ALSO IN THIS ISSUE
Spoiled for Choice?
Surgeon-patient communication could be key to increasing presbyopic IOL uptake.

New Phaco Alternative Debuts in US
Back to the future with nonultrasonic cataract extractor?

ALSO IN THIS ISSUE
Spoiled for Choice?
Surgeon-patient communication could be key to increasing presbyopic IOL uptake.

New Phaco Alternative Debuts in US
Back to the future with nonultrasonic cataract extractor?
EPICAT study continues tradition of practice-changing clinical studies.
Battling Bias in Science Developing a treatment plan for a chronic condition starts with team building.
With awareness around the environmental impact of ophthalmic procedures ever-growing, it’s becoming more important to consider all the options for reducing waste during surgery.
Enter Sophi: the phaco machine designed with sustainability at its core.
Traditional phacoemulsification machines featuring single-use cassettes leave behind piles of plastic packaging, meaning a full day of surgeries can produce a staggering amount of waste. With Sophi, single-use cassettes have been replaced with “day-pack” alternatives, drastically reducing waste and material use.
• Multi-use day pack cassette: Use for up to 10 procedures to reduce waste and material use.1
• Packaging reduction: Sophi is 19% lighter on single use pouch packaging than conventional alternatives.1
• Less plastic use: Sophi uses 75% less plastic than traditional phacoemulsification machines.1
Sophi is easy, clear and quick to operate, with fast system start-up and easy customisation to individual preferences and needs.
Sophi enables the surgical team to focus entirely on the patient, with modern assistance systems and clever control elements creating a simple surgery process. It assists theatre staff with intelligent sensor technology, and automatically makes adjustments in critical settings.
Sophi focuses on safety –without compromise. From reducing risk of crosscontamination with its automatic Cassette Slot-In System to the intelligent handpiece controlled with a sinusoidal signal to protect the eye, Sophi has an integrated safety system that provides high standards of process stability, precision and hygiene.

With the participation of the Hellenic Society of Intraocular Implant and Refractive Surgery



ESCRS Research Projects Make a Difference EPICAT study continues tradition of practice-changing clinical studies.

20 Overcoming Barriers to Presbyopic IOL Uptake
Arthur B Cummings MMed(Ophth), FCS(SA), FRCS(Edin); Basak Bostanci MD, FEBO; Terry Kim MD; Tanja Cotoaga; Tim Clover; and Yehia Hashad MD
ESCRS Update: ESCRS Officers Set for 2025; ESCRS Accepting Applications for Peter Barry Fellowship; Schedule Set for 2025 FEBOS-CR Exam; Posters Available to Inform Patients
Supriya Samak Sriganesh MBBS,
Tablao Debates:
Francesco Carones MD; Damien Gatinel MD, PhD; Basak Bostanci MD, FEBO; and Margarita Cabanás MD
22 Phaco Alternative Debuts in US
Sonia H Yoo MD; Richard B Packard MD, FRCS, FRCOphth; and Frank Seitzinger
24 Setting Limits for PRK and LASIK
Robert Edward T Ang MD
26 Treating Myopia, Inside and Outside
Ken K Nischal MD, FAAP, FRCOphth; Erin Tomiyama OD, PhD, FAAO; Dominique Bremond-Gignac MD, PhD, FEBO; and Ramesh Kekunnaya MD, FRCS
28 FIREFLEYE Next Study Updates
Andreas Stahl MD CORNEA
30 Cataract Surgery in Eyes with Corneal Disease
Damien Gatinel MD, PhD
31 Visual Rehabilitation for Keratoconus
Paolo Vinciguerra MD
32 Corneal Cross-Linking (CXL): Leaving the Epithelium On Farhad Hafezi MD, PhD, FARVO; Mark Hillen PhD; and Emilio Torres-Netto MD, PhD, FWCRS
34 Discovering Prodygy and Nirvana
Daniel C Chung DO, MA
35 Effect of COVID-19 and Vaccine on Retinal Disease
Rahul N Khurana MD
36 The Promises and Pitfalls of AI
Rebecca Berghorn and Dalith Steiger
38 Real-World Strategies for New Tech Adoption
Norbert Pesztenlehrer MD
OCULAR UPDATE
40 Battling Bias in Science
Sotiria Palioura MD, MSc, PhD

Publisher
Filomena Ribeiro
Executive Editor
Stuart Hales
Editor-In-Chief
Sean Henahan
Senior Content Editor
Kelsey Ingram
Creative Director
Kelsy McCarthy
Graphic Designer
Jennifer Lacey
Circulation Manager
Lucy Matthews

Contributing Editors





Cheryl Guttman Krader
Howard Larkin
Roibeárd O’hÉineacháin
Contributors
Laura Gaspari
Soosan Jacob
Timothy Norris
Colour and Print CitiPost
Advertising Sales
Roo Khan
MCI UK
Tel: +44 203 530 0100 | roo.khan@wearemci.com
EuroTimes® is registered with the European Union Intellectual Property Office and the US Patent and Trademark Office.
Published by the European Society of Cataract and Refractive Surgeons, Runway East Borough Market, 20 St. Thomas Street, London, SE1 9RS, UK. No part of this publication may be reproduced without the permission of the executive editor. Letters to the editor and other unsolicited contributions are assumed intended for this publication and are subject to editorial review and acceptance.
ESCRS EuroTimes is not responsible for statements made by any contributor. These contributions are presented for review and comment and not as a statement on the standard of care. Although all advertising material is expected to conform to ethical medical standards, acceptance does not imply endorsement by ESCRS EuroTimes. ISSN 1393-8983


Throughout 2024, the 75th anniversary of the first IOL implantation was observed around the ophthalmology world, starting in Frankfurt at the ESCRS Winter Meeting, then at the ESCRS Congress, and finally at the United Kingdom and Ireland Society of Cataract and Refractive Surgeons annual congress in London. EuroTimes articles reviewing the historical record showed Ridley’s inspired and brilliant innovation would not have passed muster with today’s IRBs. Indeed, it remained for subsequent researchers to develop his ideas and subject them to rigorous clinical studies to get where we are today.
Cataract surgery, already considered one of the safest of all procedures, continues to show improvement in outcomes, largely thanks to ongoing clinical research, of which ESCRS research projects have played no small part. This is particularly true when it comes to reducing serious procedure-related adverse effects.
In this issue, we present a detailed update on the ongoing European multicentre trial Effectiveness of Periocular Drug Injection in CATaract Surgery (EPICAT) study conducted by Dutch colleagues Rudy MMA Nuijts and Nienke Visser. This ESCRS-sponsored study addresses the persistent problem of postoperative cystoid macular oedema. The randomised clinical trial compares three dropless strategies, with early results indicating subconjunctival triamcinolone appears most effective in preventing CME.
We also review other landmark clinical studies conducted under the auspices of the ESCRS, including the ESCRS Endophthalmitis study, led by the great Irish surgeon Peter
EDITORIAL BOARD

Adi Abulafia (Israel)
Bruce Allan (UK)
Noel Alpins (Australia)
Juan Alvarez de Toledo (Spain)
Gerd Auffarth (Germany)
Başak Bostanci (Turkey)
John Chang (Hong Kong SAR, China)
Béatrice Cochener-Lamard (France)
Burkhard Dick (Germany)
Mor Dickman (The Netherlands)

Joaquín Fernández (Spain)
Oliver Findl (Austria)
Nicole Fram (US)
Sri Ganesh (India)
Fahrad Hafezi (Switzerland)
Nino Hirnschall (Austria)
Soosan Jacob (India)
Jack Kane (Australia)
Yao Ke (China)
Mika Kotimäki (Finland)
Barry, the PREMED (PREvention of cystoid Macular Edema after cataract surgery) study conducted by Rudy Nuijts, and the ongoing MYOPRED study led by Oliver Findl.
All the studies underscore the importance of properly designed randomised clinical trials to provide a foundation for evidence-based treatments. This requires large numbers of patients and long-term, rigorous statistical management of protocols. These studies also help evaluate the best allocation of resources during a time of ever-increasing demand. The ESCRS has the reach to accomplish these goals, with many new research protocols on the drawing board and entering the clinic. To learn more, please visit https://www.escrs.org/research/.
Joaquín Fernández MD, MSc, PhD Chairman of ESCRS Research Committee 2024 Secretary of the ESCRS 2025
For the past two decades, EuroTimes has published 10 issues per year, doubling up in the summer and at year-end. The ESCRS board has decided to revise the printing schedule to 6 bimonthly issues.There will also be 4 online-only issues published quarterly. We will continue to provide EuroTimes as a free benefit to ESCRS members. The changes will coincide with an expanded online presence offering additional news and educational opportunities via our website and enhanced social media.
Sean Henahan
Editor-in-Chef, EuroTimes

David Lockington (UK)
Artemis Matsou (Greece)
Cyrus Mehta (India)
Jod Mehta (Singapore)
Sorcha Ní Dhubhghaill (Belgium)
Rudy Nuijts (The Netherlands)
Catarina Pedrosa (Portugal)
Konrad Pesudovs (Australia)
Nic Reus (The Netherlands)
Filomena Ribeiro (Portugal)
Andreia Rosa (Portugal)
Giacomo Savini (Italy)
Julie Schallhorn (US)
Sathish Srinivasan (UK)
Paola Vinciguerra (Italy)
Shin Yamane (Japan)
Ron Yeoh (Singapore)
Mihail Zemba (Romania)
Iwas very sorry to hear of the passing of Howard Fine, a mentor and dear friend of mine.
I first met Dr Fine when I walked into his office in Eugene, Oregon, in the spring of 2001. I’d read his work and seen his pioneering videos of power modulation and clear corneal cataract surgery. I was pleasantly surprised by the ever-smiling gentleman—obviously a leader among men, loved by his doctors, staff, and patients.
In the mornings, I witnessed outstanding surgery on hard cataracts, small pupils, subluxed lenses, and other tough cases referred to him from across the continental US and abroad.
Late afternoons were for riding. I’d heard of his Harley motorcycle collection. When he heard I was also a biker, we went to the basement, where I first saw part of his gleaming bike collection.
“You must have ridden one before,” he said. I replied yes, although the only bike I had ridden was a small 100 cc Yamaha. “Let’s go,” he said at four in the afternoon when the centre closed. During the three months I learnt ophthalmology from him, we must’ve taken more than 50 rides in the Oregon countryside.
Three months passed by in a flash. I left armed with my ASCRS fellowship. He was the ASCRS president then. After I returned to India, I met him several times at ESCRS and ASCRS, where he always consented to speak at my courses and his favourite IIIC meeting. He won every award they had to give and then some. I was honoured he agreed to come to India and speak at my EyeAdvance meeting, where it was our privilege to present him with our highest honour.
Behind his chair was a plaque with a quote from JM Barrie: “You canna expect to be baith grand and comfortable.”
My condolences to Vicky, Edward, and Bill.
We will meet again Dr Fine, probably on electric bikes though.

protocols. These studies also help evaluate the best allocation of
For the past two decades, EuroTimes has published 10 issues per year, doubling up in the summer and at year-end. The ESCRS board has decided to revise the printing schedule to 6 bimonthly issues.There will also be 4 online-only issues published quarterly. We will continue to provide EuroTimes as a free benefit to ESCRS members. The changes will coincide with an expanded online presence offering additional news and educational opportunities via our website and enhanced social media.
Sean Henahan Editor-in-Chef, EuroTimes
ESCRS’s vision is to educate and help our peers excel in our field. Together, we are driving the field of ophthalmology forward.

As ESCRS begins 2025, three members are assuming new roles on the Council of Management.
Burkhard Dick, who served as secretary in 2024, is now the president-elect and will become president in January 2026. His replacement as secretary is Joaquín Fernández
Pavel Stodůlka is the new treasurer of ESCRS, replacing Thomas Kohnen, who served in this position in 2024.
Filomena Ribeiro remains as president of ESCRS in 2025, serving the second year of her term.
Scan the QR code to view the complete roster of the Council of Management.
Applications are now open for the 2025 Peter Barry Fellowship, which honours the immense contributions to ophthalmology and ESCRS by the late Peter Barry.
The Fellowship includes a stipend of €60,000 to allow a trainee to work abroad at a centre of excellence for clinical experience or research in the field of cataract and refractive surgery, anywhere in the world, for one year. Applicants must be a European trainee ophthalmologist, 40 years of age or younger on the closing
date for applications (2 March 2025), and an ESCRS member by the time of starting the Fellowship.
Eligible applications will be evaluated by an expert panel against the proposed research importance assessment criteria. Selected applicants will then be invited for an interview with the ESCRS Peter Barry Fellowship Committee.
The Fellowship recipient will be announced at the 2025 ESCRS Annual Congress, with the Fellowship starting the following year.
Scan the QR code to view the Peter Berry Fellowship application.
ESCRS will begin accepting applications on 10 January 2025 for the FEBOS-CR exam, which certifies expertise and advanced knowledge in the fields of cataract and refractive surgery.
ESCRS, in collaboration with the European Board of Ophthalmology (EBO), organises the FEBOS-CR exam to formally recognise subspecialty training and expertise in these fields. By developing exam criteria and standards, ESCRS and the EBO harmonise and improve training across Europe and define the expected level of knowledge and skills a subspecialist should acquire
to solve complex, difficult cases. Successful candidates earn the right to use the FEBOS-CR credential to show they—
• hold a superior theoretical and practical knowledge;
• can deal with more challenging cases and a complex case mix;
• appreciate the importance of evidence-based medicine and its purpose in developing scientific knowledge and clinical practice of the subspecialty; and
• are, or have the ambition to become, trainers and leaders in the cataract and refractive surgery subspecialty.
FEBOS-CR candidates must be independent surgeons with a varied case mix who regularly deal with complex situations. They must also be willing to have their expertise and theoretical knowledge tested by a rigorous theoretical examination and interviews with some of the top opinion leaders in European and worldwide ophthalmology.
Scan the QR code to view the FEBOS-CR exam application.
The ESCRS Annual Congress in Barcelona hosted not only the 2024 FEBOS-CR exam but also the inaugural meeting of exam alumni, bringing together members who have demonstrated exceptional expertise by successfully passing the exam over the past five years.
The gathering celebrated the collective achievements of the alumni, welcomed the successful 2024 exam candidates, and explored ways to leverage the alumni network to enhance career opportunities and professional access. The meeting included talks from Prof Burkhard Dick, Ben La Hood, Kris Morrill, and Prof Sorcha Ní Dhubhghaill and fostered a collaborative spirit, empowering members to advance their skills.
“We view the exam not only as a hallmark of quality and expertise in cataract and refractive surgery but as an accreditation that keeps on giving,” said Prof Ní Dhubhghaill, Chair and Head

Tof the Department of Ophthalmology at University Hospital Brussels/Vrije Universiteit Brussels, Belgium. “We see the FEBOS-CR as a stepping stone to growing within the ESCRS, opening new doors to collaboration on projects and courses for future ESCRS meetings. We have already promoted our alumni in the society—together we have submitted ICC courses to the summer meetings, participated in the international ESCRS academies, and more.”
The group hopes to carve a path for FEBOS alumni to reach greater heights within ESCRS and be of service both to their patients and to society.
The European Society of Cataract and Refractive Surgeons (ESCRS) Patient Portal is designed to guide you through every step.
• Understanding your options and potential procedures.
• The benefits and risks of surgery.
• Aftercare instructions for a smooth recovery. It’s the place to go for extensive information about cataract and refractive surgery.
Available to Inform Patients about Eye Surgery
ESCRS has created posters that ophthalmologists can display in their clinic to inform patients about the conditions related to their upcoming or recent cataract or refractive surgery.
The posters are available in both landscape and portrait formats and can be displayed as printed posters or as slides on a screen. The posters contain QR codes that link to the ESCRS Patient Portal, which is housed on the ESCRS website.
Scan the QR code to learn more!
ESCRS is the principle professional association for cataract and refractive surgeons in Europe
he next issue of the Video Journal of Cataract, Refractive, & Glaucoma Surgery is out! What better way to celebrate the 40th anniversary than to publish highlights of the ESCRS Congress in Barcelona? The issue features 27 topics presented by a multinational faculty of surgeons from 14 countries. Categories include preoperative challenges, intraoperative complications, and postoperative situations.
Founded by Robert Osher MD in the US, the VJCRGS was the first video journal in medicine, established in the day of videotape, before the internet existed. Each quarterly issue offers at least an hour of the highest quality education for the anterior segment surgeon. The journal is free to all practising ophthalmologists and teaching institutions.
The Patient Portal is split into two sections: Cataract and Refractive. Each section offers an easy-to-understand summary of the condition, including the benefits, risks, procedures, and aftercare of common conditions. Clear diagrams and a glossary of terms help convey all the information patients might need to help prepare for surgery or during their aftercare.

