FRCPath Part 2 Surgical Course
Endocrine Pathology
Eranga Nissanka-Jayasuriya William Harvey Hospital, Ashford, Kent
19/01/2023

WHO 5th Edition (2022)
Thyroid tumours


Marking Scheme
Case 1
3.5 3.0 2.5 2.0 1.5 1.0
Case 1 59-year-old Female, Thyroid nodule.










Case 1 Diagnosis
Medullary carcinoma
Discussion • Sporadic- commonest, older age, no c cell hyperplasia, best prognosis • Hereditary (25%)- RET mutation, poor prognosis • MEN2A/2B associated- c cell hyperplasia, slightly older age, aggressive • Familial medullary thyroid carcinoma (FMTC) syndrome, von Hippel-Lindau disease or neurofibromatosis • Bilateral, multicentric in syndromic patients
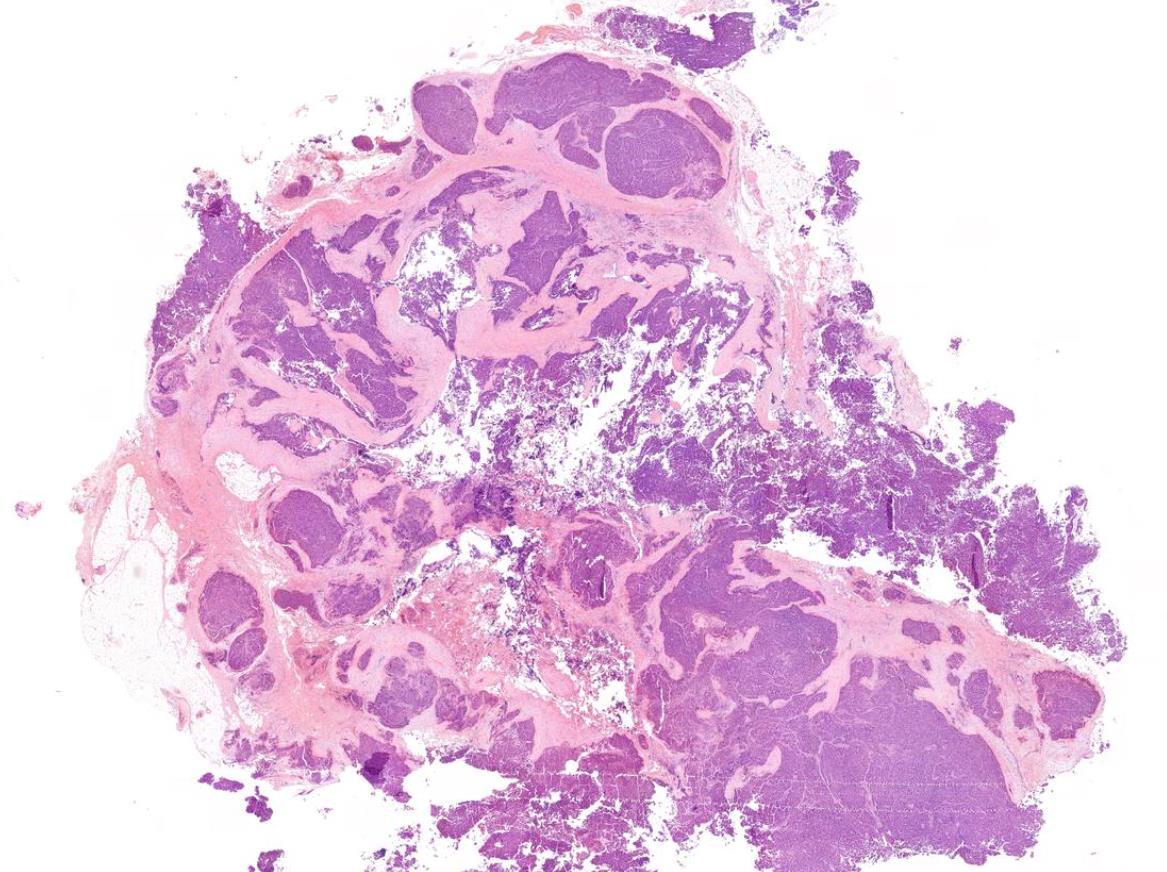
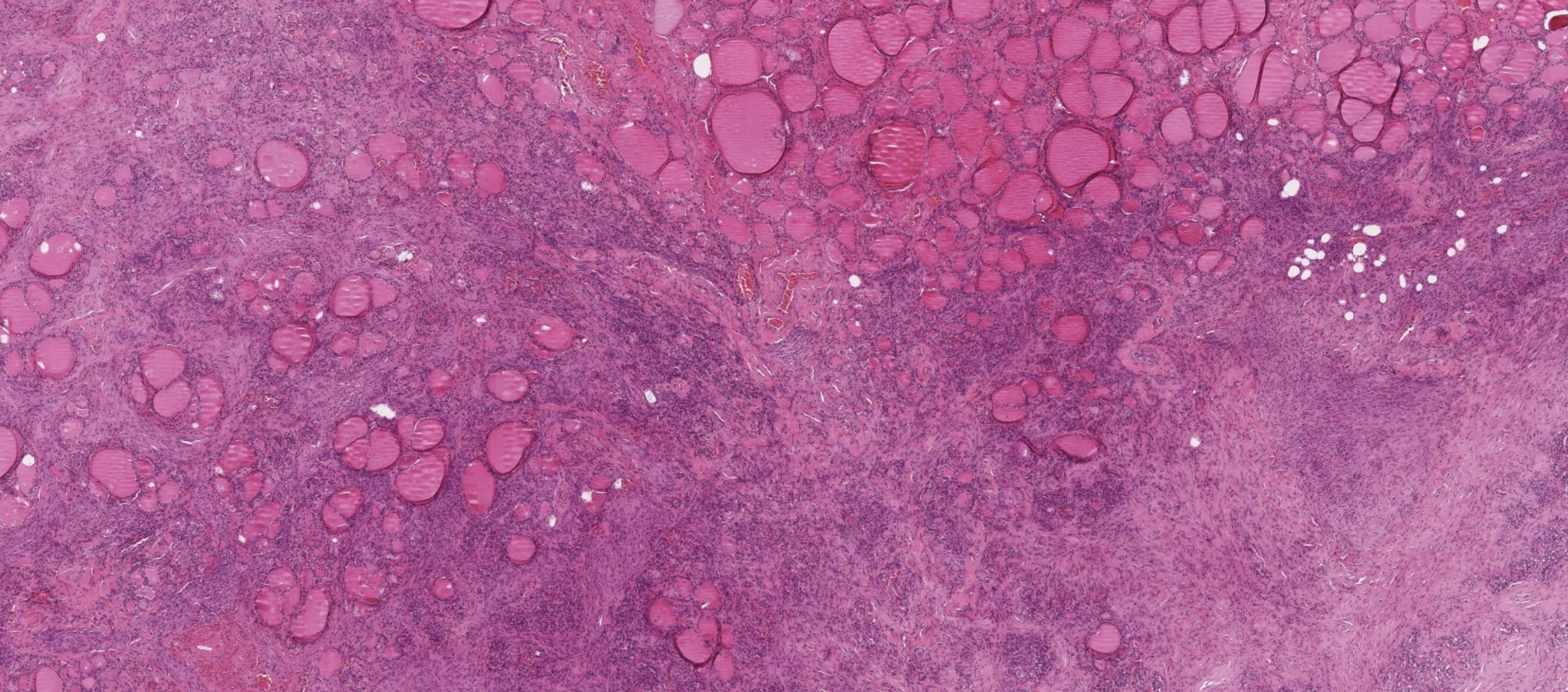
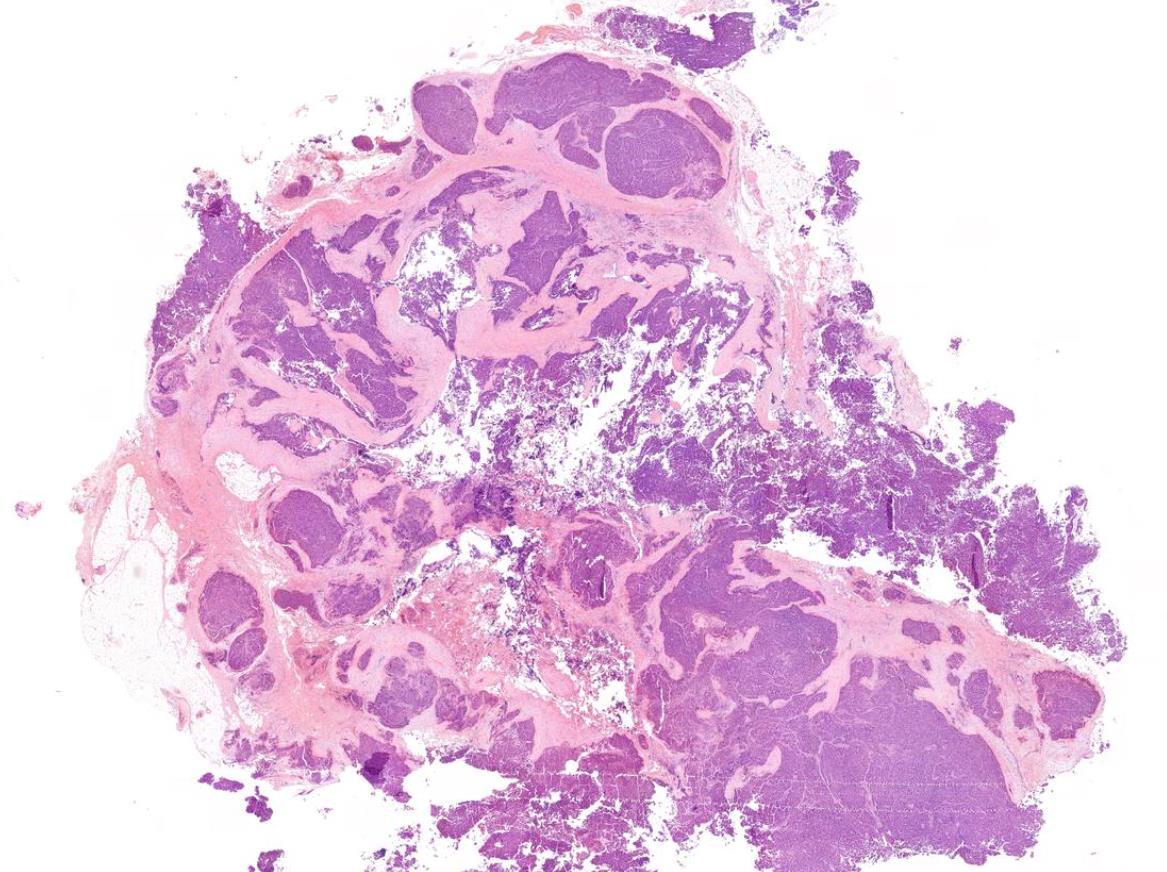
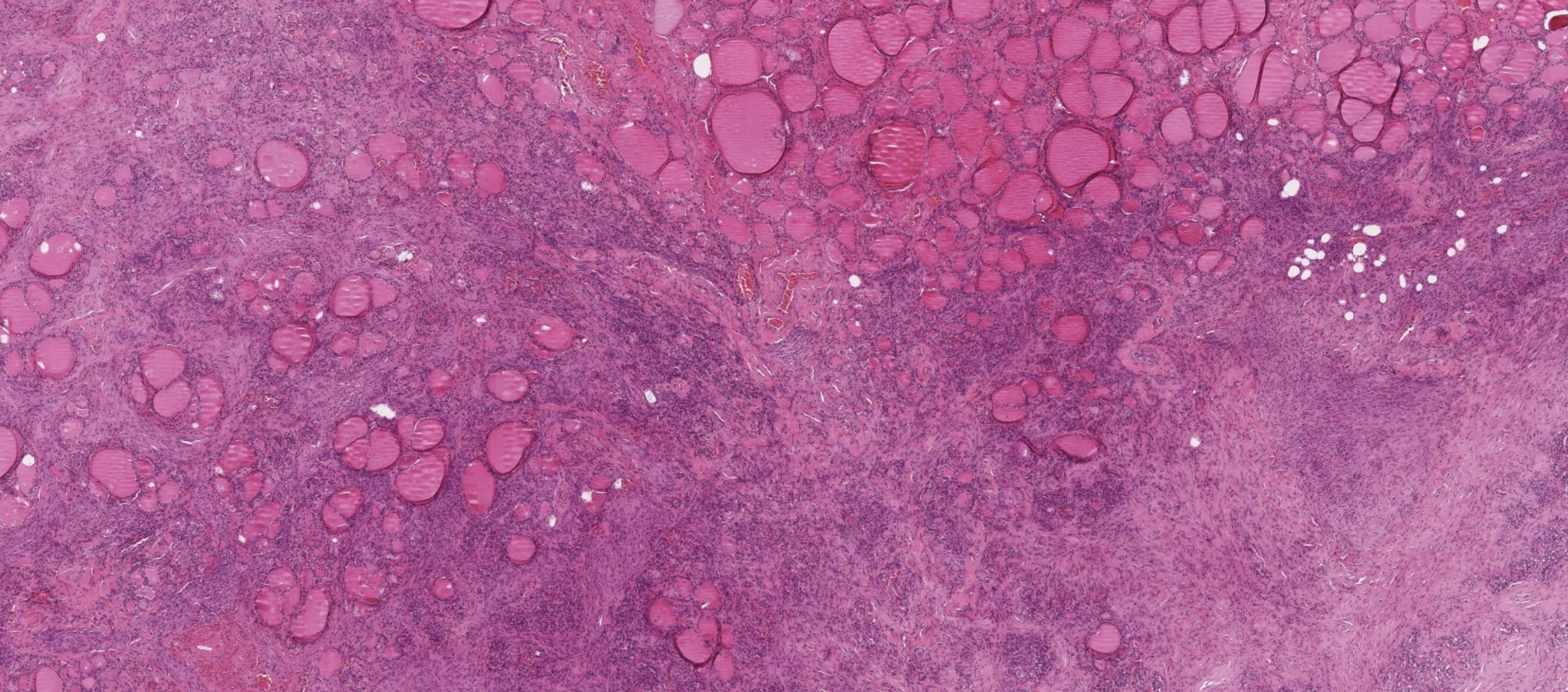
Case 2
43-year-old Female, Neck mass.






