March 2021 | Vol 26 Issue 3 SPECIAL FOCUS RETINA CATARACT & REFRACTIVE | CORNEA | GLAUCOMA PAEDIATRIC OPHTHALMOLOGY
RETINAL DYSTROPHIES
RAI Amsterdam, The Netherlands 27 – 30 August 2021
Abstract Submission Deadline: 15 March
www.escrs.org
Publisher
Carol Fitzpatrick
Executive Editor
Colin Kerr
Editors
Sean Henahan
Paul McGinn
Managing Editor
Caroline Brick
Content Editor
Aidan Hanratty
Senior Designer
Lara Fitzgibbon
Designer
Ria Pollock
Circulation Manager
Angela Morrissey
Contributing Editors
Howard Larkin
Dermot McGrath
Roibeard Ó hÉineacháin
Contributors
Maryalicia Post
Leigh Spielberg
Gearóid Tuohy
Priscilla Lynch
Soosan Jacob
Colour and Print
W&G Baird Printers
Advertising Sales
Amy Bartlett
ESCRS
Tel: 353 1 209 1100

email: amy.bartlett@escrs.org
Published by the European Society of Cataract and Refractive Surgeons, Temple House, Temple Road, Blackrock, Co Dublin, Ireland. No part of this publication may be reproduced without the permission of the managing editor.
Letters to the editor and other unsolicited contributions are assumed intended for this publication and are subject to editorial review and acceptance.
ESCRS EuroTimes is not responsible for statements made by any contributor. These contributions are presented for review and comment and not as a statement on the standard of care. Although all advertising material is expected to conform to ethical medical standards, acceptance does not imply endorsement by ESCRS EuroTimes. ISSN 1393-8983
The best of the best free papers and posters at the 38th Congress of the ESCRS Virtual 2020

P.35 CONTENTS A EUROPEAN OUTLOOK ON THE WORLD OF OPHTHALMOLOGY www.eurotimes.org PAEDIATRIC OPHTHALMOLOGY 30 Transplants for ocular surface diseases
Optic nerve anomalies to watch out for in paediatric patients REGULARS 33 Industry News 34 Inside Ophthalmology 35 Random Thoughts 36 Practice Management 38 My Life in Ophthalmology 39 Calendar SPECIAL FOCUS RETINAL DYSTROPHIES 4 Getting to grips with retinal dystrophies 6 Less severe hereditary retinopathies can result from subtle genotypic variants 8 A new era approaches in the treatment of inherited retinal diseases RETINA 10 Advanced treatments for macular holes in high myopia 11 On the front lines in the battle against COVID-19 12 The complicated and confusing area of pachychoroid 13 Dexamethasone shows promise in treatment of DME 14 Novel gene therapy can reduce injections for wet AMD 15 Promising results in trials for retinitis pigmentosa 16 The five ‘rights’ for artificial intelligence in ophthalmology 17 Diagnosis and treatment in high myopia
& REFRACTIVE 18
19 Online database for
power calculation continues to grow 20 The COVID-19 pandemic has had a heavy mental toll on physicians 21 Multifocal or monofocal intraocular lenses? 22 Weighing up lenticule removal or implantation for hyperopia 23 JCRS Highlights CORNEA 24 Takeaways from the latest information gathered by the ECCTR 25 Office-based procedures for Meibomian gland dysfunction 26 A history of antimicrobial agents 27 Nerve damage is at the root of post-refractive surgery neuropathy GLAUCOMA 28 Laser iridotomy vs lens removal in primary angle closure 29 Reactivating ‘silent’ neurons to reverse visual field defects P.5 As certified by ABC, the EuroTimes average net circulation for the 10 issues distributed between January and December 2020 was 46,748 EUROTIMES | MARCH 2021
31
CATARACT
IOL
MEDICAL EDITORS
Better times
Looking to the future and meeting once again
Iam delighted to be invited to write this Guest Editorial for the March issue of EuroTimes
The Special Focus in this issue is on Retinal Dystrophy, which will be one of the hot topics at EURETINA 2021 Virtual, which will take place from 10-12 September 2021.
The past 12 months have been very challenging for retina specialists, both personally and professionally, and with the rollout of COVID-19 vaccines across the world, we are hoping that we may gradually be able to return to normal in the months ahead.
We all hope and wish for the day when we can come together again for a “live” Congress where we can meet face to face, but the Board of EURETINA has considered the global outlook for the months ahead and decided to announce our second virtual Congress in September.
The first virtual Congress was a great success and we were very heartened by the feedback we received from more than 8,000 attendees. We have already started work on presenting a largely similar model to last year’s virtual Congress and specific details on the programme and meeting format will be announced in the coming weeks and months. We will also be developing attractive new features to enhance the virtual Congress experience so make sure to visit www.euretina.org for the latest news on EURETINA 2021 Virtual.
INTERNATIONAL EDITORIAL BOARD
Noel Alpins (Australia), Bekir Aslan (Turkey), Roberto Bellucci (Italy), Hiroko Bissen-Miyajima (Japan), John Chang (China), Béatrice Cochener-Lamard (France), Oliver Findl (Austria), Nino Hirnschall (Austria), Soosan Jacob (India), Vikentia Katsanevaki (Greece), Daniel Kook (Germany), Boris Malyugin (Russia), Marguerite McDonald (USA), Cyres Mehta (India), Sorcha Ní Dhubhghaill (Ireland)
Rudy Nuijts (The Netherlands), Leigh Spielberg (The Netherlands), Sathish Srinivasan (UK), Robert Stegmann (South Africa), Ulf Stenevi (Sweden), Marie-José Tassignon (Belgium), Manfred Tetz (Germany), Carlo Enrico Traverso (Italy)
Over the past 12 months we have seen increased use of online communications and emerging telemedicine tools. With that in mind, the EURETINA Roadmap 2025 will allow the Society to carry out a wide-ranging digital transformation in the years ahead. We will build and strengthen the value offered digitally to both members and non-members and set up the systems and tools that will help us to fulfil the needs of the Society today and for the next five-to-10 years.
The Roadmap 2025 is a very important document as it sets out an exciting vision of the future for EURETINA and I urge you to visit our website to see the full range and scope of our future plans.
I look forward to seeing you virtually in September and hopefully the day is not too far away when we can meet in person and talk about better times ahead.
Prof. Frank G. Holz, FEBO, FARVO President, EURETINA






EDITORIAL 2
GUEST EDITORIAL
Emanuel Rosen Chief Medical Editor
José Güell
Prof. Frank G. Holz
Thomas Kohnen
Paul Rosen
The past 12 months have been very challenging for retina specialists, and with the rollout of COVID-19 vaccines across the world, we are hoping that we may gradually be able to return to normal in the months ahead
A WORD FROM PROF. FRANK G. HOLZ FEBO, FARVO
EUROTIMES | MARCH 2021
46,748 * * Average net circulation for the 10 issues circulated between 1 January 2020 to 31 December 2020. See www.abc.org.uk Reach at a Glance The number of countries in which EuroTimes is distributed 169
RETINAL DYSTROPHIES
Retinal dystrophies (RD) present with visual loss ranging from night blindness, colour blindness, constricted fields, central scotomata to complete blindness. Affecting about one in 4,000 individuals, they may or may not be associated with syndromic manifestations. Mutations in more than 120 genes coding for proteins present or involved in retinal cells, rods and cones, phototransduction, visual cycle or gene regulation may be causative. Mutations within the same gene and even within the same family cause different phenotypic manifestations.
Inheritance is seen in all forms: autosomal dominant, recessive, X-linked as well as mitochondrial or digenic with sporadic cases also occurring. Genetic overlap may be seen between different non-syndromic RD.
Next-generation sequencing and chromosome microarrays provide better diagnostic abilities and pave the way for
genetic counselling, pre-natal diagnostics and therapy. Family history, proper phenotyping, electroretinogram (ERG), electrooculogram, dark adaptometry, colour vision, fundus autofluorescence imaging, spectral domain OCT (SD-OCT) and autoperimetry are helpful.
RD can be classified as rod-dominated, cone-dominated and generalised dystrophies.
ROD-DOMINATED RETINAL DYSTROPHIES
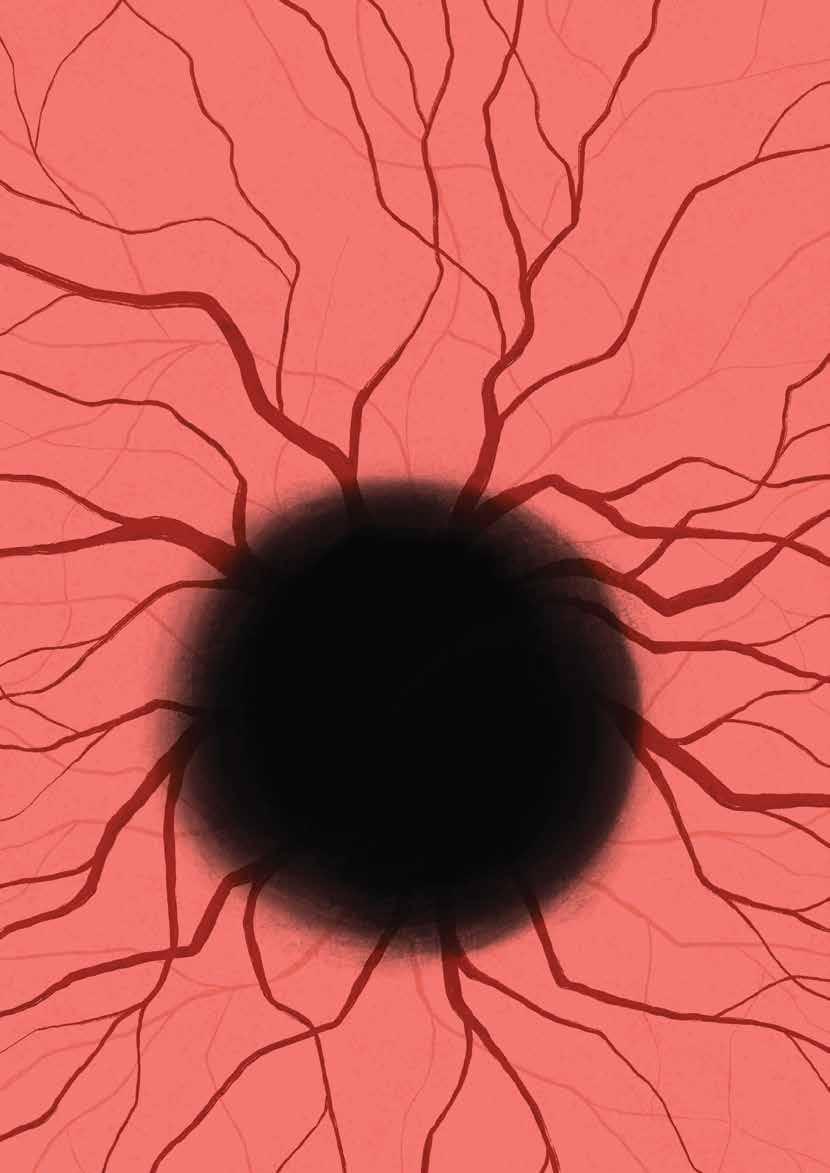
A genetically diverse group of disorders, these predominantly or first affect rods. Progressive (retinitis pigmentosa, RP) or stationary (Congenital Stationary Night Blindness, CSNB) forms occur. Patients with Retinitis Pigmentosa have early or late-onset progressive night blindness. Constricted fields and tunnel vision may progress to complete blindness if cones are also involved in the late stages. Retinal arteriolar attenuation, bone spicule intra-
retinal pigmentary changes, waxy pale disc, tessellated fundus, unmasking of large choroidal vessels and sometimes atrophic or cellophane maculopathy and cystoid macular oedema (CME) are seen. A golden metallic tapetal sheen may be seen in female carriers of X-linked disease. Posterior subcapsular cataract, high myopia, astigmatism, keratoconus and glaucoma are associated with RP. ERG shows reduced scotopic and combined responses progressing to decreased photopic responses and finally extinguished waves. Large ERG amplitudes imply good prognosis for retention of central vision. SD-OCT shows decreased ONL thickness and loss of ELM and IS/OS junctions and correlates with microperimetry and multifocal ERG. SD-OCT is also used to evaluate CME and epiretinal membranes. Syndromic associations such as Bassen-Kornzweig, Refsum, Kearns-Sayre and Bardet-Biedl syndromes are seen. Regular visual assessment is required for RP patients who drive.
EUROTIMES | MARCH 2021 SPECIAL FOCUS: RETINAL DYSTROPHIES 4
Classifying and identifying retinal dystrophies can be difficult but necessary. Soosan Jacob, MS, FRCS, DNB reports
Congenital Stationary Night Blindness shows autosomal dominant, recessive, incomplete and complete form of X-linked inheritance. Affected patients have non-progressive nyctalopia, decreased vision, nystagmus, strabismus, myopia, photophobia and colour vision impairment. Two variants exist – with normal fundus (Nougaret, SchubertBornschein and Riggs-types) and with abnormal fundus (fundus albipunctatus and Oguchi’s disease). Mizuo-Nakamura phenomenon refers to a golden sheen that disappears after a prolonged period of dark adaptation and is seen in Oguchi’s disease. There is currently no specific treatment for CSNB, though 9-cis retinal has been tried to potentially stabilise photoreceptors.
CONE-DOMINATED RETINAL DYSTROPHIES
These result in loss of central vision and colour vision and therefore are more severe. Progressive cone (COD) or cone-rod dystrophy (CORD) are rare but may occur sporadically or with autosomal dominant, recessive or X-linked inheritance patterns. Presenting in the first to second decades, patients with CORD worsen further when rod involvement also starts. Macular atrophy or pigment deposits are seen. ERG shows decrease in photopic response and flicker fusion frequency. Stationary cone dystrophy results in complete or incomplete achromatopsia with loss of all colour perception or of only specific colours.
GENERALISED DYSTROPHY
Simultaneous involvement of both rod and cone receptors is seen, often associated with progressive and severe involvement of visual functions. Leber’s congenital amaurosis (LCA) has onset at birth or within the first year of life and has very poor visual prognosis. Nystagmus, severe visual loss and absent responses on ERG are seen. An initially normal fundus may progress to macular
pigmentation, peripheral chorioretinal atrophy, mild pigmentary retinopathy, arteriolar attenuation and other changes. Repeated poking of the eyes is called the Franschetti’s oculo-digital sign. ERG is generally non-recordable. Intellectual disability, deafness and other systemic associations may be seen. Choroideremia is X-linked and shows progressive, diffuse degeneration of the choroid, RPE and retinal photoreceptors. Patients present in the first decade with night blindness and generally have severe visual loss after about 50 years of age.
MACULAR DYSTROPHY
This refers to a group of conditions with Mendelian inheritance, pathology limited to the eye and with bilateral and generally very symmetrical macular lesions. It includes Best, Stargardt, PROM1 associated disease, Sorsby, pattern dystrophy and others. When considering macular dystrophy, neuronal ceroid lipofuscinosis and drug toxicity should be ruled out by appropriate history and investigations.
TREATMENT
Corrective lenses, low-vision aids, disease course as well as genetic counselling, occupational and psychosocial support are necessary. Different filtered contact lenses, e.g., low light transmitting orange or red for achromatopsia and blue light filtering sunglasses for Stargardt may help. Drugs that modulate the visual cycle such as isotretinoin and fenretinide may be used in some conditions. Though a nutritious and well-balanced diet is recommended, there is no clear consensus. High-dose Vitamin A and carotenoids may modestly slow progression of RP; however, it is not recommended because of lack of definite evidence and possible toxicity. Vitamin A should be avoided by patients with Best and Stargardt dystrophies as it may cause exacerbation by increasing formation of bisretinoids. Vitamin E
supplementation is beneficial in BassenKornzweig syndrome with neurological manifestations. Plasmapheresis and a phytanic-acid-free diet is advised in Refsum disease. An arginine-restricted diet and oral Vitamin B6 supplementation is used in gyrate atrophy. Acetazolamide may be used for CME associated with RP. AntiVEGF therapy may be given for choroidal neovascular membranes in Best, Sorsby fundus dystrophy etc.
Newer treatment strategies directed towards stem cell and gene-based treatments are in trials. Luxturna (Spark Therapeutics) provides RPE65 gene replacement therapy delivered by viral vectors to restore the visual cycle in children with early stage LCA and has shown promise. Functional cDNA has also been delivered to the retina via viral vectors. With advanced disease or extensive involvement, gene therapy is not effective and pluripotent stem cell transplants or retinal implants may be tried. Subretinal transplantation or intravitreal injections of human embryonic stem cell-derived retinal pigment epithelial cells, autologous bone marrow-derived mononuclear cells, undifferentiated umbilical cells etc. are under trial. Application of CRISPR technology with stem cells may allow individualised and targeted treatment.
Retinal prosthetics, e.g., light-sensing microchips are implanted into the retina and transmit impulses via the remaining neural network to the brain. The Argus II Retinal Prosthetic System is one such example. These are used in advanced cases and have had success in restoring some visual perception or improvement in light detection. An intraocular implant releasing ciliary neurotrophic factor (CNTF) has been tried for CSNB.
Dr Soosan Jacob is Director and Chief of Dr Agarwal's Refractive and Cornea Foundation at Dr Agarwal's Eye Hospital, Chennai, India and can be reached at dr_soosanj@hotmail.com
EUROTIMES | MARCH 2021 SPECIAL FOCUS: RETINAL DYSTROPHIES 5
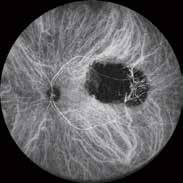
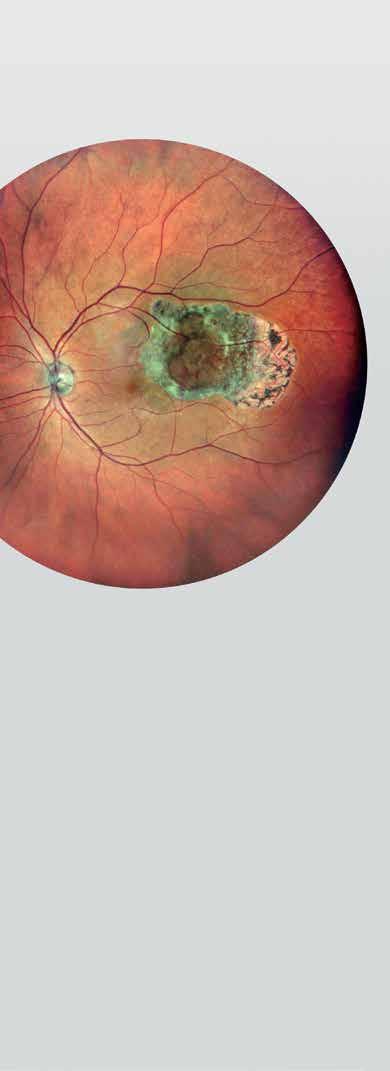
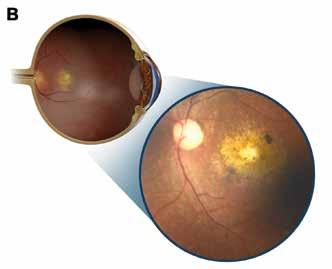
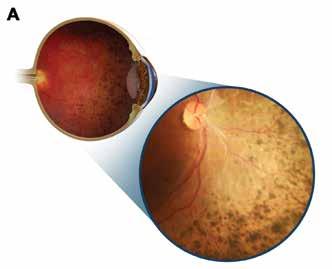
Illustrations and inset images showing retinal dystrophy with predominant mid-peripheral (A) and central (B) involvement
Inherited retinal disease
Not all hereditary retinopathies show their typical, severe phenotype and maculopathy in some cases might present at the mild end of the disease’s spectrum, according to Bart P Leroy Ghent MD, PhD, University Hospital and Ghent University Ghent, Belgium.

