



































By Sonia Yung





































By Sonia Yung
ou brought this on yourself with poor eating habits and bad lifestyle choices.”
If you or someone you know has diabetes, you have likely heard this harmful misconception or even thought it yourself.
While the federal government’s proposed pharmacare legislation has put a spotlight on diabetes – with diabetes medications to be among the first prescriptions included in a new national pharmacare plan – erroneous assumptions and negative judgments about the condition persist.
It is time that we erased the stigma surrounding diabetes – not only the one that exists in society, but also the internalized blame and shame that people with diabetes carry.
Close to four million people in Canada have been diagnosed with diabetes – type 2 is the most common form – and the number continues to rise.
Yet, despite diabetes being one of the most common chronic conditions in Canada, it is loaded with negative perceptions. I know this firsthand.
When I was first diagnosed with diabetes, doctors assumed I had type 2 – after all, who gets “juvenile” diabetes at age 50? No other chronic condition comes with feelings of guilt and shame quite like diabetes. The diagnosis left me feeling like I had failed – that it was my fault.
SEPTEMBER 2024 ISSUE
EDITORIAL: Aug. 9
ADVERTISING: Display – Aug. 23 | Material – Aug. 27
Monthly Focus:
Technology and Innovation in Healthcare/Artificial Intelligence (AI)/Patient Experience/Health Promotion/Online Education: New treatment approaches to mental health and addiction. An overview of current research initiatives Programs and initiatives focused on enhancing the patient experience and family centred care. Programs designed to promote wellness and prevent disease including public health initiatives, screening, and hospital initiatives.
Online Education Focus
2024 SPECIAL: MEDTECH Conference Pre-show Edition!
It was not until almost a year later – after medications and lifestyle changes didn’t work – that doctors discovered I had type 1 diabetes – an autoimmune condition.
When I heard that, I have to admit, my immediate reaction was one of relief. If it was not type 2, then it was not my fault – which is untrue; it’s not anyone’s fault they have diabetes.
The internalized negative attitudes towards diabetes come from the messages – spoken and unspoken – we hear regularly: you have diabetes because you are lazy, overweight, or make unhealthy food choices.
Not only are these perceptions wrong, they are harmful. They overlook important uncontrollable risk factors including genetics, environment and social determinants of health. They hurt the mental well-being of those with diabetes and they can jeopardize our health by deterring us from managing the condition – such as skipping blood glucose tests, not injecting insulin when out in public or not even admitting to having diabetes.
Seven years after my diagnosis, internalized blame and shame remain a struggle. I still sometimes feel I am being judged if I order french fries or eat a random cookie. I still sometimes feel like a failure if my glucose monitor shows my numbers are out of range. I still sometimes fail to treat a low blood sugar right away.
Continued on page 9
EDITORIAL: Sept. 6
ADVERTISING: Display – Sept. 27 | Material – Oct. 1
Monthly Focus:
Mental Health and Addiction/Patient Safety/ Research/Infection control: New treatment approaches to mental health and addiction. Developments in patient-safety practices. An overview of current research initiatives. Developments in the prevention and treatment of drug-resistant bacteria and control of infectious (rare) diseases. Programs implemented to reduce hospital acquired infections (HAIs).
Infection Control Supplement – National Infecton Control Week
THANKS TO OUR ADVERTISERS Hospital News is provided at no cost in hospitals. When you visit our advertisers, please mention you saw their ads in Hospital News.
610 Applewood Crescent, Suite 103 Vaughan Ontario L4K 0E3 TEL. 905.532.2600|FAX 1.888.546.6189 www.hospitalnews.com
Editor Kristie Jones editor@hospitalnews.com
Advertising Representatives
Denise Hodgson denise@hospitalnews.com
Publisher Stefan Dreesen stefan@hospitalnews.com
Accounting Inquiries
accountingteam@mediaclassified.ca
Circulation Inquiries info@hospitalnews.com
Director of Print Media
Lauren Reid-Sachs
Helen Reilly, Publicist Health-Care Communications
Bobbi Greenberg, Health care communications
Sarah Quadri Magnotta, Health care communications
Dr. Cory Ross, B.A., MS.C., DC, CSM (OXON), MBA, CHE Vice President, Academic George Brown College, Toronto, ON
ASSOCIATE PARTNERS:
Hospital News is published for hospital health-care professionals, patients, visitors and students. It is available free of charge from distribution racks in hospitals in Ontario. Bulk subscriptions are available for hospitals outside Ontario. The statements, opinions and viewpoints made or expressed by the writers do not necessarily represent the opinions and views of Hospital News, or the publishers.
Hospital News and Members of the Advisory Board assume no responsibility or liability for claims, statements, opinions or views, written or reported by its contributing writers, including product or service information that is advertised.
Changes of address, notices, subscriptions orders and undeliverable address notifications. Subscription rate in Canada for single copies is $29.40 per year. Send enquiries to: subscriptions@ hospitalnews.com
Canadian Publications mail sales product agreement number 42578518.






By Robyn Cox







s a Level 1 Trauma Centre, St. Michael’s Hospital receives patients from all over Ontario who have sustained sudden, severe injuries –such as injures from a car collision or a sporting accident. When a trauma patient arrives to the hospital, the trauma team springs into action to provide life-saving care.
Over the past year, the Trauma, Emergency Department, Neurosurgery and Medical Imaging teams have partnered with Unity Health’s applied AI team to develop and use a number of different AI tools to improve care and outcomes for trauma patients.
Traumatic brain injuries (TBIs) happen when a sudden strike to the head damages the brain. TBIs are the leading cause of death and disability in young people globally and 22 per cent of all injury-related deaths in Canada are the result of a TBI.
The type of treatment a patient will receive for a TBI depends on the severity of their injury – some patients may need short-term observation, while others may require an urgent, life-saving brain surgery. Neurosurgeons provide consultation on TBIs to provide an expert recommendation on treatment. At St. Michael’s Hospital, neurosurgeons provide more consultations than all other specialty services combined.
“Every patient with a TBI is triaged in the same way, even though only 20 per cent of patients will require surgery,” says Dr. Christopher Witiw, a neurosurgeon at St. Michael’s Hospital. “Whether it’s the middle of the night, the middle of the day or in the middle of another surgery, the neurosurgeon on-call needs to review the head CT scans and provide a consultation.”
ASIST-TBI is the name of an AI tool that helps to speed up triage for TBI patients by screening the CT scans for patients who come to the St. Michael’s Emergency Department with a head injury. If the model predicts the need for surgery – which it can do just as accurately as a neurosurgeon – the ED physician will consult a neurosurgeon directly, instead of waiting for the radiologist to review the CT scans first.
ASIST-TBI will also be tested and launched to the St. Joseph’s Emergency Department to help even more patients.
An intracranial hemorrhage (ICH), more commonly known as a brain bleed, can happen from an external cause, such as a TBI, or from an internal cause, such as a stroke. Brain bleeds can cause permanent brain damage and even death. Fast diagnosis and treatment is critical to recovery.
The brain bleed detection tool predicts whether a patient has a brain bleed. Neuroradiologists typically need

to review 25 to 50 head CT and MRI scans a day, and this tool helps to streamline the process.
“Implementing the brain bleed detection tool has enhanced our ability to quickly and accurately diagnose intracranial hemorrhage,” says Dr. Errol Colak, a radiologist at St. Michael’s Hospital. “This technology empowers our radiologists to focus on the most critical cases first with the aim of improving patient outcomes and saving lives.”
The AI solution is already being used in the St. Michael’s Emergency Department and correctly identifies more than 85 per cent of cases where the patient has a brain bleed.
Trauma resuscitation is the act of reviving someone from a life-threatening injury. It is extremely fast-paced and task-oriented. Trauma teams rarely have time to review bloodwork results or consider how a patient is trending so they can anticipate their future needs. Trauma AI is the name for a group of tools that will be used to support the resuscitation of severely injured patients in the St. Michael’s trauma bay.
Trauma AI will use data from monitors and devices that measure a patient’s physical state, such as their heart rate, blood pressure and oxygen levels. It will also use data from the electronic medical record, such as how the patient was injured, the patient’s



demographics and – importantly –bloodwork and lab results. Blending these different types of data, Trauma AI aims to make predictions and recommendations that will help the trauma team to personalize their care approach in real-time.
“Trauma AI will be like having a hematologist in your corner, helping to interpret some of the patient’s blood tests,” says Dr. Brodie Nolan, a trauma team leader and scientist at St. Michael’s who is one of the clinical leads on this AI project. “It will also have a predictive trajectory for patients who are becoming unstable so we can mobilize additional resources in the hospital, like getting the operating room ready.”
Hematologists are doctors who specialize in blood and bleeding. The other clinical lead on the project is Dr. Michelle Sholzberg, a hematologist and scientist at St. Michael’s and a leading expert in her field. Getting bleeding under control is one of the central ways to improve outcomes for trauma patients. Care interventions for bleeding are an area of trauma care where there is a lot of opportunity to improve and personalize care.
“The more we can tease out really individualized treatments for patients is probably the next step for where trauma resuscitation is going,” says Nolan.
Trauma AI recently received a grant from the New Frontiers in Research Fund and planning is underway to make these tools a reality over the next two years. ■ H

