Portfolio 2020
MIDO — Toolkit
By Franziska Polka
a toolkit for people with bipolar disorder
University of Leeds
Design Future Society

Portfolio 2020
MIDO — Toolkit
By Franziska Polka
University of Leeds
Design Future Society

Bipolar disorders are severe conditions from which affected people suffer throughout their whole lives (Strakowski, 2014). It is spoken of as disorders rather than a disorder because the condition covers a broad spectrum. Bipolar disorder is the sixth leading cause of disability worldwide (Wittchen et al., 2011). It is characterised by intense mood swings which alleviate between mania and depression (National Depressive and Manic-Depressive Association, 2001).

Approximately 5 per cent of the population, suffer from a disease stemming from the bipolar spectrum during the course of life (Merikangas et al., 2007). 5%
it important?
The most serious problem is that the suicide rate among people who suffer from a bipolar disorder (BD) is significantly high (Morgan et al., 2005; Parker, 2007). Suicidal ideation is especially a symptom of depressive episodes (Strakowski, 2014) It is the most common cause of premature death in BDs (Lam 1997).
Excessive behaviour due to manic episodes affect the everyday life and interpersonal relationships of affected people and therefore can lead to social isolation (National Depressive and Manic-Depressive Association, 2001). Depressive episodes also fuel this isolation due to diminished socialisation and in some cases reduced personal hygiene (Meyer and Hautzinger, 2013).
Manic phases can lead to financial ruin due to uninhibited consumer behaviour and excessive spending which in turn fuel enstrangement of relatives (National Depressive and Manic-Depressive Association, 2001). This is not only a problem for individuals but also for society (Meyer and Hautzinger, 2013).
Additionally BDs are characterised by stigmatisation (Hawke et al., 2013) which contribute to an decreased quality of life. External stigmas can lead to exclusion and denied opportunities e.g. at the workplace or at institutions. Added to this is the self stigma which describes the assimilation of stereotypes which leads to reduced self-esteem (Markowitz, 1998).
The solution should help people to seek help in everyday life and crtical situations such as depressive or (pre) manic situations. It should raise disease awareness among people who suffer from a BD and if possible, include relatives.
How may a servicedesign solution help people who suffer from bipolar disorder (BD) ease everyday life?
To tackle the design challenge I applied the human centered design approach. I choose this approach, in order to view the challenges from the human/patient perspective. Focusing on the pain- points and needs of affected people will help develop a comprehensive sufficient solution.
To empathise with people who suffer from a BD interviews were conducted and secondary research was undertaken. For ethical reasons the interviews were cancelled.
Understanding the needs of patients was accomplished by focusing on qualitative research. Especially studies which shed light on good coping patients helped understand that the concept must emphasis on empowerment.
Defining and constraining the goal assured that the concept was manageable.
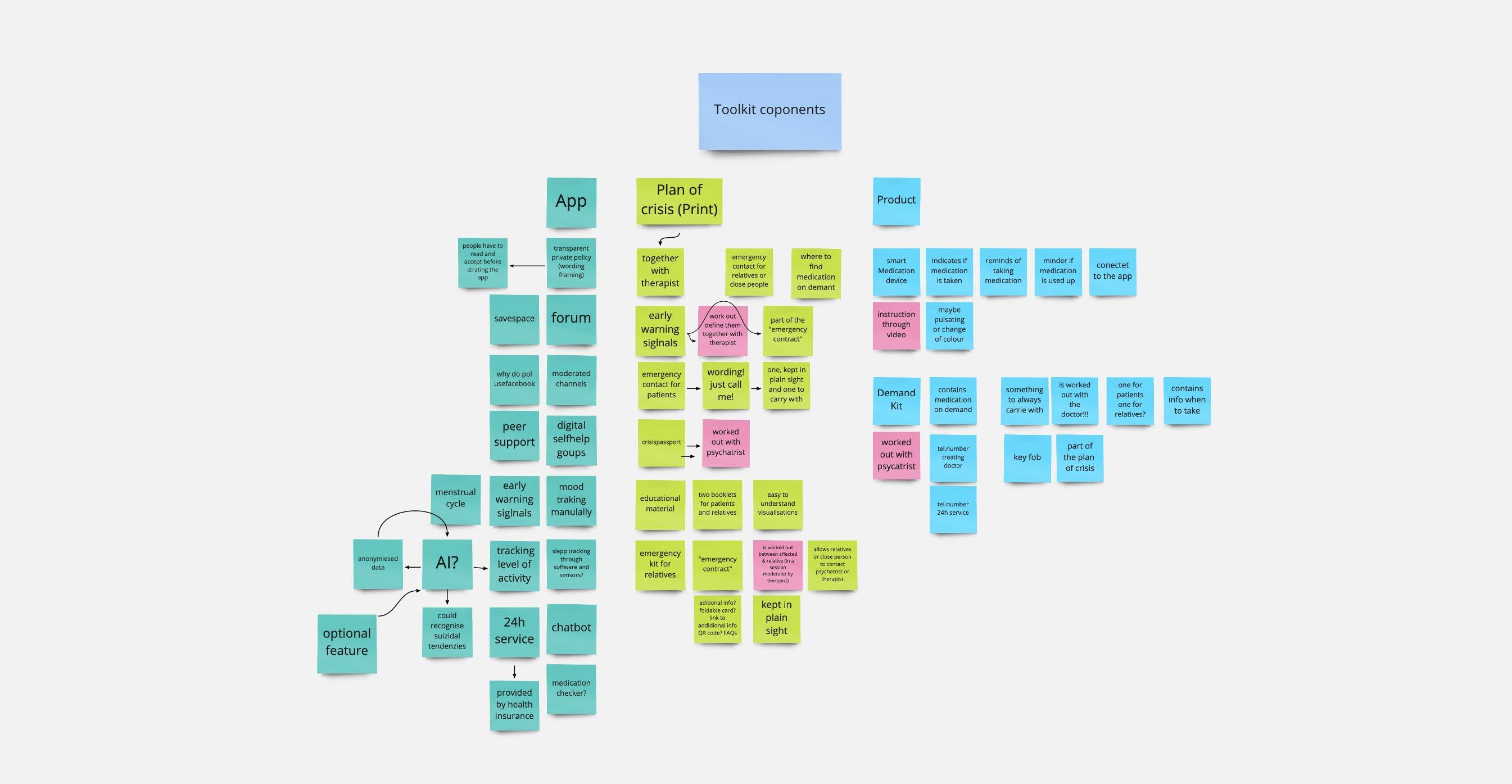
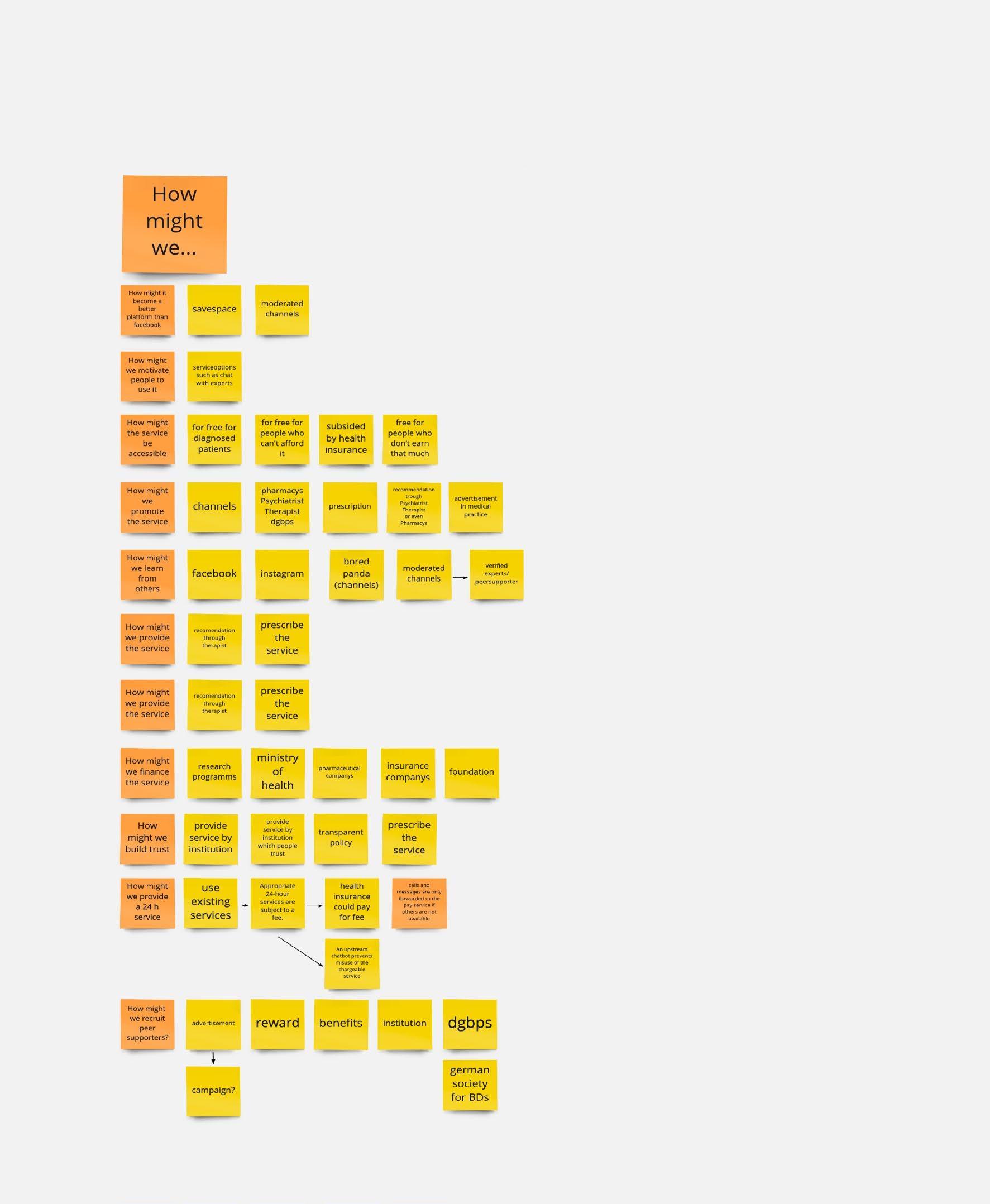
In the next step ideas were developed and the goal was redefined. The constraints helped sorting out ideas. Design thinking methods like the how might we method hepleped evaluate the ideas.
In the next step the devolpment of the concept began. Whith the help of patient jurneys, stakeholder maps and brainwriting the concept was concretised.
Testing ideas and flows constantly and in several iterations enabled a user-friendly solution that meets the needs of the patients.



