










Type 2 diabetes increased by nearly 20% in the United States between 2012 and 2022, with age, race, income level, obesity and lack of exercise all playing a role in the metabolic disease’s spread, a new study reports.
“Diabetes is increasing day by day in the U.S., and it will increase even more in the coming years,” said lead researcher Sulakshan Neupane, a doctoral student with the University of Georgia’s College of Agricultural and Environmental Sciences.
“Diabetes costs around $412
billion, including medical costs and indirect costs like loss of productivity,” Neupane added in a university news release. “That’s a huge amount, and it’s only going to increase as more people are diagnosed.”
Age is a major factor, with middle-aged people and seniors carrying a much higher risk of Type 2 diabetes, researchers found.
Seniors aged 65 and older were more than 10 times as likely to be diagnosed with diabetes as people aged 18 to 24, results show. Middle-aged folks 45 to 64 were more



than five times as likely to get such a diagnosis.
Income and education also played a role. People with high incomes were 41% less likely to develop Type 2 diabetes, and the college-educated were 24% less likely.
Black people were the racial and ethnic group hardest hit by diabetes, with just under 16% diagnosed with the disease, researchers said.
The South and Midwest in particular experienced large jumps in Type 2 diabetes cases, with Arkansas, Kentucky and Nebraska reporting
the highest increases.
In all, 10 states experienced increases of 25% or more — Arkansas, Kentucky, Nebraska, Texas, Alabama, Minnesota, Illinois, West Virginia, Delaware and Massachusetts.
“In these areas, people are at higher risk of developing diabetes, so policymakers and public health officials need to focus on these regions,” Neupane said.
For the study, the researchers analyzed data from an ongoing national health survey of more than 400,000 people conducted by the U.S. Centers for Disease Control and Prevention.
Unsurprisingly, overweight and obese people were found to be at higher risk of Type 2 diabetes, the data show.
About 1 in 5 obese people and 1 in 10 overweight people had Type 2 diabetes in 2022, researchers found.
Physical activity seemed to provide effective protection against diabetes, results show. Just under 10% of physically active people reported having Type 2 diabetes, versus a rate closer to 19% among people who are inactive, the study found.
The new study was published recently in the journal Diabetes, Obesity and Metabolism.
“Identifying these risk factors and acting to mitigate them is key,” Neupane said. “Be more active. Pay more attention to your physical health. Some risk factors like age and race cannot be modified, but you can do something to lower risk of diabetes, like healthy eating, maintaining an active lifestyle and losing weight.”
Editor’s Note: Read the Savvy Senior column in this issue for more information on diabetes.





By Chris Motola
Joshua J. Mauro, M.D.
ICU doctor at Thompson and Strong recalls experience in medical school in Australia, discusses scope of his work. “We live by the mantra ‘quick on, quick off,’
so we're fast acting but also can stop acting quickly if we need to adapt"
Q: You recently received a Shining Star Award from FF Thompson Hospital.
A: The Shining Star Award is an award given out by FF Thompson Hospital based on feedback from colleagues and patients and their families. So it was a super special honor to receive that award.
Q: What kind of feedback were you getting?
A: I had no idea, so it was a complete and utter surprise. I was actually told that one of my colleagues was getting a nomination and was super thrilled for her. I was on vacation but happened to be in Rochester still. So one of my colleagues reached out and said, “Hey,
Q: You're a member of the ICU team at FF Thompson.
A: Yes, I'm one of the attending physicians in the intensive care unit. I work at FF Thompson and also the medical ICU at Strong [Memorial Hospital]. It's a bit more subdivided at Strong.
Q: What kind of duties do you have in intensive care?
A: Either you get admitted directly to the ICU from the emergency department or you get transferred in from an outside facility. Some of the hospitals in our system, even outside of our system, in the southern region may have an intensive care unit, but they may have only one or two beds and may focus on keeping
an intensive care unit, but it's not always staffed by an ICU provider or the ICU provider may not be onsite full time. So it's either a consultant or a hospitalist-attending who admits someone to the ICU. And what those ICUs are is you'll stay under the same physician, but there's a higher nursing ratio, around two patients per nurse. At FF Thompson and Strong, on the other hand, our ICUs are staffed exclusively by intensive care physicians. It's what we call a closed ICU. We do have consultants, but at the end of the day we are the primary team for the patient.
Q: What do patients admitted to your ICUs typically present with?

A: We see a lot COPD exacerbations, heart failure exacerbations. Basically anything where a patient needs to be on BIPAP or a ventilator. If someone presents with sepsis or septic shock they generally come to us. Basically anything in the hospital that requires closer monitoring or frequent changes to the care. Because we have the closer nursing ratio and the smaller patient load we can be a bit more nimble and react quickly to changes in the patient's condition. We live by the mantra “quick on, quick off,” so we're fast acting but also can stop acting quickly if we need to adapt. We do a lot of medications that are drips, meaning that it's a slow infusion. We can increase or decrease the amount going in at intervals of one to two minutes as opposed to on the floor where, if a nurse has eight patients, they're not going to be able to do that. That's not to say they're bad nurses; that's just how the hospital system works to triage resources to the patients that are the sickest.
Q: You did some of your medical training Australia. What was that like?
A: I went to medical school in Australia. I grew up in Rochester. I am American. I went to undergrad at North Carolina State University. After that I was deciding between going into medicine or bioengineering. So I was applying to medical schools and wasn't thrilled about
the interviews I was getting. One of my mentors from undergrad was a physician who was diagnosed with something called retinitis pigmentosa when he was in his late 20s. He was a bit of an adventurer. With this disease, you generally progressively go blind over the course of 10 years. So he had to decide what he was going to do with his life: either travel around seeing everything he could see or settle down, have a family and dig in to setup. He actually opted for the former and traveled the world. He ended up working in the outback in Australia. He loved the culture, the people, made a lot of lifelong friends. So when I was applying, he said, “You know Josh, you seem like you're always up for an adventure and trying something new. You should consider Australia. It's not a third world country, they have resources, they speak English. It's a challenge, but probably right up your alley.” I applied and got in and was fortunate that I found a new program that had just started through the University of Queensland where you do your first two years in Australia and your rotations in New Orleans. So I lived in Australia for two years and did my clinical clerkships in New Orleans, with a return rotation in Australia. It was a great experience, but I knew I wouldn't be practicing in Australia. It was too far away from family.
Q: What were some of the key differences between Australia and the U.S. in terms of medicine?
A: It's a different health system with a greater focus on preserving resources because there's a much greater social aspect to their healthcare. In the United States we tend to have a shotgun approach of testing for everything and gathering as much data as possible and then deciding what's going on as opposed to Australia where it's more try, learn what you can, order a test if you think it will really make a difference and, if not, don't do it. I think one thing we can suffer from here is data overload. We have a saying that “the patient didn't read the textbook.” So we may have a diagnosis, but the patient isn't experiencing it as a textbook case. Very rarely does everything line up perfectly.
Name: Joshua J. Mauro, M.D.
Position: Critical care physician at URMC
Hometown: Rochester
Education: University of Queensland Medical School
Affiliations: FF Thompson
Hospital, Strong Memorial Hospital, URMC system
Organizations: American Board of Internal Medicine, AAMC Family: Wife, two children
Hobbies: Cars, making his kids laugh
Afew cups of coffee each morning can help protect a person against heart disease, stroke and Type 2 diabetes, a new study says.
Drinking three cups of coffee a day — or about 200 to 300 milligrams of caffeine — lowered the risk of health problems linked to the heart or metabolism, researchers found.
“The findings highlight that promoting moderate amounts of coffee or caffeine intake as a dietary habit to healthy people might have far-reaching benefits,” said lead researcher physician Chaofu Ke, a medical statistician with Suzhou Medical College of Soochow University in China.
For the study, researchers analyzed data on more than 500,000 people aged 37 to 73 participating in the long-term U.K. Biobank research project.
Out of that group, they identified more than 172,000 people who’d reported their caffeine intake, and another 188,000 who’d reported their coffee or tea consumption.
The researchers compared people’s caffeine intake to whether they had developed two or more signs of cardiometabolic disease. That term relates to risk factors that can harm heart health, such as diabetes, high cholesterol, high blood pressure and excess body weight.
Results showed that any level of coffee or caffeine intake lowered a person’s risk of suffering multiple


health problems related to heart or metabolism.
But the best results came with moderate intake of coffee or caffeine, they found.
People who drank three cups of coffee a day had a 48% lower risk of heart or metabolic disease, compared to those who drank no coffee.
And those who got 200 to 300 milligrams of caffeine daily had a 41% reduced risk compared to those who consumed none or less than 100 milligrams, researchers found.
The new study was published Sept. 17 in the Journal of Clinical Endocrinology & Metabolism.
Any lower risk would help protect a person’s health, as people with heart or metabolic diseases are four to seven times more likely to die from any cause, researchers said in a journal news release. They also have higher risk of disability and mental stress.


A monthly newspaper published by Local News, Inc. Distribution: 33,500 copies throughout more than 1,500 high-traffic locations.
In Good Health is published 12 times a year by Local News, Inc. © 2024 by Local News, Inc. All rights reserved. P.O. Box 525, Victor NY 14564. Phone: 585-421-8109 • Email: Editor@GVhealthnews.com
Editor & Publisher: Wagner Dotto • Writers: Deborah J. Sergeant, Chris Motola, George Chapman, Gwenn Voelcker, Anne Palumbo, Jim Miller, Mike Costanza
Maggie Fitzgibbon, Albert S Hartel (MD), Shaina Zazzaro, Grace R. Scism
Advertising: Anne Westcott (585-421-8109) • Linda Covington (585-750-7051)
Layout & Design: Angel Campos–Toro • Office Secretary Allison Lockwood
No material may be reproduced in whole or in part from this publication without the express written permission of the publisher. The information in this publication is intended to complement—not to take the place of—the recommendations of your health provider. Consult your physician before making major changes in your lifestyle or health care regimen.





By George W. Chapman

The CDC still recommends we get the updated vaccine, but advises us to not jump the gun and wait until later fall.
The protection afforded by the vaccine wanes after a few months so you don’t want this to hap-

The vote in the Senate to pass the Inflation Reduction Act, which authorized Medicare to finally negotiate drug prices on behalf of its 40 million mem- bers, passed by just one vote. Not one Republican voted to pass the IRA. Not one. Vice president Harris had to cast the deciding vote. However, the “good” news is that both presidential candidates are in favor of controlling drug prices. Consequently, drug manufacturers have hedged their bets. Historically, prior to the IRA, the drug lobby has fended off all attempts by Medicare to negotiate prices. While most of our elected representatives on both sides of the aisle accepted money from drug lobbyists, three to four times more money went to Republican reps than Democratic reps. This year, however, total contributions to members of the two parties are just about even.
Over the past several decades, drug costs have increased from 3% of the total cost of care to almost 10% of the total cost of care. The trend can be attributed to our increasing dependence on drugs (most per capita in the world) and to unregulated
pen during winter months when COVID-19 tends to peak. Thankfully, as more of us are immunized, deaths and hospitalizations are rarer. There were about 2,000 COVID-related deaths this past July compared to 26,000 deaths in July 2020. Virol-
costs versus physician and hospital costs which are set. GLP-1 drugs used to treat diabetes and weight like Ozempic, Jardiance and Wegovy are having a significant impact on our premiums and copays be they Medicare, commercial or private or on the government exchange. Any of these drugs could be on Medicare’s “hit list” for 2026 but will remain uncontrolled for private insurers. 57 million people or 40% of those covered by their employer could potentially be eligible for GLP-1 drugs. The eventual economic impact on premiums and copays for employees will ultimately be determined by the plan your employer selects and by arbitrary coverage limitations. Initially developed to treat diabetes, only 5% of GLP-1 drugs are prescribed to treat just diabetes. Forty-two percent of these drugs are prescribed to treat obesity. The balance of prescriptions are for other conditions. Medicare spent $57 million on GLP-1 drugs in 2018. Spending jumped to a staggering $5.7 BILLION in 2022, due to a combination of price gouging and treatment of obesity. Employees, unfortunately, are virtually locked into the plan their employer selects and are subject to whatever drug coverage attached to that plan. On the other hand, Medicare beneficiaries and those on the government exchange can use navigators to help them find a plan with the best
ahead of the game but lifted a ban in 2015. As with regulating drug costs, fortunately, both political parties are in sync when it comes to the negative impact of smartphones on student mental health and that something has to be done. Overlooked if not lost in the discussion surrounding the impact of smartphones on students is the impact on teacher morale and retention especially in districts serving predominantly underprivileged students.

ogists suggest the current variant may be less virulent this year, but still recommend getting vaccinated. Waste water analysis shows that, currently, COVID is worse in western and southern states. The CDC recommends annual updated shots because of the ever-evolving variants.
coverage of a particular drug they are on. CMS has granted $100 million to navigators who can assist seniors select an advantage plan or individuals not covered at work select a plan on the exchange.