“Mild end-of-the-spectrum retinal disease can result from pathogenic genetic variants with milder effects than the usual phenotype. The genotypic spectra of these conditions are also wider than we initially thought,” Dr Leroy told the Retina 2020 meeting, funded by the Irish patient-led charity, Fighting for Sight.
The diagnostic process in cases of suspected hereditary retinal dystrophies begins with asking patients the right questions in language they can understand about the nature of their visual complaints and the time of onset, he noted. Also important is drawing a pedigree and looking for potential causes for the disorder with specialised imaging. In addition, patients should undergo functional testing with psychophysics and electrophysiology. The clinical diagnosis should be confirmed with genotyping.
Ocular genetics has identified 307 genes for inherited retinal and optic neuropathy diseases, Dr Leroy said. He added that ocular genetics has come a long way in recent years. In particular, high-throughput molecular sequencing technology, such as whole exome sequencing, is rapidly replacing the older, Sanger sequencing.
In cases where the diagnosis is uncertain, the technology can be used to find the subtle variants of a suspect gene as well as pathogenic variants of unsuspected genes. The variants can include deep intronic variants in regulatory sequences, deep intronic mutations or subtle copy number variations. The molecular findings should be interpreted in the context of the clinical presentation, Dr Leroy said.
“Whole exome sequencing can be very powerful tool, but you have to be aware of how you communicate to patients that not all the variants identified are pathogenic and sometimes the laboratory is unable to say what is the real cause of the disease. What you then have to try and do is correlate what you see clinically with what you have genetically,” he added.
MILD STARGARDT DISEASE
Dr Leroy presented a few case studies to illustrate his approach to the diagnosis of hereditary retinopathies. In the first case, a 23-year-old woman was referred with a possibly inherited maculopathy, indicated by the presence of bilateral, relative, central scotoma. She had a best-corrected visual acuity of 10/10 vision in both eyes with no change over the past two years.
Her medical check-up was normal. Goldmann visual field showed some relative scotomata. Conventional fundoscopy showed no abnormalities. However, deep phenotyping with near-infrared autofluorescence imaging showed flecks in the central fovea area and the surrounding macula. Optical coherence tomography (OCT) also showed abnormalities in the central foveal region in both eyes.
Colour vison testing showed no abnormalities and full-field flash ERG was also normal. However, molecular testing showed the patient had two heterozygous and likely pathogenic variants of the ABCA4 gene, leading to diagnosis of mild Stargardt disease.
In another case, a five-year-old child was referred with central visual loss occurring over the previous six months with a diagnosis of Stargardt disease. Fundoscopy revealed an abnormality in the central area macula that grew over the course of two years’ follow-up. OCT showed outer retinal layer loss and flash electroretinography (ERG) was abnormal for both rods and cones.
Molecular genetic screening showed one variant of unknown significance on one allele of the gene ABCA4. However, not convinced of the Stargardt disease diagnosis, Dr Leroy and his associates performed whole exome sequencing. It revealed biallelic mutations in the MFSD8 gene, variants of which cause neuronal ceroid lipofuscinosis 7 (NCL7).
“Isolated maculopathy can be an early sign of a rapidly evolving retinal dystrophy suggestive of neuronal ceroid lipofuscinosis, before systemic signs develop,” he said.
Dr Leroy also described the case of an 18-year-old female patient who had diagnosis of retinal dystrophy at four years of age and now complained of a slowly progressive decrease in visual acuity in both eyes. She was referred by a uveitis specialist who wanted to determine if her condition was a dystrophy or was inflammatory.
Her best corrected vision was 5/10 in her right eye and 1/10 in her left eye. Fundoscopy showed a very abnormal lesion with yellowish discoloration. Blue-light autofluorescence showed satellite lesions the appearance did not change over time. Full-field flash ERG was fairly normal as was electro-oculography (EOG), indicating normal function of the pigment epithelium together with the photoreceptors.
In both eyes OCT showed a thinning and atrophic area with a conserved foveal depression. Whole exomal sequencing showed that the patient was compound heterozygous for two variants, one in exon four and one on exon six of RDH12, the Leber congenital amaurosis gene.
“I’m sure with the advent of such screening tools more surprises are ahead for us ophthalmic genetic specialists,” Dr Leroy predicted.
Less severe hereditary retinopathies can result from subtle genotypic variants. Roibeard Ó hÉineacháin reports
EUROTIMES | MARCH 2021 SPECIAL FOCUS: RETINAL DYSTROPHIES 6
Mild end-ofthe-spectrum retinal disease can result from pathogenic genetic variants with milder effects than the usual phenotype
Bart P Leroy Ghent MD, PhD
10-12 September www.euretina.org Abstract Submission Deadline: Friday 30 April, 23.59 CET
At the cutting edge of GENE THERAPY TREATMENT

A new era approaches in the treatment of inherited retinal diseases.
Leigh Spielberg MD reports
The introduction of retinal gene therapy into the clinic has been a major game changer in the field of ophthalmic genetics,” said Professor Camiel Boon MD, PhD, of Leiden University Medical Centre and Amsterdam University Medical Centre.
Dr Boon, who is a Professor of Ophthalmology and Clinical Ophthalmic Genetics, is an expert on retinal dystrophies and works on the cutting edge of this blossoming and dynamic field.
This major therapeutic advance has been received as excellent news to those of us who have ever had to gently suggest to a patient with an inherited retinal disease (IRD) that there is little hope of ever recovering lost vision or even maintaining what they currently have.
Inherited retinal diseases include retinal dystrophies, which are chronic, progressive disorders and include diseases such as Leber’s congenital amaurosis and
Voretigene neparvovec (Luxturna, Spark Therapeutics) heralds a new era, both for retinal dystrophies specifically and for human gene therapy in general
Professor Camiel Boon MD, PhD

retinitis pigmentosa. They are collectively caused by mutations in over 200 different genes, and had previously been considered untreatable. Recent advances such as the prospect of gene therapy, however, have been providing hope.
GENE THERAPY
“Voretigene neparvovec (Luxturna, Spark Therapeutics) heralds a new era, both for retinal dystrophies specifically and for human gene therapy in general,” said Dr Boon, referring to the novel gene therapy for
patients with vision loss due to biallelic RPE65 mutation-associated retinal dystrophies who have sufficient viable retinal cells. The genetic material is delivered into retinal cells via an adeno-associated virus (AAV) vector, which is injected subretinally.
The introduction of voretigene neparvovec has been widely reported, and many patients are now aware of the possibilities available.
Professor Bart Leroy agrees. “The initial success of gene therapies using AAV vector systems, as well as novel technologies such
EUROTIMES | MARCH 2021 SPECIAL FOCUS: RETINAL DYSTROPHIES 8
as antisense oligonucleotides, represent major breakthroughs. We have first-hand experience with both, and these successes have led to an explosion of clinical trials for a multitude of IRDs, which will hopefully benefit our patients as soon as possible.”
Dr Leroy MD, PhD, is an ophthalmologist and clinical geneticist who splits his time between the Ghent University Hospital in Belgium, where he is chairman of the ophthalmology department, and Professor of Ophthalmology & Ophthalmic Genetics, and The Children’s Hospital of Philadelphia (CHOP), where he is director of the Ophthalmic Genetics & Retinal Degenerations Clinics. Voretigene neparvovec was developed by Spark Therapeutics and the team at CHOP.
WHAT WILL THE FUTURE HOLD?
But those on the cutting edge are not content to rest on their laurels. Professor Leroy said that, “Apart from the classic AAVmediated gene augmentation therapies, I’m very much looking forward to an era of other custom treatments becoming more widely available. These include antisense oligonucleotide therapies, which act as a molecular patching technique at the RNA level, and CRISPR/Cas9 gene editing, as well as generic gene therapies where artificial photoreception is induced using photosensitive pigment genes ectopically expressed in the remaining bipolar or ganglion cells of the retina of IRD patients.”
Professor Boon also drew attention to the rapid advances currently being made in patient-derived induced pluripotent stem cell-based retinal organoids.
“These represent a huge advantage as a personalised in-vitro disease model that can be used to test all manner of genetic treatment strategies,” he said.
DIAGNOSTICS AND FOLLOW-UP
The advances have not been limited to therapeutics; diagnostics and follow-up modalities have also further been refined.
Dr Leroy explained: “Blue and nearinfrared light autofluorescence (BAF & NIRAF) imaging are the mainstay of imaging of IRDs, and their importance cannot be overestimated. Indeed, these techniques allow one to evaluate evolution of disease with or without functional testing. In addition, optical coherence tomography remains essential to estimate whether outer retinal cells are still present in sufficient numbers for gene therapies to be beneficial.”
But how are the results of these therapies evaluated? In other words, how do we quantify the results? Identifying reliable clinical outcome measures to assess the efficacy of gene therapy will also remain the focus of many researchers’ attention.
Professor Leroy clarified this for me: “Fullfield sensitivity testing has emerged as a straightforward outcome measure to evaluate effects of genetic therapies, and correlates well with more time-consuming
outcome measures such as multiluminance mobility testing (MLMT).” Dark-adapted chromatic perimetry and microperimetry have also proven their value, he added.
Dr Boon is not yet satisfied. “But we also have a strong need for more patientreported outcome measures as well as more large-scale natural history studies, both retrospective and prospective, for more information on the diseases’ natural course and prognoses,” he said.
Dr Boon pointed out that such largescale European collaborations represent a great example of how investigator-initiated research can also help to implement gene therapy in the clinic by delineating IRDs, their clinical characteristics and their natural history. Dr Boon is involved in a range of such multi-centre natural history studies with both national reach (the Dutch RD5000 Expertise Centre Database) and international stature such as the European Reference Network for Rare Eye Disease (ERN-EYE). Dr Leroy is also involved in ERN-EYE and the European Retinal Disease Consortium (ERDC) and European Retinal Treatment Consortium (ERTC).
Both are also very enthusiastic about the rapidly evolving digital support systems that may help patients with severe vision loss, such as the OrCam MyEye, a voiceactivated device that attaches to the wearer’s glasses and conveys visual information audibly in real time.
“We are currently performing studies on the usefulness of such aids in IRD patients,” said Dr Boon.
ONGOING CHALLENGES
And what keeps retinal dystrophy researchers like Professors Leroy and Boon up at night? What are the challenges that lie ahead?
“A major diagnostic problem is that we’re still unable to locate the causative gene in a sizeable number of patients, despite the use of the newest DNA diagnostics techniques such as wholegenome sequencing. This means that up to 30% of recessive retinitis pigmentosa cases remain unsolved,” said Dr Boon.
“Here lies a big future challenge in the field: how to find the causal gene in the big and complex soup of genes and more 'obscure' genetic regions in our human genome,” he asked. “This is a problem that will have to be solved by bio informatics,” computer-based calculations that will be able to identify the offending gene.
Professor Leroy, however, seems hopeful. “With the advent of easily accessible broad spectrum genetic screening, we are now picking up more pathogenic variants in genes than ever before in patients with IRDs.”
WHAT’S NEXT?
I asked Professor Leroy whether there are interesting therapeutic options that have been developed or are in testing or due for approval sometime soon. “I believe we’ll be seeing new viral vectors which are more efficient in transfecting the outer retinal cells even after intravitreal injection,” rather than only via subretinal injection. “Indeed, subretinal injections for photoreceptor or RPE-based disease are both more difficult and cause more complications than administration via an intravitreal approach.”
Dr Boon suggested that, despite the major strides that have been made and the further advances that we can expect, the maxim of “under-promise and over-deliver” still applies. Nevertheless: “It’s a great time to work in this rapidly-evolving, cutting-edge research field.” Indeed, “The conversations that I have with patients in my ophthalmic genetics clinic have recently changed considerably, because many patients are eager to know more about these hopeful developments.”
“I would certainly say that since we have now reached the era of interventional therapies for rare disorders such as IRDs, never has there been a more exciting time to be in ophthalmic genetics,” concluded Professor Leroy.

EUROTIMES | MARCH 2021 SPECIAL FOCUS: RETINAL DYSTROPHIES 9
The initial success of gene therapies using AAV vector systems, as well as novel technologies such as antisense oligonucleotides, represent major breakthroughs
Professor Bart Leroy MD, PhD
Blue and nearinfrared light autofluorescence (BAF & NIRAF) imaging are the mainstay of imaging of IRDs, and their importance cannot be overestimated
Professor Camiel Boon MD, PhD
Treatment options for macular holes
Special kit greatly reduces previous problems with plasma preparation.
Leigh Spielberg MD reports
In this year’s Kreissig Lecture, Prof Dr Marta S. Figueroa presented her procedural refinement of an advanced surgical approach to the most challenging macular holes in high myopia. Her lecture, entitled “Plasma Rich in Growth Factors for Macular Holes in High Myopia,” was delivered live at the EURETINA 2020 Virtual Meeting.
Dr Figueroa, of the Hospital Universitario Ramón y Cajal, Madrid, Spain, is a highly regarded vitreoretinal surgeon and this year’s recipient of the Kreissig Award. The award is given for outstanding contributions in the understanding and treatment of retinal diseases.
“The use of autologous adjuvants, such as platelet-concentrate, is not a novelty in the treatment of macular holes. However, despite promising results this technique has not yet been widely adopted by clinicians,” she said. “This is due to profound limitations such as time-consuming preparation of the adjuvants, unpredictable intraocular biologic activity and inconsistent platelet concentration.”
However, these limitations can be overcome using a readyto-use autologous platelet-rich plasma closed system such as the Endoret kit. This offers simpler and faster centrifugation processes and ensures activation of the platelet-rich plasma, leading to the desired product: “plasma rich in growth factors” (PRGF).
The procedure is straightforward and efficient: the patient’s blood sample is collected and immediately centrifuged in the Endoret machine. The platelet-rich plasma fraction is collected and then “activated” by Endoret-PRGF activator to obtain PRGF.
“PRGF results in quicker, more controlled and more predictable fibrin formation and platelet degranulation, which is what helps close the macular holes,” said Dr Figueroa.
“Once the PRGF fluid has been prepared, we perform a fluid-air exchange and release three drops of PRGF over the macula,” she explained as a video of the procedure was shown. Approximately five minutes after injection, fibrin formation becomes visible over the macula of the eye as a whitish membrane. It is this fibrinous fluid that helps close the macular hole.
Dr Figueroa described the results of her study, an interventional case series in both treatmentnaïve, high-myopic macular holes (Group 1) and persistent, highmyopic macular holes after vitrectomy with ILM peeling (Group 2)
treated with PRGF as an adjuvant to the surgery.
In both groups, ILM peeling was performed (or extended, as in Group 2), followed by fluid-air exchange. After the addition of PRGF over the macular hole, either C3F8 (Group 1, n=31) or silicone oil (Group 2, N=11) was used as a tamponade, followed by supine positioning for 30 minutes postoperatively and face-down positioning for 15 days.
“In the full cohort of patients, the macular hole closed in 90% of the cases. The external limiting membrane in the macular hole region recovered in 69% of cases, and the ellipsoid zone in 48%, with a corresponding improvement in visual acuity from LogMAR 0.82 to 0.54,” she reported.
Considering the difficulty of closing this type of high-myopic macular holes, these are impressive results.
The PRGF is clearly visible on the postoperative OCT scans as what looks like a hyper-reflective fibrinous membrane located above, within, and, in the retinal detachment cases, under the macular hole. The PRGF disappears several weeks later, upon closure of the macular hole.
Dr Figueroa and colleagues also investigated whether PRGF might be useful for macular hole retinal detachment. Starting with highmyopic eyes with macular holes associated with very small, shallow retinal detachments, she and her team then progressed to more challenging cases with large holes and large bullous detachments.
Showing a video of the sort of macular hole retinal detachments that tend to keep vitreoretinal surgeons awake at night, Dr Figueroa demonstrates how she aspirates the subretinal fluid through the macular hole and then instils five drops of PRGF over the highly staphylomatous posterior pole. These cases call for silicone oil tamponade.
Possible mechanisms of macular hole closure with PRGF include a mechanical mechanism, in which activated PRGF forms a fibrin clot acting as a physical barrier, similar to an ILM flap; and a biological mechanism, in which the trophic factors present in PRGF, may enhance Müller cell activation.
A renowned member of the audience, Dr Alistair Laidlaw, asked: “Do you use this technique in holes not associated with myopia?” Dr Figueroa replied that she does, particularly in large, persistent holes.
“As shown by the excellent surgical outcomes attained in our series, we believe that the healing capabilities of PRGF are especially useful for macular holes in highly myopic eyes, even in cases of primary surgical failure in which the ILM has already been peeled, as well as in macular hole retinal detachment cases,” she concluded.
Marta S. Figueroa: figueroa@servicom2000.com
EUROTIMES | MARCH 2021 RETINA 10
PRGF results in quicker, more controlled and more predictable fibrin formation and platelet degranulation, which is what helps close the macular holes
Prof Dr Marta S. Figueroa
In the full cohort of patients, the macular hole closed in 90% of the cases
Prof Dr Marta S. Figueroa
Retina in the pandemic
Schepens Lecture describes a subspecialty overcoming multiple challenges. Howard Larkin reports
For Julia A Haller MD, the relentless march of COVID-19 down the eastern seaboard of the United States in the early days of the pandemic brought to mind Winston Churchill and the London blitz as described by Erik Larson in “The Splendid and the Vile.”

