














Tarrant County College Leads the Health Care Talent Pipeline

The Revolution of Mental Health Big Business of Biotech AI in Health Care


s the chancellor of Tarrant County College, I’ve witnessed firsthand the vibrant spirit and resilience of our campus communities. From Fort Worth to Arlington, from Weatherford to Bedford, our students embody a tenacity that makes this region, and specifically this college, truly special.
So while my primary responsibility is to the students, faculty and staff that make TCC great, I am also a county resident, and as such, I’ve noticed the strains on our health care systems over the years. It’s a natural occurrence for a region experiencing a population boom to adjust our services—particularly in health care and wellness. That said, we face two significant challenges: 1) the pressing need for accessible health care and wellness services, and 2) more of them.
I’ve seen our local hospitals stretch to meet the needs of their patients, and I know that TCC can help with staffing and innovation on all elements of health care in our region, from doctors and nurses to dentists and medical recordskeepers. Our health care system must evolve to ensure that everyone has access to the care they deserve, and TCC can help in that regard.
That’s why I am so proud of the various educational opportunities in health care and wellness fields that can be realized at TCC. Our college is stepping up, expanding programs in nursing, social work and public health. We must encourage our students to pursue these vital careers. As a community, we can inspire the next generation of health care workers who will serve the Metroplex for years to come.
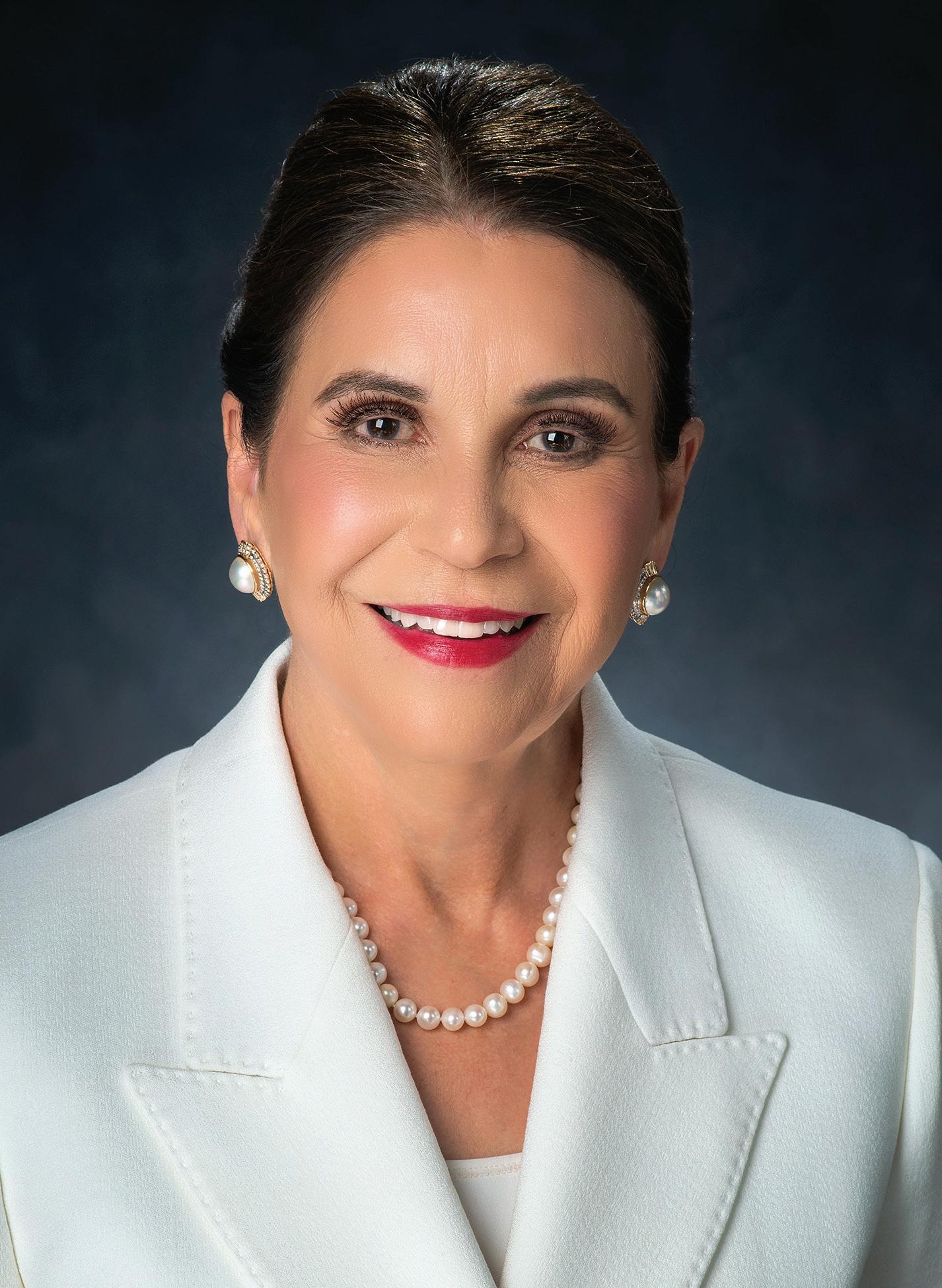
Moreover, we must focus on preventative care and wellness initiatives. I am proud of our campus programs that promote healthy living, from fitness challenges to mental health workshops. These initiatives are essential for building a culture of health on our campus and in our community. We need to empower students and residents alike to take charge of their well-being and make informed choices.
This issue of The Lens highlights Tarrant County College’s commitment to our community’s ability to expand health care and wellness offerings, and our dedication to staffing those careers with our graduates. By supporting those who dedicate their lives to helping others, we can create a healthier, more close-knit community. Together, we can ensure that every resident has access to the care they need, fostering a culture of wellness that uplifts us all.
As the chancellor, I am committed to championing these efforts. Let’s work together to build a brighter, healthier future for Tarrant County.

Elva Concha LeBlanc, PhD chancellor, tarrant county college district









jennifer blalock, edd
When I was young, my grandmother received a pacemaker, and I can vividly recall the rhythmic tick of her heartbeat, steady as a clock. I would often lay my head on her chest and listen to the powerful reminder that she was the heartbeat of our family, a constant and reassuring presence. Although she is no longer with us, her legacy lives on, echoing in the values and love she instilled in each of us.
In this issue, “Deep in the Heart of Health Care,” we take a closer look at health care in Tarrant County and beyond, exploring the essential elements that keep our communities healthy, resilient and thriving.
Much like my grandmother’s heartbeat, comprehensive wellness is at the core of any community’s vitality. It takes more than just access to health care; it requires collaboration, innovation and support to create an environment where everyone has the opportunity to thrive. And, like my grandmother’s lasting impact on our family, the work we do today in health care and community development will echo through future generations, creating a foundation of wellness and opportunity.
In Tarrant County, we’re seeing partnerships that embody this spirit of comprehensive wellness. One of the stories in this issue highlights a collaboration among Cook Children’s, JPS, Workforce Solutions of Tarrant County and Tarrant County College (page 30). Together, we are transforming a health desert by bringing much-

needed jobs, health care services and professional development to underserved areas. This initiative reminds us that a community’s heart beats strongest when every part is supported and cared for.
We also explore the growing role of biotechnology (page 14), the importance of mental health (page 44) and the transformative potential of AI and robotics in health care (page 22). And as we face pressing challenges, such as nursing (page 10) and health care workforce shortages, we’re reminded that solutions are within reach, grounded in innovation and united by purpose.
In every story, you’ll find echoes of that steady heartbeat, an unwavering dedication to the health of our people, our families and our future. It’s the heart of it all, and it’s a legacy we’re honored to build upon for generations to come.

Jacquetta Dantzler editor-in-chief,

EDITOR-IN-CHIEF
Jacquetta Dantzler
Interim Executive Vice President
SUBJECT
Drew Jackson
BUSINESS
Desmond Bibbs
BUSINESS DEVELOPMENT
Alex Cowen

CHANCELLOR
Elva LeBlanc, PhD
BOARD
Teresa Ayala, President Kenneth Barr, Vice President Jeanne Deakyne, Secretary
Leonard Hornsby, Assistant Secretary Shannon Wood Laura Forkner Pritchett
Gwendolyn Morrison
EDITORIAL ADVISOR Reginald Gates
PRESIDENT/CEO Kimberly Ferrante
GROUP
Adam Pitluk, PhD
CREATIVE
David Halloran
Becky Williams

jennifer blalock, edd
Jennifer has spent over two decades leading teams in postsecondary education and municipal government. As the CEO of InJenuity Solutions, Jennifer develops, facilitates and evaluates workforce, economic and organizational development programs.

greg fulton
Greg is a career writer whose work has appeared in daily and weekly newspapers, CNN, salon.com and many other publications. He is the former South Bureau Chief of TIME magazine and a contributor to American Way magazine.

orr
Based in Pittsburgh, Pennsylvania, Vanessa has been a freelance writer and editor for more than 25 years. Her work has appeared in hundreds of regional and national publications including the Pittsburgh Post-Gazette and Alaska Business Monthly.

heide brandes
Based in Oklahoma City, Heide is an award-winning journalist whose work has appeared in Forbes, The Wall Street Journal, The New York Times and The Washington Post, among others. She is also a historic reenactor and an avid hiker.

tyler hicks
Tyler is a writer and journalist from Austin, Texas. His work has appeared in The New York Times, Texas Monthly and many other newspapers, magazines and websites across the country.

adam pitluk, phd
Adam is an award-winning journalist and the author of Standing Eight and Damned to Eternity. He was a reporter for TIME and People magazines, and is the former editor-inchief of American Way. He is the publisher of The Lens

tom delamater
Tom is an Ohio-based writer and editor, and longtime communications consultant to corporations, nonprofit organizations and educational institutions. He is the former chief communications officer at Collin College.

terri marshall
Terri is a copy writer and an award-winning writer. She is the managing editor for World Footprints. Her publication credits include AARP, Island Soul, Girl Camper Magazine, A Girls Guide to Cars, Alaska Business Monthly, Alaska Contractor and more.

bennett root, esq Pasadena, California-based Bennett Root is a business advisor, mediator, arbitrator, attorney and author. He specializes in building innovative programs for SMBs and systems to reduce workplace conflict and build profits.

jacquetta dantzler
Jacquetta has devoted the last 18 years of her career to partnering with entrepreneurs and small business owners. Additionally, she is a published author with a diverse body of work that ranges from poetry to textbooks.

james ndone, phd James is an organizational and leadership communications scholar who specializes in crisis communication. Originally from Kenya, he has worked domestically and abroad in both education and industry. He has a PhD from the University of Missouri School of Journalism.

sally verrando Sally is an award-winning journalist in DFW. She has been published by The Dallas Morning News, KERA and other Texas media outlets. A seventhgeneration Texan, she loves travel, animals and bluebonnets.
Advertising in The Lens magazine doesn’t just align your organization with high-quality content in an award-winning publication. Being part of both the print and digital editions of The Lens also puts your business in front of thousands of readers, including Tarrant County executives, entrepreneurs and economic development professionals. Secure your spot today to reach the decision-makers you want as clients.