There is little disagreement among parents, teachers and legislators that smartphones have negatively impacted student learning, student mental health and even teacher retention. Student cyber bullying, loneliness, anxiety, depression, body dissatisfaction, eating disorders have approached epidemic proportions. Numerous studies found 50% of all students spend more than four hours a day on their phone. It’s basically an addiction and rehab will not be easy. 90% of schools report cyberbullying and 40% report the negative impact on learning when smartphones are unchecked. Seven states have banned smartphone use in schools with some exceptions for emergencies. They are Florida, Indiana, Louisiana, Minnesota, Ohio, South Carolina and Virginia. It is too soon to draw conclusions, but it is still worth gathering evidence. Once results are in, implementing any kind of restriction or total ban will be difficult. Teachers now have to worry about guns and cell phones. New York state was way
By 2030, just six years from now, 42 of our 50 states will face a severe nursing shortage. Interestingly, of the eight states that expect to be alright, six are in the northeast: Vermont, Rhode Island, Maine, Pennsylvania, Connecticut and New Hampshire. Rural hospitals are most vulnerable to a shortage of nurses which can be a major factor leading to an outright closure. About 300 rural hospitals are on the brink. 10% are in Texas and Kansas, both states with large rural populations. The closure of a rural hospital, many hundreds from the nearest hospital, impacts far more than access to acute care. More than likely, unless affiliated with or supported by another healthcare system, physicians, pharmacists and other health professionals may abandon the community as well. The lack of a local hospital will also impact schools and local businesses. The local chamber of commerce will have a difficult time attracting new businesses. Half of nurses leave their job within two years as compared to four years for all industries. A study of 50,000 nurses found that on any given day, more than half of all nurses feel a sense of depletion, emotional exhaustion or fatigue. The double whammy of the pandemic and our aging population has exacerbated the shortage. Thousands of applicants to nursing schools have to be rejected every year because there are not enough professors in the schools to teach. Since the pandemic, most health care providers (well, the smart ones anyway) are much more attuned to their cultures, working environment and stresses facing their staff. Hopefully resulting in far less turnover and dissatisfaction. Nurse salaries have increased considerably since the pandemic. Nursing schools are receiving subsidies helping them attract and retain professors. Finally, 18% of healthcare workers are immigrants. Legal immigrants. That’s almost one in five employees. So, as in many other industries, staff shortages would be FAR worse without the steady flow of immigrants.

George W. Chapman is a healthcare business consultant who works exclusively with physicians, hospitals and healthcare organizations. He operates GW Chapman Consulting based in Syracuse. Email him at gwc@gwchapmanconsulting.com.

By Maggie Fitzgibbon
Litter. Unfortunately, it’s everywhere.
The Walking for Rochester organization aims to eradicate this problem and educate people on the benefits of caring for their community.
Matt Apple, the CEO and one of the three co-founders of Walking for Rochester, shares how this group came to be.
“In 2017, I had meetings with friends to discuss the idea of developing an organization that would focus on making a change by cleaning up our community,” Apple explained. “When the pandemic hit and many people were unemployed or working from home, this was an opportunity for people to get out of the house and volunteer to clean up neighborhoods.”
Together three like-minded individuals, Apple, Michael Carroll and Zakary Martinescu, set out to make a change for the better. Walking for Rochester was incorporated in 2020 as a 501(3)(c) organization. The group takes a systemic approach to how it functions.
Walks are held twice a week, weather permitting, from April until Sept. 30. Volunteers meet at an assigned location, register and sign a
waiver before walking. Each person has gloves, grabbers, buckets and garbage bags. Walkers are encouraged to log in to the Walking for Rochester mobile app to verify and track volunteer hours.
“Community cleanups take place for about one hour. You can volunteer for one hour or attend as many of our scheduled clean-ups that fit your schedule,” Apple said.
At least two local businesses sponsor each community cleanup. Each sponsor provides monetary support and gift cards. The gift cards are raffled at the end of each cleanup. Monetary sponsorships and other donations help finance the cost of protective equipment and other organization needs, such as the development and maintenance of the Walking for Rochester mobile app.
Community cleanups currently focus on the city of Rochester neighborhoods.
Apple explained the reason.
“Our efforts are concentrated on the greatest areas of need, primarily the southeast area. However, we are planning to expand our areas,” he said.
What happens to this collected trash? A partnership with the city of Rochester makes trash disposal easy.


City sanitation workers are helping to keep the community clean by picking up the trash collected at the Walking for Rochester community cleanups.
Corporate cleanups and volunteer programs are also programs that Walking for Rochester offers. Both operate similarly to community cleanups. A corporation or business organizes a group of employees to volunteer to clean up trash in a neighborhood or area. Walking for Rochester provides and delivers the equipment and waivers for each volunteer to sign. Hours worked are tracked via the Walking for Rochester app. Unlike community cleanups, any trash collected must be properly disposed of by the business organizing the cleanup.
The Volunteer Program functions much the same but is geared toward individuals or groups and is available year-round. The required gear and waivers are delivered and hours worked are tracked via the mobile app.
“You can volunteer on your own or in a group. It’s all up to you. We ask that you contact our office to inform us where we can deliver the equipment. We request that all volunteers log into the mobile app before and after to record the hours worked. The mobile app tracks volunteers via GPS,” Apple said. “This is a great program for a high school or college student who needs volunteer hours or a community group or neighbors that wants to clean up a local park or neighborhood.”
Rochester resident Isabella Susino began volunteering for Walking
for Rochester when she moved to Rochester in 2021.
“I was looking on Reddit (a social news and forum website where users can share and view content like links, text, images and videos) for things to do in my neighborhood. I saw that Walking for Rochester had posted an upcoming event and I participated in a community cleanup,” Susino explained. She was interested in learning more about Walking for Rochester, so she researched this group, found the website and explored how she could become more involved.
“I wanted to better find my way around the city, make friends and connections. I saw the Walking for Rochester advertisement for a social media coordinator. I applied, spoke to Matt Apple and was hired,” Susino said. “My responsibilities included implementing social media practices and boosting the Walking for Rochester social media presence.”
In January of 2022, she became a board member for Walking for Rochester and took an active role in marketing, and promoting the organization. Volunteering for Walking for Rochester is a great way to give back to the community, Susino said.
She encourages anyone to join Walking for Rochester.
“You can come to a community cleanup and meet so many people. Everyone who is involved with this organization truly cares about our city, the environment and community members,” she said. “We are not just a nonprofit; we work to foster a sense of community. It’s so important that we take care of the environment in which we live. I believe that if we take care of the earth, then the earth will take care of us. I genuinely live by this philosophy.”
Apple is proud to report that the efforts of the Walking for Rochester’s volunteers have proved successful.
“On one community cleanup in early August, we collected almost 40 pounds of litter and we have collected over 1,110 pounds of litter per early August,” he said.
Interested in learning more? Follow Walking for Rochester on Facebook, Instagram, Reddit or LinkedIn. Download the Walking for Rochester app via Google Play or check out the website at walkingforrochester.org.


By Gwenn Voelckers
The howl of the wind, the shadowy silhouette of a black cat and a chill that may run down your spine: it’s that time of year again. Halloween reminds us of all things spooky and scary.
Living alone for the first time after a divorce or the death of a spouse or partner can feel like stepping into a strange, new — and sometimes frightening — world.
I know because I’ve been there. Suddenly, the comforting presence of another person is gone and the quietness that used to feel peaceful now seems unsettling.
You start noticing every little creak in the house, wondering about your financial future and grappling with a sense of loneliness you didn’t expect.
But more than anything, what rises to the surface is fear. It can show up in many ways — emotionally, physically and mentally.
• Emotionally, it’s the knot in your stomach when you hear an unexpected bump in the night or the anxiety that creeps in when you’re unsure how to manage a big decision.
• Physically, it can appear as tightness in your chest, a racing heartbeat or restlessness that keeps you tossing and turning at night.
• Mentally, fear clouds your thoughts, making small problems seem insurmountable. It causes you to doubt your ability to handle things, even though you’ve already overcome so much.
While it’s common knowledge that fear is a natural response to feeling vulnerable, it’s hard not to feel vulnerable when you’re suddenly on your own.
But while fear serves an important purpose — protecting us from danger — it can also hold us back. I felt trapped inside myself (and inside my home), afraid to step out into the world, try new things or believe in my own goodness and strength.
When we let fear dictate our choices, we risk missing out on opportunities to live fully, to grow and to discover the best version of
REACH thousands and thousands of health-conscious readers. Advertise with IN GOOD HEALTH. One ad, generating leads all month long. Free design. editor@GVhealthnews.com
ourselves.
So, how do we fear less when everything around us feels uncertain?
First, it’s important to recognize that fear is normal: it’s our brain’s way of trying to keep us safe. But we can manage it by not letting it control us.
The key is to gently face those fears, acknowledge them, and then take small steps forward.
Below are three of the most pressing fears I faced after my divorce. With help, I was able to better understand the emotional origins of my fears and find practical ways to manage them.
Loneliness is one of the most potent fears when you’re living alone, especially if you’ve recently lost a partner. A quiet home can become unbearable. I found that even simple tasks — like cooking or watching TV — felt hollow without someone at my side.
I worried my loneliness would grow deeper and become permanent. I clearly remember thinking at the time, “What if I never feel connected to anyone again?” or “What if I end up all alone for the rest of my life?”
While loneliness is very real, the fear of it growing worse is often irrational.
Loneliness is a temporary emotion, but when we give in to the fear of it, we start to isolate ourselves even more, reinforcing the very thing we’re afraid of.
The key is understanding that your loneliness doesn’t define your future — it’s a signal that you need more connection, and that’s something you can actively work on.
Start by redefining “connection.”
When we’ve lived with someone for a long time, we may unconsciously define connection as being tied to a romantic or deep, intimate relationship. But connection comes in many forms.
Start small. Reconnect with acquaintances, chat with neighbors
or join local groups. (Have you tried pickleball?) You’ll realize that human connection is accessible in many ways and doesn’t need to look like what you’ve lost.
Living alone can make every creak and shadow in the house feel ominous. Fear of safety is often heightened by the vulnerability we feel when there’s no one around to help in an emergency.
I can recall feeling fearful when I got my own home. Every faint noise in the house sounded like a potential intruder.
And my fear went deeper, making me anxious about having an accident at home or wondering, “What if something happens to me and no one is here to help?”
It’s important to recognize that our fear of danger is often irrational when it becomes overwhelming. Statistically, your home is probably one of the safest places you can be, especially if you take some precautions.
The real danger comes from letting your fears spiral out of control, keeping you from enjoying the comfort and peace of your own space.
So, empower yourself with security tools. Today’s technology offers plenty of affordable options. From security cameras to smart locks, motion-detecting lights, and apps that let you monitor your home remotely, these tools can help you feel more in control.
The goal is not just to prevent real dangers, but to give your mind the reassurance that you’re doing everything you can to stay safe.
Financial fears are especially common when living alone, particularly if your spouse managed the finances or if your income has suddenly changed after a divorce or the loss of your partner.
The thought of running out of money, being unable to maintain your lifestyle, or not having enough for medical bills or emergencies can feel very scary.
After my divorce, I was up in the middle of the night with questions swirling: “Will I be able to make ends meet?” or “What if I outlive my savings?”
Financial insecurity often arises from the unknown. It’s not just the fear of not having enough money — it’s the uncertainty of how much you actually have or what you’ll need in
Excellus BlueCross BlueShield is accepting applications for its 2024 Health Equity Innovation Awards, which provide funding to community-based organizations to support health and wellness programs that address racial and ethnic health disparities in Upstate New York.
The online application portal will close at 11:59 p.m. on Friday, Oct. 4,
“The Health Equity Innovation Award funding is designed to support initiatives that confront the fundamental causes of health disparities, particularly those linked to structural racism. By providing funding for
the future. My mind went immediately to worst-case scenarios. But more often than not, these worst-case fears are exaggerated. Once you confront your finances head-on, you may find you’re in a better position than you think.
But first things first. Get clear on your financial situation.
Sit down with your financial statements, or better yet, with a financial adviser, and go through everything step by step.
Knowing exactly where you stand — your income, your expenses, your assets —can alleviate a huge amount of anxiety. Even if the news isn’t perfect, you’ll feel more empowered knowing the facts.
I strongly recommend working with a financial adviser who can help you put your financial house in order and alleviate your financial fears.
With budgeting and planning, you’ll feel more secure in your ability to handle whatever life offers up.
The key to overcoming your fears is not to ignore or suppress them, but to face them directly. When we confront our fears — whether it’s loneliness, safety, financial insecurity, or something else altogether — we take away some of their power.
It’s natural to be afraid, but it’s equally natural to find strength in yourself that you didn’t know was there. By acknowledging your fears, taking small steps, and reaching out for support when needed, you can build a life that’s full of connections, confidence, and peace.
You’ve already overcome so much — facing your fears is just the next step on your journey.
I’m right there with you. Let’s fear less and live more!

