Congress sessions to hold the key to a promising ophthalmic
Eyes on the Horizon CORNEA








INVITATION

9th September 2024, Monday 10:30-10:50




Maximizing Patient Satisfaction: Custom Matching of Wavefront-linking EDoF and Trifocal Intraocular Lenses


















































Valeriii i S Serdiiuk Johann Kruger Johaannn





Booth #7.D20












































ELON & ELON Toric Wavefront Linking technology 1,2

Hydrophobic Preloaded To
























































Precise. Safe. Reversible. 10-14 Sf Enhanced Trifocal Performance 3,4 Superior Contrast Sensitivity 5-9



Scan the QR!









Reducing Ophthalmic Surgical Waste through Electronic Instructions
In an effort to reduce waste associated with ophthalmic surgery, four organisations—ESCRS, the American Academy of Ophthalmology, the American Society of Cataract and Refractive Surgery, and EyeSustain—have agreed to work with industry to reduce the use of the multilingual paper in-struction inserts that accompany surgical products.
The global healthcare system is a major contributor to waste and accounts for 4.4% of global greenhouse gases. Ophthalmic procedures are among the most common in medicine; almost 30 million cataract surgeries are performed globally each year. As populations continue to age in most countries, ophthalmic procedural volumes are expected to increase. This gives ophthalmology a unique opportunity to reduce unnecessary waste and, thus, carbon emissions.
Regulatory agencies, such as the European Union Medical Device Regulation (MDR) and the US Food and Drug Administration (FDA), have required manufacturers to provide detailed instructions for use (IFU) to guide safe and proper use of surgical devices and products. The IFU describe how to use the product and may include information about applications, component parts, indications and contraindications, precautions, warnings, study results, and adverse events.
In ophthalmic surgery, paper IFU accompany intraocular lenses (IOLs), IOL insertion cartridges, ophthalmic viscosurgical device syringes, dropper bottles of saline, irrigating solution, and phacoemulsification tips and sleeves. Although some IFU may be printed on the package exterior, most are separately supplied as a printed booklet or folded handout within the product package.
Paper IFU contribute significantly to unnecessary waste and heighten the adverse environmental impact from ophthalmic surgery. Compared to an e-IFU, the disadvantages of a printed IFU include smaller print, the inability to immediately update IOL IFUs stored in operating rooms on consignment, and difficulty accessing the information in the clinic when the IOL model and power are selected.
“We recommend that surgical manufacturers replace paper IFU with e-IFU whenever possible for ophthalmic surgical products,” said a statement from the EyeSustain Task Force on e-IFU. “Given the large volume of ophthalmic surgeries, transitioning from print to e-IFU will significantly reduce waste while making the same information readily accessible to surgical teams. To understand the potential benefits and disadvantages of e-IFU for virtually all ophthalmic surgical products, it is helpful to consider the example of IOLs.”
Because of the extremely high volume of ophthalmic devices used in procedures such as cataract surgery, implementing e-IFU is a straightforward way for manufacturers to reduce unnecessary waste and carbon emissions.
“We recommend that the ophthalmic surgical manufacturing industry move exclusively to e-IFU, initially prioritizing those products routinely used in high volume, such as IOLs, IOL cartridges, and OVD,” the EyeSustain statement said.
The Task Force includes Emily Schehlein MD, John Hovanesian MD, Audrey Talley Rostov MD, Aakriti Garg Shukla MD, Oliver Findl MD, and David F Chang MD.
FLACS Continues to Evolve
What is the place of femto in modern cataract surgery?
Femtosecond laser-assisted cataract surgery (FLACS) is a relative newcomer, with the first systems only becoming available in 2008. Since that time, both the hardware and software have continued to evolve. What is the place of FLACS among the options available to ophthalmic surgeons? Which patients are likely to benefit the most? EuroTimes asked Professor Burkhard Dick MD, PhD for an update.
What is your current use of FLACS?
I currently perform femtosecond laser cataract surgery on a wide range of patients. These include uncomplicated cases, people who want good postoperative visual acuity and high safety standards, and patients with complex situations (see below)—even the youngest with paediatric cataracts. We have shown in a number of studies1 , 2 how safe it is to perform laser capsulotomy in young children—not only anterior capsulotomy but also primary posterior capsulotomy (PPC), which we believe is an absolutely necessary precaution to prevent posterior capsule opacification, which tends to be fulminant in children. The predictability and accuracy of the laser in performing capsulotomies are essential in these patients who require long-term care and monitoring.
What are the known (proven) and potential advantages of FLACS?
In short, it is safe and effective. It has several advantages, although it has to be said that laser cataract surgery (LCS) is always compared to one of the most successful procedures in all of medicine, phacoemulsification. That really is a high bar that does not leave much room for improvement. And yet, the latest meta-analysis suggests that less ultrasound energy results in less corneal tissue damage, which is particularly important in the long term.3 There is greater precision and the prospect of less damage to ocular structures.
Many femtosecond laser platforms now include advanced imaging systems that provide real-time, high-resolution images of the eye to aid precise surgical planning and execution. As cataract surgery today is always refractive surgery, it cannot be overstated that femtosecond laser surgery instils a culture and strategy among surgeons to manage astigmatism. The technology allows precise corneal incisions to correct pre-existing astigmatism. When the astigmatism is not corrected by a corneal procedure but by a lens-based procedure, a perfectly centred and sized capsulotomy allows highly accurate IOL placement, which is invaluable when implanting toric IOLs.
In what situations is FLACS clearly indicated (preferred)?
Earlier, I used the term ‘all-comers approach’ to characterise the potential of femtosecond laser-assisted cataract surgery. In my opinion (more than 13,000 procedures later), there is no need to reconsider. The success rate of LCS in uncomplicated cases is convincing. But so are patients with a history of
systemic alpha-blockers, zonular instability, or pupils less than 6 mm—to name but a few conditions that can be a nightmare for both patient and surgeon. These challenging cases are probably the patients now thought to benefit most from LCS. It is the much lower impact on the corneal endothelium— compared to the application of ultrasound energy during phacoemulsification—that makes LCS so well suited for eyes with Fuchs’ degeneration and similar conditions.
LCS is not only possible in complex cases—it is often preferable, at least in my experience. Consider mature or ‘white’ cataracts. The often immense pressure inside the capsule (which can lead to an explosive rupture when touched and thus to the dreaded ‘Argentinian flag syndrome’) can be assessed by the laser platform’s OCT. The presence of intracapsular pressure can convince the surgeon to start the procedure with mini-capsulotomies (which we have performed many times and described in published work)3,4 and thus manage a potentially dangerous situation. In very advanced cataracts (now less common in developed countries), the laser pre-fragments the dense and hard lens, making it easier to remove the fragments with less ultrasound energy.
In patients with relatively dense cataracts and low preoperative endothelial cell counts, a recent meta-analysis has documented the advantages of LCS in terms of lower ultrasound energy, less endothelial cell loss, and, in the safety analysis, a lower incidence of posterior capsule tear with an OR (odds ratio) of 0.29—just to name a few parameters.5
I would also like to mention patients with Marfan syndrome who, like patients with zonular weakness for other reasons such as PEX, have benefited enormously from the precision and reduced ultrasound energy with LCS. Since the femtosecond laser does not require zonular support for capsulotomy and exerts minimal stress on the zonules during reduced ultrasound application, its advantage in treating zonular weakness and subluxated cataracts is obvious.
How would you describe the training and learning curve? Is there a perception that training (and the learning curve) are an obstacle to FLACS uptake? Not at all. Every first step looks difficult, no matter what you are starting with, and surgical techniques are certainly no exception. As with any other instrument in ophthalmic surgery, a novice needs an experienced teacher and coach to guide them. The learning curve for performing LCS is twofold: the surgeon needs to learn how to use the laser and familiarise themselves with the settings, and they also need to change the way they work. There are steps the surgeon needs to be aware of as the cortex has been truncated at the capsulotomy edge, and there may also be intralenticular or retro-lenticular gas. Nevertheless, the learning curve is not particularly daunting. In my experience, a talented surgeon can master it after 50 procedures. Recently, the authors of a meta-analysis concluded that “even in the first cases of laser surgery, complications are rare.”5 Tell
that to the novices and their trainers—in vascular surgery, plastic surgery—in any field of interventional medicine!
Are there recent developments in FLACS technology that address prior limitations not reflected in older studies evaluating its use?
First, it is important to note that the quality of recent cuts has been significantly improved by adapted settings based on controlled studies. A recent addition to the laser platform’s features is the direct import of preoperative biometry and other relevant data into the laser system, where the toric alignment calculator adapts to the surgeon’s preferences for total astigmatism and SI astigmatism with automatic cyclorotation compensation. The integrated arcuate incision (AI) nomograms are customisable (e.g., Donnenfeld and Stevens nomograms) and automatically calculate the AI parameters.
The first generation of laser platforms were quite bulky and very sensitive to room temperature. Smaller, more mobile, and less demanding systems are now available. In addition, some ancillary materials have been developed, such as a special smaller interface for use in paediatric cataract surgery. Treating astigmatism with arcuate incisions is far superior to any form of manual keratotomy—humans can’t control depth and position as perfectly as the laser can. And the ability to make intrastromal incisions is unique to the femtosecond laser.
Having said that, am I happy with the way the technology is developing? Absolutely not. The manufacturers—or, to be fair, some manufacturers—have not contributed to further improvements to the extent I hoped when LCS was introduced.
Are there forthcoming developments that could favour its wider use?
Biomorphometric detection and capsule marker use are being introduced. They are far superior to anything we have seen in the alignment of toric IOLs; there are absolutely no parallactic errors. Alignment can be checked, even months after surgery. Alternatively, the laser can place markers in the cornea to guide the surgeon when making arcuate incisions. Of course, studies without this technology show no difference. Patient safety in these procedures is unsurpassed, and iris recognition makes it almost impossible to treat the wrong eye.
A whole new generation of IOLs is being introduced that would probably not have been developed without LCS. These designs make the most of the perfectly cut and centred capsulotomy the laser performs and can be placed with high accuracy to benefit the patient’s vision. Examples include the bag-in-the-lens (BIL) IOL created by Marie-José Tassignon, the so-called Femto IOL, and the lens named after Samuel Masket, who designed it specifically to reduce negative dysphotopsia.
Other innovations we will see include (even) faster laser systems, fully three-dimensional treatment configuration on all systems, advanced iris recognition, and the use of the Helix laser.
Is there anything else about FLACS you want to mention?
Most of the criticism of LCS has not really been directed at its medical performance and documented results. How could this be? LCS is extremely safe, and the rate
of posterior capsule rupture (used by some authors as an argument against LCS) is less than 1%, according to recent randomised controlled trials.4,5 Postoperative visual acuity is good, and patient satisfaction is high. The main criticism is the cost of the procedure. There is no doubt LCS is currently more expensive than routine phacoemulsification. There is definitely room for improvement. It can be argued that once the cost of the laser machine and disposables is significantly reduced and accepted into routine practice, it could lead to a new era of refractive cataract surgery and a higher rate of premium lens implantation.
Much has been made of the potential for anterior capsule rupture during or after laser capsulotomy, at the beginning of LCS. This cannot be emphasised enough: The rate of anterior capsule rupture is very low and similar to manual surgery.
What no one talks about, however, is that in the event of a posterior capsule rupture and the need for sulcus implantation, an optimal capsulotomy for the fixation of the optic (optic capture) can be performed perfectly (posteriorly or anteriorly), depending on the situation.
Let me summarise: LCS is now a technology that can be tailored to the individual patient’s anatomy and specific cataract and refractive situation. We have been talking about personalised medicine since we were in medical school. With femtosecond laser-assisted cataract surgery, personalised patient care has become a reality—with functional results that would be the envy of any other medical discipline.