for advertising opportunities, please email our publisher at info@midwestluxurypublishing.com we look forward to working with you!
CHIEF NURSING OFFICER
• Career Outlook: Will grow by 28% from 2022 to 2032
• Where to work: hospitals or medical institutions. However, many also work in nursing homes or in an overseeing position in large health care systems.
PHYSICIAN ASSISTANT
• Career Outlook: Will grow by 27% from 2022 to 2032
• Where can you work: PAs can work in any setting that physicians do, including doctor’s offices, hospitals, surgery centers, outpatient clinics, nursing homes and other health care environments.
NURSE PRACTITIONER
• Career Outlook: Will grow by 45% from 2022 to 2032
• Where to work: hospital settings, including critical care areas, emergency rooms, in-patient and outpatient surgery and other specialty floor units. NPs also work in community clinics, nursing homes, health care centers and physician offices. In states with full practice authority for nurse practitioners, they can even run their own practices.
MEDICAL OR HEALTH SERVICES MANAGER
• Career Outlook: Will grow by 28% from 2022 to 2032
• Where to work: Medical and health services managers work in almost all hospital settings, group physician offices, nursing homes and other health facilities.
CLINICAL INFORMATICS MANAGER
• Career Outlook: Will grow by 28% from 2022 to 2032
• Where to work: large medical systems, hospitals and other medical clinics
VETERINARIAN
• Career Outlook: Will grow by 20% from 2022 to 2032
• Where to work: veterinary clinics, animal hospitals
SPEECH-LANGUAGE PATHOLOGIST
• Career Outlook: Will grow by 19% from 2022 to 2032
• Where to work: hospital setting, outpatient centers and rehabilitation facilities
Veterinarian: $103,260
Physical Therapist: $97,720 17. Occupational Therapist: $93,180 18. Radiation Therapist: $89,530 19. Speech Language Pathologist: $84,140 20. Dental Hygienist: $81,400












Area colleges are expanding partnerships and curricula to build a modern nursing workforce. by greg fulton
There is consensus among nursing program leaders in the Dallas/Fort Worth area that the COVID-19 pandemic did not create a nursing shortage, but it certainly exacerbated the critical need for bedside RNs and staffing in rural areas and hospitals.
But that emphasis for renewal alone is not enough, they say. To approach an ongoing shortage among a multitude of nursing roles means a comprehensive approach. And it seems as no coincidence that at Tarrant County College, the University of North Texas and Tarleton State University, new nursing program deans have all been announced since mid-2023.
At Tarrant County College, Divisional Dean of Nursing Nikolaos Moraros, who took over in the summer of 2023, lists more than a half dozen coordinated strategies, including the ability to expand enrollment, expand and retain faculty, streamline the programs to accelerate completion, partner with other schools and health systems, diversify the workforce, retain nurses and leverage technology.
“Combining these strategies with partnerships can help address the nursing shortage at educational and practical levels,” Moraros says.
The National Institutes of Health agrees, noting in 2023 that ongoing nursing shortages are attributed to the need for more educators, turnover rates and inequitable workforce distribution. And Moraros cites not just local, but also national strategies. The American Association of Colleges of Nursing (AACN), for example, emphasizes the impact of strategic partnerships.
Tarrant County College is embracing this approach. Traditionally offering an Associate of Applied Science (AAS) in Nursing and a
Licensed Vocational Nursing (LVN) program, TCC also offers dual enrollment toward a concurrent Bachelor of Science in Nursing with Arizona State, Grand Canyon, Tarleton State, Texas Tech, the University of Texas at Arlington and the University of North Texas. TCC also offers existing LVNs a fast-track from 24 to 15 months toward its AAS in Nursing.
And TCC doesn’t stop there. In the Dallas/Fort Worth area, the Medical City Healthcare system is well known for its 21 hospitals, 16 ambulatory surgery centers and more than 5,000 physicians. All told, the system employs more than 15,000 people.
In the Texas Two-Step Program, Medical City employees receive financial aid from the health system to enroll at Tarrant County College and other area programs. This way, says Moraros, students can get real-world clinical experience and an education to “strengthen relationships between educational institutions and health care providers, creating a pipeline for future employment and addressing staffing shortages in these critical health care settings.”
The AACN reports good news overall, stating that in 2023, enrollment in entry-level baccalaureate programs increased compared to 2022.
Until this past summer, the University of North Texas Health Science Center did not have a nursing program. Now it does, and this fall it welcomes its first students into its Bachelor of Science in Nursing and Master of Science in Nursing in Psychiatric Mental Health nurse practitioner programs.
The new College of Nursing is being led by Cindy Weston, who officially began her tenure July 1, 2024, after approvals by the Board of Regents and the Texas Board of Nursing.

“Combining
these strategies with partnerships can help address the nursing shortage at educational and practical levels.”
— Nikolaos Moraros DIVISIONAL DEAN OF NURSING, TCC

United States Chamber of Commerce (January 2024 report)
There are 193,000 annual projected job openings for RNs through 2032.
The average U.S. nurse to patient ratio: 9 per 1,000, but Texas (and Utah and Georgia) report 7 RNs per 1,000.
Nurse practitioner is the top “in-demand” health care job of the next decade with 52% growth projection. Median salary: $111,608.
The COVID impact: From 2020 through 2021, 100,000 RNs left the workforce, the largest drop in 40 years, citing exhaustion and burnout.
National League for Nursing 2022-2023 survey: 86% of responding nursing schools are actively seeking to hire new faculty.
American Association of Colleges of Nursing (May 2024 report)
Advanced Practice Registered Nurse (APRN) workforce needs are expected to increase by 39% through 2032.
The number of “baccalaureate-prepared” nurses should increase by 80% to meet workforce and patient safety needs.
The COVID impact: 66% of acute care nurses considered leaving the workforce based on experiences during the pandemic.

Her vision for the future of the College of Nursing is comprehensive and geared toward the needs of the metroplex marketplace, which she describes as calling for a mix of entrepreneurship and innovation. “We are listening, and we are collaborating on what are the needs specific to nursing to secure new pathways,” she says. “We need mental health care providers in our state; we have one of the lowest rates per capita.” Overall, the goal is to add more nursing faculty and curricula. “The mission of the health science center is solutions for healthier communities.”
Weston agrees with her peers that should start at the front lines with RNs and advanced practice RNs. “North Texas alone is about seven thousand nurses short there and anticipated to grow since the population is growing.”
She also sees a need for community-based nursing curricula and points out the areas of need besides hospitals, such as home-based care, skilled nursing facilities, long-term care and outpatient clinics.
“We are four years out of the pandemic, with nurses leaving the workforce as a result of the stressors and retirement, and now there’s a big shift of the growth of nursing in community-based settings,” Weston says. “All of this requires programs offering scalable and stackable health care credentials.”
At Tarleton State University’s School of Nursing, Dean J. Michael Leger officially began leading the program on July 1, 2024.
As a member of the American Association of the Colleges of Nursing’s policy task force, he’s considering the national statistics in the context of the needs of the metroplex. “We have to be careful how we use the nursing shortage terminology,” he says.
“We have to dissect and dig deeper.”
For example, nurses that left the bedside front lines during or immediately after COVID need to be retained in the overall workforce. “They may not have the education or experience for case management or patient safety management roles,” Leger says. “Those are areas we are going to focus on. COVID just shined a light on the issues already at hand.”
Tarleton currently offers an undergraduate Bachelor of Science in Nursing (BSN), along with a licensed vocational nurse-to-BSN and RN-to-BSN tracks. The nursing school also offers a graduate Master of Science in Nursing.
From there, Leger plans to launch a master’s program to fill the educational needs around case management and patient safety and a doctorate of nursing to create more faculty. “We are turning people away due to faculty and we need creative ways to add more teachers,” he says.
Tarleton also partners with Medical City on clinical programs within its walls to place students in clinical rounds. He also agrees with his peers that rural health care is always going to be a focus. Along with bedside care, “rural hospitals and clinics need nurses with higher degrees of education.”
At TCC, Moraros reminds everyone that the next pandemic could come, and preperation is crucial. He believes increased crisis preparedness and financial aid could attract more people to nursing, which generally pays well, from $90,000 to six figures for most nursing roles. We all remember the indelible images of nurses on the front lines of COVID.
“Nursing is perceived as tough, with high educational costs. We need to promote nursing as a rewarding career.”
Tarrant County is building for the future, no longer limiting its economic base to the cattle, oil and agriculture industries that once made up the local economy. Indeed, the Tarrant County of the 21st century boasts an array of highvalue business concerns in health care, biotechnology, aerospace, transportation and manufacturing, including manufacturing of pharmaceuticals.
This dynamic and varied blend of industrial concerns creates a strong economic foundation for the region. But the lifeblood of these high-tech, high-value businesses depends on the county’s ability to develop and maintain a highly skilled workforce trained in the intricacies of each business. And that is the challenge for Tarrant County’s governmental and educational institutions: Can they attract and train enough skilled workers to support the growing demands of the county’s emerging high-tech businesses?
High-tech businesses clearly bring value to the communities in which they are located. Consider just two obvious indicators: a community’s growing tax base and the creation of high-paying jobs for residents at a time when much of our country’s job creation delivers low-pay, minimum-wage-level jobs. Then consider, as one very successful example, the recent report released by AllianceTexas regarding the Hillwood 27,000-acre master-planned, mixed-use community in north Fort Worth.
Insight Research reported that AllianceTexas has generated roughly $111.5 billion in regional economic impact, including more than $3.4 billion in total taxes paid to local public entities during the past three decades.
“AllianceTexas is an absolute powerhouse in Fort Worth,” says Mayor Mattie Parker in a statement. “By every metric—job creation, economic impact, property tax contribution, opportunities for innovation and more—AllianceTexas proves itself year after year to be incredibly impactful.” This public-private partnership touches both Tarrant and Denton counties, having contributed more than $625 million in property taxes to Tarrant County alone.
But success stories like this do not just happen. They start with a vision, like that of late former Fort Worth Mayor Bob Bolen, who advocated for this project more than 30 years ago. And they start with a regional ability to close the inevitable “skills gap” that develops when new, high-tech businesses move into
an area. As noted in a report by McKinsey & Company focusing on the required elements of successful workforce development programs, the skills gap confronting employers takes different forms. It is characterized both by young people looking for that first meaningful job opportunity and by mid-career employees whose jobs have been outsourced or automated and who must relearn and adapt their skills to the job opportunities that will become available.
Both types of workers must be addressed. Programs that effectively address the skills gaps, McKinsey notes, are most efficient when leading employers come together to carefully and clearly define the needs that companies will be facing, when ROI goals are quantified and periodically assessed, when demand-driven training methods, such as “boot camps,” are incorporated into the training process, when learners can be prepared before they start of their respective new career paths and where there can be effective centralized monitoring and control of workforce development programs.
When these five components characterize the workforce development effort, the magic, like AllianceTexas, can happen, buoying an entire region.
When engineered thoughtfully, as with Mayor Bolen’s vision, the interaction of government, educational institutions and high-tech industries produces a virtuous cycle that supports and expands on successes like AllianceTexas. “A virtuous cycle is our [principal system or] method by which we engender transformation. It contains four phases: Perception, Formation, Transmission and Responsibility.” According to Renee Parker, Industry Services Unit Director for Workforce Solutions for Tarrant County, these phases are exactly what her organization addresses. And a virtuous cycle of training, employment, tax base generation and enhanced community strength appears to be exactly what is developing in Tarrant County.
The burgeoning health care and biotechnology sectors in Tarrant County well illustrate some of the specific institutional developments and alliances that can maintain and enhance the training, employment and community growth cycle now emerging.

