


Thank you to all who entered our Quiz. F
from all- correc t entries: Ÿ K ate E
Ÿ Anny B
Ÿ Kyosuke
Ÿ Levi
Ÿ Catherine M
Congratulations!
Your $25 voucher is on its way
hepsa.asn.au/communitynews

About the Cover: O’liver meets fellow mascot Milpa the Goanna from the Aboriginal Health Council of SA at the Tarpari Wellbeing Day (see p9); Milpa’s job is to help people learn about trachoma and how to stop it, so that kids and adults in remote communities in Australia will have good, strong eyes again.


Correspondence: Please send all correspondence to The Editor at PO Box 782, Kent Town, SA 5071, or email editor@ hepatitissa.asn.au.

Editor: James Morrison
Regular Contributors: Cecilia Lim, Joy Sims
Some photos in this publication may have been altered to disguise identifying details of members of the public. This resource was prepared and printed on Kaurna Country.

Disclaimer: Views expressed in this newsletter are not necessarily those of Hepatitis SA. Information contained in this newsletter is not intended to take the place of medical advice given by your doctor or specialist.

We welcome contributions from Hepatitis SA members and the general public.
SA Health has contributed funds towards this program.
ISSN 2651-9011 (Online)

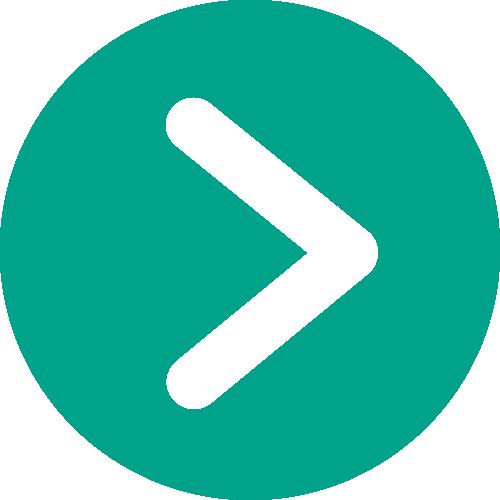
For a long time it has been standard practice to recommend anyone living with hepatitis C to get vaccinated against hepatitis B, as the two viruses together can put more strain on somebody’s health, and their liver in particular. In some good news, however, recent research indicates that having had a hepatitis B infection in the past does not increase the risk of liver cancer for someone who has then been infected with hepatitis C.
A study led by Hidenori Toyoda and published recently in the Journal of Viral Hepatitis defined patients as cured of hepatitis C in the usual way, with a sustained virological response (SVR) test showing no virus in the blood 12 weeks or more after completing treatment.
They looked at people who had achieved SVR between 1990 and 2017, meaning they included those who had been treated using both combination therapy and the more modern (and more effective) direct-acting antivirals.
By examining stored blood samples, they were able to find more than 1200 patients who, before commencing HCV treatment, had clinically significant levels of hepatitis B core or surface antibodies, indicating previous hepatitis B infection.
Despite previous research suggesting that prior hepatitis B infection made hepatocarcinogenesis more likely in people living with hepatitis C, even after being cured, this study found no such thing. In fact, only 57 patients—less than five per cent of those in the study—developed liver cancer after being cured of their hepatitis C. And in those few who did develop liver cancer, there was no correlation with how serious their old hepatitis B infection had been. The cancer rate was no worse than for those who had never been exposed to hepatitis B in the first place.
The factors that did seem to have an effect on the chance of developing liver cancer were things like age, sex, and the degree of liver fibrosis a person had. The biggest risk, though, was leaving hepatitis C untreated, which is of course also often associated with someone never getting tested for hepatitis C. This research demonstrates yet again the importance of widespread testing and treatment for hepatitis C. Not only will this help us to eliminate the virus, but it means that those who have had to live with it in the past can look forward to much healthier futures.
SEE MORE:
https://bit.ly/pasthepb
In 2022 an unusual, and probably new, form of hepatitis began to appear in a number of countries, being first noticed in the UK, then spreading to Spain and the Netherlands and on to at least 35 other countries, including the USA. Unusually, and alarmingly, all of the known cases were in children. A number required transfer to specialist children’s liver units, with some needing lifesaving liver transplants.
The most common symptoms of the mysterious hepatitis were vomiting and jaundice: jaundice is a well-known symptom of serious hepatitis, as damaged livers can lead to high levels of bilirubin (a yellowyorange bile pigment) in the body, which turns the skin and the whites of the eyes a yellow colour. We first reported on this outbreak in the Hepatitis SA Community News in 2022 (see issue #94).
Now, a world-first analysis of the outbreak by researchers at the University of Sydney has found that the primary suspect is highly likely to be an infection by multiple viruses. However, many questions still puzzle the researchers. The outbreak affected only children under the age of 10, and, within
a year, more than 1,000 children from 35 countries with hepatitis of unknown origin were reported to the World Health Organization. But after 12 months, cases seemed to stop just as quickly as they appeared.
The study found evidence that supports an existing theory that the mysterious hepatitis was caused by an infection of different viruses at the same time, but also reveals cases were higher and more severe than initially thought. In the end, six percent of the reported cases needed liver transplants.
However, inconsistent surveillance and monitoring by health agencies means that questions around the outbreak are only halfanswered, including why cases were reported only in certain countries.
“When the outbreak unfolded, the increase of cases was baffling. It was intriguing as to how these cases occurred and why there were cases from the United Kingdom as well as cases from the United States,” said study co-author Professor Guy Eslick from the Australian Paediatric Surveillance Unit at the University of Sydney. The first reported cases were in the UK, and then the US, particularly