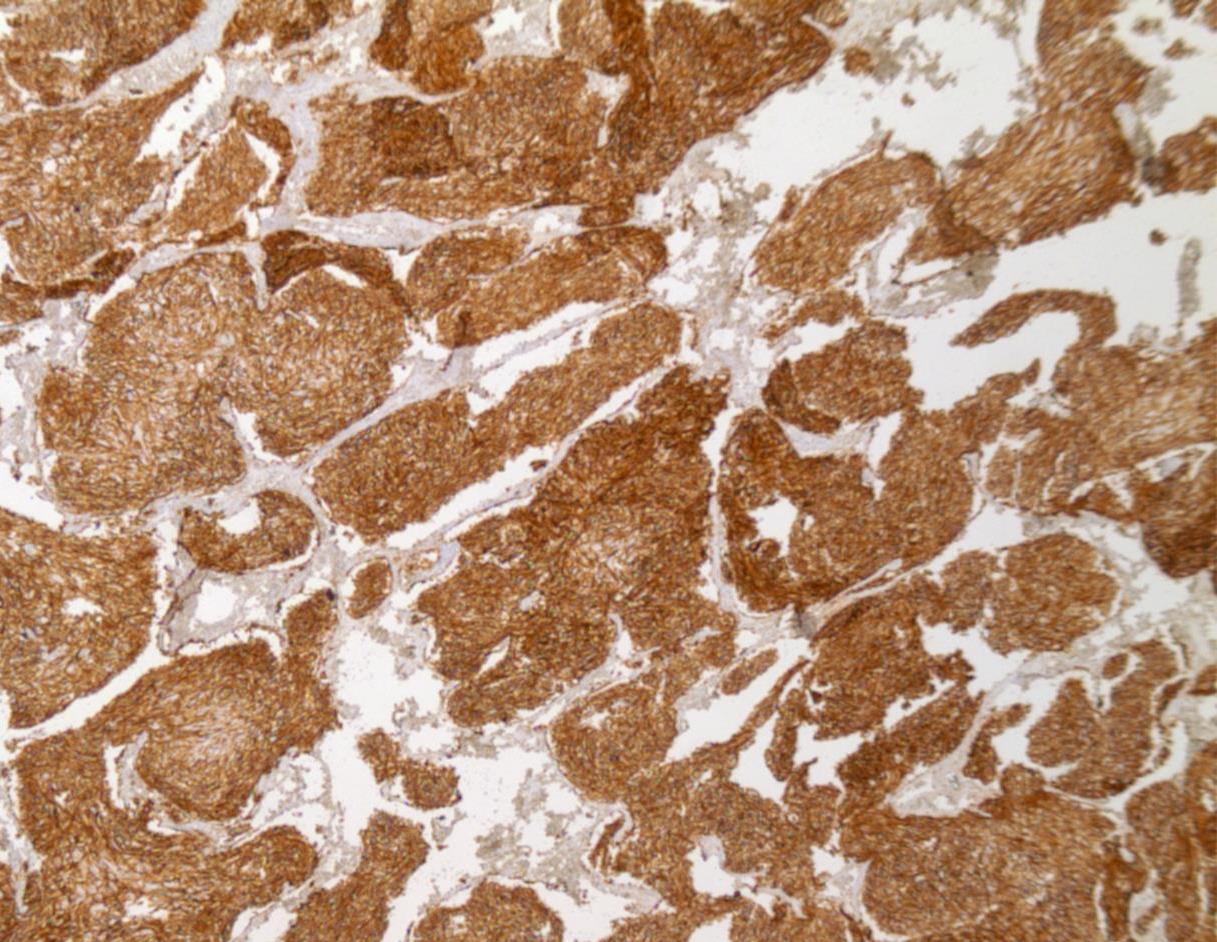
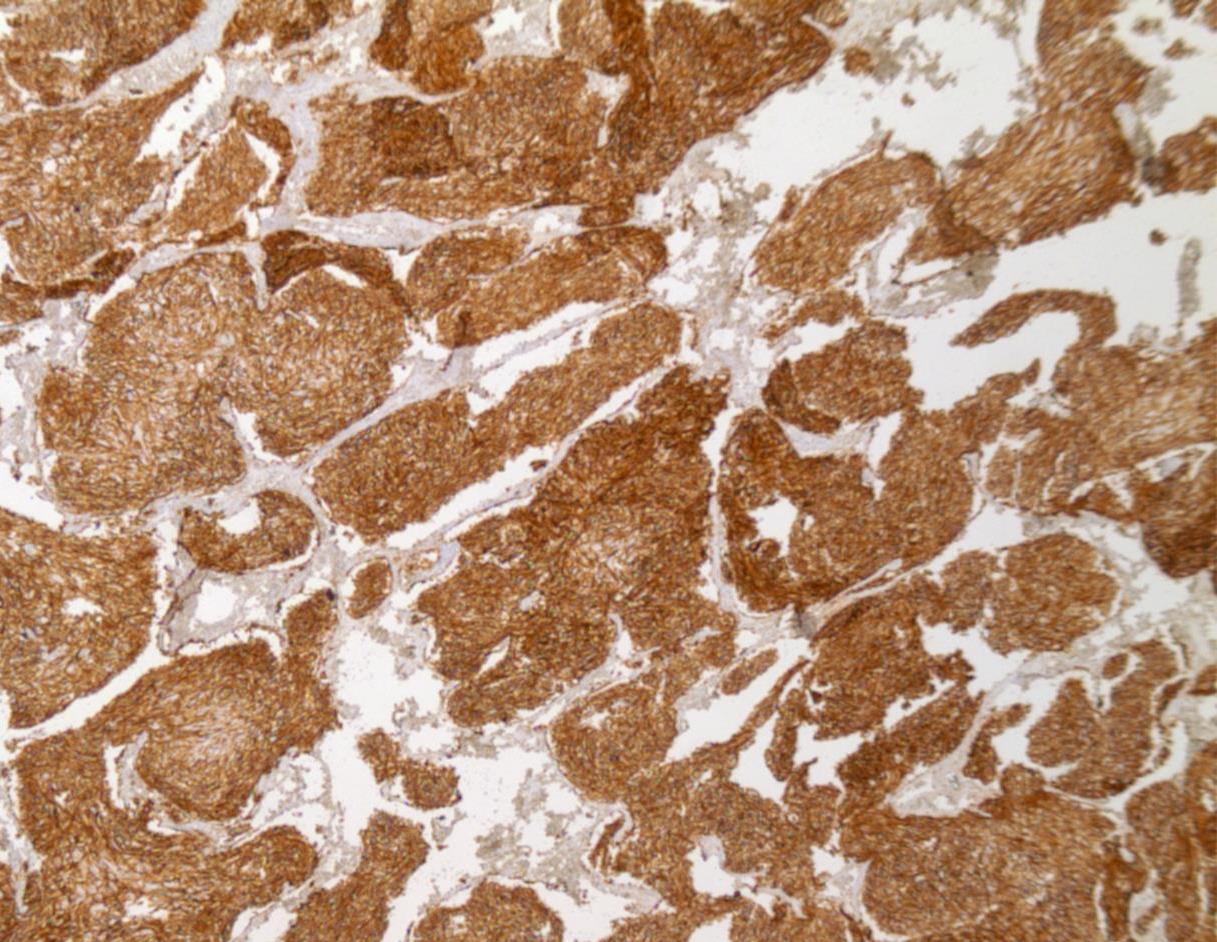
TTF1 Thyroglobulin TTF1 Thyroglobulin
Case 2 Diagnosis
Metastatic Dedifferentiated Hurthle cell carcinoma
Approach & Discussion • Working diagnosis: Poorly differentiated carcinoma • What IHC? Broader spectrum for origin including TTF1, thyroglobulin • Composed of oncocytic cells (at least 75%) in which the nuclear features of papillary thyroid carcinoma and high-grade features are absent. • Prognosis largely depends on the extent of vascular invasion • mortality >90% at 10 years • PTEN mutation syndrome (e.g., Cowden syndrome) and Carney complex (PRKARIA mutation)
Case 3
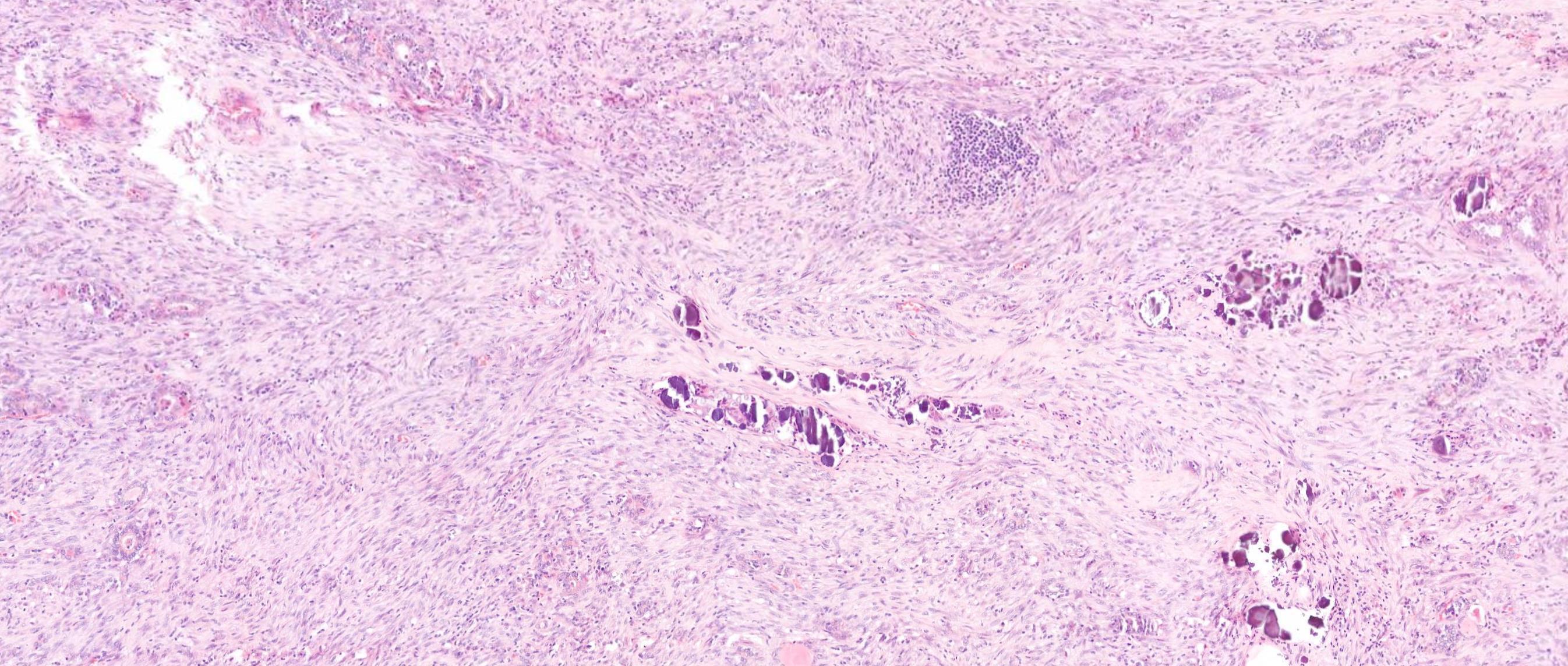
55-year-old Male, Large thyroid mass.





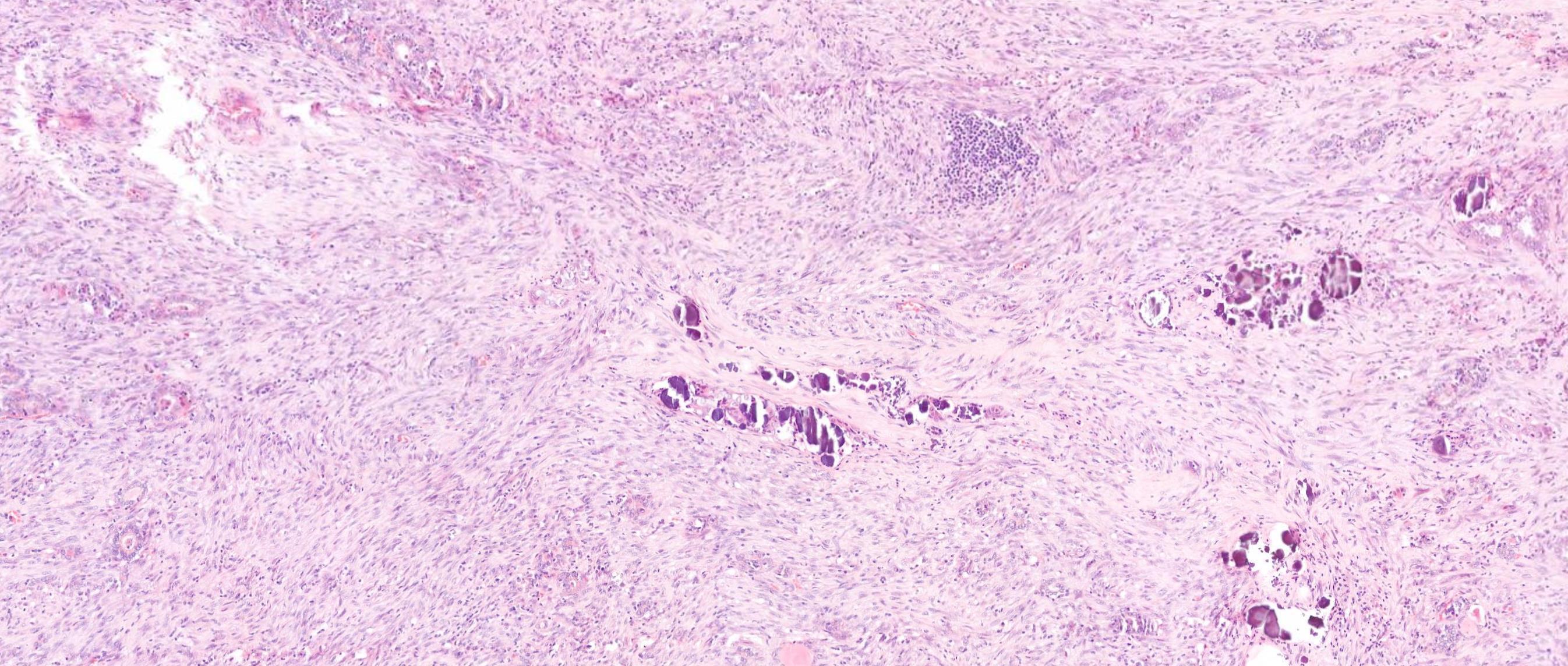


Salient points • Papillary carcinoma component • Spindle cell component • 4 possibilities for the spindle cells • Spindle cell metaplasia of follicular cells- epithelial (bland cytology) • Fibromatosis/fasciitis like spindle cell stroma- fibrous (bland cytology) • Anaplastic transformation of PTC (rare) –HG cytology • Sarcomatous transformation of PTC (very rare)- HG cytology How to make the distinction? IHC Molecular –ATC: B catenin, TP53

