




Americans have the worst health care among the world’s wealthy nations, a new report says.
People in the United States die the earliest and live the sickest lives out of 10 developed countries, even though the United States spends the most on health care, according to the annual report by health care thinktank The Commonwealth Fund.
Australia, the Netherlands and the United Kingdom rank highest out of the 10 countries included in “Mirror, Mirror 2024: A Portrait of the Failing U.S. Health System.”
“While other nations have successfully met their populations’ health needs, the U.S. health system continues to lag significantly,” said Reginald Williams II, vice president of international health policy and practice innovations with The Commonwealth Fund.
For the report, researchers compared nations’ health systems based on 70 specific measures across five

areas of performance. Other nations measured against the United States included Canada, France, Germany, New Zealand, Sweden and Switzerland.
The report found that:
• People in the United States have the shortest lives and the most avoidable deaths, ranking dead last on five out of six health outcome measures;
• Americans face the most barriers to obtaining health care. About 25 million people remain uninsured in this country, and nearly a quarter can’t afford care when they need it;
• The United States ranks lowest in health equity, with many low-income people unable to afford care and more groups reporting unfair treatment and discrimination when seeking care;
• Patients and doctors in the United States experience heavy administrative burdens when it comes to payment, billing and paperwork, with the system outranking only
Switzerland in its lack of efficiency. The United States had just one bright spot in the report.
The nation ranked second among the countries in “care process,” which includes prevention, safety and patient engagement. The Affordable Care Act’s emphasis on patient safety and preventive services partly explains the high ranking, the researchers said.
“The U.S. is failing one of its principal obligations as a nation: to protect the health and welfare of its people,” said physician Joseph Betancourt, president of the Commonwealth Fund.
“The status quo — continually spending the most and getting the least for our health care dollars — is not sustainable,” Betancourt added in a Commonwealth Fund news release. “It isn’t about lack of resources — it’s clearly about how they are being spent. Too many Americans are living shorter, sicker lives because of this failure.”
The report argues that the United States could improve its health care comparative to other nations by:
• Extending coverage to the remaining uninsured and reforming health insurance to limit out-of-pocket expenses;
• Investing in primary care providers, so more are available to patients;
• Removing health inequities faced by minority and ethnic groups, rural residents and women;
• Curbing the uncontrolled consolidation of health care systems, which is driving prices higher;
• Address social drivers of health like poverty, homelessness, hunger, gun violence and substance use.
“This report shows that by adopting proven strategies and making smart investments, America can enhance its health system to better meet the needs of its people,” Williams said. “There’s no reason we can’t elevate our standing if we choose to do so.”

Convenient access. Personalized attention.

Personal Medicine of Rochester’s physicians are dedicated to serving patients with a high standard of care and all the attention you deserve.
Benefits you can count on for an affordable membership fee
• See a physician at each visit and never feel rushed.
• Same day or next day appointments.
• Urgent need after hours? Contact your doctor directly.
• Comprehensive annual health screenings that surpass standard checkups.
• Personalized wellness plan with the resources you need to achieve your goals.
Now accepting new patients, age 18+ for a limited time.



By Chris Motola
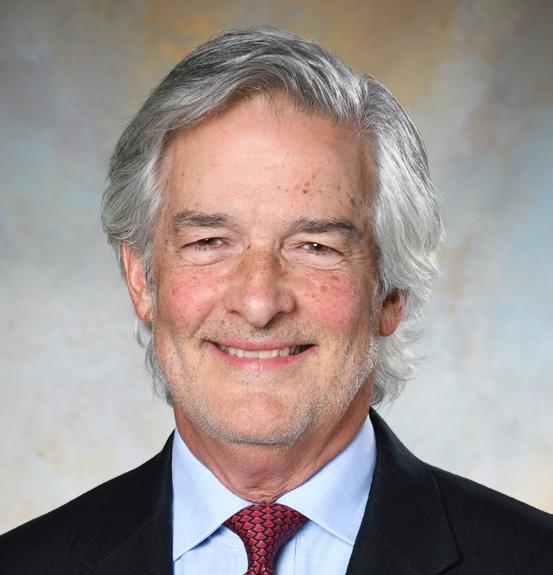
Petrescu, M.D.
Doctor who started a solo direct primary care practice in 2022, breaking away from the traditional, insurance-based healthcare system, says business is still growing
Q: We interviewed you back in 2022 when you had first started your private practice, Athena Direct Primary Care & Lifestyle Medicine. How has it developed since then?
A: Yes, we opened in January 2022, so we're on our third year now. The practice has been growing tremendously and I couldn't be happier with the move we've made to break away from the traditional, insurance-based healthcare system where we're all in a box where you have to do things based on certain protocols without the time to really listen, understand and partner with our patients. So, yes, we're still early in this venture but the practice has been growing tremendously.
Q: What do you attribute the growth to?
A: I think there's a tremendous need in our community for doctors who partner with their patients. It took a little for people to grasp the concept of direct primary care, which is a membership-based primary care prac tice. Because we live in a world of insur ance-based medicine people aren't aware of the advantages of having a partnership directly with a physician and cutting out the red tape of corporate medicine and insurance companies. But this is exactly what I do in my practice. I work for my patients. I'm here for my patients. And I'm not constricted within five-minute appointments to see my primary care patients.
Q: How much time are you able to give pa tients, on average?
A: I typically take one hour or even two hours to see my patients so I really have time to listen to my patients and create a treatment plan that really works for them. It's a true, won derful journey. So for me as a practitioner, as a physician, it's wonderful to
be able to apply my knowledge and my skills. I'm a triple-board certified physician. I have over 20 years of experience. I demand time with my patients. I cannot do good medicine in a five-minute appointment. With this practice I can take the time I need to dive into all aspects of the person's health. I'm a strong believer in whole-person care, looking at all aspects of physical health, mental health, emotional health and putting all aspects of the puzzle together not only treating symptoms. It's really fulfilling to me when I get to see patients improve and make a really meaningful change to their health. I'm happy to come to work every day. I'm in the middle of my career, so I hope to be able to expand services to more members of the community and find physicians to
for the practice to be very focused on preventive health, lifestyle intervention, nutrition, physical activity, stress management and sleep as means of staying healthy. Right now in the larger health system there's a focus on band-aids, meaning if you're sick you get a pill or prescription and off you go. We don't want to wait until you're sick to “fix” you. We're not looking to just avoid disease and exist but to optimize health and thrive. So it's very important to me that the team be aligned on those issues. We haven't found that person yet, but I think we're coming very close and have a few candidates who might fit the bill.
Q: How many patients are you able to manage with this model? What's the ideal number?
A: That is the biggest limitation. I'm one physician. I can only manage about 10% of the patients that a typical primary care doctor can take in a traditional practice.
Q: What kinds of patients have been most interested in this model? Is it getting a better reception from older or younger patients?

A: Very interesting question. My youngest patient is 18; my oldest is 97, so I'm seeing the full range. I have a lot younger patients in their 20s, 30s and 40s who are very interested in optimizing their health and staying healthy. Because of the nature of my practice, there is some self-selection bias with patients. Regardless of the age, they're people who value their health and are looking for guidance. But I do have a full spectrum of ages. I think the average patient would be in their 40s and 50s, with outliers on both sides.
Q: Do you use insurance at all?
A: That's an important question. All services in the practice are under the membership fee. However, they can use insurance for all services outside of my practice. For medications, labs, consults, other prescriptions. I can put those orders in, and the lab or pharmacy can bill the insurance. That's an important difference between my practice and concierge services. I'm not a concierge practice. I'm a direct primary care practice. I do not bill insurance for my services and there's no fee for service, just the membership fee. Concierge services bill insurance in addition to their membership fee.
Q: When you came to the U.S. from Romania, did you have a sense that you'd want to try this kind of practice or did the idea develop over time in the U.S. hospital system.
A: I didn't move to Rochester with the intention of opening a direct primary care practice. In fact, I didn't have any
‘I'm a tripleboard certified physician. I have over 20 years of experience. I demand time with my patients. I cannot do good medicine in a five-minute appointment.’
idea that such a practice model existed. I worked in a traditional practice for 20 years and came to learn about the direct primary care movement around 2019, which has also been around for about 20 years in the U.S. but was pretty new to Upstate New York. I was already at the point where I felt like I couldn't apply my skills the way I wanted to in the system. So I gave it a try despite it being a pretty new concept in New York at the time.
Q: How should other physicians go about deciding if this is a good model for them?
A: In general we need alternatives. We need options. People feel like they're stuck in the system without options. Having a private practice isn't for everyone. It carries a lot of risk. Being a business owner isn't for everyone, but if you're looking at going beyond what the existing system offers, this is a very simple alternative. It can be done. I'm the first in Rochester to prove that the concept works, but I don't think I'll be the last. I'm hoping the younger generation will see the value in doing things differently. If we want different results than what the system is producing then we have to.
Name: Laura Petrescu, M.D.
Position: Founder, and CEO of Athena Direct Primary Care & Lifestyle Medicine, Pittsford
Hometown: Iasi, Romania
Education: Grigore T. Popa University of Medicine and Pharmacy, Romania
Affiliations: Rochester Regional Health
Organizations: American College of Lifestyle Medicine; American Board of Internal Medicine; American College of Physician Executives; Direct Primary Care Alliance
Family: Husband, two sons
Hobbies: Classical music, playing piano, reading, winter sports

Workplace anxiety. Who hasn’t experienced it?
However, if that anxiety is so strong that it hurts your performance or lingers for months, you might have a problem, one expert says.
Physician Asim Shah, executive vice chairman in the Menninger Department of Psychiatry and Behavioral Sciences at Baylor Colege of Medicine in Houston, explains what can trigger workplace anxiety, how to manage it and when to seek professional help.
“The goal is not to suffer and not let your anxiety affect work performance. About 60% of people experience workplace anxiety. It is common, which means you can do something about it,” Shah said.
Workplace anxiety can be caused by surly coworkers, a demanding supervisor, small, annoying tasks or overwhelming major projects.
If you have workplace anxiety, you might notice signs like:
• Feeling overly anxious or nervous;
• Experiencing excessive sweating or trembling;
• Obsessing about a task;
• Having a lack of interest in your work.
“The anxiety becomes so overwhelming that you are unable to focus and concentrate,” Shah noted in a Baylor news release. “These feelings can impair your daily work functions.”
If that continues for more than six months, Shah said it might be time to seek professional help.
“Some employers might offer an employee assistance program where you can go for help. You can also start talking to a therapist through psychotherapy or look into medication management for your workplace anxiety,” he said.
To manage it and help to reduce stress, Shah recommends:
• Break your tasks into small pieces;
• Set small goals throughout the work week and congratulate yourself for reaching them;
• Express your emotions. Journal how you feel. Talk, laugh or cry with someone you confide in;
• Start healthy habits and do things you enjoy;
• Work within your limits. Set boundaries with your workload.
A monthly newspaper published by Local News, Inc. Distribution: 33,500 copies throughout more than 1,500 high-traffic locations.
In Good Health is published 12 times a year by Local News, Inc. © 2024 by Local News, Inc. All rights reserved. P.O. Box 525, Victor NY 14564. Phone: 585-421-8109 • Email: Editor@GVhealthnews.com
Editor & Publisher: Wagner Dotto • Writers: Deborah J. Sergeant, Chris Motola, George Chapman, Gwenn Voelcker, Anne Palumbo, Jim Miller, Mike Costanza
Shaina Zazzaro, Barbara Pierce, Mark Weimberg (M.D.), Miranda Chacon (M.D.)
Advertising: Anne Westcott (585-421-8109) • Linda Covington (585-750-7051)
Layout & Design: Angel Campos–Toro • Office Secretary Allison Lockwood
No material may be reproduced in whole or in part from this publication without the express written permission of the publisher. The information in this publication is intended to complement—not to take the place of—the recommendations of your health provider. Consult your physician before making major changes in your lifestyle or health care regimen.
November