As it was important to the concept to include all stakeholders, I set up a stakeholder map. With a stakeholder map, the actors of a project and their relationships to each other can be visualised (Stickdorn and Schneider, 2019). The map makes it possible to highlight the interests of the different stakeholders (Stickdorn and Schneider, 2019). With the help of the mapping, the needs of the groups, persons and institutions involved can be identified. It not only shows the needs of the actors, but also the exchange of goods and non-monetary items such as trust, information, security or data. This method allows developing holistic concepts which serve the various needs of involved actors.
To aim of the interviews were to gain knowledge about the everyday life of people and grasp the needs feels and pain points of people who are affected by a BD. However, only two people could be recruited to take part at the interview a third person cancelled the interview as she did not want to talk about the condition and be confronted with the fact that she suffers from a BD.
1. Do you have a diagnosis?
2. When did you get the diagnosis?
When I conducted the interview, I recognised that some questions led to discomfort among the participants. I had one question where I asked “How does your environment deal with the disease?” both participants answered that they do not have a social environment as most of their family and friends have turned away from them. Asking such a question has shown me the problem with interviewing people with a BD as they are a vulnerable group. At the end of one interview, one participant was very enthusiastic about the whole topic, and I was scared that her enthusiasm might lead to a manic episode. To interview people from such a group, a lot of ethical concerns need to be taken to account and the questions must be critically screened.
Insights:
>> people are socially isolated
>> the BD plays a signifikant role in peoples everyday life
>> a person has stated that she does not leave the house during a depressive phase and neglects her personal hygiene, however she has noted that it helps her to communicate with others on facebook and gives her energy and hope
When I have depessions I neglect my personal hygiene completely so that I cannot go out at all and also so that nobody can visit me.
I found a group on facebook and I read and wrote in it and that really got me out of the depression. When I have this depression then I sleep all the time, I get up for a moment and then lie down again, but because I had this group there, I just didn‘t lie down again.
I think that‘s really great, because there is a low barrier to do something. You really only have to take your mobile phone in your hand and go in there. It really helps me to pull me out of this total nothing.
3. How do you experience the disease in everyday life? In which situations do you feel it is a limitation?
4. Are you under psychological treatment?
5. Are you taking any medication? How do you deal with it? How often do you take medication?
6. What would help you in depressive phases?
7. What would help you during manic episodes?
8. Do you have an emergency plan? Do you have emergency medication? Where do you keep them?
9. Did you conduct a mood diary? How‘d that work?
10. How is your environment coping with the disease? Is there anything that bothers you about it?
11. Do you have any support in everyday life (e.g. mindfulness exercises)
12. What would help you in dealing with the disease?
13. Do you have any whishes?
Most literature focuses on challenges and issues that come with a BD and how people are affected by it. Nevertheless, there were a few studies that also shed light on people who are coping well with their condition. These qualitative studies investigated strategies that help people in dealing with their condition. One study found that coping also depends on the mindset towards BD. In one study the participant stated that it doesn‘t define her as a person this mindset empowered her to take control of the condition (Michalak et al., 2011). In their qualitative study Michalak et al. (2011) show that those affected are not always passive and that active management of the disease can have a positive influence on its course. Sharing this attitude of good coping individuals with others offers enormous potential and could help to mitigate self-stigma. To serve the needs of people who suffer from a BD a solution should not patronise people and should further empower them to take control of the condition. Another study found that mood assessment raises the awareness of individual mood changes and helps people take countermeasures (Lam and Wong, 1997). Sensitising oneself to one‘s mood swings has a positive influence on the course of the illness, as the mood swings can be better classified and can thus be controlled in an early stage. Encouraging patients to monitor their moods is helpful, so it would be possible to reward mood tracking in a concept. The tracked moods could then be discussed with the faithful species or therapists. Every person is different, and some people have a higher level of activity than others. A mood diary can depict this individuality.