In Canada, rates of hypertensive disorders of pregnancy (HDP) have increased, but the good news is there has been a decline in some related health conditions, according to new research published in CMAJ (Canadian Medical Association Journal).
Hypertensive disorders of pregnancy include chronic hypertension (high blood pressure), gestational hypertension, and preeclampsia or eclampsia. These disorders affect five –10 per cent of pregnancies worldwide, and cause more than 50,000 maternal deaths and 500,000 deaths in fetuses and infants every year.
A large study of more than 2.8 million births in hospital in Canada (excluding Quebec) between 2012 and 2021 dentified females with HDP, with the aim of understanding trends in HDP and related health outcomes. Over the study period, the rate of any HDP increased from 6.1 to 8.5 per cent in absolute numbers, with a relative increase of 40 per cent. Pre-existing hypertension temporally increased from 0.6 to 0.9 per cent, gestational hypertension rose from 3.9 to 5.1 per cent, and preeclampsia from 1.2 to 2.6 per cent.
The researchers noted several trends. Rates of HDP were higher in females under age 20 and in those older than 34 years. There was also variability in rates across provinces and territories, with the Northwest Territories (6.5%) and Ontario (6.9%) having the lowest rates, and the highest rate (10.7%) in Newfoundland and Labrador.
The authors adjusted for risk factors for HDP, including maternal age, number of previous livebirths, pre-existing diabetes, and rural residence, but doing so did not significantly affect the risk of HDP. “[T]he rise in HDP may be explained by factors that we did not account for, including body mass index (BMI),” writes lead author Dr. Susie Dzakpasu, senior epidemiologist at the Maternal and Infant Health Section of the Public Health Agency of Canada, with coauthors. “High BMI is a known risk factor for hypertension, including during pregnancy.”
FEMALES WITH HYPERTENSION AND OTHER DISORDERS SHOULD BE MONITORED IN THE EARLY POSTPARTUM PERIOD, YET THERE IS A SHORTAGE OF QUALIFIED HEALTH CARE PROVIDERS.
Between 2015 and 2021 in Canada, rates of overweight or obese BMI status increased from 41 to 48 per cent among females aged 18–34 years, and from 56 to 64 per cent in those aged 35-49 years. The authors also found that provinces with higher rates of overweight and obesity had higher rates of HDP.
“Downward trends in other adverse outcomes suggest that the clinical management of HDP may have improved over time,” write the authors. “This underscores the impor-
tance of standard measurement of blood pressure at each prenatal visit and the institution of evidence-based antihypertensive therapy.”
In a related editorial, Dr. Catherine Varner, deputy editor, CMAJ, writes that the “growing population of high-risk obstetrical patients should alert health policy-makers that more people need easily accessed, specialized obstetrical care.”
Females with hypertension and other disorders should be monitored in the early postpartum period, yet there is a shortage of qualified health care providers.
The findings of Dzakpasu and colleagues “highlight the increasing demand for obstetrical care providers with the expertise to care for high-risk patients, supported by appropriate models of care both before and after delivery. As the number of obstetricians will be unable to conceivably meet the needs of the growing population entering their reproductive lives with more comorbidities than the preceding generation, scaling team-based maternity care may help people receive the right care, at the right time, in the right place, by the right provider,” Dr. Varner concludes.
“Trends in rate of hypertensive disorders of pregnancy and associated morbidities in Canada: a population-based study (2012–2021)” and “Optimizing postpartum care in Canada as rates of comorbidities in pregnancy rise” was published July 29, 2024. ■ H
New research aims to help reduce the quantity of unused prescription opioids after emergency department visits and lessen the risk of opioid misuse and overdose. The study is published in CMAJ (Canadian Medical Association Journal).
Overprescribing is linked to opioid misuse and overdose, with household supplies of opioids associated with an increased risk of overdose, as many people do not dispose of unused medications safely. In Canada, more than 7,500 people died of opioid overdoses in 2021, and more than 68 000 people died in the United States in 2020 from these drugs.
A team from the Network of Canadian Emergency Researchers conducted a study at 7 emergency departments (6 academic tertiary care hospitals and 1 community hospital) in Quebec and Ontario to determine the ideal quantity of prescription opioids to control pain in patients discharged from emer-
gency departments and reduce unused opioids available for misuse.
“As higher quantities of prescribed opioids are associated with higher quantities of consumed opioids, it is important to adapt opioid prescription practices to patients’ analgesic needs for specific acute pain conditions while minimizing the number of unused opioid tablets that can be diverted or misused,” writes Dr. Raoul Daoust, Centre intégré universitaire de santé et de services sociaux (CIUSSS) du Nord-de-l’Île-de-Montréal, Hôpital du Sacré-Coeur-de-Montréal, and the Department of Family and Emergency Medicine, Université de Montréal, Montréal, Quebec, with coauthors.
The study included 2240 participants, with a median age of 51 years, who were asked in 14-day diaries and follow-up phone interviews if they filled their prescriptions, how many pills of opioids they took (converted to 5 mg morphine per tablet), and if they filled any new prescriptions. Half of participants received
a prescription of 16 tablets or more, and 63 per cent of these were not used. Consumption of opioids was low, half of patients consumed fewer than five tablets, and consumption varied significantly by type of pain condition.
“The authors suggest that clinicians could adapt prescribing quantity to the specific condition causing pain, based on estimates to alleviate pain in 80 per cent of patients for 2 weeks, with the smallest quantity for kidney or abdominal pain (8 tablets) and the highest for back pain (21 tablets) or fractures (24 tablets), and add an expiry date for use (e.g., 3, 7, or 14 days). Furthermore, since half of participants consumed even smaller quantities, pharmacists could provide half this quantity (partitioning) to further reduce unused opioids available for misuse.
“Opioid prescribing requirements to minimize unused medications after an emergency department visit for acute pain: a prospective cohort study” was published July 15, 2024. ■ H
lobally and in Canada, new cases of HIV and other sexually transmitted and blood-borne infections (STBBIs) have been rising steadily. Although significant progress has been made in developing effective therapies to combat HIV, a cure and vaccine remain elusive. Coinfections also pose unique challenges in terms of diagnosis, treatment and prevention.
Thanks to a five-year, $25-million investment from the Canadian Institutes of Health Research (CIHR), the Pan-Canadian HIV/AIDS Clinical Trials Network (CTN) will expand to address these challenges. Originally established in 1990 as a cornerstone of the federal AIDS Strategy, the CTN will broaden its focus to include all sexually transmitted and blood-borne infections (STBBIs), and will become known as CTN+. Under the leadership of National Director Dr. Marina Klein at the Research Institute of the McGill University Health Centre (RIMUHC) in Montreal, the network will undertake clinical trials to find new ways to prevent, treat and manage HIV and other STBBIs, prioritizing a community-based approach to ensure relevant solutions for Canada’s most at-risk populations. It will also invest in developing the next generation of Canadian researchers, to increase the country’s capacity to conduct clinical trials and improve the health and wellbeing of people living with and affected by STBBIs.
“The CIHR Canadian HIV Trials Network has fostered collaborative science nationally and globally for more than three decades. It has enabled important research advances and facilitated access to the latest treatments,” says Dr. Klein, Senior Scientist in the Infectious Diseases and Immunity in Global Health Program at the RIMUHC and Professor in the Department of Medicine at McGill University. “I am proud to help shape the future of the Network as it expands to focus on other important infections that affect the lives of Canadians. It will be an honour to continue building on the
CTN’s success with our colleagues and community partners across Canada and to guide the next generation of innovators and researchers in working towards eliminating HIV and STBBIs as public health threats.”
The CIHR Pan-Canadian Network for HIV/AIDS and STBBI Clinical Trials Research (CTN+) will expand upon the research framework of the CTN, decentralizing to become a country-wide network that facilitates the design, conduct and dissemination of equitable, community-informed, scientifically rigorous, and timely research across disciplines, infections, and key populations in both HIV and other STBBIs.
NEW CASES OF HIV AND OTHER SEXUALLY TRANSMITTED AND BLOOD-BORNE INFECTIONS (STBBIS) HAVE BEEN RISING STEADILY.
HIV remains an important health threat across the world and in Canada. According to the CIHR, in 2022, globally:
• 39 million people were living with HIV
• 630,000 died from HIV/AIDS
• 1.3 million people were newly infected
• an estimated 58 million people were living with chronic hepatitis C and 296 million with hepatitis B
In Canada, the challenges in treatment and prevention of STBBI vary by region. Clinical trial infrastructure is concentrated in the biggest cities, creating barriers to participation for rural, remote and isolated communities and resulting in poorer health outcomes for populations disproportionately affected by STBBI.
By renewing, diversifying and restructuring, CTN+ will address the
current landscape of HIV and STBBIs and enhance Canada’s capacity to respond rapidly to emerging infectious diseases that may prominently impact vulnerable populations. To do this, Dr. Klein will lead a diverse network with five regional teams, four specialized think tanks and a community-centred knowledge mobilization hub. These regional teams, which will include researchers, community members and Indigenous representation, will champion the knowledge needs of those in their respective communities.
Recognizing the importance of engaging community throughout the research process, CTN+ will build from a legacy of meaningful community involvement, with community perspectives incorporated throughout the leadership and operation of the Network.
“Community involvement has always been a priority at the CTN, with CTN+ we are increasing community involvement in all aspects from clinical trial research, from trial representation and trial design to knowledge sharing” says Muluba Habanyama, also a Community Co-Lead and Co-Principal Knowledge User. “Community leadership is paramount in shaping the future of research conducted by the CTN+ to ensure ’nothing about us, without us.’”
“I am very excited for CTN+’s renewed vision of involving the HIV and STBBI community in clinical trial research,” adds Enrico Mandarino, Co-Lead of the new Community Leadership Team and Co-Principal Knowledge User on the funding application. “I look forward to bringing my experience as a member of CTN’s Community Advisory Committee to provide stronger emphasis on leadership, oversight, and guidance from the community on setting the research priorities and mentoring for CTN+.”
Acknowledging the power of research and knowledge mobilization to improve health equity across the country, as well as the need to uphold Indigenous rights and move toward truth and reconciliation, the Network will also embed Indigenous knowledge users in leadership positions and integrate Indigenous perspectives into its core operations and processes.
“As someone who has spent the past 24 years working in the field of Indigenous women’s health with a focus on HIV, I see the critical need to further build capacity within Indigenous communities for research conducted by communities, rather than the historical relationship of outside researchers conducting work on communities,” says Carrie Martin, the Network’s Indigenous Principal Knowledge User. “Health inequities experienced by Indigenous Peoples in Canada include the disproportionate impact of HIV and other STBBIs. These inequities are directly linked to systemic racism and colonial policies.”
“We are delighted and honoured to welcome the CTN+ to the RIMUHC. Marina Klein has been a leader in research and care for HIV and hepatitis C coinfection for many years, and I warmly congratulate her for this nomination as National Director of the pan-Canadian interdisciplinary CTN+ network. I am confident that this network will enhance Canada’s capacity to address HIV and STBBI from prevention to cure,” says Dr. Rhian Touyz, Executive Director and Chief Scientific Officer of the RI-MUHC.
As the Canada Research Chair in Clinical and Epidemiologic Studies of Chronic Viral Infections in Vulnerable Populations, Dr. Klein is known for leading one of the largest cohorts focused on HIV and hepatitis C virus (HCV) coinfection in the world, documenting the impact of new HCV therapies on health outcomes, designing and testing tailored approaches to increase access to diagnosis and treatment, building capacity for research with Indigenous communities, and using evidence to advocate for policy change. ■ H
By Catherine Danko
In a Canadian-first procedure, a surgical team at UHN’s Peter Munk Cardiac Centre (PMCC) has eliminated an adult patient’s irregular heartbeat – arrhythmia – by accessing the heart through a vein in the liver.
The procedure, known as a trans-hepatic approach, was performed earlier this spring on a patient with a congenital heart disease who had an interrupted inferior vena cava (IVC) – the vein responsible for transporting deoxygenated blood from the lower body to the right side of the heart, which is the typical point of entry to destroy atrial arrhythmias.
“This is a new way for us to perform arrhythmia ablation for a subset of patients with congenital heart disease,” says Dr. Krishnakumar Nair, cardiac electrophysiologist at PMCC.
The catheter-based procedure was performed on 60-year-old patient Amy Shannon, the first adult to receive the surgery in Canada.
“I knew Toronto General Hospital was the best place to have my surgery done,” says Amy, a retired teacher who was born with a heart defect called anomalous left coronary artery from the pulmonary artery (ALCAPA). It was discovered at age 48 after she began experiencing shortness of breath when walking and resting, a rare diagnosis as it’s most often noticed in babies and young children.
“When I go [to TGH], I know that I’m safe and that I can trust everyone from the nurses to the doctors, which makes me feel very secure,” she says.
ALCAPA occurs when the left coronary artery arises from the pulmonary artery, carrying blood without oxygen to the side of the heart. In Amy’s case, her right coronary artery had been supplying oxygen to the left side of her heart.
After having open heart surgery for her ALCAPA, she began experiencing arrhythmias.
Amy was prescribed medication for the arrhythmia but was drug-resis-

