KNOW THE FACTS:
PRIVATIZATION:













KNOW THE FACTS:
PRIVATIZATION:

Privatizing health care will inevitably pull experienced nurses and healthcare professionals away from the public system, making a desperate staffing shortage even worse.







What is Doug Ford thinking?




















Anew survey by Compare the Market has asked over 3,000 adults across Australia, the USA and Canada what their biggest health concerns are, and the results are reasonably consistent across the board.
A clear leading concern across Australia, the USA and Canada was a potential cancer diagnosis. In the USA, as many as 41.6 per cent of respondents listed it as a concern, followed by 39.4 per cent expressing the same worry over the risk of someone they care about being diagnosed with cancer.
Canadians responded with a similar breakdown. The number one health concern in Canada was the risk of a loved one falling ill with a serious disease, at 45.7 per cent, and the risk of being diagnosed with cancer at 44.4 per cent, followed by concern for a loved one receiving a cancer diagnosis as the third biggest issue for 44.1 per cent of respondents.
It was slightly different for Australians, where the risk of a loved one getting a serious disease was the number one issue, according to 49.2 per cent of respondents, followed by a loved one’s cancer diagnosis at 48.5 per cent. A personal cancer diagnosis was the third-biggest medical concern, as noted by 48.1 per cent of Australians surveyed.
On the other hand, the issue of least concern for Australians and Canadians was not being able to afford nec-
AUGUST 2023 ISSUE
EDITORIAL: July 6
ADVERTISING:
Display – July 21 | Material – July 25
Monthly Focus:
Paediatrics/Ambulatory Care/Neurology/ Hospital-based Social Work: Paediatric programs and developments in the treatment of paediatric disorders including autism. Specialized programs offered on an outpatient basis. Developments in the treatment of neurodegenerative disorders (Alzheimer’s, Parkinson’s etc.), traumatic brain injury and tumours. Social work programs helping patients and families address the impact of illness.
essary healthcare. In the USA, it was long waiting lists for an appointment or surgery.*
Compare the Market’s survey also revealed that most people first turn to a doctor or General Practitioner (GP) when they have concerns or experience symptoms, but family and online search engines like Google are a close second and third resource across all three countries.
However, not everyone who has an issue actually plans to consult a doctor about it at all. In Australia, more than one-third of respondents (33.4 per cent) said they hadn’t been to the doctor for a medical concern and never planned to, compared to 25.5 per cent of Americans and 27.2 per cent of Canadians.
More than half of all those surveyed hadn’t yet been to the doctor, and the amount who were planning to see a doctor was very close to the amount who didn’t plan to do so, as shown in the table below.
They survey also asked respondents, “If you were admitted into hospital for a significant injury or illness, how long could you afford to stay, based on out-ofpocket costs?”
Canadians had the highest proportion who said they could stay as long as they needed to (29.3 per cent). Interestingly – despite a largely derided healthcare system –more Americans said they could go as long as they needed to than Australians, though only just (22.2 per cent of Americans as opposed to 21.6 per cent of Australians).
Continued on page 6
EDITORIAL: August 10
ADVERTISING:
Display – August 25 | Material – August 29
Monthly Focus:
Emergency Services/Critical Care/Trauma/ Emergency/Online Education: Innovations in emergency and trauma delivery systems. Emergency preparedness issues facing hospitals and how they are addressing them. Advances in critical care medicine.
+ ONLINE EDUCATION SUPPLEMENT + SPECIAL FOCUS: EMERGENCY ROOM
610 Applewood Crescent, Suite 401 Vaughan Ontario L4K 0E3 TEL. 905.532.2600|FAX 1.888.546.6189 www.hospitalnews.com
Editor Kristie Jones editor@hospitalnews.com
Advertising Representatives
Denise Hodgson denise@hospitalnews.com
Publisher Stefan Dreesen stefan@hospitalnews.com
Accounting Inquiries accountingteam@mediaclassified.ca Circulation Inquiries info@hospitalnews.com
Director of Print Media

Lauren Reid-Sachs
Barb Mildon, RN, PHD, CHE VP Professional Practice & Research & CNE, Ontario Shores Centre for Mental Health Sciences
Helen Reilly, Publicist Health-Care Communications
Bobbi Greenberg, Health care communications
Sarah Quadri Magnotta, Health care communications
Dr. Cory Ross, B.A., MS.C., DC, CSM (OXON), MBA, CHE Vice President, Academic George Brown College, Toronto, ON
ASSOCIATE PARTNERS:
Hospital News is published for hospital health-care professionals, patients, visitors and students. It is available free of charge from distribution racks in hospitals in Ontario. Bulk subscriptions are available for hospitals outside Ontario.
The statements, opinions and viewpoints made or expressed by the writers do not necessarily represent the opinions and views of Hospital News, or the publishers.
Hospital News and Members of the Advisory Board assume no responsibility or liability for claims, statements, opinions or views, written or reported by its contributing writers, including product or service information that is advertised.
Changes of address, notices, subscriptions orders and undeliverable address notifications. Subscription rate in Canada for single copies is $29.40 per year. Send enquiries to: subscriptions@ hospitalnews.com
THANKS TO OUR ADVERTISERS Hospital News is provided at no cost in hospitals. When you visit our advertisers, please mention you saw their ads in Hospital News.
Canadian Publications mail sales product agreement number 42578518.

Sunnybrook Health Sciences Centre’s Tory Trauma Program has joined an elite class of trauma centres. After a journey that began in 2019, the Program has been officially verified (accredited) as a Level 1 trauma centre by the American College of Surgeons (ACS), and also earned the honour of becoming the first hospital outside of the United States to achieve this mark of excellence.
“We are thrilled to be the first ACS-verified Level 1 trauma centre outside of the U.S.,” says Dr. Avery Nathens, Surgeon-in-Chief, Sunnybrook. “The standards put forth by the ACS reflect expectations required to deliver the highest quality of trauma care and our success reflects Sunnybrook’s outstanding ability to care for trauma patients, as well as our dedication to the highest quality of care, research, prevention, and leadership across the trauma system.”
Obtaining trauma centre Level 1 verification by the ACS is a demanding and rigorous process rooted in 350 evidence-based standards that must be met. Sunnybrook had to demonstrate excellence in all aspects of trauma care, with an emphasis on patient safety, quality, performance improvement, research and education.
“I could not be more proud of Team Sunnybrook in this moment,” says Andy Smith, President & CEO, Sunnybrook. “This is a historic achievement in the Canadian trauma community and highlights our role not only as a strong leader in Ontario’s Trauma and Critical Care system, but in Canada. Our pursuit of ACS verification has undoubtedly made Sunnybrook’s trauma care better than ever and that is a standard our patients and province can rely on in their time of need.”
As an ACS-verified Level 1 trauma centre, Sunnybrook has proven it provides trauma care for every aspect of injury – from prevention through rehabilitation.
The reviewers highlighted many strengths in their report, and at the core of them all were the individuals and high performing teams that make Sunnybrook the amazing trauma centre it is. Sunnybrook acknowledges and is grateful for the philanthropic support that has played an important role in the continued achievement and advancement of the Tory Trauma Program.
“This achievement could not have been accomplished without intense collaboration across Sunnybrook and with our external partners, including Ornge and our local paramedic services,” says Corey Freedman, Manager, Trauma Services. “Trauma care
touches almost every aspect of the Hospital, and this honour is shared with everyone who worked so hard to make this verification happen.”
Sunnybrook is the largest trauma centre in Canada. It opened in 1976 and over the years, the need for care
has grown. The Level 1 ACS verification validates its progress and achievements over the years, and also equips the Hospital to meet the challenges of the future while continuing to be there for patients today, when it matters most. ■ H