in the state of Alabama. However, there was no clear link that could explain how the outbreak crossed continents.
“It was a medical mystery we wanted to investigate. In this study, by bringing together all available evidence, we can form a clearer picture about the cause of the outbreak. This will be crucial for the identification and prevention of future outbreaks,” Professor Eslick explained.
The research team pooled evidence from all available studies reporting on cases of hepatitis of unknown origin, where doctors were unable to determine the cause. The team found that the number of cases were higher and more severe than initially thought, with the data revealing more than 3,000 cases. The mortality rate was 3.5%. As we reported at the time, there was also strong evidence supporting a leading theory the hepatitis was caused by infection of different viruses at the same time.
A common childhood virus called adenoassociated virus 2 (AAV2) was present in blood and tissue samples from the majority of children with unexplained hepatitis, and many were infected by multiple ‘helper viruses’. AAV2 cannot multiply unless there is a ‘helper virus’ to kickstart the infection, which can include other common childhood respiratory and intestinal viruses, such as
 Professor Guy Eslick
Professor Guy Eslick
adenovirus, enterovirus, rhinovirus (common cold) and herpes viruses. In some patient samples, SARS-CoV-2 (COVID-19) was also detected.
The timing of the outbreak and the COVID-19 pandemic potentially also had a role. After COVID-19 pandemic restrictions were lifted, young children who had been isolated may have had immune systems less trained to fight off common childhood infections. But many questions continue to puzzle researchers. These include how the outbreak appeared, and if there could be a genetic link that made some children more vulnerable in developing severe hepatitis than others. Another question is why certain countries were major epicentres of the outbreak, with cases concentrated in the UK and US. Although there were cases in New Zealand, there were no cases in Australia.
The findings were published in the Journal of Infection, and although they offer a clearer picture of the outbreak, Professor Eslick noted that our understanding of the 2022 hepatitis of unknown origin outbreak is still incomplete. There was inconsistent reporting and surveillance of the outbreak between countries already under pressure managing the COVID-19 pandemic.
The Australian Paediatric Surveillance Unit is continuing to monitor for hepatitis cases of unknown origin. They have been monitoring all cases of severe acute hepatitis in children and adolescents, not just the unknown cases. However, Professor Eslick said further research is required. Since the 2022 outbreak, monitoring by many health agencies overseas, such as the American CDC, for similar hepatitis cases in children has stopped.
“The lesson from all past and present disease outbreaks is the need to be continually vigilant. This is something we need to continue investigating,” Professor Eslick said.
READ MORE: bit.ly/childhep
Sydney-based researchers have discovered a new way to treat hepatocellular carcinoma (HCC), the most common type of liver cancer, and the third leading cause of cancer death worldwide. Hepatocellular carcinomas are often caused by late-stage hepatitis, and since they often show no outward symptoms, they are often diagnosed late and are hard to treat effectively in time. Though the new treatment has only been trialled in mice, it is hoped to move on to human trials soon.
The study, led by the Centenary Institute, a New South Wales-based research organisation focused on treatments for serious illness, revealed an encouraging treatment strategy involving the use of a new drug called Blockmir CD5-2.
Cancer is what happens when cells start evading their normal process of death and
renewal, which is built into their DNA. In the trials, Blockmir was combined with a drug called ‘programmed cell death protein1 antibody’ (anti-PD1 antibody). This antibody helps counteract that evasion and the combination of the two medications proved effective in reducing liver tumour size in mice. This research was published in the journal Frontiers in Immunology
Lead author of the study, Dr Ken Liu, a researcher in the Centenary Institute’s Centre for Cancer Innovations, said the discovery was exciting and had the potential to be a viable treatment for advanced liver cancer.
“The synergistic effect of the drugs Blockmir CD5-2 and anti-PD1 antibody significantly reduced the size of liver tumours in mice in our study. We believe
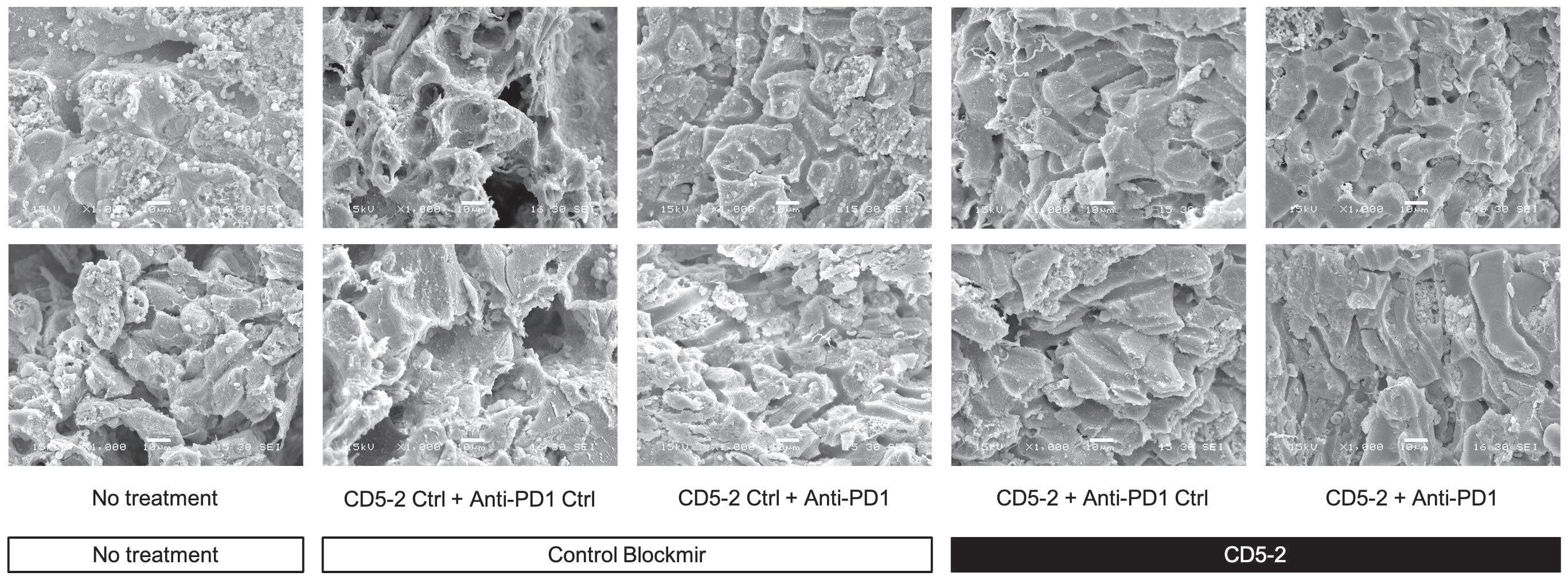
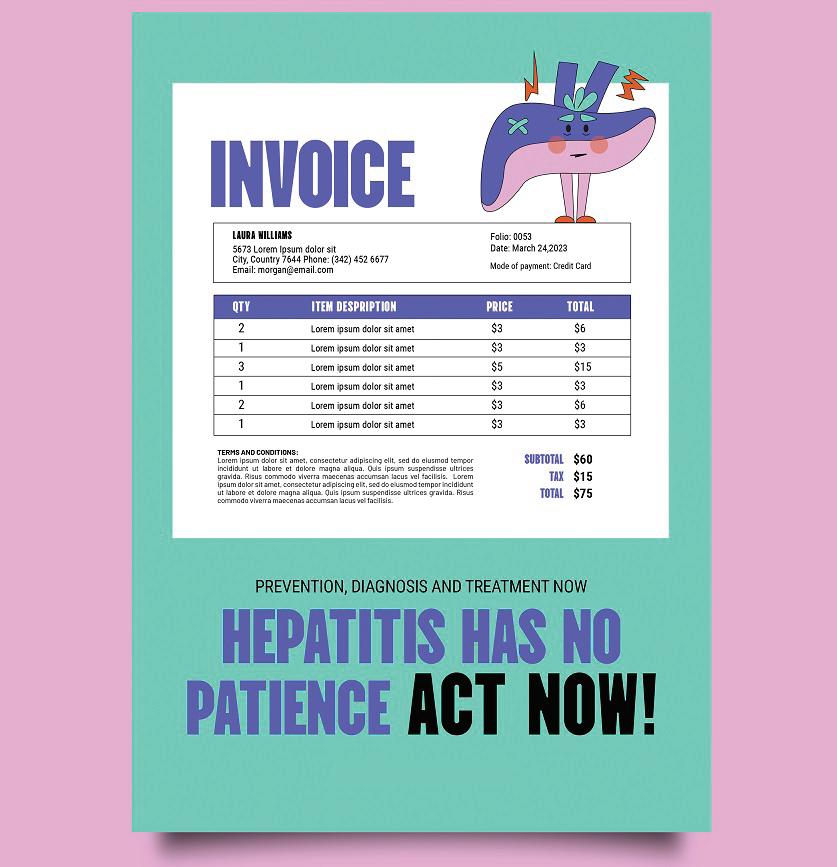
CD5-2 treatment improved tumour vessels structure. Representative scanning electron microscopy images of liver tumour blood vessels in the different treatment groups. Qualitatively, tumour blood vessels appeared to be more regular and well-organized compared in mice from groups treated with CD5-2 compared to control Blockmir or no treatment.
that this dual-drug approach enhances the immune system, rendering it more efficient in combating cancer cells and reducing tumours,” said Dr Liu.
Dr Liu explained that liver tumours often have abnormal blood vessels and low oxygen levels, creating an environment that suppresses the immune system and the body’s ability to fight cancer.