Case 3 Diagnosis
Papillary thyroid carcinoma with sarcomatous differentiation
Marking Scheme
3.5 3.0 2.5 2.0 1.5 1.0 Case 1
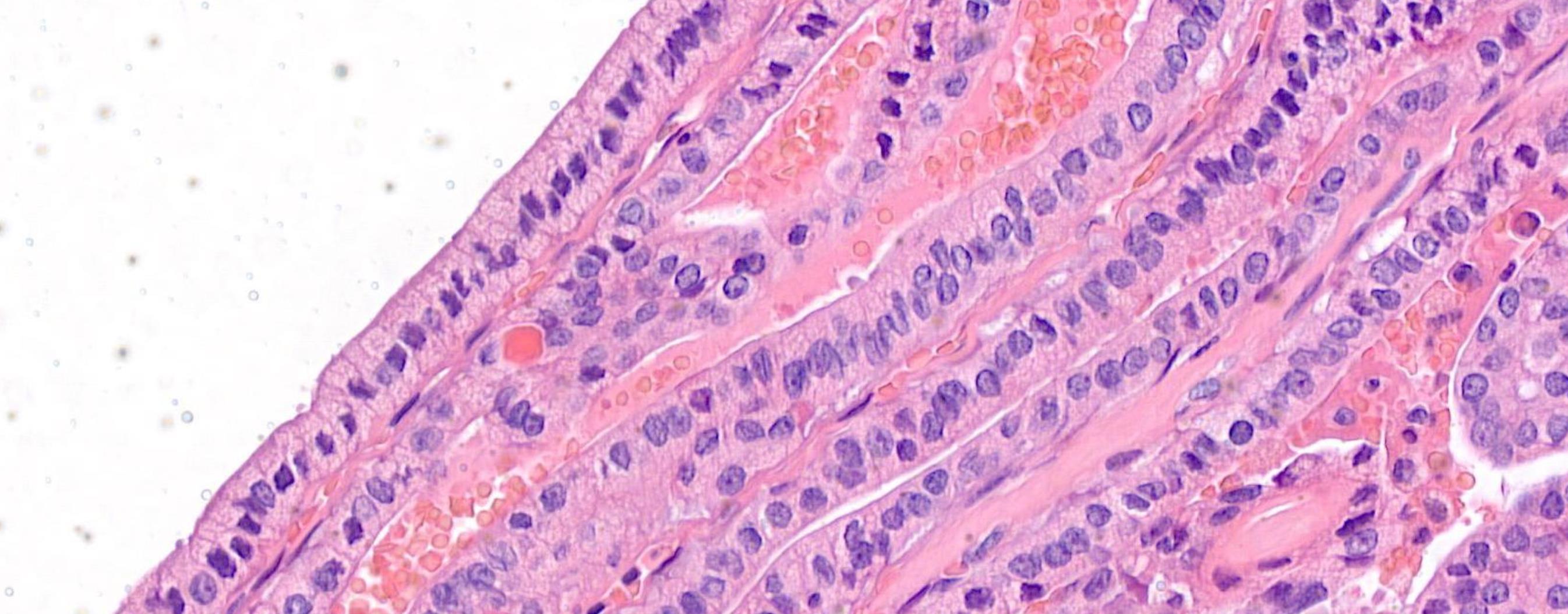
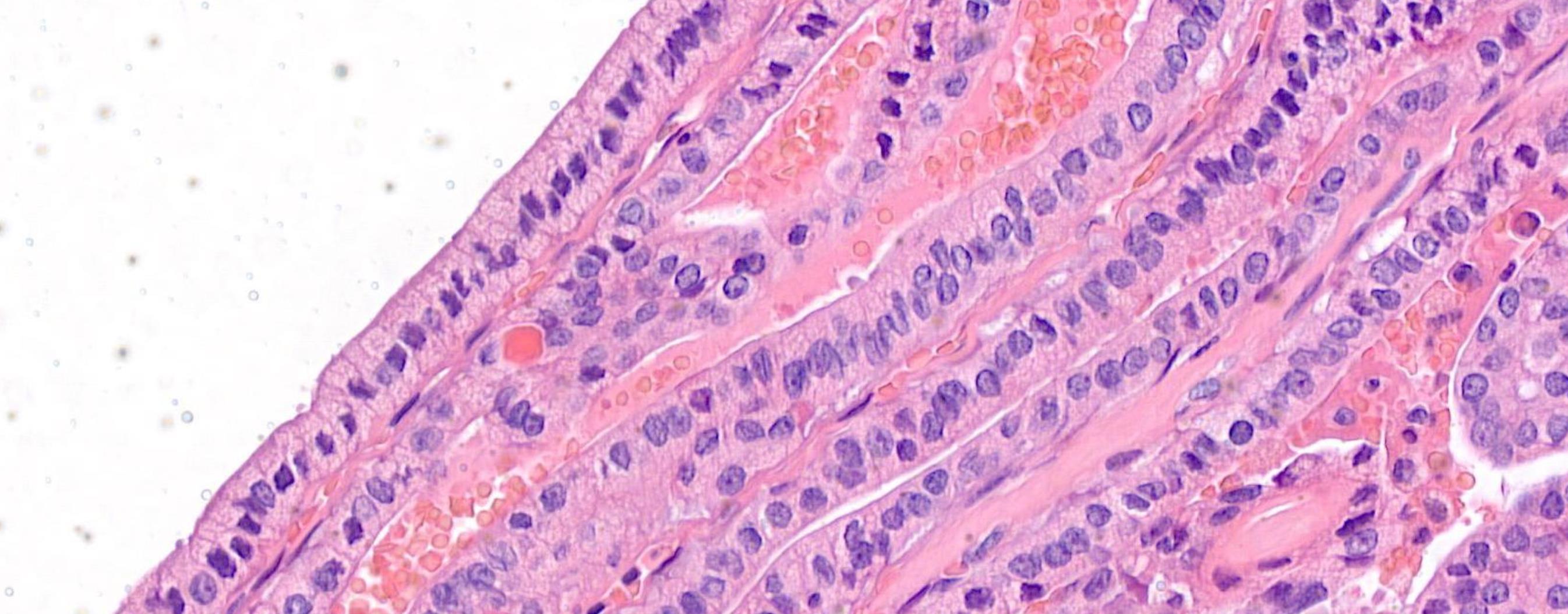
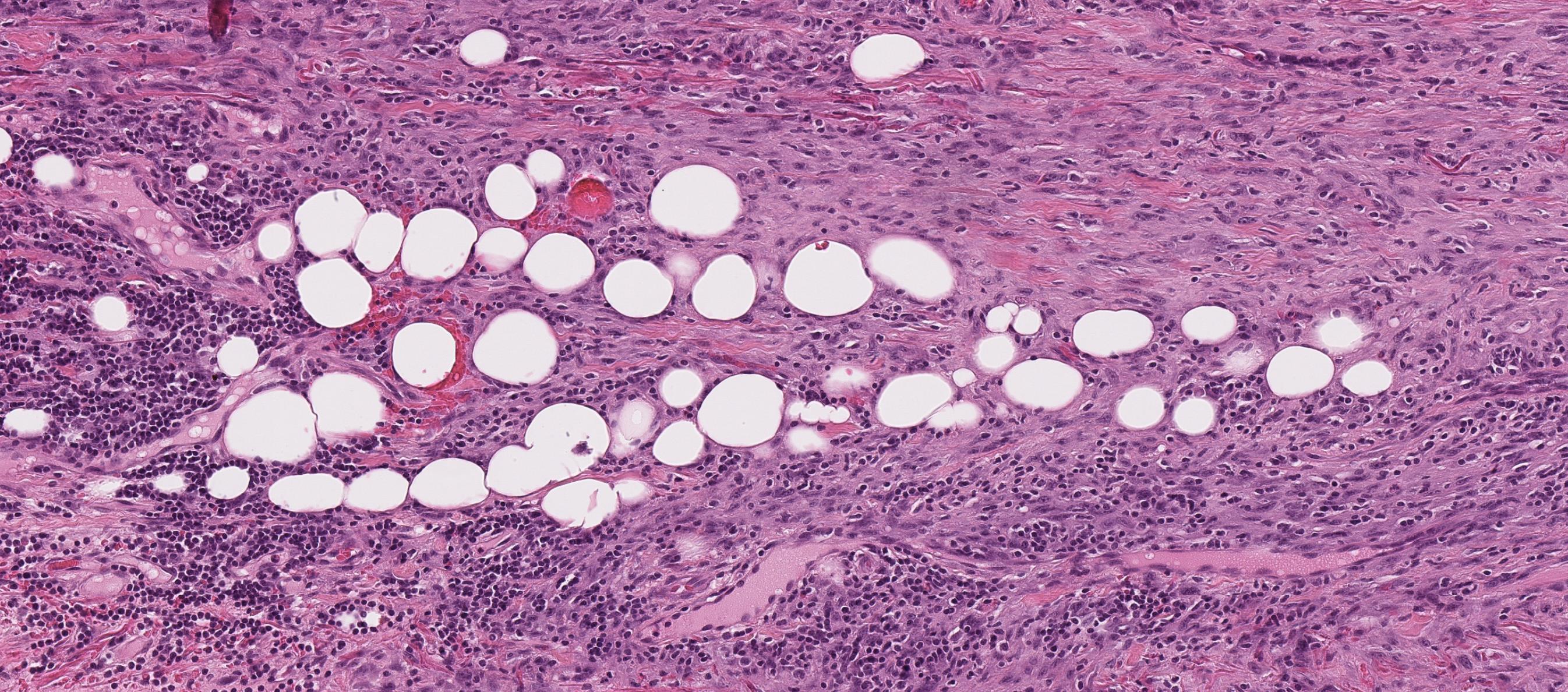
Case 4
42-year-old Female, Left level 4 lymph node.





Case 4 Diagnosis
Metastatic diffuse sclerosing variant of papillary thyroid carcinoma
PTC subtypes-risk stratification
Diffuse enlargement, Solid tumour nests with squamous metaplasia, including squamous morules, dense sclerosis, numerous psammoma bodies, background chronic lymphocytic thyroiditis This tumour is common in children and young adults BRAF mutation (50%), RET/PTC1 rearrangement (28%), RET/PTC3 (14%) Highlights
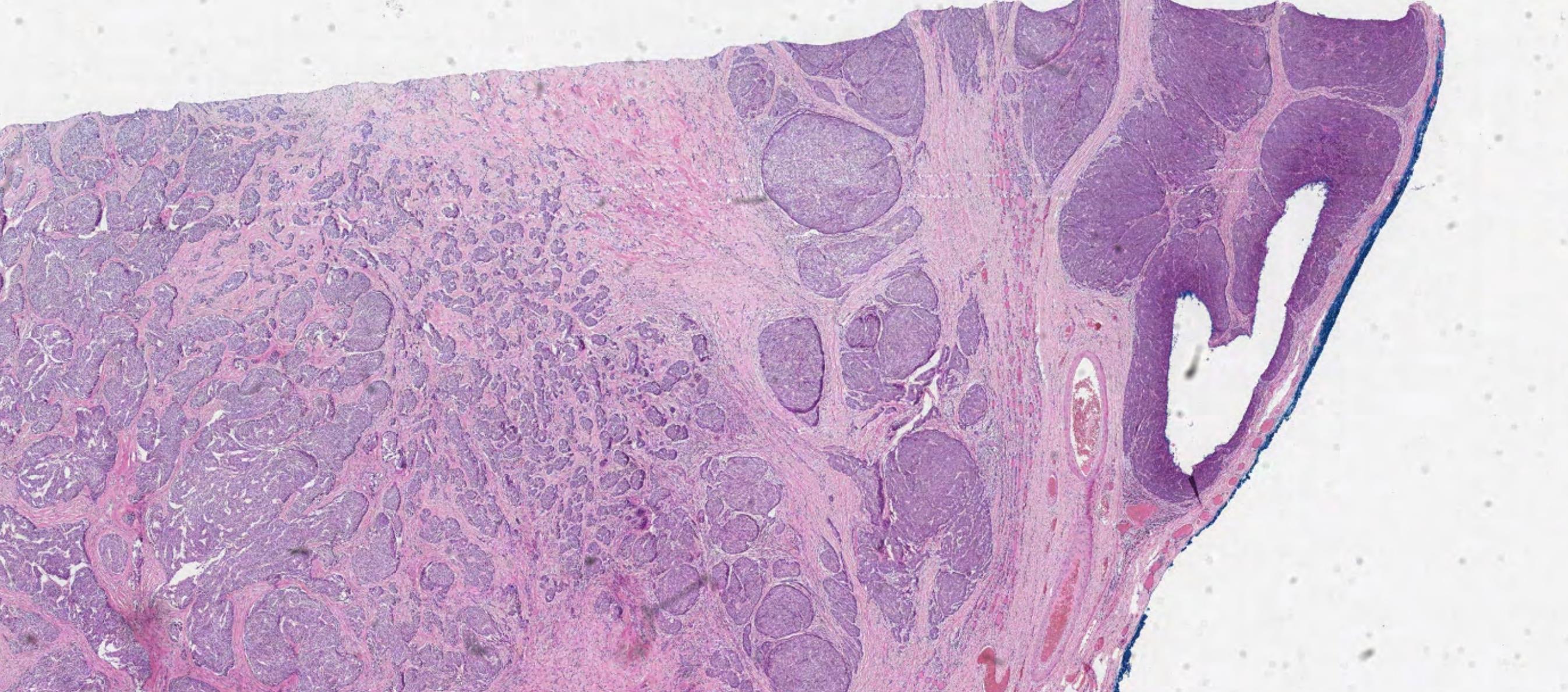
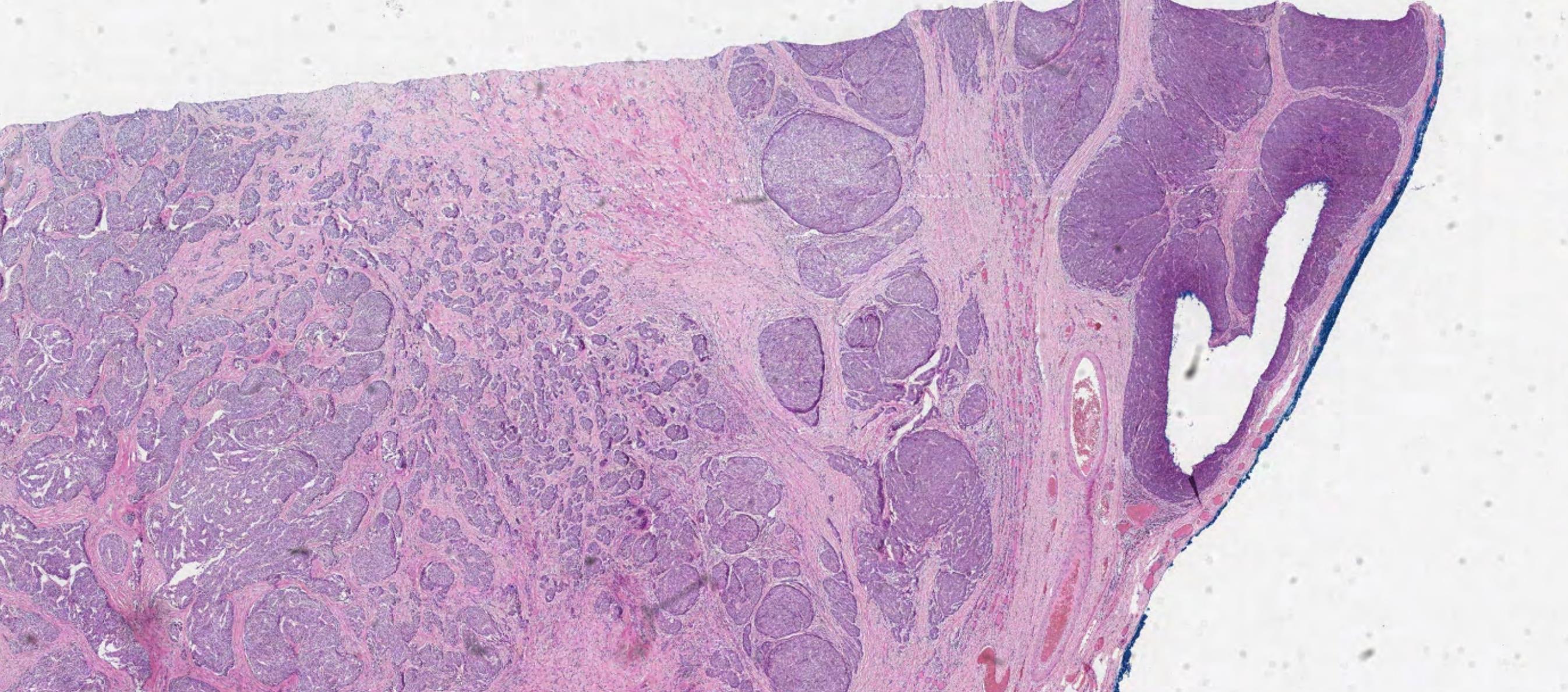
Case
5 52-year-old Female, Left thyroid lobectomy.