By George W. Chapman

The Inflation Reduction Act has already capped insulin at $35 a month for seniors on Medicare. In 2025, out-of-pocket costs for prescriptions will be capped at $2,000 a year. These alone will save members $1.5 billion a year. The Centers for Medicare and Medicaid Services (CMS) is just about done negotiating
While CMS finally negotiates drug prices for over 60 million Medicare recipients, commercial insurers that cover employees are on their own. Drug manufacturers are free to charge whatever they want. A senate committee recently grilled the CEO of Novo Nordisk, maker of Ozempic for Type 2 diabetes and Wegovy for weight loss. The difference in pricing between the U.S. and other countries is sickening if not criminal. In the U.S., Ozempic costs $969 a month. Yes — a month. It’s $59 in Germany; $71 in France; $122 in Denmark; and $122 in Canada.
pricing with drug manufacturers for the first 10 drugs under the Inflation Reduction Act. The reduced prices will be in effect 2026. CMS will begin round two of price negotiations for another 15 drugs effective 2027. These savings on just 25 drugs will be in the billions for CMS and Medi-

perverse incentive against negotiating a really low price. The FTC has released a damning report on PBMs.)
The Novo Nordisk CEO absolutely knows the real reason why we pay so much more in the U.S. He just didn’t want to admit it. All the other countries have national health and negociate prices for every drug covered, including Ozempic and Wegovy, by their national plans for every citizen. Not just 10 prices for their seniors. I’m sure there were a few senators on the committee sheepishly looking at their hands because they accept money from the ubiquitous and wealthy drug lobby.
Everyone at the hearing knew exactly what the answer was. And until we have a national plan, the drug lobby will grease palms and we will continue to be ripped off by drug manufacturers and PBMs.
care recipients. Part D premiums will decrease next year from 2024 levels. For advantage plan members, the average monthly premium will decrease from $18.29 to $17. For Medicare members with traditional coverage, the average monthly premium will decrease from $41.63 to $40.
in congress that would make the tax credit premium for fear people will drop coverage without it. Overall, 45 million of us are covered by the ACA.
‘I looked up hospitals in the broad region covering Watertown to Binghamton and Rochester to Albany. I didn’t find a 5-star facility. But I found four hospitals that received a 4-star rating: Guthrie in Cortland, Albany VA, St. Peter’s Albany and Cayuga Medical in Ithaca. All the other hospitals in the region received two or three stars.
seniors, employers must face cost reduction on their own. Premiums for commercial insurance could increase anywhere between 7% and 9% next year which means the U.S. will retain its ignominious lead in average per capita cost at $16,000. A recent survey found most employers are looking to cut costs thereby limiting cost shifting to their employees. A third of employers, however, say they will continue to shift costs to their employees via premium contributions, higher deductibles and higher copays. Twenty-one percent will offer drug discount cards and direct to consumer prescriptions and delivery. Forty-three percent will bid out their health plan. Thirty percent plan to explore narrower networks. Thirty-eight percent will reevaluate employee assistance programs like mental health. The top area of focus for all employers is drug costs, especially for weight management, cardiovascular health, cancer and women’s health.


In the U.S., Wegovy costs $1,349 a month. Again. A month. It’s $92 in the UK; $137 in Germany; $186 in Denmark; and $265 in Canada.
When pressed by the committee why, the CEO skirted the question and tried to put the entire blame on PBMs or pharmacy benefit managers. Really? While PBMs are another problem altogether, they are in no way accountable for the absurd differences in costs, (PBMs “negotiate” prices for their clients. But they get a payment of around 74 cents for every dollar eventually charged by Novo Nordisk. So, there is sort of a
Over 12 million of us purchase health insurance on the exchange. Premiums are discounted based on federal poverty guidelines. As an incentive to buy insurance, qualifying households are eligible for a premium tax credit. The average is about $800. The tax credit will expire next year. There is a bill
CVS ventured outside its pharmacy “lane” or area of expertise when it expanded into primary care clinics, pharmacy benefit management (Caremark) and insurance (Aetna Medicare) among other things. Their multifaceted business model intended to offer easy accessible, low cost, integrated care. As with many corporations, rapid overdiversification can lead to its downfall. CVS stock had fallen 20% from last year while the rest of the S&P has risen 21%. Industry experts surmise the negative press associated with PBMs and lower profits in their Medicare product could put both businesses on the chopping block.
Who isn’t? While Medicare is tackling costs via the Inflation Reduction Act and reducing premiums for

CMS surveys our nursing homes and hospitals every two to three years. Hospitals receive a detailed report and must submit a plan of correction. Failure to improve can impact Medicare reimbursement. CMS uses a 5-star rating system. Metrics include quality, safety, staffing, etc. The average score for NYS hospitals is about 2.5 stars. Thirty-four of 133 NYS hospitals received one star. That’s 26%. The national average is 10%. You can look up a hospital or nursing home rating on Medicare.gov. I looked up hospitals in the broad region covering Watertown to Binghamton and Rochester to Albany. I didn’t find a 5-star facility. But I found four hospitals that received a 4-star rating: Guthrie in Cortland, Albany VA, St. Peter’s Albany and Cayuga Medical in Ithaca. All the other hospitals in the region received two or three stars.
George W. Chapman is a healthcare business consultant who works exclusively with physicians, hospitals and healthcare organizations. He operates GW Chapman Consulting based in Syracuse.
Writer recalls the hours before hurricane Milton hit Florida … and right after it. ‘The massive destruction this storm left behind is devastating,’ she writes
By Barbara Pierce
Tuesday: Oct. 8: “There’s a category 5 hurricane coming this way!” my daughter says as I answer her call. “We’re evacuating. You should, too.”
Oncoming hurricane Milton is rapidly intensifying, surprising everyone with its rapid buildup. Hurricanes are rated category 1 to 5 — 5 being the worst.
“Catastrophic,” “life threatening,” “unprecedented,” are the words I hear when I turn on TV to learn more.
I’m sitting right in the path of where it’s expected to make landfall.
I’m in an evacuation zone, meaning I’m in a most vulnerable area and should not stay during the hurricane.
I’ve been through several hurricanes in Florida, my home state. It was difficult to sit there with the wind howling, the rains pouring and
It’s not getting through hour and hour of the hurricane’s fury — it’s the aftermath that’s heartbreaking.
I am not leaving for this hurricane. I have severe back pain. I’d spent the last days and nights in a recliner, positioned at exactly the right level, with an ice pack as that was the only thing tolerable. I couldn’t sit in my car and drive, with hundreds of others, to go to someplace strange. And hotels don’t offer recliners to sleep in.
I meet others in my building.
“Are you leaving?” wee ask each other. “We’re staying,” was often the answer. “We’re troupers. We’ve got this. We’re not scared.”
I’ve been through hurricanes before. I can do this. But they keep saying there’s never been such a powerful, forceful one. This one does seem different.
their cars, load their dogs and drive off. “You should leave,” they tell me. I drive downtown. Traffic in downtown is usually gridlocked, moving slowly along. Now there are one or two other cars. It’s eerie. Very creepy.
My brother calls from the other side of Florida. “Come stay with me. It’s not safe for you there.”
My ex calls several times. “You must leave now,” he commands. “Why aren’t you leaving?”
I can’t drive anywhere as the pain of driving would be intolerable after only a short time.
I talk to my few friends. We wish each other well. We’re all scared, really scared. “Stay safe,” we say to eachother.
Our building is only 10 years old. It seems sturdy; I should be safe here. I’m on the fourth floor. I’ll be OK if the river next to the building overflows. I’ll hide in an interior bathroom to keep safe if I need to.
As flooding is likely, I take my car out of the first-floor garage and move it to the second floor.
Wednesday, Oct. 9: Rain steady all day. By afternoon, the wind sounds like a train going overhead, hour after hour, rumbling, growling, growing louder and louder. Rain becomes intense a steady, heavy downpour.
I was fortunate because my power didn’t go out until about 10 p.m. I could watch the storm on TV. The landfall came right over us; the
buildings but killing people in their path.
After the power goes out, I sit in my recliner, hearing the loud, loud wind battering the roof. When I get up, the floor shakes from the vibrations of the wind. I trusted this sturdy building; the floor shouldn’t be trembling.
Thursday, Oct. 10: I wake up. Much to my happy surprise, my power is already back on. I watch TV with tears as I see that trees are down, power lines are down. It’s not safe to go out. The roads are blocked by downed trees and there are no traffic lights. Many homes are without power. Mobile homes have been destroyed or roofs gone. Several neighborhoods are flooded; people have lost everything.
The massive destruction this storm left behind is devastating.
It’s a bright sunny day. That makes me very angry!
Florida, you lured us here with your seductive sunshine, balmy winters, glorious blue skies and lovely fluffy white clouds. Behind this beautiful façade lies the cruelty of hurricanes, a threat becoming more and more powerful and intense each year, destroying the lives of so many people. I’m done. Time to leave Florida.




By Gwenn Voelckers
Thanksgiving is around the corner, marking the beginning of the holiday season — a time filled with food, family, joy and sometimes stress.
For many, it’s also a time of adjustment to a new way of living, especially if you’re newly on your own after a divorce or the loss of a spouse.
Maybe this is your first holiday season solo and you’re discovering that the freedom to make your own choices is both exhilarating and overwhelming.
One of the most critical lessons I’ve learned on this journey is that living alone successfully requires more than just setting the table for yourself — it requires the strength to set boundaries and say “no, thank you” when necessary.
Why is it so hard to set boundaries?
Setting boundaries, especially around the holidays, can feel incredibly challenging. I can remember not wanting to disappoint others, feeling guilty for saying no or worrying that people would think I was selfish.
Setting boundaries isn’t about being selfish; it’s about being selfaware. By saying no to certain things, you’re saying yes to your peace of mind, your health and your happiness.
You’re establishing healthier relationships by communicating your needs clearly and honestly. You’re guarding your heart and building self-respect.
The truth is, boundaries allow us to show up more fully in the relationships and activities that matter most. Without them, we spread ourselves too thin, risking burnout and
resentment.
So, this Thanksgiving, along with the turkey and pumpkin pie, let’s serve up a healthy helping of selfcare by learning how to say no when we need to.
The first time I said no to a party invitation that I didn’t feel like attending, I felt an odd mixture of guilt and relief. It wasn’t that I didn’t like the people throwing the party — I did. But the truth was, I just didn’t have the steam to go.
Here’s how I handled it: “Thank you so much for inviting me! I really appreciate being included and love spending time with you. However, I’m going to have to pass this time. I’ve been feeling overwhelmed lately and need to take some ‘me time’ to recharge my batteries. I look forward to connecting with you when life slows down.”
By expressing gratitude for the invitation and suggesting a future connection, I was able to decline in a way that felt comfortable and respectful.
Then there was the late-night request from a friend: “Can you pick me up from the airport?” The flight landed at 11:30 p.m. and while I used to be the kind of person who would bend over backward to help out, I realized that driving across town late at night was more than I was willing (or felt safe) to do.
My response? “I’d love to help, but I’m not comfortable driving that late in the evening. Can I help you
find a taxi or ride-sharing service?” By offering an alternative solution, I was still helpful without sacrificing my own comfort and safety.
Boundaries don’t just come into play with friends and family.
Sometimes, they’re necessary with neighbors or acquaintances. Like when my widowed neighbor started showing up at my house unannounced, asking for my opinions on fall cleanup and other light-hearted matters.
It was innocent at first — friendly chats, small favors — but then it started to feel uncomfortable.
One afternoon, he asked if I’d like to go to dinner. It took me by surprise and I told him, “I’m very flattered. Let me think about it.”
I knew I wasn’t interested in taking the relationship further and needed to set a boundary.
After going over several scenarios in my head, I finally arrived at what I wanted to say. With a kind smile, I simply said, “I’m sorry but I have to decline your very nice offer to take me to dinner. I value our friendship too much to do anything that might disrupt what we have. You’re a great friend and I like things just the way they are! I hope you understand.”
Yes, I was nervous, but I managed to keep my voice friendly and calm.
Thankfully, he nodded OK with a smile and I felt enormous relief as well as pride for setting a very challenging boundary.
Tip 4: Opting out of gift exchanges
Holidays often come with traditions that no longer feel right, like gift exchanges.
A good friend and I had exchanged gifts every year for decades. But last year, I realized it was beginning to feel more like an obligation than a joyful tradition.
I approached her with honesty: “I’ve loved our gift exchanges over the years, but I’m trying to simplify things this holiday season. How about we skip the gifts this year and just do something fun together instead?”
sive episode and 30% more likely to commit suicide today than they were 20 years ago,” according to a UCSF news release.
At the same time, the average U.S. tween spends 5.5 hours per day looking at a screen, the researchers said, and that rises to 8.5 hours for teenagers.
Could there be a link?
She was relieved! As it turned out, she’d been feeling the same way but hadn’t known how to bring it up.
Tip 5: Saying no to hosting a guest
Lastly, there’s the ever-persistent request from friends or family to stay at your place when they’re in town. For some people, it’s no problem, but for others, hosting can be overwhelming, especially during the holidays when life is already hectic. When a family member asked to “crash” at my place for several days, I had to be honest.
“I’d love to see you, but I’m not able to host this time around. This holiday season will be a busy one for me this year with band rehearsals and concerts. I know I’m going to need my own space to relax, practice my music and prepare for our upcoming performances. Let me help you find a nearby hotel.”
It’s important to protect your space and energy, especially when you’re still adjusting to living alone.
Encouragement for the season
As we head into the holiday season, I want to remind you — and myself — that setting boundaries is an act of self-love.
So, as you set the table this Thanksgiving, remember that you’re also setting the table for your own well-being. Say yes to what fills your heart and brings you joy and say no, thank you, to the things that drain you.
This holiday season, may you find peace, joy and the courage to prioritize yourself. Happy Thanksgiving!