“Blockmir CD5-2 addresses this issue by promoting the health of tumour blood vessels through the activation of a protein called VE-Cadherin. This results in improved blood supply and oxygen levels within the tumours,” said Dr Liu. “The enhanced blood vessel conditions within the tumours means that more cancer-targeting immune cells, specifically cytotoxic T cells, can infiltrate the tumour and effectively combat the disease.”
The researchers said that use of the anti-PD1 antibody was also a crucial component of the innovative treatment approach, helping the immune system fight cancer more effectively by blocking a protein that hinders the immune response.
Senior study authors Professor Jennifer Gamble (from the Centenary Institute’s Centre for Healthy Aging) and Professor Geoff McCaughan (from the Centenary Institute’s Centre for Cancer Innovations) said that current effective treatment options for liver cancer were limited and that the new therapeutic approach held tremendous potential for effectively treating such a challenging disease.
The next stage will be to trial this approach in humans. If it works similarly well there, it will be an invaluable weapon in the fight against a difficult and dangerous disease.
READ MORE: pubmed.ncbi.nlm.nih.gov/37795103/
Dr Ken Liu
The World Hepatitis Summit has called on governments to put words into action and take concrete steps to reduce the impact of viral hepatitis. Participants at the Summit’s final sessions expressed anger at political leaders over their disregard for the thousands of hepatitis deaths every day, and at their lack of action in moving towards hepatitis elimination despite signing up to the World Health Assembly’s hepatitis elimination goal in 2016.
Numerous speakers and delegates from the floor pointed to the alarming number of hepatitis deaths, presented in the WHO Global Hepatitis Report released at the Summit two days before. The 1.3 million deaths from hepatitis B and hepatitis C each year were, they said, totally unacceptable because effective prevention and treatments are available for these diseases.
The Global Hepatitis Report 2024 revealed that despite a decline in new hepatitis infections, hepatitis deaths had continued to climb, with hepatitis B accounting for 83 per cent of the deaths. Panelists at the “Why we must succeed” session, all of whom have lived experience with hepatitis, spoke of the sadness – and anger – they felt, knowing that those deaths were preventable.
Some, like World Hepatitis Alliance (WHA) past-President and community advocate, Danjuma Adda, said the hepatitis community had been “too quiet”. “We need to knock on doors… and shake the tables,” he said, adding that what hepatitis advocates had been doing for so long “does not work” as data is still showing that people are dying. “Let’s do something different!”
WHA board member, Dee Lee, echoed the sentiment saying hepatitis advocates – even
Continued on p11
In Australia, the media has long portrayed drug use, and those who engage in it, in a negative light, as part of the extended and hopelessly mismanaged global “war on drugs”.
This portrayal fuels stigma and misconceptions about drug use, which are reflected in how alcohol and other drugs (AOD) are depicted in news stories and other media narratives. Unfortunately, this creates a cycle where society shuns individuals dealing with AOD dependence, and support services hesitate to offer the help they need. Ironically, these attitudes only worsen the problems faced by those using AOD, and harm their communities as well.
In an attempt to start countering this kneejerk laziness and prejudice on the media’s part, a group of researchers from The South Australian Network of Drug and Alcohol Services (SANDAS) undertook an extensive study, with three main goals. First, to provide media organisations with a set of standards to evaluate their AODrelated content before publishing. Second, to assess how South Australian media outlets are presenting AOD issues. And third, to suggest improvements to existing guidelines for relevant stakeholders and policymakers, along with additional strategies for positive representation of AOD use in the media. If implemented, the resulting framework would make for much higher standards in reporting on the issue of drug use in Australia.
The findings revealed that, unsurprisingly, most of the media samples reviewed were
inadequate, with only one being rated as excellent. Consider, as an example, the framing of community concerns last year when Uniting Communities proposed opening a rehabilitation clinic in Glenelg. “Anger over Jetty Rd drug rehab clinic proposal: ‘We don’t want it to be Junkie Road’” was the Advertiser’s sensationalist framing of the issue. This and other articles on AOD in the community contained unethical and biased reporting, stigmatising language, alarmist content, lack of context, and privacy violations. They also lacked input from AOD experts and health practitioners, and failed to provide links to prevention or intervention resources.
The SANDAS study addresses these shortcomings through proposals in three main areas. These recommendations aim to promote fair, accurate, and compassionate reporting on AOD issues, ultimately working towards reducing stigma and improving support for those affected by AOD dependence.
There is a need for the Australian Press Council to modify their existing guidelines to more specifically address reporting on substance use. These modifications should emphasise the importance of ethical reporting, avoiding stigmatising language, and the responsible portrayal of individuals with lived experience of AOD.
In addition, the scope of what is considered private in the statement of privacy principles could be broadened to provide better alignment regarding human rights