Gwenn Voelckers is the author of “Alone and Content: Inspiring, empowering essays to help divorced and widowed women feel whole and complete on their own.” She welcomes your thoughts on this column as well as topic suggestion for future essays at gvoelckers@rochester. rr.com.
upon a project’s ability to demonstrate tangible improvement in racial and ethnic health equity.
Priority categories for the Health Equity Innovation Awards include:
projects that tackle social, economic, and systemic issues, we aim to create a healthcare system that is fair and equitable for everyone,” said Simone E. Edwards, vice president of health equity and community investments at Excellus BCBS.
Nonprofit 501(c)(3) organizations in the Excellus BCBS’ service area can apply for funding of up to $30,000.
Applications should propose innovative projects with measurable outcomes, expansion potential and clearly outlined goals to reduce health disparities and address social disadvantages. Funding is dependent
• Improved maternal health outcomes
• Behavioral health or mental health conditions
• Acute and chronic disease management
• Social determinants of health such as economic stability; education access, and quality; health care access and quality; neighborhood and built environment; and social and community context
For more information and to apply, go to www.excellusbcbs. com and type “community-investments-partnerships” in the search menu.
By Albert S Hartel, MD
As another brutal Rochester pollen season winds down, many allergy and asthma sufferers look forward to the first frost to put an end to the annual onslaught of pollinating trees, grasses and weeds.
However, even after the frost, another brutal outdoor allergen still remains unfazed and is actually on the rise: mold.
Indoor mold has long been a known nuisance, causing allergy and asthma symptoms from exposures in basements, bathrooms showers and areas of water damage.
But outdoor mold is often less visibly apparent and overlooked as a health concern, but is present outside in large numbers, which are rising as Rochester winters have been less intense.
While a good killing frost will stop most pollen in its tracks until spring, mold is relatively unaffected by the frost, and even a good old severe Rochester winter will usually only slow it down, causing it to form a resilient spore that can survive, continue to cause symptoms, and multiply when conditions improve.
With the recent more mild winters, rather than becoming dormant, outdoor mold has thrived — and levels have been increasing, continuing to cause those with asthma, allergies and sinus symptoms to have more frequent attacks, ongoing symptoms and continue to require more medication.
Outdoors, molds live in the soil, on plants, mulch and on dead or decaying matter. Falling leaves, picked crops and wood piles are prime spots for mold to grow.
The best treatment for mold allergy is avoiding exposures as much as possible.
Avoid going through places that can have highest mold counts, such as a piles of dead leaves, vegetation, damp areas, barns and uncut fields.
Keep your backyard and surroundings clean, dry and rake leaves and remove dead vegetation.
After coming in from outdoors, change clothes and flush out mold with nasal saline spray. Wipe pets after coming in from outside, wash them regularly and run a HEPA air purifier in the bedroom and living room, and dehumidifier in the basement.
Getting tested to identify mold and other cumulative allergies is critical, as avoidance, a treatment plan and potentially allergy shots to desensitize you and turn mold allergies off is preferred to suffering or lifetime of chronic long-term medications and recurrent allergy and sinus symptoms and asthma flares from this growing threat!

Physician Albert Hartel is a board-certified allergist-immunologist and president of Allergy Asthma Immunology of Rochester. For more information, visit https://aair.info or call 585-442-0150.
Concierge-level care at an affordable monthly rate

• Convenient, direct access to text/call/email your primary care physician
• Same day or next day appointments for sick visits
• Relaxed, unhurried in-person visits, virtual or home visits
• Address the root cause of chronic diseases using lifestyle medicine
• Menopause and hormonal therapy
• Physician supervised weight loss
• Medical micro-needling for wrinkles or scars
• Comprehensive biomarkers and metabolic testing
• Comprehensive cancer screening using cell-free DNA blood testing
• Transparent pricing, no surprise bills.

Vitiligo affects up to 2% of the global population. A new potential therapy, afamelanotide, is being evaluated as a treatment for vitiligo patients with darker skin types.
Two study treatment groups:
A. Narrowband ultraviolet B (NB-UVB) in combination with afamelanotide.
B. NB-UVB alone.
Study duration: 5 months of treatment + 6 months of follow-up.
You may qualify if you: Have generalized vitiligo on the face and body.
• Are aged 12 or more.
Have medium to dark skin.
• Do not have extensive white hair in your vitiligo patches.
• Do not have a history of melanoma, lentigo maligna or do not have any malignant (cancerous) skin lesions.
• Do not have liver diseases. Are not pregnant or breastfeeding.
Participation involves:
• NB-UVB light treatment twice per week for 20 weeks (all participants).
• Receiving an implant of afamelanotide every 3 weeks for 20 weeks (50% of participants).
• Travel costs may be reimbursed.

When it comes to mammograms, experts now advise women to get tested for breast cancer at age 40
The U.S. Preventive Services Task Force this year lowered the age recommendation for when individuals should begin getting screened for breast cancer.
The task force now advises eligible individuals who are not at high risk and who don’t have a family history of breast cancer to get screened every other year starting at age 40, which is 10 years earlier than its previous recommendation. Regular screenings are recommended to continue through age 74.
Breast cancer is the second most
common cancer among women, accounting for about 30% of all new cancers diagnosed, according to the American Cancer Society. It is the second leading cause of cancer death in women, behind lung cancer. Early detection is key, and a mammogram can detect a tumor up to two years before it can be felt by the patient or a health care provider.
“Screening for breast cancer saves lives, so it is important for everyone who is eligible to be screened to follow these new recommendations,” says physician Nicholas Mas-
sa, vice president of medical affairs at Excellus BlueCross BlueShield. “Unfortunately, not everyone who is eligible is getting a mammogram.”
About 20% of individuals in New York state who are eligible for breast cancer screening are not getting screened, according to an Excellus BCBS review of the most recent data from the National Cancer Institute. Among eligible individuals between the ages of 50 and 74, 81.4% had a mammogram in 2022.
Obstacles that may prevent someone from having routine breast
Analysis of millions of births shows one-third of birth complications occur during the six weeks following discharge and disproportionately affect Black patients.
New data shows that dangerous, unexpected birth complications often emerge weeks after the patient and baby have left the hospital, with Black patients experiencing these events at a rate 87% higher than white patients. Moreover, New York state has the highest number of these events in the nation, according to a new Blue Cross Blue Shield (BCBS) analysis.
The analysis of these birth complications, known as severe maternal morbidity (SMM), draws on nationwide data from more than 700,000 BCBS commercially insured births and data from the Centers for Medicare & Medicaid Services on more than 1.5 million Medicaid births.
Across New York state, the data revealed the rates of SMM events are higher than the national average, both overall, and for each ethnic group (Black, Hispanic, white), particularly for Medicaid members. The data also confirms racial and ethnic
disparities in SMM events in New York state.
“The statistics are alarming, but they’ve also presented an opportunity and a responsibility to confront this national crisis,” says Excellus BlueCross BlueShield’s physician Simone Edwards, vice president, health equity and community investments. “Excellus BCBS is committed to collaborating with local community organizations to support safe pregnancies and childbirth, eliminate pregnancy-related health disparities, and improve health outcomes for new mothers and babies.”

Excellus BCBS’s Bright Beginnings program is stepping in to fill necessary gaps in care like transportation, resources, and provider referrals to help new parents effectively care for themselves and their mental health.
The program, led by Kara Traverse, manager, maternity care management, includes a team of licensed social workers and registered nurses who meet with members referred by area doctors and hospitals, family, and even members themselves.
“They contact the member, listen to their concerns and screen for
cancer screening can include lack of transportation, inconvenient screening facility hours, or patient apprehension about screening discomfort and safety.
To combat the transportation barrier, some hospitals and medical practices bring a mobile mammography van out into the community. Many hospitals and clinics also offer extended hours for on-site mammography screenings, so appointments can fit most schedules.
“Screening for breast cancer can be uncomfortable, but the test only takes a few minutes,” says Massa. “The potential benefits of early cancer detection outweigh any discomfort or concerns.”
Routine breast cancer screening is a preventive service that is among the essential benefits included in all Marketplace health plans and many other plans, at no cost to the patient, even if a yearly deductible has not yet been met. Note: These services are free to the patient only when delivered by a doctor or other provider in your health plan’s network.
An individual’s risk factors determine when they should begin getting screened for breast cancer. Those at high risk or with a family history of breast cancer should ask their health care provider about the right age and frequency of screening for them.
Learn more about breast cancer and screening by visiting the U.S. Preventive Services Taskforce website at https://uspreventiveservicestaskforce.org and typing “Breast Cancer Screening” in the search box.
Submitted by Excellus BlueCross BlueShield.
depression and anxiety. From there, the case manager assesses and makes appropriate recommendations, providing resources for transportation, education, mental health support and more,” Traverse explains.
The Bright Beginnings team also collaborates with community-based partners committed to increasing maternal health care awareness and availability. From breast pump and pregnancy education to mental health screenings and arranging hospital and pediatrician visits, the Bright Beginnings program aims to help parents stay on track caring for themselves and their children.
Excellus BCBS also supports programs for maternal mental health run by community-based organizations across its operating area. Some of these efforts include Cortland-based Seven Valleys Health Coalition’s Post Partum Doula Support and Doula Partnership, Syracuse-based Contact Community Services’ Maternal Mental Health Follow Up Support, and Utica-based Integrated Community Alternatives Network’s (ICAN) Maternal Health Equity for Pregnant Homeless Teens.
Read the full report, “Improving Postpartum Maternal Health Outcomes,” part of the BCBS Health of America Report series, here: http:// bcbsa.co/6046YtIzI.
Submitted by Excellus BlueCross BlueShield.