The burgeoning health care and biotechnology sectors in Tarrant County well illustrate some of the specific institutional developments and alliances that can maintain and enhance the training, employment and community growth cycle now emerging.



Crystal Brown CEO, CIRCANOVA, INC.
The journey for biotech entrepreneurs is challenging in that facilities with sophisticated equipment and employees with special skills are often the difference between success and failure.
Consider the journey of Crystal Brown, CEO of CircNova, Inc., a developer of circular RNA therapeutics using automated drug discovery, gene therapy, and biotechnology to address “undruggable” diseases, such as triplenegative breast cancer. The company produces deep science results using generative artificial intelligence in its proprietary NovaEngine to create “RNA-folding and active structure prediction, which enables revolutionary efficiencies in the effective development of therapeutic candidates.”
All this from a founder with a Bachelor of Arts degree from the University of Michigan and an Executive MBA degree from Michigan State, illustrating just how widely backgrounds may vary for successful biotech entrepreneurs.
Brown actually started her career as an executive in Detroit’s traditional automotive industry, working for Chrysler for the better part of a decade. Eventually, she was teased away, moonlighting for a friend who needed help understanding industry finance. That company went public.
From this experience, Brown learned she could master very different work environments by understanding essential financial parameters, line item by line item. She then decided to start her first entrepreneurial venture, Great Lakes Biologics. This effort was ultimately unsuccessful, but it provided her second critical lesson for entrepreneurs: “Being a successful startup founder requires confidence, determination and drive, despite adversities” in Brown’s diplomatic phrasing. Or more prosaically, when you get thrown, pick yourself up, dust yourself off and get right back on that pony.
Brown’s success at CircNova also results from careful, sustained focus on the main objective, a lesson she learned in the automotive industry, and careful recruitment of specially trained talent. Other keys include line-byline financial control, sustained focus, selection of specialized talent and, most of all, says Brown, “determination and drive despite adversity.”
Who would be surprised to learn that Brown is well on her way to her second IPO?
As noted by Prototype: IT, “The health care and life sciences industry in Fort Worth employs over 55,000 people, with major providers like JPS Health Network and Cook Children’s Medical Center leading the way.” These, and a number of other major health care employers in North Texas, will continue to demand new employees with new skill sets to meet their consumer demand.
In a detailed report on skills now needed in health care, Pearson Labor Market Data identifies these five skill sets as critical: conducting medical procedures, administering vaccinations, maintaining sanitation standards, monitoring vital signs and providing transportation services. Jobs using these skills include nurses, home health aides, senior medical secretaries, health services team leaders and information clerks.
Additionally, Pearson Data notes the need for “digital transformation enablers” such as distribution managers, workforce planning specialists, help desk managers and risk management specialists, each capable, among other things, of using predictive analytics to manage their work responsibilities.
It would be hard to imagine a more compelling brief for workforce development, continuing skills training and even re-training.
And this is all before considering the needs for the entrepreneurial community, a key driver of the long-term success and sustainability of cutting-edge health care facilities.
Entrepreneurial development is a springboard to high-value job and enterprise creation, as can be seen from the continuing successes emerging from Silicon Valley. In Tarrant County, this kind of growth is fostered by programs such as the University of North Texas Health Science Center’s physical health accelerator program, which showcases the city’s commitment to staying ahead of the curve in health care technology. An accelerator is just that—it accelerates business growth for entrepreneurs. In
so doing, it accelerates the demand for new skills and specially trained employees.
So the need for new training programs and skillful workforce development is clear and convincing. What is developing in Tarrant County to meet this need, to keep feeding the virtuous cycle that drives value for the region and its residents? Of the several encouraging developments in Tarrant County, two stand out in terms of building toward the future.
The first is the strength of the local governmental and publicprivate institutions supporting workforce development. As Renee Parker points out, TCC’s Corporate Solutions provides both inperson and virtual classes to people in the workforce looking to upgrade their skills. And, Parker notes, much of this work can be funded through grant money available from the Texas Workforce Commission.
Additionally, BioNTX and the DFW Hospital Council have collaborated to launch the Biotechnology and Healthcare Industry Alliance of North Texas, abbreviated BHIANT. BHIANT is a consortium of business leaders and industry executives dedicated to fostering growth in North Texas by connecting regional enterprise with local communities, resources and opportunities. The alliance helps shape the future for the biotech and health care industries by fostering collaboration, empowering innovation, developing talent and expanding access to transformative resources. This is just the type of alliance McKinsey stated was critical to success.
The second development supporting the biotech and health care ecosystem comes from private concerns such as Panthera Solutions, an entity offering efficient R&D and validation services, ensuring rapid development and accelerated commercialization for innovators and companies,” in the view of Dr. Aaron BenComo, director of business development for BioNTX.

And, according to Jason Mastoris, Panthera offers a variety of business solutions for pharmaceutical and biotech entrepreneurs, including clean rooms, stability programs and incubation, and filling and processing solutions, all of which can make the treacherous journey of the biotech pioneer more easily traversed.
Workforce training and development are key requirements for the fiscal health of high-tech businesses and also for regional economic stability. Tarrant County is blessed to have public and private programs supporting this requirement. With visionary leadership, these institutions, and those that follow in their footsteps, are well positioned to keep the biotechnology and health care industries moving forward.
From patient care to quality control, opportunities abound for pharmacists. by vanessa orr
Pharmacists are in great demand across the nation, and the need for well-trained workers is only expected to grow as retail facilities, clinics, hospitals, biotechnology and life sciences companies and more try to fill an increasing number of positions. According to the Pharmacy Workforce Center, in the first quarter of 2024, there were almost 19,000 job postings for pharmacists across the country and 40,000 open positions for pharmacy techs. While the majority of jobs were in retail, there were also many positions open for clinical and hospital pharmacists and other pharmacist occupations as well as pharmacy director positions.
As a result, recent pharmacy graduates are finding a wealth of opportunities, as well as salaries and sign-on bonuses that make it worth the educational investment. In May 2023, the Bureau of Labor Statistics (BLS) reported that pharmacy techs made a median annual wage of $40,300, with pharmacists earning a median salary of $130,080. In some markets, companies are even offering signing bonuses of $50,000 or more.
While some pharmacists start with a pharmacy technician certification and work their way up, others may choose to go directly to pharmacy school to earn their degree. It all depends on the individual, as well as the path that they choose to take in the pharmaceutical field.
Maureen Cole, PharmD, an assistant pharmacy manager for Publix Super Markets, applied directly to pharmacy school and earned her degree from LECOM School of Pharmacy in Erie, Pennsylvania, by taking a three-year, yearround program. After graduating, she worked for Walgreens in Myrtle Beach, South Carolina, as a floating pharmacist, and then became a staff pharmacist.
“After doing some job shadowing, I just jumped right in, thinking that if I didn’t like it, I could always do something different,” she says. “I didn’t do what a lot of people do, which is to go to school first to be a pharmacy tech just to get some experience under my belt.”
Cole was offered the chance to step into a management role, which she did for three years before deciding to start a family. She then took a position with Target, which enabled her to work
fewer hours per week, and spent 10 years there before moving to the Publix Super Markets chain.
“Working in a grocery store chain has been absolutely wonderful; it has a different sort of vibe than working for a corporate giant, which is a little more stressful since the pharmacy is its primary source of income,” Cole says. “I love helping people and being so accessible; they can just walk up and talk to me instantly. I like that they are comfortable and confident coming to ask for recommendations.”
Depending on a pharmacist’s job and place of employment, responsibilities can vary greatly. Not only are pharmacists responsible for filling prescriptions and making sure that customers receive the right medications, but in some places, they also provide point of care/on-site testing, such as giving COVID-19 or flu shots to the general public. On the retail side, pharmacists also work with insurance companies to deal with formulary changes and costs for patients, as well as with doctors’ offices to bridge issues such as duplicate therapies or inappropriate dosages.
While pharmacists are often pictured as the white-coated professionals behind the counter, there are many other roles that they can have. In the pharmaceutical manufacturing industry, for example, pharmacy jobs can include general warehousing, maintenance and metrology, validation, quality assurance, quality control and prevention operators, with different levels of expertise required in each area.
The BLS reported that pharmacy techs made a median annual wage of $40,300, with pharmacists earning a median salary of $130,080. In some markets, companies are even offering signing bonuses of $50,000 or more.


“It’s very common for PharmD’s to join the pharmaceutical manufacturing industry as they can take analytics roles, quality assurance roles, as well as many other positions that leverage their experience from their degrees,” explains Jason Mastoris, partner and cofounder of Panthera BioSolutions. “However, if they really like dealing directly with customers, retail pharmacy might be the best path. While the patient is ultimately our customer, we don’t deal with them directly very often.”
While Panthera works as a service provider for pharmaceutical companies looking to grow, scale products or provide packaging and distribution of products for clinical trials, it also sees its mission as helping with workforce development initiatives to encourage people to come into and stay in the pharmacy industry.
“We set up a Fundamentals to Pharma training program at our facility for that exact reason; we wanted to show people the various career paths that are out there in pharmaceutical manufacturing and the life sciences industry,” says Hardik Patel, partner and cofounder of Panthera BioSolutions. “If they want, they can come in at the entry level and work toward executive leadership as their ultimate goal, depending on what area they pursue.”
There are numerous advantages for those working in the pharmaceutical manufacturing industry; most of the work is done within business hours (as opposed to midnight retail shifts), and there are also many options to not only move up in a position, but also to move horizontally into another aspect of the job. Some positions do not require a four-year college degree to start, though it may help with advancement.
Compensation is also very healthy on this side of the industry, with senior roles theoretically reaching $300,000 to $400,000 per year, as well as bonuses, stock incentives and more. An added advantage, especially for those who want to stay in Texas, is that many pharmaceutical biotech companies are located in the Dallas/Fort Worth area.
“The rapid population growth in this area is already putting a strain on the infrastructure, and we need more pharmacists,
doctors and nurses and other health care professionals,” Mastoris says. “There are a lot of roles emerging in our industry with several very large pharma campuses being built or already built; many jobs are coming as a result.”
For those who want to work their way into the field, starting with a pharmacy tech certificate can help them get their foot in the door. Tarrant County College’s (TCC) Pharm Tech program requires an applicant to have a high school diploma or equivalency degree and to complete the Texas Success Initiative test, though that requirement may be waived if a person has earned previous college credit.
The program, which is offered two times per year, includes six courses offered in the evenings, both in person and online. Courses include Introduction to Pharmacy Technician, Pharmacy Law, Pharmacotherapy & Disease, Drug Classification, Pharmacy Mathematics and Pharmacy Technician Certification Review.
According to Marisa L. Galaviz, coordinator of Health Professions Workforce Education, while studying, students may also be able to earn a “technician trainee” certification, which allows them to work in a pharmacy environment while in school. Not only does this provide on-the-job training, but may also make it easier to find a permanent position after graduation.
TCC is currently in the process of creating a stackable program that will advance from the Pharmacy Tech certificate to an associate’s degree program to prepare students who want to go on to earn a pharmacy degree.
“Typically, students need to complete a 12-week program or a two-year associates’ degree program before they can work in the field,” says Jacqueline Bennett, assistant dean of health sciences. “We are currently working on the curriculum, but also need to have a lab developed for sterile compounding, so it may take about two years to have the full program established. Students who then want to progress to pharmacy school or move into management can move onto an associate’s degree.”


