35% faster than manual assessments, and IOL power calculations were completed 30% faster. Additionally, there were 100% time savings in data transfer for surgery.4 Intraoperative time was also reduced with a digital workflow. Digital axis marking, which eliminated the need for manual marking, saved up to 3.1 minutes per case.
A truly connected workflow ... will be the key to unlocking even greater efficiencies and outcomes.
[Courtesy of Dr Glandorf]
There are six main goals of a digitally supported cataract surgery workflow: 1) minimize errors, 2) shorten surgery time, 3) improve efficiency and safety, 4) increase surgeon comfort and ergonomics, 5) amplify training and education, and 6) improve patient satisfaction.
Recent advancements have introduced tools like cloud-based surgical planning software, which integrates diagnostics with preoperative measurements and calculations to simplify preoperative planning. Additionally, computer-assisted toric IOL axis alignment and marking support decision-making. Advanced educational tools are also used to improve patient communication and enhance their overall experience. Collectively, integrating digital technologies into an OR helps create a single connected, streamlined workflow that traverses patient assessment and education, surgical planning, and treatment.
Two examples of platforms that support a digital workflow are the Zeiss Cataract Workflow and Alcon SmartCataract DX. Both systems ensure that preoperative measurements such as anterior chamber depth, keratometry, and axial length are automatically imported for precise IOL calculations and incision planning. They also eliminate the need for manual data entry, reduce errors, save time, facilitate digital guidance for IOL alignment, enhance precision and surgical outcomes. All these features are integrated into a single platform, accessible from anywhere.
Digital workflows save time at every step of the cataract surgery process (Figure 2). Rombold et al. showed that a digital cataract surgery workflow was two times
Decreasing the time commitments for preoperative assessment and for the surgical procedure not only enables surgeons to manage higher procedure volumes, but also reduces patient wait times and enhances overall satisfaction.
Another transformative aspect of digital technology is its impact on patient education and engagement. The use of patient-facing apps allows patients to complete intake forms and learn about cataract surgery and IOL options even before they set foot in the clinic. These apps also provide personalized reminders for appointments as well as pre- and postoperative instructions.
Patient education apps also improve doctors’ interactions with their patients. High-quality images, videos, and simulation tools help set realistic expectations and engage patients in shared decisionmaking. This interaction improves their understanding of the recommended technologies but also boosts their confidence in the surgical process.
Despite the myriad advancements in
Figure 2. A digital cataract surgery workflow is two times faster than a conventional non-digital workflow, with preoperative assessments and IOL power calculations completed 35% and 30% faster, respectively, and a 100% reduction in time spent on data transfer.4 [CC BY-NC 3.0]
digital technology, navigating the nuances of a digital OR setup is not without its limitations. Integration issues can pose a considerable hurdle. Tools for IOL calculations and incision planning provide excellent functionality, but when so called application programming interfaces (APIs) are missing, they do not work seamlessly with all diagnostic devices. As a result, manual data entry is still required, which is both time-consuming and prone to errors.
both surgeon comfort, patient outcomes, and supports a positive patient experience.
To fully realize the potential of digital workflows, continued advancements in system interoperability and data integration are necessary. A truly connected workflow—one that seamlessly integrates all diagnostic and surgical devices— will be the key to unlocking even greater efficiencies and outcomes. As the digital OR continues to improve, so too will our ability to meet the growing demand for cataract surgery.

Karen Glandorf, MD, FEBO, Augentagesklinik Precise Vision, Rheine, Germany k.glandorf@precise.vision
Burton MJ, Ramke J, Marques AP, et al. The Lancet global health commission on global eye health: vision beyond 2020. Lancet Glob Health. 2021;9(4):e489-e551.
2. Liu CY, Wilkins M, Kim T, Malyugin B, Mehta JS. Cataracts. Lancet 2017;390(10094):600-612.
Nevertheless, a digital OR is the future of cataract surgery. Its ability to save time, reduce errors, and improve efficiency and safety is undeniable. Moreover, by facilitating patient education and enabling precise surgical planning, it enhances
3. United Nations Department of Economic and Social Affairs. World population ageing 2019. Accessed November 20, 2024. https://www.un.org/ en/development/desa/population/publications/pdf/ageing/WorldPopulationAgeing2019-Highlights.pdf
4. Rombold F, Niederdellmann C, Pariti R, Khayat B. Time savings using a digital workflow versus a conventional for intraocular lens implantation in a corporate chain hospital setting. Clin Ophthalmol. 2024;18:113-119.
