Playing with a dog for just 15 minutes can significantly reduce a person's stress, a new study reports.
Stressed students who interacted with a friendly dog reported less stress, had a reduced heart rate and had lower levels of the stress hormone cortisol in their saliva, researchers said in the journal PLOS One.
The experience also appears to be beneficial for dogs, researchers added. Fecal tests showed that canine cortisol levels were lower a week after hanging with a human.
“Even brief interactions with dogs can significantly reduce stress levels among university undergraduate students,” concluded the research team led by senior investigator Jaruwan Khonmee with Chiang Mai
University in Thailand.
For the study, researchers recruited six friendly dogs 3 to 6 years old to interact with college students. They included five chihuahuas raised by veterinarians and a Shetland sheepdog raised by a psychologist.
None of the dogs were certified for therapy work, researchers noted. This was the first time they'd participated in any sort of canine-assisted intervention, and they participated without the presence of their owner.
In the main library of Chaing Mai University, 122 students completed a stress assessment questionnaire, had their blood pressure and pulse taken, and provided a saliva sample for cortisol testing.
They then were given 15 minutes to play with a dog after being told the pooch's name, personality traits



and preferred interactions.
The students could do whatever they wanted — look at the dog, pet it, give treats, hug it, play with it.
Afterward, they went through another round of tests to assess their stress levels.
The dogs provided fecal and saliva samples before and after their time with students, to see whether the play benefited them as well.
Students showed self-reported and physical improvements in stress following their 15 minutes with a dog, results show.
“Compared to immediately before, students' self-reported stress levels decreased by 33.5% after interacting with the dog,” researchers reported.
The students also had improvements in their pulse rate and cortisol
levels, researchers noted.
There were no changes in salivary cortisol in the dogs on the day of play, but their fecal cortisol levels were lower a week after they spent time with the students, researchers said.
“Overall, these findings contribute to our understanding of the beneficial impact of human-dog interactions on human stress levels and highlight the importance of addressing stress in both humans and animals during targeted interventions,” researchers concluded.
“In contexts where certified dogs and handlers are not readily available, non certified dogs could still offer mental health benefits,” the team added.




By Jennifer Faringer
Alcohol Awareness Month in April is an opportunity to consider the risks associated with excessive alcohol use.
According to the Dietary Guidelines for Americans, 202025, individuals should limit their alcohol intake to no more than one drink a day for women and no more than two drinks a day for men.
Women who are pregnant are recommended to abstain from alcohol throughout the duration of their pregnancy to ensure the healthiest outcome for their child. Excessive alcohol use can result in injuries and violence and is responsible for a multitude of health risks, including an increase in the risk of cancer.
Consider these additional alarming statistics for New York state:
• More than 8,050 New Yorkers die each year due to excessive alcohol use.
• Nearly 1 in 5 adults reported binge drinking in 2024.
• Among the two million adults who reported binge drinking, 25% binged at least four times a month and consume at least seven drinks per occasion.
• Excessive drinking equates to roughly $843 in preventable costs per taxpayer.
Despite its proven dangers, the perception of risks associated with alcohol use remains low and many perceive it as less harmful than other drugs. When asked which drugs they see as a serious health problem, 90% of adults believed that prescription opioid misuse was a serious health problem; 88% heroin; 83% vaping; 40% cannabis use; while comparatively 77% of adults said alcohol use.
Among teens, 13.9% of high school students in New York state reported having their first drink before age 13 compared to 15% for the United States overall.
Research tells us that those who start drinking before age 15 are 3.5 times more likely to report having an alcohol use disorder than those who delay first use until 21 or later. Use of alcohol or other drugs before that time interferes with the normal development of the brain which is not fully developed until the age of 25. Each year, more than 100 New Yorkers under 21 die due to alcohol use from motor vehicle crashes, alcohol poisoning, suicides and homicides.
To learn more about the risks and perceptions around alcohol and other drug misuse, visit our website at www.ncadd-ra.org. To attend our community workshops or request a presentation, email me at jfaringer@depaul.org.

Jennifer Faringis the director of DePaul’s National Council on Alcoholism & Drug Dependence Rochester Area. She can be reaches at jfaringer@depaul.org.

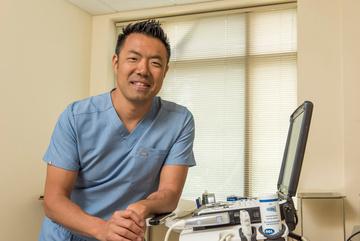
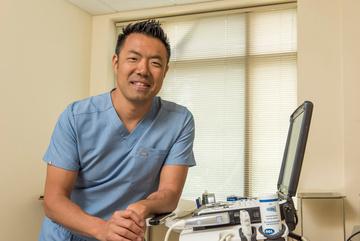
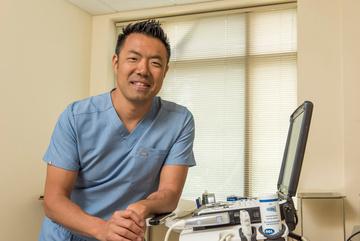
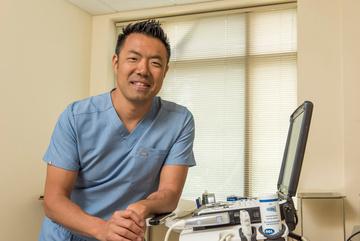
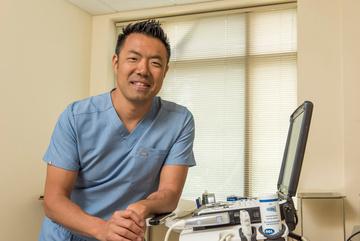
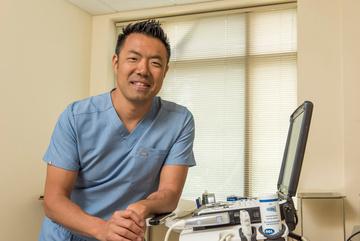
By Chris Motola
Physician reflects on accomplishments as head of Monroe County Medical Society: “I think medical societies are needed even more in today’s society as a voice for patients and physicians”
Q: You’ve finished up your term as president of the Monroe Country Medical Society?
A: Yup, we transition on May 1.
Q: What would you describe as some of your key accomplishments from your tenure?
A: Of my term? I would say working on improving physician collegiality. Medicine today is so siloed and we’re all so busy. And we’ve kind of lost that place where we all communicate with each other socially. There used to be a doctors’ lounge which no one really uses anymore. So just trying to do more outreach.
Q: When you say doctors’ lounge, do you mean a room in a hospital or practice or more of a third space where physicians gathered after hours?
A: Most hospitals had a doctors’ lounge where you could finish your notes. This was years ago. There still is one, but no one really uses it anymore.
Q: Why is that?
A: I think a lot of it is what we’re expected to do in a day has increased so we don’t really have the time. We have to meet all these thresholds. See x amount of patients in day, perform x number of procedures. So we just don’t have the time anymore. When that happens everyone starts to get isolated, and that can contribute to physician burnout. So I’ve really made an effort to do some more out reach, get physicians to get together, whether it’s on a Zoom meeting or a social event just to help with that feeling of isolation and that loss of camaraderie.
Q: How do you work around that?
A: Being more present for people. Attending numerous meet ings and putting my face out there. Reaching out to different groups. We hosted several social events after hours so that people could meet outside of the hospital and outside of their office. We’ve continued to host educational events. And for the young physicians we’ve hosted some dinner meetings to talk about finances and how to transition from residency and medical school into private practice, and how to do that with some financial knowledge. So many of us leave our training with a large amount of financial debt.
Q: What’s lost with a decline in collegiality, both from the patient and practitioners’ perspectives?
A: I think the isolation contributes to burnout, which negatively affects the patient-physician relationship. It can affect the physician’s whole life. Many aren’t able to give patients the attention they need because they’re so burnt out. Having a collegial environment can help decrease burnout. I’ve talked to physicians who are struggling with burnout and after you sit and talk with them and lend an ear to support, it can lift a huge weight off of their shoulders. And by doing that, that’s going to improve patient care. For the patients, if the physicians are feeling better about themselves, they’re going to be better able to listen, which is a common patient complaint. If we’re not as burnt out we can listen more effectively and improve that physician-patient relationship that is so fractured.
Q: I’ve heard one of the big challenges for medical societies right now is a decline in the number of the private practices that largely support them. How can you make them work at a time of increasing group and hospital-based practices?
A: I haven’t figured that one out. I grew up in an era where more physicians were employed in private practice versus hospital-employed. One of our challenges right now is how do we reach the employed

physicians and show that we do have value, because they tend to think the hospital is covering all their needs. So we’re working with Causewave Community Partners to determine what we really need to focus on to move the medical society forward. I also think we need to do a better job with all physicians in terms of communicating what the medical society actually does, because a lot of people aren’t aware of all the advocacy we do for both patients and physicians. And I think that lack of communication contributes to people not understanding the value of the medical society.
Q: What’s your elevator pitch for the Monroe County Medical Society?
A: I think medical societies are needed even more in today’s society as a voice for patients and physicians. So much of our day and medicine in general is centered around insurance companies, the payers, and big hospital systems. And I think what medical societies can do is truly advocate for that patient-physician relationship that is so important for both sides. And I think that’s important for putting the passion back in medicine, the reason why so many of us went into medicine. Some of that’s going to involve education as the payers change the way they reimburse. Some of that is just offering support to both private practice physicians and hospital-employed physicians to deal with the burnout. We still have significant burnout even though it’s decreased since COVID. Bringing passion and caring back into the profession of medicine, the medical society is critically poised to do that.
Q: What’s next?
A: I’m retired from hospital practice but still have all my credentials. I do a lot of volunteer work. I’m medical director of the Webster Comfort Home, a hospice care center. I’m a health officer for my little village in Wayne County. I’m still active in medicine, I’m just not getting paid for it now.
Name: Janine L. Fogarty, M.D.
Position: Medical director of Webster Comfort Home; former president of Monroe County Medical Society
Hometown: Sidney, New York
Education: SUNY Upstate Medical University
Affiliations: Unity Hospital
Organizations: Monroe County Medical Society; Rochester Academy of Medicine; Medical Society of the State of New York; American Medical Association
Family: Husband (Jim), two children
Hobbies: Reading, boating, cooking, lounging by the water at Sodus Bay

olks facing surgery on a Friday may want to consider rescheduling if they can based on findings from a new study.
People who undergo surgery just before the weekend have a significantly increased risk of death and complications, researchers reported March 4 in JAMA Network Open.
This “weekend effect” occurred across 25 common procedures representing multiple surgical specialties, researchers said.
"Patients who underwent surgery immediately preceding the weekend had a significantly increased risk of complications, readmissions and mortality compared with those treated after the weekend," a team led by senior investigator, physician Raj Satkunasivam of Houston Methodist Hospital in Texas, concluded.
"It is important for health care systems to assess how this phenomenon may impact their practices to ensure that patients receive excellent care irrespective of the day," researchers added.
Hospitals and health care systems tend to operate with skeleton crews during the weekend, leading to concerns that patients are more likely to receive worse care on Saturday and Sunday, researchers said in background notes. This is commonly called the "weekend effect."
This weekend effect might also apply to people undergoing surgery immediately before the weekend, who will be in the hospital recuperating after their procedure, researchers explained.
To investigate this, researchers analyzed data on nearly 430,000 patients who underwent surgery in Ontario, Canada, between 2007 and 2019.
Results showed that people who underwent surgery prior to the weekend had a higher risk of death at 30 days (9% increase), 90 days (10%) and one year (12%) compared to surgeries performed after the weekend.
Pre-weekend surgical patients also fared worse on a composite score combining death, complications and need for rehospitalization, with a 5% increased risk at 30 days and one year following surgery.
In addition to reduced personnel, there are other reasons why hospitals might provide worse care close to the weekend, researchers said.
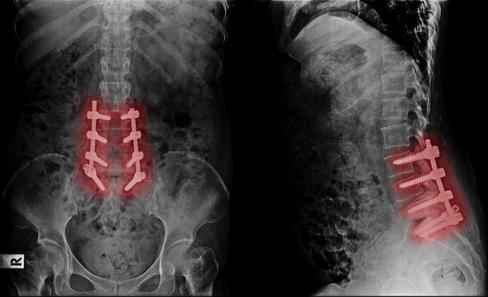
Sto Back a s

More junior surgeons with fewer years of experience operate on Friday compared with Monday, and doctors working the weekend have less access to more senior colleagues and specialists, researchers said.