OBTAINING TRAUMA CENTRE LEVEL 1 VERIFICATION BY THE ACS IS A DEMANDING AND RIGOROUS PROCESS ROOTED IN 350 EVIDENCE-BASED STANDARDS THAT MUST BE MET.
Pandemic restrictions corresponded with a significant drop in diagnoses of breast, colorectal and prostate cancers as well as melanoma, according to a new Alberta study published in CMAJ (Canadian Medical Association Journal).
“The sweeping and unprecedented measures enacted at the beginning of the COVID-19 pandemic in Alberta had an inevitable impact on cancer care,” writes Dr. Darren Brenner, an epidemiologist in Calgary, Alberta, and associate professor at the University of Calgary’s Cumming School of Medicine, with coauthors. “Even though treatment and urgent surgeries for cancers were prioritized when other procedures were delayed or cancelled, preventive and diagnostic services were greatly reduced.”
The study compared survival rates for 3 groups of patients diagnosed between (1) Jan. 16, 2018, and Mar. 15, 2019; (2) Mar. 16, 2019, and Mar. 15, 2020; and (3) Mar. 16 and Dec. 15, 2020. The researchers divided the
Continued from page 4
third period into a “state of emergency” (SOE) phase (Mar. 16 to June 15, 2020) and post-SOE phase (June 16 to Dec. 15, 2020).
Researchers saw large reductions in the number of new diagnoses for some cancer types during the SOE period, with a drop of 43 per cent (melanoma), 36 per cent (colorectal and prostate) and 33 per cent (breast). In the postSOE phase, diagnoses increased nine per cent, eight per cent and 10 per cent per month, respectively. Other cancers, such as bladder, kidney, lung and cervical, did not show decreases in diagnoses during that period.
“Our findings that early-stage breast and colorectal cancer had the largest decrease in diagnoses suggest that a reduction in screening services during the first wave of pandemic-related restrictions in Alberta resulted in asymptomatic individuals receiving a diagnosis later than they would have otherwise,” write the authors. “These results highlight the importance of screening services in reducing latestage cancer diagnoses.”
As for those who said they couldn’t afford even one night in hospital, Americans had the highest proportion at 15.4 per cent, compared to 11.9 per cent of Canadians and 11.5 per cent of Australians.
When it comes to a family history of health issues, almost half of Canadian respondents said their health concern runs in the family (45.9 per cent), with American respondents not far behind at 44 per cent.
On the other hand, Australians who have a medical concern are less likely to have a family history of it. Only 38.3 per cent of Australians said their family history included their specific health concerns, while 51.6 per cent said there was no family history.
Compare the Market’s Head of Health Insurance, Lana Hambilton, notes that with the top concerns of-
ten being about loved ones receiving a cancer diagnosis or serious illness, it’s not surprising that a family history is front of people’s minds.
“Just under half of all respondents in our survey said their health concerns run in the family,” says Ms Hambilton.
“We do know that a family history of cancer or certain illnesses can mean future generations could be more at risk. It could be prudent to talk to your family members or healthcare professional about any family history so you can be better prepared.”
For additional data, graphs, tables and information on this story, visit: https://www.comparethemarket.com. au/health-insurance/features/biggest-health-concerns. ■ H *This excludes “none of the above” answers.
Patients with colorectal cancer and non-Hodgkin lymphoma diagnosed during the pandemic period in 2020 had poorer one-year survival than those diagnosed in 2018.
By December 2020, the rate of diagnoses had returned to a level more in line with pre-SOE levels.
The findings are consistent with studies from the United Kingdom, United States, the Netherlands, Germany, Japan and other parts of Canada. In Ontario, there was a 34 per
cent drop in new cancer diagnoses in April 2020, and Manitoba had a 23 per cent reduction in the same period. An estimated 15 per cent reduction in Quebec occurred in the first year of the pandemic.
Cancer care must become more efficient and increase capacity to reduce long-term effects of the pandemic on cancer outcomes, the authors conclude.
“Impact of the COVID-19 pandemic on cancer diagnoses, stage and survival in Alberta” was published June 12, 2023. ■ H
To address health inequities that Indigenous and racialized patients can experience, collect data on racial and Indigenous identity at health card application and renewal, suggests a group of authors in CMAJ (Canadian Medical Association Journal)
“Although race is a social construct that uses perceived physical differences to create and maintain power differentials and the existence of discrete racial groups has not been shown to have any biological basis, perceived race influences how people are treated by individuals and institutions,” wrote Dr. Andrew Pinto, founder of Upstream Lab based at MAP Centre for Urban Health Solutions, part of Unity Health Toronto hospital network, along with coauthors.
Indigenous and Black patients have less access to health care, receive poorer care and have worse outcomes.
“Having data on race available for analysis can facilitate the measurement of racial inequities in health care, help to hold organizations and governments accountable for addressing these inequities and monitor progress,” the authors wrote.
Collecting self-reported identity data on health card applications and renewals could be an efficient way to obtain this information, with the caveat to plan for and prevent potential
harms of collection. The authors suggest the following:
• Asking about race and Indigenous identity in a safe and transparent manner
• Guarding against potential bias or race corrections by providing antiracism training
• Ensuring that race or Indigenous identity is not visible on health cards
• Ensuring that data are not interpreted or presented in a way that reinforces racism and discrimination
• Legislating laws that protect communities so that health data are not used to draw broad conclusions about communities
• Supporting Indigenous, Black and racialized communities to lead data collection and analysis with data sovereignty and governance frameworks
“Racism in Canada’s health care systems continues to lead to injustice, but data that would assist in tracking progress and ensuring accountability are lacking or inadequate. Near-universal race and Indigenous identity data could be collected efficiently at health card application and renewal across Canadian jurisdictions,” the authors conclude.
“Considerations for collecting data on race and Indigenous identity during health card renewal across Canadian jurisdictions” was published June 26, 2023. ■ H
The first national study of its kind to probe the impact of COVID-19 and COVID-19 mRNA vaccines on the heart has received a $2M boost from the Public Health Agency of Canada (PHAC) to expand and extend patient follow-up, and to do cardiac imaging on those affected. MYCOVACC (Canadian Cardiovascular Society National Active Surveillance Study of MYocarditis and/or Pericarditis following mRNA COVID-19 VACCination) will receive an additional two years of funding, bringing the total investment in this important initiative to $3.6M over three years. Led by cardiologist Dr. Nathaniel Hawkins of the University of British Columbia, MYCOVACC began in October 2022 in response to reports of rare cases of myocarditis (inflammation of the heart muscle) and pericarditis (inflammation of the lining surrounding the heart muscle) following mRNA vaccines and COVID-19 infection.
“The pan-Canadian study, which involves the leading experts from cardiac care centres across the country, is working to determine if people who experience these rare heart conditions are at increased risk of future health problems,” Dr. Hawkins explains. While most people make a full recovery after myocarditis and pericarditis, long-term outcomes warrant further investigation. The MYCOVACC team will provide valuable insights for clinicians, public health agencies and decision-makers to inform future vaccine programs. Adults and children who take part in the study will be assessed at intervals and then annually for up to three years by a participating specialist using a clinical protocol. They will also be asked to complete quality of life, mental health, physical activity, and health outcome questionnaires. The new funding allows for:
• continued expansion of the existing study and extended follow-up of enrolled patients;
Updated guidance published in CMAJ (Canadian Medical Association Journal) will help clinicians navigate the challenges in supporting patients who choose organ and tissue donation after medical assistance in dying (MAiD).
In 2019, a Canadian Blood Services guideline on organ donation after MAiD was published in CMAJ but the introduction of the federal Bill C 7 in March 2021 has necessitated an update.
The updated guideline includes 8 new and 2 updated recommendations in addition to the original recommendations, many of which are still current. It applies to conscious, competent patients, including those whose natural death is not reasonably foreseeable (Track 2 patients),
a new category now eligible from Bill C 7.
Recommendations focus on referral to organ donation organizations, consent, directed and conditional donation, education and training for physicians involved in organ donation, and reporting.
“The purpose of this updated guidance is to continue to inform the development of policies and practices of donation after MAiD,” writes Dr. Kim Wiebe, Shared Health Manitoba, Winnipeg, Manitoba, with coauthors. “This will help clinicians navigate the medical, legal and ethical challenges that arise when they support patients pursuing donation after MAiD.
“Deceased organ and tissue donation after medical assistance in dying: 2023 updated guidance for policy” was published June 26, 2023. ■ H
• a new project using cardiac MRI to investigate recovery of the heart;
• extended follow-up of patients with COVID-19 associated myocarditis and/or pericarditis; and,
• a study to explore reporting of adverse events following immunization to inform development of new tools.
The CCS is bringing together researchers, research networks, patients, and public health authorities from across the country to undertake the project. The Canadian Congenital and Pediatric Cardiology Research Network (CCPCRN) recently joined the MYCOVACC team to ensure strong representation of pediatric hospitals in the study.
Dr. Frédéric Dallaire, scientific director of CCPCRN, says: “We are working hard in involving a broad national representation of pediatric cardiology specialists to ensure that a majority of children and adolescents affected by this rare condition are identified, even those with the mildest forms of the disease.”
This new investment will help support public trust in vaccine safety and increase confidence in COVID-19 vaccines, especially among young people and their parents. A good understanding of what happens to those who experience rare cases of myocarditis and/or pericarditis after an mRNA COVID-19 vaccine will inform discussions with Canadians of all ages about vaccination. ■ H
Overcrowded and understaffed emergency departments are in crisis across Canada, and all levels of the health system must take immediate action to address this urgent issue, argues an editorial in CMAJ (Canadian Medical Association Journal).
Hospital staffing shortages and related bed closures, combined with high patient volumes and years of inaction to address problems, are stressing hospitals and health care workers.
“For physicians and nurses working in emergency departments in Canada, no end is in sight for growing patient volumes and crowding, and the demand for emergency care exceeds the capacity of emergency medicine health human resources in all regions of Canada, now and for the foreseeable future,” writes Dr. Catherine Varner, deputy editor, CMAJ, who is an emergency physician in Toronto, Ontario.
“This perpetual cycle is not news to most people in Canada, as it is pervasive, has lethal consequences and will continue to exhaust Canadian emergency services and providers,” she writes.
Although some attempts have been made to ease the pressure, such as virtual supports and coaching for rural and remote health care workers in British Columbia and Ontario, these measures are not enough.
“These attempts, while laudable, fall short of the necessary, system-wide response to the current crisis, which has been decades in the making and was predicted by emergency personnel and accelerated by the pandemic,” states Dr. Varner.
She urges immediate action to ensure access to care for patients, to build capacity for emergency services to offer care during external disasters, and to protect health care workers who bear the brunt of the burden of caring for extended high volumes of patients in the post-pandemic period. ■ H
No end to overwhelmed emergency departments
Patients who require diagnostic testing for unknown entities, such as growths, in and around the heart can now opt for a minimally invasive outpatient procedure, rather than open-heart surgery, thanks to innovation from UHN.
UHN’s Peter Munk Cardiac Centre is the only centre in Canada, and one of the few in the world, to offer this new outpatient testing procedure, which is dramatically reducing the hospital stay and recovery time for some patients.
Doctors depend on tumour biopsies to diagnose and determine appropriate treatment. Tissue samples from the heart are extremely difficult to retrieve and can have potentially life-threatening complications due to the continuous motion of the heart.
“There aren’t a lot of options for patients who need a cardiac or pericardial (the sac that surrounds the heart) biopsy,” explains Dr. Patrik Rogalla, Division Head, Cardiovascular and Thoracic Imaging, Joint Department of Medical Imaging, UHN.

“Up until recently, the only option for these patients was open-heart surgery. Whether the entity is malignant or benign, you’re putting the patient through a very invasive procedure (an operation), simply to determine their diagnosis.”
Dr. Robert Cusimano, a cardiac surgeon and cardiac tumour specialist at Peter Munk Cardiac Centre, sees some of the most complex cardiac cases in the country. Patients who are found to have cardiac or pericardial tumours are likely referred to Dr. Cusimano.
To better serve these patients, Dr. Rogalla and his team developed a new procedure to biopsy masses in and around the heart.
The procedure involves manually synchronizing a computerized tomography (CT) scan and fluoroscopy with the electrocardiogram (ECG) to safely
collect the sample. The synchronization device was supported by UHN biomedical engineer Ali Ursani.
The average cost of undergoing surgery to biopsy the heart is approximately $6,725. Recovery time is variable, depending on the location of the abnormal tissues and the magnitude of the operation required to collect a sample.
The average hospital stay for this type of procedure is seven days, including a day-and-a-half in the intensive care unit.
By contrast, this new testing procedure takes an average of 32 minutes. Patients typically leave the hospital following a two-hour recovery in the medical imaging day unit.
“The benefits of this form of minimally invasive cardiac or pericardi-
al biopsy are significant,” says Dr. Cusimano. “It spares the patient from surgery, which has obvious benefits.
“So if the mass is benign, the patient was spared an operation. If it’s not, treatments can be coordinated and planned without having to wait for healing to occur, saving time that may be important both for undergoing treatments sooner and for making any subsequent treatments or operations potentially safer.”
Earlier this year, Susan Bell was referred to Dr. Cusimano when doctors found a tumour on her heart. Susan was asymptomatic and had never undergone major surgery. Thanks to the pioneering efforts of Dr. Rogalla, Susan was able to avoid open-heart surgery for what turned out to be a benign tumour.
“It was very efficient,” says Susan. “It’s still hard to believe they took a sample from my heart.
“I don’t even remember the needle. There were no stitches, no scar – and I went home the same day. It’s a phenomenal procedure.” ■ H
Leading-edge research by Hamilton Health Sciences’ (HHS) Dr. Jason Roberts has the potential to revolutionize care for patients impacted by arrhythmogenic right ventricular cardiomyopathy (ARVC), a potentially fatal genetic condition affecting the heart’s muscle tissue.
As an HHS cardiac electrophysiologist, Roberts specializes in treating cardiac problems involving electrical activity and arrhythmia.
Roberts was one of four researchers honoured at the 2023 Hamilton Health Sciences Foundation Gala last month celebrating research and innovation at HHS. Each of the recipients –which also included Drs. Peter Gross, Guillaume Paré and Mark Tarnop-
olsky – received a $40,000 grant to take their innovative commercialization research projects to the next level.
Arrhythmogenic right ventricular cardiomyopathy often presents itself in young adults in their late teens to early 20s. It can cause dangerously fast heartbeats that can result in fainting and even sudden death, especially in
young athletes since exercise worsens the condition.
Currently, the standard treatment to prevent sudden death is to insert an implantable cardiac defibrillator into the heart, which can deliver shocks when these dangerously fast heartbeats occur. These shocks can be quite frequent and painful, plus they don’t prevent damage to muscle tissue caused by the disease.
Continued on page 12
“IF THERE WAS A DRUG THAT COULD PREVENT THE ONSET OF ARVC, THEN PATIENTS MAY NOT NEED THE IMPLANTABLE CARDIAC DEFIBRILLATOR.”
•In patients with VLUs and DFUs, PICO sNPWT significantly reduced wound area, depth and volume, with more frequent closure at 12-weeks than tNPWT.2


•IODOSORB Gel has reduced biofilm numbers in patients with diabetic foot ulcer.3










•ACTICOAT Dressings, used early in infection management, may help minimise progression to systemic infection.4








•Our advanced wound management solutions help manage tissue, treat infection, control exudate and close the wound edge to reduce the human and economic cost of diabetes.














When Buffalo Bills player Damar Hamlin fell to the ground after a tackle during an NFL football game, it seemed inconceivable that the athletic 24-year-old suffered a cardiac arrest. Hamlin is one of around 400,000 North Americans affected by cardiac arrests that happen outside of a hospital setting each year. While Hamlin later received treatment for his condition and recovered, too many others do not survive.
“In BC, we previously had little information about how pre- and in-hospital factors affect the long-term survival of patients, as well as whether they are readmitted to hospital or access health care services, such as residential or home care,” says Vancouver Coastal Health Research Institute researcher Dr. Christopher Fordyce.
Fordyce’s recent study, published in the Canadian Journal of Cardiology, is the first to provide longitudinal information on the complete journey of cardiac arrest patients.
Also known as sudden cardiac arrest, the condition occurs when a person’s heart stops beating, causing a loss of blood flow to the brain and other organs. This emergency situation requires immediate medical attention.
In British Columbia, the survival rate of cardiac arrest to hospital discharge is only 15 per cent. However, Fordyce’s research is helping to explain how actions taken before and after a patient is admitted to hospital can have a lasting impact on their short- and long-term health and survival.
Fordyce and his team drew from the BC Cardiac Arrest Registry, which accounts for around 75 to 80 per cent of patients treated at major health care centres in the province between 2009 and 2016, including detailed information on pre-hospital patient care and patient survival outcomes.
They combined this data with administrative data from other medical sources in collaboration with Population Data BC to create a randomized registry that can be applied to future studies.
Fordyce’ study included 10,188 adult out-of-hospital cardiac arrest patients, 3,230 (31.7 per cent) of whom survived to hospital admission and 1,325 (13 per cent) of whom survived to hospital discharge.
Notably, Fordyce and his team found that the sooner cardiopulmonary resuscitation (CPR) was provided to a cardiac arrest patient by a bystander, family member, friend or paramedic, the better the long-term patient outcomes. CPR involves providing chest compressions and ventilation to a person through their airways.
“Every minute makes a difference,” says Fordyce. “In the prehospital setting, we found that someone who received CPR from a bystander or paramedic following their cardiac arrest was around 35 to 40 per cent more likely to survive even three years after being discharged from hospital than someone who did not.”
“This research enabled us to make linkages in care provision and outcomes that were not possible beforehand.”
Hospital readmission and death within three years were also significantly reduced when one of two in-hospital procedures were given to patients. Those who received either revascularization – a procedure used to widen coronary arteries to increase blood flow through the heart – or an implantable cardioverter-defibrillator – a device that regulates heartbeats – had around a 50 per cent less chance of death three years after their cardiac arrest.
Fordyce and his team also found that only one in four patients who left the hospital required residential or home care within a year after hospital discharge.