BY KJELL GUNNAR GUNDERSEN, MD, PHD
The evolution of technology plays a fundamental role in elevating patient care. Technology helps streamline workflows, refine surgical techniques, improve predictability and effectiveness, advance safety, and enhance surgical outcomes. In cataract surgery, artificial intelligence (AI)-powered platforms and 3D visualization systems are enabling surgeons to enhance precision, efficiency, and outcomes.
A digital operating room (OR) revolutionizes the way we approach preoperative measurements, surgical planning, and execution by integrating connected tools designed to improve planning, visualization, and execution. A fully connected ecosystem that enhances both precision and efficiency improves clinical results and patient care. Two main components—a high-definition, 3D visualization platform and AI-based data integration—stand out.
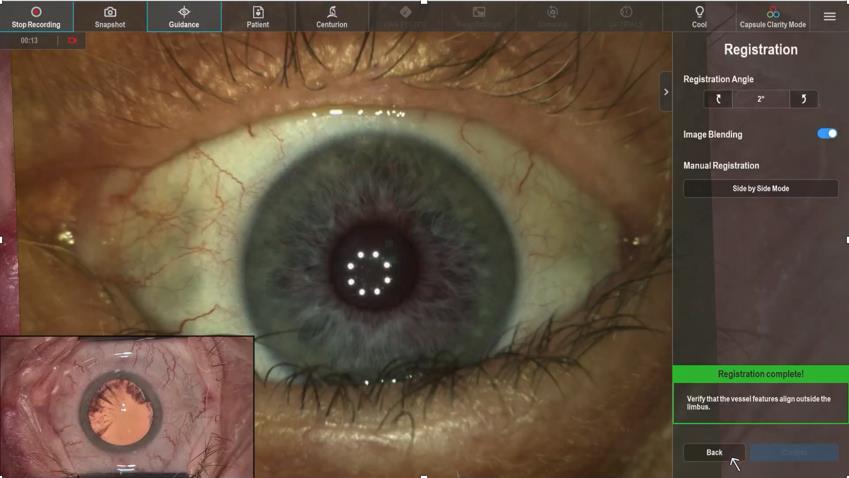
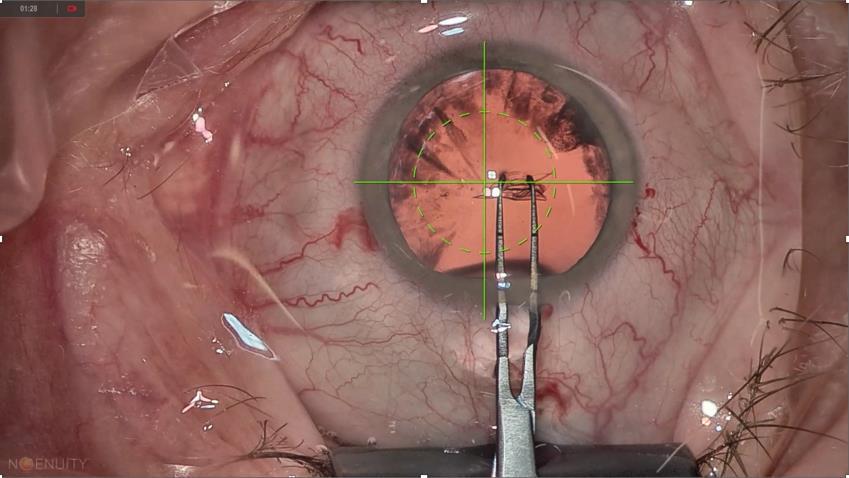
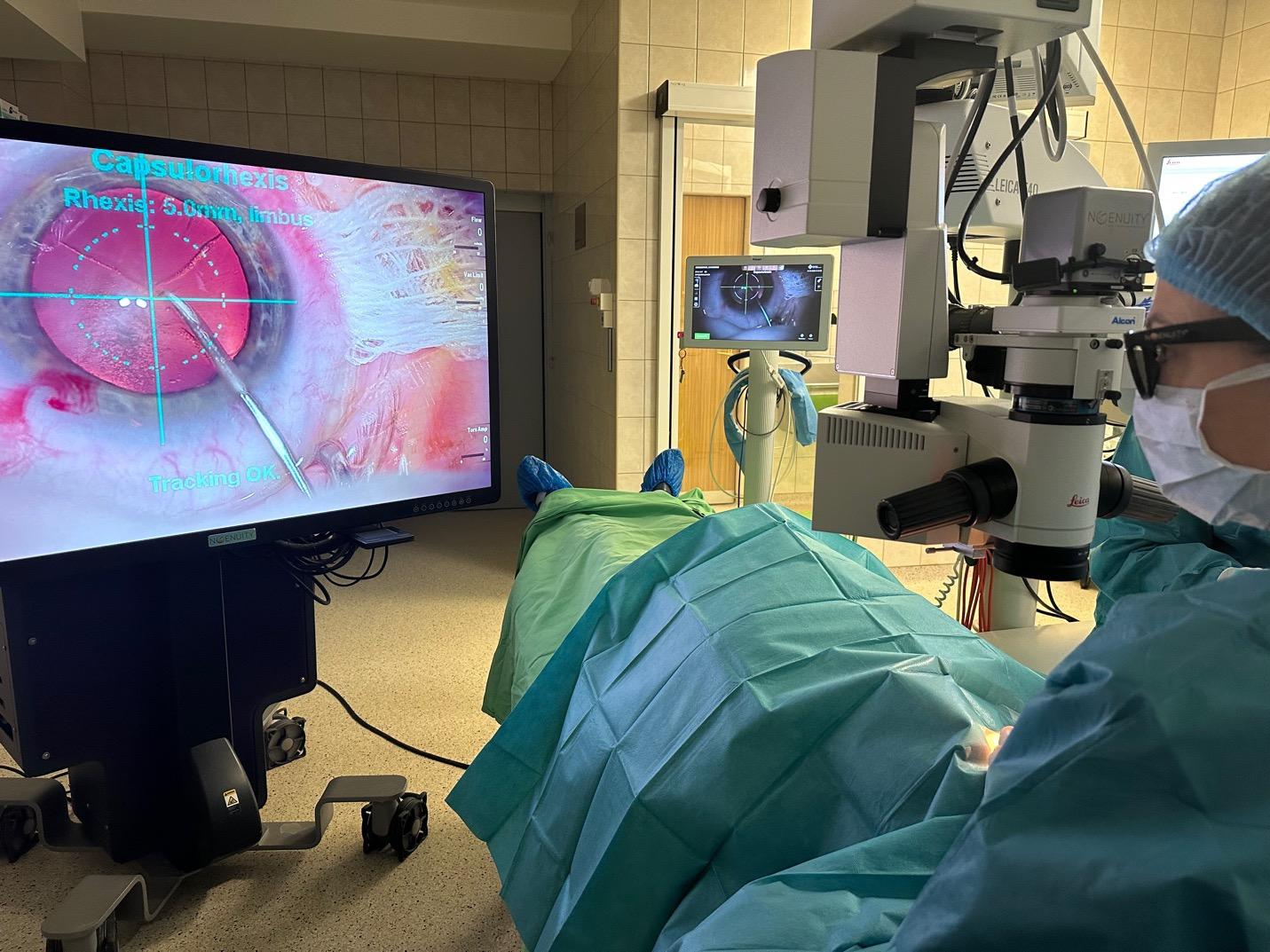
When choosing a 3D visualization system, several critical factors must be considered, including ergonomics, visual performance, surgical planning capabilities, ease of access, and cost. 3D visualization systems like the Zeiss Artevo, Alcon Ingenuity, and Heidelberg Engineering Seeluma deliver unparalleled depth and clarity, which are critical during surgery. These tools allow surgeons to observe fine details such as the depth of a crack made in the nucleus or the fine wrinkles on the posterior capsule. Overlays on the microscope help facilitate multiple steps in the procedure, including eye tracking, incisions, and capsulorhexis, a critical step in ensuring both efficacy and safety (Figure 1), thus enhancing surgeon confidence in performing these complex maneuvers.
Implementing a 3D visualization tool also benefits the surgeon and broader surgical team. The first major benefit is improved surgeon posture and ergonomics. Poor posture has

been shown to lead to musculoskeletal strain, potentially jeopardizing the length of a surgeon’s career.1-3 Digital visualization systems allow heads-up surgery, eliminating the need for traditional ocular microscopes and reducing physical strain. Secondly, visualization tools enhance the communication and collaboration of the OR team. Digital platforms enable everyone in the OR to see what the surgeon sees in real time. This transparency fosters a team environment where each member understands the surgical flow and can anticipate needs. When mistakes are avoided through clear communication, everyone benefits, especially the patient.