40 Year Anniversary Highlights of the ESCRS A Treasure Chest of Surgical Pearls Volume 40, Issue 3, 2024
PREOPERATIVE CHALLENGES
Posterior Polar Cataract ............................................................. Dr. Rohit Om Parkash, India
Nanophthalmos .......................................................................... Dr. Evripidis Sykakis, Greece
Caution: Retinal Detachment ...................................................... Dr. Hazem El-Nashar, Egypt
Small Uveitic Pupil ......................................................................... Dr. Lee Mun Wai, Malaysia
Iris Atrophy .......................................................................................... Dr. Ashraf Armia, Egypt
Traumatic Mydriasis .............. Drs. Maria Jesus Quiroz-Quiroga, Jorge Armentia Perez de Mendiola, Ester Puig Lao, Pablo Marti Rodrigo, Ana Matheu Fabra, Anna Baldaqui Baeza, & Joao Correia Fernandez, Spain
Aniridia with astigmatism ................................................................. Dr. Altan Ozcan, Türkiye
Traumatic Iris/Lens Loss ................... Drs. Tomas Jaeschke & Florencia Bellani, Argentina
Subcapsular Fibrosis..................................................... Drs. Carolina Larco, Pablo Larco Jr., & Pablo Larco, Ecuador
Silicone Oil with Plaque................................................................. Dr. Alokesh Gangoly, India
Ectopia Lentis .................................................................................... Dr. Ahmed Assaf, Egypt
Microspherophakia ....................................................................... Dr. Ramon Ghanem, Brazil
Traumatic Zonulopathy ....................................................................Dr. Debashis Dutta, India
INTRAOPERATIVE COMPLICATIONS
Argentinian Flag................................................................... Dr. Hassan Khaled, Saudi Arabia
FLACS ................................................................................................ Dr. Anagha Heroor, India
Posterior Capsule Puncture .................................................... Dr. Tushya Om Parkash, India
Nucleus Loss ....................................................................................... Dr. Mrinmoy Das, India
Zonular Dialysis .................................................................................. Dr. Gaurav Luthra, India
Capsular Delivery ..................................................................... Dr. Ran Matlov Kormas, Israel
Descemet Detachment ...........................................................Dr. Suven Bhattacharjee, India
POSTOPERATIVE SITUATIONS
Aphakia after Congenital Cataract ............................ Drs. Meriem Ouederni, Zaineb Gharbi, & Monia Cheour, Tunisia
Pseudophakic Bullous Keratopathy .......................... Drs. Nir Stanescu & Fani Segev, Israel
Polypharmacy Psychosis............................................... Dr. Lional Raj Daniel Ponniah, India
Capsular Phimosis .......................................................................... Dr. Hatem Ammar, Egypt
Decentered/Rotated Toric IOL............................................Dr. Jiri Cendelin, Czech Republic
Opacified IOL .............................................. Drs. Monia Cheour & Meriem Ouederni, Tunisia
Dislocated Iris Prosthesis ......................... Drs. Walter Sekundo & Volker Besgen, Germany

EPICAT study continues tradition of practice-changing clinical studies.
BY TIMOTHY NORRIS


Adropless strategy with a subconjunctival 10 mg triamcinolone injection is very likely to become a standard procedure for the prevention of cystoid macular oedema (CME) after cataract surgery, with the potential to improve patient outcomes and save millions of euros in healthcare costs, as shown by preliminary results of a European multicentre randomised trial.
CME is a major cause of visual acuity loss following uncomplicated cataract surgery, occurring in about 5% of patients even without risk-increasing comorbidities such as diabetes. Anti-inflammatory eye drops are the current postoperative treatment to prevent CME after cataract surgery. However, low adherence to treatment due to a lack of compliance or difficulty in self-administration may seriously reduce the effectiveness of prevention while increasing the risk of developing this complication. Also, because many patients have difficulty with self-instillation of eye drops, formal or informal care is often required.
“We know from previous studies that many patients have difficulties with the self-instillation of eye drops. These patients often need informal home care, like family members or neighbours, to help them administer the eye drops,” said lead investigator Nienke Visser MD, PhD, adding that in countries with formal home care like the Netherlands, 8 to 10% of patients currently rely on this kind of assistance after cataract surgery.
Started in 2021, the Effectiveness of Periocular Drug Injection in CATaract Surgery (EPICAT) study aimed at finding a dropless strategy for CME prevention after cataract surgery, using either intra- or periocular injections, as compared to topical drugs as the control group.
The EPICAT study evaluates three dropless strategies for CME prevention in routine cataract surgery. Main exclusion criteria were an increased risk of developing CME (e.g., diabetes), an increased risk of perioperative complications, and a history of steroid response or glaucoma. The first intervention group received a 10 mg subconjunctival injection of triamcinolone, the second intervention group received ketorolac (OMIDRIA®) during surgery, and the third intervention group received a combination of the two during cataract surgery. Patients in the control group were treated with topical dexamethasone and bromfenac, which continued in a tapering scheme for four weeks postoperatively. In the primary results, the 10 mg triamcinolone subconjunctival injection was shown as effective as topical therapy in preventing CME after cataract surgery.
“This dropless strategy is a simple step to add to an already highly optimised cataract procedure: in the EPICAT study, we used a posterior subconjunctival injection 6.0 mm from the limbus in the inferotemporal quadrant of the conjunctiva to administer 0.25 mL of a 40 mg/mL triamcinolone solution,” Dr Visser explained. “We expect this to be a game changer that only takes one minute out of the surgical time, with the added benefit of relieving patients of postoperative eye drops.”
Final EPICAT study results are expected to be taken into serious consideration by ESCRS and will surely be integrated into the upcoming cataract surgery guidelines.
“This study is pivotal for the ESCRS because it addresses one of the most pressing challenges in cataract surgery,” said Joaquin Fernández MD, PhD. “Its results already have several important implications for both patients and the field of ophthalmology.”
ESCRS became involved in the EPICAT study through its Clinical Research Award (CRA), a key Society initiative to support multinational interventional studies with a focus on cataract surgery. ESCRS awarded the EPICAT team €749,707 and started to work closely with the team to oversee the project’s progression. This included monitoring key milestones, approving protocol amendments, and ensuring the study remained on budget and met its objectives, Professor Fernández pointed out.
“It has been a challenge to complete this study during the COVID pandemic with all the issues related to patient inclusion and drug procurement. We were hesitant if this was going to happen,” co-investigator Rudy MMA Nuijts MD, PhD told EuroTimes. “Now, it is important to see how these results will get implemented into daily practice.”
Preliminary results were presented at the 2024 ESCRS Congress in Barcelona. According to Prof Fernández, the trial has the potential to transform cataract surgery, particularly in how postoperative inflammation and complications like CME are managed.
In Europe, its findings provide a strong case for adopting a streamlined, dropless approach to cataract surgery. Since it is a cost-effective, minimally invasive protocol that benefits both high- and low-resource settings, this strategy aligns with the global healthcare goals of improving outcomes while controlling costs. It establishes a new benchmark for postoperative inflammation management, impacting millions of patients worldwide.
Building on this progress, the team hope to deliver the final results to the ESCRS by the end of 2025. Simultaneously, the first article based on these findings is expected to be submitted for publication very soon, Prof Fernández noted.
Moreover, further publications are planned, including a detailed analysis of the health economics associated with the EPICAT study. The next step is to dive into the procedure’s cost-effectiveness and the vision-related quality-of-life gains. This is part of the EPICAT team’s comprehensive approach to ensure the findings are robust, actionable, and beneficial for the broader ophthalmic community.
The results of EPICAT are not only promising for CME prevention. According to both Dr Visser and Prof Fernández, there is a vast potential for applications in complicated cases, even outside cataract surgery. As the PREvention of Macular EDema after cataract surgery (PREMED) study published by Laura Wilders MD, PhD and Prof Nuijts showed, a subconjunctival injection of a higher 40 mg triamcinolone dose was effective in preventing CME in patients with diabetic retinopathy.
“After the PREMED study, we had a long deliberation process to see which dose we would use to prevent a pressure spike due to steroids, ending up with the 10 mg dose,” Prof Nuijts added.
Dr Visser and Prof Nuijts noted the PREMED and EPICAT findings could hint at a good rationale in considering further studies for the use of triamcinolone in other surgical fields that involve postoperative inflammation and are therefore prone to CME (especially retinal surgery) and in patients with epiretinal membranes, BRVO, uveitis, and diabetes. Proactively addressing inflammation, as demonstrated by the EPICAT study, could inspire similar dropless strategies to avoid complications and enhance patient outcomes.
ESCRS’s commitment to advancing evidence-based medicine and research through various awards programmes effectively encourages an exciting pipeline of ongoing and upcoming studies.
There are currently two active CRA-funded trials and three nearing completion, including high-profile projects like ETCF, which compares the outcomes of triple-DMEK with cataract surgery in patients with Fuchs’ endothelial corneal dystrophy; METACOR-2, which aims to model the corneal microbiome to better identify pathogenic microorganisms; MYOPRED, which investigates the impact of posterior vitreous detachment on RD after lens surgery in myopic eyes; and finally TORIC, which evaluates the effectiveness and cost-effectiveness of toric IOL implantation in patients with mild astigmatism.
Prof Fernández said the ESCRS is actively working to expand its research initiatives, with plans to announce a new clinical research award in 2025. “It’s a way to look ahead and further strengthen our ability to fund innovative and high-impact studies.”
Nienke Visser MD, PhD is the EPICAT lead investigator and medical specialist at Maastricht UMC+, Netherlands. nienke.visser@mumc.nl
Rudy MMA Nuijts MD, PhD is Full Professor of Ophthalmology and Director of the Cornea Clinic and the Centre for Refractive Surgery at the Department of Ophthalmology, University of Maastricht, Netherlands. rudy.nuijts@mumc.nl
Joaquín Fernández Pérez MD, PhD is the CEO and Medical Director in the Ophthalmology Department at Qvisión in Vithas Virgen del Mar Hospital, Almería, Spain. He is incoming Secretary of the ESCRS and outgoing leader of the ESCRS Research Committee. joaquinfernandezoft@qvision.es
Studies aim to benchmark best practices, improve surgical outcomes.
Major research projects undertaken by the ESCRS have made significant contributions to everyday medical practice in the field of ophthalmology, and new projects underway will continue to do so.
Endophthalmitis is still the most feared complication of cataract surgery. Based on earlier studies conducted in Sweden, the landmark ESCRS Endophthalmitis study sought to determine whether intracameral antibiotic prophylaxis could reduce the risk of this complication.1
Led by Irish ophthalmologist Peter Barry MD, the prospective, randomised, partially masked multicentre cataract surgery study recruited 16,603 patients from centres in Austria, Belgium, Germany, Italy, Poland, Portugal, Spain, Turkey, and the United Kingdom.
The study showed prophylactic intracameral cefuroxime did significantly reduce the risk of postoperative endophthalmitis. Since the study results were announced in 2007, intracameral antibiotic administration has become a standard practice in many parts of the world, particularly in Europe and the United States.
Intracameral cefuroxime acceptance was initially stymied by the lack of an approved, licensed, commercially available product. This changed with the European Medicines Agency’s approval of Aprokam (Thea), a single-dose preparation developed specifically for this purpose. A single 50 mg cefuroxime powder is mixed with a single dilution of 5.0 mL normal saline.
The PREvention of Macular EDema after cataract surgery (PREMED) study is another example of ESCRS-sponsored research that had a significant impact on ophthalmology practice.2 PREMED sought to identify the best method for preventing cystoid macular oedema (CME) following cataract surgery.
The randomised clinical trial enrolled 914 non-diabetic cataract patients from 12 European clinical centres. Patients received either topical bromfenac (an NSAID), topical dexamethasone (a steroid), or a combination of both for two weeks after surgery.
Patients receiving the combination of the NSAID and steroid drops had a lower risk of developing CME after cataract surgery than patients treated with either agent alone.
CME remains one of the most prevalent postoperative complications in cataract surgery—especially in the diabetic population, where the incidence can be as high as 31%. This landmark study provided a foundation to draw
concrete, evidence-based recommendations to prevent the occurrence of CME after cataract surgery in patients with and without diabetes.
The MYOPRED study, still in progress, looks to influence posterior vitreous detachment (PVD) on retinal detachment after lens surgery in myopic eyes.3 Led by Oliver Findl MD, PhD, the multicentre study will recruit more than 300 patients, document the postoperative presence or absence of PVD, and follow patients for up to five years to assess the influence of PVD on retinal detachment. The results of the study should improve the ability to predict retinal detachment in myopic patients depending on their preoperative status, especially in patients undergoing refractive lens exchange.
The ESCRS has also established several registries to allow surgeons to compare methods and results with surgeons throughout Europe.4 Such data also provide a rich vein of resources for additional studies. The first—and largest—of these registries is the European Registry of Quality Outcomes for Cataract and Refractive Surgery (EUREQUO). With anonymous input from surgeons across Europe, the database aggregates data to improve outcomes and facilitate benchmarking and research.
The European Cornea and Cell Transplantation Registry (ECCTR) created a central data online clearing house to help cornea surgeons assess and verify the safety, quality, and efficacy of various approaches to corneal transplantation. Working with eye banks and academic institutions, ECCTR objectives include evaluating the need for human donor tissue, studying immune reactions on a broader scale, and understanding patient-reported outcomes.
The European Registry for Childhood Cataract Surgery (EuReCCa) is the most recent registry sponsored by the ESCRS. Operating under the auspices of EUREQUO, this registry aims to capture the continent’s practice trends for paediatric cataract surgery. The ultimate goal is to improve quality of life for children with cataracts and their parents.
For citation notes, see page 44.