tant. Instead, she needed an ablation – a procedure that burns heart cells to cause scarring on the inside of the heart, breaking up the electrical signals that cause irregular heartbeats and helping to maintain a normal heart rhythm.
Because Amy’s IVC did not drain directly to the heart, Dr. Nair, her primary cardiac electrophysiologist, thought of an alternative solution to get into Amy’s heart to perform the ablation: getting access to the left atrium via one of the veins in the liver, something only a handful of specialized centres in the world have done to date – making UHN the first in Canada to use the approach on an adult patient.
Dr. George Oreopoulos and the interventional radiology team created a small surgical passage for hepatic access, enabling the subsequent ablation of the left atrium by the electrophysiology team led by Dr Nair.
The surgery went smoothly, with no complications reported during or after the procedure. Notably, the patient experienced significant improvement in her arrhythmic symptoms at the one-month follow-up.
“TGH has the world’s largest adult congenital cardiac centre, and a signif-
icant proportion of patients with operative heart disease have arrhythmias,” says Dr. Nair.
Amy has recovered well since having the surgery and says that she no longer needs cardioversion – a procedure used to return an abnormal heartbeat to a normal rhythm, something that she would often endure prior to the treatment. She continues to travel from her home in Lindsay, Ont. to TGH’s Congenital Heart Clinic for checkups.
The procedure was a department-wide collaboration between cardiac electrophysiology, congenital heart disease, anesthesiology, interventional radiology, catheterization laboratory and nursing.
“One of the strengths of UHN is that there are experts in multiple disciplines,” says Dr. Andrew Ha, cardiac electrophysiologist and Director of Electrophysiology at PMCC, who worked on Amy’s case alongside Dr. Nair.
“If you have a patient need like Amy, you can offer something that is
creative, safe, cutting edge, and you can draw on the expertise of multiple people to do it.
“The advocacy to push boundaries of patient care at UHN allows us to find safe and innovative ways to help our patients, even if it’s never been done before.”
This achievement was the result of a multidisciplinary effort involving UHN nurses, educators, the catheterization team and several physicians, including: Dr. Nair, Dr. Ha and Dr. Jayant Kakarla (fellow) of the cardiac electrophysiology team; Dr. Oreopoulos and Dr. Omid Shearkhani (fellow) of the interventional radiology team; Dr. Marjan Jariani and Dr. Adam Snyman of the anesthesiology team; and Dr. Rafael Alonso-Gonzalez of the congenital heart disease team.
“Multidisciplinary collaboration is the UHN ‘superpower’ that allows teams to offer hope to patients with the most complex problems,” Dr. Oreopoulos says. “We teach our residents and fellows the benefits of this institutional culture so that they may be a force to bring others together to help their own patients in the future.” ■ H
By Michele Sponagle
It’s difficult to define narrowly the work Kelly Davison does to advocate for the health of local communities and Indigenous people, including Métis like himself. It’s multi-faceted and spreads across multiple organizations, but health equity is always at the core.
He is a registered nurse working with the Ministry of Health in British Columbia, Insite in Vancouver’s Downtown Eastside and Lion’s Gate Hospital. He is also a research coordinator for Dr. Lisa Bourque Bearskin, the B.C. Chair of Indigenous Health Nursing Research, and a co-chair of the Sex-Gender Working Group with Canada Health Infoway and trainee with the University of Victoria’s gender, sex and sexual orientation re-
Continued from page 4
(To this day, my best friend talks about the time I had severe hypoglycemia while driving through a major traffic jam and nobody in the car had any idea until my glucose monitor alarm started really screaming.) I still sometimes silence those alerts and alarms during meetings or events because I don’t want to bring attention to myself.
Diabetes Canada is spearheading research into just how prevalent the stigma is. The insights will shed light on how it affects people with diabetes and why it is important that we change how diabetes is perceived.
A vital part of changing the conversation around diabetes is changing the internal dialogue those of us with diabetes have. For me, this includes being fine with leading the way to the buffet table at a function because my blood sugar is dropping (it’s rather hilarious how quickly a line forms behind me). This includes treating my devices as
search team. He is currently working on his PhD.
Davison’s passion for improving health care runs deep. Born and raised in Calgary, Davison moved to B.C. in 2007 to set down roots. Early on, he knew the focus would be on health.
“Everything connects to health – air and water quality, social engagement, education…,” says Davison. “This is what many people don’t appreciate. Humans are a part of the ecosystem; our lives depend on the natural environment.”
It was something he learned from Elders he worked with as an archaeologist alongside Indigenous community members doing community-based Indigenous Knowledge Research. He helped bring community voice to the assessment of potential impacts of in-
dustrial projects. The Elders talked often about the connection between life, air, water, the land, spirituality and human health. That understanding of holistic connections inspired his research supported by AGE-WELL, Canada’s technology and aging network.
In 2020, Davison was awarded AGE-WELL’s Indigenous Graduate Fellowship in Technology and Aging, a scholarship award that provided funding for him to explore the effects of virtual care on community-dwelling older adults, including the unprecedented mobilization of virtual care services during the pandemic. Collaborating with Dr. Bearskin, he has shifted his work from Two-Eyed Seeing to Wise Practices for telehealth for Indigenous communities. “Every community is different and the Wise Practices for each one will be different.”
cause not everybody wants to, or can, travel long distances to see a doctor or a specialist.”
Adding to the care disparity for Indigenous communities is the risk to individuals of “…being stigmatized, discriminated against, racialized and harmed, if you’re not from colonial culture,” as Davison points out. Being an advocate means improving the experience for Indigenous people seeking health care.
fashion accessories (who said stickers are just for kids?) and visibly wearing them.
When I was travelling through Asia last year, an American tourist stopped me and asked if the device on my arm was a glucose monitor. She had been diagnosed with type 2 and her doctor suggested she get one. She had never seen someone with one before, wasn’t sure how they worked and was nervous about wearing one.
I explained how my glucose monitor worked and, after I answered her questions, she said she was going to give one a try when she got home.
It was an important lesson learned. Because I was not hiding my diabetes, I was able to help someone feel better about managing theirs.
By talking more openly about diabetes, together, we can dispel the misconceptions and erase the stigma people with diabetes have carried for far too long. ■ H
Sonia Yung is the Board Chair for Diabetes Canada and strives to live unapologetically with Type 1 diabetes.
It’s also a chance to create change, explains Davison. “There’s always been a disparity in terms of health services in communities versus that in bigger centres. That’s an economic and geographical factor, but a cultural one as well. There is an interesting opportunity to start closing that gap, especially in more remote areas, be-
To help do that effectively, Davison’s AGE-WELL training has been a key to his success. “It provided me with an excellent foundation for my research and advocacy work,” he says. “It delved into ethics, diversity and inclusion, racism and stigma –all very important topics. The training also covered how to engage with policy change effectively and how to build networks. As an emerging scholar, health-care professional and researcher, it was invaluable.”
As an EPIC (Early Professionals, Inspired Careers) training graduate, he is focused on improving access to health care, making it easier and safer, especially for marginalized people. Davison hopes he can affect change and help create a new path for accessibility and equity. ■ H
Michele Sponagle is a freelance writer. AGE-WELL is Canada’s technology and aging network. The pan-Canadian network has mobilized a vast community of researchers, older adults, caregivers, partner organizations and future leaders to accelerate the delivery of technology-based solutions for healthy aging. For more information, visit www.agewell-nce.ca
By Shaelyn Winters
June is Stroke Awareness Month, an opportunity to raise awareness about stroke and stroke care. Stroke is a serious medical emergency, with roughly 108,000 stroke occurrences each year in Canada. This equates to about one stroke every five minutes.
Unity Health Toronto provides care for stroke patients at every stage of their journey: from hyperacute and acute care in the Emergency Departments and Stroke Unit at St. Michael’s and St. Joseph’s, to rehabilitation at Providence Healthcare, and secondary prevention services at our sites. We also train learners in various disciplines in all aspects of stroke care, including nurses, physicians, medical imaging technologists, physiotherapists, occupational therapy, dietitians, and social work, to name a few.
We asked several learners from across Unity Health Toronto to share their experiences learning about stroke treatment and care. Watch the video and read on below to hear what they had to say:
Dr. Fatma Ger Akarsu, Stroke Fellow; The learning environment at Unity Health Toronto is collaborative and supportive. Trainees are encouraged to participate in multidisciplinary discussions, which help in understanding complex cases better.
There is the opportunity for handson patient care, allowing for the direct application and refinement of skills in diagnosing and managing stroke cases. This practical experience is invaluable for professional development, enabling learning from real-world scenarios and patient interactions. The hospital’s focus on education and mentorship supports growth by providing access to experts in the field and resources for continuous learning.
Dr. Justine Itorralba, 4th Year Neurology Resident: Part of what makes Unity Health stand out is that there is good collegiality between services. For instance, if I have a question about imaging, I can just walk over to
the Neuroradiology staff’s office and review immediately. Not only have I always felt welcome doing this, but I’ve also had some of my best neuroimaging teaching during these impromptu sessions.
Some standout learning moments include when our social workers were able to get a brand new motorized wheelchair donated for one of our patients and another moment where they were able to find sponsored accommodation for a patient who was unhoused. Our Stroke Health Discipline Teams are truly the best in the city!
Emily, Occupational Therapy Student Stroke/Neuro Rehab:I became interested in stroke care as I had a family member staying in a stroke rehab unit about ten years ago. Seeing their recovery really inspired me and
it was also my first exposure to occupational therapy, which is my current career goal. Because of that, stroke care overall has a really meaningful and special place in my heart.
Learning from the patients has been incredible and being able to see their motivation and how hard they work to achieve their goals. Seeing patients go from being in a wheelchair and dependent on someone for all of their daily activities, to being more independent and being able to prepare a light meal while standing has been really incredible to see.
Megan Hird, 3rd Year Neurology Resident:The allied health and nursing team on the Stroke Unit have created a highly collegial atmosphere, providing not only excellent patient care, but a great learning environment for trainees and learners. Furthermore,
the medical staff are dedicated to trainee learning, providing invaluable teaching both formally and around cases.
On call, a very young woman came in with a catastrophic stroke, causing right-sided paralysis and an inability to speak from a very rare etiology. From the moment she arrived via EMS, the Stroke Team and Interventional Team worked quickly to treat her, successfully removing the clot. Over the upcoming days, it was incredible to see the progress she made. On my last day of the rotation, I recall meeting her in the hallway as she walked independently and spoke to me fluently. It was an unforgettable moment. ■ H
Winters works in communications at Unity Health.
By Olivia Lavery
St. Michael’s Hospital neurologist and researcher Dr. Manav Vyas has always been interested in the mysteries of the brain. ‘It’s almost like a puzzle you’re trying to solve,” Vyas says. “I like the problem solving.”
One of the most confounding mysteries comes in the form of multiple sclerosis, a disease where a person’s immune system attacks the myelin sheath – the protecting covering of nerve cells in the brain, optic nerve and spinal cord – resulting in a range of symptoms that can have massive impact on patients’ lives.
Canada has the largest population of patients with MS in the world, and in a recent study published in Neurology, Vyas examined how the proportion of life spent in Canada correlates to incidence of MS in permanent immigrants to the country.
The results of the study, which followed 1.5 million people who arrived in Canada between 1985 and 2003, suggest immigrants who have spent a greater proportion of their lives in Canada have a greater risk of developing MS than people who have spent a smaller proportion of their lives there.
Throughout the time of the study, 934 people were diagnosed with MS. Study participants who had been in Canada for 70 per cent of their lives were 38 per cent more likely to develop MS than those who had been here for 20 per cent of their lives.
Age may also play a role, with those who arrived before the age of 15 being more at risk.
Vyas says it’s important to look at MS from a global perspective. “We traditionally think of MS as a very Eurocentric disease, but we’re studying people from all over the world,” he says.
While the study does not investigate the causes of MS in immigrants, researchers believe that things like smoking rates, changes in diet and other environmental factors may play a role, as well as social determinants like inadequate access to healthy and affordable foods.
Vyas says studying MS is a long game. It can sometimes feel like every new discovery only creates more questions and mystery. Researchers and clinicians don’t know for sure what triggers MS, and at the moment there isn’t clarity on what can prevent it from happening in the first place.
But it’s also an inspiring journey to be a part of.
“I think the frustration, which becomes hope, is that we’re narrowing down potential factors that might be causative of multiple sclerosis,” says Vyas. “The research is a marathon, and the best discoveries occur when we’re all working together.” ■ H
By Dr. Nadiya Sunderji
s I reflect on my first two years as President and CEO at Waypoint Centre for Mental Health Care, I am struck by the transformative power of possibility – and hope.
Keeping pace with increased need demand for mental health, addiction and geriatric care in Ontario is challenging and requires the leadership, innovation and expertise of many team members and partners.
As leaders in system transformation and design, we work closely with partners across Ontario to create seamless care that supports patients in every way. We are grateful to work closely with the Ontario Health Mental Health and Addictions Centre of Excellence and with Ontario Health Central region in imagining a better future and engaging partners in making that dream a reality.
Construction will soon get underway on a new 20-bed acute mental health care unit, which will include the area’s first psychiatric ICU beds so that individuals with increased risk due to severe mental illness will have access to specialized care and expertise. As a regional centre, these beds at Waypoint will benefit patients across the region and relieve emergency department pressures at eight partner hospitals.
We have been pleased to lead collaborative efforts among hospitals in our

region to plan for future acute mental health capacity needs, balancing the need to serve a growing and increasingly acute and complex population with the present realities of capital redevelopment. We can be proud of our collective advocacy for investments across the continuum of care, primarily in community services that will better connect patients with the specialized assessments and care they need while further reducing pressures on emergency departments. Our proposal for expanded urgent, emergent and crisis mental health services is also supported by our co-design efforts with people who have used emergency departments for a mental health crisis, and we hope it will influence health care system design for a better future.
Waypoint serves some of the most complex and disadvantaged people in the province. Among our many specialized services, we are also the only Ontario hospital providing high-secure provincial forensic programs to patients who face the double stigma of severe mental illness and justice system involvement. Offering unwavering support, we guide patients through their darkest moments with compassion and expertise. We challenge the stigma surrounding mental illness and addiction, and foster an environment where every person is embraced with understanding and acceptance.
I am proud of and grateful to our staff, who consistently deliver high-quality

care and provide hope for a better future. Each patient’s journey is unique, and we support their recovery with compassion, dignity and inclusivity.
Waypoint’s vision – to change lives by leading the advancement and delivery of compassionate care – drives everything we do. From best-practice treatments and innovative service delivery models to cutting-edge research informed by patient perspectives, we are pushing boundaries and setting new standards.
Celebrating diversity, encouraging innovation and valuing each team

member’s unique contributions is also important to me and our senior leadership team. Looking ahead, we are committed to maintaining an environment where everyone feels inspired and supported to bring forth their gifts.
I remain humbled to work alongside Waypoint’s amazing staff, physicians and volunteers. I’m grateful to the board of directors and senior leadership team for their tremendous support, dedication and trust. I appreciate their contributions to this incredible journey. ■ H

BY Olivia Lavery
helicopter descends into Toronto’s downtown core minutes before 4:30 p.m., rotor blades whirring against a clear blue sky as it cuts a line between skyscrapers and lands on the roof of St. Michael’s Hospital.
The patient, injured in a car crash outside of the city, is rushed from the helipad into an elevator and down to the trauma bay, where physicians, nurses, respiratory therapists and imaging experts get to work.

It’s a typical evening in ‘trauma season’ at one of Canada’s top trauma care hospitals. That’s the name given to a stretch of warm summer months when injuries increase as people take to the outdoors on bicycles, boats, motorcycles and cars. Each year, roughly 1,500 patients from across Ontario are cared for by the elite trauma team at St. Michael’s, but in the warmer months between May and October, they see a surge: 855 people were cared for last year at that time. For the past three years, trauma teams were activated 434 times in August alone.
St. Michael’s, part of Unity Health Toronto health care network, is a key partner in delivering urgent care to Ontarians. It is one of only a handful of hospitals outside of the United States verified as a Level 1 Trauma Centre by the American College of Surgeons. That verification, awarded in 2023, means injured patients receive the highest quality care informed by the best available evidence from an elite trauma team with support from radiology, transfusion medicine, emergency medicine, surgery, research, rehabilitation, emergency preparedness, anesthesiology, intensive care and more.
In trauma, every minute counts, but none more so than the first 60 minutes following a traumatic event or injury.
Emergency Nurse Jannet Hudson moves a light to help Orthopaedic Surgery Resident Dr. Abdulrahman Jad as he examines a patient.



That’s why St. Michael’s has a helipad. Patients from across the province are air-lifted by Ornge helicopters to regional trauma centres like St. Michael’s to get access to specialties they wouldn’t have closer to home like neurosurgery and advanced imaging.
“There has to be a lot of collaboration between first responders and hospital teams,” says trauma surgeon Dr. Andrew Beckett, Director of Trauma at St. Michael’s. “For a patient to survive it has to be a finely tuned system.”
A former army medic and current lieutenant-colonel in the Canadian Armed Forces, Beckett served in Yugoslavia in the 1990s, and again in Iraq and Afghanistan in the early 2000s. In addition to his work as a surgeon, Beckett is a passionate researcher who has spent years investigating and advocating for better mechanisms for things like blood transfusion and pre-hospital care.
“No one is more important than anyone else,” he says of the team. “I am one cog in the machine.”
Unlike most war hospitals, St. Michael’s is home to a vast network of surgical specialties. Neurosurgeons, orthopaedic surgeons and plastic surgeons often consult and operate on cases that come in, among many other possibilities. Having this kind of expertise right in the building gives patients a better chance at not only survival, but optimal recovery from their injuries.
Shortly after 5 p.m. Beckett enters the trauma bay and is greeted by trauma team leader Dr. Garrick Mok. The patient will need scans to evaluate potential head injuries, and then further monitoring to decide whether surgery is necessary.
As a trauma surgeon, Beckett’s expertise isn’t immediately needed.
He’ll follow the patient for the next hour as Mok and the team decide on a treatment plan, and then he’ll wait for other cases that come in during the 15 hours he’s on call.
The team finishes up in the trauma bay and heads up to the imaging department. Beckett, Mok and a group of technologists and residents examine brain scans and converse on next steps.
As well as an acute care hospital in Toronto’s downtown core, St. Michael’s Hospital is a research hub and academic teaching hospital fully affiliated with the University of Toronto. More than 5,000 learners and trainees advance their medical and health care careers at one of Unity Health’s three hospital sites each year.
“There has to be a lot of collaboration between first responders and hospital teams,” says Beckett. “For a patient to survive it has to be a finely tuned system.”