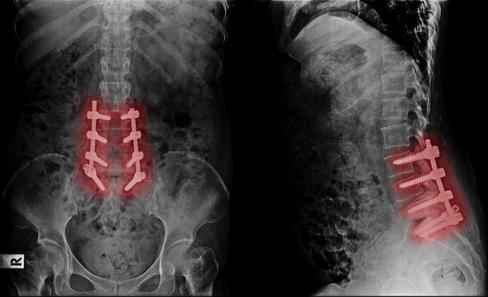
and lengthy recoveries.
Stop missing life’s greatest moments Stop planning life around pain
Regenerative Medicine is changing how back pain is solv
Stop missing life’s greatest moments Stop planning life around pain
Stop missing life’s greatest
Stop missing life’s greatest moments Stop planning life around pain
Back Pain should not mean fusion, screws, and lengthy recoveries Regenerative Medicine is changing how back pain
"Furthermore, weekend teams may be less familiar with the patients than the weekday team previously managing care," researchers noted.
Doctors also might have less access to tests and scans that could better help guide their treatment of patients, researchers added.
"Further study is needed to un derstand differences in care that may underpin these observations and en sure that patients receive high-qual ity care regardless of the day of the week," researchers concluded.

A monthly newspaper published by Local News, Inc. Distribution: 33,500 copies throughout more than 1,500 high-traffic locations.
In Good Health is published 12 times a year by Local News, Inc. © 2025 by Local News, Inc. All rights reserved. P.O. Box 525, Victor NY 14564. Phone: 585-421-8109 • Email: Editor@GVhealthnews.com
Editor & Publisher: Wagner Dotto • Writers: Deborah J. Sergeant, Chris Motola
George Chapman, Gwenn Voelcker, Anne Palumbo, Jim Miller, Jennifer Faringer Jolene Cleaver, Deborah Dittner, Colleen Holcomb
Advertising: Anne Westcott (585-421-8109) • Linda Covington (585-750-7051)
Layout & Design: Angel Campos–Toro • Office Secretary Mary Trapasso-Ayers
No material may be reproduced in whole or in part from this publication without the express written permission of the publisher. The information in this publication is intended to complement—not to take the place of—the recommendations of your health provider. Consult your physician before making major changes in your lifestyle or health care regimen.
Back Pain should not mean fusion, screws, and lengthy recoveries Regenerative Medicine is changing how back pain is solved.
Back Pain should not mean fusion, screws, and lengthy recoveries. Regenerative ng how back pain is solved

’s greatest moments. Stop around pain mean fusion, screws, e l d

Back Pain should not mean fusion, screws, d l th eries Regenerative ow back pain is solved. ur last stop ur life! V



last stop. ife!
your last stop







By George W. Chapman

Lacking an organized approach to healthcare delivery in the U.S., we experience the highest cost per capita in the world and rank 40th in overall mortality. Now, our once formidable "front line" of primary care providers is battle weary and in retreat.
Thanks to the lack of any planning at the national level, coupled with decades of chronic underinvestment, providers are leaving the front line of primary care, favoring better resources (pay) and lifestyle (time) available in non primary specialties.
Fewer primary care providers (be they MD, PA, NP) results in longer wait times for appointments across all specialties; decreased access, especially in rural areas, and higher costs due to increased use of specialists and overwhelmed emergency rooms.
Of all the things that need fixing in healthcare, price transparency is way down on the list. Way, way down. Trump recently signed an executive order reinforcing the already existing rules on price transparency that were promulgated in his first term. Briefly, the rule requires insurers to post what they agreed to pay hospitals for 300 or so procedures. Then, in turn, hospitals are to post their prices for those same procedures. For the 92% of us covered by insurance, price transparency is nice but is practically useless. Price transparency means everything if you’re without insurance or your plan doesn't cover a certain procedure. For the vast majority of us, calling hospitals to check on their price for an MRI or outpatient procedure or finding out what your insurance pays the hospital for the procedure can be a waste of your time. In just about every case, you will be directed by your provider to an MRI site, hospital or outpatient center where the provider has privileges. Going elsewhere will be considered out-of-network and you could end up paying 100%. Medical billing and payment is very complicated. If we had a universal healthcare system, calling around for the best price would be totally unnecessary.
Consequently, premiums will rise across the board.
In 2022, primary care spending was only 5% of all healthcare costs. The number of primary care providers dropped from 106 per 100,000 people in 2022 to 104 per 100,000 in 2023. The trend is well established. Medical students are gravitating away from primary care (FP, Peds, OB-GYN) and toward specialties. Efforts by Medicare to "level the playing field" between primary care docs and specialists has been slow and inadequate. The best bet for a fledgling primary care resident is to avoid the economic and mental hassles of private practice and seek employment with a large hospital-centric healthcare system. And it's totally understandable. However, the trend toward the security of employ-
This is virtually the wild west of bill ing. If you have had to use an ambulance (and God bless our first responders who often keep you alive on the way to the ER) you probably owe more out of pocket for the ambulance ride than out of pocket for the hospital and physician services combined. Insurance coverage is all over the map (and calling ahead of your emergency for a price check is clearly not an option!) Most likely, you will end up negotiating after the bill arrives. Surprise billing regulations do not cover ambulances. These regs typically apply to bills from physicians who, unbeknownst to you, do not participate in your insurance plan even though the hospital ER does. In most cases, the hospital now pays the difference between what your plan would have paid and what the non-par doc charges. You are held harmless. Both volunteer and for-profit ambulance companies operate outside the competitive market place. Let's face it. They can because you are going to take whatever ambulance arrives first. That being said, 80% of ground ambulance rides are out of network. A case in California recently got a lot of notoriety. A jogger was struck by a car and taken via ambulance to a nearby ER just a few miles away. He was treated and

ment unintentionally exacerbates the shortage of providers because (ask any doc in private practice) employed docs work fewer hours than their private practice counterparts.
PCPs are the quarterbacks of healthcare. Without their involvement and direction, we will end up meandering our convoluted, confusing and disjointed "non-system" alone. Virtual visits and even AI may provide some relief and most patients who have experienced virtual care are OK with it. (Probably had no choice?) Without an adequate supply of MDs, PAs and NPs in primary care, patient frustration and premiums will invariably increase. If we are to fix healthcare, it has to start with the foundation of primary care.
released. The ambulance bill (again, God bless our first responders) was $13,000. After months of phone calls, the Blues [Blue Cross Blue Shield] acquiesced and paid $10,000 leaving the jogger with a $3,000 bill. After another few months of calls, this time with the commercial ambulance (and the press) the company waived the $3,000. The Center for Consumer Information and Insurance Oversight was involved. They were involved in more than 650,000 similar billing disputes in 2023. Unfortunately, 15% of their staff has been eliminated by DOGE, the Department of Government Efficiency. This is just another example of what could be fixed ahead of price transparency.
To put it mildly, things have been rather chaotic at CDC/FDA/ NIH/CMS since the election. As I'm writing this column, here it is where things stand in early March. The FDA abruptly cancelled a March 13 vaccine advisory committee meeting. The meeting is attended by experts — including drug designers, scientists, manufacturing, biologists and other healthcare stakeholders — to recommend the strains for next season's flu vaccine. The unexpected delay has raised concerns that unless a decision is made sooner than later we won't have enough flu vax in the fall. Drug manufacturers face
tight deadlines every year and this is exacerbating the problem. As of this writing in early March, 910,000 people have been hospitalized with the flu. 19,000 adults and 90 children have died from flu complications.
We spend about $5 trillion annually on healthcare or just over $14,000 per capita. It's by far more than any other country. It breaks down as the following: hospitals, 31%; other personal healthcare, 16%; physicians, 15%; drugs, 9%; clinical services. 5%; nursing homes. 4%; home care. 3%. The remaining 17% goes toward net cost of health insurance (basically overhead), investments and public health activities. For hospitals, revenue comes from three main payers: commercial insurance, 40%; Medicare, 30%; and Medicaid, 20%. The remaining 10% is self-pay, grants, investments, donations. Operating margins are razor thin for the majority of hospitals. The cuts to Medicaid will have a disproportionate impact on rural hospitals.
No one is spared from the recent purge of federal employees and our veterans are no exception. They comprise 30% of the VA workforce. The VA has been ordered to cut 80,000 jobs (nurses included) or 15% of the workforce. The goal is to return to the 2019 total of 400,000 employees. There are 170 VA hospitals and 1,380 outpatient healthcare facilities across the country making it our largest healthcare system. The VA cares for 15.8 million vets.
Congress has approved a federal budget that slashes $880 billion in Medicaid funding to indigent individuals, hospitals and nursing homes.
Consequently, if the states are to continue the same level of vices they must raise taxes. If the feds impose a suggested dollar per capita cap, the states will have to come up with between $700 billion and $1.1 trillion over the next 10 years. The states that would be most impacted are Arkansas, Kentucky, Louisiana, Mississippi, New Mexico and West Virginia. All these states are "red" except for New Mexico. In addition to a state tax increase, hospitals will most likely negotiate higher rates from commercial insurers to offset losses in Medicaid funding and the increase in uninsured patients seeking care in their clinics and emergency rooms.

George W. Chapman is a retired healthcare business consultant who worked exclusively with physicians, hospitals and healthcare organizations. He used to operate GW Chapman Consulting based in Syracuse.

Preventive screenings for cancer declined during the pandemic, with lockdowns, social distancing and COVID-19 surges keeping many from needed mammograms and colonoscopies.
But breast and colon cancer screening numbers have since rebounded and have even surpassed pre pandemic screening estimates, a new American Cancer Society study has found.

Thirty-one million people, or 12% of the U.S. adult population, borrowed $74 million last year to help pay medical costs for themselves or a family member, according to the results of a survey conducted by West Health and Gallup.
The online West Health-Gallup Healthcare Survey included 3,583 U.S. adults and was conducted from Nov. 11 to 18, 2024.
The survey revealed that 18% of young adults aged 18 to 29 years needed to borrow money to pay health care costs. Adults aged 30 to 49 years reported similar rates. However, only 9 and 2% of Americans aged 50 to 64 and 65 years and older, respectively, said they needed to borrow money to help with medical costs.
Twenty percent of women younger than 50 years reported borrowing money to pay for health care compared with 14% of men younger than 50 years. Similarly, women aged 50 to 64 years were twice as likely as men in the same age bracket to report borrowing money. Although men were less likely than women
“These findings are mostly encouraging as the pandemic resulted in widespread disruptions in cancer screening in the U.S.,” lead researcher Jessica Star, an associate scientist of cancer risk factors and screening surveillance research at the American Cancer Society, said in a news release.
Unfortunately, the good news doesn't extend to cervical cancer screenings, which remain below pre pandemic levels, researchers reported March 5 in the Journal of the American Medical Association.
“The continued decline in cervical cancer screening is troubling as diagnoses of cervical cancers at an early stage, when they are more treatable, also decreased during the pandemic,” Star said. “Without returns to cervical cancer screening, prevention and early-stage diagnoses may continue to drop and put more lives at risk.”
For the study, researchers analyzed responses to the National Health Interview Survey, an annual poll conducted by the U.S. Centers for Disease Control and Prevention (CDC).
The team compared cancer screening rates in 2019, before the pandemic, to those in 2021 during the pandemic and in 2023 after the end
to borrow money to pay for health care, they tended to borrow more (51 versus 36 percent borrowing $1,000 or more).
Black and Hispanic adults were each more likely to report having borrowed money than their White counterparts (23 and 16 percent, respectively, versus 9 percent). When broken down by age, the disparities were particularly noticeable among adults younger than 50 years (29 percent versus 19 and 14 percent for Black adults versus Hispanic and white adults, respectively).
Fifty-eight percent of Americans said they are concerned that a major health event could lead to personal medical debt, including 28 percent who reported being "very concerned."
"The findings suggest that stronger public policy is needed to address the impacts of high-priced health care; without such changes, millions more may accumulate debt or be forced to make painful tradeoffs about seeking health care," according to a news release from Gallup.
of the global health crisis.
Results show that breast and colon cancer screenings in 2023 exceeded 2019 levels by 7% and 12% respectively, due to sharp increases toward the end of the pandemic.
Meanwhile, cervical cancer screening in 2023 remained 14% below 2019 levels, with no change between 2021 and 2023, researchers found.
“The persistent decline in cervical cancer screening may in part reflect longer-term declines in patient knowledge and clinicians recommending the test,” Star said. “It's imperative that we continue to advocate for returns to cervical cancer screening and efforts must also address the widening disparities in all cancer screenings by socioeconomic status.”
In addition, the rebound in screening for breast and colon cancers occurred mainly among people who make more money, have higher education and are either privately insured or Medicare recipients, researchers found.
“Health systems and health care professionals could play a major role by improving screening communications and providing patient navigators to help address structural and cost barriers,” researchers concluded in the study.



