



“The number one challenge we face is shortages.
There’s a ton of beds in the hospital – there’s beds lined up in the hallway. There’s tons of rooms. Tons of units.
But there’s actually no staff.”

Ontario deserves better.











“The number one challenge we face is shortages.
There’s a ton of beds in the hospital – there’s beds lined up in the hallway. There’s tons of rooms. Tons of units.
But there’s actually no staff.”

Ontario deserves better.






By Ivy Lynn Bourgeault and Sarah Simkin
It is welcome news that Conservative Premier Doug Ford has appointed Dr. Jane Philpott, former federal Liberal Health Minister to lead a new primary care action team in Ontario. This cross-partisan effort to solve the primary care crisis in the province is exactly the kind of ‘roll-upthe-sleeves’ approach we all need.
Will it be enough?
Every province and territory in Canada needs a dramatic reformation of the health system to help right our sinking primary healthcare ship. If anyone can fulfil this challenging mandate, Dr Philpott can make it happen. For truly sustainable change, she must prioritize robust health workforce planning.
Primary care refers to routine, regular health care and is the first point of contact an individual has with the health system – usually through a family doctor or nurse practitioner – but better yet, with an integrated healthcare team.
Dr. Philpott’s mandate is to make sure everyone in Ontario is connected to primary care within five years. This is no easy task. A new report released by the Canadian Institute of Health Information (CIHI) details how 12 to 27 per cent of adults across Canada are not attached to a primary care provider.
As more family doctors retire, this situation is likely to get worse.
JANUARY 2025 ISSUE
EDITORIAL: Dec. 6
ADVERTISING:
Display – Dec. 13 | Material – Dec. 17
Monthly Focus:
Healthcare Human Resources/Continuing Medical Education (CME)/Staffing: Continuing Medical Education (CME) for healthcare professionals. The use of simulation in training.Human resource programs implemented to manage stress in the workplace and attract and retain healthcare staff. Health and safety issues for healthcare professionals. Quality work environment initiatives and outcomes.
+ PROFESSIONAL DEVELOPMENT SUPPLEMENT
High rates of burnout, turnover, and retreat from the primary care system in whole or in part have resulted in more limited access, forcing patients to seek care in emergency departments and resulting in longer wait times. Service closures due to lack of staff are becoming commonplace. These issues, which have been longstanding in rural Canada, are starting to impact urban communities.
A variety of solutions to this multilayered crisis have been suggested.
Some advocate recruiting health workers from other countries. But this is ethically questionable, as these countries have urgent sinking ships of their own.
Others suggest the creation of a few private healthcare ‘lifeboats’ for select services – or for those who can pay for those services privately. But this will result in health workers leaving the ‘Titanic’ public healthcare system to take on more water with fewer crew.
These ‘solutions’ ignore how many of the problems we are experiencing are a result of either a complete lack of planning for the health workforce we need to meet patient and population needs or fundamental flaws in the approaches taken thus far, which tend to be isolated attempts focused on single professions and done behind closed doors with limited and inadequate data.
Continued on page 6
EDITORIAL: Jan. 8
ADVERTISING: Display – Jan. 24 | Material – Jan. 28
Monthly Focus:
Gerontology/ Public Health and Preventive Medicine/Rehabilitation/Wound Care: Geriatric medicine, aging-related health issues and senior friendly strategies. Developments in rehabilitation techniques for a variety of injuries and diseases. Effective approaches for disease prevention and health promotion. Innovation in the treatment and prevention of wounds.
+ WOUND CARE SUPPLEMENT
THANKS TO OUR ADVERTISERS Hospital News is provided at no cost in hospitals. When you visit our advertisers, please mention you saw their ads in Hospital News.
610 Applewood Crescent, Suite 103 Vaughan Ontario L4K 0E3 TEL. 905.532.2600|FAX 1.888.546.6189
www.hospitalnews.com
Editor Kristie Jones editor@hospitalnews.com
Advertising Representatives
Denise Hodgson denise@hospitalnews.com
Publisher Stefan Dreesen stefan@hospitalnews.com
Accounting Inquiries
accountingteam@mediaclassified.ca
Circulation Inquiries info@hospitalnews.com
Director of Print Media
Lauren Reid-Sachs
Helen Reilly, Publicist Health-Care Communications
Bobbi Greenberg, Health care communications
Sarah Quadri Magnotta, Health care communications
Dr. Cory Ross, B.A., MS.C., DC, CSM (OXON), MBA, CHE Vice President, Academic George Brown College, Toronto, ON
ASSOCIATE PARTNERS:

Hospital News is published for hospital health-care professionals, patients, visitors and students. It is available free of charge from distribution racks in hospitals in Ontario. Bulk subscriptions are available for hospitals outside Ontario.
The statements, opinions and viewpoints made or expressed by the writers do not necessarily represent the opinions and views of Hospital News, or the publishers.
Hospital News and Members of the Advisory Board assume no responsibility or liability for claims, statements, opinions or views, written or reported by its contributing writers, including product or service information that is advertised.
Changes of address, notices, subscriptions orders and undeliverable address notifications. Subscription rate in Canada for single copies is $29.40 per year. Send enquiries to: subscriptions@ hospitalnews.com
Canadian Publications mail sales product agreement number 42578518.

By Megan White
ccurately predicting when a patient will be ready to go home is at the centre of every effective discharge plan ensuring patients have a smooth transition from hospital to home.
Getting this timing right allows the patient’s family or care partners to prepare for their arrival home and helps staff with coordinating timely community and home supports.
But knowing exactly when a patient can go home, historically, has been informed by clinician estimations rather than real-time data.
“Traditionally, clinicians estimate patient discharge times during rounds or morning huddles,” explains Teresa O’Callaghan, executive director, Abbotsford Regional Hospital and Mission Memorial Hospital. “While clinicians are experienced, human estimations can be inaccurate. This unpredictability makes planning difficult.”
Now, thanks to an innovative artificial intelligence (AI) solution developed by Fraser Health’s Centre for Advanced Analytics, Data Science and Innovation (CAADSI) team, staff have a more precise idea of when a patient will be ready for discharge.
“Using the AI predictive discharge model, our staff and medical staff are able to see on any given day who could be ready to go home within 24 hours,” explains Teresa O’Callaghan. “This helps our staff plan and makes the discharge process smoother and more efficient.”
This custom AI model combines classical demand forecasting and generative AI to analyze more than 72 variables, including clinical data, patient history, vital signs and unstructured case notes, forecasting discharge readiness within 24 hours.
Prior to integrating the AI model into the electronic health record and deploying at Fraser Health’s 12 hospital sites, it was trained on 100,000 patient records from two years of real data and tested over two months using a third year’s data. When comparing the tool’s predictions with the actual experience in discharges, the AI’s

“USING THE AI PREDICTIVE DISCHARGE MODEL, OUR STAFF AND MEDICAL STAFF ARE ABLE TO SEE ON ANY GIVEN DAY WHO COULD BE READY TO GO HOME WITHIN 24 HOURS.”
discharge predictions achieved 86 per cent accuracy. This is four times more accurate than the traditional process which relied on human estimates.
“We took an agile approach, experimenting alongside clinical teams with how best to integrate the tool into clinical workflows,” says Sheazin Premji, executive director, CAADSI.
According to Premji, the inputs to the AI model were meticulously chosen through extensive research involving physicians, nurses, scientific literature and an assessment of Fraser Health’s data availability and data quality. Inputs include patient information such as age, gender, medical history and recent lab results, among others.
“This partnership allowed the AI model to evolve iteratively based on real-world clinical insights, reinforcing that AI thrives on continuous refinement and adaption, rather than being a one-and-done effort.”
Staff and medical staff can now access these predictions through a live dashboard, which is embedded into their current daily workflow.
This dashboard and the discharge prediction tool have proven highly
effective. Prior to implementing the AI, hospital staff might achieve 250 to 300 discharges a day, across the region. Now, with the help of this tool, it is not unheard of to complete 600 discharges in a single day.
Discharging patients as soon as safely possible is important. Patients
recover best at home in familiar surroundings where they can rest. Plus, their risk of hospital-acquired infections is reduced the earlier they leave the hospital. Discharging patients also frees up hospital beds and resources for other patients who need care.
The AI solution delivers daily, patient-level discharge probability predictions, enabling proactive discharge planning, early identification of barriers and efficient resource allocation. This innovative approach enhances care and improves patient outcomes. It’s important to note that the patient’s care team ultimately has the final say on whether the discharge plan is appropriate.
AI can uncover subtle data relationships that may not be immediately apparent to clinicians, capturing complex patterns across numerous variables and a large volume of data. This complements clinical expertise, enhancing the accuracy of discharge predictions by leveraging the vast amount of patient data available.
This success exemplifies Fraser Health’s digital health strategy in action, showcasing how the health authority is transforming health care through technology. n H