“This is good news,” says Fordyce. “It means that 75 per cent of people who leave hospital are likely doing well enough that they do not require post-hospital home care, implying generally good functional outcomes if patients can survive to hospital discharge.”
The results from Fordyce’s study are only a starting point, he notes. “With this information, we can begin to inform efforts to improve care processes and increase survival to hospital discharge.”
The process the team used to create the linked cardiac arrest registry has potential to be implemented in the study of other diseases, as well.
“We have shown that it is possible to generate valuable research from our methods,” says Fordyce. “The dream now is to fund the uploading of data to a registry like this in a timely fashion and on an ongoing basis to conduct further research and to continuously improve patient care.”
For more information on cardiac arrest care and research, visit bcresurect. med.ubc.ca. ■ H

Combined patient information is helping connect
dots
improve survival rates even three years after a cardiac arrest






The United Brotherhood of Carpenters’ Infection Control Risk Assessment (ICRA) training teaches healthcare construction protocols that save lives.

Our training educates Healthcare Personnel, Construction Professionals and Architects in ICRA best practices that protect patients by working safely during all phases of healthcare facility renovations.
Contaminants released during renovation projects can lead to deadly healthcare associated infections. This is why it’s critical for anyone working in a healthcare facility during renovation to have participated in ICRA Training.

With the UBC ICRA training, you’ll learn necessary safeguards to protect your patients from health hazards during construction.
1 in 25 hospital patients has at least one healthcare associated infection at any given moment
1.7 million patients suffer from healthcare associated infections every year nationwide

100,000 deaths resulting from healthcare associated infection occur each year
As a result, people with ARVC must limit physical activity, which can cause other health issues, especially as they age. Through their research, Roberts and his team at the Population Health Research Institute of HHS and McMaster University, are working to find a more effective treatment option.
“For those who have one of the genes that cause ARVC, it doesn’t mean this condition has to develop,” says Roberts. “If there was a drug that could prevent the onset of ARVC, then patients may not need the implantable cardiac defibrillator.”
Research involving Roberts’s team has found that a small molecule called tideglusib was successful at preventing dangerously fast heartbeats and heart muscle damage caused by ARVC in mice. This molecule has already been developed into a drug for another purpose. While it turned out not to be effective for that purpose, it was proven
to be safe for human use and is now being tested for treating muscle disorders in people. Roberts saw the opportunity to try this drug for ARVC patients.
“ARVC affects muscle tissue in the heart, and this drug is already suspected to help with muscle disorders,” he says. “Since our team has found that the tideglusib molecule prevented ARVC in mice, it now makes sense to see if this drug can prevent ARVC in people.”
Thanks to funding from Hamilton Health Sciences Foundation and Canadian Institutes of Health Research, Roberts and his team are conducting a clinical trial with this drug.

The trial is set to begin later this year and will include 120 patients from 15 sites across Canada, including HHS. Since there are multiple genes that can cause ARVC, the trial will focus on individuals that have one of
six possible genes, including one that has been labelled the “Newfoundland curse” – a gene discovered by researchers in Newfoundland that was responsible for the sudden death of seemingly healthy young adults within multiple generations of families.
“Targeted therapies that are able to directly address the abnormalities that
arise from disease-causing genetic mutations are becoming more common in the medical field and, in many instances, have been shown to be dramatically effective,” says Roberts. “We’re hopeful that our clinical trial will show that our treatment works for all genetic subtypes of ARVC, including the Newfoundland curse.” ■ H
Anew study led by a St. Michael’s Hospital scientist provides a rare contemporary prevalence estimate of cardiovascular risk in people living with diabetes who reside in the Middle East and South Africa. Individuals from both of these regions continue to be under-represented in clinical trials thus limiting generalizability of the findings.
The PACT-MEA study – led by Dr. Subodh Verma, a St. Michael’s clinician-scientist and Canada Research Chair in Cardiovascular Surgery, found that approximately 1 in 5 persons living with diabetes in these regions has heart disease.
PACT-MEA also revealed that people in these regions who live with diabetes have a high prevalence of
cardiovascular risk factors, including poor blood pressure control and high cholesterol.
“These are regions where rates of death and disability from diabetes remain quite high. Yet despite this understanding and the exponential growth of patients in these regions, there has been very little good quality data to understand overall cardiovascular risk,” said Verma. “This is what we aimed to do.”
The cross-sectional, observational study enrolled over 3,700 patients with type 2 diabetes from Bahrain, Egypt, Jordan, Kuwait, Qatar, the United Arab Emirates and South Africa. Researchers collected patient data during a doctor’s appointment using a standardized, electronic form.
Clinical research overwhelmingly take places in Western countries, and most participants are male. The
PACT-MEA study, which includes a cohort that is 47 per cent female, fills a gap in knowledge about people from non-Western regions of the world.
The study found that overall 20.9 per cent of the participants had atherosclerotic cardiovascular disease, with significant variation between countries, ranging from 37 per cent in Bahrain to 19 per cent in Kuwait.
The study also found that 99 per cent of the cohort would be considered at high risk or very high risk for future cardiovascular events, based on the 2021 European Society of Cardiology guidelines.
To reduce cardiovascular risk, doctors recommend a combination of factors, including maintaining good blood sugar and blood pressure control, lowering cholesterol, access to the appropriate vascular protective medication, a body mass index (BMI) below 25
kg/m2 and frequent exercising, said Verma.
“Strikingly, zero per cent of the patients surveyed actually met all of these goals,” he said.
Verma hopes the study highlights the importance of having global representation in clinical research – something that is critical if research results and interventions are to have broad generalizability.
“I’m passionate about this study because it helped uncover a significant gap in our current understanding of the cardiovascular risk level in people living with diabetes in an area where there’s a growing tsunami of this chronic disease,” he said.
“It’s a call to action that if we are going to be global citizens and global researchers, more people from these regions need to be represented in clinical research.” ■ H
AHamilton Health Sciences (HHS) cardiologist and her research team are exploring how remote home monitoring can help improve access to care for people experiencing heart failure, a common condition affecting 750,000 Canadians.
Heart failure is when the heart doesn’t function properly or when there’s damage to the structure of the heart. It can be the result of a heart attack or other serious heart conditions such as hypertension. It can also result from obesity, alcohol misuse, or valve disease. The dysfunction is often permanent and can’t be cured, but it can be improved through medications and lifestyle choices.
Lifelong management of heart failure can be challenging, so Dr. Harriette Van Spall and her research team are exploring how to improve access to care. As well as being an HHS cardiologist, Van Spall is a scientist at the Population Health Research Institute of HHS and McMaster University as well as at St. Joseph’s Research Institute, and an associate professor in the Division of Cardiology at McMaster.
More people are surviving cardiac events like heart attacks than ever before and hypertension is not only common but often undertreated. So, the number of people with heart failure is also on the rise.
“We’re not only seeing more people with heart failure but younger people in their 40s and 50s with many years of life at stake,” says Van Spall. “However, the typical patient is an older adult, and many can’t get to centres of excellence. This is why it’s important to provide accessible care and remote support.”
While maintaining a healthy lifestyle through diet and exercise and taking medications as prescribed is important for everyone, it’s essential for
people with heart failure. What makes it especially challenging, is that small changes can have large impacts. This means many people with heart failure end up back in hospital with persistent symptoms like fatigue, shortness of breath from fluid in the lungs, and swelling in the abdomen and legs.
“If we can provide effective ongoing support and best medical treatments to those with heart failure, they’re less likely to be re-admitted to hospital,” says Van Spall. “However currently,
many don’t get adequate enough care after they’re discharged.”


To try and meet this need, Van Spall and her team are currently testing a virtual model of care with a clinical trial called VICTORY-HF. This involves a remote monitoring system where patients regularly track health data from the comfort of their homes,
to be reviewed by their care team. Regular remote visits occur between the patient and care team to optimize medical therapy. This 3-year study will include approximately 1,400 participants at sites across Canada, including HHS.
“We want to see if a virtual model with remote monitoring can help patients feel better and ultimately prevent re-admissions to hospital,” says Van Spall. “There’s great potential for a virtual care model to improve access for those who find it challenging to attend regular appointments, and for health-care providers to intervene before health concerns become serious.”
Van Spall’s work to improve the lives of those with heart failure has been recognized by the Canadian Institutes of Health Research and the Heart and Stroke Foundation of Canada. Plus, she’s received prestigious awards for her research from the Canadian Institutes of Health Research and the American Heart Association.
Her successful career has given her the opportunity to pursue equity, diversity, and inclusion improvements within both the research community and cardiology.

She is a strong supporter of women and other under-represented groups in cardiology. She has funded a training program for students from under-represented regions in the world to join her research team. She believes that giving opportunities to a more diverse group of researchers can spur the systematic change needed to find innovative solutions for patients living with cardiovascular disease around the world.
“If we want to make serious advancements in health care, we need the contributions of the best and brightest, regardless of their age, gender, geography, or ethnic background,” says Van Spall. “We must make room at the table for everyone who wants to contribute.” ■ H
Dr. Harriette Van Spall and her research team are exploring how remote, home monitoring can help improve access to care for people experiencing heart failure. Photo credit: Bisi Alawode“IF WE CAN PROVIDE EFFECTIVE ONGOING SUPPORT AND BEST MEDICAL TREATMENTS TO THOSE WITH HEART FAILURE, THEY’RE LESS LIKELY TO BE RE-ADMITTED TO HOSPITAL.”
Eighteen inches.
Dr. Kenneth Gin vividly recalls that number.
“I recently attended a conference talk given by a General Physician (GP), who had brought a stack of papers with him on stage and measured it - 18 inches,” says Dr. Gin, Professor of Medicine and Head of Cardiology Division at Vancouver General Hospital. “ That was the stack of papers just from the last two years that he was expected to read up to stay current as a GP.”
The growth of medical information currently outpaces doctors’ abilities to keep up with it. Patients, too, are living longer - encouraging news but also challenging, as they accrue more chronic medical conditions, which tend to interact with one another, but so do their treatments.
“We are treating very complicated medical cases that require advanced knowledge that we can barely keep up with,” says Dr. Pavel Antiperovitch, Medical Development Lead for VIRTUES and an early career cardiologist at the London Health Science Centre.
To help alleviate these specific problems, the Cardiovascular Network of Canada (CANet) has evolved its proven-successful digital health platform, VIRTUES.
“With recent enhancements incorporated into VIRTUES, we have a platform designed to provide patients with the most relevant medical information, facilitate access to effective care options and connect them with clinicians who understand their medical and personal care requirements,” explains CANet’s Scientific Director, and CEO, Dr. Anthony Tang.
Patients begin their journey in VIRTUES by completing their medical profile related to their condition. They can access, review and share this critical information belonging to them at any time.
Compliant with all Canadian healthcare privacy laws, including the Personal Health Information Protection Act (PHIPA), the platform is not owned by hospitals, businesses, insurance companies, or physicians; it is in the hands of the patients who use it.
Customized proprietary algorithms developed by CANet’s team are at the heart of VIRTUES.
Unlike traditional generic guideline recommendations accessed through various tools and apps found online, VIRTUES algorithms analyze a patient’s medical history, labs, and medications activating appropriately identified CareSets. These CareSets are guidelines-driven, accurate and provide standardized treatment recommendations tailored to their unique conditions.
CANet has a strong partnership with the Canadian Cardiovascular Society (CCS) and works extensively with CCS members who develop cardiac care guidelines.
“These guidelines take a lot of work and are very well done,” Dr. Tang says. But keeping up with these guidelines and implementing them consistently has become more complex with the constant expansion of medical knowledge.
Now, with the latest version of VIRTUES, implementation of guidelines recommendations are now individualized to the specific needs of the patients such that the clinicians and the patients have the individualized recommendation at their fingertips.
Patients can view their recommendations within the VIRTUES platform and share them with their healthcare provider of choice. Their healthcare provider
will receive a copy of recommended treatment options, including the relevant information and references supporting the recommendations. The patient and healthcare provider can choose the best treatment option together. A combination of educational materials, medication infographics, and informative videos about managing their condition are provided directly in VIRTUES for the patient.
“We are a long way from implementing VIRTUES as part of standard medical practice,” Dr. Tang clarifies, adding that the coming years will consist of rigorous platform testing across Canada.
The hope is to demonstrate that using the platform results in better health outcomes for patients and increases access to quality of care and quality of life, reduces the cost to the healthcare system, and improves the efficiency of medical professionals.
Currently in use for remote monitoring and support for patients with Cardiac Implantable Electronic Devices (CIED), VIRTUES’ has also proven successful during the pandemic utilizing the platform to provide symptom tracking for COVID-19-positive patients and integral support to healthcare professionals.
With the release of the enhanced VIRTUES platform, an ongoing pilot trial involving 1400 patients across 15 clinical sites throughout Canada aims to determine the effectiveness and patient satisfaction of CareSets for patients with various cardiac conditions like Atrial Fibrillation (AF).
AF is the most common cardiac disturbance contributing to cardiovascular morbidity and mortality. Studies estimate a 250% increase in AF prevalence by 2050.
Dr. Allan C. Skanes, who focuses on AF management, is hopeful that VIRTUES will help widen the geographic scale of treatment across Canada. “Many of the drugs we use for AF management are unfamiliar to most family doctors and internal medicine specialists,” says Dr. Skanes, Professor of Medicine at Schulich Medicine and Dentistry and Director of Electrophysiology Laboratory, London Health Sciences Centre, and echoes the myriad questions medical care specialists face - How do we provide the best guidance on managing AF related rhythm disturbances? How do we choose what drugs to give, and how to monitor and manage patients?
One critical advantage of VIRTUES, he notes, will be its ability to optimize the delivery of cardiac care guidelines and guideline-directed therapy to the broader medical community more consistently.
Once validated, how does VIRTUES get integrated into the national healthcare system?
“Does it become one component of Canada’s evolving electronic health record-keeping landscape, or does it become the dominant digital health platform, with all sorts of medical and lifestyle information feeding into it?” wonders Dr. Michael D. Hill, Senior Medical Director, Cardiovascular Health & Stroke Strategic Clinical Networks TM, Alberta Health Services. With the constant expansion of medical knowledge and data collection, one will need more resources and a larger pool of experts who can collect, analyze, and communicate this information in an accessible way; he points out.
“This opens up opportunities for medical students to receive training in digital health,” speculates Dr. Antiperovitch. According to him, the training would help doctors gain knowledge of programming and interface software in a way that would help them communicate medical knowledge to software designers.
Cardiovascular Network of Canada enhances its digital health platform VIRTUES, optimizing the delivery of cardiac care to patients in all regions across Canada
The collaboration, as demonstrated by CANet’s VIRTUES team, will be vital in creating and keeping algorithms up-to-date to generate the most effective and current patient-specific treatment guidelines.