Artificial Intelligence and enhanced technology are blazing a trail through all medical industries. by jennifer blalock, edd

While some industries are embracing the integration of technology into their workspace with caution, artificial intelligence and its enhanced technologies offer a welcome opportunity for improving global health, quality of life and innovation to medical professionals, patients and the entire health care community. Today’s modern medical offices and health care facilities are slowly morphing into the futuristic realm of possibility and promise, leveraging algorithms and machine learning to revolutionize patient diagnostics, offering unparalleled accuracy and early detection.
The allure of seeing these enhanced technologies, including artificial intelligence and robotics, infused into daily medical practices lies in the inherent potential to elevate health sciences and services by significantly increasing rate of recovery and effectiveness while decreasing pain and patient downtime. Patients receiving care in every medical specialization are eager to support the continued introduction of these new technologies with optimistic curiosity and, most importantly, hope.
Introducing state-of-the-art health care equipment and advanced technical capabilities demands an urgent, real-time response for hands-on training, equipping the current and future workforce in the health care field with the skills and training necessary to fully implement the benefits of these exciting new tools. From finger scanning patient identification to 3D body scans, all the new tools create a learning curve that must be balanced by those already providing real-time patient care and the surging demand for new health care professionals already in training and professional preparation programs.
Coupled with the high growth and high demand for medical services in regions like North Texas, with Fort Worth, Arlington and all of Tarrant County documenting rapid population growth, it’s also a challenge for health care providers and educational institutions to stay on pace with the explosion of innovation in the critically important health care field.
In a recent Fort Worth Report article, David Moreno highlighted two of the area’s largest health care providers that have already incorporated AI into their daily patient care and services:
· Methodist Mansfield Medical Center is using artificial intelligence in its new neuro critical care unit. Emmanuel Rivas Valenzuela of KERA revealed the hospital is using “RAPID-AI technology by running CT scans through the software programmed to flag potential abnormalities. Once the AI finds an abnormality, the medical team is then notified. A neuro-radiologist then determines if there is a need for further medical treatment,” as Valenzuela noted in a published article in the Arlington Report
· JPS Health Network was recognized for its use of artificial intelligence in securing hospital safety. Zero Eyes, a software recognition scanner that the hospital implemented, identifies guns on the hospital grounds and connects with local law enforcement.
Managing the technological advances in the medical and health care field is a huge undertaking, and creating effective, accessible training programs to match the speed is even more complex. Julian L. Alssid, transformative workforce strategist and a partner in J. Alssid Associates, advises C-suite leaders who seek to optimize their organizations as workforce entities for transformational impact and is the host of “Workforces,” a podcast focused on preparing the world for the complex demands of a highly skilled workforce in fields like medicine and health care.
He, along with co-host Kaitlin LeMoine, advocates for an office dedicated to national talent development. Their recommended plan would incorporate customized career development plans and training in sectors they believe will “define the next century,” including artificial intelligence and quantum computing, both fields with direct implications on how medicine and health care are practiced. Further, they identify an immediate need to “leverage emerging technologies to connect workers with upto-date jobs and related training.” Nowhere is the need more imperative than in the medical sector.

Patients receiving care in every medical specialization are eager to support the continued introduction of these new technologies with optimistic curiosity and, most importantly, hope.
Just how influential is artificial intelligence in shaping the preparatory training programs and continued professional research and development of health care professionals? According to Dr. Ashraf Khan, a health care innovation and quality assurance expert, AI’s impact will be far reaching and transforming.
“I strongly believe AI is set to revolutionize patient care and delivery in the health care industry,” he says. “Our journey to understanding AI implementation in health care is ongoing, with many top educational institutions now offering certification programs tailored to health care professionals.”
Khan and others, like Dr. James Merlino, executive vice president and chief innovation officer of The Joint Commission, as well as chief clinical transformation officer for the Cleveland Clinic, are also preparing the health care sector to manage the impact of artificial intelligence. The Joint Commission, an independent, not-for-profit organization, is the nation’s recognized body for establishing standards of practice in health care innovation and accreditation. Merlino and others recently convened in Washington, D.C., to discuss responsible use of AI in health care.
“Artificial intelligence is one of the most important topics in health care today because it holds the incredible promise of disruptive innovation to improve health care for all,” Merlino says.
Higher education institutions and administrators are already recognizing the importance of weaving artificial intelligence and technological advancements into health care programming curriculum and practicums.
Dr. S. Sean Madison, president of the Trinity River Campus of Tarrant County College District, leads a team of innovators, campus executives and committed educators who manage nearly 70 health care, medical and STEM focused degrees, credentials and certificates. With over two decades of leading post-secondary institutions in both Florida and Texas, Madison understands the urgency to align health care and medical professional preparation programs with realworld technologies and patient care equipment.
“At Trinity River, we have designed signature educational and career paths for students in areas such as health care and sign language—and in a number of our general education programs— that will support careers and further study in science, technology, engineering and math (STEM) disciplines,” Madison says. “We are always looking for ways to provide educational opportunities for students in high-demand careers as well as those with emerging technologies.”
Madison’s extensive experience in building
and sustaining highly effective professional medical training programs is highly respected and resulted in an appointment to the American Association of Community College’s (AACC) Commission on Research, Technology and Emerging Trends. Madison and his faculty work collectively with area hospitals and medical experts to ensure that the classroom experience for students and faculty at both the East and West campuses of Trinity River mirror the equipment and practices of an authentic medical care facility. While this requires considerable financial investments in cutting-edge and newly released technologies, the return is invaluable. One such investment Madison and his team implemented that touches nearly every health care program offered at the campus, from its highly competitive Physical Therapy Assistant Program to Nursing, is the Anatomage Table.
While many of those who are health care veterans fondly recall their handmade note cards used for hours of memorization of the over 200 bones in the human adult body, the cutting edge Anatomage Table is a realistic and hands-on teaching tool. The interactive learning platform offers the most advanced real-human-based medical education system. This state-ofthe-art platform offers digitized human cadavers and superior medical learning tools, transforming medical education and training. According to Central USA Regional Sales Manager Jon Perry, by incorporating the Anatomage Table, institutions like


Students at Tarrant County College’s Trinity River Campus who are pursuing a variety of health care and medical degrees and credentials are given access to learn and train using top-of-the-line medical equipment, including the Anatomage Table.
According to Jon Perry, regional sales manager for the product, “Anatomage’s digitized cadavers have been the most reliable resources for learning anatomy and physiology. The Anatomage Table features real cadaveric content that helps students accurately visualize anatomy. Anatomage’s technology simulates realtime physiology in the digitized cadavers. Students can explore the physical behaviors of real tissues during the physiological activities.”
In addition to the tried-and-true methodologies of anatomy coloring books, worksheets and notecards, students can experience the human form in real time, with stunning realism and anatomical accuracy. “Anatomage Bodies offer a highly interactive experience, allowing students to manipulate anatomy in various angles,” Perry says. “This hands-on approach helps them develop a strong spatial understanding of the relationships between structures.”
Anatomage, established in 2004, prides itself on pushing technology and medical visualization to help train health care professionals today for success tomorrow. Perry, who applauds Tarrant County College’s Trinity River Campus for being among a small number of community colleges to offer the Anatomage Table, explains that the company is continuing to develop and refine its technologies, achieving beyond industry standards in volumetric visualization, 3D image segmentation and functional simulation. He adds: “The best is yet to come.”
Tarrant County College can enhance learning outcomes, lower laboratory costs and establish their technological leadership (see “Anatomy 101” sidebar).
Another technological enhancement is the new gamma camera integrated into Tarrant County College’s well-known nuclear medicine program. At 15 feet long and seven feet high, weighing more than 7,000 pounds and costing a quarter-million dollars, this camera is made to be noticed, and at that size and cost, it’s a regular highlight at campus and program open houses and showcases.
The Siemens Symbia Evo gamma camera is the crown jewel of TCC’s Nuclear Medicine Technology program, which is one of four such programs in Texas and the only one in North Texas based on a campus. According to Bill Lace, TCC News author, the camera is unique by design.
“Unlike traditional X-ray imaging, the camera employs a radioactive substance, but the substance is placed inside the patient’s body rather than in an external mechanism,” Lace says.
“The gamma camera rotates around the patient, detecting photons emitted from the patient and converting them into multiple images, much like a computerized tomography, or CT, scan.”
These impressive tools aren’t just a one-time cost, as maintenance, updates and upgrades are required to ensure they are reflective of