ffordability in Canada affects not just groceries but also medications, with 1 in 20 people unable to take their medications as prescribed because of cost, found new research published in CMAJ (Canadian Medical Association Journal).
Prescription medications are not universally covered under Canada’s 13 provincial and territorial health insurance systems. In 2021, Canadian households paid more than $7.4 billion out of pocket for prescription medications.
The study, which included a nationally representative sample of more than 223 000 respondents over age 12, was conducted to better understand the burden of prescription costs in Canada. One in 20 (5%)
Continued from page 4
respondents reported cost-related nonadherence, meaning they skip or reduce dosages, delay refilling prescriptions, or do not fill prescriptions at all because of out-of-pocket costs.
The authors found that females were 44 per cent more likely to report cost-related problems than males, as were bisexual, pansexual, and questioning individuals (43%).
“Our findings show that intersections of personal, health, and health care system factors affect whether people in Canada skip or cut back on medications because of cost. We saw this pattern in the overall population and in both males and females when looking at them separately,” says Dr. Mary De Vera, a pharmacoepidemiologist and associate professor in medication adherence in the Faculty of Pharma-
So, what is needed?
First, planning should start with patient and community needs. Once we know what services are needed, now and into the future, we can plan to deploy health workers who can provide those services.
Second, planning should take an interprofessional approach. Because healthcare is delivered in teams, it is necessary to consider all the providers involved in primary care – from family doctors and nurse practitioners to pharmacists, physiotherapists, psychologists and beyond.
Third, planning should be transparent and inclusive. It is stronger when all those involved in training, regulating, employing and supporting health workers bring their knowledge of important factors influencing the capacity of the workforce to planning tables.
Fourth, planning needs to take the whole lives of health workers into
consideration; factors such as age and gender matter. Most health workers in Canada are women and as well as caring for folks at work, they also disproportionately provide care at home.
Most importantly, planning should be an ongoing activity, embedded into health system processes and decision-making. Leading practices strongly encourage nurturing a culture of planning which allows for course correcting when needed and improves systems over time.
There are ongoing initiatives that have undertaken just such open, collaborative and interprofessional approaches, bringing needed data to assist those who make day-to-day decisions. Let’s scale these promising practices and bring together collaborative tables with improved data and robust tools for primary care planning.
Canadians deserve to know where we’re headed on this primary care ship and how we’re going to get there. n H
Dr. Ivy Bourgeault is a Professor in the School of Sociological and Anthropological Studies at the University of Ottawa and leads the Canadian Health Workforce Network. Dr. Sarah Simkin is a Family Practice Anesthetist and the health workforce planning co-Lead of the Canadian Health Workforce Network.
ceutical Sciences at University of British Columbia and Arthritis Research Canada, Vancouver, BC.
Race and ethnicity were also associated with prescription affordability, with Indigenous, Latin American, West Asian, Arab, Black, and multiracial people having 20%–67% higher odds of nonadherence. People aged 18–34 years were 9 times more likely to report cost-related nonadherence than adults aged 75 years and older.
People living in Quebec were least affected by prescription costs, as each province has its own drug insurance program.
“The lack of national standards for these programs has led to interprovincial disparities in public drug coverage related to eligibility, premiums, and cost-sharing policies (e.g., deductibles, co-payments, out-of-pocket limits) and has created the need for financing of prescription drugs via private insurance and out-of-pocket costs incurred by patients,” says Nevena Rebi, a postdoctoral fellow at the University of Toronto who led the analysis.
Previous studies have been restricted to specific populations or a narrow time frame, whereas this study is more comprehensive and includes data from 5 iterations of the Canadian Community Health Survey from 2015 to 2020.
The authors suggest that these findings can help inform public drug coverage plans, premium amounts, and other ways to reduce financial barriers to prescription medications in Canada. In October 2024, Canada took concrete steps to ensure a national pharmacare program, as it became law under Bill C-64.
“As an initial step toward full national pharmacare, it is a laudable achievement,” writes Dr. Matthew Stanbrook, deputy editor, CMAJ, in a related editorial. “Yet the legislation is low on substance, high on promises and aspirations, and vulnerable to political change. This leaves people living in Canada mired in uncertainty as to when or whether they will have the guaranteed access to medications and therapies, regardless of ability to pay, that citizens of almost all other countries with a public health care system receive.”
He urges the federal government and people of Canada to ensure that pharmacare is extended in the future.
“Predictors of cost-related medication nonadherence in Canada: a repeated cross-sectional analysis of the Canadian Community Health Survey” and “The first, fragile foundations of national pharmacare in Canada” was published November 25, 2024. n H
Outdated recommendations from the Canadian Task Force on Preventive Health Care on prostate cancer screening negatively affect the health of many Canadians, especially men at higher risk. The Canadian Urological Association (CUA), which represents urologists and urologic-oncologists across Canada, is calling on the federal government to take urgent action to correct course and shift the focus to effective prevention.
“We need to take a practical approach to prostate cancer screening,” said Dr. Ricardo Rendon, President of the CUA. “Men with risk factors for prostate cancer should be screened at an earlier age. Based on some current screening guidelines, we often see men diagnosed with late-stage prostate cancer that could have otherwise been detected and treated at an early stage.” Urologists, surgeons who diagnose and treat prostate cancer among other conditions, were not adequately consulted in the development of initial recommendations. Urologists need to play a central role in the implementation of new guidelines that focus on prevention, reflect the real health needs of Canadians, and are informed by experts. n H
An updated evidence-based guideline aimed at helping clinicians and other health care providers manage patients with opioid use disorder recommends buprenorphine and methadone as first-line treatments. The guideline is published in CMAJ (Canadian Medical Association Journal).
Opioid use and opioid use disorder are the leading causes of drug-related deaths worldwide, and Canada has seen a 184% increase is opioid-related deaths over 7 years from 2831 deaths in 2016 to 8049 deaths in 2023. Treatment options have improved with the removal of methadone prescribing restrictions in 2018 in Canada, but opioid-related harms continue to rise.
The recommendations, based on new research since the previous guideline was published, include the key change that opioid agonist treatment with buprenorphine–naloxone is no longer the sole first-line treatment and methadone is now also recommended as a first-line option.
The update is aimed at physicians, nurse practitioners, pharmacists, clinical psychologists, social workers, medical educators, clinical care case managers with or without specialized experience in addiction treatment, and other allied health care professionals who provide care for people with opioid use disorder.
done can be used as standard firstline treatment options for opioid agonist therapy
• Slow-release oral morphine can be used as second-line treatment
• Avoid withdrawal management as stand-alone treatment and ensure long-term management to ensure safety and well-being of people with opioid use disorder
• Psychosocial treatments and supports, such as therapy, should be offered as additional approaches but should not be mandatory nor prevent access to opioid agonist therapy
• Pregnant people can be offered buprenorphine or methadone as treatment options
provinces update their approaches to managing opioid use disorder to help Canadians.
“Too many people die from untreated opioid addiction in Canada,” says Dr. Peter Selby, Centre for Addiction and Mental Health and the University of Toronto. “We have medicines that help people stop using but too few are treated due to stigma and lack of prescribers knowing what to do. These national guidelines help them use proven medications to not only prevent death but actually help people recover.”
Find the full guideline, with an easyto-use table of recommendations and an infographic here.
• Buprenorphine (also refers to buprenorphine–naloxone) and metha-
“Opioid use disorder and opioid related harms have devastating outcomes for our communities across Canada and with the growing dangers associated with the illicit market, we need to ensure we are sharing the most relevant therapeutic tools and up-todate knowledge to help providers and communities address this complex issue,” says Dr. Ginette Poulin, a family physician, University of Manitoba, Winnipeg, Manitoba.
The guideline, an update to the 2018 national guideline for the clinical management of opioid use disorder from the Canadian Research Initiative in Substance Matters, focuses on oral treatments and includes special considerations for pregnant people. Injectable opioid agonist therapy, extended-release agonists, and antagonists are beyond the scope of this guideline.
“The management of opioid use disorder is a rapidly changing and ever-evolving landscape of new research and clinical considerations,” says lead author Dr. Igor Yakovenko, associate professor, Department of Psychology and Neuroscience and Department of Psychiatry, Dalhousie University, Halifax, Nova Scotia. “This guideline provides an important update to health practitioners on the latest science in the field so that Canadian providers can continue to maintain a high standard of evidence-based care.”
Canada needs to support current and future rural physicians to ensure rural areas have stable rural generalist physicians who can care for patients in these areas, authors write in an analysis in CMAJ (Canadian Medical Association Journal).
This is important for trainees, rural physicians, and, of course, patients.
“As the rural physician workforce becomes more unpredictable and dependent on locum coverage, not only do rural communities lose essential access to health care services, but medical students have increasingly limited opportunities to train in rural areas because of a lack of clinical preceptors,” writes Dr. Sarah Newbery, a family physician in Marathon, Ontario, and assistant dean, Physician Workforce Strategy, NOSM University, with coauthors.
This support includes the following:
• Ensuring contracts for rural physicians include time for teaching, academic activities, and support for professional development
The authors hope that the guideline will provide evidence-based treatment for opioid users and recommend that
“Management of opioid use disorder: 2024 update to the national clinical practice guideline” was published November 12, 2024. n H
• Access to team-based care with addictions counsellors, physiotherapists, pharmacists, social workers, home care nurses, and more
• Locum support for taking leave, whether for vacation, parental leave, elder care, or illness
• Flexible work hours, manageable call schedules, and other aspects that allow a work–life balance and prevent burnout
Governments, medical schools, and local health authorities need to adapt to medicine in the modern era and expand support for rural medicine.
“Generalist funding models need to reflect the realities of current rural practice. This includes turn-key infrastructure (i.e., no need to buy in to the clinic or fund the clinic capital costs) and funding models that ensure that the physician can focus on clinical care and teaching with reasonable workload expectations. The notion of running the business of the practice is no longer appealing for new graduates, nor is it the best approach for clinical academic settings,” write the authors.
Evidence shows that relationships and community connections are key to retaining rural physicians. Communities involved in physician recruitment have better health care and physician retention. With the shortage of physicians in Canada, international medical graduates can help fill gaps, and aiding integration of these professionals into the local community can help ensure they are connected locally.
“Strengthening the culture of rural generalism in Canada is an essential foundation to attract and retain physicians to work in rural areas and adequately mentor medical students, postgraduate trainees, and internationally trained physicians for rural practice.”
The authors suggest that a shared commitment from medical schools, licensing bodies, and provincial and local health systems is key to helping ensure the health of the rural health system.
“Supporting future and current rural physicians” was published November 18, 2024. n H
By Lise Diebel
new and unique partnership between Hamilton Health Sciences (HHS)’ Juravinski Hospital and Cancer Centre (JHCC) and the Grand River Regional Cancer Centre (GRRCC) is keeping treatment close to home for certain blood cancer patients. The partnership makes it possible for patients in Kitchener, Waterloo and Wellington to receive an autologous stem cell transplant, which uses cells from their own body, at Kitchener’s Grand River Hospital instead of travelling to Hamilton for this highly specialized, intensive, multi-day treatment.
This partnership is the first of its kind provincially, and could lead to other community hospitals with regional cancer programs offering stem cell transplants with support from large academic hospitals like HHS.
The JHCC is a leader in adult stem cell transplant and cellular therapy, and home to one of the largest and most comprehensive regional cancer programs in the province.
The JHCC’s cellular therapy and transplant team spent two years working with Grand River to train their team in providing autologous transplants, which are used to treat patients with multiple myeloma or lymphomas. With this type of transplant, healthy stem cells from the patient’s own body are used to help the body recover from high doses of chemotherapy.
As part of this process, healthy blood cells are removed and collected before high doses of chemotherapy are administered to kill cancerous cells. Healthy cells are then introduced back into the body through the transplant process to promote recovery.
“Providing today’s specialized and highly complex cancer treatments re-

Dr. Kylie Lepic is medical director of HHS Juravinski Hospital and Cancer Centre’s cellular therapy and transplant program. Her team spent two years working with the Grand River Regional Cancer Centre to train their team in providing autologous stem cell transplants. This partnership is the first of its kind provincially.
quires teamwork and collaboration of hospitals, physicians, clinical staff and patients,” says Dr. Kylie Lepic, medical director of JHCC’s cellular therapy and transplant program.
“Stem cell transplants require that collaboration to meet strict regulatory requirements and to ensure the safety and effectiveness of the treatment. We are pleased to see the autologous stem cell transplant program at Grand River launch successfully after so much preparation. It’s a true partnership.”
The GRRCC performed its first successful transplant in July, in partnership with the JHCC team, and with the support and endorsement of Cancer Care Ontario, an agency created by the province to connect and coordinate Ontario’s health care system.
“We’re happy to report that everything went to plan and that the patient is doing exceptionally well,” says Dr. Janet MacEachern, a hematologist-oncologist and medical director of transplantation and cellular therapy for GRRCC.
This procedure marks the completion of the first phase of the transplan-
tation and cellular therapy program at GRRCC.
Grand River is the seventh hospital in Ontario to provide autologous transplants. The other six are large academic hospitals: Hamilton Health Sciences (at the JHCC), University Health Network in Toronto, Ottawa Hospital, London Health Sciences Centre, Kingston Health Sciences Centre, and Health Sciences North in Sudbury.
The benefits of expanding to community hospitals such as Grand River include patient convenience, since it’s common for Ontario residents needing a stem cell transplant to travel hundreds of kilometres for this procedure at a large centre.
Expanding to other hospitals would also help build provincial capacity since demand for autologous stem cell transplants is growing. That’s partly because people are living longer, so more and more Ontario residents are being diagnosed with multiple myeloma or lymphomas.
Also, innovations in treatment mean that an increasing number of multiple myeloma or lymphoma patients are qualifying for transplants. Expansion would help meet the growing demand.
The JHCC’s cellular therapy and transplant team provided training to GRRCC team members including hematologists, nurses, lab staff and quality managers for two years to help them build the specialized skills and treatment pathways needed to perform transplants.
The JHCC’s contributions also included site visits, logistical meetings, educational sessions, and simulated transplants. The JHCC team continues to be a resource for their GRRCC colleagues and partners with them in providing patient care.
While Kitchener-area patients still visit JHCC for consultation, the bulk of their treatment is carried out at GRRCC. For example, through this partnership, patients qualifying for a stem cell transplant meet with a JHCC transplant physician in Hamilton. This specialist creates their treatment plan, and their healthy cells are collected and processed in Hamilton. The collection process can take one to three days. The patient’s processed, healthy cells are couriered to Kitchener to await transplant.
The remainder of treatment happens in Kitchener, including intensive chemotherapy leading up to the transplant to kill diseased cells, as well as the transplant itself, and follow-up care.
“This is a monumental milestone for cancer care for Waterloo-Wellington and beyond,” says Jane Martin, the GRRCC’s vice president.
“The transplantation and cellular therapy program not only supports the overall provincial health care system, it also ensures that patients receive the care they require without the need to travel out of region.” n H
Scientists at UHN’s Toronto General Hospital Research Institute (TGHRI) have developed an improved method for evaluating the performance of artificial intelligence (AI) models across various health care settings.
As health care datasets become larger and more complex, the use of AI for the analysis of these datasets is gaining traction.
Medical information can take the form of unstructured data such as medical images, electrocardiograms (ECGs), and text from clinical notes. Despite advancements in AI that have produced tools capable of analyzing medical images and clinical language, it remains challenging to predict their effectiveness in different health care settings without testing on new and varied data from each setting.
“For AI tools to be truly safe and effective for patient care, they must perform reliably across different situations and patient groups, a concept known as generalizability, which requires accurate performance estimation,” says Cathy Ong Ly, doctoral student at TGHRI and co-first author of the study.
“We sought to address this challenge of estimating AI model accuracy by analyzing 13 datasets across dif-