“VIRTUES is an extremely ambitious project with a huge amount of background work.” Dr. Gin says.

Knowing this, CANet remains steady and committed to transforming the nation’s healthcare system, driving quality and affordable care for better cardiovascular health outcomes. Dr. Tang is hopeful that the Federal government remains committed as well.
“Our strength is our network, with its vast collective expertise of healthcare professionals, academia, government, industry, not-for-profit, and patient partners across Canada,” he says.
Patient engagement, Dr. Tang notes, is often an afterthought in profit-driven digital health platforms, where patients are involved only at the end of the development process. He emphasizes VIRTUES has been a patient-controlled digital health platform since the first line of code was written, placing it in a league of its own.

“VIRTUES is a big and ambitious project, made possible by the generous and selfless voluntary contributions of highly skilled and highly qualified professionals, striving to put the patient at the centre of it all. We will continue to move forward.”








VIRTUES is a holistic, comprehensive digital health approach that provides equity of care to meet the needs of all patients, regardless of geographical, cultural, or systemic barriers.






Addressing the critical needs of patients, VIRTUES provides secured digital health tools to access efficient and quality care in all regions across Canada for improved quality of life and better health outcomes.
With patient information collected in VIRTUES, patients receive personalized CareSets for their medical conditions. Patients may receive different CareSets (modules) in VIRTUES based on their current health conditions and needs.
A CareSet is a package of Guidelines-Driven Recommendations and Educational Resources that address relevant health conditions tailored to a patient’s needs.
• Antithrombotic Management (Blood Thinning)
• Post Myocardial Infarction Care (Heart Attack)

• Rate & Rhythm Management for Atrial Fibrillation

• Lipid Management (Cholesterol)

• Hypertension Management (Blood Pressure)
• Physical Activity
• Healthy Eating
• Blood Sugar Management (Diabetes)
• Smoking Cessation
• Alcohol Reduction


• Heart Failure Management
• COVID-19
• Cardiac Implantable Electronic Devices (CIED)




Learn more at www.virtues.care

Scarborough Health Network (SHN) has introduced its new Mental Health Diabetes Clinic, providing diabetes patients, who may also be at risk for chronic kidney disease (CKD), access to necessary mental health supports in addition to regular disease monitoring and management.

“SHN’s diabetes and mental health programs are partnering to expand care for patients living with diabetes. Chronic diseases like diabetes impact many aspects of patients’ lives, including their mental health. With our new clinic, diabetes patients can now be referred to an SHN psychiatrist if they are experiencing depressive, anxiety, post-traumatic, or other psychiatric symptoms that are contributing to difficulties with self-management or engagement in care,” explained Toni Thomas, a registered nurse for SHN’s diabetes program.
The clinic reflects the comprehensive approach of SHN’s diabetes program, which has established itself as a leader in diabetes management, treatment and prevention strategies, ensuring access to timely, high-quality services in the most appropriate setting for patients. It will also support eligible CKD patients, since both kidney disease and diabetes are closely linked.
The new service also builds on support available to patients through SHN’s diabetes and kidney disease (DKD) program, which focuses on
slowing the progression of CKD and delaying the transition to dialysis. This is achieved by providing diabetes and nephrology management within one appointment. It is a collaboration with SHN’s regional nephrology program, which cares for more than 6,000 patients annually. The DKD program is paving the way for a Metabolic Clinic in the future – which aims to be a “one-stop shop” for patients including services such as mental health, cardiology, foot and much more.
“Diabetes is actually the top cause of chronic kidney disease,” emphasized Thomas. “Mental health is a largepart of managing a chronic disease and certainly managing diabetes and kidney disease; can be quite onerous on a daily basis. There are many decisions people must make, like medications, diet, and regular daily life, and it can take a toll on mental health,” she explained.
Currently the program is in its pilot stage, only accepting patients referred by SHN doctors, and using the diabetes distress scale (DDS) in identifying individuals for the clinic. The DDS is a 17-item scale that captures four critical dimensions of distress: emotional burden, regimen distress, interpersonal distress and physical distress.
“Diabetes on it’s own can present patients with many challenges, but once you add chronic kidney disease,there are several issues that can manifest. Getting patients the care they need and collaborating between
clinicians provides the best care possible for the patient, while improving their mental health,” Thomas added.
An estimated 1.2 million people in Ontario have been diagnosed with Type 1 or Type 2 diabetes, both of which can cause CKD.
Diabetes and kidney disease also have strong prevalence in individuals of Asian, South Asian and Caribbean descent, cultures that comprise much of Scarborough’s population.
Recognizing the need for care in Scarborough, Thomas said patients have more options for treatment, monitoring and mental health supports than ever before.
“Individuals with diabetes and chronic kidney disease can be at higher risk of developing depression than
others; for example, untreated or unrecognized mental health issues can make managing chronic diseases more challenging due to the overwhelming amount of responsibilities on a day to day basis,” explained Thomas.
“Diabetes distress can be caused by frustration, worry, and discouragement from dealing with daily disease care, leading some to find it difficult to engage in their daily care. It is important to offer patients effective methods of dealing with their anxiety and depression, and to ensure they are speaking with someone who has a deeper understanding of diabetes and chronic kidney disease challenges – it can be life-saving.”
Learn more about SHN’s diabetes, mental health and regional nephrology programs. ■ H
For high-risk pulmonary embolism – life-threatening blood clots in a lung – catheter-directed thrombolysis (CDT) appears to be associated with a lower risk of death and bleeding complications, according to new research in CMAJ (Canadian Medical Association Journal).
Pulmonary embolism (PE) is the third leading cause of death from heart disease after myocardial infarction (heart attacks) and stroke. Early
diagnosis is essential, as one-in-three deaths occur in the first few hours, and only seven per cent of deaths occur in properly diagnosed and treated cases.
Catheter-directed thrombolysis is a procedure that infuses low doses of medication directly into the pulmonary arteries. Research on its safety and efficacy is lacking, and treatment guidelines vary because of this uncertainty.
In a comparison of different treatments for pulmonary embolisms, Israeli researchers found that CDT was as-
sociated with a decreased risk of death and lower risks of major bleeding and brain bleeds.
The authors caution the study is not conclusive and more research is needed.
“Although this study should be interpreted as hypothesis-generating, our findings suggest that, among patients eligible for CDT and where facilities exist, CDT should be the preferred treatment, given its effectiveness, and the higher toxicity of systemic thrombolysis,” writes Dr. Bruria
Hirsh Raccah, a researcher at the Hebrew University of Jerusalem, Jerusalem, Israel, with coauthors.
“[C]entres that specialize in CDT can consider it as first-line therapy among patients with intermediate- to high-risk PE,” the authors conclude.
“Catheter-directed thrombolysis compared with systemic thrombolysis and anticoagulation in patients with intermediate – or high-risk pulmonary embolism: systematic review and network meta-analysis” was published June 19, 2023. ■ H
As Nova Scotia’s nursing regulator, the Nova Scotia College of Nursing’s (NSCN) role is to ensure that all nurses providing nursing services for Nova Scotians are qualified to do so. The public can depend on NSCN to license those who meet registration requirements and demonstrate they have the knowledge, skills, and competence required to safely and ethically practice as a nurse.
Since our formation in 2019, NSCN has applied an innovative lens to our regulatory work seeking opportunities to streamline our processes and remove potential barriers. In 2022, NSCN continued to recognize the rapidly evolving changes to our health care system and needs of the public, specifically the shortage of nurses in Nova Scotia. To address this, we built on our innovative solutions to register and license nurses quickly during the early days of COVID-19, and comprehensively reviewed our registration and licensing processes to ensure they are relevant, flexible and positively contributing to the supply of nurses.
NSCN recently implemented a new first-in-Canada approach to registration and licensure that will establish a fast and predictable pathway to licensure in Nova Scotia. Registered nurses who demonstrate good standing and good character and are licensed in Canada, the Philippines, India, Nigeria, USA, UK, Australia, or New Zealand, are eligible for registration and licensure in Nova Scotia with no additional requirements other than passing the entrance exam.
“In the past year, NSCN demonstrated our nimbleness to respond to the evolving needs of the health care system and environments in which we work,” says Sue Smith, CEO & Registrar at NSCN. “We challenged ourselves to rethink our approach to registration and licensure while ensuring our decisions were guided by safeguards that prioritize public safety.”
The new licensure process for international nurses registered and licensed in the seven designated countries took effect on May 1, 2023 and reduces the

