ALL ABOUT ACCESSIBILTY

Founded in 2015, Rochester Accessible Adventures has given hundreds of people with disabilities access to healthy recreation. Find out how they do it.

MEET MATHEW DEVINE, O.D
President of Monroe Cpunty Medical Society talks about how he rose to the top spot at MCMS and about his new position as regional dean at Lake Erie College of Osteopathic Medicine. P. 4

Physician Laura Petrescu quit her job with Rochester Regional Health to start her own membership-based practice. She says hers is the first of its type in Rochester. P.

Legalization of marijuana and implications for health

SOLO PRACTICE
9
P. 14 INSIDE GVHEALTHNEWS.COM OCTOBER 2022 • ISSUE 206 FREE









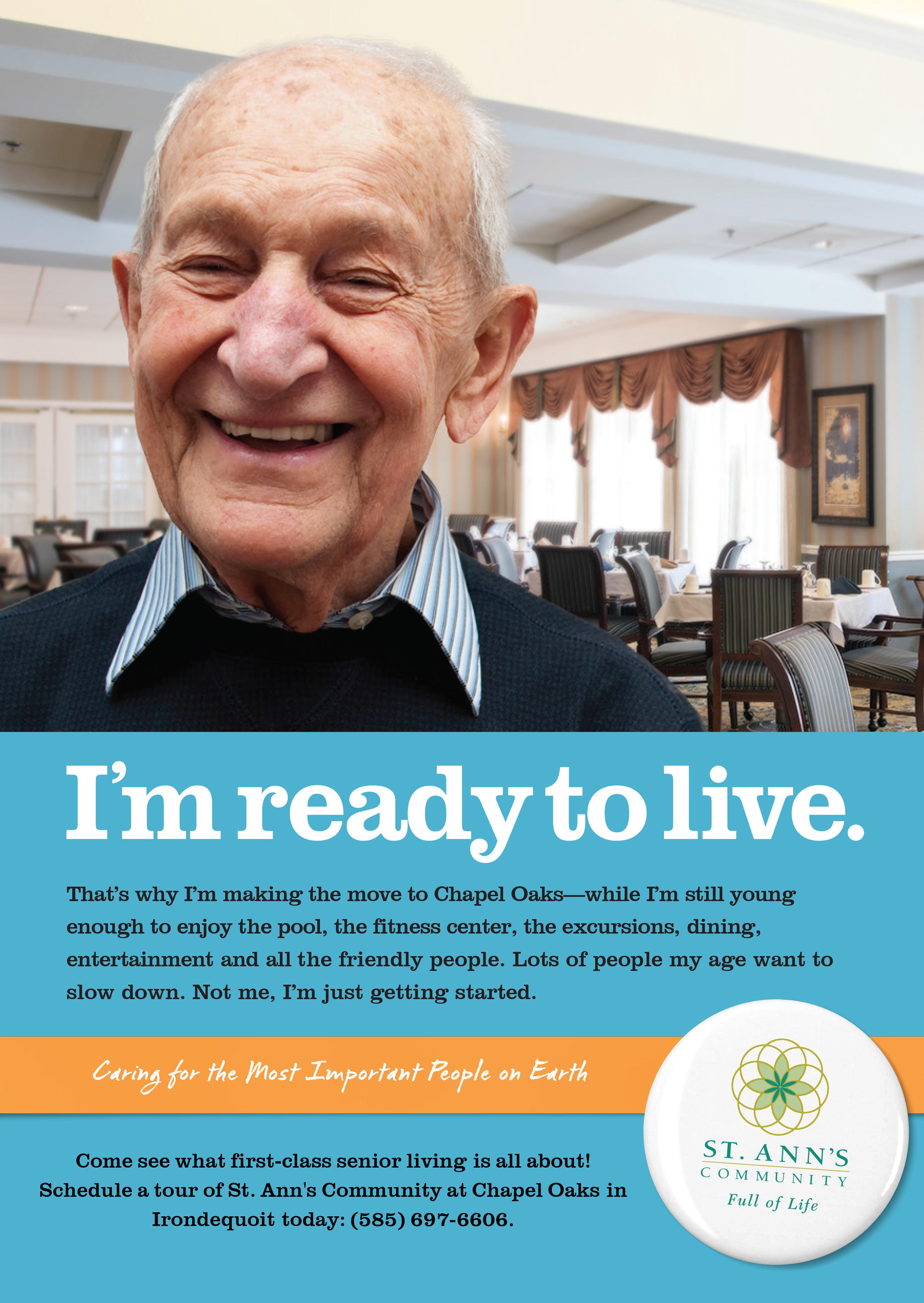
Page 2 • IN GOOD HEALTH – Rochester / Genesee Valley Healthcare Newspaper • October 2022 at Cherry Ridgeat Cherry Ridge at Cherry Ridge St. Ann’s Community at Cherry Ridge Senior living at its finest! Call today for a tour of our beautiful Webster campus, including: • Independent Living Cottages & Apartments • Assisted Living • Memory Care • Skilled Nursing 585.697.6702 900 Cherry Ridge Boulevard Webster, NY 14580 stannscommunity.com (585) 288-0890 www.rcrclinical.com Advancing Medicine. Changing Lives.
health care right at home.
The Physician House Calls practice has a team of medical professionals who provide medical care in your home. This includes routine visits, urgent visits, medication review, and care coordination with a 24-hour on call service.

A safe and secure option for adults over age 65.
If you are in need of a new primary care provider, or would like to find out more about the practice, call (585) 244-5993 or visit jslphysicianhousecalls.org.
A service of Jewish Senior Life
I can sleep well at night knowing that my dad is being taken care of by Physician House Calls.
Family Member of a Physician House Calls patient
Phys ician Hou s e Call s
Prima ry G eriatric Care at Ho me
October 2022 • IN GOOD HEALTH – Rochester / Genesee Valley Healthcare Newspaper • Page 3
Meet Your Doctor
By Chris Motola
Mathew J. Devine, D.O.
even some nursing positions. We’re hopeful we can fill those to try to get back to all the things we were doing beforehand.
Q: You’re a D.O. as opposed to an M.D. How does your osteopathic training af fect your approach to leadership and your administrative philosophy, if it does?
Dogs Have Died After Licking a Common Chemotherapy Cream, FDA Warns

Q: How did you become president of the Monroe County Medical Society?
Your
dog may like to lick your hand or face, but if you’re using a chemother apy cream that treats certain skin conditions, you should not allow it, the U.S. Food and Drug Administration advises.
The medication fluorouracil is fatal to dogs when ingested. People who keep the cream on a nightstand or counter should put it out of reach of their dogs, who may ingest it if they chew the container, the FDA advised.
The agency has received reports involving dogs that were exposed to the cream; all the dogs have died.
Although the FDA has not yet received any reports of fluorouracil poisoning in cats or other pets, it recommends that this drug be kept away from all pets.
The cream is used to treat some types of skin cancers and a condition called actinic keratosis, which can lead to skin cancer. It may also be used to treat warts in children. Occasionally it is used to treat certain cancers in horses.
It can be dispersed as an in jection, or as a topical cream or a topical solution that’s applied on the skin. Brand names include Efudex, Carac, Tolak and Fluo roplex.
Pets who ingest fluorouracil may show signs of poisoning within 30 minutes. These signs can include vomiting, shaking, seizures, difficulty breathing and diarrhea.
Affected dogs can die in as little as six to 12 hours.
If you suspect your pet has consumed fluorouracil, imme diately get veterinary care and bring the container of cream with you. Also contact your vet or an emergency vet hospital immediately even if your pet just licks the area where you applied fluorouracil, and definitely call if your pet chews the container and consumes some of the fluo rouracil.
A: I’d been working at an aca demic practice in the University of Rochester Medical Center since my residence and fellowship. Over the years, I took on a quality officer role — there’s a great quality collabora tive that’s been happening out of the medical society since the late ‘90s where they go through and update a lot of guidelines on many differ ent conditions. I’d been involved with them on a couple of reviews of different disease states. I was really impressed with the process and the organization. Typically, a lot of the hospital systems don’t have docs involved as much with the medical society, because a lot of the benefits related to malpractice are covered by the hospital systems. But I felt like it provides a huge benefit for someone with my interests. And I said I’d like to continue to be involved. I got into the process of being elected in as secretary and working my way up. My time got pushed ahead because our current would-be president had to resign to be part of her practice. So I had to pivot and make that work. We’ve all had to make a lot of sub stantial changes since this has come out.
Q: Coming in late, what do you want to be able to hand off to your suc cessor?
A: I’m more or less doing a fresh term. I just didn’t have that one year to really learn the ropes the same. I was the treasurer to the secretary, but I didn’t get that one year to go to the advocacy days and be front and center at the major leadership meetings. That said, I’m picking it up. The past-presi dent has been super helpful. Back to your point, I think the things we’re continu ing to work on is con tinuing to grow the medical society. Continue to share the
story of the value it brings members. And also to really focus in on rein vigorating those quality initiatives and work committees and other important work that we were doing pre-COVID that took a backseat during the pandemic. We’re trying to really reengage the different health systems and insurers. Within that there’s a more attention-focused project that we’re working on with adolescents and doing a better job of screening them for depression and anxiety and getting them the resourc es to address that. That’s a segment of our community that’s really suf fered from increased depression and anxiety. And, quite frankly, it needed work even before the pandemic. So it made sense to leverage that.
Q: How close to “normal” do you think we are now? Not in terms of the pathol ogy of COVID-19 itself, but in terms of the system functioning at pre-pandem ic levels?
A: That’s a really good ques tion. I would say the answer is we’re in more of a new normal in that we’re never going to return to the way things were. For example, telemedicine using video visits and updates to our technology that allow us to use that as a way to reach our patients. It really exponentially increased in a way that needed to happen during the pandemic. Now there continue to be these waves of strains. My practice and other practices have ways that we’re continuing to work through the strains, but we’re doing all of the other things that need to happen within an inpatient and outpatient setting, in hospital systems. So I think we’ve sort of had to pivot, alter resources.
The normalcy part has been difficult mostly because of the ongoing inability to fill all of our team po sitions. So there’s been that Great Resignation where there con tinues to be a lot of openings for medical assis tants, sec retarial and
A: I am; thank you for noticing. I’d like to think I bring that holis tic approach into administrative work. I try to look at all aspects of problems and situations in a way to keep a mind-body connection in mind. I think, really, I can attribute my training to being very comfort able hands-on medicine but also just being comfortable being with peo ple, asking questions and listening, taking the time to understand things. It’s something I’ve always tried to take outside the exam room and into other roles I’ve had.
Q: How do you balance this role with your practice?
A: I’m actually in the process of finishing my current role in my practice. I’m taking on a dean role at the Lake Erie College of Osteopath ic Medicine [in Erie, Pennsylvania] at the end of November. I’ll still be located regionally. I’ll be a regional dean. So I am undergoing a fairly big transition, saying goodbye to pa tients and preparing to take oversight of upwards of 150 third- and fourthyear osteopathic medical students.
Q: Are D.O. schools graduating more students to keep up with demand for doctors?

A: Last I checked less than 10% of all trained U.S. physicians are osteopaths. But there are pockets of the country that are becoming more heavy. I think with the satellite campus in Elmira, and the mother ship campus in Erie, it’s picking up in the region. And you also see a lot of osteopathic physicians coming up through M.D. residencies. I’m excited about this group of students because a lot of them are New York state residents, and many are even from the Finger Lakes. So they’re choosing to stay local for their schooling and residencies, so I think you’re going to start seeing a lot more osteopaths in Upstate New York over the next five to 10 years as they complete their training.
Lifelines
Name: Mathew J. Devine, D.O. Position: Medical director at Highland Family Medicine; president of the Monroe County Medical Society; associate professor in the department of family medicine at the University of Rochester; soon to be regional dean at Lake Erie College of Osteopathic Medicine in Erie, Pennsylvania

Hometown: Rochester, NY
Education: Medical degree from Philadelphia College of Osteopathic Medicine (2004); residency in family medicine at Highland Hospital (2005 –2008); fellowship at Highland Hospital (2008–2009)
Affiliations: Strong Memorial Hospital; Highland Hospital
Organizations: Society of Teachers of Family Medicine; American Academy of Family Physicians; Medical Society of the State of New York; Monroe County Medical Society
Family: Wife, two daughters
Hobbies: Hiking, swimming, biking, skiing
President of Monroe County Medical Society finishing his practice at Highland to become a regional dean at Lake Erie College of Osteopathic Medicine
Page 4 • IN GOOD HEALTH – Rochester / Genesee Valley Healthcare Newspaper • October 2022
NEUROPATHY?
DISCOVER THE LATEST BREAKTHROUGH THAT CAN RELIEVE PAIN AND NUMBNESS CAUSED BY NEUROPATHY
If you are experiencing debilitating pain, numbness and tingling, they are likely caused by Neuropathy. Peripheral Neuropathy is a common condition that affects 20 million Americans and once identified, can be successfully treated without the use of drugs and surgery.

HOW DO YOU KNOW IF YOU HAVE PERIPHERAL NERVE DAMAGE?