New tools allow better preoperative prediction and greater customisation.
TIMOTHY NORRIS REPORTS
Cataract and refractive surgery can be even more customisable, increasing performance and visual results at all distances when adding a correct prediction of the patient’s visual experience to the formula, according to Pablo Artal PhD.
He asserted this customisation needs to be central in present and future surgery because of its importance for today’s IOL selection and its service as a core concept for designing future lenses. In standard clinical practice, IOL selection is based on biometry results and the surgeon’s experience, focusing on just the optics—a concern for Professor Artal for the last 25 years. This has led him to think outside the box for ways to improve customisation.
What he came up with is a pretty straightforward solution: collecting data from the geometry of the eye, biometry, topography, and intraocular lens geometry using a Purkinje meter, and using raytracing for the prediction of wavefront optical aberration and chromatic modelling. While extremely important, he added these pure optical measurements are still not enough.
The visual experience must be the final ingredient, something he has been working on for many years with his start-up company Voptica SL. They developed VAO, a novel adaptive optics simulator that allows patients to experience different optics so evaluators can obtain precise measurements. It is a conceptually simple technology that uses a spatial light modulator to manipulate the wavefront of the light during visual
testing. This allows, for example, optimisation of the amount of spherical aberration that can be induced either in the cornea or through an intraocular lens, aiming for a perfect balance between depth of focus and distance quality of vision.
It’s not magic, he said, but a very important way to consider neural responses and an incredibly useful tool to make a more precise optical prediction and choose the best lens for the patient.
This approach allows the surgeon to find what Prof Artal described as the “sweetest spot” for the patient—an optimised visual acuity at far and near—and essential information on the most suitable lens type. Thanks to this testing, evaluations can be done preoperatively to avoid many refractive surprises as well as unhappy patients.
The combination of conventional optics and the results of the patient’s visual experience obtained with an adaptive optics visual simulation can provide the surgeon with ways to optimise the outcomes. Prof Artal suggested the process could soon become extremely useful for designing new lenses and a better understanding of patient selection.
Prof Artal presented at the 2024 ESCRS Congress in Barcelona.
Meet us at the ESCRS Winter Meeting 2025:
Booth M.29





specialist for easy-to-use high-tech solutions.
TOMEY is committed to very high quality, service, and innovation. This leads to early prevention, accurate diagnoses, and examinations that are as comfortable as possible.
Get to know our products in the fields of Cataract & Cornea, Glaucoma & Retina, Refraction, Refraction Units & Furniture.
Join us at the ESCRS Winter Meeting from 28 February to 2 March 2025 in Athens, Greece. Visit us at booth M.29, together with our Greek distribution partner, New Optical Solutions.

Many options for patients under age 60.
HOWARD LARKIN REPORTS
For many myopic patients with presbyopia, phakic intraocular lenses (PIOL) may be a better surgical option than laser refractive procedures or crystalline lens replacement. PIOLs, including iris claw and posterior chamber lenses, are reversible and avoid several potential complications of irreversible alternatives, according to José Luis Güell MD, PhD.
In this group of myopic patients, “lens extraction clearly has retinal risk if you do it before [age] 55 or 60 years old, and laser corneal refractive surgery … will probably limit the options for the intraocular implant in the future,” Professor Güell said. PIOLs also preserve residual accommodation, improving near vision outcomes compared with pseudophakic IOLs using comparable presbyopia-correcting technology. He outlined three scenarios in which PIOLs can help presbyopic myopes maintain near vision uncorrected until cataracts set in.
Retaining existing PIOLs
The first scenario is myopic patients who already have PIOLs implanted and are now reaching presbyopia age. Most of these patients have had minor myopia progression over the years, Prof Güell noted.
In many cases, this progressing myopia, together with residual accommodation (which tends to be greater in myopes
than in emmetropes and presbyopes), provides enough near vision to avoid near correction to at least age 50 to 55 years. With regular biometric, intraocular pressure (IOP), and corneal endothelial cell (EC) count parameters, these patients are often quite comfortable keeping PIOLs in place and using correction only in certain situations, such as night driving.
The second scenario is implanting monofocal spherical or toric PIOLs targeting monovision in patients without previous surgery. This has been Prof Güell’s go-to option for treating qualified presbyopic patients with myopia with or without astigmatism and can be done with either iris claw or posterior chamber PIOLs. It is a good alternative for younger patients, say around age 45 years, allowing delay of lens-replacement surgery until an age when retinal risk is lower, he said.
The third scenario is implanting presbyopia-correcting PIOLs in patients without previous PIOL surgery. Available options include the implantable collamer lens (ICL, STAAR Surgical) and Implantable Phakic Contact Lens (IPCL, Care Group) for posterior chamber placement. The Artiplus (Ophtec) iris claw

lens for anterior chamber placement is awaiting CE approval in Europe, but will likely be available in early 2025, Prof Güell noted. So far, he said all three demonstrate significant gains in intermediate and near vision compared with monofocal versions of the same lenses, with the IPCL performing somewhat better than the ICL in published reports.
The Artiplus is notable because it uses the same multifocal refractive optic as the pseudophakic in-thebag IOL made by the same manufacturer, Prof Güell added. An international study in which Prof Güell participated as clinical coordinator showed it provided uncorrected binocular vision exceeding 0.9 decimal at distance, intermediate, and near for most patients, exceeding the performance of competing PIOLs for near vision.
“Phakic IOLs (particularly the Artiplus model) play a very attractive role in 40- to 60-year-old myopic presbyopes,” Prof Güell concluded, emphasising additional long-term studies are needed to clarify the comparative efficacy and safety of the lenses, and surgeons should be trained in IOL exchange for both the anterior and posterior chambers.
Prof Güell made these comments at the 2024 ESCRS Congress in Barcelona.

Patients are understandably curious to learn as much as they can about their upcoming cataract or refractive surgery. ESCRS has developed a Patient Portal on its website to help inform patients about these surgeries.
The Portal is split into two sections: Cataract and Refractive. Each section provides an easy-to-understand summary of the different types of conditions, including the benefits, risks, procedures, and aftercare of common conditions. Each section is easily navigable, with clear diagrams and a glossary to convey all the information patients might need to help prepare for surgery or during aftercare.
José Luis Güell MD, PhD is a professor, founding partner, and cornea and refractive surgery specialist at the Ocular Microsurgery Institute, Barcelona, Spain. guell@imo.es
AI-powered, cloud-based system can effectively improve traineeship, save time, and increase performance.
TIMOTHY NORRIS REPORTS
Every good trainee aims at getting better, improving efficiency through practice and emulation of a mentor, noted Supriya Sriganesh. Reviewing every surgical video is also beneficial, but it is a habit almost nobody retains. A new software option may help reduce the time-consuming limitations of current technology.
Despite having an operating microscope and a reliable recording system, many surgical videos end up forgotten inside the hard disk, Dr Sriganesh observed. Based on her experience, the reason can be found in the time wasted in plugging the physical hard disk into a personal computer, selecting the right video, and waiting for the download. It is a cumbersome process due to the file size and often disorganised browsing software.
What if these videos were easily accessed on a mobile phone or laptop with just a click? A new training technology presented by Dr Sriganesh called Zeiss Surgery Optimizer is a cloud-based software program that uploads videos from the Callisto recording system, making them accessible from every compatible device. It is now possible to review all personal surgical videos regardless of location. The system features not only the user institution’s cases, but also unedited cases from surgeons all over the world.
The Zeiss Surgery Optimizer also features an AI-powered organiser that splits the videos into different surgical phases, facilitating access to selected parts of the surgery, with timestamps, biometry, OCT, and IOLMaster data included.
According to Dr Sriganesh, the most important feature, especially for training purposes, is ‘Compare.’ In this section, users can select a video from the featured cases or a mentor and place it next to a personal surgical video to learn by comparison.
In her case, it was effective enough to lower her surgical time in cataract surgery from 15 to 6 minutes. A “huge change,” she said.
Dr Sriganesh then decided to test trainees in her institution, 24 in total, tracking 30 cataract surgeries each in three months. Trainees using the Surgery Optimizer improved significantly more—achieving a very consistent International Council of Ophthalmology Surgical Competency Assessment Rubric (OSCAR) score, from an average surgical time of 45 minutes to 15 minutes after three months. Only 30% of the videos were reviewed in the non-Surgical Optimizer group, whereas the Surgical Optimizer group reviewed 100% of surgical videos, which Dr Sriganesh said really made the difference.
She suggested these data show this technique as an effective way to reduce the burden on trainers, making training much easier and more efficient.
Dr Sriganesh spoke at the 2024 ESCRS Congress in Barcelona.
Supriya Samak Sriganesh MBBS, MS, FPRS is Executive Director and Cataract and Refractive Surgeon at the Nethradhama Eye Hospital, Bangalore, India. samak.supriya@gmail.com

Finally, a presbyopia correcting IOL, with clear vision at any distance. To help presbyopia patients regain natural eye sight, with full spectacle independence.

Artiplus is a new premium solution for young presbyopes (40-60 years) to become spectacle independent. The unique, refractive optic of Artiplus with patented CTF technology employs smooth transitions between far and near zones, minimizing glares and halos and offers natural vision at all distances.
With a low add power of +2.5 D, it delivers excellent intermediate and near vision. The iris-fixated design enhances decentration tolerance and reduces cataract risk, making it also ideal for myopic patients.

“The results from the clinical study for uncorrected distance, intermediate and near visual acuity were extraordinarily good. In my experience with Artiplus, the results have been extremely consistent.”
Prof. Dr. José Güell
Binocular best distance corrected defocus curve 6 months, N=48
defocus (0.0D): -0.09 ± 0.06 logMAR
defocus (-2.5D): 0.06 ± 0.11 logMAR
The one-year follow-up from the international multicenter clinical trial demonstrates extraordinary visual acuity at all distances. Defocus curve results highlight the benefits of residual accommodation, enhancing patients’ overall vision experience.
Binocular defocus curve showed a VA ≤ 0.10 logMAR between defocus levels of +1.00 to -3.00 D (Figure 1).


Lively debate format pairs EDOF lenses with trifocals in a dance for first prize in surgery choice.
You could almost see the heel sparks as Team Abanico and Team Castañuelas pounded the Tablao platform over one of the searing questions in cataract refractive surgery—extended depth of focus (EDOF) lenses or trifocals as the first choice? This unique team debate format was part of an ongoing ESCRS effort to liven up the traditional conference presentation format.
Team Abanico fanned the flamenco for EDOF with their feature of avoiding night dysphotopsias. “In the world of presbyopia correction, there is always a compromise. And halos and night vision problems [are] a compromise that cannot be compensated,” said team leader Francesco Carones MD. EDOF lenses reduce such distortions compared with diffractive trifocals, allowing patients to better manage night situations, he said.
He further fuelled the fire by pointing out that technology has changed visual needs. “Intermediate distance is the new near because people use computers, people use tablets. … No one is reading at 30 cm like when newspapers were printed [without a] way for having a bright image.”
EDOF lenses are also more forgiving, Dr Carones said. “If you leave a little bit of residual myopia, that eye can still perform quite well at distance.” So, in most cases, 20/20 distance can still be achieved, plus the extra half dioptre gives an extra boost to intermediate and near vision. “You can really reach
the best of two worlds—avoiding night dysphotopsias as well as having spectacle independence—by having one of the two eyes slightly on the myopic side.”
In the world of presbyopia correction,
there is always
a compromise.
Concluding the first round with a flourish, Dr Carones emphasised quality of vision, especially at night, as key. “Patients are demanding. We do not want them complaining about something that cannot be compensated.” This is becoming ever more important as the average age of cataract patients declines, and they remain more active.
Reading really clicks
Team Castañuelas leader Damien Gatinel MD, PhD, recited several problems with Dr Carones’ EDOF fanfare. Unassisted reading is what matters.
“EDOF lenses are not trifocal. There is a price to be paid,” he said. “There is no near vision that patients can use to read. In some patients, yes, but it is not predictable.”


Often, patients hear ‘near vision’ and they think ‘reading vision,’ which is still needed for using smartphones, Dr Gatinel said. “If you don’t explain everything, then they are not happy.”
Trifocals, Dr Gatinel observed, give intermediate and near vision without introducing spherical aberrations. “Of course, you will have some halos with trifocals. But how many patients complain about halos severely? If it were so many, no one would use them.” Trifocals are the most-used premium lenses worldwide, he pointed out. Indeed, many patients would tolerate even worse halos in exchange for being able to read without spectacles.
EDOF lenses, on the other hand, always sacrifice some distance vision by deforming the optic to provide depth of focus, Dr Gatinel said. EDOF lenses are also less effective in reducing spectacle dependence. “We must always warn the patient that reading specs will probably be necessary, or we must do monovision. But what is monovision but a myopic shift in the non-dominant eye?” Achieving near vision with EDOF lenses, he argued, requires degrading distance vision in one or both eyes.
Finally, patient studies show that perceived visual quality and satisfaction are as high or higher with trifocal lenses, and halos are possible even with EDOF lenses, Dr Gatinel said. “So, what is the point in having halos and no near vision?”
In the end, he argued, EDOF lenses fail to make the patient fully spectacle independent. If surgeons explain the limitations of trifocals and operate on patients with cataracts, the halos and glare are minimal compared with cataracts, he concluded.
Intermediate is the new near Reinforcing Team Abanico’s strongest argument with an enthusiastic audience, Basak Bostanci MD dismissed Dr Gatinel’s arguments as mere chestnuts. Patients no longer
spend much time quietly reading at home. “We are not doing that anymore. We are doing things that require intermediate vision; more dynamic things like digital streaming, household devices, seeing the car panel when we are driving.” Plus, not everyone is a candidate for diffractive IOLs.
“I have a lot of patients and friends and family who don’t want to wear glasses anytime, anywhere, anyplace,” Margarita Cabanás MD refuted for Team Castañuelas. Counselling patients that any dysphotopsias are going to pass is essential to reach that goal. “It’s very important to convey that to my patients.”
After two more lightning rebuttal rounds, the audience rendered its verdict: EDOFs won more fans than clicks for trifocals.
All comments were made amid passionate flamenco dancing in the innovative Workshop Tablao at the 2024 ESCRS Congress in Barcelona.
Francesco Carones MD is medical director and physician CEO of Advalia-Carones Vision in Milan, Italy. fcarones@carones.com
Damien Gatinel MD, PhD is chief of anterior segment and refractive surgery at the Rothschild Foundation, Paris, France, and associate professor at Abulcasis International University of Health Sciences, Rabat, Morocco. gatinel@gmail.com
Basak Bostanci MD, FEBO is associate professor of ophthalmology at Bahcesehir University School of Medicine and cataract and refractive surgeon at Dunya Goz Hospital, Istanbul, Turkey. drbbostanci@gmail.com
Margarita Cabanás MD is associate professor at Loyola University Andalusia and the University of Seville, chief for keratoconus at Clinic Baviera, and head of ophthalmology at Virgen del Rocío University Hospital, all in Seville, Spain.
Improving technology, patient and doctor awareness, and reimbursement are keys.
HOWARD LARKIN REPORTS
Nearly half of cataract and refractive surgeons either don’t implant presbyopia-correcting intraocular lenses or do so in less than 6% of cases. Yet 80% will see their usage increasing, according to the 2023 ESCRS Clinical Trends Survey.
So why the optimism?
Ageing populations that stay active and technology advances that enable it without spectacles are two major drivers, said Yehia Hashad MD. Growing patient awareness from physicians and online resources also helps.
Some countries are adopting or considering at least partial insurance coverage for the procedure—and more may follow as clinical and cost savings evidence pile up, Dr Hashad added. “All of these will contribute to more demand.”
Balancing—and explaining—options
On the technology side, presbyopia-correcting IOL options are constantly expanding, potentially making more patients eligible, Dr Hashad noted.
Yet proliferating options also challenge physicians in understanding and explaining them to increasingly curious patients, said Terry Kim MD. To avoid confusion, he suggested physicians recommend a specific solution meeting each need. “The key factor is the surgeon has to be the driver.”
Arthur Cummings MD agreed. “You’ve got to take away confusion. The paradox of choice is a real thing, so you’ve got to break it down into something really simple where we explain the upside and the cost to make it real for them.” He uses tools including the SimVis Gekko (2EyesVision), which allows patients to see how different lenses might look.
Video is another effective tool, especially when posted on social media. And while social media is definitely raising
patient awareness of new technologies, it should be approached with caution, said Basak Bostanci MD. “You must be careful with your words. Always add that you have to go through some measurements in the clinic to see whether they are eligible for this kind of surgery.” She also uses the SimVis to help patients see how lenses might affect their vision.
Doctors also should be aware of new technologies and how to access them, Dr Cummings stressed.
“What happens is patients say they want a particular lens that maybe their friend has. If you’re not offering that specific IOL or know who to send them to who does offer it, you are not providing good service,” he advised, adding the day may come when information on advanced technology lenses must be included in informed consent.
Cost plays a big role, Professor Kim said, citing South Korea, where presbyopia-correcting IOL penetration skyrocketed to second in the world after health insurance covered them. A friend came back with no glasses, saying she had an ‘eye-washing’ procedure, he added.
Public insurance in most European countries does not cover presbyopia-correcting IOLs, and in the United States, patients must pay the difference over standard IOLs, plus any additional tests needed. Germany and France have a similar co-payment approach, and more may follow, said Tanja Cotoaga. As long-term cost and benefit evidence builds, she sees a shift towards hybrid reimbursement by payers already strapped for cash.
“The patient is the most important player for all of us,” Cotoaga said. “Across all ages, people want to engage fully