During a few minutes of down time, a general surgery resident, Dr. Noemie Elfassy, approaches Beckett with a theoretical question.
“Proximal subclavian arterial injury. What would you do?” she asks, her scrub cap decorated by rainbows and unicorns.
Beckett responds in equally impressive medical syntax. Subclavian arteries, found beneath the collarbones, move blood from the heart to the rest of the upper body. In penetrating traumas these arteries can be injured.
After a few minutes of spontaneous teaching, Beckett, Mok and the residents turn to look at brain scans on the computer screens. They decide the patient doesn’t need surgery and can be moved to the intensive care unit.
At St. Michael’s, trauma care doesn’t begin and end in the trauma bay or even in the operating room. Teams of researchers have dedicated their careers to examining how they can improve patient outcomes and the quality of care in the years to come.
Mok, who also serves as Deputy Chief of the Emergency Department, spearheaded a study that evaluates the quality of care CPR patients receive in the hospital when they are being resuscitated. Beckett, in partnership with the army, is researching the use of dried blood products to make transfusion easier and more accessible for civilians and soldiers.
Dr. Steve Lin, current Chief of the Emergency Department, is leading
a national study that examines the optimal dose of epinephrine to give patients during cardiac arrest. The study partners closely with paramedic services to ensure patients are getting the best treatment as early as possible.
Dr. Brodie Nolan and Dr. Johannes von Vopelius-Feldt, emergency and trauma physicians and scientists, are looking into the feasibility of creating critical care response teams that would meet patients at the site of injuries. New studies led by Dr. Nolan and Dr. Michelle Sholzberg, clinical hematologist at St. Michael’s, even incorporate artificial intelligence to support the treatment of head injuries and massive bleeding.
Unity Health is also home to a Simulation Program that allows clinicians to train using manikins in hyper-realistic scenarios, so that when real patients come through the emergency department doors they are ready for anything. Unity Health’s Simulation Program hosts more than 5,000 interprofessional health profession learners, hospital administrators and support staff every year. Even the layout of the trauma bay has been specifically designed based on research to ensure the team can function as efficiently as possible.
What sets St. Michael’s apart is this dedication to figuring out how to improve those first 60 minutes of care. The critical “golden hour” of trauma care as clinicians often call it.
Beckett often stays at the hospital all night during his on call shifts,
knowing from experience that anything can happen at any time.
Trauma can mean many things: violent injuries from gunshots and stabbings, closed head injuries from falls and car accidents, limb injuries and penetrating wounds. These patients are often brought to the hospital by ambulance or helicopter, and rather than being evaluated in the emergency department they are brought right to the specially equipped and designed trauma bays.
Trauma patients are often unconscious by the time they arrive at the hospital, and in many cases are sedated or intubated by the time they are brought to the operating room if surgery is required.
Trauma surgeons, as Beckett puts it, are like quarterbacks deciding on how patients’ care will roll out. Is a head injury more pressing than broken bones? Should a scan happen before sutures? Is the patient stable enough to make it upstairs to the operating room?
“No one is more important than anyone else,” Beckett says of the team. “I am one cog in the machine.”
Beckett says it can be strange to operate on people and be present for some of the most challenging times in their lives without ever having properly met them.
“I usually don’t get to meet them or know them until they’ve recovered and come back for follow up appointments,” he says.
Many patients are incredibly grateful when they do meet their surgeon, but as they physically recover, trauma patients are also grappling with the aftershocks of their experience.
The psychological toll of a traumatic experience can be massive, and Beckett has had to deliver hard news to families over the course of his career. Things like life-altering injuries, or – in the worst case scenario – news about a loved ones’ death. Social workers are present for trauma cases and help to answer family members’ and loved ones’ questions. A trauma clinic is also accessible upon referral for patients who don’t require admission to the hospital but need help through things like post-traumatic stress and concussion follow-up.
But on the other side of the coin are the many times he’s able to share good news. Patients who have – in no small part because of first responders, the trauma team and other specialties –pulled through harrowing ordeals and gone on to live full lives.
Without his experience as an army medic, Beckett likely wouldn’t have chosen trauma as a specialty.
War zones and downtown hospitals both have their unique challenges, but Beckett’s research and work have consistently proven that what happens on a battlefield can also apply to treating civilian populations.
If dried blood can help a soldier on the front lines, it could also be useful for a car crash patient who needs a transfusion right at the scene of the trauma. These are the kinds of ideas and innovations that will transform trauma care for Canadians.
With their patient in the capable hands of the St. Michael’s ICU team, Mok finishes up his long shift and gets ready to leave the hospital and Beckett returns to his office at around 7:30 p.m. to wait for other cases. ■ H
Peter Dangerfield never expected a job at Waypoint Centre for Mental Health Care would involve caring for the people who care for patients.
But making sure every employee feels supported and fulfilled is a vital objective at the Penetanguishene-based hospital and, when it comes to prioritizing staff wellness, people like Dangerfield play a key role. He is a therapist in the Frontline Wellness program, a free, confidential service to help support the mental health of health care workers. His job is to help those delivering mental health and addiction care deal with their occupational stress through counselling.
“I see nurses, doctors, support staff, managers – whoever needs it,” he said. “It says a lot about the organization that there are so many programs that support the workers.”
Waypoint is a 315-bed academic and teaching hospital that provides specialized mental health, addiction and geriatric care. It serves some of the most complex and disadvantaged individuals in Ontario, and is the sole provider of high-secure forensic mental health services in the province.
Caring for the emotional and psychological well-being of staff is deeply important to Waypoint, as is sharing expertise for the broader benefit of the health care workforce. Waypoint provides leadership to guide organizational health and well-being for all central Ontario hospitals, and is growing capacity in the system by using a collaborative approach to maturing wellness programs.
This includes adopting a Stepped Care Model – developed as a digital tool – to enable health care workers accessing the right level of care to support resilience and mental health. More than 300 leaders in hospitals and community support services in central
Ontario have participated in training to learn how to use the tool.
Another component of caring for staff is the Traumatic Incident Support Team (TIST), a peer-led initiative that provides around-the-clock support to Waypoint staff and patients. Dangerfield currently co-leads the team, whose members come when called – including after hours, in the middle of the night, on holidays or on weekends. It is a voluntary service of skilled and concerned Waypoint employees with advanced training in critical incident stress management and psychological first aid.
“Things happen at work that are sometimes unsettling or unnerving, and we’re there to help them normalize or rationalize what’s occurred,” he explained.
Dangerfield started at Waypoint six years ago in the Forensic Secu-

Peter Dangerfield is a therapist in the Frontline Wellness Program, a free confidential service to help support the mental health of health care workers.
rity Office, working part time as an operational support worker. While working toward a bachelor’s degree in social work, he landed a six-month placement on the Forensic Assessment Program (FAP), which provides comprehensive, multi-disciplinary assessments for each patient admitted from the courts, provincial and federal correctional facilities, and provincial regional psychiatric hospitals. He was later hired as a social worker on the Beausoleil Program, where staff focus on meeting the long-term needs
of patients with a major mental illness and personality disorder diagnoses. He spent a year there before returning to FAP full time, and a few years later moved to his current position in Frontline Wellness.
“Helping people improve their lives is very fulfilling,” he said. “It’s really nice when people sit before you with their challenges or with things they can’t make sense of, and then in a few weeks they’re feeling more confident and their challenges don’t seem as heavy. That’s quite gratifying.” ■ H
Scarborough Health Network (SHN) opened the doors to its new Community Mental Health Centre in June, bringing together ambulatory and community outpatient mental health services that were previously offered at multiple SHN hospitals and satellite sites into a single location, for the first time.
One of SHN’s Build It Forward capital projects, the Community Mental Health Centre was made possible entirely thanks to donors, who collectively donated $6 million to SHN Foundation’s Love, Scarborough campaign. The 15,000-square-foot space gives patients access to the RBC Youth Mental Well-Being Clinic, the Bell Seniors’ Mental Health Clinic, the
Slaight Family Foundation Cultural Psychiatry Clinic, and the Ray Gupta and Family Mood & Anxiety Clinic.
In the heart of Scarborough’s Golden Mile district at 1940 Eglinton Ave. E., this highly accessible and inclusive setting features a comforting and spacious waiting area, individual treatment and counselling areas, quiet rooms, collaboration and group spaces, psychiatrist offices, and a pharmacy for client prescriptions. It is designed to achieve:
• A “no wrong door” approach to care. This innovative model connects people to the right treatments based on their condition. This means more intensive services will be available to those who need them.
• Timely access to care. No one should have to wait for mental health care.
The centre ensures patients who require urgent care will be contacted within 14 days after receiving a referral, which significantly improves average wait times for access to mental health services.
• Less stigma. By having a beautiful, service-oriented outpatient mental health space with a street-front presence, SHN is making receiving mental health care less intimidating, and reducing the stigma people may experience when seeking treatment. SHN’s Community Mental Health Centre marks a transformation of mental health care for the Scarborough community and beyond, enabling better integrated and more streamlined access to exceptional quality care. ■ H
Astudy led by Dr. Akber Mithani, Regional Medical Director, Janice Sorensen, Research Lead and their research team examined how long-term care homes can benefit from a virtual quality improvement collaborative approach to pandemic preparedness.
Team-building and face-to-face meetings were limited during the COVID-19 pandemic. However, the long-term care team was committed to implementing evidence-based practices and sharing their learnings across long-term care homes.
“We were working with challenging circumstances when we were developing this study in the fall of 2020,” says Janice Sorensen, research lead, Long-Term Care and Assisted Living. “We thought, let’s do it virtually.”
Multidisciplinary quality improvement teams were created with dedicated people, including nurses, physicians, residents and family partners. The teams collaborated via online communication and collaboration platforms, Zoom and Slack.
Quality Improvement Coaches, Dr. Adriaan Windt and Angela Tecson, guided the teams through weekly virtual huddles. Using adapted quality improvement tools, the coaches helped the teams transform their 46 change ideas into 16 quality improvement projects for prevention, preparation and response to COVID-19 outbreaks in long-term care homes. The projects also addressed staff recognition and family visitation concerns.
“Kudos to our coaches who developed some long-term care adaptive quality improvement tools to be at a

very attainable level,” says Janice. “Everyone involved, whether resident or staff member, was on the same page to walk that quality improvement journey together.”
The virtual quality improvement collaborative approach worked well, with all but one of the projects completed within the study period.
The study found that quality improvement infrastructure and virtual supports can help conduct timely projects to improve pandemic response in long-term care homes during emergencies when in-person communication is not possible.
Crucial takeaways from the study are that flexibility and customizing approaches for each long-term care home are essential with consideration for staff time availability and capacity. Also, multidisciplinary teams, includ-
ing family members or residents, provide valuable and diverse perspectives to inform projects.
“As we reflect on the challenges during the pandemic and the outcomes of our study, it’s evident that investing in quality improvement initiatives is paramount,” says Janice.
The study was part of the ‘Implementation Science Teams – Strengthening Pandemic Preparedness in Long-Term Care’ programme led by Healthcare Excellence Canada, co-funded by Michael Smith Health Research BC and the BC Ministry of Health and supported by Health Quality BC.
Although the study was limited to six long-term care homes, the adaptive quality improvement tools and lessons learned have informed ongoing quality improvement initiatives in long-term care homes across the Fraser Health region. ■ H