By Gwenn Voelckers

remember the morning of Sept. 11, 2001, as if it were yesterday.
I was at work at the time, when we were summoned into the conference room. That’s where my colleagues and I watched TV in uncomprehending horror as the first tower collapsed and then the second.
We sat there together in stunned silence, until several coworkers abruptly stood up and ran to their offices to make phone calls to check on loved ones in New York City.
Moments later, we were dismissed for the day.
Shaken to the core, we gathered our things, slowly dispersed and went our separate ways.
I returned home in the middle of the day to a quiet house. Alone.
I made a few phone calls, but my friends and family had no words. Nor did I. We were all in shock. So, I turned on the TV and clung to the coverage as if it were a life raft. Commentators were trying to make sense of the unthinkable attack. Public figures were asking for prayers and offering reassurance.
It was all I had.
I remember longing for someone to sit beside me, to help me process the enormity of what was happening, to reassure me that we were safe, that life would go on. But there was no one.
That was my first real taste of facing a crisis alone.
And now, more than two decades later, I find myself — like so many others — struggling with those same emotions. Today, the enemy is not foreign terrorists but something that feels even closer to home.
At least half the country is grap-
pling with an overwhelming sense of fear and vulnerability under the current administration in Washington DC.
Democratic norms are being disregarded, trusted experts removed, legal, environmental and consumer protections dismantled. Mass firings and deportations occurring and the stock market is tumbling as I write this.
Most alarming is the strategic shift toward Russia, undermining longstanding alliances and jeopardizing Ukraine’s future.
Once again, I find myself longing for someone by my side during all this chaos, but over the years, I have learned that living alone does not have to mean helplessness.
There are ways to cope, to stay resilient and to find a path forward — even when the world feels like it’s unraveling.
Here are some of the strategies that have helped me and I hope they help you, too.
First and foremost, embrace self-compassion. These are extraordinary times and it is OK to feel overwhelmed. It is OK to take a moment to step back and acknowledge whatever feelings you are experiencing.
Ask yourself:
• Am I treating myself with the same kindness I would offer a friend going through a hard time?
• Am I allowing myself time to rest, recharge, meditate and pray?
• What small comforts can I give myself today — a warm drink, a cat nap, a walk outside or short drive
in the country? Listening to audio books is my healthy distraction. How can I create moments of peace within my day, even amid the chaos?
2) Connect with
Living alone does not mean being alone. You do not have to endure hard times in isolation. Connection is a lifeline, and it is more important now than ever.
Ask yourself:
• Who are the people in my life that make me feel heard and supported?
• Can I reach out to a friend today, even if it’s just a quick text, email or phone call?
• Are there local or online communities where I can engage in meaningful conversations?
• How can I be a source of support for others, knowing that connection is a two-way street?
While I believe in staying informed, I also recognize the need to protect my sense of well-being. For me, too much exposure can be emotionally draining.
Ask yourself:
• Am I consuming news in a way that informs me or in a way that overwhelms me? More and more, I’ve found that reading the news causes me less anxiety than watching it. I can do without the breaking news banners, sensationalized stories and traumatic imagery.
• Can I set designated times for news updates?
• What are some trusted, balanced sources of information that won’t amplify my anxiety?
Feeling helpless is something I struggle with during challenging times like this, but doing something — no matter how small — can be empowering.
Ask yourself:
• What causes or organizations align with my values, and how can I support them?
• Can I volunteer, donate or advocate in ways that will make an impact?
• How can I channel my frustration into constructive action? Writing this column serves this purpose. And I hope it motivates you and others to get involved.
• What practical steps can I take in my daily life to contribute to the change I wish to see?
5) Pursue Joyful Endeavors
Even in turbulent times, joy is not frivolous — it’s essential. Engaging in activities that bring you happiness can replenish your emotional reserves.
Ask yourself:
• What hobbies or creative pursuits bring me a sense of fulfillment?
• Can I set aside time to read, watch a movie or listen to music without guilt?
• How can I incorporate small moments of beauty into my day — a lit candle, fresh flowers, a beautifully wrapped package, a birdsong, a heartfelt thank you.
• What places or experiences make me feel at peace and how can I seek them out? You’ll often find me at the Lamberton Conservatory in Highland Park.
You Are Not Alone:
The truth is, these strategies can be applied to any crisis, whether it is a political upheaval, a personal loss or a medical emergency.
So, if you are living alone and struggling with uncertainty, know this: There are countless others who share your fears, your frustrations and your hopes for a better future. By reaching out, taking action and caring for yourself, you can ease the burden of solitude and cultivate a renewed sense of purpose and resilience.
Remember — you are not alone. We will find a way forward. And we will do it together.

Gwenn Voelckers is the author of "Alone and Content," a collection of inspiring essays for those who live alone. She welcomes your comments about this column and topic suggestions for future columns at gvoelckers@ rochester.rr.com





By Deborah Dittner
Asimple quote I found that says it all — “Love your feet, love yourself.”
If you take care of your feet, you are actually looking after your whole self. Of course, there is more to it than that. However, looking at proper foot health will guide you to improved mobility later in life.
Your feet carry you through life from very young in age to very old. Without proper foot care, you may miss out on certain life situations. So…how do you care best for your feet?
• Walking, or better yet, barefoot walking can help you connect with the earth. There are numerous sensory receptors on the bottoms of your feet needing to “feel” the ground and
allowing you to freely move your toes. You can’t always be barefoot so finding proper fitting shoes is essential. There are athletic shoes, dress shoes, work shoes, boots, sandals and more but finding those which suit your feet and any anatomical issues can be challenging. Some may have high arches and others may have flat feet. Bunions also create challenging footwear needs.
The footwear you choose should be comfortable and support the foot’s regular position. Some may need a wide toe box especially if bunions are a concern. A proper fitting shoe will allow your toes to move and not limit the front of the foot.
The amount of cushioning depends on the activity. If you are
By Deborah Jeanne Sergeant
Without any warning, you suddenly experience a sharp pain on the bottom of your foot.
Upon examination, you discover a corn: a small, deep formation of dry skin with a hard center surrounded by swollen skin.
Although a corn is deeper than a callous and more likely to cause pain, friction causes both of them to form.
Andrea May, owner of Andrea’s Foot Care in Rochester and a nail technician with advanced education in diabetic and geriatric foot care, explained that if a corn becomes painful, people should seek help from someone experienced in caring for these issues.
Despite the ubiquity of overthe-counter corn removal methods, “there’s very little that you can do at home because a corn is conical in shape, like an ice cream cone. It goes deep. It feels like you’re walking on glass or a stone. It can come on suddenly. I’ve had this experience. It was fine and seconds later there’s pain.”
Corn removal pads from drugstores typically contain salicylic acid to burn off the dead skin, but May
walking on cement for hours on end, you will want a shoe with increased cushioning and the wide toe box.
• Strength training for your feet. There are many exercises to choose from with numerous benefits such as improving flexibility, balance, reducing discomfort and overall strength. Here are some to consider:
Toe raises — standing on your toes for a few seconds then lower back down (great for strengthening the calves).
Heel raises — opposite of toe raises.
Toe spreads — spreading your toes wide apart, hold a few seconds, then release.
Toe taps — tap your toes individually or all together from forward to side to back (great for balance).
Toe curls — curl your toes under, hold for a few seconds then release. You can also place a towel under your feet and grasping the towel with your toes to gather.
Tree pose (yoga) — stand on one leg with the other foot held at the ankle, the calf or the thigh (never at the knee). Build up the time as your balance and strength increase.
Massage — place a tennis ball under your arch and move the ball around in a circular motion then reverse. No tennis ball? Use your hands to massage the foot. This works out tension, increases circulation and decreases any tightness.
With any type of exercise, begin slowly and increase the repetitions as tolerated. These can be done on a daily basis or at least several times a week. If any pain occurs, stop the exercise and check in with your healthcare provider.
Problem issues can also arise requiring immediate action:
• Blisters — often caused by improperly fitted shoes or shoes that did not supply the necessary support
for the activity. Shoes that support the arches and allow for proper foot alignment will help keep blisters at a minimum.
• Plantar fasciitis — the band of tissue supporting the arch of your foot becomes inflamed causing heel pain and decreased mobility. Stretching prior to and after exercising is important as this may result in discomfort up your legs and as far up as your neck. Follow up with your healthcare provider.
• Bunions — the bony bump at the base of your big toe. It is often said that bunions are caused by tight, narrow fitting and high-heeled shoes. Properly fitted footwear is the best prevention. Using toe spacers may also prevent and relieve the discomfort of bunions.
Most importantly — pay attention to any discomfort your feet may experience.
If your feet hurt at the end of the day or you have developed knee or hip discomfort, consider any changes that have occurred in your footwear.
The sooner these issues are addressed, the better the healthcare of your feet adding improved function and mobility. So before any issues occur, wear proper fitting, wider toe box shoes, use toe spacers, strengthen your feet with exercise and walk barefoot whenever you can. Your feet (and body) will thank you!

Deborah Dittner is a family nurse practitioner and health consultant. Her mission is to transform as many individuals as possible through nutrition and lifestyle changes. www. debdittner.com
warned that these can go too deep and harm healthy skin along with the corn. It’s also likely that the pads won’t entirely remove the corn or may even cause infection. A professional can remove the corn mechanically without damaging the healthy tissue near the growth.
“Moisturizers are always recommended but use those made for the skin on the feet, which is different from the skin on the rest of the body,” May said. “There are foot creams and foot lotions made specifically for the skin of the foot. Usually, the moisturizer itself is non occlusive so it won’t clog the pores. The foot doesn’t have oil glands. The foot moisturizes itself through sweat so we need to keep the sweat glands clear and open. Vaseline will clog those pores and cause problems.”
Corns develop to protect the bone from friction against the skin. May said that it’s nearly always tight shoes that cause corns. The footwear’s cost or newness doesn’t matter. They need to go if they cause pain, she said.
“If you’ve worn them for a long time and a corn appears, you’ll think

it’s something else causing the corn. But they’re shoes that are worn out.”
Many people keep shoes as long as the uppers look good and without any attention to the soles. May challenges clients to look at the soles of their shoes as if they were car tires. Would they drive a car with tires that appear that worn?
She advocates replacing shoes about every six months if they’re used regularly. It’s also helpful to rotate among different pairs of shoes as they use different muscles of the feet and supply support differently.
“I recommend people try a larger size than they’re used to,” May said. “Get your regular size and try a half size larger and see if the half size larger is a little better. We think the shoes we have are great but as we
age our feet tend to widen because of gravity.”
Check to see if the shoe slips on the heel and if it is tight against the toes. Good-fitting shoes should feel secure on the heel and allow room for toes to move.
Synthetic materials in socks prevent the feet from breathing and trap moisture against the skin. May said that contributes to friction, as do seams.
“There are more and more quality socks being made where the seam doesn’t rub,” she said. “If you’re ordering online, read the reviews. Talk with your friends. Quality socks can be expensive but they make good gifts.”