Case 5 Diagnosis
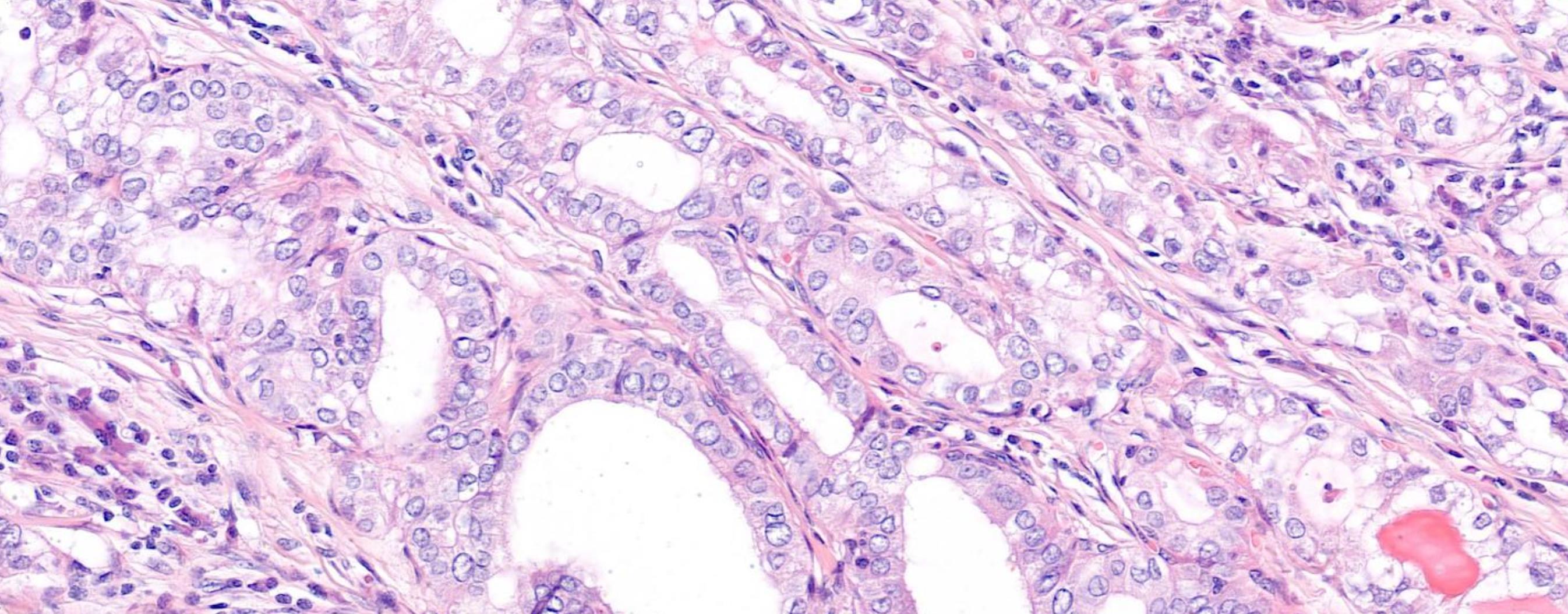
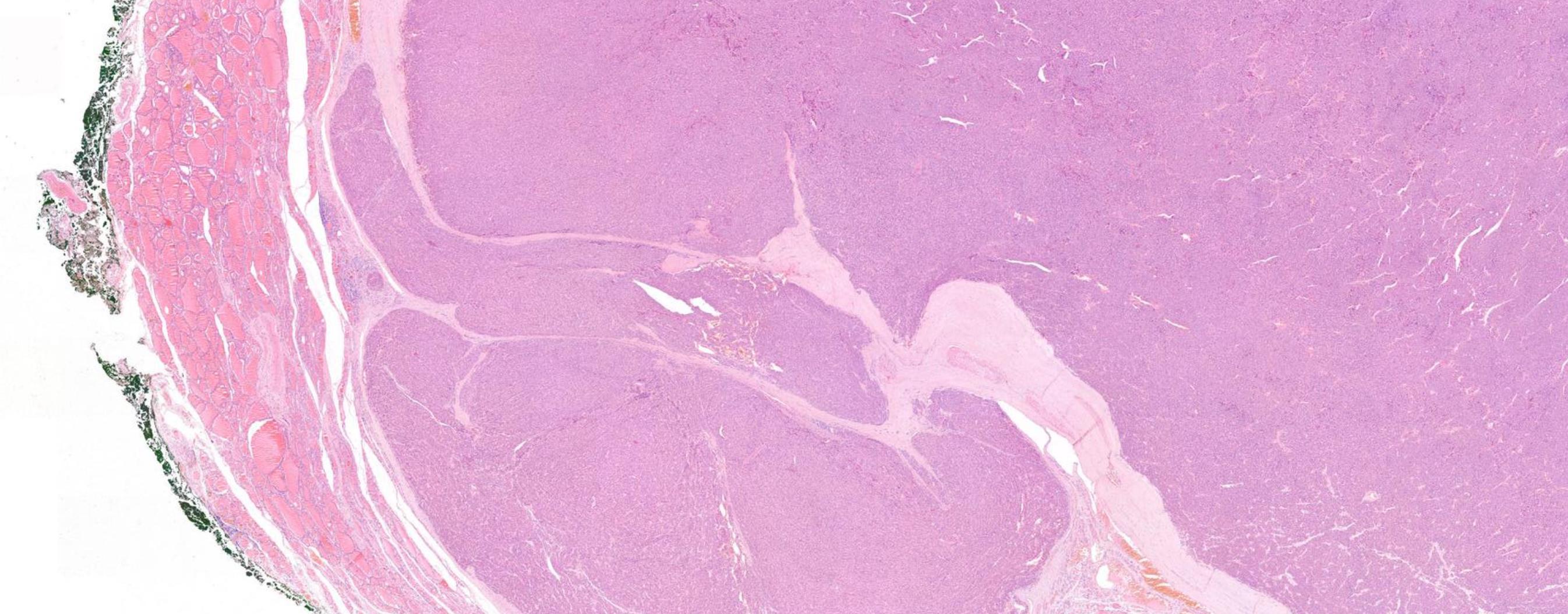
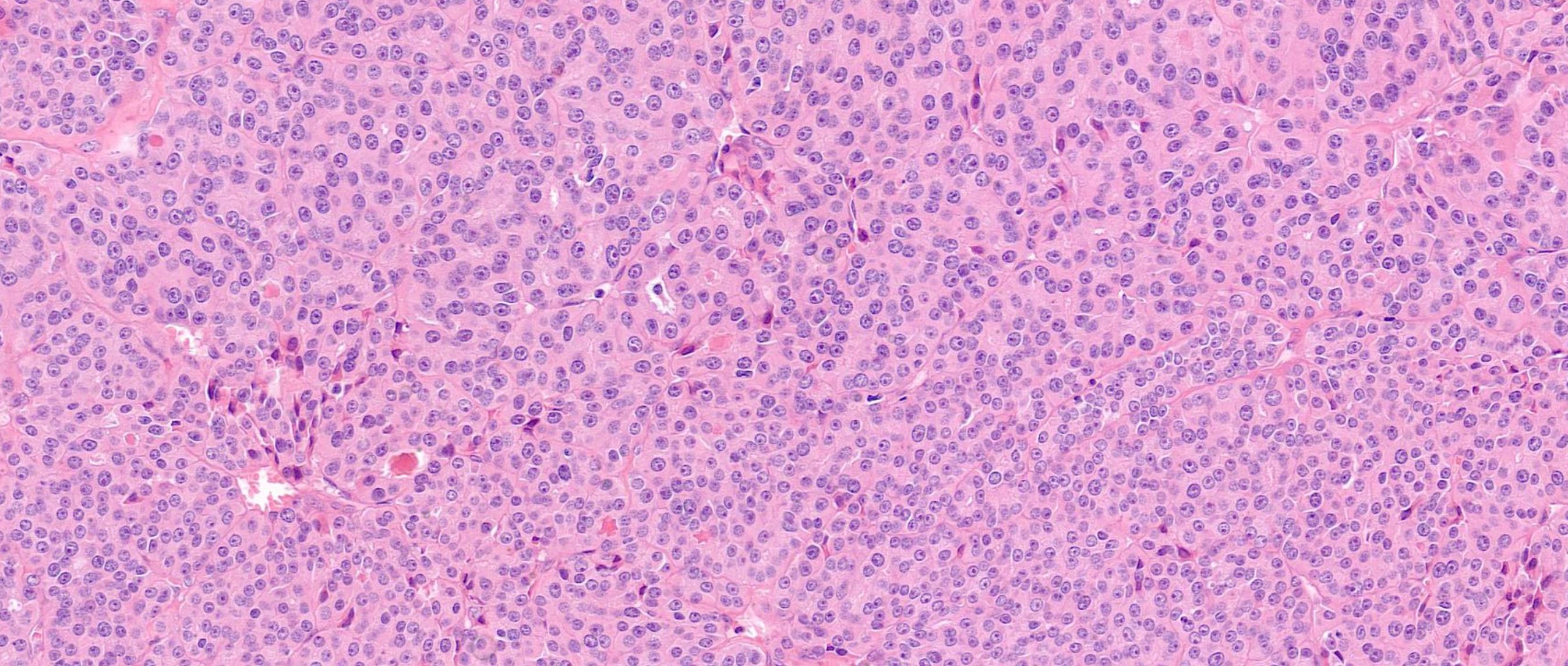
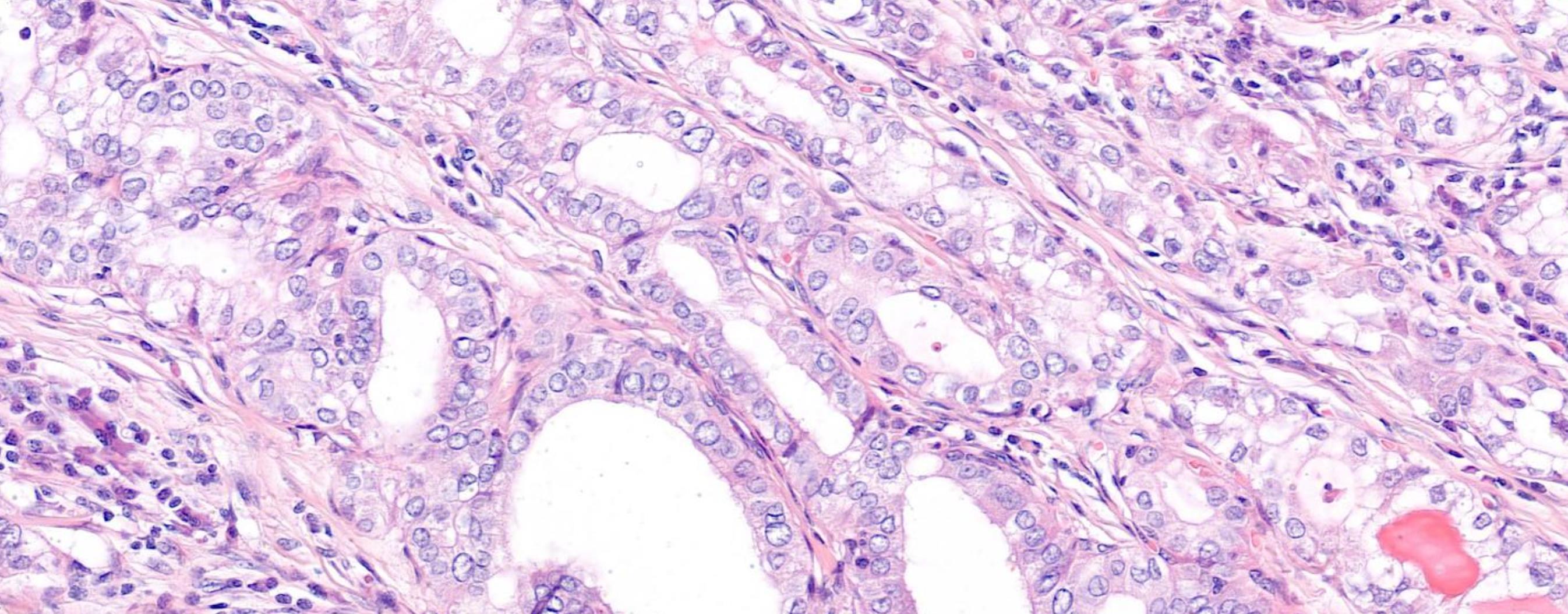
Widely invasive follicular thyroid carcinoma
Most FTC are over 20 mm
The capsule is generally thicker in FTC compared to FA/minimally invasive FTC
A diagnosis of widely invasive FTC is based on tumour grossly invading through the thyroid parenchyma often in a multinodular pattern.
Widely invasive FTC can grossly invades extrathyroidal tissue.
Some of the tumour nodules represent large tumour thrombi within vessels.
Re-visit vascular & capsular invasion


