Melissa Badowski, PharmD, MPH, FCCP, FIDSA, BCIDP, BCPS, AAHIVP
Clinical Associate Professor
Section of Infectious Diseases
Pharmacotherapy
Department of Pharmacy Practice
University of Illinois at Chicago, College of Pharmacy
Chicago, Illinois
HOW TO OBTAIN CREDIT
Lucas Hill, PharmD, AAHIVP
HIV/HCV Pharmacist Specialist

University of California San Diego Owen Clinic
San Diego, California
Jonathan M. Schapiro, MD
Head of HIV/AIDS Clinic
Israeli Ministry of Health National Hemophilia Center at Sheba Medical Center
Tel Aviv, Israel
Launch: August 25, 2023
Expiration: August 25, 2024
Participants must complete the preactivity questionnaire, complete and receive a minimum score of 70% on the posttest, and complete the program evaluation online at www.ExchangeCME.com/HIVPharmacyMonograph.
Estimated time to complete this activity is 2 hours.
This activity is jointly provided by Global Education Group and Integritas Communications. This activity is supported by an educational grant from Gilead Sciences, Inc.
EMERGING ISSUES IN HIV MANAGEMENT: ANSWERS TO PHARMACISTS’ COMMON QUESTIONS
PROGRAM DESCRIPTION
Pharmacists play many roles in the management of HIV, thus it is essential they remain up to date as the HIV field continues to advance and patients grow more complex. This activity discusses the importance of and strategies for rapid antiretroviral therapy (ART) initiation, the indications for and implementation of long-acting injectable (LAI) ART, the interpretation of resistance testing, and the complex therapeutic decision-making processes involved in designing active ART regimens for heavily treatmentexperienced (HTE) patients with HIV.
TARGET AUDIENCE
The educational design of this activity addresses the needs of clinical, specialty, and managed care pharmacists and pharmacy benefits managers involved in the care of patients with HIV infection.
EDUCATIONAL OBJECTIVES
After completing this activity, the participant should be better able to:
• Review requirements and options for rapid ART initiation
• Identify the pharmacist’s role within clinic protocols for common HIV management scenarios, such as initiating rapid ART and implementing long-acting injectables
• Describe procedures for long-acting injectable treatment initiation and maintenance
• Interpret resistance test results in HTE patients with multidrug resistance
• Discuss the most appropriate treatment regimens for HTE patients experiencing virologic failure or those who want to simplify their regimen
PHARMACIST ACCREDITATION STATEMENT
Global Education Group is accredited by the Accreditation Council for Pharmacy Education as a provider of continuing pharmacy education with Commendation.
CREDIT DESIGNATION
Global Education Group designates this continuing education activity for 2.0 contact hour(s) (0.2 CEUs) of the Accreditation Council for Pharmacy Education (Universal Activity Number - 0530-9999-23-053-H02-P)
This is an application-based activity.
GLOBAL EDUCATION GROUP CONTACT INFORMATION
For information about the accreditation of this program, please contact Global Education Group at 303-395-1782 or cme@ globaleducationgroup.com.
INSTRUCTIONS TO RECEIVE CREDIT
In order to received credit, participants must complete the following:
• Read the educational objectives, accreditation information, and faculty disclosures at the beginning of this activity.
• Complete the Preactivity Questions.
• Review the activity content.
• Achieve a grade of 70% on the Postactivity Test Questions and complete the Evaluation.
• CE credits will be uploaded to CPE Monitor within 60 days of completion.

FEE INFORMATION & REFUND/CANCELLATION POLICY
There is no fee for this educational activity.
DISCLOSURES OF RELEVANT FINANCIAL RELATIONSHIPS
Global Education Group adheres to the policies and guidelines, including the Standards for Integrity and Independence in Accredited CE, set forth to providers by the Accreditation Council for Continuing Medical Education (ACCME) and all other professional organizations, as applicable, stating those activities where continuing education credits are awarded must be balanced, independent, objective, and scientifically rigorous. All persons in a position to control the content of an accredited continuing education program provided by Global Education Group are required to disclose all financial relationships with any ineligible company within the past 24 months to Global Education Group. All financial relationships reported are identified as relevant and mitigated by Global Education Group in accordance with the Standards for Integrity and Independence in Accredited CE in advance of delivery of the activity to learners. The content of this activity was vetted by Global Education Group to assure objectivity and that the activity is free of commercial bias.
All relevant financial relationships have been mitigated. The faculty have the following relevant financial relationships with ineligible companies:
Melissa Badowski, PharmD
Nothing to disclose.
Lucas Hill, PharmD Speakers’ Bureau: Gilead Science, ViiV Healthcare
Jonathan M. Schapiro, MD Consulting Fee (e.g., Advisory Board): Gilead Sciences, GlaxoSmithKline, Merck, Moderna, Pfizer, TibotecJanssen, Teva, ViiV Healthcare
Honoraria: Gilead Sciences, GlaxoSmithKline, Merck, Moderna, Pfizer, Tibotec-Janssen, Teva, ViiV Healthcare
The planners and managers at Global Education Group and Integritas Communications have no relevant financial relationships to disclose.
DISCLOSURE OF UNLABELED USE
This educational activity may contain discussion of published and/or investigational uses of agents that are not indicated by the FDA. Global Education Group and Integritas Communications do not recommend the use of any agent outside of the labeled indications.
The opinions expressed in the educational activity are those of the faculty and do not necessarily represent the views of any organization associated with this activity. Please refer to the official prescribing information for each product for discussion of approved indications, contraindications, and warnings.
DISCLAIMER
Participants have an implied responsibility to use the newly acquired information to enhance patient outcomes and their own professional development. The information presented in this activity is not meant to serve as a guideline for patient management. Any procedures, medications, or other courses of diagnosis or treatment discussed in this activity should not be used by clinicians without evaluation of patient conditions and possible contraindications on dangers in use, review of any applicable manufacturer’s product information, and comparison with recommendations of other authorities.
Introduction
Great strides have been made in HIV management and outcomes in the last 30 years. With the introduction of combination antiretroviral therapy (ART), HIV infection rates have been decreasing, along with the morbidity and mortality rates associated with HIV infection. Unfortunately, despite numerous initiatives, such as “Getting to Zero” and “Undetectable=Untransmittable” (U=U), and the implementation of pre-exposure prophylaxis (PrEP), the incidence of HIV infections has remained high in certain risk groups such as young Black men who have sex with men [MSM] and in certain geographic areas, including the southern US.1,2 This highlights the challenges in HIV management that still exist, such as engagement and retention in care and achieving and maintaining virologic suppression across all patient populations, especially those that struggle with adherence to ART. Moreover, the prevalence of people living with HIV (PWH) is increasing because people are living longer with HIV.3 Therefore, health care providers (HCPs) have to consider the comorbidities that occur with normal aging, along with the comorbidities that occur as a result of living with HIV. HIV management is complex in and of itself and the presence of age-related comorbid conditions can increase the risk of adverse events (eg, drug-drug interactions [DDIs]), accenting the need for effective communication among subspecialists and carving out a distinct role for pharmacists on multidisciplinary teams.
Although ART has been the mainstay of HIV treatment for decades, it has continuously evolved to increase rates of virologic suppression and reduce morbidity and mortality through more-effective and -tolerable regimens (eg, fewer and smaller pills, fewer side effects). Among key recent advances are antiretroviral (ARV) therapies with high barriers to resistance that allow for same-day initiation of ART, long-acting injectable (LAI) formulations, and advances in pharmacologic options for heavily treatment-experienced (HTE) PWH. Rapid ART is an important strategy to engage patients in health care as early as the day of HIV diagnosis, to quickly achieve virologic suppression, therefore improving outcomes and reducing transmission. Research and development advances have added 2 LAI injectable options to the ARV armamentarium. These LAI ARVs combat some of the barriers to ART adherence (eg, pill burden), and 1 option provides a novel mechanism of action to overcome drug resistance in HTE PWH. However, to capitalize on the benefits afforded by these strategies and treatment options, it is necessary to employ a multidisciplinary team to meet the complex needs of the expanding and aging HIV population. With their breadth of knowledge and experience, pharmacists are an integral part of HIV care teams across all clinical settings. Therefore, the following educational content was designed to provide clinical and managed care pharmacists the information they need and the strategies they can employ to facilitate rapid initiation of ART, implementation of LAI ART, and optimization of complex ART regimens in HTE patients with HIV to improve outcomes.
PART 1: Rapid
Antiretroviral Therapy
Why is rapid initiation of ART important?
The Ending the HIV Epidemic (EHE) initiative aims to achieve reductions in new HIV infections in the US of 75% by 2025 and at least 90% by 2030. Globally, the Joint United Nations Program on HIV/AIDS has set a goal of 95-95-95: 95% of PWH to know their HIV status, 95% of people with diagnosed HIV infection to receive ART, and 95% of all people receiving ART to have viral suppression by 2025.4,5 Based on the goals of these initiatives, decreasing new HIV infections and increasing the uptake of test-and-treat strategies have been prioritized. Additionally, results of the START and TEMPRANO trials support expanded HIV guideline recommendations to initiate ART in all PWH, regardless of CD4+ count.6,7 Rapid initiation of ART after diagnosis, defined as same day (immediate start) or at least within a week, reduces the incidence of both AIDS- and nonAIDS–related events through faster and improved rates of virologic suppression.6 By achieving an earlier undetectable viral load (VL), rapid ART can decrease HIV transmission rates (eg, U=U). Additionally, there are some data suggesting that rapid ART improves linkage to care (Table 1).8
The RapIT trial was the first study to evaluate rapid ART initiation compared with standard management and demonstrated that significantly more patients in the rapid arm achieved virologic suppression compared with patients in the standard of care arm.9 In the CASCADE trial, same-day home-based ART initiation after new HIV diagnosis increased rates of linkage to care within 3 months and virologic suppression at 12 months compared with standard of care management.10 The RAPID trial evaluated rapid ART initiation in a high-risk population of patients where 51% had substance use disorder, 48% had a major mental health disorder, and 31% were unstably housed. With more patients in the early referral group achieving virologic suppression than the delayed referral group, this model demonstrated that rapid initiation of ART was not only beneficial, but that it could be achieved even in the presence of barriers.11 The DIAMOND trial evaluated rapid ART initiation with darunavir (DRV)/cobicistat (COBI)/emtricitabine (FTC)/tenofovir alafenamide (TAF) in a patient population that was 75% young MSM, which is similar to the current US population with the highest incidence of new HIV diagnoses. Virologic suppression (<50 copies [c]/mL) was achieved in 84% of patients at week 48 and there were no DRV or TAF resistance–associated mutations (RAMs) observed.12 These published studies demonstrate the benefits of rapid ART in multiple patient populations in terms of increased virologic suppression and linkage to care. It is important to note that all of these studies used different definitions of rapid ART.
3
TABLE 1. Pertinent Published Studies Evaluating the Effectiveness of Rapid ART on Outcomes
Rapid Initiation of Treatment (RapIT)9
CASCADE10 RAPID11 DIAMOND12
Location South Africa Lesotho, Africa Ward 86 Clinic, San Francisco, California, US US
• Unblinded RCT
Study Design
Time to ART Initiation
Outcome(s)
• May 2013-August 2014
• Standard of care (n=190): visit 6*
• Rapid ART (n=187): visit 1*
• Both groups started within 90 days of study enrollment
• Virologic suppression (≤400 c/mL) at 10 months
• Multicenter openlabel RCT
• February-July 2016
• Standard of care (n=137): minimum of 2 monthly clinic visits before ART initiated
• Rapid ART (n=137): ART initiation same day as diagnosis
• Virologic suppression (≤100 c/mL) at 12 months
• Retrospective review of clinic-based cohort
• July 2013-December 2017
• Delayed referral (n=26): ART initiation 30 days to 6 months after diagnosis
• Early referral/rapid ART (n=190): ART initiation within 30 days of diagnosis
• Virologic suppression (<200 c/mL) at last measurement
• Prospective, phase 3, open label, single arm, multicenter
• DRV/COBI/FTC/TAF
• ≤2 weeks from HIV diagnosis
• 64% of patients in the rapid ART arm compared with 51% of patients in the standard of care arm (RR 1.26; 95% CI, 1.05-1.50)
• 50.4% of patients in the rapid ART arm compared with 34.3% in the standard of care arm (P<0.007)
• Linkage to care within 3 months: 68.6% of patients in the rapid ART arm compared with 43.1% in the standard of care arm (P<0.001)
Other programs where virologic suppression and linkage to care have been evaluated include the Rapid Entry and ART Clinic for HIV (REACH) program and the CrescentCare Start Initiative (CCSI).13,14 The REACH program retrospective cohort study demonstrated that rapid entry was feasible and had a positive impact on HIV transmission at the population level. Time to first attended provider visit decreased from 17 to 5 days and time to ART initiation decreased from 21 to 7 days when rapid ART was initiated, compared with usual care (P<0.0001).13 The CCSI focused on enhancing navigation, expediting clinic intake, and initiating rapid ART, resulting in 92% of patients being linked to care and starting ART within 72 hours of diagnosis. As compared
• 93.7% of patients in the early referral group compared with 80.8% of patients in the delayed referral group (P=0.022)
• Virologic suppression (<50 c/ mL) at 48 weeks
• 84% of patients achieved HIV-1 RNA <50 c/mL
with a historical cohort with a mean time to linkage of 30 days and median time to viral suppression (<200 c/mL) of 68 days, the CCSI cohort had a mean time to linkage of 1.3 days and a median time to viral suppression of 30 days (P<0.0001).14 These studies were able to achieve high proportions of rapid ART initiation due to their structure and ability to avoid prior authorizations for ART and other insurance/payment barriers. Together, these two pivotal studies lend support to rapid ART as an important strategy to link newly diagnosed patients with HIV to health care and to rapidly decrease time to viral suppression, resulting in better patient outcomes and reduced HIV transmission.
4 EMERGING ISSUES IN HIV MANAGEMENT: ANSWERS TO PHARMACISTS’ COMMON QUESTIONS
ART, antiretroviral therapy; c, copies; COBI, cobicistat; DRV, darunavir; FTC, emtricitabine; RCT, randomized controlled trial; RR, relative risk; TAF, tenofovir alafenamide.
Which ART regimen should I choose for rapid initiation?
Historically, first-line ART regimens with nonnucleoside reverse transcriptase inhibitors (NNRTIs) were associated with high rates of transmitted drug resistance and eventual virologic failure.15,16 Use of NNRTI-based regimens as first-line ART in newly diagnosed patients with HIV required genotyping, which delayed the initiation of ART and worsened outcomes as a result.16 One of the initial concerns regarding effective rapid ART was the potential for transmitted drug resistance and the possibility of prescribing a regimen that might lead to virologic failure. The development of second-generation integrase strand transfer inhibitors (INSTIs), with their associated high barriers to resistance, has significantly decreased the risk of virologic failure and opened the door for the implementation of rapid ART initiation.
Rapid ART initiation, same day as or within 7 days of diagnosis, can be successful in realizing virologic suppression without fear of transmitted resistance mutations using the Department of Health and Human Services (DHHS)-recommended ART regimens, including oral second-generation INSTI-based regimens. If necessary, ART regimens can be modified based on genotyping once results are obtained.