By Deborah Jeanne Sergeant
Deer ticks, also known as black -legged ticks, can carry and transmit the bacteria that cause Lyme disease.
The illness was named for Lyme, Connecticut, where it was first identified in the US.
Unless tick bite patients infected with Lyme are treated early with antibiotics, the disease causes patients to experience swollen knees, paralysis, skin rashes, headaches and severe chronic fatigue.
Late-term use of antibiotics is not always as effective.
Not every tick transmits Lyme disease. Still, avoiding deer tick bites can prevent infection. Once the weather reaches above 40 degrees F., ticks can emerge. The New York State Department of Health states that deer ticks are most active from April through mid-May and also in early fall.
It may seem like it would be easy to spot a tick on your leg, but Matthew Hanggi, registered nurse
and Ontario County Public Health’s communicable disease control coordinator, said that nymphal ticks are the size of a poppy seed.
Unlike fleas, crawling is the only way that ticks move.
“They crawl toward a host or hitch a ride when humans, deer, mice, chipmunks, et cetera brush up against the grass, leaves and weeds of their preferred habitats, which are shady, moist areas from ground level to more than 24” above the ground,” Hanggi said.
He encourages people who spend time outdoors to:
• stay in the center of hiking trails
• tuck their pants into their socks
• wear light-colored clothing (this makes ticks easier to see)
• apply Picaridin or DEET when entering wooded areas
• physically check for ticks when leaving those areas
Although it should not be applied directly to the skin but on
clothing, backpacks and footwear, permethrin can help deter ticks.
“It lasts about a month, though some clothing purchased from LL Bean, REI and other companies comes pre-applied and can last longer,” Hanggi said.
Keep permethrin away from cats. While it is wet, it’s highly toxic to cats.
Another monthly tick prevention is providing dogs with prescription parasite medication such as Simparica Trio, which guards against ticks, fleas and heartworm. Check the animal’s fur, especially between the toes and behind the ears, for ticks after time spent outdoors.
“Protecting pets is good for the animal and good for humans as it prevents them from carrying ticks into the house or bed if shared,” Hanggi said. “Allowing pets to sleep in your bed certainly adds to the risk quotient.”
After spending time outdoors, take a good shower. It takes ticks 24 hours to crawl to where they typically like hiding, such as in a bodily crevice or above the hairline. Hanggi also advises placing clothing in the dryer on high heat for 10 to 15 minutes.
“Ticks are more susceptible to dry conditions than they are to cold,” he said. “The act of drying at high heat will kill any ticks on clothing.”
in sunny areas and away from the property edges where overgrowth is typical.
“There are professionally applied pesticide options folks can apply to lawns to control ticks, but these can be expensive, detrimental to lake health and have diminished effectiveness if many of their neighbors don’t undertake similar actions,” Hanggi said.
Keep wildlife away from the home by minimizing attractants like food, water and shelter. Leaving out pet food and water bowls invites wildlife to help themselves and bring along ticks. Block off any cracks where critters can crawl into outbuildings.
Challis Mathes, diagnostician for Cornell Cooperative Extension Monroe County, said that the organization’s agents do not test ticks for Lyme but can identify what type of tick residents find on themselves or their pets. Have ticks tested at locations listed at https://nyticks.org/.

“If you go to the doctor and say you had a tick, they’ll give you an antibiotic,” Mathes said. “It’s pretty high likelihood of preventing Lyme if you catch it soon enough.”
He said that older adults tend to have tick bites more
often than younger people, likely because they generally do not shower as often.
Although we tend to think of picking up ticks while hiking, the encroachment of wild animals near homes can mean simply gardening in the flowerbed can expose homeowners to ticks. Hanggi has read case reports of people picking up a tick while walking to their mailbox.
He recommended installing fencing, moving wood piles and bird feeders toward the edges of the property and keeping grass cut short. Keep children’s play equipment
Mathes encourages people to leave opossums alone and to not shoo them from their property.
“Opossums are our friends; they eat an incredible number of ticks each year,” he said. “Their body temperature is very low for a mammal. They tend to not carry rabies. I don’t think there are any records of them carrying rabies. They’re relatively harmless.”
Chickens, ducks and guinea fowl are also natural tick predators.

“From





Really,
By Anne Palumbo
We hear a lot about “superfoods” these days — foods that offer high levels of desirable nutrients that are believed to offer simultaneous health benefits beyond their nutritional value.
These foods, as defined in the Merriam-Webster Dictionary, are “rich in compounds (such as antioxidants, fiber or fatty acids) considered to be beneficial to a person’s health.”
But what about “superbadfoods” — foods that offer high levels of undesirable nutrients that clog arteries, add pounds, raise blood pressure, trigger diseases, and shorten lives? Foods that we mindlessly eat or (gasp!) feed to our kids or grandkids? Where’s Merriam’s definition for those disastrous foods?
While there are dozens of unhealthy foods out there, we’ve mentioned some alarming — perhaps surprising — foods that our bodies could regularly do without.
Just how bad are they?
Well, when you compare what these superbadfoods offer up in a single serving against what the experts recommend for an entire day, you may be persuaded to rethink your eating habits.
Average daily recommendations from accredited institutions:
• Sodium: less than 2,300 milligrams per day (equal to about 1 teaspoon of table salt) and no more than 1500 milligrams per day with high blood pressure.
• Sugar: no more than 100 calo ries per day (about 6 teaspoons or 24 grams) for most adult women and no more than 150 calories per day (about 9 teaspoons or 36 grams) for most men.
• Fat: should contribute 20% to 35% of total daily calories (about 4578 grams) with no more than 20 to 30 grams of saturated fat.
ing you never fraternize with another Frito again. Moderation is the key here: daily, devoted, mindful moderation. As the saying goes, “Man and woman cannot live on junk food alone.”
What do years of regularly eating processed meats and health have in common?
Cancer.
According to the World Health Organization, regular consumption of processed meats — bacon, sausage, hot dogs, ham and cold cuts — has been associated with an increased risk of cancer (especially colon

• Cholesterol: no more than 200 milligrams a day (if risk factors for heart disease present); no more than 300 milligrams a day (if no risk factors).
• Overall calories: Calorie needs vary depending on the person and their personal health goals, but an average starting number is around 2,000 calories per day.
Of course, no one is suggest-

grams total fat (7g saturated), and 660 milligrams salt. Three slices of bacon have 150 calories, 12 grams total fat (3 grams saturated), and 550 milligrams salt. With early-onset colon cancer rates on the rise for younger adults, it should give all of us pause. Many experts do say, however, that eating a small amount of processed meat occasionally, such as once or twice a month, is unlikely to significantly harm health.
is why many states have actively banned the sale of sodas in high schools. Coke Original, America’s most popular soft drink, has 2-3 times our average daily sugar needs in one serving! Why worry about consuming too much sugar? In the short term, it may contribute to acne, weight gain, tooth decay and fatigue. In the long term, excessive sugar consumption increases the risk of Type 2 diabetes, obesity, heart disease, certain cancers, high blood pressure and depression. Of course, some sugar (which the body converts to glucose) is essential for energy production and proper brain function.
Tips: Gradually replace soda with nutritious alternatives: water infused with fresh fruits and herbs, sparkling water with a splash of fruit juice, homemade iced or herbal tea, reduced-sugar fruit juices and smoothies, and good old plain water.
and stomach), as well as heart disease and diabetes. All meat that has been smoked, salted, cured, dried or canned is considered processed. Nitrates and nitrites — whether synthetic or natural (i.e. celery powder) — are the processing agents behind the elevated risk. Chemicals aside, many processed meats are high in calories, fat (especially saturated fat) and sodium. One classic Zweigles hot dog (minus the bun and fixings) has 220 calories, 19
Tips: Check out plant-based alternatives. Swap red-meat processed foods for white-meat processed foods, which generally have less total and saturated fat. Consider canned or pouched tuna or salmon instead of classic lunchmeats like ham, pastrami, roast beef or salami.
Drinking soda is like guzzling liquid candy, no thanks to its high concentration of sugar. Sugary drinks are a major contributor to our country’s obesity epidemic, which
Oh, how we love our Lay’s, Doritos, Cheetos and Rice Krispies Treats here in America! Indeed, they fly off our supermarket shelves to the tune of $52 billion per year. Despite being convenient and addictive to boot, chips, like most other ultraprocessed snacks, are astoundingly unhealthy (one serving of Lay’s classic: 160 calories, 10 grams of fat, 170 milligrams sodium). What’s more, they defy everything — everything — a snack is supposed to do: give your body a nutrient-dense, long-lasting pick-me-up between meals. Research has shown that because today’s ultraprocessed snacks contain a lot of fat, sugar, salt and carbs, they are better at activating the brain’s reward system. Translation? We can’t stop eating them. The unfortunate consequences? We develop many of the same chronic diseases as those associated with sugar-loaded soft drinks.
Tips: Opt for snacks with protein, fiber, and healthy fats that take longer to digest and help keep you full throughout the day. A few suggestions: nuts, Greek yogurt


with fruit, hard-boiled eggs, cheese with whole-grain crackers, popcorn, homemade trail mix and protein smoothies.
Although soups may be the perfect meal when you’re feeling chilly, under the weather or not particularly hungry, some canned and chain-restaurant soups are not so perfect for your health. From sodium to fats, calories to cholesterol, soups can foil your good intentions in just a few slurps. Are you sitting down?
One cup of Campbell’s Chicken Noodle Soup, their most popular soup, has 1780 milligrams of sodium — a whopping 78% of daily needs knocked off in one bowl (over 100% for those with high blood pressure). Panera’s popular broccoli cheddar soup has 1560 milligrams of sodium without the bread bowl and a staggering 2140 milligrams with. While sodium is an essential nutrient that controls blood pressure and is needed to make nerves and muscles work properly, too much sodium can lead to high blood pressure, heart disease, kidney strain, and stroke. It can also drain calcium from bone.
Tips: When dining out, choose broth-based soups over cream-based; when buying canned, opt for lower-sodium broth-based soups; and when making soup, go easy on the salt, substitute cream or whole milk with reduced-fat milk, use whole grains versus refined, and up the veggies.
Most of us think salads are automatically healthier foods: low in calories, sodium, and fat; high in vitamins, protein, and fiber. The ones we make at home: perhaps; the ones we order out: perhaps not. For example, Chick-fil-A’s Cobb salad with avocado-lime ranch dressing—high in calories (830), fat (60 grams), and sodium (2220 mg)—is no day at the healthy-diet beach! And building a Chipotle salad with lettuce, chicken, guacamole, corn, cheese, and chipotle-honey vinaigrette, chased with a side of queso blanco and chips, could quickly turn that healthy-sounding lunch into a calorie bomb. Nonetheless, salads are an important part of a healthy diet because they are a year-round source of essential vitamins, nutrients, and beneficial antioxidants that can help reduce the risk of chronic diseases such as heart
disease, diabetes, cancer, and obesity.
Tips: Whether taking out or making at home, assemble salads wisely: forgo caloric toppings (bacon bits, croutons, candied nuts) and baked shell bowls, go for dark greens, add healthy protein sources, bump up the veggies, opt for vinaigrette- or yogurt-style dressings over cream-, cheese-, or mayo-based ones, and request dressing on the side. Oh, and stay away from “crispy” and “crunchy” protein sources, as the description implies “deep-fried.”
From French fries to onion rings, doughnuts to funnel cakes, many of us find fried foods irresistible. Unfortunately, compared to other cooking methods, deep frying adds a lot of calories and fat. For example, one small baked potato contains 120 calories and 0.2 grams of fat, while the same amount of French fries contains 430 calories and 20 grams of fat. What’s more, fried foods are typically high in trans fats, the worst kind of fat you can eat. Unlike other dietary fats, trans fats do a number on cholesterol: raising “bad” while lowering “good.” Research has shown that a diet laden with trans fats increases the risk of heart disease, the leading killer of adults. But the badness of fried foods doesn’t end there. Regularly eating fried foods puts you at a greater risk of developing Type 2 diabetes and obesity, two conditions that, over time, can lead to high blood pressure, some cancers, nerve damage, sleep apnea, dementia, heart disease, asthma, and more. Yikes.
Tips: Avoid or severely limit your intake of fried foods. When frying at home, choose safer, more stable oils: coconut, olive, or avocado over canola, corn or sesame oil (to name a few). Consider healthier cooking methods: steaming, roasting, stir- or air-frying.
Read product labels and restaurant menus carefully, from nutritional information to ingredients. Consider how something is prepared: baked versus fried. Think about health in the long run, from yourself to your loved ones to those on the way.
Anne Palumbo writes the column Smart Bites, which is published every month in In Good Health.