One of the most persistent barriers to better integrating care for patients is access to data, especially in a system that has traditionally operated in siloes. Integrated Decision Support (IDS) was developed to address these data “blind spots” through its data sharing platform and is now empowering a host of connected subscribers including hospitals, home and community care, primary care, community health centres, community mental health, and paramedic services. Today, IDS is Ontario’s most mature and widely used collaborative solution for sharing integrated health partner data.
Through its platform, IDS offers data at a patient level across a continuum of health care services giving subscribers a line of sight into the patient journey, even when they cross regional boundaries. IDS links patient data for over 100 health care organizations, covering 9.8 million unique patients and over 180 million patient encounters. IDS also integrates province-wide Statistics Canada Population Census information and the Ontario Marginalization Index, allowing population health equity questions to be married with health care data utilization in a population health management approach right to the patient level. These data are used for system planning, performance management and efficiencies, analytics, reporting, integrated care planning, outcome measurement and evaluation – all focused on improving quality of care for Ontarians.
Guided by the principle of “oncefor-many”, IDS is a provider-driven, collaborative community that simplifies data integration and common analytical challenges, supported by customer-focused training, education
BY PUTTING ANALYTICAL POWER IN THE HANDS OF ITS SUBSCRIBER COMMUNITY, INTEGRATED DECISION SUPPORT (IDS) IS EMPOWERING A HOST OF CONNECTED SUBSCRIBERS, INCLUDING HOSPITALS, HOME AND COMMUNITY CARE, PRIMARY CARE, COMMUNITY HEALTH CENTRES, COMMUNITY MENTAL HEALTH, AND PARAMEDIC SERVICES, TO DELIVER BETTER INTEGRATED PATIENT CARE. TODAY, IDS IS ONTARIO’S MOST MATURE AND WIDELY USED COLLABORATIVE SOLUTION FOR SHARING INTEGRATED HEALTH PARTNER DATA.
and knowledge transfer. Harnessing data from a well-organized repository and set of tools, such as pre-built reports and dashboards, IDS helps save time for busy analysts and enables standardization and comparability of initiatives and indicators amongst subscribers. Paired with IDS’s powerful Tableau analytics platform, these reporting templates – developed in response to requests from the subscriber community – provide validated, readymade reports that can be tailored to meet local needs. IDS supports care delivery organizations with a view into their shared patients and the ability to cohort and segment populations by patient condition, patient geography, age, cost, and many more factors.
For example, IDS recently released two new Stroke Distinction Tableau reports which provide subscribers participating in the Accreditation Canada program convenient, easy access to their organization’s stroke distinction key quality indicator results in just one click. The reports provide results for 13 stroke quality indicators for specific organizations and enable benchmarking with peers across 9 indicators. Quarterly and annual indicator results are readily available making monitoring and submission to Accreditation Canada effortless, and built-in flexibility allows IDS analysts to save cus-
tomized versions of these reports for their organization.
Subscribers benefit from several features and services that set IDS apart, including timely access to data, and most notably, its unique ability to support local integration activities such as Ontario Health Teams (OHTs), bundled care, and Integrated Care Programs. Consultations with 37 OHTs in 2023 have resulted in new geographical-based catchments that equip IDS subscribers with the ability to easily select practical cohorts to support timely OHT-related analytics and planning efforts. Now live on the platform, these OHT Catchments complement the Ontario Health OHT Attributed Population, allowing IDS subscribers to drill into patient-level details to discover drivers and patterns of health care utilization, and much more. IDS continues to add to its OHT reporting catalogue, which now includes hospital metrics for OHT Catchments, palliative care cohort monitoring, and frail seniors’ care transitions. Subscribers also benefit from more granular collaborative Quality Improvement Plan (cQIP) measures that help evaluate the success of OHT initiatives. Groundbreaking work with the Guelph Wellington OHT is a great
example of IDS in action. Leveraging IDS to share data across providers is now enabling the OHT to segment their population by complexity of needs which, in turn, is helping inform the development of care plans tailored to patients’ specific requirements across a range of providers. This has led to better care coordination and optimal use of the OHT’s available resources. Additionally, by incorporating the Hospital-Patient One-Year Mortality Risk (HOMR) tool into IDS, the OHT can now use IDS’s integrated data to identify patients who would benefit from a palliative approach to care. This allows the care team to proactively initiate an integrated care plan that includes all aspects of palliative care, including advanced care planning, serious illness and symptom management conversations, etc. Benefits are two-fold: for providers, informing them which individuals may benefit from wrap-around care, and at the system level, allowing the OHT to predict required palliative care capacity across the Guelph Wellington population and plan accordingly. The HOMR score is now available to the IDS network of subscribers via IDS’s once-for-many approach.
Through active listening, IDS will continue to expand its offering with new datasets, tools and insights of the greatest interest to its user community. For example, currently in the pilot stage are integrations with community support services and hospital ambulatory clinics – both non-traditional datasets – as well as long-term care. As more organizations join the IDS network, ever-richer data is being made available to improve health service delivery across the province. By putting analytical power in the hands of its subscriber community, IDS is working to support a vision of an integrated and patient-focused system of care. Learn more about how IDS can support your organization, or reach out directly to Wendy Gerrie, Director, IDS, at wgerrie@oha.com. n H
By Shahana Gaur
Humber River Health (Humber) has embarked on an ambitious and transformative journey to enhance its ambulatory care services, with a clear focus on meeting the needs of the North West Toronto community. This community, which has higher disease prevalence compared to surrounding regions, deserves equitable, quality care right where they live. Humber’s 2023-2026 Ambulatory Strategic Plan is designed to strengthen local partnerships, deliver cutting-edge outpatient medical care and extend patient care by collaborating with community health partners. This plan reflects Humber’s commitment to delivering comprehensive quality care closer to home and enhancing patient experiences and outcomes.
This Ambulatory Strategic Plan emerged primarily from extensive community engagement that was conducted during the development of Humber’s corporate strategic plan. “This is Humber’s first ambulatory strategy,” explains Carol Hatcher, Executive Vice President, Chief Nursing Executive, and Chief of Clinical Programs. “Community engagement sessions highlighted an opportunity to review and optimize Humber’s current bundle of ambulatory services to ensure they meet the needs of our community.”
Research conducted to gauge the opinions of Toronto residents in the Humber River Health catchment area revealed key insights, including their awareness of services offered at Humber. Notably, residents were most aware of Humber’s Apotex Emergency Department (ED), compared to other services and programs offered, with close to six in ten reporting awareness. This data aligns with the reality that Humber’s ED is the busiest in the province, hosting almost twice as many ambulances as neighbouring hospitals.
Ambulatory care encompasses a wide range of care offered in an out-
patient setting, including diagnosis, observation, consultation, treatment, rehabilitation and minor procedural services. The focus is broad, from investigations and treatments to preventative care. “Our intention is provide a comprehensive care pathway for patients that may require pre and post-acute care, supporting the whole patient journey,” says Carol.
A collaborative effort began to develop Humber’s ambulatory strategy in September 2023, involving tailored internal and external stakeholder interviews, research on leading global and national ambulatory care systems, and working sessions with Humber leadership, patients, community partners, staff, and physicians. The planning process included extensive environmental scans, state assessments, and community engagement to ensure a well-rounded and effective strategy. Environmental scans researched innovative approaches to ambulatory care by local and international peers to identify best practices and opportunities for Humber. State assessments analyzed Humber’s cross-ambulatory programs to better understand growth, utilization, virtual adoption, and resource allocation. Facilitated community engagement sessions gathered input from residents on their top healthcare concerns and needs for integrated care.
The development of this strategy aimed to refine and align ambulatory-specific strategic goals, directions, objectives, and outcomes, and is crucial in identifying gaps in services and exploring opportunities to better meet community needs. “It was clear from our initial analysis that there was an opportunity to re-imagine what our ambulatory services look like at Humber,” says Carol. “This strategy is very much centered around community need.”


The culmination of these efforts will be a robust three-year ambulatory strategic plan with a strategic decision framework, set to drive Humber’s decision-making processes across various ambulatory initiatives.
Key strategic objectives underpinning this plan include developing community partnerships to deliver local, patient-centered care, leveraging Humber’s three major locations to enhance equity and accessibility of ambulatory services, and improving care delivery so patients feel at the centre of their healthcare journey. Additionally, Humber is committed to delivering equitable care, prioritizing innovation not just within the hospital but also at community outpatient sites, and ensuring staff coordination across all locations.
This strategic approach underscores the importance of accessibility, effi-
ciency, patient experience, equity, and value in healthcare delivery. Humber’s focus on providing care close to home will improve patient outcomes and experiences. Empowering patients to become partners with their healthcare team, ensuring equitable access to care, and making the most of available resources are central to Humber’s mission.
Humber River Health’s new ambulatory care strategy is a testament to its dedication to lighting new ways in healthcare. Through comprehensive planning, community partnerships, and a relentless focus on patient-centered care, Humber is poised to transform ambulatory care in North West Toronto, delivering high-quality, equitable healthcare that meets the diverse needs of its community. “Our goal is to provide comprehensive, quality care closer to home and ensure our community receives the best possible healthcare,” says Carol. ■ H
veryone living in Canada desires and deserves a healthy life. We collectively imagine a future where children, youth, and their families thrive, have access to a livable income, safe housing, and clean water; enjoy food security; and feel a sense of belonging. Living well also depends on access to equitable, evidence-informed, high-quality healthcare services, which, these days, is a luxury many Canadians do not enjoy. Mounting evidence shows that children now wait longer than adults for essential healthcare services, a reality that paints a bleak picture for their –and our – future.
Recent research commissioned by Children’s Healthcare Canada demonstrates that delays in access to care come with costs – both human and financial. For example, the Conference Board of Canada estimates the annual costs to treat anxiety and depression amongst children and youth to be $4 billion (CDN); a figure that balloons to nearly one trillion dollars over a lifetime without timely access to interventions. While waiting for community-based mental health services, hospital-based surgical and diagnostic interventions, or children’s development services, many children experience physical or emotional pain, they may fall behind in school, miss social development milestones and, often, their conditions worsen, in some cases, irreversibly. As parents, caregivers, and guardians, we can no longer ignore the mounting evidence of profound impacts of inaction.
To inspire and ensure healthy futures for children and youth, Children’s Healthcare Canada, along with our member organizations and partners, embarked on a quest to define a vision for “right-sized” children’s healthcare systems and the path to realize that vision. Through seven virtual roundtables and two in-person consultations, we convened over 600 champions for children (families,

Emily Gruenwoldt, CEO and President, Children’s Healthcare Canada

healthcare providers, researchers, social service providers, and others) to contribute lived- and living experience and expertise to inform and guide the development of recommendations targeting provincial/territorial and federal governments, but also healthcare delivery organizations, and advocacy organizations like Children’s Healthcare Canada. These recommendations were issued in a report released earlier this spring called Beyond Bandaids: Delivering a Future Fit for Kids.
Collectively, Children’s Healthcare Canada and its members imagine a future where right-sized children’s healthcare systems are accessible, equitable, connected, and purpose-built to meet the needs of children, youth, and their families, and the highly specialized workforce that serves them. To achieve this vision, there was broad agreement on the necessary conditions for children’s healthcare systems transformation:
Emily Gruenwoldt, CEO and President, Children’s Healthcare Canada.
• Dedicated and protected funding envelopes for children’s healthcare systems across the continuum of care, including child health research;
•Publicly accessible child health data captured under national health data strategies;
•The highly specialized health workforce that cares for children and youth must be an intentional focus of national health workforce planning initiatives.
The Association, along with our members and partners, are calling on the federal government to take a leadership role, declaring children’s health and well-being a national priority, launching a National Children’s Strategy, and creating a Chief Children’s Health Officer to ensure progress towards specific goals.
As a result of the work led by Children’s Healthcare Canada, there is visibility and momentum for change. This May, the House of Commons Standing
Committee on Health (HESA) released findings of their 2022-23 study on child health, Fostering Healthy Childhoods: A Foundation for Resilient Generations. Many child health leaders testified in front of the committee, and as a result there is alignment between the recommendations of the HESA report and those issued in the “Beyond Bandaids” report.
The HESA committee recommends, amongst other things, that the government establish an office tasked with accountability for child and youth health, implement a national pediatric data and workforce strategy, and increase mental health funding for children and youth. These recommendations, in conjunction with other child-centred policies and structures (improving access to high-quality childcare, improving parental leave benefits, incorporating child impact assessments, and increasing the Canada Child Benefit for example) will put children on a path to thrive.
There is reason to be hopeful. At the same time, it will take continued collaboration across sectors and partnerships with governments of all levels, guided by the lived experience of youth and families to effect change.
Our Association is on a mission to measurably improve the health of children. To join us and shape a vibrant future for kids in Canada, consider participating in conversations taking place in St. John’s, Newfoundland and Labrador, October 20-22, 2024, during our annual conference, or through any number of dynamic networks our Association hosts, convening child health leaders across the continuum of care. For more information on these opportunities, please visit our website www.childhealthcan.ca
Together, we are making progress. Together, we are one step closer to right-sized healthcare systems that ensure Canada is home to vibrant, healthy children and youth now and into the future. ■ H












Kairo, who was prone to self-injurious and eloping behaviours, can now go to the park with his mom and had his first visit with the dentist ever in his life at the age of five. ‘Jennifer,’ who had a significant needle phobia that put her health at risk, can now tolerate having her bloodwork done. Matthew faces many developmental complexities such as autism, ADHD and anxiety, but now is feeling more confident in himself and is thriving.
These children are just three of more than 1,200 children and their families who have been receiving individualized and vital wrap-around supports through a unique program run by three children’s hospitals in Ontario: CHEO, Holland Bloorview Kids Rehabilitation Hospital and McMaster Children’s Hospital.
“The families we’re caring for would otherwise slip through the cracks; they have complex needs and the system wasn’t built for them. Extensive Needs is changing that,” says Taylor Johansen, director of neurodevelopmental health at CHEO. “This first-of-its kind treatment is as precise and unique as each child it serves. These families have been through a lot and they deserve to access care that is designed with and for them.”
Launched in April 2023 and co-funded by the Ministry of Health and Ministry of Children, Community and Social Services, the Extensive Needs Service (ENS) proof-of-concept program – the first of its kind in Canada – is a service that works with children, youth and their families to provide individualized care that addresses their unique and complex health care needs, including developmental, behavioural, and mental health. It is designed to reduce barriers that families can face navigating a complex healthcare system, and provides access to timely, evidence-based and trauma-informed treatment for some of the most vulnerable children in Ontario.
Upon intake, families are connected to an interdisciplinary care team to collaborate and develop personalized