“It felt as if there were uncanny parallels between the unrelenting bombardment of London in the 1940s and the onslaught of coronavirus. Shops were shuttered, traffic was absent and we were facing a foe as menacing as any squadron of approaching Nazi Messerschmitts. The COVID blitz was upon us,” said Dr Haller in the Charles L Schepens lecture at AAO 2020 Virtual Retina Subspecialty Day. In addition to his transformational contributions to vitreoretinal surgery, Dr Schepens was himself a resistance fighter who helped dozens of refugees escape during the second world war, she noted.
“We found ourselves in a different but very real war, the COVID-19 pandemic, in which our field of retina has stood on the front lines of battle fighting blindness,” said Dr Haller, who is ophthalmologistin-chief at Wills Eye Hospital and chair and professor of ophthalmology at Sidney Kimmel Medical College at Thomas Jefferson University, both in Philadelphia, USA. As to her own role in her subspecialty’s response to the pandemic, Dr Haller quoted Churchill, who in 1954 said: “It was the nation that had the lion’s heart. I had the luck to be called upon to give the roar.”
Dr Haller detailed Wills’ response to the pandemic as an example of the order of battle.
“We closed our ambulatory surgery network, funnelled all entrants into one access point at Wills, created new signage, posted encouraging safety messages and informational videos online, and conducted a warp-speed makeover, with hand sanitising and screening at the entrance, masking for one and all, distanced standing and seating, even an elevator attendant who wiped down the buttons with disinfectant and warmly welcomed our patients to their allotted spots.”
Overall, ophthalmology was the medical specialty most affected by limiting care to urgent and emergency only, Dr Haller noted. Surgery volumes plummeted 81% with the nadir in April and mid-May, followed by an upturn in June and July, returning to normal

volumes in October. Retinal surgeries also declined but accounted for more than their normal proportion during the downturn.
Wills’ scholarship also continued, with the pandemic itself a major new research focus, Dr Haller said. Among the topics were a study of how academic and private practices across the USA responded to requests for appointments for refraction, cataract evaluation and posterior vitreous detachment during the first viral wave as of 30 April 2020.
“They found resounding compliance with AAO guidelines both for types of care and COVID safety screening.” (Starr MR et al. JAMA Ophthalmol. 2020;138:981-988.)
Remote patient care technology also flourished. “We used the pandemic to permanently expand our portfolio of telemedical solutions. As our oncology service, led by Dr Carol Shields, put it, ‘Cancer never stops and neither do we,’” Dr Haller said.
Using a hybrid model, the Wills oncology service opened testing sites with telemedical review and consultation. In the Emergency Department, analysis of a remote phone-triage system for evaluating eye problems found that it significantly improved the accuracy of diagnosis for sight- and life-threatening emergencies (Deaner JD et al. Ophthalmology. 2020 Jul 27. Epub ahead of print).
Yet another Wills study found that patients seen for emergency problems during the stay-at-home orders were more likely to lack insurance, travel farther to seek care and have a delay in presentation, Dr Haller reported.
“Truly, our patients faced a host of new challenges in this pandemic.” (Wu C et al. Curr Opin Ophthalmol. 2020 Sep;31(5):423-426.)
Analysis of more than 2 million retina patient records found that the changes Wills experienced were widespread across the USA, Dr Haller said. Retinal outpatient visits, new patient visits, intravitreal antiVEGF injections and imaging declined in
the early stages of the pandemic, though injections declined less than office visits (Xu D et al. Curr Opin Ophthalmol. 2020 Sep;31(5):427-434).
Through October, new patient visits nationally were affected more severely than existing patient visits. Moreover, mean visual acuity was reduced for new patients in the COVID era compared with before. Similarly, due to treatment delays, detached retinas treated at Wills were more likely to present macula-off and with primary PVR during the pandemic than in the year before (Patel LG et al. Ophthalmology 2020 Oct 13. Epub ahead of print).
Training and continuing education went online as well, resulting in an actual increase in attendance at many retina conferences, Dr Haller said. Clinical trials also have rebounded following a drop off in the early pandemic.
“Retina has risen to the challenges to every aspect of our mission with leadership and courage … Good job, Retina, in this pandemic. Keep on roaring!” Dr Haller concluded.
EUROTIMES | MARCH 2021 RETINA 11
It felt as if there were uncanny parallels between the unrelenting bombardment of London in the 1940s and the onslaught of coronavirus
Julia A Haller MD
Courtesy of Julia A Haller MD
A patient receiving intravitreal injections with a surgical mask taped to his face
Ambiguity of pachychoroid
New findings will significantly change ideas about central serous chorioretinopathy and allied diseases. Leigh Spielberg MD reports
This year’s EURETINA Lecture was delivered at the EURETINA 2020 Virtual Meeting by Richard Spaide MD, who took a hard look at the meaning of pachychoroid.

It turns out that pachychoroid is more complicated and confusing than we had previously thought, and Dr Spaide helped set the record straight.
What is pachychoroid, exactly? Dr Spaide, based in New York City, had the same question in mind when he decided to review all papers published between September 2013 and April 2020 and available on PubMed.
“Curiously, 17 of the 47 papers about pachychoroid contained no actual definition of pachychoroid. “Choroidal thickening” was the definition for seven papers. Another 19 papers defined the amount of choroidal thickness in micrometers without any agreement about how thick the choroid should be to be considered pachychoroid,” he said. The thresholds were set at levels that were normal or even below normal levels for choroidal thickness.
Still other papers defined pachychoroid based simple on the appearance of the choroid, such as the presence of directly visible pachyvessels with or without choroidal vascular hyperpermeability.
“This resulted in the remaining 30 papers containing a total of 22 different definitions for pachychoroid. Many of these definitions would end up classifying normal eyes as having pachychoroid.”
One of the integral components of pachychoroid is pachyvessels, but
there was a similar disagreement in papers regarding the definition of the latter.
“In a total of 25 papers on pachyvessels, five papers had no definition, eight papers had a simple definition and 12 papers contained seven complex definitions of the condition.”
Dr Spaide also questioned the precision with which a subgroup of choroidal vessels, the choriocapillaris, could be measured. Since the axial resolution of the most precise OCT devices is currently no smaller than 7 microns, it is not possible to see thinning of the choriocapillaris with the current generation of OCTs.
“What about other causes of a thick choroid?” he asked. “More than 20 distinct conditions, such as Vogt-Koyanagi-Harada syndrome, nanophthalmos, and domeshaped macula in pathologic myopia, cause either generalised or focal thickening of the choroid, but are not considered to be pachychoroid syndrome.”
More recently, the definition of pachychoroid has been expanded. “In fact, the choroid does not even have to be thick to be considered pachychoroid.” So, what does it have to be? Dr Spaide suggested choroidal vascular hyperpermeability, but, he countered, “this occurs in more than 20 different, unrelated conditions that are not included in the pachychoroid spectrum – why not?”.
“So, I think you’ll agree that pachychoroid spectrum is incomplete, poorly defined and lacks thematic focus. Is it even a spectrum if most of the entities that could be included are not?”
Dr Spaide suggested that the term ‘pachychoroid’ might have utility as a term simply used to describe things, much like the term “white-dot syndrome”.
Dr Spaide then shifted his focus from choroidal thickness to the choroidal circulation itself, in which both the arterial supply and the venous drainage are segmental. Experimental occlusion of vortex veins shows poor communication between adjacent systems. In non-pathologic eyes, they are separated by watershed zones between the vortex veins where large vessels do not normally cross.
However, in central serous chorioretinopathy (CSC), large intervortex
venous anastomoses are present. These are big vessels that cross the watershed zones and are concentrated in the macular region. In peripapillary pachychoroid syndrome, there are anastomotic vessels around the nerve.
In cases of CSC that have resulted in choroidal neovascular membranes, “giant” anastomotic vessels can be seen on indocyanine green angiography (ICG). Similar findings can be seen in cases in which CSC has progressed to polypoidal choroidal vasculopathy (PCV).
An online viewer asked, “Do these anastomoses form in a neovascular fashion?” Dr Spaide answered: “No, they seem to represent expansion of previously existing channels, and the pulsatile motion of the blood flow suggests that there might be a venous outflow problem in CSC.” These new observations about choroidal vascular anatomy may lead to a new concept of pathophysiology of central serous chorioretinopathy and its allied disorders.
Not only the large vessels are of interest, but also the tiny vessels of the choriocapillaris. Dr Spaide concluded that “choriocapillaris parameters might be more important than choroidal thickness itself”, he said.
Dr Spaide investigated the choriocapillaris in patients with normal choroidal thickness and those in the 95th percentile of choroidal thickness and found no difference in choriocapillaris parameters. However, the choriocapillaris in patients with CSC was really quite different, he said.
“However, looking at the choroid is still useful, because CSC-related diseases such as choroidal neovascularisation and PCV have been found to have choroidal vascular similarities not previously detected. We really need to look at the choriocapillaris to determine what is going on in these diseases.”
He concluded that pachychoroid is not that useful a term because of the diversity of definitions about every component, and because a thick choroid does not necessarily suggest pathology. The intervortex venous anastomoses are a new and important finding and have the potential to cause a paradigm shift in our understanding of disease.
EUROTIMES | MARCH 2021 RETINA 12
Many of these definitions would end up classifying normal eyes as having pachychoroid
Richard Spaide MD
New topical steroid for DME

Dexamethasone in novel drug delivery technology shows efficacy in phase II trial. Cheryl
reports
The novel topical dexamethasone product OCS01 showed promising results in a phase II study for the treatment of diabetic macular oedema. The compound, delivered using a proprietary nanoparticle delivery system, was more effective than vehicle in reducing macular thickness and improving vision, said Ramin Tadayoni MD, PhD, at the EURETINA 2020 Virtual meeting.
“This phase II study shows that OCS-01 has the potential to be the first clinically validated topical therapy for DME. It is also a positive proof-of-concept of topical SNP technology to develop additional topical therapies for retinal diseases,” said Dr Tadayoni, Professor of Ophthalmology, University of Paris, Paris, France.

Patients enrolled in the study all had DME for less than three years, BCVA ranging from 20/40 to 20/320, and central macular thickness (CMT) >310 µm. A total of 144 patients were randomised 2:1 to three times daily use of OCS-01 or vehicle for 12 weeks. Patients were followed off-treatment until week 16.
At the primary endpoint at 12 weeks, data analyses showed differences favouring OCS-01 versus vehicle in mean change from baseline in central macular thickness (CMT; -53.68 vs -16.87µm) and BCVA (+2.9 vs +1.7 letters). Compared with the control group, higher percentages of patients treated with OCS-01 demonstrated gains of ≥10 ETDRS letters (14.1% vs 5.1%) and ≥15 ETDRS letters (5.1% vs 0%).
Treatment benefit with OCS-01 was already noted in analyses of CMT and BCVA data collected at two weeks. At the end of the four-week off-treatment observation period, the OCS-01 group maintained the BCVA improvement achieved at week 12, whereas mean CMT increased towards the level of the control group.
“These data show the power of the OCS-01 drops, the penetration of dexamethasone to the retina and proof that the decrease in CMT in the OCS-01 group was related to the drug,” Dr Tadayoni said.
The adverse event review showed 21% of patients treated with OCS-01 had an increase in IOP. Intraocular pressure increased in the OCS-01 group during the 12-week treatment period by a mean of 4.53mmHg, but it returned to the baseline level at the end of the observation period.
“Increased IOP is expected with dexamethasone, and again these data are proof that the drug penetrated to achieve a good concentration inside the eye. The return to normal IOP at study end shows we can stop the drop if a side-effect occurs. That is a benefit of the topical treatment compared with intravitreal steroid injections,” Dr Tadayoni said.
Faros ™ MAKING THE DIFFERENCE WITH LEADING INNOVATION
Precision and efficiency in eye surgery
The Faros surgical platform enables cataract, vitrectomy and glaucoma surgery of the highest level while constantly remaining comfortable and intuitively operable. The reliable flow control makes the surgeon’s work even easier and safer than before. In addition, the Faros impresses with versatility, innovative technologies, exceptional functionality and ease of use.
Make the difference –with the Faros:
www.oertli-instruments.com