By Anne Palumbo

Basmati rice is my go-to rice, and here’s why: it’s healthier than popular white rice; it boasts a subtle, nutty flavor; and it’s slightly lower in arsenic than most rice.
Let’s begin with why it’s healthier than America’s most-consumed rice.
White rice has a high glycemic index, meaning it can cause rapid blood sugar spikes. These yo-yo spikes, while unhealthy for all, are particularly harmful for those with diabetes or insulin resistance. Basmati rice, on the other hand, especially

whole-grain brown basmati rice, is considered a low-to-medium glycemic index food.
Consuming foods that are lower on the glycemic index is important for many reasons.
It helps regulate blood sugar levels, potentially reducing the risk of developing diabetes (one of the top 10 leading causes of death in the U.S.). It can help with weight control by promoting satiety and reducing the urge to eat during blood-sugar fluctuations. And it may reduce the risk of heart disease, certain cancers
and other chronic conditions, according to trusted studies.
Basmati rice, like most rice, is enriched with certain nutrients to help boost its nutritional value. In particular, basmati boasts decent amounts of iron, B vitamins like folic acid, thiamine and niacin, which together help convert food into energy, and selenium, a powerful antioxidant that helps keep cells healthy.
I always opt for whole-grain brown basmati rice over the refined white version because it’s got more fiber: about 2-3 grams per serving versus less than 1 gram in white. In addition to the obvious benefits of keeping us regular, fiber is your heart’s best friend: it lowers cholesterol; it lowers blood pressure; it helps with weight management; and it improves blood sugar control. Top your basmati with some legumes and vegetables and you’ve created a trifecta of fiber goodness!
In addition to the nutrients listed above, an average 1-cup serving of brown basmati rice has about 200
Serves 6
3 cups cooked basmati rice, cooled
3 tablespoons olive oil
2 leeks, thinly sliced (white and light green parts)
12 ounces asparagus, sliced on the diagonal in one-inch pieces
2 garlic cloves, crushed
2 teaspoons dried basil
Salt and pepper to taste
1 cup shelled edamame, defrosted if frozen
lemon juice and zest
¼ teaspoon red pepper flakes (optional)
Turns out, Americans may be drinking less coffee, soda and tea, but they're getting more caffeine than ever.
A new study of more than 49,000 U.S. adults found that while fewer are sipping caffeinated drinks, those who do are choosing much stronger doses, with coffee taking the lead.
The result? Caffeine intake is rising, even though the average consumption is still below 400 milligrams of caffeine per day. That's the amount health experts consider safe.
“We are all aware that the
caffeinated beverage market has changed dramatically over the past 10 years, yet no comparable, comprehensive caffeine intake data have been published in recent years," study author Diane Mitchell of the Institute for Advancing Health through Agriculture, Texas A&M AgriLife, said in a news release.
Coffee now accounts for 70% of total caffeine consumption, up 15% from the previous 2010-2011 survey, Mitchell's team reported.
What's more, carbonated soft drinks now contribute only 15% of
½ cup nut of choice, chopped (optional)
1. Prepare rice according to instructions. Let cool. (Can be made a day ahead.)
2. In a large non-stick skillet, heat 2 tablespoons olive oil to medium. Add the sliced leeks and sauté until wilted, about 2 minutes (okay if some get crispy). Next, add asparagus and cook for 5 minutes more, stirring frequently, until the asparagus is
Consider reducing your rice consumption if arsenic levels concern you. According to many studies, big rice eaters (about ½ cup of rice per day) have consistently high arsenic levels, no matter the type of rice. Research has shown that, over time, arsenic can harm your health and potentially increase your risk of certain cancers. To reduce arsenic, some suggest rinsing raw rice before cooking and using a large amount of water to cook rice, which is then drained.
calories, 4g of protein, and 34g of carbohydrates (the complex kind that take more time to break down).

tender-crisp.
Anne Palumbo is a lifestyle columnist, food guru, and seasoned cook, who has perfected the art of preparing nutritious, calorie-conscious dishes. She is hungry for your questions and comments about SmartBites, so be in touch with Anne at avpalumbo@aol.com.
3. Add garlic, basil, salt and pepper and stir for 1 minute more. Gently mix in edamame. Remove from pan and set aside.
4. With heat still on medium, add the remaining tablespoon of olive oil to pan, swirl around, then add rice, pressing down to make a single layer to brown rice. Let the rice cook, undisturbed for 5 minutes. Stir in vegetable mixture and cook until heated up, about 2 minutes more.
5. Serve; sprinkle with some lemon juice and zest; garnish with optional ingredients. Enjoy!

caffeine intake, a 27% decrease from a decade ago. Tea consumption has also dropped significantly, with 50% fewer tea drinkers overall.
However, the remaining tea drinkers nearly doubled their caffeine intake from tea, suggesting those who stuck with the beverage are, in fact, drinking more. Energy drinks, which were less common a decade ago, now account for 6% of total caffeine intake, as the
number of available brands has jumped from 559 to 970. Despite these shifts, average caffeine intake remains below the federal government's recommended limit of 400 milligrams per day — about two to three 12-ounce cups of coffee.
“With a constantly evolving market of caffeinated beverages and the potential impact it has on beverage consumption patterns, continued monitoring of caffeine intakes is warranted," the authors concluded.
By Shaina Zazzaro
The 80/20 rule. What is it?
I asked my husband what I should write about in this next article and this one was his idea. So shout out to Mike.
He mentioned the 80/20 rule since it is how he has lost weight and how we live. So what is it?
Basically, you eat super on point for 80% of the time — healthy meals, no junk food. I don’t mean you have to eat carrots and chicken all day. You can have a huge variety of portioned meals, like the ones we offer at Effortlessly Healthy — portioned meals.
There are 21 meals in a week, seven breakfasts, seven lunches and seven dinners. So this means eat 16 of your meals stricter than up to four of them. I will tell you right now, if you do your own meal prep, or buy a meal prep it will make your life easier for following this rule. Being on the go, going through the drive-thru will make it so you are more 20/80 not 80/20. Going out to eat is the easiest way to overeat without realizing it.
For exam ple: Break fast. I think breakfast is probably the easiest meal of the day to eat super healthy, but beware of what you perceive to be super healthy. A smoothie or a açaí bowl can add up to be heavy on calories and sugar.
I personally opt for always having protein, whether it is a protein yogurt or eggs. Trust me, you need protein and if you eat a whole egg you’re getting so many natural vitamins (eggs really are nature's vitamin) and fats that keep you fuller longer.
Switch your cereal for eggs and toast and I bet you will be able to make it to lunch without a snack. (I wish my daughter would listen to me on this one!)
Lunch: now here is where people will start to have a hard time. There is nothing wrong with packing a lunch with you. I will pack my lunch and walk right into an event, because if I don’t want to eat what they are serving (unless it’s Effortlessly Healthy) I can pull out my meal and not ruin my 80/20

people are afraid to carry around a lunch box, I love having my drinks and lunch available to me at all times. Maybe I’m the anomaly of the world!
Dinner: now here is where I personally like saving my 20%
eating out at least once a week and I want to enjoy myself. I won’t skip an appetizer. I love trying new foods! So think about it, you can bring your lunch to work five days a week and then you

•
•
can go out to dinner, enjoy appetizers, some wine and a great meal and not ruin your diet for the week! See, life in moderation!
Dessert you ask? I always save room for dessert and if you put a chocolate chip cookie in front of me I cannot ignore that cookie! Give me a warm cookie skillet and really make my day. Life in moderation. Eat healthy 80% of the time so that 20% when you have that indulging food you are still able to reach your healthy goals and still feel great! I’m not trying to keep plugging my company, but I created Effortlessly Healthy to help people on the go enjoy healthy meals, effortlessly. So if you are someone that is finding yourself spending a lot of money and calories on takeout, look into meal prep. If you don’t want to use EH, no hard feelings, there are many companies out there. But know that meal prep companies can help you stay on track and in line to go out to dinner.
Since we are really getting to know each other — if you’re curious to know where I love to eat out, my favorite restaurants are as followed: Rocco for Italian, and for steak I always choose Max Chophouse or Black & Blue Steak & Crab. Try O’Reins in Greece for gelato that you will crave every day of your life. Trust me.
If you have a restaurant I need to try, shoot me a message @ShainaZazzaro
Local News Inc. is hiring drivers to distribute copies of In Good Health – Rochester Healthcare Newspaper in Monroe County. It’s not a regular job. Once or twice a month. No heavy lifting.
The job consists of getting the monthly publication in our storage near Kodak and distribute it to various locations, mostly at doctor’s offices, hospitals, healthcare centers and other high traffic locations. We provide a list of places that receive the paper regularly.
The job needs be performed during the day, roughly from 9 to 5 from Monday through Wednesday. In general, pick up is on the first Monday of the month around 9 a.m. (once a month). A reliable car with a good size trunk is a must.
$15.50 an hour plus mileage allowance (30 cents per mile). It amounts to about $200 per job.
Great for active retirees and for stay-at-home moms who have some free time.
For more information, call (585) 421-8109 and ask for Mary T.

Shaina Zazzaro is a devoted wife and mother of two, blending her roles with a passion for health and wellness. She is the owner and chief executive officer of local meal delivery service, Effortlessly Healthy. For more information, visit www.ehmeals.com.


By Deborah Jeanne Sergeant
Receiving a diagnosis of autism is not important only for tapping resources from the New York State Office for People With Developmental Disabilities.
Even for those who do not need that level of support, it’s good to know.
Nym Dawson, peer mentor at Golisano Autism Center in Rochester, was diagnosed at age 19. Now 30, Dawson said that autism is “one way the brain works. In discovering how your brain works, it doesn’t matter if it’s ‘neuromajorative,’ it’s the operating system. When you understand in the mode your brain operates, things make more sense.”
Dawson also believes that having a diagnosis is important for identity, understanding, developing coping mechanisms and possibly directing one’s career path.
“Right around when I got my diagnosis, I was working as a teaching assistant,” Dawson said. “I was working with autistic children and seeing similarities. I saw we weren’t that different, though there is a broad spectrum in autism. I help with life planning and that sort of thing. It’s given me an entire direction. And helped me understand who I am as a person.”
A misdiagnosis of bipolar as a teen didn’t fit Dawson’s experience. But working with a psychologist and reading an article about autism pointed towards autism. After testing, it was clear that autism was the answer. Dawson received a diagnosis through a now retired psychologist.
Unlike with children seeking a

diagnosis, “seeking adult diagnosis is difficult,” Dawson said. “There are not a lot of places that do it that accept insurance. It’s private pay or you have to be seeking OPWDD services to get a diagnosis. It’s fairly inaccessible because of the expense.” Thankfully, Dawson’s father paid the test’s $2,000 fee. Helping clients at the Autism Center figure out how to afford the test, which can range from $600 to $2,000 is one way Dawson helps more people access services and better understand how they think.

“I don’t diagnose, but I talk with people about it,” Dawson said. “I’m a big supporter of self-diagnosis because of how hard it is to get a diagnosis. Most people who self-identify aren’t people who see one video on the internet. They’ve gone through immense research. No one goes through life and says, ‘Yes! I’d like to be autistic.’ I will help people have those conversations and help people get answers.”
Dawson wishes that “fear mongering” about autism would stop — especially when used by organizations to raise more donations, as if it’s the “worst thing to happen to your child,” Dawson said. “Autism isn’t a good thing or bad thing. It just is. It’s neutral. If I do x, y, and z for myself, I’ll be OK. In the neurodiversity movement, we tend to view autism as something that is neutral and something that is good about ourselves. It’s part of self-esteem. I would not trade my brain for the world. As much as I have challenges, I wouldn’t want it to be anyway than what it is.”
Neurodiversity has helped shape Dawson into a more effective advocate for people with autism, a considerable asset for this type of work. The Autism Center has provided a few accommodations as required by ADA law. However, nearly all of how Dawson works is just like any other employee.
“In my office, fluorescent lighting is a terrible sensory thing,” Dawson said. “I have a light cover that makes it easier for me to work. I also have flexibility in my work schedule
which is important.”
Sensory input that is bothersome varies among people on the autism spectrum, both in intensity and in type. Some autistic people may struggle to understand interpersonal relationships and to follow more subtle nuances of communication. It’s helpful to work for an employer that “gets” autism. Not all employers would be this supportive and Dawson appreciates this, commenting, “I’ve worked with people who’ve had a hard time getting listened to. It does happen. But I’m lucky. When we talk about sensory challenges, it causes physical pain to our bodies. It’s not just bothersome; it hurts me.”
Having a diagnosis in hand helps people on the autism spectrum receive the accommodations they need. But more than any of that, Dawson is glad to have a diagnosis to feel a true identity with others who share the same experience.
“There’s a lot of isolation of being autistic as an adult and not knowing,” Dawson said. “We socialize in a completely different way than neurotypical people and that can be extremely isolating. A lot of people I work with don’t have a good community of people who they feel understand them. Once you identify yourself that way, you open up a world of people who are just like you and shakes off some of that loneliness.”
Loneliness can significantly harm mental health. Dawson added that the life expectancy of autistic people is much lower than the general population because of suicide.
Dawson invites anyone in the Rochester area to reach out and learn more about autism if they would like additional information or direction to resources that can help.
“Find other autistic adults whether online or in a local group or anything like that,” Dawson said. “Being with other autistic people will be helpful.”


