Learning Objectives

• Discuss the causes and consequences of nonadvanced systemic mastocytosis (SM), focusing on potential clinical manifestations and the rationale for new targeted therapies
• Differentially diagnose SM, including indolent disease, based on symptoms and appropriate use of laboratory and genetic testing
• Describe recent clinical trial evidence and regulatory status for targeted treatment options in nonadvanced SM
• Individualize therapy for patients with nonadvanced SM to reflect clinical evidence for efficacy and safety, patient-reported outcomes, and shared clinical decision-making
SM Is a Rare Clonal MC Disorder

• SM is characterized by the abnormal expansion and accumulation of mast cells (MCs) in 1 or more organ systems1
• SM affects approximately 1 in 10,000 people1
Nonadvanced SM (~88%-95%)2-4
• Bone marrow mastocytosis (BMM)
• Indolent SM (ISM; 88% of cases)3
• Smoldering SM (SSM)
Advanced SM (~5%-12%)2-4
• SM with associated hematologic neoplasm (SM-AHN)
• Aggressive SM (ASM)
• Mast cell leukemia (MCL)
• No apparent sex or ethnic bias5
1. Brockow K. Immunol Allergy Clin North Am. 2014;34(2):283-295; 2. Cohen SS, et al. Br J Haematol. 2014;166(4):521-528; 3. Ungerstedt J, et al. Cancers (Basel). 2022;14(16):3942; 4. Mesa RA, et al. Cancer. 2022;128(20):3700-3708; 5. American Society of Clinical Oncology (ASCO). 2023. https://www.cancer.net/cancer-types/mastocytosis/statistics.
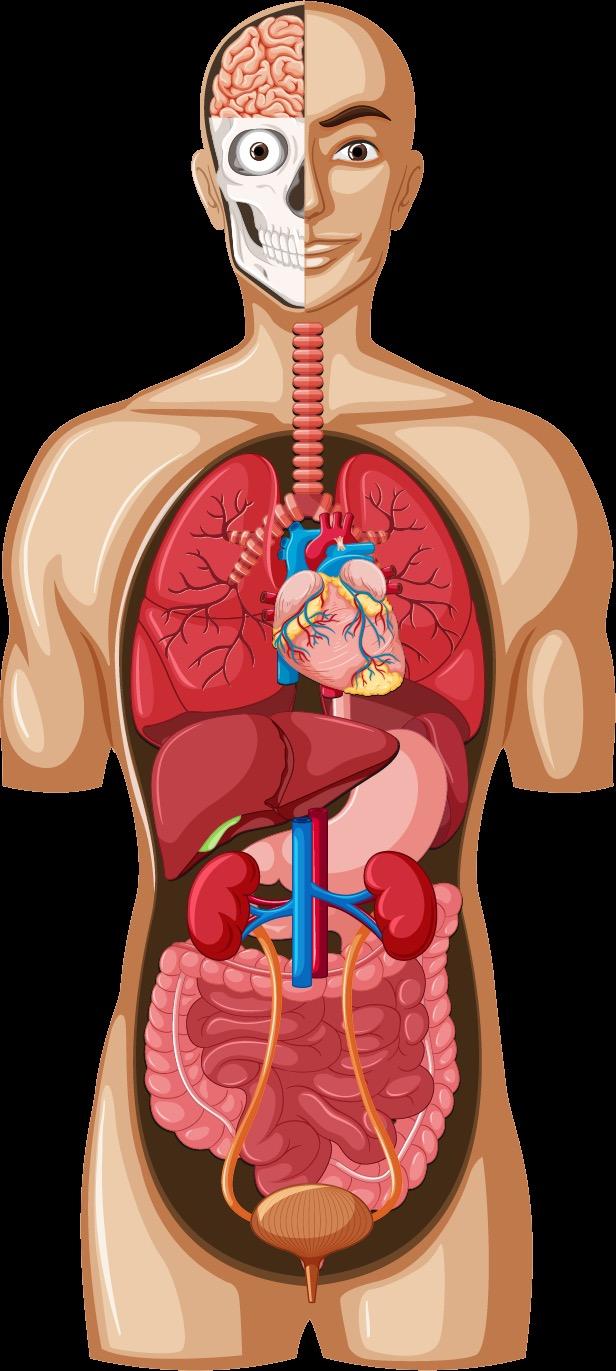
Symptoms Associated With SM