Gwenn Voelckers is the author of “Alone and Content: Inspiring, empowering essays to help divorced and widowed women feel whole and complete on their own.” She welcomes your thoughts on this column as well as topic suggestion for future essays at gvoelckers@rochester. rr.com.
daily time spent staring at screens had a 10% higher odds for depression, a 7% higher risk for conduct issues, and a 6% higher risk for ADHD, compared to children with lower rates of screen use.
Astudy tracking almost 10,000 9- and 10-year olds for two years finds a link between time spent watching TV and other screens with a higher odds for ADHD and depression.
“Screen use may replace time spent engaging in physical activity, sleep, socializing in person and other behaviors that reduce depression and
anxiety,” said study lead author, physician Jason Nagata, of the University of California, San Francisco (UCSF). His team published its findings Oct. 7 in the journal BMC Public Health.
As Nagata’s group noted, mental health issues have been on the rise among adolescents.
“Adolescents are 50% more likely to experience a major depres-
To find out, Nagata’s team tracked data for 2016 through 2018 for 9,538 adolescents aged 9 and 10 enrolled in a major child brain development study. The children’s daily screen time and their rate of diagnoses for conduct disorders, depression, ADHD and other mental health issues were monitored.
The study couldn’t prove cause and effect, but the team did find small but significant associations.
“Higher total screen time was associated with all mental health symptoms,” the researchers reported.
Kids with the highest levels of
“The specific screen types with the greatest associations with depressive symptoms included video chat, texting, videos and video games,” Nagata and colleagues noted. The effect also seemed stronger for white adolescents than for Black adolescents.
“For minority adolescents, screens and social media may play a different role, serving as important platforms to connect with peers who share similar backgrounds and experiences,” said Nagata, an associate professor of pediatrics at UCSF. “Rather than displacing in-person relationships, technology may help them expand their support networks beyond what’s accessible in their immediate environment.”
By Eva Briggs, MD
Recently a friend asked me about the Inspire device to treat sleep apnea. I wasn’t familiar so I looked it up. Here is what I learned. Sleep apnea refers to stopped breathing occurring during sleep. There are several types: obstructive, central and mixed.
• Obstructive sleep apnea occurs when changes in the shape of the mouth and throat during sleep block air passage. It becomes more common with age. Examples include the tongue falling back against the soft palate or large tonsils. Symptoms include snoring or gasping during sleep, feeling drowsy during the day, trouble concentrating, dry mouth and headaches. But even children, such as those with enlarged tonsils or adenoids, can have OSA.
• Central sleep apnea occurs when the brain and nervous system fail to signal the body to breathe. Symptoms include daytime sleepiness, awakening feeling panicked or short of breath and insomnia. Causes include sedating drugs, sleeping at high altitudes and congestive heart failure. Some cases are idiopathic meaning there is no known underlying cause.
• Mixed sleep apnea combines both OSA and central sleep apnea.
The Inspire device treats OSA. Other treatments for OSA include CPAP (continuous positive airway pressure), surgical interventions to change the shape of the upper airway and oral appliances. The Inspire can treat patients that have tried and failed less invasive treatments.
The Inspire is designed to stimulate the genioglossus muscle, a muscle whose contraction moves the tongue forward thus opening the airway.
There are three components to the device. First is a small impulse generator, which is implanted under the collar bone. Second is a breathing sensor tunneled from the impulse generator to the chest wall muscles. This detects when the person is inhaling, telling the impulse generator to send a signal to the tongue to move forward. The third piece is a lead that tunnels from the impulse generator to a nerve stimulator lead placed on a branch of the hypoglossal nerve at the base of the tongue.
Candidates for this procedure must meet strict criteria. First is age, it’s used in adults older than 21. Second is moderate to severe OSA. The patient must have a body mass index less than 33. Patients must have first tried CPAP and have had trouble
E-cigarette use is highest in young adults aged 18–24 years, according to reports
By Miranda Chacon, M.D.
As vaping becomes increasingly prevalent on college campuses, it is of the utmost importance that we address not only the well-established negative health effects, but also the lesser-known detrimental impact it may have on a student’s academic performance.
The addictive nature of nicotine can lead to decreased focus, impaired concentration and diminished cognitive abilities. Additionally, time spent vaping can lead to a decline in productivity and hinder time management skills important for academic success.
While students may recognize that vaping is not beneficial for their health, it is less likely that they acknowledge the impact it can have on their academic performances and, by extension, their future careers.
While traditional cigarette use has decreased in this population, electronic cigarette use has not had such improvement. In fact, e-cigarette use is highest in young adults aged 18–24 years, with a study from JAMA Network reporting as many as 19.7% of individuals in this age

group having vaped at some point. Given the prevalence in this population, colleges must prioritize policies and services that explicitly address both e-cigarettes and vape devices. Tobacco-free policies should be accompanied by educational campaigns that raise awareness about the risks and consequences of vaping, while emphasizing the importance of maintaining a healthy and supportive campus environment. Moreover, counseling services and support
Stimulation lead
Generator
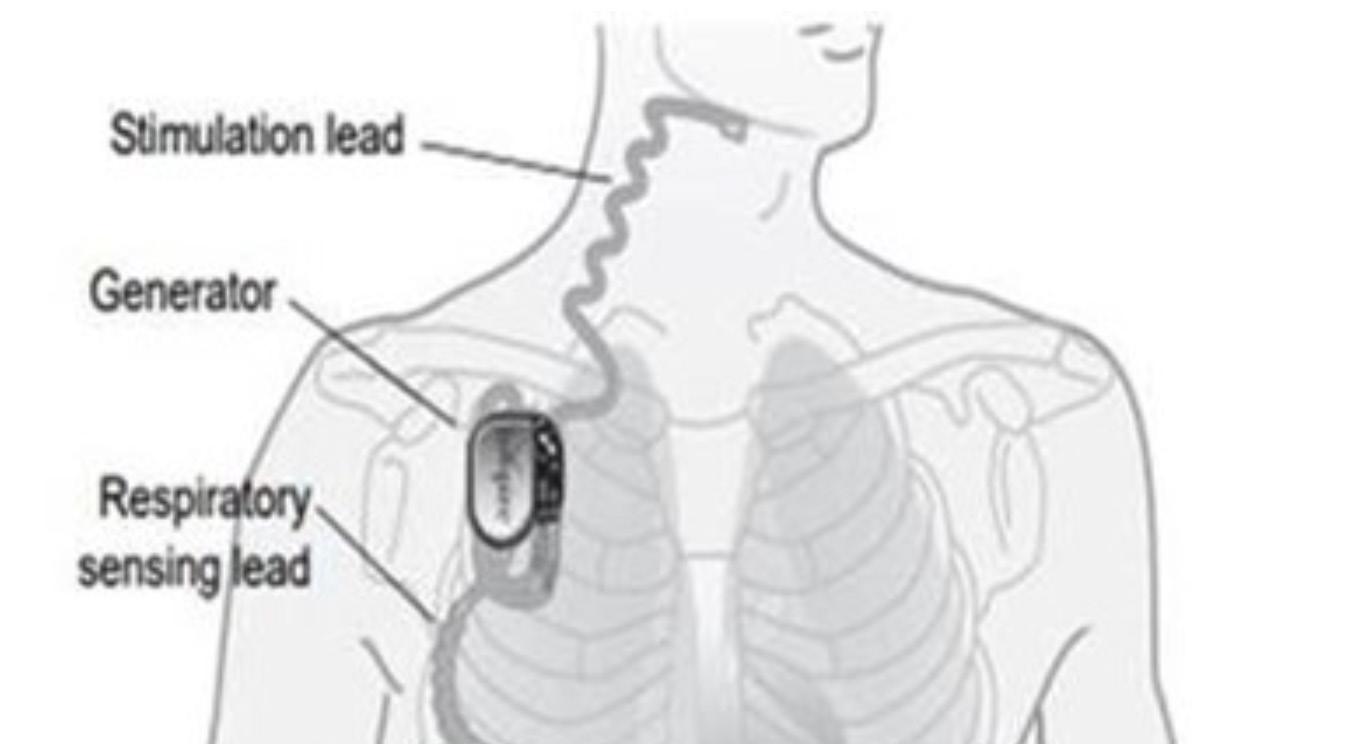
Respiratory sensing lead
tolerating it. Candidates for the procedure must not have significant additional medical problems such as neuromuscular disease, severe heart disease, severe lung disease or significant psychiatric illness. There should be no pronounced upper airway anatomic abnormalities. The patients must also undergo endoscopy during drug-induced sleep that demonstrates airway changes that could be helped by the device.
The procedure for eligible patients is as follows. It is done as an outpatient. There are two incisions. One is under the collarbone to place the battery-powered device. A second incision under the chin is used to place the lead wiring connecting to the nerve at the base of the tongue. The surgery takes about two hours and is performed with general anesthesia. The patient can go home the same day.
After one month, when sufficient healing has occurred, the patient returns for follow up at which time the device is activated. The patient can then use a remote to activate the device in the evening and turn it
groups should be readily available to provide resources for effective cessation. Increasing discussion around campus related to cessation support can normalize such assistance and reduce social stigma, increasing the likelihood that services will be utilized. By offering tailored cessation programs and promoting healthier alternatives, colleges can empower students to make informed choices and support their efforts to quit vaping.
While most are aware of the health effects related to e-cigarette use, the impact of vaping on college students' academic performance should be a larger part of the discussion. Students should be knowledgeable of the ways vaping could inhibit their academic success. It is imperative that colleges take proactive measures by implementing strong policies, raising awareness, and providing support services to ensure the well-being and success of their students.
In addition, if you are a smoker considering quitting, talk with your doctor and contact the New York State Quitline at 1-866-NY-QUITS (866-697-8487) or www.nysmokefree.com, or text DROPTHEVAPE to 88709. Miranda Chacon is a preventive medicine resident physician at University of


off in the morning. The Inspire will require periodic adjustment. The battery is expected to last 10 years before requiring replacement.
As with any surgery, there are risks including bleeding, infection, tongue weakness, tongue numbness, facial weakness, voice change, lung collapse (pneumothorax), limitations of the ability to undergo MRI and tooth movement.
So, as you can see, it is not simple to determine who is a good candidate for the Inspire device. And it is a somewhat involved procedure. So, interested people would need to consult with an appropriately trained specialist.

Eva Briggs is a retired medical doctor who practiced in Central New York for several decades. She lives in Marcellus.