By Jolene Cleaver
Jenniferand Benjamin Bailey have four children: three daughters and their youngest — a son, 7-year-old Connor.
Though the youngest, he has managed to teach his family the most life lessons.
This is his story.
The Oneida, Madison County, resident was diagnosed at 19 months old with profound autism.
According to a report released in 2023 by the Centers for Disease Control and Prevention (based on data collected from 2000-16), 26.7% of people diagnosed on the autism spectrum have profound autism.
His mom said that from the very beginning, the family was able to jump feet first into the pool to find resources for Connor.
When he was formally diagnosed, the family had a collective, “Oh, this is who he is now,” Jennifer remembered.
In the very beginning, as the family was acclimating, the mother said habilitative services were key in helping her family enter Connor’s world and help him connect with his environment at his pace, instead of the reverse where he would be tasked to constantly try to fit into the world around him.
But the journey to that mental point started several months prior, as questions about his development as an infant began to rise.
“When he was around 9 months old, his babbling stopped,” she said.
Then there were the missed developmental benchmarks — his eye
contact while being fed lessened and he needed more support to sit up.
Along the road to getting diagnosed, doctors briefly thought he might have a hearing deficit. Testing ruled that out. A few months after that, doctors assessed all the data and made the diagnosis.
Then, the real work for the family began.
“We had to figure out a way to make the world ‘less’ so he could engage,” she said. “Today is just so demanding.”
Part of that came in the form of learning that her son had a love of the outdoors. Wind and water being tactile sensory engagements that he craves. So now, splash parks, lakes, beaches, hikes all factor in his world where he can relax and be himself.
She can visibly see Connor’s shoulders relax when watching waves splash on a lake or walking on a path through the woods.
Along the way, the family learned to slow down, To take respite and retreat opportunities. To look at the world around them as a unit.
The current day to day
“Connor’s never still,” his mother said. “He’s often jumping, moving, stimming.”
The challenge is getting his body to coordinate with what his mind wants to do, she added.
He is non speaking —which is different from being non verbal, she pointed out — and attends Willard Prior Elementary School in a specialized classroom. He can say words with an effort, his mother said. But he largely uses an augmentative and alternative communication (AAC) unit to converse.

Every week, he receives at least 25 hours of applied behavior analysis therapy plus occupational speech and physical therapy and adapted physical education.
Among services, through the New York State Office for People With Developmental Disabilities, he attends respite at the ARC of Madison Cortland’s kids club, attended a week-long camp at ARISE at the Farm in Chittenango last summer and engages in programming through Families FIRST, an organization which provides person-centered support for people living with disabilities.
He also regularly has appointments for neurology, a developmental pediatrician, pulmonary, geneticist, infectious disease, an ear, nose and throat specialist, an optometrist — the list can go on.
The Baileys also work full time. Jennifer is an occupational therapist and Benjamin works remotely for The Hartford.
But the family makes their busy schedule work.
“That’s our non stop lives that we never anticipated. Profound autism has changed everything and it’s certainly been an adjustment. Our Connor was diagnosed at 19 months old and I could name off all his milestones, but what the paperwork won’t say is how he’s changed us from the inside out. We faced questions of faith, justice and what love really meant. Connor has an incredible capacity for joy. He is a sensory seeker and the experiences that bring him joy are so full of light and depths of belly laughter, you can’t help but be moved,” she said.
“It is also heartbreaking to watch him crumble under the weight of a lack of ability to communicate. His ability and intelligence in navigating electronic devices, picking up on vocabulary and even to spell and read are incredible. Functional
communication, daily life skills and sensory regulation are challenges that wreak havoc on his life daily. We watch, pray and support as best we can to help him to grow through it,” she added.
Over the years the family has grown right along with Connor.
“His sisters’ compassion has grown. Their awareness has grown. As a family, we’ve slowed down and take in more. We’re the lucky ones, but you don’t process that unless you slow down,” she said.
She added that her son — who is on permanent disability — will need support for the rest of his life. So, while families need to live in the moment and the day-to-day to help family members with autism achieve goals, there are always long-range plans that need consideration and work, she said.
Her advice to parents of children who receive a diagnosis: “Remember to love your kid where they are at. And it’s the hardships [in life] that help reveal the beauty underneath.
“The thing with autism is you have to expect the unexpected and find those special moments to enjoy.”
Like the splashing of waves. The wind between your fingers. Or the sun on your face. And sharing it together with your family.
The Bailey family will host an autism walk at 10 a.m., April 26. at Higinbotham Park, 116 Broad St. in Oneida. The city of Oneida is co-sponsoring. Get more details here: https://tinyurl.com/2fahfn86
By Deborah Jeanne Sergeant
The COVID-19 pandemic highlighted the need for greater availability of nursing home and assisted and independent living opportunities for older adults.
Too few staff and too few residences mean that this population has few choices when they begin to need more support.
The same is true of people with developmental disabilities as they come of age.
As parents of people with disabilities grow older and die, parental support will not be available. But those who want to and are able to live independently of their families as young adults have few places to go.
Group homes are in short supply as are workers who support them.
Typical setups include a private bedroom and bathroom for each resident with shared living rooms and kitchens. Workers staff the group home 24-7 with the level of assistance needed to help residents with activities of daily living.
The Office for People with Developmental Disabilities in Albany provides certified housing support to more than 35,000 people with developmental disabilities statewide. The OPWDD invests more than $5 billion annually to maintain and develop more housing options for people with developmental disabilities.
“Frontline staff, such as direct support workers, are critical to helping people with developmental disabilities reach their goals and be active and inclusive members of our communities, as well as ensuring people’s health, safety and wellbeing,” said Jennifer O’Sullivan, director of communications for OPWDD.
Brittany Jencik, president of Parents Helping Parents Coalition of Monroe County, mothers 21 children, 14 of whom have intellectual and developmental disabilities.
“Professionally, I most often hear ‘Who will care for my child when I’m gone’ and ‘Where will my child live as an adult?’” she said.
“These concerns are very valid and very challenging to find individual solutions, especially given shortages of resources, program cuts and the housing crisis.”
The Arc Ontario in Canandaigua operates 15 residential group homes and supervised apartments. The latter are for people who are capable of living more independently, but still receive oversight and support as needed.
Jenine J. Cleary, senior certified human resource professional and HR director at The Arc Ontario, said that both staffing shortages and availability of appropriate housing impede the organization from opening more facilities.
“Some of our homes are two-story dwellings, which proves challenging based on the accessibility of the individual,” Cleary said. “The state prioritizes individuals for housing. If we have one bed available, they give us a list of the top 50 needs and we determine based on the space available. You’re looking at the ability to accommodate the individual. If we say none of these 50 are available because this is a two-story home and the individual needs accessibility, they send us a new list. We have three open spaces right now, but we’re working through the list.”
As for staffing, the organization has tried to mitigate this difficulty


by cross-training staff so that people who work in a day program could also pick up shifts as needed to support residential individuals, for example. The Arc sends out a group text to let employees know about shifts available.
For people who cannot find placement in a group home or independent living apartment, they simply must wait for an opening.
“Certainly, from the parents’ perspective that they share with me, there’s a high need for placement options for their children and the wait list can be years for them, even when there’s an urgent need,” said Lorna Patanella, pediatric nurse practitioner UR Golisano Division of Developmental and Behavioral Pediatrics. “What I hear is that they are under-staffed, which limits the availability of residential placements for families who need them. We’d prefer to have a home fully staffed with qualified providers than risk someone being placed in a home that’s not fully staffed.”
She thinks that additional funding would help organizations offer more enticing wages and thus hire more employees.
Families who can afford to do so may hire help for their adult children or look at community habilitation and day programs, which work for individuals whose behavior is appropriate in those settings.
“The harder part is for children who have very dysregulated behaviors because of their disabilities,” Patanella said. “They can be aggressive towards themselves and others and that can limit their day program options. Those are families in greater need of residential placement.
“It's frustrating to everyone involved, including clinicians like myself and certainly the families.”
The OPWDD maintains that funding increases and other efforts should improve the situation.
“New York has taken aggressive action over the past several years to counteract the workforce shortage being experienced by OPWDD and our provider agencies, as well as most human services organizations across the country, including enhanced wages and bonuses, professionalization of the workforce and through our #MoreThanWork recruitment campaign,” O’Sullivan said.
The state’s executive budget proposes a 2.1% targeted inflationary increase for all OPWDD providers to further address rising operating costs and cost of care. O’Sullivan said that when added to funding that has been provided since 2022 for cost-of-living increases, rate updates, bonuses and American Rescue Plan projects, the proposals add up to almost $4 billion invested in the developmental disabilities service system over the last four years.
Training support workers is also a big priority to OPWDD, which has been working with SUNY and National Alliance for Direct Support Professionals to offer credentialing and certification to direct support workers.
These efforts “improve retention among staff and professionalizing the career,” O’Sullivan said. “More than 2,000 DSPs and frontline supervisors having earned their national certification — as well as college credits and stipends — in the last year.”
Is the community up to providing needed resources?
Deborah Jeanne Sergeant
People with Down syndrome are living a lot longer.
Research indicates that in 1950 the median life expectancy for someone with Down syndrome was age 4. Life expectancy for someone born with the condition in the 2010s is 58.
Although the availability of abortion in current times allows more women to choose to abort a fetus with Down syndrome, the increase in the number of women delaying pregnancy until their 30s and 40s — a risk factor for Down syndrome — has led to an increase of people with Down syndrome.
Are healthcare providers and the community in general ready to meet their unique needs in middle age and older adulthood?
Many adults with Down syndrome and other developmental delays struggle to find employment.
Kristin Housel, speech language pathologist and director of operations at GiGi’s Playhouse Rochester, said that this can provide an “opportunity for employers looking for good workers.”
“They’re very capable. We just piloted a career development program. With the right support and training, they’d be assets to many businesses,” she added.
Working a job helps bring additional meaning and personal pride to the lives of people with Down syndrome, but during the pandemic, many employment training programs lost workers.
“Some are not as functional or impactful as they should be,” she added. “We should be providing education and support beyond school and academics. That’s the real world. Individuals with Down are very employable. They just need resources and tools. They make take a different route to get there, but they can work jobs.
“Finding something that’s meaningful like volunteering or a paid position that keeps them going helps. You have to keep pushing and having high expectations. Finding the right fit for someone will help them want to be successful.”
She hopes that more businesses start programs to hire and coach people with Down syndrome.
Housing represents another issue. As someone with Down syndrome achieves greater independence, a group home or other arrangement can be an ideal situation. But Housel said that’s an area that “still needs to be addressed” as these homes are lacking in the area.
Because some people with Down

Kristin Housel is speech language pathologist and director of operations at GiGi’s Playhouse Rochester: "Individuals with Down are very employable. They just need resources and tools. They make take a different route to get there, but they can work jobs," she say.
syndrome are outliving their parents, setting up guardians for their care should be a vital part of the parents’ end-of-life planning. Housel said that many parents focus so hard on academics and schooling that they ignore this aspect of planning — and some financial planners neglect to mention it.
Social workers, service coordinator, advocates and navigators may help, but Housel said that they are overwhelmed with people needing guidance.
People with Down syndrome have a few different medical needs than the general population owing to their physical differences. Living longer means that they also have a greater risk for age-related conditions.
“Now that as the population is growing older and is the least funded within the medical field, it’s a place where everyone needs to focus,” Housel said. “There are definitely things that come up like Alzheimer’s, dementia and regression disorder which can happen at any age but does happen in adulthood. Medical research funding is something that needs to be addressed.”