There are 4 major organizations that provide guidelines for HIV management: DHHS, European AIDS Clinical Society (EACS), International AIDS Society (IAS), and World Health Organization (WHO). These organizations all recommend rapid initiation of ART, although verbiage varies slightly between the guidelines. For example, pertinent to US-based HIV management, both DHHS and International AIDS Society USA (IAS-USA) recommend rapid ART initiation as soon as possible, with preference given to starting the same day as HIV diagnosis.17,18 In addition to recommending immediate ART initiation, DHHS and IAS-USA recommend specific ART regimens that have high barriers to resistance (Table 2).17 In real-world clinical settings, the majority
Recommended for Rapid Start
• BIC/TAF/FTC
– 1 pill PO daily
• DTG + (TAF or TDF) + (3TC or FTC)
– DTG 50 mg PO daily
– TAF/FTC, TDF/FTC, or TDF/3TC: 1 pill PO daily
• (DRV/r or DRV/COBI) + (TAF or TDF) + (3TC or FTC)a
– DRV/COBI/TAF/FTC: 1 pill PO daily with food
of newly diagnosed patients with HIV would benefit from rapid initiation of bictegravir (BIC)/TAF/FTC due to its single-tablet regimen, high barrier to resistance, efficacy, and tolerability/safety. If insurance coverage is an issue, then dolutegravir (DTG) + TAF/FTC is typically the second-line option. Although boosted DRV-based regimens are also viable options, there are many DDIs across multiple drug classes frequently prescribed by other subspecialists (eg, fluticasone by pulmonologists, statins by cardiologists) in this patient population, complicating management. These increasingly become a concern as patients with HIV age or in patients diagnosed at a later age. Common side effects that should be discussed prior to starting ART include nausea, vomiting, diarrhea, and headache. These side effects can be managed with supportive care and frequently resolve within a few weeks of starting treatment.
Special Populations: Pregnancy
Special populations may require different considerations in designing a rapid ART regimen. The preferred rapid ART regimen for pregnant persons is currently a 2-tablet DTG-based regimen because boosted DRV-based regimens require twice-daily dosing in pregnancy and there are insufficient data on BIC use in pregnancy.17 A potential association between DTG and neural tube defects (NTDs) was first described in 2018 in an observational study in Botswana, leading to a recommendation to avoid the use of DTG in pregnant women with HIV.19 These concerns, fortunately, were unfounded. The risk for NTDs was not increased compared with other ART regimens after additional data gathering. The guidelines have since been updated to include DTG (along with folic acid supplementation) as a preferred agent in pregnant women with HIV due to its high resistance barrier and favorable adverse effect profile. In clinical practice, the small difference in NTDs reported must be weighed against the potential for improved maternal health and reduced HIV vertical transmission with DTG administration.20
NOT Recommended for Rapid Start
• NNRTI-based regimens
• 2-drug regimens (DTG/3TC, DTG/RPV, CAB/RPV)
• Regimens requiring ABC
3TC, lamivudine; ABC, abacavir; ART, antiretroviral therapy; BIC, bictegravir; CAB, cabotegravir; COBI, cobicistat; DRV, darunavir; DTG, dolutegravir; FTC, emtricitabine; IAS-USA, International AIDS Society USA; NNRTI, non-nucleoside reverse transcriptase inhibitor; PO, per os (by mouth); PrEP, pre-exposure prophylaxis; r, ritonavir; RPV, rilpivirine; TAF, tenofovir alafenamide; TDF, tenofovir disoproxil fumarate.
aPreferred regimen (DRV/COBI/TAF/FTC) if there has been exposure to CAB as PrEP; otherwise not recommended by the IAS-USA for rapid ART.
5
TABLE 2. Recommendations for Rapid ART Regimens17,18
Special Populations: Cabotegravir Use in PrEP
Another special population with considerations that impact rapid ART selection is individuals exposed to cabotegravir (CAB) for PrEP. If a patient is currently taking CAB or took it at the time of HIV infection or since HIV infection, there is a concern that RAMs have developed. In such a case, the DHHS recommends starting a boosted DRV-based regimen while awaiting the results of the genotype assay.21 In general, past ART/ PrEP exposure does not prohibit the initiation of rapid ART, but the choice of ARV regimen should be clinically evaluated. For patients with potential barriers to daily therapy, such as those with substance use disorder, depression, unstable housing, or other challenges in social determinants of health, ART initiation should not be delayed. In these patients, it is vital to address specific adherence concerns.
If none of the 3 regimens has any definitive contraindications for the patient, prioritizing a singletablet regimen such as BIC/TAF/FTC may improve adherence. Starter packs containing a 3- to 5-day supply of the selected ART regimen are useful for getting medication into the hands of the patient on the day of diagnosis. They ensure that patients can actually begin ART on the day of diagnosis and bypass any delays in obtaining ART due to insurance or pharmacy-level issues.21
In addition to DHHS-recommended rapid ART regimens, there are also regimens that are specifically NOT recommended. As mentioned earlier, NNRTIbased regimens have higher rates of transmitted drug resistance compared with INSTI-based regimens, and 2-drug regimens are not recommended due to high rates of NNRTI or nucleoside reverse transcriptase inhibitor (NRTI) drug resistance and the increased risk of virologic failure in patients with a high VL.21 Finally, regimens containing abacavir (ABC) should also be
avoided until human leukocyte antigen (HLA)-B*5701 test results are available due to the fatal hypersensitivity reaction that can occur in patients with this allele.22
What information and laboratory tests, if any, do I need to get before starting ART?
Although there are 3 ART regimens recommended for rapid start, certain information should be gathered prior to their initiation, while other results can be obtained after ART initiation (Table 3). These laboratory tests can be ordered at the first appointment. An observational retrospective study supports that initiating ART at the first available opportunity without baseline laboratory testing results does NOT reduce its efficacy or safety.23 In fact, the data suggest that the benefits of rapid virologic control and high rates of retention in HIV care that result from rapid ART outweigh any risks.
Of critical importance is determining if the individual newly diagnosed with HIV has symptoms of cryptococcal or tuberculous meningitis because they would be at high risk of immune reconstitution inflammatory syndrome (IRIS) if ART is initiated. IRIS occurs secondary to the restoration of a pathogen-specific immune response when ART is initiated and has an incidence ranging from 5% to 40% in PWH.24 Rash is a common presentation of IRIS that patients need to be cognizant of when starting ART; if a rash occurs, patients should notify their provider immediately. Although IRIS is typically a self-limiting complication, occasionally patients will require glucocorticoids and even hospitalization. It is also important to note that when ART is initiated with INSTI-based regimens, the plasma HIV RNA VL declines at a faster rate compared with other regimens, elevating the risk of IRIS. In fact, in a study of interstitial pneumonitis, development of IRIS was associated with a greater VL decline at 1 month after ART initiation, a baseline CD4:CD8 ratio of <0.1, and a shorter interval (<7 days) between the diagnosis of opportunistic infection and the initiation of ART.24 Importantly, the mortality rate associated with IRIS is only increased
Prior to Rapid ART Initiation
• Confirmatory HIV testing (if not already available and current)
• No suspicion of cryptococcal or tuberculous meningitis
• Complete patient history of medical conditions, reproductive plans and use of contraceptives, and chronic medications
• History of prior use of PrEP
• Pregnancy test in a person of childbearing potential
Results Not Needed Prior to Rapid ART Initiation
• Metabolic panel (eg, creatinine, electrolytes, glucose, LFTs)
• CD4+ cell count
• HIV RNA (viral load)
• HIV genotype
• Hepatitis A/B/C/D status
• HLA-B*5701 status
• STI screening results
ART, antiretroviral therapy; HLA, human leukocyte antigen; LFT, liver function test; PrEP, pre-exposure prophylaxis; STI, sexually transmitted infection.
6 EMERGING ISSUES IN HIV MANAGEMENT: ANSWERS TO PHARMACISTS’ COMMON QUESTIONS
TABLE 3. Information Needed for Rapid ART Initiation17
when IRIS affects the central nervous system, such as in those with cryptococcal or tuberculous meningitis. In these circumstances, the mortality rate can be as high as 20%.24 Therefore, symptoms of cryptococcal or tuberculous meningitis require confirmatory testing (eg, cryptococcal antigen screen if CD4+ count ≤100 cells/ mm3) and delay of ART initiation.
The results of hepatitis testing are not necessary before initiation of ART because all of the recommended regimens include tenofovir (TFV) plus 3TC or FTC, which has dual activity against both HIV and hepatitis B virus (HBV).8 Eventually, renal function needs to be evaluated because TDF and TAF should be avoided in patients with estimated creatinine clearance (eCrCl) <50 mL/ min/1.73 m2 and <30 mL/min/1.73 m2, respectively, unless they are already on hemodialysis.17 In general, the results of the other laboratory tests listed are not necessary prior to initiation of rapid ART because of the chosen ARV options’ high barriers to resistance and the benefits imparted from rapid ART (eg, early virologic suppression, linkage to care) outweighing the potential risks (eg, baseline metabolic dysfunction).
Other important information to gather before rapid ART initiation includes a current medication list to assess for potential DDIs, exposure to PrEP, and the potential for pregnancy. For example, DRV, ritonavir (r), and COBI are all strong cytochrome P450 (CYP) 3A4 inhibitors and the absorption of INSTIs is reduced by polyvalent cations such as multivitamins and antacids.
Does rapid initiation of ART change how I monitor my patient with HIV?
After rapid ART initiation, it is imperative to closely monitor the patient. Patients often need additional education and extra support in the days and weeks that follow their HIV diagnosis and ART initiation. Within 1 to 2 days, the patient should be contacted by phone or preferred means of communication to assess for adverse effects, answer any questions, and encourage adherence. Once the baseline laboratory results are available, the patient should return for a follow-up visit and the ART regimen should be assessed and adjusted as necessary to account for important factors, such as the presence of RAMs or reduced renal function. Then, 4 weeks after ART was initiated, a repeat VL should be obtained to assess the treatment response.25 At every appointment, ART adherence should be evaluated, side effects should be screened for, and patient questions should be answered.21
Are there circumstances when ART initiation should be delayed?
A brief delay in initiating ART is reasonable if there is concern for an active comorbid condition or an active opportunistic infection due to the potential for serious DDIs and overlapping drug toxicity, or IRIS. As mentioned previously, this is especially true in cases of meningitis secondary to tuberculosis, cryptococcus, or disseminated coccidioidal infection. Depending on
the type of opportunistic infection, ART can usually be initiated within 2 weeks, and early initiation of ART has been shown to be effective in reducing mortality among patients who present with opportunistic infections at the time of HIV diagnosis.18,26,27 Early initiation of ART, and the resultant increase in CD4+ count, is also especially important when certain infections are unable to be or only marginally treated with anti-infective therapy (eg, progressive multifocal leukoencephalopathy, cryptosporidiosis).18
What are the roles for pharmacists in rapid initiation of ART?
In addition to their primary roles in the pharmacy setting, pharmacists are well positioned to assess patient readiness, provide patient education, evaluate DDIs, resolve medication access issues (eg, insurance), and recommend patient-specific ART regimens. A preliminary retrospective analysis at a large HIV clinic in Rhode Island demonstrated that a pharmacist-driven rapid ART protocol, which offered ART to patients on the same day as diagnosis, reduced the time from intake to both ART initiation and to virologic suppression compared to standard care (≥2 weeks before ART initiation). Furthermore, this study showed that medication access issues were preemptively resolved in 61% of the patients involved in this pharmacistdriven rapid ART protocol.28 Additional data from an analysis of new ART regimen initiations also shows that pharmacists improve long-term adherence to ART within multidisciplinary teams.29 Maximal increase in ART adherence occurred with a multidisciplinary team composed of a pharmacist, non-nurse care coordinator, and a primary care provider (PCP) compared with patient exposure only to an HIV specialist.29 These findings demonstrate the integral role of pharmacists in the multidisciplinary care team.
Current data confirm that rapid ART not only can increase rates of virologic suppression regardless of baseline VL, but can also increase rates of linkage to care and retention in care and reduce HIV transmission. However, barriers to rapid ART still exist and need to be overcome if the US is to meet the goals set by the EHE initiative. One barrier is patients who need more time to process their new HIV diagnosis or even deny their diagnosis.30 This represents an opportunity for patient education that can be facilitated by pharmacists during the initial encounter and during follow-up. Patient education can include information about partner PrEP and how important it is to prioritize ART to achieve virologic suppression and reduce the risk of HIV transmission.
Other barriers include those at the HCP and administrative levels. A study in Memphis, Tennessee, that conducted process mapping and in-depth interviews identified 4 modifiable rate-limiting rapid ART barriers: laboratory-based confirmatory HIV results requirements, eligibility documentation requirements for Ryan White-funded services, insufficient HIV clinic medical provider availability, and variability in ART
7
initiation timing among HIV clinic providers. 31 These modifiable and systemic barriers to clinic flow and patient-level outcomes may represent areas where pharmacists can help implement rapid ART. For example, pharmacists involved with HIV management through collaborative practice agreements can relieve the burden on HIV clinic medical providers so that availability and timing of ART can be improved. In fact, in a small study evaluating outcomes related to a pharmacist-driven rapid ART protocol, all of the pharmacist-recommended ART regimens were accepted and implemented by HIV medical providers, demonstrating pharmacists’ ability to fulfill this role. 28
Clinic workflow can greatly impact the implementation of rapid ART initiation in practice. Ideally, patients with newly diagnosed HIV can be evaluated the same day as their diagnosis. This is easier to accomplish when HIV is diagnosed during an inpatient hospital stay because an infectious diseases consult team is readily available to counsel the patient and prescribe ART. Unfortunately, once discharged, unless ability to pay (eg, insurance preauthorization) has been confirmed, PWH may stop ART regimens due to cost and access. In the outpatient setting, provider and patient availability have more variability, and rapid ART paperwork and testing requirements can prove to be insurmountable for some patients (and clinics). The REACH program
demonstrated that streamlining workflow, eliminating unnecessary paperwork and testing requirements, and incorporating a patient navigator could improve rapid ART uptake.13 Furthermore, once a medical evaluation is completed by HCPs, other members of the team can facilitate rapid ART. For example, clinical pharmacists can begin counseling, which can include both patient education and assessment of a patient’s readiness to begin treatment, as well as determine the appropriate rapid ART regimen to initiate (Table 4).
Despite evidence that rapid ART is safe, quickly and effectively reduces VL, and improves linkage and engagement in care, implementation is not universal in the US. The operational structure of rapid ART programs is tailored to the individual clinical setting, so a onesize-fits-all protocol is not feasible; however, successful rapid ART programs in 3 distinct clinical settings, an HIV clinic, a Federally Qualified Health Center, and a sexual health and wellness clinic, were evaluated through key informant interviews and elucidated 7 essential elements associated with successful rapid ART implementation.32 Some or all of these elements can be incorporated into clinics that want to initiate a rapid ART protocol or improve their current rapid ART uptake. They also may serve as solutions when challenges arise or to gain perspective into the aspects that are important to patients newly diagnosed with HIV.
• Counseling –
Assessing patient readiness to begin treatment
– Answering patient questions and concerns
– Assessing the individual need for wraparound services (eg, childcare, case management, emergency financial assistance, food banks, housing services, substance use services, psychosocial support, treatment adherence counseling)
– Assessing the need for partner PrEP
• Education –
Understanding of ART in management of HIV
• Goal: to achieve an undetectable viral load and reduce risk of transmission (U=U)
– Importance of adherence to ART regimen
– Recognition of potential side effects
• Supportive care management for side effects
• Evaluation of any potential drug-drug interactions
• Resolution of medication access issues
• Recommendation of patient-specific rapid ART regimen
• Provision of antiretroviral medications for the patient to leave the clinic with and begin immediately
• Follow-up phone calls with patients 1 or 2 days after ART initiation
ART, antiretroviral therapy; PrEP, pre-exposure prophylaxis; U=U, undetectable=untransmittable.
8 EMERGING ISSUES IN HIV
TO PHARMACISTS’ COMMON QUESTIONS
MANAGEMENT: ANSWERS
TABLE 4. Potential Roles for Pharmacists in Rapid ART Initiation32
Seven Essential Elements, Across Settings, Associated With Successful Rapid Antiretroviral Therapy (ART) Programs32
1. Presence of an implementation champion
2. Comfort and competence prescribing rapid ART regimens
3. Expedited access to ART medications
4. Expertise in benefits, linkage, and care navigation
5. Rapid ART team member flexibility and organizational adaptive capacity
6. Patient-centered approach
7. Strong communication methods and culture
How do PWH feel about rapid ART initiation?