AI plays a critical role in linking preoperative biometry, surgical planning, and postoperative analysis (Figure 2). Automated calculations and data shared through the cloud facilitate more accurate planning, risk assessment, and outcomes optimization. Additionally, integrating AI and digital tools into the surgical workflow can reduce the carbon footprint by decreasing paper use and eliminating common errors such as typing mistakes during surgical planning. Further, having all preoperative information from one or several sources in one place simplifies surgical documentation and data analysis, making the entire process more seamless and effective.
Cataract surgery is well-suited to the digital and AI revolution. The integration of 3D visualization systems and AI-based workflows not only enhance safety and efficiency but also build a foundation for improved ergonomics and better team dynamics. While the benefits of digital technology in the OR are clear, challenges such as system compatibility and cost must be addressed before there is widespread adoption. The availability of more open-access systems that integrate with various microscopes and biometric tools should ease the transition to a digital OR setup, offer flexibility and help justify the financial investment. As these advancements are further explored, the potential for improved patient care through both immediate benefits and long-term impact is boundless.
Intraoperatively, real-time data analysis allows precise toric IOL alignment, and risk stratification features improve decision-making. Postoperatively, AI-powered analytics can be used to compare outcomes across datasets, support technique refinement, and help surgeons calculate their personal surgically induced astigmatism. Collectively, these innovations result in safer procedures and better outcomes for patients.

Kjell Gunnar Gundersen, MD, PhD, Private practice, iFocus Eyeclinic, Stavanger and Haugesund, Norway kg@ifocus.no
FINANCIAL DISCLOSURE:
Consultant (1stQ/Medicontur, Alcon, Haag Streit, Heidelberg, Glaukos, Santen); Shares (Eyecheck)
1. Kitzman AS, Fethke NB, Baratz KH, Zimmerman MB, Hackbarth DJ, Gehrs KM. A survey study of musculoskeletal disorders among eye care physicians compared with family medicine physicians. Ophthalmology 2012;119(2):213-220.
2. Dhimitri KC, McGwin Jr G, McNeal SF, et al. Symptoms of musculoskeletal disorders in ophthalmologists. Am J Ophthalmol 2005;139(1):179-181.
3. Masket S. Ergonomics is everything! American Academy of Ophthalmology. May 13, 2020. Accessed November 21, 2041. https://www.aao. org/senior-ophthalmologists/scope/article/ergonomics-is-everything
BY SUPRIYA SRIGANESH, MBBS, MS, FPRS(RGUHS)
Many surgeons, especially trainees, ask themselves how to refine their skills and improve efficiency while also shorten the learning curve. Whether it’s performing a faster capsulorhexis or mastering hydrodissection, thanks to digital operating room (OR) technologies, the answers are more accessible.
At a foundational level, surgeons tend to reproduce what they are taught. The review of surgical videos therefore is key for skill enhancement. Watching and analyzing procedures performed by experts alongside personal procedure videos helps identify subtle nuances and areas for improvement. Recording and reviewing surgical videos, however, can be cumbersome and inefficient. It requires a good microscope, a good recording system, a physical hard disk, hefty file transfers, and substantial time spent organizing and locating cases. Sometimes, the inconvenience of the process may translate to deprioritizing the analysis of surgical videos themselves.
Some of today’s digital visualization systems incorporate AI-powered applications that automatically upload recordings of surgical procedures to a cloud-based software, making them instantly accessible from a smartphone or laptop. This shift eliminates the barriers to reviewing videos, offering a level of support that accelerates skill acquisition and enables trainees to analyze their performance in high definition, anytime and anywhere.
AI-powered surgical video apps organize videos into distinct surgical phases (e.g., capsulorhexis, phacoemulsification, hydrodissection), allowing users to focus on specific steps of the procedure. Surgical techniques can be compared side-by-side with those of experienced surgeons, spotting inefficiencies and adopting best practices to streamline procedures and reduce surgical time (Figure 1).

