






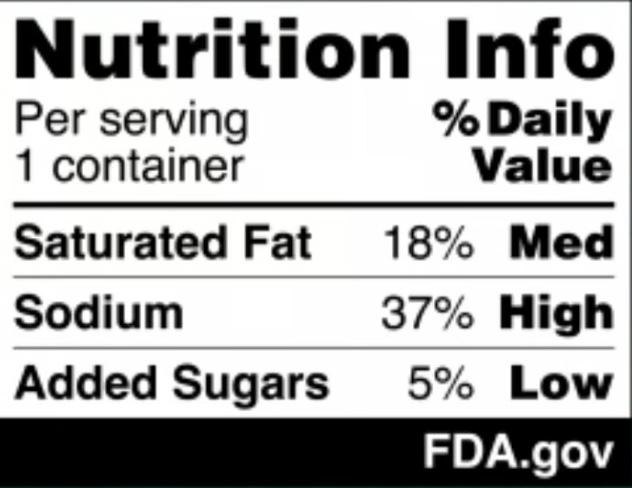
The U.S. Food and Drug Administration (FDA) has proposed a new rule requiring bold, easyto-read nutrition labels on the front of food and beverage packages.
These labels, which would highlight content of sugar, salt and saturated fat, aim to make it easier for shoppers to make healthier choices in the grocery aisle — helping to tackle the rising rates of obesity and conditions such as Type 2 diabetes, heart disease and high blood pressure, a media report from The New York Times states.
These chronic illnesses affect over 60% of American adults and contribute to an estimated $4.5 trillion in annual health care costs, according to the FDA.
“Nearly everyone knows or cares for someone with a chronic disease that is due, in part, to the food we eat,” physician Robert Califf, the commissioner of the FDA, said in a statement released by the administration. “It is time we make it easier for consumers to glance, grab and go.”
The black-and-white labels would appear on the front of products, unlike the current back-of-package Nutrition Facts panel, which lists dietary facts such as calorie counts, serving sizes and ingredients.
The new proposal is the result of three years of research by FDA scientists, who studied similar frontof-package labeling systems used in
Focus group testing of 10,000 people found that the proposed labels were easier to understand and effective at conveying nutrition information, according to the FDA. If the labels are finalized, food manufacturers would have up to four years to comply.
countries like Canada, the United Kingdom and Chile.
consumers, although we wish the administration had selected a nutrition warning format which is more likely to favorably affect purchasing decisions,” Peter Lurie, executive director of the Center for Science in the Public Interest, an advocacy group that first petitioned the FDA to require frontof-package labels in 2006, told The Times.
Focus group testing of 10,000 people found that these proposed labels were easier to understand and effective at conveying nutrition information, the FDA said.
If the labels are finalized, food manufacturers would have up to four years to comply.
weak” to address the real dangers of ultra-processed foods, which make up a majority of calories consumed by Americans regularly.
Some experts believe the frontof-package labels could encourage food companies to reformulate products to avoid “high” levels of sugar, salt or fat.
9.75” WIDE X 6.69” HIGH
The proposed rule has drawn praise and criticism.
“This proposal is a real step forward in our efforts to better inform
The food industry, however, pushed back. Sarah Gallo of the Consumer Brands Association said the labels lack important details, such as calorie counts and the presence of nutrients essential for a healthy diet.
Senator Bernie Sanders also criticized the plan, calling it “pathetically
“If you're a retailer selling something that's just above the threshold, you have a lot of incentive to take a little bit of sugar out of your breakfast cereal so it doesn't bear the high label,” Anna Grummon, the director of the Stanford Food Policy Lab, told The Times. “That's a win for consumers.”

At Hematology-Oncology Associates of CNY, you are never just a diagnosis or a number. We see you...the whole person, with passions, hopes, dreams, histories, and loved ones who share in your journey. From diagnosis, to treatment, to survivorship – our personalized care focuses on truly understanding and planning for your unique needs. We provide genuinely compassionate support, collaborating with you, your family, and caregivers every step of the way. Learn more about HOA today. We’ll see you and care for you – body, mind and spirit.



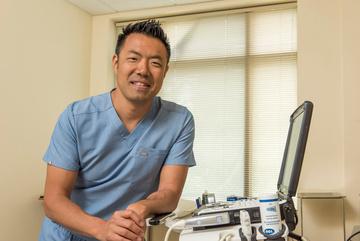
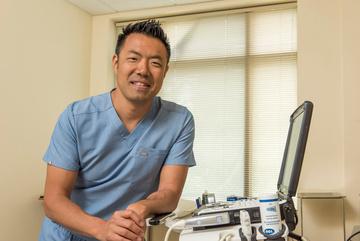
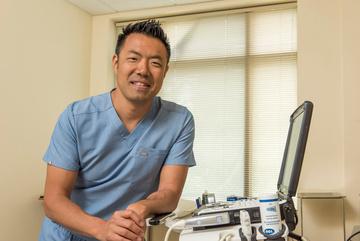
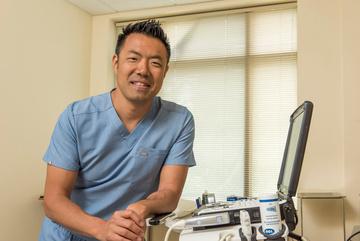
By Chris Motola
Q: You practice an unusual combination of specialties: emergency medicine and palliative medicine. Which did you start with and how did you come to be interested in the other?
A: I did emergency medicine first. I trained in Wisconsin and then practiced emergency medicine for around five years. I found that there were some themes that came up in emergency medicine one of which was seeing people with a lot of chronic disease who would come to the ED and then need a lot of emergency medicine-based testing done that ultimately didn't help them feel better or provide more clarity on
why they were sick. So it seemed like there was this cohort of patients who were missing out on symptom management and support. That started to shift my interest toward how to take care of that population outside of the ED.
Q: What types of patients would this describe?
A: I always felt like taking care of cancer patients in the ER was a difficult but meaningful experience because when they hit the ED they're usually pretty sick and there's a lot of complexity in figuring out why they might be sicker. And, in some

ways, I just felt a connection to that population in terms of providing care for them. Palliative care gives me some upstream interaction with these patients before I see them in the ER. So that cultivated an interest. I also knew an ED doctor who had transitioned into working in palliative care. And he wrote these notes that were unlike any other notes I'd read. They kind of addressed the whole of the person instead of just the medical problem, like maybe things were more complex for that person. I wanted more of that in my life, so I reached out to him and that started the process of getting into a fellowship and training.
Q: I think a lot of people tend to confuse palliative with hospice care since they're often paired together. How would you describe it in the context of emergency medicine?
A: It's a little tricky to answer in terms of how it integrates into emergency medicine. It's parallel care throughout the healthcare system. It's symptom management care for people who are receiving active treatment for all sorts of different diseases. We're focused on making sure that, despite the treatment of the disease — some of which can make the patient sicker in the process of getting better, like chemotherapy — we're managing the leftover symptoms whether it's pain, shortness of breath, anorexia, nausea. So we're doing parallel treatment for that in a way that has nothing to do with hospice.
Q: What would be an example of how that upstream and parallel knowledge can help you be more effective in the ER?
A: Someone described palliative medicine as being a black bag specialty. To me that means it's a really individualized approached, like if you were seeing a patient at home. It all plays into the person's life beyond the disease. When they're in the ER, I'll know what they need in terms of testing, but I also might know what it is they want to talk about in terms of what they want to get out of the visit. We may want to go through it like any other ER visit and often that will be the case since they're there for ER medicine. But when we get results from the test there's a better sense of what we do with that info. Sometimes it helps shape a different plan even if they're admitted to the hospital, in which case I'll see them there in my palliative care role. And it helps them because they know me from another context. While it's unfortunate in one regard, I do get a lot of professional satisfaction from being able to follow them from one context to another. And I do oversee palliative care in a hospice context as well, so if patients do get sicker I can help them understand what those services offer.
Q: How important is institutional support in balancing these roles?
A: It's of very high-level importance. FF Thompson has been supportive of the entire process. When I left to do the fellowship training and
looking for a way to combine the two jobs, Thompson created a position to combine those job descriptions. The University of Rochester was also very supportive of the appointment process part of it. It's been really helpful to have all the professional connections that I have with people through that division even working exclusively through Thompson. There's a lot of opportunity to collaborate on very complicated cases. I don't think it would have even been possible without a supportive community institution and the affiliation with a supportive university system. I talk to people who do these types of splits and I think what I have here is very unique.
Q: How do you allot your time between the two?
A: I basically have a 50/50 split between emergency medicine and palliative care.
Q: The pacing of those two specialties has to be very different. How do you switch between them effectively?
A: There is a huge difference when there's no overlap. The skills I have in palliative care help with understanding pain medications and things like that, but for the most part it's its own thing. With palliative medicine there's probably more integration of emergency medicine because these cases are usually pretty complicated. There are some days where it's harder than others to flip between roles, but more and more it just feels like a spectrum of care. I'm not a surgeon, but it might be comparable to being in the operating room versus the clinic.
Q: Do you have any advice to other physicians who are looking to adopt hybrid practices?
A: I think mentorship is pretty important but also just finding something you're interested in, have the aptitude and can persevere in along with whatever primary training you're in. I think mentorship can really help with that. When you partner with someone who trusts and sees your potential you can gain the confidence to pivot to something that may be difficult but can open up more opportunities to you.
Name: Adam Cardina, M.D.
Position: Emergency medicine and palliative care physician at FF Thompson Hospital
Education: Medical College of Wisconsin; University of Rochester Medical Center
Certifications: American Board of Emergency Medicine
Hometown: Trumansburg
Affiliations: FF Thompson
Hospital; Strong Memorial Hospital
Organizations: UR Homecare Board
Family: Wife, three children
Hobbies: Outdoor activities, water sports, skiing, music, cars

For many, coffee is a beloved morning ritual, fueling the day ahead. But what if the time you drink it could influence how long — and how well — you live?
New research published Jan. 8 in the “European Heart Journal” suggests that when you enjoy your cup of Joe might be just as important as how much you drink.
The study shows consuming coffee only in the morning was linked to a 16% lower risk of premature death and a 31% reduced risk of dying from cardiovascular disease compared to non-coffee drinkers.
"This is the first study testing coffee drinking timing patterns and health outcomes," lead study author Lu Qi, a professor of public health at Tulane University, said in a news release.
"We don't typically give advice about timing in our dietary guidance, but perhaps we should be thinking about this in the future."
Researchers analyzed data from over 40,000 adults aged 18 and up using dietary records collected between 1999 and 2018. Coffee consumption was divided into three timeframes: morning (from 4 a.m. to 11:59 a.m.), afternoon (from 12 p.m. to 4:59 p.m.), and evening (from 5 p.m. to 3:59 a.m.)
Results show that those who
drank coffee exclusively in the morning benefited the most in terms of longevity and heart health.
Meanwhile, folks who drank coffee throughout the day saw no significant reduction in risk.
The findings held true regardless of whether participants drank caffeinated or decaffeinated coffee, and the amount consumed — whether they drank less than one cup or more than three — didn't impact the benefits.
So, why does timing matter?
Experts agree that the timing of coffee intake may influence your circadian rhythm and hormone levels. Drinking coffee later in the day, even if we feel like we need it, may disrupt melatonin production, a hormone that regulates sleep and influences heart health.