H Burkhard Dick MD, PhD is Professor of Ophthalmology and Chairman, Ruhr University Eye Hospital Bochum, Bochum, Germany. He is also Secretary of the ESCRS. burkhard.dick@kk-bochum.de
Scan the QR code to see the original letter to the editor.
Literature
1. Alio JL, Dick HB, Osher RO. Cataract Surgery. Advanced techniques for complex and complicated cases. Springer, Cham (Switzerland), 2022.
2. Dick HB, Gerste RD, Schulz T. Femtosecond Laser Surgery in Ophthalmology. Thieme (New York), 2018.
3. Chen DZ, Chee SP. “Femtosecond laser-assisted cataract surgery for complex cataracts – A review,” Indian J Ophthalmol, 2024; 72(5): 629–936.
4. Levitz LM, Dick HB, Scott W, et al. “The Latest Evidence with Regards to Femtosecond Laser-Assisted Cataract Surgery and Its Use Post 2020,” Clinical Ophthalmology. 2021;15: 1357–1363.
5. Pichardo-Loera NS, Corredor-Ortega C, Castro-Monreal MA, et al. “Femtosecond laser-assisted cataract surgery versus conventional phacoemulsification: A meta-analysis of randomized controlled trials,” Eur J Ophthalmol. 2024 Jan 30: 11206721241229129. doi: 10.1177/11206721241229129
IOL for Cataract Patients with Macular Disease
Lens appears useful in many macular conditions.
An extended macular vision IOL appears to provide long-term safety in patients with macular disease undergoing cataract extraction, a new study concludes.
Dr Federico Badalà will present the latest results with the EyeMax Mono IOL (Sharpview Ophthalmology) in a free paper session this afternoon.
He will report a retrospective case series of patients undergoing phacoemulsification and implantation of the extended macular vision IOL designed to optimise image quality up to 10 degrees from the foveal centre. Criteria for implantation included centre-involving macular lesion (e.g., dry AMD, stable wet AMD, macular hole, Stargardt disease), stable choroidal neovascularisation (no intra- or sub-retinal fluid), and no retinal treatment for 6 months before surgery. Eyes without a functioning retina within approximately twodisc diameters (10 degrees) of eccentricity from the foveal centre were excluded from the study. Eyes were categorised into four groups depending on the cataract density.
Some 269 eyes of 215 patients (mean age 72.5±9.8 years) were included in the study and followed up for a mean of 46.1±25.6 months. Mean CDVA and CNVA improved by 0.26 logMAR and 0.15 logMAR (both with p<0.001), respectively. The subgroup of eyes with visually insignificant cataract (NC1; n=147) showed a mean improvement in visual acuity: 0.22 logMAR of CDVA (11 ETDRS letters; p<0.001) and 0.9
logMAR of CNVA (4 ETDRS letters; p<0.001). Of those eyes, 35.4% gained ≥3 CDVA lines and 16.5% gained ≥3 CNVA lines. Hypermetropia was targeted in most eyes to provide magnification when corrected with spectacles. NC1 eyes with postoperative spherical equivalent <1.0 D (n=12) had a mean CDVA improvement of 0.24 logMAR (p=0.003).
“Visual improvement in patients with macular lesions who underwent cataract removal and were implanted with the EyeMax Mono IOL appears to be jointly influenced by the surgical removal of the cataract and the optical design of the IOL,” Dr Badalà said. “Notably, the vision enhancement for eyes with visually insignificant cataracts underscores the IOL’s ability to optimise the use of healthy retinal areas. Future research will evaluate the respective contributions of the IOL design and cataract surgery to the overall enhancement of visual function in this patient population.”
The EyeMax Mono IOL is a single piece, square edge, aspherical soft, hydrophobic, acrylic, yellow-tinted IOL. It has a refractive index of 1.525 and is available in 11–25 D, in 2.0 D steps.
Dr Badalà will present his research at 14:18, Free paper podium 1.
Federico Badalà MD is based at Micro Chirurgia Oculare, Milan, Italy.

Green and clean
Innovative eco-design saves resources
Less waste and lower disposal costs
Swiss made Medicel quality










































































































What’s New in Early Diagnosis of Keratoconus Progression
Instructional course opening new horizons for corneal surgeons worldwide.
TIMOTHY NORRIS REPORTS
Using a holistic approach to analyse and better understand the pathophysiology of keratoconus, a roundtable of international cornea experts will examine the condition to find new and more effective solutions and therapeutic options.
The course, “What’s New in Early Diagnosis, Pathophysiology, and Prevention Strategies of Keratoconus,” features several international key opinion leaders in cornea and corneal surgery, including Dr J Bradley Randleman, who will talk about biomechanics through advanced diagnostics such as Brillouin microscopy; Dr Pooja Khamar on the search for biomarkers in keratoconus; and Dr Davide Borroni, who will discuss the role of microbiota in keratoconus.
New aspects of this disease will be taken into consideration for the first time in such an international and prestigious stage, said Dr Cosimo Mazzotta, chair of the course.
Even though there will be talk about cross-linking protocols, there will be a focus on less known mechanisms and aspects of the disease because keratoconus treatment options do not stop at CXL and corneal transplant. “There is much, much more,” he stressed.
While many of the themes considered during the course may look secondary, they do have a meaningful impact on the onset and course of the disease. It is the first time nutraceuticals, microbiomes, biomechanics, and multiple pieces of news regarding alternative approaches will condense in a one-and-a-half-hour course.
The course also includes a talk by Dr Farhad Hafezi— who will give pearls on prevention strategies involving epion cross-linking—and the very first presentation of a new technique from Dr Marco Zagari on the invention
and experience with AFXL CAIRS, an approach aiming to give the surgeon faster and more effective allogenic intrastromal rings.
Dr Mazzotta will close the session with a discussion of how a nutraceutical approach could be a valid prevention strategy for patients with high risk of developing keratoconus.
“What’s New in Early Diagnosis, Pathophysiology, and Prevention Strategies of Keratoconus” will take place on Monday at 14:00 in Room 8.1 P.
Cosimo Mazzotta MD, PhD, FWCRS is Professor of Ophthalmology at the University of Siena; Anterior Segment Surgeon at Alta Val d’Elsa Hospital; and founder and scientific director of the Siena Crosslinking Centre of Siena, all of Italy. cgmazzotta@libero.it
J Bradley Randleman MD, Professor in the Department of Ophthalmology at the Emory University School of Medicine and director of the Cornea, External Disease, and Refractive Surgery Section at the Emory Eye Center, Atlanta, US.
Pooja Khamar MD, PhD is from the Narayana Nethralaya Eye Institute, Bengaluru, India.
Davide Borroni MD, PhD is Chief Scientific Advisor at Eyemetagenomics LTD, London, UK.

Farhad Hafezi MD, PhD, FARVO is Professor of Ophthalmology at the University of Geneva, Switzerland.
Marco Zagari MD is based in Aci Castello, Italy.