”...it’s something that I manage but it is not who I am“
Participant in (Michalak et al., 2011, p.217)

a comprehensive service toolkit that empowers people to manage their condition and that helps people in critical situations
Agreement of crisis
MIDO APP PassporCrisis t info i
App — provides support and raises disease awareness
Products — ease life with the condition
Plan of crisis — involve relatives and help prevent relapses
Promotion material — for patients, doctors and therapists

>> only for people who are undergoing psychiatric treatment
>> accompanying psychotherapy
>> it is not a replacement for any therapy or medication
>> it cannot heal the disease
>> toolkit should empower people and not patronize

The user journey map or in this case the patient journey map visualises the process and the different stages of a service. It helps to observe touchpoints and allows to see where and when the user interacts with what or whom (Stickdorn and Schneider, 2019). It can represent parts of a service or the full experience. With this tool, it is easy to identify which information a user need at what point (Stickdorn and Schneider, 2019). The journey map takes a look at the users‘ pain points and sheds light on opportunities within the process (Stickdorn and Schneider, 2019).














To get a feeling for the dimensions I made a rough cardboard mock up. Obviously the first mock up was much too big, because I had difficulties to grip the lid due to its size. The cardboard model saved me a lot of time. In the course of time I built another cardboard model so I could estimate how much space is available for the technical equipment and which dimensions are easy to grip with one hand. Afterwards I started to make and design a CAD model. In the next step I printed and tested the model in 3D.




With the what-if method, the concept can be evaluated and allows to play through possible scenarios (Stickdorn and Schneider, 2019). The method helps to view the design from the perspective of the critic in order to explore possible problems at an early stage. On the one hand this makes the design more secure. On the other hand, the design can be better argued. For example one risk which was detected through the method was that peer supporters might be overstrained. Answering the what-if question ensures the development of a satisfactory solution that also takes ethical concerns into account.
The how might we method helps to reframe challenges, requirements and goals (Interaction Design Foundation, 2020). The method helps formulating a better design challenge and turn these challenges into opportunities (Interaction Design Foundation, 2020). The method stimulates the imagination and enables to view challenges from a new point of view and opens up possibilities. For example, the question of how the service might be promoted came up, which led to the decision that the concept must involve psychiatrists who then prescribe toolkit. Thinking about how the service might be financed opened the discussion of including pharmaceutical companies in the solution.

Target group are people who are diagnosed with a bipolar disorder and who are aware of their condition. The toolkit is aimed specifically at people who are willing to work on dealing with their condition. As the toolkit includes an app and a smart device, the focus is mainly on people who are open to new technologies. Furthermore it is a oportunity for people who live in rural areas.
Problem
people with BD are stigmatized and socially isolated poeple who undergo manic phases sometimes spend enormous amounts of money which leads to financial ruin this in turn leads to costs for society huge costs for the health system due to hospitaisation
high suicide rate among peole who suffer from a BD
high DALY rate
promote the service
recruit peer supporters
more testing iterations with more participants
developing and producing the device
programing the app
a comprahensive servicewhich meets and serves the needs of affected people and that empowers them to manage their condition
a service that is accessible for isolated people and people in rural areas
a service wich allows patients to get in touch with their peers
Key ressources
medical know how (pharmaceutical company)
marketing
programming
Key ressources
>> marketing
>> support
>> development
>> promotion material
>> recruitment/training peer supporters
>> 24 hour service
24/7 help service with experts
concept which is emeded in the therapy concept
support from trained peers forum which serves as a savespace
people with a clear diagnosis of BD
patients who are aware that BD is a disease
people who are aware of their condition an who are willing to work on it
people who are open to use technologies
Channels
therapists & psychiatrist
medical practice boards
pharmacy magazines (e.g. Apothekenumschau)
Revenue streams
>> prescriptions
>> public funding
Key partners
pharmaceutical industry
health insurance companys
psychiartrists
psychologists
Agreement of crisis
MIDO APP PassporCrisis t info i
App — provides support and raises disease awareness
Products — ease life with the condition
Plan of crisis — involve relatives and help prevent relapses
Promotion material — for patients, doctors and therapists