overall processing time from up to two years to a matter of months. Applicants will apply and have their application assessed by NSCN directly, removing the need for the National Nursing Assessment Service (NNAS) for applicants from these identified countries. The process for nurses registered and licensed in Canadian jurisdictions took effect on March 29, 2023 and reduces the processing time to 24 hours.
“The majority of NSCN’s international nurse applicants come from the seven designated countries listed. A significant amount of data from 10 years of NNAS Advisory Reports, and review of nationalized curriculums, entry-level competencies and success rates of entry-to-practice exams has allowed us to confidently make this decision,” explains Smith. “When a nurse meets the registration and licensure requirements in one of these seven countries, it means they have demonstrated they have the necessary education, preparation and foundation to safely practice in the RN scope of practice similar to what is required in Nova Scotia.”
As of June 20, 2023, NSCN has received more than 14,000 applications from nurses in the seven designated countries with 440 applications in progress and 74 licences issued. From other Canadian jurisdictions, 647 applicants have been licensed and are ready to practice in Nova Scotia.
“While our new approach significantly decreases licensing time, it does not cut corners or reduce requirements. Every applicant must still meet the same registration requirements. We have not changed that. We have however, changed our approach to the type of evidence we assess to determine an applicant has met our requirements,” says Smith. “We anticipated there would be a lot of interest, but this is beyond our expectations. We are pleased that this will allow for more nurses to be licensed to practice in Nova Scotia and to be eligible to be employed as nurses in our province.”
To manage the influx of applications, NSCN has taken on temporary full-time staff and the Registration Services team is working hard to process applications and manage the information received to date.
NSCN continues to collaborate with health system partners to support nurses as they transition to practice in Nova Scotia. In early May, NSCN held a special stakeholder roundtable with the intent of developing an International Nurse Task Force. The task force includes partners such as the Office of Healthcare Professionals Recruitment, Nova Scotia Immigration, Nova Scotia Health, IWK, Department of Health, Continuing Care, Long Term and Seniors Care, Nova Scotia Housing, Department of Ad-
vanced Education, Nova Scotia Housing and long-term care employers. The task force is responsible for developing sector-specific workgroups to look at immigration, recruitment, employment, settlement, housing and education to ensure there is a coordinated effort to leverage the unprecedented number of applicants.
Nova Scotia Health has a program, Nova Scotia’s International Community of Healthcare Workers Engagement (NICHE), whose role is to provide wraparound support for international healthcare workers coming to Nova Scotia. On behalf of NICHE, NSCN sent out a survey to the international nurse applicants in our process to help them access the comprehensive immigration, settlement, and employment supports in Nova Scotia. So far, more than 9,000 applicants have responded to NICHE.
“We are thrilled to work with our health care system partners to ensure that these nurses have the support they need – it is a group effort. NSCN continues to deliver solutions that align with government’s direction to all health system partners in the province to think differently and move quickly. We are certainly doing that and continue to be innovative in our approach to enable nurses to deliver safe, competent, ethical and compassionate care to all Nova Scotians,” says Smith. ■ H
Researchers have discovered that a peer-to-peer diabetes mentorship program yielded positive health outcomes for peer leaders. Published in the Canadian Journal of Diabetes, the first North American study of its kind provides a compelling case for further integration of relatively low-cost peer support into diabetes care.

“Prior research has largely examined the impact of peer support for individuals who receive rather than deliver support,” says senior author and Vancouver Coastal Health Research Institute researcher Dr. Tricia Tang.
Around
Type 2 diabetes is a progressive disease caused by the accumulation of sugar on a protein in red blood cells called hemoglobin. Clinicians test for diabetes using a simple A1C blood test, which measures the percentage of red blood cells with too much sugar on their hemoglobin.
Percentages below 5.7 are considered normal, while people with 5.7-6.4 per cent have pre-diabetes and people with 6.5 per cent blood sugar and higher are diagnosed with diabetes.
Afshar’s study involved 52 volunteer peer leaders aged 21 years or older with either type 1 or 2 diabetes and a self-reported A1C of eight per cent or less. Peers received 30 hours of training, based on Tang and colleagues’ Peer-Led, Empowerment-based Approach to Self-management Efforts in Diabetes (PLEASED) training program.
Peer leaders were matched with participants with type 2 diabetes. Leaders and participants met face-to-face for the first session and then weekly or bi-weekly over the phone for a year.
Peer leaders were encouraged to follow a general structure during their calls with participants that included discussing self-management challenges, questions and goals, along with problem-solving and sharing feelings.
Researchers tested peer leaders’ A1C, blood pressure, body mass index, waist circumference, diabetes distress and depressive symptoms at the start of the study, and then three and 12 months after.
At the 12-month mark, researchers found the clinical and mental health measures that were in target range at baseline remained in target range, including peer leaders’ A1C percentage.
“This finding is quite significant,” notes study co-author Dr. Rowshanak Afshar. “Because diabetes is a progressive disease, A1C levels often increase by approximately 0.2 per cent per year on average.”
Peer leaders shared with the research team that the experience opened their eyes to the potential consequences of poorly controlled diabetes and the potential benefits of proper diabetes self-management. It also helped them expand their diabetes knowledge and management skills.
“With so much available information about how to treat and manage diabetes today, people living with
diabetes can be overwhelmed with the mental burden of this process-demanding condition,” notes Afshar.

“They need to take their medications at a certain time and amount, follow a specific diet, exercise regularly, etc.”
One peer leader mentioned to the research team that he was able to “clean up his own life in the process of helping somebody else.”
While results from the peer support program are promising, Afshar says that more research is needed to highlight its potential cost savings and show how it can be integrated into other care settings.
“Maintaining the benefits shown in this study could require the integration of an ongoing peer support program into hospital or community care centres in order to make the program more accessible to people living with diabetes.” ■ H
 11 per cent of British Columbians are living with a diabetes diagnosis, a number that is estimated to increase to 13 per cent by 2032.
11 per cent of British Columbians are living with a diabetes diagnosis, a number that is estimated to increase to 13 per cent by 2032.
PEER LEADERS WHO PARTICIPATED IN A YEAR-LONG STUDY MAINTAINED STABLE BLOOD SUGAR LEVELS AND EXPERIENCED MENTAL HEALTH BENEFITS.
How do homelessness and poverty impact metabolic diseases like diabetes? How can healthcare systems and healthcare providers help people who face social disadvantages better manage chronic health conditions?
the University of Calgary has dedicated much of his research to determining links between homelessness and

How did you get interested in social disparity and disease?
way that political and economic environments disease and everybody can do things to ask them to by virtue of their circumstances. of chronic diseases like diabetes with their lives and what kind of things we—as a system and as individual providers—could do to meet them on their terms.
What are some of your research highlights to date?
interventions in a large group of low-income seniors with diabetes or heart disease. One group received free medication which made them slightly more likely to take their medications but did not have an impact on health outcomes. The second was an educational intervention provided in an engaging and interactive way that resulted health education in a more engaging way to improve health outcomes.
Any other takeaways from your research?
providers to really understand how to tailor their care to the circumstances
REGISTER TODAY!
The Diabetes Canada/CSEM Professional Conference at Vascular 2023.
Vascular 2023 is a world-class event, bringing together separate conferences from Canadian organizations involved in the treatment and care of vascularpeople annually. With one registration fee, access program content from Diabetes Canada/CSEM and all other host organizations as well as shared vascular programming.
circumstances. When it comes to can do for somebody rather than
OCTOBER 25-29 MONTRÉAL, QUÉBEC
DC/CSEM Pre-Conference Workshops:
Wednesday, October 25
Full DC/CSEM Conference Program:

Thursday, October 26 and
Saturday, October 28
Vascular Day: Friday, October 27
Save 20% with the early bird price until August 8. For more information visit vascular2023.ca
Dr. David Campbellt is the most comprehensive patient education resources in the country that addresses the unique aspects of heart disease in women.
When Nazli Parast, APN, was studying to become a cardiac nurse, she was surprised at how little she learned about women’s heart health and the specific risk factors for heart disease unique to women.
Today, some fifteen years later, Nazli has a master’s degree in nursing, and she is one of the country’s only advanced practice nurses with expertise in women’s cardiovascular health.
At the University of Ottawa Heart Institute (UOHI) where she works in the women’s heart health clinic, she is passionate about educating her patients and ensuring her colleagues can learn what she was never taught as a student.
“I was disappointed nursing students don’t receive as much education [on women’s heart health] while they are completing their training,” said Nazli. “As future nurses, students must have opportunities to learn about women’s heart health so they can become better advocates for their patients.”
“Everything we know in a comprehensive, all-in-one resource”
Two years ago, Nazli began noticing a pattern in her conversations with patients of the women’s heart health clinic.
“I received many similar inquiries from women who had experienced cardiovascular events,” she remembered. “There were a lot of important questions these women had, and they kept asking me if I could refer them to something specific that could help them understand what they were going through, something that would help them connect the dots.”
At the time, no guides comprehensively addressed the specific needs and experiences of women with heart disease. Nazli recognized a gap needing to be filled.
What began as a passion project quickly developed into something more. With the support of her col-
leagues, including empowerment and leadership from her manager, Bonnie Quinlan, lead physicians in the clinic at the time, Thais Coutinho, MD, and Michele A. Turek, MDCM, and significant help from her volunteer student, Ana Spasojevic, Nazli developed the first comprehensive guide tailored specifically to women with heart disease. Offered in English and French, the guide combines the expertise of several disciplines to provide women with accurate medical information all in one place.
Cardiologists, nurses, dietitians, psychologists, physiotherapists, and other medical professionals all contributed to the guide’s development, but what makes it so unique, “so powerful,” said Nazli, is that patient partners played a significant role throughout the process.
“We enrolled three patient partners in the project to review the guide during key stages of its development, to ask questions and seek clarifica-
tion, and to ensure that the information presented was relevant to their individual needs,” Nazli said. Patient testimonies are included in the guide, but the names of patients are kept confidential. “The stories we share in the guide are intended to help others who may need them to connect, relate and understand their own experiences.”
“Individuals with lived experience must have a seat at the table for everything we do”
Thais Coutinho, MD recently cochaired an international meeting of experts in women’s heart, brain, and vascular health in Vancouver, BC, during which actions to help close the gaps that prevent women from receiving the health care they need were discussed.

“It is abundantly clear that individuals with lived experience must have a seat at the table for everything we do,” she said. “Among the most important takeaways from the Canadian
Women’s Heart Health Summit is the importance of including the voices of individuals with lived experience with cardiovascular disease in research, clinical programming, advocacy, and policy development. Their voices need to be heard to achieve meaningful change.”
During the Summit, patients like Michelle Logeot, who suffered cardiac arrest and a debilitating heart attack in 2017, spoke to the need for women to advocate for themselves.
Michelle, who is now 56, delivered her talk, Not taking no for an answer, to an audience of medical professionals and patients. She shared her harrowing experience with heart disease in interviews with The Toronto Star and on Global News.
“After six months of going to the doctor – knowing I wasn’t feeling well; I was sweating a lot, I was really fatigued all the time, I could barely function – many times they would misdiag-
nose me,” Michelle told Global News Morning BC’s Sonia Sunger. “Even though I had a strong family history of heart disease, they never looked at that.”
Michelle’s message to women is clear: “You know your body better than anyone. If you feel you have something wrong and you’re being dismissed, don’t be scared to get a second opinion or challenge your doctor. If something feels off, it likely is.”
It’s in hearing Michelle’s story – and hundreds more like it – Nazli Parast and Thais Coutinho recognize patient advocacy is not enough to address the gender gaps and inequities still present in research and healthcare today.

“It’s obvious to me that to really have a meaningful impact will require leadership from the top,” said Dr. Coutinho, who in a recorded message shared via Twitter said:
“To really close the prevention, care, and outcomes gaps for cardiovascular disease in women, we really need
action to come from above. There are many of us who are health care providers and scientists who have been working on these issues from our little corners of the world and making small
impacts surrounding us, but to really have meaningful and widespread impact across Canada, we need a national strategy that will be the national standard that everyone will follow.”
“Information is powerful, but it is not enough,” said Dr. Coutinho. “We are preaching to the choir and the chorus is small,” she said. “What we need now is action.” ■ H
The authors of A Guide to Women’s Heart Health acknowledge a lack of research available on the heart health of the 2SLGBTQ+ community. If you have questions about your individual health and the risks that may be specific to your identity, please talk to your doctor or care team.

Like most kindergarten kids, classmates Julia and Ainsley were learning their ABCs and 123s. But the five-year-old girls were also introduced to the world of science and nutrition at this very young age, after being diagnosed one week apart with type 1 diabetes (T1D).
T1D is an autoimmune insulin deficiency that prevents the body from producing insulin on its own, or very little of it. Insulin is a hormone that helps your body turn food into energy, and regulate blood sugar levels. An individual with T1D must intake insulin via injection or insulin pump in order to survive.
Working with their parents and McMaster Children’s Hospital (MCH) health-care teams, the girls – now 11 years old and good friends – have learned how to keep on top of their sugar levels, calculate carbohydrates, and give themselves insulin. When it comes to managing their disease, they love the support of having a ‘diabestie’ with the same diagnosis.





When Julia was five years old, she was losing weight and always very thirsty. After a visit to her family doctor, test results showed she had high blood sugar, a sign of diabetes. Shortly after receiving care at MCH, she started feeling better.
When Ainsley was also five, she was so thirsty at night that she would wake
up crying from discomfort. Her family doctor administered a simple urine test, and results immediately showed glucose in her urine; a sign of T1D. She was sent to MCH for further care.