ferent modalities such as X-rays, CT scans, ECGs, clinical notes, and lung sound recordings.”
When the team tested various AI models on this data, they found that their performance was often overestimated by about 20 per cent on average.
“We propose that this overestimation is due to data acquisition bias (DAB), a natural occurrence when data for these studies is retrospectively collected from regular medical care,” says Dr. Chris McIntosh, a scientist at TGHRI and senior author of the study.
“Generally speaking, AI might focus on irrelevant patterns in the data instead of what really matters for the task,” adds Dr. McIntosh,” who is also an assistant professor in the Department of Medical Biophysics at the University of Toronto (U of T).
“Different hospital departments may use different equipment or settings and have different patient acquisition conditions,” says Dr. McIntosh,
who also holds the Chair in Artificial Intelligence and Medical Imaging at the Joint Department of Medical Imaging at UHN and the Department of Medical Imaging at U of T. “These variations, which might be imperceptible to researchers and clinicians, can be detected by AI algorithms.
“When models are trained on this data, they might rely on these subtle differences – like how a medical image was taken – rather than the actual medical content, to make predictions.”
An example of this bias is how patients suspected of having interstitial lung disease are often directed towards specific imaging techniques meant to confirm the diagnosis, while those without suspicion get more general scans.
The algorithm will appear highly accurate at the hospital the data was trained on, but when deployed for clinical care at another hospital with different scanners, the accuracy will drop, potentially putting patients at risk.
To address this issue, the researchers developed and proposed an opensource accuracy estimate called PEst that corrects for bias and provides more accurate estimates of a model’s external performance.
“Our method, which corrects for hidden patterns and biases in the data, predicts models performance on new datasets with an accuracy margin within four per cent of the actual results,” says Balagopal Unnikrishnan, doctoral student at TGHRI and co-first author of the study.
Given how crucial the accuracy of AI models is in health care, where recommendations can significantly impact patient outcomes, these findings will help enable safer and more widespread use of AI and support the development of new medical AI technology.
This study was a truly multidisciplinary effort across UHN to measure the impact of these biases in a diverse array of modalities and diseases. n H
This work was supported by the Natural Sciences and Engineering Research Council of Canada (NSERC), The Princess Margaret Cancer Foundation, and UHN Foundation. Data for this study was supported by foundation investments in the Digital Cardiovascular Health Platform including UHN’s Peter Munk Cardiac Centre and Ted Rogers Centre for Heart Research and MIRA through Cancer Digital Intelligence. Dr. Chris McIntosh is an Assistant Professor in the Department of Medical Biophysics at the University of Toronto (U of T). He holds the Chair in Artificial Intelligence and Medical Imaging at the Joint Department of Medical Imaging at UHN and the Department of Medical Imaging at U of T.
By Deb Galet
s Canada faces the challenges of an aging population, Baycrest, like many of its partners, is managing present-day demand while keeping an eye on the future of dementia care and how to best serve the changing needs of the communities we serve as the prevalence of dementia continues to surge.
The Alzheimer Society of Canada’s report, Navigating the Path Forward, estimates that over 600,000 Canadians currently live with dementia – a number expected to double by 2050. This growth will pressure our healthcare systems, caregivers, and communities.
In Ontario alone, the healthcare system is already straining to meet the rising demand, according to a recent submission by Provincial Geriatrics Leadership Ontario (PGLO) to the Ontario Standing Committee on Social Policy that notes home care needs and hospital admissions for individuals with dementia are climbing rapidly.
There is also the financial impact of dementia on our health care system, which is staggering. Individuals with dementia and comorbidities represent one of the most expensive care groups in Ontario. In 2019, within the two Ontario Health Teams (OHTs) Baycrest participated in, care costs for this population totalled $155 million. Across the province, these costs are estimated to reach billions annually.
Beyond economics, the emotional toll on families and caregivers is immeasurable. Many caregivers face burnout, financial hardship, and declining mental health as they navigate the complexities of providing care. The CBC recently reported that the growing demand for home care and the increasing cost of healthcare services risk overwhelming our current system unless transformative immediate action is taken.
Both the immediate and longer-term needs of treating people living with dementia are at a critical point, and coordinated action at every level – personal, organizational, and governmental–is required to ensure a brighter future for people living with dementia and their families.
At Baycrest, we are acutely aware of this challenge and are stepping up as leaders in dementia care, research, and advocacy.
For more than a century, Baycrest has been at the forefront of demen tia care and research. Today, we are amplifying our efforts through an en hanced strategic focus on dementia, aiming to lead innovative approaches to care and support.
Our recently released strategic plan for 2024-2029, entitled Exceptional Aging powered by Baycrest, embodies our passion and underscores our com mitment to providing an extraordinary aging experience. It also signifies our dedication to enhancing the quality of life for older persons, ensuring they live with purpose, fulfillment, and dig nity. It also focuses on the future and our aspirational goals: transforming the perception of aging and highlight ing the potential for growth, learning, and joy in every stage of life.
We are bringing our strategic plan to life through Baycrest’s Virtual Be havioural Medicine program (VBM), one example of recent innovation de signed to improve dementia care.
VBM helps individuals living with dementia promptly access highly specialized care while re maining in their homes. VBM works by ensuring patients who
Deb Galet is the Interim President and CEO, Baycrest Hospital and Long-Term Care
exhibit these behaviours receive appropriate pharmacological and non-pharmacological interventions. This program has not only proven to reduce pressure on acute care hospital beds but has also avoided unnecessary and upsetting changes in patients’ physical environments. It has also created capacity throughout rural areas of the province for patients requiring this level of care.
VBM showcases how Baycrest fos-
has the care, support and resources they need, both now and in decades to come.
Addressing the dementia crisis requires a multi-pronged approach. Governments must invest in health system infrastructure, caregiver support, and affordable long-term care options. Organizations like Baycrest must continue leading research and innovation while directly supporting individuals and families. Communities and individuals can also play a role by fostering inclusivity and awareness.
As we forge ahead, it is essential to recognize dementia is not just a challenge – it is an opportunity for us to redefine how we care for our aging population. At Baycrest, we remain unwavering in our vision to build a

It’s impossible not to smile when George is around. That’s because he’s usually playing a guitar and singing a song. And at 99 years of age, he’s been doing that for a long time.
At Christie Gardens, we celebrate George—his career, his personality and his incredible musical gift. A gift that is shared, and received, with joy.



By Shahana Gaur
s we look to the future of healthcare, Humber River Health (Humber) stands at the forefront, transforming healthcare into a modern, innovative, and inclusive experience. The organization does not just aim to provide quality healthcare – they are reshaping it to meet the needs of their community through technological advancements, strategic partnerships, and a patient-centric approach. At Humber, the future of healthcare is not just a distant goal; it is here today.
Innovation is embedded in Humber’s DNA. As North America’s first digital hospital, they have harnessed technology to streamline workflows, enhance safety, and improve the patient experience. Their state-of-theart Command Centre, the first of its kind in Canada, optimizes care delivery by using real-time data and artificial intelligence to manage patient flow and prevent delays.
Organizations and fellow hospitals from around the world visit Humber to tour its advanced facility and explore other innovative practices. These visits allow them to learn from Humber’s ground-breaking approaches, often inspiring the implementation of similar advancements within their own facilities to enhance efficiency, safety, and patient care.
Humber’s embrace of robotics exemplifies how technology can redefine patient outcomes. With the Da Vinci surgical robot and the ROSA® knee system, Humber leads in minimally invasive techniques, allowing patients to recover faster with fewer complications. Recently, they performed Toronto’s first fully robotic bladder cancer surgery, demonstrating their commitment to being a pioneer in surgical innovation.
Safety is at the core of Humber’s commitment to providing the highest quality care for its patients and staff. In recent years, Humber has made remarkable strides in enhancing patient safety and clinical outcomes, as Humber’s safer care numbers are more than 60 per cent better than the average of all Ontario and Canadian hospitals, and have maintained this for the last 6 years. In addition, a 10 per cent yearover-year reduction in sepsis cases, a 40 per cent year-over-year decrease in code blues, and a medication error rate of 0.009 per cent.
As one of Ontario’s busiest cardiology centres, Humber is committed to expanding access to essential cardiac care in their community. Their plans for a state-of-the-art Cardiac Catheterization (Cath) Lab will provide critical diagnostic and treatment services to their patients without needing transfers to other hospitals, eliminating delays and reducing risk. The addition of this Cath Lab will also support their expanded device clinic, including an Implantable Cardioverter Defibrillator (ICD) program, which will bring lifesaving services closer to home for their patients.
In their nephrology program, Humber is at the forefront of personalized kidney care, performing over 62,000 hemodialysis treatments annually and supporting home hemodialysis at rates significantly above the provincial average. Humber was one of the first hospitals in North America to establish a nocturnal home dialysis program, allowing patients the freedom to live independently while receiving essential treatment. With initiatives such as the Glomerulonephritis (GN) Clinic and the Transition Care Unit (TCU), Humber is delivering comprehensive kidney care, where patients are managed within their own community.

To further strengthen their community impact, Humber launched their first Ambulatory Strategic Plan, which enhances their outpatient services to provide care closer to home. This strategy emphasizes equitable access to a full spectrum of services, from preventative care to complex treatments. With a focus on local partnerships, their 2023-2026 Ambulatory Strategic Plan enables them to deliver high-quality care in a setting that is both accessible and convenient for their patients. This approach addresses higher disease prevalence in their region, ensuring that patients can receive care in a familiar, community-based environment.
Humber’s Finch Campus is home to The HUB@2115, a visionary project launched by the North Western Toronto (NWT) Ontario Health Team (OHT), addressing barriers to healthcare access by integrating health and social services in a single, centralized location. This “one-stop shop” for mental health support, diabetes education, employment services, and more, is designed to meet the needs of North Western Toronto’s diverse and underserved population. By consolidating crucial services under one roof, The HUB@2115 not only reduces wait times, but also helps patients navigate what can often feel like a fragmented system.
Humber’s commitment to addressing the shortage of primary care providers in their community is evident with the Schulich Family Medicine Teaching Unit (FMTU). As an official teaching site for the University of Toronto’s Family Medicine Residency Program, the Schulich FMTU provides specialized training for first and second-year medical residents while helping their underserved community. This initiative is expected to address the needs of over 10,000 unattached patients by 2026, helping to close the gap in access to primary care.
As they continue to innovate and expand their services, Humber River Health remains steadfast in their mission to provide high-quality, equitable, and accessible healthcare. The future of healthcare lies not only in technological advancements but also in ensuring these advancements improve care outcomes and enhance the patient experience. At Humber, they are building this future every day, empowering their community and healthcare providers alike.
At Humber River Health, we’re finding a cure for healthcare. Learn more at HealthcareLives.ca. n H
landmark study published in The New England Journal of Medicine has demonstrated the superiority of catheter ablation over antiarrhythmic drug therapy for patients with ventricular tachycardia, a potentially life-threatening heart rhythm disorder. Conducted by the VANISH2 Study Team with funding from the Canadian Institutes of Health Research and the Cardiovascular Network of Canada (CANet), this research represents a significant advancement in arrhythmia management. It highlights the role of Canadian innovation in global healthcare.
The international study compared the standard treatment for suppressing these dangerous rhythms with antiarrhythmic drugs against catheter ablation, a minimally invasive procedure that targets and neutralizes abnormal heart tissue causing short circuits in the electric system of the heart. Results showed that catheter ablation reduced the incidence of recurrent arrhythmias and death more effectively than drug therapy. Furthermore, patients undergoing ablation did not have an increase in severe side effects, highlighting its potential to improve the quality of life for those battling ventricular tachycardia.
Focusing on safety and efficacy, the VANISH2 team noted that ablation provides long-term benefits by directly addressing the underlying electrical disturbances in the heart. These findings suggest a paradigm shift in treatment approaches, positioning catheter ablation as a preferred first-line therapy for many patients.
“Our findings demonstrate that catheter ablation should be considered a reasonable first-line treatment for ventricular tachycardia. By directly addressing the heart’s electrical dysfunction, we can significantly reduce arrhythmias and shocks from defibril-
lators, offering patients a better quality of life,” said Dr. John Sapp, CANet Network Investigator and principal lead of VANISH2.
The study was spearheaded by investigator collaboration. Many investigators are associated with CANet, which provided significant funding and support. CANet’s commitment to fostering groundbreaking cardiovascular research underscores its vision of improving patient care through innovation. By funding the trial, CANet has reinforced its status as a leader in bridging research, clinical practice, and patient outcomes.
“The multicenter, randomized trial exemplifies how CANet accelerates impactful research that improves patient outcomes and reshapes clinical practice. This study validates the efficacy of catheter ablation and underscores the importance of funding and collaboration in driving innovations in cardiac care,” said Dr. Anthony Tang, CANet CEO and Scientific Director.
CANet’s collaborative model brings together researchers, clinicians, and patients across Canada, facilitating large-scale studies like VANISH2. This inclusive approach ensures that research outcomes translate effectively into real-world settings, enhancing the accessibility of advanced treatments for Canadians.
Beyond individual patient outcomes, the study’s findings have significant implications for healthcare systems. Ventricular tachycardia is associated with high hospitalization rates and considerable healthcare costs. Early interventions like catheter ablation could significantly reduce these burdens, offering substantial savings and improving overall system effi-