Nearly 8 in 10 Americans go through the day in a fog that interferes with their jobs, their moods and their relationships.
Chalk it up to sleepiness: A new survey shows that 54% of Americans think they just don't get enough sleep.
"Daytime sleepiness is more than just an inconvenience — it can affect our ability to function our best, impacting everything from work productivity to personal relationships," said sleep specialist Alexandre Abreu, a spokesman for the American Academy of Sleep Medicine (AASM), the survey sponsor.
The online poll of more than 2,000 adults was conducted in mid-May and revealed that daytime sleepiness is taking a big toll.
Nearly half (47%) of respondents said it hampers their productivity, making it hard to focus and complete work efficiently. One-third (31%) said sleepiness affects the quality of their work — a complaint more often voiced by men than by women.
A similar percentage (34%) of respondents see effects of sleepiness on their memory and mental recall, and 16% said it affects their reaction time behind the wheel.
Notably, nearly a quarter (24%) said it affects their relationships with family and friends.
"These statistics paint a clear picture of the widespread impact of daytime sleepiness," Abreu said in an AASM news release.
The academy says adults need seven or more hours of sleep a night. It recommends maintaining a consistent bedtime, creating a restful environment for sleep and discussing sleep problems with a doctor.
"It's crucial for individuals to recognize the importance of healthy sleep and seek help if they are struggling to sleep well on a regular basis," Abreu said.

New director of the Spiritus Christi Mental Health Center wears many hats in her new position
By Mike Costanza
Q: You spend about 60% of your time on the job working directly with clients. Could you tell the readers what you do as a mental health counselor for the Spiritus Christi Mental Health Center?
A: I have a caseload of nine clients, co-lead a group for survivors of childhood sexual trauma and conduct initial assessments and intake sessions. A person calls and now I have to figure out the level of urgency, whether we’re a fit for them or they’re better off somewhere else. If they are not a fit for us for some reason, then I will refer them out. I also handle crisis calls from our clients. If they are in crisis, they call me and I either connect them to their therapist or address the situation myself, as indicated. I also provide limited case management services for clients, and engage in case consultations with our therapists.
Q: What kinds of clients do you and the other counselors work with?
A: The problems that we do take on are those of people who are not
Nonprofit providing mental health care served more than 300 people last year. It has a current budget of just $250,000 and all of its services are free.
Q: You were in your mid-50s when you decided to obtain a degree in mental health counseling. Have you always been drawn to that field?
A: From the time I was in my early 20s in college, I felt drawn to counseling as a profession. I actually majored in sociology and minored in psychology and social work and even did an internship in a group home in college. Over the years, I made a few attempts at going back to school for social work or counseling, and something always got in the way of that.
Q: It appears that your time at the mental health center was a catalyst for career change. Is that right?
A: The director at the time, Maureen Marlow, asked me to consider applying for the director’s job when she left. We both agreed that it would be much better for a person who is also a clinician to be in this job — so much of it is clinical. In my mind I envisioned, like, this road that had just opened up. So, I did it.
Q: Are there ways you would like to grow as a mental health counselor during, say, the next five years?
interested in medication at all and simply want psychotherapy. They want some help with depression, anxiety, grief, those kinds of things and they either don’t have insurance or can’t afford the cost given their insurance. Low income plus high deductible plan means “I can’t find anybody who will see me.”
Q: Are there cases that you find particularly challenging?
A: Cases that I find particularly challenging are when the person’s system outside of the counseling room is so lacking that they can’t really show up fully for counseling. Their housing is unstable, the transportation is unstable, they don’t really have a support system around them — family or friends — and yet, they want to work on their depression. Of course, depression is part of what you’re dealing with because of all this other stuff in your life and if there’s so little stability and support outside of here then it’s really hard to work on.
A: I’m still pretty young in this profession. I feel like a lot of what I’m still working on is just increasing my capacity and my skill set for both assessment and for meeting different needs. Different approaches work for different people. You can’t just have three different tools in your toolbox and just apply them to everyone.
Q: Do you have goals you’d like to achieve as director?
A: We used to have psychiatrists here and the last of our psychiatrists retired. That so limits who we can see. Since I took the directorship, I’ve been trying to find someone to provide psychiatry. Something like 67% of our support comes from individuals. Most of that is from Spiritus Christi parishioners and our annual Riverwalk fundraiser, which is held every October. We serve the Greater Rochester area and so one of my goals is for us to expand our base of support and have more individuals throughout the Greater Rochester area investing in us. We’re making this a more healthy community.
For more information on the Spiritus Christi Mental Health Center or to support its mission, go to: https://spirituschristi.org/spiritusministries/mental-health-center.
Shaina Zazzaro at the gym.
"Trust me. I lost 50 pounds. I was stuck in a rut of cardio, cardio, cardio."

By Shaina Zazzaro
ased on my personal experience with using a personal
I can tell you I would never go back to not having one.
There is just something about trusting someone to keep you accountable that makes all the hard work in the gym just feel more worthwhile.
Personal trainers will:
• Become your mentor — a good trainer will be the one person on your side when every other person you know is wondering why you are so into fitness and health.
• Become your teacher — most of us do not know what to do in the gym without some guidance. A good trainer will be a great expert for you
• Get you into the best shape of your life!
Trust me. I lost 50 pounds. I was stuck in a rut of cardio, cardio, cardio. I tried trainer after trainer and then I discovered one that worked well for me. I still do my cardio, but I do light cardio after my hour-long strength training and that combina-
tion has put me into the best shape of my life.
I am stronger, more confident, and feel amazing. Healthy eating (order meal prep and trust me, it will keep you on track) and strength training will put you into the best shape of your life.
If you cannot afford a personal trainer, you can do online classes, find different programs, hire a trainer who can set up a personalized online training course for you, or find trainers like my trainer, Ivan’s Fitness, who do small group training (I love it because I have gained a lot of great friends along the way too!).
Remember, you can’t out-train an unhealthy diet, so always, always eat healthy!
Shaina Zazzaro is a devoted wife and mother of two, blending her roles with a passion for health and wellness. She is the owner of local meal delivery service, Effortlessly Healthy. For more information, visit www.ehmeals.com.







By Deborah Jeanne Sergeant
Of course, prescribed contact lenses help wearers see better. But MySight Lens, an FDA-approved soft, daily disposable lens, can help children slow the progression of myopia, commonly called nearsightedness. Cooper Vision manufactures the lenses.
The lenses are approved for children aged 8-12, the time of peak progression for myopia.
“Often, depending on the degree of myopia, you can use them at any time or age,” said Marc Deeley, optometrist and contact lens specialist with Rochester Regional Health.
He explained that with nearsightedness, light rays focus in front of the retina. Glasses or contacts decrease the power of the eye and bring light to the retina for distance vision. The standard soft lenses create a flat plane of power.
“There’s one power in the lens to bring light to the retina,” Deeley said. “The issue with that with pediatric patients is the globe is round and the retina is round. In the periphery of the eye, you have light that focuses
behind the retina. The eye views those areas as blurry, which stimulates continued eye growth. That’s when prescription starts getting worse.”
The MySight lens offers a dual focus optic design with concentric rings of power throughout the lens, one for nearsightedness and the others for treatment. The treatment zones operate in a similar way to a multi-focal lens.
“They take the peripheral light that was focused behind the retina and create light in front of the retina and decrease stimulus for further eye growth while maintaining good visual acuity,” Deeley said. “It’s creating a power plane that matches the shape of the eye itself. The cool part of this by implementing this lens in patients 8-12, it decreases the progression of nearsightedness by 59%. Forty-one percent of those eyes had no progression at all over the course of three years.”
Typically, providers keep patients in the lens throughout puberty or until there are no signs of progres-

sion and then discuss taking them off those lenses and fitting them with standard contact lenses.
Although transitioning from glasses to contact lenses used to represent another teenager rite of passage, Deeley said that the younger children do a good job of handling and cleaning their lenses and he has experienced no problem with these young lens wearers.
Letting myopia progress unchecked can lead to problems. Deeley listed those as early detached retina, glaucoma, cataracts, floaters “and other conditions that can be devastating.”
Another newer lens innovation is multifocal lenses for adults that

provide near vision.
As contact lens technology progresses, they will continue to provide new benefits to wearers.
“There are considerations for using contacts for glucose monitoring or medication release,” Deeley said. “These may be in the pipelines. There’s a whole other realm of specialty contact lenses for treating eye diseases.
“There are a lot of advances in scleral lenses; they’re developed to be fully customized to the patient based on their eye shape and who have eye conditions that limit them from wearing standard contact lenses.”
Scleral lenses extend to cover part of the white of the eye.
Prepare for new opportunities that stimulate engagement, feed your curiosity, and inspire a fresh desire for learning. St. John’s full array of service options address evolving needs within compassionate community settings.
• Independent Senior Living
• Enhanced Assisted Living
• Respite Care
• Rehabilitation
• Skilled Nursing Care
• Dementia Resource Center
• Hospice Care
Many life-enhancing choices await you.
SCHEDULE A TOUR TODAY. 585-760-1300 | stjohnsliving.org
It's called the MIND diet and its primary aim is to help guard against thinking and memory declines as you age. But does it work?
Yes, claims new research that found following the MIND diet for 10 years produced a small but significant decrease in the risk of developing thinking, memory and concentration problems.
“With the number of people with dementia increasing with the aging population, it's critical to find changes that we can make to delay or slow down the development of cognitive problems,” lead study author, physician Russell Sawyer, an assistant professor of clinical neurology and rehabilitation medicine at the University of Cincinnati's Gardner Neuroscience Institute, said in a news release on the study. “We were especially interested to see whether diet affects the risk of cognitive impairment in both Black and white study participants.”
How does the diet work its magic?
The MIND (Mediterranean-DASH Intervention for Neu-
rodegenerative Delay) diet joins elements of the Mediterranean diet and the DASH diet, which focuses on reducing blood pressure.
“Among the MIND diet components are 10 brain-healthy food groups — green leafy vegetables, other vegetables, nuts, berries, beans, whole grains, seafood, poultry, olive oil and wine,” Sawyer told CNN.
Meanwhile, five unhealthy food groups — red meats, butter and stick margarine, cheese, fried and fast foods, and pastries and sweets — are very limited in the MIND diet, Sawyer added.
“The MIND diet has all the key features — notably an emphasis on real food, mostly plants — required to reduce systemic inflammation, facilitate weight loss, improve the health of the microbiome, ameliorate insulin resistance, lower elevated blood lipids [fats], and slow atherogenesis [clogging of arteries],” physician David Katz, a specialist in preventive and lifestyle medicine who founded the lifestyle as medicine nonprofit True Health Initiative, told CNN.


“That such effects would translate into protection of the brain is anything but a surprise,” Katz added. “This study of association does not, by itself, prove that the MIND diet protects cognitive health, but given the clear mechanisms in play, it certainly suggests it does.”
People who followed the MIND diet more closely were 4% less likely to develop memory and thinking problems than those who did not adhere to it, the study found. The finding held even after factoring in exercise, education, smoking, body
mass index, medical conditions, age and anxiety or depression.
For women, the risk fell even more — they were 6% less likely to develop cognitive impairment.
“These findings warrant further study, especially to examine these varying impacts among men and women and Black and white people, but it's exciting to consider that people could make some simple changes to their diet and potentially reduce or delay their risk of cognitive issues,” Sawyer said in a journal news release.
Employees can fill up to two large bags of food essentials at no cost
JewishHome recently opened its new employee grocery store.
The grocery store will be stocked with staples, produce, frozen goods and more, all free to the majority of employees.
With significant increases in cost of goods such as gas, utilities and rents over the past several years, food insecurity is a real fear of many.
“We saw an opportunity to help address the need with employees at Jewish Home,” says Michael S. King, president and CEO. “This is a unique

offering in our community and we are incredibly pleased to offer this service to our staff.”
The employee grocery store will be open a minimum of twice per month and eligible hourly employees can fill up to two large bags of food essentials at no cost.
“I’m grateful Jewish Home made this accessible to employees,” says Rose Machado, an adir at Jewish Home’s GreenHouse Cottages. “This is a fantastic idea that will definitely help with increased food costs.”