• Anxiety
• Decreased concentration and memory
• Cognitive dysfunction/brain fog
• Depression
• Headaches/Migraines
• Insomnia
• Aches
• Bone pain
• Joint pain
• Muscle pain
• Stiffness
• Angioedema
• Generalized itching
• Shortness of breath/wheezing
• Chest pain
• Abdominal pain
• Bloating
• Diarrhea
• Nausea
• Vomiting
• Bladder pain, urgency and frequency
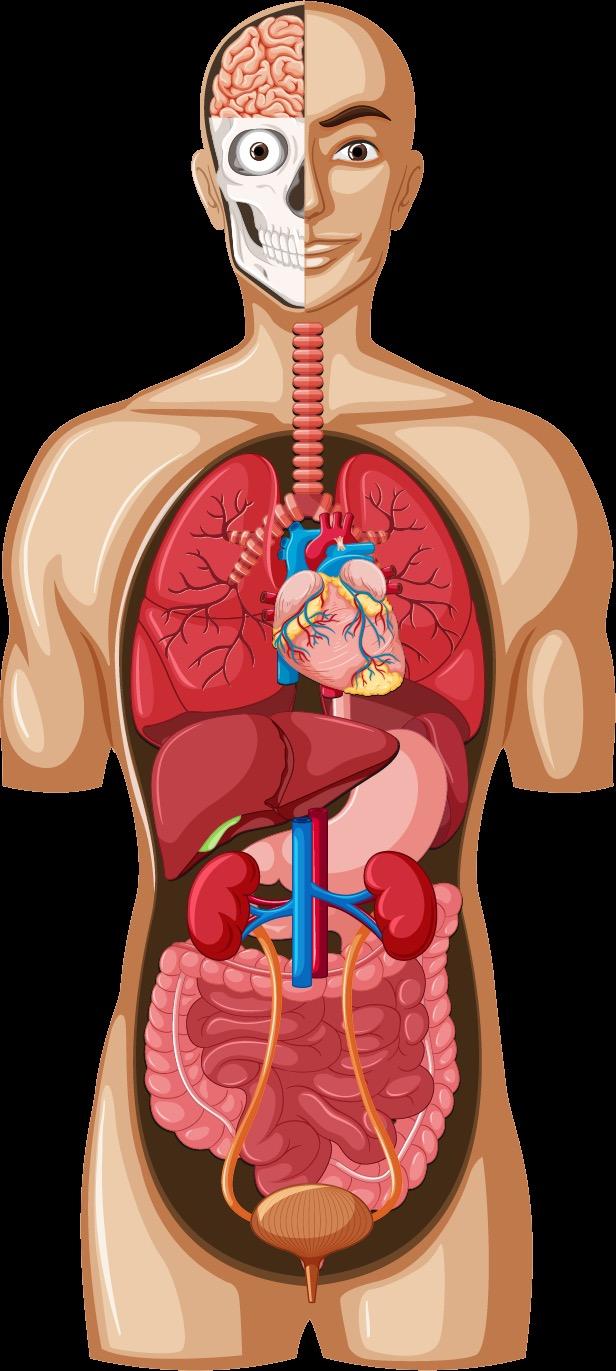
• Nasal congestion/itching
• Runny nose
• Difficulty swallowing
• Oral itching and swelling
• Flushing (of the face, neck and upper chest)
• Hypotension/Hypertension/ Blood pressure instability
• Syncope/Near syncope
• Tachycardia
• Osteopenia
• Osteoporosis
• Gastroesophageal reflux
• Hives
• Other skin rashes
• Pruritus
• Urticaria
Jennings SV, et al. Ann Allergy Asthma Immunol. 2023;127(4):407-409.
Generalized Symptoms
• Fatigue
• Malaise
• Weakness
• Weight loss
ANAPHYLAXIS
Women
• Uterine cramps and/or bleeding
Men
• Prostatitis
• Sexual dysfunction
Clinical Characteristics of Nonadvanced SM
Most Bothersome Symptoms

Patients with SM experience an average of 14 SM-related symptoms throughout the course of their disease.
N=56 patients with nonadvanced SM. Mesa RA, et al. Cancer. 2022;128(20):3691-3699. 18 16 13 11 0 2 4 6 8 10 12 14 16 18 20 Anaphylactic episodes Abdominal/Stomach pain Diarrhea/Loose stools Fatigue
Patients, %
QoL and Symptom Assessment Tools