ciency, providing a strong motivation for healthcare policymakers to adopt these findings.
As arrhythmia-related hospitalizations continue to rise globally, the study sets a precedent for adopting evidence-based, cost-effective treatments. It also aligns with CANet’s broader mission of integrating patient-focused solutions, as evidenced by VIRTUES, their digital health platform, which enhances patient-provider communication and care delivery.
The publication of the trial marks a milestone in cardiac arrhythmia treatment, but it is also a call to action for further research and implementation. As the healthcare community begins to integrate these findings into clinical guidelines, patients and providers alike stand to benefit from more effective, personalized treatment options.
“This study is a testament to the transformative potential of Canadian-led cardiovascular research. By prioritizing patient-focused approaches, we are advancing science and ensuring that our healthcare system delivers the best possible outcomes for individuals and families across the country,” Dr. Ratika Parkash, CANet Associate Scientific Director and Network Investigator.
CANet’s involvement highlights the value of Canadian-led research in shaping the future of global healthcare. By prioritizing collaborative, patient-centric initiatives, CANet continues to set a standard for excellence in cardiovascular science and innovation.
In addition to his leadership role at CANet, Dr. Anthony Tang was essential in the trial’s conception and execution. From the study’s early design stages to its final implementation, Dr. Tang provided invaluable mentorship to the investigative team, emphasizing the importance of collaboration between seasoned experts and emerging researchers.
“This trial is a prime example of the power of multigenerational investigator involvement,” Dr. Tang stated. “By fostering a collaborative environment where experienced and early-career researchers work together, we ensure that innovative ideas are grounded in rigorous methodology, ultimately driving impactful, patient-centred outcomes.” For more information about this groundbreaking study, visit CANet’s website or explore its publication in The New England Journal of Medicine at NEJM.org. To learn about CANet’s initiatives, visit www.canetinc.ca n H
nity Health Toronto and Oak Valley Health are creating a streamlined care pathway to provide patients with timely access to advanced cardiac procedures and interventions at St. Michael’s Hospital. This collaboration marks a significant milestone for Oak Valley Health – which includes Markham Stouffville Hospital, Uxbridge Hospital and the Reactivation Care Centre – as it works towards a Level 4 Regional Cardiac Program status, expanding clinical care for its patients.
The partnership will support cutting-edge research and clinical trials by advancing education and training between clinical experts. Teams will also share best practices and maintain quality assurance, ensuring a high level of care from start to finish.
“As one of the leading community hospitals in Ontario, our partnership with St. Michael’s Hospital is vital for advancing cardiac care at Oak Valley Health. Clinicians will work together to improve patient outcomes, strengthen immediate access to acute care, and lay the foundation for ongoing advancements, benefiting our communities and ensuring the highest standard of care. Together, we remain dedicated to delivering an extraordinary patient experience,” said Terri Stuart-McEwan, Vice President of Clinical Programs and Chief Nurse Executive, Oak Valley Health.
As a globally-recognized acute care hospital in downtown Toronto, St. Michael’s Hospital, a site of Unity Health Toronto, will provide a comprehensive range of advanced cardiac services, including coronary procedures, advanced electrophysiology, structural heart procedures, and cardiac surgery. Oak Valley Health will continue to play a crucial role in ensuring continuity of care for inpatients. Together, this partnership will enhance cardiac care capacity, support patients, and foster seamless hospital integration.
“St. Michael’s Hospital is proud to partner with the dedicated teams at Oak Valley Health to provide ad-

vanced cardiac care to the communities they serve. We are a committed partner in Ontario’s health care system and this new care pathway expands our ability to provide world-class cardiac care to all in need,” said Sonya Canzian, Executive Vice-President of Clinical Programs, Unity Health Toronto.
The partnership is aligned with the framework set by Ontario Health’s CorHealth Regional Cardiac Program, which provides strategic leadership to improve cardiac, stroke and vascular care in the province.
“Over the years, the Heart, Lung and Vascular program at St. Michael’s has grown into a national and global leader in heart and vascular care. As a Level 8 Regional Cardiac Program, we are proud of our wide-ranging expertise, including in minimally-invasive and catheter-based procedures, structural heart interventions, surgical valve repair, and complex arrhythmia management. We look forward to working with Oak Valley Health to build healthier communities,” said Dr. Howard Leong-Poi, St. Michael’s Hospital Heart, Lung and Vascular Medical Director.
Plans for additional cardiac care at Oak Valley Health include launching a pacemaker clinic in early 2025, enhancing its Level 2 coronary care unit,
and developing comprehensive device implantation services and a diagnostic cardiac catheterization lab. This partnership aims to improve the efficiency and accessibility of cardiac services across Ontario, offering more patients the same access to care.
“Cardiac patient visits are on the rise, and by 2030 our hospital could serve a population close to 500,000. To provide the care our rapidly growing and aging community deserves, we are committed to expanding our patient-centred cardiac services. Our valued CODE-STEMI program, in partnership with Southlake Regional Health Centre, continues to provide life-saving treatment for acute myocardial infarction. Additionally, our new collaboration with St. Michael’s Hospital will further strengthen our efforts to deliver comprehensive, first-class cardiology care closer to home,” said Dr. Paul Hacker, Lead Cardiologist, Oak Valley Health.
“For the past few months, the dedicated members of the Heart, Lung and Vascular team at St. Michael’s have been preparing for this new partnership with Oak Valley Health. I would like to thank our team members for their hard work and collaboration, particularly between clinicians and ad-
ministrators, to facilitate this new care pathway which sees patients receive the care they need, when they need it.” – Desa Hobbs, St. Michael’s Hospital Senior Clinical Director
“The entire Cardiology team at St. Michael’s Hospital, Unity Health Toronto are thrilled to begin a very important relationship between Oak Valley Health and the entire Heart and Vascular program. We have always worked very well together, and this formal relationship will help the teams at both Oak Valley Health and St. Michael’s provide the highest quality, and timely care to the communities of Markham, Stouffville and Uxbridge.” – Dr. Kim Connelly, Division Head, Cardiology, St. Michael’s Hospital
“The Division of Cardiac Surgery at St. Michael’s Hospital has always had a wonderful working relationship with the phenomenal doctors at Oak Valley Health. We are thrilled to formalize this partnership. The communities of Markham-Stouffville-Uxbridge will surely benefit from our close collaboration.” – Dr. Bobby Yanagawa, Division Head, Cardiac Surgery, St. Michael’s Hospital
“At Oak Valley Health, we are committed to delivering exceptional, compassionate care that prioritizes both safety and quality. As we continue to advance community-based care, we look forward to developing our partnership with St. Michael’s Hospital, putting patients first, enhancing our collective efforts and expanding access to a comprehensive range of cardiac services. Together, we are building something greater for patients and the communities we serve.” – Carnett Howell-Belle, Patient Care Director, Acute Medicine, Oak Valley Health
“With combined, excellent leadership and dedicated cardiac teams, we are growing our cardiac services to be increasingly patient-centred. Health care is our top priority, and access to better, comphrensive care is a goal we strive for no matter the place we deliver care. Oak Valley Health and St. Michael’s Hospital’s partnership
signals innovation, growth, and hope, bridging the gap and bringing the same quality of care to patients in Toronto and the York and Durham regions.”
– Dr. Douglas Wan, Cardiologist, Oak Valley Health
Unity Health Toronto is one of the largest health care networks in Ontario with a wingspan across Toronto’s core. The wide range of services we offer, supported by our university affiliation, strong community partnerships, and global reputation in research, education, and innovation, positions us as a leader in delivering collaborative, integrated, and high-quality care.

team.
an integral part of Toronto’s neighbourhoods for generations, providing compassionate, quality care in direct response to the changing needs of the communities they serve. That shared legacy bonded them as they became one network in 2017, and it continues today as we develop a path forward to-

Our motto – Caring hearts. Leading minds – captures the dual commitment everyone carries at Unity Health Toronto to compassionate patient care
and excellence in education, research and innovation. We are advancing healthcare for all united by one vision: The best care experiences, created together.
For media inquiries please contact Communications@UnityHealth.to
Oak Valley Health is one of Ontario’s leading community health care organizations. Across our two
hospitals, Markham Stouffville Hospital and Uxbridge Hospital, as well as our Reactivation Care Centre, we deliver safe, high-quality care to more than 441,000 patients annually through diagnostic and emergency care services, clinical programs in acute care medicine and surgery, addictions and mental health, and childbirth and children’s services. Oak Valley Health is proud to be part of the Eastern York Region North Durham Ontario Health Team. With over 600 professional staff, over 3,300 dedicated staff, and more than 900 active volunteers, we are committed to celebrating our people, fostering connections, and driving innovative growth. We provide integrated care for healthier communities and deliver an extraordinary patient experience through our honoured to care culture to residents of Markham, Whitchurch-Stouffville, Uxbridge, and beyond. For more information, visit oakvalleyhealth.ca. n H
For media inquiries, please contact: Alysia Burdi Senior Communications Specialist, Oak Valley Health aburdi@oakvalleyhealth.ca
Major advances made at the RI-MUHC could help improve counselling for individuals suffering from infertility, premature ovarian insufficiency, recurrent miscarriages and androgenetic hydatidiform mole.
A molar pregnancy, also known as a hydatidiform mole, is an abnormal human pregnancy with no embryo and an overgrowth of the cells that form the placenta. The common form of molar pregnancies affects one in every 600 pregnancies in Quebec. Half of these moles are androgenetic, i.e., they contain only the father’s chromosomes with no chromosomes from the mother, and their frequency increases 10 times with advanced maternal age. Because of the hyperproliferation of their cells, androgenetic moles may become malignant and lead to a placental cancer in up to 15 per cent of cases.
Scientists at the Research Institute of the McGill University Health Centre (RI-MUHC) recently discovered six new genes – FOXL2, MAJIN, KASH5, SYCP2, HFM1 and MEIOB – that cause recurrent androgenetic moles, recurrent miscarriages and infertility when mutated on both alleles (copies of the same gene) in the patients. Five of these genes are essential for Meiosis I, the process of cell division necessary for the production of sperm and eggs in humans. Previous studies have linked defects in some of the six genes to premature ovarian failure, a well-known cause of female infertility. In addition, five of these genes have been linked to male infertility.
These findings, just published in The Journal of Clinical Investigation, will improve the molecular diagnosis of recurrent molar pregnancies, premature ovarian failure and infertile women and men.
“Our findings suggest that recurrent androgenetic moles are a sign of ovarian ageing. They will change current clinical practice by introducing the evaluation of ovarian reserve for patients with recurrent moles,” says Rima Slim, PhD, corresponding and co-senior author of the study, Senior Scientist in the Child Health and Human Development Pro-
THE
gram at the RI-MUHC and Professor in the Department of Human Genetics at McGill University.
The six new genes add to four other genes that are also responsible for recurrent molar pregnancies and that were previously discovered by the same team (NLRP7, discovered in 2006, and MEI1, TOP6BL and REC114, discovered in 2018).
In collaboration with Jacek Majewski’s team, Investigator at the RI-MUHC and Professor of Human Genetics at McGill, the researchers performed exome sequencing on 75 unrelated patients referred by physicians from around the world. These patients had at least two hydatidiform moles and did not have mutations in the previously described genes associated with the condition.
The researchers then checked whether the patients who were negative for biallelic mutations (on both alleles of a gene), had only one defective allele in genes with roles in Meiosis I and ovarian functions. They added
240 patients with other forms of reproductive failure – referred primarily from the MUHC Repeated Pregnancy Loss clinic, founded by Dr. William Buckett, and the Réseau des Maladies Trophoblastiques du Québec, founded by Dr. Philippe Sauthier. This second group of patients had either a molar pregnancy and at least one miscarriage, or at least two miscarriages without a molar pregnancy.
They found that 14 per cent to 28 per cent of these patients had one defective allele that appeared to be most frequent in patients with at least two molar pregnancies.
“Our data suggest that these monoallelic variants could be contributing, with other factors, to the genetic susceptibility of these patients for reproductive failure. Our study provides an explanation of the increased frequency of androgenetic moles with advanced maternal age,” explains Prof. Slim.
The authors of the study explain that “patients with monoallelic variants in these genes can conceive and have healthy children; however, they are at higher risk for infertility, premature ovarian insufficiency and re-
productive loss than women from the general population.”
In order to better elucidate the mechanisms underlying this health and reproductive problem, the researchers modelled the disease in mice with deficiency in the HFM1 gene.
“We observed several defects that affect the meiotic progression, some of which were previously observed by our team in mice with deficiency in the Mei1 gene, another gene responsible for the causation of recurrent androgenetic moles,” explains Teruko Taketo, PhD, co-senior author of the study, Senior Scientist in the Child Health and Human Development Program at the RI-MUHC and Professor in the Department of Surgery at McGill University. “In this study, using live-cell imaging, we were able to visualize and understand for the first time how the eggs from Hfm1 deficient mice lose all their chromosomes.”
The authors emphasize that the identification of the same mechanism in two mouse models supports its plausibility at the origin of androgenetic mole formation in humans.
“Androgenetic moles have been described in 1977. Today, we can better explain to the patients the formation of these aberrant conceptions and the genesis of androgenetic moles,” says Prof. Slim. n H
By Catherine Danko
Courtney Lindsay never envisioned that her work as a nurse practitioner (NP) would one day be conducted through a computer screen.
As an NP who splits her time between UHN’s online and in-person Emergency Department (ED), learning to consult patients virtually has become an integral part of her work duties.
“It was a learning curve because as an emergency provider, I’ve always worked in the hospital in a face-toface environment,” says Courtney, who meets with patients via video calls twice a week to help treat and diagnose a variety of urgent conditions that are not life threatening such as rashes, sprains and minor injuries, eye infections and cold and flu viruses.
For Courtney, one advantage of working in the virtual ED is its UHN-centralized approach. This means the patients she treats are already familiar with the internal specialized services, making it easier for her to help guide them through their medical situations.
“As UHN emergency providers, we have specialized knowledge in treating some of our UHN sub-specialized populations across the province, which may be more challenging in a peripheral Emergency Department or walk-in clinic,” says Courtney, whose role encompasses the same scope as that of a physician when it comes to assessment, treatment and diagnosis in the ED.