Final government data finds the number of U.S. births falling by 2% last year compared to 2022, continuing a decades-long decline.
Overall, annual U.S. birth numbers have fallen by 17% since peaking in 2007, according to the new report from the U.S. Centers for Disease Control and Prevention. The general fertility rate (births per 1,000 women) has also tumbled by 21% over that time period, the report found.
Births to females in their teen years (ages 15 to 19) are part of this trend, declining by 4% from 2022 to 2023, say a team led by Joyce Martin, of the CDC's National Center for Health Statistics (NCHS).
In total, there were 3,596,017 births recorded in the United States last year, compared to 3,667,758 the year previously.
In other CDC birth data, fewer pregnant women received adequate
By Deborah Jeanne Sergeant
Beyond the idea of skewing the stereotype, not becoming a “little old lady” is important for aging well. Losing muscle and bone in older age and becoming frail can raise risk for earlier death. Frailty isn’t just “getting older.”
“Frailty in older women is multifactorial,” said Maria Enecilla, a geriatrician at Rochester Regional Health.
She explained that it’s characterized by a loss of physical and cognitive reserve which can lead to an increased risk of illness and injury. Women lose their ability to perform activities of daily living. They must rely more and more on others and this causes even more decline in health as they do less for themselves.
The reasons for the onset of frailty include chronic health conditions, hormonal changes, isolation and little social support. Letting chronic disease go unmanaged matters.
“Diabetes, hypertension chronic obstructive pulmonary disease, coronary artery disease, arthritis: all decrease physical and functional abilities which can lead to frailty,” Enecilla said. “Osteoporosis increases risk of fracture which leads to physical decline.”
Taking unnecessary prescriptions also makes a difference in falling.
“A lot of people have a long list of medications that can interact with each other and the body and lead to side effects that lead to frailty, like fatigue, dizziness and confusion,”
Enecilla said.
Oftentimes, falls begin a downward spiral in health if the woman breaks a hip and becomes further deconditioned. Thirty percent of adults experiencing a hip fracture die within a year, according to the American Family Physician Journal.
To fight the risk factors associated with frailty, Enecilla encourages women to stay physically active. One means is through strength training. This can include bodyweight exercise, lifting free weights, using a weight machine or stretching exercise bands. All of these can help address age-related muscle and bone loss.
“The lack of estrogen in menopause affects our bones and our muscle mass,” said Maureen Slattery, OB-GYN and certified menopause practitioner with Rochester Regional Health. She encourages women to improve their resistance training, including core strength and balance.
Incorporate activity that improves balance such as tai chi, yoga or dance to reduce the risk of falls.
Try aerobic exercise like brisk walking, cycling and swimming, which have a low risk of injury yet provide a means to keep the heart healthy and build muscle.
Enecilla added that diet should support building muscle.
“Adequate protein intake is crucial for muscle mass,” she said. “One study shows higher protein intake is associated with lower levels of frailty.”
care in 2023 compared to 2022. The number of women who received prenatal care during their first trimester fell by 1%, and the percentage who got no prenatal care at all rose by 5%, continuing a trend noted in 2021 to 2022.
"Late and no-care levels have risen steadily since 2016," Martin's team noted in the report.
About 10.4% of births were premature in 2023; about the same as 2022. Early-term births (during the 37th and 38th week of pregnancy) rose by 2%.
"Since the most recent low in 2014, preterm birth rates have risen 9% and early-term births by 21%, while full-term and late- and postterm births have declined," the NCHS team wrote.
The new findings were published Aug. 20 as an NCHS Data Brief.

Many women benefit from supplementing with calcium and vitamin D. Ask your care provider if these would help you.
Managing chronic conditions like autoimmune diseases and diabetes and following up with a primary care provider and any appropriate specialists can help reduce risk of frailty. Don’t let maintenance medications run out or necessary lab work fall by the wayside.
Keeping the mind busy and healthy can also contribute to avoiding frailty. Enecilla said that poor mental health can increase risk for frailty.
“Make sure you stay engaged and manage things like depression and anxiety,” she added.
Overall, avoiding frailty is about remaining engaged with life.
“Aging doesn’t equate frailty,” Enecilla said. “Some seniors lead robust, active lives. Target factors that lead to frailty and look at possible causes already present. It enhances quality of life and reduces risk of severe health consequences and leads to a more active lifestyle.
“I see 80- and 90-year-olds at the Y doing Silver Sneakers. Aging doesn’t always mean decline.”

on North Clinton Avenue. A third one that’s under construction, Persimmon Place, is located in the Bulls Head area on the southwest side of Rochester. That one will add 12 more units of family housing. In addition to helping women, we also provide services for fathers. We often will have single dads, men that are part of a family unit and they need shelter for them and their children.
Q: Could you describe your longterm housing program?
A: Our long-term housing program actually spans across the city. The difference between that and the shelter program is that these women live in their individual rooms and have leases. This is where they call home.
Q: How many housing units does this program offer?
Eliminate racism and empower women are among the main goals of the YWCA of Rochester & Monroe County, says its president and chief executive officer. One of the tools to achieve this is through housing, she adds
By Mike Costanza
Q: What is the YWCA of Rochester & Monroe County’s mission?
A: To eliminate racism and empower women. We share that mission with our sister associations across the country. We let that mission drive us to work directly with the community and those who are most vulnerable in our community. Those folks are often not from the dominant group, so minorities and those who are unhoused and the like.
Q: How does your nonprofit try to accomplish its mission?
A: Through housing. We have three housing programs. All of our residents have some experience with being unhoused or are at the risk of being homeless. That’s how they come to us. Our housing programs are structured on what we call a continuum of housing care. That continuum may start with emergency shelter and get them out of shelter into permanent housing. Our goal is getting them housing-stable.
Q: Can you tell the readers about
your emergency housing program?
A: Our emergency housing program consists of two emergency shelters, one for individual women, one shelter for families. The individual women have their own rooms, communal kitchens, where they have family-style dinners nightly, communal bathrooms and a communal laundry. The family units are apartments. Those do have a full kitchen, as well as their own bathroom facilities. While they’re there, we connect them (the clients) with resources that can help them find permanent housing and often permanent supported housing. Everyone that comes through our emergency housing program, they have an immediate need for shelter.
Q: How big are these facilities and where are they located?
A: The individual emergency shelter is 13 units. The housing for families has seven apartments that can hold up to a family of nine. The units are located in downtown Rochester in our flagship building,
A. We have 47 units of single-room-occupancy in our flagship building. They do have shared kitchens, shared bathrooms, shared laundry facilities. We also have 14 units of one-bedroom apartments. These are permanent supportive housing units, so they (clients) receive case management services year-round. They’re all affordable housing units. We also own and operate two apartment buildings on the northeast side of town that are also permanent supportive housing. Those are one-, twoand three-bedroom apartments.
Q: What other services do you provide for those in your housing programs?
A: If they come through our emergency housing program, they receive case management services. Our employees, most of them, are case managers. They work directly one-on-one with residents to be a support to them as they’re getting their footing in life. Some meet with our residents weekly. That may be making sure they’re keeping their apartments clean, making sure they pay their rent, making sure they’re being a good neighbor. There may be some clients that don’t need such a high-touch level of care and may check in with their case managers once a month. It really is on an individual basis. We meet folks where they are.
Q: The YWCA also offers the Steppingstone Supportive Living Residential Treatment Program. Can you describe it for the readers?
A: That’s 13 residential addiction recovery units. Individuals can stay with us for up to 18 months while they’re going through addiction recovery. The addiction can be alcohol, it could be drugs. While they are here, they also receive services and treatment. That treatment could be through group meetings and counseling. What is unique about our program is that the individuals who are going through the addiction recovery program are allowed to have their children 12 and under with them while they’re going through recovery. We also provide drop-in day care for our clients that are part of our Steppingstone Supportive Program while the parents are in treatment or at a doctor’s appointment.
Q: Does the YWCA charge for its services?
A: There is no cost to participate in any of our programs, in terms of people having to pay a monthly fee or program fee. None of our longterm tenants pay more than 30% of their income for housing. That could be zero, or up to 30% of the rent. In the case of the emergency housing program, the majority of the people who come to see us do not pay us directly. We’re subsidized through the (Monroe County) Department of Human Services. That too is based on income. If you can afford it, then there may be a small stipend that you have to pay while you’re here.
Q: How important are the YWCA’s housing programs?
A: I’ve had conversations recently with women who have had very public physical fights with their significant others and they felt as if they were in danger. They would see a YWCA in the distance and feel in their minds “If I could just get there, I know I’ll be safe.” That sense of safety and that sense of just knowing that someone will be there to care for me in my time of need has been a through-thread through our work for more than 100 years.
For more information on the YWCA of Rochester & Monroe County and its programs, go to: www.ywcarochester.org.
Adrug under development could provide a much needed option for women seeking relief from hot flashes and other menopausal symptoms, new research shows.
The drug, elinzanetant, cut the frequency of hot flashes by an average of about 56% after one month of use, and by more than 65% after three months.
Overall, about 62% of more than 300 postmenopausal women in two trials experienced "at least a 50% reduction in [hot flash] frequency," wrote a team led by physician JoAnn Pinkerton, from University of Virginia Health in Charlottesville.
The drug also appeared to reduce the severity of hot flashes.
The two trials were funded by elinzanetant's maker, Bayer, and published Aug. 22 in the “Journal of the American Medical Association.”
Based in part on these results, Bayer announced in September that it

had filed a new drug application for elinzanetant with the U.S. Food and Drug Administration.
According to Pinkerton's team, up to 80% of women will experience hot flashes -- medically known as menopausal vasomotor symptoms (VSM) -- during menopause, sometimes lasting for many years.
Hot flashes can be debilitating and difficult to predict, and there are few therapeutic options to treat them.
At the start of the trials, the average participant said she suffered through about 14 hot flashes during every 24-hour period.
However, by week 4 of one of the trials, that number had fallen to less than 8 per day among women taking the placebo, and to less than 6 per day among those taking elinzanetant.
By week 12, daily hot flashes had been reduced to less than 8 per day for women taking placebo and to just 4.7 per day for women on elinzanetant.

The latter number represents a 65% reduction in hot flash frequency compared to the beginning of the trial.
When hot flashes did occur they also tended to be less severe for those taking elinzanetant, participants reported. Women taking the drug also reported significant improvement in their sleep, the study authors said.
By the end of both 26-week trials, "more than 80% of participants had
achieved at least a 50% reduction" in hot flash frequency, the researchers said, suggesting that the benefits were maintained over the longer term.
As to side effects, about half of participants did complain of issues such as headache or fatigue, Pinkerton's group said. "Most events were of mild intensity, and none were severe," they noted.









By Deborah Jeanne Sergeant
Lower back pain, neck pain,
sciatica, tendonitis, plantar fasciitis, arthritis and joint injuries are all tough to manage non-invasively and without medication.
That’s why Chance Lowry, owner of Northeast Pain Solutions, is so excited about shockwave therapy.
His facilities in Rochester, Canandaigua and Geneva offer SoftWave Therapy, a form of shockwave therapy that uses sound waves to stimulate healing in damaged tissues.
These sound pulses use high positive pressure with a fast and steep rise time followed by comparatively small negative pressure.
Lowry explained that the therapy modulates inflammation, creates a localized stem cell response to increase the repair efforts, stimulates blood flow at the injury site and breaks up scar tissues in cases with chronic injuries.
The benefits include pain relief, anti-inflammatory response, antibacterial effects, improved blood flow, tissue growth and regeneration, stem cell activation and tissue generation.
“This has completely changed the way we practiced,” Lowry said. “We can help a lot of injuries that were difficult to work with like
tendonitis. It’s hard to conservatively work with these, but our success rate is through the roof.”
Northeast Pain Solutions has expanded to three offices because of the therapy.
He said that originally, the therapy was used for nonunion bone fractures and then providers began using it with soft tissue issues.
“We don’t use it for that as we’re not an orthopedic office,” he added.
“For tendon and ligament injuries, they’re poorly vascularized so they heal poorly. There’s lack of blood supply. This increases blood supply by 400% so tissues heal on a biological level. It’s not just reducing pain but it regenerates tissue. A lot of things in the medical world have claims but not patents to back it up. These patents are very well accepted.”
Some providers use soundwave therapy in urology to treat kidney stones and erectile dysfunction. It’s also used for wound care and women’s urologic and sexual health at other providers. Lowry said that in Europe, providers use it to promote healing after cardiac surgery and for spinal cord injuries.
Lowry uses SoftWave to promote

healing with soft tissues like ligaments and tendons.
The therapy is not covered by insurance. It may take four to eight sessions to treat an area and cost $50 to $100 per session, depending upon its size. Most patients receive a degree of immediate pain relief,
about 30-40%. Within four to eight treatments, many receive 70 to 100% pain reduction.
“I’m a skeptic as an individual because most things in medicine are overplayed,” Lowry said. “This is phenomenal.”