“Artificial intelligence is one of the most important topics in health care today because it holds the incredible promise of disruptive innovation to improve health care for all.”
what’s going on in real-world hospital care. Ena Hull, an EdTech and education expert and CEO of Ventana Partners, says the start-up and recurring costs of these pricey pieces of equipment are great long-term investments and should be considered an expected cost of solidifying the value of the training program.
“To truly mirror real-world health care, education providers must forge strong partnerships with both hospitals and the technology vendors supplying them,” she says. “Establishing advisory boards with representatives from both sides ensures that labs and programs remain up to date with the latest advancements in medical technology. Additionally, sourcing grant and investment initiatives with tech providers and private industry is vital to ensuring that financial resources do not hinder an institution’s ability to provide cutting-edge equipment and tools in the classroom. This collaboration enables nursing, diagnostic sonography and Allied Healthcare programs to offer students the most current hands-on training, empowering them to thrive in modern health care environments. It’s this synergy among education, health care and industry that fosters innovation and drives excellence in health care education.”
Nearly every health care service and profession will continue to be touched by technology. Thanks to the onset of telehealth, current and future health care professionals must not only be familiar with using artificial intelligence and technology tools in person, but also be able to master the integration of such platforms into their online patient care plans.
According to the American Psychological Association, the use of digital therapy options via mobile applications and digital platforms continues to rise, and practitioners must be comfortable not only using them, but also coaching their clients on their use and safety. The Trinity River Campus also offers a variety of certificates and degrees in the mental health space, including associate degrees in substance abuse counseling and mental health and human services. Patient confidentiality, equity of access and quality of care are all key considerations integrated into the curriculum to ensure that future practitioners are prepared to deliver what their patients need across a variety of platforms, including via telehealth.
Another of Trinity River Campus’ signature health care programs is long-term care administration, one of just a few in the nation offered at the community college. The program prepares professionals to manage skilled nursing facilities. It, too, has made space in the curriculum to reflect the influence of artificial intelligence and technology.
According to an article by Padhan et al, published in the medical journal, Cureus, artificial intelligence offers many benefits to the quality of life and services provided in these facilities. “AI-powered systems can assist older adults in performing daily
activities, such as medication management, fall detection and navigation, enabling them to live independently for longer.” The long-term care administration students are seeing these types of tools in real-world placements and practicums at facilities with which the college partners for the program’s required clinical placements.
There’s simply no question that artificial intelligence, with the enhanced technology equipment that integrates it, is the perfect prescription for high-quality health care and medical workforce preparation. Tarrant County College continues to leverage the influence of community stakeholders and advisory boards, boasting renowned representatives from every major medical and health care sector, to guide and direct its continued prioritization of technology and artificial intelligence investments in equipment and associated training for both faculty and students.
With in-person and online options, as well as credit and noncredit programs, the college continues to expand and evolve its curriculum. Its dynamic and robust listing of health care training and workforce preparation offerings reflects an authentic commitment to integrating technology at the forefront and reaffirms the collective emphasis on preparing a highly skilled workforce through high-quality, hands-on, affordable and accessible training by Dr. Madison and the entire Trinity River Campus leadership. Some other highlighted health care programs with cutting edge technology infused include:
· Computed Tomography: Students learn to use specialized CT equipment to capture detailed diagnostic images of internal organs, bones, soft tissue and blood vessels. These computerized X-ray images help doctors diagnose and plan patient treatment.
· Diagnostic Medical Sonography: Students learn to use specialized ultrasound equipment to collect 2D, 3D or 4D images of organs and tissues in the body that help doctors diagnose and plan treatment of their patients.
· Health Information Technology: Students learn how to use technology to manage and store patient information with accuracy and integrity.
· Magnetic Resonance Imaging Technology (MRI) : Students learn to use specialized MRI equipment, which uses radiofrequency pulses and magnets to create pictures of cross-sections of human anatomy. Doctors use these detailed 3D images to diagnose and plan patient treatments.
“Our health care training programs are empowering our students to achieve the best balance of quality patient care that celebrates technology without sacrificing the human touch,” sums up Madison, offering a perfect prescription for health care preparation and workforce training success.
Cook Children's, JPS, Tarrant County College and Workforce
Solutions strike a collaborative coalition, bringing wellness and career opportunities to a health desert. by tyler hicks
hey came from a variety of backgrounds, some drastically different. Several were veterans; others were formerly incarcerated. Some didn’t have a high school diploma or GED. But they had plenty in common.
They were laborers, and classmates, and they were skeptical about the idea of soft skills training.
The class was part of a partnership among Tarrant County College (TCC), the Tarrant Regional Water District and Upspire, a social enterprise work program. Each partner wanted to upskill entry-level employees and help them attain jobs with good wages.
“We designed custom courses for this program to give our workforce more opportunities,” notes Jacquetta Dantzler, TCC’s interim executive vice president of Corporate Solutions. And the courses were backed by plenty of data.
A Harvard University study found that 85% of job success can be attributed to “soft skills” like communication, teamwork and problem-solving.
Even still, the classmates weren’t convinced—not at first, that is.
“They were very vocal that they did not need these types of classes or training,” Dantzler recalls. “But by the end of it, they were upset that it was over.”
In fact, according to Dantzler, some members of the class returned to their bosses and told them, “the next group you hire, they have to go through this program.”
Those gratifying responses are often the best part of Dantzler’s job—and she hopes to see plenty of them as a similar project looms ahead.
In her role, Dantzler oversees the development of comprehensive training programs for local businesses and their employees. She sees it as an opportunity to invest in the Fort Worth community and, hopefully, change some lives along the way. She’ll have a
chance to do exactly that as part of the team for the sprawling Las Vegas Trail medical complex, which broke ground in late 2023 and will open its doors in 2025.
The complex, situated on nearly four acres at the corner of Calmont Avenue and Cherry Lane, aims to bring much-needed relief and resources to an underserved health desert in west Fort Worth. It’ll boast two stories, 40,000 square feet and a litany of valuable support for the residents of the Las Vegas Trail neighborhood, including primary care offices, a police substation, a job training center and both pediatric and adult health care services.
"This is a catalyst for change," City Councilman Michael Crain said on the brisk November day when the groundbreaking took place. "It really will change the trajectory of the Las Vegas Trail community."
TCC and its partners are playing a pivotal role in that change, and as the grand opening nears, their work is heating up.
Dantzler and her colleagues are designing three programs that will include 27 classes and provide training for hundreds of medical professionals and office leaders per year. What’s more, the Texas Workforce Commission will cover the cost of attendance, travel and childcare, making the career opportunities even more accessible for people throughout the city.
And that’s just part of the story.
Las Vegas Trail will be a joint clinic led by two local health care titans: Cooks Children’s and JPS Health Network. While Dantzler and her TCC colleagues bring their passion for training to the clinic’s future staff, those health systems’ devoted leaders will focus on the patients.
"Being able to help launch these careers is really exciting,” Dantzler notes. “Especially when you think about all of the people they’re going to be able to help. I think this project will have a life-changing impact—in more ways than one.”





Veronica Tolley VICE PRESIDENT OF PRIMARY CARE AND SPECIALTY SERVICES, COOK CHILDREN'S
“We need to define health as wellness. All of the factors of health are connected, and at Cook Children’s, we’re trying to create solutions for greater wellness.”
As a child, Veronica Tolley was a frequent visitor to doctor’s offices and, eventually, hospitals. She suffered from a series of progressively worse ear infections, and since her parents were not native English speakers, they had difficulty navigating the often complex health care system after moving from Mexico to Fort Worth. Worse yet, their questions and concerns were often not taken seriously.
The same was true for her grandfather, who she saw “really struggle” with diabetes.
“It wasn’t because he didn’t take care of himself or my mother didn’t take care of me,” she says. On the contrary, her mother cleaned houses during the day and took English classes at night to prepare for her citizenship test, all while her father worked in construction to keep a roof over their heads and food on the table. “A lot of the time, we just didn’t know where to go, or how to pay for things, or how to work the health care system.”
Ultimately, her infections created significant damage, necessitating surgery to prevent her from going deaf in one ear.
Decades later, it’s clear that this harrowing childhood experience has stayed with Tolley, motivating her to become the person and leader she is today. She once dreamed of becoming a doctor, but college felt unattainable, let alone medical school. However, thanks to a sterling academic record, she earned degrees in sociology and health care administration, paving the way for her current role as vice president of primary care and specialty services at Cook Children’s.
She notes, “when we do our jobs well and for a consistent period of time, we give people more opportunities. That’s how children grow up into adults who can contribute.”
In other words, the Las Vegas Trail clinic—for which Tolley will play a key role—is precisely the kind of place she needed growing up.
Once, not too long ago, this particular neighborhood thrived as a lively, close-knit community. Life revolved around the former Carswell Air Force Base, a U.S. air support training facility that also served as the neighborhood’s central hub. The surrounding single-family homes and apartments housed military families from all over the nation.
Then, in 1993, the base closed, followed by the move or shuttering of grocery stores, health care providers and vital businesses that provided jobs and catered to Carswell families. An area once known for its prevalent military ties became known for its crime.
Although Las Vegas Trail accounts for only one percent of Fort Worth’s population, it experiences four percent of the city’s crime. The median household income in the neighborhood is just $31,495—nearly half that of Fort Worth—resulting in 32% of residents living below the poverty line. Additionally, most local children are raised by single parents in apartments that often fall into disrepair.
Worse yet, Las Vegas Trail is both a food and a health desert, lacking essential resources that contribute to overall well-being.
To Tolley, the “desert” distinction is critical—and it’s a clear-cut reason why a comprehensive clinic is urgently needed in this community.
“We need to define health as wellness,” she says. “All of the factors of health are connected, and at Cook Children’s, we're trying to create solutions for greater wellness.”
The clinic, whose official title is the Las Vegas Trail Neighborhood Health Center, will include a food pantry provided by WestAid Community Services, as well as a demonstration kitchen and a full-time nutritionist. (Because what good is healthy food, Tolley points out, if you’re not exactly sure how to cook it?)
The nutritionist will be joined by a full-time family therapist, who will help address the burgeoning mental health crisis affecting the neighborhood. According to a needs assessment compiled
“I think this project will have a life-changing impact—in more ways than one.”

Jacquetta Dantzler
INTERIM EXECUTIVE VICE PRESIDENT OF CORPORATE SOLUTIONS, TARRANT COUNTY COLLEGE
by Cook Children’s a few years ago, more than one-third of children in the area have a diagnosed mental health need, and the true number could be even higher.
Tackling diverse needs through a project like this is the main reason Tolley has worked for Cook Children’s for 26 years. Her recurring joke (which actually isn’t a joke at all) is that one of her “conditions of employment” is that she be able to work in a neighborhood center for as long as she remains at her current employer.
“I told that to my boss, and he thought I was kidding,” she says. “But I was dead serious. This is the kind of work I want to do forever, because any one entity can't do it alone. Health is much bigger than medical care, and it takes a much bigger group of people to create the ripple effect we want.”
It’s worth noting that there was one pediatrician in particular whom Tolley remembers from her childhood. He was caring and professional, and he took her and her family’s questions seriously.
Later, he would be hired by Cook Children’s, making them coworkers.
Although both health networks have been operating in Tarrant County for over a century, this project marks the first time they’ll be working together under one roof.
Cook Children’s will provide pediatric care, while JPS will care for adults across the hall. Literally. Tolley emphasizes the importance of this dual effort. Often, physicians treating a child may discover that the parent suffers from an undiagnosed health issue (or vice versa).
“What’s different about this is that it’s not just one health
care entity coming in and providing a service—it’s taking the whole patient and family unit in mind,” says Joy Parker, senior vice president of operations for JPS. “We’re meeting those social drivers of health that are often ignored or especially difficult to care for, and we’re also providing a place you can visit if you’re struggling with your apartment because of code enforcement. It’s a one-stop shop for elevating your quality of life.”
Parker is eager to talk about all of the health care resources that will be available by summer 2025, but she is also keen to point out that the historic partnership between her organization and Cook Children’s is a continuation of the community’s momentum.
In 2017, the Fort Worth Star-Telegram published a story laying bare the struggles of the Las Vegas Trail neighborhood. Readers and leaders were shocked by the lack of well-being present mere miles from their own doorsteps, and one reader in particular wanted to turn her outrage into community work.
Paige Charbonnet grew up in nearby Ridglea Hills, so she felt a personal connection to the struggles described in the Star-Telegram story.
“I realized that I could easily read the article and continue with my daily life, or I could take a stand and make a meaningful difference,” Charbonnet told a reporter. “So, I decided to volunteer at the local primary school to get involved.”
Regular volunteering quickly turned into broader activism, as Charbonnet worked alongside city officials and other concerned Cowtown residents to assemble a revitalization plan that would ultimately lead to the creation of LVTRise: a nonprofit that wants to provide long-term solutions for the neighborhood. Thanks in large part to the work of Charbonnet and her newfound team, the neighborhood’s RISE Community Center opened in 2020. Las
“Everyone has their role, and together, we get to create stronger futures for this neighborhood.”

Vegas Trail residents had a new resource for meal assistance, afterschool programs, counseling services and more, and according to Parker, these efforts were the perfect foundation for the health care project arriving next year.
“We want to build trust with the neighborhood,” she says, “and you can’t have trust without investment.”
Speaking of investment: Parker emphasizes that a wealth of data has been accumulated to help her team and Cook Children’s pinpoint the specific needs of this community. That’s why features like the police substation and on-site kitchen were incorporated into the project. Leaders saw an opportunity to improve relationships with the police while also fulfilling the need for fresh food.
On Parker’s side of the complex, the data assessment turned into a focus on women’s health.
“There are a lot of single mothers in this community,” she notes, “so we want to show that we’re listening, and we’re prepared with the resources they need.”
Parker adds that the many teams bringing this project to life continue meeting regularly, “and every time, we make great progress.” She relishes the chance to serve not just one person or one family, but an entire neighborhood. And of course, serving a full community requires plenty of staff. That’s where the TCC team plays a critical role.
After receiving a comprehensive breakdown of each position the clinic will need (including detailed descriptions for each job), Dantzler and her colleagues got to work curating classes for three programs: administrative leadership, medical terminology and office assistance.
Dantzler stresses that each course in the three programs will be fully customized to meet the specific needs of the new clinic and the neighborhood it serves.
Christine Hernandez is the new workforce development specialist for Cook Children’s, and she joined the health system at the perfect time. Her personable and passionate approach—not to mention her decades of talent acquisition experience—will be incredibly valuable as the clinic staffs up. Hernandez is filling hyper-specific roles like pharmacy technician, a job that also involves a lot of turnover. Yet, as she notes, being part of a uniquely diverse and collaborative community is a huge boon to professionals in the medical space—or any industry—and it could make people want to stay longer than they planned.
“Relationships are really important to what I do, and relationships are a fundamental part of the LVT project,” she says. “When you have an alignment like that, it’s a really special set-up.”
In a way, this work reminds Hernandez of the recruiting she did for the city of Fort Worth, where she worked prior to her new post. No one thinks about how a city is run, she says, but depending on the size of the community, you need hundreds or thousands of people to keep it running. The same is true for a health clinic, particularly one that does as much as Las Vegas Trail.
“Everyone has their role, and together, we get to create stronger futures for this neighborhood,” she says. “What’s cooler than that?”
Without knowing it, she is echoing something Tolley often reiterates based on her own trials.
“When you have good health, you’re set up for financial stability,” Tolley says. “You’re set up, really, for a brighter future—a brighter life.”