OUR MISSION
Working hand in hand with healthcare professionals to deliver transformative patient outcomes in both diagnostic and treatment via our collective expertise and advanced solutions.
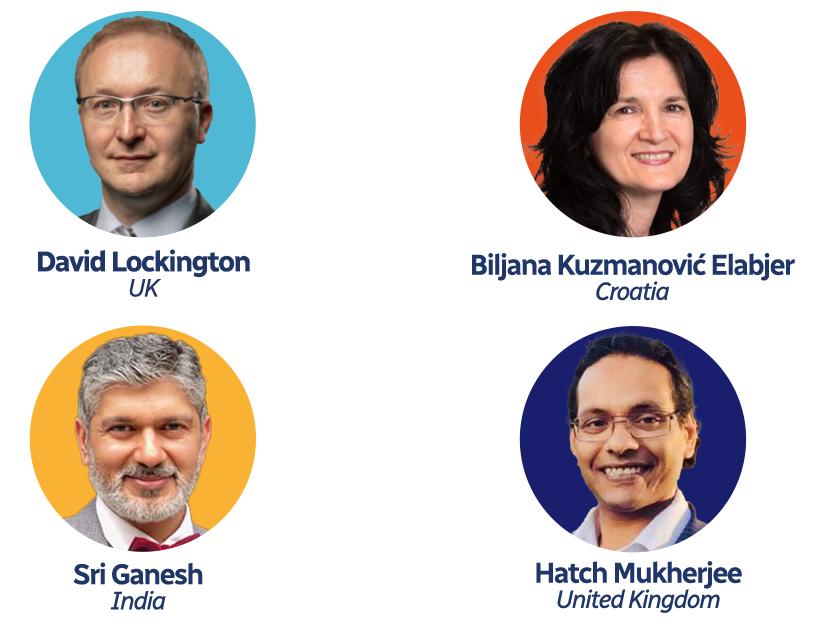
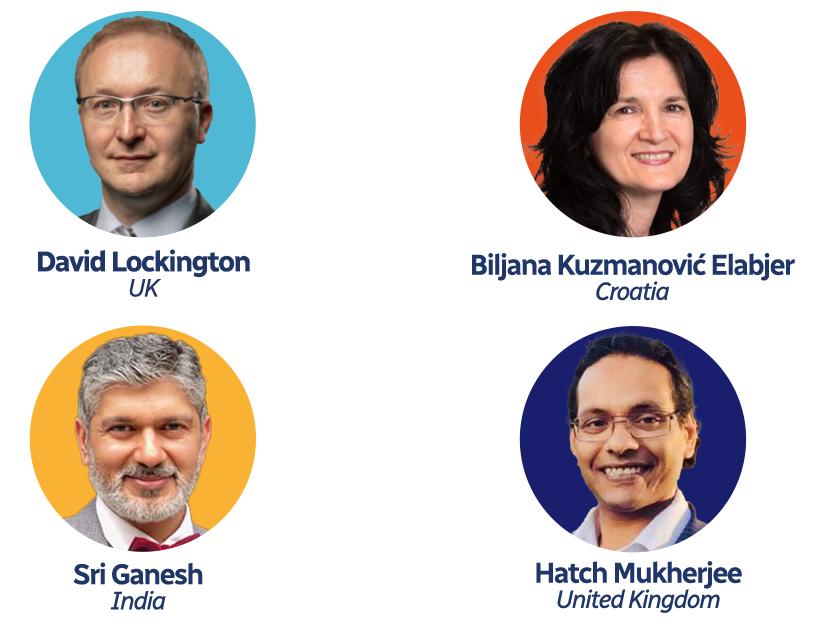
First-Ever Speed Mentoring Sessions to Debut at ESCRS
The Building Our Sustainable, Inclusive Society (BOSS) team will introduce the first-ever Speed Mentoring Sessions at ESCRS 2024. Scheduled 6–9 September, these sessions offer a new format for professional development by facilitating brief, focused interactions between emerging talent and more than 40 experienced experts in ophthalmology.
Founded by ESCRS President Filomena Ribeiro, 2024 also marks the inaugural launch of the ESCRS inclusivity initiative. “The purpose of BOSS is to foster an environment within ESCRS where everyone feels they have a place,” said Kristine Morrill, ESCRS consultant and BOSS member. “We’ve created a year-round programme that gives opportunities for members to network and create an environment for career and personal development.”
Each mentorship session will last one hour and allow mentees ten-minute discussion rotations with six mentors, offering the opportunity to benefit from diverse perspectives and expertise with mentors coming from various domains within ophthalmology, including ESCRS leadership, prominent ophthalmologists, and industry innovators. The overwhelming interest in these sessions has already led to a complete booking of all available spots, reflecting the high demand for mentorship opportunities at the Congress.
“We’ve been really surprised and grateful by the response,” explained Morrill. “The mentors are senior leaders in
the industry, key opinion leaders from all around the world, and even the first and second female presidents of ESCRS, Marie-José Tassignon and Béatrice Cochener-Lamard.”
These interactions are designed to provide valuable career advice, share insights into various sub-specialties, and offer guidance on navigating the ophthalmic field. Mentees can expect personalised feedback and answers to specific questions during the one-on-one discussions.
The sessions will cover a range of topics, including the latest trends in ophthalmology, research advancements, and career development strategies. This tailored approach ensures participants gain relevant insights to stay ahead in their profession and can help foster networking connections that could benefit their careers for years to come.
Expected to be a standout feature, the introduction of Speed Mentoring at ESCRS 2024 highlights the importance of mentorship in professional development. Studies have consistently shown mentorship plays a crucial role in career success, and these sessions provide mentees with the opportunity to build their professional networks.
In addition to the speed mentorship, BOSS has organised a series of events designed to foster inclusivity and networking among attendees, including the Boss Networking Mocktail Party. This new initiative underscores the Society’s dedication to supporting the growth and development of the next generation of ophthalmology professionals.

Minimising Residual Refractive Error
Key for maximising outcomes and patient satisfaction after presbyopia IOL surgery.
CHERYL GUTTMAN KRADER REPORTS
Achieving patient satisfaction when implanting presbyopia-correcting IOLs depends on hitting the refractive target. The keys to reducing postoperative refractive error include obtaining precise diagnostic measurements and accurate IOL calculations, said Dr Joaquin Fernández.
Referring to a recently published study that stratified monocular visual outcomes after cataract surgery in patients implanted with monofocal and multifocal IOLs, Dr Fernández showed the chance of postoperatively achieving 20/20 UCVA fell off considerably even with minimal amounts of residual spherical error. Results from the same study also showed the percentage of patients who were satisfied or very satisfied after surgery was significantly impacted by minimal amounts of residual spherical error.
Speaking in an ESCRS Refractive IOL IME Forum focusing on integrating presbyopia correction into the everyday cataract practice, Dr Fernández provided pearls for mastering preoperative diagnostics and IOL calculations to avoid refractive surprises.
One key consideration for obtaining accurate diagnostic information for surgical planning is to detect and manage ocular surface problems preoperatively.
“Ocular surface disease is common in cataract surgery patients, and studies have shown that patients with dry eye disease are often asymptomatic,” Dr Fernández noted. “Results of the most recent ESCRS Clinical Survey show that 63% of respondents are very likely or likely to postpone cataract surgery in a patient with moderate dry eye until the disease is better managed.”
To ensure surgeons capture accurate corneal power measurements, he recommended obtaining measurements with multiple devices representing different technologies before comparing the data, checking for inconsistency. Lack of agreement signals the need to recheck the ocular surface condition and repeat the measurements.
Discussing IOL calculations, Dr Fernández provided a listing of current IOL formulas showing they can be grossly divided into empirical and theoretical groupings and that the theoretical formulas, which are all based on geometrical optics, include thin and thick lens paraxial geometrical optics formulas and exact geometrical optics formulas. He contended, however, that there are no clinically relevant differences in the prediction accuracy between the current calculation formulas in normal eyes.
“Our main recommendation [for achieving a high rate of cases with an achieved refraction within 0.5 D of target] is to work with an optimised constant formula instead of averaging formulas without prior adjustments,” Dr Fernández said.

He illustrated this point by discussing early outcomes achieved using a formula his group developed optimised for the surgeon, the biometer, and the IOL model.
Although he noted modern biometers provide reliable data, Dr Fernández reinforced the importance of using optimised constants for each biometer. He made his point by discussing a study comparing IOL power calculations performed using data from a standard partial coherence interferometry-based biometer and a Scheimpflug-based device that showed the results of the two devices were not interchangeable.
“Surgeons need to know that almost all the constants are optimised to the IOLMaster,” he said. “If you use another biometer, you need to optimise the constant to the instrument you are using.”
Joaquín Fernández MD, PhD is CEO and Medical Director of the Ophthalmology Department at Qvisión in Vithas Virgen del Mar Hospital, Almería, Spain. JoaquinFernandezoft@ Qvision.es


New Alternative to Cyclodestructive Therapy
A micro solution to a macro problem?
Micropulse transscleral cyclophotocoagulation (mCPC) appears to offer an effective alternative to cyclodestructive therapies used for refractory glaucoma management, a new study suggests.
Dr Luis Miguel Oviedo Plathi presented a poster comparing mCPC to three cyclodestructive therapies for refractory glaucoma management.
He conducted a comparative, longitudinal, randomised study with a sample of 80 patients with refractory glaucoma submitted to mCPC therapy, transscleral cyclophotocoagulation, mixed treatment, and cyclocryotherapy. The study tracked IOP preoperatively and at day one, week one, month one, month three, and month six. The protocol also tracked the presence of pain prior to surgery and at month six, as well as medication use at baseline and six months after the procedure.
The mean baseline IOP in all groups was 46.91 mmHg. All groups achieved a reduction in IOP at six months of 53–69% of baseline. There were no statistically significant differences between the groups. All groups showed an
effective reduction in pain compared to baseline. Regarding the reduction in the use of drugs, the average of the groups was three drugs less compared to the baseline; all groups presented minor complications and rapid resolution.
The study suggests that all cyclodestructive techniques and mCPC are effective for IOP control in refractory glaucoma and pain reduction. All were also found to be effective in reducing the number of drugs used, being superior in reducing IOP with an acceptable safety profile, he said.
“In my experience, mCPC is a good tool not only for reducing the IOP and pain. I see the benefit of reducing the amount of eye drops in patients with primary open-angle glaucoma who have vision, ocular surface problems, feeling discomfort, or, in case of non-compliance, in medication,” Dr Oviedo Plathi reported. “In patients with refractory glaucoma, I have a 50–60 % rate of decrease in intraocular pressure.”
Luis Miguel Oviedo Plathi MD is based at Hospital Universitario de Maracaibo, Venezuela.

A New Era of Intraocular Surgery: Introducing the Intensity Pentafocal Lens
Author: Yoram Gonen, CEO Hanita Lenses
For over 40 years, Hanita Lenses has been at the forefront of manufacturing high-quality IOLs, competing successfully and achieving consistent global growth. In the last 15 years, we have transitioned from a local, conservative company into a dynamic, premium, and innovation-focused organization. This transformation, driven by a talented, cohesive, and energetic team with strong engineering and manufacturing expertise, has allowed us to bring new and exciting solutions to ophthalmologists who seek the most advanced and reliable products - ultimately providing patients with true spectacle independence
The INTENSITY Pentafocal Lens, based on our proprietary Dynamic Light Utilization (DLU) technology, exemplifies the spirit of innovation that has become a cornerstone in how we think and create. Over 30,000 patients worldwide have experienced its outstanding optical performance, enjoying smooth vision at all distances with minimal disturbances. This success has been demonstrated time and again in patient satisfaction surveys and clinical studies. The overall feedback is nothing less than WOW.