By Anne Palumbo
Ever since I discovered that kefir

— a fermented milk product with more probiotics than yogurt — could benefit my achy gut, I jumped on it.
From the health benefits to the tangy taste to the ease of consumption, it checks all the boxes.
Plus, I’m tired of skipping activities because of my finicky gut, and, so far, kefir is doing the trick.
Fermented foods — like kefir, yogurt, sauerkraut, kimchi and kombucha — teem with probiotics, the “good” bacteria that can help restore the natural balance of bacteria in your gut and decrease signs of gut inflammation. Reducing inflammation is important, especially since longterm gut inflammation can increase the risk of chronic diseases over time.
What’s more, a healthy gut can boost the immune system, help keep blood glucose levels stable, and may even influence moods and mental health, according to the Mayo Clinic.
I’m also hooked on kefir because it’s a rich source of calcium, protein and B vitamins.
Forever seeking ways to strengthen my bones and prevent loss, I look forward each day to the 300-400 mg of calcium per cup that kefir provides. Same goes for the impressive dose of protein that kefir delivers per cup: 9 grams. Protein is a building block for muscles, cartilage, skin, and — yes! — bones.
Kefir is rich in energy-boosting
vitamins, most notably vitamins B2 (riboflavin) and B12. This powerhouse combo helps turn food into fuel, build red blood cells and minimize the risk of birth defects. Also, both vitamins can help slow cognitive decline as well as nuke toxic free radicals, whose buildup in our bodies can cause chronic disease and premature aging. Especially good news for those seeking stronger bones: Both vitamins may support bone health and prevent osteoporosis.
Not a big fan of bananas, the go-to food for potassium? Reach for kefir, whose potassium levels rival a banana’s. An essential mineral for all body functions, potassium is your heart’s best friend: it keeps the beat regular, reduces the effect of sodium (present in table salt) on blood pressure and lowers your risk of cardiovascular disease.

Anne Palumbo lifestyle columnist, food guru, and sea soned cook, who has perfected the art of preparing nutritious, calorie-conscious dishes. She is hungry for your questions and comments about SmartBites, so be in touch with Anne at avpalumbo@aol.com.
Read nutrient labels carefully (some flavors have more sugar than others). Pair kefir with foods high in “prebiotics” — such as bananas, apples, and berries — for a synergistic combo that optimizes gut health function. Some kefir brands (like Lifeway low-fat kefir) are up to 99% lactose-free, which may make them tolerable for those with mild lactose intolerance.

1 cup kefir of choice (I used Lifeway low-fat vanilla)
½ cup blueberries
½ cup sliced strawberries
½ cup sliced peaches
By Shaina Zazzaro
Summer is over, fall is here. Time for you to get in gear (did you like my rhyme?)
Summer allows us to make excuses for staying consistent. We only get a few months a year in Rochester to enjoy sunshine and warm weather, so naturally we go out to parties more, out to dinner more, and lack planning our food more.
I am here to help guide you to begin planning more to set you up for success until at least Christmas.
Let’s stop making excuses and get to work!
The easiest way to start is to evaluate your current eating habits and to review and make positive changes.
When people ask me about losing weight, I tell them for a week to track their food on My Fitness Pal, a health and fitness tracking smartphone app and website. The app is available for Android and iOS devices.
You can be as accurate as you
are able to be, and then in a week to review and see what habits you may have.
It can be a habit as simple as knowing that every Monday you lack preparation and eat Grubhub, not only costing you more money than if you were to plan for your food, but having high fat, high calorie lunch; or some thing like eating out every Tuesday because your kids have football practice.
The first step of change is to recognize the change so you can make a
sprinkling of favorite toasted nuts or granola
Place everything in a bowl and enjoy! Or make a smoothie with kefir and your favorite fruits.

positive adjustment to your lifestyle. By observing these habits, you can recognize an opportunity to preplan your lunch or dinner for the specified dates and times, and to pack yourself a nice, healthy
It is little adjustments that set you up for the future.
If you are looking to lose weight and live in Rochester email me at shainazazzaro@ ehmeals.com and I can walk you through options for nutrition coaching and healthy meals.
If I can lose 50plus pounds three times, you can do it too!
Rates Upstate are even worse than some other areas of New York, according to latest figures
By Deborah Jeanne Sergeant
Arecent study by an organization affiliated with Columbia University indicates that compared with the rest of the nation, New York showed higher incidence rates for prevalent cancers, especially among those aged 25 to 49 for several cancers, including breast, colorectal, thyroid, kidney, renal pelvis and leukemia.
Physician Jonathan W. Friedberg, director of UR Medicine’s Wilmot Cancer Institute, noted that in the 27 counties Wilmot serves, which include more than 3 million people, there’s a disproportionately high incidence of cancer. “Indeed, if this catchment area were a state, it would have the second highest incidence of cancer in the country behind only the state of Kentucky.”
It's challenging to point to a specific reason for the higher rates of cancer incidence. Friedberg noted a few factors include an aging population, high rates of tobacco use and sedentary lifestyle, rural healthcare
access challenges and poverty.
“Wilmot has established an office of community outreach and engagement to track these cancer statistics and ensure our research programs are addressing these challenges,” Friedberg said. “We have an aggressive effort to decrease tobacco use and ensure adherence to cancer screening guidelines for early detection. We are also exploring other potential drivers of cancer, for example pesticide use and other toxins in the environment. It is part of our mission to overcome this disparity in cancer incidence.”
Of course, factors like aging and genetics can’t be changed. But many other factors can be. Charles Kamen, Ph.D., assistant director for community outreach and engagement at UR Medicine’s Wilmot Cancer Institute, said that genetic risk predicts only up to 10% of cancers.
“For those who have first-degree relatives — mother, father, sisters, brothers, children — with cancer or
Excellus BlueCross® BlueShield® is working to make quality care more accessible. With low or no cost plans and programs that support families, we are focused on improving access in your community.
To find coverage that’s right for your family, visit ExcellusBCBS.com
many family members with the same type of cancer, genetic counseling and testing may be appropriate to assess genetic risk for cancer,” Kamen said. “Overall, factors like smoking and obesity predict more cancers than genetic factors do and so the best thing anyone can do for their health is work on these controllable risk factors.”
He cited as an example that since smoking has been linked to at least 16 different types of cancer, quitting is vital for good health. Wilmot Tobacco Quit Center can help.
“People who are over age 50 and who have been smoking for 20 years or more should consider getting a lung cancer screening,” Kamen said. “Lung cancer is the most deadly cancer in our catchment area, but screening can catch it early and increase the chance that treatment will be successful.”
In a CDC study from 2017 to 2020, New York ranked among states with a self-reported sedentary rate of 25% to 29%. A handful of Southern states ranked worse. However, New York ranked worst in the Northeast.
Long, cold winters may help explain the low rates of physical activity in the area. However, sedentary lifestyle should be avoided for many reasons, including the fact that it

contributes to higher rates of obesity. Obesity is a risk factor for many diseases and illnesses, including cancer.
“Walking, yoga, or resistance training with weights can improve overall health, help people attain or maintain a healthy body weight and thereby reduce cancer risk,” Kamen said.
Choosing an activity that is enjoyable and also meets health goals can help people stick with it.



Two generations ago, a cancer diagnosis felt like a death sentence. Thanks to medical advances in treatment, more people can survive the disease. But that doesn’t take the sting out of hearing a doctor say, “You have cancer.”
In some cases, what patients do next can affect how well they cope and even their chances of survival.
1. Avoid the internet.
“The internet is the enemy of mental health,” said Lynn Acquafondata, licensed mental health counsel or and owner of Crossbridge Counseling and Crossbridge Wellness in Rochester. “There’s a lot more to it than reading something on the internet. Different things affect different people in different ways. Especially for those with high anxiety; stay off the internet and talk with your doctors. Doctors may recommend a website if they think it’s appropriate for a particular person.”
By Deborah Jeanne Sergeant
with someone. Reach out to support groups.”
4. Don’t hide the news from loved ones.
“Some people hide cancer diagnoses,” Acquafondata said. “That’s destructive. You don’t have to necessarily post it on Facebook, but at least have some close people to you to talk with about how you’re affected by it.”

5. Don’t assume the worstcase scenario.
“Keep things in perspective,” Acquafondata said. “Not every cancer is a death sentence. There are treatments and many ways to move forward.”
6. See what can be done.
sue treatment and that’s their right. No question is a dumb question. You don’t know what you don’t know, so always ask.”
9. Get organized.
“Start with a trapper folder so you can keep all your information together in one place,” said nurse Anna Morrison, a lymphoma nurse navigator at James P. Wilmot Cancer Institute. “Write down a list of your medications including prescription and over-the-counter medications, vitamins and supplements. Include dose and frequency and keep up to date during this time.

information given and use recommended sites for disease specific information.”
11. Accept help.
2. Take time to mourn.
“When a person gets a cancer diagnosis or any other serious diagnosis, there’s a grieving process,” Acquafondata said. “There’s a loss of health and who you thought you are. You’re faced with your mortality.”
3. Seek mental health help.
“Counseling could be helpful for the person and their family members,” Acquafondata said.
“Get support if you need it or even if you don’t think you need it. Go to a couple’s counseling sessions. Walk through it
“Explore your treatment options,” said Bethany Walton, senior oncology social worker and collaborative care therapist for Rochester Regional Health. “Just because one doctor is telling you one thing, that doesn’t mean it’s absolutely the way to go. You can get a second opinion if you want. We want you to get the best treatment for you. Ask your doctor if you’d like to seek a second opinion.”
7. Seek helpful resources.
“Ask to meet with a social worker,” Walton said. “Every office has social workers available to patients. The social worker might think of things that didn’t even cross your mind like financial grants, transportation to appointments and things you’ll need to plan for in the future.”
8. Discuss what you want.
“Talk with your doctor and your care team about what your goals are for care,” Walton said. “Make sure they know what your goals are. We have patients who don’t want to pur-
“Write out your family history — include parents, siblings, grandparents, aunts and uncles and children. What medical history runs in your family: diabetes, hypertension, stroke, cancer? Make a list of surgeries and medical diagnosis including year and physicians involved. Have name and phone numbers of your other treating doctors, primary care, cardiologist, dermatologist so that they can be included on notes and aware of what you’re going through,” she said. “Write out the story of what transpired prior to your diagnosis. Include when you noticed things, who you saw and what tests were done. These will be the first questions you will be asked when you meet your oncology team and being prepared gives more time to discuss the important aspects of your diagnosis.”
10. Bring a scribe.
“Determine who can be with you at the first appointment to act as a second set of ears,” Morrison said. “This is overwhelming news. There will be much information at your first appointment and it is important to be able to listen. Ask the nurse or physician if they mind being recorded or ask your spouse or a friend to be your scribe during the appointment so that you have notes to look back on. Read through the
“Look to those who can offer support,” Morrison said. “It takes a village to successfully get through difficult times. Make a list of people who you could ask for assistance if needed. Things that you can call on others for: rides, meals, light house cleaning, lawn mowing. Patients often tell me they don’t want to ask others for support, but friends, family and community do want to help. It makes others feel good if they can do something and being specific with a task is so much better than leaving them up to guess what would be helpful. ‘Can you make me a few meals that I could freeze in case on treatment days I am lacking the energy to be able to cook?’
Ask your neighbor if they know anyone who could mow your grass or shovel your driveway during this time and see what happens.”
12. Pick your team.