Tumour cells within vascular lumina unassociated with thrombus, and tumour cells underlying intact endothelium could represent “pseudoinvasion” given the fenestrated endothelial network of endocrine organs.
Invasion of tumour cells through a vessel wall as well as thrombus formation in association with tumour>over 1 /3 cases had distant metastases
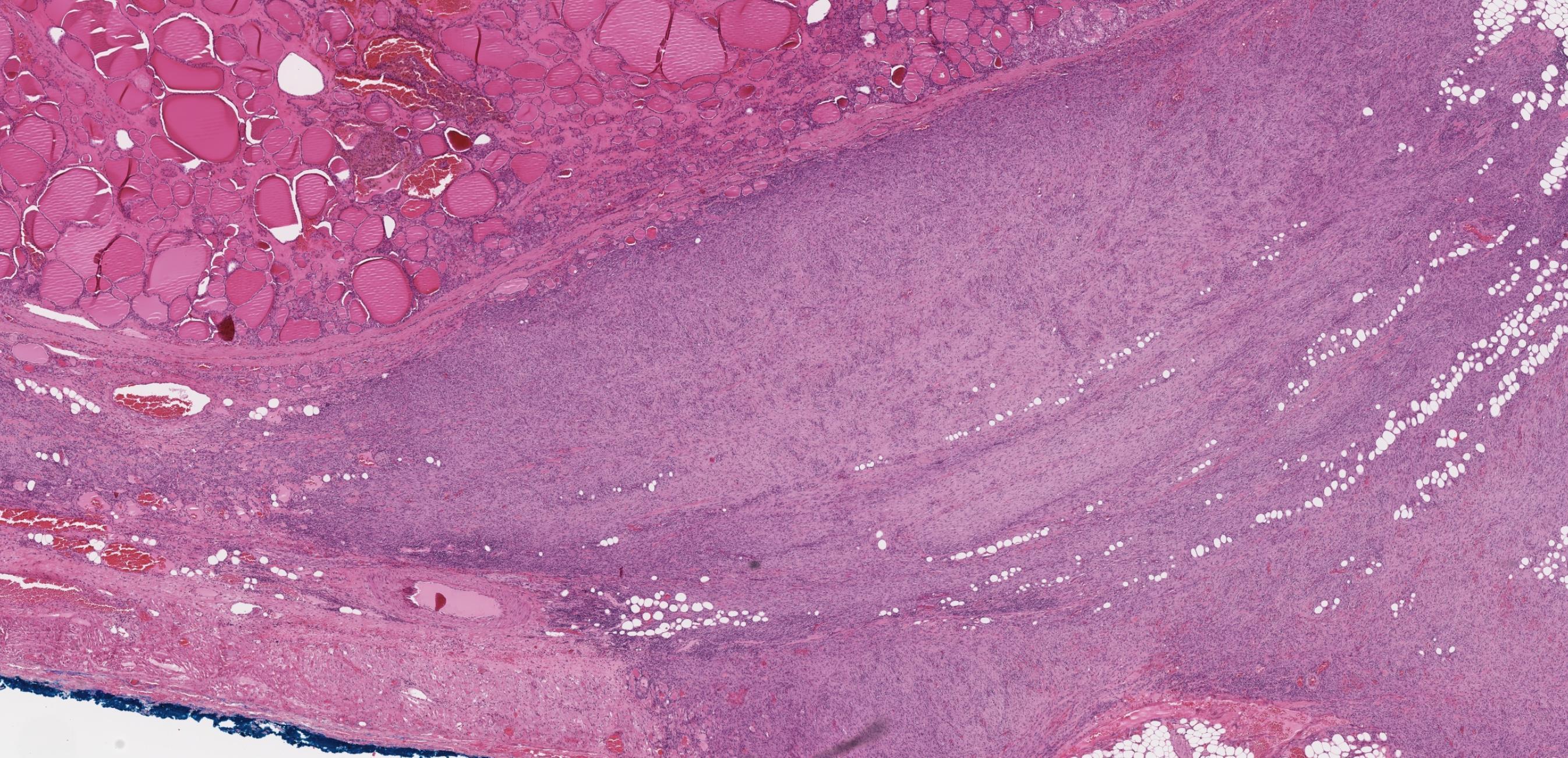
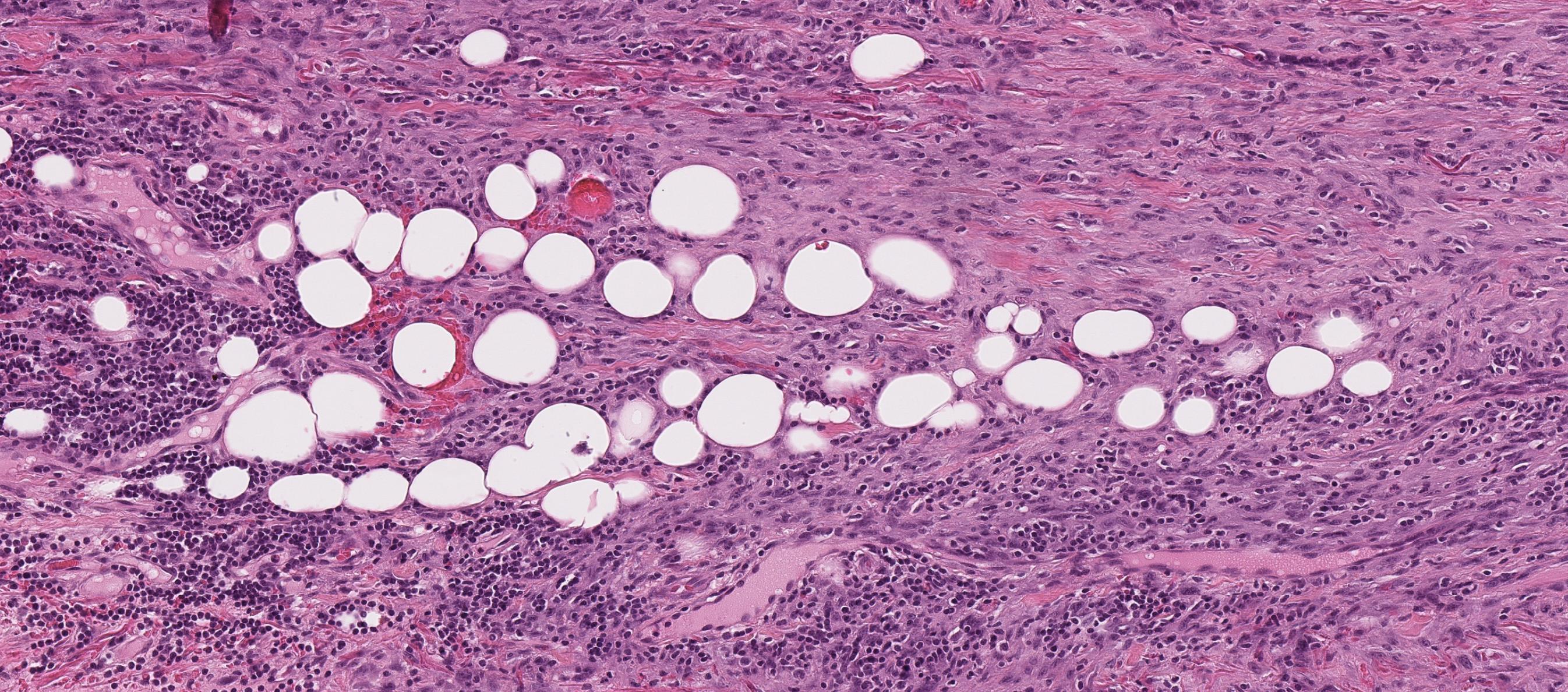
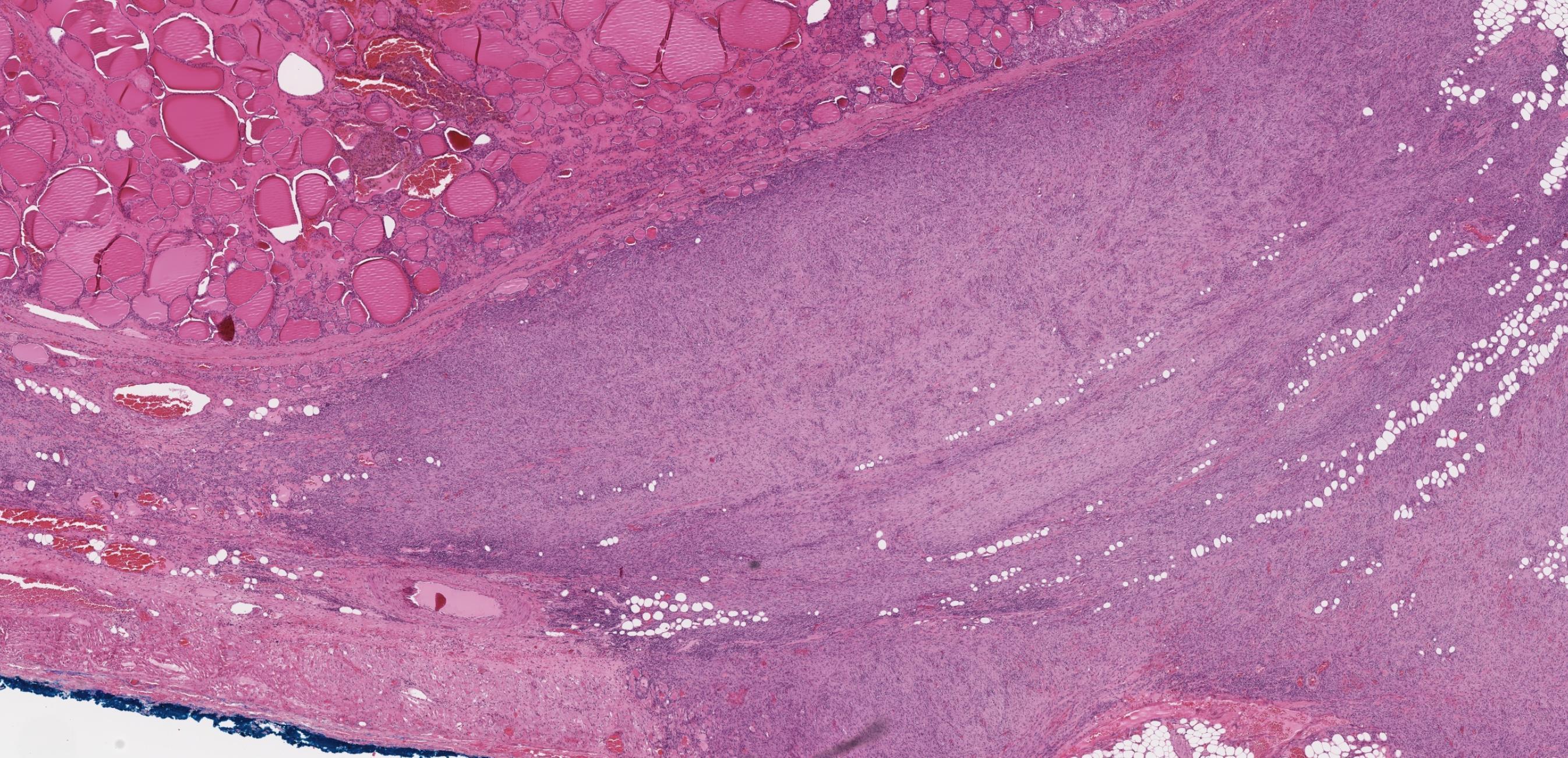
Case 6
32-year-old Female, Right thyroid lobectomy.