To understand the broader impact of comparing videos on surgeon training, a study was conducted with six cataract fellows at Nethradhama Supercpeciality Eye Hospital in Bangalore, India. Three had access to an AI-powered app for surgical videos1 and three did not. Over 3 months, each fellow performed 30 surgeries. Improvements in total surgical duration, duration of individual surgical steps (i.e., corneal incisions, OVD injection, capsulorhexis, hydrodissection, phacoemulsification, irrigation/aspiration, IOL insertion, idle time, effective phacoemulsification time, and cumulative dissipated energy), and objective structured assessment of cataract surgical skill (OSCAR) scoring were assessed.2
The fellows who used the video app showed greater and quicker improvements to their total surgical duration, improved their OSCAR scores from 70 to 98 (Figure 2), and reduced their phaco time substantially. The fellows who did not use the software
scores improved more significantly for those who had ac-
to those who did not (B). [Courtesy of Dr Sriganesh]
saw less consistent improvement in the same parameters and had a higher average complication rate (15.6% vs 11.1%).3
Technologies like these also eased the burden on trainers, allowing them to focus on providing targeted guidance rather than rehashing basics repeatedly while accelerating skills development, reducing the risk for complications, and enhancing trainee confidence in the OR. For patients, the impact of incorporating surgical video reviews into training programs is profound. Shorter surgical times, consistent outcomes, and lower complication rates translate into better care and higher patient satisfaction.
Digital tools are reshaping ophthalmic surgical education and empowering trainees to become confident, skilled surgeons in less time.

Supriya Sriganesh, MBBS, MS, FPRS(RGUHS), Executive Director, Nethradhama Super Specialty Eye Hospital, India dr.supriyasriganesh@nethradhama.org
FINANCIAL DISCLOSURE: Consultant Zeiss
REFERENCES
1. ZEISS Surgery Optimizer. Accessed January 2, 2025. https://www. Zeiss.com/meditec/en/products/surgery-optimizer.html#benefit2
2. Bharucha KM, Adwe VG, Hegade AM, Deshpande RD, Deshpande MD, Kalyani VKS. Evaluation of skills transfer in short-term phacoemulsification surgery training program by International Council of Ophthalmology-Ophthalmology Surgical Competency Assessment Rubrics (ICO-OSCAR) and assessment of efficacy of ICO-OSCAR for objective evaluation of skills transfer. Indian J Ophthalmol. 2020;68(8):1573-1577. doi: 10.4103/ijo.IJO_2058_19. PMID: 32709779; PMCID: PMC7640864.
3. Umali MIN, Castillo TR. Operative time and complication rates of resident phacoemulsification surgeries in a national university hospital: a five-year review. Clin Ophthalmol. 2020;14:4065-4072. doi: 10.2147/OPTH. S283754. PMID: 33262571; PMCID: PMC7699982.
BY NORBERT PESZTENLEHRER, MD
Not only has digitalization in the operating room (OR) revolutionized surgical workflow and simplified preand postoperative case management, but it improves patient outcomes.
Transitioning from manual processes to digital tools may dramatically improve cataract surgery outcomes, especially with toric IOLs. In our practice mean residual astigmatism decreased from 0.41 to 0.26 D through the use of digital tools. By incorporating a modern IOL calculation formula (Barrett Universal II) and a 3D surgery system, mean residual
Postoperative residual astigmatism w/T-IOL implantation
Figure 1. Improvements in postoperative residual astigmatism after toric IOL implantation seen from 2013 with a manual marking system to 2021 with digital marking, modern IOL calculations, and sweptsource OCT. [Courtesy of Dr Pesztenlehrer] Abbreviations: T-IOL, toricl IOL; cyl, cylinder; subj., subjective; obj, objective
astigmatism further improved from 0.17 to 0.08 D. When switching to swept-source OCT biometry there were benefits to postoperative outcomes and refined results from 0.08 to about 0.07 D (Figure 1). However, these improvements are not just a testament to the technology but also to the dedication of a motivated and well-trained team.
To make the most of a digital OR, three main elements must be in place: a good leader, a plan, and command of the situation. Each element requires precise control, good staffing, organization, and coordination (Figure 2). When implemented successfully, a digital OR can enhance a practice’s performance and augment the patient experience.
Figure 2. Three elements for successful implementation of DOR technologies are a good leader, a plan, and command of the situation. Good staffing, organization, and precise coordination are further crucial components. [Courtesy of Dr Pesztenlehrer]
Adapting to the digital revolution requires managing a cultural shift within an ophthalmology practice. Baby boomers and early Gen X practitioners may be more hesitant to change whereas younger colleagues tend to embrace new technologies readily. The best chance for staff acceptance is for surgeons to embrace digitalization. Three helpful tips to bridge the gap are the following:
No. 1: Build confidence. Provide ample opportunities for hands-on training and emphasize the tangible benefits of digital tools, such as improved precision and reduced residual astigmatism.
No. 2: Offer positive reinforcement. Acknowledge progress and successes, no matter how small. Positive feedback, coaching, and consistent encouragement help nurture and maintain morale.
No. 3: Leverage peer insights. Encourage team members to share their positive experiences with digital technologies and solutions to common problems or bottlenecks in the practice. This fosters collaboration and demonstrates that change is manageable.