The app combines several functions. On the one hand, it is a savespace where peers can exchange information and advice. On the other hand it offers the possibility to document one‘s own mood in order to develop a better picture of individual moods and thus to better understand one‘s own illness. In addition, the app offers a 24 hour service for emergencies and other requests concerning the illness. The medication device is also managed and adjusted via the app.
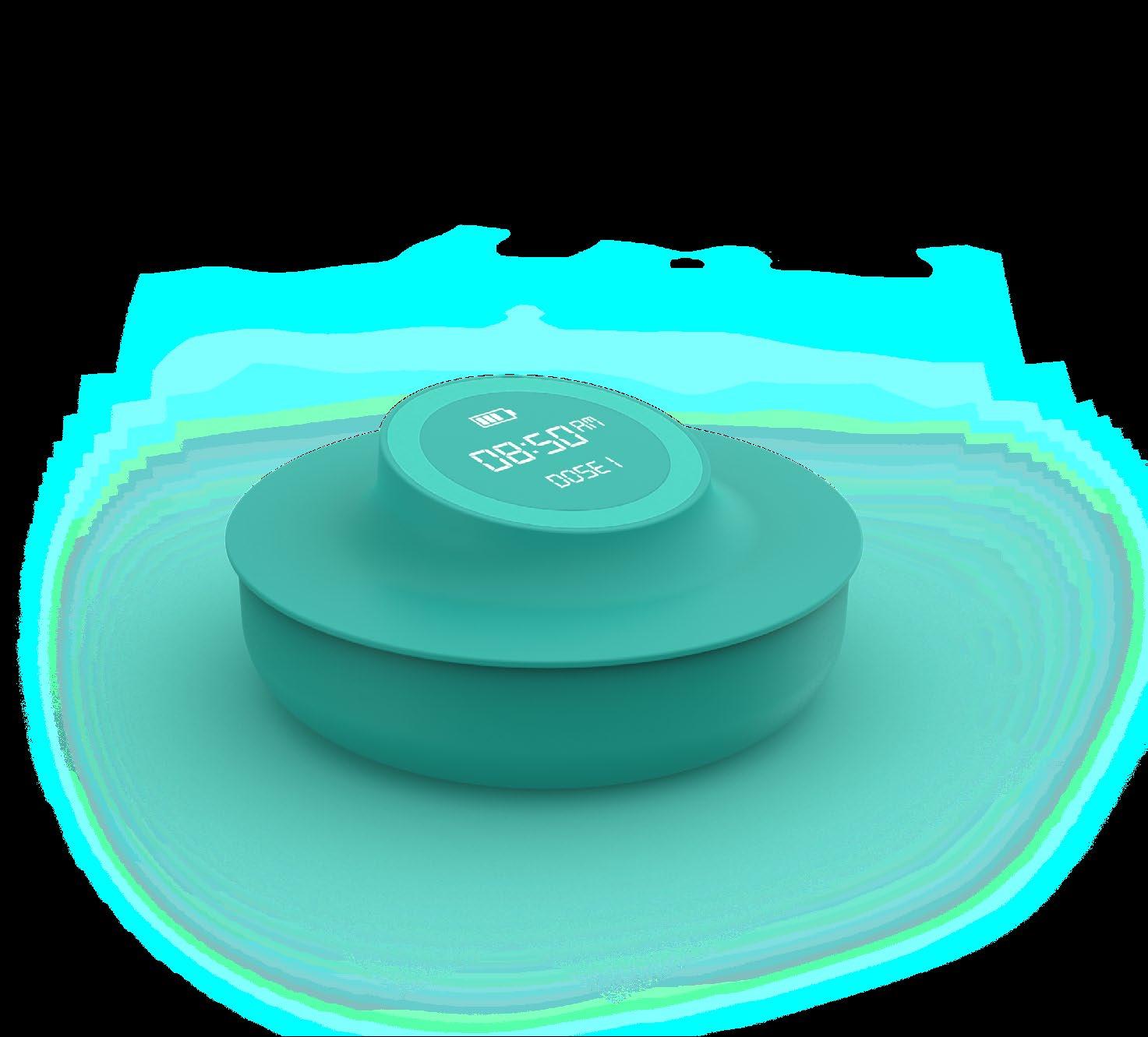
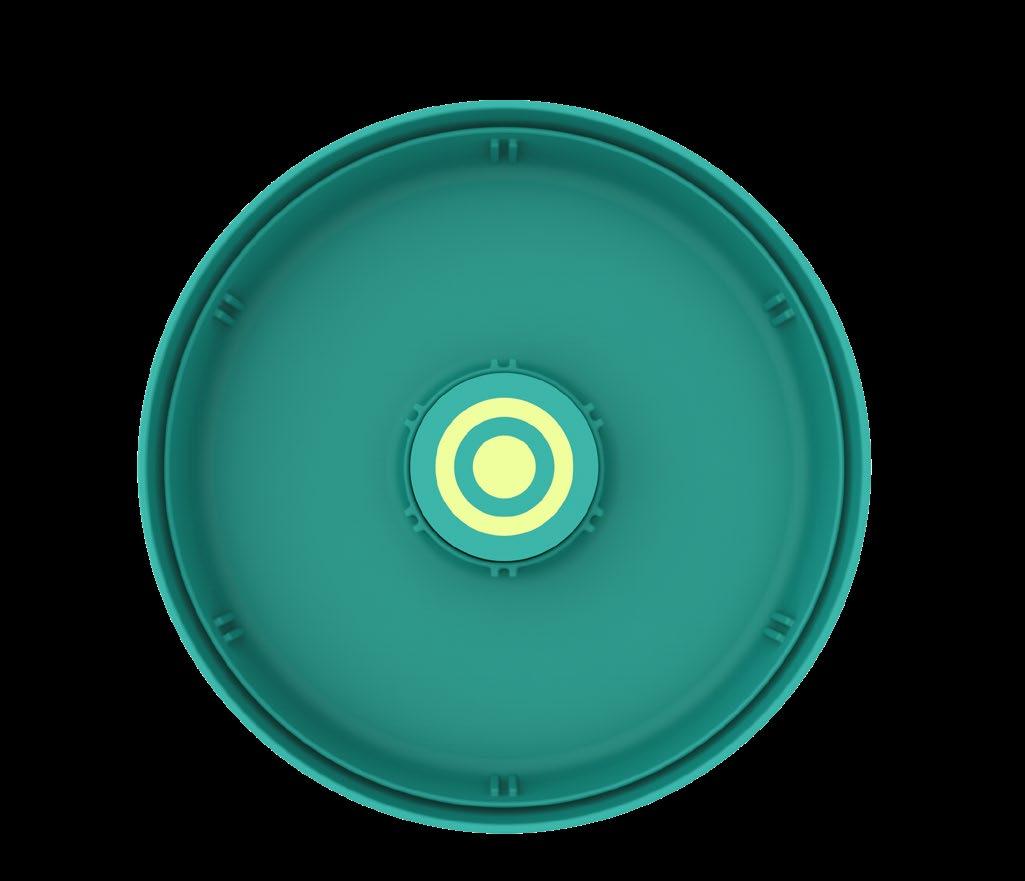
The smart medication device is used to remind the patient to take the medication and to indicate if the medication has been taken. The device is also a much nicer alternative to the clinical looking drug dispensers on the market. The device also functions as a clock. The fob contains the medication on demand and a dose of the standard medication. This ensures that patients always carry the emergency medication with them.