in daily activities. They are also willing to pay more for personalised medical care.”
Building the evidence base is key, requiring a mix of controlled, randomised trials that exclude patients with comorbidities to focus on core lens performance, plus real-world studies to see how lenses perform in typical populations, Prof Kim said.
For example, he said the Vivity registry study involving 41 European sites showed the lenses performed consistently. It also yielded valuable information about how the lenses function with monovision, post-refractive surgery, and diseases such as dry eye, glaucoma, and mild retinal pathologies.
Such information, combined with new technology, is critical to improve patient satisfaction, said Tim Clover. And while 95% sounds good, he said it still leaves five dissatisfied patients if surgeons perform 100 procedures. “The technology isn’t quite there yet; people are trading range of vision for dysphotopsias. ... [Rayner’s] new tech takes several steps towards better range of vision,” he said, referring to the recent Galaxy spiral optic IOL.
But informing patients of the trade-offs is critical, Dr Cummings said. “You can tell patients ‘I promise I will get the best range of vision that I can and at the same time protect your quality of vision as much as I can.’” He generally takes a custom match approach of implanting a diffractive trifocal in the non-dominant eye. After one week, if the patient loves it, they get the same in the dominant eye. If not, they get a non-diffractive IOL in the dominant eye.
All comments were made at iNovation Day at the 2024 ESCRS Congress in Barcelona.

As a renowned authority in the field of cataract and refractive surgery, ESCRS facilitates global connections amongst ophthalmic professionals, fostering collaboration and the exchange of knowledge.
Our events span across continents, providing a platform for pioneering research, advanced surgical techniques, and continuous professional development.
Arthur B Cummings MMed(Ophth), FCS(SA), FRCS(Edin), is an ophthalmologist at the Wellington Eye Clinic and Beacon Hospital, Dublin, Ireland. abc@wellingtoneyeclinic.com
Basak Bostanci MD, FEBO is an associate professor of ophthalmology at Bahcesehir University School of Medicine and a cataract and refractive surgeon at Dunya Goz Hospital, Istanbul, Turkey. drbbostanci@gmail.com
Terry Kim MD is professor of ophthalmology at Duke University, Durham, North Carolina, US, and chief medical officer and vice president of global safety for Alcon, Geneva, Switzerland, and Fort Worth, Texas, US. globalmedia.relations@alcon.com
Tanja Cotoaga is global marketing director at VSY Biotechnology, Leinfelden-Echterdingen, Germany. contact@vsybiotechnology.com
Tim Clover is CEO at Rayner, Worthington, UK. feedback@rayner.com
Yehia Hashad MD is an ophthalmologist and executive vice president of research and chief medical officer at Bausch + Lomb, Vaughn, Ontario, Canada.
Using the interactive map on our website, we invite you to explore our global presence by viewing upcoming events and academies.
Join us to network with esteemed experts, access the latest advancements, and contribute to the enhancement of eye care on a worldwide scale.

MICOR non-ultrasonic cataract extractor provides fingertip control.
HOWARD LARKIN REPORTS
Phacoemulsification is safe and effective for removing cataracts—so much so that it dominates the procedure in wealthier countries.
Yet the ultrasound upon which phaco relies also can harm endothelial cells, burn corneal wounds, inflame ocular tissues, and even increase cystoid macular oedema risk. So, throughout its 57-year history, cataract surgery technologies and techniques have progressively developed to reduce phaco ultrasound use.
Now, a lens extraction device that eliminates ultrasound while preserving the advantages of smaller incision cataract surgery is widely available in the US. After years of development and limited release, Zeiss Medical Technology commercially launched the FDA-cleared Zeiss MICOR 700 in September 2024. Pending CE registration trials, it could come to Europe in a few years—and sooner in other parts of the world, a Zeiss spokesperson said.
MICOR offers many potential safety, efficiency, and cost advantages over phacoemulsification, according to surgeons who have used it. This could enable more office-based surgery in the near term. It has the potential to largely replace complex and costly phaco machines, particularly for patients with lower density cataracts. Eventually, it could even expand global access to smaller incision cataract surgery.
“This is very different from the technology that currently exists. It has the potential to provide safe and effective cataract extraction that is potentially more efficient and more cost effective,” said Sonia H Yoo MD. Along with international colleagues, she recently published a study of the MICOR and how it performed in her first 51 patients.1
This is very different from the technology that currently exists. It has the potential to provide safe and effective cataract extraction that is potentially more efficient and more cost effective.
With cost, resource, and environmental pressures building, safe, efficient, greener solutions are increasingly important in cataract surgery, Professor Yoo added. “It checks all the boxes, so I was interested in what MICOR could do.”
Benefits and limits
In place of phaco ultrasound, MICOR uses mechanical energy to fragment the lens nucleus without cavitation. At 40 Hz, its oscillation frequency is about 1,000 times less than phaco. This reduces heat, virtually eliminating phaco hazards such as incision burns and potentially mitigating others, including endothelial cell loss and anterior chamber inflammation. Its blunt tip may also reduce the risk of iris and posterior capsule damage, potentially allowing its use closer to these delicate structures. Together with greatly reduced irrigation fluid use, these could make the device safer than phaco.
MICOR’s mechanisms, including its vacuum pump, are all contained in a device the size of a fat pen controlled by a fin-
ger switch. An irrigation bag is its only external connection. It thus eliminates the need for a separate phaco console—along with the foot pedal, wires, and tubes that connect the pieces and the accompanying operating room space.
MICOR also eliminates the upfront cost of a phaco machine, which runs as high as €80,000, plus maintenance costs. A disposable extraction tip greatly reduces turnaround time between MICOR cases, enabling efficiency gains and cost savings. The pump portion of the handpiece can be sterilised or draped during surgery for further reductions.
Prof Yoo reported the learning curve for using MICOR is short, with mean lens extraction and total surgical times dropping significantly in each of the 7 days she operated on her first 61 eyes. However, in its current state of development, the device does better with certain surgical techniques than others, she said. Chopping works well, but the device does not support a divide-and-conquer approach. “It is not a sculpting device.”
While the blunt, unbevelled extractor tip increases safety, its smaller surface area can increase extraction time compared with a bevelled tip, Prof Yoo added. Similarly, operating the machine with a finger instead of a foot pedal offers finer control. Yet MICOR also relies on gravity infusion rather than a pump to maintain anterior chamber pressure.
“You tend to have a little less stability and a little more post-occlusion surge because you don’t have positive pressure from the machine,” Prof Yoo explained. “As they develop the technology, I think they will be able to do things in that handpiece to further stabilise the anterior chamber.”
So, can MICOR replace phaco in all cases? Doing so could be the key to success, said Richard B Packard MD, who is familiar with the device but has not used it. “The cost issue is in its favour if it works very efficiently. But if you still [need] a phaco machine, there is no cost advantage.”
In her study, Prof Yoo found MICOR performed efficiently in grade 1.0 to 2.0 nuclear sclerotic cataracts, with extraction times similar to phaco. However, the device was less efficient with harder cataracts. For denser cataracts, she said pre-chopping or using Zeiss’ miLOOP nitinol loop devices can be helpful.
Prof Yoo limits her use of the device to patients under age 70 as a surrogate for cataract density, though she noted she has not tested that cut-off. She does not recommend MICOR for harder cataracts so early in the learning curve.
However, MICOR has been shown effective up to grade 3.5 in tests, though miLOOP helps for harder cataracts, said Frank Seitzinger, Zeiss’ business head for anterior segment surgery. And some surgeons working with Zeiss in a limited-release programme say they can use it for all cases, though it does require some technique modifications. The device will be developed further based on market feedback, he added.
Prof Yoo sees the device as useful for refractive lens cases and younger patients, as well as for surgeons looking to add an in-office or expand an existing operating theatre without the upfront investment of a new phaco machine. Seitzinger
Think back to the earlier iterations of ultrasound phaco machines; they were nothing like they are today.
sees a big role for premium surgery focusing on non-ultrasound lens extraction (NULEX), providing a safer, more comfortable patient experience.
Zeiss released MICOR in the US first in part because the European approval process now takes 18 to 24 months and requires additional studies, Seitzinger said. The company is actively considering CE registration but plans to market it in countries that recognise FDA clearances for now. Zeiss is also considering developing it for use in areas where traditional phaco machines cannot be used.
Those plans will likely be essential to MICOR’s future success, Mr Packard said. “It looks very neat, and it’s very clever. It’s truly disruptive that everything is in the handpiece.” But it remains to be seen if it can compete with phaco, which took decades of development and the introduction of foldable lenses before it was widely used. He noted STAAR Surgical released a sonic lens extraction machine in 2001 that did not make it, despite favourable test results.
Prof Yoo expects further development for the device, broadening its functionality—possibly even including a battery pack to allow use in areas with unstable electricity. “Think back to the earlier iterations of ultrasound phaco machines; they were nothing like they are today. The technology always improves.”
For citation notes, see page 44.
Sonia H Yoo MD is professor of ophthalmology and biomedical engineering, associate medical director, and holds the Greentree Hickman endowed chair in ophthalmology at Bascom Palmer Eye Institute of the University of Miami Miller Medical School, Florida, US. syoo@med.miami.edu
Richard B Packard MD, FRCS, FRCOphth is an ophthalmologist in London, UK. eyequack@vossnet.co.uk
Frank Seitzinger is Head of Business Sector Surgery Anterior Segment for Zeiss Medical Technology. renae.cazet@zeiss.com
Clinical evaluation and personal judgment come into play.
HOWARD LARKIN REPORTS
Photorefractive keratectomy (PRK) and laser-assisted in-situ keratomileusis (LASIK) are two of the oldest and most common refractive surgeries. But just because surgeons can use them doesn’t mean they should, especially when other treatment options exist, said Robert Edward T Ang MD.
Dr Ang pointed out excimer laser treatment range recommendations vary considerably by manufacturer, from up to -12.00 D to -16.00 D for myopia and +3.00 D to as much as +9.00 D for hyperopia. For astigmatism, recommendations range from -3.00 D to -7.00 D.
“But of course, like my car, I don’t drive 300 km per hour even if the speedometer will allow me to,” he observed. “We have our own comfort levels and go from there, even though the lasers can do this much treatment.”
Corneal anatomy and biomechanics, published literature, personal experience, and alternative treatments should all be considered when setting limits for PRK and LASIK, he added.
Thickness and topography
Dr Ang stressed the importance of calculating the residual stromal bed, achieved by deducting the flap thickness and the amount of tissue to remove from the preoperative total corneal thickness.
“Most systems have planning software,” he noted.
The literature suggests leaving at least 250 microns of residual stroma, but many surgeons who have been burned by ectasia opt for a thicker remaining cornea.
So, is there a maximum amount of tissue that can be ablated with PRK or LASIK? Higher treatments are associated with decreased outcome accuracy, regression, induction of higher-order aberrations, ectasia, and corneal scarring, Dr Ang noted. “The higher you go, the more risk you take on.” He sets boundaries and limits to avoid complications such as ectasia and postoperative haze and to aid in screening, counselling, and considering treatment alternatives.
Other factors that affect limits include topography and tomography. Compromised preoperative biomechanics will cause corneal decompensation, leading to ectasia. Dr Ang recommended using as many screening metrics as possible, including irregular and asymmetric bowtie topographies and Pentacam and Corvis corneal indices, such as BAD, TBI, and CBI.
“It’s not only about corneal thickness,” he explained. “Suspicious irregularities are as important, or maybe even more so.”
That goes for all forms of corneal refractive surgery, including PRK and SMILE, he added. “I actively look to disqualify from LASIK. It is a proactive approach.”
But a disqualification for LASIK isn’t the end of the road, Dr Ang said. For suspicious but not abnormal or forme fruste corneas, he considers PRK or implantable collamer lenses (ICL). As for refraction, he does LASIK up to -5.00 D myopia with up to -2.00 D cylinder and hyperopia up to +3.00 D. For PRK, he will go to -7.00 D myopia with up to -2.00 D cylinder and does not do hyperopic PRK.
Dr Ang will not perform LASIK on corneas under 500 microns, regardless of topography or refractive error. He does no tissue ablation above 120 microns and leaves at least 300 microns of residual stromal bed for LASIK and 350 microns for PRK.
Limits, boundaries, and risk tolerance are based on screening data and personal judgment, with limits reducing with experience, Dr Ang concluded. “I know this lowers your volume of patients, but you sleep better at night.”
Dr Ang spoke at the 2024 ESCRS Congress in Barcelona.
Robert Edward T Ang MD is a senior consultant and head of cornea and refractive surgery at the Asian Eye Institute, Makati City, Philippines. angbobby@hotmail.com