Tips from geriatrician Ahmed Rab, affiliated with Rochester Regional Health:
1 “Have a purpose. Engage in lifelong learning. People with purpose have less dementia. Acquiring new skills supports brain health.
2 “Another thing that resonates well is being as functional as possible and keeping their minds sharp.
3 “Manage stress through mindfulness and meditation. Try yoga: it can lower stress, lower blood pressure and promote longevity.
4 “Focus on cognitive fitness. Puzzles, reading and learning new languages can prevent cognitive decline. Those who stay mentally and physically active have lower risk of cognitive decline.
5 “Maintaining a safe home environment is extremely important. When people have falls and fractures, it sets them back in their ability to live independently at home. Add grab bars, add lighting, make sure the floor is clutter-free and avoid rugs that raise fall risk.
6 “Embrace technology. I have patients who order on Amazon at age 100.
ing, department of medicine at University of Rochester Medical Center:
9 “Stay connected. We are social animals who rely on social connections for our survival. Being socially disconnected — whether being isolated from others or feeling lonely — increases risk for mortality. And some research suggests it is as dangerous to survival as smoking, obesity and being sedentary, the well-known contributors to early mortality. Being socially engaged and feeling connected to and supported


7 “Get depression screenings and get help. As we get older, we lose a spouse. They maybe had experiences with war and kept their feelings buckled in. A lot of my patients are living in senior communities where they have others who have experienced these things. That can help.
8 “Take your medications. As we get older, remembering what to take is hard. We need reminders. I have a couple patients who have alarms go off at certain times so they can stay independent.”
Tips from Kathi
L. Heffner, Ph.D,
professor of nursing, psychiatry and medicine and associate chief of research, division of geriatrics and ag-
Local experts share tips on how we can become healthy centenarians.
By Deborah Jeanne Sergeant
injuries. This restorative aspect of sleep is critical to maintaining our health, both mentally and physically. Inadequate sleep affects the body and brain in ways that heighten risk for illness and chronic disease — our food consumption increases, blood pressure increases, and those toxins don’t get cleared out in the brain, raising risks for Type 2 diabetes, cardiovascular disease or Alzheimer’s disease.
Poor sleep is also tied to feeling more stress and negative emotions. Unless you are a naturally short sleeper that feels refreshed after fivesix hours of sleep a night, most of us need seven or more hours of sleep.
noted, keeping yourself connected to people that make you feel good and getting enough sleep are both great ways to keep your emotions regulated and stress at bay. Taking breaks throughout the day for yourself to do slow, paced breathing, write down or think about what you are grateful for or take a mindful walk where you pay attention and notice what is around you, are evidence-based, daily actions that can quiet the mind and body. While the research is ongoing to determine if these activities can slow biological aging reflected in our DNA, we do know that they help regulate our emotions and body systems, building resilience and protecting our health and wellbeing.”

A good way to tell if you’re getting enough



by others contributes to health and longevity in a number of ways: by providing emotional or tangible support (such as financial resources) to help us through tough times; by keeping us active and our brains stimulated through day-to-day social interactions and by fostering our feelings of value and belonging, which are fundamental needs we have as humans.
10“Get enough sleep. Evidence suggests that people who get adequate sleep live a bit longer than those who don’t. Some large epidemiological studies suggest two to five years longer. So much goes on in our bodies while we sleep, including consolidating memories, clearing out toxins in the brain and healing

sleep is whether you wake up naturally and/or feel refreshed and rested after getting up.
11 “Take breaks. Research is accumulating to support that stress exposure can accelerate our biological clock, which can be measured from our DNA and reflects faster biological aging. Having long-time exposure to stressors, such as managing ongoing medical needs for a child with serous chronic illness, caring for a spouse with dementia or experiencing ongoing psychological distress from childhood trauma, is associated with maladaptive changes to a host of body systems — hormonal, immune, brain — and such changes can both reflect and contribute to accelerated biological aging.
How can we manage stress and keep our body systems regulated? As
Tips from geriatrician Sharon Brangman, faculty at SUNY Upstate Medical University, chairwoman of geriatric medicine and director of the Upstate Center of Excellence for Alzheimer's Disease:
12 “You can be healthy and still have medical problems. The main thing we look for is someone who still has brain power and can get around for the most part. They might need a little help. It doesn’t mean you age without a medical problem.
13 “Everyone needs social engagement. Find something that has meaning and you find has value. So many older people feel marginalized and that they’re no longer contributing.
14 “Find something that you can do with others. Find something you want to learn more about, especially if it involves other people. We learned during the pandemic that people by themselves had increased risk of dementia and overall increase in diseases. Maintain that social engagement. It’s so important. It can be harder as you get older and friends die and family lives far away. Look to senior centers and other programs.”

New research shows that the dramatic increases in life expectancy seen during the 19th and 20th centuries have slowed
lished a paper in the journal Science in 1990 that said that people were approaching a ceiling for life expectancy at about 85. Others disagreed, forecasting that advances in health care would lead to further gains.
The new study — published Oct. 7 in the journal Nature Aging — forecasts that gains in life expectancy will continue to slow as more people experience the unyielding effects of aging.
breakneck speed.”
Even though more people may live to 100, they’ll be the exception, he said. That’s just the opposite of thinking among insurers and wealth-management firms, who make calculations based on the assumption that most people will live to be 100.
“This is profoundly bad advice,” Olshansky said.
While the study notes that









Cataracts are one of the most common eye conditions affecting people as they age. They occur when the lens of the eye becomes cloudy, leading to blurry vision and, if untreated, significant vision loss.
Despite being a prevalent issue, there are still many misconceptions and unanswered questions surrounding cataracts and cataract surgery. More than 20 million Americans are living with cataracts, according to the American Academy of Ophthalmology.
“Without treatment, cataracts can cause severe vision loss, including blindness,” said physician Naveen Mysore, a cataract and cornea specialist at UR Medicine Flaum Eye Institute.
He offers six valuable facts about cataracts.
1.What are the symptoms of cataracts?
The primary symptoms of cataracts include hazy vision, difficulty seeing at night, sensitivity to glare and seeing halos around lights. Colors may appear faded and double vision in one eye can also be a sign. As cataracts progress, these symptoms can become more pronounced, making daily activities increasingly challenging. Most cataracts result from natural changes to the lens in our eyes. The lens bends (refracts) light rays that come into the eye to help you see. A healthy lens is clear. As we age, proteins get deposited in the natural lenses and they become opaque.
Cataracts can cause vision to be blurry and colors may not be as
brilliant. Some people describe it as looking through a foggy or dusty car windshield, said Mysore.
2.When might you need surgery?
Almost everyone older than 50 has some form of a cataract. They can be slow-growing and you may go a few years before it becomes visually significant. During that time, you may have multiple changes in your prescription eyeglasses to compensate for the cataract.
Surgical removal of the cataract and replacement of the lens is the gold standard treatment. This surgery is performed by an ophthalmologist and patients recover at home.
“The time to move forward with elective surgery is when it is affecting your daily activities,” said Mysore. “When considering it, you should ask yourself if vision problems affect your level of independence, can you safely do your job and to drive, is it difficult to cook, shop, do yard work, climb stairs or take medications and do you have problems reading or watching television?”
3.Myths and misconceptions about cataract and cataract surgery
One common myth is that cataract surgery is only for the elderly. In reality, cataracts can develop at any age, though they are more common in older adults. Another misconception is that cataracts are related to cancer. In truth, cataracts are not cancerous; they are a result of the clouding of the eye’s natural lens. Additionally, some believe that cataract surgery is painful or risky,
By Ernst Lamothe Jr
but modern techniques make the procedure relatively painless and safe, with a high success rate.
Young adults and children can be diagnosed with cataracts for a variety of reasons, including genetics, injuries or extended use of some medications. And uncontrolled diabetes or uveitis which is inflammation in the eye can lead to development of cataracts. Many people are surprised that surgery isn’t just removing the cataract. We remove the cataract and replace it with an artificial lens. People think cataracts are removed with laser surgery, but the vast majority of these surgeries are performed by using ultrasonic energy to pulverize the cataract.
4.Is there a family history component to it?
Genetics can play a role in the development of cataracts. Individuals with a family history of cataracts may be at a higher risk of developing them. While aging is the most significant risk factor, a hereditary predisposition can make some people more susceptible to cataract formation at an earlier age.
“Family history results in cataracts developing at a younger age. Congenital cataracts have a prevalence of one in 4,000 to 10,000,” said Mysore.
5.What are the risks for surgery?
Cataract surgery is generally safe, but like any surgery, it comes with potential risks. These include infection, bleeding, retinal detachment and persistent inflammation. Some patients may experience visual dis-
turbances like glare or halos around lights post-surgery. However, these risks are relatively low and the vast majority of patients experience significant improvement in vision.
Surgical removal of the lens and cataract is the only successful treatment for cataracts. It is an outpatient procedure performed by ophthalmologists. It is a routine elective surgery and complete recovery can take up to four weeks, depending upon the density of the cataract. Your ophthalmologist will explain the potential risk for complications, which include but is not limited to infection, loss of support for the lens, retinal detachment, swelling in the retina. They do not occur frequently and most are treatable. In extremely rare cases, blindness can occur.
6.What is the healing process?
The healing process after cataract surgery is usually quick. Most people notice an improvement in vision within a few days. Post-operative care typically involves using prescribed eye drops to prevent infection and reduce inflammation. Patients are generally advised to avoid strenuous activities and heavy lifting for a few weeks. Follow-up appointments are necessary to ensure proper healing and to monitor for any potential complications.
For most people it takes about one to two weeks, depending on the density of the cataract. Your ophthalmologist will prescribe eye drops and provide protective eyeglasses. They will also recommend you delay driving until your eyes are healed.


By Deborah Jeanne Sergeant
They look a bit wobbly and peculiar compared with traditional dumbbells, but kettlebells are gaining in popularity for people who want to grow stronger.
Kettlebells have been used for strength training for thousands of years, possibly originating in ancient Greece. Kettlebells offer a few important differences from dumbbells.
“Kettlebells are most useful for full-body workouts that improve functional fitness: strength, power and endurance,” said Jean Sica, certified tai chi instructor and owner of Kokoro Way in Rochester. “Dumbbells, aka hand weights, are primarily for isolating muscles and building muscle mass. Each tool is valuable and useful in its own way.”
She especially likes how kettlebells are effective in training for specific sports because each sport has a particular movement pattern. Trainers and athletes can tailor kettlebell exercises to meet the needs of the particular sport and the athlete’s needs and goals.
“Pickleball is so popular now,” Sica said. “There is a lot of side shuf-
fling in the sport. The kettlebell can be used to improve lateral quickness, engaging your core and legs. Start with a lightweight bell, eight pounds for instance if you're a woman and swing the bell laterally from one side of your body to the other. Work up to three sets of 12 to 15. I want to emphasize here that proper form is especially critical when working with kettlebells in order to avoid injury. If possible, work with a coach or watch detailed tutorials.”
Kevin Webb, owner of KW Fitness in Vestal, Fayetteville and Cicero, said that the cannonball-with-a-handle shape is what makes kettlebells effective.
“It allows for a range of movements that engage multiple muscle groups, promoting functional strength and endurance,” Webb said. “One of the key benefits of kettlebells is their ability to provide a total-body workout. The off-center weight forces your stabilizing muscles to work harder, improving balance and coordination.”
He said that kettlebells target the core, back and legs, while still
providing great upper-body engagement, unlike dumbbells, which lend towards use for isolated, linear movements. Bicep curls and shoulder presses are two examples.
“While both kettlebells and dumbbells are great for building strength, kettlebells shine when it comes to explosive, swinging motions like the kettlebell swing or clean and press,” Webb said. “These movements generate momentum, which not only builds strength but
also improves cardiovascular endurance. Dumbbells, on the other hand, are better suited for controlled, isolated lifts.
“Whether you're looking to build strength, increase flexibility or boost endurance, kettlebells offer a powerful, dynamic option to elevate your workout.”
Always consult with your healthcare provider before engaging in a new form of exercise.