“This means that we can provide timely and efficient care to all patients through our virtual platform, whether the condition is an episodic complaint or complex,” she says.
At UHN, there are about 160 NPs across all five hospitals providing a wide range of services, including assessing and triaging patients, ordering and interpreting diagnostic tests, diagnosing illnesses, developing treatment plans and referring as required.
Investing in the expansion of NPs is a key solution in advancing UHN’s mission of A Healthier World.
“Discovering innovative solutions to decrease wait times and increase access in the EDs and provide primary and specialized care to patients is a key priority at UHN,” says Tara Bolden, Nurse Practitioner Lead, Collaborative Academic Practice.
Tara emphasizes this investment in NPs is ongoing, with UHN continually exploring inventive ways to ensure they work to their full scope of practice to optimize contributions to patient care, scholarship, education and leadership across the organization.
“NPs are integral to these solutions, as they play such a crucial role in the areas they work in, bringing a holistic perspective that isn’t solely focused on a single pathological issue,” she says. “Giving consideration to all elements and factors that impact a patient’s health and wellness is key in providing high quality, comprehensive care.”
Toronto’s Virtual Emergency Department, which includes UHN and
Courtney Lindsay, a nurse practitioner in UHN’s virtual Emergency Department, says the scope of her work allows her to find innovative ways to care for patients who might not otherwise have access to primary care.
“DISCOVERING INNOVATIVE SOLUTIONS TO DECREASE WAIT TIMES AND INCREASE ACCESS IN THE EDS AND PROVIDE PRIMARY AND SPECIALIZED CARE TO PATIENTS IS A KEY PRIORITY AT UHN.”
Sunnybrook Health Sciences Centre, is a virtual care program supported by Ontario Health that offers online urgent care services from emergency nurse practitioners and physicians across the city.
Initially operated solely by physicians, the program has evolved significantly since its inception in 2020. In 2023, the Ontario Ministry of Health provided funding to expand the program to be NP-led.
NPs often work in collaboration with physicians and other health care professionals to deliver comprehensive care, and they play a crucial role in promoting health and preventing disease.
Since the virtual ED is staffed by just one NP at any given time, skills such as autonomy and independence are crucial.
“It’s an interesting role because nurse practitioners typically work within a large team where there’s lots of direct consultation available,” says Courtney.
“Those of us working virtually have excelled in maintaining a NP-
led program, which has involved establishing standard operating procedures and protocols for managing patients, developing training documents and resources for our newer NPs joining the team, and providing a pathway for follow-up from our EDs.”
What Courtney loves most about working in emergency medicine –whether virtually on in-person – is the “hands-on skills” that she gets to do, exercising her full scope of practice and seeing a diverse portfolio of patients independently.
“What’s been most rewarding virtually is being able to find innovative ways to provide care to patients, especially when we know that many people don’t have great access to primary care,” she says.
“Being able to expand our urgent care services and expertise beyond the walls of the hospital and demonstrate that a virtual ED can be NP-led is something I am very proud of.” n H

As the development of artificial intelligence (AI) continues to accelerate, it is becoming increasingly evident that these cutting-edge solutions hold immense potential for enhancing radiology and the broader healthcare sector. Not only can AI significantly improve workflows, thereby boosting productivity, but it also presents a viable solution for addressing the ongoing challenge of providing comprehensive health coverage and expanding access to medical imaging for Canadians.
A variety of AI solutions have found their way into radiology departments both within Canada and internationally. The extent of AI solutions being utilized in Canada is an unknown. Nevertheless, the CAR supports the incorporation of these technologies within radiology departments and clinics across the country, provided there are proper checks and balances which are contingent on human oversight. While deploying AI solutions, it is important to proceed with caution given their evolving learning capabilities. The CAR strongly believes that there
THE EXTENT OF AI SOLUTIONS BEING UTILIZED IN CANADA IS AN UNKNOWN.
needs to be national oversight for AI applications, particularly as they relate to patient care. Best practices, rules, and regulations are necessary and should be monitored at a federal level. Despite the numerous benefits that AI could bring to patients and healthcare professionals, we must also remain cognizant of the potential risks associated with its application.
In response to the introduction of this new type of technology in healthcare, the CAR has set up a Healthcare AI Validation Network (HAIVN). This assembly consists of AI specialists in the field of radiology tasked with assisting with post-market assessment of AI applications. As a resource, HAIVN would serve as the national body responsible for evaluating the performance of these technologies and
pre-identifying any potential issues that may affect patient care.
Dr. Jaron Chong, Chair of the CAR’s Standing Committee on Artificial Intelligence, is leading the charge on the HAIVN project. He has authored many publications on AI and has also been a contributing author on CAR’s five white papers focused on AI. Dr. Chong also sits on Health Canada’s Scientific Advisory Committee on Digital Health Technologies (DHT). He is an Assistant Professor at the Department of Medical Imaging at Western University and completed his diagnostic radiology residency training at McGill University with an Abdominal Imaging fellowship at Yale New-Haven Hospital and a master’s in health informatics at the University of Toronto. His clinical interests include cross-sectional abdominal imaging, Abdominal/GI oncologic imaging in MRI and CT modalities, with research
interests in the appropriate utilization of medical imaging and AI-assisted augmented radiology. As part of the CAR’s overall advocacy strategy, Dr. Chong and the CAR has held several meetings and discussions with the Ministry of Innovation, Science, Economics and Development Canada and Health Canada regarding HAIVN and is exploring how HAIVN can assist these federal branches of government in the validation process of emerging technologies.
“AI has the capacity to impact healthcare delivery in a positive way. There are currently many AI applications specific to radiology that show promise in terms of enhancing workflows and streamlining medical imaging procedures,” said Dr. Chong. “Many of these technologies have been integrated into healthcare systems outside of Canada with favourable results. However, before broadly introducing them to the Canadian healthcare system, it is essential that a national regulatory framework has been developed which includes expert oversight to maximize safety and value.” n H
hile Canada comparatively lags in implementing Clinical Decision Support (CDS) systems into hospital workflows at a national level, the CAR is currently working with a handful of strategic partners like Choosing Wisely Canada on constructing guidelines to support their implementation in institutions across Canada. Most recently, the CAR hosted a day of meetings focused on digitizing referrals in Canada with a variety of stakeholders, including representatives from the Canadian Medical Association, radiologists from several provinces, and doctors from the United Kingdom who spoke about implementing CDS systems in their healthcare system. Even before our referrals program, CAR members have done the extra work to make referrals better. An example of this commitment to positive change is Dr. Steve Herman. The overall purpose of CDS implementation, Dr. Herman says, is to help physicians and patients make better, more informed decisions regarding medical imaging tests and treatment.
Today, Dr. Herman works for the Joint Dept of Medical Imaging at UHN, Mt Sinai, and Women’s Col-
lege Hospitals, and knows the benefits of implementing CDS systems are well established.
“These systems have the potential to significantly improve patient care by ensuring the right test gets done the first time. This shortens queues for procedures which reduces wait times and exposure to ionizing radiation for patients. They also have the potential to save healthcare systems labour and resources by avoiding performing studies that do not provide patient benefits.”
Dr. Herman’s entry into CDS systems came while reporting chest CTs, as he began questioning the value of many of the scans he was reading. He approached a colleague to conduct research on the impact of the tests on patient survival.
“We selected a specific group of lung cancer patients to study and published our work in the Journal of Thoracic Oncology showing that the routine CT scans we were doing on post-lobectomy patients did not impact survival. This demonstrated that the problem was real, so we asked ourselves, what could be done about it? We thought that if we put guidelines in front of doctors when
they were ordering tests, perhaps we could affect their behaviour toward choosing a more appropriate test, which sometimes meant ordering no test at all.”
Other studies in Canada and elsewhere have arrived at the same conclusions as Dr. Herman regarding the efficacy of ordered tests. A study from Ontario’s Ministry of Health found that doctors changed their testing requirements when given an option before ordering 85 per cent of the time.
Dr. Herman has done more than research the area – he has since founded MedCurrent, a CDS company focused on improving the quality of care and managing health system costs.
There are pockets of CDS throughout Canada. There are pockets of CDS throughout Canada. The first hospital in the country to implement a system was North York General Hospital in Toronto. The chief of radiology there, Dr. Ryan Margeaux, is now leading the CAR’s efforts in creating CDS guidelines. As well, Dr. Huy Le is Chief of Radiology at Jewish General Hospital (JGH) in Montreal and says JGH is at Canada’s forefront of implementing CDS because of its history of integrating technology.
“Dr. Lawrence Rosenberg, the CEO of our institution, had a vision for adopting digital health many years ago, which included pertinent applications in medical imaging.” Dr. Le says this approach led JGH to successfully create an electronic Order Entry System (OES).
The UK is a world leader in implementing CDS for radiology. In 2021, the National Health Service (NHS) for England was provided £11M GBP ($18M CAD) to implement CDS systems, which over half of the nation’s hospitals have done. While meeting with MPs and government health officials during Day on the Hill in October, one of the CAR’s primary points of conversation was the necessity of federal investment in CDS systems on a national scale.
After enduring years of a pandemic, it has become obvious how much strain can be pressed upon Canada’s healthcare system. Using data-based CDS systems to perform the labour of determining the correct tests with a high degree of efficacy is an effective way to alleviate this strain in the present and will provide a sustainably optimal health care experience for patients in the long-term. n H
T Whe autumn season offers the CAR the opportunity to vocalize the needs of Canadian radiologists and patients to the federal government through our advocacy initiatives. This year, the 9th Annual Day on the Hill took place on Tuesday, October 29 and consisted of meetings with key federal ministers and medical imaging equipment demonstrations on-site.
Engaging with officials in the federal government is critical to ensuring that the priorities for Canadian radiologists are clearly and adequately conveyed to key governmental decision-makers,
and to raise awareness of the crucial role of radiologists in Canada’s healthcare system.
The CAR focused on several key issues with federal ministers:
1. That the federal government spearheads a national effort to recruit and retain radiologists, medical radiation technologists, and sonographers as part of a national health human resource strategy.
2. That parliamentarians include the voices of radiologists in their deliberations, particularly deliberations related to breast cancer screening guidelines, of which radiologists are
integral players to maintain standards and deliver service.
3. That the federal government invests in a cost-neutral manner to evolve the medical device licensing process to include post-market surveillance through Health Artificial Intelligence Validation Network.
4. That the federal government supports ensuring provinces integrate Clinical Decision Support into their electronic medical record systems.
5. That the federal government guide an investment of $2 billion over three years for radiology equipment
to improve access to modern medical imaging equipment.
An additional feature of this year’s Day on the Hill was the mobile MSK and ultrasound clinics that were onsite to provide real-time demonstrations. Having imaging equipment in-person allowed the CAR to better demonstrate the radiologist’s role in imaging different body parts and to provide evidence of the CAR’s objectives grounded in real-life context.
The CAR is grateful for the opportunity to advocate on behalf of Canadian radiologists and patients to the federal government. n H
By Sarah Ripplinger
recent study led by Vancouver Coastal Health Research Institute researcher Dr. Ilker Hacihaliloglu is the first to test the viability of a selection of image-to-image synthesizing technologies used to generate magnetic resonance imaging (MRI) images from ultrasound scans of prostate cancer.
Within the past two years, researchers have made incredible advances in image synthesizing technology. Similar to the popular OpenAI generative artificial intelligence (AI) algorithm that can create images and transform imag-
es into other images, synthetic image generation is a sophisticated AI computer algorithm.
Researchers feed image synthesizing technology thousands of patient diagnostic scans to train it on identifying disease characteristics, such as images of variations of a certain type of cancer.
The more images input into the algorithm, the better it will be at accurately generating a synthetic image, explains Hacihaliloglu. For example, the software image synthesizing technology examined in their study can quickly translate a single ultrasound scan into another medical diagnostic image, such as an MRI image, with the click of a button.
“THIS EMERGING TECHNOLOGY HAS THE POTENTIAL TO REDUCE THE NEED FOR MANY MRI AND CT DIAGNOSTIC SCANS.”
A study conducted at Grand River Hospital demonstrated the benefits of the Reveal 35C dual-energy X-ray detector in the ICU, including better image quality, faster or unchanged reading times, increased diagnostic confidence, and reduced time to potential intervention. The study also highlighted its potential to reduce CT imaging needs.
Quoting directly from the study: “In certain cases, especially when computed tomography (CT) is not an option, dual-energy X-ray can permit improved visualization of soft tissues by subtracting unwanted structural noise […] and simultaneously reducing unnecessary radiation exposure. Medical lines and tubes can be better visualized using the bone image that dual-energy X-ray detectors also produce.”
Results were positive for more than half of the physicians in all areas, with reported better image quality, no added or faster reading times, increased confidence in diagnosis, and a reduction in time to potential intervention.
Another outcome observed was the potential for CT diversion. In addition to the self-reported reduction trend noted by intensivists, the study showed a 37.5% reduction in chest CTs compared to the previous three months and a 16.67% decline year-over-year during the study period.
Findings were presented at the American Society of Emergency Radiology Meeting.