Lifestyle changes and ophthalmic interventions play a role in treating paediatric myopia.
Combining behavioural interventions, such as ensuring children spend at least 2 hours a day outside, with optical or pharmaceutical treatments may do a better job of preventing and slowing childhood myopia than relying on a single treatment, according to Ken K Nischal MD.
Professor Nischal pointed to differences in outcomes for children treated with low-dose atropine to prevent or slow myopia progression and axial elongation. Studies in Singapore, Taiwan, China, and Hong Kong clearly show it works, he noted. But a study last year in the US found no effect.
So, what’s the difference? Public health policies, Prof Nischal suggested. These may include requiring schools to limit reading and other near work to 30 minutes at a time, ensuring adequate lighting, and providing an hour of outdoor activity every day, as well as encouraging parents to get children outside 2 hours a day.
Starting with South Korea in 1997, countries throughout East Asia have adopted such policies, but the US and Europe have not, Prof Nischal noted. “If you have a public health policy, it makes sense anything you do above that will be more efficacious than if you don’t. We need to look at the public health background when we read these studies.” However, the authors of the US study wrote that differences in study design and genetic differences in the study groups may be at play.1

Other research supports combining myopia treatments, said Erin Tomiyama PhD. “We see studies adding atropine to [orthokeratology] or soft multifocal contact lenses as more effective.” It may be that different therapies have different mechanisms of action, “so we are hitting myopia from more than one angle,” she added. Early intervention is also critical, with a year of prevention equal to 3 years of treatment.
Prof Nischal cautioned that understanding the specific cause of myopia is essential for successful treatment. “Not every myope has a long eyeball. Some have steep corneas.”
But treatment does work, and slowing myopia progression or preventing it altogether can have a massive impact on a patient’s life, Prof Nischal added. “What we do today will affect millions of children and adults 20 years [from now]. Can anybody think of an intervention in ophthalmology that will prevent disease like this?”
So how can general ophthalmologists address childhood myopia in daily practice? Dominique Bremond-Gignac MD, PhD suggested three actions.
First, when treating adults for refractive myopic errors, counsel them to get any children they have screened for myopia because they have a higher risk than the general population, Prof Bremond-Gignac said. Parents should also be reminded of environmental preventive steps such as going outside frequently and participating in sports. Early screening can help spot pre-myopia in young children who have less hyperopia than normal for their age, allowing for preventive treatment.
Second, when seeing children with myopia, the diagnosis should be made by cycloplegic refraction. “You need an accurate baseline to detect later progression, even if it is a low myopia, such as -0.50 D.”
Third is treatment. Even if referring to a paediatric ophthalmology subspecialist, explain to parents that treatment is available to reduce progression beyond environmental prevention, Prof Bremond-Gignac said. This may include
defocus contact lenses, orthokeratology, or low-dose atropine. Referring for an initial evaluation and then following in a general practice is an option, she added.
When talking with parents about their children with pre-myopia or myopia, explain that treatments are available and why they are needed, said Ramesh Kekunnaya MD. Not only can treatment improve vision and prevent future complications such as retinal tears and glaucoma, but it can also reduce the hidden psychosocial effects of wearing high-refraction spectacles for their entire life.
“Parents don’t want to see their children go from -1.00 D to -6.00 D,” he said. “When you give them this perspective, adherence to suggested modalities becomes much better. Generally, it takes a few minutes to explain. Education of patients—children—and their parents is the most important.”
Specific recommendations depend on the child’s condition, Dr Kekunnaya added. “For pre-myopes, we focus on behaviour modifications. For those with myopia already, we talk about behavioural modifications, plus either a pharmacological or optical treatment.”
Dr Kekunnaya emphasised conveying accurate information and addressing any misinformation, such as drops correcting astigmatism, which they can’t. He recommended parental brochures from the World Society of Paediatric Ophthalmology and Strabismus, available in English, Spanish, Mandarin,
and Portuguese. Public health messages in bus stops and other high-traffic areas can also help increase awareness. “Buy-in from parents is extremely important.”
All verbal comments were made on iNovation Day at the 2024 ESCRS Congress in Barcelona.
For citation notes, see page 44.
Ken K Nischal MD, FAAP, FRCOphth is professor and chief of pediatric ophthalmology and strabismus at UPMC Children’s Hospital of Pittsburgh, Pennsylvania, US. nischalkk@upmc.edu
Erin Tomiyama OD, PhD, FAAO is assistant professor of optometry at Marchall B Ketchum University, Anaheim, California, US. etomiyama@ketchum.edu
Dominique Bremond-Gignac MD, PhD, FEBO is professor and head of the ophthalmology department at University Hospital Necker-Enfants-malades and Paris University, Paris, France. dominique.bremond@aphp.fr
Ramesh Kekunnaya MD, FRCS is director of the Child Sight Institute, Eye & Brain lab, Center for Technology Innovation and network director at the L V Prasad Eye Institute, Hyderabad, India. rameshak@lvpei.org

Need a quick introduction or refresher about a surgical procedure? Have a tip to share about a technique or approach you use that makes surgery easier?
The ESCRS 100 is the place to go. It’s a library of short (roughly 100 seconds), high-quality instructional videos about all fields of cataract and refractive surgery.More than a dozen videos have already been created, and additional videos are being uploaded each month. Current videos include the following topics:
• Descemet membrane stripping
• DALK: how to get to Descemet membrane
• Hydrodissection
PUT THE ESCRS 100 VIDEO SERIES ON YOUR LIST OF MUST-WATCH EDUCATIONAL RESOURCES ! ESCRS 100

Anti-VEGF agent maintains favourable efficacy and safety profile in a prospective trial.
CHERYL GUTTMAN KRADER REPORTS
Intravitreal aflibercept 0.4 mg to treat acute-phase retinopathy of prematurity (ROP) in extremely preterm or very low birthweight infants is effective and well-tolerated with follow-up of participants through three years of age, suggest the interim results from the FIREFLEYE Next study.
FIREFLEYE Next is an extension of the FIREFLEYE study, the first phase 3b study investigating aflibercept for ROP. In FIREFLEYE (the original core study), 113 infants were randomised 2:1 to receive aflibercept or laser photocoagulation. Stage 3+ was the most common stage of ROP among participants in the core study. One hundred infants entered FIREFLEYE Next, of which 90 were seen at three years of age.
“In this pre-planned interim analysis of FIREFLEYE Next, efficacy outcomes for the group treated with aflibercept in FIREFLEYE were well sustained, no new ocular or systemic safety concerns emerged, disease reactivation was rare, and visual function was age appropriate given the limitations of obtaining accurate measurements at this age,” reported Andreas Stahl MD. “Now we are looking forward to the results from follow-up to five years of age, which should be available in 2026.”
At entry into this study, children had a chronological age of nine months, and 84% had no ROP. Among aflibercept-treated eyes, 80% achieved complete retinal vascularisation by two years of age.
Unfavourable structural outcomes were analysed as a key endpoint in FIREFLEYE Next, and the overall rate of these events was around 6% in both the aflibercept and laser groups. ROP reactivation was rare in the aflibercept group until two and three years of chronological age (1.5% and 1.7%, respectively) and absent among laser-treated eyes.
“All reactivations in the aflibercept group occurred before the child reached 50 weeks of chronological age, and the reactivation rate within the first few weeks to months after treatment was similar to what has been reported with other anti-VEGF agents,” Professor Stahl said.
Four patients in the aflibercept group were treated for ROP complications after entry into FIREFLEYE Next and before reaching one year of age. The complications included pre-existing retinal detachment (two patients), reactivated plus disease (one patient), and retinal neovascularisation that was not further specified (one patient). In addition, a single aflibercept-treated patient was found to have a retinal detachment at age three years that was a progression of an earlier documented macular fold.
At three years, BCVA was ≥20/200 in close to 100% of eyes in both groups, ≥20/40 in 66.7% of aflibercept eyes, and 47.8% of lasered eyes. Refractive outcomes were consistent with findings in other trials of anti-VEGF treatment for ROP, showing a higher incidence and greater severity of myopia in the laser-treated arm compared to the aflibercept group, Prof Stahl reported.
There were no clinically relevant differences in growth parameters between groups, and overall, growth parameters were consistent with what is expected in a prematurely born paediatric population. Adverse events during FIREFLEYE Next were also consistent with those expected in this population.
Prof Stahl spoke at the 2024 EURETINA Congress in Barcelona.
Andreas Stahl MD is Director and Chair of Ophthalmology, Greifswald Medical School, Greifswald, Germany. andreas.stahl@med.uni-greifswald.de
The Fellowship of €60,000 will allow a trainee to work abroad at a centre of excellence for clinical experience or research in the field of cataract and refractive surgery, anywhere in the world, for 1 year. The application deadline is 2 May 2025.
Applying information from preoperative diagnostics guides surgical planning.
CHERYL GUTTMAN KRADER REPORTS
Cataract surgeons operating on eyes with corneal disease need to understand how different abnormalities impact quality and quantity of vision, said Damien Gatinel MD, PhD.
“The effect of a diseased cornea on outcomes of cataract surgery is an important topic, considering the cornea accounts for more than 60% of ocular power,” Dr Gatinel said. “Power is not everything, however, because a diseased cornea also affects optical quality.”
Modelling with a new device that uses interferometry technology and wavefront propagation aberrometry to analyse the optical quality of IOLs (NIMO TEMPO, Lambda-X) allows insight into the interactions between different corneal abnormalities and different IOL optic designs.1 Dr Gatinel illustrated this point with a series of examples showing how modulation transfer function, point spread function, and depth of focus can be dramatically affected in eyes with keratoconus or different amounts of corneal spherical aberration compared to those with a ‘normal’ cornea.
“The consequences for postoperative visual performance are important to keep in mind during our surgical decision-making,” he explained. “But there is another problem cataract surgeons face when operating on eyes with a diseased cornea: the issue of IOL power.”
Understanding of the latter issue is gained through evaluations performed with different types of diagnostic instruments, and Dr Gatinel highlighted this point by discussing another group of cases. In one example, he showed wavefront analysis and corneal topography imaging would predict poor visual acuity after cataract surgery in an eye with keratoconus where there is power distortion from the anterior cornea.
“Putting a contact lens on the same eye results in improved visual acuity, which confirms the cornea is the cause of the problem,” he said. “It also indicates the contact lens will do a
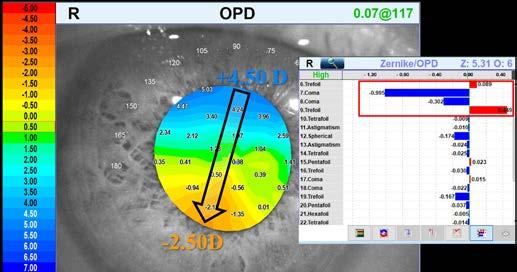
better job correcting this patient’s vision than any toric pseudophakic IOL.”
As further support for his point, Dr Gatinel presented a case of a keratoconic eye implanted with a toric IOL. Although the measured refractive outcome was good, the topography and wavefront analysis showed a vertical gradient of uncorrected power due to persisting coma asymmetry (see image).
The effect of a diseased cornea on outcomes of cataract surgery is an important topic considering the cornea accounts for more than 60% of ocular power.
“I dare anyone to [guess] the refraction of that eye in which there is a 7.0 D power change from the top to the bottom of the pupil,” he said.
Dr Gatinel also discussed the evaluation and management of eyes with a loss of corneal transparency that can occur because of dystrophies, haze, scarring, or oedema. He recommended measuring light scatter in these cases to assess the potential impact on post-cataract surgery visual quality, mentioning a recently published paper describing an objective approach for detecting subclinical oedema developed by applying artificial intelligence to the analysis of corneal OCT images.2
A final case involved a patient with extreme corneal opacity and aniridia who was able to function until a cataract developed. Given the situation, Dr Gatinel said he was reluctant to perform either cataract surgery or a corneal transplant. Ultimately, he proceeded by trephining the cornea, removing the cataract, implanting an IOL, and replacing the trephined tissue.
“Postoperative BCVA was dramatically improved to 20/200, which allowed the patient to function without dependence,” he said. “The lesson I learned from this case is it is still worth removing an opaque crystalline lens in an eye with an opaque cornea because having two opacities is still worse than one.”
Dr Gatinel spoke during Cornea Day at the 2024 ESCRS Congress in Barcelona.
For citation notes, see page 44.
Damien Gatinel MD, PhD is Head of Anterior Segment and Refractive Surgery, Rothschild Foundation Hospital, Paris, France. gatinel@gmail.com
Concepts regarding best techniques shift based on learnings from longer follow-up.
CHERYL GUTTMAN KRADER REPORTS
Long-term follow-up of patients with keratoconus treated with combined corneal cross-linking (CXL) and excimer laser surface ablation is causing Paolo Vinciguerra MD to raise a red flag and caution colleagues and patients about the potential for massive corneal flattening as a late-onset occurrence.
“This is a new finding, and it indicates surgeons should be aware that combining CXL and refractive surgery can be very dangerous,” Dr Vinciguerra said. “Therefore, they should be prepared to expect a surprise many years after patients undergo a combination procedure with CXL to stabilise disease progression and excimer laser surface ablation for visual rehabilitation, and they may need to warn patients that the long-term outcome is unpredictable.”
Having been an investigator in the clinical trial conducted to gain regulatory approval of CXL for keratoconus, Dr Vinciguerra has accrued a group of patients he has been following for almost two decades. This cohort now includes more than 20 patients whose keratometry remained stable for 10 to 14 years, but then manifested significant central flattening of 5.0 to 6.0 D and peripheral steepening resulting in hyperopic refraction.
Imaging of these eyes showed stability of epithelial thickness and corneal pachymetry. However, changes in anterior and posterior corneal elevation maps were documented along with shallowing of the anterior chamber depth. In addition, the CXL demarcation line was very deep centrally and became progressively more superficial, extending out to the periphery.
Dr Vinciguerra proposed minimising/avoiding tissue ablation might offer a solution for avoiding late-onset flattening. With that idea in mind, he expressed an interest in Phototherapeutic keratectomy-Assisted Customised Epi-on corneal cross-linking (PACE-CXL), introduced by Farhad Hafezi MD, PhD and colleagues at the ELZA Institute in Zurich, Switzerland.
“PACE-CXL involves only a localised epithelial ablation followed by a proprietary irradiation protocol specifically designed to improve corneal shape. Although it is a promising technique, longer follow-up is needed to establish its efficacy and safety compared to other approaches,” Dr Vinciguerra said.
“The deeper question is whether we fully understand the long-term remodelling dynamics of cross-linked corneas and how different techniques (e.g., epi-on vs. epi-off) and energy delivery methods interact with the corneal biomechanics. Until we have more data, it would be prudent to individualise

treatment plans, focusing on minimal tissue ablation when excimer laser ablation is needed and leaning toward approaches like PACE-CXL when corneal stability is the priority.”
To rehabilitate vision in eyes with keratoconus, Dr Vinciguerra now performs a customised ablation based on the total corneal wavefront that targets the most visually significant aberration in keratoconic eyes while minimising tissue ablation. It uses Schwind’s ORK-CAM planning software and links the total wavefront map obtained with the company’s combined topographer/aberrometer (Peramis) to the Amaris excimer laser. The system discriminates between coma and astigmatism and prioritises correction of coma that impacts visual acuity by >0.5 D, regardless of sphere and cylinder.
“Coma is the most important HOA in eyes with keratoconus, but it should not be fully corrected on the anterior surface, considering there will be compensation from posterior surface coma,” Dr Vinciguerra explained. “Because this custom ablation treats only the most vision-impairing aberrations, it is very shallow and tissue-saving and therefore maintains corneal stability.”
Dr Vinciguerra spoke at the 2024 ESCRS Congress in Barcelona.
Paolo Vinciguerra MD is Professor and Head of the Ophthalmology Unit, Humanitas Research Hospital, Milan, Italy. paolovinciguerra@me.com