Case 6 Diagnosis
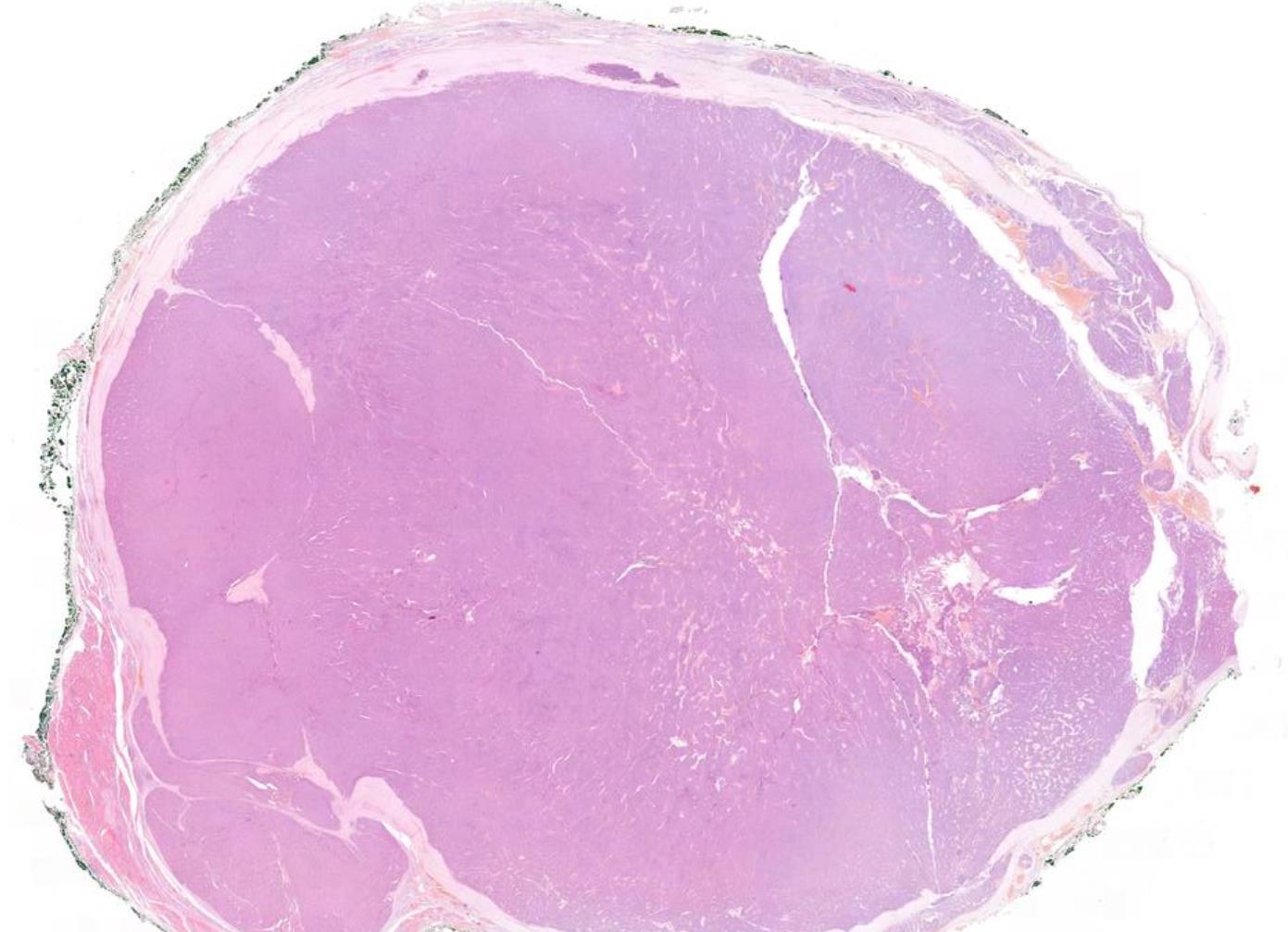
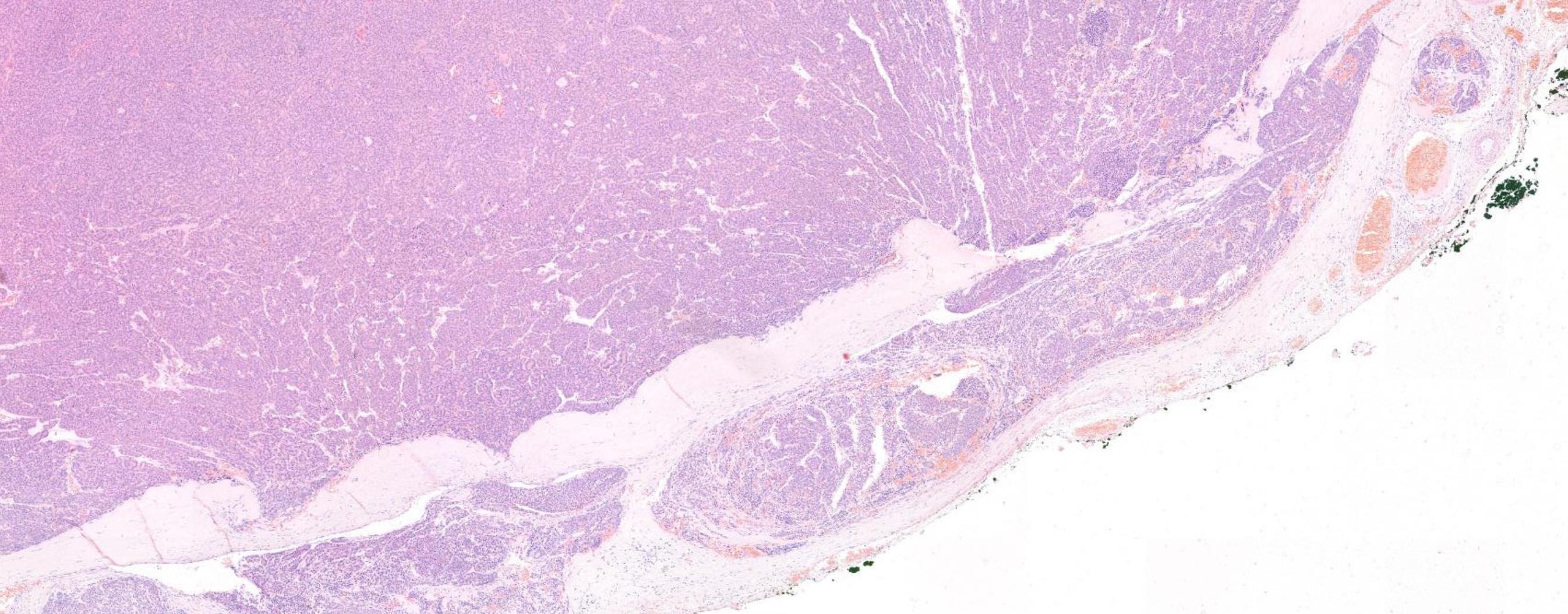
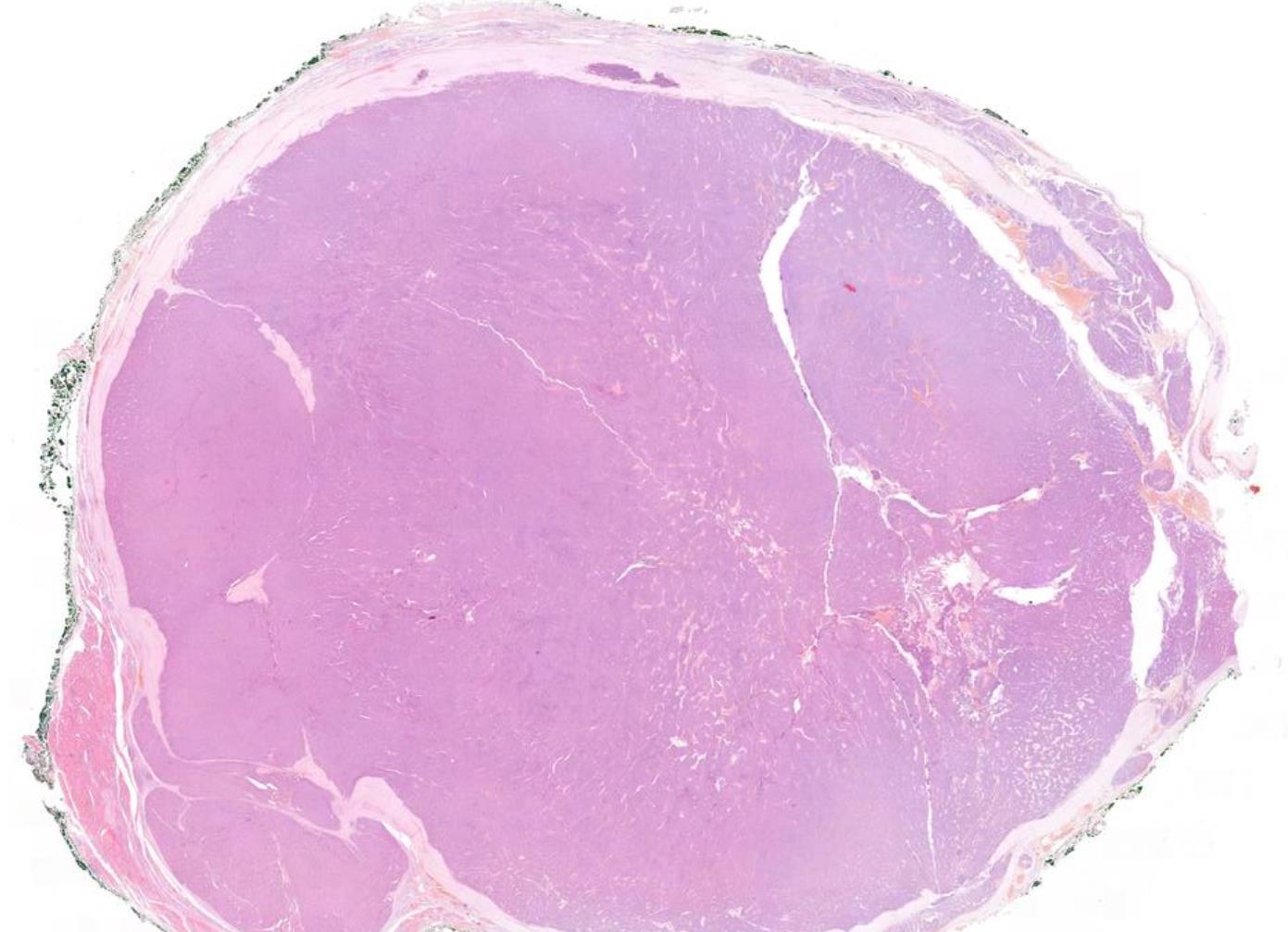
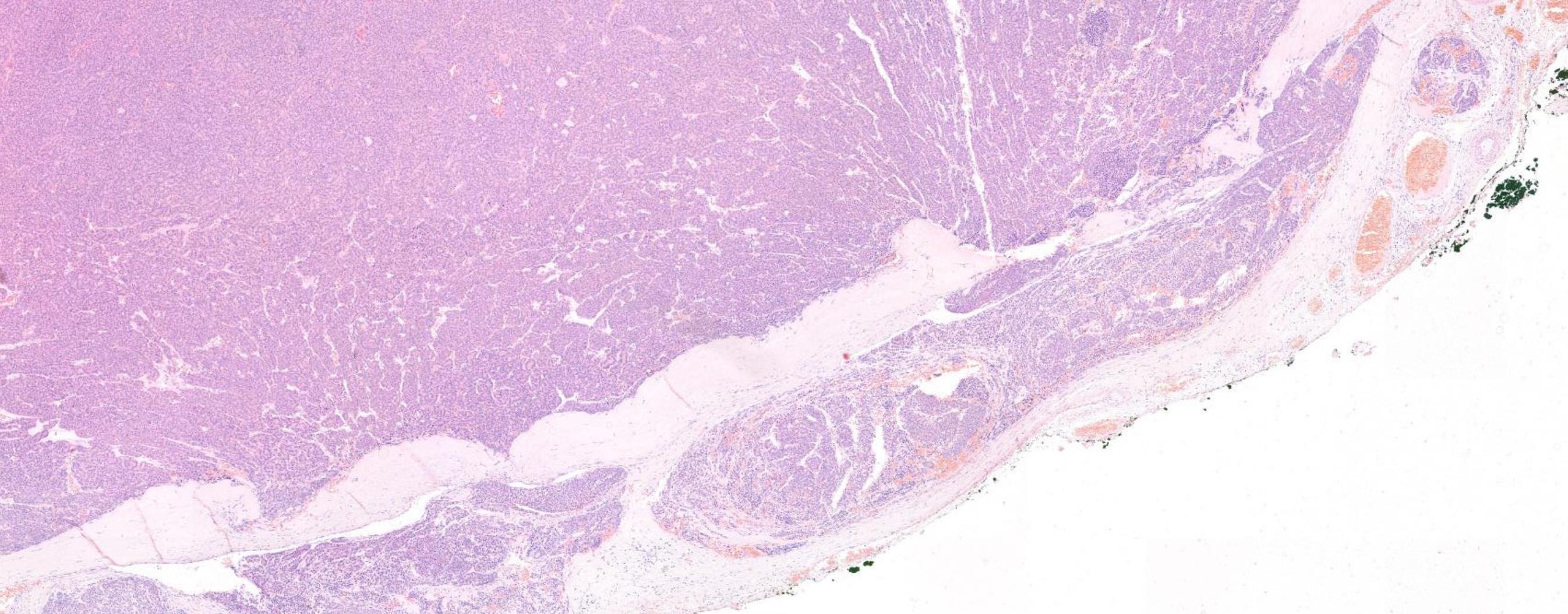
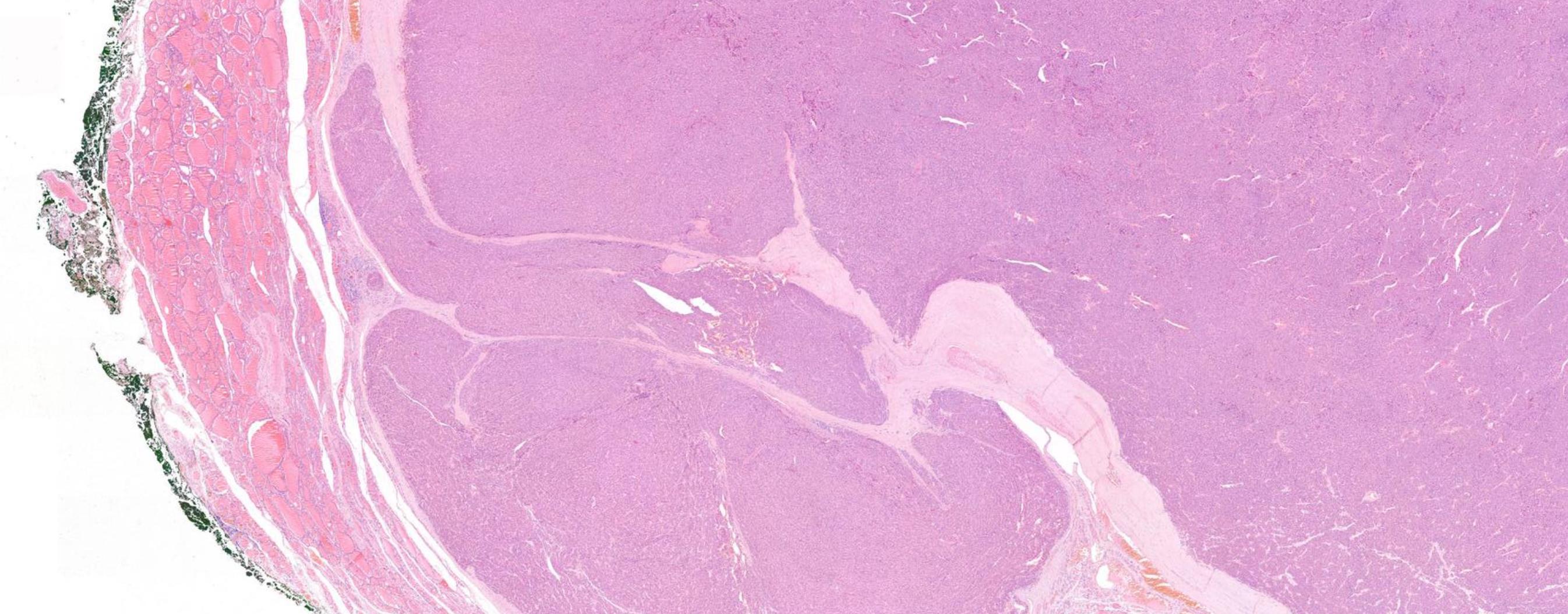
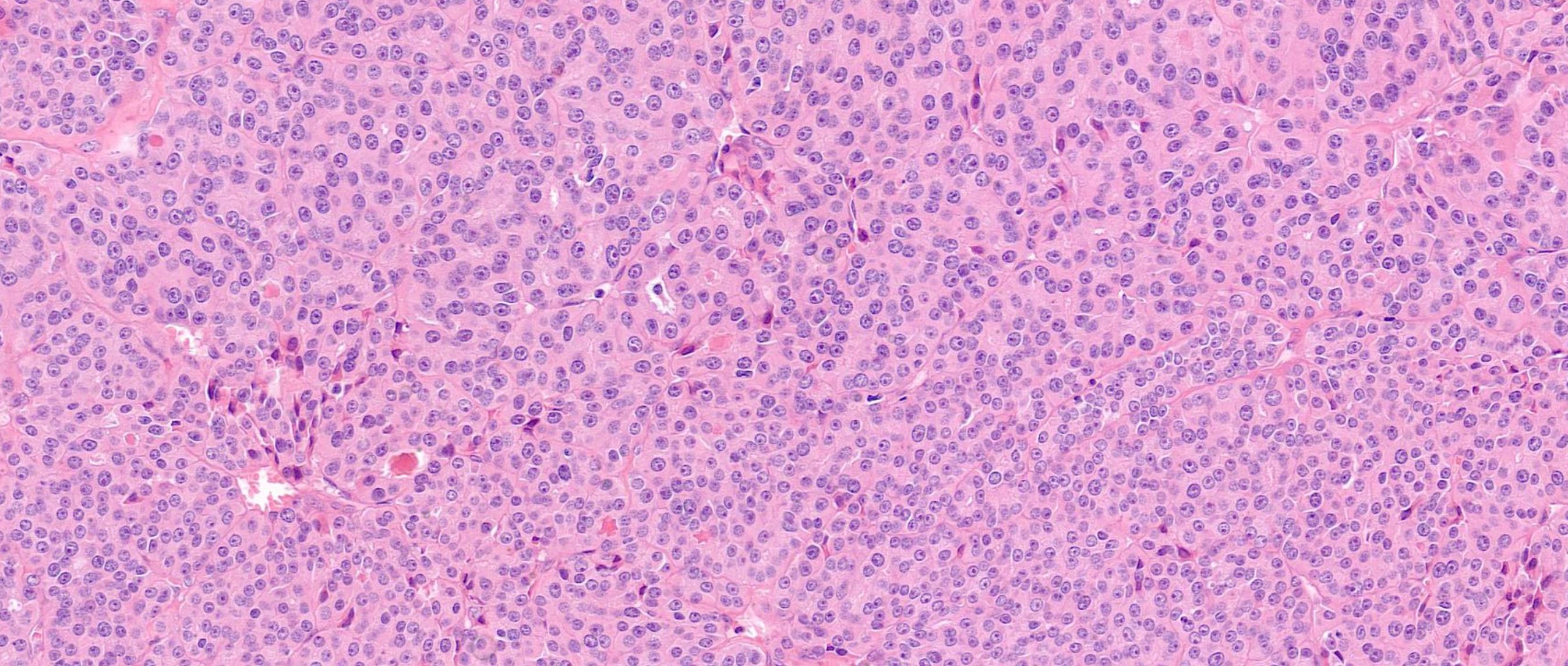
Consistent with parathyroid carcinoma
Discussion Differential diagnoses • Parathyroid adenoma with post-biopsy reactive changes • Secondary/tertiary parathyroid hyperplasia with high proliferative activity, fibrosis • Atypical parathyroid tumour • Parathyromatosis • Sporadic • HPT-JT syndrome • Familial isolated hyperparathyroidism • Most cases CDC73 mutations (CDC73 encodes for parafibromin)
Parathyromatosis ?? • Parathyroid tissue growth around site of a former surgery due to implantation of lesional parathyroid tissue • Sometimes indistinguishable from parathyroid carcinoma Atypical parathyroid tumours • Coagulative tumour necrosis, atypical mitotic figure, or loss of parafibromin may represent parathyroid carcinomas. • Perform parafibromin immunohistochemistry -parafibromin deficient atypical parathyroid tumours have an increased risk of recurrence or metachronous disease in other glands, and would warrant long term follow-up
Case 7 59-year-old
Male, Left thyroid lobectomy.