See how the industry is adjusting to an ever-changing landscape.
by tom delamater

Health care in the United States isn’t just an industry, a political talking point or even, as some would contend, a basic right. Sooner or later, it’s a reality for everyone.
Which is what makes it surprising that a recent Harris poll indicated that more than 70% of adult Americans feel the country’s health care system fails to meet their needs.
From the high cost of insurance and hospital procedures to the perception that medical professionals advocate for expensive treatments and the patients rely on pharmaceuticals over preventive care and wellness, the health care industry is often in the hot seat.
Other factors, including an aging population, a shortage of health care workers and the prospect of more public health crises occurring (like the COVID-19 pandemic) contribute to the challenges facing the U.S. health care system.
At the same time, industry professionals are working hard to provide innovative solutions, particularly through the use of technology.
“We’ve seen a lot of changes in health care technology over the past several years and expect that to continue over the next five years,” says Jared Shelton, president of Texas Health Harris Methodist Hospital Fort Worth.
One example is the growth in cutting-edge techniques like robotic surgeries. While allowing for greater precision and accuracy, Shelton notes that another important benefit of robotics “is smaller surgical incisions, which in turn means patients will have less downtime recovering.”
Robotics have led to other important advancements. Sylvia Trent-Adams, president of the University of North Texas Health Science Center in Fort Worth, says grant funding enabled their Institute for Translational Research to build a fully automated robotic system “that allows for significant capacity to process and analyze blood samples.”
“This robotic system lets researchers test for a number of proteins in the blood, including those linked to Alzheimer’s disease,” she notes, meaning a blood test could soon be developed to detect Alzheimer’s and other neurodegenerative conditions.

Health care providers can use the constant stream of data coming from a patient’s wearable to identify anomalies and patterns that can lead to problems.

Tools like the Da Vinci Surgical System allow doctors to perform minimally-invasive procedures.
“We’ve seen a lot of changes in health care technology over the past several years and expect that to continue over the next five years.”









— Jared Shelton PRESIDENT, TEXAS HEALTH HARRIS
METHODIST
HOSPITAL FORT WORTH






















Technology has also opened the door to more at-home treatment options. “You’re going to see a lot of treatment that ties into wearables,” says W. Stephen Love, president and CEO of the Dallas-Fort Worth Hospital Council.
Wearable technology involves health monitoring devices worn by the patient that collect and report health data digitally. “They can play a big role in improving patient care and overall patient outcomes,” Love says.
The pandemic cast a spotlight not only on the quality and urgency of care but also on vaccines—which, says Love, should be viewed as an essential part of prevention and wellness. Preventive care doesn’t only involve identifying potential health issues before they become major problems. “It also includes proactive steps that patients can take on their own,” he says.
The UNT Health Science Center promotes a “Whole Health Initiative” to empower people to care for their body, mind, spirit and environment. Trent-Adams says that emphasis effects “how we teach our students and how we care for our patients.”
The goal is to help patients take charge of their health and encourage them to make decisions for healthier futures. The center provides health coaches who encourage patients to take control of improving their health. One way they can do that is to take feedback and advice from their physicians and break it down into attainable, sustainable goals.
Fort Worth is at the forefront of the wellness movement in the United States, thanks in part to an initiative known as the Blue Zones Project. Launched locally in 2015 and spearheaded

by Texas Health Resources, the project is a community-led, wellbeing improvement initiative aimed at making healthy choices easier in places where we live, work, worship and play. Nearly 100,000 Fort Worth residents and 500 area organizations are involved, making Fort Worth the largest Blue Zones community in the country.
Wellness and prevention remain important considerations as people age. “Obviously, people want to spend their retirement years as active as possible, so continuing to be focused on wellness and preventive health is key for elder care,” Shelton says.
An increasing challenge facing older Americans is isolation and loneliness, which Surgeon General Vivek Murthy said had reached “epidemic proportions” in a 2023 report.
That’s why the mental aspect of wellness is so critical, says Shelton. “It’s important to stay engaged in social settings, whether that’s through church or local senior centers or even moving into a senior living center with an active social program,” he says.
With more emphasis on wellness and the ever-improving standard of medical care in general, people are living longer than ever before. That presents its own set of challenges for the health care industry.
“Senior and assisted living centers are facing a staffing crisis, often resulting in a lack of qualified health care workers to care for residents,” says Trent-Adams.
In response, institutions across North Texas have established more robust nursing education programs—including UNT’s Health Science Center, which offers bachelor’s and master’s degrees in
nursing and will introduce an MSN degree in psychiatric mental health in the fall of 2025.
Baylor Scott & White, the largest nonprofit health care system in Texas, operates an academic medical center in Fort Worth, where more than 6,000 nurses are in training and more than 1,000 physicians are in residency and fellowship programs.
“This commitment to medical education and training is more important than ever, as Texans now face a projected shortage of nearly 10,000 physicians by 2032,” says Charles Williams, Baylor Scott & White’s president in Fort Worth.
The rising cost of health care stems from multiple factors, says Trent-Adams, including increasing drug prices driven by pharmaceutical patents and exclusivity.
“Administrative complexities associated with insurance claims, regulations and electronic health records also add to the expense,” she says. “Additionally, while technological advancements bring benefits, they are often costly to implement and maintain.”
Trent-Adams offers several strategies that health care facilities are employing to offset rising expenses:
Price transparency initiatives, which help patients make informed decisions by providing up-front cost information.
· Pay-for-performance models, which reward providers for high-quality, cost-efficient care.
· Telehealth, which uses video calling and other technologies to help patients see their health care providers from a
remote location, typically at a reduced cost for both the patient and the provider.
· Policy reforms to address issues such as drug pricing and administrative inefficiencies.
Another factor contributing to the high cost of health care is the ability to attract and retain talent.
A nationwide shortage of 100,000 critical health care workers is expected by 2028, according to a report from Mercer, a global health care consulting firm. Reasons cited include ongoing resignations coming out of the COVID-19 pandemic, continued worker burnout and non-competitive compensation for some roles.
Health care facilities are responding not only with more competitive compensation packages but also with strategies like flexible schedules and opportunities for professional development. New generations of workers are having an effect both on hiring practices and the workplace in general. Millennials and members of Generation Z are now well-established in the workforce, presenting employers with a much different outlook on the role their careers play in their lives.
“Younger generations want more of a work-life balance,” says Love, and are bringing with them expectations centered around meaningful work and growth opportunities.
“These generations seek employers who align with their values and provide flexible work arrangements,” says Trent-Adams. “Cultivating a positive work culture that prioritizes well-being and recognition is also critical, as is investing in technology to reduce burnout and improve care.”

Higher education plays a major role in helping people meet their mental health needs. by heide brandes
The mental health care landscape is undergoing a seismic shift, with telehealth emerging as a dominant force. As of September 2022, 88.1% of mental health treatment facilities offered telehealth services, a trend accelerated by the COVID-19 pandemic but rooted in earlier initiatives.
Rachel Totten, a licensed independent clinical social worker practicing in Vermont, North Carolina and South Carolina, has witnessed this transformation firsthand.
“I began offering online therapy in Vermont in 2018,” Totten says. “When the pandemic hit in March 2020, my entire caseload transitioned to online therapy.”
The rise of telehealth has brought significant advantages to both providers and clients. Not only does it offer clients greater flexibility, but with limited childcare options and more people working remotely, online therapy allows them to fit sessions into their schedules—whether it’s during a lunch break or between meetings—without the burden of long commutes.
However, the transition to telehealth is not without challenges.
“One of the biggest challenges for traditional mental health facilities transitioning to or expanding telehealth services is ensuring compliance with HIPAA and other privacy regulations,” Totten says. “Finding and implementing technology that meets these standards can be costly, creating a financial burden for facilities.”
Training therapists to meet the demand is also a growing movement as more clients rely on remote connections to deal with mental health.
The number of telehealth services in Texas Medicaid increased by over 500% between fiscal years 2019 and 2021. The growing reliance on telehealth for mental health and behavioral health services peaked during the COVID-19 pandemic, when telehealth accounted for 40% of mental health and substance use outpatient visits in Texas.
Data from a study titled “Telehealth and In-Person Mental Health Service Utilization and Spending, 2019 to 2022,” by the peer-reviewed Journal of the American Medical Association showed that during the acute phase of the pandemic, telehealth visits for mental health services increased tenfold nationwide (1019.3%) compared to the previous year.
At the same time, the percentage of mental health treatment facilities offering telehealth services in Texas more than doubled, from 39.4% in 2019 to 88.1% in 2022, illustrating the rapid adoption of telehealth in providing behavioral health services in Texas, especially during and after the pandemic.
In Virginia, a survey of 574 behavioral and mental health providers conducted by the Virginia Telehealth Network (in 2022) indicated that 97% of providers had expanded their use of telehealth due to the pandemic, with 91% intending to maintain or further expand telehealth services.
“Telehealth has dramatically improved access to mental health care for rural populations like ours,” Totten says. “It provides a level of privacy that allows people who may have been hesitant before to seek mental health services more comfortably.”
Despite these advancements, barriers remain. The most prominent challenge is the lack of high-speed internet in many rural communities, Totten says.
“Some areas rely on cell service for the internet, which isn’t always dependable,” she says.
But as telehealth continues to evolve, it is crucial for education programs, health care providers and policymakers to work together to ensure equitable access to mental health services. By addressing technological barriers and providing comprehensive training, the industry can harness the full potential of telehealth to meet the growing demand for mental health care.
Universities are now offering telehealth services to the community, with many embracing actual courses in how to provide remote counseling.
Oklahoma State University provides virtual behavioral health emergency room consults, and virtual hospitalist services will soon be available at the Northeastern Health System in rural Oklahoma. Tele-stroke services are now offered at hospitals in various Oklahoma communities through the hospital, while virtual cardiology services are ongoing with Choctaw Nation in Poteau.
“Oklahoma State University has been pioneering telehealth services for more than 25 years,” says Dr. Johnny Stephens, president of the OSU Center for Health Sciences. “OSU continues to innovate as the leader in telehealth and virtual care, as technology continues to broaden the possibilities of reaching across the state to provide specialty care. Through these efforts, we are working to address both patient needs as well as health care workforce shortage issues.”
Despite this growing demand for telehealth within the field over the past four years and the expansion of telecare to the community, education programs for mental health professionals still rely heavily on the traditional in-person care model.
Michelle Strain, director of counseling services at Mid-America Christian University, noted that colleges and universities have Clinical Mental Health Counseling programs, with MACU having one of the largest. While in-person counseling is preferred by many
According to telehealth.hhs.gov, the COVID-19 pandemic significantly impacted mental health, intensifying the need for behavioral health services across the U.S.
Despite the challenges, the pandemic spurred advancements in health care services, notably in behavioral telehealth, enhancing access to mental health care, particularly for patients in rural and underserved communities.
The most common form of telebehavioral health is individual teletherapy, which can be conducted via video or audio-only services. Various forms include:
• Virtual Talk Therapy: Addresses emotional and psychological concerns
• Telepsychiatry: Provides prescriptions and medication management
• Online Apps: Track and monitor mood
• Text Therapy: Allows anonymous communication with health care professionals
Group teletherapy involves a few people meeting with one or more therapists remotely. It is an effective and affordable alternative to individual therapy, offering community support, reduced feelings of isolation and new perspectives.
Substance use disorder telehealth treatment is also on the rise. With in-home care, patients can access providers who understand substance use disorder while also working with their regular therapist or provider. Home-based telehealth allows providers to see how patients manage treatment in their environment.
For more information on behavioral telehealth services, visit telehealth.hhs.gov.
for its deeper connections, telehealth offers cost-effectiveness and convenience, especially since the COVID-19 pandemic.
Telehealth also allows for firsthand internships for counseling students to gain practical experience, despite the financial burden on agencies hosting interns.
“All clinical mental health students and counseling students are required to do an internship and a practicum,” Strain says. “The practicum in Oklahoma has a requirement of 100 hours, and the internship required is 300 hours, with 210 being direct face-to-face type of counseling. We have several interns here that I manage in our clinic, and they all are doing telehealth.”
Current telemental health training, where available, is transitioning to offer this essential component of professional development. The University of Texas at Arlington, for instance, offers an undergraduate certificate in Telehealth and Health Informatics.
“Telehealth has dramatically improved access to mental health care for rural populations like ours. It provides a level of privacy that allows people who may have been hesitant before to seek mental health services more comfortably.”
Rachel Totten CLINICAL SOCIAL WORKER