Recent interviews conducted with PWH in East London provided insight into their perspectives regarding rapid ART. Overall, 4 themes were elucidated: being offered rapid ART is acceptable, rapid ART is a way of taking control of their health, there is a need for information and support soon after HIV diagnosis, and rapid ART can provide an individualized approach to care, which is desirable.30 Rapid ART can be facilitated by providing comprehensive information about treatment options, recognizing and managing potential side effects, and offering options for peer support. It is also important that the clinical team be supportive and maintain a nonjudgmental attitude, while being approachable, reassuring, and encouraging.30 Although not all patients will be ready to start treatment on the same day they are diagnosed with HIV, those without any contraindications to early ART initiation should be fully informed of the benefits and offered rapid ART initiation. It is also important to assess newly diagnosed patients’ need for wraparound, or non-medical, services so that measures needed to provide those services can be implemented as soon as possible. Non-medical services are core components of HIV medical care that maximize the chance that patients will remain in care, adhere to ART regimens, and achieve positive health outcomes, including virologic suppression.33
Overall, the earlier that ART is initiated, the quicker virologic suppression can be achieved, leading to undetectable VLs and decreased risk of transmission. Additionally, rapid ART may improve linkage and continued engagement in care. Through their knowledge and experience, pharmacists are not only able to counsel and educate patients with HIV, but can also recommend specific ART regimens, evaluate potential DDIs, and access and resolve any medication access issues that may act as barriers to rapid ART initiation. These roles are critical for expanding rapid ART uptake and improving long-term patient outcomes.
Part II: Long-acting injectable ART
Although the development of effective and welltolerated ARV agents has reduced morbidity and mortality related to HIV infection, until recently, the effectiveness of ART regimens has depended on consistent daily oral intake by patients. In PWH, ART nonadherence can result in RAMs, leading to treatment failure, disease progression, and risk of HIV transmission. Even when PWH are adherent to oral ART, pharmacokinetics and DDIs can negatively affect efficacy. For example, the efficacy of rilpivirine (RPV) is dependent on gastric acidity for absorption; therefore, common over-the-counter (OTC) acid suppressants (eg, proton pump inhibitors) can greatly reduce RPV efficacy when these agents are taken together orally.
As an alternative to daily oral ART, US Food and Drug Administration (FDA)-approved long-acting injectable (LAI) ART options are currently available. LAI ART has the potential to overcome adherence issues by decreasing pill burden while improving patients’ privacy and reducing the social stigma associated with the daily oral intake of ART. LAI agents inherently have both benefits and risks. Their parenteral administration may avoid troublesome DDIs related to the administration of simultaneous oral medications and their long-acting nature allows for less-frequent administration compared with daily oral ART; however, the long pharmacokinetic (PK) tail of LAI ART agents can increase the risk of certain DDIs (eg, uridine 5’-diphospho-glucuronosyltransferase [UGT] 1A1 and/or CYP3A enzyme inhibitors or inducers), potentially expose patients to long durations of adverse effects, and increase the risk of RAMs if LAI ART is discontinued without transitioning to the appropriate oral ART regimen. Furthermore, long-term planning is necessary with regard to pregnancy and future ART selection after discontinuation of LAI ART.
The LAI ART options currently FDA approved for specific patient populations include CAB + RPV, a combination INSTI and NNRTI, and lenacapavir (LEN), a novel capsid inhibitor. CAB + RPV is FDA approved for PWH aged≥12 years weighing at least 35 kg who are virologically suppressed (HIV-1 RNA <50 c/mL). These patients must be on a stable ART regimen for ≥6 months with no history of treatment failure and no known or suspected resistance to CAB or RPV.34,35 LEN is FDA approved for use in HTE adults with multidrug-resistant (MDR) HIV who are failing their current ARV regimen due to resistance, intolerance, or safety considerations and must be given with an optimized background regimen of oral ART.36-38
What clinical trial data on efficacy and safety support the use of LAI CAB + RPV in practice?
Several pivotal clinical trials (FLAIR, ATLAS, ATLAS2M) evaluating LAI CAB + RPV demonstrated its high efficacy and safety as a maintenance strategy in those suppressed on oral ART.39 In the FLAIR study, treatmentnaive PWH in the treatment arm were required to
9
achieve virologic suppression on an oral ART regimen before receiving CAB + RPV. At week 48, 93.6% of those receiving CAB + RPV and 93.3% receiving only oral ART without transitioning to CAB + RPV achieved HIV RNA <50 c/mL (Figure 1).40 This study demonstrated that CAB + RPV was noninferior to oral ART regimens in treatment-naive patients at 48 weeks after achieving suppression on oral therapy. Injection site reactions were seen in 86% of those receiving CAB + RPV, but these reactions decreased to 20% by week 48.40 In the ATLAS study at week 48, 92.5% of treatmentexperienced PWH receiving LAI CAB + RPV and 95.5% receiving oral therapy had achieved HIV RNA <50 c/mL (Figure 2).41 This study demonstrated that LAI CAB + RPV was noninferior to oral ART regimens at 48 weeks. Injection site reactions were seen in 81% of those receiving CAB + RPV, but these reactions decreased to 11% at week 48. In the ATLAS-2M study at week 48, 94% of treatment-experienced PWH receiving LAI CAB + RPV every 8 weeks and 93% receiving CAB + RPV every
4 weeks achieved HIV RNA <50 c/mL (Figure 3).42 This study demonstrated that, by 48 weeks, CAB + RPV every 8 weeks was noninferior to CAB + RPV every 4 weeks. Injection site reactions were rated as mild to moderate by 98% of participants who experienced them.42
In a post hoc multivariable analysis of pooled data from the FLAIR, ATLAS, and ATLAS-2M clinical trials, approximately 1% of patients who received LAI CAB + RPV experienced virologic failure. In the ATLAS-2M trial, there was a numerically greater number of virologic failures in the every-2-month arm; however, the type of dosing regimen was not associated with virologic failure in the post hoc multivariable analysis (Figure 4).43
The following factors were associated with increased risk of confirmed virologic failure (CVF), with the presence of 2 or more factors resulting in the highest rate of virologic failure: proviral RPV RAMs at baseline, HIV subtype A6/A1, and higher baseline body mass index (BMI).44,45
3TC, lamivudine; ABC, abacavir; ART, antiretroviral therapy; c, copies; CAB, cabotegravir; DTG, dolutegravir; IM, intramuscular; LAI, long-acting injectable; RPV, rilpivirine.
N=618 adults with HIV who had not previously received ART were given 20 weeks of DTG/ABC/3TC. Those who had HIV RNA <50 c/mL after 16 weeks were randomly assigned to continue their current regimen or switch to oral CAB + RPV for 4 weeks, followed by monthly IM injections of LAI CAB + RPV for 48 weeks.
ART, antiretroviral therapy; c, copies; CAB, cabotegravir; IM, intramuscular; LAI, long-acting injectable; RPV, rilpivirine.
N=618 adults with HIV who were virally suppressed for ≥6 months on standard oral ART regimens were randomly assigned 1:1 to continue their current regimen or switch to oral CAB + RPV for 4 weeks followed by monthly IM injections of LAI CAB + RPV for 52 weeks.
10 EMERGING ISSUES IN HIV
TO PHARMACISTS’ COMMON QUESTIONS
MANAGEMENT: ANSWERS
100 80 60 40 20 0 HIV RNA <50 c/mL 93.6 93.3 2.1 2.5 4.2 4.2 HIV RNA ≥50 c/mL No virologic data
Oral therapy Participants, %
CAB + RPV
100 80 60 40 20 0 HIV RNA <50 c/mL 92.5 95.5 1.6 1.0 5.8 3.6 HIV RNA ≥50 c/mL No virologic data CAB +
Oral therapy Participants, %
FIGURE 1. FLAIR: LAI CAB + RPV Was Noninferior to Oral ART at 48 Weeks in Treatment-Naive Patients40
RPV
FIGURE 2. ATLAS: LAI CAB + RPV Was Noninferior to Oral ART By 48 Weeks in Treatment-Experienced Patients41
FIGURE 3. ATLAS-2M: LAI CAB + RPV Q8W Was Noninferior to Q4W by 48 Weeks42
ART, antiretroviral therapy; c, copies; CAB, cabotegravir; IM, intramuscular; LAI, long-acting injectable; RPV, rilpivirine; Q4W, every 4 weeks; Q8W, every 8 weeks; RPV, rilpivirine.
N=1045 adults with HIV who were virally suppressed and participated in the ATLAS study (rollover) or who were taking standard oral ART regimens were randomly assigned to LAI CAB + RPV every 4 weeks or every 8 weeks and followed for 48 weeks.
Risk Factors For Virologic Failure With
LAI CAB + RPV45
• Presence of ≥2 proviral RPV RAMs
• HIV-1 subtype A6/A1
• BMI ≥30 kg/m2
BMI, body mass index; CAB, cabotegravir; LAI, long-acting injectable; RAM, resistance-associated mutation; RPV, rilpivirine.
Furthermore, BMI ≥30 kg/m2 was associated with low RPV trough concentrations. Additionally, the presence of baseline RPV RAMs reflects either prior NNRTI exposure with acquired drug resistance, transmitted drug resistance, or, occasionally, naturally occurring polymorphisms leading to reduced susceptibility to RPV. Although RPV RAMs were associated with the
greatest increase in risk of CVF, with an incident rate ratio of 21.7 (5.8-80.8), only 1 out of 31 participants with RPV RAMs alone (without BMI >30 kg/m2 or HIV-1 subtype A6/A1) experienced CVF in these studies.44 To minimize resistance to LAI ART, careful selection of patients with anticipated high adherence to injectable treatment is necessary so that doses are not missed. If CVF is experienced and resistance results are still pending, a protease inhibitor (PI)-based regimen can be initiated. If it is known that there are no INSTI RAMs, it is also feasible to consider initiating an INSTIbased regimen.17
The phase 3b SOLAR study compared the efficacy of switching virologically suppressed adults with HIV to LAI CAB + RPV every 2 months vs continuation of oral BIC/FTC/TAF. At the end of month 12, CAB + RPV demonstrated noninferior virologic efficacy compared with BIC/FTC/TAF, with 3 CVFs in the CAB + RPV arm and none in the BIC/FTC/TAF arm.46
11
100 80 60 40 20 0 HIV RNA <50 c/mL 93 94 1 2 6 4 HIV RNA ≥50 c/mL No virologic data CAB + RPV Q4W CAB + RPV Q8W Participants, %
Parameter Every 4 Weeks (n=1129) Every 8 Weeks (n=327) Every 4 Weeks Every 8 Weeks (n=195) Overall (N=1651) VF, % 1 2.4 2 1.4 Patient-Year 2621 936 734 4291 Incidence Rate (per 100 Patient-Year) 0.42 0.85 0.54 0.54 1.00 0.95 0.90 0.85 0.80 0 16 32 48 64 80 96 112 128 144 160 176 192 208 224 240 Every 4 weeks Every 8 weeks Every 4 weeks every 8 weeks Expanded Scale Proportion Suppressed Time to Virologic
LAI,
Failure, Weeks CAB, cabotegravir;
long-acting injectable; RPV, rilpivirine; VF, virologic failure.
FIGURE 4. Prevalence of VF With LAI CAB + RPV43
What is the specific prescribing information for LAI CAB + RPV?
As briefly mentioned previously, LAI CAB + RPV is FDA approved for PWH aged ≥12 years weighing at least 35 kg who are virologically suppressed (HIV-1 RNA <50 c/ mL) on a stable ART regimen for ≥6 months, with no history of treatment failure and no known or suspected resistance to CAB or RPV.34,47 A clear contraindication for LAI CAB use is in patients with concomitant HBV infection. LAI CAB is administered by gluteal intramuscular (IM) injection at 2 separate sites, one for CAB and another for RPV. A longer (2-inch) needle
for injection may be necessary in patients with a BMI ≥30 kg/m2 in order to achieve appropriate drug levels.48 The important prescribing information is further outlined below ( Table 5). LAI CAB + RPV can be administered with or without an oral lead-in, then either every 4 weeks or every 8 weeks ( Table 6).
In instances where there is a planned missed dose (±7 days from the target treatment date), oral CAB + RPV (or any other fully suppressive oral ART regimen) should be administered for up to 2 consecutive months prior to resuming IM therapy. When an unplanned missed dose occurs, it should be confirmed that resumption of LAI
• PWH aged ≥12 years weighing at least 35 kg
• Virologically suppressed (HIV-1 RNA <50 c/mL) on a stable ART regimen for ≥6 months
Indications
Contraindications
Common Adverse Events
• No history of treatment failure
• No known or suspected resistance to CAB or RPV
• Administration with other medications that can lower concentrations of CAB or RPV
• Prior hypersensitivity reactions to CAB or RPV
• Mild to moderate injection site reactions (pain, redness, swelling)
• Pyrexia
• Fatigue
• Headache
Special Considerations
• Musculoskeletal pain
• Nausea
• Sleep disorders
• Dizziness
• Rash
• HBV coinfection would not be treated with CAB + RPV
• May need to use a longer needle in patients with BMI ≥30 kg/m2
• May not be able to use in patients with buttock implants or dermal fillers
• Not approved during pregnancy
• More-frequent monitoring of LFTs necessary in patients with pre-existing liver disease
ART, antiretroviral therapy; BMI, body mass index; c, copies; CAB, cabotegravir; LAI, long-acting injectable; LFT, liver function test; PWH, people with HIV; RPV, rilpivirine.
12 EMERGING ISSUES IN HIV MANAGEMENT: ANSWERS TO PHARMACISTS’ COMMON QUESTIONS
LAI CAB + RPV
Induction Dosing Maintenance Dosing Schedule First Dose (Day 0)a Month 1 Month 2 Month 3 After Month 3 Every 4 Weeks CAB 600 mg (3 mL) and RPV 900 mg (3 mL) IM CAB 400 mg (2 mL) and RPV 600 mg (2 mL) IM CAB 400 mg (2 mL) and RPV 600 mg (2 mL) IM CAB 400 mg (2 mL) and RPV 600 mg (2 mL) IM CAB 400 mg (2 mL) and RPV 600 mg (2 mL) IM every month thereafter Every 8 Weeks CAB 600 mg (3 mL) and RPV 900 mg (3 mL) IM CAB 600 mg (3 mL) and RPV 900 mg (3 mL) IM No injection CAB 600 mg (3 mL) and RPV 900 mg (3 mL) IM CAB 600 mg (3 mL) and RPV 900 mg (3 mL) IM every 2 months thereafter
TABLE 5. Prescribing Information for LAI CAB + RPV34,35,48
30
CAB, cabotegravir; IM, intramuscular; LAI, long-acting injectable; PO, per os (by mouth); RPV, rilpivirine. aOptional lead-in can occur prior to this
dose: CAB
mg +
RPV
25 mg PO daily for ≥28 days (must be taken with a meal).
TABLE 6. LAI CAB + RPV Dosing Schedules35
CAB + RPV is clinically appropriate. If so, and the patient is on an every-8-week dosing schedule and it has been ≤1 month since the missed target treatment date, injections should be resumed as soon as possible. If it has been >1 month since the missed target treatment date, repeat initiation injections 1 month apart for 2 consecutive months should be started as soon as possible (Figure 5).35
If the patient is on an every-4-week dosing schedule and it has been ≤1 month since the missed target treatment date, injections should be resumed as soon as possible. If it has been >1 month since the missed target treatment date, repeat initiation injections should be started as soon as possible (Figure 6).35
HIV clinics may need to maintain an inventory of LAI CAB + RPV; therefore, it is important to note that it requires cold-chain supply and storage (2° C-8° C; 36° F-46° F) and must be brought to room temperature before administration, but not for longer than 6 hours. Furthermore, it can only remain in syringes for up to 2 hours before injection and should not be cycled in and out of refrigeration.34,47
What do we know about LAI CAB + RPV pharmacokinetics?