THIS IS THE THIRD OF A THREE-PART SERIES BY PROFESSOR FARHAD HAFEZI MD, PHD; MARK HILLEN PHD; AND EMILIO TORRES-NETTO MD, PHD.
Leaving the corneal epithelium intact during CXL (‘epion’ CXL) had long been desired, pushing researchers to quickly develop two main approaches to getting riboflavin through the epithelial cell tight junctions and into the stroma: iontophoresis1,2 (where an electrical current is applied to electrostatically force riboflavin molecules through the epithelium) and the use of penetration enhancers such as ethylenediaminetetraacetic acid (EDTA) or trometamol that degrade the tight junctions and allow riboflavin to pass between the epithelial cells.3
Once again, these approaches resulted in lower cross-linking efficacy than Dresden protocol CXL (sometimes to quite an extent)4 and left efficacy on the table. The reason was simple: not only does an intact epithelium act as a barrier to oxygen diffusion into the stroma—it also absorbs up to a fifth of the UV fluence administered.5 Again, approaches like supplemental oxygen were used to try to optimize that aspect of the CXL procedure, and again, the delivery of higher UV fluences helped to close the efficacy gap.6
Customized and combination CXL:
Laser refractive surgery involves the removal of stromal tissue, which weakens the cornea’s biomechanical strength. Most corneas have more than enough strength in reserve for this surgery to be performed safely, but in thin corneas or ones with forme fruste ectasias, the procedure’s safety can be compromised. This is why comprehensive screening is necessary before undertaking any refractive laser procedure.
CXL strengthens the cornea and may allow the laser procedure to be performed with a higher degree of confidence a corneal ectasia will not develop later (these are called ‘Xtra’ procedures).7 However, recent long-term follow-up studies suggest no additional benefit in visual or safety outcomes achieved by prophylactically cross-linking corneas undergoing laser refractive surgery.8,9
Therapeutic laser surgery is also possible in ectatic corneas, where the aim is not perfect refractive correction (which would be unachievable) but to regularize the cross-linked and
therefore strengthened cornea to reduce certain higher-order aberrations and improve visual quality, often in combination with special contact lenses. The first examples of these procedures were the combinations of CXL and topography-guided PRK (Athens10,11 and Cretan protocols12), and these approaches appear to bring sustained visual acuity and astigmatism reduction benefits.11,13–15 Further attempts to optimize (such as Miguel Reichichi’s STARE-X16 and Rohit Shetty’s TREK17) aim to achieve these benefits while minimizing the amount of stromal tissue ablated by the excimer laser.
CXL alone typically causes, on average, around 1 dioptre (D) of corneal flattening; the issue is the amount of flattening is highly variable and unpredictable.18 But in ectatic corneas, any flattening of the cone is of value as it partially rehabilitates the shape of the cornea and, with it, patients’ vision.
Topography-guided CXL, which attempts to selectively flatten the thinnest or steepest areas of the ectatic cornea, was developed. This approach uses specialized equipment to deliver higher UV fluences to these regions, along with an eye tracker to accurately target the UV energy.19 This resulted in corneal flattening responses of approximately 2–4 D,20–22 even when supplemental oxygen was used.23
A second-generation customized CXL technique, PTK-assisted customized epi-on CXL (PACE), has since been developed.24 PACE involves three steps. First, an epithelial map-driven phototherapeutic keratectomy (PTK) is performed to remove a limited region of the epithelium over the cone while sparing stromal tissue. This makes PACE a partial epi-on/epi-off procedure, which means when riboflavin is applied in the next step, it generates a concentration gradient that peaks over the cone. Finally, the cone region receives a higher total fluence than the rest of the cornea.
Preliminary results demonstrate a more pronounced flattening effect compared to first-generation customized CXL, with observed reductions in corneal asymmetry of up to 12 D within the first month following the procedure.24 This larger flattening enables a greater amount of visual rehabilitation.
Both first- and second-generation customized CXL approaches offer the advantage that, after corneal stabilization, PTK, PRK, intracorneal ring segment surgery, or a combination thereof, can further enhance corneal symmetry and reduce aberrations.
PACK-CXL and beyond: expanding indications CXL’s potential extends beyond corneal ectasias. As mentioned above, CXL kills keratocytes in the stroma; it also kills pathogens. The ROS generated by the UV-riboflavin reaction directly attacks and damages pathogen cell membranes (leading to lysis) and intercalates with pathogen nucleic acids, inhibiting replication.25,26 This is the same method blood banks use to sterilize blood products.
Not only does this property of CXL support its use in an office-based setting (such as at the slit lamp),27 it is also a valuable tool in treating infectious keratitis and a method that sidesteps the issues of pathogen antimicrobial drug prophylaxis. A phase III trial has shown a single treatment with this
‘photoactivated chromophore for keratitis-CXL’ (PACK-CXL) procedure can be as effective as standard-of-care antimicrobial drug therapy for treating infectious keratitis of bacterial, fungal, or mixed bacterial/fungal origin.28
Unlike with CXL for ectasia, it also appears increasing the UV intensity does not significantly compromise its efficacy; like CXL for ectasia, higher UV fluences increase efficacy.29,30 The main reason is corneas with infectious keratitis are typically opaque, and UV transmission reduces significantly with ulcer depth.31 This also means higher fluences can be used safely concerning the corneal endothelium under these circumstances.
It is worth noting that other chromophore/light combinations are under investigation for PACK-CXL, principally rose Bengal and 532 nm green light (as seen in the image with this article). These have also shown good pathogen-killing efficacy and can be combined with riboflavin/UV CXL.32
Conclusion: the future of CXL
CXL has gone from a single-indication ectasia treatment (keratoconus) to one used to treat several conditions, including iatrogenic post-refractive laser surgery ectasia, Terrien 33 and pellucid marginal degenerations, 34 and even keratoglobus. 35 Customized CXL protocols like PACE mean CXL can now be used not only to arrest ectasia progression but also to rehabilitate the shape of the cornea and improve patients’ vision.
PACK-CXL is a valuable addition to cornea specialists’ arsenal for treating infectious keratitis. As PACK-CXL can often succeed after a single treatment, it can hold particular value in low- to middle-income countries (LMICs), where physician and treatment costs are high and patients often lack the resources for a first (let alone a second) medical appointment. Indeed, the pathogen-killing nature of CXL, which enables it to be performed as safely in a doctor’s office as an operating room, is a cost-saving feature that can be particularly beneficial to LMICs.27
The future of CXL probably encompasses further optimization of existing techniques, either when used alone or in combination with other procedures. One exciting prospect may be two-photon CXL, in which a femtosecond laser can be used to selectively cross-link parts of the cornea at specific points in three-dimensional space.36–38 What value this might have—perhaps refractive, as a treatment for myopia and astigmatism in general, or rehabilitating irregular corneas—remains to be seen. But CXL still appears to have a great deal of potential yet to be revealed.
Part one of this series appeared in the November 2024 issue; part two appeared in the December issue.
For citation notes, see page 44.
Farhad Hafezi MD, PhD, FARVO is the medical director of the ELZA Institute in Zurich, Switzerland, and is an ESCRS board member.
Mark Hillen PhD is the communications director of the ELZA Institute.
Emilio Torres-Netto MD, PhD, FWCRS is a cornea, cataract, and refractive surgeon at the ELZA Institute.
New gene-agnostic treatments for inheritable retinal disease.
Anew gene-agnostic therapy called SPVN06 (SparingVision) has shown favourable safety and tolerability profiles in patients with retinitis pigmentosa in the Phase I/II PRODYGY clinical trial, said Daniel C Chung.
“With gene-agnostic therapy, we can probably reach a broader range of patients,” he said. “We can treat those with very rare genotypes that may not ever get any kind of clinical development done.”
He noted SPVN06 was designed to counteract cone photoreceptor degeneration in eyes with moderate to advanced retinitis pigmentosa. Using a subretinally injected adeno-associated virus (AAV) vector, SPVN06 delivers two distinct isoforms of the NXNL1 gene—rod-derived cone viability factor (RdCVF) and RdCVF long form (RdCVFL)—to the cones and retinal pigmented epithelium (RPE).
In healthy eyes, RdCVF is secreted by the rods, which initiates a metabolic pathway that increases glucose metabolism and carbohydrate synthesis when it reaches the cones, Dr Chung explained. Eyes with retinitis pigmentosa find the depletion of rods leads to an absence of RdCVF and, ultimately, cone death. RdCVFL is a potent antioxidant that protects cones against oxidative stress.
The ongoing clinical trial involves patients with retinitis pigmentosa of the alpha and beta rhodopsin phosphodiesterase genotypes. In the first dose escalation phase of the study, three dosage cohorts of three patients—each with vision of 20/200 or worse and visual fields of 20 degrees or less—will receive low, intermediate, and high dosages, respectively. The trial extension will involve three cohorts of patients with less advanced vision loss and primary and secondary endpoints of safety and efficacy at a one-year and five-year follow-up.
“We’re in the third dosing cohort right now, and if everything works out, we hope to have this fully enrolled by the end of 2024,” Dr Chung said.
He noted the first two dosage cohorts had no serious adverse events, no dose-limiting toxicities, and minimal inflammation. In the second cohort, nearly all patients developed hyperaemia—one patient had a macular hole (which resolved on its own), another patient had a reduction in visual acuity at six months (which later resolved), and one patient had a very slight reduction in visual acuity.
Dr Chung and his associates at SparingVision have developed another gene-agnostic therapy called SPVN20, designed to restore function to dormant cones with degenerated outer segments from retinal dystrophies. Like SPVN06, SPVN20 has an AAV vector but is administered intravitreally rather than subretinally, potentially in an office procedure. The treatment delivers a gene to induce membrane expression of G protein-gated inwardly rectifying potassium channel (GIRK), which creates a short transduction cascade within the dormant cones.
“In preclinical studies, once you put that in, phototransduction is restored,” he said. “So we are hoping to be able to restore function. This is restorative—a little different from RdCVF06, which is more about slowing or stopping the cone degeneration.”
SparingVision is planning a trial, which they have dubbed “NIRVANA, with SPVN20 in 2025, most likely starting with patients with no light perception,” Dr Chung said.
Dr Chung presented his paper at the 2024 Retina International Congress in Dublin.
Daniel C Chung DO, MA is Chief Medical Officer at SparingVision, Philadelphia, Pennsylvania, US. daniel.chung@sparingvision.com

Registry-based studies indicate risk for retinal vascular occlusions have not increased.
CHERYL
GUTTMAN KRADER REPORTS
Multiple cases, case series, and cohort studies report the development of retinal disease after COVID-19 and COVID-19 vaccination, and knowledge that COVID-19 can cause vascular damage and coagulopathy provides biologic plausibility implicating the infection and vaccination in these events. Thus far, however, findings from research analysing clinical registry data show no proof of causality, according to Rahul N Khurana MD.
“Establishing causality is extremely challenging when there is a high incidence of both the possible causal factor and its effect,” Dr Khurana noted. “I think the answer for doing so lies with big data.”
Reviewing research investigating a cause and effect relationship between COVID-19 infection and retinal disease, Dr Khurana discussed a study using the American Academy of Ophthalmology IRIS registry as a data source to determine rates of retinal vein occlusions (RVOs) in the 3 years preceding the start of the pandemic (2017–2019) and the first 3 years from its onset (2020–2022).1 Results showed the number of branch RVOs and central retinal artery occlusions did not increase during the pandemic era, while central RVOs decreased. Another study using the Vestrum Health database of medical records from more than 65 private US retina clinics as a resource generated consistent findings.2
“Ophthalmic care utilisation was suppressed during the pandemic, and so more severe diagnoses accounted for a larger percentage of our clinic visits, which gives us the impression that their incidence was higher,” Dr Khurana explained.
Although the findings from both studies seem compelling, neither database had information on COVID-19 diagnosis. A nationwide population study in South Korea that included data from more than 8.5 million patients overcame that limitation. This more definitive study found no increase in either retinal artery occlusion (RAO) or RVO within 60 days after a COVID-19 diagnosis.3

or tetanus/diphtheria/pertussis vaccination in a propensity score-matched control group.
The study from South Korea provided further evidence that COVID-19 vaccination does not increase retinal vascular occlusive events by showing no increase in RAO or RVO within 60 days after vaccination.3 A subgroup analysis showed a possible small increase in RAO among women who received an mRNA vaccine, but the incidence was low (0.0028%), Dr Khurana said.
A third piece of evidence comes from a retrospective analysis of data in the Centers for Disease Control Vaccine Adverse Events Reporting System.5
“This system involves passive surveillance, and so there could be underreporting,” Dr Khurana stressed. “Nevertheless, a study reviewing more than 2 billion vaccines administered globally found only 1,351 reported RVOs with very low crude rates for each of the three vaccine types. These data show a low concern about retinal safety of COVID-19 vaccination.”
Research investigating a cause and effect relationship between COVID-19 vaccination and retinal disease also provides reassuring findings, Dr Khurana said.
In a study using the TriNetX Analytics platform, which includes deidentified medical records of more than 100 million patients from 77 healthcare organisations across 9 countries, researchers found a very low rate of RVO (0.003%) 3 weeks after a first COVID-19 vaccination among 3 million vaccine recipients.4 Moreover, the RVO rate was similar after influenza
Dr Khurana spoke about this topic at AAO 2024 Retina Subspecialty Day in Chicago, US.
For citation notes, see page 46.
Rahul N Khurana MD is Chief Executive Officer and Partner at North California Retina Vitreous Associates, Mountain View, California, US. rnkhurana@gmail.com