The crisis plan is worked out together with the psychologist and the psychiatrist. It consists of a crisis agreement that the patient and his relatives agree on and a crisis pass that the patient carries with him.




























The MIDO forum offers support from expert patients. Expert patients are users that have been managing their bipolar disorder effectively for 2 years or more and have received training to provide support. They are not allowed to recommend medication.
Proudfoot et al. (2009) found that it is beneficial for newly diagnosed patients to recieve support from trained peers who also have the diagnosis of a BD (and are coping well with it). Recently diagnosed patients feel understood and are more open to confiding their struggles (Proudfoot et al., 2009). Further, communicating with these trained peers reduced selfstigmatisation, as exchanges with affectet people who were coping well reduced their feeling of being different (Proudfoot et al., 2009). In the concept the expert patients are recruited by cooperating psychiatrists who are provided with promotion material. The psychiatrists can assure that these patients are managing their condition well. The training is finaced by the social health insurance. To motivate peers to take part in the program expert patients are rewarded (eg. Vouchers for massage or cinema).

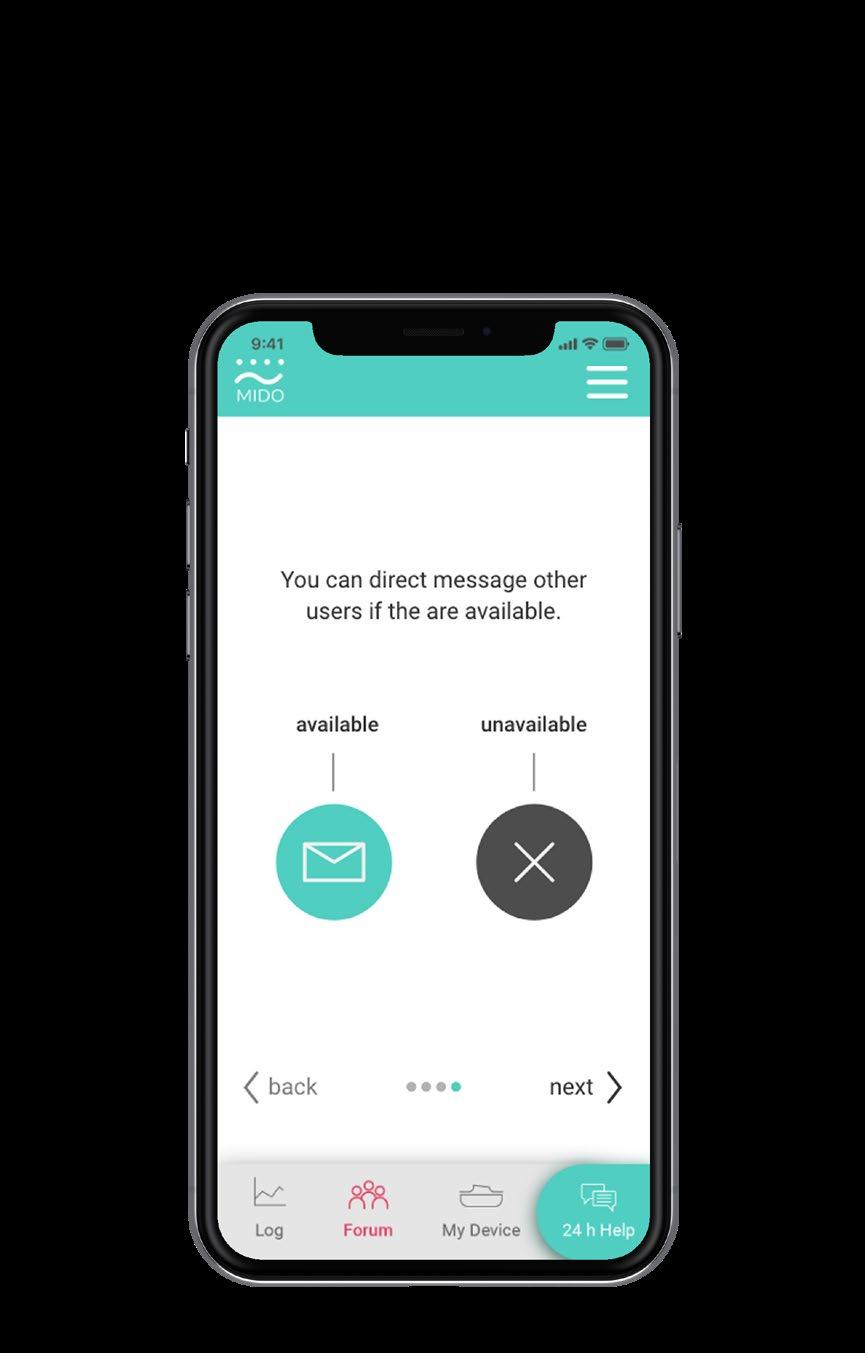
To prevent expert patients from being overstrained, they can choose and indicate in the forum whether they are available or not.