EYE SURGERY. SWISS MADE.
Not available for sales in the US Faros_93x266.indd 1 08.02.2021 17:16:55
Guttman Krader
EUROTIMES | MARCH 2021 RETINA 13
This phase II study shows that OCS-01 has the potential to be the first clinically validated topical therapy for DME
Ramin Tadayoni MD, PhD
Gene therapy for severe wet AMD
Novel subretinal treatment shows promise for disease control with reduction in anti-VEGF injection burden. Cheryl Guttman Krader reports
Subretinal RGX-314 gene therapy continues to be well-tolerated and show efficacy for dramatically reducing the anti-VEGF injection burden among patients with severe wet age-related macular degeneration (AMD), according to interim results of an ongoing phase I/IIa clinical trial.
RGX-314 delivers a coding sequence for a soluble anti-VEGF protein using an adeno-associated viral vector. Data from the phase I/IIa dose-escalation study were presented by Robert Avery MD at the EURETINA 2020 Virtual meeting.
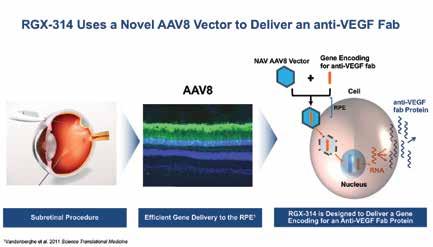
Dr Avery reported that therapeutic effects were observed in the three higher dose cohorts and are durable after available follow-up of one-to-two years. The data also show a dose-dependent and stable increase in the expression of RGX-314 protein that does not seem to be affected by pre-existing neutralising antibodies.
“Planning of a pivotal phase III trial of subretinal RGX-314 for wet AMD is under way, and enrolment has begun in a phase II study of RGX-314 for wet AMD with treatment delivery into the suprachoroidal space,” said Dr Avery, private practice, Santa Barbara, CA, USA.
The phase I/IIa dose escalation study enrolled 42 patients across five cohorts and evaluated doses ranging from 3x109 to 2.5x1011 GC/eye. The subretinal injection was delivered following vitrectomy and without any corticosteroid therapy other
than standard postperative drops. The 42 participants had a long-standing history of severe wet AMD, having received an average of 33 prior anti-VEGF injections and approximately 10 injections during the 12 months prior to RGX-314 injection.
Safety was evaluated as the primary outcome measure of the phase I/IIa study, and the review showed most adverse events were mild (77%). Many adverse events were transient and expected following vitrectomy, Dr Avery said.
A single serious adverse event considered possibly drug-related occurred. It involved a patient who entered the trial with retinal pigmentary changes and a history of 94 antiVEGF injections over a period of 12 years. She developed additional retinal pigmentary
changes involving the macula and experienced a 25-letter BCVA loss from baseline at week 50.
“The patient’s wet AMD was well-controlled without any need for rescue anti-VEGF treatments during the study period,” he said.
Patients in the two lowest-dose cohorts showed minimal-to-no change in antiVEGF injection burden but patients in dose cohorts 3 and 4 had a 61-to-62% reduction in the first year, and the injection burden was reduced by 85% compared with the preceding year in the highest dose cohort. Visual acuity was stable-to-improved over time in dose cohorts 3 and 4. A mean twoletter loss in cohort 5 was attributable to the patient with the serious adverse event.
Robert Avery: bobave@gmail.com
Convenient
Web-Based Registry
Cataract, Refractive and Patient Reported Outcomes in One Platform
The patient-reported outcome is linked to clinical data in EUREQUO. This enables better knowledge of indications for surgery and o ers a tool for clinical improvement work based on the patients’ outcome.
EUREQUO is free of charge for all ESCRS members
EUROTIMES | MARCH 2021 RETINA 14
Join Track the EUREQUO Platform your Surgical Results
www.eurequo.org
Courtesy of Robert Avery MD
Gene therapy developments
Phase I/II clinical trial progressing based on initial favourable data. Cheryl Guttman Krader reports
Nine months of follow-up in a phase I/II clinical trial of AAV-RPGR gene therapy for RPGRassociated X-linked retinitis pigmentosa show encouraging results, reported Michel Michaelides MD, at the EURETINA 2020 Virtual meeting.
He presented findings from the dose-escalation phase of the study that enrolled adults and included low-, intermediate- and high-dose cohorts. The safety review showed that, so far, the treatment was safe and well-tolerated with no dose-limiting adverse events, with the majority of recorded adverse events being anticipated from the surgical procedure.
Efficacy assessments in the low- and intermediate-dose cohorts showed patients achieved significant improvement in vision-guided mobility at low light levels and clinically meaningful improvements in retinal sensitivity across multiple metrics and modalities.
“Given the robust safety and efficacy signals observed, the low and intermediate doses are being further explored with analyses at additional data time points in an ongoing, randomised, controlled dose expansion phase of the study,” said Dr Michaelides, Professor of Ophthalmology, University College London Institute of Ophthalmology and Moorfields Eye Hospital, London, UK.
The dose-escalation phase of the phase I/II trial is the first of three parts. The trial is being undertaken at five sites in the United States and United Kingdom. The dose-escalation study enrolled three patients each into the low- and high-dose cohorts and four into the intermediatedose cohort. All patients received a single injection into the worse seeing eye. Mean age of the 10 patients was 24 years and mean baseline BCVA was 69 ETDRS letters.
The efficacy endpoints included measurements of retinal sensitivity with full field static perimetry that showed statistically significant differences between the treated and untreated eyes among patients in the low- and intermediatedose cohorts in analyses of mean retinal sensitivity, the central 30º hill of vision, and also using a pointwise analysis.
Dr Michaelides reported that a significant difference in retinal sensitivity between the treated and untreated eyes was observed by three months, which was the timing of the first post-treatment measurement. A strong indication of clinical activity in the low- and intermediate-dose cohorts was also evident in analyses of mesopic microperimetry, he said.
Functional vision was assessed using data from mobility maze testing. The results showed time taken to navigate the maze was significantly improved from baseline to nine months at 1 lux, which was the lowest light level used for testing, and also at 4 lux.
Continue your education all year with our range of online resources Visit education.escrs.org Ready when you are. • ESCRS Research Study Portals (ESCRS-funded research projects) • ESCRS Podcasts
EyeJC (The ESCRS Journal Club)
Case Studies
EBO – ESCRS Examination
ESCRS Media Player
ESCRS On Demand
ESCRS iLearn
Astigmatism Double Angle Plot Tool and more...
•
•
•
•
•
•
•
EUROTIMES | MARCH 2021 RETINA 15
...a significant difference in retinal sensitivity between the treated and untreated eyes was observed by three months
Michel Michaelides MD
Five ‘rights’ for AI and the eye
Leigh Spielberg MD reports
2020 2021
Applications are open for the Peter Barry Fellowship 2021. This Fellowship commemorates the immense contribution made by the late Peter Barry to ophthalmology and to the ESCRS.
The Fellowship of €60,000 is to allow a trainee to work abroad at a centre of excellence for clinical experience or research in the field of cataract and refractive surgery, anywhere in the world, for 1 year.
Applicants must be a European trainee ophthalmologist, 40 years of age or under on the closing date for applications and have been an ESCRS trainee member for 3 years by the time of starting the Fellowship.
The Fellowship will be awarded at the ESCRS Annual Congress in 2021, to start in 2022.
To apply, please submit the following:
A detailed up-to-date CV
A letter of intent of 1-2 pages, outlining which centre you wish to attend and why
A letter of recommendation from your current Head of Department
A letter from your potential host institution, indicating that they will accept you if successful
Closing date for applications is 1 May 2021
Applications and queries should be sent to programme@escrs.org
Artificial intelligence represents the fourth industrial revolution, and its application in ophthalmology has clearly begun,” said Daniel Ting, Singapore National Eye Centre, Singapore at EURETINA 2020 Virtual. Dr Ting brought viewers along for a ride through a world of technological developments that most ophthalmologists barely know even exist.
Dr Ting and his team have already published two major review papers on the topic, on both artificial intelligence (AI) and deep learning.
“In these papers, we outline what AI can already achieve with deep learning based on fundus imaging for conditions like diabetic retinopathy, glaucoma suspects, AMD and retinopathy of prematurity,” he said.
“It is also becoming increasingly evident that AI can see things that we as ophthalmologists cannot see,” said Dr Ting.
Based on deep learning, AI software can determine both the age and the gender of a patient based on a simple fundus image of the posterior pole. More usefully, papers have been published regarding the prediction of cardiovascular risk factors from retinal fundus photographs via deep learning.
But what about for patients with eye disease?
“Even more relevant for practising retinal specialists, AI has been shown to be able to predict conversion from dry to wet AMD, better than retinal specialists.”
Okay, AI machine learning sounds great. But how does one get started?
Dr Ting said: “You have to start with the ‘Five Rights’. You have to ask the right questions, identify the right clinical data, identify the right technical partner, understand the right concepts and identify the right enabler who can implement and commercialise the final product.”
Most important for ophthalmologists and researchers working in the field, asking the right question involves identifying an unmet clinical need, such as screening large populations for diabetic retinopathy.
So how will AI and deep learning get a chance at acceptance by physicians?
“It seems that the current pandemic crisis has stimulated more widespread acceptance of AI,” he said, referring to an article describing how physicians, faced with staff shortages and overwhelming patient loads, are starting to use artificial intelligence to triage COVID-19 patients.
“Once they’ve proven their worth, these tools may be here to stay,” concluded Dr Ting.
“We know that the patients, physicians, regulators, providers, funders are becoming more willing to fund some of these technologies in the healthcare setting,” he said, before quoting Sir Winston Churchill: “Never let a good crisis go to waste.”
In the recent Expertscape ranking (2010 – 2021), Dr Ting is also ranked 1st on deep learning (among 35K candidates) across all medical and technical domains. https://expertscape.com/ex/deep+learning
Daniel Ting: daniel.ting.s.w@singhealth.com.sg

Artificial intelligence already proving useful in retina diagnostics.
EUROTIMES | MARCH 2021 RETINA 16
Daniel Ting
Approaching high myopia
Dedicated session examined diagnosis and treatment in myopic eyes. Priscilla Lynch reports
Macular buckling represents a safe and effective surgical option for foveoschisis and fullthickness macular holes (FTMH) in highly myopic eyes, said Lin Lu MD, China, speaking during the dedicated myopia session at EURETINA 2020 Virtual, which addressed pathogenesis, diagnosis and treatment of high myopia.
Outlining three-year outcome data on this complicated surgical technique, Dr Lu said macular buckling showed a high closure rate and virtually no tendency to recur. In this approach, visual acuity can be improved and axial length can be preserved for longer.
His study involved 28 patients (28 eyes) with foveoschisis and 21 patients (21 eyes) with FTMH with macular detachment. Retinal reattachment was achieved in all cases, while macular hole closure was achieved in 76.19%. BCVA significantly improved one year postoperatively in the foveoschisis cases and two years in the FTMH cases. The mean axial length decreased by 2.09mm postoperatively.
During this session, Yasushi Ikuno MD, Japan, compared various surgical approaches for myopic macular diseases. Standard techniques include vitreous cortex removal from the retinal surface, epiretinal membrane if present, internal limiting membrane (ILM) peeling and gas/air tamponade, which remains very controversial.
Within foveoschisis, there are three subtypes (retinoschisis, foveal detachment and macular holes), which have different surgical results, varying from being most effective in foveal detachment to limited benefit in macular holes, he explained. Macular holes are a significant risk factor post-surgery, occurring in about 20-to30% of eyes according the literature, “with IOS/OS in OCT and foveal detachment identified as a high-risk group”.
Dr Ikuno discussed an interesting new FS surgery technique – the foveola non-peeling technique in ILM: “In this technique you peel the ILM in a doughnut fashion and save the ILM as a central part to limit the damage of the foveola.”
Unresolved issues in macular hole retinal detachment (MHRD) include low retinal reattachment rates, and macular hole closure rates despite surgical improvements. The inverted ILM flap method is the most promising method for macular hole closure, he stated.
Tzyy-Chang Ho MD, Taiwan, addressed the thinking processes and practices in the management of vitreoretinal interface disorders in pathological myopia, looking at ‘internal’ and ‘external’ surgical approaches.
“For the external approach I prefer posterior scleral reinforcement with a pliable Gore-Tex strip to support the staphyloma without protrusion.”
With the internal approach, Prof Ho said the key point is the recovery of microstructures, ie foveola layers (outer nuclear layer/external limiting membrane, ellipsoid zone), adding: “I prefer the foveola non-peeling ILM technique. The ILM margin must not be elevated.”
He discussed his own large series (95 eyes) long-term results of C-shaped temporal inverted ILM flap in macular hole retinal detachment in highly myopic eyes. The fovea was flattened and the macular hole sealed in 93 eyes (97.8%)
“In the two eyes that failed the ILM flap was found to flip back to the temporal side of the flap and the ILM flap was elevated at the margin to cover and seal the hole in the secondary vitrectomy.”
There was retinal detachment with new peripheral break in two eyes in the study, which were reattached after secondary vitrectomy.
The same ILM non-peeling technique can be used for lamellar macular holes with epiretinal proliferation, added Prof Ho, concluding: “I advocate the concept of foveolar reconstruction in the repair of vitreoretinal interface disorders.”
IMAGING
Also addressing this session, Kyoko OhnoMatsui MD, Japan, said that ultra-widefield swept source OCT produces high-resolution and extended-size tomographic images of various tissues from the vitreous to the sclera. “This technology is a valuable method to identify how vitreous and sclera become pathological and how such pathologies lead to vitreoretinal tractional diseases in synchronicity.”
In another imaging presentation, Xiaoxin Li MD, China, reviewed the use of structural OCT to differentiate between punctate inner choroidopathy (PIC), PIC-choroidal neovascularisation (CNV) and myopic CNV.
The three inflammatory lesions look similar on spectral domain (SD)-OCT but the treatment is different – myopic CNV and PIC-CNV need anti-VEGF treatment while PIC is a self-limited disease that does not, thus accurate diagnosis is essential, she explained.
Prof Li quoted study data looking at the structural characteristics of inflammatory lesions on SD-OCT using OCT-angiography (OCT-A) in myopic (at least -5D) patients with acute blurred/distorted vision, who were followed up for a minimum of two months and had active hyper-reflective lesions on SD-OCT.
The data showed that disruption of retinal pigment epithelium (RPE)/Bruch’s membrane is a definite sign for CNV, while hyper-transmission is a sign for PICCNV within four weeks (100%), with hypo transmission together after four weeks.
In addition, hypo transmission was shown to be a sign for myopic CNV, while neither transmission changes or disruption of RPE/ Bruch’s membrane were found in PIC.
Thus this form of imaging provides a convenient, non-invasive strategy for accurate diagnosis and treatment of these lesions, concluded Prof Li.
EUROTIMES | MARCH 2021 RETINA 17
...macular buckling showed a high closure rate and virtually no tendency to recur
Lin Lu MD
Best of the best 2020
Experts discuss the best ESCRS papers and posters. Dermot McGrath reports
Acomprehensive study of rebubbling after Descemet’s Membrane Endothelial Keratoplasy (DMEK), the long-term outcomes in paediatric patients using an innovative bag-in-the-lens technique and a new fluid-filled, modular accommodating IOL for presbyopia were among some of the topics discussed in a special ESCRS online review session of the best free papers and poster prize winners from the 38th Congress of the ESCRS.
Co-chaired by Oliver Findl MD and Boris Malyugin MD, the review session brought together a panel of international experts –Béatrice Cochener-Lamard MD, PhD, from France, Rudy Nuijts MD, PhD, from the Netherlands and Marie José-Tassignon MD, PhD, from Belgium – to discuss the issues raised in the winning papers and posters and their significance on current and future clinical practice.
The session commenced with the best free paper for cornea from Sebastian Siebelmann et al entitled “The Cologne Rebubbling Study – an analysis of 624 rebubblings after Descemet’s Membrane Endothelial Keratoplasy (DMEK)”. Based on the study, the authors recommended performing rebubbling less than 10 days after surgery if the detachments were more than one-third of the graft area, and later than 10 days for similar size detachments depending on the clinical course and in cases of strong curling tendency of the transplant.
Dr Nuijts said he was a little surprised by the outcomes given that the Cologne centre performed a lot of DMEKs and the surgeons are experienced in this type of surgery. “The rate of one-third of patients having a detachment is pretty high I think.” He noted that data from the Dutch corneal transplant registry indicated a detachment rate of about 25%. Despite a lot of studies, he said it was still something of a mystery why detachments occurred so often, even in the hands of such very experienced surgeons as our German colleagues.
“We can do a perfect surgery and it still occurs. Is it something correlated to the storage medium that we use, with or without dextrane, or perhaps the positioning of the patient at home after surgery and whether they respect the instructions to remain in the supine position? There are still a lot of unanswered questions,” he said.
fixation was feasible in over 90% of patients and a clear visual axis was maintained in 95% of children with a low rate of complications.

Commenting on the poster, Marie-José Tassignon, the creator of the BIL fixation technique, said that the results were very much in line with her own experience with the lens and the learning curve involved. “We have published our own results in the JCRS and the complication rate was very low. It is why we have been able to push the indications for this lens and we can now operate on children as young as two months with very good results,” she said.
The next study under review was a free paper by Liliana Werner MD, PhD, et al on the long-term capsular bag clarity of a new fluid-filled, modular accommodating IOL. The Juvene IOL (LensGen Inc.) integrates a base lens supported by capsule-filling circumferential haptics and a fluid-optic, curvature-changing lens that allows for continuous range of vision.
The panel expressed reservations about the long-term capacity of the lens to resist fibrosis, pointing out that the study was in a rabbit model with just six months' follow-up. Dr Nuijts added that the 3.0mm incision required for implantation would probably also impede uptake of the lens for many surgeons.
Prof Cochener-Lamard said the lens followed in a long line of presbyopia-correcting IOLs over the past decade, none of which had really satisfied all the criteria required for widespread adoption. “It always returns to the same question – the predictability of the lens and the duration of the effect and its ability to remain transparent over time. I am also not sure that the ophthalmological community will accept a larger incision and to put these heavy materials into the capsular bag,” she said.
In the refractive poster category, the review panel discussed a study by Emilio Torres-Netto MD that looked at a photoactivated chromophore for infectious keratitis cross-linking (PACK-CXL) and concluded that 89% of eyes treated with this approach healed without the use of antimicrobial therapy. Prof Cochener-Lamard said she would have ethical concerns about using this approach for treating serious infections when tried-and-trusted antimicrobial treatments are already available. “I think we need to be very cautious and not be seen to promote the idea that riboflavin cross-linking treatment might be sufficient on its own for treating infections,” she said. Dr Nuijts
18
CATARACT & REFRACTIVE VISIT OUR WEBSITE FOR INDIAN DOCTORS www.eurotimesindia.org INDIA
IOL Con database awaits input
International internet database updates and optimises IOL constants. Howard Larkin reports
Getting the A-constant right is essential for accurately calculating intraocular lens (IOL) power. And optimising standard A-constants to reflect systematic biases in surgeons’ unique measurement and surgical processes is an important step. The IOL Con online database offers a modern and convenient solution, Sibylle Scholtz PhD told the 38th Congress of the ESCRS.
Since its introduction in 1999, optical biometry has transformed cataract surgery planning, said Dr Scholtz, of the Institute of Experimental Ophthalmology, Saarland University, Homburg/Saar, Germany. That same year, Wolfgang Haigis PhD, professor at the University of Würzburg, Germany, set up the User Group for Laser Interference Biometry (ULIB) database of IOL constants. It was based on optical biometry that he calculated based on surgeon reports, paving the way for effective use of the new technology.
However, using offline spreadsheets and static constant lists, ULIB no longer meets modern requirements, Dr Scholtz said. To meet modern standards, Achim Langenbucher PhD, professor of medical optics, Saarland University, built on Prof Haigis’ ideas of an internet database to develop IOL Con in 2017.
Prof Langenbucher envisioned the modern database as an interactive, open concept, accessible by all IOL and biometer manufacturers, as well as surgeons. The webbased design is easy to use, providing all relevant lens data at a glance, using XML as a public and documented data transfer format. Its data are provided by two user groups, manufacturers and ophthalmic surgeons, and are constantly updated. This makes it an up-todate overview of available IOLs, with all relevant technical, geometric and material characteristics, Dr Scholtz said.
IOL Con features easy uploading and downloading of data on biometry and implanted IOLs, including postoperative refraction, which are needed to optimise personal constants. It also continuously updates global constants based on community data. IOL Con is free of charge for ophthalmic surgeons.