With the right strategies, a motivated team, and reliable partners, the transition to digital can be both smooth and rewarding.
Transitioning to a digital OR also involves rethinking workflows to integrate new tools such as advanced biometry devices, surgical planning software, digital markers, and 3D surgery systems seamlessly. The key is a methodical, step-bystep approach, implementing only one or two changes at a time and evaluating their impact before scaling. Collaborating closely with the manufacturer also can be beneficial to better understand how to integrate the system effectively into the existing OR setup.
Another pivotal tactic in ensuring the successful adoption of digital OR technologies is staff training. It’s not enough to install advanced equipment; a team must know how to use it
effectively. Structured learning via in-person and online training as well as reviewing case studies and real-life scenarios help highlight the practical benefits of new tools. Additionally, ongoing support through open lines of communication is key. A leader must be available to answer questions, troubleshoot issues, and provide technical guidance as needed.
Finally, processes should be analyzed regularly to further streamline workflows and promote continued optimization. Highlighting the improved patient outcomes associated with digital tools such as reduced postoperative residual astigmatism and enhanced visual quality may help motivate staff to embrace digitalization of the practice. Peer feedback and open discussions with colleagues often provide valuable insights.
The rise of digital tools in healthcare requires indorsing a good command of all aspects of implementation, including the adoption of new systems to safeguard patient data. Compliance with regulations like the EU’s General Data Protection Regulation is mandatory. The most important steps are to become familiar with both national and local privacy laws and to implement safeguards such as the use of secure networks and data encryption. Strict access controls must be established to minimize risks to the practice. Additionally, collaboration with manufacturers to ensure their software meets regulatory requirements may be necessary.
A digital OR is becoming essential for delivering the highest standard of care. Embracing its use, however, isn’t just about adopting the latest tools but rather rethinking how care is delivered. Digitalizing the OR requires fostering a culture of continuous improvement, prioritizing data security, and committing to excellence. With the right strategies, a motivated team, and reliable partners, the transition to digital can be both smooth and rewarding.

Norbert Pesztenlehrer, MD, Head, Petz County Hospital, Györ, Hungary pesztenlehrern@gmail.com
FINANCIAL DISCLOSURE: Consultant Alcon, Medicontur
BY KAREN GLANDORF, MD, FEBO, AND NORBERT PESZTENLEHRER, MD
The amount of information on the digitalization of operating rooms can be overwhelming. In this article, Drs. Glandorf and Pesztenlehrer take a deep dive on the topic and provide valuable insights into the nuances of a digital OR, exploring the problems it addresses, the steps for implementation, and the benefits it offers to a practice based on their personal experiences.
Dr. Glandorf’s digital OR setup begins with a preoperative assessment, where all examinations are centralized in a data
management system. She has experience with the EQ Workplace (Zeiss) for IOL calculations, where the data is seamlessly integrated with the Callisto eye system for computer-guided surgical assistance. During surgery, every procedure is recorded and uploaded to the Zeiss Surgery Optimizer for postoperative review (Figure 1).
Dr. Pesztenlehrer’s digital OR includes the Argos (Alcon), a network-linked swept-source OCT biometer
connected to multiple workstations across the department, allowing surgical planning from any location. Data is transferred to the OR, where Alcon SmartCataract DX and the Alcon Ngenuity 3D Visualization System enhance precision and ergonomics. Data is exported back to the biometer after surgery for further analysis, ensuring a smooth and integrated workflow (Figure 2).
A traditional cataract surgery workflow poses several challenges, especially for high-volume cataract surgeons. Preoperative assessments and surgical planning are time-consuming and can create bottlenecks. Additionally, managing paperwork such as preoperative measurements and surgical records introduces the risk of errors, which in the worst case can lead to incorrect lens implantation.
Markerless Toric IOL Alignment Software
Postoperative evaluations may also be delayed due to the extensive paperwork involved.
Dr. Glandorf highlights the limitations of intraoperative visualization in traditional workflows. Without digital systems, surgeons must mark the toric IOL axis on the patient’s cornea while they are upright and unsedated, disrupting the workflow. Further complicating matters, marking additional landmarks such as opposite clear corneal incisions can be impractical and overly complex during surgery.
Traditional microscopes, while providing adequate visualization, are not optimal for teaching or creating high-quality surgical videos. In contrast, digital microscopes with 4K capabilities enhance visualization, reduce the learning curve for residents, and give surgeons better control over their performance. Digital systems also enable real-time marking and data recording during surgery. For instance, toric IOL alignment is now measured within 1º of accuracy compared to 10º with manual marking.