The following symptoms may start gradually and then worsen:
• Numbness
• Diabetic nerve pain
• Sharp, electric-like pain
• Burning or tingling
• Muscle weakness
• Difficulty sleeping from leg or foot discomfort
• Sensitivity to touch

• Pain when walking
If you suffer from any of these symptoms, call us today at (585) 670-0020!
“WHEN I SAW THE AD, I TOOK A LEAP OF FAITH...”
and started using the home equipment. I went from 81% sensory liss in my feet, which is almost permanent nerve damage to 21-24% in just 4 months. My feet were always cold. Pins and needles all over. Now I’m feeling better! - Marsha
“We’ve had the privilege of helping hundreds of people in our community relieve their pain without the use of drugs or surgery.”
Seminar Topic
Drug-free Treatment for Peripheral Neuropathy
You will discover:
• What REALLY causes peripheral neuropathy
• Dangers associated with medications typically prescribed for peripheral neuropathy
• How to stop nerve damage before the effects are irreversible
• How our revolutionary protocol provides outstanding results for sufferers of peripheral neuropathy
Riddle Wellness
October 2022 • IN GOOD HEALTH – Rochester / Genesee Valley Healthcare Newspaper • Page 5
SEMINAR DETAILS CALL FOR DATE & TIME LOCATION: Riddle Wellness 435 West Commercial St., Suite 4 East Rochester, NY 14445 FREE! SEATING IS LIMITED Call Today to Make Your Reservation (585) 670-0020 RIDDLEWELLNESS.COM
Neuropathy Treatment Breakthroughs Non-Surgical,
How the Inflation Reduction Act Will Lower Your Drug Costs
By Jim Miller
$7,050 in 2022, you enter catastrophic coverage but are still responsible for 5% of your prescription drug costs, with no limit.
But in 2024, people with Part D coverage will no longer be responsi ble for any out-of-pocket drug costs once they enter catastrophic cover age. This is significant for seniors who use expensive medications for conditions like cancer or multiple sclerosis.
drugs will be capped at $2,000 per year. This will be a major savings for the more than 1.5 million beneficia ries who currently spend more than $2,000 out-of-pocket each year.
2026
The
climate, tax and health care bill known as the Inflation Reduction Act that was passed by Congress and signed into law by President Biden in August includes significant improvements to the Medicare program that will kick in over the next few years.
These changes will lower pre scription drug prices for millions of seniors by allowing the government to negotiate drug prices for the first time and capping seniors’ out-ofpocket drug costs at $2,000 annually. Some other popular changes will include free vaccinations, lower insu lin costs and expanded subsidies for lower income seniors.
Here is a breakdown of the changes to expect in Medicare and when they will roll out.
2023
Starting this January, all vac cines covered under Medicare Part D, including the shingles vaccine, will be free to beneficiaries. And the skyrocketing cost of insulin will be capped at $35 per month. This will be a significant saving for the more than 3 million Medicare enrollees who currently use insulin to control their diabetes.
Also starting in 2023, drug mak ers will be penalized in the form of rebates that they would be forced to pay to the government if they impose price increases that exceed general inflation.
2024
Cost sharing for catastrophic coverage in Part D will be eliminat ed. Under the current Part D benefit, once your out-of-pocket costs reach
Also starting in 2024 through 2029, Part D premiums will not be allowed to grow faster than 6% per year.
And for lower-income Medicare beneficiaries, eligibility for the Part D Low Income Subsidy (also known as Extra Help) will be expanded to 150% of the federal poverty level, from today’s limit of 135%. This change will mean about 500,000 more seniors will qualify for financial assistance to help pay some or all of their prescription drug premiums and deductibles.
2025
One of the biggest cost reduction measures for Medicare beneficiaries will begin in 2025 when out-of-pock et spending on Part D prescription
When Medicare’s Part D pro gram was enacted in 2003, negotiat ing lower drug prices was forbidden. But because of the Inflation Reduc tion Act, starting in 2026 Medicare will be empowered to begin nego tiating prices with drug companies for 10 of the most expensive drugs covered under Part D. In 2027 and 2028, 15 drugs would be eligible for negotiations and in 2029 and sub sequent years, 20 drugs would be chosen.
And, in addition to all the Medi care improvements, the Inflation Re duction Act also extends the Afford able Care Act (Obamacare) premium subsidies for three years that have helped millions of Americans gain coverage before they’re eligible for Medicare.
Jim Miller is the author of Savvy Senior column, which runs every month in In Good Health newspaper.
HealthcareinaMinute
By George W. Chapman
Hospitals Facing Shaky Finances. Outlook: From ‘Neutral’ to ‘Deteriorating’
After slowly climbing back from the devastation caused by the pandemic, July median hospital operating margins plunged a staggering 64% from June op erating margins, according to industry consultants Kaufman Hall.
Its survey of 900 hospitals revealed an average year-to-date margin of negative 1%.
KH attributes this trend to lower outpatient volumes, more acute and expensive inpatient cases and an end to COVID-19 relief and PPP from the federal government.
Financial services company Fitch Ratings has reduced its hospital out look from “neutral” to “deteriorat ing.” Shaky finances are the driving force behind hospital mergers and
Accountable Care Organizations
Typically, an ACO is a partner ship between physicians and one or more hospitals to participate in the Medicare Shared Savings Program (MSSP). The goal is to cooperate in exceeding quality benchmarks and reducing per capita cost benchmarks established in advance by Medicare. ACOs submit their bills, physician and hospital, to Medicare per usual. ACOs that reduce per capita costs will share in the savings with Medi care. If ACO costs per capita go up, the ACO must return money to Medicare. The MSSP is designed to encourage and reward the delivery of care by a cooperative of physicians
acquisitions. Not price fixing as skep tics have speculated. To survive and deliver care to their respective com munities, hospitals must be allowed to freely explore opportunities to increase fragile operating margins via shared over head, operating savings, and improved credit without onerous regulato ry oversight. At stake, in many cases, is the survival of smaller rural hospitals. While mergers might save hospitals, there could be a point where there are diminishing returns. For example, the 20-hospital Cleve land Clinic lost just over $1 billion the first half of 2022. While $628 million is attributed to investment losses, the system still lost close to $400 million on operations.
and hospitals working as a team to exceed common goals. An “every man for himself” model won’t work. And it never has. Medicare has learned that the more primary care physicians in the ACO, the better at reducing per capita costs. This makes sense. Effective primary care deliv ery can reduce illness, unnecessary referrals to specialists and overall hospitalization. Last year, 99% of ACOs beat quality benchmarks and 58% beat per capita costs. ACOs beat per capita costs benchmarks by $3.6 billion.
Apple Watch Study
In 2018, the FDA approved the
Apple watch for EKGs. Who would have thought? Now, the NIH has granted $37 million to researchers at Northwestern and Johns Hopkins (and others) to study it. By moni toring atrial fibrillation, the watch can prevent strokes and reduce the amount of expensive blood thinners patients with Afib are receiving. Afib affects 2.5 million to 5 million of us. That is predicted to be 12 million by 2030. The seven-year study will involve 5,400 people with Afib. Some in the study will continue to receive the standard regimen of continuous expensive blood thinners to prevent strokes. Others will have their Afib monitored by the watch and receive targeted blood thinner therapy only when at risk of a stroke.
No More Free Vax
Congress has discontinued fund ing the government’s COVID-19 vac cine program effective next year. That means it will no longer purchase the vaccine from manufacturers and distribute it for free. It has turned the keys over to Big Pharma. Pfizer and Moderna must be licking their chops. (Is this what it took for Big Pharma to finally agree to negotiate some drug prices?) The government has already dropped free home testing due to lack of funds. Both drug giants claim that with the feds out of the way, they can be “more competitive” in an open market versus a govern ment-controlled contract market. Both also claim they can now focus on “branded education” which is in their area of expertise. It remains to be seen if Medicare and commercial insurers will charge for the vaccine or make it available for free.
ACA Adds Navigators
The Biden administration and Congress has approved close to $100
million in funding for ACA naviga tors who help people select an insur ance that fits their needs and budget. The increased funding should add 1,500 new navigators. The ACA has been a widely successful program now insuring more than 36 million people. The uninsured rate is at an all-time low below 8%. Open enroll ment begins Nov. 1. To hamstring the ACA, the Trump administration slashed navigator funding to $10 million.
Medicare Advantage Plans

Just about half of all Medicare beneficiaries, or 28 million, are now covered by a commercially operated advantage plan. Sixty-six percent of the beneficiaries are individually covered; 18% are insured via employ er or union; and 16% are enrolled through special programs. Market shares for the largest carriers are Humana 28%; United 18%; and BCBS 14%. Cigna, Centene and Kaiser com bine for 24% market share.
Advantage plans are Part C Medicare. They draw members away from traditional Medicare by offering perks such as dental, vision, OTC drugs, transportation and even meals. Unlike traditional indemnity Medicare, most advantage plans require preauthorization for certain procedures.
George W. Chapman is a healthcare busi ness consultant who works exclusively with physicians, hos pitals and healthcare organizations. He op erates GW Chapman Consulting based in Syracuse. Email him at gwc@gwchapman consulting.com.

Page 6 • IN GOOD HEALTH – Rochester / Genesee Valley Healthcare Newspaper • October 2022
How Many Steps a Day (and How Fast) to Lengthen Your Life?
There’s
an easy way to reduce your risk for dementia, heart disease and cancer: Start walk ing.
Getting in those recommended 10,000 steps a day makes a real differ ence, new research affirms, but even fewer will pay big dividends. No matter how many you log, however, step up your pace for the biggest benefit.

For every 2,000 steps you log, up to about 10,000 a day, your risk of early death drops by between 8% and 11%, researchers found.
“So, 10,000 steps maximizes the chances of getting all these benefits, but also for inactive people who can’t engage in so many steps — any steps have benefits — every step counts,” said lead researcher Borja del Pozo Cruz of the Center for Active and Healthy Aging at the University of Southern Denmark in Odense.

And, he added, it’s never too late to get going.
“The range of participants that we had in the study went from 40 to 79,” Cruz said. “That means that any person can actually get the benefits.”
This study, however, doesn’t prove that walking 10,000 steps a day has a health benefit, only that number of steps is associated with a reduction in heart disease, cancer, dementia and early death.
Cruz said that the power of the study lies in its large size and in researchers’ ability to isolate walking from other exercises.
For the greatest health benefit, the sweet spot was 9,800 steps a day, which slashed dementia risk by 40%. But just 3,800 steps lowered it by 25%, the investigators found.
Over and above the number of steps, walking at a brisker pace — about 80 steps a minute — brought the greatest reduction in dementia, heart disease, cancer and premature death, Cruz noted.
But all that walking doesn’t have to happen all at once. It can be spread out during the day, the researchers said.
The study drew from data from 78,500 adults in the United Kingdom who were followed for a median sev en years, meaning half were followed even longer. They wore wrist sensors that measured their physical activity over seven days.
Cruz said that wearable devices like Apple watches and Fitbits that track steps can be useful if you use them faithfully.
“What we know about those devices is in the beginning people take them very seriously, but after a while,” use tapers off, he said. “We also know that you need to create the habit.”
A
newspaper published by Local News, Inc.
33,500 copies throughout more than 1,500 high-traffic locations.


October 2022 • IN GOOD HEALTH – Rochester / Genesee Valley Healthcare Newspaper • Page 7
monthly
Distribution:
In Good Health is published 12 times a year by Local News, Inc. © 2022 by Local News, Inc. All rights reserved. P.O. Box 525, Victor NY 14564. Phone: 585-421-8109 • Email: Editor@GVhealthnews.com SERVING MONROE AND ONTARIO COUNTIES Editor & Publisher: Wagner Dotto Writers: Deborah J. Sergeant, Chris Motola, George Chapman, Gwenn Voelcker, Anne Palumbo , Mike Costanza, John Addyman, Rekha Shrivastava, Jennifer Faringer, Ernst Lamothe Jr. • Advertising: Anne Westcott (585-421-8109) • Linda Covington (585-750-7051) • Layout & Design: Angel Campos-Toro • Office Manager: Ahme Cruz No material may be reproduced in whole or in part from this publication without the express written permission of the publisher. The information in this publication is intended to complement—not to take the place of—the recommendations of your health provider. Consult your physician before making major changes in your lifestyle or health care regimen. Age in Place While keeping your independent and active lifestyle. Evergreen Place Senior Living Community We‘re Local. We’re Passionate We Care. Call for a tour of our beautiful newly renovated community. Small pets welcome! 585-637-3140 www.pegasusseniorliving.com/evergreen-place/ 90 West Avenue, Brockport, NY 14420 See How Our Passionate Services Change Families Lives SHARING the SECRETS OPEN MEETING – on NURSING HOMES RESIDENT RIGHTS * LAWS & REGULATIONS * ADVOCATING for RIGHTS October 20, 2022 2:00 – 3:00PM presented by ELDER JUSTICE COMMITTEE of METRO JUSTICE Pittsford Library – Fisher Meeting Room 24 State Street, Pittsford, NY 14534 ejcevent@elderjusticecommittee.org (585)-397-3537
By Gwenn Voelckers
October: The Perfect Time to Turn Over a New Leaf
from time to time, I don’t recom mend it as a steady diet.
In my experience, there’s no better way to start your day than to wake up early. In the early morning’s peace and quiet, there is glorious time to reflect and feel gratitude. I use this important “me time” to meditate and set my intentions for my day.
As the morning brightens, my energy grows, as does my apprecia tion for the precious day ahead me.
I’ve discovered a few simple and manageable ways to bring people into my world and into my home. One way is to organize a gathering around a TV show or series — yes, around the TV, as odd as that might sound.
For years, I invited my single friends over to watch “Downton Abbey” with me on Sunday nights. I provided the soup and salad; they provided the good company.
Fall
is such a special time of year. For me, it means all good things: relaxing in front of a cozy fire, making pumpkin soup on Sunday afternoons, donning my well-worn leather jacket for long walks and turning my attention to all those inside projects I neglected over the summer.
The brilliant colors, autumnal aromas and industriousness that arrive with the falling leaves really appeal to me. But this hasn’t always been the case.
After my divorce, the month of October left me feeling melancholy. I missed sharing the beauty of the season with a special someone. And I missed the sunshine as daylight waned.
Nostalgia and wistfulness would creep in, and I just wanted to retreat into myself. For those who live alone, the month of October has unique challenges.
Not one to wallow in a “poor is me” state of mind, I began to develop and employ some strategies to rekin dle my love of the fall season. It can be a great time to mix it up, get busy and expand your horizons.
Below are elements of my annual fall game plan. Take a look and see if one or more of these suggestions might not add a little color to your life palette this fall:
■ Tackle indoor projects. Fall is a great time to accomplish all those
nagging in door projects on your to-do list. I have a long list and I keep it right in front of me — a daily reminder that I have plen ty of home improvements to tackle, both large and small.
Too much idle time is not a friend at any time of year, but it can become downright unfriendly when gray clouds appear and the tempera ture drops. Now is the time to get busy: organize your storage space, do some touch-up painting, update your wardrobe, or clean the garage.
There’s nothing like being pro ductive to beat the autumn blues.
Don’t I know it. I just finished coating my flat-roof porch with a sticky tar sealant. Confession: it was messier than it was fun, but still ... I’m proud of my accomplishment. It lifted my spirits.
■ Get up and get going. Staying ac tive when there’s a chill in the air can be difficult. I can remember many a cold morning when all I wanted to do was hit the snooze button, pull up the covers, and stay in bed.
As nice as sleeping in can be
■ Start moving and enjoy the great outdoors. Fresh air, sunlight and even a gentle rain can be invigorating first thing in the morning. I find a sunrise walk boosts my energy and kickstarts my day. Do I feel like layering up and taking a walk every morning? No. Do I feel better after I make the effort? Yes, without fail.
I love a long solitary walk to clear my head and be mindful. But I also love a walk with my sister Anne or good friend Kate to enjoy their company and avoid the siren’s song of isolation as the days grow short and get colder.
■ Learn something new. Going back to school and fall go hand-inhand. Who among us isn’t reminded of the nervous excitement associated with returning to school in the fall? It’s a great time to expand your intel lectual horizons.
Each fall I identify a new skill or subject to learn. Last year, I re searched how to divide and relocate perennials (my irises and peonies); this fall, I’m signing up to learn French on Duolingo, the free lan guage-learning app.
Continuing education opportuni ties are abundant in this community and online. Check out colleges and universities, community centers, arts and cultural institutions, your local library, and workshop listings for class and workshop offerings.
■ Invite people in. Over the years,
So, what’s your pleasure? Wheth er it’s football, a favorite weekly sitcom, or “Ted Lasso” on Apple TV+ — all of these and other TV shows can become reasons to bring friends and family together. The benefits? You’ll hone your cooking skills (boy, do I now have some great soup reci pes!) and you’ll connect with people you care about.
What better way to enjoy a nice fall evening.
There are so many wonderful and meaningful strategies to enjoy the fall season and to ward off the blues that can sometimes emerge during this changing time of year. But these strategies require effort –conscious, creative effort.
If you are feeling sluggish, lonely, or isolated, try a few of the strategies above. They have stood me in good stead and have reinvigorated my love for the fall season.
If you, too, are ready to turn over a new leaf, October is the perfect time!
Gwenn Voelckers is the founder and facilitator of Alone and Content, empowerment workshops for women and author of “Alone and Content,” a collection of inspiring essays for those who live alone. For information about her workshops, to purchase her book, or invite her to speak, visit www. aloneandcontent.com

One App Is Especially Bad for Teens’ Sleep
sleep outcomes, researchers said.
Many
teens look at screens at bedtime, but some apps are more likely to keep them awake than others, leading to sleep problems.
That’s the upshot of a new study in which researchers found YouTube fans experienced consistent and neg ative effects on sleep. Surprisingly, traditional TV was associated with earlier bedtimes.
“We’ve been seeing teenagers who have sleep problems in our clin ic,” said co-author Michael Gradisar, head of sleep science at Sleep Cycle in Adelaide, Australia. “A lot of them have tried refraining from using technology, and clearly that hasn’t worked for them. Many of them mentioned that they would watch YouTube as they try to fall asleep. They find it entertaining without it
being overly stimulating.”
While many studies have been done on devices, little research has looked at the effects of specific apps on sleep, he said.
“We wanted to learn if there were specific apps that people should avoid, so that they could continue using their devices in a healthy way that didn’t affect sleep,” Gradisar said.
For the study, the researchers asked more than 700 12- to 18-yearolds how much time they spent using technology. That included mobile phones, gaming consoles and TV, as well as apps before going bed and in bed before falling sleeping.
While the study looked at the streaming service Netflix as well as YouTube, YouTube was the only app consistently and negatively related to
For every 15 minutes teens spent watching YouTube, they had a 24% greater chance of getting fewer than seven hours of shuteye. Watching YouTube and using gaming consoles both were associated with greater odds of getting insufficient sleep.
Contrary to the classic advice to keep TV out of the bedroom, tradi tional TV was associated with earlier bedtimes.
Gradisar said that might be because teens don’t interact with a TV in the same way they do with a phone. Instead, they just sit back and watch.
A half-hour in bed using phones, laptops, tablets and watching You Tube delayed lights out by seven to 13 minutes.