An example of what not to do, identified in the SANDAS report: July 28, 2023 | Advertiser, The (Adelaide, Australia)
Author/Byline: Agnes Gichuhi | Page: 6 (via NewsBank)
and respect, preventing the unintentional disclosure of sensitive details and avoiding potential negative consequences for individuals seeking assistance for AODrelated concerns.
Journalists should use first-person language and non-stigmatising terms, and avoid sensationalising. They should present balanced views and give a comprehensive picture rather than focusing narrowly and one-dimensionally on AOD. It’s important to clearly identify AOD as a health issue rather than a moral issue, and refrain from alarmist tones and avoid an overfocus on crime related AOD content.
2. Direct training/education for journalists
Arrange for information sessions by AOD experts to discuss stigma towards those with AOD dependence problems. This is especially significant for any future plans of opening AOD support centres in specific

locations. Mandate stronger guidelines that require journalists to provide data, referral to support services, cite sources, and to involve health professionals in any AOD report (similar to guidelines on reporting suicide and mental health issues).
3. Target policy and community leaders, including politicians
Provide training and education to community leaders, including politicians, to ensure that they have the knowledge necessary to speak in a health informed way about AOD issues. Also, provide guidance to policy advisers and community leaders on the risks associated with politicising AOD treatment and support issues in the media. Incorporate media engagement as an essential element of planning AOD treatment and support services implementation.
READ MORE: bit.ly/sandasaod

Harmony Day 2024 at Community Access and Services SA was fun-filled, happy and uplifting.
This year’s theme was ‘Everybody Belongs’. There were the cultural display tables, including Aboriginal craft, but this year, some lucky service organisations, like Hepatitis SA, were invited to have tables as well. We were happily sandwiched between SA Police and our friends from PEACE Relationships Australia.
A disaster was averted when a very helpful CAaSSA worker, Dung, helped to repair our banner which had gone berserk and torn itself. With that drama behind us, we had an enjoyable, fruitful time talking to the streams of adults and kids (on school holidays) who came by, and although we brought publications in seven languages, we still missed some—an indication of the many different cultural communities who turned up.