IOL Con has grown steadily. As of Sept 2020, it included data on 414 IOL models from 28 manufacturers and featured 19,000 clinical data sets on 105 IOL models. Biometry manufacturers are integrating IOL Con data into their devices, including, with the next software update, Zeiss’s IOLMaster 700, Dr Scholtz said.
“IOL Con offers much more than a simple static table. It is a global interactive, up-to-date, modern internet platform that provides ophthalmo-surgeons with all IOL characteristics, which are updated constantly. By implementing IOL Con a biometry database is already available today to meet the future demands of ongoing developing ophthalmo-surgery,” Dr Scholtz concluded.
Sibylle Scholtz: sibylle.scholtz@gmx.de
Your Professional
Dry Eye Assistant
OCULUS
Keratograph 5M with JENVIS Pro

Dry Eye Report:
All relevant information at a glance!
The new JENVIS Pro Dry Eye Report helps you perform comprehensive screenings, using the measuring results as a basis for diagnosing dry eye syndrome. The workflow is optimized for time saving and patient friendliness. All results are documented and summarized for you and your patient in a neat and easily understandable printout.
19 www.oculus.de
Eurotimes Keratograph Dry Eye, JENVIS - nur Produkt 93x266 e 4c 01.21 v2.indd 1 29.01.2021 16:56:36
EUROTIMES | MARCH 2021 CATARACT & REFRACTIVE
...using offline spreadsheets and static constant lists, ULIB no longer meets modern requirements
Sibylle Scholtz PhD
Psychic toll of coronavirus
Protecting ophthalmologists from COVID-19 burnout is a top priority. Howard Larkin reports

While physicians are conditioned to manage pressure from their earliest training, the added stress of COVID19 is creating a burden that is pushing many past their ability to cope. So much so that AAO CEO David W Parke II MD regularly hears from colleagues who are burned out or depressed, including one who was suicidal, he reported at AAO 2020 Virtual.
It’s part of a broader problem in medicine, said Saul Levin MD, CEO and medical director of the American Psychiatric Association. “Our health system was broken before but now it is severely broken.”
The pandemic is taking an even greater toll on Black and Latinx minorities who have less access to care in the best of times, Dr Levin added. In addition, people with existing mental illness and substance use disorders tend to do worse in health crises, and the pandemic has been no exception.
Dr Levin pointed out that care providers need to look after themselves as well as others – and reach out when they are feeling burned out or depressed. Even taking part in social hour calls at meetings such as the AAO Virtual can help, Dr Levin said.
“I was a little bit sceptical but I’ve got to tell you when I do [participate in virtual social gatherings] I leave feeling a lot more uplifted that I am not alone.”
WARNING SIGNS
Dr Levin recommended that everyone stop and consider who they can reach out to when they are feeling stressed, and pointed out some warning signs to watch for. Consider whether you are just tired or if, when you get up in the morning or get home at night, that you just want to be left alone, or your appetite is gone or unusually strong.
“If you hear a colleague – or yourself –say ‘I feel like I can’t go on’, take it as a sign of impending burnout or even depression, which often overlap in symptoms, Dr Levin
said. “If you hear even more concerning statements, such as ‘I want to die,’ do not dismiss it as just a sign of exhaustion. This could be an important outreach for help. Make sure he or she knows where to turn for help such as a national suicide hotline. Ensure that other people in the colleague’s home, such as a spouse or family member, know of his or her distress.”
Physician suicide is not talked about enough within the medical community and it contributes to stigma and physicians being afraid of seeking help. The COVID pandemic has only made the challenging work of being a physician more stressful. “It takes great courage to ensure your colleague gets help, regardless of commitments made,” but it does help in the end, Dr Levin said.
EUROTIMES | MARCH 2021
CATARACT & REFRACTIVE 20
I was a little bit sceptical but I’ve got to tell you when I do [participate in virtual social gatherings] I leave feeling a lot more uplifted that I am not alone
Saul Levin MD, CEO
Multi vs monofocal
Should cataract patients with previous corneal refractive ablations receive multifocal (MFIOL) or monofocal intraocular lenses? The answer depends upon the type and degree of correction previously applied, surgeons’ corneal measurement capabilities and informed patient preferences, according to debaters at the JCRS Symposium at the 38th Congress of the ESCRS Virtual.
Arguing for monofocal lenses was Ruth Lapid-Gortzak MD, PhD, cornea, cataract and refractive surgeon at the Amsterdam University Medical Centers, of the University of Amsterdam, and medical director of Retina Total Eye Care, Driebergen, the Netherlands. Dr. Lapid presented the opinion that monofocal lenses are preferable in most cases due to the difficulty of achieving acceptable visual outcomes with MFIOLs, though she does not hold this position herself.
Arguing in favour of judicious use of MFIOLs was José F Alfonso MD, PhD, head of cornea and lens surgery at the Fernández-Vega Ophthalmological Institute, Oviedo, and lecturer at the University of Oviedo, Spain. His extensive research suggests that the key to meeting patient demands for spectacle independence is analysing how refractive surgery has changed the cornea, and finding a lens that can work with the aberrations present.
ABERRATED EYES
Dr Lapid pointed out that LASIK and PRK change the cornea in ways that make it difficult to measure its power. The ratio between the anterior and posterior surfaces changes, and there is a forward shift of the posterior cornea that makes it difficult to correctly estimate effective lens position.
“So, it doesn’t work with regular formulae.” Dr Lapid said.
Other complicating factors include decentred ablations and induced higherorder aberrations, particularly spherical aberrations (SA). Small treatment zones, which are common for older ablations, are troublesome because they induce moreacute changes in cornea shape, Dr Lapid said. “All these factors go together.”
Multifocal IOLs have a host of sideeffects that make them unsuitable for patients with high visual demands, Dr Lapid said. For example, even in extended
depth of focus lenses the gain in depth of focus was offset by a decline in both peak VA and contrast sensitivity (Bellucci et al. JCRS 2019;45:919-926). Modulation transfer function is also lower in multifocal IOLs than in monofocal IOLs and is highly dependent on pupil size (Tandogan et al. JRS 2017;33:808-812).
“We are really affecting the quality of vision with multifocal IOLs. The bottom line is I should be saying monofocal lenses are the only option, but there is no one-size-fits-all, and judicious use of preoperative screening make multifocal lenses an option.” Good biometry and shared consent are essential to reach patients goals, she advised.
OFFSETTING SA
Dr Alfonso pointed out that controlling SA is essential for a good cataract surgery outcome after laser refractive surgery. Myopic photoablation induces positive SA commensurate with the dioptres of error corrected. For example, a -3.0D correction induces about +0.1 microns SA, while a -9.0D correction induces about +0.3 microns. Hyperopic ablation is the reverse with a +2.0D correction inducing about -0.1 microns SA and a +4.0D about -0.2 microns. While a small amount of SA results in greater defocus tolerance and depth of field in ablated eyes – indeed, a young healthy, unablated eye has about +0.1 microns – it is essential to keep it within ±0.2 microns, which results in a loss of visual acuity of about one line and a gain in depth of focus of about 0.5D.
So, Dr Alfonso chooses a lens that will balance the existing SA of the postrefractive surgery cornea with a lens that will offset it to bring total SA within ±0.2 microns, which maintains good distance and acceptable intermediate vision. For example, a patient who received a myopic
LASIK correcting -1.0 to -4.0D can do well with a trifocal diffractive lens with -0.1 microns, such as the FineVision.
“We obtain standard distance vision and preserve the trifocal performance of the lens.” A higher myopic correction of -7.0D to -10.0D might induce a +0.3 microns cornea, requiring a lens with greater negative SA, such as the Eyehance with -0.27 SA, to achieve best results.
Dr Alfonso’s research suggests that diffractive trifocal lenses do not perform as well after higher LASIK myopic corrections resulting in mean corneal power equal or less than 38D, limiting distance-corrected vision. With myopic corrections greater the -7.0D, two lines of vision can be lost.
“This problem does not occur with nondiffractive extended depth of focus lenses such as the Vivity, which would be indicated in a patient who received a myopic LASIK correction between -5.0 and -6.0D.”
Conversely, in patients after hyperopic photoablation, negative corneal SA is induced. Implanting a neutral monofocal lens does not increase the corneal aberration. With a mild myopia refractive target of -0.5D, this results in standard distance vision and functional intermediate vision. With diffractive lenses, Dr Alfonso’s research shows a loss of one line of corrected distance vision in corneas with high hyperopic corrections.
Dr Lapid congratulated Dr Alfonso on the depth of his research. She pointed out that assessing higher-order aberrations involves extra steps. “It is expensive and time-consuming, so the patient has to understand what you are doing and why.” Her research with instruments available in every cataract clinic has shown that with simpler screening methods one can evaluate which post-LASIK eye will do well with multifocal IOLs (Vrijman et al JCRS 2017; 43:909-914).
EUROTIMES | MARCH 2021 CATARACT & REFRACTIVE
Both options can be effective for patients following previous corneal refractive surgery. Howard Larkin reports
21
We are really affecting the quality of vision with multifocal IOLs. The bottom line is I should be saying monofocal lenses are the only option, but there is no one-size-fits-all
Ruth Lapid-Gortzak MD, PhD
SMILE or implant for hyperopia?
Intrastromal lenticule implantation may be a future treatment for hyperopia, but SMILE more effective now. Roibeard
The advent of intrastromal implantation of femtosecond laser-sculpted lenticules has brought refractive surgery full circle to José Barraquer’s original idea of tissue additive corneal re-shaping, Dan Z Reinstein MD told the 38th Congress of the ESCRS.
“The accuracy and repeatability of the VisuMax femtosecond laser has made Barraquer’s concept a reality,” announced Prof Reinstein, Medical Director of London Vision Clinic, London, UK.
The concept of tissue additive corneal refractive surgery dates back to 1980 when Dr Barraquer in his textbook on keratomileusis introduced a technique for myopia or hyperopia he called pocket intrastromal keratophakia, wherein a lathed disc of stroma is inserted into a lamellar pocket dissected in the cornea.
However, it was not until 2004 that the procedure was revived, this time in a new form that involved mechanical de-epithelialisation, lamellar microkeratotomy, hyperopic LASIK and a circumferential side-cut to remove the lenticule. The lenticule was then placed beneath a LASIK-style flap in the patients’ eye (Jankov et al, J Refract Surg Jan-Feb 2004;20(1):79-84).
In a hyperopic and amblyopic eye that had undergone previous refractive surgeries, the endokeratoplasty procedure improved mean best spectacle-corrected visual acuity from 20/200 to 20/70 and improved manifest refraction from +8.00 -1.00 x 130 to +1.00 -2.25 x 120 at two months postoperatively. Corneal topography showed a more regular cornea with increased curvature in all meridians. Central corneal thickness increased to 600 µm.
The next attempt was in 2015 where a +10.00D lenticule obtained from a myopic small-incision lenticule extraction (SMILE) procedure was implanted into an aphakic eye of a patient who had undergone removal of a congenital cataract in childhood. The patient’s hyperopia improved from a preoperative value of +12.00D to +1.00D at two days postoperatively, but regressed to +8.00D at four months (Pradhan et al. J Refract Surg. 2015;31:60).
Prof Reinstein noted that the reason for the regression was that although the front surface had steepened by the desired amount, the back surface had flattened, causing a hyperopic shift. Subsequent finite element model analysis using OptimEyes software predicted both the anterior and posterior corneal changes, he added (Studer et al. J Refract Surg. 2015;480-486).
In another study, intrastromally implanted cryopreserved lenticules were used to treat eight hyperopic eyes and one aphakic eye. The postoperative residual spherical equivalent was
+4.10D for the aphakic eye and had a mean value of +0.60D in the hyperopic eyes. None of the eyes showed evidence of rejection or loss of corrected distance visual acuity (CDVA) (Ganesh et al, J Refract Surg. 2015;31: 374-9).
One patient developed interface haze in both eyes at the end of six months, Dr Reinstein noted. However, lenticule exchange restored corneal clarity. One eye that underwent implantation of a -9.50D lenticule to correct +9.00D of hyperopia had a postoperative residual refraction of +2.50D. Relaxation of Bowman’s membrane using a Barren’s trephine reduced the hyperopia to +0.75D.
Dr Reinstein noted that research into the use of intrastromal lenticule implantation continues for a variety of indications including hyperopia, high astigmatism, presbyopia and, perhaps most importantly, keratoconus.
HYPEROPIC SMILE SHOWING PROMISE
Meanwhile, hyperopic SMILE may hold more immediate prospects for the treatment of hyperopes than intrastromal lenticular implantation. Recent studies show that hyperopic SMILE produces results comparable to those of hyperopic LASIK in terms of safety, visual outcome and refractive predictability, Dr Reinstein said.
He cited a prospective study in which he and his associates performed hyperopic SMILE in a series of 93 eyes with a maximum attempted hyperopic meridian between +1.00D and +7.00D. Initial phase safety studies showed that treatment centration was similar to hyperopic LASIK (Pradhan et al, J Refract Surg. 2017;150-156), as were topographic optical zone diameter and spherical aberration induction (Pradhan et al, J Refract Surg. 2017;370-376). The optical zone diameter was 6.3-to-6.7mm, with a 2.0mm transition zone, 30μm minimum thickness and 120μm cap thickness (Pradhan et al, J Refract Surg. 2019;442-450).
At 12 months’ follow-up, the spherical equivalent was within ±0.50D of target refraction in 59% of eyes and within ±1.00D of target in 76% of eyes. There was also no significant difference between spherical equivalent at one day postoperatively and at the last follow-up visit.
In addition, among 37 eyes targeted for emmetropia, postoperative uncorrected distance visual acuity (UDVA) was the same or better than postoperative CDVA in 78% and was within one line of CDVA in 86%. Overall, at 12 months’ follow-up 17% of eyes lost one line of CDVA and no eyes lost two or more lines.
Furthermore, vector analysis showed that the refractive cylinder was corrected within 0.50D of target in 95% of eyes and within 1.00D of target in 99% of eyes.
“Lenticule removal and implantation has shown promise, for keratoconus and corneal transplant, However, for hyperopia, SMILE has shown promising early results,” Dr Reinstein added.
Dan Z Reinstein: Dzr@londonvisionclinic.com
Ó hÉineacháin reports
EUROTIMES | MARCH 2021 CATARACT & REFRACTIVE 22
The accuracy and repeatability of the VisuMax femtosecond laser has made Barraquer’s concept a reality
Dan Z Reinstein MD
THOMAS KOHNEN European Editor of JCRS
JCRS HIGHLIGHTS




VOL: 47 ISSUE: 2 MONTH: FEBRUARY 2021
25 YEARS OF INTRAOCULAR LENSES

Intraocular lenses have undergone a remarkable evolution since first being imagined by Harold Ridley. The Journal of Cataract and Refractive Surgery, now celebrating its 25th anniversary, has reported developments in lens design for this period, and continues to do so today. Noted researchers Prof Liliana Werner, who began her career working with the legendary David Apple, discusses the long arc of IOL development in a special editorial. She also worked with Dr David Leaming, who she credits for his valuable annual practice surveys, which show how trends in lens design are adopted in the clinic. She explains how IOL designs have evolved to deal with problems such as posterior capsule opacification, glistenings, and potential UV light risk. She also discussed attempts to develop a lens for presbyopia treatment, including the recent development of extended depth of focus technology. L Werner, “Intraocular lens evolution in the past 25 years as told by the Journal of Cataract and Refractive Surgery”, Vol. 47, #2, 147-149.
ESCRS INTRACAMERAL CEFUROXIME DEBATE



Appearing in the JCRS 15 years ago, the ESCRS Intracameral cefuroxime study remains the single most important study of antibiotic prophylaxis for ophthalmic surgery, says guest editorialist Dr David Chang. Spearheaded by Dr Peter Barry in Dublin, the study (J Cataract Refract Surg 2006;32:407–410) continues to stir debate. In 2006 the common practice for intraoperative antibiotic prophylaxis was a topical approach. The study instead looked at using cefuroxime in an intracameral approach. The result was a remarkably low incidence of endophthalmitis. While initially met with some resistance, the use of intracameral prophylaxis has now been widely, but not universally, adopted. DF Chang, “The ESCRS Intracameral cefuroxime study: the debate continues”,Vol. 47, #2, 150-152.


NEW ENHANCED MONOFOCAL IOL

The conventional monofocal IOLs effectively restore distance vision, but typically fall short at other distances. The TECNIS Eyhance IOL, Model ICB00 appears to be the first monofocal IOL to demonstrate an improvement in intermediate vision with comparable distance vision and photic phenomena as a standard monofocal IOL. Researchers report results from a multi-centre prospective randomised controlled study in which 139 patients received the new lens or the standard Tecnis ZCB00 monofocal IOL. At six months’ follow-up, patients receiving the enhanced IOL showed significantly better mean distance corrected and uncorrected intermediate visual acuity compared with those that received the standard lens. Distance vision, contrast sensitivity and photic effects were similar for the two groups. The investigators explain that the design of the new IOL resembles the standard lens in most ways but has a higher-order aspheric anterior surface. GU Auffarth, “Clinical evaluation of a new monofocal IOL with enhanced intermediate function in patients with cataract”, Vol. 47, #2, 184-191.