The issue with YouTube in partic ular may be that it’s so easy to finish
one video and click on a related one, said physician Alon Avidan, director of the UCLA Sleep Disorders Center.
Even homework done on screens late at night can be harmful, added Avidan, who reviewed the findings.
Watching Netflix was also asso ciated with greater sleepiness during the day.
Gradisar said one takeaway for parents is that not all technology use before bed is bad for their teen. Mom and Dad can also apply the findings to their own sleep health, he said.
“We often recommend that people do their own experiments with their tech use before sleep,”
Gradisar said. “Find something that’s enjoyable so you don’t develop a bad relationship with your bed or bed room. The tech you’re using should be relaxing, but also be aware if it’s controlling your bedtime.”
Practical tips, advice and hope for those who live alone
Page 8 • IN GOOD HEALTH – Rochester / Genesee Valley Healthcare Newspaper • October 2022
Live Alone & Thrive
Doctor Who Made Her Home in America Offers
Refreshing New Approach to Medicine
Physician Laura Petrescu quit her job with Rochester Regional Health to start her own membership-based practice
 By John Addyman
By John Addyman
Physician Laura Petrescu has become a direct primary care physician, in the mold of the doctors some of us remember from a long time ago — doctors who would sit with you and treat you in an un hurried fashion, someone you called by their first name, almost a respect ed neighbor with a stethoscope.
She’s Romanian, coming to America with her software-engineer husband Catalin, who had taken a job in Silicon Valley in 2007.
“When Catalin got the job offer, our son was 18 months, and I said, ‘I’ll go with you.’ I had absolutely no desire or plans to leave Romania,” she said. “I had no idea what it takes to be a doctor in America — I had no clue. I said to him, ‘I’m going to be with you, but I’m going to be a doctor there — whatever it takes. I don’t speak English. But I’m going to be a doctor.’”
For almost two years, Petrescu — who was a doctor in her native Romania — worked her way through board and certification exams, and finally got matched for a residency all the way across the country — at Rochester General. The program director, physician Paul Bernstein said she would become a good chief
resident.
“He was a wonderful mentor for all of us. He told me I would do a wonderful job and I had to trust him, more than I trust myself.”
Catalin had taken a job in Roch ester, too. The Petrescus were ready to settle down here.
“Rochester is very similar to my own hometown, Iasi, [pronounced “YAH-shee”]. The weather is exactly the same — four seasons and snow and beautiful fall. For me, being in Rochester felt a lot like home. Mov ing to Rochester, I felt at peace. I like the community, there are lots of things to do. It’s a really good place to raise a family and I felt comfort able with my small child. I loved the community at Rochester General where I trained.”
She rose through the ranks, joined the teaching faculty, became chief medical resident and spent a busy 14 years in the Rochester Re gional system.
“I worked in patient, outpatient, hospital, surgery, internal medicine — a little bit of everything. At the end of the day, I knew deep down my calling is to be a doctor. I cannot imagine myself doing anything else on the planet.
“But how do you reconcile your time?” she asks. “There are still just 24 hours in a day. How do you manage to put enough time into a career and do a meaningful job and be there for your family and yourself and other things you need to do to be happy?”
Time and substance became big issues for her.
“In primary care you get 15 min utes on the clock to see a patient. Out of those 15 minutes, patients need to check in and check out with the secretary and the nurse, so face-toface time for the doctor – I have five to seven minutes. That is the reality,” she said.
“Primary care has become the gateway of referrals. You have a headache, you go see the neurologist. You have a foot pain, you go see the foot doctor. Or I give you a pill…a pill for every ill. There is no time to sit down and really listen and come up with a plan that makes sense for the patient. I had 25-27 patients to see in a day. It was like a hamster wheel. There is no quality of care in that. It’s not meaningful to me as a physician to feel rushed like that.
“I’m sure it doesn’t feel good on the patient side to be rushed out the door, get out and get a prescription, and go see a different doctor. It’s a lot of wasted time and energy and money because you go see so many specialists for things a primary care physician can do.”
Petrescu started studying some thing that has been around for de cades — direct primary care — where a doctor charges a monthly subscrip tion or membership fee and accepts a limited number of patients to care for. Petrescu said in today’s health care systems, a primary care doc might have 3,000 to 5,000 patients. She feels 300 patients is a much better number to deliver consistent quality care.
“What I’m hoping to offer in this practice is time. I’m not restrict ed by corporate medicine to have
five-minute appointments, and I’m not restricted by insurance compa nies to tell me what box I need to click on the computer for them to reimburse me. I’m just driven by patient care. There’s no middleman rules or restrictions there. That’s the biggest difference in our primary care. I can take 30 minutes, an hour, two hours. My regular appointments are one hour but I always allow for two hours if that’s necessary to really listen and understand what’s going on with the person. We come up with a plan that really makes sense.”
But the final decision to leave corporate medicine and set up her own shop came about after a visit from fate.
“What really triggered me and helped me make that final decision was surprise! surprise! — getting pregnant before menopause. I had my second child.”
After consulting with three attorneys and getting things ironed out with three accountants, Petrescu opened Athena Direct Primary Care in Pittsford on Jan. 3.
She doesn’t have a waiting room — it’s a lovely “meet and greet area” — because she only sees one person at a time, and it’s usually for an hour. There’s virtually no waiting. She hap pily schedules her patients in sameday or next-day appointments.
Patients communicate with her by phone, text, email and through telemedicine video. She is always on call.
In August, a patient texted her from a conference he was attending in Tennessee: he thought he was having a stroke.
“I got on the phone right away to see what was going on,” she related. “I was able to coordinate care and help him and walked him through what he needed to do to get back home safe and sound. I saved him a ton of money and unnecessary stuff that would have otherwise happened. A physician who did not know him or trust him would have sent him to an emergency room. But me knowing him, I managed to get him back to Rochester safe and he was beyond happy.
“This is the kind of service that makes a difference in someone’s life,” she said.
‘What I’m hoping to offer in this practice is time. I’m not restricted by corporate medicine to have five-minute appointments, and I’m not restricted by insurance companies to tell me what box I need to click on the computer for them to reimburse me.
I’m just driven by patient care.’
October 2022 • IN GOOD HEALTH – Rochester / Genesee Valley Healthcare Newspaper • Page 9
When the Body Turns on Itself: Autoimmune Disorders
The bad news? No cures exist for autoimmune conditions
By Deborah Jeanne Sergeant
About 80 autoimmune disor ders exist, depending upon how these conditions are classified.
Although affecting different areas and systems of the body, this group of disorders has a few similar ities.
Some share a few core symp toms, such as fatigue, body aches, fever, swelling, difficulty in focusing, weight fluctuation and skin changes. Most autoimmune conditions present with other specific issues. Some au toimmune conditions inexplicably go into remission and flare up later but in most cases are lifelong.
Medical care and good self-care can usually make living with an autoimmune condition much more comfortable. No cures exist for auto immune conditions.
“The effects of having an auto immune disease extend beyond the physical symptoms, as depression and anxiety frequently co-exist with autoimmune disease,” said Molly Murray, president and CEO of the Autoimmune Association in Clinton Township, Michigan.
“Autoimmune patients can feel stressed from navigating healthcare
coverage and treatments, having to go to frequent medical appointments, and trying to balance their condition with other life responsibilities. They can feel isolated and misunderstood and can grieve the lifestyle they had before their diagnosis. Autoimmune patients should know they are not alone. Mental health providers can provide coping tools, and we encour age everyone to share their stories and connect with other patients,” Murray said.
Some autoimmune conditions are “invisible” or minimized by outsiders.
Crohn’s disease and colitis cause diarrhea, urgency, abdominal pain and cramping, bloody stool, fatigue and weight loss and “it is not just ‘tummy pain’ or diarrhea,” said Becky Johnson Rescola, vice presi dent of education and community engagement at the Crohn’s & Colitis Foundation in New York City. “Many people don’t understand the fatigue, chronic pain and day-to-day accom modations that are part of coping with these diseases.”
The organization operates a chapter in Rochester that serves all of Western New York.
How Hypnosis Can Change Your Life
By Rekha Shrivastava
The definition of hypnosis is a re laxed state of consciousness and focused attention. Hypnosis can be used to help you gain control over undesired behaviors or to help you cope better with anxiety, pain and other issues.
Guided by a trained and certified hypnotist or hypnotherapist, hyp nosis helps you bring about positive changes in your behavior, thoughts, memories and emotions. It’s import ant to know that although you’re more open to suggestion during hypnosis, you don’t lose control over your behavior. You typically remain
aware of what happens during hyp nosis.
Recently, hypnosis has become very popular and even medical practitioners are referring patients to certified hypnosis professionals.
• Post traumatic stress. Hypnosis can help eliminate issues and scars from PTSD. Sessions addressing emotional baggage, negative memo ry release, tuning into emotions, and flashback relaxation help people get over the trauma, move on, and find inner peace.
• Phobias and anxiety. Hypno sis can be an effective method for
Alopecia areata is another example of an autoimmune condi tion. Sherry Schaefer of Penfield was diagnosed 23 years ago.
“I felt initially like my body be trayed me,” Schaefer said. “I’ve since grown to accept it but one of the most difficult things with alopecia areata is it’s a roller coaster.”
Hair would fall out in patches, then grow in. Sometimes she would lose all her hair for months and then it would grow back. All told, she has lost her hair four times and it has regrown three times. As a hair dresser, alopecia areata negatively affected her professional life until she embraced her condition and began helping women and girls with med ical hair loss find and fit hairpieces at her salon, Alternative Hair. Now she only sees new clients through her virtual wig fitting business, My Wig Coach.
She encourages anyone with an autoimmune disorder seek informa tion through a reputable, national organization and seek support from others with the same condition because other people likely will not understand.
“I would recommend being gen tle but firm with them when having to back out of plans or mention you may not be able to make it to the hol iday dinner because you’re having a bad day,” Schaefer said. “It’s hard when you have a disease like fibro myalgia and other hidden diseases. Give others grace; not everyone is going to ‘get it.’ Try not to hold it against them. It’s human nature. Peo ple want you to be part of your life. When an autoimmune disease rears its heads, we can’t be part of their lives and people are disappointed by the effects of the disease, not you personally.”
Thea Chassin, president and founder of non profit organization Bald Girls Do Lunch, Inc. in West chester County, raises awareness for alopecia areata. She was diagnosed with alopecia areata universalis—to tal hair loss—in 1997.
She noted that people with au toimmune diseases often experience more than one, such as alopecia and eczema.
“Many people with an autoim mune disease also have something like fibromyalgia, Sjogren’s and rheu matoid arthritis,” she said. “It’s not that one causes the other, but if you have autoimmune tendencies, you may have more than one.”
coping with fears and anxiety. Fear of flying, driving on expressways, public speaking, etc. can be overcome after releasing your specific fears and phobias.
• Depression. Techniques includ ing healing white light, release of negative thoughts, positive thinking and happiness visualization empow er clients with a positive attitude and reduces depressive symptoms.
• Low self-esteem. Hypnosis sessions utilizing empowerment, dial up confidence, and ego strengthening can greatly improve self-esteem— which can help with facing fears, improving relationships, and quitting addiction to food, cigarettes, tobacco, alcohol and drugs.
• OCD. Hypnosis can be effective with OCD symptoms. Hair pulling, nail biting, etc., can be treated with appropriate subconscious sugges tions.
Hypnosis also has been used
Common Autoimmune Disorders

• Rheumatoid arthritis, in which the immune system destroys the joints, followed by the organs.
• Psoriasis/psoriatic arthritis causes skin cells to build up and form inflamed scales on the skin. About one-third of people with psoriasis also have psoriatic arthritis.
• Multiple sclerosis attacks the myelin sheath which surrounds the central nervous system’s nerve cells, slowing impulses from the brain to the body, resulting in difficulty in movement.
• Systemic lupus erythema tosus causes joint pain, severe body fatigue and skin rashes.
• Inflammatory bowel dis eases include Crohn’s disease, inflaming any portion of the GI tract and ulcerative colitis, which affects the colon and rectum.
• Addison’s disease affects the how much hormones the adrenal glands produce, which regulates how the body uses and stores carbohydrates and regulates sodium in the blood stream.
• Although in different ways, Graves’ disease and Hashimoto’s thyroiditis affect the thyroid, a gland important for controlling the metabolism.
• Sjögren’s syndrome attacks the glands that produce saliva and tears, meaning the patient experiences dry eyes and a dry mouth.
• Celiac disease causes the immune system to attack and inflame the small intestine whenever the patient eats foods containing gluten, a naturally occurring protein in wheat and rye. Gluten is not harmful to people without celi ac disease or sensitivity. Gluten sensitivity is not an autoim mune disease.
successfully to address pain manage ment, weight loss, and codependency issues.
Hypnosis is a very effective treat ment modality which helps clients learn a variety of tools and anchors to apply whenever they are faced with stress and anxiety-provoking situa tions. Clients become symptom free and are better able to reach a higher level of functionality in their lives.
Rekha Shrivastava, MS, is a certified hypnotist and certified rehabilita tion counselor. She operates Blossom Hypnosis in Roch ester. For more information, visit blossomhypnosis. org or call 585281-2988.

Page 10 • IN GOOD HEALTH – Rochester / Genesee Valley Healthcare Newspaper • October 2022
JOIN OUR TEAM! NOW HIRING DIRECT SUPPORT PROFESSIONALS
Legalization of Marijuana and Implications for Health
Just the facts, know the risks!
By Jennifer Faringer
NewYork state enacted the Marijuana Regulation and Taxation Act (MRTA) earlier in 2021, legalizing and regulating the use and possession of cannabis for adults ages 21 and older.