“Our goal is for image-to-image technology to advance to the point at which it can be used in health care settings to reduce wait-times and travel time for high-quality clinical imaging, such as MRI, and reduce radiation exposure from CT, X-ray or mammography scans,” states Hacihaliloglu.
MRI technology uses magnetic field waves and computer-generated radio waves to take detailed images of internal tissue structures, including bones, blood vessels, organs and muscles. While non-invasive, the technology is presently only available as non-portable machines that may not be available outside of major city centres. The same is the case for CT scanners, which are a radiating technology that takes a series of detailed X-ray images of internal soft tissues and bones.
Ultrasounds, on the other hand, are a non-radiating technology that uses sound waves to produce images of tissues, such as organs, inside the body. Available as handheld, portable machines, ultrasounds are a convenient and accessible means of generating real-time pictures of internal tissues. Available in remote areas that may be far from other scanning technology, such as MRI or CT scanners, ultrasounds are an ideal choice as a rapid
medium from which to generate synthetic MRI or CT images.
MORE RESEARCH IS NEEDED
For their study, Hacihaliloglu and his team evaluated the quality of synthetic MRI images generated from 794 ultrasound scans of prostate cancer using five widely recognized image-to-image translation networks in medical imaging: 2D-Pix2Pix, 2D-CycleGAN, 3D-CycleGAN, 3D-UNET and 3D-AutoEncoder. Five doctors with over five years of experience reading MRI scans were then given a random selection of 15 synthesized MRI images.
The team found that, while the synthetic MRI images were around 85 per cent similar to those of the MRI scans, they lacked too many important clinical features to be useful in diagnostics at this stage.
“This technology has great potential to be used in clinical diagnostics, research and medication development,” says Hacihaliloglu. “As such, there is a pressing need for further refinement of image-to-image translation networks to enhance its performance.” n H
Negotiating is a profession al skill that needs to be learned and developed, and while some are great at negotiation, it does not come nat urally to most. In February, the CAR partnered with the University of To ronto (U of T) Department of Medical Imaging to host Women in Radiolo gy: Negotiation Skills, an informative evening dedicated to discussing the importance of negotiation in radiol ogy careers, share stories of personal negotiation experience, and outline steps on how women in radiology can improve this skillset.
Women radiologists packed the host venue, the Elmwood Spa in To ronto, making for an engaging and upbeat evening of learning, discussion, and socializing. The event quickly reached its full registration capacity,




n an era where medical imaging is at the forefront of diagnostic innovation, the field of radiology is evolving rapidly, shaped by technological advancements and groundbreaking research. To navigate the complexities and opportunities within this dynamic discipline, we turned to some of the brightest minds in radiology. In this special feature, thought leaders share their insights on pressing questions facing radiology today. From the integration of AI in diagnostic imaging to the future of patient-centered care, these expert answers offer a glimpse into the challenges, innovations, and transformative shifts shaping the future of radiology. Join us as we dive into the perspectives of pioneers who are redefining the way we look at health, technology, and patient outcomes.
WITH THE RISE OF PERSONALIZED MEDICINE, HOW DO YOU SEE RADIOLOGY EVOLVING TO PROVIDE MORE TAILORED DIAGNOSTIC AND TREATMENT PLANS FOR PATIENTS?
Medical imaging occupies a keystone role with personalized medicine, with many advanced imaging modalities, such as functional MRI and molecular imaging, already helping us characterize disease activity at the cellular level and direct therapy. Most importantly, medical imaging is uniquely positioned to offer these diagnostic and therapeutic capabilities in a non-invasive and continuous fashion in follow-up, which differs from the work of other fields. In the near term, efforts will focus on validating and experimenting with these new imaging techniques to determine their value in patient care while addressing their limitations and ensuring judicious use in resource-limited healthcare systems.
– Dr. Jaron Chong – Chair, CAR AI Standing Co
HOW HAVE ADVANCEMENTS IN ARTIFICIAL INTELLIGENCE
AND MACHINE LEARNING IMPACTED THE FIELD OF RADIOLOGY, AND WHAT DO YOU FORESEE AS THE NEXT MAJOR INNOVATION?
Artificial intelligence (AI) and machine learning (ML) have significantly enhanced the field of radiology by improving the speed and accuracy of image analysis. As these two fields continue to progress, the very latest technologies in Large Language Models (LLM’s) and Vision Language Models (VLM’s) will offer the next round of capabilities to further advance radiologist analysis and accelerate efficient and accurate workflow. These techniques are generalized enough that the impact of tools could be broad, from mundane tasks like proof-reading reports, to executing population based screening and preventative recommendations, and begin to impact administrative burdens in the medical imaging workflow.
– Dr. Jaron Chong – Chair, CAR AI Standing Co
AS IMAGING TECHNIQUES CONTINUE TO IMPROVE, HOW DO YOU THINK RADIOLOGY WILL INFLUENCE EARLY DETECTION AND PREVENTION OF DISEASES, PARTICULARLY CANCERS OR NEUROLOGICAL DISORDERS?
Improved imaging techniques are continuously revolutionizing the early detection and prevention of diseases. High-resolution imaging and advanced modalities like PET/MRI are making it possible to identify precancerous lesions and early-stage cancers with remarkable precision. Similarly, advanced neuroimaging techniques are helping to detect biomarkers of neurological disorders like Alzheimer’s disease, oftentimes well before symptoms appear. By identifying diseases at an earlier stage, radiology is empowering clinicians to intervene sooner, improve patient outcomes, and even prevent disease progression through early lifestyle or therapeutic interventions. With the proliferation of AI/ML tools,
we may now also begin to offer these functions at a greater volume and on a wider scale than previously attainable.
– Dr. Jaron Chong – Chair, CAR AI Standing Co
HOW DO YOU SEE THE ROLE OF RADIOLOGISTS EVOLVING IN MULTIDISCIPLINARY CARE TEAMS, ESPECIALLY WITH THE GROWING FOCUS ON COLLABORATIVE HEALTHCARE MODELS AND INTEGRATED PATIENT CARE?
The role of radiologists is evolving from traditional image interpreters to pivotal collaborators in multidisciplinary care teams. As healthcare shifts towards integrated patient care, radiologists are uniquely positioned to serve as information curators and clinical consultants.
In multidisciplinary care, radiologists will provide real-time insights, integrating imaging data with clinical, genomic, and pathology information to guide diagnostic and therapeutic decisions. Their expertise combined with advanced imaging techniques, such as AI-powered radiomics and 3D/4D imaging, will enable more personalized and precise care.
Radiologists will also take on a leadership role in managing and interpreting aggregated patient data. With platforms like Sectra’s “Pixel EMR” approach – where imaging data from various specialties is centralized – radiologists can contextualize findings across disciplines, fostering a comprehensive understanding of a patient’s condition.
Technology will further amplify the impact of radiologists, requiring them to adapt and expand their expertise. As AI and deep learning (DL) become integral to imaging workflows, radiologists must understand these technologies to ensure their safe application. Familiarity with DL algorithms will be essential for providing critical clinical oversight, validating AI outputs, ensuring accuracy, mitigating biases, and integrating AI-generated insights into comprehensive clinical interpre-
tations. By combining their expertise with AI, radiologists can enhance diagnostic precision while maintaining the human touch in patient care. Moreover, radiologists will play a critical role in patient-facing care. With seamless integration into EMRs - like Epic, radiologists’ insights will be readily accessible to the broader care team. As imaging findings increasingly inform treatment plans, radiologists will directly engage more with patient care teams to explain results and options, build trust, and enhance patient outcomes. The future radiologist will be central to integrated care, leveraging technology, data, and collaboration to deliver precise, patient-centered outcomes. This evolution elevates their role and aligns radiology with the overarching goals of multidisciplinary, value-based healthcare.
– Stephen Harrold, Director, Strategy & Innovation, Sectra Canada Inc.
Imaging plays a central part in the health care journey of most patients, including diagnosis, interventions, and follow-up during and after therapy. Radiologists’ interpretations of images affects other physician and surgeon decision-making, as well as allied health providers. Thus, the role of radiologisst in multidisciplinary care will continue to grow given the increasing needs for effective communication between various health professionals to coordinate care of patients in a health care system which has limited resources.
– Dr. Ania Kielar – CAR President
WHAT ARE SOME OF THE MOST EXCITING OR UNDERAPPRECIATED AREAS OF RESEARCH IN MEDICAL IMAGING THAT COULD SIGNIFICANTLY CHANGE THE WAY WE APPROACH DIAGNOSIS IN THE NEAR FUTURE?
It’s remarkable to see how far we’ve come through innovation, developing new equipment, new techniques, and doing things that were certainly unimaginable for Roentgen, the
father of X-rays. And as we see advanced modalities gaining more and more features, it is sometimes underappreciated that plain old X-ray or as it is now called, Digital Radiography (DR) itself still has room for improvement and innovation that can lead to better outcomes. DR or Digital X-ray is the first step in the diagnostic process – and sometimes the only one available, especially in low-resource settings.
Improving Digital X-ray, therefore, is paramount. The rise of new technologies that make Digital X-ray better – such as quantitative single-exposure dual-energy subtraction – can add significant value. When you can better detect and quantify diseases right from the start, in both fixed and mobile settings, you can optimize the entire chain of hospital care. When you can offer more insights at the bedside, in emergency rooms, in outpatient clinics, it’s one less patient you have to move around the hospital for follow-up imaging and improve time to diagnosis and intervention. The impact can be huge.
Let’s take the example of the ICU: what is the burden of advanced imaging on staff and hospital operations? If you can alleviate the need to move patients for a CT scan with something as simple as a spectral digital bedside X-ray, the difference can be significant. As another example, let’s talk about remote or low-resource areas that might not even have advanced equipment available. There is a gap in healthcare and the very foundation of radiology, DR, through spectral imaging, might be the missing piece in this puzzle.
– Amol Karnick, President and CEO, www.kaimaging.com
RADIOLOGY IS A CRITICAL PART OF MANY MEDICAL DIAGNOSES, BUT THERE ARE CONCERNS AROUND RADIATION EXPOSURE. HOW DO YOU BALANCE THE NEED FOR DIAGNOSTIC IMAGING WITH MINIMIZING RISKS TO PATIENTS?
Radiologists, like other physicians, follow guidelines and evidence-based
practice to determine the best imaging for the question at hand, based on the patient’s symptoms and past medical history. The Canadian Association of Radiologists publishes various practice guidelines which are created and updated by experts in the field. This includes radiologists as well as physicians who are involved in the care of patients related to a particular guideline. Radiologists follow the ALARA principle with regards to radiation exposure (As Low as Reasonably Achievable) for patients, choosing imaging tests such as ultrasound and magnetic resonance imaging (MRi) when appropriate. When x-ray, computed tomography (CT) and Positron Emission Tomography (PET) is the most appropriate imaging test to perform, we work to perform the test using the lowest radiation dose possible, while maintaining high quality images.
– Dr Ania Kielar, CAR President
HOW HAS THE ROLE OF RADIOLOGISTS CHANGED WITH THE INCREASED USE OF REMOTE IMAGING AND
TELERADIOLOGY, ESPECIALLY IN UNDERSERVED OR RURAL AREAS?
Regardless where radiologists report a study, they are responsible to ensure highest quality imaging for each patient. The Canadian Association of Radiologists is working to expand accreditation of imaging facilities across the country to help ensure best practices and protocols are available for all types of patient imaging. Radiologists are key members of multidisciplinary case conferences ()MDC), where physicians caring for patients with specific conditions can discuss cases in an environment with key experts in the field to ensure best care for each individual; this can include certain types of cancers, endometriosis and other non-cancerous conditions. Since COVID, these MDC are increasingly taking place in a virtual format, thereby allowing specialists from many different disciplines to participate without having to travel, and thus, allow improved access to expert discussions and consensus building.
– Dr Ania Kielar, CAR President
n H