“Chose a physician that spe cializes in your disease,” Morri son said. “Have they written any published journals? Are they leaders in their field? Are they able to talk with you as a partner in this journey? Listen to their recommendations and try not to make up your mind before hearing all their recommendations. Sometimes people say, ‘I would never do chemotherapy’ before it is even mentioned. Things have progressed in cancer care, so don’t let experiences from years ago set the tone or paint your perception. Have a list of questions, ask how things work — who is your medical care point person to call, take a tour of facility where you will be treated, ask when blood work needs to be done, review calendars and schedules.”






By Mike Costanza
Things were going well for Sonia Olsen back in January of 2021. Olsen had recently moved with her husband from Liberty to Webster and was looking forward to spending more time with her daughter, Erica, who had come to the area to work as a registered nurse.
She had also just retired from her job as a registered nurse for a New York state correctional facility and taken a part-time job with UR Medicine inoculating people against COVID-19.
Then a routine mammogram uncovered evidence that her left breast might be cancerous. A biopsy confirmed the diagnosis.
“My body immediately recoiled and I went numb,” the 65-year-old said. “I felt as if a death sentence had been pronounced.”
Subsequent testing found that her right breast was cancerous as well.
Though the disease was in the early stages, Olsen immediately decided to undergo a bilateral mastectomy and reconstruction.
“I wanted to live and I wanted to do whatever it takes,” she said.
In a nutshell, in a bilateral mastectomy and reconstruction, the surgeon removes both breasts, then replaces them either with artificial implants or with tissues that are taken from other parts of the patient’s body. Once healed, the reconstruction should recreate the look of the patient’s breasts.
In March of that year, a surgeon at UR Medicine’s Highland Hospital removed Olsen’s breasts and began reconstructing them using mus-
cles from her back and fat from her abdomen. In addition, the surgeon removed some of the lymph nodes of Olsen’s arms in order to determine whether cancer had spread to other parts of her body. Luckily, it hadn’t.
Complications from the surgery on Olsen’s abdomen led to blood loss and she had to undergo three blood transfusions. As a result, instead of staying in the hospital for no more than two days after her surgery, it was as much as five days before Olsen could return home. When she did, she was in a great deal of pain and generally unable to get around.
“The recovery from the initial surgery was intensive,” Olsen said. “I required care and compassion, which, gratefully, my spouse of nearly 36 years provided.”
Charles, Olsen’s husband, daughter Erica and a friend who is a physician helped her get around and recover from the surgery. One of their tasks was to tap the drains that the surgeon had implanted in Olsen’s sides in order to remove excess fluids.
“I had six drains coming out of my body,” Olsen said. “I felt like a Christmas tree with Christmas ornaments hanging. It was bad.”
After about a month at home, Olsen returned to working for UR Medicine. The following July, she returned to Highland so the surgeon could finish reconstructing of her breasts.
In addition to undergoing surgery for her cancer, Olsen takes Anastrozole, an aromatase inhibitor that reduces the risk that her cancer will return. Though her disease is in remission, the drug’s side effects pack quite a punch.
“While keeping the reoccurrence of the disease at bay, it also negatively causes me joint pain, hot flashes, trigger fingers, osteopenia and weight gain,” Olsen said. “That tiny pill causes a lot of problems.”
Osteopenia, a reduction of bone density, can make the bones more prone to breaking. To counteract this side effect of her cancer treatment, Olsen receives injections of the medication Prolia every six months and takes vitamin D each day.
Trigger finger is a painful condition that makes your fingers or thumb lock when you bend them.
“You have to move them with your other hand to unlock them,” Olsen said. “It does cause pain.”
Physical therapy and regular injections of steroids have given Olsen normal use of most of her fingers, but three on her right hand required surgery. She now has normal use of both of her hands.
Olsen initially refused to reach beyond her circle of friends and family for support. Then, on the first anniversary of the day her cancer was found to be in remission, she punched the address of a local bicycle shop into her GPS and set off the buy a new bike. The GPS malfunctioned and she found herself parked in front of the Breast Cancer Coalition of Rochester’s offices on Rochester’s University Avenue.
“Recalling how scared and anxious I was when I was newly diagnosed, I now saw a beacon of hope,” she said. “I ran inside and introduced myself.”
Through the nonprofit, Olsen has been able to learn more about her disease and the way to life fully as a survivor. She’s also been able to attend therapy and support groups, dance classes and exercise classes for survivors like herself.
“The coalition has altered my perceptions of the disease, and has literally enhanced my life,” Olsen said.
She also volunteers for the Breast Cancer Coalition as an advocate for better treatment of those who suffer from breast cancer. Right now, the nonprofit is trying to convince the US Senate to pass the Metastatic Breast Cancer Access to Care Act.
Under current law, those who have been diagnosed with metastatic breast cancer — breast cancer that has spread to other parts of the body — usually have to wait until five months after the disease has been discovered to begin receiving Social Security Disability Income benefits and an additional 24 months before they are eligible for Medicare. For some who are living with metastatic breast cancer, the waiting periods are too long.
“It takes so long that by the time they get approved, it’s too late to get proper care,” Olsen said.
The Metastatic Breast Cancer Access to Care Act, which has bipartisan support in the Senate, would eliminate those waiting periods. Whenever possible, Olsen pushes local politicians to express their support for the act.
“Women should not have to wait so long,” she said.
Olsen currently works as nurse for UR Medicine at the nonprofit’s Center for Perioperative Medicine. When on the job, she tries to give the cancer patients she works with the benefit of her experiences as a breast cancer survivor. She’s also ready to tell them about the Breast Cancer Coalition’s programs and the treatment options that UR Medicine offers to those who have been diagnosed with the dread disease.
“If I can make a little bit of a difference, I did a great big thing,” she said.
Each time she starts work, Olsen powers up her computer and reads the message that she’s programmed it to show.
“I am a warrior. I had the armor of bravery and strength. I conquered cancer with all my might and I won the battle!”
When cancer strikes, you could easily go into debt, even with health insurance in place, according to a new survey from the American Cancer Society.
The survey, based on responses from nearly 1,300 cancer patients and survivors from March 18 through April 14, found that 47% had medical debt. Half of those respondents said that debt exceed $5,000.
Two-thirds had struggled with debt for more than a year and a third had dealt with it for more than three years.
Almost all — 98% — said they had health insurance when their debts began mounting.
“While people are insured, sometimes they don't have very good insurance,” Arthur Caplan, head of the division of medical ethics at NYU Langone Medical Center in New York City, told NBC News.
He said many cancer patients with medical debt have high-deductible insurance plans in which a lot of expenses need to be paid for out-ofpocket before coverage kicks in.
But cancer care can stretch even gold-plated insurance plans, Caplan added.
“These cancer treatments can go on and on,” he said. “They can also
cost a lot of money for diagnostic testing, genetic testing, and pretty soon you say, 'Well, I have a policy of a million dollars and it's gone.' "
Karen Knudsen is CEO of the American Cancer Society. Speaking with NBC News, she noted that the new survey uncovered significant disparities, with Black and Hispanic patients more likely to fall into medical debt than whites.
Medical debt also hits the young particularly hard: Nearly three-quarters of patients aged 35 to 44 were behind on health care bills, the survey found.
“We were really dismayed to see that,” Knudsen said. “That strain has been shown to be durable in their lifetime, impacting their choices, their ability to take jobs and of their choice to have a life that they would like.”
Besides the financial and emotional strain that debt incurs, health care can also suffer, she said. Many patients end up skipping cancer screenings or medications due to cost, Knudsen explained.
The bottom line, she said, is that even with insurance, "cancer care is really devastating to people's financial position.”


















Nonprofit donates more than a half a million to cancer patients
By Stefan Yablonski
It all started with a chicken barbecue. Embrace Your Sisters (EYS) provides emergency financial support for residents with breast cancer within 13 New York counties. Founded in 2006, it honors a woman who was diagnosed with breast cancer.
“She worked and had insurance — but as she was going through her treatment, she was finding that

she was picking her treatments ala carte because she couldn’t afford them,” said Krista Jackson, a board member of EYS. “And so, a group of her girlfriends said, ‘if you’re going through this and you have insurance, then there has to be plenty of others that have breast cancer and are going through the same thing.’”
They started with a chicken barbeque to they raised funds. It’s mor-

phed into two signature events they do every year to raise funds. One is a fashion show, held in May. They also do a walk called Positively Pink.
“It’s always held the last Sunday in September,” she added.
EYS is a completely 100% volunteer organization.
“The money we take in goes directly back into the hands of applicants,” Jackson said.
People apply through an application, which is reviewed by a committee.
“If we are able to grant someone financial assistance, we grant funding to pay for things such as utilities, rent, mortgage, cell phone bills, medical co-pays, car payments and car insurance — things that basically keep your financial situation afloat while you focus on your treatment,” she explained. “We do grant funding one time a calendar year. So the first three times that we help you, we can consider any types of bills, except credit card bills. If you come to us

a fourth year for assistance, we can only consider medical bills.”
“I can’t disclose exactly what we do give out; but it’s very generous. It’s not just a couple hundred dollars,” she said. “We have given out, I think, more than a half a million over the years we’ve been doing this.”
Some people donate to EYS during the annual giving campaign, which is in October.
“Some people just pick us to make a donation any time,” she said. “We’re the lucky recipient of a lot of donations — a lot of schools do projects. A soccer team does a pink out game. We have a swim team that’s going to do a pink out swim meet. Kids will wear pink garb and they’ll solicit donations and give them to us. We just had a benefit golf tournament at a local golf course.”
They’re all volunteers; a group of

Jackson about seven people right now — “a lot of us are still working full-time jobs. We have a couple retirees, but the rest of us are all still working folk,” she said. EYS, which is based in Canandaigua, uses the federal poverty level as a guideline. So there is a financial piece that you’d have to disclose, she said.
For more information, visit www. embraceyoursisters.org or send an email embraceyoursisters@yahoo. com or call 585-624-9690.
Frank Guido couldn’t be happier he had a choice for treating his prostate cancer!

To hear more of Frank’s story and learn if CyberKnife is right for you, visit hoacny.com

Frank chose non-surgical CyberKnife® at HOA –offering 5 treatments instead of 35!
“The original diagnosis was to treat my prostate cancer with seven weeks of radiation, five days a week. I was kind of upset that I was never given the option of CyberKnife,” said Frank. “The precise radiation achieved by CyberKnife, far fewer treatments, and the personalized care I received from Dr. Chin and his team made my decision an easy one. Better, the treatment was a real success!”
Annual mean wage for a physician assistant in the Rochester area is $124,070
By Deborah Jeanne Sergeant
Veronika McGraw, physician assistant with Rochester Regional Health, moved to the US from Ukraine to attend college. She had always wanted a profession where she could help people.
However, “the options for professions are limited overseas,” she said.
While working on her premed degree at Roberts Wesleyan University, McGraw shadowed a physician assistant in the emergency room, an experience that proved life-changing.
“I was amazed by the job and all the experience people brought to the table,” McGraw said. “It’s been eye-opening and rewarding and seeing all the needs met by PAs in all the specialties.”
primary care,” McGraw said. “As long as you do the master of PA studies, you can specialize with on-thejob training for most specialties.”
She has enjoyed the impact she can have with patients and the responsibility she carries when a
done for a problem. We can consult with supervising physician, but a lot of the time, we really don’t have to.” Currently, nurse practitioners can practice independently and have their own patients. However, McGraw believes that eventually, PAs will move towards that model because of the shortage of physicians.
“We can have a simple issue of a patient noticing a mole and their dermatologist is telling them they can have an appointment in three to four months,” McGraw said. “In the meantime, a patient will come see us and we have the experience and trained medical eye that we can see if it’s something where timing is important versus something that can be seen in three months. We can call our colleague and send a photo to a dermatologist or surgeon. That access can be life-changing for people.”
She completed her master’s degree in physician assistant at Daemen University in Buffalo in 2012. McGraw likes the broad education offered to PAs. Nurse practitioners have similar job duties, “but we can go between different specialties and
patient comes for an appointment.
“As a PA you have to handle whatever is in front of you with your own skills to take care of patients,” McGraw said. “It’s great responsibility to care for patients day to day. We are expected to do what needs to be

She likes working with a primary care office because it helps her build relationships with patients. In turn, that means patients place a great deal of trust in her.
“You’ll have a very positive impact which will have a ripple effect,” McGraw said. “Maybe this will be the day the patient will quit smoking. It affects their family and workplace. When they come back and say they lost 20 pounds we were trying to motivate them to lose, it’s a rewarding thing. If they’re seriously depressed and you refer them to a provider and they get help, it’s like giving them the tools.”