The measure paves the way for marijuana dispensaries and mar ijuana lounges, with dispensaries expected to begin opening by the end of 2022.
While some view this as a busi ness opportunity, it’s important to recognize the potential health risks and impact on our communities, families and our youth. It is import ant to have the facts, know the risks and remember that legal does not equal safe. Marijuana remains an addictive drug.
While we continue to focus on the overdose epidemic, primarily caused by the increase in availability and sales of illicit fentanyl, it’s im portant to keep in mind that opioids are rarely the first drug of use. Alco hol, nicotine (vaping) and marijuana are the top three drugs that most sig nificantly place young people at risk. With the legalization of marijuana comes a corresponding decline in the perception of risk which results in an increase in use, according to research and surveys. Marijuana is often the first drug teens try, but not the last!
• The impact of marijuana on brain development is of concern for youth with research showing a decrease in IQ by six to seven points with early, regular use.
• While teens report using mar ijuana to cope with anxiety and de pression, recent studies have shown that using marijuana only worsens both.
• Marijuana smoked or vaped damages lung tissue similar to to bacco use. Studies have also shown that marijuana decreases the body’s ability to fight infection thus weaken ing the immune system.
• With the increasing potency of tetrahydrocannabinol (THC) over the last several decades from 1% to 4% in the 1960s to now 20% to up to 90% THC found in concentrated forms, the risk increases.
When ingested, the effects of marijuana are not felt as quickly as when smoked or vaped. For those ingesting edibles intentionally, this delayed reaction often leads to taking more to feel the expected effect and may result in effects ranging from
drowsiness and lethargy, to loss of muscle coordination, agitation and irritability, and confusion.
Edibles are of a particular concern as reports are pointing to increasing instances of pediatric poisonings as a result of children ac cidentally ingesting marijuana-laced food products and candy which are often packaged in a way that can be indistinguishable from actual food products. With children under age 3, the impacts of pediatric poisoning are more critical and may include respiratory depression and seizures.
Another concern is an increase in drugged driving. Driving while impaired is illegal no matter what substance is being consumed. In New York, it is illegal for both the driver and passengers to use marijuana. While an individual under the influ ence of marijuana may feel in control and focused, what they are experi encing is a fixation of focus, along with a decrease in peripheral vision and a slowed reaction time. It’s no wonder that after alcohol, marijuana is the most identified drug in deadly crashes. Impaired or drugged driving jeopardizes the safety of all who trav el on the roads and highways.
As marijuana potency increases, it’s not a surprise that the risk of be coming addicted has also increased, nor is it a surprise that marijuana is often the number one reason teens seek treatment. Despite legalization, marijuana remains an addictive drug!
For more information and a wide range of resources for parents and the community, visit our website awareness page at: https://ncaddra.org/resources/awareness-cam paigns/marijuana/.

To schedule a presentation con tact jfaringer@depaul.org.

The staff at Mary Cariola Center's six residential homes strive to provide attentive and compassionate care for our residents with developmental disabilities and complex medical conditions
Jennifer Faringer is the director, De Paul’s NCADDRA (National Council on Alco holism & Drug Dependence-Roch ester Area).
 MARYCARIOLA.ORG
MARYCARIOLA.ORG
October 2022 • IN GOOD HEALTH – Rochester / Genesee Valley Healthcare Newspaper • Page 11
D E P AUL 585 271 0761 INFO@MARYCARIOLA.ORG WWW.MARYCARIOLA.ORG
/WORKING-HERE
Golden Years &
Special
Q & Awith Heather Newton
CEO of NAMI Rochester talks about mental health, addiction, suicide prevention and ways her nonprofit is helping the community. She says demand for service is growing steadily
By Mike Costanza
AMI Rochester offers peer support programs and educational courses to those affected by mental illness and their
The nonprofit, which is part of the National Alliance on Mental Illness, served close to 3,000 people last year, a great increase over the average 2,200 it served annually pre pandemic.
It has just six employees, about 60 active volunteers and a current budget of $430,000. In Good Health spoke to CEO Heather Newton about NAMI Rochester’s programs and challenges.

Q: What is NAMI Rochester’s purpose?
A: Our mission is to provide sup port, training and advocacy around mental health for our community. Our primary audience is people who are seeking support in a nonclinical setting. We’re a community-based organization and we’re advocates. Nothing we do is clinical.
Q: How is NAMI Rochester different from other nonprofits that support those who have mental health condi tions?
A: Whether you work here or whether you are a facilitator for one of our programs, you had a mental health story in the past or one that you are working through now, and
you are using that experience to help and support other people through very similar experiences.

Q: Could you tell us about some of your nonprofit’s support programs?

A: We have support groups that are for peers and run by peers. Some of those people have a diagnosis and some of those people do not have a diagnosis. That is irrelevant to us. If you feel that you need support around your own mental health condition or if you are supporting a family member or friend who has a condition, we are here to help. You can come anytime. We want you to come when you need support.
Q: Some people living in the Rochester area have specific needs that general support groups might not meet. How does NAMI Rochester help them?
A: We have more specific sup port groups for particular groups in the community that have come to us. For example, we have a group called Warrior Moms that is specifi cally for moms who are supporting their children who live with mental illness or a co-occurring substance use disorder. We have similar groups for dads, senior citizens, LGBTQ, and for Black and brown men. We also have a group for those who have lost someone in their life to addiction— meaning overdose—and for those specifically who have lost someone
in their life to suicide. It’s called the Suicide Loss Bereavement Group.
Q: Why is it important to focus upon suicide prevention?
A: When you talk about mental illness you must also include conver sations about substance use disorder, meaning addiction and suicide pre vention. You cannot untangle mental illness, substance use disorder and suicidal thoughts and actions, they’re inextricably linked. We also oversee the Monroe County Suicide Preven tion Coalition. We get together other community members and organiza tions who are interested in the ways we can reduce the suicide numbers in the community.
Q: Does NAMI Rochester also offer edu cational programs for peers?
A: Those are eight-week pro grams where folks are welcome to sign up. Those educational programs get a little bit more in depth in terms of brain health and brain science. They are two-and-a half hours for eight weeks in a row. So you really need to be at a point in your life where you feel like you can do that.
Q: NAMI Rochester received a $12,500 pilot grant from the Suicide Prevention Center of New York for developing a countywide LOSS Team. What is a LOSS Team?
A: That acronym stands for “Lo cal Outreach to Suicide Survivors.” It’s based on a national model called the LOSS Team model. The team is made up of people who have expe rienced a loss in their family by sui cide. Those people are acting as peer support for people who have asked for that support. They would be the family members or loved ones of those who have died by suicide. We have this dedicated phone line where we’re dispatching these folks.
Q: As part of its outreach efforts, NAMI Rochester has passed out “resource cards” in the community. What are they?
A: Our pocket-sized resource cards provide free local resources for individuals and their families who are in need of mental health support. The cards list brief descriptions of local resources, as well as their phone numbers and websites. The cards contain 24/7 hotline information as well as local supports for peers and family members. In addition to NAMI Rochester, some examples of resources listed are: 211/LIFE LINE, the Rochester Regional Health Behavioral Health Access and Crisis Center (mental health urgent care), Self-Help Drop-In Support Services, the Veterans’ Outreach Center, RO Covery Fitness, Trilllium Health, St. Joseph’s Neighborhood Center and Compeer Rochester.
Q: Where have you distributed the cards?
A: Since March 2020, we have produced and distributed more than 35,000 cards to first responders, clinics, therapists, restaurants, coffee shops, barber shops, salons and other community locations to educate our community about the free mental health supports available to them.
Q: How has the COVID-19 pandemic affected the demand for NAMI Roches ter’s services?
A: I have more people seeking more intense support, more frequent ly coming to support groups and more frequently calling out for help.
Page 12 • IN GOOD HEALTH – Rochester / Genesee Valley Healthcare Newspaper • October 2022
■ Free online hearing tests you can take at home ■ Mistakes to avoid when choosing a Medicare plan ■ Top senior discounts to improve good health ■ Home sharing: A growing trend among baby noomers ■ Vistion awareness — How to stay sharp
Senior
Don’t miss the next issue of In Good Health. Some of the stories we’re working on: To advertise in this special issue of In Good Health, please call sales representative or send an email to editor@GVhealthnews.com
SmartBites
By Anne Palumbo
The skinny on healthy eating
What Makes Apples Such a Nutritious Fruit?
Helpful tips
To get the most out of ap ples, leave the skin on, as it con tains half the fiber and most of the polyphenols. Eat them raw, if possible, since cooking can deplete some nutrients. Wash all apples (including organic) before preparing or eating. Apples stored in the refrigerator can last six to eight weeks. Kept at room temperature, apples last about a week.
When
my kids were young, I used to call all fruit “na ture’s candy.” The nickname won them over, especially when it came to apples. As a family, we de voured apples by the bushelful!
Although the kids are long gone, apples continue to be my go-to fruit and here’s why: they’re delicious; they’re always available; they last forever in the fridge; and they’re loaded — absolutely, positively load ed — with powerful health benefits.
Let’s begin with apple’s most bountiful nutrient: fiber.
Apples are a good source of both soluble and insoluble fiber, with one medium apple providing about 20% of our daily needs. Soluble fiber protects against heart disease by lowering bad cholesterol, while insoluble fiber keeps us regular and feeling full. Both fibers, along with an apple’s high-water content, help with weight control, which further benefits the heart by lowering the risk of high blood pressure.
Apples are packed with polyphenols, an import ant group of antioxidants that might help prevent cancer. Antiox idants protect our bodies from disease and accelerated aging by

neutralizing free radicals — harmful by-products of daily living— that can wreak havoc with healthy tissues.
Many studies suggest that eating an apple a day (or more) is associated with a reduced risk of certain can cers, including colorectal, oral, lung, prostate and breast cancers. Al though the results so far look prom ising, researchers point out that more studies are needed.
Eating apples may also reduce your risk of Type 2 diabetes, a chron ic condition that results in too much sugar circulating in the blood stream. Even though apples taste sweet, they have a low glycemic index, which means your blood sugar levels don’t spike when you eat them. Research ers at Tufts University found that people who ate one or more apples a day had up to a 23% lower risk of Type 2 diabetes than non-apple eat ers. Experts say the fruit’s fiber helps stabilize blood sugar, along with its high concen tration of antioxi dants.
Just under 100 calories, nutrient-rich apples are also a decent source of im mune-boost ing vitamin C and have no fat, cholesterol or sodium.
Are Big Breakfasts the Key to Weight Loss?
Dieters who believe that eating a big breakfast followed by a small dinner is the surest way to lose weight will likely be very dis appointed by the findings of a new, small study.

What did the researchers dis cover? Eating the largest meal early in the day is unlikely to make any difference.
“The notion of timing of eating to influence health has been around for a long time,” said study author Alexandra Johnstone, a registered nutritionist and professor in the school of medicine, medical sciences and nutrition with the Rowett Insti tute at the University of Aberdeen in Scotland.
Johnstone acknowledged that the advice to “breakfast like a king and dine like a pauper” has plenty of adherents.
And prior research has in fact “suggested that eating earlier in the day enhanced weight loss, affecting energy metabolism, compared to
eating later in the day,” she noted.
Still, “chrono-nutrition” — the relationship between food intake and time of day — “is a relatively young science,” Johnstone cautioned.
To try to separate myth from fact, she and her colleagues decided to conduct a diet test involving 16 men and 14 women. For a month, each participant was randomly assigned to follow a morning-heavy diet or an evening-heavy diet, the study authors explained.
All meals were based on a 30% protein, 35% carbs and 35% fat break down, while total daily calorie intake was fixed.
But those on the morning-heavy diet consumed 45% of their daily calories at breakfast, followed by 35% and 20% at lunch and dinner, respec tively.
In contrast, those on the eve ning-heavy diet followed a 20%, 35% and 45% daily calorie split.
At the end of the month, all participants took a one-week break,
Apple Walnut Quinoa Salad
Adapted from twopeasandtheirpod.com
Serves 4-6
Maple-mustard dressing:
¼ cup olive oil
1 tablespoon fresh lemon juice
2 tablespoons apple cider vinegar
½-1 tablespoon pure maple syrup
2 teaspoons Dijon mustard
1 clove garlic, minced
Kosher salt and black pepper, to taste
Apple quinoa salad:

2/3 cup quinoa, rinsed
1¼ cups water
4 cups mixed greens
2 cups chopped apples
½ cup dried cranberries
½ cup crumbled goat, feta or Gor gonzola cheese
½ cup chopped walnuts Kosher salt and black pepper, to taste
which was then followed by a switch: for the following month all the morning-heavy eaters became eve ning-heavy eaters, and vice versa.
The result: “We found weight loss was similar with both diets,” Johnstone said.
All participants did lose a nota ble amount of weight, with an aver age loss of about 7 pounds during each of the one-month periods. It’s just that neither dietary pattern prompted more weight loss.
However, Johnstone and her colleagues did identify one big differ ence between the two styles of eating: diminished hunger among those on the morning-heavy diet.
While “there was no impact on energy expenditure,” she noted, “there was a positive influence of big breakfast to control appetite through out the day, with less hunger.”
And that could give a morn ing-heavy diet a leg up in the long run, she said.
“Hunger is one of the main reasons that people fail to comply to a weight-loss or calorie-restricted diet,” said Johnstone. “So if we have diet strategies that can help control hunger, then it would be beneficial in the real world.”
Johnstone and her team also
First, make the quinoa. Combine the quinoa and water in a medium pot. Bring to a boil, cover, reduce the heat and simmer for 15 minutes. Remove from the heat and let it sit, covered for 10 more minutes. Fluff with a fork.
While quinoa is cooking, make the maple-mustard dressing. In a small bowl, whisk together all the dressing ingredients. Set aside.
In a large bowl, add the mixed greens, cooked quinoa, apples, dried cranberries, crumbled cheese, and walnuts. Toss until the salad is combined. Then, drizzle with dressing (add the amount that suits you) and toss again. Season to taste with more salt and pepper, if needed.
Anne Palumbo is a lifestyle colum nist, food guru, and seasoned cook, who has perfected the art of preparing nutritious, calorie-conscious dishes. She is hungry for your questions and comments about SmartBites, so be in touch with Anne at avpalumbo@aol.com.

stressed that there is unlikely to be a one-size-fits-all approach to how dietary planning affects metabolism. Yet broadly speaking, “our work sug gests that the distribution of calories throughout the day does not influ ence energy metabolism or weight loss,” she said.
The findings were published online Sept. 9 in the journal Cell Metabolism.
October 2022 • IN GOOD HEALTH – Rochester / Genesee Valley Healthcare Newspaper • Page 13
Making Recreation Accessible

 By Mike Costanza
By Mike Costanza
Rochester
Accessible Adventures stepped into the spotlight at the US Open in August when USTA Eastern, a part of the United States Tennis Association, named the nonprofit a Diversity, Equity and Inclusion Champion. The small orga nization earned the prestigious title through its efforts to support tennis instruction for all people, including those who are disabled.
“We’re working with USTA Eastern on how they can train tennis professionals on how to teach tennis to people with and without disabili ties,” said Anita O’Brien, the founder and executive director of Rochester Accessible Adventures.
O’Brien, a certified therapeutic recreation specialist, helped people with disabilities enjoy therapeutic recreation while with a number of local nonprofits, until she came to find her role too limiting.
“I was ending up being a gate keeper to people who experience something that I feel is pretty much
a right, that we have access to health and wellness through recreation,” O’Brien said.
She founded RAA in 2015 to help local businesses and nonprofits give those who have disabilities access to healthy recreation.
“We go to recreational businesses and help them provide equitable ac cess,” O’Brien said. “We want to train them on how to bring the 26% of the population with a disability that they’ve most likely been missing.”
A business or nonprofit that con tracts with RRA begins its training by having its employees view a 10-hour online program on working with people with disabilities.
“Once we have that as our foun dational knowledge base, we know that all sitting at the table have at least that same base of knowledge,” O’Brien said.
RRA then helps the organization assess its ability to serve people with disabilities, and develop a plan for developing or improving those ser
vices. A library, for example, might need to have tables which can be adjusted to different heights so that people in various types of wheel chairs can make use of them. Once that plan has been developed, RAAQ helps its client put it to use.
“They actually begin imple menting best practices and inclusion, which begins to change the culture of their organization,” O’Brien said.
As part of that process, which can stretch on for a year or more, RRA helps its clients pick out the equipment or assistive devices that it needs to serve those with disabilities. The nonprofit, which has just two employees and about 36 volunteers, has worked with 15 local nonprofits and businesses since it was founded.
Pete Abele, the founder and owner of the Erie Canal Boat Com pany, turned to RAA for help when he wanted to expand his clientele to include more people with disabilities.
“You want to try to cater to the widest spectrum (of disabilities) pos
sible,” Abele said.
Abele took RAA’s training course, then sat down with the non profit to pick out the equipment he needed.