While AI shows potential in healthcare, experts agree it requires bias mitigation and human oversight.
LAUREN BLANCHARD REPORTS
Artificial intelligence (AI) has immense potential to improve healthcare efficiency and address existing inequities. At the 2024 ESCRS Annual Congress in Barcelona, experts gathered at a BOSS (Building Our Sustainable Society) symposium, “Hidden Bias in Science,” to discuss concerns surrounding AI adoption as well as how this rapidly evolving technology can support the healthcare field.
“The biggest possibility for artificial intelligence is in the prediction or the prognosis for patients and really giving us that chance to optimise therapy, so maybe we can move toward personalised medicine,” explained Rebecca Berghorn, head of digital health at Zeiss Medical Technology. She clarified that, despite what many believe, AI’s role is not to replace healthcare professionals but to “aid and guide” them toward better outcomes.
Dalith Steiger, co-founder of Swiss Cognitive, echoed this sentiment. “Every day we have more and more devices connected, gaining intelligence and producing more data,” she said. “Because of the power of computers, we are capable of developing and implementing cognitive technologies. We’re getting more and more insights, and the more insights we have, the better we can focus on solutions.”
As AI evolves, public perception of AI is also shifting. Steiger referenced a study indicating that 75% of the population is open to using cognitive technology in their daily lives. This
finding is not consistent across cultures—as Berghorn noted, a higher percentage of people in Japan believe “AI can partly replace eye care specialists” than in Australia, reflecting different levels of trust in the technology’s capabilities.
To understand the specific concerns of healthcare professionals, Zeiss conducted a survey of 316 ophthalmologists from 11 countries to gauge their views on AI. Results revealed three main concerns: the risk of AI errors, potential misuse, and bias affecting patient outcomes.
When questioning why AI has bias, Berghorn suggests we look inward. “Humans have biases and they influence our decisions, interactions, and research, even when we’re not aware of them,” she said. “So it should come as no surprise that AI also has biases, because we tell it what to do. We are the ones bringing bias to the system.”
“Technology is not the problem; it’s us, the human being,” Steiger agreed. “We need to gather more diverse data and be conscious of the biases.”
Berghorn outlined three types of biases affecting AI in healthcare: data bias (when certain groups are under- or overrepresented in data sets), algorithmic bias (inconsistent data labelling, which can skew outcomes), and human bias, which includes automation bias (where professionals over-rely on AI).
Berghorn noted that Zeiss has established five pillars in AI development: interdisciplinary collaboration, high-quality and diverse data, compliance with international standards, advanced methodologies, and a robust global infrastructure to support AI solutions. The company’s adherence to these pillars was recently demonstrated in their development of an AI IOL calculator, which received CE approval (the European Union’s mandatory conformity marking for regulating goods sold within the European Economic Area).
Zeiss’s medical ecosystem is also instrumental in addressing biases within AI. Their health data platform integrates and stores information from diverse sources, including third-party technologies and electronic medical records, thereby supporting the development of more inclusive algorithms.
“It’s extremely important throughout the development of AI to think about having established processes and techniques to help mitigate the bias,” Berghorn explained. She emphasised the value of an interoperable, end-to-end medical ecosystem, noting that it can help support multiple AI solutions and ensures access to the extensive data available.
Berghorn stressed that prioritising transparency and encouraging healthcare professionals to understand and question how AI algorithms function can help foster a culture of accountability and collaboration with patients. “Understand, question, and get the information because you need to
understand it and discuss it with your patients to use on the full patient population,” she noted.
Both Berghorn and Steiger underscored the irreplaceable role of human expertise. “It’s important to educate doctors on the benefits of artificial intelligence, but also to understand that it is not telling you what to do,” Berghorn explained. “You make the final decision as a human. You are the one responsible for the patient and the patient’s care.”
“We have to make sure we’re not giving over the responsibility of our thinking to technology,” Steiger added. “When you look at patients and data, it always needs your gut feeling, your experience. This is something that technology is not able or capable of taking away from you.”
This discussion took place during the 2024 ESCRS Congress in Barcelona. The ESCRS BOSS programme (Building Our Sustainable Society) is a key initiative to address issues of diversity, equity, and inclusion in ophthalmology. For more information, scan the QR code.
Rebecca Berghorn can be reached at rebecca.berghorn@zeiss.com.
Dalith Steiger can be reached at dsteiger@swisscognitive.com.

ESCRS iLearn is an online learning platform, free for ESCRS members.
Visit elearning.escrs.org to access over 30 hours of interactive, assessed, and accredited e-learning content, including surgical videos, diagrams, animations, quizzes, and forums.
Step by step real-world experience shows improvement in clinical outcomes.
TIMOTHY NORRIS REPORTS
Successful implementation of new technology in the operating theatre requires preset goals, teamwork, and communication with manufacturers, advised Norbert Pesztenlehrer MD.
Dr Pesztenlehrer speaks from experience, having introduced many digital technologies into his hospital in Győr, a Hungarian city between Budapest and Vienna. He has collected objective and subjective data on the transition from the standard manual to a completely digital OR.
With more than ten thousand toric IOLs implanted since 2012, he decided to implement digital marking in 2015, first adopting the Verion system (Alcon) before implementing a 3D visualisation system to accommodate a hernia caused by bad posture. He then added an SS-OCT biometry system in 2019 and has begun using the ESCRS online calculator to increase precision.
Better visual quality must be the main destination, he said, emphasising the Hippocratic oath of improving patient health above all else. For this reason, everything must focus on improving surgical performance, step by step. Implementing technology for this purpose requires an easy-to-learn workflow, with reliable features like proper device interconnectivity that may reduce the rate of error—human and software alike.
As Dr Pesztenlehrer experienced, this is not an easy task for the producer. New technology must comply with all sorts of regulations—the privacy and security issues requested by the European guidelines and all the national and local regulations. While this is a problem of the manufacturer, it is something surgeons must navigate.
Dr Pesztenlehrer further explained implementing digital technology into a professional practice is now thoroughly guided by companies, from practice to organisation up to control and confirmation of changes. However, he stressed it is important to change one or two variables in the process, check the results, keep track of the processes, and optimise workflow.
During the presentation, he highlighted how much space an open platform can leave for optimisation, especially with the extremely reliable software manufacturers provide. He observed there is always room for collaboration with the company to develop a simpler, faster, and more reliable method, with the addition of a seamless integration of many systems. As a surgeon, he admitted he and colleagues are not dealing with an electric car “that you get in and push a pedal,” but with something that requires regular training and self-improvement.
The change is a digital revolution that may find some resistance among baby boomers and Gen X, but high acceptance among millennials and Gen Z, he said.
To further support the benefits of this implementation, Dr Pesztenlehrer showed some data from his surgical experience. Starting with the manual implantation of the 2013–2015 period, mean postoperative astigmatism was between 0.48 and 0.39 D. With the implementation of digital marking, Barrett formulas, a 3D system, and an SS-OCT, the average gradually lowered to 0.07 D of cylinder.
The implementation of 3D and SS-OCT showed the same positive trend of subjective data. There is a constant improvement, he observed.
Finally, for success with new technology, he stressed having a motivated team—adding pivotal technological support from the manufacturers can trigger that enthusiasm, setting the course for further development and innovation.
Dr Pesztenlehrer spoke in a session on new technology at the 2024 ESCRS Congress in Barcelona.
Norbert Pesztenlehrer MD is Head of Ophthalmology at Petz County Hospital, Győr, Hungary. pesztenlehrern@gmail.com



Have your knowledge and expertise in cataract and refractive surgery tested and o icially acknowledged by sitting the EBO-ESCRS Subspecialty Exam. Successful candidates will be awarded the Fellow of the EBO Subspecialty Cataract & Refractive Surgery Diploma (FEBOS-CR). This diploma is recognised as proof of advanced knowledge and competence in this field
The exam will take place at the ESCRS Annual Congress in Copenhagen. Applications are now open.
Hidden biases in science impact careers and patient care.
LAUREN BLANCHARD REPORTS
Diversity, equity, and inclusion (DEI) are hot topics in many fields, but why are they so important in science? This was the question posed by Sotiria Palioura MD, PhD at an ESCRS BOSS “Hidden Bias in Science” symposium.
“After all, we’re trained to be objective and to provide equal treatment to all, irrespective of their background, gender, or socioeconomic status. Yet we’re all part of a system that creates unconscious biases, and this starts early in life.”
Dr Palioura cited the “Draw-A-Scientist” studies, which show children overwhelmingly depict scientists as male, shaping how girls see themselves in scientific roles. This bias can extend beyond childhood perceptions: “Just five years ago, a Google search for famous scientists showed men with only one woman, Marie Curie, and no person of colour.”
In another study, researchers evaluated identical resumes with the names John, Jamal, or Jennifer for a postdoc position. Both male and female reviewers rated John as more competent, hireable, and a stronger leader than Jennifer and Jamal, who were both offered lower salaries.
This pattern persists in clinical practice. While 46% of residents are women, only 25% become full professors. Disparities are worse for underrepresented ethnic groups, who make up 35% of the US population but only 7% of full professors.
While 46% of residents are women, only 25% become full professors.
In ophthalmology, women hold fewer than 20% of department chair positions and are fewer than 40% of residency programme directors. As of 2019, ophthalmology was one of five specialties with no female editor-in-chief among its top 10 journals. Women are senior authors of less than 30% of publications in these journals while men dominate invited editorials by more than 75%.
Women receive less grant funding, hold half as many industry partnerships as men, handle fewer surgical cases, and earn 42% less than men, even after adjusting for age, location, and specialty.
These inequities affect patient care too. It wasn’t until 1993 that law mandated the inclusion of women in NIH research. “So, for decades, the research we relied on to diagnose disease and guide patient treatment has been based on only half the patient population.”
Steps towards inclusivity
“Now that we’ve diagnosed the problem, we need to come up with the treatment plan,” Dr Palioura continued. “There’s

evidence that incredible breakthroughs are the result of people from different fields coming together to find a place for their ideas to meet, collide, and build on each other.
“When building your team—whether hiring staff, faculty, trainees, or students—you should look for diversity of expertise, as it’s a key factor for team success.”
And what’s the solution to fixing inequities with gender and underrepresented groups? “We need to cite them, invite them to speak, nominate them for awards, mentor, and support people outside of our usual network. We must recognise unconscious biases and identify barriers,” she stressed.
“Now that you are aware of these issues, you’re not going to be part of the problem—you’re going to be part of the solution.”
Dr Palioura spoke during the 2024 ESCRS Congress in Barcelona.
The ESCRS BOSS programme (Building Our Sustainable Society) is a key initiative to address the issues of diversity, equity, and inclusion in ophthalmology. For more information, scan the QR code.
Sotiria Palioura MD, MSc, PhD is a US-trained Surgeon Ophthalmologist from Greece who is certified both by the American and the European Boards of Ophthalmology.

Ophtec announced it has received CE Mark approval for its Artiplus phakic IOL for young presbyopes. Based on the Artiflex platform, the iris-fixated lens has a unique segmented optic that uses Continuous Transitional Focus (CTF) technology to generate multiple elongated focal points to provide smooth transitions from near to distance vision with minimal glare and halos.
ophtec.com
The FDA has officially accepted Aldeyra Therapeutics’ resubmitted new drug application (NDA) for reproxalap in treating dry eye disease. The FDA has set a Prescription Drug User Fee Act (PDUFA) target date of 2 April 2025. Reproxalap is a novel small-molecule drug that inhibits reactive aldehyde species (RASP), which are elevated in a variety of inflammatory diseases. In clinical trials, topical treatment with reproxalap demonstrated reduced signs and symptoms of dry eye disease with no significant safety concerns and mild, transient eye irritation reported as the most common effect.
aldeyra.com
Alkeus Pharmaceuticals announced on 18 November 2024 that the US FDA had granted rare paediatric disease and fast-track designations to gildeuretinol (ALK001), its oral therapy candidate for Stargardt disease. Interim data from the Phase II TEASE-3 study showed that early-stage Stargardt patients treated with gildeuretinol had no disease progression and remained asymptomatic while on therapy for two and six years. ALK-001 is designed to reduce the dimerization of vitamin A and thereby prevent retinal degeneration. The novel molecule is identical to vitamin A except for the replacement of three hydrogen atoms by deuterium atoms.
alkeuspharma.com
Eyenovia has discontinued its Phase III CHAPERONE trial of low-dose atropine spray, MicroPine, in paediatric myopia after meeting its primary endpoint of less than 0.5 dioptres of myopia progression over three years.
eyenovia.com
The FDA has granted authorisation to LumiThera, allowing the company to market its Valeda Light Delivery System for dry age-related macular degeneration. This approval, made under the de novo authorisation pathway, makes Valeda the first FDAauthorised device to treat vision loss in patients with dry AMD. The Valeda therapy uses photobiomodulation (PBM), a noninvasive, light-based technology to stimulate photoreceptor mitochondrial activity. In the US LIGHTSITE III trial, the Valeda treatment met its primary endpoint, showing both safety and efficacy in improving and maintaining visual acuity over two years.
lumithera.com
Sandoz announced in November 2024 that the European Commission (EC) had granted marketing authorisation for Afqlir (Enzeevu, aflibercept), an Eylea biosimilar for the treatment of neovascular age-related macular degeneration, macular oedema following retinal vein occlusion, diabetic macular oedema, and myopic choroidal neovascularisation. The announcement follows the positive recommendation for Samsung Bioepis and Biogen’s aflibercept biosimilar, Opuviz, from Europe’s Committee for Medicinal Products for Human Use in September 2024 and the EC’s approval of Biocon Biologics’ first biosimilar to Eylea, Yesafili, in September 2023.