Back a s ou d ot ea us o , screw and lengthy recoveries. Regenerative Medicine is changing how back pain is solv
According to study authors, some inflammatory markers in the blood have their own clocks. And the anti-inflammatory effects of coffee may be more effective when consumed in the morning, when these markers peak.
However, the study was observational and cannot prove causation, noted Vanessa King, a registered dietitian nutritionist and spokesperson for the Academy of Nutrition and Dietetics who wasn't involved in the study, told CNN.
Stop missing life’s greatest moments Stop planning life around pain
Stop missing life’s greatest moments Stop planning life around pain
Stop missing life’s greatest moments Stop planning life around pain
A monthly newspaper published by Local News, Inc. Distribution: 33,500 copies throughout more than 1,500 high-traffic locations.
In Good Health is published 12 times a year by Local News, Inc. © 2025 by Local News, Inc. All rights reserved. P.O. Box 525, Victor NY 14564. Phone: 585-421-8109 • Email: Editor@GVhealthnews.com
Editor & Publisher: Wagner Dotto • Writers: Deborah J. Sergeant, Chris Motola, George Chapman, Gwenn Voelcker, Anne Palumbo, Jim Miller, Mike Costanza Shaina Zazzaro, Eva Briggs (MD), Mark Winsberg (MD)
Advertising: Anne Westcott (585-421-8109) • Linda Covington (585-750-7051)
Layout & Design: Angel Campos–Toro • Office Secretary Allison Lockwood
No material may be reproduced in whole or in part from this publication without the express written permission of the publisher. The information in this publication is intended to complement—not to take the place of—the recommendations of your health provider. Consult your physician before making major changes in your lifestyle or health care regimen.
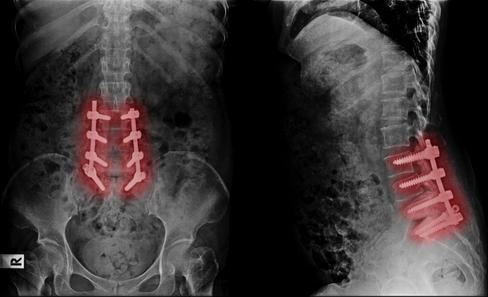
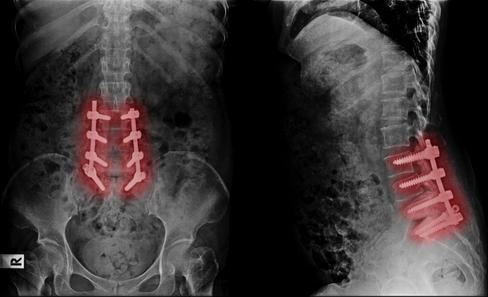
Back Pain should not mean fusion, screws, and lengthy recoveries Regenerative Medicine is changing how back pain is solved.
Back Pain should not mean fusion, screws, and lengthy recoveries. Regenerative ng how back pain is solved
Stop missing life’s greatest mome planning life around pain. B k P in should not mean fusio i Regenera g g w back pain

’s greatest moments. Stop around pain mean fusion, screws, e l d
Back Pain should not mean fusion, screws, d l th eries Regenerative ow back pain is solved. ur last stop ur life! V


Rich last stop
your last stop Th e your life! Y O U







By George W. Chapman

As previously reported, the Inflation Reduction Act (IRA) caps out-of-pocket copays for drugs at $2,000 annually starting this year. This is great news for seniors, many of whom paid a lot more than $2,000 a month in copays.
Unfortunately, the $2,000 cap does not apply to consumers covered by employer commercial plans. Medicare is able to cover the additional cost associated with the $2,000 cap by paying billions less for drugs. That is accomplished by the Inflation Reduction Act (part two) which gives CMS the authority to finally negotiate prices with manufacturers.
Until the IRA, negotiating drug prices was literally prohibited by law which is testament to the power wielded by the drug manufacturers lobby. CMS is allowed to negotiate the price of 10 drugs effective next year. Congress has begrudgingly agreed to allow CMS to negotiate. Why not negotiate all drugs, you ask? It might have a little to do with campaign contributions from the drug lobby. In 2023, members of both sides of the aisle received an average of $57,000. Be that as it may, 10 is better than nothing. If the new administration is looking to cut costs, then what Medicare pays for drugs is a great place to start.
Medical debt has forced many people into personal bank ruptcy. The $2,000 cap on out-of-pocket costs for drugs estab lished by the Inflation Reduction Act may well prevent many bankruptcies for seniors in the future. The Federal Consumer Financial Protection Bureau just issued regulations which (at least) bars medical debt from affecting your credit rating. Credit agencies cannot include your medical debt on credit reports. The regulation also precludes lenders from considering medical debt when considering loans for borrowers. But despite the media

The chart below shows the negotiated price, deemed the MFP or maximum fair price, (fair to whom?) of the 10 drugs prices effective next year, versus the average price paid by countries with universal healthcare. (I couldn't find the current 2025 price per drug paid by Medicare.)
Despite our best effort at negotiations, we are still paying way more than other countries. Imagine the copay for Imbruvia at $10,619 a dose without the $2,000 cap!
The second chart shows the approximate total population in millions of the countries that pay (still) far less than the US despite our-soonto-be "reduced" 2026 price. Medicare
Jardiance $204 $52 $152
Farxiga $182 $54 $128
Eliquis $249 $76 $173
alone covers 70 million people. That is more than the total population of seven of the 10 countries listed. Where is our strength in numbers when it comes to negotiations? Where is our volume discount? The amount of money that would be saved if Medicare could negotiate on behalf of our total population (335 million) would be hundreds of billions. I'm including the savings that would also be achieved by commercial insurers as well. But until the stranglehold the drug lobby has on congress is eliminated, don't expect much improvement in healthcare costs let alone delivery. Austrailia 28 Canada 42 France 70
Enbrel $2,335 $764 $1,571
Januvia $117 $39 $78
Novolog $134 $50 $84
Xarelto $200 $82 $118
Entresto $314 $139 $175
Imbruvia $10,619 $5,670 $4,949
Stelara $4,490 $2,822 $1,668
frenzy and uproar over healthcare equity created by the murder of United Healthcare CEO Brian Thompson, don't expect any substantial changes to how healthcare is delivered for the foreseeable future.
Understandably, post-COVID-19, we are hyper aware of any potential epidemic. Bird flu has been getting a lot of attention lately. As of early January, there has been just one death attributed to bird flu or the H5N1 virus. The deceased was a senior (older than 65) resident of Louisiana with multiple underlying medical conditions. He was exposed to a backyard flock of wild birds. To date, there has been no indication the virus
if any patients are directly impacted by physician charges as third-party insurance establishes physician reimbursement. Withdrawing from Medicare and commercial insurance and going 100% self-pay is financial suicide. Compounding the Medicare cut is the potential for commercial carriers to mimic Medicare reimbursement and lower their physician payments. The Medicare cut is just another reason for physicians to eschew private practice.
Hacking patient records costs U.S. healthcare almost $2 million a day. In the past six years, breaches have cost U.S. healthcare almost $22 billion. Healthcare organizations incur 17 days of down time per occurrence, according to a report by Comparitech. Six hundred and thirty-four attacks in the last six years affected more than 88 million patient records. Razor-thin operating margins make total cyber security impossible. Medicare and commercial payments do not take into consideration the added costs of cyber security. The advent of AI will only make it easier for the bad guys to hack into information systems. To add insult to injury, Medicare actually penalizes healthcare organizations when they are hacked.
is spreading person to person.
The January bill to fund the govern ment another three months did not include a provision to halt an illogical and unfair 2.8% cut in Medicare physician reimbursement. Considering that inflation is hovering around 3%, the 2.8 % reduction is tantamount to a 5.8% cut. Like all businesses, medi cal practices content with increasing labor, supply and insurance costs. But unlike other businesses, medical practices cannot compensate for ris ing costs by increasing charges. Few
If you're having trouble finding a mental health provider, you're not alone. Roughly half of mental health providers accept insurance and almost as many don't accept new patients. According to a Wall Street Journal survey, only 44% of Ph.D.s and psychologists accept insurance, let alone new patients. Many people are frustrated because the dearth of in-network providers creates long wait times of often several months. Online therapy is attempting to fill the void. Forbes Health has rated online providers. The top nine are: BetterHealth, Talkiatry, Cerebral, Talkspace, Brightside, Regain, Team Counseling, Faithful Counsel and Our Ritual. Services include depression, anxiety, stress, anger management, insomnia, panic attacks, eating disorders, trauma, relationships, life counseling, bereavement and more. Per Forbes, the best online therapy options were broad telehealth sites that include therapists: Amwell, Doctor On Demand and MD Live. You can get traditional therapy appointments focused on live video sessions. Ongoing therapy may require a subscription. It is best to contact your insurer before proceeding.


George W. Chapman is a retired healthcare business consultant who worked exclusively with physicians, hospitals and healthcare organizations. He used to operate GW Chapman Consulting based in Syracuse.