Kairo, a client who is currently receiving services through the Extensive Needs Service at Holland Bloorview, is one of over 1,200 children with urgent and complex needs who are being supported with wrap-around care through this unique program funded by the Ministry of Health and Ministry of Children, Community and Social Services.
treatment plans aimed at improving a child’s abilities, mitigating challenging behaviours and addressing underlying health issues. The overall goal of the unique program is to augment existing services available as well as work with the child and their family to learn skills needed to support them in their home, school and community.
Each of the three hospitals tailor the program to meet the families’ needs. For instance, McMaster Children’s Hospital’s ENS program offers Family Check-Up, a strengths-based and collaborative service for the family members of the child or youth in the ENS program to support their physical and mental well-being.
“The clinician and parent work together to identify areas of strength for the family, and help the family identify
what they need and set goals,” says Dr. Rebecca Shine, a clinical psychologist at McMaster Children’s Hospital.
“There would have been a time where I thought that my son wouldn’t still be in my house at this point. It was very volatile at the beginning, and I think we’ve grown together. It has strengthened our bond. I feel like I’m closer to him,” said Matthew’s mother, Christine. “The Extensive Needs Service has transformed our lives.” In just over a year, Extensive Needs Service has had immeasurable impacts on the families served so far, expanded a community of practice, created new models of wrap-around care, and created the opportunity for underserved populations with complex needs to access extensive care in a streamlined manner.
Across the three lead hospitals, the program has demonstrated significant impacts, including:
• Reduced hospital stays for clients receiving services through the Extensive Needs Service program by over 90 per cent;
• Reduced emergency room visits by 80 per cent; and
• Reduced average missed school days by 90 per cent.
• Families in the program also have reported their level of stress has fallen by nearly 40 per cent.
Moreover, the program has expanded its community partnerships across southern Ontario to give families easier access. At Holland Bloorview, this includes local community partners including the Children’s Treatment Network, Michael Garron Hospital, and Grandview Kids. Surrey Place provides dedicated service coordinators who work closely with families to access the Extensive Needs Service program at Holland Bloorview as well as providing expert support to navigate the health and social service sector for families with complex and urgent needs. McMaster Children’s Hospital has established a growing network of expert community partners across the Hamilton, Niagara, Haldimand-Norfolk and surrounding regions to ensure families have more access to the services they need closer to home.
Looking to the future, plans are afoot to expand the program provincially, particularly in northern Ontario and remote regions, and even across the country.
For Kairo’s mom, Nikki Pacheco, the extensive needs service program at Holland Bloorview has been transformative for their family.
Diagnosed with autism at the age of two, Kairo, now five, is a happy, energetic child with a big imagination. Since receiving services through ENS in January 2024, he is more social and feels more at ease with transitions.
“I’m so thankful for the team’s efforts to see my child just be a child. I now have hope and truly have found a place that just understands.” ■ H
Like most babies, Nathan Bonner had his tiny foot pricked to collect a drop of blood when he was just a day old, as part of routine newborn screening. The test came back with a screen positive result for a metabolic disorder called phenylketonuria (PKU). Nathan was referred to Hamilton Health Sciences’ McMaster Children’s Hospital (MCH), one of five hospitals in Ontario with a newborn screening program, for follow-up care.
A genetic counsellor shared the screening results when he was just six days old. That same afternoon, the family went to MCH’s Genetics & Metabolics Clinic for further testing and confirming diagnosis.
With PKU, Nathan’s body is unable to break down an amino acid called phenylalanine. Without immediate discovery and treatment, infants can develop rashes, seizures and permanent brain damage. With early diagnosis and treatment, babies with PKU have normal development like their peers.
“We were in shock, but we felt like we were in good hands from day one,” says Nathan’s mom Stephanie.
The main treatment for PKU is a very restricted diet that Nathan will have to continue for the rest of his life to prevent brain damage from built-up phenylalanine.
“Treatment involves eliminating all high protein foods, tracking protein intake daily, and including specialized metabolic formula to support normal growth and development,” says registered dietitian in the Genetics & Metabolics clinic, Amy Pender.
“Patients like Nathan complete weekly blood work to monitor and adjust the diet to ensure that levels are in a safe range to prevent serious health issues.”
With PKU, Nathan can’t eat regular sources of protein, including bread, pasta and rice. Instead, phenylalanine-free PKU formula will be a life-
The Bonner Family

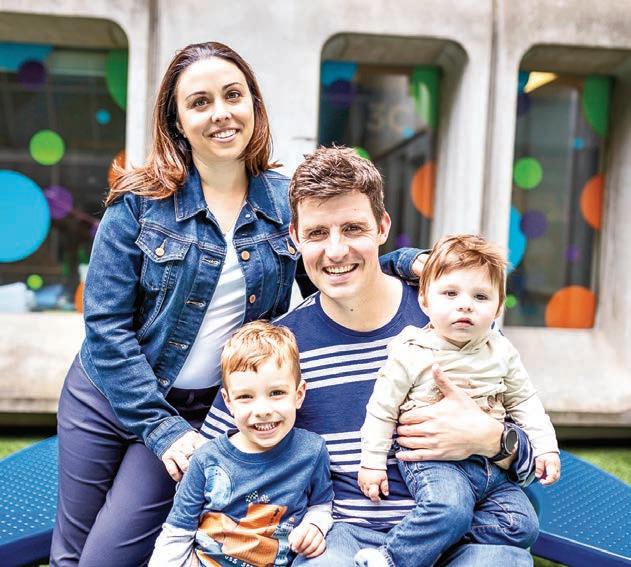
SINCE THE LAUNCH OF MCH’S NEWBORN SCREENING PROGRAM IN 2006, THE NUMBER OF CONDITIONS SCREENED FOR HAS GROWN SIGNIFICANTLY FROM TWO TO AROUND 30.
long part of Nathan’s diet to meet his protein needs.
Mealtimes involve a ton of planning. Nathan’s food gets weighed before every meal and any food left behind, so his parents can keep track of exactly what he’s consuming.
The team at MCH help his parents understand options through education and monitoring.
Since the launch of MCH’s newborn screening program in 2006, the number of conditions screened for has grown significantly from two to around 30. The number of infants referred to MCH with positive results has also grown. MCH now provides follow-up care to about 150 babies with positive
results annually, out of 25,000 babies born within the region each year.
Less than one per cent of babies receive a positive newborn screening result. Each of these kids can have different conditions. When they receive a patient referral, staff work with doctors from the appropriate hospital clinics, such as metabolics, respirology, endocrinology, hematology or immunology, depending on what condition the baby was diagnosed with.
Thanks to government funding, MCH’s has added a nurse, dietetic assistant, genetics assistant, and social worker to this team. This additional support means infants receive timelier follow-up for diagnostic testing, and earlier treatment for those who go on to have a diagnosis confirmed.
Allison Pottinger is the new dietetic assistant, helping over 250 patients
with different life-saving metabolic diets requiring close management.
Pottinger’s role includes ordering specialized metabolic formulas and foods; communicating information to patients; requesting and calculating a patient’s food record so the team has accurate data to adjust care plans as needed; and sharing resources with families about specialized diets.
Registered nurse Rebecca Carpenter also joined the clinic. She facilitates diagnostic testing for newborns; cares for patients during their appointments and manages treatment plans; educates families about metabolic disorders; and provides emotional support.
Patient advocacy is also a huge part of Rebecca’s role, including applying for funding, facilitating referrals, and working with schools and workplaces to accommodate a patient’s needs. This involves working with other health care professionals, advocating for policy changes, and empowering families to become advocates for themselves.
“We worry about when he goes to school and the social aspects of growing up,” says Ashley.
To the health-care team, the small joys are important. Pottinger has been working on a list of low protein foods available in local grocery stores and food options that can be used for special occasions, like pizza day, while fitting within the PKU diet for children like Nathan.
While PKU is a lifelong condition, there is a medication treatment that may or may not work when used in conjunction with the PKU diet.
“We hope to trial this treatment with Nathan in the coming months,” says Pender.
Stephanie and Ashley’s main goal is for Nathan to feel comfortable and confident.
“We hope he has the confidence to feel like himself,” says Ashley. “The fact that there’s investment in this area and that we have support is just awesome. We’re just so thankful for that.”
the “genetic landscape” of aggressive and deadly
osterior fossa group A (PFA) ependymoma are rare, treatment-resistant pediatric tumours of the central nervous system that originate in the brain and spinal cord. They have the highest recurrence rate and poorest prognosis of all childhood cancers, due to the lack of effective treatment.
Hope is on the horizon now that an international research team led by scientists at Baylor College of Medicine in Texas, USA, and the Research Institute of the McGill University Health Centre (RI-MUHC) in Montreal, Canada, have identified unique 3-dimensional features called TULIPs in the genome of PFA ependymoma that could eventually be targeted in the development of more effective therapies. The findings appear in Cell.
“PFA ependymomas are lethal. One of the reasons behind the little progress toward the development of effective treatments for these tumours is that the majority of PFAs lack clear genetic mutations driving tumour growth. Without a clear genetic target against which we could design specific therapies, we investigated another aspect of the tumour, how the DNA is packed inside the nucleus of the cell,” says senior and lead author, Marco Gallo, Associate Professor of pediatrics, hematology-oncology at Baylor and Texas Children’s Hospital.
“Our work was driven by a simple fact: PFA ependymoma are usually diagnosed in very young children, and
have no efficient treatment. Radiation therapy, the only treatment currently available, is not effective and causes serious developmental and cognitive issues. That’s a reality we hope to change,” says Canada Research Chair in Pediatric Oncology Dr. Nada Jabado, co-senior author of the study, Senior Scientist in the Child Health and Human Development Program at the RI-MUHC and a pediatric hemato-oncologist at the Montreal Children’s Hospital of the MUHC.
Every cell in the body has about 6.6 feet (2 meters) of linear DNA that is stored in its nucleus in a manner that enables the cell to easily access the genes it uses most often and set aside those less used. This would be like organizing the closet with the clothes most frequently used at the front and those rarely worn on the back. To fit in the tiny nucleus, the long DNA molecules are folded, twisted, looped, which results in specific 3D conformations, some tighter, some more relaxed, that can ultimately help the cell express the genes needed to do its job.
In this study, the researchers looked closely at what we might call the “geography” of the PFA ependymoma cell genome (the entire set of DNA instructions found in the cell).
“We investigated the unique ways PFAs cells organize their DNA in 3D, by orchestrating strong interactions

between regions of the genome that are normally very far apart. We discovered specific regions that are not present in other types of pediatric brain cancer and that recur at predictable genomic locations. We named them TULIPs, for Type B Ultra-Long Interactions in PFAs,” says Dr. Michael D Taylor, co-senior author of the study and Professor of pediatrics, hematology – oncology and neurosurgery at Baylor and Texas Children’s. He also is the Cyvia and Melvyn Wolff Chair of Pediatric Neuro-Oncology at Texas Children’s Cancer and Hematology Center.
The researchers used the Hi-C technology to profile the 3D architectures of the entire genomes of PFA tumours and compared them with those of a large cohort of samples from different tumour types and nonmalignant tissues. In the process, TULIPs appeared as specific regions of very tightly compacted, thus hard-to-access, DNA, a sign that the cell may not use the genes in that region often.
“TULIPs also tend to interact with each other over very long distances. A TULIP might be at the end of a chromosome and another TULIP at the other end of the same chromosome, and they find their way to interact with each other with surprising strength,” explains Prof. Gallo. “TULIPs on different chromosomes can also converge and strongly interact with each other.
We also found that regions outside TULIPs appear more relaxed overall. This is important because TULIPs are linked to the cell’s function.”
According to the study findings, TULIPs carry a methyl group on histone H3K9, a protein associated with DNA that can act as a chemical tag. Indeed, when the research team inhibited the tagging of H3K9 in PFA patient-derived cultures, they witnessed weaker interactions between TULIPs and impaired PFA cell survival. These observations suggest that TULIP interactions are important for PFA cell viability, opening up new potential targets for treatment.
“We believe that TULIPs are ephemeral structures present at an early stage of cancer development in progenitor cells – cells that descend from stem cells and precede the creation of mature cells, very early in life. However, more research is needed to understand the mechanism by which TULIPs arise and mediate cancer cells behaviour,” says Dr. Jabado, who is also a professor in the Department of Pediatrics at McGill University. “By further investigating this mechanism, we may be able to explore treatment strategies to remove them to promote tumour elimination.” ■ H
Every child develops differently. Many meet their developmental milestones; some don’t. A 2015 Ontario report found one in nine kids has a disability or developmental need; it’s one in eight if you follow the latest US Centre for Disease Control data.
Ontario’s robust network of highly specialized organizations staffed by Regulated Health and other professionals provides pediatric expertise when families have concerns about their child’s development--care they cannot get anywhere else, all under one roof in communities across the province. Each team is part of the continuum of healthcare together with community pediatricians and pediatric hospitals.
More than 200,000 Ontario kids and youth are supported by this network of community-based pediatric healthcare partners.
When kids miss out on critical support, their needs tend to become more


complex, requiring more treatment over a longer period, or are never resolved. The longer term can be harder academically, behaviourally, socially, and developmentally.
The good news is treatment in a timely way is often the least costly and gives the greatest impact. Pediatric surgeries for example, need to align with developmental milestones

or occur early enough in a child’s life to prevent complications and optimize outcomes. If a child with mobility challenges can get physiotherapy as a toddler, they could become more mobile and have increased independence by the time they’re old enough to go to school.
Many challenges that kids face can be managed – and managing them
early in a child’s development is key to managing them successfully.
Sooner is always better.
We know there are windows of opportunity that can change the trajectory of a child’s life. Setting a child up for success is not just about addressing immediate concerns, it’s about laying a strong foundation for their future well-being.
There’s an economic return too, that has to do not just with impacting the cost to raise a child with disabilities, which studies find is four times the cost to raise and educate a child without disabilities.
There is a better chance that kids who receive early intervention will be productive and integrated adults in society. Just two years ago, the employment rate for those with disabilities was 65 per cent compared to 80 per cent for those without disabilities.
A child’s developmental health has a direct impact on their health and well-being throughout life. H

Early intervention can change the trajectory of a child’s life. Our members—communitybased pediatric partners with based pediatric expertise in developmental developmental health—know that setting a child up for success is not only child up only about addressing immediate concerns, it’s about laying a strong foundation for their future well-being.