An arthritis sufferer’s joints start to get ornery when the weather turns colder, getting stiff and achy as the mercury drops.
Cold weather doesn’t cause arthritis, but it can make it worse, experts say.
“Our joints operate best in temperate weather,” said physician Mariko Ishimori, interim director at the Cedars-Sinai Division of Rheumatology in Los Angeles. “When the
weather gets cooler, the synovial fluid that acts like motor oil in our joints becomes more like sludge.”
Frigid temperatures also can increase a person’s pain sensitivity, slow their blood circulation, and promote muscle spasms, the Arthritis Foundation says.
And if that weren’t enough, your joints detect and respond to changes in air pressure that accompany weather fronts.
“A drop in barometric pressure can cause muscles and tendons to expand, which can put more stress on an already crowded joint,” Ishimori said in a Cedars Sinai news release.
“When your joint cap expands, you can feel that.”
But there are some simple steps that people with arthritis can take to protect themselves against joint pain caused by cold weather, experts say.
• Stay warm. Wear hats, gloves
and scarves, and use heating pads and blankets to keep warm while napping. A hot bath also can soothe stiff joints.
• Get moving. Exercise can keep joints loose, boost energy and release a flood of feel-good hormones. Aim for at least 150 minutes of moderate-intensity exercise weekly, including two rounds of strength training.
• Stretch. Be sure to stretch your muscles regularly, especially prior to exercise. Roll the wrists and ankles, do some knee bends and stretch out the fingers and hands.
• Eat healthy. A good diet can help reduce inflammation and boost the immune system, as well as strengthening bones. Be sure to get enough omega-3 fatty acids, which reduce inflammation, as well as bone-strengthening vitamin D.
• Maintain a healthy weight. The more weight a person carries, the more pressure placed on bones, joints and tissues. Dropping some pounds can help reduce pain and stiffness.
• Tread carefully. A simple fall can cause lasting pain, and a person’s sense of balance can be altered by arthritis-damaged joints. Take your time while walking, and wear proper footwear.
These recommendations will vary between people. Ishimori recommends that each person explore how cold weather affects their joints, then pursue the lifestyle changes most apt to make them feel better.
“There’s a lot we can do to ease joint pain and stiffness,” Ishimori said. “You don’t need to suffer in silence.”





By Mark Winsberg, MD
Substance use disorders are often seen as a problem primarily affecting younger people. But they are increasingly prevalent among the elderly.
This trend is concerning because substance use in older adults is often overlooked, despite the fact that its effects can be particularly harmful due to changes in metabolism, overall health and life circumstances.
As baby boomers continue to age, a growing number of older individuals are struggling with substance use disorders involving alcohol, marijuana, opioids, cocaine and benzodiazepines. Understanding the causes, effects and challenges associated with these disorders is crucial for providing effective treatment and support.
Why is substance use a growing problem?
Several factors contribute to the rise in substance use disorders among older adults. The baby boomer generation, born between 1946 and 1964, is living longer than previous generations and many members of this group have used drugs or alcohol earlier in life. As they age, their familiarity with these substances can lead to continued use, which may develop into substance use disorders. Additionally, older adults face significant life changes that can trigger or worsen substance use.
Many are retiring and may feel a loss of purpose or direction, which can lead to increased feelings of loneliness, depression and boredom. Chronic illnesses, aches and pains can become more prevalent with age and some older adults may self-medicate with alcohol or drugs.
Others may turn to substances as a way to cope with grief following
ry loss and increased risk of falls.
The interaction of substance use and prescribed medications
One of the greatest risks associated with substance use as we age is the combination of recreational or illicit drugs with prescribed medications. Many older adults take multiple medications to manage chronic conditions like hypertension, diabetes and arthritis. When alcohol or other substances are added to the mix, the side effects can intensify and lead to serious health consequences. For instance, alcohol can interfere with blood pressure medications, leading to dangerously high or low blood pressure levels. Similarly, combining benzodiazepines with opioids can depress the central nervous system, increasing the risk of overdose.
addressing loneliness and providing mental health support.
• Physical health constraints: Treatment options such as intensive exercise programs or group therapy sessions may not be feasible for all elderly individuals, especially those with limited mobility or other physical health issues.
• Social isolation: Older people who are socially isolated may have fewer family members or friends to recognize the problem and encourage them to seek help.
• Financial limitations: Many older adults are on fixed incomes and may struggle to afford the cost of treatment. In some cases, Medicare or insurance may not fully cover the expenses associated with addiction treatment.
the loss of a spouse, friends or family members.
of substances commonly used
Aging adults are vulnerable to several types of substance use, including both legal and illegal drugs. Common substances that older adults use include:
1. Alcohol: Alcohol remains one of the most frequently used substances among older adults. Social drinking can gradually develop into a habit and many seniors do not realize how alcohol can exacerbate health problems or interact dangerously with prescribed medications.
2. Marijuana: With the legalization of marijuana in many states, older adults may view it as a safer option for managing pain, anxiety or sleep issues. However, marijuana use can have various negative effects on an aging body, including cognitive impairment and increased fall risks.
3. Opioids: Prescription opioids like oxycodone or morphine are commonly prescribed to manage pain from arthritis, surgeries or chronic illnesses. Unfortunately, aging adults may develop a dependency on these medications, leading to misuse and addiction.
4. Cocaine: Though less common than other substances, cocaine use is still a concern among some older individuals. Its stimulating effects can place additional strain on aging cardiovascular systems, increasing the risk of heart attacks and strokes.
5. Benzodiazepines: These medications, such as Valium and Xanax, are often prescribed to treat anxiety and insomnia. Older adults are at a higher risk of becoming dependent on benzodiazepines and prolonged use can lead to issues such as memo-
As the body ages, metabolism slows down and organs such as the liver and kidneys become less efficient at processing substances. This means that drugs and alcohol stay in the system longer and have a stronger impact on the body. Older adults who consume the same amount of alcohol or drugs as they did when they were younger may experience more severe side effects, including confusion, dizziness and impaired motor skills. Additionally, long-term substance use can exacerbate chronic illnesses, increase the risk of falls and fractures and negatively impact mental health.
One major challenge in addressing substance use disorders among older adults is that these issues often go unrecognized. There are several reasons for this:
1. Ageism and stereotypes: Many people assume that substance use disorders primarily affect younger individuals, so they may not consider the possibility that an older person is struggling with addiction.
2. Similar symptoms: The symptoms of substance use disorders can mimic other conditions common in older adults, such as dementia, depression and side effects from medication. For example, cognitive decline, confusion and memory loss could be attributed to age rather than substance use.
3. Reluctance to seek help: Older adults may be less likely to seek help for substance use issues due to feelings of shame, stigma or denial. They may not realize that they have a problem or they may feel that it is too late to change.
While substance use disorders in the aging are treatable, there are several barriers to treatment:
• Limited access to age-appropriate treatment: Many addiction treatment programs are designed for younger people and may not address the specific needs and challenges faced by older adults. Elderly individuals may benefit more from tailored programs that focus on managing chronic pain,
Despite these challenges, it’s essential to remember that substance use disorders among older people are treatable. Early recognition is key. Family members, caregivers and healthcare providers should remain vigilant for signs of substance misuse, such as changes in mood, withdrawal from social activities, unexplained injuries and fluctuations in weight or appetite.
Treatment approaches for older adults should consider their unique needs. For instance, therapies may focus on managing chronic pain in safer ways, such as through physical therapy, mindfulness practices or non-addictive medications. Counseling and support groups specifically for older adults can also provide emotional support and help individuals feel understood and less alone in their struggles.
Substance use disorders among people over 60 are a growing issue that requires attention and compassionate care. The aging baby boomer population, coupled with changes in life circumstances and health, has led to an increase in substance use among older adults. Recognizing and addressing these disorders can help these individuals lead healthier, more fulfilling lives. While there are challenges in treating substance use disorders in this population, it’s never too late to seek help. With the right support and understanding, older adults can overcome addiction and truly “get a new lease on life.”

Physician Mark Winsberg is a board-certified addiction medicine specialist and former medical director of Rochester Regional Health's chemical dependency services. He is in solo practice in the Rochester area offering completely private, confidential treatment for people just starting to admit they have substance use issues. Contact him by phone 585-565-5220, email at drmark@ winsbergmd.com or through his website: winsbergmd.com. Winsberg is happy to speak to local organizations about any topics related to substance use disorders.
By Deborah Jeanne Sergeant
Information released this summer by FAIR Health indicates that in a population of people 65-plus who have commercial health insurance, diagnoses of sexually transmitted diseases increased by almost 24% during the COVID-19 pandemic compared with just 5% in the population overall.
Those between 55 and 64 represented the next largest group with a 16% jump. These statistics mirror those published by the Centers for Disease Control and Prevention for those 55 and older between 2012 and 2022.
So why are the numbers going up? Part of the reason may be statistical.
Matt Hanggi, nurse and communicable disease coordinator at Ontario County Public Health and working in emergency medicine at Thompson Health, said that more people aged 60-plus have some sort of health coverage and have other health issues going on, so they’re more likely to seek healthcare and thereby get diagnosed with an STI.
“They’re getting tested more and that’s how they’re getting diagnosed more,” Hanggi said. “The rate of uri-

nary tract infections in older adults are through the roof. Almost all are cultured out. They take the urine and culture it out and would discover some STIs that way.”
The spike in STIs during the latter part of the pandemic may also reflect more people seeking routine healthcare after the quarantine period, when non-urgent healthcare needs were paused.
“This all incubated and once people returned to their normal medical care, it exploded,” Hanggi said.
Jenna Weintraub, sex educator for Rochester Center for Sexual Wellness, guessed longevity may have something to do with why more older adults are getting STIs.
“People are living longer and staying healthier until older ages,” she said. “Many can maintain an active sex life for many more years.”
During the pandemic, many people made a major life shift such as separation and divorce, closing a small business or retiring. Reevaluating one’s life trajectory can cause changes in behavior and not all of those are good.
Better attention to healthcare has caused more people to maintain bet-



ter health later in life. In addition to enjoying a vigorous retirement, older adults continue with sexual activity well into their later years because of modern medicine. Men do not have to struggle with erections, thanks to erectile dysfunction medication and women no longer struggle with waning libido or vaginal dryness because of hormone replacement. This all means that older adults are enjoying a longer sexual life than in previous years.
During the retirement years, with more time on their hands and “gray divorce” increasing, more older adults are entering sexual relationships with multiple partners: a huge risk factor for the spread of STIs.
More than ever, older adults access dating apps, which allows them to cross paths with more random encounters with veritable strangers instead of meeting a friend-of-afriend for lunch and developing a relationship naturally from serendipitous interactions. Weintraub also indicated that living in intentional communities geared towards older adults increases their dating pool, as does the tendency for women to outlive their husbands.


Not only do older adults have more opportunity for exposure to STIs, but those factors directly related to their age also increase their risk.
“Since menopause causes the vagina skin to become thinner, less acidic and cervical mucous diminishes, this makes the skin more prone to infection,” Weintraub said.
A generational gap in STI knowledge also contributes. No longer fearing pregnancy, older adults may erroneously feel freer to engage in promiscuous sex. However, “these folks are less educated about STIs and safer sex, most of whom were sexually active before the AIDS epidemic,” Weintraub said.
She cited a National Institutes of Health study that indicated people ages 65-94 “had many misconceptions about STIs. Using protection like condoms and dental dams is important and providing sex education on safer sex and sexual health is important for these populations.”
Weintraub encourages more medical providers to screen their patients for STIs and start conversations about sexual health.



Anew, large study from France underscores the link between adult hearing loss and dementia.
"Given the major burden of cognitive decline and the absence of curative treatment, identifying modifiable risk factors is of importance," a team led by physican Baptiste Grenier, of the Université Paris Cité, wrote Oct. 1 in the journal JAMA Network Open. They said thinking skills may decline not only because people with hearing loss become socially isolated but also because they go for a long periods without auditory input.
In addition, hearing loss is linked to loss of volume in critical areas of the brain.
Even so, researchers said hearing aids for patients with disabling hearing loss should be prescribed based on potential benefit to quality of life and not to ease cognitive decline. For that, they wrote, more research is needed.
For the study, Grenier's team analyzed data from more than 62,000
people in France (average age 57) recruited between January 2012 and December 2020. Participants aged 45 and older underwent cognitive testing at the outset.
In all, 49% had normal hearing; 38% had mild hearing loss; and 10% had disabling hearing loss but did not use a hearing aid; 3% wore a hearing aid.
Participants took both hearing and cognitive tests.
In all, 27% of participants with mild hearing loss and 37% with disabling hearing loss had cognitive scores indicative of impairment. That compared to 16% of participants whose hearing was normal.
Researchers found no meaningful difference in the risk of cognitive impairment between individuals with disabling hearing loss who wore a hearing aid and those who did not.
A related analysis suggested that hearing aids may reduce the risk of cognitive impairment in people who have disabling hearing loss as well as depression.