"A patient that gets the Intensity lenses enjoys a life that is uncompromised. With the Intensity Pentafocal IOL, the patient forgets about their lenses because vision is a non-issue."


— Prof. Dr. med.

Gerd Auffarth


These studies show that the Intensity lens delivers photopic and mesopic vision levels comparable to the phakic population, with patients reporting freedom from glasses and the ability to engage in any activity. A particularly notable study from Japan looked at the number of patients satisfied with night driving – the number of Intensity patients was twice as high as the patients using older presbyopiacorrecting lenses.








The Intensity lens delivers photopic and mesopic vision levels comparable to the phakic population, with patients reporting freedom from glasses and the ability to engage in any activity.





Defocus Curve
Visual Acuity(logMAR)
Monocular (356 eyes) Binocular (241 patients)
Defocus (D)
Figure 1: real-world data reveals that from distance to 40 cm, patients achieve a visual acuity of 0.1 LogMAR or better without any drop in visual performance across the full range of vision - a common limitation in older-generation lenses.
Guided by our belief that "Everyone deserves to see the world's beauty," we are committed to developing technologies and solutions that provide unique added value to patients. We collaborate with our global advisory board, university experts, and research institutions to stay at the forefront of medical advancements in the field.
Monocular VA at different distances
Visual Acuity(logMAR)







Distance (cm)




Figure 2: monocular visual acuity, real-world outcomes of 1118 eyes. High visual acuity is maintained along the whole visual range.
To better support our high-end premium clients, we have established five subsidiaries in key markets across Europe and Asia. In 2025, we will launch a second advanced manufacturing site to meet the demands of our fastgrowing Asian markets.
We strive for excellence in every aspect of our business, eager to succeed, and ready to embrace the challenges ahead.
Refractive Full Range of Vision IOL Succeeding in Clinical Trial
HOWARD LARKIN REPORTS
Anew refractive hydrophobic acrylic intraocular lens (IOL) designed to deliver a full range of vision (FVR) is safe and effective for patients undergoing bilateral cataract extraction, Professor Béatrice Cochener-Lamard said in the EU Clinical Trial Spotlight Symposium. The goal is to create an extended depth of focus lens that meets the new ESCRS criteria for FVR.
Expected to launch in the EU in 2025 pending CE marking, the LuxLife IOL (Bausch + Lomb) is a four-haptic, single-piece lens with a 6.00 mm optic preloaded for insertion through a 2.2 mm incision. It has a 2.0 mm central aspheric zone that uses a 4th- and 6th-order spherical aberration combination of opposite signs to provide intermediate vision at 2.2 D and near vision at 3.4 D in the IOL plane. A patented transition zone extends the spherical aberrations to the monofo-cal periphery to ensure no loss of light while providing a full range of vision from near to far.
In an ongoing multicentre clinical trial, distance vision results were statistically similar between 241 eyes of 121 patients implanted with LuxLife and 121 eyes of 61 patients receiving a monofocal control. Ninety-nine per cent of LuxLife and 100% of control patients achieved monocular corrected distance visual acuity (CDVA) of 0.2 logMAR (20/32) or better in the first eye implanted. All patients in both groups achieved at least 0.2 logMAR CDVA six months after surgery, said Prof Cochener-Lamard, the medical monitor for the study. “We are achieving the targets.”
However, the LuxLife delivered significantly better intermediate and near vision. Binocular uncorrected
intermediate visual acuity of 0.2 logMAR or better was achieved by 99% of LuxLife patients but only 55% of monofocal patients. Similarly, 99% of LuxLife but only 3% of monofocal patients scored uncorrected near visual acuity of 0.2 logMAR or better. Overall, the LuxLife provided a 3.1 D depth of focus at 0.2 logMAR.
As for quality of vision, no statistically significant differences were seen in halos between the two groups. Glare size was graded significantly larger in the LuxLife group, though glare intensities were statistically similar.
Patient-reported outcomes also favoured the LuxLife. Eighty per cent of LuxLife patients reported no need for spectacles compared with 14% of controls. Significantly more LuxLife patients reported less difficulty with intermediate and near vision tasks, such as seeing prices while shopping and reading newspapers.
Safety was also strong: of 174 eyes implanted with LuxLife, 1 developed cystoid macular oedema and 2 required secondary intervention unrelated to the device. No secondary surgical interventions were required due to the optical properties of the lens, Prof Cochener-Lamard noted.
Based on the new ESCRS FVR definition, “we are getting to that level,” she said.
Béatrice Cochener-Lamard MD, PhD, FEBO is Professor and Head of the Department of Oph-thalmology, CHU Morvan Brest – UBO University, Brest, France. beatrice.cochenerlamard@chu-brest.fr







ESCRS Has Its Eyes on the World
Special project in Mozambique reaching the most vulnerable.
ESCRS supports a number of ophthalmology training projects around the world. One of these projects is a collaboration with the Eyes of the World Foundation in Inhambane, Mozambique. The Inhambane region faces the difficulties of displacement in rural areas and the economic and socio-cultural barriers that hinder the population’s access to health services.
ESCRS President Filomena Ribeiro recently visited Inhambane with ophthalmologist Mark Wevill and ESCRS Managing Director Tom Ogilvie-Graham. She witnessed and assisted with the hard work of the Foundation’s team on the ground. The following is an excerpt of an interview with Prof Ribeiro conducted by the Eye of the World team.
How important are the projects supported by the Charity Committee for ESCRS and for you, personally?
The projects supported by the Charity Committee are of vital importance both for ESCRS and for me. For the ESCRS, these projects represent an opportunity to fulfil our mission to improve the quality of ophthalmic care worldwide by promoting research, education, and the development of new technologies. Furthermore, through these initiatives, ESCRS can extend its impact beyond congresses and scientific activities, reaching communities and regions that need it most.
From a personal perspective, supporting these projects is deeply gratifying. Seeing the positive impact they have on the lives of people and communities is an enriching experience. Moreover, participating in these projects allows me to contribute in a tangible way to improving global visual health, which I consider a duty and a privilege as an ophthalmology professional.
During your visit to Inhambane, what was your overall impression of the work done by Eyes of the World? What specific aspects of the eye health improvement project had the greatest impact on you, and why?
During my visit to Inhambane, I was deeply impressed by the work done by Eyes of the World. The dedication and commitment of the team to improving eye health in the region is evident in each of the activities I witnessed.
One of the aspects that struck me most was the surgery campaign at the Inhambane Provincial Hospital. The organisation and efficiency with which the surgeries were performed, as well as the postoperative care provided to the patients, demonstrate a high level of professionalism and a clear concern for the quality of life of the people served.
Furthermore, the visit to the mobile optical activities in the Homoine district underlined the importance of bringing
eye care services to more remote communities, ensuring more people have access to these vital services.
Another notable aspect was the promotion of gender equality in Massinga through HOPEM – Homens per la Mudança. This initiative addresses not only visual health problems but key social issues—promoting positive and sustainable change in the community.
Finally, the training activity led by the medical supervisor in the district of Maxixe—focusing on cataract screening, glaucoma detection, and refraction—underlines the comprehensive and educational approach of the project. Ongoing training of local professionals is essential to ensure the sustainability and long-term impact of these initiatives.
In short, Eyes of the World’s work in Inhambane not only improves the visual health of the popultion but also strengthens local capacities and promotes gender equity, creating a profound and lasting impact on the community.
How would you describe the visual health situation in the most vulnerable population of Inhambane, and could you share any stories or cases that touched you during your visit?
The eye health situation in the most vulnerable population of Inhambane is extremely precarious and has very few
resources. During my visit, what impressed me most was the hope the development of the new ophthalmology department at the Provincial Hospital, a project being developed by Eyes of the World, brings to this population. This development promises to significantly improve access to, and quality of, ophthalmology services in the region.
One story that touched me deeply was that of an elderly woman who had been suffering from cataracts for years. Due to a lack of resources and access to adequate eye health services, she had lost almost all her vision and was completely dependent on her relatives for the most basic tasks.
During the surgery campaign organised by Eyes of the World, she was operated on. The next day, when the bandage was removed, she was able to see clearly for the first time in years. The emotion and gratitude in her eyes are moments not to be forgotten. This case highlights not only the urgent need for these services but also the transformative impact they can have on people’s lives.
To read the entire interview, please visit https://www.ullsdelmon. org/.
Images beyond all expectations




Annual ESCRS Clinical Trends Survey Underway: Your Participation is Essential!
Survey participants will be entered into a raffle to receive free delegate registration for the 2025 ESCRS Annual Congress in Copenhagen and a summary report before publication.
Th e 10th annual ESCRS Clinical Trends Survey is launching at the 2024 Congress in Barcelona. This survey builds upon the success of prior surveys, which have included more than 14,000 participants.
The survey asks ESCRS delegates key questions regarding issues they regularly face in their practice. The goal is to obtain opinions from a significant percentage of delegates for ESCRS leadership to review. Using previous surveys as a foundation, the 2024 edition adds questions in evolving clinical and technology areas such as retina.
Data from prior surveys have helped develop content for many of the symposia at this year’s ESCRS Clinical Forum IME programmes. Information from the upcoming survey will continue to drive these efforts and discover new areas of education.
The 2024 ESCRS Clinical Trends Survey includes a wide range of contemporary topics, such as:
• Cataract extraction
• Presbyopia correction
• Astigmatism management
• Ocular surface disease
• Glaucoma
• Cornea- and lens-based refractive surgery
• Retina
• Medical education