The cancer death rate continues to decline in the U.S. but new cases are rising among women, potentially undermining progress against the nation's second-leading killer, according to a new report from the American Cancer Society (ACS).
The cancer death rate declined by 34% between 1991 and 2022, representing about 4.5 million deaths averted by early detection and improved treatments, the ACS said in its Cancer Statistics 2025 report published today.
However, new cancers among women and younger adults are increasing, the report found.
What's more, Native American and Black people still have much higher cancer death rates than whites.
“Continued reductions in cancer mortality because of drops in smoking, better treatment and earlier detection is certainly great news,” lead researcher Rebecca Siegel, senior scientific director of surveillance research at the American Cancer Society, said in a news release.
“However, this progress is tempered by rising incidence in young and middle aged women, who are often the family caregivers, and a shifting cancer burden from men to women, harkening back to the early 1900s when cancer was more common in women,” Siegel said.
For example, cancer rates among women 50 to 64 have now surpassed those of men, with about 832 versus 830 cases for every 100,000 people, the report says.
And women younger than 50 now have an 82% higher cancer rate than men that age, about 141 versus 77 cases for every 100,000.
This shift can be partially blamed on increases in breast and thyroid cancers, which make up nearly half of all cancers in this age group and mostly impact women, the report stated.
Cancer rates in men younger than 50 are increasing for the four leading cancers — colon, testicular,
kidney and leukemia — but are offset by declines in cancers like melanoma, non-Hodgkin lymphoma and prostate.
Additionally, “alarming inequalities in cancer mortality persist,” an ACS press release says.
Native American people bear the highest cancer death rates, and are two to three times higher than white people to die from kidney, liver, stomach, and cervical cancers, the report says.
And Black people are twice as likely as white people to die of prostate, stomach, and uterine corpus cancers, and 50% more likely to die from cervical cancer, which is preventable, according to the report.
“Progress against cancer continues to be hampered by striking, wide static disparities for many racial and ethnic groups,” senior researcher Ahmedin Jemal, a physician and senior vice president of surveillance and health equity science at ACS, said in a news release.
“It's essential to help end discrimination and inequality in cancer care for all populations. Taking this step is vital to closing this persistent gap and moving us closer to ending cancer as we know it, for everyone,” Jemal added.
Other findings from the report:
• Progress is lagging against pancreatic cancer, which is the third-leading cause of U.S. cancer deaths. New cases and deaths are both increasing, and the five-year survival rate now stands at just 8% for nearly all cases.
• New colon cancer cases are rising among men and women younger than 65.
Cervical cancer cases have increased in women 30 to 44.
• Cancer cases among children 14 and younger have declined in recent years, but continue to increase among teens 15-19.
• Cancer death rates have dropped by 70% in kids and 63% in teens since 1970, largely due to improved treatments for leukemia.






By Gwenn Voelckers
By Gwenn Voelckers
In 1993, I purchased the home I still live in today.
At the closing, I became the proud owner of someone else’s dream home, complete with bright green shag carpet, a Pepto Bismal pink powder room and lacy bedroom curtains hanging in the living room.
What was I thinking?!
But I was convinced of the home’s potential and began a gradual, thoughtful and very rewarding process of making this home my own.
Looking back, I now realize that creating a home that is joyful, inspiring and uniquely mine was one of the most empowering things I did for myself after my divorce.
It was an essential part of starting my life over as a woman on her own.
If you are now living alone — whether due to a divorce, the loss of a partner or some other major life change — know that, while daunting, a fresh start can be incredibly liberating.
Designing your space for the person you are now, not the person you used to be, can support your journey toward happiness and fulfillment.
Let your home be your launchpad for the next phase of your life.
So, how do you design a space that reflects your singular style and spirit, especially if you are navigating
life on your own for the first time?
Here are some insights and tips that have helped me along the way.
Intuitively, I knew I needed to walk through my new front door and into my very own “warm embrace,” a place where I would be surrounded and uplifted by all things familiar and friendly.
So, I set out to create a retreat — a personal sanctuary where I could feel safe and sound, inspired and creative.
One of the first things I did when I bought my home (after I tore out the green shag carpet) was to frame and display photographs of family and friends. I wanted to see their faces when I entered a room, to be reminded of good times and the love that surrounds me.
In addition to photos, I adorned my living space with original pieces of art (now more boho!) and artifacts or souvenirs I collected on my travels. These cherished mementos and images lifted my spirits back then and continue to do so.
I encourage you to surround yourself with treasured items that reinforce both who you are and who you want to become. Whether it’s art, books you love, fresh flowers or
a favorite blanket, infuse your space with décor and possessions that make you smile.
Japanese author and organizer Marie Kondo’s famous phrase, “Does it spark joy?” became my mantra when I started the process of decluttering.
As she instructed, I took a deep breath and asked myself: "Does this truly make me happy? Does this piece of furniture, these old clothes, or that vase from my wedding still bring me joy?"
It was hard at first. There were items that carried sentimental value or that I thought I should keep because "that’s what you do." But once I embraced the idea of letting go of anything that didn’t spark joy, I felt an incredible weight lift off my shoulders.
If an object doesn’t bring you joy, let it go. By clearing your space of things that no longer align with who you are today, you make room for the things that truly do resonate with the person you aspire to be.
I’ll get to the point: Anything that makes you feel bad when you look at it should be thrown out, donated or repaired. Ratty dishtowels, old lampshades and faded curtains, for example, can dampen your mood and erode your self-esteem.
Don’t underestimate the negative power of unsightly or outdated objects.
I walked into my kitchen last week and cringed (for the 100th time) when I looked at my faded and frayed kitchen mat. I threw it out and grabbed a small oriental rug from my guest bedroom to put in its place. It looks and works great! Yes, it’s a little unconventional for the kitchen, but I feel good every time I see it. What took me so long? I need to
follow my own advice!
Create Spaces That Inspire, Lift You Up and Nurture Personal Growth
One of the most powerful things about living alone is that you have the freedom to design your home exactly how you want it. No compromises, no negotiations. You get to choose every color, every piece of furniture and every layout.
Over the years, I’ve come to realize that my home is more than just a place to live — it’s a place that inspires and supports my continuously evolving self.
For example, as my passion for music grew, my home gradually transformed into a tangible expression of this newfound love.
My living room now sports my drum kit, bongos and assorted percussion instrument. Again, unconventional, but it reflects who I am today.
Designing spaces in your home that nurture your growth — whether it’s a meditation corner, a cozy writing desk or a place for artistic expression — can help you move forward.
Creating a home that is joyful, authentic and aligned with your true self is one of the most empowering things you can do for yourself.
Remember, you are not defined by your past, your circumstances or your former relationships. Your home can become an oasis of creativity and independence — a place that’s unconditionally yours, absent of compromise. Claim it.
Once you make your personal space your own, there’s no place like home!
Gwenn Voelckers is the author of "Alone and Content," a collection of inspiring essays for those who live alone. She welcomes your comments about this column and topic suggestions for future columns at gvoelckers@rochester.rr.com
Too much screen time can sabotage preschoolers' sleep, potentially turning them into terrors around the house, a new study warns.
Bad sleep can exacerbate children's struggles with poor attention, hyperactivity and moodiness, researchers reported Dec. 12 in the journal “Early Child Development and Care.”
Worse, kids can wind up in a downward spiral, with screen time and poor sleep feeding off each other.
“Our results suggest the presence of a positive feedback loop, wherein increased screen time and sleep disturbances exacerbate each other
through cyclic reinforcement, heightening the risk of hyperactive attention problems, anxiety and depression,” said researcher Bowen Xiao, an expert in children's socio-emotional functioning and developmental psychopathology with Carleton University in Canada.
For the study, researchers surveyed the mothers of 571 preschool children between the ages of 3 and 6 who were attending seven public kindergartens in Shanghai.
Moms reported the amount of time their kids spent with a TV, smartphone, computer or other screen device. They also answered questions to assess any behavioral

problems their kids might have, as well as the quality and duration of their sleep.
“Our results indicate that excessive screen time can leave the brains of preschool children in an excited state, leading to poor sleep quality and duration,” said researcher Yan Li, an expert in preschool education from Shanghai Normal University.
Researchers also noted that prior research has indicated that screen time can lead to hyperactivity and emotional problems among kids.
This study suggests that screen time might be the reason why, researchers said.
“This poor sleep may be due
to postponed bedtimes caused by screen viewing and the disruption of sleep patterns due to overstimulation and blue-light exposure,” added lead author Shujin Zhou, a doctor of psychology with Shanghai Normal University.
“Screen use might also displace time that could have been spent sleeping and increase levels of physiological and psychological arousal, leading to difficulties in falling asleep,” Zhou said in a journal news release.
These results could point the way toward future treatments for hyperactivity and mood problems among young children, Zhou said.
By Eva Briggs, MD

On Jan. 3, the United States Surgeon General Vivek Murthy issued an advisory regarding the link between alcohol consumption and cancer risk.
An important reason for this advisory is the general lack of awareness among the general population that alcohol increases the risk of cancer.
Less than half of people know that alcohol is a cancer risk factor.
It’s the third most common preventable risk factor after tobacco and obesity.
The data is not new. It is the culmination of many studies over the past several decades.
First the definition of what constitutes a serving of alcohol. A standard drink contains 14 grams (0.6 fluid ounce) of pure alcohol. This is the amount found in 5 ounces of wine, 12 ounces of beer, or 1.5 ounces of liquor.
Previous recommendations advised that up to one drink per day for women or two drinks per day for men, was a safe limit. But the evidence now shows that drinking even at low levels imparts an increased risk for cancer.
How can alcohol cause cancer? There are at least four known ways.
• First, alcohol breaks down in the body to a chemical called acetaldehyde. This substance harms DNA. Damaged DNA can allow a cell to grow uncontrollably leading to cancer.
• Second, alcohol also produces reactive forms of oxygen leading to oxidative stress which damages DNA, proteins and cells.
• Third, alcohol alters many hormones. It increases estrogen levels which increases the risk of breast cancer.
• Fourth, alcohol dissolves other cancer-causing chemicals such as those found in cigarette smoke. It also alters the cells of the mouth and throat. This makes those toxic substances more easily absorbed, raising the chance of mouth and throat cancers.
Drinking alcohol increases the risk of seven types of cancer:
1. Mouth and oral cavity 2. throat
Over my career I have cared for patients with every one of these cancers.
Quitting or reducing alcohol won’t prevent all of these cancers. But all of them are so unpleasant that reducing the chance of acquiring any of these diseases is worth considering.
How significant is the risk of cancer from drinking alcohol?
The risk that a woman who drinks less than one drink per week will develop cancer in her lifetime is about 17 per 100 individuals. One drink per day increases that risk to 19 per 100 individuals and two drinks per day further increases the risk to 22 per 100 people. That means that five more women out of 100 (or one out of 20) who drink higher levels of alcohol will develop cancer during their lifetime.
For men, the risks are about 10% for those who drink less than one drink per week, to 11% for those who drink one drink per day and 13% for those who drink two drinks daily.
The surgeon general report made the following suggestions for steps to reduce alcohol-related cancers.
Update the health warning label on alcoholic beverages to warn about cancer risks. Reassess the recommended limits for alcohol consumption. Increase efforts to expand general awareness and educate the public. Inform patients during clinical encounters about the link between alcohol consumption and cancer risk.
We already know from past experience — prohibition — that making alcohol illegal is not the answer. But it’s up to us health care providers to make the public aware of these facts so that people can make informed decisions.
