“We sat down and reviewed some of the equipment that might be useful to various individuals with different disabilities,” Abele said.
His company’s rolling stock now includes three-wheeled, adaptive bicycles, some of which are powered by the rider’s arms instead of his or her feet. Even someone who is para lyzed from the waist down can ride.
“They can just crank along with anybody else,” Abele said.
The Erie Canal Boat Company also provides special kayak seats that hold paddlers with disabilities stay upright and little pontoons called outriggers that keep the crafts from tipping over.
In addition to working with local nonprofits and businesses, RAA sponsors three sports teams. Adults with or without disabilities can
LEFT AND BOTTOM: Chase Marcott, who is paralyzed from the waist down due to spina bifida, became one of the first people to pedal on Hog Hollow, a new trail in Victor. BELOW: Ten-year-old Caleb Muller on a special bike.
Page 14 • IN GOOD HEALTH – Rochester / Genesee Valley Healthcare Newspaper • October 2022
play wheelchair basketball with the Rochester Wheels or mount sleds and head to the ice with the Rochester Sled Hawks. For youth 9 years old and older, there’s the Rochester Rock ets wheelchair basketball team.

Chris Muller brought Caleb, his 10-year-old son, to the Erie Canal Boat Company in August for a pre-season get-together with other members of the Rochester Rockets and their parents. Muller said Caleb, who is paralyzed from the waist down due to spina bifida, has really gained from his time on the basket ball court.
“It’s been tremendous for his self-esteem,” the Victor resident said. “He feels like he can do any thing when he’s on the floor with his peers.”
Caleb put it a little more precise ly.
“I just enjoy basketball,” he said.
A short time later, he was wheeling down the canal path in a hand-operated three-wheeler.
In addition to helping kids like Caleb get on the basketball court, RAA has helped local towns make their facilities and trails more acces sible to those with disabilities, or inclusive.
The Town of Victor Parks and Recreation Department began work ing with RAA about five years ago.
“Our department, with RAA, has been working on programmatic and physical steps towards inclusion for all residents of our community,” said Brian Emelson, the department’s director.
Though the town had made its trails accessible to those with dis abilities, it recently turned to RAA to improve them further.
“We assessed several of our park facilities to look at creative ways that we could make changes to facili ties, including bocce courts, fishing docks… to take them to the next level of accessibility physically, as well as programmatically,” Emelson said.
The results of the assessment led the town to install signs at the heads of its trails indicating that they are accessible to those with disabilities.
RAA also helped Emelson’s department obtain grants totaling $9,500 for the purchase of a mountain bike that is specifically designed for those with disabilities. The first of its kind to appear in the Rochester area, the Lasher Sport adaptive mountain bike has shock absorbers for all three of its wheels. Though it’s pedaled by hand, it also has an electronic battery and motor.
“A person that needs a little more support getting up a steep incline or a slope, it …can help assist them if they need,” Emelson said.
Bicycle riders can enjoy riding on Victor’s newest bike on the town’s latest outdoor attraction.
Hog Hollow is the first trail in the Greater Rochester area that was purposely designed to be used by those with disabilities. Chase Mar cott, who is paralyzed from the waist down due to spina bifida, became one of the first people to pedal the new trail on the town’s adaptive mountain bike back in July.
“It felt amazing,” said the Victor resident. “I’m really glad there’s accessible trail near.”
Emelson said anyone can make use of the new mountain bike just by contacting his office.
Founded in 2015, Rochester Accessible Adventures gives those who have disabilities access to healthy recreation

 TOP: Anita O’Brien (left) is the founder and executive director of Rochester Accessible Adventures. Next to her is Dee Mascari, the group’s inclusion specialist.
RIGHT: Special kayak seats help paddlers with disabilities stay upright and little pontoons called outriggers keep the crafts from tipping over.
BOTTOM: Members of the Rochester Rockets basketball team.
TOP: Anita O’Brien (left) is the founder and executive director of Rochester Accessible Adventures. Next to her is Dee Mascari, the group’s inclusion specialist.
RIGHT: Special kayak seats help paddlers with disabilities stay upright and little pontoons called outriggers keep the crafts from tipping over.
BOTTOM: Members of the Rochester Rockets basketball team.
October 2022 • IN GOOD HEALTH – Rochester / Genesee Valley Healthcare Newspaper • Page 15
New Medication to Address Alopecia Areata Seen with Caution
Penfield resident diagnosed 23 years ago with the condition says she will wait to use new medication: “There are a lot of side effects and the results, as with most medications, are not guaranteed”
By Deborah Jeanne Sergeant
The
FDA announced in June its approval of baricitinib (brand name Oluminant, among oth ers) to treat alopecia areata.
Many people experience hair thinning and loss related to aging or medication.
Alopecia areata is different.
The autoimmune disease causes sudden, round patches of hair loss all over the head. The patches may grow in size and come and go in different areas over weeks and months. Alo pecia totalis means that all of the hair on the patient’s head falls out and al opecia universalis refers to complete bodily hair loss.
About 6.8 million Americans have alopecia areata.
For Sherry Schaefer, a Penfield resident diagnosed 23 years ago, the benefits of baricitinib seem overshad owed by the side effects.
“There are a lot of side effects and the results as with most medica tions are not guaranteed,” she said.
“In fact, based on the clinical trial of 1,200 people, Brett King, dermatol ogist with Yale School of Medicine, said that the clinical results showed that 20% to 44% of the people regrow a respectable amount of hair. That’s less than 50%.”
At this point, she has decided to wait, but understands if others want to try it, especially people who have
other autoimmune conditions barici tinib could simultaneously treat.
Schaefer also acknowledges that her hair loss experience differs from many others. She has parlayed her lifelong experience in hairdressing into fitting custom wigs and hairpiec es. She helps women with medical hair loss through Alternative Hair, her salon for her existing customers and her newer business born of the pandemic, My Wig Coach, where she remotely fits wigs and hairpieces for clients.
“I have an extreme comfort level with appearing without wigs,” she said. “For the average person, it’s a more difficult decision to make.”
Along with King, Louis J. Papa, primary care physician at URMC, and Thea Chassin, founder of West chester County-based Bald Girls Do Lunch, Schaefer appeared on Joan Lunden’s “Second Opinion” show airing on public television stations nationwide March 28. For most of the segment, Schaefer wore one of her many wigs—she models them for her My Wig Coach Facebook page—but removed the wig partway through the segment.
Schaefer finds that taking good care of herself with meditation, rest and modalities of holistic health precedes the times when her hair regrows and stressful periods often
Pot Use in Early Pregnancy Linked to Long-Term Mental Health Issues in Kids

Using marijuana after the first weeks of pregnancy is linked to mental health issues in children that linger well into early adolescence, a new study shows.
Exposure to cannabis after about five to six weeks of fetal development was associated with attention, social and behavioral problems, according to the findings. These problems con tinued as the children reached ages 11 and 12, raising the risk of mental health and substance use disorders in the teen years.
Researchers from Washington University in St. Louis cautioned against using the drug during preg
nancy.
The team used data from the ongoing Adolescent Brain Cognitive Development (ABCD) Study, which gathers information on brain devel opment and health in 12,000 children and teens in the United States.
As part of the ABCD study, investigators regularly measure par ticipants’ brain structure and activity using MRI scan. They also collect psychological, environmental and cognitive information.
The study only found an associ ation and not a cause-and-effect link between pot during pregnancy and children’s mental health outcomes.
precede when her hair falls out. However, it’s not a guarantee.
“For me, it’s very stress-relation,” she said. “When mine first hit, I was almost 40. It started two weeks after a near-death experience. The hair loss started and within three months I was bald.”
Diagnosed in 1997, Chassin founded Bald Girls Do Lunch, Inc. She decided that baricitinib is not right for her, but she can also un derstand why many women with alopecia areata feel eager to try the medication.

“The stigma of female hair loss is very big in our culture,” Chassin said. “Women feel less feminine and have concerns about their looks and acceptance should they choose to go without supplemental hair. There’s a lot of worry about feeling normal and feeling they fit in. Our society prizes hair, not just in the US. Hair is a defining part of a woman in most cultures. A lack of hair is a very big deal. It affects self confidence and self-esteem.”
While Chassin appeared on Lunden’s program with her bare pate exposed, she knows that many wom en do not feel that is the right choice for them.
Beyond appearance, a lack of hair otherwise affects health. Without eyebrows and eyelashes, dust and
sweat get into the eyes easier and mucus flows readily out of the nose without hairs to stop it. Chassin said that some people with alopecia areata have painfully brittle fingernails.
She views wearing wigs, scarves, hats, turbans or nothing at all on one’s head as daily choices that women with alopecia areata can make, depending on their situation or preference. Chassin’s hair fell out slowly in patches and in overall thin ning for three decades. Eventually, it had fallen out to the point where it “was hair, but not a hairdo,” she said.
She likened her appearance then to Bozo the clown.
“When I shaved it off, I felt like a huge weight had been lifted off me,” she said. “It was truly a step forward to self-acceptance.”
She also felt a powerful sense of control over a situation which had previously spun out of control for years.
For women interested in medi cation, Chassin views baricitinib as “a game-changer. There are many people who have been waiting for a medication that they can try. Pre viously, the options were limited. It’s an opportunity for people to try something if they’re not contra indicated. It doesn’t work 100% in everybody, but for those who want to try it, it’s FDA-approved.”
Nevertheless, THC, which is the main psychoactive sub stance in cannabis, can cross the placenta and potentially af fect brain development, accord ing to past research on cannabis use in pregnancy.
About 3% of pregnant women used cannabis in 2002, but that grew to 7% in 2017. Those numbers were 4.7% in 2018 and 5.4% in 2019, accord ing to the National Survey on Drug Use and Health.
The study was supported by the U.S. National Institute on Drug Abuse (NIDA) and was published Sept. 12 in JAMA Pediatrics.
Thea Chassin, founder of Bald Girls Do Lunch in Westchester County and Brett King, dermatologist with Yale School of Medicine. “The stigma of female hair loss is very big in our culture,” Chassin says.
Page 16 • IN GOOD HEALTH – Rochester / Genesee Valley Healthcare Newspaper • October 2022
OMEN'S HEALTH
5Things You Should Know About Breastfeeding
By Ernst Lamothe Jr.
3.Breastfeeding trends
Breastfeeding
is one of the healthiest things a mother can do for her newborn baby. It helps create a deeper connection be tween mother and child and provides children the vital nutrients they need for survival and growth.
It’s also something that doesn’t always come natural to everyone and can provide stress for a new mother if her intention was to breastfeed.

Nearly two out of three infants aren’t exclusively breastfed for the initial recommended six months, according to the World Health Orga nization.
“Breastfeeding can be wonderful and challenging all at the same time. There are resources to help parents get started, if they are having issues, or for ongoing support. Reach out for help or questions,” said Michele Burtner, associate medical director of breastfeeding and lactation services at the University of Rochester Medi cal Center.

Burtner discusses five aspects of breastfeeding.

1.Myths
When it comes to breastfeed ing, myths run rampant. Common ones include the notion that breast feeding hurts and a laundry list of certain foods to avoid while breast feeding.
“It is true there can be some discomfort in the first few days of learning to breastfeed. However, getting help to latch an infant cor rectly can reduce this discomfort and ultimately help avoid sore and dam aged nipples. If any pain persists, parents should seek lactation help,” said Burtner. “With food, lactating parents should eat a well-balanced diet, just like the rest of us. Remem
ber, infants are exposed to all types of foods the mother ate while they were pregnant.”

Another myth she wants to dis pel occurs when the mother is going back to work.
“Many mothers continue breast feeding when they return to work. It can provide challenges, but with the right support and breast pump, it is very doable,” said Burtner. “Breast feeding does not have to be all or none, so if a mother chooses to sup plement her baby, she can still breast feed as much or as little as desired. It is helpful for parents to take a pre natal breastfeeding class while they are pregnant to learn more about the process and what to expect.”
2.Breastfeeding benefits
There are many benefits of breastfeeding, for both the lactating parent and infant. Breastfeeding can help protect babies against some short- and long-term illnesses and diseases.
“Breastfed babies have a low er risk of asthma, obesity, Type 1 diabetes and sudden infant death syndrome,” she added. “Breastfed babies are also less likely to have ear infections and stomach bugs. A really cool fact is that the mother’s milk changes as the baby grows, in order to meet the baby’s nutritional needs.”
Maternal health benefits of breastfeeding include reduced risk of breast and ovarian cancer, Type 2 diabetes and cardiovascular disease. Recovery from childbirth can be quicker and with less risk of heavy postpartum bleeding.
“There is, of course, typically an emotional benefit and bonding for mother and infant,” she said.


With so many different kinds of breast pumps, a new moth er may feel overwhelmed. A breast pump is typically held in place by hand or by a nursing bra, a breast pumping bra or a band. There are three kinds — manual, battery-pow ered and electric. Burtner said an oversupply of breast milk can also be created if the parent pumps much more than their baby needs, which can create other issues. But with so much information people often turn to social media. This could be helpful if the advice is from lactation trained people. But there can also be misin formation out there.
“We recommend checking in with a lactation consultant if there are questions about whether a breast pump is needed or any questions about a particular pump,” she said. “There are many local support groups and lactation-consultants if families have questions or need support.”
4.COVID-19 and breastfeed ing
Current evidence suggests that breast milk isn’t likely to spread the virus to babies. If you have COVID-19, wash your hands before breastfeeding and always wear a mask within six feet of your infant. Get a lot of rest and take good care of yourself.
Follow CDC recommendations regarding isolation from others.