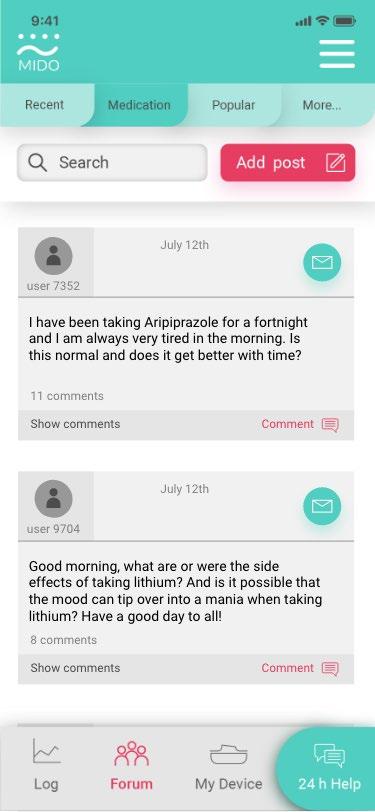


In order to make the forum safe, some channels are moderated. Besides, there is the possibility to block or remove content if people break the rules.





Open the lid of the device and put in dose 1, then close the lid and press „calibrate dose 1“
Calibrate dose 1



Perfect, dose 1 is now callibrated! Add dose



Introduction video Link with crisis pass


To ensure that the information in the crisis pass is up to date, users can link the medication to the crisis pass
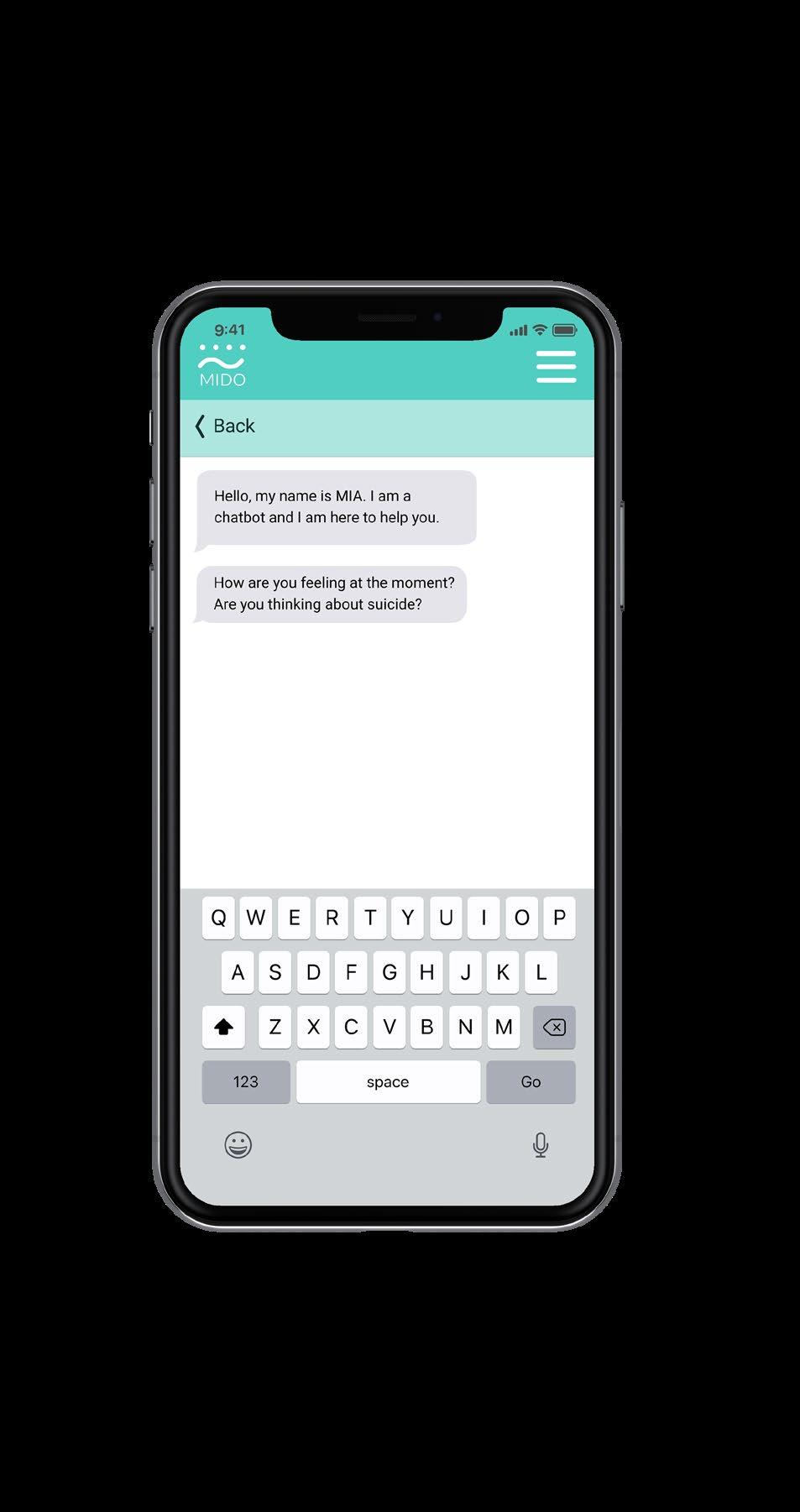
The 24h help section is mainly used to avoid crisis situations or to help in crisis situations. Suicide prevention is the first priority. In general, suicidal thoughts should be addressed openly and directly (Smith et al., n.d.). There are also various warning signals for suicide (American Foundation for Suicide Prevention, n.d.). The chatbot therefore first clarifies whether there is a risk of suicide. If the bot recognises suicidal thoughts, the patient is immediately referred to an expert. If there is no risk of suicide, the chatbot starts with a further anamnesis. With specific questions, the chatbot tries to find out if the patient is manic or depressive and asks if there were any deviations in stimulation behaviour etc. If the bot detects a dangerous situation, the patient will be forwarded to an expert. Simple questions such as which drugs can be combined or what possible side effects are can be answered by the chatbot.