“I called the school to let them know Ainsley’s situation and how she was going to be away for a few days, and they told me another parent made the same phone call shortly before me,” says Kate Adams, Ainsley’s mom.
The pair were diagnosed a week apart, and were both in the same junior kindergarten class at Spring Valley Elementary School in Ancaster. Shortly after, the two kids and their moms became close friends, embarking together on the same journey. Julia and Ainsley are still at the same school, now in Grade 6 but in different classes this year.




Children with type 1 diabetes manage the disease with insulin that’s administered by injection or infused via insulin pump into the bloodstream continuously and increased before every meal and major snack. They need to check and monitor their blood sugar levels frequently as well to keep insulin and glucose balanced. This can be done through finger pokes or other new sensor technologies. High blood sugar can lead to a rapid heartbeat, vision problems and other symptoms. And too much insulin can lead to low blood sugar causing shakiness, disorientation or even loss of consciousness.
“They have to think about so many different things,” says Dr. Ereny Bassilious, a pediatric endocrinologist at MCH who works with both girls. “It is difficult as a young child with T1D because of the complexity of it. There are so many steps that go into managing diabetes such as checking sugar, counting carbohydrates, calculating insulin dose, and administering the insulin.”
Using technology to make life easier
A newer technology known as continuous glucose monitoring (CGM) happens through a device worn on the body that tracks blood glucose (sugar) levels every few minutes throughout the day and night. These readings are sent to the patient, caregiver, or health-care provider via a digital device for fast and accurate readings, minimizing the need for finger pokes.


Both Ainsley and Julia use a CGM system that tracks blood sugar levels and sends frequent readings to a paired smart device. It allows for both moms to also pair their phones to the device and monitor their daughters’ sugars while they are at school.
“CGM technology allows the patient and caregivers to monitor blood sugars continuously, to observe trends, and to be able to act on a high or low blood sugar in a timely way,” says Dr. Bassilious.
Instead of frequent needles, many young people may choose to use an insulin pump, which is a clear little tube that administers insulin to the body

when told to, and is attached to them at all times.
For their insulin, both Ainsley and Julia use a pump, eliminating the need for multiple daily injections. Base insulin deliveries are programmed into the pump by their health care team. Insulin delivery for meals or for correction of high blood sugars is delivered when the child or their caregiver enters a blood sugar or carb amount into the pump.
“There are lots of elements involved in diabetes management,” says Bassilious. “With young children, we strongly recommend a partnership between health-care providers and parents, before slowly transitioning over to the child doing things on their own.”
MCH cares for about 665 young patients with diabetes. Along with a treating physician, there is a whole team that helps families with learning about the disease and how to manage it. The team consists of a diabetes nurse, dietitian, child life specialist, and social worker.
“As a parent, you are overwhelmed at first,” says Sarah Fairfield, Julia’s mom. “It’s a whole new routine, a new lifestyle. There is a lot to learn in the beginning. A caregiver of a young active child with diabetes can make over 100 treatment decisions a day. There is so much planning that goes into it.”
As much as the girls find support in each other, their moms also have com-

fort in knowing that their daughter’s friend has a family who knows how to handle their health needs.
“Things like sleepovers can be tricky,” says Adams. “You have to know a little bit of what is going on. As the mom, you can only plan so much with packing snacks and everything else. When Ainsley goes to Julia’s for a sleepover, I know I don’t have to worry.”
Fairfield adds, “It gives an incredible peace of mind to have someone who understands the day-to-day challenges. You problem solve together.”

The `Golden Unicorn’ friendship
Ainsley and Julia are the only students in their grade at their school with T1D. “Whenever our levels would match up, we used to make jokes about how we were golden unicorns,” says Julia.
Ainsley adds, “If I ever needed anything I can go to Julia. If I need something like Dextabs at school I would be able to ask her for some. I remember one day at school, I saw Julia a little




shaky and I ran over right away because I knew the signs of what was happening.” Ainsley is referring to a situation where she noticed Julia was experiencing signs of low blood sugar levels.
Both girls attend Diabetes Canada Camp every summer, along with Bassilious, a camp doctor, who is referred to as one of their “camp buddies.” Adams agrees. “I think they are both amazing examples of kids who are thriving despite what they have to do on a daily basis.”
“Kids still need to be kids,” says Bassilious. “They need to eat in order to grow, and do all the things they enjoy. Diabetes is manageable – it doesn’t define who they are.”
Ainsley is a competitive dancer who does jazz, lyrical, hip-hop, contemporary, tap, and ballet. She plans ahead to manage her sugars on long dance nights. “I have to keep on top
Ainsley and Julia became best friends after being diagnosed with type 1 diabetes a week part when they were five. Now age 11, they support each other and share how they manage their disease.

of it. You can still do all of your activities and eat, just make sure you plan, monitor, dose and don’t let it hold you back,” says Ainsley.
When Julia isn’t bike riding or getting her favourite slushies, she is a talented gymnast. She doesn’t let diabetes get in the way of her jumps, flips, and twists.
Both parents express the importance of breaking the stigma of stereotypes around T1D. “You hear so many ste-
reotypes about diabetes – people think it’s because you don’t eat healthy or you’re not active,” says Adams. “That is not the truth at all.”
“The biggest thing is making sure children remain children throughout all of it,” says Bassilious. “Whether it be trick-or-treating or having pizza and cake at a birthday party or playing their favorite sport, it is important children and youth living with T1D continue to do what they enjoy.” ■ H
Kristen LoSchiavo works I communications at Hamilton Health Sciences.
An AI-powered tool in Canada’s largest Multiple Sclerosis (MS) clinic is integrating tens of thousands of patient notes into individualized patient histories, saving countless administrative hours for staff and doctors and freeing them to focus on what matters most: the people in their care.
MS is an autoimmune disease that can impact vision, memory, balance and mobility. People who have MS can experience times when their symptoms are more severe and periods when they have few or no symptoms. It can also be progressive, meaning that symptoms get worse over time.
“MS is a disease that lasts decades. Often when a clinician is seeing someone for the first time, they have ten or more years of medical notes to go through,” says Dr. Jiwon Oh, clinical director of the BARLO MS Centre at St. Michael’s Hospital. “The goal of MuScRAT is to – in a quick snapshot – summarize a person’s relevant clinical history in MS.”
Neurologists and other staff in the BARLO MS Centre at St. Michael’s Hospital are using MuScRAT, which stands for Multiple Sclerosis Reporting and Analytics Tool, to get quickly up to speed on new patients, prepare for upcoming appointments and plan next steps in their care. The tool is an example of the partnership between Unity Health’s Data Science and Advanced Analytics (DSAA) team and clinical teams at the network, which has developed more than 40 AI tools since launching in 2016. The DSAA is one of the first applied artificial intelligence (AI) departments in a Canadian hospital and operates using a unique model that brings together healthcare providers, data scientists and data and software engineers to build AI solutions and put them into action. We connected with some of the people behind the MuScRAT tool to learn more about how they created it and how it works:
Ashley Jones joined the MS program at St. Michael’s as a research assistant in 2015 to develop the MS Clinic Registry, a centralized database for the nearly 9,000 patients the clinic follows. She began working with the DSAA team to see how AI could be used to help ease the burden of data entry for the registry, which was an entirely manual process.
“Entering data is very time consuming, very labor intensive and – because we have a large volume of patients at the clinic – it was challenging to keep the registry up-to-date,” says Jones.
One of the key data points used to create individual patient timelines in MuScRAT is the Expanded Disability Status Scale (EDSS) score, a value used to measure and monitor a patient’s level of disability due to MS. Jones worked closely with the DSAA team to translate her method for evaluating clinical notes to determine a patient’s EDSS score so the AI tool could mimic her process.
“Creating the algorithms came very naturally,” says Jones. “I have a very algorithmic way of looking at things, even without knowing it, so it worked really well.”
Jones enjoyed her experience working with the DSAA team so much that she went back to school to get her master’s in health informatics and joined the DSAA team as a project manager in January 2023. In her new role she oversees AI projects with the MS team, along with projects in other clinical areas.
“I wanted to learn more and gain experience in project management,” says Jones. “It’s expanding my field, but also going back to my roots with MS. I really enjoy that I’m still able to work with Dr. Oh and the MS team.”
Chloe Pou-Prom is a data scientist with the DSAA team at Unity Health. She is one of the data scientists who helped develop the algorithms for MuScRAT.
The tool uses two main sources of information to create patient timelines. The first is the previously mentioned MS Clinic Registry database. The second is clinical notes on the MS clinic’s electronic medical record.
“Our role as data scientists on this project was to create AI models to help augment the existing database,” says PouProm. “When a clinician wants to look at a patient’s history, we can pull the existing information from the database but it might be missing more recent data.”
MuScRAT uses natural language processing – a type of AI that interprets language in speech or text to complete a task – to add the most up-to-date data. In this case, the tool interprets the text of clinical notes from patient appointments and physical exams and populates a timeline for each patient, saving countless administrative hours for staff and doctors.
Pou-Prom also notes the important role of software developers on the DSAA team in creating the dashboards and interface for AI tools. They help to ensure that data appears to clinicians and hospital staff in a way that is intuitive and easy to understand.
One of Pou-Prom’s favourite things about being a data scientist at Unity Health is how her work is put into action.
“I like that I can work on projects that people actually use,” says PouProm. “Clinicians are using the tools we develop in their everyday decisions. I think that’s really cool.”
Dr. James Marriott is a neurologist with the MS program at St. Michael’s. He also does MS research and runs the centre’s clinical trials program for new MS treatments. He joined the team in October 2022 and – while he wasn’t involved in the development of MuScRAT – he has become an avid user.
“I’m taking on care for some people who we’ve been following for years or decades or more,” says Marriott. “Having a synopsis of how they’ve been treated and how they’re responding to treatment up until now has been useful.”
Without MuScRAT, Marriott would need to go through each patient’s electronic medical records to map out their disease history and prepare for their appointment. This would involve sifting through individual clinical notes and files – a tedious and time-consuming process.
While Marriott will still review documentation in the electronic medical record when needed, MuScRAT saves him time by streamlining the process significantly.
“It’s helpful for discussions with patients that I’m meeting for the first time,” says Marriott. “I hope it’s also helpful from the patient perspective that I’m able to get up to speed sooner and can focus more on getting to know them as people, and on the next steps in their care.”
Dr. Jiwon Oh is the Medical Director for the BARLO MS Centre and a world-renowned MS researcher. Her role on the MuScRAT project was helping the team vision what the new tool could achieve and providing clinical input throughout its development.
When she and her team began working with the DSAA team their goal was to improve and build upon the centre’s existing database.
“We recognized that our existing database and records were really difficult to use, and we wanted something better,” says Oh. “We also wanted to look at what could we do with the registry data to improve clinical care.”
They’re also looking at AI models that will help clinical staff anticipate a patient’s future care needs.
“Our goal is to apply AI to try to predict: who are the patients that are at high risk of developing a relapse in the next year or two? Who are the patients that are at high risk of developing neurological progression?” ■ H
(From left to right) Chloe Pou-Prom, Ashley Jones, Dr. James Marriott and Dr. Jiwon Oh pictured in the BARLO MS Centre, Canada’s largest MS clinic. Robyn Cox works in cmmunications at Unity Health.Laura McArthur is used to saving lives – not having her life saved. The 66 year old runs a sanctuary for 300 farm animals, taking in horses, pigs and cows, among other animals, that no longer have a home. A former farmer, McArthur puts her heart into her rescue.
“My approach is: ‘Let’s do some good,’” she says.
That same philosophy shapes the work carried out at the Centre of Excellence in Aortic Disease at the Peter Munk Cardiac Centre. Researchers, surgeons, interventional radiologists and anesthesiologists work in tandem to carry out some of Canada’s most complex surgeries performed on the aorta, the main artery which carries blood through the chest and body. They treat patients with aortic aneurysms – dangerous bulges in the aorta – and aortic dissections – a life-threatening condition that occurs when the aorta ruptures, causing internal bleeding. And they give them another chance at life.
“We get calls from medical teams everywhere for insight and advice,” says Dr. Tom Lindsay, a vascular surgeon at the Peter Munk Cardiac Centre. “We’ve developed expertise and continue to bring in new people with new expertise from the most experienced places in the world to build an aortic team that can manage the entire aorta.”
“It’s why we get a high percentage of the tough cases.”
McArthur was one of them. In 2019, she noticed the veins in her arms would swell dramatically day to day. She visited her doctor and after a battery of tests and a CT scan, it was discovered she had multiple aortic aneurysms. Though their cause is unknown, in McArthur’s case, the aneurysms were linked to an autoimmune condition called giant cell arteritis, which causes blood vessel inflammation – a disease she didn’t know she had. “It was pretty scary,” she recalls of her shocking diagnosis, which can lead
to sudden death. “It’s not what I ever felt would happen to me.”
She was referred to Dr. Jennifer Chung, a cardiac surgeon at Peter Munk Cardiac Centre in the Sprott Department of Surgery at University Health Network (UHN), who conferred with her multidisciplinary team. Dr. Chung and the team perform the full spectrum of aortic surgeries, from open surgery, to endovascular procedures – which involves using x-ray imaging to guide a catheter through the femoral arteries up into the aorta – as well as hybrid surgery, which is a combination of both.
McArthur was impressed by how quickly she was assessed and a treatment plan was formulated. “She jumped right in,” she says of Dr. Chung, who performed open surgery, a technique during which a surgeon, through incisions in the abdomen and/or chest, directly reconstructs the aorta. During this reconstruction, the damaged areas of the aorta are replaced with a synthetic fabric metal tube.
After months of recovery, McArthur underwent four more procedures under the care of Dr. Lindsay, who is also part of the Sprott Department of Surgery. He performed minimally invasive surgery on the smaller aneurysms, a procedure called endovascular aneurysm repair, which involves relining the aorta with stent grafts with openings to allow reattachment of the arteries to the bowels, kidneys and legs. These surgeries were done through precisely made small holes located directly above the damaged areas, which are identified through imaging.
“We put the graft (piece of synthetic tube) through the top of the leg and
line up all the connections,” explains Dr. Sean Crawford, a recent vascular surgery staff recruit who brings a background in bioengineering to the team. “There’s a 97% success rate of lining up those holes.” Then, the connections are made using grafts that are ballooned into place.
The Centre of Excellence in Aortic Disease at the Peter Munk Cardiac Centre brings together an impressive team with the wide-ranging skills needed to tackle any aortic emergency. Headed by Dr. Lindsay and Dr. Maral Ouzounian, Head of the Division of Cardiac Surgery at the Peter Munk Cardiac Centre, it’s the team’s collaborative, multidisciplinary approach that provides key insights into finessing novel surgical approaches.
Dr. Lindsay, who has been at UHN for the past 30 years, has performed more than 250 advanced endovascular surgeries. “There’s been huge progress in what’s available and our ability to perform these surgeries,” he says, “allowing for extremely sophisticated surgeries.” Plus, the procedure can be used in very sick patients, often in their 70s and 80s, who would not be good candidates for open aortic surgery.
The main benefits of minimally invasive procedures are fewer complications and faster recovery times. “The quicker and shorter the procedure, the faster patients are back to baseline,” says Dr. Crawford.
Dr. Chung also brings a biomechanical engineering lens to the team and is very involved in developing ways of identifying the highest-risk patients. “Some patients with aortic dissection
have huge aneurysms, necessitating urgent surgery,” she says. However, there is a huge population of patients with smaller aneurysms whose treatment path is less clear, as doctors are unsure whether their aortas will remain unchanged – or rupture.
“We’d like to get at the heart of why certain aortas fail and how to predict that,” says Dr. Chung.
To continue ensuring patients who present with aortic aneurysms are assessed and treated as accurately and promptly as possible, research at the Centre of Excellence in Aortic Disease at the Peter Munk Cardiac Centre will assess how imaging can determine the strength of the aortic wall and its susceptibility to rupture. This research will provide clinicians with key insights on how to best treat each patient, whether through careful monitoring or immediate surgery to replace the aorta.
“There’s no region of the aorta that we wouldn’t be able to tackle,” says Dr. Chung.
What fuels the advancement of aortic surgery at the Peter Munk Cardiac Centre’s Centre of Excellence in Aortic Disease, is the “meeting of minds,” says Dr. Lindsay. And this drives new approaches for increasingly complex cases.
“We’ve created a team of people with complementary expertise,” he says. In addition to cardiac and vascular surgeons, medical imaging physicians, interventional radiologists and geneticists work to deliver and advance aortic therapies. “We discuss problems and solutions and have a conversation about the patients,” says Dr. Lindsay. “The multidisciplinary input is huge.”
Dr. Crawford, agrees. “We work fantastically as a team,” he says.
That team-based approach translates into exceptional patient care. McArthur was impressed with how well her procedures were communicated and how sensitive the team was to her situation. “They were so wonderful and kind,” she says. ■ H
Anna Sharratt works in communications at University Health Network.
The University of Ottawa Heart Institute (UOHI) is establishing a network to improve cardiovascular disease (CVD) prevention and care in women. The Public Health Agency of Canada (PHAC) and the UOHI Foundation are funding the project, valued at more than $1.2M plus inkind contributions.