Founder of Rochester Accessible Adventures talks about how her nonprofit has worked to improve access to places for thousands of people with disabilities

Q. Your website states that RAA was founded because of a recurring problem. What was that problem?
A. The problem is when people wake up on Saturday and they turn to their family and say “What do you want to do today?” For those that have a family member with a disability, it wasn’t an easy answer. That gap is what we want to fix. We are looking at the space of health and wellness through recreation sports and tourism. We’re looking within that space, and in those industries, and saying “Let’s help make these spaces be accessible and inclusive, so people with and without disabilities come together and participate together in the activities that they want to be doing.”
Q. How is RAA trying to give people with and without disabilities the chance to participate in recreational activities together?
A. Our solution is to develop a model that would allow us to go into those spaces and mentor them, to be able to understand and apply knowledge for them to become inclusive in their operations. Every day that a business is open, anybody and everybody can come in and participate together. Recreation, sports, tourism. Typically, these might be municipal recreation centers, community recreation centers, concert venues, things that people do for enjoyment, for health and wellness. It could be a kayak rental company, a museum, a game hall. We’re working with libraries to make sure they’re inclusive as well.
welcoming welcome mat that one could roll out for their business. That starts way back on their website, way back on any kind of brochures or fliers about their business and what it is that people perceive as the invitation. Now, these businesses that we’re working with have accessibility tabs where they’re able to list out things that they have, that they’ve done, that allow for more inclusive experiences.
Q. What might a library, for example, do to become more welcoming of people with disabilities?
A. One of the libraries intentionally lowered their computers. They had had the browsing computer at a standing height, so that meant anybody coming in on a scooter or in a wheelchair could not use the browsing computer to go find a book. They put that on an adjustable stand so that now no matter what height they [patrons] are, they’re able to move that so they can use it correctly. They have adjustable-height desks in their computer areas now. They have scooters that are available for patrons to use around the library.
Q. What services does RAA offer directly to members of the disabled community?
Q. How does your nonprofit help organizations become more inclusive?

fence. Though the nonprofit has just four employees and 75 volunteers, its services benefited 10,560 adults and
therapeutic recreation specialist who


Good Health spoke to her about her nonprofit, its services and challenges.



A. Our model was to go in with this mentored consultation. If you have the right knowledge base and understanding around disability culture, and you have knowledge around how to apply inclusive principles, you can apply those principles so that there are some definitive changes.
Q. Can you give some examples of such changes?
A. In essence, creating the most
A. We work closely with people with disabilities, understanding what they’re interested in, what their situation is and matching them to some places where they’re able to go. Erie Canal Boat Company, people can kayak and cycle there. Ludus Fencing Studio, people can learn to fence there. We also have a youth wheelchair basketball program, wheelchair lacrosse, wheelchair tennis, pickleball.
Q. What challenges does RAA face?
A. We as a society need to understand that inclusion is for all of us. The person with the disability is somebody’s child, somebody’s parent, somebody’s relationship. It would be really swell if people would just realize this isn’t special, its 26% of the population. It's all of us.







By Ernst Lamothe Jr
The New Year is often filled with hope and high expectations. By the end of the month, all that can turn to disappointment.
That occurs because people put all their efforts into living their best life and year in the early weeks and when things slightly fall off, they become dejected. However health professionals want you to know your healthy journey can always be reset. They suggest starting with the basics of overall time-tested nutritional foods.
“Please consider eating more fruit, vegetables, beans, legumes, seeds and whole grains. These are low-calorie foods that fill us up and are nutritious,” said Miyeon Oh, an internal medicine physician with Rochester Regional Health.
It’s easy to lose weight on a diet; but as soon as you stop following the restrictive rules of that diet you gain it all back and then some. Most diets work on the basis of limitations by cutting out entire food groups. Despite their strict guidelines, these diets remain effective only because they reduce your over-
all calories.
Oh encourages people to get back to the basics.
“Diets are a short-term fix, not a sustainable solution. They often take away the joy of eating and limit our connection with others, which is one of the reasons diets don't work long-term. Instead, we need to find healthy eating habits that are enjoyable and therefore, sustainable,” said Oh.
Healthy eating seems daunting. And too often fad diets require you to completely eliminate food that you enjoy, which ultimately becomes the first step to failure. This strategy gets in the way of feeling able to succeed, leading many to get discouraged at the slightest missteps and unwilling to make changes that seem so unattainable. In addition, people also have many time-honored misconceptions.
“Not all carbohydrates are bad for you. Carbohydrates from vegetables, fruits, whole grains and beans are packed with essential nutrients that support your health,” said Oh.
“Also you don’t need to rely
solely on animal protein to meet your needs. While animal products contain protein, they also have saturated fat. Plant-based proteins, like beans, lentils, nuts and whole grains, are rich in fiber, vitamins, minerals and phytonutrients. For instance, one cup of beans provides about 18 g of protein, while one cup of tofu offers around 10 g of protein.
“Milk and dairy aren’t the only sources of calcium. Plants are actually the original source, as they absorb minerals from the soil. For example, one cup of soybeans contains 100 mg of calcium, while two cups of broccoli provide 125 mg of calcium.”
Oftentimes healthy living makes people creative in a negative way. They look to short-sided shortcuts to achieve success.
“Try swapping soda for water, flavored water, or sparkling water instead! It's a refreshing change that can keep you hydrated and feeling great,” she said.
Many physicians recommend using the American Heart

Association guideline of 150 minutes of moderate intensity aerobic activity every week. Moderate intensity exercise should elevate your heart rate and make you start to sweat. Walking doesn't cost a thing and can be done just about anywhere. It is also important to add in weight and resistance training for muscle and bone health and stretching for flexibility.
“Exercise is a great way to support both your mental and physical health, especially as we age. It helps keep your bones strong and boosts your mood, making you feel better inside and out,” said Oh.
Lifestyle decisions early in life play major roles in the conditions we deal with later on. Rates of conditions like diabetes, heart disease, hypertension and obesity are all drastically increasing.
“Most of my patients tell me they want to live a long, healthy life so they can be there for their family. They’re motivated to stay strong and active to enjoy more time with loved ones,” she said.
By Shaina Zazzaro
How many times have you heard someone say to count your calories?
So many!
What about macros?
Tracking your macros is a great way for you to stay healthy, lose weight, gain weight or maintain weight. It is a great way to eat a consistent amount of food to reach whatever your goal may be — but you must be consistent.
Here, let me break it down for you.
Macros are macronutrients. These are the three main categories of nutrients that make up calories in foods. The main macros are protein, fats and carbohydrates.
You can lose weight, gain weight or maintain weight by following a macro plan.
I hate saying “diet” because it is not a diet. Macros teach you what to



eat and help you live by my favorite rule: eat whatever you want, in moderation.
Want a slice of pizza? Fit it in. Ice cream sundae? Go for it! Just fit it into your macros.
I’m going to break this down for you in Shaina terms- let’s forget about all of the technical terms! You need carbs for energy. I don’t care what people say about not eating them, don’t listen to them. You can enjoy carbs, but in moderation.
I had a HUGE New Jersey bagel this weekend. I tracked it as one and a half of a regular bagel and then made sure not to overindulge in carbs the rest of the day. That meant no ice cream for dessert. See, moderation!
You need to eat protein to feel full, to build muscle and to not lose your muscle, so eat your protein! And, no, eating protein isn’t going to make you look like a professional bodybuilder (unless you pair it with super strict diet and exercise!)
Fats. Fats won’t make you fat — again, as long as you eat them
energy, heart health, brain health and for energy storage so, yes, you need to eat fats. I am not encouraging you to eat bacon for breakfast, lunch and dinner, but if you happen to see your favorite healthy food truck this summer and get a chicken, bacon and avocado healthy trash plate, remember I told you that it is OK!
Bottom line is this: you need to figure out what the best macro balance is for your personal goals and for yourself, so find a trainer. I use Ivan’s Fitness to tell me the best balance, but you can use whoever you find that you are comfortable with and trust to help you on your macro tracking journey.
Just do me a favor, OK? Don’t go to My Fitness Pal and do a default, one size fits all 1,200 calorie diet, because that just isn’t being fair to yourself.
Peace, love and health!
Shaina Zazzaro is a devoted wife and mother of two, blending her roles with a passion for health and wellness. She is the owner and chief executive officer of local meal delivery service, Effortlessly Healthy. For more information, visit www.ehmeals.com.