• QoL: Mastocytosis Quality-of-Life
Questionnaire (MQLQ)1
• HRQoL: Mastocytosis Quality-of-Life
Questionnaire (MC-QoL)2
• Symptom assessment:
– Direct questions about symptom response to treatment
– Mastocytosis Symptom Assessment Form (MSAF)1
– Mastocytosis Activity Score (MAS)3
– ISM Symptom Assessment Form (ISM-SAF)4
• Validated tool used in clinical trials
ISM-SAF4
ISM Symptom Scoring
Abdominal pain
Diarrheaa Nausea Spots
Itching
Flushing
Brain fog
Headache
Dizziness
Bone pain
Fatigue
Symptoms scored daily over a 24-hour recall period
0 = no symptom
10 = worst imaginable symptom
TSS (0-110)
≥28 indicates moderate to severe symptoms
HRQoL, health-related quality of life; QoL, quality of life.
aDiarrhea frequency is scored separately but contributes to total score.
1. National Comprehensive Cancer Network (NCCN). Systemic Mastocytosis 1.2024. 2023. https://www.nccn.org/professionals/physician_gls/pdf/mastocytosis.pdf; 2. Siebenhaar F, et al. Allergy. 2016;71(6):869-877; 3. Siebenhaar F, et al. Allergy. 2018;73(7):1489-1496; 4. Taylor F, et al. Orphanet J Rare Dis. 2021;16(1):414.
Triggers
Venoms
Food
Drugs
Infection
Temperature
Stress
Allergens
Fatigue
Physical triggers
Surgery
Procedures
Vaccinations
Known Triggers for MC Activation Events
Examples
Bee, wasp, mixed vespids, fire ants
Alcohol consumption
Opioids, NSAIDs, some antibiotics (eg, vancomycin), contrast dyes
Viral, bacterial, or fungal
Heat, cold, sudden changes in temperature
Emotional, physical, pain
Pollen, pet dander, dust mites
Lack of sleep/sleep deprivation
Mechanical irritation, friction, vibration, exercise
Anesthesia (eg, atracurium)
Colonoscopy, endoscopy, interventional radiology

NSAID, nonsteroidal anti-inflammatory drug.
NCCN. Systemic Mastocytosis 1.2024. 2023. https://www.nccn.org/professionals/physician_gls/pdf/mastocytosis.pdf.
Mechanical

Pharmacologic
Temperature Changes
• Medications (eg, atracurium, mivacurium, nefopam)
• Hypothermia
• Hyperthermia
Main Corresponding Symptoms
Patients With SM Require Perioperative Management to Manage Triggers 1 1. Dewachter P, et al. Anesthesiology. 2014;20:753-759; 2. Pardanani A. Am J Hematol. 2021;96(4):508-525; 3. The Mast Cell Disease Society, Inc (TMS). https://tmsforacure.org/wp-content/uploads/2023/03/TMS_FullPatient-Guide_r6.pdf. Consult with anesthesia and surgical teams, review prior anesthetic records, use “safer” agents (eg, fentanyl, tramadol, ketamine, propofol).2,3
Triggers
Perioperative
Examples
• Tourniquet use
• Mild trauma to the skin • Surgery Skin: pruritis, flushing, erythema, urticaria
Cardiovascular signs: tachycardia, hypotension
Diagnostic Algorithm for SM1

• Suspected MCA-associated symptoms
OR
• Anaphylaxis
AND/OR
• Increased serum tryptase level
OR
• Biopsy-proven adult-onset mastocytosis in the skin (MIS)

• Evaluation for SM
– BM biopsy or biopsy of organ with suspected extracutaneous involvement
– High-sensitivity molecular testing for KIT D816V; if needed, additional KIT gene sequencing
– MC immunophenotyping using flow cytometry and/or immunohistochemistry
– Screen for FIP1L1-PDGFRA if eosinophilia is present and KIT D816V is negative
Serum tryptase should be measured between 30 minutes and 2 hours after the start of an anaphylactic event, with a baseline level obtained many days later.2

1. NCCN. Systemic Mastocytosis 1.2024. 2023. https://www.nccn.org/professionals/physician_gls/pdf/mastocytosis.pdf; 2. American Academy of Allergy
& Immunology (AAAAI). https://www.aaaai.org/conditions-treatments/related-conditions/mcas.
FIP1L1-PDGFRA, factor interacting with PAPOLA and cleavage and polyadenylation specificity factor (CPSF1) platelet derived growth factor receptor ; MCA, mast cell activation
Asthma
Variable
1

The REMA Score
BST, basal serum tryptase; REMA, [Spanish Network on Mastocytosis].
aFor tryptase values ranging from 15 to 25 ng/mL, proceed with BM evaluation when REMA score ≥1.