EUROTIMES | MARCH 2021
CATARACT & REFRACTIVE 23 JCRS is the official journal of ESCRS and ASCRS
Update on ECCTR
European registry highlights practice patterns in corneal transplantation. Dermot McGrath reports
The first peer-reviewed publications to emerge from the European Cornea and Cell Transplantation Registry (ECCTR) mark an important step forward in understanding the safety, quality and efficacy of corneal transplantation in Europe.
The two studies, which look at European practice patterns and outcome data for corneal transplantation respectively, have recently been accepted for publication by the Journal of Cataract and Refractive Surgery.
“This is significant because I think for the first time these papers give us a picture of what’s really happening in Europe in terms of practice patterns and outcomes for corneal transplantation,” said Mor Dickman MD, PhD, Maastricht University Eye Clinic, Netherlands. “What type of patients are undergoing cornea transplantation? What kind of donors give their corneas for transplantation? Which diseases are the most prevalent?”
Dr Dickman said that while this information might seem banal to some, the reality is that registry data constitutes a mine of valuable data that benefits practitioners and patients.
“Everybody is always looking for the latest invention or technological advancement, but the big picture in terms of what are we doing and who are we doing it for and what are the outcomes thereof – that information or big picture was simply not there. That’s the true significance of these publications – for the first time we have a European endeavour that looks at what we’re doing and gives us a comprehensive overview of our outcomes in the field of corneal transplantation,” he said.
Established in 2016, the ECCTR has now collected data on 13,000 transplants from 12 countries and includes information on the recipient, donor and eye bank processing, transplant procedure and twoyear follow-up including graft survival and failure and patient-reported outcome measures (PROMs).
“There are a lot of interesting findings in the data,” said Dr Dickman. “For example, the youngest patient in the registry is a one-year-old infant with Peter’s anomaly and the oldest person is 101 who underwent a regraft. While these are anecdotal cases, it is nevertheless quite interesting to see that cornea transplantation is being used to help patients across all the entire spectrum of the human life-span,” he said.
REPEAT GRAFTING
Fuchs’ endothelial dystrophy is the number one reason for corneal transplantation, noted Dr Dickman. “This makes sense because it’s quite prevalent among Europeans. But what really stands out is the fact that repeated transplants are the second most common indication for corneal transplantation,” he said.
One question this poses, added Dr Dickman, is how cornea transplant care should be organised to optimise outcomes and try to reduce the current high levels of repeat grafting.
“The regrafting rate has to do with the introduction of novel techniques and the learning curves that are associated with them, but also recognising that when we look at the long term, endothelial decompensation and graft rejection do play a role in limiting the survival of grafts. So, the ageing of the population needs to be factored into the equation, as we know that with each retransplant the outcomes are generally less favourable,” he said.
BENCHMARKING
Dr Dickman stressed that the primary purpose of the registry is to allow benchmarking and drive quality improvement.
“I think this data is mostly useful for benchmarking, in the sense that it can be used to see what other surgeons are doing and how results compare. There’s a possibility for surgeons to create their own reports in the ECCTR in order to
benchmark their outcomes and get a sense of how well they are performing compared to other European centres,” he said.
Looking at the current spread of participating centres, Dr Dickman said that greater involvement from southern and eastern Europe would be a welcome development.
“In northern Europe, there is a culture of registries going back many years. The acceptance is also driven by insurance companies in countries such as the Netherlands, and in the UK by the requirements of auditing in order to renew one’s license as a practising surgeon. Some donor banks also require registry data as a prerequisite for using their services,” he said.
Looking ahead, Dr Dickman said that the next step is the addition of a limbal stem cell transplant component to the registry.
“This is a very exciting development. For limbal stem cell transplants, we have now a stem cell therapy. Patients undergo this therapy for a myriad of indications. It will be very interesting to know what are the long-term outcomes of these transplants and collect this data on an independent platform” he concluded.
Outcomes of corneal transplantation in Europe: Report by the European Cornea and Cell Transplantation Registry
(ECCTR) https://journals.lww.com/jcrs/ Abstract/9000/Outcomes_of_corneal_ transplantation_in_Europe_.99642.aspx
EUROTIMES | MARCH 2021
CORNEA 24
This is significant because I think for the first time these papers give us a picture of what’s really happening in Europe in terms of practice patterns
Mor Dickman MD, PhD
The youngest patient in the registry is a one-year-old infant with Peter’s anomaly and the oldest person is 101 who underwent a regraft
Mor Dickman MD, PhD
New therapies for dry eye disease
New office-based procedures for Meibomian gland dysfunction. Dermot McGrath reports
Avariety of new office-based treatments show significant promise in the treatment of dry eye disease (DED) associated with Meibomian gland dysfunction (MGD), according to Shahzad Mian MD.
“We do have an increasing range of options available even though the management of dry eye often leaves patients and practitioners unhappy with the lack of relief of symptoms. Despite the high prevalence and significant impact on quality of life, there is little understanding of the aetiology and success of treatments,” Dr Mian said at the World Ophthalmology Congress 2020 Virtual.
Dr Mian illustrated the difficulty of treating DED with reference to a 72-year-old Caucasian female patient who presented with sensations of grit, burning and tearing in her eyes with intermittent blurry vision. She had a history of hypertension, which was being treated. A slit-lamp exam showed moderate inferior punctate keratopathy and significant inspissation of the Meibomian gland.
“The diagnosis here was Meibomian gland dysfunction with evaporative dry eye. However, the patient had already undergone many different treatments including hot compresses, artificial tears, topical steroids, antiinflammatories and punctal plugs without any relief,” he said.
Dr Mian said that other treatments to consider for patients with MGD include autologous serum tears, tea tree oil, amniotic membrane grafts, scleral lenses, thermal pulsation systems and Intense Pulsed Light (IPL).
Autologous serum tears are a useful adjunct for patients who have been using other forms of treatment including artificial tears or anti-inflammatories.
“We know from studies that they do help patients in terms of signs and symptoms of DED. Objective measures such as Schirmer scores and fluorescein staining were shown to improve with treatment,” he said.Tea tree oil, which is indicated in patients with Demodex blepharitis, works by eradicating mites and has antibacterial, antifungal and anti-inflammatory properties.
“Patients with demodex treated with tea tree oil for a minimum of six weeks showed dramatic resolution of ocular irritation, conjunctival inflammation and all inflammatory signs,” he said.
Amniotic membrane grafts are commonly used to promote wound healing and corneal re-epithelisation in indications such as recurrent corneal erosion, corneal abrasion, neurotrophic keratitis, corneal exposure from incomplete blink and severe dry eye, said Dr Mian.
Scleral contact lenses are another option for the management of severe inflammatory DED such as graft versus host disease, ocular cicatricial pemphigoid, neurotrophic keratitis, exposure keratopathy and for mechanical protection, he added.
In the end, Dr Mian’s 72-year-old patient was successfully treated with Intense Pulsed Light (IPL).
“This causes changes in the superficial blood vessels, eliminates some of the flora and raises skin temperature. The patient told us after IPL treatment that it was like ‘having a vacation from my eyes for the last month’,” he said.
Results published in the scientific literature show objective improvement in ocular surface disease index and tear breakup time, he concluded.
Shahzad Mian: smian@med.umich.edu
European Union Web-Based Registry
The aim of the project is to build a common assessment methodology and establish an EU web-based registry and network for academics, health professionals and authorities to assess and verify the safety quality and efficacy of corneal transplantation.
your Surgical Results
www.ecctr.org
ECCTR is a project funded by the ESCRS with initial support from the EU
EUROTIMES | MARCH 2021 CORNEA
the ECCTR Registry Join Track
25
ANTIMICROBIAL AGENTS: past, present & future
Donkey teeth, mouldy bread and the ongoing battle against infection. Dermot McGrath reports
The cycle of history has much to teach us when it comes to understanding the evolution and development of antimicrobial agents in the age-old fight against infectious diseases, according to Harminder Dua CBE, FRCS, FRCOphth, PhD.

In a presentation on the past, present and future of antimicrobial agents, Prof Dua outlined how ancient civilisations used a wide variety of animal, mineral and plant products to try to treat infections, some of which have surprisingly strong parallels to modern therapies.
“It is well known that the past determines the future, but to that I would add that the past is often the future,” said Prof Dua at the 11th EuCornea Congress.
For example, ancient Egyptian artefacts record at least 95 prescriptions for various eye diseases, explained Prof Dua.
“There were several extracts from plants and from animals that were used for a variety of applications and indications – garlic, resin, leaves, minerals and extracts from crocodile or flies, bone marrow from donkey teeth and even healthy pigs’ eyes which were mixed with ochre and honey to make concoctions to be poured into the eye or ear,” he said.
Prof Dua said that while many of these concoctions may seem rudimentary or eccentric from a modern perspective, we should not be too hasty to judge our ancestors.
“Ancient civilisations used extracts from donkey teeth and today we are using stem cells extracted from dental pulp for tissue regeneration. The ancient Egyptians also applied mouldy bread to infected wounds, not knowing that this would one day lead to the game-changing antibiotic penicillin,” he said.
LANDMARK BREAKTHROUGHS
The 20th Century saw a number of important landmark breakthroughs in combating infection with the discovery of sulphonamides, penicillin, aminoglycosides, macrolides, and agents such as tetracycline, chloramphenicol and cephalosporin, said Prof Dua.
“In the 1950s and 1960s we had a rich harvest of antibiotics such as colistin, vancomycin and, most noteworthy for ophthalmologists, fluoroquinolones, which are still the most popular antibiotics we use today. The introduction of azithromycin was also a game-changer in the trachoma eradication programme,”he said.
The picture became more sombre in the 1980s and 1990s as drug resistance started to emerge as a major problem.
“The magnitude of this problem is so immense that in 2016 the O’ Neill Report commissioned by the UK government suggested that without action, antimicrobial resistance will cause the deaths of 10 million people a year by 2050. This problem is compounded by the fact that the number of antibiotics produced dropped from 16 in the years 1983 to 1987 down to only two between 2008 and 2012,” said Prof Dua.
The main reason for the decline in drug production stems from the lack of profitability in developing new antibiotics.
“For every 100 drugs developed only one or two make it to market. At $2.5 billion spent developing each antibiotic drug, antibiotics are not profitable enough to recoup losses. My take on this is that governments have to join hands with industry in combating antimicrobial resistance and in developing new agents,” he said.
Highlighting some of the more interesting agents currently under
development, Prof Dua cited Teixobactin, a new class of antibiotics which has a novel mechanism of action by binding to lipid II and lipid III, important precursor molecules for forming the cell wall, and Cefpodoxime, which has activity in the presence of some beta-lactamases of Gram-negative and Grampositive bacteria.
Another exciting breakthrough is the antibiotic Halicin, the first drug of its kind to be discovered using artificial intelligence (AI).
“It can learn new patterns unknown to human experts. It has a novel mechanism of action of disrupting the flow of protons across a cell membrane. In initial animal tests it also seemed to have low toxicity and to be robust against resistance,” he said.
AMPS FOR OCULAR USE
A lot of research has also been devoted to antimicrobial peptides (AMPs), which are naturally occurring eukaryotic analogues of antibiotics, said Prof Dua.
“They are very effective against a range of organisms, namely Gram positive and negative bacteria and fungi and enveloped viruses with a low tendency for resistance. Because of the mechanism of action there is very little chance for the organism to develop resistance to these agents,” he said.
AMPs may turn out to be more effective for ocular use in combination therapies with antibiotics, said Prof Dua. He cited a recent publication by his group which showed that vancomycin, which is normally not very effective against pseudomonas, can be combined with a peptide (FK16) for greater efficacy than if using either agent individually.
Prof Dua also highlighted the promising work of Mario Nubile and Leonardo Mastropasqua in creating a stromal lenticule from a donor eye that can then be loaded with various chemicals or molecules for therapeutic effect before being implanted back into the eye.
“The lenticules can be taken and decellularised and impregnated with microparticles or nanoparticles for antimicrobial and wound healing effects and tissue regeneration. This will deliver a sustained delivery of the drug at the site of action,” he concluded.
EUROTIMES | MARCH 2021
CORNEA 26
Ancient civilisations used extracts from donkey teeth and today we are using stem cells extracted from dental pulp for tissue regeneration
Harminder Dua CBE, FRCS, FRCOphth, PhD
in the severity and duration of symptoms and can lead to depression and suicidal impulses in some patients, according to



 Vincent Borderie MD, PhD.
Vincent Borderie MD, PhD.
“Corneal neuropathy is a leading cause of patient complaints after corneal refractive surgery.


A library of symposia, interviews, video discussions, supplements, articles and presentations








Spotlight on:
Toric IOLs and Presbyopia



Glaucoma
Ocular Surface Disease
Corneal Therapeutics







Refractive IOL Patient Journey
Phaco Fundamentals
Prevention is always better than cure, so we really need to provide patients with very precise, preoperative information. We should always assess corneal sensation before refractive surgery and to avoid corneal refractive surgery in eyes with impaired corneal sensation,” Dr forum.escrs.org

EUROTIMES | MARCH 2021 CORNEA
NEW Online Education
27
Modules
Young ophthalmologists are invited to write an 800-word essay on “Has COVID-19 changed long-term clinical practice?”
The winner will receive a €500 bursary and the John Henahan Prize trophy.
CLOSING DATE FRIDAY 26 MARCH 2021
Entries to be sent to: henprize@eurotimes.org
For further information visit: www.escrs.org
Laser iridotomy vs lens removal
Lens removal more effective for angle closure; too many LPIs may be performed. Howard Larkin reports
Lens removal is more effective in controlling intraocular pressure (IOP) in primary angle closure glaucoma than laser peripheral iridotomy (LPI) and LPI has limited benefit for preventing angle closure, according to recent studies. These and other findings suggest too many LPIs are being performed, said David S Friedman MD, MPH, PhD, Albert and Diane Kaneb professor and director of the glaucoma service at Massachusetts Eye and Ear, Harvard Ophthalmology, Boston, USA, at AAO Virtual 2020.
Regarding LPI vs lens extraction for acute primary angle closure attacks, Dr Friedman cited two studies that found patients treated with phaco were more likely to control IOP without medications up to 80 weeks after the closure attack (Lam DS et al. Ophthalmology. 2008 Jul;115(7):1134-40) and 24 months after the attack (Husain et al. Ophthalmology. 2012 Nov;119(11):2274-81).
Similarly, for chronic angle closure, the EAGLE trial, involving 419 eyes in the UK, Asia and Australia, reported that lens extraction was better than LPI at IOP control, requiring fewer medications at a mean of 0.4±0.8 v 1.3±1.0, and providing better patientreported quality of life at 36 months. Early lens extraction was also likely to be cost-effective for treating patients with newly diagnosed primary angle closure (with intraocular pressure 30mmHg or higher) and primary angle closure glaucoma. On the downside, lens extraction runs a risk of posterior capsule rupture so treatment decision should consider individual risk factors, Dr Friedman said. The EAGLE results are also not generalisable to other types of primary angle closure or primary angle closure glaucoma (AzuaraBlanco et al. Lancet. 2016 Oct 1;388(10052):1389-1397).
A study involving 889 patients in Guangzhou, China, with angle closure without disease and one eye randomised to LPI found that while LPI was protective in reducing peripheral anterior synechiae, overall rates of PAS of one clock hour or more as well as IOP over 24mmHg and acute angle closure attacks were very low in the population studied. Just two control eyes over six years suffered acute attacks outside of dilation (three attacks occurred with dilation), leading Dr Friedman to conclude that “we may be doing too many LPIs”.
Adding iridoplasty to LPIs did not add value, another study found. In addition, a 2016 Cochrane review concluded that LPI is not effective for treating pigment dispersion, Dr Friedman noted.
As for location of LPIs, studies are inconsistent as to whether a superior v nasal or temporal position causes more dysphotopsias, though one study found more linear disturbances with a superior position and more pain with a temporal position, Dr Friedman said.
David S Friedman: friedman@meei.harvard.edu
EUROTIMES | MARCH 2021 GLAUCOMA
28
The EAGLE results are not generalisable to other types of primary angle closure or primary angle closure glaucoma
David S Friedman MD, MPH, PhD
Optic nerve stimulation

Visual field defects can be reversed by reactivating “silent” neurons using electronic microstimulation of the eyes and brain, Prof Bernhard

A Sabel, PhD told AAO 2020 Virtual.

Prof Sabel, who heads the Institute of Medical Psychology at the Otto-von-Guericke University of Magdeburg, Germany, described a device that delivers electrical pulses through pads on the forehead above the eyes. Stimulation travels through the eye and the optic nerved to the brain’s frontal cortex, 40 minutes per day for 10 days.
In six years of clinical studies involving more than 600 patients, 84% experienced an increase in their visual functions, which confirms earlier reports of a clinical trial where visual field size improvement averaged 24%, with 60% better vision in the impaired visual sector, Prof Sabel reported. However, individual patient responses are highly variable, ranging from “no change” to dramatic improvements (Gall et al., PLoS ONE 2016).
REACTIVATING ‘SILENT’ CELLS
This amount of improvement in 10 days cannot be explained by the growth of new cells, rescuing cells from death or regeneration, Prof Sabel said.
“We rather propose that there is a large number of hypometabolic, or ‘silent,’ nerve cells, which survive the disease and can, in principle, be re-activated.”
Evidence for this reactivation includes changes in the brain functional network with increased neural signaling from the occipital cortex to the frontal cortex after stimulation, a communication channel that is lost in patients suffering from optic nerve damage, Prof Sabel explained. Likewise, microcurrent stimulation increased brain oxygenation is seen in these areas after stimulation.
On a cellular level, electronic stimulation stimulates the “silent” neurons to fire more nerve signals, called “action potentials”, which leads to potassium release. This elevated potassium is sensed as tiny currents (ion flow) by nearby blood vessels and triggers upstream dilation. Disruption of this “neurovascular coupling” mechanism, as in vascular dysregulation in glaucoma, renders the cells inactive.
“However, we believe that with microcurrent stimulation we mimic this natural mechanism by stimulating artificially both the neurons and the blood flow to function. This is the basis of the reactivation of silent neurons and subsequent visual field improvement,” he suggested.
TREATING OTHER RETINAL DISEASE
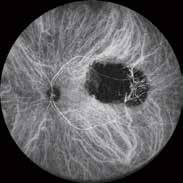