“Most often, it is safe to con tinue breastfeeding if the mother is

sick,” Burtner said. “She needs to get herself treated and let her providers know she is breastfeeding, as well as getting rest, staying hydrated and well fed. Most often, there are antibodies made that help fight the illness and can be passed on to the infant.”
5.Breastfeeding timeline
The World Health Organi zation and the American Academy of Pediatrics recommend infants be exclusively fed breast milk for the first six months of life, then continue breastfeeding along with introducing of appropriate complementary foods for up to 2 years of age or longer.
Michele Burtner, a certified nurse midwife, is associate medical director of breastfeeding and lactation services at the University of Rochester Medical Center.
October 2022 • IN GOOD HEALTH – Rochester / Genesee Valley Healthcare Newspaper • Page 17 OMEN'S HEALTH
Experience the Direct Primary Care Difference! Are You Feeling Heard by Your Primary Care Physician? Convenient, exclusive direct access to your own personal physician Members only cell phone line to the doctor Same day or next day appointments Unlimited in person or telemedicine visits Comprehensive, personalized primary care services Whole person care All services included in a low monthly fee! 30 Office Park Way, Pittsford Call to Schedule a Free “Meet & Greet” (585) 662-5510 athenadirectcare.com Accepting New Patients Limited Time Only Laura Petrescu MD, CPE Internal Medicine Specialist Lifestyle Medicine Specialist Certified Physician Executive LARGEST INVENTORY OF TOP QUALITY WIGS IN WESTERN NEW YORK! . , Grasta’s Beauty And Wig Studio grastasbeautyandwigstudio.com 409 Parma Center Rd. (Rte 18) Hilton Just minutes from Greece Ridge Mall! CUSTOM MADE EUROPEAN HUMAN HAIR, WIGS & TOPPERS - HATS & SCARVES TOO We specialize in professional, personal, and confidential service. We enjoy making clients feel beautiful from the inside out CALL 585-392-7823 - NO TEXTING Due to COVID-19, strict safety policies are in effect and apply to EVERYONE. We cover our styling chair in disposable vinyl. I also wear protective coverings. There is no way an operator could be three feet apart from a client while working, which is why the client and I are covered. You will receive foot coverings, vinyl gloves and a sheer vinyl cape which you will wear out to your car and discard at your convenience. Temperature will be taken at the door. No wigs are touched by bare hands. ONLY THE CLIENT IS PERMITTED INSIDE! • NO PICTURES-FACETIME ONLY “She made me feel beautiful...” “Sharon was so kind & understanding and she had lots of hairpieces to choose from. She knew exactly what I needed. I loved her right away because she showed me what was good on me & the ones not good on me. Sharon was always patient with me... Sharon loves her customers and it shows in how wonderful she treats them: like family.” - Mrs Ann M. Colarertalo BY APPOINTMENT ONLY•ABSOLUTELY NO WALK INS• MUST CALL FOR APPOINTMENT SHARON M. GRASTA (RUSSO) -owner & operator
Man Recalls Struggle with Prostate Cancer
Aretiree
from Rochester, who asked that his name not be used, received his prostate cancer diagnosis in 2019.
“It was pretty shocking,” he said. “I was seeking other insights for a doctor. It just oc curred to me I never had a PSA test done. I was 69 years old.”
To his surprise, his pros tate-specific antigen was elevat ed indicating prostate cancer. His was the aggressive type.
“That was the scariest night, trying to keep anxiety under control,” he said. “I thought I might be dead in a few months or a year, but everyone’s cancer is different and I wasn’t educat ed about treatments.”
He chose surgery over radiation, as that would better allow him to receive radiation if he needed it. Going for radia tion first may have meant any warranted surgery would be more difficult afterwards.
“I presumed that there was emotional support connected to the surgeon’s office,” he said. “I asked if he had a list of support services. He said, ‘Not really.’ I was shocked.”
He felt himself slipping into depression about his surgery’s side effects. After prostate sur gery, many men become at least temporarily incontinent and impotent, although these may improve over time.
An online search led him to seek help from the Roches ter chapter of Us Too for men with prostate cancer. The group offered valuable moral sup port, along with The Reluctant Brotherhood, a wholly online group, whose irreverent humor encouraged him.
Last year, his PSA was on the rise, so he received radia tion. His providers continue to monitor his PSA.
“It’s a precarious place to be,” he said.
He tells anyone newly diagnosed to “be your own best self-advocate. Assemble a good team of healthcare providers. You need to read the literature, be fully informed for possible treatment options. Some guys are adamant against surgery. There’s watchful waiting if the numbers aren’t that high, radia tion, prostatectomy, brachyther apy, where they implant radio active seeds.”
He said that information from reputable online sources like the Mayo Clinic can be helpful also.
“Cancer changes your whole perspective,” he said. “You appreciate your life one day at a time. We always say these are areas we should have improved in before cancer but cancer wakes you up to it.”
Cancer Survivors Share Their Stories
By Deborah Jeanne Sergeant
Cancersurvivors all have a different story, as everyone’s journey in life and cancer is unique. Nonetheless, most say that their experience has given them a new perspective on life after un dergoing the devastation of their diagnosis, the struggle to select their next step, their treatment and their recovery.
The support of family, friends and their medical team helped in ways they never expected.
Sue Schwartz of Rochester re ceived her breast cancer diagnosis in
2017 after a routine mammogram.
“It totally came as a shock as there was no history of it in my family,” Schwartz said. “I have been a very active person, never sick a day in my life. I didn’t believe it.”
A biopsy and second opinion convinced her. She discussed her op tions with her care team. A lumpecto my would not remove all the cancer as it had infiltrated the ducts. Told that it could metastasize soon, she decided to undergo mastectomy with TRAM flap surgery reconstruc tion. The surgeon uses tissue from
the lower belly area to form a breast shape before placing it in the breast area.
“The recovery was worse than the whole shebang,” Schwartz said. “I had drains in my chest and belly that had to be emptied. I’m really squeamish.”
Because of her early diagnosis and successful surgery, chemother apy was not warranted. Schwartz receives mammograms annually.
“I couldn’t have had a better team of doctors working on me,” she said.
She also feels gratitude for friends living nearby who helped her through the ordeal. She works parttime as a coordinator at the American Cancer Society Hope Lodge, which provides housing for people who need cancer treatments in Rochester but live farther than 40 miles away.

“Get as much information as you can,” she tells people newly diag nosed. “Have a really good support group.”
Deb Havert, 57, of Canandaigua, also received a breast cancer diagno sis in 2017 after a routine mammo gram.
Mastectomy was the best course for treating Havert. Further testing after her surgery indicated that che motherapy and radiation would not make any difference as to whether or not she would have cancer again.
“Initially, I had a lot of panic attacks and just felt uncomfortable in life, in living with myself,” she said. “I was constantly anxious and not being able to find anything that brought me any comfort.”
She stayed at Hope Lodge for a month, as her home at the time was in the Adirondacks, far from the level of medical care she wanted. Since then, she has not experienced any recurrence.
Havert takes hormone-modify ing medication which can affect bone health, so she regularly receives bone density tests and at first received in fusions to improve her bone density. She also follows up with her oncolo gist regularly.
Havert tells anyone newly diag nosed to “be your best own advocate. Make sure that you ask questions and don’t be afraid to question the doctors and nurses. The best that you can grasp a hold of what’s happen ing, the more comfortable you’re going to feel with your choices.”
She has discovered that creating visual artwork has proven a comfort ing activity. She has also developed more confidence in public speaking as she promotes the importance of mammograms.
Deb Havert, 57, of Canandaigua, received a breast cancer diagnosis in 2017 after a routine mammogram.
Page 18 • IN GOOD HEALTH – Rochester / Genesee Valley Healthcare Newspaper • October 2022 Cancer
Restoring hair
Out-of-Pocket Costs for Cancer Care Keep Climbing
Cancerpatients already have a lot to deal with emotionally and physically. But research shows that insured patients under 65 are also paying more for their treat ments out-of-pocket than ever before.
The study highlights the “grow ing financial burden for non-elderly patients with cancer with private health insurance coverage,” said senior study author Robin Yabroff, scientific vice president of health services research at the American Cancer Society (ACS).
“Policy initiatives to mitigate financial hardship should consider cost containment as well as insurance reform, as most Americans will not be able to afford such an unexpected expense,” she said in an ACS news release.

Affordable
ed surgery, intravenous systemic therapy and radiation. The research team calculated associated total and out-of-pocket costs.
The study found that the total mean costs per patient increased from $109,544 to $140,732 for breast cancer patients, an increase of 29%. Costs increased from $151,751 to $168,730 for lung cancer treatments, or 11% jump. Those costs grew from $53,300 to $55,497 for prostate cancer, about 4%. The increase for colon can cer, went from $136,652 to $137,663, which was not considered statistical ly significant.

and
1425 Jefferson Rd., Saginaw Plaza, 2nd
NY 14623
272-7320
Researchers from the ACS and the University of Texas MD Ander son Cancer Center found that as costs of cancer treatments rise, this led to greater out-of-pocket costs for the four most common types of cancer in patients younger than 65 who were privately insured.
Those out-of-pocket costs went up more than 15% between 2009 and 2016, to more than $6,000 for those being treated for breast, colon and lung cancers, and to $4,500 for those receiving treatment for prostate cancer.
To study the issue, researchers analyzed 105,255 breast, 23,571 colon, 11,321 lung, and 59,197 prostate cancer patients using claims from the Health Care Cost Institute.
The data included cancer-relat

Restoring hair Restoring confidence
“This trend of rising OOP [outof-pocket] costs among patients with private insurance is concerning because high-deductible plans are becoming more common in the pri vate insurance market,” said study author Ya Chen Tina Shih, a professor of health services research at MD Anderson.

at Baldness.com.
“The recently passed Inflation Reduction Act is a step toward ad dressing this challenge, focusing on reductions in pricing for high-cost Medicare drugs and limiting out-ofpocket costs for seniors,” Shih said in the release.


Researchers found that the use of intravenous systemic therapy and radiation statistically significantly in creased, except for lung cancer. Can cer surgery costs increased for breast and colon cancer, while decreasing for prostate cancer.
The findings were published Sept. 13 in the Journal of the National Cancer Institute.


October 2022 • IN GOOD HEALTH – Rochester / Genesee Valley Healthcare Newspaper • Page 19
Cancer Highest Prices Paid We BUY TEST STRIPS We will pick up and pay on the spot We pick up 6 days a week. 11am to 6:30pm One Touch Ultra & Freestyle Lite. All Brands Considered. Up to $50. (585)-284-3455 811 Ridge Rd./Five Mile Line Rd. Webster NY (Webster Woods Plaza) Inclusion WELLNESS SPA 585-347-6100 www.inclusionspa.com Look Years Younger! Facial Skin Tightening Non-invasive. No down time. Certified Laser Technician. Special Offer: $199 before after Results may vary The Spa with a Heart Make In Good Health your advertising choice in 2023 Reach nearly 100,000 health-conscious readers in the Rochester and Finger Lakes area. 33.500 copies distributed each month. Call your sales representative today and request a media kit. Schedule your complimentary, confidential hair loss evaluation today and see how easy it is to be yourself again! Call now! (585) 272-7320 We specialize in both permanent and non-permanent techniques, gradual hair replacement, and system integration. We can provide topical hair loss treatments and laser hair rejuvenation. Check out Virtual Reality Hair Replacement for men & women at Baldness.com. Serving Men, Women and Children Restoring hair Restoring confidence Affordable Financing. Onsite service and repairs. 1425 Jefferson Rd., Saginaw Plaza, 2nd floor Rochester, NY 14623 • 272-7320 Rochester’s Hair Replacement Specialists Schedule your complimentary, confidential hair loss evaluation today and see how easy it is to be yourself again! Call now! (585) 272-7320 We specialize in both permanent and non-permanent techniques, gradual hair replacement, and system integration. We can provide topical hair loss treatments and laser hair rejuvenation. Check out Virtual Reality Hair Replacement for men & women
Serving Men, Women
Children
Financing. Onsite service and repairs.
floor Rochester,
•
Rochester’s Hair Replacement Specialists Schedule your complimentary, confidential hair loss evaluation today and see how easy it is to be yourself again! Call now! (585) 272-7320 We specialize in both permanent and non-permanent techniques, gradual hair replacement, and system integration. We can provide topical hair loss treatments and laser hair rejuvenation. Check out Virtual Reality Hair Replacement for men & women at Baldness.com. Serving Men, Women and Children
Restoring confidence Affordable Financing. Onsite service and repairs. 1425 Jefferson Rd., Saginaw Plaza, 2nd floor Rochester, NY 14623 • 272-7320 Rochester’s Hair Replacement Specialists Schedule your complimentary, confidential hair loss evaluation today and see how easy it is to be yourself again! Call now! (585) 272-7320 We specialize in both permanent and non-permanent techniques, gradual hair replacement, and system integration. We can provide topical hair loss treatments and laser hair rejuvenation. Check out Virtual Reality Hair Replacement for men & women at Baldness.com. Serving Men, Women and Children Restoring hair Restoring confidence Affordable Financing. Onsite service and repairs. 1425 Jefferson Rd., Saginaw Plaza, 2nd floor Rochester, NY 14623 • 272-7320 Rochester’s Hair Replacement Specialists
Post-Cancer Health: A Few Steps for Good Health



 By Deborah Jeanne Sergeant
By Deborah Jeanne Sergeant


Anyone who has received a clear bill of health after cancer treatments wants to maintain their good health. Although nothing can guarantee cancer won’t come back, people in remission can cer tainly increase their chances of good healthy by taking a few steps.
“Survivorship is a key part of cancer care,” said Arnold Baskies, chairman of the Global Health Ad visory Council, and past chairman of the board of directors, American Cancer Society, Inc. “The Commis sion on Cancer has recommended that all hospitals and providers pro vide a survivorship plan to patients. The American Cancer Society also recommends it. It includes informa tion on the treatment rendered and what should be done in terms of follow-up and surveillance.”
Since 14 million people each year in the U.S. have survived cancer —

and Baskies estimates it will likely swell to 20 million in the next five to 10 years —developing survivorship plans will only increase in impor tance.
“The specific recommendations are relative to the type of cancer and treatment rendered,” Baskies said. “A specific survivorship care plan should be personalized.”
For example, a colon cancer survivor may have scheduled colo noscopy and blood tests or for lung surgery, CT scans and other tests. General recommendations typically include healthful diet, exercise, stress management and smoking cessation.
Baskies noted that any time sur vivors change providers outside their health system, “they need to take with them the information of what treatment they had and what needs to be done going forward.”
Pittsford resident Mark Richard
son, 73, received his prostate cancer diagnosis seven years ago.

“When I was diagnosed, it was devastating because I didn’t know anything about it, the risks and side effects of different treatments like surgery, radiation or active surveil lance,” Richardson said.
He joined Us Too, a local prostate cancer support group, which helped him learn more before treatment and support his recovery. Richardson found the group’s support so help ful that eventually, he and his wife, Peggy, took over leading the Us Too chapter.

He said that group members often wonder about how to know if the cancer has returned and what symptoms they should look for.
“Emotional health is very important,” Richardson said. “My wife has been my rock in giving me support and encouragement.”
He also cares for his physical health by walking about three miles or using the elliptical machine at the local YMCA. He finds that lower body exercise specifically has helped him improve his pelvic floor muscles.


“Maintaining these increases
your ability to hold urine correctly and not leak,” he said. “That’s a huge side effect for radiation and surgery. You don’t need to go nuts being Jack LaLanne or Charles Atlas.”