In his Welcome to Country, Ngarrindjeri-Kaurna cultural awareness promoter Petiola Wilson said, “You come here from another country for a fresh start, but you still bring your culture with you. Aboriginal culture has been taken away from us that’s
why we are where we are in our country. Engagement is how we share our story and through things like this, that’s how we reconnect… it’s important for us to give that sense of belonging to our next generation and that’s what we’re doing here. We say welcome, and thank you for bringing us together.”
Read more online at bit.ly/ saharmony.
Cecilia Lim
Recently two educators from the Hepatitis SA Education team attended the Tarpari Wellbeing Day. This familyfriendly free biennial event for the whole community was held on 17 April at Memorial Park in Port Pirie.
This year’s theme was ‘715 Deadly Unna’ with a focus on increasing the number of people having an Aboriginal Health Check. This event celebrated Aboriginal culture and health, with over 50 agencies from across the state attending who provided information on health and wellbeing.
O’liver also came along for the day, and he was very busy engaging with children and families: lots of selfie shots



were taken, and he even got to hold a snake at the animal stall. At our Hepatitis SA stall, we liaised with well over 100 people, with 78 people taking part in the hepatitis quiz with a chance to win a $50 voucher. If people didn’t know the answers it provided an ideal opportunity to speak about treatments and the hepatitis virus in general. As well as the quiz we had handouts for the younger people, with bubbles and bags of popcorn. It was a marvellous success! Tarpari is a great, well-run community event, and one which we love being part of.
Gary Spence
The Health Expo 2024
Wellness Wonderland was an absolute hit, packed with exciting activities and experiences! Organised by the Australian Refugee Association (ARA), Hepatitis SA joined in the fun as one of the stallholders. The day kicked off with an amazing Aboriginal dance performance, and Rosemary Wanganeen, an awesome griefologist, moved everyone with her story of personal healing. Plus, there were

yoga sessions, henna stations, arts and crafts, and drumming, all well situated for kids and adults alike, ensuring that everyone, regardless of age, could have fun and experience the joy of community and cultural exchange. Additionally, the fair offered a variety of health info stalls—truly something for everyone to explore and enjoy, including Diabetes SA, Relationships Australia, the Department of Health and Aged Care, pharmacy and dental services, SHINE SA, STTARS—and of course, Hepatitis SA was there too, mixing in to thrill the party!
Our awesome educators attended the Health Expo to spread the word about our services and all things related to hepatitis. They brought along some cool stuff too, like recipe books that are good for your liver and super-fun storybooks that make learning about hepatitis a fun and interactive experience. To boost the fun at the Health Expo, we rolled out a quiz with a $50 voucher as the prize. Nineteen visitors officially joined the quiz, eager to freshen up their knowledge about hepatitis C and B. However, we engaged with well over that number at our stall, connecting with many more through our interactive displays and educational materials. Our educators were all



ears, absorbing personal stories and clearing up any confusion, such as when one visitor was unsure about her hepatitis vaccination. Quick on the draw, our education officer explained that while there’s a vaccine for hepatitis B, hepatitis C can be treated with a cure.
But that’s not all—our stall was buzzing with excitement over our adorable, selfdesigned ‘cutie-wootie’ badges. Kids and adults alike were thrilled to pick and wear their favourites, from ‘Kargoo’ to ‘Koala’ to ‘I ♥ My Liver,’ etc. Made right on the spot, these badges were a hit, adding a smile to everyone’s faces. These activities didn’t just educate; they connected us. From quizzes to quick facts, quirky badges, and recipe books, we engaged the community from every angle, making health information not only accessible but also enjoyable. Our stall was more than just a learning hub—it was the heart of the expo, pulsing with caring and love!
The ARA Health Expo was a wonderfully organised event, and we highly recommend other services to participate. We thoroughly enjoyed our time there and are eagerly looking forward to joining again in the future.
Yingbin Xuthose competing for the same funding – need to work together to get decision-makers’ attention, knock on the doors of parliament members or maybe, metaphorically, “just try to burn down something”.
Speakers and delegates from the floor point to the many medical advances in the field in the last 15 years – the increase in drug options for hepatitis B management, immunoglobulin for newborn babies of mothers with hepatitis B, and the “miraculous” direct-acting antivirals for hepatitis C. Despite these clinical tools people continue to die from hepatitis.
Speaking from the floor, Dr Garaba Danjuma, from Taraba, Nigeria, said despite his state’s health authority holding weekly meetings to look at data for HIV, viral hepatitis, TB and Malaria, they “truly don’t give very much attention to viral hepatitis” – something he aims to change going forward.
Delegates online called on supporters/funders of the Summit for help in their home countries and regions. “Those people who support this kind of summit, why didn’t [they do] the same to the civil society to save those lives?” asked one. Another said: “I am also in need for the accessibility of medicines for HBV for the underprivileged population in South India. We do a service but unable to help them in full diagnosis and treatment aspect. Could anyone help us in this?”
One delegate from Nepal, asking speakers to address the “issue of South Asia”, described the hepatitis C treatment there as “a nightmare” due to the high cost. This was echoed by a Burundian delegate who said the issue was the same throughout SubSaharan Africa.
While there was anger, there was also optimism. One delegate from India shared his experience in the HIV movement providing secretarial support to parliamentarians, regularly feeding them information and sensitising them to the issues, recruiting 50
MP champions out of 750 parliamentarians, keeping their issue topical and generating discussions in parliament.
Fungisai Siggns, founder of Hepatitis Zimbabwe, likened everyone in the movement to ingredients in a cake. “Everybody is important so we must work together. We must succeed because people are dying, people are sick.” The speaker from Guatemala, Patricia Velez-Moller said, “we will succeed because we must… Fifteen years ago there was no World Hepatitis Day, ten years ago there was no cure for hepatitis C,” she said pointing to advances in community organisation and medical treatment.
Zipporah Achieng from the National Syndemic Disease Council, Kenya, said she would not wait for governments to move, echoing other voices from the floor urging delegates to keep talking about hepatitis when they return to their work and home countries after the meeting. She said advocates need to keep talking about hepatitis every day, to people who are affected by the disease as well as those not. “Even if I have nothing else, I have my mouth, and I can speak,” she said.
She believes that by 2030, hepatitis will be gone, and she won’t be hearing children say, “I have hepatitis,” as she had to say when she was a child.
Let’s hope governments and funding bodies hear her.