I’m









































I’m





















With the help of AI, the chatbot finds out if a patient is manic or depressive. Deviations are asked for, and the tonality is evaluated.
The size of the device is chosen in such a way that even people with small hands can easily open it with one hand. It is a more elegant alternative to solutions available on the market. These often look very clinical. At first glance, the device does not reveal that it is intended for medication; it is reminiscent of a watch or an alarm clock.

The device reminds people of taking their medication with an alarm signal. Additional the device recognises if the medication is taken. A sphere around the digital display starts illuminating if the medication is not taken. The illumination gets brighter over time.
1

2

3
medication device
Configurable tray
Weight sensors
Space for battery

Display with light sphere
Tag indicating the dose
Concentric contacts to connect with display
Configurable partition walls allow separating different doses from each other.


The medication on-demand in the keyfob is packed in individual zipper bags which contain leaflets with information about dosage and application. The medication is prepared in consultation with the treating psychiatrist.


The agreement of is drawn up in a therapy session together with relatives so that the wishes of both, patients and relatives can be considered and brought in neutrally. The therapist is mainly a mediator and helps to include the needs of both sides.In a previous session, the patient is asked to think about early warning signals. The therapist has already given the patient a questionnaire for this purpose.

The crisis pass contains essential information about the patient. The patients‘ address, emergency contacts to be contacted in case of a crisis, treatment requests, helpful medication in case of crisis and information about which medication is not helpful.
The passport also contains the name of who the provisional power of attorney, care order, patient disposition and the treatment agreement is available from.
The passport contains a QR code is which leads to information about current medication. The QR code is linked to the app. If changes in the medication occur, people are asked in the app whether they want to update the information.


I decided to conduct a survey instead of an interview as it is more anonymous than an interview and people can easily terminate the interview, which is more demanding in a face to face conversation. However, when I analysed the results of the survey, I recognised that the answers were concise and quite negative.
Only Question number six „Are there situations where professional help is available but something prevents you from accessing it?“ helped me. It has shown that there is a Berrier of seeking help and that an appropriate service must take these barriers into account. These other results led to the assumption that participants were in a depressive episode.
The findings taught me that in order to get qualitative output, it must be assured that participants are neither in a depressive nor in a manic episode. Testing if people are in an episode exceeds my competence and the scope of the work. Therefore, I decided to go back to literature research but search for qualitative studies.
What would help you when you are in a depressive mood?
What would help you when you are heading towards a manic episode? Survey questions
1. What role does Bipolar Disorder play in your life?
2. What would help you when you are in a depressive mood?
3. What would help you when you are heading towards a manic episode?
4. Where do you seek help?
5. When do you seek help?
6. Are there situations where professional help is available but something prevents you from accessing it? What are these barriers?
Where do you seek help?
self help group/doctor“
When do you seek help?
nothing silence medikation medikation nowhere never day clinic psychiatrist I am constantly in treatment silence exercise lots of silence and music friendsfamily/therapist when it is no longer possible Better too early than too late when I realize: now I feel bad a woodland walking slope a woodland walking slope
Are there situations where professional help is available but something prevents you from accessing it?
no Hospitalisation shame, fear
I am not sure about my condition and do not want to „disturb“ anybody
The concept includes promotional material that informs about MIDO. The individual components of the toolkit are explained and described. Furthermore, the brochure contains information about cooperating health insurance companies. There is one brochure for patients and one for doctors and therapists. The brochure for patients is in a more straightforward language.


The concentric contacts allow the lid to always be in the correct position. There is enough space in the lid for the display and an additional battery.

You’re almost done!
Only three more steps…
The MIDO forum offers support from expert patients.
Create avatar
Skip back next

This is how you can distinguish expert patients from general users: general users expert patient
Create avatar Skip back next
Expert patients are users that have been managing their bipolar disorder effectively for 2 years or more and have received training to provide support