The Cummings Graduate Institute for Behavioral Health Studies offers a discount on telehealth training from Telebehavioral Health Institute to students, faculty and alumni, and the Stony Brook University School of Medicine offers a Tele-Preventive Medicine (TPM) program that teaches virtual preventive medicine and lifestyle medicine interventions.
The University of Kansas Center for Telemedicine and Telehealth also has a program in Digital Mental Health in collaboration with the KU School of Medicine-Wichita Department of Psychiatry and Behavioral Sciences. So the word is out nationally about the value of telehealth training for mental health providers.
Scott Healy, CEO of Psych Hub, the leading platform for mental health continuing education, emphasizes the importance of upskilling providers in best practices to improve mental health care delivery and outcomes.
Because higher education programs recognize the growing demand for telehealth, many are working to fully integrate tele-mental health training into their core curricula. Some offer elective courses or certifications,and courses are being designed to address the practical and ethical aspects of virtual care more comprehensively.
“Deeper courses on how to be an effective online therapist are important because remote therapy presents its own unique
challenges and opportunities,” Healy says. “Virtual care requires a different skill set compared to in-office sessions, such as managing technology, building rapport in a virtual space and addressing privacy concerns.”
One challenge of adding telehealth training to clinical education is ensuring this training is robust enough to cover both practical and ethical aspects of virtual care. To overcome this, organizations like Psych Hub offer targeted online continuing education and training in evidence-based practices for licensed clinicians.
“While Psych Hub doesn’t work directly with universities, we play a crucial role in helping mental health practitioners upskill through our online continuing education courses,” Healy says.
Training mental health providers in telehealth-specific care is critical as teletherapy continues to gain popularity and reach new patients, especially in rural areas.
“What has resulted is people have a way of finding a counselor they connect with, and they suddenly have a lot more options because there are a lot more counselors who live in their same state and not just in their own personal community,” Strain says. “So that has been a real bonus to telehealth.”
The future of mental health care delivery lies at the intersection of technology and human connection. For businesses in the health care and education sectors, investing in telehealth infrastructure and training represents not just a market opportunity but a chance to make a significant impact on public health and well-being.


Tarrant Small Business Development Center (SBDC) provides management and technical assistance to local small businesses and aspiring entrepreneurs throughout Tarrant County The consulting services provided are at no cost and training services are at a nominal fee
Business consulting services are customized, one on one face-to-face or virtual at no cost Consulting services provided are business plan development, capital acquisition, marketing, regulatory compliance and more. The Tarrant SBDC provides services to a diverse population, including special emphasis groups; women, minorities and veterans who are seeking to start or grow their business.


The Tarrant SBDC is hosted by Tarrant County College and is one of twelve field centers of the North Texas SBDC Network Funded in part through a cooperative agreement with the U S Small Business Administration (SBA) SBA’s funding is not an endorsement of any products, opinions or services.

Accounting & Bookkeeping
Business Planning
Cash Flow Models
COVID-19 Support
Disaster Services
Financial Planning
Government Contracting
Legal Structures
Licensing & Permits
Market Research
Startup Cost
Target Marketing
Special arrangements for the disabled will be made when requested in advance Advising services are offered by the Tarrant Small Business Development center without regard to race, color, age, national origin, religion, sex or disability. Special provisions will be made for limited-English speaking individuals.
For accommodations, please contact the Tarrant SBDC at 817-515-2600
www tarrantsbdc org


When it comes to groundbreaking medical technology and products, Tarrant County is the gold standard. by terri marshall
As the saying goes, everything’s bigger in Texas. This tagline rings true for biotechnology and pharmaceutical advancements. According to a report by the Texas Economic Development Corporation, more than 5,200 biotechnology and life sciences-related manufacturing and research and development firms operate in the state, making Texas an industry leader in biopharma innovation.
The report also notes that biotech and life sciences companies continue to plant roots in Texas, creating new jobs and investing in local communities. Top Fortune 500 companies, including Kimberly-Clark, Celanese and McKesson are based in Texas. Additionally, global industry leaders, including Abbott, Alcon, Allergan, Johnson & Johnson, Lonza and Medtronic, have major operations within the state.
Founded in Fort Worth in 1945, ophthalmic leader Alcon’s pharmaceutical successes continue to grow. The company began when Fort Worth pharmacists Robert Alexander and William Connor combined the first letters of their last names to open a small pharmacy. Now a global company, Alcon’s leadership remains grounded in cutting-edge innovation and breakthrough technology, focused on transforming the treatment of eye diseases and conditions. The company boasts the widest array of eye care offerings in the industry, with products organized into two businesses: Surgical and Vision Care.
One example of the exciting new innovations happening in Tarrant County was Alcon’s opening of a research clinic in the summer of 2024. This welcome addition offers Fort Worth locals the opportunity to participate in clinical trials using never-
before-seen, cutting-edge technologies. The new clinic follows a successful clinical research facility that the company opened in 2018 in Johns Creek, Georgia. The Georgia clinic allowed Alcon to quickly test new vision care products through collaborations with chemists, clinicians and engineers.
“The results of this recipe, both scientifically and culturally, worked really well,” says Dr. Raj Suryakumar, Alcon’s vice president and global head of clinical research and development. “So, as we expand our surgical, pharmaceutical and vision care R&D footprints, we wanted to replicate that success in Fort Worth. Alcon is committed to engaging the communities where we live and work. Opening a research clinic in the heart of the city where some of our most innovative ideas have come to life felt like a natural extension of that commitment.”
The Fort Worth facility is fully dedicated to Alcon, which gives the company complete control over the research process. This benefits the R&D process in several ways, including allowing for more productive collaboration between clinicians and scientists, creating more efficiency and accelerating the clinical trials process.
“Many eye care professionals (ECPs ) are interested in participating in our clinical programs as investigators or collaborators to advance research,” Suryakumar says. “Sometimes, not everyone who wants to participate can, especially in more rigorous trials that require clinics to have certain infrastructure or equipment. Our new Fort Worth research clinic will allow ECPs in the Dallas-Fort Worth metroplex to participate in a more flexible capacity, enabling them to be at the forefront of informing on cutting-edge Alcon innovation.”

According to a report by the Texas Economic Development Corporation, more than 5,200 biotechnology and life sciences-related manufacturing and research and development firms operate in the state, making Texas an industry leader in biopharma.
“As scientists, we can be very particular about our ideas coming to life exactly as we intended.”


Dr.
Raj Suryakumar VICE PRESIDENT AND GLOBAL HEAD OF CLINICAL RESEARCH AND DEVELOPMENT, ALCON
Located in the heart of Fort Worth’s downtown medical district, the Alcon Research Clinic primarily focuses on non-invasive feasibility trials. Local patients who volunteer to participate in the studies experience brand new technologies designed to help shape the future of eye care.
“As is the case with all trials conducted with the highest levels of integrity, patients will have the opportunity to understand the trial details, the benefits of participating and the time commitment we’ll need from them,” Suryakumar says. “At the end of the day, though, participants will be exposed to the latest eye care technology, gain a better understanding of their vision and vision science and, hopefully, become ambassadors for the important work we’re doing in Fort Worth and the research community we’re building as a result.”
R&D remains at the forefront of Alcon’s mission. In 2023, the company spent $828 million on R&D, more than any other eye care company worldwide. Alcon currently has over 90 active projects in the R&D pipeline. Alcon approaches R&D projects by conducting a range of studies, accessing devices and evaluating their performance. This enables their scientists to make datadriven, informed decisions, which in turn optimizes product development.
“As scientists, we can be very particular about our ideas coming to life exactly as we intended,” Suryakumar says. “I’m thrilled to say we achieved that with this research clinic, and we’re so excited for its potential to bring new ideas to fruition in the same way.”
One of the most notable trends in health care is the expanded use of artificial intelligence (AI). Tarrant County’s Medtronic utilizes AI and other technologies and therapies to treat numerous health conditions. AI plays a pivotal role in Medtronic’s colonoscopy and endoscopy systems, insulin pumps and robotic-assisted surgery platforms.
In April 2024, Medtronic announced the latest advancements in AI for endoscopic care by unveiling ColonPRO, the latest-generation software for the GI Genius intelligent endoscopy system. GI Genius was the first commercially available computer-aided detection system that used AI to identify colorectal polyps. Its significant impact has been well researched with more than 30 academic peer-reviewed publications across a combined total of 23,000 patients.
Based on the current global install base, the GI Genius system has the potential to impact 2.7 million patients annually. Now, with the launch of ColonPRO software, the GI Genius system takes a significant leap forward in AI-driven polyp detection by introducing an enhanced algorithm, supported by a dataset that is double the size of the previous one, resulting in a notable improvement in its detection capabilities.
Wearable technology has increased in use as more individuals are using smartwatches as fitness and health tools. Now, electrocardiogram technology has been added to products to measure heart activity and reveal potential abnormalities. Additionally, continuous glucose monitoring sensors provide 24/7 monitoring to help individuals with Type 1 diabetes track their blood sugar and adjust accordingly.
The next generation of wearable health technology includes electronic skin patches. Adhering directly to the skin, the patches monitor vital signs, deliver medications, provide wound care and detect motion. The sensors in the patches contain wireless transmitters that allow clinicians continuous remote access to data.
With the health care industry’s continued growth throughout Texas, students have ample opportunities to pursue interests in the pharmaceutical sector. For example, through co-op programs and internships, Alcon provides real-world impact and work experience to university students in the areas of engineering, finance, human resources, marketing, research and development, sales, supply chain management and technology.