Veronika McGraw is physician assistant with Rochester Regional Health: “It’s been eye-opening and rewarding and seeing all the needs met by PAs in all the specialties.”
According to the Bureau of Labor Statistics, the annual mean wage for a physician assistant in the Rochester area is $124,070. Their employment can include hospitals, doctors’ offices, surgical centers, specialty offices and at institutions such as schools.




By Grace R. Scism
Melissa Mueller-Douglas was raised in Rochester by a mother who is white and from the United States and until the age of 3, a father who is Black and from the Cayman Islands.
Throughout her youth, she often struggled with a sense of belonging.
“I thought that was a personal struggle. But later learned, as I went to college and started a career, that it’s not a ‘me thing;’ it’s a ‘we thing,’” she said.
Trained as a licensed master social worker, Mueller-Douglas’ origin story was the impetus for her business, MYRetreat — a place where people could gain a sense of belonging and connection and feel supported.
At her brick-and-mortar space in East Rochester, Mueller-Douglas would welcome individuals, who typically didn’t know anyone else in the room, for a one-hour mindfulness experience.
“People would say, ‘I’ve never spoken with someone with this background or from this place,’’’ Mueller-Douglas said. “They realized they had more in common than they had

In the MYRetreat app, a Bonafide Collective chocolate subscription is offered so participants can enjoy a small piece of chocolate during their three-minute mindfulness sessions. Photo credit: Beatrice Correea
late,” she explained.
Mueller-Douglas calls this concept “habit stacking,” where you use something that you already love and enjoy as a tangible reward.
She has even joined the Fine Chocolate Industry Association so that she can meet different chocolate makers and connect with those that are paying fairly throughout the supply chain.
“They care about the farmers and sustainability aspect in the way they do business, which is very important to me,” she said.
Mueller-Douglas wanted to bring the chocolate mindfulness experience to more people and began to serve groups from the same company or organization to help perpetuate a positive workplace culture.
“People in leadership roles and human resources have the capacity to curate spaces to make those bonds happen, to help people feel closer and more connected and supported,” she said.
people’s faces light up because it’s chocolate!”
While the MYRetreat business was built on an one-hour experience and then daily meditations through the app, the experience left some clients wanting more. At the start of 2024, Mueller-Douglas added a question to her post workshop survey, “Would you like to come to a retreat in the Cayman Islands?” Well, as one might imagine, a lot of people checked that box.
“I always dreamed of bringing chocolate mindfulness to Grand Cayman,” said Mueller-Douglas, who has many relatives there. “[I want] to be able to bring people to my people and have them connect with our intention, which for this retreat is ‘Be Boldly Confident.”
different from each other, which was really inspiring to me.”
Mueller-Douglas’ mindfulness retreats are unique in that she starts each session with a piece of chocolate.
“I lead with chocolate. Give people the chocolate and ask, ‘how do you feel while you’re eating it?’ Relaxed, not worrying about anything. OK, that’s our starting point,” she said.
In fact, at the first chocolate mindfulness retreat, participants enjoyed a slice of Cheesy Eddie’s chocolate cheesecake.
“They weren’t thinking about the past. They weren’t worrying about the future. It was all about the cheesecake!” Mueller-Douglas said.
Realistically, there’s no way one could indulge in a piece of chocolate cheesecake every day, so she began incorporating small pieces of chocolate instead.
“I wanted to create an experience so that when you see a piece of chocolate, you remember to prioritize yourself by doing a meditation. Do something good for yourself and then gift yourself that piece of choco-
During the pandemic, Mueller-Douglas held virtual chocolate mindfulness retreats allowing her to make even more connections and build a community that would eventually lead to her next goal — a mindfulness application that lets participants experience chocolate mindfulness anytime anywhere. The MYRetreat app is free and offers daily three-minute meditations that mirror her 60-minute workshops. Each day focuses on one area: intention setting, body scan, guided imagery, chocolate mindfulness and gratitude journaling.
She has also partnered with Charmain Jackman, a renowned psychologist who she met through Babson College’s WIN Lab, a 12week virtual accelerator designed for early-stage female business entrepreneurs. Jackman provides the weekend meditations on the app, enhancing its effectiveness in promoting mental well-being.
To further enhance the app experience, MYRetreat offers a chocolate subscription — milk, dark, white or a combination, that can be purchased through the app. Each month’s bag has 33 little pieces of chocolate that participants can keep in their briefcase, desk, purse or wherever and then enjoy one small piece after listening to the daily meditation.
During employee wellness month in June, Mueller-Douglas brought jars of chocolate to different companies and organizations with a code to scan for the app.
“I wanted to uplift the tradition of the month, which I don’t think gets a lot of attention,” she said. “It’s an easy way to say thank you and
When a person’s inner confidence is wavering or they need more support developing it, Mueller-Douglas believes it’s important to get outside of the daily grind and do three things — connect, play and relax.
The retreat will take place March 1-6, 2025 at an intimate, gorgeous resort where there will be a private chef to nourish the group, while Mueller-Douglas nourishes their souls. Guest speakers with whom she has built relationships over the years will be on hand to inspire and educate. There is an application process to attend and the retreat is open to only seven women.
“I want the people who are open to connecting with themselves and with others who are ready to play,” she explained. “I want this to be the most intentional retreat experience of a lifetime where people will go home and will realize how well they treated themselves.”
Mueller-Douglas said she believes mindfulness is a superpower that, whether for a minute or an hour, helps people relax when they need to, gather their thoughts, tether themselves to their intentionality and own values and to recognize how they want to proceed.
“To be mindful is the catalyst for being creative, being present, being whole,” she said.
Mueller-Douglas is married to Ya’qub Shabazz, owner of Sankofa Studios and co-founder of the Ninth Floor Artists Collective. The couple have two children, Nurah, 11, and Nasir, 7.
For more information on MYRetreat, visit www.chocolatemindfulness.co. The MYRetreat mobile app is available in the App Store and on Google Play. For more information on the Grand Cayman retreat, visit https://grandcayman.my.canva.site.
Researchers at University of California San Diego School of Medicine and international collaborators have led a worldwide, advanced study demonstrating the potential of tirzepatide, known to manage Type 2 diabetes, as the first effective drug therapy for obstructive sleep apnea (OSA), a sleep-related disorder characterized by repeated episodes of irregular breathing due to complete or partial blockage of the upper airway.
The results, published in the June 21 online edition of the New England Journal of Medicine, highlight the treatment’s potential to improve the quality of life for millions around the world affected by OSA.
“This study marks a significant milestone in the treatment of OSA, offering a promising new therapeutic option that addresses both respiratory and metabolic complications,” said physician Atul Malhotra, lead author of the study, professor of medicine at University of California San Diego School of Medicine and director of sleep medicine at UC San Diego Health.
OSA can result in reduced oxygen levels in the blood and can also be associated with an increased risk of cardiovascular complications, such as hypertension and heart disease. Recent studies, also led by Malhotra, suggest that the number of OSA patients worldwide is close to 936 million.
Conducted in two Phase III, double-blinded, randomized, controlled trials, the new study cohort involved 469 participants diagnosed with clinical obesity and living with moderate-to-severe OSA. They were recruited from sites in nine different countries, including the U.S., Australia and Germany. Participants either


or did not use continuous positive airway pressure (CPAP) therapy, the most common sleep apnea treatment which uses a machine to maintain an open airway during sleep, preventing interruptions in breathing. Patients were administered either 10 or 15 mg of the drug by injection or a placebo. The impact of tirzepatide was evaluated over 52 weeks.
Researchers found that tirzepatide led to a significant decrease in the number of breathing interruptions during sleep, a key indicator used to measure the severity of OSA. This improvement was much greater than what was seen in participants that were given a placebo. Importantly, some participants that took the drug reached a point where CPAP therapy might not be necessary.
Considerable data suggest that a drug therapy that targets both sleep apnea and obesity is beneficial rather than treating either condition alone.
Additionally, the drug therapy improved other aspects related to OSA, such as reducing the risk factors of cardiovascular diseases and improved body weight. The most common side effect reported was mild stomach issues.


Snoring can be a sign of Sleep Apnea. There are three types of apnea: obstructive, central and mixed; of the three, obstructive is the most common. People with untreated sleep apnea stop breathing repeatedly during the night, maybe hundreds of times.
If you experience any of the following symptoms, you may suffer from a sleep disorder:
• Daytime fatigue
• Morning drowsiness
• Insomnia
• Gasping for breath in the middle of the night
• Snoring
Can lead to:
• High blood pressure
• Memory problems
• Impotence
• Cardiovascular disease
• Weight gain
• Headaches
• Depression
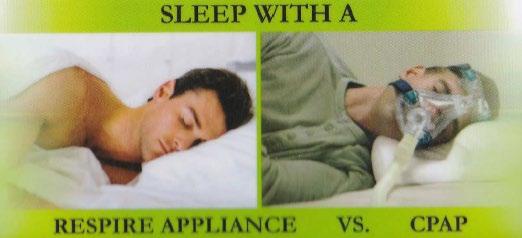
Oral Sleep Appliance
Oral Sleep Appliances can be used to treat sleep apnea and snoring. This is a customized oral device worn by patients during the night to maintain an open airway (reducing snoring and sleep apnea).





By Holly Carmona
It may sound odd, but if you're admitted for inpatient rehab services at St. Ann's Community, we start planning your discharge the day you arrive.
It's true. Our goal, from the day you arrive from the hospital, is to return you to your previous level of activity, get you home safely as soon as possible, and help you avoid a return to the hospital.
That much is clear.
But the question many people have is, “What's the process for getting out of the hospital and into rehab, and what role does Medicare play?”
Let's walk through the steps.
Let's say you've had hip surgery and the hospital is recommending a short-term rehab stay. The hospital's clinical team will provide documentation of your need for rehab to your insurance provider. This includes documentation of your:
• Medical history
• Current medical event (the reason you were hospitalized)
• Your baseline level of function, and
• Your current level of function.
If your insurer determines that you qualify, they will authorize the stay (granting “prior authorization”) and you're cleared to enter rehab.
For people age 65 and older who've received prior authorization, the cost of inpatient rehab services is covered by Medicare. Those services include physical therapy, occupational therapy, speech-language pathology, meals, nursing services and prescription drugs.
Medicare is the national health insurance program administered by the Centers for Medicare & Medicaid Services. It covers people aged 65 or older, as well as others who meet specific eligibility criteria.
Now the tricky part: Medicare coverage is not guaranteed for the duration of your rehab stay. Coverage is determined based on your daily participation in therapy and demonstrated progress toward your recovery goals.
Upon entering rehab, you will
be visited by the members of your care team. At St. Ann's, this includes professionals from our medical, therapy, nursing and social work departments as well as others depending on your needs. Working with you and your family, the team will develop a discharge plan with goals to reach to ensure you can return home safely.
This is important: To continue qualifying for Medicare coverage (“continued stay coverage” in technical terms), you must actively participate in therapy and demonstrate progress toward those goals. If for whatever reason you do not participate, coverage will end.
Also important, and something many people misunderstand: while Medicare does provide “continued stay coverage” for up to 100 days, it is not unlimited coverage for that whole period. You'll have no copays or deductibles for up to your first 20 days in rehab, including all equipment, supplies, medications and nursing care. However, from day 21 to day 100, you will be responsible for a daily co-pay per Medicare guidelines (in general, roughly $200 per day). Be sure you and your family don't misinterpret this.
And don't forget: where you go for rehab is up to you. If you preplan your stay at the rehab facility of your choice, you can be sure there will be a room waiting for you. You won’t have to worry about making last-minute decisions or settling for someplace that doesn’t meet your needs. Contact the admissions office of your preferred rehab center to preplan your stay.