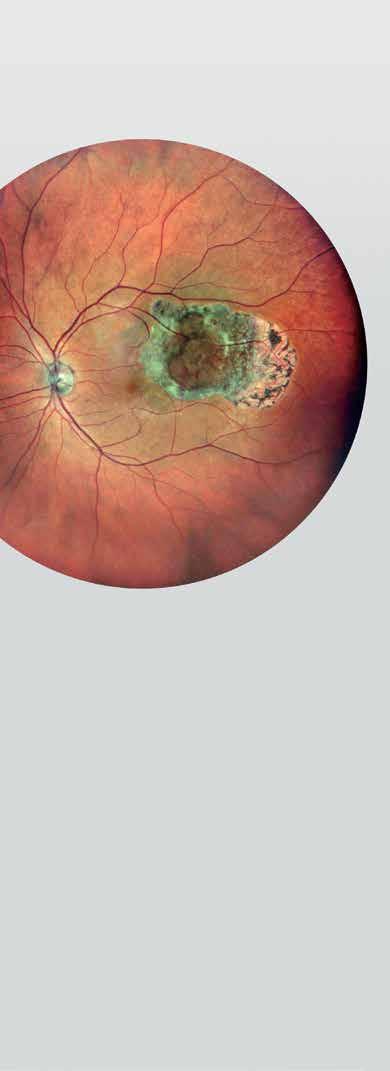
This technique has the potential to restore visual function not only in glaucoma, but also optic nerve damage and retinal trauma, diabetic neuropathy, vision loss after stroke or brain trauma and macular degeneration, Prof Sabel said. The treatment has no sideeffects, and its effect is stable in most patients. But about 16% of patients do not respond and duration ranges from several months to years. The causes of this variability are currently being studied.
“My ‘audacious’ proposal is visual field defects can be reversed by reactivating ‘silent’ neurons,” Prof Sabel concluded. “There is more light at the end of the tunnel of blindness.”
Bernhard A Sabel: imp@med.ovgu.de www.savir-center.com
EUROTIMES | MARCH 2021 GLAUCOMA
Device reverses some glaucomatous visual field loss, may treat other disease. Howard Larkin reports
29
World

Transplantation for severe OSD
Good results with cultivated oral mucosal epithelial transplantation. Dermot McGrath reports
Cultivated oral mucosal epithelial transplantation (COMET) is a very effective surgical modality that avoids graft rejection and complications when treating patients with severe ocular surface diseases such as StevensJohnson syndrome, ocular cicatricial pemphigoid or chemical injury, according to Tsutomu Ben Inatomi MD, PhD.
At WSPOS, we believe that “Expertise Resides ALL Over the World”
Free Membership
“It works very well for these severe cases. The transplantation of oral mucosal epithelium maintains the original characteristics of the tissue and is beneficial for stabilisation and conjunctival reconstruction. However, very strict postoperative follow-up of the reconstructed ocular surface is essential for a successful long-term prognosis,” Dr Inatomi said at the World Ophthalmology Congress 2020 Virtual.
Dr Inatomi, a researcher at the Kyoto Prefectural University of Medicine, Kyoto, Japan, said that cicatrising ocular surface disorders are typically very difficult to treat because of the loss of the stem cells and the scarring of the tissue.
“To overcome these issues, we have developed several advanced approaches such as intraoperative mitomycin C to inactivate the fibroblasts, amniotic membrane transplantation to promote epithelialisation, and also cultivated epithelial sheet transplantation, which has yielded some promising results for these difficult cases,” he said.
The advantages of cultivated epithelial sheet transplantation include rapid wound healing of the ocular surface, and easy expansion of large cell numbers from a small biopsy, said Dr Inatomi.
Join our society and become part of one of the largest networks of paediatric ophthalmologists in the world.
You’ll gain access to our wide library of videos, including our “Masters in Surgery” archive and also get the chance to collaborate on our global case report quiz.
“The sheet can contain a high content of progenitor cells, which is very helpful for ocular surface maintenance, and also if we use non-ocular cells as with COMET, we can treat bilateral disease with autologous tissue. Since we are using amniotic membrane substrate, we can prevent corneal scarring at the same time,” he said.
Auto-corneal epithelial transplantation is ideal for cases of unilateral disease, whereas either allo-corneal epithelial transplantation or auto-oral mucosal epithelial transplantation are better options for bilateral cases, said Dr Inatomi.
The COMET procedure entails harvesting a small amount of oral mucosa by biopsy, which is then cultured on amniotic membrane with feeder cells.
“Since these are autologous tissue non-ocular cells there is no risk of rejection. Oral mucosa is a very easy region for biopsy, and it can be repeated many times. The oral tissue has a high potential for proliferation, and there are a lot of phenotypic similarities between the oral and corneal epithelial surfaces,” he said.
Contact Info: WSPOS, Temple House, Temple Road, Blackrock, Co. Dublin, Ireland
Tel: +353 1 288 3630 Fax: + 353 1 209 1112 Email: wspos@wspos.org
Dr Inatomi said that his group has been using COMET for various types of ocular reconstruction in recent years and has obtained good results with this approach.
“It is useful, for instance, to treat acute stem cell loss because of rapid epithelisation, cicatrising ocular surface diseases with stem cell deficiency and conjunctival reconstruction,” he said.
COMET can also be used in conjunction with various keratoplasty techniques in order to obtain better visual recovery and a stable ocular surface. Limbal-supported hard contact lenses can also be used to correct irregular astigmatism, added Dr Inatomi.
EUROTIMES | MARCH 2021 PAEDIATRIC OPHTHALMOLOGY
is available
Membership to WSPOS
for FREE on www.wspos.org
Society of Paediatric Ophthalmology and Strabismus
30
Five congenital optic nerve anomalies to watch out for.
Roibeard Ó hÉineacháin reports
Anomalies in the Optic nerve at a Glance
There are five important congenital hereditary and non-hereditary optic nerve anomalies that require early diagnosis in order to preserve and enhance vision, Yair Morad MD, Shamir Medical Centre, Tel Aviv University, Israel, told the 2020 WSPOS Virtual Meeting.
The first of these is optic nerve coloboma. It results from incomplete closure of the embryonic fissure during the fifthto-seventh week of gestation. It usually involves unilateral or bilateral infero-nasal defects that may include the optic nerve, choroid, retina, iris and lens. Extended defects usually cause microphthalmia. Optical correction and patching are necessary in these children in addition to genetic counselling and renal ultrasound. Serous retinal detachment occurs in up to 45% of patients.
Optic pit is another important optic nerve anomaly. It is a congenital excavation of the optic nerve head that appears to result from defected fissure closure. It can appear in any sector, but is usually located temporally. Secondary serous retinal detachment occurs in 25-to-75% of affected eyes and becomes symptomatic in the third or fourth decade of life, though it can occur in children.
Morning glory disc anomaly is characterised by an enlarged disc, with a pink orange colour and white glial tissue in its centre. Other features of this condition include peripapillary excavation and pigmentation and an increased number of blood vessels. Visual acuity in affected eyes usually ranges from 6/60 to finger counting, although some eyes can have normal visual acuity.
Optical correction and a trial of patching is indicated in these patients. They should also be monitored for serous detachment. In addition, magnetic resonance imaging is also advisable because of the condition’s association with basal encephalocele and the rare vascular disorder Moyamoya disease.
Another optic nerve anomaly is tilted disc syndrome, in which the superotemporal part of the disc is elevated and the inferonasal part is posteriorly displaced, resulting in an oval-shaped disc with its long axis obliquely oriented. Many patients have a bi-temporal hemianopia that results from posterior bowing of parts of the retina causing a refractive scotoma due to myopic shift in these areas. However, this visual defect can be eliminated by additional minus lenses.
Reach
Yair Morad MD
46,748 *
Finally, there is the optic disc with myelinated nerve fiber layer, in which there is myelination of the afferent visual pathways starting from the lateral geniculate body and terminating in the lamina cribrosa. Some patients with the condition have normal vision but most have myopia and amblyopia. In some cases, the amblyopia does not respond to aggressive patching due to hypoplastic optic nerve or hypoplastic macula.
* Average net circulation for the 10 issues circulated between 1 January 2020 to 31 December 2020. See www.abc.org.uk
EUROTIMES | MARCH 2021 PAEDIATRIC OPHTHALMOLOGY
31
Years in print 25
Optical correction and a trial of patching is indicated in these patients.
• Reduced Registration Fees for ESCRS Congresses
• Subscription to Journal of Cataract & Refractive Surgery
• Access to ESCRS Grants, Bursaries and Research Awards
Access to:
• ESCRS iLearn
Online CME accredited interactive courses
• ESCRS On Demand

Online library of presentations from ESCRS Congresses
• EUREQUO
European Registry of Quality Outcomes for Cataract and Refractive Surgery
• ECCTR
European Cornea and Cell Transplantation Registry
5 year membership for trainees Join today. www.escrs.org
ESCRS Membership FREE
NEWS
Successful artificial corneal implant

Cornea Vision has announced that the CorNeat KPro, which the company describes as the first artificial cornea that completely integrates with the eye wall with no reliance on donor tissue, has been successfully implanted in a human. The surgery was performed on a bilaterally blind, 78-yearold male at Rabin Medical Center, Israel, by Professor Irit Bahar, Director of the Ophthalmology Department.
Dr Gilad Litvin, CorNeat Vision’s Co-Founder, Chief Medical Officer, and the inventor of the CorNeat KPro, said: “This is an extremely important milestone for CorNeat Vision, key in our journey to enable people around the world to fully enjoy their vision potential.”www.corneat.com
MARKETING AUTHORISATION

Aerie Pharmaceuticals has announced that the European Commission (EC) has granted a marketing authorisation for Roclanda (netarsudil and latanoprost ophthalmic solution)
0.02%/0.005% for the reduction of elevated intraocular pressure in adult patients with primary open-angle glaucoma or ocular hypertension for whom monotherapy with a prostaglandin or netarsudil provides insufficient IOP reduction. The marketing authorisation application for Roclanda was accepted for review by the European Medicines Agency in January 2020.
www.aeriepharma.com
NEW CLINICAL DIRECTOR
Heidelberg Engineering has announced that Mr Steve Thomson has joined the company as Clinical Director to further strengthen the company’s Anterior Segment product development team.
He has a background in ophthalmic imaging followed by more than 30 years’ professional experience in the ophthalmic industry said a spokesperson for Heidelberg.
“We are convinced that Steve is ideally placed to demonstrate how highquality imaging combined with comprehensive data canfoster confident treatment decisions and transform clinical workflows,” said Arianna Schoess Vargas, Heidelberg Engineering Managing Director.
www.heidelbergengineering.com/
Be everywhere. See everything Catch up on what you’ve missed www.escrsondemand.org With ESCRS On Demand, members can view the presentations from any conference. Catch up on all the sessions at a time and place that suits you. EUROTIMES | MARCH 2021 INDUSTRY NEWS INDUSTRY
33
Prof. Irit Bahar and Dr. Gilad Litvin during the first-in-human CorNeat KPro implantation
Lockdown limbo
From vaccines to definitions, life trundles on. Clare Quigley reports

Lockdown status: level 5. Government movement restriction: 5km. Hospital activities: urgent or emergency care only.
Sprawled out on the carpet with Duplo and wooden blocks scattered all around, Michael and I were busy. I was occupied building an elaborate tower of blocks, and he was engrossed in pulling pieces of Lego apart, holding aloft the shapes that he liked most, exclaiming at them, and at 14 months old, chewing on them too. When my phone rang out with the hospital’s number flashing up on screen, I was surprised. During my free evening time – when I was not on call – why would they be looking for me?
“Hello?”
“Clare?” It was Aideen, one of the ward managers. “The vaccine has arrived, we’re going to start vaccinating tomorrow. Do you want it?”
“Yes please,” I sat up.
Around this time Ireland had the worst COVID numbers in Europe, recording a seven-day rolling average of 1,267 cases per million in early January. This was after we had excellent numbers at 50 cases per million in early December.
That morning the jab was quick, almost painless. As synthetic messenger RNA was being translated into COVID spike protein in my shoulder
It seemed that as a nation we had relaxed and mixed too much over the Christmas break.
Getting vaccinated would be a relief. For my family, I am definitely the riskiest contact. My husband is working from home, not seeing people. Our child-minding system for Michael includes a shared nanny, a Brazilian woman who minds Michael together with his cousins in my brother’s house. I am careful at work, but I know that I am the most likely to get exposed, and go on to bring COVID home, and from there spread it on to my brother’s family and their two children. Getting vaccinated should reduce that risk by 95%, going by the Pfizer/BioNTech data.
Excited, even giddy, we waited for our shots the next day. The cataract unit, a dedicated theatre to allow for a higher volume of patients, had been repurposed as the vaccination centre for the hospital. That first day of vaccinating, there were about 60 doses arriving. Not enough for everyone, so some doctors and nurses would not get it straight away. People were anxious, enquiring about their place on the priority list. Clerical and admin staff wanted it, and needed it, as their work takes them in and out of the clinical areas of the hospital, but there were not enough doses to cover everyone just yet.
That morning the jab was quick, almost painless. As synthetic messenger RNA was being translated into COVID spike protein
in my shoulder, I went back upstairs to the main operating theatres. There was one urgent case that needed to go ahead – a tarsorrhaphy for a man admitted with a nasty Stenotrophomonas keratitis, who had a dangerously thinned cornea. It was a short procedure for me to suture the lids together, after excising a thin strip off the surface of the posterior lamella, with bolsters in place.
In January changeover happened, and I moved to the cornea team. The theatre lists, which were previously filled with cataracts, grafts, pterygiums and other anterior segment procedures, are empty now. Emergencies only. We have to cut down the clinic numbers as much as possible too. Some patients, though, still need to be seen. I work in a cornea clinic for the first time since my senior house officer years; I am a specialist registrar now, not so far from finishing training. After five years or so in ophthalmology, rotating through different units and specialist clinics, I feel confident that I have seen most common things. Day one in clinic the Consultant Barry Quill asked me to look at a patient and describe what I saw.
“There is vascularisation of the cornea...”
“What else? What level are those opacities at?” Mr Quill asked.
“Superficial stroma... With clear cornea in between.” The patient sat patiently as I puzzled at her eye.
I paused, unable to recall the eponym.
“Salzmann’s,” Mr Quill said.
I knew then that I would need to get back into my books. I had treated myself to the updated version of Kanski last year, but most of its pages still had that suspiciously fresh smell, despite my aims to have re-read the whole thing by now. Studying while being a parent and working full time must be possible. Lockdown at least adds time for reading, if only I can manage to overcome ennui and focus.
At the end of the working day I cycle back home. Arriving at the small square we live on, I wave at the neighbours. They are another family of three; the father is a professional actor, who has acted in plays in Dublin’s national theatre, and in film. Ten months and counting for closure of his industry here. I am reminded that everyone faces their own problems, directly or indirectly, because of this virus.
Clare Quigley is a resident at the Royal Victoria Eye and Ear Hospital, Dublin, Ireland
EUROTIMES | MARCH 2021 INSIDE OPHTHALMOLOGY 34
Illustration by Eoin Coveney
Memories of togetherness
Reflecting on last year’s ESCRS Winter Meeting as we look to the future. Aidan Hanratty reports
This time last year many of us travelled to Marrakech in Morocco for the 24th ESCRS Winter Meeting. The multiple pleasures of travel to new locations, seeing old friends and advancing knowledge make international conferences a wonderful experience.
These have been lost, like many other aspects of life we may have taken for granted, in the wake of COVID-19. Perhaps this loss is temporary, but perhaps our lives will be changed utterly. For now, we sit at home and log on to catch up on the latest science and technology.
Marrakech sees temperatures of up to 37 degrees Celsius in summer and in February it gets to a balmy 20 degrees, perfect for those of us in more temperate or extreme climates who might be used to colder, wetter weather throughout the winter. Getting to walk around in the sunshine without bundling up was a treat we wouldn’t enjoy again until a brief summer came some months later.
While the novel coronavirus disease was named COVID-19 on 11 February,
and guidance was issued regarding handwashing and general advice regarding cleanliness and vigilance, COVID-19 was only declared a pandemic by the World Health Organization on 11 March 2020.
With that announcement, workplaces around the world sent their staff home and governments prepared for the worst. Words like lockdown and social distancing became commonplace. It was a world away from the togetherness and camaraderie of the Winter Meeting.
For many it was the last opportunity to spend time with friends and colleagues, to enjoy restaurants safely and to sit back and learn from experts in the field of ophthalmology surrounded by a crowd of fellow interested parties.
This would be the last chance to browse eposters and discuss ideas with colleagues, to examine new offerings from companies at the exhibition.
A short drive from the conference centre, the historic Jemaa el-Fnaa is the centre of Marrakech’s medina, a hive of activity with snake charmers and salesman, selling everything from pottery and


clothing to drums and cuddly toys (some of the items this writer came home with).
Tourism came to a halt in midMarch with the country declaring a state of emergency. Tourists and traders alike will look back at this time with bittersweet memories.
The 25th ESCRS Winter Meeting Virtual 2021, in conjunction with the Polish Society of Cataract and Refractive Surgery, took place online from 19-21 February. While these virtual meetings mean we miss out on seeing new places, they do mean we can avoid the time-consuming travel that such conferences entail.
While we can’t meet friends for a drink, we can switch off the laptop after a meeting and go down and see family, not missing them for days at a time. If you missed out on any of the sessions for any reason, you can always catch them on demand for a month after the event.
We all look forward to the day we can meet again, to shake hands and embrace one another. Until then, let’s make the best of all the digital realm has to offer.
EUROTIMES | MARCH 2021 RANDOM THOUGHTS
35
Reopening clinics safely in a pandemic
Adaptability, efficiency and focus on improving patient experience keys to success, according to these two experts. Howard Larkin reports
Adaptability, adaptability, adaptability wins the day.”
That’s what Arthur B Cummings MMed(Ophth), FCS(SA), FRCS(Edin), PCEO, said of the successful reopening of his Dublin, Ireland, cataract and refractive surgery clinic after seven weeks shutdown during the first wave of the COVID-19 pandemic.