he Canadian Association of Pediatric Nurses (CAPN) is a national network of nurses passionate about children’s health and the Pediatric nursing specialty. Our mission is to protect and promote the health and well-being of Canadian children, by advancing Pediatric nursing through education, learning, and advocacy.
Recognising the growing complexity of health care needs of Canadian children and their families, CAPN published the Canadian Pediatric Nursing Standards in 2017 after extensive meetings with Pediatric nursing leaders across the country, literature reviews, and in-depth surveys. CAPN revised these standards in 2022, to ensure they reflect current Pediatric clinical practice. The standards identify five unique domains of Pediatric nursing practice. Each standard contains a clear description, Pediatric elements of care which should always be met, and competencies required to achieve that standard. A story is included with each standard which highlights its principles, to assist nurses to incorporate the standard into their care. This article, summarising the revised Canadian Pediatric Nursing Standards, contains only the standard, its description, as well as the associated Always Events®. Please refer to the full document on the CAPN website (www.paednurse.ca) to view each standard’s competencies and story.
child/youth and/or family as partners
• Recognises and fosters the parent/ caregiver role
• Respects child and youth definitions of family
Delivering developmentally appropriate care
Pediatric nurses perform assessment based on growth and development and deliver appropriate care.
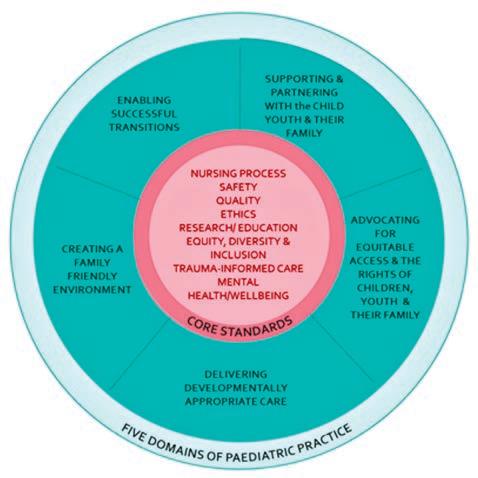
Advocating for equitable access and the rights of children, youth and their family
Pediatric nurses demonstrate their understanding of social determinants and other systemic factors that impact health. They comprehensively assess needs/risks, take action to support navigation of the system, empower self-advocacy, and provide mentorship and coaching that improves health outcomes for children and families.
The Pediatric Nurse always:
Supporting and partnering with the child, youth and their family
Pediatric nurses partner with the child, youth and their family engaging and empowering them to achieve optimal health and well-being leading to resilient families and healthy communities.
The Pediatric Nurse always:
• Establishes equitable and inclusive therapeutic relationships
• Respects and supports goal setting, decision making and consent
• Collects and uses contextual information to inform care with both
• Completes a comprehensive assessment considering social determinants of health and child and youth well-being
• Facilitates an appropriate environment to perform assessment and intervention, considering privacy and confidentiality
• Builds capacity in the child/youth and their family to self-advocate
• Maintains current knowledge of resources by engaging in Pediatric communities of practice
• Supports navigation of the healthcare system
The Pediatric Nurse always:
• Identifies and uses appropriate pronouns
• Demonstrates knowledge of typical development and variations
• Demonstrates knowledge of safety risks and performs safety assessments appropriate for developmental stage
• Uses validated screening tools to identify high risk activities or behaviours
• Provides anticipatory guidance on typical development and safety related to developmental stage
• Incorporates developmentally appropriate play and recreational activities into care
• Performs age and developmentally appropriate biopsychosocial assessments
• Uses developmental strategies when preparing for and performing interventions
• Understands that development may be influenced by factors such as gender, ethnicity, spirituality, and culture
• Creates a culturally safe environment
Creating a family friendly environment
Pediatric nurses play an essential role in creating family friendly environments that are welcoming and facilitate the health and wellness journey. They understand the environment changes as the child/youth grows and may be influenced by psychological, spiritual, social and cultural factors.
The Pediatric Nurse always:
• Establishes inclusive communication strategies that meet needs
• Completes a child/youth and family assessment
• Demonstrates cultural competency and humility
• Engages in a respectful, non-judgmental, culturally safe manner
• Recognises and fosters strengths and supports, despite boundaries and limitations

• Uses strategies to support and foster resiliency
• Demonstrates caring and compassion
• Fosters and promotes safe/brave spaces
Enabling successful transitions
Pediatric nurses support the child/ youth and family through health care transitions to maximise their well-being. This may include, but is not limited to: hand-off between providers, admission/discharge, and facility transfer or transition.
The Pediatric Nurse always:
• Uses effective communication strategies
• Assesses readiness and supports safe transitions
• Engages in planning of health education and coaching prior to each transition
• Involves the child/youth in self-care as developmentally appropriate
• Provides health education and information to optimise transitions
• Anticipates and uses resources to support transitions
• Plays an active role in facilitating effective transitions
The Canadian Pediatric Nursing Standards aim to have a positive impact on ensuring consistent, high-quality Pediatric nursing across all healthcare sectors. Pediatric nurses are well-positioned within the Canadian healthcare system to influence and advance the protection and promotion of the well-being of children. From acute to community care, from indigenous to immigrant health, implementation of these standards will guide uniform excellence in Pediatric nursing care for all Canada’s children and youth. ■ H


ith only 16 specialty Pediatric hospitals serving the entire country, travel to access healthcare is essential for two out of three Canadian families.
As the only national organization enabling access to Canada’s Pediatric healthcare system, Ronald McDonald House Charities (RMHC) is proud to work closely with, and alongside, Pediatric healthcare partners in 23 cities to support caregivers navigating their child’s medical journey.
For 40+ years RMHC has supported over 468,000 families with sick children through accommodation, meals and wellness programming that help ease distinct and significant challenges, providing community, relief from social isolation and financial burden (saving families $57 million in out-of-pocket expenses annually). Today, RMHC remains committed to partnering with the sector on the efforts towards right-sizing Pediatric healthcare to achieve a connected, equitable and accessible system designed for children and their families.
As the need to offer specialized care closer to home grows, greater family support in community hospitals is essential. This makes the partnership between RMHC and local hospitals
a great example of how holistic integrated systems of care can better serve families.
Many families in the Niagara region who require specialty Pediatric care must travel to McMaster Children’s Hospital in Hamilton. While being treated at hospital, 1,000 out-oftown families (40% of whom are from Niagara) stay at the RMHC South Central Ontario (SCO) House, steps away from McMaster, and thousands more use their Family Room inside the hospital.
On August 7, Niagara Health, together with RMHC SCO will open a Family Room in the Marotta Family Hospital in St. Catherines. This will be the 19th Family Room in Canada and will provide a much-needed non-medical space for families inside the hospital to find a moment of respite away from the medical environment.
“Parents are expected to be by their child’s bedside and hold it together, but they also need support” says Mario DeDivitiis, RMHC SCO CEO, adding “We know that with a well-cared for family by their side, sick children get stronger.”
RMHC Family Rooms provide families with a warm, living-room-style space to recharge, enjoy nourishing meals and access laundry facilities at no cost, without having to leave their child.
“The RMHC Family Room reflects our unwavering dedication to patient-centered care,” says Heather Paterson, Executive-Vice President,
Clinical Operations, Niagara Health. “We are thrilled about the strong and collaborative partnership with RMHC South Central Ontario and how we’ll continue working together to meet the needs of families at the Marotta Family Hospital.”
In the Niagara Region, where one in five households are food insecure (the national average is 18%), access to nutritious food is top of mind.
Not surprisingly given the soaring cost of living and inflation pressures faced by many Canadians, food programming has become RMHC’s second most demanded program across the country after accommodation (+44% in 2023 vs. 2022). And for families with sick children, these pressures are compounded by unexpected out-of-pocket expenses like lodging, parking, and meals.
“Parents aren’t patients while their child is in hospital so, unfortunately, parents aren’t fed” said Mario DeDivitiis, RMHC SCO CEO, adding “No parent should have to choose between parking expenses and feeding themselves, but we know that is the reality for some families.”
The hospital takes care of the sick child while RMHC takes care of the family. To measurably improve health
outcomes of children, collaboration in the sector is important. This is why, across the country RMHC works closely with hospital partners to find new and innovative ways to bridge gaps and augment support for families across physical, social and mental health dimensions.
For example, Niagara Health and RMHC developed a unique model to better support patients and their families by jointly training, engaging, and leaning on the same group of volunteers. Furthermore, Niagara Health provides access to their processes and infrastructure. Together, there is a shared commitment to keep the Family Room open 24/7, as well as meet the community’s most pressing need: meal programming (available during select hours).
Local support for community projects is essential. Silvergate Homes, a local family-run business, oversaw the development and construction of the new space. Local McDonald’s Franchisees, long-term supporters of RMHC, did not waver from their support. And notably, many to-go meal options offered within the RMHC Family Room are prepared and donated by students at Niagara College’s Culinary Program.
“At the end of the day, we have the same goal; enabling better outcomes for children across Canada” said Kate Horton, RMHC Canada CEO adding “it truly takes a village.”
Learn more about RMHC programs across Canada at rmhc.ca. ■ H
By Anna Nguyen and Certina Ho
ccording to Health Canada (https://www.canada. ca/en/health-canada/services/drugs-health-products/compliance-enforcement/ good-manufacturing-practices/guidance-documents/policy-manufacturing-compounding-drug-products. html), compounding corresponds to the mixing or combination of two or more ingredients (of which at least one is a drug or pharmacologically active ingredient) to create a customized medication for a patient. Compounding may involve raw materials or a variation or reformulation of commercially available products.
For many years, the quality control, quality assurance, and consistency of the compounding process have been controversial. Medication incidents
and patient safety events have been reported. The implications of compounding, particularly in times of drug shortages, on patient and medication safety should not be underestimated. In March 2012, the Institute for Safe Medication Practices Canada (ISMP Canada) alerted in their Safety Bulletin “Drug Shortages and Medication Safety Concerns” (https:// ismpcanada.ca/wp-content/uploads/ ISMPCSB2012-03_Drug_Shortages. pdf) that the potential for errors and mistakes was high if a pharmacy or a facility tries to perform compounding from raw materials or other active ingredients but without the adequate expertise, facilities, equipment, or other supporting resources to ensure the quality, safety, and accuracy of the final product.
The National Association of Pharmacy Regulatory Authorities (NAPRA) released three Model Standards for Pharmacy Compounding pertaining to (1) Non-Hazardous Sterile Preparations (https://www.napra.ca/ publication/model-standards-for-pharmacy-compounding-of-non-hazardous-sterile-preparations); (2) Hazardous Sterile Preparations (https:// napra.ca/publication/model-standards-for-pharmacy-compounding-of-hazardous-sterile-preparations); and (3) Non-Sterile Preparations (https://www.napra.ca/publication/ model-standards-for-pharmacy-compounding-of-non-sterile-preparations), providing guidance to safe compounding practices. Implementation of the above model standards is under the authority of the respective provincial, territorial, or Canadian Armed Forces pharmacy regulatory authorities, of which each has their own policies and procedures for implementing these standards in their jurisdiction.

tencies-for-pharmacists-and-pharmacy-technicians-in-canada/) – which defines competencies for compounding pharmacy professionals to ensure safe and quality compounding practices. These competencies are further broken down to align with the above three Model Standards for Pharmacy Compounding of (1) Non-Hazardous Sterile Preparations; (2) Hazardous Sterile Preparations; and (3) Non-Sterile Preparations. In other words, all pharmacy professionals who are involved in compounding are expected to demonstrate the competencies that are defined in the corresponding category of compounding. Compounding pharmacy professionals should be aware of and adhere to their provincial or territorial regulations of practice. For instance, in Ontario, the Ontario College of Pharmacists (OCP) has adopted the NAPRA’s Model Standards for Compounding, with full implementation for non-hazardous and hazardous sterile preparations (https://www.ocpinfo. com/practice_resource/sterile-compounding) on January 1, 2019, and non-sterile preparations (https://www. ocpinfo.com/practice_resource/compounding) on January 1, 2022.







In Canada, the compounding of drugs is practiced primarily by pharmacy professionals and is regulated under the jurisdiction of their respective provincial regulatory authorities as mentioned above.














In July 2022, NAPRA released a resource document – Model Compounding Competencies for Pharmacists and Pharmacy Technicians in Canada (https://www.napra. ca/new-napra-document-published-model-compounding-compe-
The goal of the above standards and regulations is to advance safe compounding practices and to ensure quality patient care. As the recipient of care and the final compounded preparation, patients should always consider the five questions to ask about their medications (https://www. ismp-canada.org/medrec/5questions. htm) during a clinical encounter with their healthcare providers. Patients should always be well informed of their medications, including compounding preparations. ■ H
fter a Canada-wide competition, a team of researchers at Royal Victoria Regional Health Centre (RVH) have received a $668,968 grant to help reduce the administrative burden physicians face when conducting goals of care discussions.
Led by RVH intensivist and Chief Research Scientist, Dr. Giulio DiDiodato, the two-year project – made possible through the Health Care Unburdened Grant program established by the Canadian Medical Association, MD Financial Management Inc., and Scotiabank, – will support the dissemination of an innovative e-tool that facilitates a new clinical standard for how hospitals, family health teams, and long-term care homes conduct goals of care discussions.
Goals of care discussions are conversations between patients, families, and doctors and are vital in under-
standing the patient’s values, preferences, and desired outcomes for their medical treatment.
“Knowing what is most important to our patients in terms of their health, quality of life, and personal values is considered an essential component of high-quality care,” says Dr. Chris Martin, co-applicant on the grant and RVH’s Chief of Critical Care. “This is especially important for life-threatening illnesses, where goals of care discussions may focus on more complex treatments that prolong life, but may also involve significant burdens or risks.”
Despite the critical nature of these conversations, there is no systematic or standardized practice for conducting goals of care discussions. And of the few tools that have been developed, none can be applied across all diseases or offer validated prognostic models that would ensure widespread use throughout the health system.