What can people with disability do if they make enough money at a job that makes them ineligible to get SSI money?
By Deborah Jeanne Sergeant
n addition to their everyday challenges, people with disabilities who receive Supplemental Security Income and work must avoid working so much that they exceed the maximum income threshold to receive benefits that they could not afford through employment alone.
The average federal SSI payment in 2025 is $698 and the New York average payment is $659 (state and federal payments are separate in most states). People who make too much would lose those benefits, even if what they earn would not support them.
Drew Richardson, 38, currently works for three human services agencies in the Rochester region. He formerly received SSI for nearly a decade before transitioning off SSI several years ago. Autism made social situations and maintaining employment very difficult. As he developed tools to meet these challenges, he began shifting off of SSI by finding competitive employment in a secure position.
Consulting with a benefits specialist helped him evaluate several scenarios and timeframes for transitioning off benefits, such as how long he could keep benefits once he started accruing above certain income thresholds, his wage per hour and what benefits he would lose. (The benefits specialist is no longer in business.)
In addition to SSI, at that time Richardson received a rental subsidy, SNAP, HEAP, Medicaid and Medicare. He lived mostly independently in a condo and had his driver’s license.
Once he earned more than the threshold, he became ineligible for the rental subsidy, HEAP and SNAP. But he made enough money to support himself thanks to his higher income.
Richardson currently receives Medicaid and Medicare and was recently re certified for SNAP.
However, he no longer receives any SSI.
“For the most part, I have been fairly successful at being competitively employed. However, now I have moved on to a more ‘freelance’ type of field, doing per-diem community habilitation for other adults with disabilities,” Richardson said. “While it’s not a stable 40 hours a week job, it provides me flexibility in my current situation. However, I have to take into account that I have to meet a budgetary threshold in order to pay my bills and provide for myself.
“With adults with disabilities, many receive benefits such as SSI that unfortunately place a limit upon how much an individual may earn before their SSI benefits start being reduced or paused altogether.”
He believes that at the federal level, a few changes could help alleviate the problem, including amending the substantial gainful activity (SGA) amount to reflect the local minimum wage.
“Currently, the SGA amount for SSI is calculated through indexing the national average wage. However, as New York state has a higher minimum wage than what is currently offered federally due to a higher cost of living, this reduces the amount of hours that a person earning SSI can work in a specific timeframe,” Richardson said. “Amending this will allow individuals receiving benefits to work more without having to worry about losing or jeopardizing their federal disability benefits.”
He also thinks that increasing the federal Medicaid asset limit — currently $2,000 — would help, as that has not been changed since 1989, nearly 40 years ago.
“With each passing year, it becomes more and more difficult for individuals with disabilities to qualify for benefits, as inflation is an unfortunate reality of life,” Richardson said. “Amending this to a higher limit, such as $10,000 — and additionally
indexing it to the federal inflation rate — would benefit more individuals with disabilities who wish to become gainfully employed.”
Not everyone is capable of transitioning off SSI like Richardson.
In some situations, individuals will never work more than part-time or at jobs that pay minimum wage.
In fact, the US Bureau of Labor Statistics states that disabled people are twice as likely to work part-time. People with disabilities are typically under-employed. According to the bureau’s 2024 information, 22.7% of people who are disabled have employment compared with 65.5% of those who do not have a disability.
This affects the family of Brittany Jencik, president of Parents Helping Parents Coalition of Monroe County. She mothers 21 children, 14 of whom have intellectual and developmental disabilities. Her advocacy organization helps families navigate the early challenges of suspecting delays, seeing evaluations, receiving diagnoses and putting support services in place.
“I certainly have personal concerns for my children’s futures but also have insight into a broader set of concerns given my role as an advocate,” Jencik said. “Our biggest concerns for our children’s futures are that they are supported in ways that allow them to reach their greatest potential and have the quality of life they deserve.”
She believes this includes employment, as well as hobbies and interests. All people should feel like what they do matters, she said.
But if that employment teeters between too much and not enough income, that’s tough.
One mitigating factor could be obtaining additional training to help young adults acquire employment skills. Among people with developmental disabilities, this could include vocational resources. However, some parents do not take full advantage of these opportunities.
“Unless you’re a knowledgeable consumer, you don’t know what to ask for and what you should be receiving,” said Lorna Patanella, pediatric nurse practitioner at UR Golisano Division of Developmental and Behavioral Pediatrics. “You have to be an advocate for your child if your child can’t advocate for themselves.”
One such resource is The Arc Ontario in Canandaigua. The organization provides a myriad opportunities for people with developmental disabilities to further their employable skills through their pre-vocational programming. This includes training in virtual reality and in a hospitality suite to find employment with a hotel or hospital providing custodial or housekeeping services.
Jenine J. Cleary, senior certified human resource professional and HR director at The Arc Ontario, said that the next step is expanding the training center to include culinary training.
“Once you are involved in our agency, you can go on job exploration ‘flights’ to learn about agriculture or retail,” she said. “It’s great to see the partnerships we have with so many businesses in the community. We offer vocational support in supported employment.”
This includes helping people find work and dispatching job coaches that accompany individuals as they embark on new jobs to assist in reviewing and reinforcing job skills as needed.
“We don’t want that burden to fall on the employer,” Cleary said.
As individuals gain competency, the job coaches reduce their involvement until they are no longer needed.
The Arc also operates Bad Dog Boutique (a dog grooming service and retail store), Northstar Café, Spot On Cleaning Company and FLX Premier Bottling. These businesses provide individuals with employment experience and community involvement.
By Jim Miller
Dear Savvy Senior,
What are the risk factors for kidney disease? My mother died from kidney failure a few years ago at age 75 but didn’t even know she had a problem until it was too late.
Inquiring Daughter
Dear Inquiring,
Anyone who has diabetes, high blood pressure, heart problems or has a family history of the disease is at increased risk for chronic kidney disease, a condition in which the kidneys can no longer effectively filter your blood.

According to the Centers for Disease Control and Prevention, around 37 million U.S adults have chronic kidney disease, and millions more are at risk of developing it, yet most people don’t realize it.

That’s because kidney disease develops very slowly over many years before any symptoms arise. But left untreated, the disease can even tually require people to spend hours hooked up to a dialysis machine or get a kidney transplant. Even mild kidney problems can double a per son’s risk of heart attack and stroke, as well as cause anemia and bone disease.
your

ARBs are good choices because of their proven ability to protect the kidneys.
• Control your diabetes: diabetes, keep your blood sugar as close to normal as possible. Diabetes medications called SGLT-2 inhibi tors have also shown to be effective in helping slow the progression of kidney disease, even in non diabetic

The reason kidney disease has become so widespread today is because of the rise of obesity, Type 2 diabetes and high blood pressure which all strain the kidneys.
Another factor is the increasing number of people who take multiple medications, which can overtax the organs. People over age 60 are especially vulnerable both because they tend to take more drugs, and because kidney function normally declines somewhat with age.

Because kidney disease is often symptomless, it’s usually undiagnosed. The only way to catch it before it advances is to have a routine blood and urine test by your doctor. So, anyone that has diabetes, high blood pressure or heart disease, or is age 60 or older needs to be tested annually.

If your lab tests show a decline in kidney function for more than three months in a row, you might be diagnosed with kidney disease and referred to a nephrologist. You also need to know that while kidney damage cannot be reversed, there are a number of effective lifestyle steps and treatments that can help contain the damage, including:

Adjust your diet: ly means reducing the amount of protein and phosphorus you eat and cutting back on sodium, sugar and possibly potassium. Your doctor can help you determine an appropriate eating plan, or you may want to talk
• Watch your meds: Dozens of commonly used drugs can damage the kidneys, especially when taken in high doses over long periods — most notably NSAIDs like ibuprofen and naproxen. Proton pump inhibitor (PPI) medications taken for heartburn and GERDS, and herbal supplements can also be problematic. Talk to your doctor about all the prescription, over-the-counter and herbal products you take to identify potential problems and find alternatives.
• Exercise and lose weight: If you’re overweight and inactive, start an aerobic fitness routine (walk, swim, cycle, etc.) that gets your heart pumping. This will help lower blood pressure, control diabetes and help you lose excess weight all of which will help your kidneys.

• Control your blood pressure: If you have high blood pressure, get it under 130/80. If you need medication to do it, ACE inhibitors and
Stay hydrated: Dehydration can affect kidney function, so try to drink at least six to eight 8-ounce glasses of
Quit smoking: If you smoke, quit. Smoking damages the kidneys and doubles the rate of progression to end-stage renal failure.

Send your senior questions to: Savvy Senior, P.O. Box 5443, Norman, OK 73070, or visit SavvySenior. org. Jim Miller is a contributor to the NBC Today show and author of “The Savvy Senior” book.













By Colleen Holcomb
When we hear the word “volunteering,” we think of helping others. That's certainly true, and it's the primary reason people choose to volunteer. But new research shows that people who volunteer are also helping themselves in extraordinary ways.
Studies show that serving others provides mental health benefits including increased happiness and a decrease in depression and anxiety. Scientifically speaking, this is the result of our bodies releasing serotonin, dopamine and endorphins: the body's “feel-good hormones.”
Volunteering is also connected to better physical health: lower stress, lower blood pressure and reduced rates of heart disease, stroke and general illness, all of which contribute to a longer life.
Cathy Quinn has been volunteering at St. Ann's Home for 23 years, starting right after she retired. “I got in and got hooked,” she says.
Most recently, she's been the “prize lady” at bingo and a clue reader at crossword puzzle sessions with residents. She also helps transport people to and from activities. “For someone who's retired, it's a little bit of exercise,” she says. “That's how I get my steps in!”
Like other volunteers, Quinn cites numerous benefits.
“It gets me out of the house, and I look forward each week to seeing the friends I've made among residents, staff and other volunteers. It just makes me happy,” she says. “You get to know the residents as real people, not just 'old people.' They've got real stories, real families, real accomplishments. It's interesting and rewarding to know them on that level.”
Like Quinn, many of our volunteers are community volunteers — retirees and young people alike! These volunteers are individuals who help elders with activities, assist at parties, support our pastoral care program with lecturing, share their hobbies, or spend one-on-one time with elders during visits. Opportunities can be tailored to the volunteers’ interests and schedules.
Organizations and student groups are also actively involved with St. Ann’s Community. M&T Bank has been supporting St. Ann's elders for several years in a variety of ways. Recently, employees made and delivered 650 valentines, one for every elder. They were also on hand at Christmastime, helping deliver presents. This type of connection helps our elders feel seen and cared for and contributes to their quality of life.
When student groups from grade schools and local universities volunteer, they not only bridge the generational gap but also experience personal growth and emotional benefits. One student, whose grandmother had recently moved into a

skilled nursing community, found that engaging with the elders at St. Ann’s reduced her anxiety and fear about her grandmother’s move. This positive interaction improved her well-being and confidence, leading her to ask her mom, “When we visit Grandma, can we bring games to play with her?” At St. Ann's, we offer pre-scheduled volunteer days, perfect for students seeking to fulfill community service requirements.
It also contributes to the volunteers' own emotional and spiritual well-being. They enjoy a sense of purpose and appreciation, both given and received, by taking part in a cause larger than themselves.
The social interaction involved satisfies a basic human need and reduces isolation, loneliness and alienation. Volunteering allows us to develop empathy, meet new people, and bond with others who share our interest in giving back to the community.
I often tell people that volunteering with elders differs from other types of volunteering because it offers instant gratification. You can see the impact immediately. That's a great feeling, one which has multiple benefits for both giver and receiver.

at cholcomb@ mystanns.com.
April 10
Medical society to host wellness symposium for health professionals, students
The Monroe County Medical Society will host a Wellness Symposium from 12:30 to 5:30 p.m., April 10, at the Rochester Academy of Medicine at 1441 East Avenue, Rochester.
The symposium on human-centered wellness, titled “You Can’t Stop the Waves but You Can Learn to Surf,” is desgned for physicians, advanced practice providers, medical residents/students, nursing and all healthcare workers.
“The Monroe County Medical Society is committed to fostering the well-being of our members and the communities we serve. This wellness symposium serves as a vital platform to explore innovative strategies and collaborative efforts aimed at enhancing wellness across the Finger Lakes region”, said Monroe County Medical Society CEO Lucía Castillejo.
The focus will be for attendees to learn how clinician and health team wellbeing support all aspects of the Quintuple Aim, which includes better outcomes, advancing health equity, improving patient experience,
lowering costs, and helping caregivers to thrive. Presentation topics will include: “A Health System Perspective on Burnout in Academic Health Care,” “Peer Support for Second Victims in the Healthcare Setting,” “AI and Wellness-Centered Leadership” and more.
“When we prioritize clinician wellbeing, we strengthen every pillar of the Quintuple Aim, leading to better care for both healthcare workers and patients. This symposium is a vital step toward a healthier, more sustainable future for our medical community,” explains MCMS President Janine Fogarty, M.D.
Ticket prices range from $0 to $75. Sponsors of the event include the Rochester Academy of Medicine, Rochester Regional Health, University of Rochester Medical Center and Tend Health.
To reserve your tickets, please visit www.mcms.org/event-6083437
Save-the-date for the 18th Annual Embrace Your Sisters (EYS)
Fashion Show Fundraiser, which will take place at 2 p.m. Sunday, May 4, at Casa Larga Vineyards & Winery in Fairport. Doors open at 12:30 p.m.
The fashion show is one of two annual events which are coordinated by the volunteer EYS board members to raise money in support of breast cancer patients across Monroe County and the neighboring 12 counties, providing them with short-term emergency funding.
• In Person: A critical mass of attendees makes the silent auction, liquor and wine pull in handcrafted bags, jewelry, music, appetizers, desserts, beverages, speakers and, of course, the runway fashions, even more enjoyable. Buy your ticket or a table of 10 at www.embraceyoursisters.org.
• Online Silent Auction: For all interested participants, the online silent auction will open for public online viewing of the product and service items. Schedule: April 30, noon: the online silent auction will open for public viewing of the product and service items. May 3, 2 p.m., online bidding begins. Register at: https://e.givesmart.com/events/ Gkq/
Join DePaul’s National Council on Alcoholism and Drug Dependence – Rochester Area (NCADD-RA) for its annual luncheon from 11:30 a.m. to 2 p.m. on Wednesday, May 21, at the DoubleTree by Hilton at 1111 Jefferson Road in Rochester. Keynote
speaker Bertha Madras, a professor of psychobiology at Harvard Medical School, will present “Marijuana and Psychedelics: Essential Facts Everyone Should Know.”
Madras’ research has focused on neurobiology, pharmacology, brain imaging, drug discovery for addiction, neuropsychiatric disorders and drug policy. She is author of over 200 scientific manuscripts, articles, book chapters and co-editor of books involving addiction, the effects of drug abuse on the human nervous system and including “The Cell Biology of Addiction, Effects of Drug Abuse on the Human Nervous System, Imaging of the Human Brain in Health and Disease.” Madras is a recipient of 19 U.S. and 27 international issued patents with collaborators.
The NCADD-RA provides research-based and evidence-based substance use disorder and problem gambling prevention services to a diverse population through education, support, resources, advocacy and referral.
NCADD-RA staff provide community education and awareness presentations on a variety of addiction-related topics tailored to requesting school or community groups. NCADD-RA also provides a wide array of training opportunities for professionals in the addictions, education, and health and human services community.
For more information visit https://ncadd-ra.org/wp-content/ uloads/2025/01/2025-NCADD-RALuncheon-Registration-Rev-1-13-25. pdf. To register for the NCADDRA’s annual luncheon by May 7, click https://ncadd-ra.org/register-for-the-2025-annual-luncheon.
At Hematology-Oncology Associates of CNY, you are never just a diagnosis or a number. We see you...the whole person, with passions, hopes, dreams, histories, and loved ones who share in your journey. From diagnosis, to treatment, to survivorship – our personalized care focuses on truly understanding and planning for your unique needs. We provide genuinely compassionate support, collaborating with you, your family, and caregivers every step of the way. Learn more about HOA today. We’ll see you and care for you – body, mind and spirit.