Both CAB and RPV exhibit absorption rate–limited PK tails following IM injection, with mean apparent half-life estimates of 5.6 to 11.5 weeks and 28 weeks, respectively.49 Even after LAI CAB + RPV discontinuation, both agents may remain measurable in the plasma for more than a year (Figure 7).49
The main concern regarding DDIs with CAB + RPV is administration with other medications that may lower the concentration of CAB or RPV. During its use and even after its discontinuation, potential DDIs that may occur with LAI CAB + RPV include34,47:
• Rifamycins
• Anticonvulsants (carbamazepine, oxcarbazepine, phenobarbital, phenytoin)
• St. John’s wort
• Dexamethasone (if more than a single dose)
• Methadone
• Tecovirimat ≤1 >1
Resume injections as soon as possible. Continue with every-2-month dosing schedule thereafter.
Resume injections as soon as possible, 1 month apart for 2 consecutive months. Continue with every-2-month dosing schedule thereafter.
Resume injections as soon as possible. Continue with once-monthly dosing schedule thereafter.
Repeat initiation injections as soon as possible. Continue once-monthly dosing schedule thereafter.
13
Month Since Missed Target Treatment Date Month Since Missed Target Treatment Date
CAB, cabotegravir; LAI, long-acting injectable; RPV, rilpivirine.
FIGURE 5. Restarting Every-8-Week LAI CAB + RPV After Unplanned Missed Injections35
≤1 >1
Month Since Missed Target Treatment Date Month Since Missed Target Treatment Date
CAB, cabotegravir; LAI, long-acting injectable; RPV, rilpivirine.
FIGURE 6. Restarting Every-4-Week LAI CAB + RPV After Unplanned Missed Injections35
For further information on specific potential DDIs that may occur with LAI CAB + RPV (and other ARV agents), information can be obtained from the University of Liverpool HIV drug interaction checker online (https:// www.hiv-druginteractions.org/checker).50
Do I have to change my standard approach to monitoring when using LAI CAB + RPV?
One option for VL monitoring after initiating LAI CAB + RPV is to get a VL at month 1 and again at month 3 to align with injection schedules, then every 3 to 6 months after, although more-frequent monitoring can also be considered. If there is a subsequent increase in VL >200 c/mL, recheck the VL, check the genotype resistance assay (knowing that for some laboratories, results are only accurate for VL >500 c/mL), assess for DDIs, and confirm correct and timely administration of LAI CAB + RPV. To minimize resistance to CAB and/ or RPV, careful selection of patients who will maintain adherence to injectable treatment is critical. If doses are missed, there is a risk of developing treatmentemergent resistance, which may lead to virologic failure and disease progression.
Can LAI CAB + RPV be used in PWH who are failing an oral ART regimen and are viremic at baseline?
Although the current FDA-approved indication for LAI CAB + RPV is for use in virologically suppressed PWH, LAI ART could greatly benefit individuals who may struggle with adherence to oral regimens, leading to virologic failure. A recent study evaluated the efficacy of monthly LAI CAB + RPV in PWH who were viremic at baseline (n=57). It demonstrated that 97.5% achieved virologic suppression by 24 weeks; all but 2 patients were able to achieve virologic suppression (HIV RNA <30 c/mL) by 42 weeks despite two-thirds experiencing unstable housing and/or substance use.51 Two other small studies demonstrated similar rates of virologic
suppression in PWH who were viremic at baseline.52,53 Furthermore, using electronic health records data from the Observational Pharmacoepidemiology Research and Analysis (OPERA) cohort, all ART-experienced adults, including those with VL ≥200 c/mL, who received at least 1 LAI CAB + RPV dose for the first time between January 21, 2021, and February 28, 2022, were followed until March 13, 2022, the majority of whom received monthly dosing. These patients were evaluated for rates of virologic suppression and demonstrated that 91% of those with VL ≥200 c/mL at LAI CAB + RPV initiation achieved HIV RNA <200 c/mL, with a median followup time of 4.4 months (Figure 8).54 Despite these trial results, using CAB + RPV in a viremic patient population is not a recommended strategy at this time. More (and larger) studies, including those evaluating every2-month dosing regimens, will need to be performed because the consequence of virologic failure is a risk of 2-class drug resistance.
How does LEN’s novel mechanism of action benefit HTE PWH?
LAI LEN was FDA approved in December 2022 for HTE adults with MDR HIV who are failing their current ART due to resistance, intolerance, or safety considerations. Although the definition of HTE is not standard, typically it is a term used to describe PWH who have ≤2 ARV classes available for use, with limited fully-active ARV agents within each class.55 Fortunately, the prevalence of HTE PWH has declined from 7.5% in 2006 to <1% in 2012 thanks to the introduction of the INSTI ARV drug class in 2007.56 Despite the low prevalence, HTE patients can be complex to manage even for the mostexperienced HIV providers.
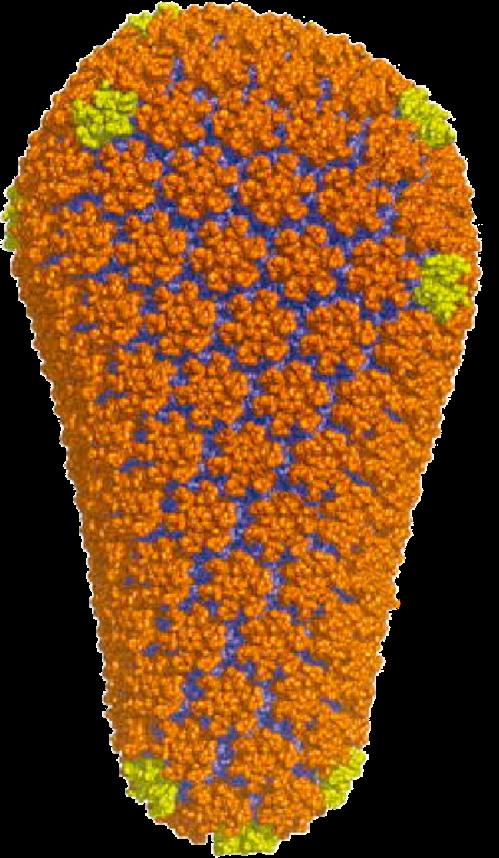
LAI LEN’s novel mechanism of action as a capsid inhibitor positions it to be exceedingly valuable in the HTE population because there is no overlap with treatmentemergent resistance of other ARV drug classes (eg, PIs, NNRTIs). Furthermore, LEN interrupts the HIV life cycle
14 EMERGING ISSUES IN HIV MANAGEMENT: ANSWERS TO PHARMACISTS’ COMMON QUESTIONS
0 0 1 1 3 3 6 6 9 9 12 12 Plasma CAB, µg/mL Plasma RPV, µg/mL Time Post Final Injection, Months Time Post Final Injection, Months 10 100 1 10 0.1 0.025 (LLOQ) 1 (LLOQ) CAB PA-IC90 (0.166 µg/mL) RPV PA-IC90 (12 ng/mL) Q4W (LATTE-2, ATLAS, n=29) Q4W (LATTE-2, ATLAS, n=24) Q8W (LATTE-2, n=5) Q8W (LATTE-2, n=5)
CAB, cabotegravir; LAI, long-acting injectable; LLOQ, lower limit of quantification; PA-IC90, protein-adjusted IC90; Q4W, every 4 weeks; Q8W, every 8 weeks; RPV, rilpivirine.
FIGURE 7. Pharmacokinetic Tails After Discontinuation of LAI CAB and RPV49
FIGURE 8.
CAB +
Effectiveness in the First Year: OPERA Cohort54
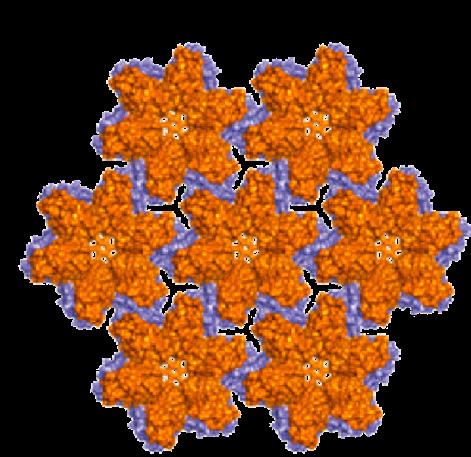
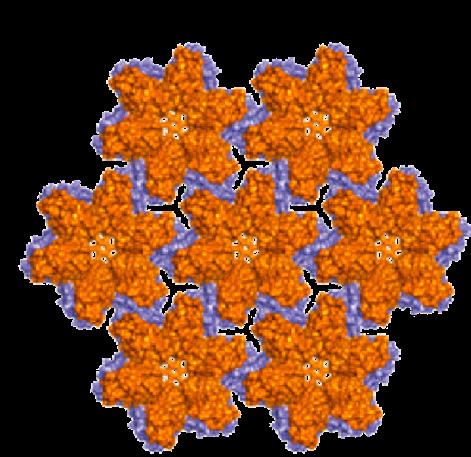
at numerous stages, unlike other ARVs that focus on one particular point, such as HIV viral DNA integration into host DNA in the case of INSTIs (Figures 9 and 10).57
HIV’s capsid core is composed of capsid monomers (P24) that combine into hexamers (and sometimes pentamers). The shape and integrity of the capsid core structure is essential for multiple stages of the HIV life cycle: capsid-mediated nuclear uptake of HIV-1 proviral DNA, virus assembly and release, and capsid core formation. LEN acts as a capsid inhibitor in a multitude of ways. LEN binds the capsid monomers within the hexamers and pentamers to make them less pliable. This inhibits both the ability of the capsid to be transported through the nuclear pores into the host nucleus and its disassembly in the nucleus; therefore, in the presence of LEN, viral DNA cannot be integrated into the host DNA (Figure 11). Furthermore, human proteins (eg, CPSF6) are utilized to assist capsid entry into the nucleus; however, LEN blocks the binding of capsid with nuclear pore proteins. Finally, if the virus manages to proceed through its HIV life cycle,
LEN causes the formation of the capsid core to be misshapen and decreases its infectivity.57
As mentioned earlier, LEN’s utility for treatment of HTE PWH is its ability to be unaffected by RAMs associated with other ARV classes; however, treatment-emergent resistance can still occur in patients taking LEN, and these RAMs map to locations where the drug binds to capsid (eg, L56I, M66I, Q67H, K70N, N74D/S, T107N).36
What clinical trial data on efficacy and safety support the use of LAI LEN in practice?
The two pivotal clinical trials evaluating the efficacy and safety of LEN to date are the CAPELLA and CALIBRATE studies. In the CAPELLA trial, 72 patients with HIV, whose current regimens were failing and who had documented resistance to ≥2 ARVs from ≥3 of the ARV classes, were assigned to randomized cohort 1 or nonrandomized cohort 2. In the first cohort, 24/36 participants were randomized to oral LEN plus their failing regimen for 2 weeks, whereas placebo was added for the other 12 participants to evaluate the proportion of participants with ≥0.5 log copies/mL reduction in HIV RNA from baseline (primary outcome). In the second cohort, 36 participants were assigned to oral LEN plus an optimized background therapy (OBT) for 2 weeks (Table 7). On day 15, patients in both the treatment arm of cohort 1 and cohort 2 received subcutaneous (SQ) injection of LEN along with an OBT. Patients in the placebo arm of cohort 1 began a 2-week oral lead-in with LEN, followed by SQ LEN along with an optimized background regimen. After 26 weeks, 81% and 83% in cohort 1 and 2, respectively, achieved virologic suppression (P<0.001) (Figure 12).36 At week 52, 78% of patients had achieved VL <50 c/mL. Importantly, 8 participants had emergent LEN resistance, all of whom either had evidence of poor adherence to the OBT (n=4) or did not have any fullyactive agents in
15
the OBT (n=4).58
HIV-1 RNA <50 c/mL at LAI CAB + RPV initiation (n=234)
HIV-1 RNA <200 c/mL at LAI CAB + RPV initiation (n=252)
100 80 60 40 20 0 Participants, % Last HIV-1 RNA <50 c/mL Last HIV-1 RNA <200 c/mL Achieved HIV-1 RNA <200 c/mL CVF CVF 95 94 99 99 91 n≤5a n≤5a n≤5a
HIV-1 RNA ≥200 c/mL at LAI CAB + RPV initiation (n=21)
c, copies; CAB, cabotegravir; CVF, confirmed virologic failure; HIPAA, Health Insurance Portability and Accountability Act; LAI, long-acting injectable; RPV, rilpivirine.
aExact numbers/% for ≤5 observations cannot be specified because of HIPAA rules.
LAI
RPV
HIV Core (capsid, capsid core)
FIGURE 9. HIV Structure57
Lenacapavir inhibits multiple steps in the HIV life cycle
Capsid Disassembly and Nuclear Transport
Virus Production
Capsid Assembly
Capsid
Reverse Transcriptase
Integrase
Gag/Gag-Pol
(Capsid Precursors)
HIV RNA
HIV DNA
1. The outer lipid membrane of HIV encloses the inner capsid core that protects the viral RNA genome, protease, RT, and integrase, which all play an essential role in HIV replication
2. HIV attaches and fuses to the host CD4 cell membrane and releases the capsid core into the cytoplasm
3. Once in the host cell cytoplasm, the viral RT begins transcribing viral RNA into viral DNA while the capsid is transported to the host cell nucleus
4. The capsid core binds to nuclear import proteins to gain entry into the nucleus
5. Reverse transcription is completed and the capsid core disassembles
6. Viral DNA is integrated into the host cell DNA with the help of viral integrase
7. Viral precursor and polyproteins are translated and capsid precursor proteins assemble at the plasma membrane of the host cell
8. Immature noninfectious virions bud from the infected host cell
9. Inside the virions, capsid precursor proteins (HIV Gag) are cleaved by the viral protease and then assemble into a mature cone-shaped capsid shell that is now able to infect other host cells
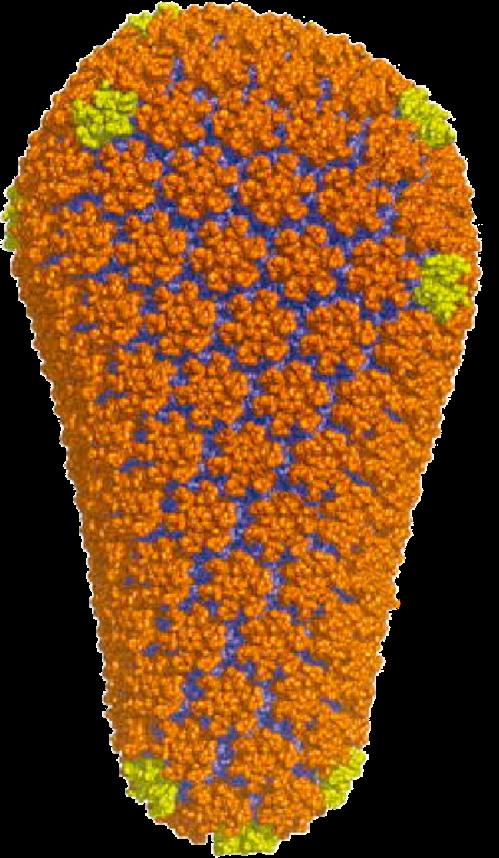
RT, reverse transcriptase.