“Currently, doctors carry the sole responsibility for leading goals of care discussions, which should occur for every patient encounter involving a major clinical decision,” says Dr. DiDiodato. “But with so many patients to see, it can be difficult to find time to have these very personal, very empathetic conversations.”
Even the most skilled doctors may still struggle to find the right words at the right time when discussing sensitive and emotional topics with their patients and families.
“With the use of our e-tool to guide the process, any trained caregiver can now initiate and navigate goals of care discussions for any condition in a safe and confident manner,” adds Dr. DiDiodato. “We are excited to potentially save hundreds of thousands of administrative hours every year for physicians across Canada.”
Over the past five years, Dr. DiDiodato and the team at RVH have
developed and validated these new clinical standards, first through a small pilot study, then through a large randomized clinical trial supported through a grant from the Alectra Fund for Health & Social Innovation in 2022.
“Building on these initial successes, the Health Care Unburdened Grant now paves the way for us to share this homegrown innovation with our healthcare peers across the province,” says Dr. Jesse McLean, RVH’s Director of Research and co-author on the grant. “We will also be working with several community partners to help spread the tool, including teams at Georgian College’s School of Computer Studies and Henry Bernick Entrepreneurship Centre, as well as Barrie and Area Ontario Health Team, and the University of Toronto’s Family Medicine Teaching Unit located at RVH”. ■ H
By Tara Hutchison, Justice Seidel, and Heather Ross
kiskinohtahiwewak, derived from the Moose Cree language meaning “they who show the way,” is a program revolutionizing the recruitment and retention of healthcare professionals from the western James Bay and Hudson Bay region. Established in 2021, the kiskinohtahiwewak program, or kiskino for short, focuses on increasing the representation of First Nations healthcare providers from the region working for the Weeneebayko Area Health Authority (WAHA).
The beginning of kiskinohtahiwewak
In 2021, Dr. Max Boulet, a resident physician, and Justice Seidel, a Moose Cree First Nation member and
community-based researcher, both working for WAHA, discovered their shared vision of increasing the number of local First Nations physicians serving the region’s communities. With a population of approximately 12,000 people, to date, only two local First Nations community members have ever returned to the Weeneebayko region to practice medicine. This realization led to the birth of the kiskinohtahiwewak program.
kiskino’s first outreach events took place in 2022 at high schools in the Ontario communities of Moosonee and Moose Factory. Students were provided hands on learning experiences through interactive activities like practicing CPR and pediatric first
aid techniques. The Northern Ontario School of Medicine University, Queen’s University and the University of Toronto all gave presentations on the various medical programs offered at each of their schools.
Community mentorship
Mentoring resources are often lacking in rural and remote First Nations communities. kiskino’s unique approach uses a mentor and mentee model with students from high school through post-secondary and graduate school/medical school. Mentors are paired with mentees from the same community to build relationships based on shared cultural understanding and show mentees a successful career in healthcare is achievable.
Mentors help student mentees navigate competitive application processes for healthcare programs and provide ongoing support throughout the mentees’ academic journey. Many mentees become mentors to the next wave of high school students interested in healthcare careers.
Success stories and future goals
Over the past three years, kiskino has engaged more than 500 students through outreach events that provide hands-on healthcare experiences, aiming to inspire and guide them towards medical careers. Currently more than 20 people are being mentored in nursing, medicine, and physiotherapy. In the long term, kiskino has set a target of 50 per cent of all WAHA medical
itrous oxide (N2O) is an important contributor to climate change; not only is it a greenhouse gas (GHG), it is also an ozone-depleting agent. It is the third most significant GHG in the atmosphere after CO2 and methane, and is the largest remaining threat from ozone-depleting substances in the stratosphere1. N2O is a medical gas that is used as an inhaled drug in a select few areas in a hospital for its anesthetic and anti-anxiety effects. In Canadian hospitals, N2O is often administered through a centralized system. It is typically stored in a bulk tank or large central cylinders and is delivered through gas distribution piping. Studies in Canada2,3, the US4 and Europe5 have shown that these tanks and distribution piping can leak significantly even with regular preventative maintenance, venting N2O directly to the surrounding environment.
Engineers and facility experts across Canada are evaluating existing systems and have found that N2O leakage can be very high, accounting for
as much as 85-99 per cent of its total use. In 2023, one health system in Ontario emitted the equivalent of 1050 tC02 from N2O; approximately 90 per cent of these emissions were the result of leaked N2O from distribution piping (M. Apostol, personal communication, April 26, 2024). Fixing these leaks is labour intensive and costly and the areas from where a leak can develop are unpredictable, raising significant concerns for exceeding occupational health and safety limits of the gas in patient and staff areas.
Nitrous oxide has limited clinical use in current medical practice. Routine use of nitrous oxide in patients having surgery and requiring general anesthesia has decreased considerably with the awareness of its environmental impact. As well, many studies have confirmed that nitrous oxide, as an adjunct to other anesthesia drugs, confers no clinical advantage. For that reason, the Canadian Guidelines to the Practice of Anesthesia: Revised Edition 20236 suggest that N2O use in anesthesia be eliminated. However,
N2O continues to be used for women in the birthing suite who are in active labour. Inhalation of N2O somewhat lessens the pain of labour, though most parturients eventually transition to a more effective form of labour analgesia. N2O can easily and more efficiently be delivered to labouring patients using portable cylinders without the disadvantages of leakage.
While many existing health systems are working toward N2O mitigation by decommissioning central N2O infrastructure and changing to small point-of-use portable cylinders, new hospital developments should not install centralized N2O delivery systems at all. Policy papers from the US7 and UK8 support the omission of centralized delivery systems in new hospitals. The Centre hospitalier de l’Université de Montréal is a new build that was completed in 2017. In 2022, maintenance and leakage led to N2O release more than ten times greater than estimated clinical use. After discussion with clinicians, to prevent future leaks and lower ongoing maintenance costs,
the central N20 tank and piping was decommissioned. N2O delivery was replaced with portable cylinders, reducing greenhouse gas emissions, maintenance requirements and costs (S. Williams, personal communication August 29, 2023).
Health care engineers are in a unique position to work with their architects, designers and clinical teams, in order to educate about the disadvantages of centralized N2O delivery systems. There appears to be no advantage of having a centralized supply at all.
N2O delivery from portable systems or E-cylinders are more environmentally and economically efficient for all areas of delivery. Existing systems should be evaluated and new hospital builds avoid the installation of centralized N2O infrastructure, which will save money, reduce direct greenhouse gas emissions, and protect the ozone layer. The authors are collaborators with the Canadian Coalition for Green Health Care. For feedback, please contact Anita Rao: anita.rao@thp.ca ■ H
staff being First Nations community members from the region in the next decade.
Justice Seidel’s journey epitomizes kiskino’s impact. Initially unaware of her potential for a career in medicine, Seidel’s collaboration with Dr. Boulet and later mentorship led to her application and acceptance into the Northern Ontario School of Medicine University (NOSM University). Now a second-year medical student, Seidel, has signed a return of service agreement to practice as a family physician with WAHA after graduation.
“The essence of kiskinohtahiwewak is rooted in uplifting community members to achieve their full potential in a culturally supportive way. This is modeled by my own experience of being mentored and encouraged by Dr. Max Boulet in a way that respected and valued my cultural and lived experience as a First Nations person, which led to my admission into medical school. The collective success of kiskino is further strengthened by the work and perspectives of the rest of our leadership and advisory circles, making this program truly rooted in community,” said Justice Seidel, kiskino mentor and sec-

ond-year medical student at NOSM University.
The kiskinohtahiwewak program is a pioneering initiative in Canada, driven by First Nations community members for the benefit of their own communities, marking a significant step forward towards equitable healthcare


Max
Mentorship
representation and service in the western James Bay and Hudson Bay region.
The Weeneebayko Area Health Authority (WAHA) provides acute and ambulatory healthcare services to communities along Ontario’s western James Bay and Hudson Bay coasts. We serve over 12,000 people through hos-
Advancement

pitals in Moose Factory, Fort Albany, and Attawapiskat, and a health centre in Moosonee. We also operate regional outpatient programs, as well as paramedicine services throughout the region, including in Kashechewan and Peawanuck. WAHA is affiliated with Queen’s University. ■ H



SEPTEMBER FOCUS: Technology and Innovation in Healthcare/ Artificial Intelligence (AI)/ Patient Experience/Health Promotion
Online Education:
New treatment approaches to mental health and addiction. An overview of current research initiatives Programs and initiatives focused on enhancing the patient experience and family centered care. Programs designed to promote wellness and prevent disease including public health initiatives, screening and hospital initiatives.
Annual Medtech Technology Supplement & Distribution To Medtech Conference Attendees. Plus: Annual Online Education Focus

OCTOBER FOCUS: Infection Control Supplement / Mental Health and Addiction/Patient Safety/Research/:
New treatment approaches to mental health and addiction. Developments in patient-safety practices. An overview of current research initiatives. Developments in the prevention and treatment of drug-resistant bacteria and control of infectious (rare) diseases. Programs implemented to reduce hospital acquired infections (HAIs).
Annual National Infection Control Week (Oct.14-18) Supplement

n a recent study, scientists at UHN’s KITE Research Institute found that individuals with concussions are at a higher risk of experiencing visually-induced motion sickness.
This finding has important implications for the use of virtual reality in the assessment and rehabilitation of concussions.
Concussions, a common type of mild traumatic brain injury, can lead to a range of symptoms including balance problems, memory impairments, dizziness and headaches.
Research suggests that individuals with concussions rely more heavily on visual cues due to impairments in
their balance and sensory integration systems. This increased dependence on visual cues can make individuals more prone to visually-induced motion sickness (VIMS).
Virtual reality has become a popular method for assessing and rehabilitating concussions due to its immersive and controlled environments, which can visually simulate real-world scenarios for therapeutic purposes. However, the increased risk of VIMS among individuals with concussions highlights the importance of careful design and use of virtual reality in treating concussions.
Drs. Behrang Keshavarz and Jennifer Campos, Senior Scientists at KITE, led
a team of researchers to investigate the effect of concussions on VIMS when exposed to virtual reality environments.
The research team exposed 31 participants, including 16 individuals with concussions and 15 healthy individuals, to a virtual reality scene simulating motion through a grocery store aisle at varying speeds.
Individuals with concussions were found to experience more severe VIMS compared to healthy individuals, suggesting that the presence of concussion symptoms notably increases the risk and severity of VIMS.
“These findings underscore the importance of meticulously evaluating visual stimulation in concussion
Of course your mother wants to stay in her own home. She’s lived there for 60 years, from when you and your siblings were kids. While alone now since your dad passed away and everyone’s moved out, she has family and friends over, and loves the place. But you still worry.
You know that older adults are more likely to fall. And you get the feeling your mother’s been getting more forgetful lately.
Dr. Jie Liang and his startup company, AltumView, had you – and the global aging population – in mind when they decided to use their expertise in engineering to create technology that can assist older adults to live more safely – and with an eye on changes in their evolving health.
“Most of the existing technology available for remote monitoring of older adults is very old and there has been little focused on the seniors sector,” says Dr. Liang, professor in the School of Engineering Science at Simon Fraser University in Vancouver. “We have expertise in the video and image processing and Artificial Intelligence (AI) areas and thought that we could apply that to a new way for families and caregivers to make sure their loved ones are safe at home.”

Dr. Jie Liang
normal movements are detected, Sentinare will send an alert to the person’s contacts via their smartphone.
And there’s a critical privacy-preserving feature Dr. Liang says is distinctive from traditional surveillance cameras: Sentinare will only send stick figure animations of the person, instead of the real video.
“Privacy is important. After all, Sentinare is used in places where people go about all the activities we do in our homes. So, if your mother is using the bathroom and she falls, you will be notified with a stick figure animation to show what happened, not a full video of her.”
Sentinare also provides daily analytics that offer a wealth of health information about, for example, sleep habits and the amount of physical activity a person is getting.
In fact, that aspect has served the inventor and his family well.
been selling well, with customers in about ten countries, says Dr. Liang. In particular, in 2022, it was selected by Amazon as one of only three fall detection devices in its Alexa Together emergency service, and has received the best customer review. Most Amazon customers purchase Sentinare for their parents living independently, but their positive reviews have helped AltumView to get Sentinare into the residential care and remote patient monitoring sectors as well.
AltumView was recently selected as one of five Canadian companies to expand their healthy aging solutions into the UK and even Europe as part of the coveted UK Canada AgeTech Innovation Exchange program.
Their solution is the Sentinare smart activity sensor.
Sentinare uses AI algorithms to perform a number of functions. One is around the safety of a person in their home. Sentinare mounted throughout the home monitor physical movement. If a fall out of bed, a slip or other ab-
Dr. Liang had Sentinare installed in his mother’s home. “She is 80 and lives alone. Early last year I began to notice changes in her daily activity. I did not pay much attention at the beginning, but a few months later her situation was worse and she was diagnosed with dementia. I then realized that Sentinare really has the potential to help identify some disease symptoms earlier.”
The product was a CES 2021 Innovation Award Honoree, and has
Dr. Liang is thankful to AGEWELL for its support, which included a $50,000 post-discovery grant to test Sentinare, valuable feedback from an older adult/caregiver insight panel, and a session with AGE-WELL’s volunteer chief entrepreneur, Michael Tamblyn.
Dr. Liang feels the time is right for Sentinare, given what the world has experienced over the past few years.
“The pandemic showed us that we need a big overhaul of how we care for seniors. The average lifespan is increasing. So we need to ensure that we can provide a safe home environment now more than ever before.” ■ H
management,” the researchers explain.
“Understanding the link between concussion symptoms and VIMS can help develop better strategies for employing virtual reality in concussion rehabilitation without exacerbating VIMS.
“Importantly, virtual reality could be effectively implemented in the rehabilitation of visually-induced symptoms during concussion.”
As virtual reality technology becomes more prevalent in clinical settings, ensuring that it is safe and effective for use in vulnerable populations, such as individuals with a concussion, remains a priority.
These insights offer a valuable foundation for further exploration into optimizing virtual reality-based interventions, ultimately improving recovery experiences for concussion patients.

Participants in the study were exposed to a virtual reality (VR) scene of a grocery store aisle, (R), in a dome-shaped VR laboratory at UHN’s KITE Research Institute.

This work was supported by the Canadian Institutes of Health Research and UHN Foundation. Dr. Jennifer Campos is a Canada Research Chair for Multisensory Integration and Ageing and a professor in the Department of Psychology at the University of Toronto


As the only national organization enabling access to paediatric healthcare, RMHC across Canada is proud to partner with children’s hospitals in support of families with sick children.
Together, we can ensure even more families have a place to stay, access to nutritious meals, mental health and wellness programming, and a community of support when it’s needed most.
Learn more at RMHC.ca