Moreover, digital systems streamline workflows by seamlessly integrating patient data across devices and workstations. Patient data is transferred via a network directly to the OR, eliminating delays and enabling greater efficiency without disrupting routine activities.
Studies show that traditional workflows have reduced surgical and clinical efficiency.1,2 By comparison, digital workflows can be up to twice as fast, with an estimated cost reduction of about 35% per patient due to decreased staff and surgery-related expenses. While all diagnostics are carried out by just one employee, the lens calculation and planning of a workstation can already take place in the background. For patients, the streamlined and quicker process translates into an enhanced overall experience.
Dr. Glandorf stresses that efficiency of her practice has improved across all aspects of the workflow. Preoperative assessments, IOL calculations, and data export are now faster. In the OR, digital tools save up to 3 minutes per surgery, contributing to a noticeable faster and more efficient overall workflow. In addition to time savings, surgical precision has also benefited from computer-based axis marking. Studies show that IOL misalignment rates are significantly lower with digital systems.3
Dr. Pesztenlehrer highlights the significant benefits of a 3D visualization system, which enhances the surgeon’s focus, control, and accuracy. Advanced visualization tools such as 3D imaging make it much easier to assess and navigate complex anatomy during surgery. These tools provide a level of detail and clarity that’s hard to achieve with traditional methods, which ultimately makes procedures smoother and more efficient.
Patients experience more predictable results, especially with advanced procedures like toric IOL implantation. They are impressed by the advanced technology, which boosts their confidence in the quality of care. The improved predictability and precision of outcomes represent a clear advancement over manual approaches.
Furthermore, better efficiency in real-time data transfer and intraoperative digital marking reduces preoperative planning and surgery time and eliminates the risk for transcription errors. Integrating the system into the OR requires only minor adjustments, such as positioning a 3D surgical monitor near the operating table, but the benefits far outweigh this minor change.
According to Dr. Pesztenlehrer one of the most practical benefits is the integration of data from multiple devices into a single interface. Instead of switching between different machines or screens to access imaging or patient information, everything is consolidated. This saves time and puts the focus more on the procedure itself.
Overall, the workflow becomes smoother, more efficient, and less error-prone.
A digital workflow can improve ergonomics, data integration, and patient communication, highlights Dr. Glandorf. Dr. Pesztenlehrer has experienced spine and neck pain due to traditional microscopes and the transition to a 3D visualization system has allowed him to maintain a more ergonomic posture, reducing fatigue during long surgeries.
Digitizing informed consent forms and incorporating visual aids such as educational videos enhance patient education by making it more accessible and engaging. Dr. Pesztenlehrer notes that this transition has helped him be more transparent with patients, enabling clearer communication about superior outcomes and predictable results. Moreover, working with cutting-edge technology fosters a sense of pride and collaboration among the surgical team, as everyone can view and anticipate each surgical step in real time.
Automated data recording and analysis not only streamline workflows but also reduce energy consumption. Common frustrations are alleviated, as staff no longer need to print, scan, or manually file documents. This saves time
and minimizes errors, while digital workflows prevent issues like misfiled documents, allowing staff to focus on higher-priority tasks. Routine activities like documenting cases and preparing for surgeries become much more intuitive and efficient due to better systems integration. For example, data is automatically synchronized across devices, reducing the need for manual data transfers and minimizing stress. This automation allows the team to focus on patient care rather than administrative tasks.
Dr. Glandorf also highlights the benefit of easy access to
Traditional microscopes, while providing adequate visualization, are not optimal for teaching or creating high-quality surgical videos.
surgery recordings. For instance, after a complication like a posterior capsule rupture, reviewing the surgery recording helps to understand what went wrong, ensuring that mistakes are not repeated.
Infrastructure was the most significant challenge to Dr. Glandorf, particularly the lack of interoperability between certain devices. Although the digital OR is designed to support staff with minimal additional training, having an onsite IT specialist proved helpful for smooth integration. Costs vary depending on a clinic’s baseline setup, but the long-term benefits outweigh the initial investment.
For Dr. Pesztenlehrer, cost was less of a concern; instead, adapting to the new technology posed challenges, particularly for older generations of surgeons. Initial resistance is common among those accustomed to analog methods. However, attitudes shift as the tangible benefits, such as reduced physical strain and improved outcomes, become evident. The system’s intuitive design, combined with training, allowed even skeptics to feel comfortable using the new tools.