By Mona Mollaeizadeh and Certina Ho
CCJ, a 50-year-old female, walks into the pharmacy, excited to learn that pharmacists can now prescribe for minor ailments, such as gastroesophageal reflux disease (GERD). She asks for a renewal of Pantoprazole (a proton pump inhibitor or PPI) for her GERD, mentioning that she has been taking it daily for years and is afraid to stop.
Proton pump inhibitors (PPIs) are one of the most commonly used medications in a variety of healthcare settings (e.g., ambulatory care, hospitals, or community care, etc.). They are often indicated for gastrointestinal disorders, such as, acid reflux, Helicobacter pylori (H. pylori) infections, esophagitis, GERD, and/or peptic ulcer disease. PPIs work by suppressing stomach acid secretion to help relieve heartburn and acid reflux.
PPIs might be taken longer than necessary, most often unintentionally. Although PPIs are very useful for various indications, they can also cause a variety of adverse effects with prolonged use. Oftentimes patients are prescribed a PPI during their hospital stay; and upon discharge, they may continue to take it without a pre-determined stop date. Some of the long-term side effects of PPIs include kidney and heart related disorders, osteoporosis related fractures, infections, and micronutrient deficiencies, etc.
There are several reasons why patients are prescribed short-term PPIs. For instance, PPIs are commonly prescribed for one to two weeks alongside antibiotics to treat H. pylori infections. Additionally, a course of four to 12 weeks may be recommended for individuals with stomach or small
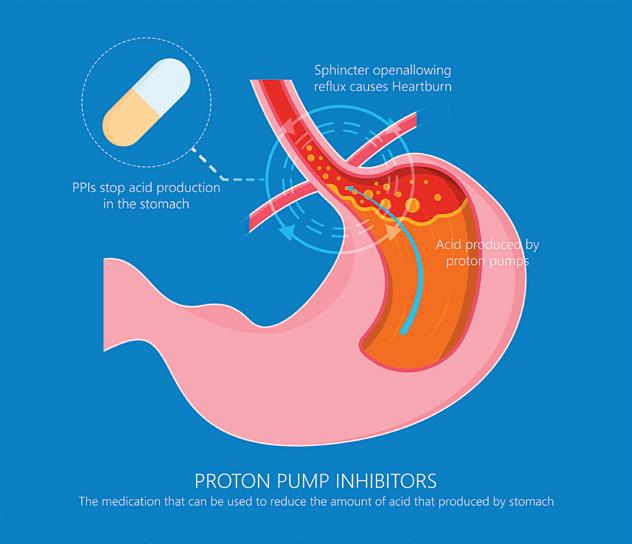
As time goes by, her GERD symptoms have begun to subside. She does not need to continue her PPI medication long-term. During a medication review with the pharmacist, it becomes evident that CJ should discuss with her health care provider about potentially coming off the PPI since it is no longer needed.
The American Gastroenterological Association’s Best Practice Advice Statements recommend deprescribing considerations when there is no clear indications for PPIs use. Deprescribing PPIs aims to reduce unnecessary use and long-term risks by gradually lowering the dose or frequency for patients who would benefit from it. This process should be managed by a healthcare professional to avoid rebound acid reflux. Patients should consult their physician or pharmacist before making changes to their PPI use to optimize their medication therapy management (i.e., to maximize benefits and minimize risks or side effects). Patients are also advised to regularly review their medications with their pharmacist.
intestine ulcers, or for esophageal inflammation.
Some patients with specific conditions may need to take PPIs long-term, however it is important for them to discuss a potential stop date with their healthcare providers when initiated on long-term PPIs. Although GERD is often a chronic condition, it may not always require ongoing acid suppression, so patients should consult their prescriber to determine if continuous PPI use is necessary or not.
Using PPIs long-term has been linked to an increased risk of various side effects. As mentioned above, studies have found mild-to-moderate association with long-term PPI use and issues like bone fractures, C. difficile infections, pneumonia, vitamin and mineral deficiencies, kidney disease, and dementia. However, since many of these side effects are uncommon, the overall risk for patients on PPIs is quite low.
CJ was prescribed Pantoprazole (a PPI) initially to help with her GERD.
Deprescribing.org has resources on deprescribing guidelines, including the Proton Pump Inhibitor evidence-based deprescribing guideline (that was published in the Canadian Family Physician, the official journal of the College of Family Physicians of Canada. It also provides a consult decision aid – “Should I Keep Taking my Acid Reflux Medication?
Choosing Wisely Canada also has a resource titled “Bye Bye PPI: A toolkit for deprescribing proton pump inhibitors in electronic medical record (EMR)-enabled primary care settings”. n H
By Lise Diebel
Orthopedic surgeons at Hamilton Health Sciences (HHS) Juravinski Hospital and Cancer Centre (JHCC) performed their first hip replacement surgery this month using a new, state-of-the-art orthopedic surgical robot designed specifically for hip and knee replacements.
The Mako Rio Surgical Robotic System is considered the most accurate and advanced robotic surgical system in the world for hip and knee replacements, including partial knee replacements which can be complex surgeries.
The system is currently being used at JHCC for hip replacements only, with plans to expand to knee and partial knee replacements. The HHS Foundation contributed $300,000 in funding, to support 200 robotic hip procedures per year at JHCC.
“It’s so encouraging to see how the innovation and commitment to quality at Juravinski Hospital and Cancer Centre, combined with the generosity of community donors, can create such impactful outcomes,” says Anissa Hilborn, chief executive officer for the HHS Foundation.
“So many lives will be changed for the better, and that should be an incredible source of pride for this region.”
Orthopedic surgeons use the robot for greater precision when preparing a bone for the implant, and accurately placing the replacement joint. The robot performs the procedure, with the surgeon maintaining overall control of programming and robotics.
“The robot is assisting to give surgeons more precision,” says Dr. Kamal Bali, an HHS orthopedic surgeon and clinical teaching unit director for resident doctors at JHCC. “This will potentially further reduce risk of both shortterm and long-term issues with hip replacements like dislocation and premature wearing out of an artificial hip.”
Bali is the first JHCC surgeon to use the robot along with Dr. Daniel Tushinski, head of service for JHCC orthopedics and McMaster University’s orthopedics and spine fellowship director.
Hamilton Health Sciences surgeons specializing in joint replacement and reconstruction are among leaders in the province for minimally invasive, muscle-sparing hip replacement surgery. “Using robotic technology will further add to our hospital’s reputation as a centre of excellence in joint replacement surgery,” says Bali.
The hospital performs 800 to 1,000 hip replacements each year, and the 200 patients per year receiving their surgery with the robot will be selected on a case-by-case basis. Tushinski and Bali hope to see the program eventually expanded so that this technology could be offered to all patients needing hip replacements.
Damage from arthritis is the most common reason for needing a hip replacement. Left unchecked, inflammation can lead to significant damage, causing a loss of function and disability. Arthritis can impact almost any part of the body, but most often affects the hip, knee, spine or other weight-bearing joints. One in five Canadians lives with arthritis, and there’s no cure, according to Arthritis Society Canada.
Surgery can reduce pain and help people become more mobile, so they can once again enjoy their daily activities.
“People’s quality of life is vastly improved through hip and knee replacements,” says Tushinski. “As well as having less pain and increased mobility, they also have improved energy levels because they’re not constantly disabled by pain.”
Research suggests that patients whose surgeries used the robot enjoy a smoother and faster recovery with less

Orthopedic surgeons at HHS Juravinski Hospital and Cancer Centre performed their first hip replacement surgery this month using a new, state-of-the-art orthopedic surgical robot designed specifically for hip and knee replacements. The Mako Rio Surgical Robotic System is considered the most accurate and advanced robotic surgical system in the world. Surgeons use the robot for greater precision when preparing a bone for the implant, and accurately placing the replacement joint.
pain and less chance of complications, such as wearing out the new joint prematurely.
Hamilton Health Sciences is a top 10 Canadian research hospital, and

having the surgical robot opens the door for new JHCC-based research aimed at improving outcomes for patients undergoing joint replacements, says Tushinski. n H










With cold and flu season upon us, the National Institute on Ageing (NIA) is introducing a series of resources designed to help older adults make informed choices about recommended immunizations to protect them from respiratory and other diseases. These resources include practical guides and reports aimed at closing critical gaps in preventative health measures for older adults who are the most vulnerable to severe disease outcomes.
Among the new releases is the NIA’s fully updated Guide to Vaccines for Older Canadians, a comprehensive resource tailored for older adults looking to stay healthy throughout the fall and winter months and beyond. The Guide covers the importance of vaccines in enabling healthy ageing and provides details on vaccines for COVID-19, Influenza, RSV, Pneumococcal (Pneumonia), Shingles, Tetanus and Diphtheria, including the most recent recommendations from the Public Health Agency of Canada’s National Advisory Committee on Immunization (NACI). Furthermore, this updated Guide will be available in 18 languages over the coming weeks.
In addition, the NIA brings attention to one of Canada’s top killers, pneumonia with its updated report As One of Canada’s Top Killers, Why Isn’t Pneumonia Taken More Seriously? This report calls for urgent action to improve awareness, prevention, and vaccination rates to combat pneumonia and pneumococcal disease across the country. The report sheds light on Canada’s long-standing struggle to meet vaccination targets. Despite the Public Health Agency of Canada’s (PHAC) goal of achieving 80 per cent pneumococcal vaccination coverage for adults 65 and older, only 54.7 per cent of this group had received the vaccine by 2023.
Furthermore, the NIA’s report, Addressing the Significant Impact of RSV Infections among Older Canadians. It’s Time for Action, underscores the need for improved awareness and access to RSV vaccines for older adults. While several

“VACCINATION REMAINS THE MOST EFFECTIVE WAY FOR OLDER ADULTS TO PROTECT THEMSELVES FROM INFLUENZA, PNEUMONIA, AND OTHER RESPIRATORY ILLNESSES THAT CAN HAVE DEVASTATING EFFECTS ON THEIR OVERALL HEALTH AND INDEPENDENCE”
provinces, including Alberta, Manitoba, New Brunswick, Nova Scotia, Ontario, and Québec, now provide public coverage of the RSV vaccine Abrysvo for specific groups of older adults, much more work is needed to ensure that older Canadians understand and easily access RSV vaccines.
“Vaccination remains the most effective way for older adults to protect themselves from Influenza, Pneumonia, and other respiratory illnesses that can have devastating effects on their overall health and independence,” said Dr. Samir Sinha, Director of Health Policy Research of the NIA. “Our resources are here to empower
older adults with the information they need to make proactive choices that help them stay healthy, active, and confident.”
The NIA is calling on Canadians, health care providers, and policymakers to take action and increase influenza and other vaccination rates among older adults. When looking at strategies to Improve Vaccination Rates Against Influenza and Other Respiratory Illnesses Among Older Adults, the NIA recently demonstrated that older adults are most likely to get vaccinated when convenient and accessible options encourage uptake. Of older adults who reported getting vaccinated last cold and flu season,
59 per cent received their flu shot at a pharmacy, 14 per cent at a physician’s office or medical clinic, and 14 per cent at a community-based public health clinic.
“By working together, we can help older adults stay healthy and resilient throughout the current cold and flu season and beyond,” said Alyssa Brierley, Executive Director of the NIA. “Health care providers and policymakers can promote vaccination and ensure accessible immunization options.”
The National Institute on Ageing (NIA) improves the lives of older adults and the systems that support them by convening stakeholders, conducting research, advancing policy solutions and practice innovations, sharing information and shifting attitudes. Our vision is a Canada where older adults feel valued, included, supported and better prepared to age with confidence. n H
Agrowing number of Canadian patients are opting for home-based care as a more comfortable and convenient alternative to in-hospital stays. Vivalink, shares results from a new survey of over 500 Canadians aged 40 and older, revealing their perspectives on participating in a Hospital-at-Home (HaH) program.
According to the survey, nearly 90 per cent of Canadian respondents said they were likely to participate in HaH if it meant they could go home sooner. Of those who had already participated, 81 per cent reported positive experiences, with 48 per cent describing their experience as very positive and 33 per cent as positive. The results signal a clear shift: Canadians are ready to bring healthcare closer to home, and comfort and convenience are driving the transformation.
Key findings from the survey include:
• Nearly 70 per cent of respondents cited comfort and convenience as the primary reasons for opting for HaH monitoring following hospital discharge.
• 74 per cent of respondents said they’d trust their provider’s recommendation to use HaH monitoring.
• Among those who participated in HaH, the most common conditions monitored were cancer, cardiac, and diabetes.
• About 33 per cent of respondents would prefer mostly at-home care, while 34 per cent favor a combination of hospital and at-home care.
The survey also compared Canadian and U.S. patient perspectives on HaH.
Although fewer Canadians participated in HaH programs compared to Americans surveyed earlier this year, a greater number of Canadians were keen to try it. While only 39 per cent of Canadians heard of HaH programs (compared to 66 per cent of Ameri-
cans), 52 per cent of Canadians said they were very likely to opt for HaH to get home sooner, versus 39 per cent of Americans.
The survey also uncovered insights based on age:
• Respondents in their 40s were more likely to have heard of HaH programs (46 per cent ) than those in their 60s (31 per cent ).
• Participation rates were higher among those in their 40s (13 per cent ) than their 60s (3 per cent ).
• Willingness to participate in HaH to return home sooner remained high across all age groups, with 87 per cent of respondents in their 40s, and 90 per cent in both their 50s and 60s expressing interest.
• Preferences for care varied by age, with 41 per cent of those in their 60s preferring mostly at-home care with occasional in-office or hospital visits, compared to 28 per cent of those in their 40s. Most in their 40s (36 per
cent ) favored a combination of athome and hospital care.
“Patients in Canada are showing a clear preference for care that prioritizes their comfort and convenience,” said Aaron Timm, Chief Commercial Officer at Vivalink. “As we work to bring innovative digital healthcare solutions to hospitals and clinics across Canada, it’s evident HaH programs offer a promising path to improving patient outcomes and the efficiency of the healthcare system.”
HaH programs have rapidly expanded across Canada, with provinces like British Columbia (BC) leading the way. Several BC hospitals have integrated HaH into their system, delivering acute-level care in patients’ homes for conditions ranging from chronic illnesses to post-surgical recovery. This expansion highlights a growing recognition of HaH as a solution to alleviate healthcare capacity issues while improving patient outcomes in Canadian healthcare. n H






















