≥2 is considered to be associated with high probability of SM2
1. Alvarez-Twose I, et al. Int Arch Allergy Immunol. 2012;157:275-280; 2. Zanotti R, et al. Mediterr J Hematol Infect Dis. 2021;13(1):e2021068. Score Sex Men +1 Women -1
Absence of urticaria, pruritis, and angioedema +1 Urticaria, pruritis, and/or angioedema -2 Presyncope and/or syncope +3 BSTa <15 ng/mL -2 >25 ng/mL +2
Clinical Symptoms
Decision to Perform BM Biopsy in an Adult With Suspected SM
YES

Does the patient have skin lesions consistent with MPCM/UP? NO

Perform
• Serum tryptase
• CBC/Diff
• High-sensitivity assay for KIT D816V mutational analysis on PB (if available)
Does the patient experience presyncope, syncope, signs of recurrent mediatorrelated symptoms, anaphylaxis, unexplained osteoporosis?

YES
NO

Perform BM biopsy



Is tryptase >20 ng/mL?


Perform high-sensitivity assay for KIT D816V mutational analysis on PB (if available)

SM not likely YES NO


Mutation not detected or not available
Mutation detected
BM biopsy may be needed in the future; continue to monitor patient
Perform BM biopsy
CBC/Diff, complete blood count and differential; MPCM/UP, maculopapular cutaneous mastocytosis/urticaria pigmentosa; PB, peripheral blood. Figure adapted from Zanotti R, et al. J Clin Med. 2021;10(7):1420.

Considerations When Ordering a BM Biopsy
• NGS panel – other myeloid gene mutations
•
Lab capable of/experienced in:
– MC flow cytometry
– MC staining panel
– Tryptase, CD25, CD117, CD30 (if CD25 negative)
Dr Tracy George, personal communication.

Differential Diagnosis HαT
• Autosomal dominant condition1
• ~6% of general population, accounting for 90% of cases with elevated BST levels1
• Due to duplications of TPSAB1 (encodes alpha-tryptase), which increases BST levels (>8 ng/mL)2,3
– ~9- to 10-ng/mL increase in tryptase for every extra copy of TPSAB11
– Symptoms consistent with MCA4
• KIT
D816V–negative, no evidence of MC aggregates or markers of MCA in BM biopsy4
– Patients often do not have elevated MC urinary metabolites as seen with SM
• Significant association with greater risk of severe anaphylaxis and elevated serum tryptase level in patients with mastocytosis5
– Presence of HαT is elevated in all subtypes of SM, including advanced SM6
– 17% to 18% of patients with SM7
1. Glover SC, et al. Ann Allergy Asthma Immunol. 2021;127:638-647; 2. Lyons JJ, et al. Nat Genet. 2016;48(12):1564-1569; 3. Lyons JJ. Immunol Allergy Clin North Am. 2018;38(3):483-495; 4. Giannetti MP, et al. J Allergy Clin Immunol. 2022;150(5):1225-1227; 5. Picard M, et al. Clin Ther. 2013;35(5):548-562; 6. Polivka L, et al. J Allergy Clin Immunol. 2024;153(1):349-353; 7. Li JY, et al. Cancers (Basel). 2023;15(23):5626.
Diagnosing HαT

• Expected level of tryptase can be calculated via
1
• If copy number is:
– Compatible with expected tryptase level, HαT confirmed
– Not compatible with expected tryptase level, determine KIT D816V status and consider hematologic workup
Beyens M, et al. Diagnostics. 2023;13:3662.
BST
+ extra copy numbers of TPSAB1 Total Rise In Peripheral Tryptase After Systemic Event (TRIPTASE) Calculator
https://triptase-calculator.niaid.nih.gov/