The digital OR is poised to become the standard in surgical practice. Its advanced efficiency and precision will likely render it indispensable, to the extent that future surgeons may not even remember a time when it wasn’t an integral part of their workflows.
As the digital OR continues to evolve, the integration of AI will play a pivotal role in enhancing decision-making, precision, and overall efficiency. Emerging technologies such as augmented reality (AR) and advanced imaging are set to further expand its capabilities, paving the way for safer and more effective surgical procedures.
AI holds tremendous promise for transforming the digital OR, revolutionizing processes across preoperative planning, intraoperative decision-making, and postoperative evaluation.
Its capabilities can enhance critical functions such as IOL calculations, patient data analysis, and surgical performance assessments. For example, AI could generate surgeon-specific nomograms to tailor and optimize outcomes for individual patients. However, while AI can provide invaluable support, surgeons ultimately bear the responsibility for the results, making it essential to rigorously verify AI-generat ed calculations and recommendations.
Moreover, AI can potentially analyze intraoperative data in real time, offering techniques suggestions or issuing alerts about potential complications before they arise. This capability represents a future we’re heading toward.
Despite its vast potential, the integration of AI into the digital OR is not without challenges. Data security is a primary concern, as AI systems rely on vast amounts of sensitive patient information. Safeguarding this data and ensuring ethical usage will be crucial. Additionally, there is the risk of over-reliance on AI. While these systems can enhance decision-making, they should complement not replace, the expertise and judgement of surgeons. Striking the right balance between technological assistance and human oversight will be key to successfully integrating AI into the future of surgical practice.
Other emerging technologies
Improved interconnectivity between devices and clinic software is becoming increasingly critical. Future advancements may include AI systems that not only analyze patient outcomes but also monitor clinic workflows, identifying inefficiencies or errors.
it’s a pathway to elevating both surgical practice and patient care.

Karen Glandorf, MD, FEBO Augentagesklinik Precise Vision, Rheine, Germany k.glandorf@precise.vision
FINANCIAL DISCLOSURE:
Head, Petz County Hospital, Györ, Hungary pesztenlehrern@gmail.com

FINANCIAL DISCLOSURE: Consultant Alcon, Medicontur
Instead of switching between different machines or screens to access imaging or patient information, everything is consolidated.
We are at an exciting juncture where a host of technologies has the potential to further revolutionize the digital OR. Intraoperative OCT and advanced imaging modalities are being increasingly integrated into surgical workflows, allowing surgeons to adjust their techniques mid-procedure based on real-time data. Additionally, AR and virtual reality hold enormous promise, not only for training but also for real-time surgical guidance. Imagine AR overlaying critical anatomical landmarks directly onto the surgical field, enhancing precision and significantly improving outcomes.
Advanced robotics is another area to watch closely. While robotic systems are already being used across various specialties, their applications in ophthalmology are becoming more refined. These systems promise greater accuracy, dexterity, and control in performing delicate procedures, making them invaluable in precision-driven fields like ophthalmology.
Finally, the role of telemedicine and remote collaboration tools is expanding. In a seamlessly connected digital ecosystem, surgeons and experts from across the globe could collaborate in real time on complex cases, exchanging insights and collectively enhancing patient care.
For surgeons hesitant about adopting a digital OR, one practical step is to visit a clinic that has already implemented one and compare workflows. Traditional workflows may still suffice for those primarily using monofocal IOLs, but high-volume practices performing premium surgeries will find digital tools indispensable for staying competitive and efficient.
Embracing the digital OR is a step toward transformative change. While there may be an initial learning curve, the long-term advantages—such as improved patient outcomes, reduced physical strain on surgeons, and enhanced workflow efficiency—far outweigh the costs and challenges. The digital OR is not just a tool;
1. Rombold F, Niederdellmann C, Pariti R, Kyayat B. Time savings using a digital workflow versus a conventional for intraocular lens implantation in a corporate chain hospital setting. Clin Ophthalmol. 2024;18:113-119.
2. Shetty N, Saxena A, Singh VM, Fernandes M, Garg P, Venkiteshwar M. Effect of digital cataract workflow on time and resource efficiencies in cataract surgery: time and motion study. J Cataract Refract Surg. 2024;50(12):1208-1214.
3. Elhofi AH, Helaly HA. Comparison between digital and manual marking for toric intraocular lenses: a randomized trial. Medicine (Baltimore). 2015;94(38):e1618.