How to participate
The survey can be completed in person at the ESCRS Congress in Barcelona at the Survey Lounge in Exhibit Hall 6 on 6–8 September. Seating and refreshments will be provided to those who participate. If you are unable to complete this survey during the Congress, we encourage you to take this 15-minute survey by going to https://tfgedu.questionpro.com/ESCRS2024. Please complete the survey as soon as possible, as it will close in October.
By completing the survey and filling in an email address, respondents will be entered into a raffle to win free registration for the 2025 ESCRS Congress in Copenhagen. Additionally, every participant will be emailed a summary of the data shortly after it’s compiled. Finally, and most importantly, by completing the survey, respondents will provide essential data that helps drive future education programming. Respondents can remain anonymous, if desired, and still give ESCRS important feedback.
It’s Time for the Timelines
This year’s ESCRS Congress sees the launch of two interactive timelines on our website. The first takes you on a self-paced journey through the history of cataract surgery. Starting in ancient Babylon to the present, the ‘History of Cataract Surgery’ demonstrates a comprehensive overview of the milestones that shaped one of the oldest and most transformative medical procedures in human history. Whether you are a medical professional, a student, or simply someone interested in the history of medicine, this timeline offers an engaging and informative exploration of cataract surgery’s rich heritage.
The second timeline walks you through the ‘History of Refractive Surgery,’ delving into the fascinating advancements that have transformed the way we correct vision. From early methods to the latest cutting-edge technologies, uncover the key milestones in the quest for perfect vision.
Join us as we trace the remarkable journey of refractive surgery, celebrating the technological advancements and scientific breakthroughs that have made clear vision accessible to millions.
The ESCRS timeline web page also features video interviews with some of the pioneers of the 20th century. In the first interview, Sean Henahan (EuroTimes) and Dr Richard Packard (Packard Medical Practice) sit down with Professors Thomas Neuhann (EuroEyes Clinic Group) and Hans-Reinhard Koch (University of Bonn) to discuss IOL visionaries past and present. Profs Neuhann and Koch recount the evolution of IOL surgery from perilous to commonplace, describing early phaco surgery uncertainties, industry struggles, and the genius of visionaries like Dr Charles Kelman and Dr Richard P Kratz. Get ready for a whole lot of insight—sprinkled with a pinch of laughter!
While at the Barcelona Congress, you won’t want to miss the ESCRS Heritage Tunnel Walk, where you can get a close look at the technical changes that got us where we are today.




ophtec.com/precizon-family























Breaking Presbyopia-Correcting IOL Procedure Barriers
Strategies for addressing barriers to presbyopia IOL procedures provides a pathway for increasing uptake.
CHERYL GUTTMAN KRADER REPORTS
Presbyopia-correcting technologies still account for a small minority of lenses implanted in patients undergoing cataract surgery. Speaking at an ESCRS Refractive IOL IME Forum on Sunday morning, Dr Ramza Diamanti offered ideas for addressing barriers to incorporating presbyopia IOL procedures into the everyday cataract practice.
Referring to results from the 2023 ESCRS Clinical Trends Survey, Dr Diamanti pointed out that cost to the patient, concern over nighttime quality of vision, and concern over loss of contrast visual acuity represented the top three concerns respondents had for not performing more presbyopia-correcting IOL procedures.
To tackle patients’ cost concerns, Dr Diamanti undertakes a cost-benefit discussion as part of the initial counselling. The education covers how a presbyopia-correcting IOL offers improved quality of life, visual acuity, range of focus, and spectacle independence—but also acknowledges the option involves an out-of-pocket expense and carries the potential for quality of vision issues and residual spectacle dependence.
“Some surgeons take patient life expectancy into consideration as well,” she said. “I do not do that because I believe all patients can benefit from having presbyopia correction.”
When cost emerges as an issue for a patient, she suggested strategies including offering a reliable presbyopia-correcting
IOL that is more affordable, using a mix-and-match approach, or suggesting a pay-by-instalment plan.
Recognising the potential for patient dissatisfaction because of postoperative dysphotopsia, Dr Diamanti underscored the need to consider the relationship between lens design and risk for visual disturbances.
“We all know that with extended depth of focus/ extended range of vision (EDOF/ERV) IOLs and multifocal (trifocal) IOLs there is a balance between depth of field, visual quality, and dysphotopsia,” she said.
To help guide IOL selection for an individual wanting presbyopia correction, Dr Diamanti uses a sixitem questionnaire in which one of the questions asks patients about their willingness to compromise achieving good distance and mid-range or near vision without glasses for the possibility of seeing some rings or starbursts around lights at night. Patients who are not willing to accept the trade-off are considered candidates for an EDOF/ERV IOL instead of a multifocal IOL.
In order to have happy patients, we try to mitigate postoperative errors, and so we need to be ready to do an enhancement or IOL exchange, if necessary.
Dr Diamanti also advocated for having a preoperative strategy for addressing postoperative refractive error, recognising the latter problem cannot always be avoided.
“In order to have happy patients, we try to mitigate postoperative errors, and so we need to be ready to do an enhancement or IOL exchange, if necessary,” she said.
“In addition, we always need to stand by our patients with counselling and support, and we need to wait and not jump into more surgery. With presbyopia-correcting IOLs, we change the physiology of vision, and this means there is a need for neuroadaptation.”
Concluding her talk, Dr Diamanti reminded attendees that presbyopia-correcting IOL surgery is not for everyone.
“Careful patient selection is critical,” she stressed. “Whether our patients wind up with or without glasses, we want them to be happy.”
Ramza Diamanti MD, MRCOphthl, FEBO is head of the surgical department at the OMMA Oph-thalmological Institute of Athens, Greece.


TOMEY is committed to very high quality, service, and innovation. This leads to early prevention, accurate diagnoses, and examinations that are as comfortable as possible. Get to know our products in the fields of:
Cataract & Cornea
Glaucoma & Retina
Understanding IOL Technologies and Patient Needs
Session notes these as critical for success in presbyopia-correcting surgery.
CHERYL GUTTMAN KRADER REPORTS
Cataract surgeons can choose from a wide range of IOLs for presbyopia correction in patients who want to reduce their dependence on spectacles. The drawback of access to this huge variety, however, is it can create a lot of confusion for surgeons, said Dr Ramin Khoramnia.
Understanding the features of the different technologies and applying that knowledge when choosing an IOL for each patient, Dr Khoramnia emphasised, will help optimise the outcomes and address their preferences and needs.
Historically, the main options for presbyopia correction were to create monovision with monofocal IOLs or choose a multifocal implant. However, each of these approaches suffer limitations. In particular, monofocal IOL monovision results in loss of depth perception and suboptimal intermediate visual acuity, while multifocal IOLs carry an increased risk for visual disturbances and reduced contrast sensitivity.
“The recent introduction of enhanced monofocal (monofocal plus) and extended depth of focus/extended range of vision (EDOF/ERV) IOLs addresses these gaps by providing improved intermediate vision, reduced risk of visual disturbances, and better contrast sensitivity,” Dr Khoramnia said.
“Nevertheless, these IOLs may not be ideal for patients who demand full spectacle independ-ence at near.”
In his talk, Dr Khoramnia provided an overview of the monofocal plus and EDOF/ERV IOL categories and
outlined recommendations for IOL selection based on consideration of specific patient characteristics.
He noted that the currently available monofocal plus IOLs are not comparable, as they differ in optic design.
“However, these implants only slightly enhance depth of focus, so patients gain just about one line of intermediate vision compared with a standard monofocal IOL from the same manufacturer,” Dr Khoramnia said, questioning whether this could be considered true presbyopia correction.
Available EDOF/ERV lenses also differ from each other in their optic design, although Dr Khoramnia presented study results showing lenses with different technologies provided excel-lent visual outcomes for uncorrected distance and intermediate vision with good near vision and low rates of visual disturbance from dysphotopsias.
“Keep in mind, however, that it is not only the optic that influences visual disturbances. Dry eye or vitreous problems can also lead to these phenomena. Therefore, I do not guarantee that patients will not suffer these issues,” he said. “I only say they have the same risk as compared to having a monofocal IOL.”
Outlining the patient characteristics he considers when selecting between a monofocal plus and an EDOF/ERV IOL for individuals wanting to increase their spectacle independence after cataract surgery, Dr Khoramnia said the list includes risk tolerance for dysphotopsias, lifestyle, visual demands at different distances, personality, and ocular health.

He also mentioned a small-aperture IOL based on the pinhole principle to increase depth of focus as another option to increase spectacle independence after cataract surgery.
“This type of IOL is a great choice for patients with prior monovision, and it is also used for patients with iris trauma, an irregular or scarred cornea, keratoconus, or a history of refractive surgery,” he said. “However, a small aperture IOL should be avoided in anyone with macular disease or proliferative diabetic retinopathy.”
Ramin Khoramnia MD, FEBO is professor in the department of ophthalmology at Heidelberg University, Heidelberg, Germany. ramin. khoramina@meduni-heidelberg.de

Francesco Blasetti (Italy)
The programme is incredibly rich and brilliant, offering a wide array of interesting courses and posters. My favourite part was the main symposium on telemedicine. It’s a topic that’s gaining momentum and could play a significant role in the near future. I’d love to see more focus on this in upcoming programmes.
Visit OASIS at ESCRS Booth #6.F10

OASIS® manufactures a wide variety of high quality ophthalmic microsurgical knives from PremierEdge® for use in cataract, refractive, retinal and glaucoma surgery.
PremierEdge® Microsurgical Knives provide trustworthy performance during surgical procedures with enhanced precision on the cutting tip and ergonomic handle design. Also available: PremierEdge® has safety scalpels designed for one-handed use.
• Disposable
• Plastic handle
• Stainless steel micro blades
• Sterile blister pack
To see if this product is available in your country, please contact international@oasismedical.com