Case 7 Diagnosis
Papillary thyroid carcioma with tall cell areas
>30%
Discussion •
tall cell component • BRAF V600E mutation (100%) • TERT mutation (22%)
Molecular genetics
Figure 1. Stepwise dediffeent iat ion of fol licul ar cel l-derived thyr oi d cancer .
It h ld b k t i i d th t t ll th ti ft h d i ll di i i t

Case 8
Female 51 years Thy 3a left hemithyroid.



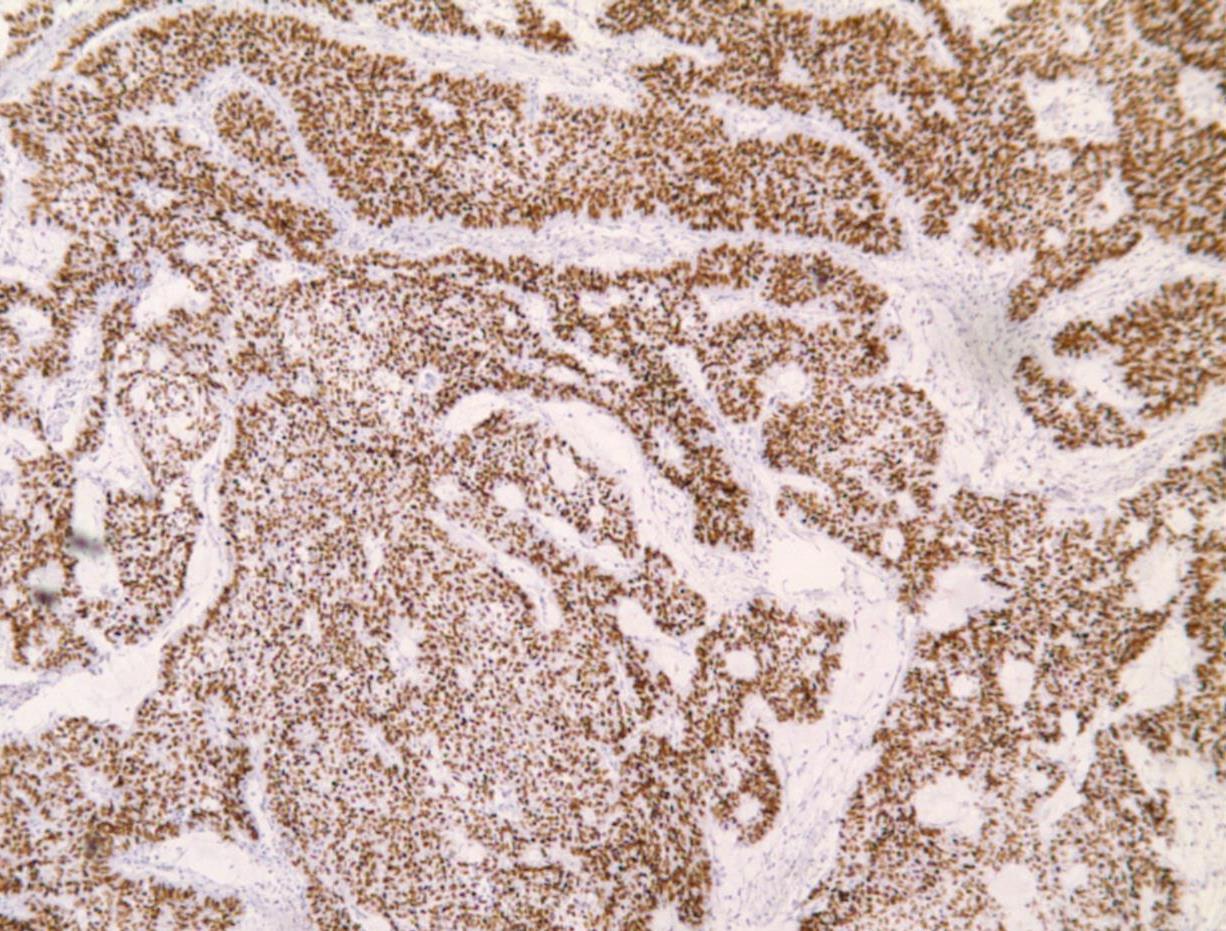
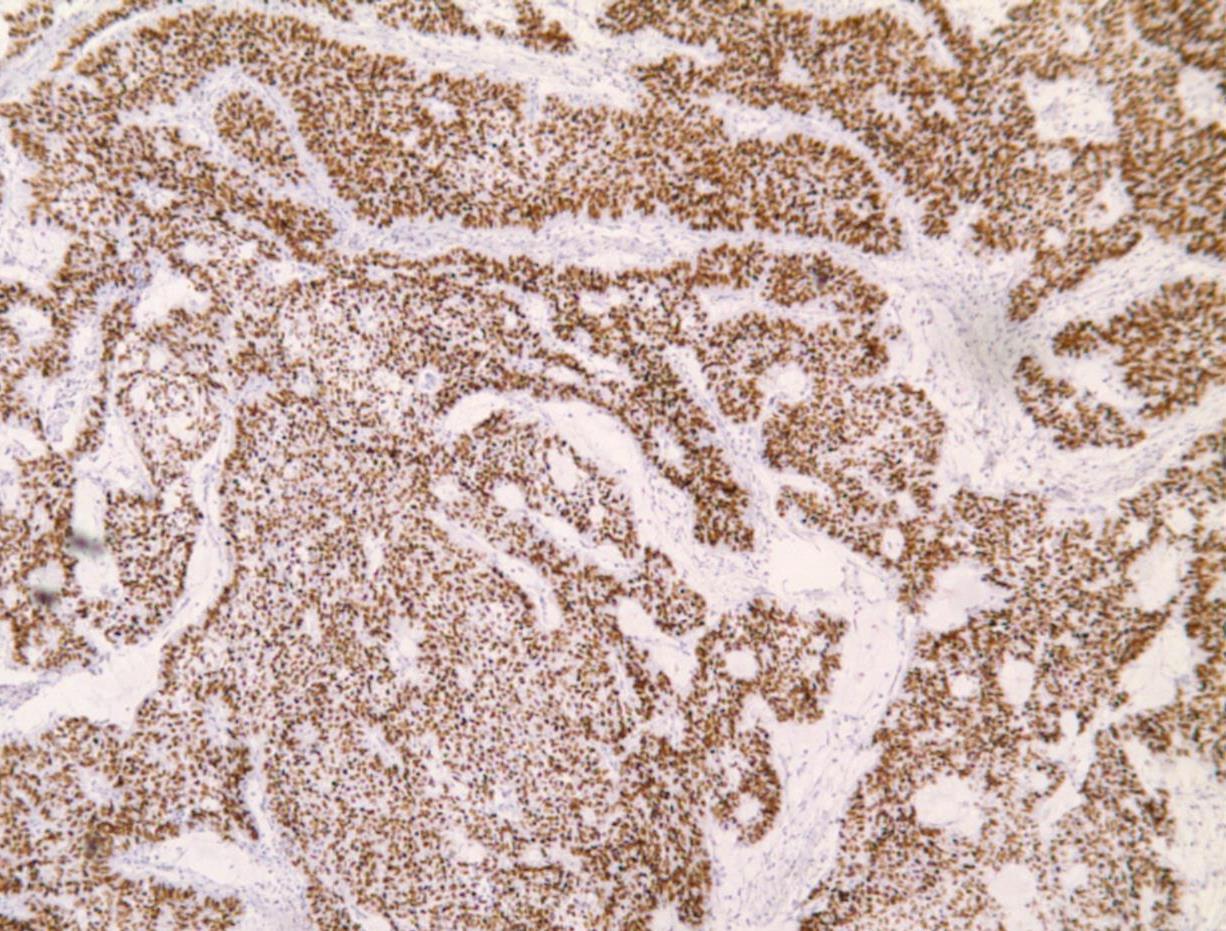
Case 8 Diagnosis
Poorly differentiated thyroid carcinoma arising possibly in a columnar cell variant of Papillary thyroid carcinoma
Discussion-Follicular-derived carcinomas, high-grade Subtypes • Poorly differentiated thyroid carcinoma (PDTC)- Insular carcinoma • Differentiated high-grade thyroid carcinoma (DHGTC) Turin consensus criteria for PDTC (i) presence of a solid/trabecular/insular pattern of growth in a tumour diagnosed as malignant based on invasive properties; (ii) absence of conventional nuclear features of papillary carcinoma; (iii) presence of at least one of the following: convoluted nuclei, mitotic count ≥ 3 per 2 mm2 , tumour necrosis DHGTC- ≥ 5 mitosis per 2 mm2 in hot spot + tumour necrosis, at least partially preserved normal tumour histology and immunoprofile
Immunoprofile • Positive for keratins, thyroglobulin, TTF1, and PAX8 • Thyroglobulin expression is typically reduced
• Ki67/MIB-1 usually 10-30%
and focal in poorly differentiated areas often with a peculiar dot-like paranuclear pattern.
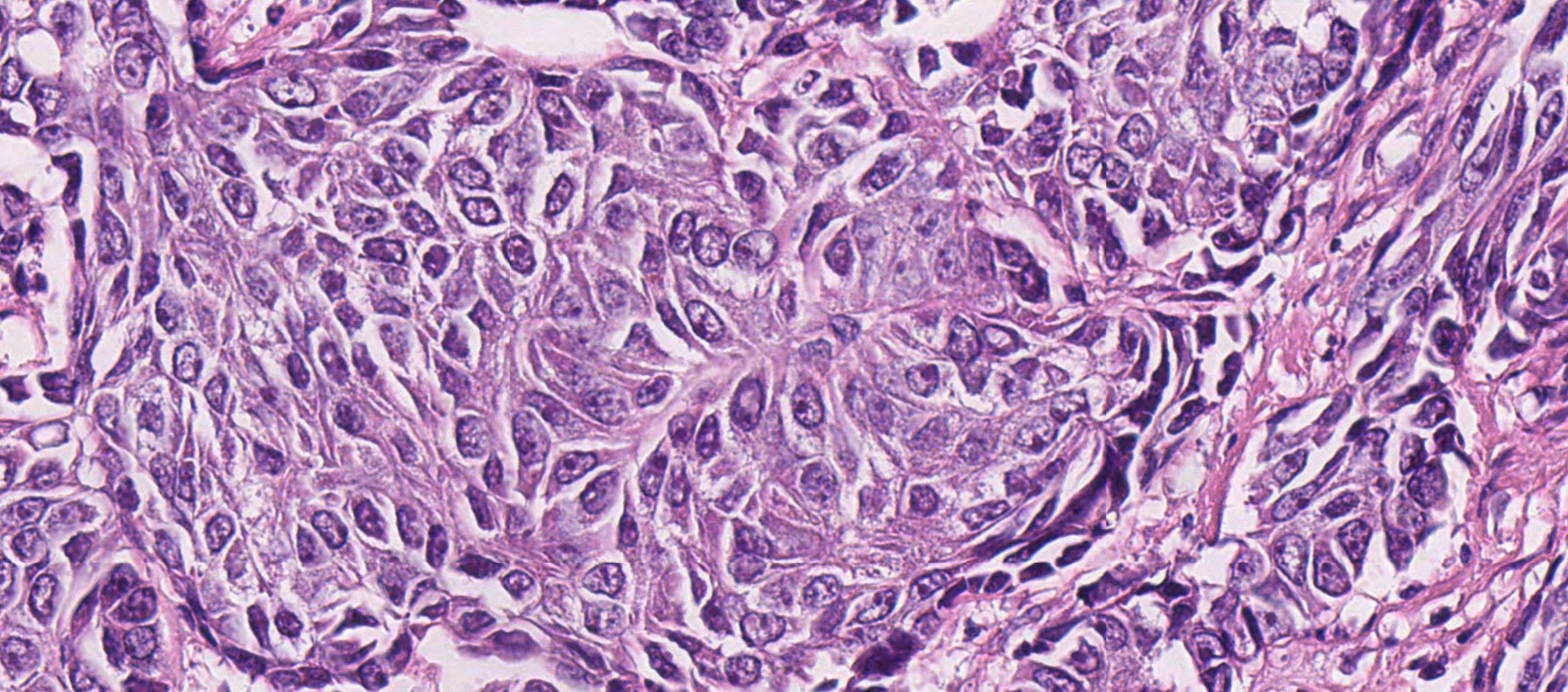
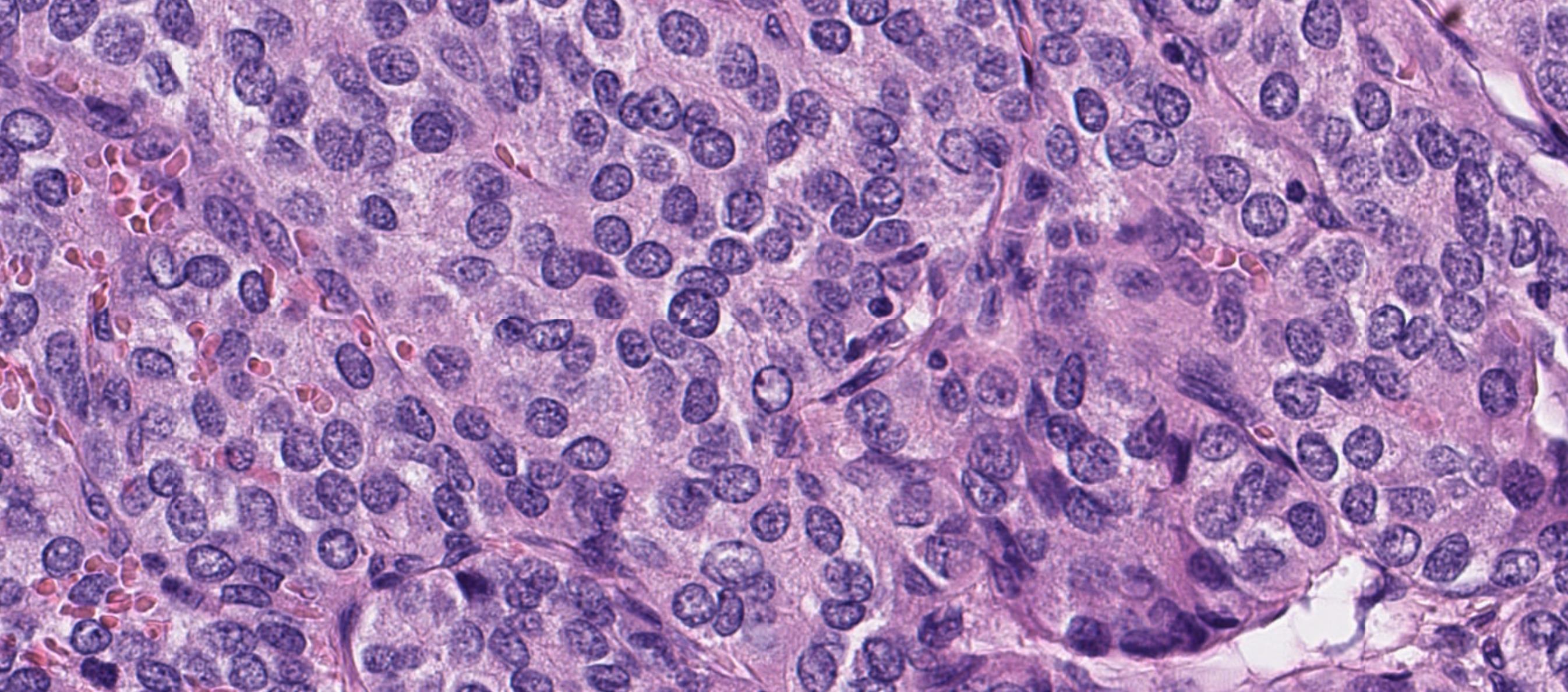
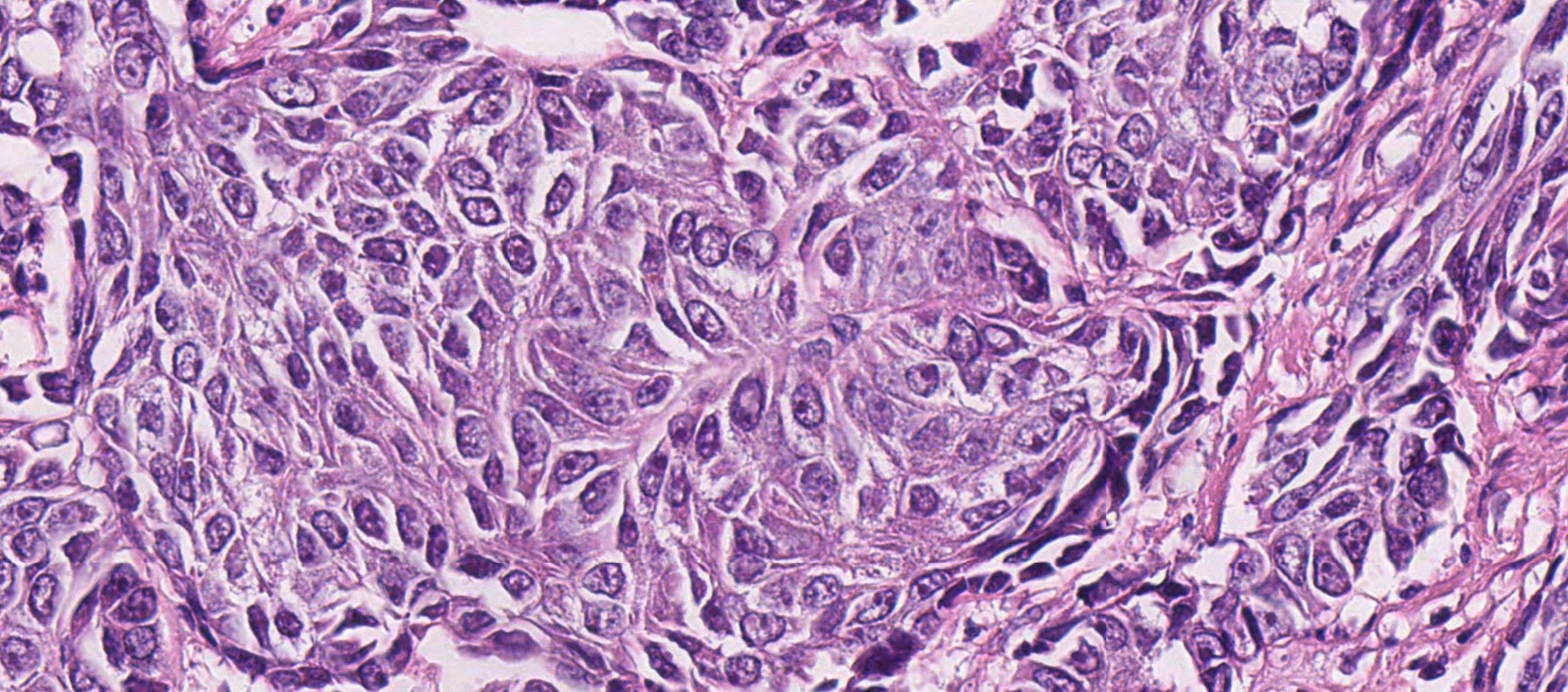
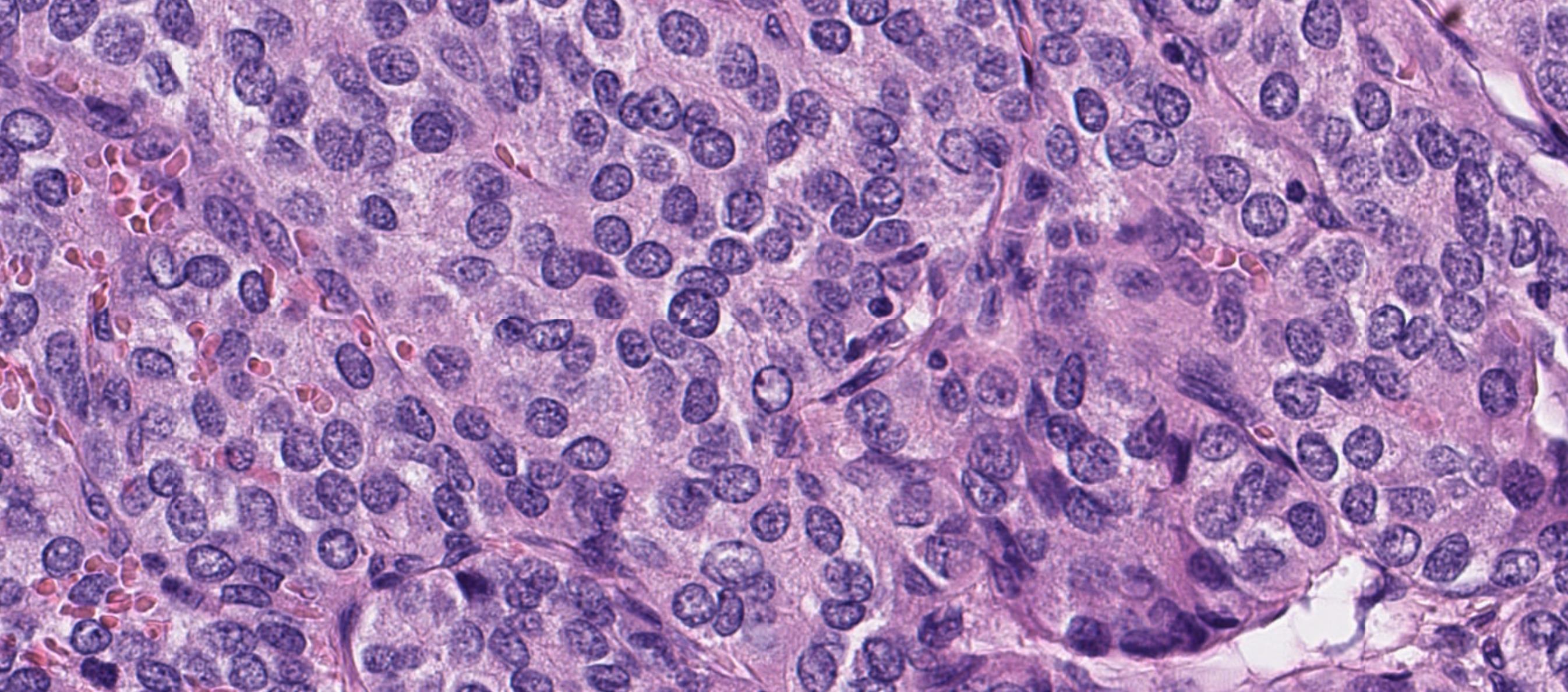
Case 9
Female, elderly. Thyroid, U3, THY3a.





Case 9 Diagnosis
Anaplastic thyroid carcinoma
Immunoprofile • ATC usually shows some cytokeratin expression (75% ) • A minor subset of cases focally express TTF1. • Thyroglobulin is almost always negative with very rare cases focally expressing in epithelioid cells • PAX8 is positive in half of ATCs • p53 is expressed in >50% cases • Ki-67 proliferative rate is usually high
Differential diagnoses