CVD is the leading cause of death in women over 35 worldwide, accounting for more deaths every year than all cancers combined. So, then, given this alarming truth, why are women still so in the dark when it comes to their heart health?
Dr. Thais Coutinho heads the UOHI’s Division of Cardiac Prevention and Rehabilitation and chairs the institute’s Canadian Women’s Heart Health Centre (CWHHC), the driving force that powers the Canadian Women’s Heart Health Alliance and their annual Wear Red Canada Day event in February. She said heart disease is declining among men but rising among women.
“Any step toward closing the gaps to ensure women are as well-informed and well-cared for as men is a giant leap forward,” Coutinho told The Beat. “We want to see more women living longer, healthier lives, more women being proactive about the management of their heart health, more women who can identify their risk factors and prevent heart and vascular disease, and more women who can identify the signs and symptoms of heart disease before it is too late.”
Dr. Kerri-Anne Mullen is program director at the CWHHC and will co-lead the project alongside Coutinho. She said systematic processes for screening and treating cancers early have long been in place, incentivized at many levels, yet there is currently no such system for detecting CVD and its risk factors despite affecting substantially more women in Canada.
A women’s CVD prevention network will work to improve the awareness of risk factors that disproportionately or uniquely affect women – for example, certain pregnancy-related
conditions, autoimmune rheumatic diseases, and menopause. Understanding this, the network will look to systematize processes for prioritizing and tailoring screening, assessment, diagnosis, and treatment of CVD and its risk factors in women.
“We need a better, more informed and integrated system that connects women to resources and interventions in their community earlier, before their conditions progress,” explains Dr. Mullen.
Team members from the CWHHC will support the network at its nucleus. Together, the network will draw on the expertise of cardiovascular specialists, primary care providers, Indigenous and South-Asian healthcare groups, obstetricians, gynecologists, mental health practitioners, physical activity leaders, dietitians, smoking cessation experts, and policymakers across Ontario.
Women with lived experience, those with and at-risk of CVD, and especially women who are Indigenous, of South-Asian descent, or who have experienced a hypertensive disorder
pregnancy (for they are at elevated risk), will support and inform the network across the project timeline.

“Our staff will devote themselves to the background work, completing needs assessments, gathering evidence around the gaps in awareness and care delivery, and investigating whether there are other successful models we can leverage in the design of our network,” said Dr. Mullen. “We’ll be interviewing and surveying people to understand the wants and needs of women and health providers. We want to know what we are doing well, where we can improve, and where the gaps exist.”
The CWHHC and its partners and stakeholders will converge for a thinktank event where key groups will review background information, define problems, brainstorm, and prioritize ideas and solutions for moving forward. It is the aim of the CWHHC to identify key projects to then prototype and pilot.
Some anticipated examples of such projects include developing awareness products, educational resources, female-specific risk factor screening
protocols, management and follow-up algorithms, decision support aids, feedback and reporting structures, practice incentives, infographics, and technology applications. An evaluation period will inform which prototypes are worth developing, scaling, and implementing in the next leg of the project.
If improving CVD prevention and care for women is going to be a long road, the UOHI’s announcement is a significant step in women’s heart health herstory.
“I think what’s important is that we now have the opportunity to lay much-needed groundwork for some of the implementation work we envision for the future,” said Dr. Mullen.
The PHAC’s Healthy Canadians and Communities Fund invests in projects that address health inequalities, encourage multi-sectoral participation in chronic disease prevention, and uncover new ways to address the risk factors for chronic disease.
The PHAC has awarded upward of $568,000 in support to the project, which the UOHI Foundation has matched. ■ H
In a Canadian first, St. Joseph’s Health Care London (St. Joseph’s) and Lawson Health Research Institute (Lawson), in partnership with GE HealthCare, will become a centre of excellence in personalized treatment of cancer and other diseases by advancing the powerful blend of precision diagnostic imaging and targeted therapy.
This rapidly emerging field of medicine is called molecular imaging and theranostics (MIT). Molecular imaging provides detailed imaging at the molecular level and theranostics is a term that combines the words therapeutics and diagnostics. Together, MIT is a two-pronged approach to diagnosing and treating cancers and other diseases that merges imaging with the use of radiotracers that can not only identify the location and extent of diseased tissues but also selectively destroy the abnormal cells while leaving surrounding healthy cells undamaged.
“The centre will confirm St. Joseph’s and the wider London medical and scientific community as national and international leaders in advancing MIT in the diagnosis of disease, for instance in the identification of cancer and its sub-types, to allow more treatment options for patients,” says Dr. Narinder Paul, Lawson Scientist, Chief, Medical Imaging at St. Joseph’s and Physician Executive, Medical Imaging at London Health Sciences Centre (LHSC). “It will also allow for an expansion of scientific collaborations, increased numbers of scientific and medical learners, and access to the latest software to acquire and integrate imaging science with other patient information.”
The partnership with GE HealthCare will see St. Joseph’s become the first hospital in Canada to install the latest generation, state-of-theart PET-CT from GE, which will be delivered to St. Joseph’s Hospital by September 2023. The new PET-CT will mean faster exams, better patient experience, more detailed images and increased accuracy in diagnosing disease at a lower dose of radiation for patients. It will also expand clinical
care at St. Joseph’s by significantly enhancing research through the Imaging Research Group at Lawson, working together with researchers at LHSC, the London Regional Cancer Program, and Western University.
“We will leverage the combined scientific expertise and innovation of scientists from GE HealthCare and Lawson to maximize the future opportunities of molecular imaging theranostics made possible through PETCT imaging and be leaders in Canada in this area of medical science,” says Dr. David Hill (D.Phil), Lawson’s Scientific Director.
As a dedicated MIT centre of excellence, St. Joseph’s will…
• Advance innovation and expand the science in precision imaging of disease through Lawson, and broaden the potential of PET-CT imaging
• Develop new treatment options for patients with cancer and other diseases
• Examine how to maximize the opportunities of digital health technologies to improve access for patients across Canada and optimize their treatment journeys
• Create a knowledge dissemination hub for Canada to educate and train others in the use of advanced imaging technologies, including how to organize hospital services to maximize access to patients and improve the health care system for all Canadians.
“St. Joseph’s is proud to be in partnership with GE HealthCare on this exciting opportunity to transform the care journey and outcomes for patients with cancer and other diseases, not only locally and regionally, but also nationally,” says Roy Butler (PhD), President and CEO of St. Joseph’s.
For patients seen in London, the benefits will include expanded use of PET-CT, the ability to extract more information from their diagnostic images more rapidly and with less radiation exposure compared to current procedures, greater diagnostic and treatment accuracy, and new options for treatment, particularly for cancers that are more difficult to treat.

“A personalized approach to medical care requires a very detailed understanding of the localization of
disease and potential response to different treatment options,” says Dr. Paul who is also the Chair of Medical Imaging at Schulich School of Medicine & Dentistry at Western University. “We will be able to offer patients across our region access to the latest therapeutic options based on a deeper understanding of the nature of their individual disease conditions gained through next generation medical imaging.”
At its core, theranostics is about treating each patient as an individual, “recognizing that the same treatment plan doesn’t work for everyone – with the goal of providing more efficient and effective medical care,” adds says Mike Hamilton, President, GE HealthCare Canada. “This collaboration aims to advance this practice for the benefit of clinicians and patients around the world.”
The new PET-CT at St. Joseph’s will replace an aging machine and has been made possible in part through the generosity of donors to St. Joseph’s Health Care Foundation, which is contributing $1 million to state-ofthe-art machine. ■ H

Research Nova Scotia is investing an additional $1.1 million to test whether UV lights installed in longterm care (LTC) facilities will reduce respiratory viral infections (RVI) infections among LTC residents.
“The foundational work completed as part of a pandemic response has established Nova Scotia as a leader in this area of research world-wide,” says Stefan Leslie, CEO of Research Nova Scotia. “We now have access to better UV technology and have an updated understanding on how to ensure that it is completely safe. We are leveraging new information to expand our research into the role far-UVC can play in preventing infections in long-term care.”
Nova Scotia has the highest proportion of seniors in Canada. Elderly people who have multiple health problems are at higher risk of illness from RVIs. This is especially true for residents in LTC because the usual methods of infection control are sometimes difficult to manage and often residents do not show typical symptoms of infection, like fever.