We have many ways to partner with your organization:
Volunteer Engagement
Employee Giving
Matching Gifts
Naming Opportunities
Philanthropic Investment
Sponsorships and so much more…

Take a look inside dentistry’s workforce crisis with perspectives from public and private practice. by james ndone, phd
Just like many other industries, the dental sector is facing a post-pandemic workforce crisis. Staffing shortages, increasing patient demand, and technological changes are stretching both private practices and public health clinics to their limits. It’s a challenge that spans the entire field, and it’s something Dr. Derrick Joseph, a private practitioner, and Dr. Anya Harris, a leader in public health dentistry, know all too well. Despite working in different sectors, both face remarkably similar hurdles, stressing the broad shifts the entire dental industry is experiencing.
For Joseph, CEO of Pristine Dental Care, the struggle to find and retain qualified dental hygienists and assistants has been a constant battle since the pandemic started. “Currently, private practices are facing challenges recruiting and retaining skilled staff like dental hygienists and assistants,” Joseph explains. “On top of these shortages, we also have the influx of patients post-pandemic that delayed treatment, and patients prioritizing aesthetics like clear aligners, whitening and veneers, leading to increased workloads and burnout among existing employees.”
The shortage issue is particularly pronounced in the Metroplex. Brandy Cowen, a registered nurse who is also an assistant professor at Texas A&M University’s College of Dentistry, says that D/FW is uniquely positioned to demonstrate to the country how to fill the profession’s gap.
“Like the U.S., Dallas/Fort Worth is also experiencing a growing shortage of dental and allied dental professionals like dentists, dental hygienists and dental assistants,” she says. “This is especially true in underserved areas within our communities. These shortages lead to longer wait times and reduced access to oral health care. However, the demands are increasing through metropolitan growth, our aging population and the increased awareness of the importance of oral health in overall health.”
Dental and allied dental educators, Cowen says, are trying to get ahead of demand. Many programs are seeking state and local grants and funds to expand their educational capacities for would-be dental professionals. The challenge, however, is that there is a shortage of dental and allied dental educators.
“Some institutions are introducing accelerated programs for dental hygiene and dental assisting to enter the workforce more quickly,” Cowen says. “This reduces the educational timeline without sacrificing the quality of training. Several programs are partnering/increasing off-site rotations within the community health centers and clinics. This collaboration helps prepare
students for the workforce while addressing immediate gaps in care for underserved populations.”
Harris, director of dental services at Hamilton Community Health Network, echoes these concerns from the public health side. “There has been an increase in demand for dental public health services since the pandemic,” she says. “Like many occupations, we’ve suffered workforce shortages. During the pandemic, many dentists left the profession and/or retired. We saw a decline in dental assistants as well. Private offices became more aggressive in their compensation offers, which has impacted public health support staff retention.”
The competition for talent is fierce in both the public and private sectors. On the public health side, Harris notes that “funding and resources limit public health dentists’ ability to regularly address oral health disparities among underserved populations.” While both sectors want to retain their workforce, limited resources remain a constant challenge for public health. Although private practices offer higher wages that public health clinics often can’t match, they also grapple with several problems. “Private practices struggle with insurance reimbursements, leading offices to go fee-for-services or offer in-house membership plans to reduce dependency on insurance plans,” Joseph points out.


“Offering competitive salaries, bonuses and benefits helps attract and retain staff in a competitive market. Providing flexible work hours and accommodating schedules helps reduce burnout and improve work-life balance.”


Patient demand, meanwhile, continues to rise across the board. This has created significant pressure on both private and public practices to keep up, often with reduced staff. “We’ve seen an increased demand in public health dentistry,” Harris says. “With so many individuals being unemployed and losing health care benefits in recent years, we’ve seen an increase in patients utilizing state-funded insurances like Medicaid and Medicare.”
The use of technology is one area where both private and public health practices are making strides, but this too has implications for workforce dynamics. “The use of technology, like digital impressions and AI, has influenced staffing needs in private dental practices by increasing the demand for skilled employees who can operate these new tools,” Joseph says. On the other hand, he notes, “workflows are more streamlined, reducing manual tasks and allowing practices to function more efficiently with reduced staff.”
In public health, tele-dentistry is proving to be a game changer. “Many public health dental programs have integrated (or have begun integrating) telehealth solutions to better reach underserved populations, particularly those struggling with transportation access,” Harris explains.
Both Joseph and Harris agree that the key to navigating these challenges lies in strategic workforce management and professional development. Joseph stresses the importance of flexibility and growth opportunities: “Offering competitive salaries, bonuses and benefits helps attract and retain staff in a competitive market. Providing flexible work hours and accommodating schedules helps reduce burnout and improve work-life balance.”
For Harris, government policies play a vital role in shaping the public health workforce. “Government policies are essential to establishing a robust and responsive dental public health workforce. Federally Qualified Health Centers (FQHCs) are government-funded, typically surviving on grants and Medicaid reimbursement.”
Looking ahead, both practitioners foresee ongoing challenges but also recognize opportunities for innovation. “Continued staffing shortages, increased demand for services and technological integration will impact private dental practices in the next few years,” Joseph says.
In both public and private sectors, the dental industry is at a turning point. As Joseph advises, “Investing in your workforce is crucial for the long-term success of private dental practices. Prioritizing staff training, fostering a supportive culture and adapting to changing patient needs will not only enhance employee satisfaction but also improve patient care.”
Many academic programs, according to Cowen, are incorporating new technologies, such as teledentistry, into their curriculum to help expand the reach and promote more efficient and effective deliveries of oral health care through evidenced-based research.
For her part, Harris encourages young dentists to explore public health opportunities: “You are needed, and the work you do means so much to the communities you serve. As our communities become more focused on overall health and interdisciplinary collaboration efforts become more widespread, we will see increased utilization of dental services.”

Test your knowledge about the health care industry.
by jacquetta dantzler
Welcome to our “Deep in the Heart of Health Care” quiz! Texas is leading the way in medical innovation, community health and health care education. Whether it’s groundbreaking biotech developments, the expansion of telehealth or the rise of AI-driven diagnostics, health care in Tarrant County and beyond is transforming rapidly.
Test your knowledge of the incredible advancements, fun facts and future trends that make the heartbeat of health care stronger every day. Let’s see how well you know the landscape that’s shaping a healthier tomorrow.
Hint: Some answers can be found in this issue of The Lens
1. According to the chancellor of TCC, what is a major health care challenge in Tarrant County?
a) Increasing agriculture workforce
b) Access and availability of health care services
c) Managing tech industry expansion
d) Reducing student enrollment
2. What percentage of mental health treatment facilities offered telehealth services as of September 2022?
3. What program at TCC’s Trinity River Campus integrates new tech like the Siemens Symbia Evo gamma camera?
a) Nursing Program
b) Diagnostic Medical Sonography
c) Nuclear Medicine Technology Program
d) Health Information Technology
4. What consortium focuses on connecting health care industry needs with workforce training in North Texas?
a) BioNorth Texas Alliance
b) Biotechnology and Healthcare Industry Alliance of North Texas (BHIANT)
c) Tarrant County Healthcare Partnership
d) Fort Worth Healthcare Initiative
5. What is a key feature of electronic skin patches in wearable technology?
a) Ability to perform X-rays
b) Real-time heart surgery assistance
c) Monitoring vital signs and administering medication
d) Wireless blood transfusion
6. Which of the following programs does TCC offer to prepare students for health care roles with emerging technologies?
a) Medical Coding and Billing
b) Biomedical Equipment Technology
c) Health Information Technology
d) Veterinary Technology
7. Tarrant County College (TCC) offers a unique program in which of these health care fields, which are rarely available at other community colleges?
a) Diagnostic Radiology
b) Long-Term Care Administration
c) Physical Therapy Assistant
d) Dental Hygiene
8. In the U.S., what percentage of health care spending goes toward chronic disease management (e.g., heart disease, diabetes, cancer)?
a) 20%
b) 40%
c) 60%
d) 85%
9. Which health care innovation was co-developed in Texas and has become a widely used life-saving procedure?
a) CPR (Cardiopulmonary Resuscitation)
b) LASIK eye surgery
c) The artificial heart
d) Fluoride treatments
10. In 2020, which health care field was predicted to grow the fastest in Texas, largely due to an aging population?
a) Cardiovascular Surgery
b) Physical Therapy
c) Home Health Aides
d) Geriatric Nursing
11. In Texas, telehealth usage surged due to the COVID-19 pandemic. By how much did telehealth visits increase for behavioral health services?
a) 200%
b) 350%
c) 500%
d) 1,000%


by adam pitluk, phd | photography by terri glanger
Jesus Chavez was broken. His right rotator cuff was torn, and his left ACL was ripped. The injuries occurred within minutes of each other, and the searing, flaming-hot pain reared up in waves, first emanating from his right shoulder down his arm and into his fingertips, followed closely by a similar pain starting at his left knee and streaming down his leg into his toes.
Chavez was in trouble. He struggled to raise his right arm even to his waist while he hobbled on a diminished left leg. The situation was bad for him, but to make matters worse, he was still expected to put up a fight—figuratively and literally— against one of the best pound-forpound boxers in the world.
It was Feb. 28, 2004, and a soldout audience packed the storied MGM Grand Garden Arena in Las Vegas for a boxing match that was simultaneously broadcast on HBO. This was a bout that not only boxing faithful anticipated, but that the city of Austin, and more broadly, the state of Texas, had circled on the calendar months before. Jesus ‘El Matador’ Chavez was a local legend in Austin. Many articles (and a book called Standing Eight) had been written about the twice-deported ex-con who was now a professional fighter making his permanent and legal home in the state capital. He rose through the ranks in the court system and the World Boxing Association, ultimately culminating with the Super Featherweight Championship of the World.
But his first title defense wasn’t against an easy mark. Rather, his first
defense was against a world champion in his own right. Erik ‘El Terrible’ Morales was already a two-time world champion at Super Bantamweight and Featherweight. He moved down in weight to fight Chavez at Super Featherweight because he was on a mission: He wanted to be the first Mexican-born boxer to be a world champion in four different weight classes. But he’d have to notch number three first, and that meant going through El Matador.

Morales did indeed triumph in a 12-round decision. But Chavez became a legend in that fight: Even after he tore his dominant rotator cuff in the second round, and notwithstanding that he had to stand relatively still and take all of Morales’ incoming punches on account of a torn ACL suffered in the third, Chavez did not quit. He sustained what amounted to two career-ending injuries at the same time, and yet he fought the two-time world champion on HBO and in front of the Las Vegas capacity crowd with one arm, and on one leg. In time, Morales would indeed go on to make history and become a champion in four different weight classes. Chavez, on the other hand, would go back to Austin, where doctors performed several surgeries over many months to patch him back up. He rehabilitated his injuries while working vigorously with his boxing and athletic trainers. And because of his work ethic (and especially because of his medical staff), Chavez would make an unexpected return to the ring in 2005 to become the Lightweight champion of the world.
















