By Marlene Leung
St. Michael’s Hospital researcher is launching a first-of-its-kind global trial to test the impact of MDMA, commonly known as ecstasy, on chronic nerve pain compared with a placebo.
Pending regulatory approval, the St. Michael’s MDMA clinical trial will recruit 30 patients with chronic nerve pain from across Canada. These patients will be randomly assigned to receive either MDMA and psychotherapy or the active placebo methylphenidate, commonly known as Ritalin, and psychotherapy. The trial team, led by Anesthesiologist Dr. Akash Goel, is aiming to start recruitment in January 2025 and completion is scheduled for June 2026. It is the first active-placebo controlled trial of its kind, and Goel recently won $150,000 from the St. Michael’s Hospital Foundation Research Innovation Council to help launch the study.
“Currently, around one in five Canadians suffer from neuropathic pain, and many have no recourse for improvement,” said Goel, noting that common causes of neuropathic pain include diabetes, cancer, surgery and Multiple Sclerosis. “Of these patients, one in five rate their pain as worse than death, so there’s clearly an important need for innovation in this space.”
MDMA, which is short for methylenedioxymethamphetamine, is a synthetic psychoactive drug that works by affecting chemicals in the brain that play key roles in regulating mood, energy and social behavior. MDMA is known for altering mood and perception, and can cause increased feelings of happiness, empathy, energy and can heighten the user’s senses.
First created by Merck in the early 1900s, MDMA was used experimentally to enhance psychotherapy in the 1970s. In the 1990s it became associated with the underground rave scene and is now considered illegal in many jurisdictions, including Canada. Despite its illegal classification, Health
Dr. Akash Goel,

Gabe Ramsay
Canada allowed limited distribution of MDMA for medical and research purposes in 2022.
In recent years, there’s been renewed interest in studying MDMA as a treatment for pain and mental health disorders, said Goel. The results from a 2023 clinical trial found that MDMA significantly improved symptoms of post-traumatic stress disorder (PTSD) in patients compared to placebo and psychotherapy. The trial also found that MDMA significantly improved pain-related disability for a sub-group of participants with chronic pain.
However, the FDA raised concerns with the trial design, in particular, the lack of an appropriate active-placebo, as 90 per cent of patients correctly guessed if they had received MDMA or the placebo.
The St. Michael’s MDMA trial is the most recent study from the Pinnacle Research Group to investigate the effects of psychedelic drugs on chronic neuropathic pain. The Pinnacle Group is conducting similar trials testing the impact of ketamine and psilocybin.
Research suggests that MDMA creates feelings of empathy and openness, so that patients with trauma – and living with chronic nerve pain is trauma – can face it more openly, Goel said.
“This is called fear extinction. They’re able to revisit and explore that trauma in a way that helps them
understand their experiences,” he said.
“This can help them adapt principles of psychotherapy into their daily lives in a more meaningful way and could leave a lasting positive impact on their life.”
There’s also mounting debate over whether MDMA improves neuroplasticity, which is the ability of neural networks in the brain to change through growth or reorganization, Goel adds. MDMA may create an opportunity for someone with chronic pain and unhealthy brain connections to lay down new, healthier neural frameworks, he said.
“I compare it to our aging highway system in Toronto. The highways were built decades ago, and they’re not really set up for the 2020s. What you need to do is lay down a completely new map.
“These are some of the reasons we believe MDMA could be a potential
game changer in the area of pain medicine, as well as other mental health disorders.”
MDMA has side effects, including rapid heartbeat, dehydration, blurred vision, fatigue, depression and anxiety. As such, all participants will be doing psychotherapy while in the trial to ensure that they have stable and constant access to mental health supports, said Goel. The trial team will also touch base with participants regularly to see if they are experiencing prohibitive side effects. Patients who show active suicidality or have a history of psychosis will be excluded from the study to prevent serious adverse events, he said.
“Our research group has a solid infrastructure here at St. Michael’s to ensure that we have the right protocols in place, the right drug manufacturer and we develop our network to ensure that this clinical trial can be executed in a safe manner,” Goel said.
The St. Michael’s pain trials could bring relief to patients like Gabe Ramsay, who’s been suffering from debilitating chronic nerve pain after having elective laser eye surgery in 2018. Following his surgery, Ramsay developed dry eyes and inflammation of his corneas, which eventually developed into corneal neuropathic pain.
“I had a terrible time recovering from the surgery. I’ve had a constant, burning and stabbing pain in my eyes, that’s spread to parts of my face as well,” Ramsay said, noting that his pain drove him to leave work for a few months and even prompted him to decline entering a university Master’s program.
“It’s totally changed my life and everything I do. I’ve been battling it for six years.”
Ramsay had tried different treatments and procedures and even arranged to see a specialist in Boston. Because most of the treatments were
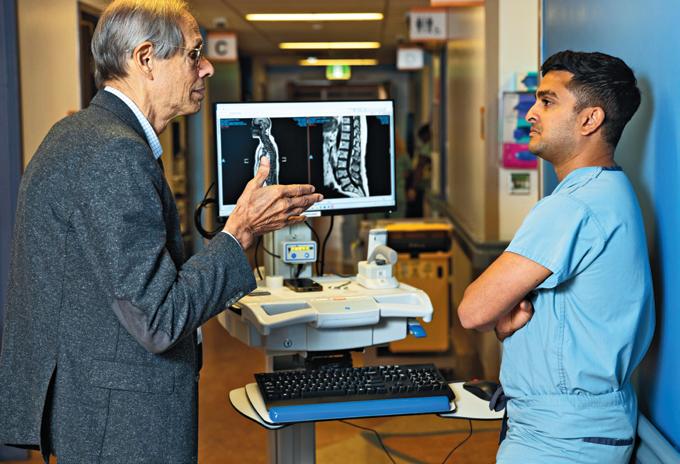
is pictured with Dr. Akash Goel.
not covered by OHIP, he paid for most of them out of pocket.
While he’s made some progress and has returned to work, Ramsay’s still dependent on a number of treatments, including eye drops and medications, which he says make him groggy and affect his short-term memory. He’s still looking for a more effective treatment.
“There’s a psychological aspect of chronic nerve pain, especially when


JANUARY FOCUS: Healthcare Human Resources / Continuing Medical Education (CME)/ Staffing: Continuing Medical Education (CME) for healthcare professionals. The use of simulation in training. Human resource programs implemented to manage stress in the workplace and attract and retain healthcare staff. Health and safety issues for healthcare professionals. Quality work environment initiatives and outcomes.
ANNUAL PROFESSIONAL DEVELOPMENT SUPPLEMENT
Advertising Booking Deadline December 13th, 2024
Material Deadline December 17th, 2024
For more info email advertising@hospitalnews.com
there are no good treatment options,” he said. “The future is just so uncertain, and the pain can get worse. It can spread. This makes it hard psychologically to prepare for the future or think ahead.”
Goel says Ramsay’s experience is one he commonly sees in patients. “It’s not just the pain, it’s how the pain impacts relationships, careers, families,” he said. “It’s an experience.” n H


FEBRUARY FOCUS: Wound Care/ Gerontology/Public Health and Preventative Medicine/Rehabilitation: Geriatric medicine, aging-related health issues and senior friendly strategies. Developments in rehabilitation techniques for a variet of injuries and diseases. Effective approaches for disease prevention and health promotion. Innovation and treatment and prevention of wounds.
WOUND CARE SUPPLEMENT
Advertising Booking Deadline January 24th
Material Deadline January 28th
For more info email advertising@hospitalnews.com

MARCH FOCUS: Facilities Management and Design/Health Technology/Greening Healthcare/Infection Control:
Innovative and efficient healthcare design, the greening of healthcare and facilities management. An update on the impact of technology, including robotics and artificial intelligence on healthcare delivery. Advancements in infection control in hospital settings.
INFECTION CONTROL SUPPLEMENT

Advertising Booking Deadline February 20th
Material Deadline February 24th For more info email advertising@hospitalnews.com


By Melissa McDermott
Canadian startup Incluzia Inc. has won the 2024 AGE-WELL National Impact Challenge: Solutions for Healthy Aging for its evaluation tool that identifies safety risks, generates data-driven recommendations and facilitates collaboration to make a person’s home safer and more accessible.
In making the winning pitch, Marnie Courage, Founder and CEO of Incluzia Inc., said the ultimate goal of the MyHomeFX product is to help older adults, people with disabilities and their care providers make informed decisions about whether to modify their home to make it safer and more accessible or move to a new home to meet their needs. She noted the product is also designed to improve health care service delivery efficiencies and cost savings by reducing falls-related hospitalizations, discharge delays and premature admissions to long-term care.
“In my 20 years of clinical experience as an occupational therapist (OT) working with older adults, people with disabilities and their caregivers, I have seen firsthand the effects of people living in unsafe and inaccessible homes,” said Courage. An OT clinic owner, she pointed to inefficiencies with traditional OT home assessments typically done with pen and paper, a fillable form or spreadsheet, taking hours of manual reporting time – none
“LIKE MANY ENTREPRENEURS, I LAUNCHED MY STARTUP, BUILT A TEAM OF EXPERTS, AND THROUGH RESEARCH COLLABORATIONS, I DEVELOPED THE SOLUTION TO THE PROBLEMS I WANTED TO SOLVE.”
of which facilitates robust data collection, she said.
Courage validated her frustrations in a joint research study with the University of Manitoba by surveying 164 OTs from across Canada about the current methods used for home assessments. She reported that the survey results overwhelmingly confirm the need and desire for the MyHomeFX solution.
Said Courage, “Like many entrepreneurs, I launched my startup, built a team of experts, and through research collaborations, I developed the solution to the problems I wanted to solve.”
There are two versions of MyHomeFX.
MyHomeFX is a free online screening tool for older adults, people with disabilities and their caregivers. It identifies health and home safety risks early and offers data-driven recommendations to increase safety and accessibility at home.
MyHomeFX Pro is a subscription-based digital health assessment
and home evaluation tool for health care professionals. It includes more than 40 health and performance areas of assessment and has a dynamic home evaluation component with features including room measurements, floor plan sketching and photo annotations. It offers health care professionals evidence-based care plan intervention options.
“This tool connects health care and housing,” shared Courage, based in Winnipeg, Manitoba. “One of the challenges right now is that the construction business is nothing like the health care business. They have two different languages. With this solution, we can generate a health care report and redact personal health information for the health care professional to communicate useful information to construction specialists or renovators. It works as a conduit between these two industries to have better outcomes for clients.”
Examples of home modifications that may result from an evaluation include changes to the main en-
trance (e.g., landscaped zero-step entrance or a ramp), adding a bathroom to the main floor, or bathroom adaptions (e.g., grab bars, no-step showers).
Courage explained that the $25,000 cash prize from the AGEWELL National Impact Challenge will help build team capacity, test the business plan, and execute the marketing strategy to hopefully bring MyHomeFX and MyHomeFX Pro to market in late spring 2025. Incluzia Inc. will begin working with the University of Manitoba on acceptance and usability testing, and a pilot will follow in settings within the Manitoba health care system. Courage and her team will also focus on connecting with Indigenous groups to make MyHomeFX a culturally safer option by seeking feedback and making the necessary adjustments before it goes to market.
Courage said, “I am deeply honoured and absolutely thrilled to have won AGE-WELL’s 2024 National Impact Challenge. The other pitches were amazing, so being recognized within that calibre of tech entrepreneurs is really humbling.”
One of Canada’s most exciting startup competitions, this year’s AGEWELL National Impact Challenge was held at the AGE-WELL Annual Conference in Edmonton, Alberta, to

recognize top startups and support entrepreneurship in Canada’s AgeTech sector.
rent and emerging products to support healthy aging,” said Dr. Alex Mihailidis, Scientific Director and CEO of AGE-WELL, Canada’s technology and aging network. “Our pitch competition underscores the talent depth in Canada’s AgeTech sector, which is leading huge technological advances and bringing real solutions to the market that make a difference in the lives of older adults and caregivers.”
and Thriving.ai Inc. came out on top. Thriving.ai has created a digital platform uniting remote care, AI, wearables and the Internet of Things (IoT) to streamline care for older adults and those with chronic conditions.
Four finalists participated in this year’s pitch event, showcasing how their technology-based solution can support healthy aging.
“All four finalists presented pitches that demonstrate the dynamic energy and innovative thinking behind cur-
The runner-up prize of $5,000 went to Fallyx Inc., developers of a wearable, clip-on sensor for fall monitoring. It leverages machine learning to detect falls using location and motion data.
The People’s Choice Award garnered hundreds of online votes,
The 2024 AGE-WELL National Impact Challenge was generously supported by returning key sponsor, the Ontario Brain Institute (OBI), with additional support from the Centre for Aging + Brain Health Innovation (CABHI) and Smart & Biggar.
For more information about the finalists and the competition, visit https://agewell-nce.ca/national-impact-challenge n H
Melissa McDermott is an Ottawa-based communications consultant. AGE-WELL is Canada’s technology and aging network. The pan-Canadian network has mobilized a vast community of researchers, older adults, caregivers, partner organizations and future leaders to accelerate the delivery of technology-based solutions for healthy aging. www.agewell-nce.ca











John Carl Pidlaoan is a Voyago Health Independant Contractor and one of our inspirations serving the Non Emergency Medical Transfer industry.
Along with his dedicated team of Performance Makers, John Carl has consistantly demonstrated truly heroic efforts, delivering the highest level of Patient Centred Care.











Work Ethic ignites motivation, yet it's the fervor and commitment that unlock the door to triumph. Trust in your capabilities, and there's no limit to the remarkable feats you can accomplish. JCP