The Burnout Factory
BY IDOIA GOÑI GUARRO MD
Dear reader,
As we embark on this journey of introspection, I must forewarn you that this contemplation may claim a few precious minutes of your time. And if the notion of time’s passage already flutters in your mind, beckoning you to swiftly skip to what lies beyond these words, I must confess—you’ve unwittingly stepped foot into the realm of burnout.
Burn Baby Burn
It is true the inherent characteristics of work in the health field determine a context prone to instances of great stress given the nature of the activity and the frequent imbalance between external demands, self-demand, and often the resources available to efficiently comply with the objectives. The intensity and uncertainty of the events in the last three years determined in health professionals that coping with these situations in such a prolonged and continuous manner became in itself a burden, generating in some cases and increasing in many others symptoms of emotional exhaustion, frustration, and lack of motivation for the profession. Inadequate coping abilities may result in emotional fatigue, diminished success, and dehumanization of patients, culminating in a mechanical approach to procedures and interactions. These indicators collectively contribute to what is commonly recognized as ‘burnout syndrome,’ where individuals experience a sense of being overwhelmed and depleted by the demands of their work.
The ‘always on’ culture
In the realm of ophthalmology, burnout syndrome often flies under the radar, potentially due to misconceptions about the profession. Despite assumptions of high job satisfaction and low stress levels, ophthalmologists are just as susceptible to burnout as other medical professionals. Recognizing this disconnect between perception and reality is essential to address burnout within the field and support the well-being of current and future ophthalmologists.
A recent study by Jessica A Sedhom and Leonard K Seibold surveyed 592 ophthalmologists in the US, revealing a notable 37% showing symptoms of burnout syndrome. Distinctions among subspecialties showcased varying rates, ranging from 30.8% to 45.4%. Notably, female ophthalmologists reported higher burnout rates, potentially influenced by gender-specific patient interactions. Hospital-employed ophthalmologists also faced elevated burnout risks compared to their counterparts in private practice, prompting a call for healthcare institutions to address these contributing factors.
Additionally, other research has highlighted the significant impact of early career stages on burnout prevalence among ophthalmologists. Alarmingly high rates of emotional exhaustion and depersonalization among residents emphasizes the pressing need for intervention and support mechanisms at the onset of a practitioner’s career to combat burnout effectively.
It is known to everyone the usual shortage of time for consultations is compounded by the incessant flow of protocols, the increase in administrative tasks, social distancing, fear of contagion, error, and very importantly, the assiduous feeling of not practising the profession as desired and the lack of attention to other patients.
However, beyond what the statistics and studies reveal, it is important to consider that behind what these numbers represent there are real individuals with emotions, struggles, and vulnerabilities. This needs to serve as a reminder to truly appreciate the human element with its corresponding complex experiences.
In the world of ophthalmology, where personal and professional spheres often overlap, finding a harmonious equilibrium is key.
The importance of self-reflection
Navigating burnout in the medical field requires a multifaceted strategy that addresses the well-being of healthcare providers on individual, collective, and institutional levels. By implementing early interventions and support systems, not only can we safeguard the mental health of professionals but also maintain the standards of patient care in the medical industry.
In the world of ophthalmology, where personal and professional spheres often overlap, finding a harmonious equilibrium is key. Mitigating stress through a blend of activities such as exercise, meditation, seeking counselling, socializing, indulging in hobbies, embracing spirituality, and ensuring adequate rest can aid in maintaining a healthy work-life balance.
When considering upheavals within a practice, it’s vital to pace changes thoughtfully. Introducing too many modifications at once, even if beneficial, can overwhelm the system. For example, during a period of transition like relocating or expanding services, it may be prudent to hold off on additional transformations such as partnerships or new ventures to avoid unnecessary strain. Recognizing one’s tolerance for stress and upheaval is essential, as it differs from person to person. By proactively planning for changes and managing the overall flux in various facets of life, individuals can navigate challenges more effectively and safeguard their well-being in the long run.
Therefore, dear reader, it’s crucial to keep in mind that burnout can quietly encroach. Surrounding yourself with individuals capable of identifying stress indicators is a priceless asset. It’s not just about handling acute stress, but also about recognizing and managing long-term stress that can lead to burnout. Prioritize self-care and be proactive in seeking support when necessary. By doing
so, you can effectively minimize avoidable stress during training and practice, setting the stage for a thriving and enduring career.
Dr Guarro came third in the 2024 John Henahan Writing Prize answering the prompt ‘Burnout is a chronic issue in ophthalmology, leading a growing number to abandon the field early in their careers. What should be done to reduce unnecessary stress in training and practice, allowing for a successful long-term career?’. She is an ophthalmology resident at KBC Sestre Milosrdnice, Zagreb, Croatia.
Bibliography:
1. Martínez Pérez, A. “El síndrome de Burnout. Evolución conceptual y estado actual de la cuestión,” Vivat Academia, 2010; 0(112), 42–80. doi: 10.15178/ va.2010.112.42-80
2. Cheung R, Yu B, Iordanous Y, Malvankar-Mehta MS. “The prevalence of occupational burnout among ophthalmologists: a systematic review and meta-analysis,” Psychol Rep, 2021; 124(5): 2139–2154.
3. Alotaibi AK, Alsalim A, Alruwaili F, et al. “Burnout during ophthalmology residency training: a national survey in Saudi Arabia,” Saudi J Ophthalmol, 2019; 33(2): 130–134.
4. Feng S, Taravati P, Ding L, Menda S. “Burnout in ophthalmology residency: a national survey,” Journal of Academic Ophthalmology, 2018; 10(1): e98–e107.
5. Cruz OA, Pole CJ, Thomas SM. “Burnout in chairs of academic departments of ophthalmology,” Ophthalmology, 2007; 114(12): 2350–2355.
6. Méndez Iglesias SM. “Reflexiones sobre el burnout de los profesionales de atención primaria tras la pandemia,” Atencion Primaria, 2022; 54(6): 102314. doi: 10.1016/j.aprim.2022.102314
7. Panagioti M, Geraghty K, Johnson J, Zhou A, et al. “Association between physician burnout and patient safety, professionalism, and patient satisfaction: A systematic review and meta-analysis,” JAMA Intern Med, 2018; 178(10): 1317–1330.
8. “Strategies to avoid burnout,” (n.d.). CRSToday. Retrieved June 14, 2024, from https://crstoday.com/ articles/2019-june/strategies-to-avoid-burnout
9. ArtsSEC. (2020, June 12). “Burnout, de qué se trata? Reflexiones y aprendizaje,” Medium. medium.com/@ArtsSEC/burnout-reflexiones-y-aprendizaje1b85d6141ebb
Gemetric Trifocals Show High Quality
The trifocals also show significant range of vision and low visual disturbances.
TIMOTHY NORRIS REPORTS
Vivinex Gemetric trifocal by Hoya can achieve significant range and quality of vision, with high levels of spectacle independence, high contrast sensitivity, and very low visual disturbances, as shown in three studies presented by Dr Francesco Carones during the EU Clinical Trial Spotlight Symposium held at the 2024 ESCRS Congress in Barcelona.
The key optical elements of this trifocal lens are a proprietary Vivinex platform aspheric refractive design, proprietary Gemetric Gaussian diffractive optics, truncated diffractive zone, and three different focal points of distance. Of particular note were intermediate and near—with intermediate at 1.75 D and near at 3.5 D, Dr Carones said.
Three trials investigating the trifocal were conducted on 526 subjects across 8 countries, in 35 centres. The study did consider both toric and non-toric models.
For context, Dr Carones noted the first pivotal trial obtained the CE mark in June 2020, while the second was a post-market study for 124 bilateral subjects. Finally, he added the third trial enrolled 63 subjects in Japan. Results showed the mean uncorrected visual acuity is better than 0.1 across the entire viewing range. The comparison with the reference monofocal model shows how at a distance, the uncorrected visual acuity is very much overlapping.
On the other hand, he added results showed an important gain—especially in near visual acuity—of more than four lines of gain, even in mesopic conditions. Binocular photopic showed good results by staying in the very tight 0.1 logMAR almost to the 3.5 D defocus range, which Dr Carones explained demonstrated the very wide range of vision these lenses provide.
A subjective investigation also showed more than 95% of patients implanted with Vivinex Gemetric reported never using spectacles for intermediate and far, while 88.2% reported not using glasses for near vision. The spectacle independence achieved is quite high, Dr Carones said, adding there is a little but not significant loss of contrast sensibility in terms of clinical results and statistical analysis, as expected.
Studies also reported only four cases of explantation due to poor neuroadaptation, which he noted pretty much aligned with the rate expected by the leading market competitors.
Quality of vision questionnaires were administered to all participants in the trial, with collected data differentiated into three categories of visual disturbances: frequency, severity, and bothersome (as compared to Vivinex monofocal values). The scores on a Rasch model for the Gemetric Trifocal were higher than the reference lens. However, there was also a trend for both lenses, where the higher frequency, severity, and bothersome visual disturbances decreased, something Dr Carones said may require further investigation.