Richardson also promotes eating a healthful diet with less sugar, fat and processed foods to support over all good health.
He and Peggy tried a completely plant-based, whole food regimen for two weeks, which he said was healthful but difficult to maintain. Since then, he has tried to include more whole foods and increase his intake of produce.
“You don’t want to go into an ex treme mode,” he said. “Eating good food allows us to live a long, healthy life but it won’t cure cancer. Modify your diet more for heart health and longevity.”
Richardson also stays hydrated with plenty of water.
Since his diagnosis, he began keeping a journal to notice any lifestyle changes that seemed to help and to track his progress, a practice that he has discovered kept him mo tivated to stick with positive changes.
Arnold Baskies
Mark Richardson
Page 20 • IN GOOD HEALTH – Rochester / Genesee Valley Healthcare Newspaper • October 2022 Cancer
Timeless Remedies Handcrafted Goodness from the Hive! Store Hours: Tues 4pm-7pm; Wed & Thurs 10am-4pm; Fri 10am – 2 pm; Sat 10am-3pm. Closed Sun & Mon Local Delivery & Curbside Pickup Available Visit us at 27 North Ave. (Rt. 250), Webster NY 585.213.2292 | www.thenorthbeeshop.com Beekeeping Sensory Room For Kids Honey Tasting Available Your headquarters for Plant-Based Healthy Products Propolis is tree resin collected by bees with proven medicinal properties for a variety of ailments. The Amazing Power of Bee Propolis *Talk to your healthcare provider about any supplements you plan to take Antibacterial • Antioxidant • Antifungal • Antiviral • Anti-inflammatory Antimicrobial • Promotes Healthy Bone Tissue • Effective Wart Treatment Helps Control Blood Sugar Level • Helps Heal Cold Sore Stock Up Now Before Cold & Flu Season Available raw or in tinctures, honey, salves & sprays.* Phobias ▪ Anxiety ▪ Weight Loss ▪ PTSD Depression ▪ Smoking ▪ Addictions HYPNOSIS: An integrative approach to holistic health care ONLINE or IN-PERSON SESSIONS FSA and HSA eligible. Rekha Shrivastava, MS, CRC Certified Hypnotist & Certified Rehabilitation Counselor 20 Years Experience in Cognitive Behavioral Therapy Phobias ▪ Anxiety ▪ Weight Loss ▪ Depression ▪ Smoking ▪ Addictions HYPNOSIS: An integrative approach to holistic health care FSA and HSA eligible. Rekha Shrivastava, MS, CRC Certified Hypnotist & Certified Counselor 20 Years Experience Cognitive Behavioral Therapy “I was struggling with depression around the pain that divorce was causing me and my teen girls. I feel like a different human now. Rekha loves her patients and cares deeply about our healing. Run, don’t wait. She works miracles.” —J.K., Pittsford, N.Y.
Group


























October 2022 • IN GOOD HEALTH – Rochester / Genesee Valley Healthcare Newspaper • Page 21 Comprehensive Healthcare Resources Guide Inside Children Free Health Clinics Hospitals Mental Health Seniors Support Groups Volunteering Women & more ROCHESTER FINGER LAKES Published by In Good Health — Rochester’s Healthcare Newspaper 2019 R O C H E S T E R / F I N G E R L A K E S WWW.GVHEALTHNEWS.COM Advertise and reach thousands of health-conscious readers! 2023 HEALTHCARE GUIDE DON’T MISS OUT Published by In Good Health, Rochester’s Healthcare Newspaper ROCHESTER – FINGER LAKES WWW.GVHEALTHNEWS.COM GUIDE Comprehensive Resources Guide Women’s Services Children, Seniors Mental Health Support Groups Volunteering PLUS: Leaders in Healthcare PUBLISHED BY Comprehensive Resource GuideWomen’s Services Children Seniors Mental HealthSupport Groups Volunteering Free Health Clinics & more! ROCHESTER / FINGER LAKES Healthcare GUIDE 2022 GVHEALTHNEWS.COM PROFILES • INFORMATION ON ALL HOSPITALS • HEALTH-RELATED FEATURE STORIES • LARGE RESOURCES DIRECTORY ONLINE AND IN PRINT CONTACT YOUR SALES REPRESENTATIVE Anne Westcott | anneIGHsales@gmail.com | 585-421-8109 Linda Covington | lindalocalnews@gmail.com | 585-750-7051 Nutrition Education & Counseling Physical Activity Nicotine Cessation Stress Management We help people lead healthier lives. Our programs help people make small changes they can maintain for life Offered virtually and in person, programs cover topics including: Free
Programs Promote Health Prevent Cancer An eight week program aimed at empowering participants to make and maintain changes in diet, physical activity and exposures that can reduce the risk of cancer and other chronic diseases This program is offered both in person and virtually Commit to Quit! A six session virtual program that provides an interactive and understanding environment designed to support your quit journey Each 60 minute session is led by trained lifestyle counselors and nicotine cessation experts Call us at (585) 602 0801 to learn more For additional information, call the Center for Community Health & Prevention at (585) 602 0801 Discovery. Inspiration. Transformation.
Napping Linked with Higher Stroke Risk
 By Deborah Jeanne Sergeant
By Deborah Jeanne Sergeant
Anewstudy released in a recent issue of the journal Hyperten sion indicates that daytime sleep sessions may increase risk of hypertension and ischemic stroke.
However, local experts do not lay the blame with napping itself.
The study included 358,451 UK participants. It found an association, but that does not establish a causal relationship between napping and higher stroke risk.
Many people with a sleep dis order nap to make up for their sleep deficit. For example, some people need to nap to make up for sleep
lost because of sleep apnea, a condi tion for which obesity is a high-risk factor.

Sleep apnea “very much disrupts and disturbs sleep,” said Laurie Ma lotte, sleep center coordinator at The Sleep Disorders Center in Canandai gua. “Some people can be aware of it as they snore themselves awake, coughing, gasping and panicking, short of breath. Others aren’t aware of it at all and are told by someone else there’s a problem.”
She also said that obesity is a risk factor for sleep apnea, as is COPD, congestive heart failure and hyper
tension.
“The sleep apnea can cause or ex acerbate these issues,” Malotte said.
These issues also raise risk for stroke. Napping is not directly relat ed to the increased risk for stroke. Someone who exercises and works hard but is overall healthy would have no reason to think naps lead to stroke instead of someone with med ical problems that disrupt sleep and concurrently raise risk of stroke.
“The study describes an asso ciation between frequency of naps and stroke and not a cause effect,” said Ali El-Solh, associate chief of staff for Research at Veterans Health Administration at Western New York Healthcare System in Buffalo. “First the study was based on self-reporting and not on an objective measure of naps and did not include duration of naps. So, is napping for 30 minutes, one hour, or two hours more likely to result in stroke? The article does not address this question.
“Second, napping could be indicative of another disease that could be linked to stroke. For exam ple, patients with congestive heart failure may nap more because they feel tired. Congestive heart failure is known to be associated with stroke. We assume that napping causes stroke while in reality it is a symptom of another disease linked to stroke. The bottom line is that the study raises more research questions but should not change practice or behavior yet.”
Napping can help people who occasionally need more rest. People who cannot make it through the day without napping should contact a sleep specialist to determine the un derlying reason for their lack of rest.

Soda Kuczkowski, sleep health
educator and founder of Start with Sleep in Buffalo, said a “power nap” of 10 to 20 minutes can help a person feel recharged after staying up too late or an occasional poor night’s sleep.

“Someone who is not power nap ping but sleeping 45 minutes to three to four hours: that can leave you groggy,” Kuczkowski said. “When it comes to sleep, it’s about balance.”

She referenced a study that found that people regularly napping had a sleep duration of only six hours, not eight.
“If you’re having to substitute with naps during the day, it’s a sign your sleep is not healthy,” Kuczkow ski said. “As we get older, older than 65, we revert back to childhood sleep patterns. Going to bed earlier and getting up earlier. A nap may be needed.”
But for most people, napping “is not a substitute for good, consistent sleep,” she said.
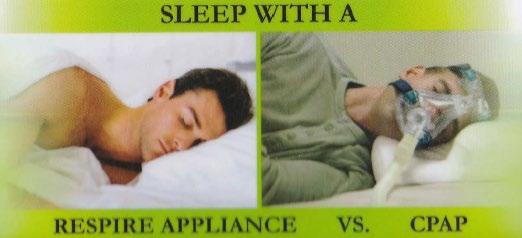
“You need sleep hygiene.”
Sleep hygiene refers to creating the right context for sleep, including a dark, cool, quiet room used. The bed should be used only for rest and intimacy, not watching television or other activities. The bedroom should be comfortably appointed and should not contain items that induce stress, such as a basket of unfold ed laundry or stack of bills. People should exercise earlier in the day, not directly before bed as that can raise their body temperature. Engag ing in quiet activity before bed and avoiding screens can help promote a restful night’s sleep.
Kuczkowski encourages clients to stick with a consistent sleep sched ule, even on weekends.
Sleep Disorder Symptoms
Page 22 • IN GOOD HEALTH – Rochester / Genesee Valley Healthcare Newspaper • October 2022
Do You Snore? Snoring can be a sign of Sleep Apnea. There are three types of apnea: obstructive, central and mixed; of the three, obstructive is the most common. People with untreated sleep apnea stop breathing repeatedly during the night, maybe hundreds of times.
If you experience any of the following symptoms, you may suffer from a sleep disorder: • Daytime fatigue • Morning drowsiness • Insomnia • Gasping for breath in the middle of the night • Snoring Can lead to: • High blood pressure • Memory problems • Impotence • Cardiovascular disease • Weight gain • Headaches • Depression Oral Sleep Appliances can be used to treat sleep apnea and snoring. This is a customized oral device worn by patients during the night to maintain an open airway (reducing snoring and sleep apnea). Oral Sleep Appliance Emery & Scuro DMD, PC has been recognized as one of the top Rochester Dentistry practices. Verified by Opencare.com $20 OFF Drs. Emery & Scuro would love to meet you. Please enjoy $20 OFF any service for your first visit! Call to schedule your appointment today! 585-247-7110 Emery and Scuro DMD, PC 2184 Chili Ave, Rochester, NY 14624 (585) 247-7110 | www.drsemeryandscuro.com Sleep Disorder
Dear Worrywart,
There are actually several differ ent types of check-in services, along with some simple technology devices that can help keep your mom safe at home while providing you some peace of mind. Here are some top options to look into.
• Check-in app: If your mom uses a smartphone, a great solution to help ensure her safety is Snug (SnugSafe.com), a free app that would check in on her every day to confirm she’s OK. This app is used by thousands of elderly seniors who live alone and want to make sure that if something happens to them, their loved ones will be notified quickly so they can receive help in minutes, rather than days.
Here’s how it works. After down loading the app, your mom will choose what time(s) throughout the day she’d like for Snug to check in. Snug will send a push notification at those times asking your mom to check in by tapping the big green check button on her smartphone screen. If she doesn’t check in within 10 minutes or respond after multiple pings, Snug will notify her emergen cy contacts and share her last known location so that she can receive fast help.
For extra peace of mind, your mom can purchase Snug’s premi um plan ($10 per month) where in addition to notifying her emergency contacts, Snug will request an in-per son wellness check by a police officer who will visit her house to confirm she’s OK and provide assistance as needed. The app works with iPhone and Android smartphones.
• Check-in calls: If your mom doesn’t use a smartphone, another option to help ensure her safety is a daily check-in call service program. These are telephone reassurance programs usually run by police or sheriff’s departments in hundreds of counties across the country and are usually provided free of charge.
Here’s how they work. A comput er automated phone system would call your mom at a designated time
mergency number. You should also check with the local county office of the aging in your mom’s area — call 800-677-1116 for contact information.
If, however, her community doesn’t have a call check-in pro gram, there are businesses like CARE (Call-Reassurance.com) and IAmFine (Iamfine.com) that offer similar ser vices for under $15 per month.

• Technology devices: You may also want to invest in some simple technology aids to keep your mom safe. One of the most commonly used devices for this is a medical alert sys tem that cost about $1 per day. These systems come with a wearable “help button” that would allow her to call for help 24/7.

Another option that’s becoming increasingly popular is smart speak ers, like Amazon Alexa or Google Home. These devices work with third-party applications — AskMy Buddy.net and MySOSFamily.com — that would let your mom to call multiple emergency contacts with a simple verbal command.
And be sure to check out Ama zon’s Alexa Together (Amazon.com/ AlexaTogether), a new $20 month ly subscription service that helps families support and keep tabs on their older loved ones who live alone through an Alexa-enabled device.
Send your senior questions to: Savvy Senior, P.O. Box 5443, Norman, OK 73070, or visit SavvySenior. org. Jim Miller is a contributor to the NBC Today show and author of “The Savvy Senior” book.

October 2022 • IN GOOD HEALTH – Rochester / Genesee Valley Healthcare Newspaper • Page 23
Buffalo Niagara Rochester Syracuse (716) 463-2966 (585) 532-5558 (315) 530-1645 www.carepatrol.com D E P AUL
Ask St. Ann’s
Why Should Seniors See a Geriatrician?
Are you ready to live a long life? Choosing the right health care pro vider for your age can help.



Just as pediatricians specialize in the growth and development of newborns through young adulthood, geriatricians help the elderly with age-related frailty and impairment maintain their best quality of life.
Serving as both the primary care provider and specialist, geriatricians focus on the prevention and treat ment of disability and disease in old er age. They provide family-centered care and work with a team of provid ers to address the medical, emotional, mental health and spiritual needs of patients and their family caregivers. Also, shared decision making around healthy aging, advanced care plan ning, and end-of-life care provide everyone with peace of mind.
Adapting to change, managing stress and bouncing back from illness becomes more challenging with age because of fewer physical, cognitive and social reserves. Trips to multi ple specialists and invasive medical treatments often only complicate matters more.
Comfort with the complexity and ambiguity surrounding most elder care situations requires geriatric ex pertise. By considering the patient’s age, values and current conditions, geriatricians help sort out the situa tion and find the best solution.
Also, unlike mainstream primary care providers, geriatricians under stand the differences between each level of care in senior living settings. Working within the regulations that govern nursing homes and assisted living facilities, they’re able to access the resources necessary to make a positive impact on an elder’s health in these environments.


St. Ann’s Community embraces geriatric care as a complement to its continuum of care philosophy. What matters most to their residents, they say, is symptom control that enables them to function as long as possible with dignity, purpose and impor tance.


A few practices from days gone by help these physicians provide the best outcomes possible:

• Care Coordination — Transi tions can leave families and patients feeling lost. The geriatrician under stands what’s going on and how it affects the big picture. The doctor reviews medications, helps interpret directions and guides patients and families through the next steps of a loved one’s care while safeguarding the advanced directives in place.
• Quality Time — A 30-minute ap pointment every quarter is common practice for geriatricians, giving am ple time to examine your loved one and consult with you and healthcare staff. The frequency picks up after an acute health event like hospitaliza tion until the person’s stabilized.
• House Calls — Best of all, geria tricians provide care at home. Mobile X-ray and laboratory services bring phlebotomy and diagnostic testing there, too.
• Support for Caregivers — Having one doctor oversee medical issues frees family and friends to handle the many other responsibilities that come with caring for a loved one, includ ing taking time for themselves.