Although LAI LEN is only currently FDA approved for HTE patients with HIV, it has been evaluated in treatmentnaive HIV patient populations. In the CALIBRATE study, 182 treatment-naive patients with HIV were randomly assigned to 4 treatment groups (2:2:2:1), stratified by plasma HIV RNA load (≤100,000 or >100,000 c/mL) at screening59:
1. SQ LEN + oral daily FTC/TAF for 28 weeks, after which virologically suppressed participants continued a 2-drug maintenance regimen of SQ LEN with daily TAF
2. SQ LEN + oral daily FTC/TAF for 28 weeks, after which virologically suppressed participants continued a 2-drug maintenance regimen of SQ LEN with BIC
3. Oral daily LEN + FTC/TAF
4. Oral daily BIC/FTC/TAF
In this treatment-naive population, LEN was noninferior to BIC/FTC/TAF after 54 weeks.59 These data, along with future studies, may lead to expanded FDA approval for LEN as a first-line therapy in treatment-naive patients with HIV.
16 EMERGING ISSUES IN HIV MANAGEMENT: ANSWERS TO PHARMACISTS’ COMMON QUESTIONS
FIGURE 10. Overview of the HIV Life Cycle57
p24 hexamer
LEN, lenacapavir.
FIGURE 11. LEN Binds Between Capsid Monomers (P24)
TABLE 7. Composition of Optimized Background Therapy36
Week 26 (presented at IAS 2021)
Week 52
What is the specific prescribing information for LAI LEN?
Secondary to the long PK tail, DDIs can still occur within 9 months of the last SQ dose of LEN, and residual drug concentrations may remain in the systemic circulation for ≥12 months after the last dose. Because LEN is a substrate of CYP3A, P-glycoprotein (P-gp), and UGT family 1 member A1 (UGT1A1), coadministration of LEN with combined P-gp, UGT1A1, and strong CYP3A inhibitors is not recommended because they may significantly increase plasma concentrations of LEN.38 Furthermore, LEN is a moderate inhibitor of CYP3A4 and can affect the concentration of other medications. LEN should be avoided with strong or moderate CYP3A4 inducers. It is also important to note that LAI LEN is not a complete regimen on its own and must be combined with other ARV agents for a complete active regimen (Table 8).
LEN is available in oral and SQ formulations and is given SQ every 6 months. It can be initiated using one of two dosage regimens (Table 9).38 It is stored at 20° C to 25° C (68° F–77° F) and excursions are permitted to 15° C to 30° C (59° F-86° F). If an unplanned missed injection occurs and it has been >28 weeks since last injection, restart from day 1 using one of the two dosage regimens if the patient is still deemed to be a good candidate for LAI LEN therapy.38
What are the roles for pharmacists in overcoming barriers to and administration of LAI ART?
Barriers to LAI ART can be gleaned from other fields of medicine where LAI medications have been used for decades, such as psychiatry. Some potential barriers include (1) lack of ancillary support to provide counseling and reminders for patients, as well as
17
Composition of OBT, % Cohort 1 Cohort 2 All Patients (N=72) LEN (n=24) Placebo (n=12) LEN (n=36) NRTI 96 75 81 85 INSTI 67 75 61 65 PI 50 75 67 62 NNRTI 25 33 39 33 IBA 38 25 14 24 MVC 8 33 11 14 FTR 12 0 14 11 T-20 4 17 6 7
FTR, fostemsavir; IBA, ibalizumab; INSTI, integrase strand transfer inhibitor; LEN, lenacapavir; MVC, maraviroc; NRTI, nucleoside reverse transcriptase inhibitor; NNRTI, non-nucleoside reverse transcriptase inhibitor; OBT, optimized background therapy; PI, protease inhibitor; T-20, enfuvirtide.
HIV-1 RNA cutoff 50 c/mL 200 c/mL 100 80 60 40 20 0 Participants, % Virologic Suppression Virologic Failure Virologic Suppression No Virologic Data Virologic Failure No Virologic Data 81 88 19 11 0 0 83 88 14 11 3 3
c, copies; IAS,
International AIDS Society.
FIGURE 12. Efficacy of LEN in the CAPELLA Randomized Cohort (n=36)58
TABLE
Information
Indications
Potential contraindications
Common adverse events
Special considerations
LAI LEN
• HTE adults with multidrug-resistant HIV failing their current antiretroviral regimen due to resistance, intolerance, or safety considerations
• Concomitant administration with strong CYP3A inducers increases risk of virologic failure
• Concomitant administration with strong CYP3A inhibitors increases risk of adverse events
• Mild to moderate injection-site reactions (pain, redness, swelling)
• Nausea
• Insufficient data on use during pregnancy or in pediatric patients
• Not a complete regimen on its own (must be combined with other ARV agents)
administration of the medication in the clinic setting; (2) personal patient preference for oral agents or needle phobia; (3) limited insurance coverage; and (4) lack of HCP comfort, including unease related to the long PK tail and potential for side effects.61,62 Fortunately, pharmacists have the ability and knowledge base to alleviate many of the system-related barriers to LAI ART. For example, pharmacists can aid in identifying and selecting the appropriate patients (eg, no risk factors for nonadherence, evaluation of ARV resistance, assessing HBV status), counsel and educate patients regarding adherence, potential side effects, and DDIs, investigate insurance coverage and assist with out-of-pocket costs, manage medication inventory, send timely injection reminders to patients, and administer the IM and SQ injections to patients. Moreover, pharmacists can aid in confirming and obtaining information regarding patient insurance coverage.
One of the unique intricacies related to LAI therapies is their extended half-life, with their corresponding
long PK tail after discontinuation. Although this can be beneficial by allowing for less-frequent injections, it also increases to the risk of side effects, especially serious ones, and DDIs that can occur numerous months or even a year after the last LAI ARV dose has been administered. Pharmacists have both experience and education on the nuances of pharmacokinetics, making them ideally positioned to manage these issues.
Because LAI ART is administered in the health care setting, it may be covered as a medical or a pharmacy benefit under a patient’s insurance.63 There are 2 types of insurance coverage for LAI ART: buy-and-bill and whitebagging. With the buy-and-bill approach, the provider purchases the drug from a specialty distributor and stores it for the patient until the time of administration, when the claim is submitted for reimbursement to the patient’s insurance. With the white-bagging approach, insurance companies make coverage of drugs contingent on the medication being distributed directly from a third-party specialty pharmacy to the provider’s
18 EMERGING ISSUES IN HIV MANAGEMENT: ANSWERS TO PHARMACISTS’ COMMON QUESTIONS
ARV, antiretroviral; CYP, cytochrome P450; HTE, heavily treatment-experienced; LAI, long-acting injectable; LEN, lenacapavir.
Induction dosing Maintenance dosing Option 1 Day 1 Day 2 Every 6 months (26 weeks) ± 2 weeks LEN 927 mg SQ 600 mg PO 600 mg PO 927 mg SQ Induction dosing Maintenance dosing Option 2 Day 1 Day 2 Day 8 Day 15 Every 6 months (26 weeks) ± 2 weeks LEN 600 mg PO 600 mg PO 300 mg PO 927 mg SQ 927 mg SQ LEN,
8. Prescribing
for LAI LEN36, 37,60
lenacapavir; PO, per os (by mouth); SQ, subcutaneous.
TABLE 9. LEN Dosing Regimens61
office. Buy-and-bill is typical of medications covered as a medical benefit; white-bagging is typical of medications covered as a pharmacy benefit.63 Not only does this complicate matters for patients, but clinics must separate buy-and-bill and white-bag inventories before they can be administered to patients and address patient out-ofpocket responsibilities for each method of acquisition. Although there are many complex details that need to be addressed regarding LAI ART administration, the phase 3b CUSTOMIZE study demonstrated that LAI CAB + RPV was not only successfully implemented across a range of US healthcare settings, but also that barriers were mitigated with minor process adjustments.64 At 4 months and 12 months, the proportion of staff-study participants (SSPs) who experienced barriers to LAI implementation at baseline decreased in all categories evaluated except patient injection/soreness, which stayed consistent (Figure 13).64 Additionally, 78% of SSPs reported optimal implementation of LAI CAB + RPV in their clinics
within 3 months. Based on SSP interviews, successful implementation was achieved through teamwork, using a web-based treatment planner, and having a designated person to track appointment scheduling.64
How do PWH feel about LAI ART?
In addition to systemic barriers to LAI ART administration, patients must be willing and able to adhere to LAI regimens to achieve positive outcomes from this therapy. The results of a recent self-administered patient questionnaire revealed that 74% of PWH would be willing to accept injections every month.65 Patients’ perceived advantages of LAI ART were being able to stop taking oral pill(s) every day, being more certain about efficacy, and being certain that they would not forget to take their ART (Figure 14).65 On the other hand, PWH’s most common perceived drawbacks of LAI ART were a fear of adverse effects and concern that the
19
Stop taking cART every day 73% Being certain of efficacy for a period of time 42% Being certain not to forget cART treatment 39% Hiding that I take cART treatment 0% No need to think of treatment every day 28% Forget the disease 19% Other 11% None 11% 0 20 10 40 30 60 50 70 80 PWH, % ART, antiretroviral therapy;
cART, combination antiretroviral therapy; LAI, long-acting injectable; PWH, people with HIV.
ability to keep monthly appointment Patients’ transportation for monthly appointment Flagging/Awareness of missed visits Staff resourcing for clinic flow Rescheduling missed injections Patients failing CAB + RPV LAI due to missed dose/visit Management of patients with other needs Patient injection/soreness 0 20 40 60 80 100 Proportion of SSPs, % Baseline (n=26) Month 4 (n=24) Month 12 (n=23)
FIGURE 14. PWH’s Perceived Advantages of LAI ART65
Patients’
CAB, cabotegravir; LAI, long-acting injectable; RPV, rilpivirine; SSP, staff-study participant.
FIGURE 13. Most Commonly Endorsed Barriers to Implementation Among SSPs64
clinic appointments would be too much of a constraint (Figure 15).65 Understanding PWH’s perceptions regarding LAI ART can help to guide shared decisionmaking discussions and reduce the risk of missed doses (nonadherence) and the development of treatmentemergent resistance patterns. Adherence is especially critical in HTE PWH because the armamentarium of active agents available to them is small.
In the SOLAR study mentioned previously, patient treatment preference was assessed, and it was found that 90% of patients preferred every-2-month injections compared with oral daily ART. Furthermore, more than 80% of the total respondents preferred LAI CAB + RPV because of convenience and not having to worry about remembering to take their HIV medication every day (Figure 16).46
Overall, LAI ART is a welcome addition to the HIV treatment armamentarium and will likely benefit many PWH through its less-frequent administration schedule, especially for patients who are concerned about the stigma associated with daily oral ART intake or are inconvenienced by high pill burden (possibly leading to nonadherence). Because each PWH has unique preferences, social situations, and feelings toward their HIV diagnosis and management, it is imperative that all members of the HIV care team implement shared decision-making strategies and continue to educate and counsel patients about the importance of adherence to ART regimens to achieve and maintain virologic suppression.
I don’t have to worry as much about remembering to take HIV medication every day
It is more convenient for me to receive injections Q2M
I do not have to carry my HIV medication with me
I do not have to think about my HIV status every day
I don’t have to worry about others seeing or finding my HIV pills
Proportion of Participants
BIC/FTC/TAF No preference
20
EMERGING ISSUES IN HIV MANAGEMENT: ANSWERS TO PHARMACISTS’ COMMON QUESTIONS
6% 29% 29% 6% 14% 17% 7% 9% 21% Loss of freedom Fear of adverse effects Fear of injections Fear of being treated as a guinea pig It would not change anything Already taking other treatments Too much a constraint Other None 0 10 5 20 15 30 25 PWH, % ART, antiretroviral therapy; LAI,
long-acting injectable; PWH,
people with HIV.
85% 83% 75% 61% 59%
FIGURE 15. PWH’s Perceived Drawbacks of LAI ART65
0 40 20 80 60 100
90% 5% 5%
CAB + RPV LAI Q2M
CAB + RPV LAI Q2M (n=382)
n=425 BIC, bictegravir; CAB, cabotegravir; FTC, emtricitabine; LAI, long-acting injectable; PWH, people with HIV; Q2M, every 2 months; RPV, rilpivirine; TAF, tenofovir alafenamide.
FIGURE 16. Treatment Preferences of PWH From the SOLAR study46
Part III: Heavily TreatmentExperienced PWH
How does the presence of drug-resistant mutations affect the management of HTE individuals?
As mentioned briefly with regard to LAI LEN, HTE patients with HIV are typically defined as those having ≤2 ARV classes available for use, with limited fully-active agents within each class.55 Along the same lines, MDR HIV refers to strains with reduced susceptibility to multiple ARV classes.17 Fortunately, the prevalence of HTE patients with HIV has declined dramatically, from 7.5% in 2006 to <1% in 2017, related to the introduction of high barrier to resistance drugs, including boosted PIs and second-generation INSTIs such as DTG and BIC.55 Despite their low prevalence, HTE patients are complex to manage even for the most experienced providers. The ultimate goal of ART is to create a regimen that will suppress viral replication to below the limit of detection.55 Effective HIV management maximally suppresses plasma HIV RNA, preventing disease progression and the emergence of drug-resistant virus. Maintaining an undetectable VL improves patient outcomes (eg, morbidity and mortality) and reduces the risk of HIV transmission,55 therefore benefitting both the patient and the community. In order to design an active ART regimen, providers must have a detailed understanding of the underlying processes that caused previous treatment failures, diagnostics to define the amount and mechanisms of resistance present, and available ARVs to achieve viral suppression in the face of multiple resistance mutations. The complexity involved in understanding previous and current individual drug-resistance mutations cannot be overstated, and designing an active ART regimen can be time consuming and challenging, especially in patients with numerous comorbidities and medications that may increase the risk of DDIs. Additionally, the dosage of certain ARVs may be different for these patients.
Drug-resistant mutations can predate the initiation of a specific ART regimen or can develop when viral replication continues in the face of ongoing drug pressure.17 The cause of MDR HIV is multifactorial and can vary greatly between patients. Many factors can contribute to an MDR virus, including the intrinsic biology of HIV, genetic barriers to resistance, ART regimen potency, pharmacokinetics of ARVs, and drug-taking behavior.17 HIV inherently has high rates of replication and an error-prone reverse transcriptase. This combination leads to the spontaneous occurrence of mutations, most of which decrease the fitness of the virus. Suboptimal drug levels that are unable to suppress viral replication allow the virus to continue to replicate and accumulate mutations. There are many potential causes of low serum trough concentrations. Specific pharmacokinetics of older ARVs, such as the unboosted PIs (eg, saquinavir) that had low bioavailability and very
rapid clearance resulted in rapid mutation accumulation and treatment failure. But low serum drug concentration can also can occur due to DDIs (eg, poor absorption, competing CYP or transporter metabolism), varying half-lives between agents in combination ART, and poor drug-taking behavior (such as missed doses) that allows viral replication in the face of suboptimal drug exposure.66 Mutations can persist in proviral HIV DNA in resting CD4+ memory T cells even if HIV RNA suppression is achieved with a subsequent, more-potent regimen. If in the future drugs to which viable proviral mutations exist are used, mutants can reemerge in the plasma viral RNA and either cause overt virologic failure or become more drug resistant through the gradual accumulation of additional resistance mutations.
The genetic barrier to resistance is a complex concept, and finding an exact definition can be elusive. In general, it describes how hard it is for the virus to become resistant to a specific drug. HIV can more easily (and quickly) become resistant to a drug with a lower barrier to resistance than to one with a higher barrier. Resistance should be seen as a continuum, not an absolute high or low barrier.67 Additionally, drug exposure is a key component of the barrier to resistance; therefore, the same drug given at a higher dosage will result in a higher barrier to resistance (eg, DRV/r dosed once or twice a day). Individual ARVs have higher or lower genetic barriers to resistance. In general, when ARVs have a higher barrier to resistance, they lose clinical utility only after the accumulation of multiple mutations. On the contrary, when an agent has a low barrier to resistance, one mutation is usually enough to cause virologic failure. High barrier to resistance drugs require longer periods of viral replication to become resistant and fail than low barrier drugs; therefore, they are more tolerant and forgiving of poor drug-taking behavior. They also require fewer additional active agents than low-barrier drugs.67
How do I approach decision-making when a patient with HIV presents with virologic failure?