November 6, 10-11:30 am Wills – An Overview
November 9, 9 am-noon Pre-retirement Saturday
November 11, 10-11:30 am Navigating Hospital, Rehab & Home Transitions
November 12, 10-11:30 am Managing Income to Minimize Taxes
Learn more and register at lifespanrochester.org or call 585-244-8400, ext. 201
November 15, 1-4:30 pm Technology & Supportive Services Aging-in-Place Fair
November 19, 2-3 pm Transportation Options
November 22, 1:30-3 pm Supportive Housing Options
November 22, 2-3:30 pm
A Geriatrician’s Approach to the Pharmacy Aisle Lifespan offers these

experience and made it great.”
That’s just one of the comments we’ve received from a patient who has had postsurgical rehab at St. Ann’s. We’re proud to offer first-class care that gets you healthy and home as soon as possible. Preplan your stay. Call (585)697-6565 or visit
By Deborah Jeanne Sergeant
No one alive today has died before. And most people have not experienced sitting with a loved one whose death is anticipated. Even those who have could still use support.
That’s where death doulas come in.
Also known as end-of-life doulas, these professionals make dying easier on the patient and family by offering a comforting, non-medical presence through practical, emotional and spiritual guidance during death.
Lauren Sample, an end-of-life doula, operates In Due Time in Rochester.
“I was not someone who you’d expect to be in end-of-life work and would’ve done anything to keep death as far away as possible,” Sample said.
That all began to change when she birthed a daughter not expected to live. She defied the odds and survived for 15 years. Her close calls during this time helped Sample become more at ease with death. She also learned about end-of-life work and became interested in becoming
a death doula. After a few years, Sample received training and became certified in 2019.
In addition to support, death doulas provide education about what’s happening and what to expect as death draws closer and what to expect after. Most help families know what to do immediately after, like final affairs.
“We are available to sit at the bedside as death draws nigh to give them a break or sit with the family as things change. We can help them learn comfort measures,” Sample said. “We might help decorate the space. We might talk with the dying person ahead about what they’d like the end of their life to look like and what they’d like around them.”
That might include who the person wants or doesn’t want near the bed.
The end-of-life doula may also serve as a liaison between the intown and out-of-town family members and suggest ways that they can offer support from afar.
The services are not covered by insurance as they’re not medical.
However, some hospitals and hospices have end-of-life doulas as part of their staff.
Sample charges a sliding scale fee to keep it affordable for people with lower income. End-of-life doulas typically charge between $50 and $100 per hour.
Karen Bennett, who offers endof-life support in Rochester as The Dying Well Doula, stumbled upon the concept while visiting Nepal 20 years ago. She began volunteering at a hospice and those experiences taught her how to serve as a caregiver to her husband when he was dying in 2021.
“There’s a calling for it,” Bennett said.
There’s also big demand, as the aging baby boomers don’t often live near their adult children. Even if they did, most households are dual income and cannot take off months from work with unpaid leave.
and frightening time.”
Some also run errands and perform household chores, help with planning final arrangements and suggest a legacy project to create a comforting memory.
Bennett suggests enlisting an end-of-life doula once the patient is in hospice care.

“We work alongside the hospice team assigned to the patient,” Bennett said. “Our services are mainly there to comfort and support the dying and family members around them. It can be very calming and supportive in what can be a chaotic
“It’s just as important as will and power of attorney,” she said. “It’s crucial for people to know who you want around you and where you want to be so everyone’s on board with it.”
Many people believe that once a patient is on hospice care, they receive 24/7 care. However, Bennett said that most of the care falls to family members with only an aide or visiting nurse coming for a couple of hours daily. Death doulas can offer more relief and support.
“I think it’s an important role that everyone can benefit from,” Bennett said. “It’s such an emotional time for a lot of people. Having that calming, supportive presence in the home can relieve so much stress and chaos.”


By Jim Miller
Dear Savvy Senior,
I would like to arrange a simple cremation that doesn’t cost me, or my family, a lot of money. Can you offer any tips that can help me with this?
Still Kicking
Dear Kicking,
If you’re looking for a simple and affordable way to go, cremation is an excellent choice, and one that’s become exceedingly popular in the United States. About 60 percent of Americans are now choosing cremation over a traditional burial, versus only around 20 percent in the mid1990s.
Why the big shift? Price is a key reason. A basic cremation can cost as little as $700 to $1,200, depending on your location and provider, versus $7,500 or more for a traditional funeral and cemetery burial. Geography is another factor, as many families are spread across the country, making future gravesite visits less common.
Here are a few tips to help you arrange your cremation and ensure you get a good deal.
You can arrange a cremation through a funeral home or a cremation-only business, but it’s wise to shop around because prices vary widely. It’s not unusual for one funeral home to charge $1,000, while another charges $4,000 or more for the same service.
Call five or six funeral homes or cremation-only businesses in your area and ask them how much they charge for a “direct cremation,” which is the most affordable option there is. With direct cremation, there’s no embalming, viewing or memorial service. It only includes the essentials: transportation of the body; required paperwork such as death certificates; the cremation itself; and return of the ashes to the family, usually within a week.
If you want a viewing, memorial service or anything beyond what a direct cremation provides, ask the funeral home for an itemized price list so you know exactly what you’re paying for. All funeral providers are required by law to provide this.
To locate nearby funeral homes, Google “cremation” or “funeral” followed by your city and state. You can also shop and compare prices from funeral homes in your area at Funeralocity.com.
The urn is another item that can drive up your cremation costs. Funeral home urns usually cost around
$100 to $350, but you aren’t required to get one.
After cremation, your family will receive your ashes in a thick plastic bag inside a cardboard box. This is all they need if you intend to have your ashes scattered, but if your family wants something to display, Amazon.com and Walmart.com both sell a wide variety of urns for under $50.

If you’re an environmentally conscious person, there’s also a green cremation option you should know about called “alkaline hydrolysis” that chemically dissolve the body. This is a gentler, more eco-friendly process than traditional cremation, which uses combustion. It’s legal in more than 20 states, and costs around $2,000 to $3,500. Alkaline hydrolysis is not currently legal in New York state.
If you’re interested in a free final farewell, you may want to consider donating your body to a university medical facility.
After using your body for medical research or surgical practice they will cremate your remains for free, and either bury or scatter your ashes in a local cemetery or return them to your family, usually within a year.
In Upstate New York, the departments of anatomy of SUNY Upstate Medical Center and University of Rochester School of Medicine are some of the places that accept body donations. To find other medical schools that offer the service, the University of Florida offers an online directory at Anatbd.acb.med.ufl. edu/usprograms.
Whatever arrangements you end up making, make sure you tell your family your wishes so they will know what to do and who to call after your death. Also, if you have a written agreement with any funeral or cremation provider, give them a copy to let them know if you’ve prepaid or not.

Send your senior questions to: Savvy Senior, P.O. Box 5443, Norman, OK 73070, or visit SavvySenior. org. Jim Miller is a contributor to the NBC Today show and author of “The Savvy Senior” book.

Our family-owned business has been providing excellent service to the community for over 30 years.

In 2025, some health insurance options have significant changes. You change annually, too! Investigate best-fit health insurance through the Webster Chamber’s licensed, certified, and experienced health insurance enrollment staff. They work with multiple major carriers, including the New York State Marketplace and Child Health Plus.


By Cassie Curry
The onset of colder weather means fewer opportunities for outdoor activity, especially if you're an older adult. It doesn't mean, however, that your physical fitness has to hibernate. There are simple exercises you can do in the warmth and safety of “the great indoors” to maintain good physical health over the winter.
Walking is always nicest on the sidewalk on a warm summer day. But you can get the same benefits (minus the sunshine) from walking indoors. Go back and forth down the hallway of your home and, if you're able, up and down the stairs. It's a low-impact way to keep your muscles strong, improve balance and support cardiovascular health.
At St. Ann's Community at Cherry Ridge, I suggest this to our elders: While you're sitting watching TV, use the commercial breaks to get in a little exercise. March in place or do stand-up sit-downs during the commercials, then rest when your show returns. It's good for your body and a nice diversion from those pesky ads!
Here's another activity that can be done while sitting: Pick up your feet, point your toes down like a ballerina, then flex your foot upward and repeat. You can also rotate your ankles in a circular motion. These movements can improve joint mobility, alleviate stiffness and help with circulation and blood flow back to the heart. And they can be done anywhere, from the living room to the waiting room to the passenger seat of the car.
If the weather keeps you from hitting the weight room, use soup cans or bottles of water in place of dumbbells. Hold them at shoulder height then raise them over your head and back down. Or try curls: hold the weights at your sides and then, bending your elbows, raise them up to your chest and back down. A weight workout is good for the muscles and joints and builds bone density, which can reduce the risk of breaks or fractures.
Even time in the shower can be used for fitness. With the warm water relaxing your muscles, try these gentle movements of the head, neck, and shoulders, one at a time, repeating each several times:
• Roll your shoulders forward and backward.
• Bring your right ear toward your right shoulder, then do the same to the left.
• Bring your chin down to your chest then back up.
• Gently roll your neck in a circle.
These not only feel good but the stretching helps alleviate stiffness and increases flexibility.
Adding music to your daily routine is also a good way to stimulate movement, increasing circulation and stability. Turn up the tunes while you're cooking or cleaning and do what comes naturally: tap your feet, sway your arms, gently twist your hips and torso. For an added cardio benefit, sing along with your favorites! Good for the body, good for the spirit.
All of the above are simple ways to maintain flexibility, balance, coordination and agility. They keep us moving so we can do more of the things we love. Moving also increases blood flow, which stimulates the brain. And simply thinking about which movement you're going to do next means you're working your brain as well as your muscles.
Remember to take periodic breaks and don't overdo.
Listen to your body; if you're in discomfort or feeling a strain, stop what you're doing.
As with any home exercise routine, check with your health-care provider and see what activities and levels of exertion are right for you.
It may have been years or even decades since you thought about how much you earned at your first job. Did you know that you can find out how much you made that first year? Or any year you worked and paid Social Security taxes?
Your earnings history is a record of your progress toward your future Social Security benefits. We track your earnings so we can pay you the benefits you’ve earned over your lifetime.
That is why it’s so important for you to review your earnings record.
Even though it’s your employer’s responsibility to provide accurate earnings information, you should review your earnings history and let us know if there are any errors or omissions. Otherwise, your future Social Security benefits could be lower than you should receive. It’s important to identify and report errors as soon as possible. If too much time passes, it could be hard for you to get older tax documents. Also, some employers may no longer exist or be able to provide past payroll information.
The best way to verify your earnings record is to visit www.ssa.gov/ myaccount and create or sign in to your personal My Social Security account. You should review your earnings carefully every year and confirm them using your own records, such as W-2 forms and tax returns. Keep in mind that earnings from this year and last year may not be listed yet. When you have a personal My Social Security account, we send you an email once a year, three months before your birthday, to remind you to check your earnings and to get future benefit estimates.
If your Social Security earnings record is incorrect and does not
Q.: I didn’t enroll in Medicare Part B back when my Part A started a few years ago. Can I enroll now?
match your personal records, you may be able to submit a correction request online using your personal My Social Security at www.ssa.gov/ myaccount. If that feature is available in your personal My Social Security account, you can use the online process to correct missing earnings, inaccurate earnings from a valid employer, or earnings from an employer you did not work for. You’ll need to provide:
• Your address if we need to contact you about your request.
• Details about your correct earnings and employer.
• Evidence or proof of correct earnings, if available.
You can electronically upload your proof (W-2, W-2C, tax return, wage stub, pay slip, etc.) in a JPG or PDF format. After you successfully submit your evidence, you can print or save a receipt.
Earnings corrections cannot be processed online if they are for:
• The current or prior year, which may not be recorded yet.
• Self-employment.
• Railroad Board.
• Certain years before 1978. Also, you cannot submit an earnings correction online if you:
• Receive Social Security benefits, Supplemental Security Income (SSI), or Medicare.
• Have applied for Social Security benefits or SSI.
If you cannot correct your earnings online, call us at 1-800-772-1213 (TTY 1-800-325-0778), Monday to Friday, 8:00 a.m. to 7:00 p.m. to request a correction.
Start a conversation today. Ask a family member or friend about their first job and let them know they can find out what they earned that year!
Cassie Curry is senior wellness coordinator at St. Ann's Community at Cherry Ridge. She can be reached at ccurry@ mystanns.com.
A.: It depends. The general enrollment period for Medicare Part B (medical insurance) runs from Jan. 1 through March 31. Keep in mind that although there is no monthly premium for Medicare Part A, there will be a premium for your Medicare Part B. In most cases, that premium goes up each 12-month period you were eligible for it and elected not to enroll. If you are covered by a group health plan based on your employment or the employment of a spouse, you may be eligible for a special enrollment period. Special enrollment periods may be processed at any point during the year but require proof
of coverage. To find out more about Medicare, visit www.medicare.gov or www.ssa.gov/medicare/sign-up.
Q.: My child, who gets Social Security, will be attending his last year of high school in the fall. He turns 18 in a few months. Do I need to fill out a form for his benefits to continue?
A.: Yes. You should receive a form, SSA-1372-BK, in the mail about three months before your son’s birthday. Your son needs to complete the form and take it to his school’s office for certification. Then, you need to return page 2 and the certified page 3 back to Social Security for processing. If you can’t find the form we mailed to you, you can find it online at: www.ssa.gov/forms/ssa-1372.pdf.
By Deborah Jeanne Sergeant
f your mouth feels unusually dry, it’s more than just a bother and it’s not just another unpleasant sign of growing older. It could indicate a health problem that’s potentially serious.
Dentist David K. Skeels, with University of Rochester Medical Center explained that the condition happens when the body’s salivary glands make too little saliva.