To find a geriatrician, ask your loved one’s current primary care doctor for a referral. You might also find a local geriatrician through the Monroe County Medical Society website at www.mcms.org.
Brian Heppard is a medical doctor and cer tified medical director at St. Ann’s Commu nity and Pillar Med ical Associates, PC, a geriatrics practice pro viding outpatient care for seniors in assisted living and independent living. He is board-certified in family medicine, geriatrics, and hospice and palliative care. To learn more, visit www. pillarmedical.com.
Brian Heppard, MD
Page 24 • IN GOOD HEALTH – Rochester / Genesee Valley Healthcare Newspaper • October 2022
Carol McCoon, LMT, MS Ed, is an EM Level 4 Practioner Call (585) 742-1969 - singingwindsoundtherapy.com Email Carol for more information: singingwind00@hotmail.com Wheeler Healthy U - 308 Bluff Dr. - East Rochester Singing Wind Sound Therapy is now providing Biofield Tuning Sessions & Eminus Mirus (EM) Energy Medicine Both the Sound Healing & Distance Healing Methods Encourage: - Deep Relaxation - Increased Energy - Reduced Pain and Anxiety Sessions Available By Appointment Tuesdays & Thursdays - 8:30 am to 2:00 pm Check website for pricing. at Wheeler Healthy U in East Rochester In 2023 Make In Good Health your advertising choice Providing Independent and Enriched Living Apartments to Seniors in the Finger Lakes for over 20 years. 190 Ashton Court Clifton Springs Providing Independent and Enriched Living apartments to seniors in the Finger Lakes for over 20 years. Family Owned, Family Operated, Family Atmosphere 315.462.3140 | AshtonPlaceNY.com 190 Ashton Court Clifton Springs 315.462.3140 | AshtonPlaceNY.com
Highland’s Chief Operating Officer Set to Retire
has a reputation as a high-quality community hospital known for its patient- and family-centered, com passionate care.”
Community leaders join Excellus advisory boards
Two community leaders have joined the regional advisory and governing boards of Excellus Health Plan, Inc., and its parent and subsidi ary companies.
• Seanelle Hawkins, Ed.D., presi

dent and chief executive officer of the Urban League of Rochester, has been named as director to the Excellus Health Plan, Inc. govern ing boards of directors. Haw kins has also served for more than a year on Excellus BlueCross BlueShield’s Rochester regional advisory board.
Seanelle Hawkins
Hawkins, as leader of the Urban League, focuses on helping individ uals build self-sufficiency through education, skills development, em ployment and homeownership.
Prior to joining the Urban League, Hawkins was executive director of Sojourner Home. She also serves as a board member for RochesterWorks!, the Greater Roch ester Housing Partnership and the Women’s Council, an affiliate of the Greater Rochester Chamber of Com merce. Hawkins received her Doctor of Education from St. John Fisher University in 2013. Hawkins resides in Rochester.
• Matt Parrilli, retired manag ing partner and tax partner of the Rochester office of Pricewaterhouse Coopers (PwC), has been named as director to the Excellus Health Plan, Inc. governing boards of directors. Parrilli has also joined Excellus BCBS’s Rochester regional advisory board.
In his 37 years with the firm, Parrilli led the office on community issues and new business develop ment.
Cindy
Becker, Highland Hospi tal’s chief operating officer and vice president, has announced that she will be retiring from her position in December to spend more time with her family.

“After 34 years at Highland Hos pital, and 23 years as chief operating officer, I’ve decided that it is time to transition from my role,” said Becker. “I have thought long and hard about this, and while it is still surreal to write, I will retire on Dec. 2 of this year.”
Becker has been employed at Highland Hospital since 1988 and served as vice president and COO since 1999. During this time, the hos pital grew significantly — from an average of 50 to 60 patients in 1999 to nearly 24,000 discharges, 43,000 emergency department visits, and
14,000 operating room cases in 2021. The hospital occupancy now regu larly meets or exceeds its licensed 261-bed capacity.
Throughout her tenure, and alongside Steven I. Goldstein, president and CEO and its board of directors, Highland has achieved numerous milestones, including achieving multiple Joint Commission certifications for Evarts Joint Center, Geriatric Fracture Center, Gynecolog ic Oncology and Palliative Care.
“Cindy epitomizes excellence in leadership, compassion in com munity advocacy, and commitment to Highland Hospital, the patients it serves, and its employees and providers,” said Goldstein. “I serve as president and CEO of Highland, but I can attest that it’s because of Cindy’s leadership that Highland
“Cindy embodies Highland Hospital’s mission,” said Mark A. Eidlin, immediate past chairman of the Highland board of directors. “On behalf of the board of directors, the leadership team, all employees and providers, and most importantly, the hundreds of thousands of patients served during Cindy’s tenure, we thank her for her transformational and inspirational leadership. We are inspired by Cindy and are sincerely grateful for her dedication and devo tion to Highland Hospital.”
“As I reflect on our hospital’s history and its impact on our com munity, I am inspired and excep tionally proud. Working together, we’ve helped millions of people lead healthier lives,” said Becker. “We have created a unique and very spe cial culture that serves a higher pur pose for our patients, their families, and our employees and providers. I am confident that this will endure.”
Parrilli also serves as treasurer of
Matt Parrilli
the board of directors for the United Way of Greater Roches ter and the Finger Lakes and is chairman of its finance commit tee. Additionally, Parrilli serves on the Al Sigl Foundation board of gover nors.
Parrilli is a New York state cer tified public accountant (CPA) and a 1982 graduate of Binghamton Uni versity. Parrilli resides in Pittsford.
“As a local health plan, our mission is to help people in our communities live healthier and more secure lives through access to high-quality, affordable health care,” said Jim Reed, CEO and President, Excellus BCBS. “Our board members, with their wide range of experience
and expertise in community impact, business, health care and more, add breadth and depth to our board as we work to fulfill our mission.”
Janczak promoted to VP at Thompson Health

UR Medicine Thompson Health
recently named Mathew Janczak of Farmington as its new vice president of long-term care.

Freedom.
Janczak holds a doctorate degree in physical therapy from the Univer sity of Pittsburgh and a New York State Nursing Home Administrator license.
One year after joining Thomp son as a physical therapist in 2012, Janczak became manager of the rehabilitation services department at its 178-bed M.M. Ewing Continuing Care Center. He was named assistant administrator of the facility in 2020.
“As a valued member of Thomp son’s long-term care leadership team for nine years, Matt has established himself as a compassionate and highly-effective individual who lives our corporate CARES Values and has a deep commitment to both the staff and residents of the continuing care center,” said Thompson Health Pres ident/CEO Michael F. Stapleton Jr.
Mathew Janczak
Janczak holds a bache lor’s in systems engineering from the United States Naval Acade my. He served in three combat deployments while in the Navy, earning two Air Medals in support of Operation Iraqi
John Hayes Named Chairman of St. Ann’s of Greater Rochester Board of Directors
St. Ann’s of Greater Rochester announced the appointment of John Hayes as chairman of St. Ann’s board of directors. The SAGRI (St. Ann’s of Greater Rochester Incorporated) board of directors is comprised of a team of community leaders commit ted to St. Ann’s mission to promote the highest level of independence and physical and spiritual well-being of older adults.
“I am deeply honored to have been appointed chairman of St. Ann’s Community board of directors,” said Hayes. “There has never been a more important time to look forward to provide seniors the services they want and need, while advocating to ensure they continue to have access.”
Michael E. McRae, St. Ann’s president and chief executive officer

said, “I’m sincerely grateful to John for his commitment to sharing his talents and time as our new chair man. I’m equally excited for what the future holds, and the opportunity to work with John and our entire board of directors, to continue to positively impact the lives of older people in the Rochester area.”
Hayes is president and chief op erating officer of GLC Business Ser vices. GLC provides on-site support services for professional firms across the country and management con sulting services to the legal industry.
“We are incredibly fortunate to have him at Thompson.”
October 2022 • IN GOOD HEALTH – Rochester / Genesee Valley Healthcare Newspaper • Page 25 Health News Hayes resides with his wife Dorothy in Irondequoit. He enjoys spending time with family including his 10 children, 26 grandchildren, and one great grandchild.
John Hayes


Acupuncture Center USA 7th Generation Rui Wang, LLC Clinton Crossings Medical Center Building C, Suite 105, 919 Westfall Road, Rochester, NY 14618 Tel1: 585-358-6186; Tel2: 315-378-5556; Tel3: 607-372-2082 Ancient Wisdom Integrated with Modern Medicine LIFE CHANGING MEDICINE, MOVING MEDICINE FORWARD ONE OF THE BEST ACUPUNCTURE CENTERS IN THE WORLD Acupuncture is a general practice alternative medicine, it can help a wide range of health problems at different extents. Ask for professional, confidential, personalized evaluation / consultation appointment before starting any treatment Balance Immune System Build Stronger Immunity www.AcupunctureCenterUSA.com 7th Generation Medical Acupuncture Rui Wang, MD of China, L.Ac. Featuring RUI Anti-Inflammatory Acupuncture, Medical Oncology Acupuncture, and Neuromedicine Acupuncture Pain? And Hard to Relieve? Autoimmune Diseases? Neuropathy? Arthritis? Cancer Care? Post-COVID-19 Conditions? Experienced in both Western Medicine & Traditional Chinese Medicine Experienced in both Academic & Private Practice Experienced in both Basic Science & Clinical Science Experienced in Cancer Research at Major Medical Centers in USA THE WORLD’S GREATEST TREASURE OF MEDICINE
CALENDAR
HEALTH EVENTSof
Oct. 8
Walk to End Alzheimer’s starts at Frontier Field
Rochester area residents will join the fight to end Alzheimer’s disease at the Alzheimer’s Association Walk to End Alzheimer’s — the world’s largest event to raise awareness and funds for Alzheimer’s care, support and research. The event will take place starting at 9 a.m. (registration), Oct. 8, at Frontier Field.
To register and receive the latest updates on this year’s walk to End Alzheimer’s, visit alz.org/walk.
For more information, visit alz. org or call 800.272.3900.
In New York state alone, there are more than 410,000 people living with the disease and 563,000 caregiv ers.
Oct. 4, 20, 25
Hearing loss group holds meetings
Hearing Loss Association of America /Rochester Chapter is hold ing several meetings in October. They
are free and open to the public.
— Oct. 4
• 10 to 11 a.m. Hearing Other People’s Experiences (HOPE). In person. St. Paul’s Episcopal Church, East Avenue at Westminster Road, Rochester, 14607 across from the George Eastman Museum.
Prospective, new or experienced hearing aid users can share their ex periences, questions and hearing loss journeys in an informal discussion.

• 11 to 11:30 a.m. Socializing. In person. St. Paul’s Parish Hall.
• 11:30 a.m. to noon. Business meeting and announcements. In per son. St. Paul’s Parish Hall.
• Noon to 1 p.m. Your identity as a person with hearing loss. In person. St. Paul’s Parish Hall and virtual on Zoom. Speaker: Michael Harvey, clinical psychologist who has written over 50 articles about hearing loss. He also published a book, titled “Listen with the heart: Relationships and Hearing Loss and The Odyssey of Hearing Loss: Tales of Triumph.”
— Oct. 20
• 10 a.m. to 2 p.m. Assistive listening devices demo center. Tech nology Team. In person. Lifespan, 1900 S. Clinton Ave, Rochester. At
this free demonstration area, con sumers are invited to view and try out a selection of assistive listening devices before actually buying them. Included are captioning-capable and amplified telephones, signaling-alert ing devices and smart phone APP’s related to hearing enhancement . Chapter members are on hand to answer visitors’ questions.
— Oct. 25.
8 to 9 p.m. “Hear Together.” Pre sented by Kristin Bergholtz, speech language pathologist. Virtual on Zoom. Learn more about your child’s hearing loss, services to benefit them, and tips to support their language development while connecting with other advocates of these youngsters. To register, contact kristinbslp@ gmail.com
For more information, view the organization web site at hearingloss rochester.org or telephone 585 266 7890.
Oct. 13
Expert to talk about ageism

Lifespan is hosting a free talk by Tracey Gendron, Ph.D., author of “Ageism Unmasked: Exploring Age Bias & How to End It,” from 5:30 to 7 p.m., Thursday, Oct. 13, at the Rochester Museum & Science Cen ter’s Eisenhart Auditorium, 657 East Ave., Rochester. Gendron is chair woman of the department of geron tology at Virginia Commonwealth University. She says, “Everything you know about aging is wrong. It’s
not your fault. Everything you’ve been taught about aging is wrong.” Light appetizers will be served from 5:30 to 6 p.m. followed by Gendron’s presentation.
Reservations are required by Oct. 6 at www.lifespanrochester.org or by calling 585-244-8400.
Oct. 17
Nurse to speak about resiliency
Tim Cunningham, vice president of practice and innovation at Emo ry Healthcare, will deliver the 2022 Sischy Lecture at 6 p.m., Monday, Oct. 17, at the Rochester Academy of Medicine, 1441 East Ave., Roches ter. His talk, “Keeping Wellness and Resilience Relevant while Riding the Waves of Our New Normals,” focus es on well-being support for physi cians and staff in healthcare settings.
Cunningham holds an appoint ment as adjunct assistant profes sor at the Nell Hodgson School of Nursing at Emory University. He is a fellow in the American Academy of Nursing. His publications focus on compassion and wellness. He has co-authored textbook, “Self-Care for New and Student Nurses” where he challenges the way healthcare pro viders approach the critical practices of caring for themselves so that they may care for others.
The lecture is free and open to the public. To register, go to http:// event.urmc.edu/sischy22. For more information, contact Brooke Whowell at 585-276-4716.
EXERCISE
TRY SOMETHING NEW
or old
Community Check-in. Find it wherever you listen to podcasts.
October 2022 • IN GOOD HEALTH – Rochester / Genesee Valley Healthcare Newspaper • Page 27
A nonprofit independent licensee of the Blue Cross Blue Shield Association CARING FOR THE WHOLE YOU. BODY AND MIND. Now more than ever, your emotional wellbeing is key to overall health. Having meaningful connections with others is important for both physical and mental health. CONNECT Spend time with family and friends. Connections and support are important for your emotional health.
You don’t have to pump iron or run a marathon. Short walks around the block throughout the day have big benefits.
Find a new hobby
one. Or sign up to volunteer somewhere. You’ll give your brain and mood a boost. Check out our podcast episode, “An Honest Conversation About Mental Health” in the
Page 28 • IN GOOD HEALTH – Rochester / Genesee Valley Healthcare Newspaper • October 2022






























 By John Addyman
By John Addyman





 MARYCARIOLA.ORG
MARYCARIOLA.ORG








 By Mike Costanza
By Mike Costanza



 TOP: Anita O’Brien (left) is the founder and executive director of Rochester Accessible Adventures. Next to her is Dee Mascari, the group’s inclusion specialist.
RIGHT: Special kayak seats help paddlers with disabilities stay upright and little pontoons called outriggers keep the crafts from tipping over.
BOTTOM: Members of the Rochester Rockets basketball team.
TOP: Anita O’Brien (left) is the founder and executive director of Rochester Accessible Adventures. Next to her is Dee Mascari, the group’s inclusion specialist.
RIGHT: Special kayak seats help paddlers with disabilities stay upright and little pontoons called outriggers keep the crafts from tipping over.
BOTTOM: Members of the Rochester Rockets basketball team.













































 By Deborah Jeanne Sergeant
By Deborah Jeanne Sergeant