Experience in phacoemulsification appears to speed a surgeon’s acquisition of skill in manual small-incision cataract surgery (MSICS), according to the findings of a prospective controlled experimental study. The study involved 29 residents or specialists in ophthalmology with no prior MSICS experience or training. Among the participants, 11 were proficient in phacoemulsification surgery on the EyeSi simulator and 18 had no prior extensive experience with the simulator or in phacoemulsification as a primary surgeon. The study showed that, when assessed with HelpMeSee’s standardised simulator scoring system, the group with previous phacoemulsification experience had a significantly higher pass rate (72%) on their MSICS performance than the inexperienced group (22%). The subanalysis of individual modules showed the significant differences were exclusive to the capsulorhexis and cortex removal modules.
AQD Le, et al. “Phacoemulsification to manual small-incision cataract surgery: transfer of skills study in a simulated environment,” 50(12): 1202–1207.
CATARACT SURGERY EFFICIENCY
Integrating a digital workflow into a cataract surgery clinic can significantly reduce the overall time and resources required to plan and perform cataract procedures, according to a prospective time and motion study. The study involved two clinics and analysed the cataract surgery workflow time in 85 patients. Both clinics first used their current electronic medical record (EMR) system in a series of patients, followed by a digital workflow system with integrated data management, a surgical planner, and data transfer to the operating room for a second set of patients. The study showed that integrating a digital workflow into an existing EMR workflow reduced the mean time for preoperative measurements by 25.3%, surgical planning by 55.1% (P = .008), and surgical procedures by 22.6%. In addition, the digital workflow system significantly reduced the number of support staff required per procedure.
N Shetty, et al. “Effect of digital cataract workflow on time and resource efficiencies in cataract surgery: time and motion study,” 50(12): 1208–1214.
NEW ALGORITHM PROVIDES ENHANCED DETECTION OF FORME FRUSTE KERATOCONUS
A new machine learning algorithm appears to discriminate eyes with forme fruste keratoconus (FFKC) from normal eyes with greater sensitivity and equal specificity compared to the AI-derived Ectasia Screening Index (ESI) score provided by the SS-OCT CASIA 2, a retrospective case-control study suggests. To develop the algorithm, the study’s authors used SS-OCT CASIA topography data from 108 eyes with keratoconus, 88 with FFKC, and 162 with normal corneas. After analysing and processing the data, they used random forest (RF) and logistic regression (LR) machine learning models to develop a multiclass classifier for automated early keratoconus detection. The researchers found that for an FFKC diagnosis, the sensitivity of the LR model was 100% and 84% for the RF model, compared to 28% for the ESI. The LR model and ESI specificity were 100% and the RF model specificity was 90%.
E Mourgues, et al. “Forme fruste keratoconus detection with OCT corneal topography using artificial intelligence algorithms,” 50(12): 1247–1253.
Explore IOL solutions and demystify common misunderstandings with insights into a refractive future that offers more improved postoperative outcomes—exclusively on the ESCRS website.
ESCRS Research: Past, Present, and Future
Page 11
1. Endophthalmitis Study Group. J Cataract Refract Surg, Jun; 33(6): 978–988.
2. Wielders, et al. Cataract Refract Surg, 2018 Apr; 44(4): 429–439.
3. ESCRS: Influence of posterior vitreous detachment on retinal detachment after lens surgery in myopic eyes (MYOPRED). 2024. www.escrs.org/education/research-portals/ influence-of-posterior-vitreous-detachment-on-retinal-detachment-after-lens-surgery-in-myopic-eyes-myopred/
4. ESCRS Registries. 2021. https://registries.escrs.org/
Phaco Alternative Debuts in US
Page 22
1. Beniz LA, Chatzea MS, Zarei-Ghanavati S, et al. “Finger-Controlled Nonultrasonic Lens Extractor,” J Cataract Refract Surg, 9 Oct 2024. doi:10.1097/j.jcrs.0000000000001561.
Treating Myopia, Inside and Outside
Page 26
1. JAMA Ophthalmol, 2023 Aug; 141(8): 756–765.
Cataract Surgery in Eyes with Corneal Disease
Page 30
1. Stern B, Saad A, Flamant R, Joannes L, Gatinel D. “Intra-observer and inter-observer variability of intraocular lens measurements using an interferometry metrology device,” Diagnostics, 2024; 14(2): 216.
2. Zéboulon P, Ghazal W, Gatinel D. “Corneal edema visualization with optical coherence tomography using deep learning: proof of concept,” Cornea, 2021; 40(10): 1267–1275.
Corneal Cross-Linking (CXL): Leaving the Epithelium On Page 32
1. Vinciguerra R, Legrottaglie EF, Tredici C, Mazzotta C, Rosetta P, Vinciguerra P. “Transepithelial Iontophoresis-Assisted Cross Linking for Progressive Keratoconus: Up to 7 Years of Follow Up.” J Clin Med, 28 Jan 2022; 11(3). doi:10.3390/ jcm11030678
2. Mastropasqua L, Nubile M, Calienno R, et al. “Corneal cross-linking: intrastromal riboflavin concentration in iontophoresis-assisted imbibition versus traditional and transepithelial techniques,” Am J Ophthalmol, Mar 2014; 157(3): 623–30 e1. doi:10.1016/j.ajo.2013.11.018
3. Hafezi F. “Corneal Cross-Linking: Epi-On,” Cornea, 2022; 41(10): 1203–1204. doi:10.1097/ICO.0000000000003075
4. Soeters N, Wisse RP, Godefrooij DA, Imhof SM, Tahzib NG. “Transepithelial versus epithelium-off corneal cross-linking for the treatment of progressive keratoconus: a randomized controlled trial,” Am J Ophthalmol, 2015; 159(5): 821-8 e3. doi:10.1016/j.ajo.2015.02.005
5. Torres-Netto EA, Kling S, Hafezi N, Vinciguerra P,
Randleman JB, Hafezi F. “Oxygen Diffusion May Limit the Biomechanical Effectiveness of Iontophoresis-Assisted Transepithelial Corneal Cross-linking,” J Refract Surg, 2018; 34(11): 768–774. doi:10.3928/1081597X-20180830-01
6. Mazzotta C, Pandolfi A, Ferrise M. “Progressive high-fluence epithelium-on accelerated corneal crosslinking: a novel corneal photodynamic therapy for early progressive keratoconus,” Front Med (Lausanne), 2023; 10: 1198246. doi:10.3389/fmed.2023.1198246
7. Rajpal RK, Wisecarver CB, Williams D, et al. “LASIK Xtra® Provides Corneal Stability and Improved Outcomes,” Ophthalmol Ther, 2015; 4(2): 89–102. doi:10.1007/s40123015-0039-x
8. Hira S, Klein Heffel K, Mehmood F, Sehgal K, Felix De Farias Santos AC, Steuernagel Del Valle G. “Comparison of refractive surgeries (SMILE, LASIK, and PRK) with and without corneal crosslinking: systematic review and meta-analysis,” J Cataract Refract Surg, 2024; 50(5): 523–533. doi:10.1097/j.jcrs.0000000000001405
9. Dong R, Zhang Y, Yuan Y, Liu Y, Wang Y, Chen Y. “A prospective randomized self-controlled study of LASIK combined with accelerated cross-linking for high myopia in Chinese: 24-month follow-up,” BMC Ophthalmol, 2022; 22(1): 280. doi:10.1186/s12886-022-02491-y
10. Kontadakis GA, Kankariya VP, Tsoulnaras K, Pallikaris AI, Plaka A, Kymionis GD. “Long-Term Comparison of Simultaneous Topography-Guided Photorefractive Keratectomy Followed by Corneal Cross-linking versus Corneal Cross-linking Alone,” Ophthalmology, 2016; 123(5): 974–983. doi:10.1016/j.ophtha.2016.01.010
11. Kanellopoulos AJ. “Management of progressive keratoconus with partial topography-guided PRK combined with refractive, customized CXL—a novel technique: the enhanced Athens protocol,” Clin Ophthalmol, 2019; 13: 581–588. doi:10.2147/OPTH.S188517
12. Kymionis GD, Grentzelos MA, Karavitaki AE, et al. “Transepithelial Phototherapeutic Keratectomy Using a 213-nm Solid-State Laser System Followed by Corneal Collagen Cross-Linking with Riboflavin and UVA Irradiation,” J Ophthalmol, 2010; 146543. doi:10.1155/2010/146543
13. Grentzelos MA, Liakopoulos DA, Siganos CS, Tsilimbaris MK, Pallikaris IG, Kymionis GD. “Long-term Comparison of Combined t-PTK and CXL (Cretan Protocol) Versus CXL with Mechanical Epithelial Debridement for Keratoconus,” J Refract Surg, 2019; 35(10): 650–655. doi:10.3928/108 1597X-20190917-01
14. Nattis A, Donnenfeld ED, Rosenberg E, Perry HD. “Visual and keratometric outcomes of keratoconus patients after sequential corneal crosslinking and topography-guided surface ablation: Early United States experience,” J Cataract Refract Surg, 2018; 44(8): 1003–1011. doi:10.1016/j. jcrs.2018.05.020
15. Nattis AS, Rosenberg ED, Donnenfeld ED. “One-year visual and astigmatic outcomes of keratoconus patients
following sequential crosslinking and topographyguided surface ablation: the TOPOLINK study,” J Cataract Refract Surg, 2020; 46(4): 507–516. doi:10.1097/j. jcrs.0000000000000110
16. Rechichi M, Mazzotta C, Oliverio GW, et al. “Selective transepithelial ablation with simultaneous accelerated corneal crosslinking for corneal regularization of keratoconus: STARE-X protocol,” J Cataract Refract Surg, 2021; 47(11): 1403–1410. doi:10.1097/j.jcrs.0000000000000640
17. Shetty R, Vunnava K, Khamar P, Choudhary U, Sinha Roy A. “Topography-Based Removal of Corneal Epithelium for Keratoconus: A Novel and Customized Technique,” Cornea, 2018; 37(7): 923–925. doi:10.1097/ ICO.0000000000001580
18. Randleman JB, Khandelwal SS, Hafezi F. “Corneal cross-linking,” Surv Ophthalmol, 2015; 60(6): 509–523. doi:10.1016/j.survophthal.2015.04.002
19. Kanellopoulos AJ, Dupps WJ, Seven I, Asimellis G. “Toric topographically customized transepithelial, pulsed, very high-fluence, higher energy and higher riboflavin concentration collagen cross-linking in keratoconus,” Case Rep Ophthalmol, 2014; 5(2): 172–180. doi:10.1159/000363371
20. Seiler TG, Fischinger I, Koller T, Zapp D, Frueh BE, Seiler T. “Customized Corneal Cross-linking: One-Year Results,” Am J Ophthalmol, 2016; 166: 14–21. doi:10.1016/j. ajo.2016.02.029
21. Nordstrom M, Schiller M, Fredriksson A, Behndig A. “Refractive improvements and safety with topography-guided corneal crosslinking for keratoconus: 1-year results,” Br J Ophthalmol, 2017; 101(7): 920–925. doi:10.1136/bjophthalmol-2016-309210
22. Cassagne M, Pierne K, Galiacy SD, Asfaux-Marfaing MP, Fournie P, Malecaze F. “Customized Topography-Guided Corneal Collagen Cross-linking for Keratoconus,” J Refract Surg, 2017; 33(5): 290–297. doi:10.3928/1081597X-20170201-02
23. Mazzotta C, Sgheri A, Bagaglia SA, Rechichi M, Di Maggio A. “Customized corneal crosslinking for treatment of progressive keratoconus: Clinical and OCT outcomes using a transepithelial approach with supplemental oxygen,” J Cataract Refract Surg, 2020; 46(12): 1582–1587. doi:10.1097/j.jcrs.0000000000000347
24. Hafezi F. “PACE (2nd generation customized CXL),” presented at International CXL Experts’ Meeting, 10 Dec 2022; Zurich, Switzerland.
25. Tabibian D, Mazzotta C, Hafezi F. “PACK-CXL: Corneal cross-linking in infectious keratitis,” Eye Vis (Lond), 2016; 3: 11. doi:10.1186/s40662-016-0042-x
26. Raiskup F, Herber R, Lenk J, Pillunat LE, Spoerl E. “Crosslinking with UV-A and riboflavin in progressive keratoconus: From laboratory to clinical practice—developments over 25 years,” Prog Retin Eye Res, 2024: 101276. doi:10.1016/j.preteyeres.2024.101276

27. Hafezi F, Richoz O, Torres-Netto EA, Hillen M, Hafezi NL. “Corneal Cross-linking at the Slit Lamp,” J Refract Surg, 2021; 37(2): 78–82. doi:10.3928/1081597X-20201123-02
28. Hafezi F, Hosny M, Shetty R, et al. “PACK-CXL vs. antimicrobial therapy for bacterial, fungal, and mixed infectious keratitis: a prospective randomized phase 3 trial,” Eye Vis (Lond), 2022; 9(1): 2. doi:10.1186/s40662-021-00272-0
29. Lu NJ, Koliwer-Brandl H, Gilardoni F, et al. “The Antibacterial Efficacy of High-Fluence PACK Cross-Linking Can Be Accelerated,” Transl Vis Sci Technol, 2023; 12(2): 12. doi:10.1167/tvst.12.2.12
30. Lu NJ, Koliwer-Brandl H, Hillen M, Egli A, Hafezi F. “High-Fluence Accelerated PACK-CXL for Bacterial Keratitis Using Riboflavin/UV-A or Rose Bengal/Green in the Ex Vivo Porcine Cornea,” Transl Vis Sci Technol, 2023; 12(9): 14. doi:10.1167/tvst.12.9.14
31. Hafezi F, Torres-Netto EA, Hillen MJP. “Re: Prajna et al.: Cross-Linking-Assisted Infection Reduction: a randomized clinical trial evaluating the effect of adjuvant cross-linking on outcomes in fungal keratitis (Ophthalmology, 2020; 127: 159–166),” Ophthalmology, Jan 2021; 128(1): e6. doi:10.1016/j.ophtha.2020.07.011
32. Hafezi F, Messerli J, Lu N, Aydemir E, Hillen M. “Successful Combination of Riboflavin/UV-A and Rose Bengal/ Green Light PACK Cross-Linking in Acanthamoeba Keratitis,” presented at European Society of Cataract and Refractive Surgeons Annual Meeting, 8–12 Sept 2023; Vienna, Austria.
33. Hafezi F, Gatzioufas Z, Seiler TG, Seiler T. “Corneal collagen cross-linking for Terrien marginal degeneration,” J Refract Surg, 2014; 30(7): 498–500. doi:10.3928/108159
7X-20140527-02
34. Spadea L. “Corneal collagen cross-linking with riboflavin and UVA irradiation in pellucid marginal degeneration,” J Refract Surg, 2010; 26(5): 375–377. doi:10.3928/108159
7X-20100114-03
35. Hafezi F, Torres-Netto EA, Randleman JBH, Nikki L, Mazzotta C, Ambrósio R, Kollros L. “Corneal Cross-linking
for Keratoglobus Using Individualized Fluence,” Journal of Refractive Surgery Case Reports, 2021; 1(1). doi:10.3928/ jrscr-20210527-01
36. Kwok SJJ, Kuznetsov IA, Kim M, Choi M, Scarcelli G, Yun SH. “Selective two-photon collagen crosslinking in situ measured by Brillouin microscopy,” Optica, 2016; 3(5): 469–472. doi:10.1364/OPTICA.3.000469
37. Batista A, Breunig HG, Hager T, Seitz B, Konig K. “Early evaluation of corneal collagen crosslinking in ex-vivo human corneas using two-photon imaging,” Sci Rep, 2019; 9(1): 10241. doi:10.1038/s41598-019-46572-3
38. Chang L, Zhang L, Cheng Z, et al. “Effectiveness of collagen cross-linking induced by two-photon absorption properties of a femtosecond laser in ex vivo human corneal stroma,” Biomed Opt Express, 2022; 13(9): 5067–5081. doi:10.1364/BOE.468593
Effect of COVID-19 and Vaccine on Retinal Disease
Page 35
1. Lum F, Li C, Khurana RN. “Retinal vascular occlusions did not increase since the start of the coronavirus disease 2019 pandemic,” Ophthalmol Retina, 2024; 8(4): 415–417.
2. Al-Moujahed A, Boucher N, Fernando R, et al. “Incidence of retinal artery and vein occlusions during the COVID-19 pandemic,” Ophthalmic Surg Lasers Imaging Retina, 2022; 53(1): 22–30.
3. Park HS, Lee NK, Lee CS, et al. “Retinal artery and vein occlusion risks after coronavirus disease 2019 or coronavirus disease 2019 vaccination,” Ophthalmology, 2024; 131(3): 322–332.
4. Dorney I, Shaia J, Kaelber DC, Talcott KE, Singh RP. “Risk of new retinal vascular occlusion after mRNA COVID-19 vaccination within aggregated electronic health record data,” JAMA Ophthalmol, 2023; 141(5): 441–447.
5. Singh RB, Parmar UPS, Gupta R, et al. “Retinal vascular occlusion following SARS-CoV-2 vaccination: A VAERS database analysis,” Ophthalmol Sci, 2023; 4(1): 100354.
Contact: YO@ESCRS.org YO.ESCRS.org



February 28–March 2
29th ESCRS Winter Meeting
Athens, Greece
April 25–28
ASCRS
Los Angeles, US
May 23–25
EuCornea
Prague, Czech Republic
June 7–9
European Society of Ophthalmology (SOE)
Lisbon, Portugal
June 12–14
2nd World Keratoconus Congress (WKC 2025)
Athens, Greece
September 4–7
EURETINA
Paris, France
September 12–16
2025 ESCRS Congress
Copenhagen, Denmark
September 25–28
German Ophthalmology Society
Berlin, Germany
October 18–20
American Academy of Ophthalmology
Orlando, Florida, US

25 Apr


28 Feb
23 May

12 Sept 7 Jun

We are a society of surgeons who specialise in improving vision and restoring clarity. Since 1991, ESCRS has promoted the education and research of implant and refractive surgery. With over 7,500 members from 130 countries worldwide, ESCRS is a vital global platform for the field of ophthalmology.