“You may have a sore throat, trouble swallowing, tasting, or even speaking,” Skeels said. “Dry mouth is not a normal part of aging.”
The symptom of dry mouth could indicate diabetes, Sjogren disease or Parkinson disease, among other health conditions.
Medication could also be to blame for dry mouth, as those indicated for depression, antihistamines, decongestants, pain killers, diuretics

and high blood pressure all may contribute to that cotton mouth feeling.
Typically, dry mouth associated with a passing illness or seasonal allergies resolves with the other symptoms such as a scratchy throat and itchy, watery eyes.
Treating dry mouth is important because “without enough saliva to rinse away food pieces from your teeth, you can develop tooth decay,” Skeels said.
inadvisable to drink beverages containing sugar or acid, such as soda, juice, sweet tea or lemonade as these are harmful to tooth enamel. Hydrating with water is the best idea.
Patients should also reduce their intake of alcohol, caffeine and tobacco, all of which can dry the mouth.
have difficulty chewing, swallowing and speaking, which severely hampers quality of life,” Skeels said.
Depending upon the reason for dry mouth, a visit to the primary care provider, rheumatologist or dental professional can help.
“Your dentist can prescribe a medicine to help your salivary glands work correctly,” he said.


“Your dentist or healthcare provider also may suggest using artificial saliva and oral rinses,” Skeels said. “These are available at most pharmacies. Some people find it helpful to suck on sugar-free hard candy or gum to stimulate the flow of saliva.”
Many people who have a different autoimmune disease such as rheumatoid arthritis or lupus also experience Sjögren’s and some of the symptoms overlap among the autoimmune diseases. The glands in the patient’s eyes and mouth are affected so that they do not produce enough tears and saliva. The most common age to develop Sjögren’s is older than 40 and as with other autoimmune diseases; women are affected more often than men.

Lifestyle interventions may also play a role in improving dry mouth. Skeels advises patients with dry mouth to drink plenty of water. It’s

An autoimmune disease, Sjögren’s syndrome can cause dry mouth and eyes, along with vaginal dryness, dry skin, dry cough and joint pain and stiffness.
“Sjögren’s patients experience dry mouth due to a lack of saliva and
Typically, doctors address the symptoms of Sjögren’s to bring patients relief. It can also help to monitor and address any other autoimmune diseases present.







St. Ann’s of Greater Rochester

Incorporated (SAGRI) recently announced the appointment of Cheryl A. Ryan as chairwoman of the St. Ann’s board of directors. The board is composed of dedicated community leaders committed to St. Ann’s mission of promoting the highest level of independence and the physical and spiritual well-being of older adults.
Ryan currently serves as chief human resources officer at Highland Hospital and brings over 30 years of leadership experience to her role.
She holds a bachelor’s degree from Cornell University and an MBA from St. John Fisher University. Before becoming chairwoman of the St. Ann’s board, she served as the head of its human resources committee.
“This position is meaningful to me because, as someone who was born and raised here, I am honored to be a part of an organization that has such a rich history of serving older adults in the greater Rochester area for over 150 years,” she said.
Michael E. McRae, president and CEO of St. Ann’s, said, “I’m sincerely grateful for Cheryl’s dedication as our new board chair. With her leadership, along with the support of our entire board of directors, we will continue to grow and enhance St. Ann’s services to better serve our community.”
Pluta Cancer Foundation names new leader
Pluta Cancer Foundation recently

appointed Dawn Stever as president & CEO. Stever brings two decades of progressive fundraising and healthcare philanthropy experience — spanning the full continuum of development strategies. Most recently, she served as vice president of operations for Rochester Regional Health Foundations. Stever has also worked in higher education with leadership positions at Hartwick College and Rensselaer Polytechnic Institute in addition to serving as a senior consultant at Ruffalo Noel Levitz.
“We are thrilled to have Dawn join our team as the president & CEO of Pluta Cancer Foundation,” said board chairman Ron Pluta. “Her tremendous track record of executive philanthropic leadership and health-system acumen position Dawn as the ideal choice to lead our foundation to the next level while
honoring our rich history. Dawn epitomizes our patient and employee-centric culture.”
Stever will lead strategic, philanthropic, and operational components of the foundation, whose mission is to support patients through integrative oncology and financial support.
“Pluta is known in the community for the caring environment and excellence in comprehensive breast care—and the foundation is a vital component to the overall experience for patients and families. It is such an honor to join this dedicated team,” said Stever.
Stever holds a master’s degree in business administration from Binghamton University, a bachelor’s degree from Elmira College, and is a certified fund raising executive (CFRE).
St. John’s Home announced the

Dan Morphet appointment of Dan Morphet as vice president of skilled services. Morphet brings 33 years of experience in the long-term care industry to his new role, having led operations at some of New York state’s largest skilled care facilities.
As vice president of skilled services, Morphet will oversee St. John’s skilled nursing operations, including Penfield’s Green House Homes and the main campus, which is home to 300 residents.
He will also manage rehabilitation services and will be responsible for developing a non-medical model of long-term care.
Morphet will be instrumental in the expansion of St. John’s services, such as the introduction of a chronic dialysis unit and pediatric skilled care, as part of the recently announced collaboration with University of Rochester Medical Center.
“Under Dan’s leadership, St. John’s will continue to advance its mission and evolve our services to provide the highest quality of care for our residents and their families,” said president and CEO Charlie Runyon.
Morphet joins St. John’s from Park Ridge Living Center in Rochester, where he served as the administrator of the 120-resident facility.
He previously held the position of senior administrator at Loretto Health and Rehabilitation in Syracuse, managing four facilities with a total of 1,846 residents and an annual operating budget of $180 million.
Morphet holds a Bachelor of Science in business administration and healthcare administration from Alfred University.
Excellus has new community investments and partnerships director
Excellus BlueCross BlueShield

Matthew Wagstaff
recently named Matthew Wagstaff as community investments and partnerships director for the company's Rochester region. His responsibilities in this role include overseeing strategic investments, advancing health equity to improve health outcomes and drive strategy-aligned employee engagement with community-based organizations through board involvement and other volunteer opportunities.
Wagstaff has been with the Excellus for more than 17 years, serving most recently as a corporate development and strategy director. Other leadership roles include corporate strategy and administration director, marketing and competitive intelligence manager, and retail markets new sales channels manager.
Wagstaff is active in the Rochester community, serving as a member of the board of directors for Junior Achievement Central Upstate NY, Leadership Rochester and Brighton Junior Bruins Youth Football and Cheer. He and his family reside in Rochester.
KyShara Penns is the new

KyShara Penns director of obstetrical nursing for F.F. Thompson Hospital in Canandaigua. At the hospital, which is part of UR Medicine Thompson Health, Penns now oversees the birthing center, which has perinatal advanced certification from The Joint Commission and is designated by Excellus BlueCross BlueShield as a Blue Distinction “Center+ for Maternity Care.” Nearly 750 babies were delivered there in 2023.
A graduate of Monroe Community College who obtained her Bachelor of Science in nursing at Roberts Wesleyan University, Penns is pursuing a Master of Science in leadership of healthcare systems at the University of Rochester School of Nursing, where she is expected to graduate in May 2025.
Penns is a former adjunct instructor at the St. John Fisher University School of Nursing who since 2021 worked at Golisano Children’s Hospital, first as a registered nurse and most recently as an assistant nurse manager.
Prior to Golisano, she worked as a registered nurse at Highland hospital, for two years on a medical surgical unit followed by more than seven in the hospital’s family maternity center.
Jewish Home has been ranked as the No. 1 nursing home in New York state on Newsweek’s prestigious America’s Best Nursing Homes list for 2025. This is the fourth consecutive year the organization has made this list.
Newsweek partners with global data research firm, Statista, to assess and rank the top nursing homes in each state based on four pillars: performance data, recommendations of medical professionals, accreditations and resident satisfaction.
This year's list recognizes the nation’s top 1,050 nursing homes across the 25 states with the highest number of facilities, according to data from the Centers for Medicare & Medicaid Services, and is intended to assist older adults and their families when considering long-term care options.
“It’s a tremendous honor to be recognized by Newsweek for the fourth time,” says Michele Schirano, senior vice president and administrator at Jewish Home. “Making the list of America’s Best Nursing Homes year after year only reinforces the high quality of life we provide at the Jewish Home and across our entire continuum of care—but being ranked No. 1 in New York state for 2025 is truly the icing on the cake! Each and every day, we have the privilege of providing the best and most compassionate care to the people we serve. To receive this ranking is a testament to all the work our employees do to keep our residents, patients, families, and guests happy and healthy. We couldn’t achieve No. 1 without their efforts.”
Pediatrician Katelyn Nevin

Katelyn Nevin recently joined the pediatrics department at UR Medicine Thompson Health’s Canandaigua Medical Group, an affiliate of F.F. Thompson Hospital. A native of Caledonia in Livingston County who now lives in Rochester, Nevin obtained her Bachelor of Science degree in molecular genetics from the University of Rochester and her Doctor of Medicine from Loyola University’s Stritch School of Medicine in Chicago. She completed her residency in pediatrics at the University of Rochester Medical Center’s Golisano Children’s Hospital.
Nevin is a member of the American Academy of Pediatrics and the American Medical Association.






MISS THE
Holidays — Shortage of nurses, doctors … Santas?
• Fitness— Traveling personal trainer Anja Jabs-Devins is all about keeping clients and students moving
• Entrepreneurship — Penfield inventor develops patented skincare applicator
Photography—Scott’s Photo by Rowe on East Ave. has been in operation since early 1980s
Cover — Curiosity and a desire to help others have fueled the career of Dr. Lisa Harris of Excellus BCBS
to 55Plus, the
• Pets —Things you need to consider before adopting
•Jobs — Forced retirement: What should you do next?
• Vintage — Chubby vintage nana from Albion is a social media sensation
• Money — Smart money moves for 2025
• New Year —Get organized in 2025. We show how to do it ...and so much more!