• Sarcoma (synovial sarcoma, malignant peripheral nerve sheath tumour, angiosarcoma, leiomyosarcoma and rhabdomyosarcoma) • melanoma; • medullary thyroid carcinoma; • mucoepidermoid carcinoma; sclerosing mucoepidermoid carcinoma with eosinophilia; • Riedel thyroiditis; • NUT carcinoma; • intrathyroid epithelial thymoma • spindle epithelial tumour with thymus-like differentiation.
Molecular genetics
Figure 1. Stepwise dediffeent iat ion of fol licul ar cel l-derived thyr oi d cancer .

It h ld b k t i i d th t t ll th ti ft h d i ll di i i t
RAS (10-50%) and BRAF (10-50%) mutations are early molecular events. TP53 (40-80%) and TERT (30-75%) promoter mutations
Case 10
Male 66 years, Compressive Goitre. 89g thyroid with ill-defined, yellowish haemorrhagic and fleshy nodule, 65mm..




PAX-8

TTF1

PTH
Case 10 Diagnosis
Metastatic clear cell renal cell carcinoma
Case 11
Female 66 years Total thyroidectomy, 62mm tumour on cut surface.



Case 11 Diagnosis
Papillary thyroid carcinoma, solid variant
• Common in children and has been reported in >30% of children following the Chernobyl accident
• All or nearly all of a tumour not belonging to any of the variants has a solid, trabecular, or nested (insular) appearance.
• presence of solid, trabecular or nested growth pattern in >50% of tumour mass
• Because of its growth pattern, ST-PTC should not be mistaken for aggressive high grade follicular cell derived thyroid carcinoma.
Points
• ST-PTC lacks tumour necrosis or high mitotic rate • RET/PTC rearrangement (43%)
Case 12
Female 45 years Total thyroidectomy and bilateral neck dissection.







Case 12 Diagnosis
Papillary thyroid carcinoma, metastatic, in a background of granulomatous lymphadenitis
TNM 8 staging of thyroid tumours


WHO 5th Edition (2022)
Thyroid tumours

Borderline tumours-2017 WHO
Introduction of borderline tumours



NIFTP
NIFTP is in essence a follicular adenoma with PTC nuclear features



Hyalinizing trabecular tumour (HTT) • Rare benign follicular neoplasm characterized by thick trabeculae and cells with nuclear elements shared with PTC • Interlobular DPAS positive hyaline material • TTF1+,TTG+, calcitonin neg, • Mib1 monoclonal antibody against Ki67membranous stain+
• No BRAF mutations or
were identified in HTT. 2019- GLIS fusions found in 100% of HTT especially PAX8-GLIS3 No BRAF, RAS, RET/PTC found in HTT GLIS3 not found in over 100 papillary carcinomas used in this study
Is HTT a type of PTC?
RAS mutations