Holly Carmona is an Admissions Nurse at St. Ann's Community. She can be reached at hcarmona@ mystanns.com. For more information about rehab at St. Ann’s, scan the QR code.
If you receive Social Security, you can help to make sure we pay you the right benefit each month. You can do that by telling us about relationship or other life changes that could affect your eligibility for retirement, survivors, or disability benefits – or the benefit amount.
You and your family may miss out on additional payments you may be due if you don’t report changes to us in a timely manner. Or you may be overpaid benefits and have to pay us back. What you need to tell us
To make sure you are paid correctly and receive the payments for which you are eligible, let us know right away if:
• You get married or divorced.
• Your spouse or former spouse dies.
• You become the parent of a child (including an adopted child).
• The child (or stepchild) who gets benefits on your record gets married.
• The child (or stepchild) who gets benefits on your record no
longer lives with you. Note: We will need the name and address of the person with whom the child is living. How to report changes
We offer several ways to report changes:
• Call us at 1-800-772-1213 (TTY 1-800-325-0778), Monday to Friday, 8:00 a.m. to 7:00 p.m.
• Call your local Social Security office.
• Fax, mail, or deliver your updates to your local office.
You can use our office locator at www.ssa.gov/locator to find your local office.
If you get retirement, survivors, or disability benefits and need to update your address, phone number, or direct deposit, it’s easy to make those changes using your personal my Social Security account www. ssa.gov/myaccount. Or you can use our automated telephone services at www.ssa.gov/agency/contact/ phone.
Get the right check, in the right amount, at the right time, by reporting changes right away!

By Jim Miller
Dear Savvy Senior,
What are the early signs and symptoms of diabetes? I’m 60 years old, and in pretty good shape, but was just diagnosed with Type 2 diabetes. What did I miss?
Diabetic Dan
Dear Dan,
The signs and symptoms of Type 2 diabetes can be so mild that many people miss them. That’s why testing is so important.
Here’s what you should know.
According to the Centers for Disease Control and Prevention, more than 38 million Americans have diabetes today, and another 97 million have prediabetes, but many of them don’t even know they have it.
Type 2 diabetes is a disease that develops slowly over decades. Most people have prediabetes for a long time before the disease becomes full-blown diabetes and, even then, it progresses gradually.
Diabetes occurs when your blood glucose, also called blood sugar, is too high. This excess blood sugar damages blood vessels and affects circulation, putting you at risk for a host of ailments, from heart attack and stroke to blindness, kidney failure and nerve damage.
So how can you tell if you have diabetes?
The earliest signs, which are usually subtle, including urinating more frequently (often at night), being thirster and hungrier than usual, weight loss without trying, feeling very tired, having dry itchy skin and blurry vision.
And the symptoms that can indicate advanced diabetes and longterm damage has occurred includes cuts or sores that heal slowly, having more infections than usual, and pain or numbness in your feet or legs.
Because prediabetes typically causes no outward symptoms, and the signs of early Type 2 diabetes can easily be missed, the only way to know for sure if you have it is to get a blood test.
Everyone age 45 years or older should consider getting tested for diabetes, especially if you are overweight with a body mass index (BMI) above 25. See CDC.gov/bmi to calculate your BMI.
If you are younger than 45 but are overweight or have high blood pressure, a family history of diabetes, or belong to an ethnic group (Latino, Asian, African or Native American) at high risk for diabetes, you should get checked too.
To help you determine your risk for diabetes, the American Diabetes Association (ADA) has a quick, online risk test you can take for free at Diabetes. org/risk-test.
There are three different tests your doctor can give you to diagno sis diabetes. The most common is the “fasting plasma glucose test,” which requires an eight-hour fast before you take it. There’s also the “oral glucose tolerance test” to see how your body processes sugar, and the “hemoglobin A1C test” that measures your average blood sugar over the past three months. It can be taken anytime regardless of when you ate.
Most private health insurance plans and Medicare cover diabetes tests, however, if you’re reluctant to visit your doctor to get tested, an alternative is to go to the drug store, buy a blood glucose meter and test yourself at home. They cost around $20.



If you find that you are prediabetic or diabetic, you need to see your doctor to develop a plan to get it under control. In many cases lifestyle changes like losing weight, exercising, eating a healthy diet and cutting back on carbohydrates may be all you need to do to get your diabetes under control. For others who need more help, many medications are available.
For more information on diabetes and prediabetes or to find help, join a lifestyle change program recognized by the CDC (CDC.gov/diabetes-prevention). These programs offer in-person and online classes in more than 1,500 locations throughout the U.S.

Send your senior questions to: Savvy Senior, P.O. Box 5443, Norman, OK 73070, or visit SavvySenior. org. Jim Miller is a contributor to the NBC Today show and author of “The Savvy Senior” book.









Maura Snyder has been appoint

ed as Highland Hospital’s new chief operating officer.
In this role, Snyder will be responsible for a range of duties, including overseeing patient-care services, clinical departments and ancillary-support services; facilitating the achievement of hospital goals through a multidisciplinary approach to problem-solving; and fulfilling the hospital’s commitment to patientand family-centered care.
Snyder brings more than 25 years of healthcare leadership experience to this position. Most recently, she served as associate chief operating officer at Rochester General Hospital. Before that, she served as vice president of operations, eastern region, and senior director of operations at Clifton Springs Hospital and Clinic/ Newark-Wayne Community Hospital.
“Highland Hospital is a special community asset, and we are pleased that Maura Snyder will be our next COO,” said Steve Goldstein, Highland Hospital President and CEO. “We identified Maura as the best candidate following an extensive national search, and we thank the search committee for their efforts and commitment throughout this process.”
Kathy Parrinello, incoming Highland Hospital president and CEO, said, “Maura Snyder is a dynamic, results-driven healthcare leader, and I am excited to work with her to lead Highland Hospital into the future. Working together, we will further Highland’s mission as an academic
community hospital that delivers outstanding, compassionate patient care.”
Snyder earned her master’s degree in health administration from Roberts Wesleyan College and her bachelor's degree in management from Grove City College in Pennsylvania.
Physician Mary Wilsch has been

Mary Wilsch appointed as Highland Hospital’s new chief of obstetrics and gynecology.
Wilsch has practiced at Highland and Genesee Valley Obstetrics and Gynecology for more than a decade. Previously, she practiced with Rochester Gynecologic and Obstetric Associates before relocating to Syracuse.
A graduate of SUNY at Buffalo School of Medicine & Biomedical Sciences, Wilsch earned her bachelor’s degree in nursing from D’Youville College. She completed her residency in obstetrics and gynecology at the University of Rochester, receiving numerous awards for teaching, research and compassionate care, including the residency teaching awards for OB-GYN in 2014, 2015 and 2021 and for family medicine in 2017 and 2019.
“Dr. Wilsch is known to be an excellent clinician, a collaborative colleague and an exceptional teacher,” said physician Eva Pressman, Henry A. Thiede professor and chair of the department of obstetrics and gynecology at the University of Rochester Medical Center. “We look forward to seeing OB-GYN grow under her leadership.”


Sherri Salvato has joined HCR

Home Care as human resources director. In this role, reporting to the agency’s senior director of human resources, she is responsible for employee relations.
Salvato brings to the position more than 30 years of HR leadership experience and a passion for home care.
Most recently, she served as human resources, payroll and listings manager at High Falls Sotheby’s International Realty. Previous roles also included serving as vice president of human resources at another home care agency and as human resources manager at Nextel Communications.
Salvato studied business administration at Alfred State, and she is a licensed real estate agent. She resides in Irondequoit.
Bethany Miller, a family nurse

practitioner, recently joined Victor Family Practice, an affiliate of UR Medicine Thompson Health’s F.F. Thompson Hospital. A Naples native currently residing in Victor, Miller obtained her Bachelor of
Master of Science in advanced practice nursing as a family nurse practitioner from St. John Fisher University in Rochester.
Certified by the American Nurses Credentialing Center, Miller has worked as a family nurse practitioner in the region for 17 years, with the past 15 spent within Highland Family Medicine and Highland Family Planning.
Stephanie Friel, a family nurse

practitioner, recently joined The Mary Clark Thompson Family Practice, an affiliate of F.F. Thompson Hospital located at the Sands Family YMCA in Canandaigua. A Canandaigua resident, Friel received her Master of Science in nursing, as a family nurse practitioner, from Upstate Medical University (SUNY Upstate) in Syracuse. She has a Bachelor of Science in nursing from Roberts Wesleyan College and is a graduate of the registered nursing program at Finger Lakes Community College. She is certified by the American Nurses Credentialing Center.
Friel first joined Thompson as a nurse assistant, later becoming a floor nurse and then a charge nurse. From 2008 through 2015, she was nurse leader of a medical-surgical unit. After becoming a service line coordinator for Thompson’s quality and safety department, she served for the past seven years as the quality improvement coordinator for the department.

ELEMENTAL MANAGEMENT GROUP
Hybrid Nurse Aide Training Program
Hybrid Nurse Aide Training Program
Hybrid Nurse Aide Training Program ELEMENTAL MANAGEMEN UP




Hybrid Nurse Aide Training Program ELEMENTAL MANAGEMENT GROUP
















OUP
MANAGEMENT GROUP

Equip your facility with our unstoppable HYBRID CNA program, empower your team to deliver top-notch care with the strength of a champion.
Equip your facility with our unstoppable HYBRID CNA program, empower your team to deliver top-notch care with the strength of a champion.
Equip your facility with our unstoppable HYBRID CNA program, empower your team to deliver top-notch care with the strength of a champion.
Equip your facility with our unstoppable HYBRID CNA program, empower your team to deliver top-notch care with the strength of a champion.
Are you looking for an innovative way to attract CNA students? We have your answer
Are you looking for an innovative way to attract CNA students? We have your answer
Are you looking for an innovative way to attract CNA students? We have your answer
Are you looking for an innovative way to attract CNA students? We have your answer
Are you looking to minimize and most importantly eliminate agency use? We have your solution
Are you looking to minimize and most importantly eliminate agency use? We have your solution
Are you looking to minimize and most importantly eliminate agency use? We have your solution
Are you looking to improve morale by increasing your direct care PPD? Reach out to us to hear more
Are you looking to minimize and most importantly eliminate agency use? We have your solution
Are you looking to improve morale by increasing your direct care PPD? Reach out to us to hear more
Are you looking to improve morale by increasing your direct care PPD? Reach out to us to hear more
Are you looking to improve morale by increasing your direct care PPD? Reach out to us to hear more
Are you looking to captivate and motivate the newer generation by offering unique and rewarding training opportunities? Look no further contact us today
Are you looking to captivate and motivate the newer generation by offering unique and rewarding training opportunities? Look no further contact us today
Are you looking to captivate and motivate the newer generation by offering unique and rewarding training opportunities? Look no further contact us today
Are you looking to captivate and motivate the newer generation by offering unique and rewarding training opportunities? Look no further contact us today
CONTACT:

Peg Reith BSN, RN
CONTACT:
Phone: 315-529-3267
CONTACT:
Peg Reith BSN, RN
CONTACT:
Phone: 315-529-3267
Email: CNA_Training@elementalmgt.com
Peg Reith BSN, RN
Email: CNA_Training@elementalmgt.com
Phone: 315-529-3267
Peg Reith BSN, RN
Phone: 315-529-3267
Email: CNA_Training@elementalmgt.com
Email: CNA_Training@elementalmgt.com




