Skip back next


You can direct message other users if the are available. available unavailable
If people click on the expert patient icon, a pop-up window opens informing the user that this icon indicates expert patients.
Skip back next
Pic 1: Coste, R [online]. [Acessed 08 November 2020]. Available from: http://www.unsplash.com/
Pic 2: Curran, R [online]. [Acessed 08 November 2020]. Available from: http://www.unsplash.com/
Pic 3: Pechy, M [online]. [Acessed 08 November 2020]. Available from: http://www.unsplash.com/
Pic 4: Anon. [online]. [Acessed 08 November 2020]. Available from: http://www.unsplash.com/
Pic 5: Chandrinos, G. [online]. [Acessed 08 November 2020]. Available from: http://www.unsplash.com/
Pic 6: Hume, C. [online]. [Acessed 08 November 2020]. Available from: http://www.unsplash.com/
Pic 7: Eye for Ebony. [online]. [Acessed 08 November 2020]. Available from: http://www.unsplash.com/
Pic 8: Sobczak, P. [online]. [Acessed 08 November 2020]. Available from: http://www.unsplash.com/
Pic 9: Williams, R. [online]. [Acessed 08 November 2020]. Available from: http://www.unsplash.com/
Pic 10: Watt, P. [online]. [Acessed 08 November 2020]. Available from: http://www.unsplash.com/
Pic 11: Sullivan, A. [online]. [Acessed 08 November 2020]. Available from: http://www.unsplash.com/
Pic 12: Curran, R. [online]. [Acessed 08 November 2020]. Available from: http://www.unsplash.com/
American Foundation for Suicide Prevention n.d. Risk factors and warning signs AFSP. [Accessed 11 November 2020]. Available from: https://afsp.org/risk-factors-and-warning-signs.
Baldessarini, R.J. and Tondo, L. 2003. Suicide Risk and Treatments for Patients with Bipolar Disorder. Journal of the American Medical Association. 290(11), pp.1517–1519.
Dunleavy, B.P. 2019. Bipolar Disorder: Symptoms, Types, Causes, Treatment, and More | Everyday Health. online. [Online]. [Accessed 11 June 2020]. Available from: https://www.everydayhealth.com/bipolar-disorder/guide/.
Faedda, G.L., Tondo, L., Baldessarini, R.J., Suppes, T. and Tohe n, M. 1993. Outcome After Rapid vs Gradual Discontinuation of Lithium Treatment in Bipolar Disorders. Archives of General Psychiatry. 50(6), pp.448–455.
Hessel, F. 2008. Burden of Disease of disease(s) In: Encyclopedia of Public Health. Springer Netherlands, pp.94–96.
Interaction Design Foundation 2020. Define and Frame Your Design Challenge by Creating Your Point Of View and Ask “How Might We” Interaction Design Foundation. [Accessed 29 October 2020]. Available from: https://www.interaction-design.org/literature/article/define-and-frame-your-design-challenge-by-creating-your-point-of-view-and-ask-how-might-we.
Lam, D. and Wong, G. 1997. Prodromes, coping strategies, insight and social functioning in bipolar affective disorders. Psychological Medicine. 27(5), pp.1091–1100.
Markowitz, F.E. 1998. The Effects of Stigma on the Psychological Well-Being and Life Satisfaction of Persons with Mental Illness. Journal of Health and Social Behavior. 39(4), pp.335–347.
Merikangas, K.R., Akiskal, H.S., Angst, J., Greenberg, P.E., Hirschfeld, R.M.A., Petukhova, M. and Kessler, R.C. 2007. Lifetime and 12-Month Prevalence of Bipolar Spectrum Disorder in the National Comorbidity Survey Replication. Archives of General Psychiatry. 64(5), p.543.
Meyer, T.D. 1968- and Hautzinger, M. 1950- 2013. Bipolare Störungen kognitiv-verhaltenstherapeutisches Behandlungsmanual; mit Online-Materialien. Weinheim: Beltz. Morgan, V.A., Mitchell, P.B. and Jablensky, A. V. 2005. The epidemiology of bipolar disorder: Sociodemographic, disability and service utilization data from the Australian National Study of Low Prevalence (Psychotic) Disorders. Bipolar Disorders. 7(4), pp.326–337.
National Collaborating Centre for Infectious Diseases n.d. Understanding Summary Measures Used to Estimate the Burden of Disease: All about HALYs, DALYs and QALYs – National Collaborating Centre for Infectious Diseases. [Accessed 24 October 2020]. Available from: https://nccid.ca/publications/understanding-summary-measures-used-to-estimate-the-burden-of-disease/.
National Depressive and Manic-Depressive Association 2001. Living with Bipolar Disorder: How Far Have We Really Come? Constituency Survey [Online]. [Accessed 23 May 2020]. Available from: www.ndmda.org.
Parker, G. 2007. Bipolar disorder. Australian Family Physician. 36(3), pp.240–242.
Proudfoot, J.G., Parker, G.B., Benoit, M., Manicavasagar, V., Smith, M. and Gayed, A. 2009. What happens after diagnosis? Understanding the experiences of patients with newly-diagnosed bipolar disorder. Health Expectations. 12(2), pp.120–129.
Smith, M.M.A., Segal, J.P.D. and Robinson, L. n.d. Suicide Prevention - HelpGuide.org. https://www.helpguide.org.
Stickdorn, M. and Schneider, J. 2019. This Is Service Design Thinking: basics — tools — cases [Online] 8th ed. Amsterdam: BIS Publishers. [Accessed 29 October 2020]. Available from: https:// www.zvab.com/9789063692797/Service-Design-Thinking-basics-tools-906369279X/plp.
Strakowski, S.M. 2014. Bipolar disorder. New York, UNITED STATES: Oxford University Press Inc. Tanis, M. 2012. Online social support groups In: N. Joinson, K. Y. A. McKenna, T. Postmes and U.-D. Reips, eds. Oxford Handbook of Internet Psychology. online: Oxford University Press.
Wang, D., Ma, J., Tan, L., Chen, Y., Zhou, X., Wang, H., Guo, J., Li, X. and Liu, X. 2019. Characteristics of help-seeking behavior among bipolar disorder patients: A study in Hunan, China. Medicine. 98(46), p.e17687.
Wittchen, H.U., Jacobi, F., Rehm, J., Gustavsson, A., Svensson, M., Jönsson, B., Olesen, J., Allgulander, C., Alonso, J., Faravelli, C., Fratiglioni, L., Jennum, P., Lieb, R., Maercker, A., van Os, J., Preisig, M., Salvador-Carulla, L., Simon, R. and Steinhausen, H.-C. 2011. The size and burden of mental disorders and other disorders of the brain in Europe 2010. European Neuropsychopharmacology. 21(9), pp.655–679.
World Health Organization: WHO 2014. WHO Metrics: Disability-Adjusted Life Year (DALY). WHO. www.medizininfo.de n.d. Formen bipolarer Störungen. [Accessed 7 November 2020]. Available from: http://www.medizinfo.de/kopfundseele/bipolar/formen.shtml.