Nevertheless, benchmarking showed a dramatic improvement in the quality of vision scores following lens exchange, with the entire range of disturbances in the normal range. All the Vivinex lenses perform very well, with the monofocal even under the ‘green zone,’ as a testimony of how these monofocal perform very well, Dr Carones underlined. Bilateral residual error was within 0.25 D of emmetropia, well below the scores achieved by the validation group.
He concluded studies confirmed the Gemetric trifocals can achieve high levels of satisfaction and spectacle freedom, with very low levels of visual disturbances.
Francesco Carones MD is the medical director and physician CEO at Carones Vision Advalia, Milan, Italy. fcarones@ carones.com



The Key to Effective Team Collaboration
LAUREN BLANCHARD REPORTS
Effective team collaboration is crucial for both organisational success and employee satisfaction, according to Celine Reibel, a practice development consultant at SanaConsult in France.
During Sunday’s session of the ESCRS practice management programme, Leadership, Business, and Innovation (LBI), Reibel presented “Team Collaboration from the Team Perspective”.
“There’s a great deal of literature about team cooperation and management, but not that much about the team’s point of view. Teams are the foundation for all work practices. Any organisation depends on how well the employees collaborate, and it ultimately improves the job satisfaction of employees,” Reibel explained.
In her presentation, Reibel cited employee surveys, including one conducted with employees from four small ophthalmology structures in French-speaking Switzerland.1 The study aimed to assess the need for structured management within these health facilities. The findings underscored the connection between well-managed teams and overall workplace satisfaction, reinforcing Reibel’s argument that effective collaboration is at the heart of successful organisations.
When discussing obstacles to team collaboration, the biggest challenges identified were differences in personalities, lack of communication, and a high workload. “We have more and more regulations, more administrative work, and new demands put on the team,” she said. “As this happens, they often feel the workload they already have is not taken into consideration.
“One thing that really caught my attention when we did the survey was the clear need for communication,”
Reibel added, noting a link between team collaboration and meetings.
Of the 25% who reported rarely or never engaging with their teams, these individuals were generally the least satisfied with the quality of community in their workplace. They also reported lower feelings of recognition and a sense of not being valued by their peers and leaders.
Conversely, the survey found that those who reported having weekly or monthly meetings generally had a much more positive view of collaboration in their workplace. Despite citing high workloads and personality differences as obstacles, these individuals were generally more satisfied with their teamwork and felt a stronger sense of recognition.
When asked how to improve the effectiveness of their workplace, 43% of respondents suggested better-defined roles, 46% advocated for stronger leadership, 62% emphasised the need for improved communication, and 65% called for more training.
“Team members feel like they lack training in skills like communication, conflict management, the use of certain devices, and team building.”
Reibel wrapped up her presentation by reminding attendees, “Team collaboration is not just a means to an end—it’s a vital process to foster personal growth, and it’s an important way to bring the organisation success.”
Dury, S. (2024) Small health structures in the field of ophthalmology in Switzerland: a qualitative study describing the perception of employees on the functioning of management. [Master’s Thesis, University of Geneva].
The Origins of the Phacoemulsification Revolution
Heritage Lecture to explore the history of the innovative procedure.
This year’s ESCRS Heritage Lecture will recount the story of phacoemulsification from the moment its inventor, Dr Charles Kelman, conceived of it during a eureka moment in a dentist’s chair.
The lecture, “High Wire Act to the Standard of Care: Charlie Kelman and the History of Phacoemulsification,” will be delivered by Dr Richard Packard.
Dr Packard, who first started to perform phacoemulsification in 1979, qualified as a doctor in 1970 from the Middlesex Hospital Medical School after residency at Moorfields Eye Hospital. In December 1978 he went to Charing Cross Hospital as senior registrar, working under Eric Arnott.
Dr Packard retired as senior consultant at Arnott Eye Associates in London in 2022. He had been surgeon at the internationally renowned Prince Charles Eye Unit in Windsor, England.
In 1981, Dr Packard published the first description in the medical literature of the use of a folded soft lens in cataract surgery. Since then, he has continued to
teach phaco techniques as well as participate in the development of new intraocular lenses, phaco machines, and other instrumentation.
He was a board member of ESCRS from 1999 to 2007 and has chaired the ESCRS Video Competition Judging Panel since 2000. He is on the Society’s Education Committee and runs the Cataract Surgery Didactic Course.
He has lectured in more than 60 countries and presented many named lectures, including the IIIC Medal Lecture for 2014, the ESCRS Binkhorst Lecture in 2015, the Fyodorov and King Khaled Memorial Lectures in 2018, and the UKISCRS Choyce Medal Lecture in 2021.
In 2018 Dr Packard was the honoured guest of the American Society of Cataract and Refractive Surgery. In 2019, he published The History and Evolution of Modern Cataract Surgery with Lucio Buratto, with whom he published The History of Refractive Surgery the following year.
The lecture takes place at 10:30 in the Plenary Hall.

Inside ESONT’s Comprehensive 2024 Programme
Targeted sessions empowering ophthalmic professionals at this year’s Congress.
At meetings like the ESCRS Congress, the focus is often on ophthalmologists, which can leave other ophthalmic professionals sidelined. To address this oversight, the European Society of Ophthalmic Nurses and Technicians (ESONT) was founded, giving nurses, optometrists, technicians, and other specialists a space to connect, share knowledge, and grow their careers.
As an integral part of the Society, ESONT plays a key role in improving all aspects of ophthalmic care and enhancing patient outcomes worldwide. This year, ESONT is hosting a diverse programme of 10 courses, symposiums, and workshops covering topics such as implementing innovative technologies and managing unhappy patients.
“Ophthalmic nurses and technicians are dealing with a few big challenges right now, like keeping up with all the new developments in their field, especially in areas like cataract, cornea, and refractive surgery, where things are changing quickly,” explained Shanna Honings, ESONT programme committee member. “The ESCRS/ESONT programme was designed to help with these challenges. It offers sessions that provide the latest information on important topics in ophthalmology and gives professionals a chance to share their experiences and learn from each other. This is important for their growth and for maintaining high standards of care.”
The ESONT 2024 Programme
The ESONT programme kicked off Saturday with a biometry overview course chaired by Dr Nikos Astyrakakis, with insights from orthoptist Lynette Millbank. Immediately afterwards, attendees learned about imaging techniques from Dr Robert Jan Wijdh in “The ABCs of tomography and anterior segment OCT,” chaired by Sofi Navarro Santos and Susanne Albrecht.
The morning concluded with a symposium titled “Unhappy patient, expectations and outcomes of cataract surgery,” which covered topics such as predicting patient satisfaction, managing poor vision post-surgery, and understanding vision problems like positive and negative dysphotopsias. Speakers included Susanne Albrecht, Prof David O’Brart, and Dr Catarina Pedrosa.
After lunch, a session on managing complications addressed complex cases, including post-cataract surgery problems like double vision and complications from refractive surgery. The day wrapped up with a course about sustainability—led by Dr Andreia Rosa and Shanna Honings—that explored strategies for making highvolume surgeries and OR settings more sustainable.
Sunday began with a practical course on how to test vision chaired by orthoptists Clare Sheehan and Liz Tomlin, with speakers Dr Manuel Ruiss and Dr Carlo Bellucci. Next,
a Spanish symposium on myopia dived into managing and treating myopia, particularly in children.
A workshop on successfully implementing innovative technology guided participants through the process of evaluating, purchasing, and integrating new high-tech equipment into clinical practice, with insights from Dr Sheraz Daya. This was followed by a session on bilateral cataract surgery, where Dr Frank van den Biggelaar and Prof Rudy Nuijts explored the details of this approach.
The ESONT programme concluded with a session titled “How to Order, Perform, and Read Visual Fields,” featuring a workshop limited to 30 participants. Through this and other well-designed sessions, ESONT helped ensure every ophthalmic professional can continue to grow, contribute, and thrive in an ever-changing medical landscape.

What is your favourite part of the programme thus far?
Maria Artigues Martinez (Spain)
My favourite part of the programme so far has been the refractive surgery session. It’s always fascinating to hear about the latest advancements. The main symposium on the latest developments in IOL was also a highlight for me.
Laura Flores Villarta (Spain)
I really enjoyed the Young Ophthalmologist programme. It was dynamic and engaging, offering a fresh perspective for those early in their careers. The visual presentations were particularly impressive, making the content both accessible and impactful.
Enhance Your ESCRS 2024 Experience
Join leading experts for an in-depth look at two important issues in ophthalmic surgery: mastering complex cases in phacoemulsification and optimising astigmatism management in cataract surgery.
A panel of distinguished ophthalmic surgeons will share their expertise in each forum. Don’t miss these opportunities to enhance your ESCRS 2024 experience!
ESCRS PHACO IME FORUM Keys to Mastering Common Complex Cases
Monday, September 9th | 09:00 to 10:15 CEST Room 8.0 J | Fira Barcelona Gran Via, Spain
Optimizing Astigmatism Management in Cataract Surgery
Monday, September 9th | 13:00 to 14:00 CEST Room 8.0 J | Fira Barcelona Gran Via, Spain



Isofocal IOL Improves Depth of Focus with Little Visual Compromise
HOWARD LARKIN REPORTS
Apremium monofocal intraocular lens (IOL) using patented isofocal optical technology significantly improves intermediate vision with little impact on distance vision or quality of vision, Dr Robert Edward T Ang said in the EU Clinical Trial Spotlight Symposium.
The Isopure IOL (BVI/PhysIOL) applies negative spherical aberrations up to the 10th order across the full optic diameter of both the anterior and posterior optical surfaces, Dr Ang explained.
“There is a continuous increase in spherical aberration from the centre of the lens all the way to the periphery,” he said. “It is a progressively adjusted spherical aberration.”
Adjusting both surfaces allows customisation of the negative spherical aberrations to the specific power of the lens, fine-tuning the patient’s extended range of vision. This is important because the profiles of IOLs range from convex anterior surfaces for a higher power lens for short or hyperopic eyes to flatter or even concave anterior surfaces for lower power lenses for longer or myopic eyes. Posterior surfaces and optic position are also customised for each lens power, Dr Ang added.
Compared with a standard monofocal IOL, the Isopure increases depth of focus by about 50% with only a 12% decrease in maximum modulation transfer function (MTF), Dr Ang said, which is equivalent to approximately 1.0 D of extended depth of focus.
“There is no way we cannot sacrifice anything, so we gain some intermediate vision, but we also need to sacrifice a little light energy at distance.”
In a randomised single-masked study involving 250 patients comparing bilateral Isopure lenses with a comparable
Micropure standard monofocal design, 84.6% of Isopure eyes and 98.3% controls achieved binocular uncorrected distance visual acuity of 0.0 logMAR, Dr Ang reported. All members of both groups measured 0.2 logMAR or better.
At intermediate distances, the Isopure lens patients did better. At 80 cm, 55.4% of Isopure patients reached 0.0 logMAR compared with 16.3% of controls, and 96.9% and 77.4%, respectively, reached 0.2 logMAR. At 66 cm, 40% of Isopure patients and 14.5% of controls reached 0.0 uncorrected, and 90.8% and 71% (respectively) achieved 0.2 logMAR or better.
Regarding photic phenomena, halo and glare size were similar between the two groups. Binocular contrast sensitivity under mesopic conditions with glare was also nearly identical across all spatial frequencies. However, Dr Ang said photopic contrast sensitivity trended slightly lower at higher spatial frequencies.
“Our study shows we can target (very accurately) the refractive outcome with both lenses,” he concluded. “We give excellent visual acuity and contrast sensitivity for distance vision with similar photic phenomena, and, the Isopure provides better unaided intermediate vision performance.”
The study results were published in Clinical Ophthalmology in 2023.
Robert Edward T Ang MD is a senior consultant and head of cornea and refractive surgery, and research and training at the Asian Eye Institute, Makati City, Philippines.