This study is testing whether a safe form of ultraviolet light can be effective as an extra method of disinfection, in additional to manual cleaning, against airborne and surface viruses that can cause respiratory infections.
“In 2020 we began to develop a clinical trial of whether whole room, direct exposure of far-UVC light helps to prevent the spread of COVID-19,”
Quick Facts:
• In 2021, Research Nova Scotia invested $1.7 million in Dr. Rockwood’s clinical trial, one of 23 COVID-related research projects funded since 2020.
• Provincial funding for the project was allocated from the 50-million contribution to the Nova Scotia COVID-19 Response Council
• This research project is designed by Nova Scotia Health
• Phase 1 participating sites included Northwood’s Halifax Campus and Windsor Elms Village in Falmouth
• Phase 2 participating sites include Northwood’s Halifax Campus, Windsor Elms Village in Falmouth, and The Cove Guest Home in Sydney, Cape Breton
says Dr. Kenneth Rockwood of Nova Scotia Health, and the lead researcher on the project. “While vaccines effectively mitigated the spread of early SARS-CoV-2 variants, there is uncertainty surrounding future variants,
and we remain concerned about all RVIs which are the cause of significant harm and reduced quality of life for LTC residents.”
Recent laboratory and simulation-based research shows that not
only do far-UVC lamps significantly reduce the levels of airborne pathogens following single exposures, but the levels are also reduced even when infectious people remain present.

“This exciting research is helping us improve infection prevention and control strategies in our long-term care facilities and will enhance experiences of care for our residents and their families and caregivers,” says Dr. Gail Tomblin Murphy, Vice President of Research, Innovation and Discovery and Chief Nurse Executive at Nova Scotia Health. “The innovative nature of this work is a great example of how Nova Scotia is positioned to be a leader in the space of cutting-edge research on innovations, innovative technologies, and models of care in Canada and internationally. We are grateful for the contributions of Dr. Rockwood, who has made significant contributions as a world-leading researcher, innovator and as a clinician to enhance care and access for older adults in Nova Scotia.”
Dr. Rockwood and his research team hope to determine if this technology can serve as an effective infection control strategy in LTC. This next phase of the research uses the
latest in UV technology and has added a third LTC site. Not just a technology design experiment, this research has






















engaged with the LTC facilities and staff, residents, caregivers, and families from the beginning. This is novel and

ground-breaking research on a priority population in the province, nationally, and internationally. ■ H
Speci cally designed for elderly, fragile skin


The Centre for Aging + Brain Health Innovation (CABHI), powered by Baycrest, recently announced funding of over $1.9 million to support the development and validation of 40 innovations aimed at improving the quality of life for older adults, people living with dementia, and caregivers.
The funding is offered through CABHI’s Spark Program, which supports the development of grassroots innovations by frontline healthcare workers and researchers to solve real-world care challenges. Spark goes beyond providing financial support by offering coaching, mentorship, and networking opportunities, guided by CABHI’s team of experts, to ensure projects are poised for success, sustainability, and maximum impact.
The latest cohort features innovation projects covering CABHI’s priority themes of caregiver support, aging in place, care coordination and navigation, and cognitive and mental health. Nearly every province and territory across Canada is represented in this cohort, underlining the geographic breadth of CABHI’s impact on the country’s seniors’ care landscape. Projects are already underway and will continue to make advancements over the coming year.
Among the funded innovations:
• A first-of-its-kind low-cost, personalized, remotely managed virtual reality intervention program that can improve visual perception in older adults

• A dementia empathy training toolkit for care partners of people living with dementia
• A soft, flexible, and stretchable tactile sensor array for the prevention of pressure injuries
• A compact cycle ergometer to help maintain functional capacity in older adults
See the full list at cabhi.com/spark.
“Through the Spark Program, CABHI accelerates homegrown innovations to support Canada’s aging population. Healthcare workers and researchers hold a wealth of knowledge on the unique challenges faced by older adults, people living with dementia, and caregivers. Yet, they don’t always see themselves as innovators or entrepreneurs,” says Dr. Allison Sekuler, President & Chief Scientist at CABHI. “The Spark Program empowers these frontline care workers to translate their insights and grassroots ideas into early-stage innovations that improve the quality of life and wellbeing of older adults at their home organizations and beyond.”
“Together, with important partners like CABHI, we will keep supporting
innovations that help to improve the quality of life for older adults, people living with dementia, their families, and caregivers. Through this latest cohort of CABHI’s Spark program, there will be better support for caregivers, more support to help older adults age at home, improved care coordination and navigation, and healthier cognitive and mental health. These projects continue the implementation of Canada’s national dementia strategy to help improve the lives of so many Canadians,” said the Honourable Jean-Yves Duclos, Minister of Health.
“Ontario’s health care providers have key insights and hands-on experience that can make a powerful
difference in the quality of life for older adults,” said Jill Dunlop, Minister of Colleges and Universities. “That’s why our government is proud to support 40 innovative projects through CABHI’s Spark Program, tapping into the expertise of health care workers and researchers to ensure caregivers have the tools, resources and support they need to improve the wellbeing of their loved ones who are living with dementia.”
CABHI gratefully acknowledges the support of its funders: the Government of Ontario through the Ministry of Colleges and Universities, and the Government of Canada through the Public Health Agency of Canada. ■ H
While severe outcomes from COVID-19 have decreased with each new wave, a new study suggests the risk of cardiovascular (CV) hospitalization has persisted or increased – particularly for younger men, aged 18 to 45. The study was conducted by the Peter Munk Cardiac Centre at the University Health Network, ICES, and Women’s College Hospital.
Studies around the world have pointed to male sex, old age, and pre-existing health conditions as independent risk factors for increased severity of COVID-19 infection, disease and death.
“Initially, interactions between sex and certain health conditions were found to have a greater impact on women, who were more likely to expe-
rience severe outcomes like intubation or death,” says Bahar Behrouzi, MD/ PhD candidate at the University of Toronto, and study lead. “But there was no analysis yet of possible sex differences by age for severe outcomes, particularly in North America, that honed in on cardiovascular hospitalization.”
The retrospective cohort study, published in JACC: Advances, included almost all patients in Ontario with laboratory-confirmed SARS-CoV-2 infection during the first three waves.
The study showed that across all waves and in all age groups, men experienced higher rates of a severe outcome (e.g., requiring hospitalization for a cardiovascular complication, intensive care, a breathing machine, or dying) compared with women, although the magnitude varied by age.
While the difference between men and women in the risk of all-cause death was highest during Wave One – with young men at four-fold higher risk – younger men and women were at similar risk by Wave Three, which could be due in part to vaccinations and non-pharmaceutical interventions. However, for CV hospitalization, with each subsequent wave, there was little to no change in the increased risk borne by men versus women for all age groups. In general, across all waves, middle-aged men (ages 46 to 65) were at two- to three-fold higher risk compared to women of the same age.
“We know that adopting an ageand sex-informed approach to patient care has improved outcomes,” says Dr. Jacob Udell, cardiologist and
Anew pilot program at St. Michael’s Hospital provides mentorship to high school students from communities that are under-represented in the field of cardiac surgery, in the hopes of developing more diversity in the profession.

The Next Surgeon program, launched earlier this year by Unity Health Toronto and Toronto Community Housing, brought about 25 high school students into St. Michael’s to study cardiac surgery over the winter.Dr. Bobby Yanagawa, head of the Division of Cardiovascular Surgery, founded the program with medical school students Akachukwu Nwakoby and Lina Elfaki as a way to tackle the lack of diversity in the field.
“If you look at the cardiac surgeons across the country, only about 10 per cent are female, and we don’t have much ethnic diversity. Never in the history of this country have we had a
clinician-scientist at the Peter Munk Cardiac Centre, ICES, and Women’s College Hospital, University of Toronto, and principal investigator of the study. “Accounting for this variation in risk is especially crucial in early decision-making for patient treatment. Our findings suggest that in the first month after a positive COVID-19 test, patient care should be tailored to better prevent cardiovascular events, particularly among younger men.”
The findings highlight the need for further efforts to examine clinical, biological, psychosocial, and health system factors contributing to the growing disparity between the sexes in the risk of cardiovascular hospitalizations following COVID-19.

The study, “Sex-based differences in severe outcomes, including cardiovascular hospitalization, in adults with COVID-19 in Ontario, Canada” was published in JACC: Advances. ■ H
Black heart surgeon, and we’ve only had one Indigenous heart surgeon,” said Yanagawa.

“We want the best and brightest to become heart surgeons, and it’s my belief that talent is equally distributed in all people. If we’re only getting talent from one group of people, then we’re missing out on some brilliant future surgeons.”
At first, the three wanted to develop a program that would encourage more diversity at the residency level. They soon realized that if they wanted to be impactful, they had to start outreach earlier, said Yanagawa.
Through a contact at Toronto Community Housing, a group of interested high school students signed up to complete the program, which included mentoring, Q&A’s with prominent Black cardiologists and anesthesiologists, and a skills training, where students completed an online suturing course.

The students also met with Nwakoby and Elfaki, two Black medical school students, to hear about their journeys to medical school, and get tips and tricks about perfecting their university applications.
“Growing up, I was one of the few Black male students in my science classes in both high school and university. I rarely saw Black medical students and Black doctors, let alone Black cardiac surgeons,” Nwakoby said.
“I wanted the students to see that medicine and surgery is a very possible career path for them, despite being from an under-represented group. I also realize that by virtue of my background, I may share unique experiences with some of the students.”
Nwakoby credits his own mentors and a high school co-op placement he completed at Credit Valley Hospital with sparking his desire to become a physician. “My supervisor (at Credit Valley) was the only Black male in my department. He went above and beyond to make me feel integrated in the hospital,” he said.

Participating students said they enjoyed the program, and particularly valued the chance to speak with mentors who represented their communities.
“It was just very uplifting to be able to work with mentors who know how I feel and have gone through similar experiences as me,” one Grade 10 student told CBC News.
The program, which Yanagawa hopes to grow with the help of sponsors, also allowed participants to form new friendships with like-minded students who are also interested in science.
And as much as the students gained from the program, it was just
as rewarding for the physicians and mentors involved.
“Seeing the students ask thoughtful questions and attempt to sew simulated blood vessels re-kindled the spark I have for teaching and mentorship,” said Nwakoby. “It was also very rewarding to hear that some of them became interested in medicine and got accepted to their top university choices.” Yanagawa agrees.
“The kids always give you a lot of energy – energy that comes from their aspirations and dreams. It’s a wonderful feeling to contribute to that,” he said. “Oftentimes I would say that we adults got more satisfaction and joy from it than the students themselves.” ■ H
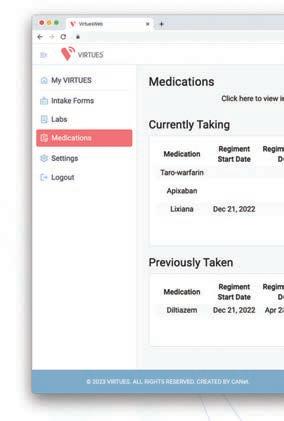

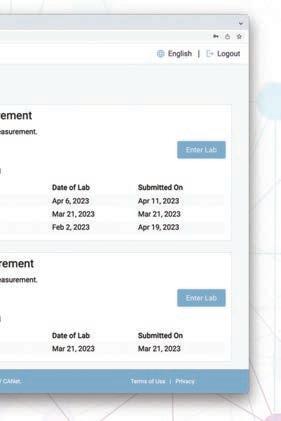
Educational Resources and implementation of CanadianClinical Practice Guidelines recommendations such thatthe clinicians and patients haveindividualized .





CANet provides innovative digital health solutions for the management of complex cardiovascular conditions.












Our vision is a transformed healthcare system, driving quality and affordable care for better cardiovascular health outcomes.
CANet’s digital health platform, VIRTUES, is a holistic, comprehensive digital health approach thatprovidesequity of care to meetthe needs of allpatients,regardless ofgeographical, cultural, orsystemic barriers.





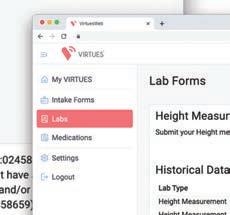













Learn more at www.virtues.care