You may be able to get Supplemental Security Income (SSI) even if you already receive Social Security benefits.
About 2.5 million adults and children get SSI and Social Security at the same time.
We pay Social Security benefits to workers and their eligible family members based on the worker’s earnings. SSI is a needs-based program that provides payments to people with little or no income and few resources.
People younger than 65 must be blind or have a disability and meet SSI income and resource limits, while people 65 and older do not have to have a disability. About 1.4 million people 65 and older receive both SSI and Social Security.
What do we mean by “little or no income”?
In 2025, you may be eligible for SSI if your total income — including your Social Security benefit — is less than $987 per month (the 2025 SSI monthly federal benefit rate plus $20).
We consider income from all nonwork sources, including pensions,
Q.: What is the estimated average Social Security payment that a person receives each month?
A.: The estimated average monthly Social Security benefit for a retired worker in 2025 is $1,976.00. The average monthly Social Security benefit for a worker with a disability in 2025 is $1,580.00.
Q.: Why should I sign up for a personal My Social Security online account?










A. My Social Security is a personal online account you can securely use to check your Social Security information and do business with us. With a personal my Social Security account you can:
• Keep track of your earnings and verify them every year.
• Get an estimate of your future benefits if you are still working.
• Request a replacement Social Security card in most states.
• Get a letter with proof of your benefits if you currently receive them.
veterans’ benefits, unemployment and Social Security disability, retirement and survivor benefits. We also count some — but not all — earnings from work, including self-employment.
What do we mean by “few resources”?
Resources are things that you own that you could change to cash and use to support yourself. They include vehicles (if you own more than one) and money in bank accounts, stocks and bonds. We do not count your home and the land it’s on, as long as you live there. To be eligible for SSI, your resources cannot be worth more than:
– $2,000 for a single person.
– $3,000 for a married couple living together.
For more information visit our blog article, You May Be Eligible for SSI and Social "Security Benefits" at blog.ssa.gov/you-may-be-eligible-for-ssi-and-social-security-benefits.
Please share this information with others who may benefit – and post it on social media.
• Manage your benefits:
– Change your address or telephone number. (Social Security beneficiaries only)
– Start or change your direct deposit. (Social Security beneficiaries only)
– Get a replacement Medicare card.
– Get a replacement SSA-1099 or SSA-1042S for tax season.
To find all the services available and set up an account, go to www. ssa.gov/myaccount.
Q.: I plan to retire soon. When are Social Security benefits paid?
Social Security benefits are paid each month. Generally, new retirees receive their benefits on either the 2nd, 3rd, or 4th Wednesday of each month, depending on the day in the month the retiree was born. If you receive benefits as a spouse, your benefit payment date will be determined by your spouse’s birth date. Here’s a chart showing how your monthly payment date is determined:








By Deborah Jeanne Sergeant
Although physical therapists treat patients of all ages, American Physical Therapy Association states that many physical therapy patients (36.1%) are older than 65.
As that cohort of the population increases, it’s clear that the demand for physical therapists isn’t going down anytime soon.
“It’s one of the more growing careers,” said Maureen Loyal, physical therapist and director of rehabilitation and physical therapy for Finger Lakes Health. “The population is aging and we treat a lot of older folks.”
Falls and other injuries, deconditioning from hospital stays and recovery from surgeries are among the top reasons many older adults need physical therapy.
Loyal has worked as a physical therapy supervisor for 25 years, mentoring young physical therapists and teams.
In addition to treating older patients, physical therapists treat athletes and children with motor delays in schools, and “weekend warrior” adults in clinics. They also
work in home health, delivering care to people recovering from surgery or injury and in long-term care facilities to help “keep folks functionally mobile and safe,” Loyal said. “Having physical therapy in your house can help keep you mobile there. That’s a great place to work.”
Physical therapists who travel to clients’ homes can better assess their daily living environment for safety and tailor exercise regimens that use familiar items they already own. They can address the particular challenges their homes present, such as front steps, a dimly lit hallway or an uneven floor.
Physical therapists “assess, plan, organize and participate in rehabilitative programs that improve mobility, relieve pain, increase strength and improve or correct disabling conditions resulting from disease or injury,” states the Bureau of Labor Statistics.
Loyal felt drawn to the profession of physical therapy as a young athlete. She experienced knee surgery which required subsequent physical therapy. She appreciated the efforts

By Deborah Jeanne Sergeant
After learning about occupational therapy while a freshman in college, Kelly Christensen, now an occupational therapist for Finger Lakes Health, knew that was the career path for her.
“I love having the opportunity to help people achieve even the smallest milestone,” she said.
At Finger Lakes Health, the organization offers short-term rehabilitation, long-term care and out-patient rehabilitation. In each of those areas, occupational therapists can help patients strategize ways to use their arms and hands to complete activities of daily living (ADLs), especially those related to self-care.
“We look at what’s needed for that individual to return home,” she said.
In general, occupational health

of her physical therapist and felt she also wanted to “help get people back to their life,” Loyal said.
She has always worked in a hospital or acute setting. Many of her patients have had strokes or amputations.
“Getting those folks so they will get over that mentally and physically and get them mobile and home again has been so rewarding,” Loyal said. “You’re helping people and also you have to challenge your mind to have a successful outcome.”
She likes that physical therapists have direct access so that most insurance companies do not require a referral from a physician and will cover 30 days or 10 visits, whichever comes first.
“Having that autonomy, we should be able to in the future order MRIs,” Loyal said.
with them is helpful.”
The career requires a master’s level education and doctorate and post-professional doctorate programs are also available.
Julie Kunisch, a doctor of occupational therapy, clinical associate professor and chairwoman and program director of the department of occupational therapy at Nazareth University, noted that the Bureau of Labor Statistics foresees that occupational employment is expected to grow “faster than average” and that “U.S. News & World Report named OT No. 4 in the best healthcare careers.”
She believes that the aging population represents a key reason for this expansion. People want to remain independent and at home as they age and OT can help. The higher awareness of mental health is also fueling this growth.
Physical therapists must earn a doctorate degree before sitting for licensing exams.
“The rationale is to have evidence-based practice to use research to show what we do is valuable and to do the best things to help patients,” Loyal said.
According to the Bureau of Labor Statistics, the annual mean wage for a physical therapist in the Rochester area is $83,130.
A physical therapist in the Rochester area makes an annual mean salary of $83,130, according to the Bureau of Labor Statistics.
greater ability to live independently.
“As these trends continue to evolve, the demand for OTs is expected to keep growing, making it a dynamic and rewarding career,” Kunisch said.
She has been working in the field since 1996 and finds it fulfilling because of “the overall meaningful impact of the work and the personal rewards of the profession. OTs make a direct difference by helping others regain independence, improve their quality of life and achieve their goals which is highly rewarding.”
She also likes that occupational therapy is a dynamic field in which practitioners continuously learn and adapt to new research, techniques and technology.
can serve patients from youngsters in early intervention through end-of-life care.
Although this sounds a lot like physical therapy, occupational therapy looks at what is important to the individual for completing activities of daily living and the hobbies and occupation important to the person: functional skills.
“The profession is great for those looking to help someone,” Christensen said. “There’s a component of teaching too, so we’re often teaching a new way to do a skill. The ability to talk with people is important. And the ability to form relationships. When people are at their worst or lowest is when we’re helping them. Something hard has happened to them. We’re working with them in a vulnerable space. Being able to bond
“OTs are essential mental health providers and can help people develop coping strategies to engage in meaningful activities,” Kunisch said. “More and more people are living with chronic conditions and disabilities. OTs are experts in promoting independence using adaptive strategies and environmental modifications.”
The healthcare world is also shifting to a prevention and early intervention model. Kunisch views OTs are important for these emphases. As holistic practitioners, they treat the whole person, not just the aspect of their health that hampers their ability to function independently.
In addition to aiding young children and older adults, OTs also work with people of all ages who have injuries and disabilities. Because medical technology has advanced to allow more people to live, OTs can help rehabilitate patients and foster a
“This professional growth and opportunities to specialize in different areas like pediatrics, mental health, hand therapy and geriatrics support a fulfilling career,” Kunisch said. “OT is fulfilling work because it allows practitioners to make a profound impact on people’s lives, fosters meaningful relationships, offers variety and professional growth and provides meaningful rewards from seeing tangible improvements in people’s wellbeing and quality of life.”
According to the Bureau of Labor Statistics, the annual mean wage for an occupational therapist in the Rochester area is $82,960.
A occupational therapy in the Rochester area makes an annual mean salary of $82,960, according to the Bureau of Labor Statistics.
Hybrid Nurse Aide Training Program
Hybrid Nurse Aide Training Program ELEMENTAL MANAGEMEN OUP
Hybrid Nurse Aide Training Program ELEMENTAL MANAGEMENT GROUP















MANAGEMENT GROUP



Equip your facility with our unstoppable HYBRID CNA program, empower your team to deliver top-notch care with the strength of a champion.
Equip your facility with our unstoppable HYBRID CNA program, empower your team to deliver top-notch care with the strength of a champion.
Equip your facility with our unstoppable HYBRID CNA program, empower your team to deliver top-notch care with the strength of a champion.
Are you looking for an innovative way to attract CNA students? We have your answer
Are you looking for an innovative way to attract CNA students? We have your answer
Are you looking for an innovative way to attract CNA students? We have your answer
Are you looking to minimize and most importantly eliminate agency use? We have your solution
Are you looking to minimize and most importantly eliminate agency use? We have your solution
Are you looking to improve morale by increasing your direct care PPD? Reach out to us to hear more
Are you looking to minimize and most importantly eliminate agency use? We have your solution
Are you looking to improve morale by increasing your direct care PPD? Reach out to us to hear more
Are you looking to improve morale by increasing your direct care PPD? Reach out to us to hear more
Are you looking to captivate and motivate the newer generation by offering unique and rewarding training opportunities? Look no further contact us today
Are you looking to captivate and motivate the newer generation by offering unique and rewarding training opportunities? Look no further contact us today

Are you looking to captivate and motivate the newer generation by offering unique and rewarding training opportunities? Look no further contact us today

CONTACT:

Peg Reith BSN, RN
CONTACT:
Phone: 315-529-3267
Peg Reith BSN, RN
Email: CNA_Training@elementalmgt.com
CONTACT:
Phone: 315-529-3267
Email: CNA_Training@elementalmgt.com
Peg Reith BSN, RN
Phone: 315-529-3267
Email: CNA_Training@elementalmgt.com