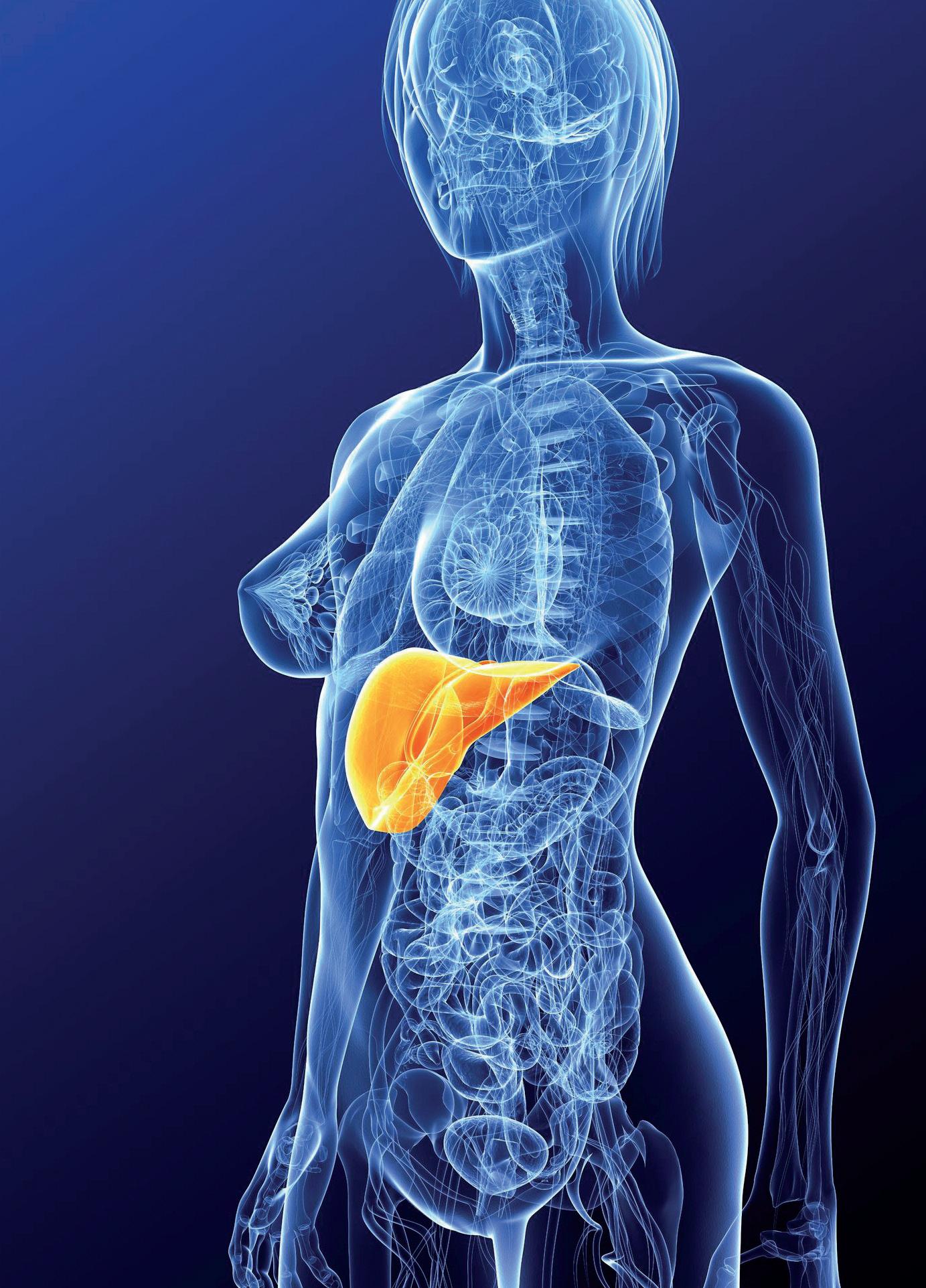
Why are people with hepatitis C three times more likely to develop diabetes?
Most people don’t know of the link between viral hepatitis and diabetes, two chronic conditions common in Australia. Understanding the relationship between these diseases can help in their management and minimise poor outcomes.
The connection between diabetes and hepatitis lies in the liver’s key role in storing glucose in the body. Diabetes is a disease caused by too much glucose in the blood so when the liver’s ability to process and store glucose is impaired, the risk of diabetes increases. Studies have shown that people with chronic hepatitis B and hepatitis C— especially hepatitis C—are at greater risk of developing diabetes. On the other hand, people with diabetes are found to be at greater risk of succumbing to viral hepatitis.
Not surprisingly, the demographic groups with higher rates of these two chronic diseases are similar, so Hepatitis SA and Diabetes SA have come together to look at providing shared education sessions to some of these communities. Topics covered will include the basics of diabetes and hepatitis, how to prevent them, how to manage the conditions if you have them and where to get treatment and support.
According to the Australian Bureau of Statistics, diabetes prevalence in Australia has increased from 3.3% in 2001 to 5.3% in 2022. It is the seventh leading cause of death in Australia. Most people would be aware that there are two types of diabetes: Type 1 and Type 2.
Your pancreas produces insulin which is needed to properly process glucose. Type 1 diabetes develops when your pancreas can’t produce insulin and Type 2 occurs when your pancreas can’t make enough insulin, or your
body is unable to use it properly.
Our body’s glucose is stored in the muscles and liver. Liver disease can lead to a fatty or scarred liver compromising its ability to work properly. This can lead to high blood glucose levels.