By Anne Palumbo
Ahem. Before I enumerate the powerful benefits of eating beans, I’d like to ask you a personal question: Do you suffer from “bean hesitancy,” a common phenomenon marked by a reluctance to eat beans for fear of increased flatulence?
Yes?
Rest easy, you’re not alone. No thanks to jokes, children’s songs, and personal experience, many shy away from this “musical fruit.”
Let’s hope after reading this month’s column, you will—to paraphrase John Lennon—“give beans a chance.” That’s all we are saying.
To begin with a bang: Black beans have a nutritional profile like no other bean. While high in plantbased protein like most beans, black beans contain a unique slew of nutrients that other beans either lack or have negligible amounts.
• Diabetes warrior: According to medical experts, Type 2 diabetes is a national epidemic, with more chil-
dren, teens and young adults developing Type 2 diabetes than in the past due to rising obesity rates and unhealthy diets. Black beans help manage blood sugar levels in three remarkable ways: their low GI (glycemic index) won’t spike blood sugar levels and cause an aggressive insulin response; their high fiber content slows down digestion and the release of glucose into the bloodstream; and, lastly, their particular antioxidants support blood sugar control. Takeaway? Managing this disease can improve life expectancy.
• Sleep promoter: When it comes to better sleep, consuming black beans may be your express ticket to the land of Nod, and, according to the Mayo Clinic, a longer life. Thanks
to an abundance of three important nutrients—tryptophan, magnesium and fiber—your sleep may improve with regular consumption of this soporific bean. Specifically, tryptophan contributes to the production of sleep-boosters serotonin and melatonin, magnesium helps regulate melatonin production and muscle relaxation, and fiber helps prevent disruptive energy crashes by regulating blood sugar levels.
• Heart protector: Eating black beans has been shown to reduce high blood pressure, high cholesterol and obesity, which are all key risk factors for heart disease and premature death. How exactly do beans aid weight loss? Because this mighty legume teems with two nutrients that take longer to digest—protein and fiber—they often enhance feelings of fullness, which can result in eating less. Hearts also love black beans for their bounty of folate, a B vitamin that helps the heart

Drain and rinse canned beans thoroughly (to reduce both sodium and the production of gas). Scour labels and select canned beans with reduced or no sodium. Rest assured that 95% of food cans are now BPA-free.
stay healthy by reducing an amino acid that can damage artery walls and increase the risk of heart disease and stroke.
Circling back to the toots: I now present some valuable intel from the Bean Institute. 1) The more beans you eat on a regular basis, the less likely you’ll experience gas. 2) Drinking more water as you eat more beans helps your body better process a bean’s fiber. 3) Gas in the gut is generally considered a good sign because it indicates that healthy bacteria are hard at work!


Anne Palumbo is a lifestyle columnist, food guru, and seasoned cook, who has perfected the art of preparing nutritious, calorie-conscious dishes. She is hungry for your questions and comments about SmartBites, so be in touch with Anne at avpalumbo@aol.com.
Ingredients
Serves 6-8 Adapted from Eatingwell.com
1 tablespoon oil
2 medium sweet potatoes, washed
1 medium onion, chopped
1 garlic clove, minced
1 teaspoon chili powder (or more if you like heat)
1 teaspoon ground cumin
½ teaspoon salt (or less) ¼ teaspoon coarse black pepper
Directions
1. Preheat oven to 400 F. Lightly coat a 9 x 13 baking dish with oil or cooking spray.
2. Soften sweet potatoes in microwave: Pierce skin with a fork, then place on a microwave-safe plate and microwave for about 5-6 minutes, until sweet potatoes are soft enough to easily peel and cut into ½ cubes. Transfer to a large bowl.
3. Heat oil in a small nonstick skillet over medium heat. Add chopped onions; cook, stirring occasionally, until soft and golden, 4-6 minutes. Add minced garlic; cook 1 minute more, then add chili powder, cumin, salt and pepper; cook, stirring con-
1 (14.5 oz can) petite diced tomatoes, drained
1 (4 oz can) mild diced green chiles, drained
1 (15 oz can) reduced-salt black beans, drained and rinsed (or 2)
1 (8.5 oz can) sweet corn, drained
1 tablespoon lime juice
1¼ cups shredded cheese of choice
Optional garnish: cilantro, avocado slices, sliced scallions, lime wedges
stantly, for 30 seconds.
4. Transfer contents of skillet to bowl with sweet potatoes; gently stir in diced tomatoes, diced chiles, black beans, corn, lime juice, and ¾ cup cheese. Transfer this mixture to the prepared baking dish. Scatter the remaining ½ cup cheese on top. Cover dish with foil; bake for 15 minutes. Remove the foil; bake until the sweet potatoes are tender and the cheese is melted, about 10 minutes more. (Quickly broil if you like a crispier top.) Garnish with toppings of choice.
Note: Want some crunch? Add a layer of tortilla chips or broken-up taco shells before sprinkling the last ½ cup of cheese.
CDC: More than 14 million older people (25%) report falling — it has become the top cause of injury-related death for people over 65
By Deborah Jeanne Sergeant
The Centers for Disease Control and Prevention reports that falls are the top cause of injury-related death for people 65 and older.
Falls in this age cohort are common.
The CDC states that more than 14 million older people (25%) report falling — and that does not include those who fall but do not report it.
“The age-adjusted fall death rate increased by 41% from 55.3 per 100,000 older adults in 2012 to 78.0 per 100,000 older adults in 2021,” the CDC states.
But why are falls so harmful to older adults?
“As we age, our bodies lose the ability to quickly heal and recover from things as small as a bump or bruise; the timeline increases,” said Season Bonino, physical therapist and Nazareth University clinical associate professor of physical therapy.
A fall that would end with a rueful laugh and a bruise can mean “something much more significant,” said Bonino, who is also a board-certified geriatric specialist in physical therapy. “Even if it’s a minor fracture like limiting their weight bearing activity, it can have dramatic effects because of being sedentary for a while. A fall that can seem minor at the time can have a cascade of events with that person being in a very different place down the road.”
After a fall, many frail older


adults do not regain the same level of vitality as they had before.
Beyond the pain experienced during a fall, the consequences of falling can be severe for older adults. Preventing falls can help avoid these outcomes.
How people move can make a difference in whether or not they fall.
“People tend to take short, shuffling steps because they don’t want to stand on one foot at a time,” Bonino said. “But what they don’t recognize is they’ve narrowed their base of support. If someone bumps into them, they’re going to fall.”
A longer, more natural stride is safer.
The home environment makes an enormous difference. Poor lighting, clutter on the floor, throw rugs, uneven flooring and multi-level living spaces all contribute to a higher risk of falling. Upgrading the bathroom and bedroom — the most fall-prone rooms of the house — can reduce fall risk.
“Where you get in and out of the tub, could we put in a grab bar?” Bonino suggested.
Grab bars by the toilet also assist in stability, as does a bedrail in the bedroom.
Seeing where you’re going helps you stay on your feet. Bonino recommends nightlights and placing lamps where they can be turned on upon entering the room.
“In a lot of older homes, you have to cross the room to get to a light switch,” she said.
Bonino asserts that physical therapists can help prevent falls.
A 2018 study at Nazareth indicated a significant reduction in falls in people who completed training with a slip trainer, a device physical therapists use to safely trip patients without any risk of injury. Patients wear a safety harness so that when the therapist initiates the fall, an injury is not possible. The equipment allows patients to practice falling so their brains relearn how to elicit a recovery response quickly enough to prevent a fall.
“It’s an ‘inoculation for falls,’” Bonino said. “It’s like getting a flu shot or tooth cleaning. Research finds that perturbation-based balance training takes 20 minutes and we see results that last for months.”
‘Use it or lose it’
Becoming less active to prevent falls is counterproductive, according to Maureen Loyal, physical therapist and director of rehabilitation and physical therapy with Finger Lakes Health.
“Fear of falling has you do less outside the home,” she said. “You become deconditioned and it’s a cycle. Do the opposite of what people do, which is confine themselves to

New York designates physical therapists as direct access providers, meaning patients can see a PT for 30 days or 10 visits (whichever comes first) without a physician referral.
their homes and have people do errands for them. People who are older should park farther away so they’re walking more. ‘Use it or lose it’ is important. It’s never too late to have balance exercises.”
She encourages older adults to seek help to improve their endurance, strength, flexibility and balance if they begin to experience instability while walking. Too many people reach for a cane or walker early on when improving their physical condition would prevent that reliance.
Instead of performing random exercise movements, Loyal focuses on functional movement that will help people better carry out activities of daily living like carrying grocery bags, standing and sitting and climbing stairs.
“We want to keep that function throughout life,” she said, “And you do that by keeping your strength. You may weigh the same, but you can see there’s more fat than muscle. You may think you have the same muscle capacity, but you don’t. I try to focus on functional exercises, not sitting in a chair and kicking your legs up. When do you ever do that movement?
“Do sit-to-stand exercises where you stand and then slowly sit down. If you can keep your quad muscles strong, it decreases risk for falls and keeps you independent in the community.”




Born between 1946 and 1964, the oldest members of the baby boomer generation will turn 80 starting in 2026. Does the Rochester area have sufficient resources available to meet their needs in older age?
Geriatrician Ahmed Rab, medical director of the Episcopal Church Home and the lead physician for Unity Geriatrics, discussed what is available in Rochester and what is still lacking.
“I think that it’s great we’re
investigating how to be prepared for this,” he said. “Eighty percent of people 65-plus have a chronic health condition. One out of nine adults over 65 will have one form of dementia. One out of four of those 65-plus will fall. Getting prepared for these changes is important for Rochester.”
He added that affordable longterm care represents a huge issue, as 50% of seniors on Medicare have incomes that fall 200% below the federal poverty line. As many as
one-quarter of older adults experience malnutrition because of an inability to access or prepare sufficient food. He explained that this can cause muscle weakness, slower recovery from illness and injury and health conditions caused by poor nutrition.
Having no reliable transportation can harm health, as older adults may not be able to shop for supplies, pick up medications, make it to doctor’s appointments or socialize frequently.
“Social isolation affects mental health,” Rab said. “One-third of those over 80 are isolated. It places them at risk for dementia, depression and premature death.”
He believes that programs managed by the Office for the Aging in Rochester can help direct people in finding resources in many of these areas — care, nutrition, transportation and socializing — but sufficient staffing of organizations remains a problem.
“By 2030, the number of geriatric specialists will fall far below the level needed,” Rab said. “We’re always recruiting geriatricians to meet the need.”
The same holds true for many positions in healthcare, especially those relating to older adults such as home health workers and those working in independent living, assisted living and long-term care facilities.
Rab said that organizations like ElderOne and Lifespan collaborate with hospitals to help discharged older people who need help. For some, receiving rehabilitative care at home can help them recover to a better state independence and prevent re-hospitalization.
“There’s definitely an increased need for home care services,” Rab said. “Oftentimes if we can’t get wound care to the house or physical therapists or occupational therapists, it’s because there’s not enough services. That can lead to longer stays in the hospitals and nursing home rehabs taking away beds from people who need it. Increasing the staffing will help people be better prepared.”
Technology can help reduce staffing woes. Rab said that telehealth is one example of ways that the healthcare system can reduce urgent care and emergency department visits. Although some older people resist using technology for telehealth, Rab added that he has patients 100-plus who feel completely at ease with technology.
Rab also believes that preparing for older age matters. For example, “automating” tasks such hiring a lawn care and snow removal company can prevent injury from these activities.
Scheduling regular delivery of groceries and supplies can make shopping simpler. Signing up for automatic payments ensures these bills won’t be skipped.
“It can help you to find ways to have people you can rely on,” Rab said. “It's super important to prepare for end-of-life care and advanced directives. If you don’t address these issues when you’re of sound mind, it can lead to conflict in the family. Think about having an advanced care directive and have your healthcare wishes well documented.
“Think about your long-term care and prepare for it. People don’t realize how expensive it is.”