Just as important is focusing on improving the patient experience while increasing clinic efficiency, noted Guy Sallet MD, FEBO, of Aalst, Belgium. Drs Cummings and Sallet outlined the steps they took to reopen their private clinics
in the ESCRS Practice Management & Development Webinar “Rebuilding Your Practice in a Challenging Environment”, which took place in January and is available free of charge online.
ACTIVELY INVOLVING STAFF
At Dr Cummings’s Wellington Clinic, which does about 2,000 procedures annually with 90% in cataract, refractive and keratoconus, the road to reopening began as soon as the clinic closed on 27 March 2020. “The very next morning after the lockdown was announced, the team got together; myself, [clinic manager] Lisa [McLoughlin RGN, RM, BSc] and
[clinical support/research manager] Liz [Brennan BSc, MSc] to think about how we would get through.”
The most immediate concern was cancelling appointments over the next few weeks. Wellington was able to do it quickly and efficiently using the text messaging capability built into its electronic medical record (EMR), Dr Cummings said. Inbound phone calls were routed to the clinic manager’s cell phone.
Next, they did a staff analysis, dividing staff into four groups; critical, essential, helpful and not essential. Then staff processes were reviewed with an eye toward limiting staff-patient contact
EUROTIMES | MARCH 2021
PRACTICE MANAGEMENT 36
as much as possible, for example by conducting postoperative visits online or by phone when appropriate, Dr Cummings said. Other early steps included setting up connections so key staff could work remotely, sourcing vital personal protective equipment (PPE) and setting up an online shared appointment tracker to keep everyone informed of cancellations and restarting the clinic.
During the lockdown, optometrists and nurses phoned patients for postoperative appointments and virtual visits, reducing the wait list for reopening. Weekly staff meetings via Zoom helped keep the full team up to date and brainstorm work return plans. “This was more often meeting than before, but we felt it was necessary to keep everyone up to date.” Virtual consultations were offered to continue some services to patients.
One month before returning, Dr Cummings asked each staff member to submit suggestions on reworking the patient journey and process changes in writing. These were consolidated and discussed during a half-day Zoom meeting. The team voted on the best ideas and the final processes developed were a hybrid of all the staff ideas. A new patient appointment diary was configured to allow all the new processes, which were designed for maximum safety and efficiency.
Process changes included creation of an e-pack for prospective patients that includes all they need to get started. “It used to be we got all the information in a lengthy phone call. Now the phone call is quite short and all one needs is an email or text address and we send the e-pack,” Dr Cummings said. It includes a link to Wellington’s online medical history form using FormStack (formstack.com). Online payment options include Stripe and PayPal to further reduce time in the clinic. Involving all staff in developing the new processes had multiple benefits, Dr Cummings said. “Many heads are better than one but it also helps to provide a sense of control to a team in uncertain times and it encourages their adoption of new processes.”
MINIMISING CONTACT, MAXIMISING EFFICIENCY

Dr Sallet took similar steps early on at his Eye Institute, including creating a new patient flow and scheduling template allowing all preliminary diagnostic testing
to be completed before patients see the doctor with an eye toward minimising clinical contact. For cataract this includes, topography, biometry, fundus camera and OCT; for glaucoma, perimetry, non-mydriatic fundus photography and OCT; and for pre-refractive, topography, tomography, biometry, fundus camera, dry eye assessment and cycloplegia. The doctor reviews the results and has a good idea of the case before seeing the patient.
“This means the patient spends less time in the doctor’s office but the contact with the doctor is more intense. We are not looking at our files at that moment so we have more time for the patient,” Dr Sallet said. The result is a more professional approach and better patient experience, he added.
Dr Sallet’s clinic also relies on technologies such as OCT and nonmydriatic photography to reduce reliance on perimetry, which reduces the frequency of visits to monitor glaucoma progression. To reduce visits for cataract surgery, he is moving toward doing more same-day bilateral procedures, though this is a financial challenge because currently the second procedure in a day is not reimbursed in Belgium.
At Dr Cummings’s clinic most cataract and refractive surgery day-one appointments (except for LASIK) are now done remotely “and it is working absolutely, perfectly well”.
REARRANGING OFFICE SPACE
Meeting patient expectations for safety is critical, and that begins with rearranging offices and installing plexiglass shields throughout the clinic to protect both patients and staff, Dr Sallet said. In his case, he was fortunate that his clinic was undergoing renovation, so creating larger exam rooms was easier – though it comes at the expense of seeing fewer patients in a larger space. Dr Cummings followed similar steps before reopening.
Having less waiting room capacity and the need to schedule fewer patients to avoid crowds and make room for emergencies further cuts the number of patients each doctor can see in a day, but is necessary both for safety and to reassure patients that the practice is safe, Dr Sallet said. “Patients expect less crowding.” Upon reopening, Dr Cummings introduced temporary longer opening hours to address this need for
social distancing and reduce an extensive waitlist from appointments cancelled during the lockdown.
Actively communicating the steps taken to protect patients is also essential, Dr Sallet added. He does this through announcements and posting on the clinic web site. Emphasising the safety steps he is taking has helped patients feel more comfortable coming to his ambulatory surgery centre than to public hospitals, a trend he expects will continue after the pandemic.
Indeed, the pandemic has pushed him to think more directly in terms of improving patient experience and flow rather than relying on approaches such as seeking accreditation, which is expensive and does little to affect patient experience. “COVID-19 has taught us some things that can improve patient experience after the pandemic.”
REFRACTIVE RECOVERY
Another bright side of the pandemic is it has renewed interest in refractive surgery, in part to help patients cope with masks fogging eyeglass lenses, Dr Sallet said. Increased disposable income due to less travel and eating out is also driving the trend, as is a renewed focus on personal health and comfort brought about by the need to stay home most of the time, Dr Cummings said. In addition to laser refractive surgery, he is seeing greater interest in multifocal IOLs for cataract patients.
The increase in refractive procedures has helped Dr Sallet’s clinic offset some of its losses from closing and serving fewer patients. At Dr Cummings’s clinic high interest in refractive procedures allows him to fill appointment cancellations almost as fast as they occur – which is essential for the clinic’s survival.
“To remain financially viable, you have to do enough procedures,” said Dr Cummings, whose private clinic was among the four out of 14 refractive clinics in Dublin to survive the 20082009 financial crash. He recommended keeping up with consumer confidence and economic trends as much as clinical developments, and constantly adapting to keep pace and provide the best possible patient experience and outcomes.
EUROTIMES | MARCH 2021 PRACTICE MANAGEMENT
37
COVID-19 has taught us some things that can improve patient experience after the pandemic
Guy Sallet MD, FEBO
Many heads are better than one but it also helps to provide a sense of control to a team in uncertain times and it encourages their adoption of new processes
Arthur B Cummings MMed(Ophth), FCS(SA), FRCS(Edin)
Keep learning. Whenever, wherever.
The journey is the reward
In India when I was a child there were two options that were always there for anyone who liked science. One was to be a doctor and the other was to be an engineer. I definitely didn’t want to be an engineer so I chose to become a doctor.
Once I started medical school, I found that I liked the surgical field better and when it was time to choose the surgical field, I chose ophthalmology simply because I thought it was a much more elegant form of surgery –the microscopic nature and views, the small and delicate structures that you’re dealing with, the finesse that is there in these surgeries that you don’t see in other surgeries – bloodless, clean and beautiful! This together with the fact that here is a field where you can almost always directly see the operative field before and after surgery giving great clarity to decision-making processes and the ability to study postoperatively, the exact outcomes of what our surgical manoeuvres have brought about. Best of all, ophthalmology is capable of bringing life-changing improvements for our patients. You end up making a lot of difference to people’s lives. India has a burden of blindness of about 10 million which is close to the population of London and Paris combined, so I’m very happy about the choice I made.
I started working with Professor Amar Agarwal in Dr Agarwal’s Eye Hospital, Chennai, India. This was a place always full of innovation and inviting new ideas and new thinking. I think that really made a lot of difference to me and changed my outlook to ophthalmology. It made me start thinking about new things and new ways to do things.
Learn online in your own time, with self-paced and assessed ESCRS iLearn courses on:

∙ Cataract Surgery
∙ Cornea
∙ Refractive Surgery
∙ Visual Optics
Trainers: use the task list to assign courses for trainees and monitor their progress.
Learn more at https://elearning.escrs.org
There have been many other big influences in my life, including my parents, right from my childhood. They moulded me to become an inquisitive person and to try and find answers. My husband is huge source of support for me. Being a cardiologist, he understands the medical field, of course, and I am fortunate to get a lot of encouragement and advice from him. My children are terrific and luckily have taken to the challenge of a working mother well.
My principle is to delegate what you don’t absolutely need to do yourself and do what you know that only you can do. You only have a limited amount of time and you need to use that wisely. You have to have a well-rounded life and the only way to do that is not to waste time.
If I was asked for advice from a young surgeon who is just starting out, I would tell them to start steady, aim high and keep thinking and keep going.
You have to understand that the journey is the reward.
Dr Soosan Jacob, MS, FRCS, DNB is Director and Chief at Dr Agarwal’s Refractive and Cornea Foundation, Chennai, India. This interview is based on an interview with Dr Jacob in the EuroTimes Eye Contact series https://player. escrs.org/eurotimes-eye-contact/five-questions-withsoosan-jacob-paris-2019

EUROTIMES | MARCH 2021 MY LIFE IN OPHTHALMOLOGY
Dr Soosan Jacob on why she became an ophthalmologist and the influences that shaped her career
38
Soosan Jacob, MS, FRCS, DNB
Due to the COVID-19 virus, a number of meetings have been cancelled or rescheduled. The information in this calendar is correct at the time of going to print; please check the meeting website or email the conference organisers to confirm all meeting dates.
↙ LAST CALL
MARCH 2021
AICCER Congress Online
Virtual Meeting
19 – 21 March
https://aiccer.it/congressi/congresso-2021
APRIL
6th San Raffaele OCT & Retina Forum
Virtual Meeting
9 April: 17.30 – 20.00
23 April: 17.30 – 20.00
30 April: 17.30 – 20.30
https://www.octforum2021.eu/
American Association for Pediatric Ophthalmology and Strabismus 2021 (AAPOS 2021)
Virtual Meeting
9 – 11 April https://aapos.org/meetings/ meetings-future
MAY
ARVO 2021
Virtual Meeting
1 – 7 May
https://www.arvo.org/
MAY
NEW
WEBINAR CHIRURGIA
Virtual Meeting
8 May
https://aiccer.it/congressi/congresso-2021
JUNE
AECOS 2021
European Symposium
3 – 6 June
Florence, Italy
https://aecosurgery.org/ 2021-european-symposium/

EUROTIMES | MARCH 2021 CALENDAR 39
3↙
The AECOS 2021 European Symposium will take place in Florence, Italy
JUNE
46th Meeting of the European Paediatric Ophthalmological Society
– EPOS 2021
Virtual Meeting
18 –19 June
https://epos2021.dk/
JULY
AECOS 2021 Summer Symposium
15 – 18 July
Utah, USA
https://aecosurgery.org/ 2020-summer-symposium/
2021 ASCRS Annual Meeting
23 – 27 July
Las Vegas, Nevada
https://ascrs.org/news/ ascrs-news/2021-ascrs-annualmeeting-update
33rd APACRS–
SNEC 30th Anniversary
Joint Meeting
Virtual Meeting
30 – 31 July
https://apacrs-snec2020.org/
AUGUST
39th Congress of the ESCRS
27 – 30 August
Amsterdam, The Netherlands
https://www.escrs.org/
SEPTEMBER
49th European Contact
Lens and Ocular Surface Congress (ECLSO)
3 – 4 September
Paris, France
https://www.eclso.eu/
SEPTEMBER
EURETINA 2021 Virtual 10 – 12 September
https://www.euretina.org/
OCTOBER
Joint event: 14th National Congress of Bulgarian Society of Ophthalmology and Conference
Innovation in Ophthalmology 2021
14 – 17 October
Borovets, Bulgaria

https://mareamedical.com/en/events/ ophthalmology_oct_2021_english/
NOVEMBER
AAO 2021
12 – 15 November New Orleans, USA https://www.aao.org/ annual-meeting
DECEMBER
SOE Congress 2021
2 – 4 December Prague, Czech Republic https://soe2021.soevision.org/
EyeJC (ESCRS Journal Club)
Advanced Instructional Courses
Eye Contact Interviews
Video of the Month
Video Journal of Cataract, Refractive & Glaucoma Surgery
Young Ophthalmologists Videos: “My Early Surgeries”
the latest video content from ESCRS
on the ESCRS Player player.escrs.org
Watch
and EuroTimes, FREE
EUROTIMES | MARCH 2021 CALENDAR 40
The AAO 2021 Annual Meeting will take place in New Orleans, USA
Joint event: The 14th National Congress of Bulgarian Society of Ophthalmology and Conference Innovation in Ophthalmology 2021 wil take place in Borovets, Bulgaria

Belong to something energetic. Join us. Are you ready for the next step? Visit www.escrs.org for information about membership & benefits
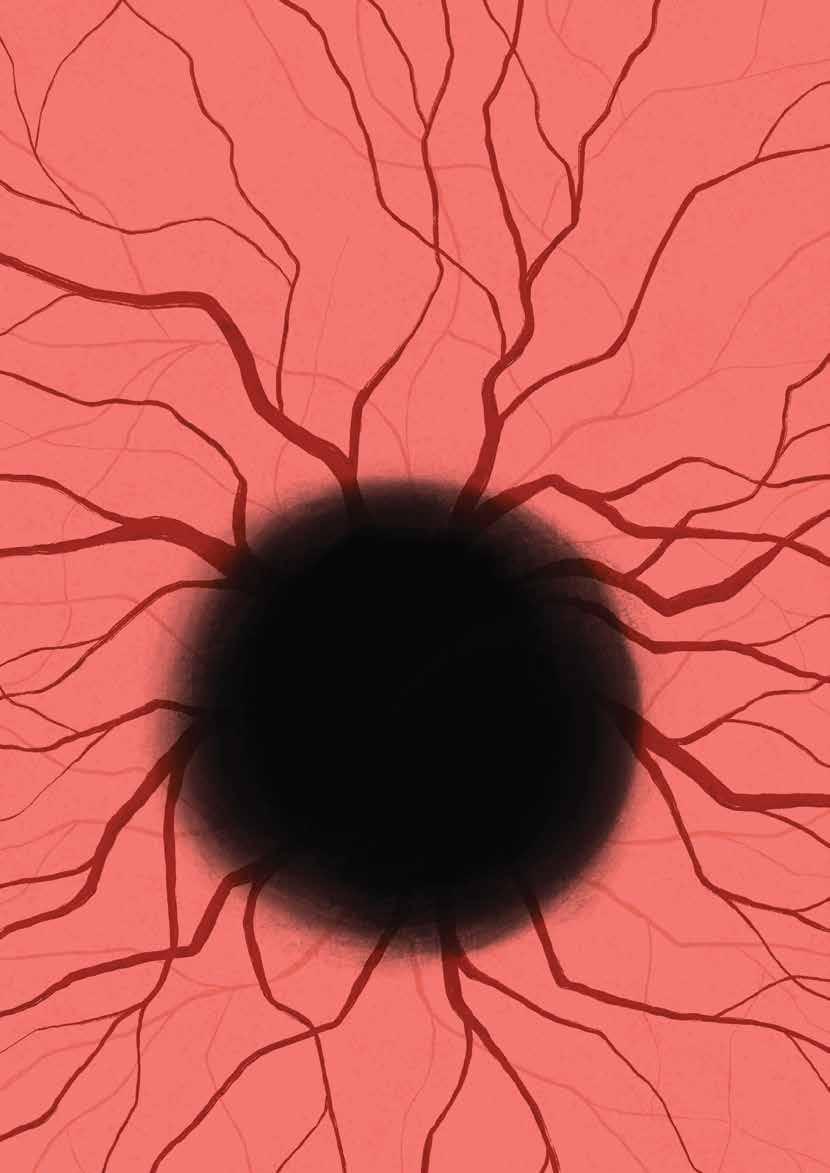








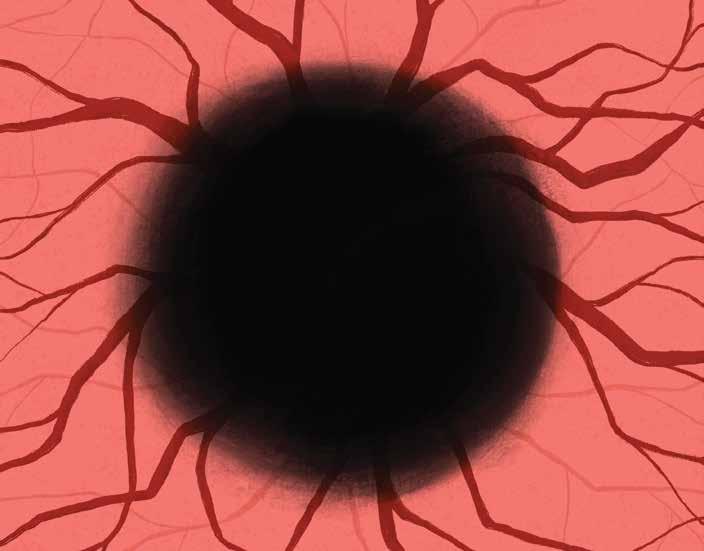
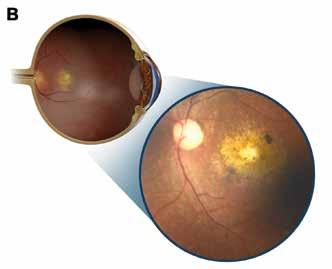
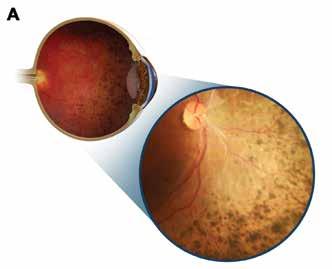










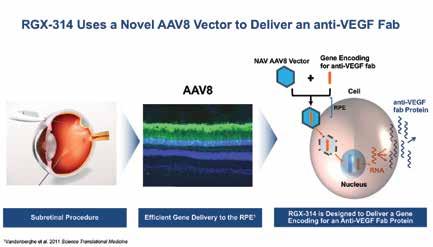




















 Vincent Borderie MD, PhD.
Vincent Borderie MD, PhD.