There are many potential causes of virological failure, and HCPs must make every effort to determine which of these are contributing to the loss of viral suppression. The first step is to examine drug-taking behavior, such as missed doses. Once proper adherence has been established or associated barriers to adherence (eg, intolerance to side effects or pill burden, issues with medication procurement, difficulty swallowing pills) are resolved, treatment issues related to pharmacokinetics (eg, DDIs leading to poor absorption or rapid clearance) should be explored and ruled out.55 It is important to investigate the use of OTC medications and food supplements with patients taking ARVs, as well as reconciling their known prescription medications. Examples of common DDIs include acid-suppressant OTC medications that can prevent the absorption of oral acid-dependent absorption ARVs (eg, RPV, atazanavir) and medications with polyvalent cations
21
Where to Check for ARV Drug-Drug Interactions
Liverpool HIV Drug Interactions: https://www.hiv-druginteractions.org/checker
New York State Department of Health AIDS Institute: https://www.hivguidelines.org/antiretroviral-therapy/ddis/ Department of Health and Human Services: https://clinicalinfo.hiv.gov/en/guidelines/hiv-clinical-guidelinesadult-and-adolescent-arv/drug-interactions-overview
(such as magnesium, calcium, iron, or aluminum), including multivitamins, that may cause chelation of INSTIs and reduced absorption when coadministered.55 Moreover, medications that significantly induce the CYP3A4 pathway (eg, carbamazepine, rifamycin) can drastically reduce levels of many ARVs and are often contraindicated.55 For more specific information about individual drug interactions with ARVs, the University of Liverpool has an online database of HIV drug interactions that is useful to check (either on their website or smartphone app) before new medications are added to a PWH’s regimen, or to confirm that there are no current DDIs that may be contributing to virologic failure.50
What resistance testing should be performed?
For all patients whose ART regimen is not successful, genotypic resistance testing should be performed while the patient is still on the regimen or immediately after stopping. It is also very helpful to have complete historical genotype results, if possible, because results often change when new drugs are used. Circulating genotypes generally require an HIV VL of >200 c/mL (frequently even >500 c/mL is necessary) to be completed but this is lab dependent.55 Proviral DNA testing is a potential option, although currently not validated as a useful clinical tool, when the VL is between 200 and 500 c/mL. Genotype testing typically screens for mutations on the 3 major HIV enzymes: reverse transcriptase, protease, and integrase (which in some labs needs to be ordered separately). Because combinations of mutations can be synergistic or mitigating, interpreting test results and applying them to develop a new active ART regimen can be extremely challenging. There are a number of interpretation systems available to assist. Examples include the Stanford HIV Drug Resistance Database (online and free) and assistance from the “HIV warmline,” a national clinical consultation center operated by the University of California, San Francisco, that can be utilized for assistance.68,69 Using the Stanford database, an individual’s resistance can be assessed by entering known resistance mutations, which generates the level of resistance to each drug and ARV class. This information can then be used to develop an active ART regimen.
Rarely, phenotypic and tropism testing may be considered. Phenotypic resistance testing reports the concentration of drug needed to inhibit 50% of viral growth. This may be useful when many RAMs are present, but it is more expensive and takes longer to receive
results compared with genotype testing.55 Phenotypic tests have also not been clinically validated for many of the currently used drugs and, in general, should be ordered only in consultation with experts. Tropism screening is used to determine which coreceptor an individual’s specific HIV variant uses during the viral entry process. This is required when evaluating whether or not to include maraviroc (MVC) in an ART regimen because MVC requires C-C chemokine receptor type 5 (CCR5) as the only coreceptor in order to be effective.55 Although not commonly used in treatmentnaive patients, MVC may be useful in HTE individuals if tropism testing confirms activity.
How do I select an active ART regimen for an HTE individual with HIV?
When choosing a new ART regimen for an HTE individual, both resistance results and ARV history should be considered.55 Regimens for HTE individuals are often complex and may require twice-daily dosing and multiple pills. Therefore, counseling the patient and motivating them are the keys to success. If possible, it is also beneficial to simplify the regimen to promote adherence, but only if antiviral potency is not sacrificed. Ideally, resistance testing should be performed when a patient is either on the failing regimen or within 3 to 4 weeks of regimen discontinuation, to maximize the detection of all resistance mutations present. Because previous resistance mutations may not result from current circulating HIV, archived resistance testing may be useful, but caution is necessary because false-positives or -negatives are possible.17 Proviral DNA testing for archived resistance and its interpretation should only be done with expert advice. Other important considerations when selecting an ART regimen include the presence or likelihood of DDIs, either between ARVs or between medications for comorbid conditions, and the presence of coinfection with HBV, that will require treatment with tenofovir, FTC, and/or 3TC.55 Discontinuing agents aimed at HBV treatment can result in an acute hepatitis flare even if these ARVs are not currently active against the individual’s HIV. Also, use of 3TC or FTC as the sole HBV drug is contraindicated. If HBV infection has not been ruled out, regimens containing TDF/TAF with 3TC/ FTC cannot be discontinued.70 Medication history may also help guide treatment decisions, as patterns of ARV use may suggest common resistance to those agents. This is especially important in the absence of previous resistance testing as a guide.
In extremely HTE individuals or some resourcelimited settings, a fully-suppressive ART regimen may
22 EMERGING ISSUES IN HIV MANAGEMENT: ANSWERS TO PHARMACISTS’ COMMON QUESTIONS
not be possible. It is important to note that it is not recommended to add one fully-active ARV agent to the failing regimen nor to place the patient on treatment interruption. An active ART regimen should be created with a combination of ARVs with ≥2 known fully-active agents (overall activity score of 2, with each agent getting a score between 0 and 1, with 0 being no activity, 0.5 being partial activity, and 1 being full activity). Drugs with a high barrier to resistance should be preferred, if at all possible, and should be used at the highest dose approved (eg, DTG 50 mg × 2). If only one of these classes is fully active, other partially-active agents may be used to complete the regimen.17 Selecting a salvage regimen is individualized to the patient, based on their unique pattern of resistance; however, there are certain ARVs that are more likely to remain active in this population (Table 10A-D).55 Drugs utilizing new mechanisms of action such as fostemsavir (FTR) and LEN remain fully active in these patients and should be included in the regimen if there is doubt about there being sufficient activity.
Based on our knowledge of resistance mechanisms in HIV, certain clinical considerations are particularly important: FTC and 3TC are both commonly used in HIV regimens, and the most prevalent NRTI-associated mutation, M184V, results in high-level resistance to these drugs. But the presence of M184V reduces viral fitness and actually increases sensitivity to some NRTIs (eg, tenofovir).71,72 Furthermore, concurrent K65R and M184V mutations may return partial activity to tenofovir. Studies
A: Major NRTI Resistance Mutations
have shown 3TC continues to have a suppressive impact on HIV RNA levels (about 0.5 log), even when M184V is present. Thus, continuing 3TC or FTC may have clinical value even when M184V is detected. Furthermore, a K65R + M184V mutational profile does not negate a contribution to viral suppression if tenofovir with either 3TC or FTC is prescribed in combination with a boosted PI or DTG.73,74 Some of the pivotal clinical trials evaluating ARVs in HTE patients can help guide the individualized selection of an active ART regimen (Table 11); however, given the breadth and intricacy involved in interpreting results of resistance testing and then designing an active ART regimen in HTE patients, it is imperative that only experienced HIV providers undertake this task in clinical practice. Input from a pharmacist with expertise in HIV drugs can be extremely helpful.
Overall, some of the basic principles in the management of HTE PWH include using DTG and/or a boosted PI (preferably boosted DRV) as the new regimen if sufficiently active and especially if resistance to multiple agents is present. Both boosted DRV and DTG have a higher barrier to resistance when dosed twice daily and are needed for many advanced HTE PWH. In general, the new regimen is designed by combining drugs with remaining activity to build a regimen with a sufficiently high barrier to resistance to avoid future failure while minimizing DDIs, toxicity, and complex dosing schedules. Although this process must be individualized, there are some basic principles that can be considered55:
3TC, lamivudine; ABC, abacavir; AZT, zidovudine; d4T, stavudine; DRM, drug-resistance mutation; DRV, darunavir; DTG, dolutegravir; FTC, emtricitabine; Ins, insertion; INSTI, integrase strand transfer inhibitor; MDR, multidrug resistance; NRTI, nucleoside reverse transcriptase inhibitor; PI, protease inhibitor; r, ritonavir; TAM, thymidine analog mutation; TAF, tenofovir alafenamide; TDF, tenofovir disoproxil fumarate; TFV, tenofovir; VF, virologic failure.
Bold underline: High-level reduced susceptibility or virologic response. Bold: Reduced susceptibility or virologic response. Plain text: Reduced susceptibility in combination with other NRTI-resistance mutations. Asterisk: Increased susceptibility.
M184VI: Although they cause high-level in vitro resistance to 3FTC, they are not contraindications to 3FTC because they increase TFV and AZT susceptibility and decrease viral replication fitness. K65R: The most common DRM in patients with VF on a TFV-regimen. It causes a clinically relevant 2-fold reduction in TFV susceptibility. However, K65R + M184VI reduces TFV susceptibility <1.5-fold. INSTI-/PI-naive patients with K65R + M184VI who receive TFV/3FTC and a highly potent third drug (eg, DTG or DRV/r) respond as well or better than those receiving AZT/3TC, even though K65R increases AZT susceptibility. TFV, TDF, and TAF: TDF and TAF are TFV triphosphate prodrugs. Although TDF and TAF have similar resistance profiles, TAF attains higher intracellular levels.
Additional TFV-selected mutations of uncertain phenotypic and clinical significance include A62V, K65N, K70GQNTdel, and L74I. TAMs: Selected by AZT and d4T; facilitate primer unblocking. Non-TAMs prevent NRTI incorporation. T215SCDEIVALN (T215 revertants) emerge from T215YF in the absence of NRTIs. MDR: T69 insertions occur with TAMs. Q151M occurs with non-TAMs and the accessory mutations A62V, V75I, F77L, and F116Y.
23
Non-TAMs TAMs MDR 184 65 70 74 115 41 67 70 210 215 219 69 151 Cons M K K L Y M D K L T K T Q 3TC VI R Ins M FTC VI R Ins M ABC VI R E VI F L W FY Ins M TFV *** R E F L R W FY Ins M AZT ** ** * L N R W FY QE Ins M
TABLE 10 A-D. Major HIV-1 Drug Resistance Mutations68
TABLE 10 A-D. Major HIV-1 Drug Resistance Mutations68
B: Major NNRTI Resistance Mutations
DOR, doravirine; EFV, efavirenz; ETR, etravirine; NNRTI, non-nucleoside reverse transcriptase inhibitor; NVP, nevirapine; RPV, rilpivirine.
Bold underline: High-level reduced susceptibility or virologic response. Bold: Reduced susceptibility or virologic response. Plain text: Reduced susceptibility in combination with other NNRTI-resistance mutations.
Additional Mutations: A98G (DOR, EFV, ETR, NVP, RPV); E138GQKR are nonpolymorphic mutations associated with intermediate/high-level RPV resistance. E138A is a polymorphic mutation associated with low-level RPV resistance. Y188CH are associated with intermediate/high-level resistance to EFV; G190Q is a rare mutation that may have an effect similar to G190E; P225H (DOR, EFV); L234I (DOR); Y318F (DOR, NVP).
Synergistic combinations: V179D + K103R reduce NVP and EFV susceptibility >10-fold. Y181C + V179F cause high-level ETR and RPV resistance.
DOR and ETR often require multiple mutations: DOR—high level with Y188L, V106A, F227L/C, M230L, or any combination of V106 and F227 mutations.
ETR: L100I, K101P, Y181C/I/V, M230L. But multiple non-DOR mutations at common positions such as Y181 and G190 can produce intermediate levels of reduced DOR susceptibility.
C: Major INSTI Resistance Mutations
BIC, bictegravir; CAB, cabotegravir; DRM, drug-resistance mutation; DTG, dolutegravir; EVG, elvitegravir; INSTI, integrase strand transfer inhibitor; RAL, raltegravir.
Bold underline: High-level reduced susceptibility or virologic response. Bold: Low-level reduced susceptibility or virologic response.
Plain text: Reduced susceptibility in combination with other INSTI-resistance mutations.
Additional mutations: T97A is a polymorphic mutation (1%-4%) in INSTI-naive patients. In combination with Q148 + G140/E138 DRMs, it causes high-level BIC/DTG resistance. H51Y, F121Y, S147G, S153YF, and S230R are additional nonpolymorphic INSTI DRMs. E92GV, Y143HKSGA, P145S, Q146LP, Q148N, G149A, V151AL, and N155ST are rare nonpolymorphic mutations that reduce RAL and/or EVG susceptibility. L74M, V151I, E157Q, G163KR, and D232N are common polymorphic accessory DRMs. Mutations outside of IN in the polypurine tract have also rarely been reported to reduce INSTI susceptibility.
D: Major PI Resistance Mutations
ATV, atazanavir; DRV, darunavir; LPV, lopinavir; NFV, nelfinavir; PI, protease inhibitor; r, ritonavir.
Bold underline: High-level reduced susceptibility or virological response. Bold: Reduced susceptibility or virological response. Plain text: Reduced susceptibility in combination with other PI-resistance mutations.
Additional mutations: L10F, V11I, K20TV, L23I, L33F, K43T, F53L, Q58E, A71IL, G73STCA, T74P, N83D, and L89V/T are common nonpolymorphic accessory resistance mutations. L10F, V11IL, L33F, T74P, and L89V are accessory resistance mutations associated with reduced DRV/r susceptibility. D30N and N88D are nonpolymorphic resistance mutations selected by NFV. L10RY, V11L, L24F, M46V, G48ASTLQ, F53Y, I54S, V82CM, I84AC, N88TG are rare nonpolymorphic variants.