Age, family genetics and gender make it nearly impossible for older adults to avoid becoming a chronic disease statistic.
According to NCOA research, 94.9% of adults aged 60 and older have at least one condition, while 78.7% have two or more.
You probably have a parent or grandparent who is managing a condition right now or perhaps you are managing one yourself.
And obesity, which impacts about 42% of adults 60 and older, can increase your risk for conditions like heart disease, Type 2 diabetes, and some cancers.
With these kinds of odds, you might wonder if there is anything you can do to prevent the onset of a chronic medical condition or make managing an existing one easier. The answer is yes.
Here are 10 common chronic conditions adults 65-plus on Medicare were treated for in 2018, and what you should know about each.
Nearly 12% of older adults on Medicare were treated for Alzheimer’s disease or another form of dementia. Alzheimer’s disease is one specific type of dementia — a condition that causes memory loss and difficulty thinking or problem-solving to the point that it interferes with every day activities. Dementia is not a normal part of aging and is caused by changes in the brain over time.
The biggest risk factors for these chronic conditions are things you often can't control, including age, family history and genetics. But studies have suggested incorporating the following habits into your lifestyle could slow or prevent onset:
• Exercise. Staying active isn't just good for your heart; it's also great for your brain.
• Sleep. Your brain does important stuff while you are sleeping, so getting at least seven hours of deep sleep a night is crucial. Upgrading to the best mattress for you could help.
• Be smart about your diet. Research suggests that some foods can negatively affect your brain.
Sixteen percent of older adults sought treatment for depression — a treatable medical condition that is not a normal part of aging. Depression causes persistent feelings of sadness, pessimism, hopelessness, fatigue, difficulty making decisions, changes in appetite, a loss of interest in activities and more.
Steps you can take to help with depression include:
• Manage stress levels. Reach out to family and friends during rough spells and consider regular meditation.
• Eat a healthy diet. What you put into your body can affect your mood, so focus on foods that are high in nutrients and promote the release of endorphins and those "feel good" chemicals, and limit consumption of things like alcohol, caffeine, artificial sweeteners, and highly processed foods.
• Routine exercise. Exercise has a number of physical and psychological benefits, including improving your mood through the release of endorphins and other "feel good" brain chemicals, boosting self-confidence and self-worth through meeting goals and improving your physical appearance, and increased socialization through interactions at gyms and group classes.
• Talk to your doctor. If you've ex-
Nearly 95% of adults 60 and older have at least one chronic condition, while nearly 80% have two or more.
perienced any of the warning signs of depression, talk to your doctor, and ask about your treatment options. Antidepressant medications or psychotherapy could be right for you.
If you’re in severe emotional distress, one of the first things you should do is tell someone else about it — such as a trusted friend or family member. You can also dial or text 988 from your phone to speak with a counselor who is specially trained in suicide prevention. The 988 service is free, confidential, and available to everyone in the United States 24 hours a day, seven days a week.
About 5% of older adults were treated for heart failure — a condition that occurs when the heart cannot adequately supply blood and oxygen to all of the organs in the body. The heart might become enlarged, develop more muscle mass or pump faster in order to meet the body’s needs, causing you to feel tired, light headed, nauseous, confused, or lack an appetite.
Steps you can take to prevent or diminish symptoms of heart failure:
• The best prevention is to follow a doctor's recommendations to decrease your risk for coronary heart disease and high blood pressure.
Nearly 25% of older adults were treated for chronic kidney disease (CKD) or a slow loss in kidney function over time. People dealing with CKD have an increased risk for developing heart disease or kidney failure.
Steps you can take to prevent or diminish symptoms of CKD:
• Understand what damages your
kidney. Diabetes and high blood pressure are the greatest risk factors for kidney damage, so taking steps to prevent these diseases is your best strategy.
• Early detection and treatment. Talk to your doctor regularly, stay current on screenings, and keep up on prescriptions you need to diminish symptoms.
Twenty-seven percent of older adults were treated for diabetes — a disease that occurs when your body is resistant to (or doesn’t produce enough) insulin. Insulin is what your body uses to get energy from food and distributes it to your cells. When this doesn’t happen, you get high blood sugar, which can lead to complications such as kidney disease, heart disease, or blindness. Chances of having diabetes increases after age 45.
Steps you can take to keep you from developing diabetes or to manage this condition:
• Eating a healthy diet, including monitoring your carbohydrate and calorie intake, and talking to your doctor about alcohol consumption.
• Exercising for 30 minutes five times a week to keep your blood glucose levels in check, and to control weight gain.
• Safely losing 5-7% of body weight if you are diagnosed with pre-diabetes.
Nearly 29% of older adults were treated for ischemic heart disease — a condition that is caused by a build-up of plaque that narrows the arteries leading to the heart. Narrow

or blocked arteries decreases the amount of oxygen-rich blood delivered to the heart. This can cause other complications like blood clots, angina or a heart attack.
Steps you can incorporate to help if you have ischemic heart disease:
• Avoid saturated and trans fats, and limit sugar and salt intake
• Get seven to eight hours of sleep each night
• Keep your stress levels in check
• Do regular cardio exercises
• Abstain from smoking
• Talk to your doctor about the major risk factors, including high cholesterol and high blood pressure
About 35% of older adults were treated for arthritis — an inflammation of your joints, which causes pain and stiffness and is more common in women.
Steps you can take to delay the onset of arthritis or manage the symptoms:
• Exercise at least five times per week, for 30 minutes each time, to improve function and decrease pain. Try to include a mixture of aerobic, strength-building, and stretching movements.
• Stay within the recommended weight for your height — losing one pound can remove four pounds of pressure on your knees.
• Make sure your back, legs and arms are always supported.
• Take precautions to avoid joint injuries.
• Do not smoke.
About 40% of adults 65 and older are living with obesity, a chronic disease linked to more than 200 chronic conditions. The National Council on Aging (NOAA) is pressing to define quality obesity care as a universal right. That includes the right to coverage for treatment with access to the full range of treatment options.
Tips for addressing obesity include:
• Understanding what obesity treatments are covered by Medicare
• Empowering yourself with knowledge about nutrition
• Educating others and being your own advocate
More than 50% of older adults were treated for high cholesterol — a condition that occurs when your body has an excess of bad fats (or lipids), resulting in your arteries getting clogged, which can lead to heart disease.
Steps you can take to prevent or manage high cholesterol:
• Abstain from smoking and
excessive alcohol consumption
• Be active each day
• Manage your weight
• Minimize saturated fats and trans fats in your diet
Nearly 60% of older adults were treated for hypertension — a common condition that involves both how much blood your heart pumps, as well as how resistant your arteries are to the blood flow. When your heart pumps a lot of blood, and you have narrow arteries which resist the flow, that’s when you get high blood pressure, also known as hypertension. The danger of hypertension is not only that you can have it for years and not know it, but it can cause other serious health conditions, like stroke and heart attacks.
Steps you can take to prevent or reduce high blood pressure:
• Maintain a healthy weight. Losing just 10 pounds can reduce blood pressure
• Regulate your stress levels
• Limit salt and alcohol consumption
• Exercise daily, including a combination of moderate to vigorous-intensity aerobic activities, flexibility and stretching, and muscle strengthening
• Check your blood pressure regularly—the quicker you catch pre-hypertension, the more likely you are to prevent high blood pressure
Another common chronic conditions for adults over 65 is chronic obstructive pulmonary disease (COPD), which includes two main conditions: emphysema and chronic bronchitis. COPD makes it hard to breathe and causes shortness of breath, coughing, and chest tightness.
Steps you can take to manage COPD include:
• The best way to prevent COPD — or slow its progression — is to quit or avoid smoking. Also try to avoid secondhand smoke, chemical fumes and dust, which can irritate your lungs.
• If you already have COPD, complete the treatments that your doctor has prescribed, get the flu and pneumonia vaccines as recommended by your doctor, and continue to remain active.
This article was published in May 2024 on the website of the National Council on Aging (NOAA), www.ncoa.org.

Dr. Mark Winsberg, MD, former Medical Director for Rochester Regional Health’s Chemical Dependency Services, is a seasoned Addiction Medicine Specialist with over 16 years experience in the field of Addiction in both inpatient and outpatient settings. He currently holds dual board certification in Addiction Medicine and Family Medicine. In recovery for over 21 years from his own bout with addiction, Dr. Winsberg truly understands and empathizes with the challenges you may be facing.
Available for both individual consultations and speaking engagements to your groups or clubs.



Gene therapy for treating hearing loss is not FDA-approved and therefore is not available in the United States. Continued research and clinical trials must first show that such therapies are both safe and effective.
If approved in the future following successful clinical trials, gene therapy could potentially benefit people who are diagnosed with hearing loss caused by a genetic variant.
Even then, treatments would likely focus on a type of congenital hearing loss called monogenic. Monogenic hearing loss stems from variations in a single gene and can be inherited. In contrast, polygenic deafness involves multiple genes and potentially environmental factors, making it more complex to treat with gene therapy.
Gene therapy clinical trials are underway for congenital hearing loss caused by variations in a specific gene known as the otoferlin gene (OTOF). Otoferlin is a protein in hair cells that helps convert sound into a signal that can be interpreted by the brain. Otoferlin gene variations cause 1 to 8% of congenital hearing loss cases. When otoferlin does not function correctly, severe to profound hearing loss occurs, despite other functioning hearing structures. Replacing the faulty otoferlin gene with a functioning version could be

an approach to restoring hearing in those with otoferlin-related hearing loss.
To develop future targets for gene therapy, scientists are investigating the structure, function and processes of the genes and proteins in the inner ear.
The National Institute on Deafness and Other Communication Disorders (NIDCD)-supported research has led to the identification of many genes, including otoferlin, that can cause hearing loss when mutated or missing. To date, more than 150 such genes have been identified. As with earlier work on otoferlin, NIDCD-funded researchers are using models to confirm that these genes are potential targets for gene therapy. These studies are essential to defining workable treatments. These are the first steps before eventual clinical trials with human participants.
Researchers are also working to advance gene therapy technology by developing new methods and delivery systems. Gene-editing technologies, such as CRISPR, could one day be used to modify genes associated with hearing loss.
If approved for treatment, gene therapy may become one of several options to address genetic hearing loss, according to the NIDCD.
Prepare for new opportunities that stimulate engagement, feed your curiosity, and inspire a fresh desire for learning. St. John’s full array of service options address evolving needs within compassionate community settings.
• Independent Senior Living
• Enhanced Assisted Living
• Respite Care
• Rehabilitation
• Skilled Nursing Care
• Dementia Resource Center
• Hospice Care
Many life-enhancing choices await you.
SCHEDULE A TOUR TODAY. 585-760-1300 | stjohnsliving.org
By Jim Miller