Continue Your Journey with ESCRS!
Keep your professional journey moving forward after the Congress by becoming an ESCRS member.
You’ll join a network of leading ophthalmologists dedicated to advancing the science and business of cataract and refractive surgery.
For more information about ESCRS membership, visit the ESCRS booth in the exhibition hall or visit us online at escrs.org. You can also follow us on major social media outlets including LinkedIn, X, Facebook, and Instagram.

Call Open for Pioneer Research Award

The European Society of Cataract & Refractive Surgeons (ESCRS) is inviting ophthalmologists to submit applications for the Pioneer Research Award (PRA), which aims to support and encourage independent clinical research in the field of anterior segment surgery.
The competition is open to ophthalmologists and visual scientists up to the age of 45. Eligible participants must hold a full-time clinical or research position at a clinical or academic centre in the European region.
The purpose of the Pioneer Award is to—
• Support, encourage, and fund individuals interested in starting clinical research activities in the field of cataract and refractive surgery;
• Introduce and develop a body of clinical research work, addressing a challenging problem to devise a practical solution; and
• Facilitate and support an independent culture of study for the ultimate benefit of patients.
The Pioneer Award aims to fund various new initiatives, which may include:
• A novel research idea for the development of clinical trial studies;
• A non-interventional or observational study;
• A natural history/epidemiological study;
• A comprehensive series of retrospective case-control studies; and/or
• A patient or disease registry.
Successful applicants will receive up to €50,000 for a project with a project duration of no longer than two years.
How to Apply
Interested applicants are invited to submit their expressions of interest through the ESCRS PRA web page. An applicant to a PRA application requires clear reference to a current systematic review and meta-analysis, if available, published on the topic to which the applicant wishes to apply. Supervision of an established researcher is requested by ESCRS.
Deadline
Interested ophthalmologists have until 13:00 CET on 15 October 2024 to submit an application for the ESCRS Pioneer Research Award. Further details and the application form can be found on the ESCRS website. For additional information, please contact clinical.research@research.escrs.org.
The best of Barcelona
Memorable moments from the ESCRS 2024 Congress, capturing key connections and collaborations.









Can't-miss symposia!
IME symposia at ESCRS
Sessions will cover hot topics in cataract and refractive surgery.
Delegates will find a stimulating variety of clinical discussions by leading ophthalmic surgeons in the Independent Medical Education (IME) Symposia during the Congress. These sessions aim to provide balanced, non-branded, category-based education with expert faculty presenting meaningful, independent content for sincere peer-to-peer education. A common thread running through the various sessions is the use of information gained from the ESCRS Clinical Surveys.
Phaco IME Forum:
Location:
8.0 J, Fira Barcelona Gran Via
Date:
Monday, 9 September, 2024
Time: 9:00–10:15 CET
Grant Supporters: Alcon (Platinum), Zeiss (Bronze), Bausch + Lomb (Bronze)
Toric IME Forum:
Location:
8.0 J, Fira Barcelona Gran Via
Date:
Monday, 9 September, 2024
Time: 13:00–14:00 CET
Grant Supporters: Alcon (Platinum), Zeiss (Bronze)
Main Symposium
The final main symposium of the conference will focus on IOL Exchange Surgery. Hosted by Jorge L Alió and Filomena Ribeiro, topics include why IOL exchange is necessary, the treatment decision process, lens opacification, neuroadaptation failure, refractive surprise management, and whether to refix or exchange the lens.
IOL Exchange Surgery
Tuesday, 10 September, 11:00–13:00, room 8.0 A
The Orbis Symposium
Join Orbis Trustee John Ferris to learn how innovative solutions are improving access to high quality cataract surgery training across the globe, all of which are equally applicable to European training programmes! He’ll moderate an engaging session discussing democratising cataract surgery training and improving access in low- and middleincome countries.
The Orbis Symposium
Monday, 9 September, 10:30–12:00, room 8.0 A
Best of the Best
Ehud Assia and Oliver Findl will co-chair a session considering the best videos, papers, and posters from this year’s Congress. The session will feature dynamic discussions from presenters like Filomena Ribeiro, Sorcha Ní Dhubhghaill, Rafael Barraquer, Mayank Nanavaty, Sérgio Canabrava, Ruth LapidGortzak, Joaquín Fernández, among others.
Best of the Best
Tuesday, 10 September, 13:00–15:00, room 8.0 B
Today' s Congress Highlights
Day three of the 2024 ESCRS Annual Congress looks back and ahead, with Richard Packard delivering the Heritage Lecture and the main symposium examining the implications and opportunities of telemedicine in ophthalmology. Global issues are also on the programme, with sessions on democratising cataract surgery and training programmes across countries and continents.
Got some openings in your schedule? Check out these featured presentations.
PLENARY HALL
CSCRS Symposium: My Refractive Surgery Path 08:15 – 10:15
Heritage Lecture: Richard Packard 10:30 – 11:00
Main Symposium: Telemedicine in Ophthalmology 11:00 – 13:00
GLOBAL OPHTHALMOLOGY
Democratising Cataract Surgery in Low- and Middle-Income Countries
10:30 – 12:00, Room 8.0 A
Cataract Surgery Training Across the World 15:30 – 16:45, Room 8.1 N / Arena
SURGICAL PEARLS
Room 8.1 N
Surgical Pearls: Cataract 08:30 – 09:10
Surgical Pearls: Cataract 09:10 – 09:50
TABLAO ARENA
Room 8.1 N
Debate: A Simulated Curriculum is Mandatory! 14:50 – 15:30

BOSS: BUILDING OUR SUSTAINABLE, INCLUSIVE SOCIETY
Room 8.0 H
Leadership and Mentorship in an Inclusive Society 09:00 – 11:05
NOTES

STOP! Glaucoma Disease Progression
iStent ® technologies have been proven to stabilize visual fields loss and glaucoma disease progression with a favourable risk-benefit ratio1 -0.024
+3 YEARS FOLLOW-UP

15 STUDIES ON ISTENT TECHNOLOGIES
1,115 EYES

26.6 % MEAN IOP REDUCTION WAS SUFFICIENT TO ACHIEVE THIS FUNCTIONAL EFFECT
DBS/YEAR MEAN RATE OF PROGRESSION SIMILAR TO THAT REPORTED IN NONGLAUCOMATOUS EYES
1. Gillmann K, Hombeak DM. BMJ Open Ophth 2024;9:e001575.doi:10.1136/bmjophth-2023-001575. iStent inject ® W IMPORTANT SAFETY INFORMATION INDICATION FOR USE: The iStent inject ® W, is intended to reduce intraocular pressure safely and effectively in patients diagnosed with primary open-angle glaucoma, pseudo-exfoliative glaucoma or pigmentary glaucoma. The iStent inject ® W, can deliver two (2) stents on a single pass, through a single incision. The implant is designed to stent open a passage through the trabecular meshwork to allow for an increase in the facility of outflow and a subsequent reduction in intraocular pressure. The device is safe and effective when implanted in combination with cataract surgery in those subjects who require intraocular pressure reduction and/or would benefit from glaucoma medication reduction. The device may also be implanted in patients who continue to have elevated intraocular pressure despite prior treatment with glaucoma medications and conventional glaucoma surgery. CONTRAINDICATIONS: The iStent inject ® W System is contraindicated under the following circumstances or conditions: • In eyes with primary angle closure glaucoma, or secondary angle-closure glaucoma, including neovascular glaucoma, because the device would not be expected to work in such situations.
• In patients with retrobulbar tumor, thyroid eye disease, Sturge-Weber Syndrome or any other type of condition that may cause elevated episcleral venous pressure. WARNINGS/PRECAUTIONS:
• For prescription use only. • This device has not been studied in patients with uveitic glaucoma. • Do not use the device if the Tyvek® lid has been opened or the packaging appears damaged. In such cases, the sterility of the device may be compromised. • Due to the sharpness of certain injector components (i.e. the insertion sleeve and trocar), care should be exercised to grasp the injector body. Dispose of device in a sharps container. • iStent inject ® W is MR-Conditional; see MRI Information below. • Physician training is required prior to use of the iStent inject ® W System. • Do not re-use the stent(s) or injector, as this may result in infection and/or intraocular inflammation, as well as occurrence of potential postoperative adverse events as shown below under “Potential Complications.”
• There are no known compatibility issues with the iStent inject ® W and other intraoperative devices. (e.g., viscoelastics) or glaucoma medications. • Unused product & packaging may be disposed of in accordance with facility procedures. Implanted medical devices and contaminated products must be disposed of as medical waste. • The surgeon should monitor the patient postoperatively for proper maintenance of intraocular pressure. If intraocular pressure is not adequately maintained after surgery, the surgeon should consider an appropriate treatment regimen to reduce intraocular pressure. • Patients should be informed that placement of the stents, without concomitant cataract surgery in phakic patients, can enhance the formation or progression of cataract. ADVERSE EVENTS: Please refer to Directions For Use for additional adverse event information. CAUTION: Please reference the Directions For Use labelling for a complete list of contraindications, warnings and adverse events. ©2024 Glaukos Corporation. Glaukos, iStent inject ® and iStent inject ® W are registered trademarks of Glaukos Corporation PM-EU-0317