24 EMERGING ISSUES IN HIV MANAGEMENT: ANSWERS TO PHARMACISTS’ COMMON QUESTIONS
100 101 103 106 181 188 190 227 230 Cons L K K V Y Y G F M DOR I E AM IV L SE LC L EFV I EP NS AM CIV L ASE LC L ETR I EP CIV L ASE C L RPV I EP CIV L ASE C L NVP I EP NS AM CIV L ASE LC L
66 92 118 138 140 143 148 155 263 Cons T E G E G Y Q N R BIC K Q R KAT SAC HRK H K CAB K Q R KAT SACR HRK H K DTG K Q R KAT SAC HRK H K EVG AIK Q R KAT SAC HRK H K RAL AIK Q R KAT SAC RCH HRK H K
32 46 47 48 50 54 76 82 84 88 90 Cons V M I G I I L V I N L ATV/r I IL V VM L VTALM ATFS V S M DRV/r I VA V LM V F V LPV/r I IL VA VM V VTALM V AFTS V M
TABLE 11. Overview of Pivotal Clinical Trials Evaluating the ARVs in HTE PWH
ARV Drug Class
Etravirine (ETR)
Dolutegravir (DTG)
DUET 1 and 275:
Pivotal Clinical Trials
• ETR 200 mg BID (n=599) vs placebo (n=604) with OBT for all HTE participants
• All patients in both groups received DRV/r
• At week 96, 57% of the patients in the ETR group vs 36% in the placebo group had VL <50 c/mL (P<0.0001)
SAILING76:
• DTG 50 mg per day (n=354) vs RAL 400 mg BID (n=361), both with OBT
• At week 48, 71% of patients on DTG had VL <50 c/mL compared with 64% of patients on RAL (P=0.03)
VIKING-377:
• HTE patients with INSTI-resistant HIV (N=183)
• DTG 50 mg BID while continuing failing regimen (without RAL or EVG) through day 7, then the regimen was optimized with ≥1 fully-active drug + DTG
• 69% of patients achieved VL <50 c/mL at 24 weeks (P<0.001)
BRIGHTE78,a:
Fostemsavir (FTR)
• 2 groups of patients with VL ≥400 c/mL: (1) those with 1 or 2 remaining active classes although unable to construct a fully-active regimen among remaining agents (n=272) and (2) those with no remaining active classes (n=99)
• FTR 600 mg BID added to OBT
• 60% of group 1 and 37% of group 2 were able to achieve a VL <40 c/mL at week 96
• CD4 cell counts and CD4/CD8 ratios continued to improve throughout the study
TMB-30179:
• Adults with multiple regimen failures, resistance to ≥1 drug in 3 different classes, and an elevated VL >1000 c/mL (N=40)
Ibalizumab (IBA)
• IBA loading dose of 2000 mg IV, then IBA 800 mg every 14 days, along with an OBT containing ≥1 fully-active agent
• 43% achieved a VL <50 c/mL at week 25
• Mean reduction from baseline in the VL was 1.6 log10 c/mL and the median reduction was 1.8 log10 c/mL
MOTIVATE 1 and 280,a:
• Patients with CCR5 HIV only who have experience with or resistance to ≥3 different classes of ARVs and VL >5000 c/mL (N=1049)
• MVC once daily (n=414) vs MVC BID (n=426) vs placebo (n=209); all with OBT
Maraviroc (MVC)
• 39% and 41% of patients receiving MVC daily or BID, respectively, achieved VL <50 c/mL at week 96
• Among patients with VL <50 c/mL at week 48, 81% and 87% of patients receiving MVC daily or BID, respectively, maintained this response at week 96
• At week 96, median CD4+ T-cell counts increased from baseline by 89 and 113 cells/mm3 with MVC daily and BID, respectively
CAPELLA37:
Lenacapavir
(LEN)
• Patients with failing regimens who had resistance to ≥2 ARVs from ≥3 of the ARV classes were randomized 2:1 to oral LEN + failing regimen for 2 weeks then LEN SQ for 6 months + OBT or placebo + failing therapy for 2 weeks then oral LEN for 2 weeks and SQ LEN for 6 months, both with OBT (randomized cohort 1; n=36) or oral LEN with OBT on days 1 through 14; subcutaneous LEN was then administered once every 6 months starting on day 15 (nonrandomized cohort 2; n=36)
• In cohort 1, a decrease of ≥0.5 log10 c/mL in the VL by day 15 was observed in 88% of patients in the LEN group and in 17% of patients in the placebo group (P<0.001)
aStatistical analysis was not reported in this reference.
ARV, antiretroviral; BID, twice daily; c, copies; CCR5, C-C chemokine receptor type 5; HTE, heavily treatment-experienced; INSTI, integrase strand transfer inhibitor; ISL, islatravir; ITT, intention-to-treat; IV, intravenous; OBT, optimized background therapy; RAL, raltegravir; SQ, subcutaneous; VL, viral load.
25
• Either DTG or DRV/r can be given and do not need to be combined if there is no resistance to their ARV class and there is at least one fully-active agent that can be combined with them
• If there is PI resistance, DTG should be preferred
• If INSTI resistance, DRV/r should be preferred
• If there is both PI and INSTI resistance, both should be used, along with at least one additional active drug(s). This may often be a drug from a novel class, such as fostemsavir (FTR) or LEN
• These drugs from a novel class should be used whenever a fully-active regimen cannot be designed with an NRTI, NNRTI, PI, and INSTI. Delaying use of these novel agents should be discouraged
BIC and DOR are not approved for use in treatmentexperienced patients. Use of these drugs in HTE individuals should only be in the context of a clinical trial or with consent for off-label use. A recent study evaluated the safety and efficacy of switching HTE PWH from RPV/FTC/TAF + DTG to BIC/FTC/TAF + DOR in men aged ≥45 years with documented viral resistance to PIs, NRTIs, and/or NNRTIs but no resistance to RPV or DOR and no K65R or T69 insertion mutations who were virally suppressed for ≥6 months (HIV RNA ≤50 c/mL). The results of this study showed that BIC/ FTC/TAF + DOR was well tolerated, with no serious or treatment-related adverse events reported and no appreciable change in BMI from baseline to week 48. At week 48, 100% of participants (N=20) had HIV RNA ≤50 c/mL.81 This study suggests that patients who are well suppressed on a regimen of RPV/FTC/TAF + DTG and have no RPV or DOR resistance and no K65R or T69 insertion mutations can be switched to BIC/FTC/ TAF + DOR. Further study of the role of BIC and/or DOR, either dosed once or twice a day, in treatmentexperienced patients would be very helpful and might increase options for these patients.
As a rule, ART regimens should be kept as simple as possible to promote adherence, although this may be exceedingly difficult to achieve in HTE individuals. A common mistake is to simplify a regimen in advanced HTE (eg, switching from twice-daily to once-daily dosing, or reducing the number of pills), without making sure the new regimen has a sufficient barrier to resistance. As these patients with multiple class resistance may not have any remaining options, such failure can have dire clinical consequences. For some patients, adhering to a complex regimen can be exceedingly difficult, even with support, especially when required for many months or years, and contributes to virologic failure. The HCP team needs to balance the desire for a regimen the individual can adhere to with the need for sufficient antiviral activity—not always an easy task.17 It is important to remember that not all HTE patients are the same and there is a broad spectrum, going from those with one or two failures and a small number of mutations, to those with multiple failures and a large number of mutations. In the former case, simplifying to a less-complex and demanding regimen may be possible (including once-
daily dosing), but in the latter case, this is often simply not possible and will lead to an insufficiently-potent regimen and failure. In the past, new drug classes for HTE patients required IV administration (ibalizumab [IBA]) or twice-daily dosing (FTR). But the recently approved capsid inhibitor, LEN, provides both a new mechanism of action with no cross-resistance to other ARVs and exceptionally convenient twice-yearly SC dosing, offering a new opportunity to simplify regimens while maintaining potency.38 When using FTR and IBA, HCPs must remember they are not high barrier to resistance drugs and cannot replace DRV/r or DTG unless there are other fully-active drugs to protect from failure.82 Lastly, HCPs designing a new regimen for HTE individuals must always keep in mind that shared decision-making conversations and individualization of ART regimens are critically important for achieving optimal patient outcomes.
What should be done if an HTE individual cannot achieve complete virologic suppression?
For HTE patients with MDR HIV, VL testing should be obtained 3 to 4 weeks after initiating the new regimen, and HIV RNA levels should be monitored at 4- to 8-week intervals until the VL is undetectable.55 In cases of incomplete virologic suppression, in which a patient with HIV has two VLs >200 c/mL at least 4 weeks apart and 24 weeks after initiating a new regimen, the HCP must urgently seek the cause of unsuccessful suppression by revaluating drug-taking behavior, exploring potential DDIs, and examining if the current regimen is sufficiently potent. Repeat genotypic resistance testing should be performed and evaluated for further accumulation of resistance. A new regimen should be considered and implemented as soon as possible. Treatment interruption or ARV discontinuation in these cases is associated with negative clinical and virologic outcomes.83,84 In the rare and unfortunate case in which there is simply no effective regimen, the HCP and patient must make hard decisions. Both stopping therapy and continuing a partially suppressive regimen are associated with poor outcomes, and one must decide which is the lesser evil. Discontinuing all drugs may lead to rapid loss of CD4+ and clinical progression, whereas continuing a partially suppressive regimen will ultimately lead to accumulation of mutations and complete loss of all drugs in the regimen. There are some short-term benefits of continuing a partiallysuppressive regimen due in part to highly resistant virus often being less fit and therefore replicating more slowly than wild-type HIV, resulting in lower VL, which prevents or delays CD4+ loss.85 Stopping all ARVs has the short-term benefit of preventing further resistance but will likely lead to CD4 loss and clinical progression and, ultimately, death. Factors such as current CD4+ levels, nadir CD4+ and peak HIV RNA, and the potential for new drugs to become available in the near future, as well as patient preferences, are key in making the decision. If the decision is to continue
26 EMERGING ISSUES IN HIV MANAGEMENT: ANSWERS TO PHARMACISTS’ COMMON QUESTIONS
partially-suppressive therapy, the HCP should consider stopping low barrier to resistance drugs such as NNRTIs and continuing 3TC/FTC and high barrier to resistance drugs such as boosted DRV.
What are the roles for pharmacists in HIV management of HTE patients?
Similar to their roles in rapid ART and implementation of LAI ART, pharmacists are integral members of the multidisciplinary HIV care team. Knowledge and expertise in the pharmacologic characteristics of ARVs, as well as co-medications (and vitamins/supplements) being prescribed are crucial for caring for these complex HTE individuals. Co-medications, underlying comorbidities such as renal or hepatic impairment, and need for high levels of ARV exposure, make selecting drugs and doses extremely complex, and having a pharmacist on the team greatly improves the chances of success. A large part of supporting PWH involves counseling and education on medication administration and procurement, potential side effects, and adherence.
List of Abbreviations
3TC Lamivudine
ABC Abacavir
ART Antiretroviral therapy
ARV Antiretroviral
ATV Atazanavir
AZT Zidovudine
BIC Bictegravir
BMI Body mass index
C Copies
CAB Cabotegravir
CCR5 C-C chemokine receptor type 5
CCSI CrescentCare Start Initiative
COBI Cobicistat
CVF Confirmed virologic failure
CYP Cytochrome P450
DDI Drug-drug interaction
DHHS Department of Health and Human Services
DOR Doravirine
DRM Drug resistance mutation
DRV Darunavir
DTG Dolutegravir
Pharmacists can not only provide these services, but they can also engage social workers and wraparound services, all leading to improved patient outcomes. Without question, pharmacists have a central role in the care of HTE individuals.
Concluding Comments
Recent US and global HIV initiatives are aimed at improving rates of virologic suppression in PWH, as well as reducing the incidence of new HIV infections. Rapid initiation of ART and treatment advances, such as LAI ARVs, can be implemented to achieve these goals by quickly achieving virologic suppression in both patients newly diagnosed with HIV, as well as HTE patients, and by improving adherence and linkage to care across the spectrum of PWH. Pharmacists play integral roles in multidisciplinary HIV care teams and, with the proper education, can be relied upon not only to counsel and educate patients, but also to select and implement ART regimens in even the most complex patients with HIV.
EACS European AIDS Clinical Society
eCrCl Estimated creatinine clearance
EFV Efavirenz
EHE Ending the HIV Epidemic in the US
ETR Etravirine
EVG Elvitegravir
FDA US Food and Drug Administration
FTC Emtricitabine
FTR Fostemsavir
HBV Hepatitis B virus
HCP Health care provider
HLA Human leukocyte antigen
HTE Heavily treatment-experienced
IAS International AIDS Society
IBA Ibalizumab
IM Intramuscular
INSTI Integrase strand transfer inhibitor
IRIS Immune reconstitution inflammatory syndrome
LAI Long-acting injectable
LEN Lenacapavir
MDR Multidrug resistance
27
EMERGING ISSUES IN HIV MANAGEMENT: ANSWERS TO PHARMACISTS’ COMMON QUESTIONS
MSM
Men who have sex with men
MVC Maraviroc
NNRTI Non-nucleoside reverse transcriptase inhibitor
NRTI Nucleoside reverse transcriptase inhibitor
NTD Neural tube defect
NVP Nevirapine
OTC Over-the-counter
PCP Primary care provider
PI Protease inhibitor
PrEP Pre-exposure prophylaxis
PWH People with HIV
r Ritonavir
References
1. Centers for Disease Control and Prevention. HIV in the United States by Region: HIV Incidence. https://www.cdc.gov/hiv/statistics/ overview/incidence.html. Accessed May 1, 2023.
2. Centers for Disease Control and Prevention. HIV Diagnoses. https:// www.cdc.gov/hiv/statistics/overview/in-us/diagnoses.html. Accessed May 1, 2023.
3. Department of Health and Human Services. Aging with HIV. https:// www.hiv.gov/hiv-basics/living-well-with-hiv/taking-care-of-yourself/ aging-with-hiv/. Accessed May 1, 2023.
4. Frescura L, Godfrey-Faussett P, Feizzadeh AA, El-Sadr W, Syarif O, Ghys PD. Achieving the 95 95 95 targets for all: a pathway to ending AIDS. PloS One. 2022;17(8):e0272405.
5. Heath K, Levi J, Hill A. The Joint United Nations Programme on HIV/ AIDS 95-95-95 targets: worldwide clinical and cost benefits of generic manufacture. AIDS. 2021;35(suppl 2):S197-S203.
6. Lundgren JD, Babiker AG, Gordin F, et al. Initiation of antiretroviral therapy in early asymptomatic HIV infection. N Engl J Med. 2015;373(9):795-807.
7. Danel C, Moh R, Gabillard D, et al. A trial of early antiretrovirals and isoniazid preventive therapy in Africa. N Engl J Med. 2015;373(9):808-822.
8. García-Deltoro M. Rapid initiation of antiretroviral therapy after HIV diagnosis. AIDS Rev. 2019;21(2):55-64.
9. Rosen S, Maskew M, Fox MP, et al. Initiating antiretroviral therapy for HIV at a patient’s first clinic visit: the RapIT randomized controlled trial. PLoS Med. 2016;13(5):e1002015.
10. Labhardt ND, Ringera I, Lejone TI, et al. Effect of offering sameday ART vs usual health facility referral during home-based HIV testing on linkage to care and viral suppression among adults with HIV in Lesotho: the CASCADE randomized clinical trial. JAMA. 2018;319(11):1103-1112.
11. Coffey S, Bacchetti P, Sachdev D, et al. RAPID antiretroviral therapy: high virologic suppression rates with immediate antiretroviral therapy initiation in a vulnerable urban clinic population. AIDS. 2019;33(5):825-832.
12. Huhn GD, Crofoot G, Ramgopal M, et al. Darunavir/cobicistat/ emtricitabine/tenofovir alafenamide in a rapid-initiation model of care for human immunodeficiency virus type 1 infection: primary analysis of the DIAMOND study. Clin Infect Dis. 2020;71(12):3110-3117.
13. Colasanti J, Sumitani J, Mehta CC, et al. Implementation of a rapid entry program decreases time to viral suppression among vulnerable persons living with HIV in the southern United States. Open Forum Infect Dis. 2018;5(6):ofy104.
RAL Raltegravir
RAM Resistance-associated mutation
REACH Rapid Entry and ART Clinic for HIV
RPV Rilpivirine
d4T Stavudine
TAF Tenofovir alafenamide
TAM Thymidine-analog mutation
TDF Tenofovir disoproxil fumarate
TFV Tenofovir
U=U Undetectable=Untransmittable
UGT Uridine 5'-diphospho-glucuronosyltransferase
WHO World Health Organization
14. Halperin J, Butler I, Conner K, et al. Linkage and antiretroviral therapy within 72 hours at a Federally Qualified Health Center in New Orleans. AIDS Patient Care STDS. 2018;32(2):39-41.
15. Šablinskaja A, Pauskar M, Jõgeda EL, et al. No transmitted drug resistance to HIV integrase strand-transfer inhibitors after their scaleup in Estonia in 2017. J Glob Antimicrob Resist. 2023;33:83-88.
16. Rutstein SE, Chen JS, Nelson JAE, Phiri S, Miller WC, Hosseinipour MC. High rates of transmitted NNRTI resistance among persons with acute HIV infection in Malawi: implications for first-line dolutegravir scale-up. AIDS Res Ther. 2019;16(1):5.
17. Department of Health and Human Services. Guidelines for the Use of Antiretroviral Agents in Adults and Adolescents with HIV. https:// clinicalinfo.hiv.gov/en/guidelines/hiv-clinical-guidelines-adult-andadolescent-arv/initiation-antiretroviral-therapy. Accessed May 1, 2023.