Dear Savvy Senior,
What types of mental health services does Medicare cover? I struggle with anxiety and depression, and my primary care provider recommended I see a therapist or psychiatrist.
Anxious Annie
Dear Annie,
Medicare actually covers both outpatient and inpatient mental health care services and programs to help beneficiaries with anxiety, depression and many other mental health needs. Here what you should know.
If you’re enrolled in original Medicare, your Part B coverage will pay 80% (after you’ve met your annual $257 Part B deductible) for a variety of counseling and mental health care services that are provided outside a hospital, such as in a doctor or therapist’s office, hospital outpatient department or community health center. These services can also be received via telehealth.
You or your Medicare supplemental (Medigap) policy is responsible for the remaining 20% coinsurance.
Medicare also gives you the expanded option of getting treatment through a variety of health professionals such as psychiatrists, psychologists, clinical nurse specialists, clinical social workers, nurse practitioners, physician assistants, marriage and family therapists and mental health counselors.
To get this coverage, you’ll need to choose a participating provider that accepts Medicare assignment, which means they accept Medicare’s approved amount as full payment for a service.
If you choose a nonparticipating provider who accepts Medicare but does not agree to Medicare’s payment rate, you may have to pay more. And if you choose an opt-out provider that does not accept Medicare payments at all, you will be responsible for the entire cost.
To locate a mental health care professional in your area that accepts Medicare, go to “Medicare.gov/ care-compare,” click on “doctors & clinicians” and type in your location, followed by “clinical psychologist” or “psychiatry” in the “Name &
Keyword” box. You can also get this information by calling Medicare at 800-633-4227.
If you happen to need mental health services in either a general or psychiatric hospital, original Medicare Part A covers this too, after you’ve met your $1,676 Part A deductible. Your doctor should determine which hospital setting you need. If you receive care in a psychiatric hospital, Medicare covers up to 190 days of inpatient care for your lifetime. And if you use your lifetime days but need additional care, Medicare may cover additional inpatient care at a general hospital.
In addition to the outpatient and inpatient mental health services, Medicare also covers yearly depression screenings that must be done in a primary care doctor’s office or clinic. Annual depression screenings are covered 100 percent.
And if you have a Medicare prescription drug plan, most medications used to treat mental health conditions are covered too.
If you get your Medicare benefits through a private Medicare Advantage plan, they too provide the same coverage as original Medicare does, but may impose different rules and will likely require you to see an in-network provider. You’ll need to contact your plan directly for details.
For more information, call Medicare at 800-633-4227 and request a copy of publication #10184 “Medicare & Your Mental Health Benefits,” or you can read it online at Medicare. gov.

Send your senior questions to: Savvy Senior, P.O. Box 5443, Norman, OK 73070, or visit SavvySenior. org. Jim Miller is a contributor to the NBC Today show and author of “The Savvy Senior” book.






By Rose Callea
The winter months can seem like they go on forever. With the holiday festivities over, it can be difficult to see the sunlight at the end of the long winter tunnel. That's especially true for those who live alone, including older adults.
Just as we protect our bodies from the winter cold, we should protect our souls from the impact of loneliness and isolation. One way to do that is by maintaining a healthy spiritual life.
Research shows that spiritual and religious practices are positive forces in the lives of older adults. They make us more resilient, contribute to a positive state of mind and enable us to cope with life's stresses.
Our ability to cultivate a spiritual relationship with God doesn't end when we get old. In fact, it can grow stronger as we take time to reflect on life and its blessings. The solitude of winter makes it the perfect time to do this.
The pastoral care team at St. Ann's Community is always focused on supporting our elders' spiritual well-being. While rooted in the Catholic tradition, we offer spiritual support and comfort to all who need it. Many of the practices we use can be applied to everyday life, whether you reside with us or live on your own.
• Spiritual reflection. As the Gospel of John tells us, “God is love. Whoever lives in love lives in God, and God in them.” Remembering that can nourish the soul and guide us through challenging times. Set aside time each day to read a favorite passage from scripture or a literary verse that comforts you, as we do in small groups at St. Ann's. Consider the grace and beauty around you and think about how God's love is present in your life.
• Meditation. Use simple medi
tative techniques to create a sense of calm. Focus on your breathing, gently inhaling and exhaling, and feel the physical response of your body. Clear your mind and focus on the present moment instead of the past or future. This can help alleviate anxiety and achieve a feeling of inner peace, warming the soul and renewing the spirit.
• Socialization. In winter it's easy to isolate ourselves. But too much time alone can result in loneliness, boredom and depression. At St. Ann's, we encourage socialization year-round by offering our elders attendance at mass if they so choose, social gatherings to participate in and musical performances to enjoy. Take advantage of opportunities in your life to share joyful experiences with others. You'll be surprised at how uplifting it can be.
• Being present. Even small, oneon-one interactions can have a positive effect when we are fully present in the moment. Make that phone call you've been putting off, chat with a neighbor over coffee, and enjoy the time spent together. If you know of someone who's alone, make the effort to call or visit without distraction and focus on listening; it's good for the spirit—both yours and the person you reach out to.
Remember: darkness always gives way to light. And no matter how long it takes to get here, spring will always arrive with its promise of

Rose Callea is director of pastoral care at St. Ann's Community. She can be reached at rcallea@mystanns.com.
When your child turns 18 years old, they legally become an adult. This is an important time to consider their financial future, especially if they need additional care into adulthood. Here are five things that may help you prepare for this milestone:
When your child legally becomes an adult, you can no longer make certain decisions for them about their health and welfare. However, you can stay involved through our representative payee program. Social Security will determine who best serves as a representative payee for your child’s benefits. To learn more about the representative payee program, read our webpage at www.ssa.gov/ payee/index.htm. Please note Social Security does not recognize power of attorney.
SSI provides monthly payments to adults and children with disabilities, as well as people 65 and older, who have little or no income and resources.
If your child receives SSI, when they turn 18 we will review their eligibility for continued SSI payments based on the disability rules for adults. For more information, please review the publication, “What You Need To Know About Your Supplemental Security Income (SSI) When You Turn 18” at www.ssa.gov/pubs/ EN-05-11005.pdf. Please be sure to review this with your child. We also encourage you to check out Social Security’s youth toolkit webpage at www.ssa.gov/youth.


If your child attends school, they have a few options to continue their education, such as pursuing:
• A diploma: They may pursue further education in college or trade programs with an individualized education program (IEP). More information on the IEP is available at www.ssa.gov/pubs/EN-64-118.pdf.
• A certificate: They may have the opportunity to continue in a transitional program in their high school even after they complete their senior year. Most are permitted to remain until they turn 22.
• Employment: Local vocation-
al rehabilitation services can assist with employment options during pre-graduation IEP meetings.
Once your child turns 18, they may choose or qualify for different living arrangements depending on the services they already receive. If your child receives therapy services at school, how will they receive them once they leave? They could receive them through a Medicaid waiver or private insurance.
Qualification for respite services may also look different. Respite services allow family caregivers time to step away from their duties. It is essential you understand all the benefits and options available to your child after they complete high school and before deciding on living arrangements and services.
• Special needs trust: Update estate planning documents before your child turns 18. Otherwise, inheritance may terminate your child’s governmental benefits.
• ABLE account: You can deposit funds into this account up to a certain limit each year. However, there are limits on what its funding covers. More information on ABLE accounts is available at www.ssa.gov/payee/ able_accounts.htm.
The above is informational only and does not constitute financial advice or an endorsement of ABLE products or ABLE organizations by the Social Security Administration. There may be other financial options that could be a better fit for some individuals. You must use your best judgement to determine which option is best for your situation.
Children receiving benefits on a parent’s record may continue to receive those benefits until age 19 if they’re a full-time elementary or secondary school student. People who have a disability that began before age 22 may also be eligible to receive child’s benefits at any age. For more information, please review the publication, “Benefits for Children” at www.ssa.gov/pubs/EN-05-10085. pdf. As your child enters adulthood, consider these issues while you navigate their financial future.
Please share this information with your friends and loved ones who may need it.