developing Type 2 diabetes. Studies have shown that they can be up to three times more likely to develop diabetes than those without hepatitis C. Although liver disease in general is linked to the development of Type 2 diabetes, studies have shown a stronger link with chronic hepatitis C.
The higher rate of diabetes in people with chronic hepatitis C could be due to the fact that they are more likely to develop fatty liver than people with other liver diseases. Additionally, the hepatitis C virus affects not only the liver but other organs as well,
affecting the body’s ability to turn food into energy and get rid of waste. Studies have found hepatitis C virus in the pancreas; this could affect the pancreas’ ability to produce insulin.
consistent as it is for chronic hepatitis C, some studies have found a higher rate of diabetes among individuals with hepatitis B compared to the general population. This could be due to damage to liver cells caused by the hepatitis B virus. One of the liver’s important roles is maintaining normal glucose levels in the bloodstream; that function could be impaired when liver cells are damaged. Interestingly, another study has found that those who have been successfully vaccinated against hepatitis B were less likely to develop diabetes compared to those who have not received the vaccine, with the risk of diabetes onset reduced by up to 33%.
Studies have also shown that pregnant women with hepatitis B have a higher risk of developing gestational diabetes which may cause complications at birth.
Coming from the other direction, studies have found that the risk of hepatitis B or hepatitis C infection was higher in people with diabetes than in those without. One study found that people with diabetes are 1.7 times more likely to have chronic hepatitis C than people without diabetes.
The association between lower income and diabetes is similar to the association between poverty and chronic hepatitis C. People with diabetes are at increased risk for blood-borne infections if they don’t have their own diabetes-care equipment such as syringes, insulin pens, blood glucose meters and finger-stick devices and need to share them with others. Blood contaminants on the equipment, plus the more frequent use of injecting equipment in some cohorts could exacerbate the risk of contracting hepatitis C. Hepatitis B can be prevented with an effective vaccine and health agencies often recommend hepatitis B vaccination for people with diabetes who don’t already have hepatitis B immunity.
Hepatitis C can be cured with tablets in eight or twelve weeks and, in Australia, is covered by Medicare. Hepatitis SA recommends that people with diabetes consider testing for hepatitis C and going on treatment should the test show they have the virus.
Although there is no cure for diabetes, regular monitoring and lifestyle changes can help you stay healthy and avoid bad health outcomes.
Cecilia LimREAD MORE:
Diabetes SA: diabetessa.com.au, or phone 1300 198 204
References: bit.ly/hepdiabetesrefs
Being aware of the functions of the liver, and the effects of liver disease, may help to encourage more healthy behaviours. Likewise having reliable information about hepatitis means less time spent on trying to sort the facts from the misconceptions – especially around transmission (and there are many misconceptions out there!)
LiverHealth
A great place to start: covers subjects that you might want to be familiar with if you have any form of liver disease, with topics such as: bile, sleep, liver transplantation, iron deficiency or overload, herbs and supplements, hepatitis, cirrhosis etc. Presented by 3 liver doctors (hepatologists) in a series of accessible and easy to listen to podcasts. apple.co/4aX9BQu

5
This series of ‘mythbusters’ covers many of the misconceptions about hepatitis B and C. Presented in a series of 5 myths each time they cover statements such as breastfeeding, pregnancy, sharing clothes/food/intimacy, drinking etc. Brief, practical information for personal use - or to pass on to family and friends. hepsa.asn.au/hep-myths

If you have been diagnosed with hepatitis you’ll be facing more contact with health and other services. This can be dauntingbut with preparation and some extra knowledge you can make the best of your time spent with doctors, nurses etc. The following resources can assist in planning for appointments or tests, and in managing medications.
The role of a GP
HealthDirect, Aust. Govt. Dept. of Health and Aged Care, Canberra,2022. 2p. plus video. Particularly useful for those who are new to the Australian health system: explains what a General Practitioner is, what they can do, how to find a GP, things to consider when choosing one for yourself or your family, access to interpreters if needed, and costs. Available in Arabic, Bengali, Chinese, English and Vietnamese. bit.ly/gprole