18. Gandhi RT, Bedimo R, Hoy JF, et al. Antiretroviral drugs for treatment and prevention of HIV infection in adults: 2022 recommendations of the International Antiviral Society-USA Panel. JAMA. 2023;329(1):63-84.
19. Zash R, Makhema J, Shapiro RL. Neural-tube defects with dolutegravir treatment from the time of conception. N Engl J Med. 2018;379(10):979-981.
20. Zash R, Holmes L, Diseko M, et al. Neural-tube defects and antiretroviral treatment regimens in Botswana. N Engl J Med. 2019;381(9):827-840.
21. Coffey S, Bacon O. Immediate ART Initiation and Restart: Guide for Clinicians. https://aidsetc.org/sites/default/files/resources_files/ncrcrapid-art-6-10-21_0.pdf. Accessed May 1, 2023.
22. Dean L. Abacavir therapy and HLA-B*57:01 genotype. In: Pratt VM, Scott SA, Pirmohamed M, Esquivel B, Kattman BL, Malheiro AJ, eds. Medical Genetics Summaries. Bethesda, MD: National Center for Biotechnology Information (US); 2012.
23. Al-Hayani AWM, Cabello-Úbeda A, Del Palacio-Tamarit M, et al. Initiation of antiretroviral therapy in treatment-naive adults with HIV infection at the first specialist appointment. J Antimicrob Chemother. 2022;77(6):1741-1747.
24. Chen KH, Liu WD, Sun HY, et al. Immune reconstitution inflammatory syndrome in people living with HIV who presented with interstitial pneumonitis: an emerging challenge in the era of rapid initiation of antiretroviral therapy. Microbiol Spectr. 2023;11(2):e0498522.
25. Radix A, Fine SM, Vali RM, et al. Rapid ART Initiation. https://cdn. hivguidelines.org/wp-content/uploads/20230209143050/NYSDOHAI-Rapid-ART-Initiation_2-9-2023_HG.pdf. Accessed May 1, 2023.
28
26. Blanc FX, Sok T, Laureillard D, et al. Earlier versus later start of antiretroviral therapy in HIV-infected adults with tuberculosis. N Engl J Med. 2011;365(16):1471-1481.
27. Zolopa A, Andersen J, Powderly W, et al. Early antiretroviral therapy reduces AIDS progression/death in individuals with acute opportunistic infections: a multicenter randomized strategy trial. PloS One. 2009;4(5):e5575.
28. Brotherton AL, Shah RB, Garland J, McCarthy ML, Gillani FS, Sanchez MC. Pharmacist-drive rapid ART reduces time to virologic suppression in Rhode Island. Poster presented at: CROI 2020; March 8–11, 2020; Virtual.
29. Horberg MA, Hurley LB, Towner WJ, et al. Determination of optimized multidisciplinary care team for maximal antiretroviral therapy adherence. J Acquir Immune Defic Syndr. 2012;60(2):183-190.
30. Dhairyawan R, Milner A, Thornhill JP, et al. Experiences of initiating rapid antiretroviral therapy among people newly diagnosed with HIV in East London: a qualitative study. Sex Transm Infect. 2023;sextrans-2022-055682.
31. Pettit AC, Pichon LC, Ahonkhai AA, et al. Comprehensive process mapping and qualitative interviews to inform implementation of rapid linkage to HIV care programs in a mid-sized urban setting in the southern United States. J Acquir Immune Defic Syndr. 2022;90(suppl 1):S56-S64.
32. Koester KA, Moran L, LeTourneau N, et al. Essential elements of and challenges to rapid ART implementation: a qualitative study of three programs in the United States. BMC Infect Dis. 2022;22(1):316.
33. Melvin SC, Gipson J. The Open Arms Healthcare Center’s integrated HIV care services model. Prev Chronic Dis. 2019;16:E135.
34. Department of Health and Human Services. Drug-Drug Interactions. https://clinicalinfo.hiv.gov/en/guidelines/hiv-clinical-guidelines-adultand-adolescent-arv/drug-interactions-overview?view=full. Accessed May 3, 2023.
35. Extended-release cabotegravir + rilpivirine. Prescribing information. https://gskpro.com/content/dam/global/hcpportal/en_US/ Prescribing_Information/Cabenuva/pdf/CABENUVA-PI-PIL-IFU2-IFU3. PDF. Accessed June 1, 2023.
36. Segal-Maurer S, DeJesus E, Stellbrink HJ, et al. Capsid inhibition with lenacapavir in multidrug-resistant HIV-1 infection. N Engl J Med. 2022;386(19):1793-1803.
37. Department of Health and Human Services. Lenacapavir Drug Information. https://clinicalinfo.hiv.gov/en/drugs/lenacapavir/ patient#:~:text=Another%20possible%20side%20effect%20of,or%20 small%20mass%20or%20lump. Accessed May 3, 2023.
38. Lenacapavir. Prescribing Information. https://www.gilead.com/-/ media/files/pdfs/medicines/hiv/sunlenca/sunlenca_pi.pdf. Accessed June 1, 2023.
39. Bares SH, Scarsi KK. A new paradigm for antiretroviral delivery: longacting cabotegravir and rilpivirine for the treatment and prevention of HIV. Curr Opin HIV AIDS. 2022;17(1):22-31.
40. Orkin C, Arasteh K, Górgolas Hernández-Mora M, et al. Long-acting cabotegravir and rilpivirine after oral induction for HIV-1 infection. N Engl J Med. 2020;382(12):1124-1135.
41. Swindells S, Andrade-Villanueva JF, Richmond GJ, et al. Long-acting cabotegravir and rilpivirine for maintenance of HIV-1 suppression. N Engl J Med. 2020;382(12):1112-1123.
42. Overton ET, Richmond G, Rizzardini G, et al. Long-acting cabotegravir and rilpivirine dosed every 2 months in adults with HIV-1 infection (ATLAS-2M), 48-week results: a randomised, multicentre, open-label, phase 3b, non-inferiority study. Lancet. 2021;396(10267):1994-2005.
43. Orkin C, Schapiro J, Perno C, et al. Expanded multivariable models to assist patient selection for long-acting cabotegravir + rilpivirine treatment: clinical utility of a combination of patient, drug concentration, and viral factors associated with virologic failure over 152 weks. Paper presented at: HIV Glasgow 2022; October 23-26, 2022; Glasgow, Scotland.
44. Orkin C, Schapiro JM, Perno CF, et al. Expanded multivariable models to assist patient selection for long-acting cabotegravir + rilpivirine treatment: clinical utility of a combination of patient, drug concentration, and viral factors associated with virologic failure. Clin Infect Dis. 2023;ciad370.
45. Cutrell AG, Schapiro JM, Perno CF, et al. Exploring predictors of HIV-1 virologic failure to long-acting cabotegravir and rilpivirine: a multivariable analysis. AIDS. 2021;35(9):1333-1342.
46. Ramgopal M, Castagna A, Cazanave C, et al. SOLAR (switch onto long-acting regimen) 12-month results–randomized switch trial of CAB + RPV LA vs. oral BIC/FTC/TAF. Paper presented at: CROI; February 19-22, 2023; Seattle, WA.
47. US Food and Drug Administration. Cabenuva. https://www. accessdata.fda.gov/drugsatfda_docs/label/2021/212888s000lbl.pdf. Accessed May 3, 2023.
48. Jucker BM, Fuchs EJ, Lee S, et al. Multiparametric magnetic resonance imaging to characterize cabotegravir long-acting formulation depot kinetics in healthy adult volunteers. Br J Clin Pharmacol. 2022;88(4):1655-1666.
49. Ford S, Crauwels H, Han K, et al. Cabotegravir and rilpivirine PK following long-acting HIV treatment discontinuation. Paper presented at: CROI; March 8-11, 2020; Boston, MA.
50. University of Liverpool. HIV Drug Interactions. https://www.hivdruginteractions.org/checker. Accessed May 5, 2023.
51. Gandhi M, Salazar J, Hickey MD, et al. High virologic suppression rates on long-acting act in a safety net clinic population. Paper presented at: CROI; February 19-22, 2023; Seattle, WA.
52. Collins LF, Corbin-Johnson D, Asrat M, et al. Early experience implementing long-acting injectable cabotegravir/rilpivirine for human immunodeficiency virus-1 treatment at a Ryan White-funded clinic in the US South. Open Forum Infect Dis. 2022;9(9):ofac455.
53. D’Amico R, Cenoz Gomis S, Moodley R, et al. Compassionate use of long-acting cabotegravir plus rilpivirine for people living with HIV-1 in need of parenteral antiretroviral therapy. HIV Med. 2023;24(2):202-211.
54. Sension MG. Real-world effectiveness of long-acting CAB + RPV in the first yr in the US in the OPERA cohort. Paper presented at: ID Week; October 19-23, 2022; Washington, DC.
55. Spivack S, Pagkalinawan S, Samuel R, Koren DE. HIV: how to manage heavily treatment-experienced patients. Drugs Context. 2022;11:2021-9-1.
56. Bajema KL, Nance RM, Delaney JAC, et al. Substantial decline in heavily treated therapy-experienced persons with HIV with limited antiretroviral treatment options. AIDS. 2020;34(14):2051-2059.
57. McFadden WM, Snyder AA, Kirby KA, et al. Rotten to the core: antivirals targeting the HIV-1 capsid core. Retrovirology. 2021;18(1):41.
58. Ogbuagu, Segal-Mauer S, Brinson C, et al. Long-acting lenacapavir in people with multidrug resistant HIV-1: week 52 results. Paper presented at: CROI; February 12-16, 2022; Virtual.
59. Gupta SK, Berhe M, Crofoot G, et al. Lenacapavir administered every 26 weeks or daily in combination with oral daily antiretroviral therapy for initial treatment of HIV: a randomised, open-label, activecontrolled, phase 2 trial. Lancet HIV. 2023;10(1):e15-e23.
60. Lencapavir. Prescribing information. https://www.accessdata.fda. gov/drugsatfda_docs/label/2022/215973s000lbl.pdf. Accessed May 3, 2023.
61. Getzen H, Beasley M, D’Mello DA. Barriers to utilizing longacting injectable antipsychotic medications. Ann Clin Psychiatry. 2014;26(1):33-38.
62. Lindenmayer JP, Glick ID, Talreja H, Underriner M. Persistent barriers to the use of long-acting injectable antipsychotics for the treatment of schizophrenia. J Clin Psychopharmacol. 2020;40(4):346-349.
63. Kaplan DA. How ‘White Bagging’ Affects Patients, Physicians, and 340B Funding. https://www.managedhealthcareexecutive.com/view/ how-white-bagging-affects-patients-physicians-and-340b-funding. Accessed May 3, 2023.
64. Czarnogorski M, Garris CP, Dalessandro M, et al. Perspectives of healthcare providers on implementation of long-acting cabotegravir plus rilpivirine in US healthcare settings from a Hybrid III Implementation-effectiveness study (CUSTOMIZE). J Int AIDS Soc. 2022;25(9):e26003.
65. Slama L, Porcher R, Linard F, et al. Injectable long acting antiretroviral for HIV treatment and prevention: perspectives of potential users. BMC Infect Dis. 2023;23(1):98.
66. Rhee SY, Sankaran K, Varghese V, et al. HIV-1 protease, reverse transcriptase, and integrase variation. J Virol. 2016;90(13):6058-6070.
67. Clutter DS, Jordan MR, Bertagnolio S, Shafer RW. HIV-1 drug resistance and resistance testing. Infect Genet Evol. 2016;46:292-307.
29
EMERGING ISSUES IN HIV MANAGEMENT: ANSWERS TO PHARMACISTS’ COMMON QUESTIONS
68. Stanford University. HIV drug resistance database. https://hivdb. stanford.edu/. Accessed May 4, 2023.
69. University of California San Francisco. National Clinician Consultation Center. https://nccc.ucsf.edu/clinician-consultation/hiv-aidsmanagement/. Accessed May 5, 2023.
70. Department of Health and Human Services. Considerations for Antiretroviral Use in Patients With Coinfections. https://clinicalinfo.hiv. gov/en/guidelines/hiv-clinical-guidelines-adult-and-adolescent-arv/ hepatitis-b-virus-hiv-coinfection?view=full. Accessed July 10, 2023.
71. Nicastri E, Sarmati L, d’Ettorre G, et al. Replication capacity, biological phenotype, and drug resistance of HIV strains isolated from patients failing antiretroviral therapy. J Med Virol. 2003;69(1):1-6.
72. Whitcomb JM, Parkin NT, Chappey C, Hellmann NS, Petropoulos CJ. Broad nucleoside reverse-transcriptase inhibitor cross-resistance in human immunodeficiency virus type 1 clinical isolates. J Infect Dis. 2003;188(7):992-1000.
73. Wensing AM, Calvez V, Ceccherini-Silberstein F, et al. 2022 update of the drug resistance mutations in HIV-1. Top Antivir Med. 2022;30(4):559-574.
74. Wolf K, Walter H, Beerenwinkel N, et al. Tenofovir resistance and resensitization. Antimicrob Agents Chemother. 2003;47(11):3478-3484.
75. Katlama C, Clotet B, Mills A, et al. Efficacy and safety of etravirine at week 96 in treatment-experienced HIV type-1-infected patients in the DUET-1 and DUET-2 trials. Antivir Ther. 2010;15(7):1045-1052.
76. Cahn P, Pozniak AL, Mingrone H, et al. Dolutegravir versus raltegravir in antiretroviral-experienced, integrase-inhibitor-naive adults with HIV: week 48 results from the randomised, double-blind, non-inferiority SAILING study. Lancet. 2013;382(9893):700-708.
77. Castagna A, Maggiolo F, Penco G, et al. Dolutegravir in antiretroviralexperienced patients with raltegravir- and/or elvitegravir-resistant HIV-1: 24-week results of the phase III VIKING-3 study. J Infect Dis. 2014;210(3):354-362.
78. Lataillade M, Lalezari JP, Kozal M, et al. Safety and efficacy of the HIV-1 attachment inhibitor prodrug fostemsavir in heavily treatmentexperienced individuals: week 96 results of the phase 3 BRIGHTE study. Lancet HIV. 2020;7(11):e740-e751.
79. Emu B, Fessel J, Schrader S, et al. Phase 3 study of ibalizumab for multidrug-resistant HIV-1. N Engl J Med. 2018;379(7):645-654.
80. Hardy WD, Gulick RM, Mayer H, et al. Two-year safety and virologic efficacy of maraviroc in treatment-experienced patients with CCR5tropic HIV-1 infection: 96-week combined analysis of MOTIVATE 1 and 2. J Acquir Immune Defic Syndr. 2010;55(5):558-564.
81. Sterman FL, Lalezari JP, Kowalczyk UM, et al. Bictegravir/ emtricitabine/tenofovir alafenamide plus doravirine in highly treatment-experienced men with multidrug-resistant HIV. AIDS. 2023;37(7):1057-1064.
82. Charpentier C, Le Hingrat Q, Ferré VM, Damond F, Descamps D. Future of antiretroviral drugs and evolution of HIV-1 drug resistance. Viruses. 2023;15(2):540.
83. Deeks SG, Hoh R, Neilands TB, et al. Interruption of treatment with individual therapeutic drug classes in adults with multidrug-resistant HIV-1 infection. J Infect Dis. 2005;192(9):1537-1544.
84. El-Sadr WM, Lundgren J, Neaton JD, et al. CD4+ countguided interruption of antiretroviral treatment. N Engl J Med. 2006;355(22):2283-2296.
85. Barbour JD, Wrin T, Grant RM, et al. Evolution of phenotypic drug susceptibility and viral replication capacity during long-term virologic failure of protease inhibitor therapy in human immunodeficiency virus-infected adults. J Virol. 2002;76(21):11104-11112.
30