The ‘DXA’ can help see if your bones are at risk
By Deborah Jeanne Sergeant
Of course, you will likely receive an x-ray if you break a bone so the provider can set the bone.
But did you know that there’s a diagnostic scan that can look at your bones’ density?
The DXA (also called a “dexa”) scan looks at the mineral content of your bones to help providers determine if you have osteopenia or osteoporosis.
Using low level radiation, the DXA typically scans the spine and pelvic area, which are common areas
Imaging offers providers a glimpse inside our bodies without opening up the skin. But what are the differences among the various types of exams?
Efficient and painless, X-rays are typically used to get a good look at the bones and soft tissues. Patients may lie, stand or sit near the equipment for about 15 minutes. Because radiation is used, providers will not be present in the room. Repeated exposure such as X-raying patients daily could cumulatively endanger providers. The patient may wear a lead covering to protect areas that do not need to be X-rayed, such as the apron available at dentist’s offices. Typically, X-rays focus on the area in question. Providers note X-rays in their patients’ charts to ensure that they do not receive unnecessary X-rays. Any imaging involving X-rays is not recommended for pregnant women.
A computer uses numerous X-ray images to create a 3D style image with the CT scan. Providers can look at bones, soft tissues, tumors and clots. Some of these procedures
for bone breaks in older adults. But other populations may want to ask their providers about a DXA as well.
Physician Carole Peterson, who provides women’s healthcare at URMC’s Perinton Medical Center, said that the risk factors include being a small-framed, post-menopausal woman; celiac disease; being a man over age 65; decreased bone density from medications; anorexia, wheelchair use; family history of bone breaks and metabolic disease.
Other factors could include some autoimmune diseases; tobacco use;
more than three servings of alcohol daily; vitamin D deficiency; and use of certain medications. These include corticosteroids, some kinds of cancer medication, some types of immunosuppressants, hormone suppressants, some types of seizure medications, proton pump inhibitors that treat acid reflux and GERD, and Heparin, a blood thinner.
“It’s important to have the scan,” Peterson said. “There are 200 million in the US who have osteoporosis, and a significant number will have a fracture. People who fracture the
By Deborah Jeanne Sergeant
require patients to have a contrasting dye in their system, either through an IV or by drinking it. Patients lie on a table in a room separated from the technician. The table slides into a large tube and then the X-ray equipment moves around the patient. The whole process takes about 15 minutes. Like standard x-rays, providers are not in the room to prevent cumulative radiation damage.
MRIs use magnets, radio waves and a computer to take a look at organs and soft tissues. Similar to CT scans, patients lie on a table that moves into the MRI equipment, which can be noisy at times. The scan can take up to an hour to complete. Providers can use MRIs to diagnose conditions such as aneurysms, multiple sclerosis, strokes, spinal cord
spine or hip, their fatality rate is 20% in the next year. They may lose independence. As we age, we lose bone. DEXA is an intervention.”
The scan doesn’t treat fragile bones; however, it can give providers and patients and idea of whether the bones are at risk for fracture and what steps they can take to reduce that risk.
Geriatrician Ahmed Rab, medical director of the Episcopal Church Home and the lead physician for Unity Geriatrics, said that people with more risk factors may be screened earlier, but most people 65-plus should have the scan. Younger people who may qualify have “a family history of osteoporosis; those with history of fractures; low body weight or BMI of less than 19; heavy steroid use or smoking; for men, those over 70 get screened and those younger than 70 with the above risk factors or low testosterone.”
The scan takes mere minutes and is painless. Patients may eat and drink normally but are asked to forgo any calcium supplements for 24 hours before the test. Pregnant women should not receive a DXA scan. Patients must also wear loose, comfortable clothing without metal trim or closures like zippers or buckles.
According to the Cleveland Clinic, the best ways to strengthen your bones are:
Exercising more often: Regular physical activity strengthens your bones. Walking, yoga and strength training are great ways to stay active and prevent bone loss.
Supplements or eating specific foods: Your provider might suggest that you take a vitamin D or calcium supplement to support your bone health. You might need to eat more foods high in certain vitamins and minerals.
Medication: Your provider might prescribe medications that help slow down bone loss and prevent fractures. Some medications for osteoporosis may help build your bone density.
sound to detect fetal development in pregnant women. The technician lubricates the skin with gel and uses a handheld probe against the skin with firm pressure. Ultrasound procedures can take 30 to 60 minutes, depending upon the reason for the ultrasound, which can include diagnosing a plethora of diseases, blood flow problems, genital issues, tumors and more. Ultrasound can also help guide providers taking a biopsy.
problems, tumors and injuries to the joints or tendons.
To watch movement inside the body in real time, providers may use fluoroscopy. This type of imaging uses pulses of X-ray beams along with dye to help diagnose heart or intestinal diseases, guide surgery or injections or in orthopedics. Regular x-rays are like still photos, but fluoroscopy is more like videography. Providers can look in organs, joints, muscles and bones.
As the name denotes, ultrasound uses sound waves to develop images (sonograms) of organs within the body. It’s commonplace to use ultra-
PET scans (positron emission tomography) use a safe, radioactive tracer to help providers find diseased cells, typically for cancer, heart disease and conditions affecting the brain. Like the CT scan, the patient lies on a table that passes into the examination equipment. The radiotracer helps create images of the diseased cells because they absorb larger amounts of the material than healthy cells. The scan can take up to two hours. Some providers may use both the PET and MRI at the same time to make high contrast images, typically for tracking cancers in soft tissue areas.
Becker’s
Rochester Regional Health (RRH)

recently announced Becker’s Healthcare has named Jennifer Eslinger one of America’s COOs to Know. This list features standout healthcare leaders nationwide who “expand service lines, foster employee engagement and spearhead transformative organizational improvements.” It celebrates executives who “lead the charge in crafting and executing initiatives that elevate operational efficiency and fuel success across their organizations.”
“This honor only cements what we at RRH already know – that Jennifer Eslinger is a skilled leader who supports the continued success of this organization and, by extension, the health of our community,” said Richard “Chip” Davis, Ph.D., CEO of Rochester Regional Health. “Her wealth of healthcare experience, visionary leadership, and care for our team members and patients are measurable by her many accomplish-
ments. We at RRH are proud to work alongside Jennifer and celebrate this well-deserved recognition of her incredible contributions to our purpose and the communities we serve.”
Eslinger serves as president of healthcare operations and chief operating officer at Rochester Regional Health. She is a seasoned healthcare executive with almost 25 years in the industry and proven experience establishing, growing and managing complex, efficient hospital and health system operations. She has worked extensively in both for-profit and nonprofit healthcare sectors.
Since joining RRH in 2022, she has led a system-wide reorganization with a focus on expanding and supporting rural healthcare. She has implemented transformative workstreams that have enhanced efficiency and streamlined processes throughout the care delivery model. Furthermore, she successfully integrated and standardized operations across the Rochester Regional Health nine hospitals in Western New York, the Finger Lakes and St. Lawrence region.
A native of Georgia, Eslinger earned her undergraduate degree from Georgia Southern University and a Master of Business Administration from the University of Georgia. She is a fellow of the American College of Healthcare Executives and a Baldrige Executive Fellow.
“From my room to the food to the excellent doctors and techs…they took what could have been an unpleasant experience and made it great.”
That’s just one of the comments we’ve received from a patient who has had postsurgical rehab at St. Ann’s. We’re proud to offer first-class care that gets you healthy and home as soon as possible.
Preplan your stay. Call (585)697-6565 or visit stannscommunity.com.
Family nurse practitioner Katie

Schaeffer McCool recently joined the internal medicine department at the Farmington office of UR Medicine
Thompson Health’s Canandaigua Medical Group.
Born and raised in Canandaigua, McCool is a resident of
Shortsville who first joined Thompson in 2008 as a pharmacy technician. Most recently, she was an urgent care provider for the health system, where she has also worked as a registered nurse in the ICU and as an eRecord-credentialed trainer.
Certified by the American Association of Nurse Practitioners, McCool obtained her bachelor’s in nursing from the St. John Fisher University Wegmans School of Nursing in Rochester and her master’s as a nurse practitioner — with a certificate in education — from SUNY Upstate Medical University in Syracuse. McCool is based in the medical group’s Farmington office, at 1160 Corporate Drive.
Excellus BlueCross BlueShield announced the recipients of its Health Equity Innovation Awards, designed to support community programs and services that focus on combating racial and ethnic health disparities across Upstate New York.
Last year, Excellus BCBS called on organizations to apply for grants that would fund initiatives, programs and research that confront the fundamental causes of health inequities, with an emphasis on the impact of structural racism.
The health plan hopes the awards will help to enhance the physical and mental health of local communities, reduce social disparities in healthcare, and promote equitable access to health services.
The funding, which totals more than $500,000, will benefit 19 nonprofit 501(c)(3) organizations in the Rochester, Central New York/Southern Tier and Utica/North Country regions.
Recipients were chosen from an application pool of nearly 300 submissions based on their well-defined objectives and quantifiable results aimed at diminishing health disparities and advancing health equity.
Funding from the Excellus BCBS Health Equity Innovation Awards will support the following initiatives:
• Ibero American Action League, Inc.: Funding will support the community resource center as it offers English for Speakers of Other Languages (ESOL) classes for adults and their children, starting in 2025.
• Partners in Community Development – BIPOC PEEEEEEK Parent Mental Health Project: Program will support mental health peer advocates to bring their direct experiences, along with an understanding of the culture and the stress and traumas they experience, to community resi-
dents.
• Prosper Rochester: Program will support the expansion of local students' access to timely mental health services by strengthening school-community partnerships and leveraging shared resources.
• Rochester General Hospital: Program will support a train-the-trainer model and will use Rochester Regional Health-branded CPR training kits and American Heart Association CPR educators.
• Finger Lakes Community Action: Program will support free early intervention screenings for children aged 12-60 months throughout Wayne County.
in Central New York, Southern Tier and Mohawk Valley
Excellus BCBS also awarded several nonprofit organizations in the Central New York, Southern Tier, Utica and the North Country regions. They are:
• Cayuga County Community Health Network, Inc.;
• Cortland Area Communities That Care Coalition, Inc.;
• Crouse Health Foundation;
• Farnham Family Services;
• Hopeprint, Inc.;
• SAGE Upstate;
• Syracuse Community Health Center;
• Broome County Council of Churches;
• CareFirstNY;
• Economic Opportunity Program;
• Family Service Society;
• Meals on Wheels of Chemung County;
• MV Resource Center for Refugees;
• Planned Parenthood of the North Country.
For the latest information on Excellus BlueCross BlueShield’s ’s community investments and partnerships, visit, ExcellusBCBS.com/ community.
Hybrid Nurse Aide Training Program ELEMENTAL MANAGEMENT GROUP




Hybrid Nurse Aide Training Program ELEMENTAL MANAGEMENT GROUP







Equip your facility with our unstoppable HYBRID CNA program, empower your team to deliver top-notch care with the strength of a champion.
Equip your facility with our unstoppable HYBRID CNA program, empower your team to deliver top-notch care with the strength of a champion.
Are you looking for an innovative way to attract CNA students? We have your answer
Are you looking for an innovative way to attract CNA students? We have your answer
Are you looking to minimize and most importantly eliminate agency use? We have your solution
Are you looking to minimize and most importantly eliminate agency use? We have your solution
Are you looking to improve morale by increasing your direct care PPD? Reach out to us to hear more
Are you looking to improve morale by increasing your direct care PPD? Reach out to us to hear more
Are you looking to captivate and motivate the newer generation by offering unique and rewarding training opportunities? Look no further contact us today
Are you looking to captivate and motivate the newer generation by offering unique and rewarding training opportunities? Look no further contact us today

CONTACT:

Peg Reith BSN, RN
Phone: 315-529-3267
CONTACT:
Email: CNA_Training@elementalmgt.com
Peg Reith BSN, RN
Phone: 315-529-3267
Email: CNA_Training@elementalmgt.com