Question builder
HealthDirect, Aust. Govt. Dept. of Health and Aged Care, Canberra, 2017. Interactive webpages.
A really useful tool with lists of questions relevant for GP or specialist visits. It covers symptoms, tests, treatment, medications (and side effects), self management, support and follow up. Once the most relevant questions have been selected the list can be printed to take to the next appointment.
bit.ly/qbuild

What you need to know about telehealth for hep (B or C)
Hepatitis NSW, Sydney, 2022. 3p.
Information about eligibility, the benefits, how to book an appointment, additional services (such as Aboriginal Liaison or interpreters), what to expect,
blood tests (and availability of Dried Blood Spot home testing), and follow up appointment information.
bit.ly/telehepc
bit.ly/telehepb

Worried about getting a blood test? 5 tips to make them easier (and still accurate)
The Conversation, Melbourne/ Sydney, 2023. 4p.
Discusses the different ways of preparing for a variety of blood tests, how the test is carried out, tips for improving the experience, and what may happen after the test.
bit.ly/bloodtesttips

Tips for managing medications:
Hepatitis SA, Adelaide, 2017. 4p. wallet sized booklet
This handy wallet sized booklet contains tips for helping you remember your medicines and includes a 12 week check-off chart and links to adherence tools including smartphone apps. Read only online – contact admin@hepsa.asn.au for free hard copies.
bit.ly/adherecard

Side effects from your medicines? 5 questions to ask NPS Medicine Wise, Sydney, 2021. 2p. factsheet.
5 questions to ask your GP if you are experiencing any symptoms, even if they’re mild. If it’s caused by your medicines, they can suggest ways to manage or decrease side effects. Available in 13 languages.
bit.ly/sidetrans image 8

There are many more resources in our online library to assist you to with health appointments and any treatments you may need to undertake. Just go to the library home page (hepatitissa. asn.au/library) click on the green ‘search catalogue’ button, then click on any of the relevant headings in the Australian Community Resources list. For more information or assistance with accessing any of these resources please contact us (admin@hepsa.asn.au)

Hepatitis SA provides free information and education on viral hepatitis, and support to people living with viral hepatitis.
Postal Address:
Kaurna Country PO Box 782
Kent Town 5071
(08) 8362 8443 1800 437 222
www.hepsa.asn.au
Community News: hepsa.asn.au/ communitynews
Library: hepsa.asn.au/library


@HepatitisSA
@hep_sa
Resources: issuu.com/hepccsa
Email: admin@hepatitissa.asn.au
hepatitis A, B and C information, confidential and non-judgemental
referrals and printed
We can help. Talk to us. Call or web chat 9am–5pm, Mon–Fri
HEPATITIS SA BOARD
Chair
Arieta Papadelos
Vice Chair
Bill Gaston
Secretary
Sharon Eves
Treasurer
Michael Larkin
Ordinary Members
Lindy Brinkworth
Bernie McGinnes
Janice Scott
Lucy Ralton
Joshua Riessen
Kerry Paterson (CEO)








Hepatitis SA has a wide range of hepatitis B and hepatitis C publications which are distributed free of charge to anyone in South Australia.
To browse our collection and place your orders, go to hepsa.asn.au/orders or scan the QR code below:

Viral Hepatitis Nurses are nurse consultants who work with patients in the community, general practice or hospital setting. They provide a link between public hospital specialist services and general practice, and give specialised support to general practitioners (GPs) to assist in the management of patients with hepatitis B or hepatitis C. With advanced knowledge and skills in testing, management, and treatment of viral hepatitis, they assist with the management of patients on antiviral medications and work in shared care arrangements with GPs who are experienced in prescribing medications for hepatitis C or accredited to prescribe section 100 medications for hepatitis B. They can be contacted directly by patients or their GPs:
CENTRAL ADELAIDE LOCAL HEALTH NETWORK
Queen Elizabeth Hospital
Phone: 0423 782 415, 0466 851 759 or 0401 717 953
Royal Adelaide Hospital
Phone: 0401 125 361 or (08) 7074 2194
NORTHERN ADELAIDE LOCAL HEALTH NETWORK
Phone: 0401 717 971 or 0413 285 476
SOUTHERN ADELAIDE LOCAL HEALTH NETWORK
Phone: 0466 777 876 or 0466 777 873
Office: (08) 8204 6324
Subsidised treatment for hepatitis B and C are provided by specialists at the major hospitals. You will need a referral from your GP. However, you can call the hospitals and speak to the nurses to get information about treatment and what you need for your referral.
• Flinders Medical Centre Gastroenterology & Hepatology Unit: call 8204 6324
• Queen Elizabeth Hospital: call 8222 6000 and ask to speak a viral hepatitis nurse
• Royal Adelaide Hospital Viral Hepatitis Unit: call Anton on 0401 125 361
• Lyell McEwin Hospital: call Bin on 0401 717 971
Visit hepsa.asn.au - no need to log in, lots of info & pdates
Follo the HepSAY blog - hepsa.asn.a /blog
Order print resources - hepsa.asn.a /orders/ Follo s on T i er @hep_sa or Facebook @Hepa sSA

Full range of syringes and needles. Water and filters also available in limited quantities for free.
Feel safer around blood, and better able to assist patients living with viral hepatitis.
Session includes:
Overview of hepatitis A, B & C (some HIV info)
Overview of testing and treatment
Transmission risks & myths
Best practice after blood exposure
Post-Exposure Prophylaxis
Available services

bookings via https://www.trybooking.com/CRLCC or the