Differential Diagnoses
Other Conditions to Consider
• Cardiovascular1-3: coronary hypersensitivity,a labile hypertension, orthostatic hypotension, paroxysmal arrhythmias
• Digestive1-3: adverse food reaction,a celiac disease, GERD, gluten enteropathy, IBS
• Endocrinologic1-3: carcinoid syndrome, insulinoma, parathyroid/thyroid carcinoma, pheochromocytoma, thyrotoxicosis
• Immunologic1-3: autoinflammatory disorders,a familial hyper-IgE syndrome, vasculitisa
• Neurologic1-3: anxiety, chronic fatigue syndrome, depression, fibromyalgia, headaches/migraines, hyperventilation, multiple sclerosis, panic attacks, postural orthostatic tachycardia syndrome, seizure disorder, somatization disorder, stroke
• Skina,1-3: angioedema, atopic dermatitis, chronic urticaria
• MMAS4:
– KIT D816V present
– Symptoms consistent with MCA and evidence of clonal population
GERD, gastroesophageal reflux disease; IBS, irritable bowel syndrome; MMAS, monoclonal mast cell activation syndrome.
aLocalized MCA can occur.
1. Scherber RM, Borate U. Br J Haematol. 2018;180(1):11-23; 2. Theoharides TC, et al. N Engl J Med. 2015;373(2):163-172; 3. Castells M, Butterfield J. J Allergy Clin Immunol Pract. 2019;7(4):1097-1106; 4. Picard M, et al. Clin Ther. 2013;35(5):548-562; 5. Dranitsaris G, et al. Blood. 2023;142:3800.
Potential Predictors of Poor Prognosis in SM1,2
• Disease subtype
• Aged >60 years
• Hemoglobin <10 g/dL
• Platelets <100/150 × 109/La
• BST level
• Higher allele burden (VAF) of KIT D816V in PB

Nonadvanced SM Subtype
Risk of Progression BMM
Very Low ISM Low SSM Intermediate
• Elevated serum alkaline phosphatase (≥100 U/L)
• Other genetic mutations (eg, SRSF2/ASXL1/RUNX1, EZH2, ASKL1/CBL)
• Splenomegaly
aDependent on whether the WHO mutation-adjusted risk score (MARS) for advanced SM or Mayo Alliance Prognostic System (MAPS) for mastocytosis is used. 1. NCCN. Systemic Mastocytosis 1.2024. 2023. https://www.nccn.org/professionals/physician_gls/pdf/mastocytosis.pdf; 2. Valent P, et al. J Allergy Clin Immunol Pract. 2022;10(8):1999-2012.
Life Expectancy Is Equivalent in Patients With ISM vs Control Population
Mayo Clinic1,a 1976-2007

UP, urticaria pigmentosa; US, United States.
Denmark2,b 1997-2010
Denmark general population
SM (subtype unknown)
SM with associated clonal disease
ISM (including UP)
Aggressive SM
Years From Diagnosis
aN=342 patients with SM aged ≥18 years, median follow-up 1.7 years, retrospective cohort; bN=548 patients with SM aged ≥15 years, median follow-up 6.1 years, retrospective cohort.
1. Lim K , et al. Blood. 2009;113(23): 5727-5736; 2. Cohen SS, et al. Br J Haematol. 2014;166(4):521-528.
From Diagnosis Survival, % 0 10 20 ISM, (n=159) MCL, (n=4) 100 80 60 40 0 20 ASM, (n=41) AHN, (n=138) Expected age/ sex-matched US survival
Years
Survival, % 0 2 4
1.0 0.8 0.6 0.4 0 0.2
MCL
6 8 10 12 14 16

Treatment Considerations for Nonadvanced SM
Counsel patient and monitor for signs and symptoms of disease, including QoL
• H&P, CBC/Diff, CMP
• DEXA scan
• Total IgE and insect venom IgE panel

• Rescue and prevention plans for anaphylaxis
• Assess symptom burden
Observation or clinical trial

Asymptomatic Symptomatic

Treat MCA symptoms with antimediator drug therapy
Restage in case of no adequate response or progression

Refer to
Continue treatment if adequate response without progression
Mastocytosis 1.2024. 2023. https://www.nccn.org/professionals/physician_gls/pdf/mastocytosis.pdf.

specialized
expertise
SM.
center with
in
CMP, complete metabolic profile; DEXA, dual-energy X-ray absorptiometry; H&P, history and physical. aShould not be used in patients with platelets <50 × 109/L.. NCCN. Systemic
Symptom-Directed Treatment
Strategies1,2
Organ Involvement/Symptom
Skin: pruritus, flushing, urticaria, angioedema dermatographism
First Line

Gastrointestinal: abdominal pain, cramping, diarrhea, heartburn, nausea, vomiting
Neurologic: headache, cognitive impairment (eg, brain fog, poor concentration and memory), depression
Hypotensive Episodes/Anaphylaxis
Osteopenia/Osteoporosis
H1 R antagonist and H2 R antagonist
H2 R antagonist
H1 R and H2 R antagonist
Epinephrine IM (acutely), supine positioning
Supplemental calcium and vitamin D, bisphosphonate; bone mineral density assessment
Treatment
2. Leukotriene receptor antagonist
3. Aspirin
4. Ketotifen
5. Cromolyn sodium ointment
2. Cromolyn sodium
3. Proton pump inhibitor
4. Leukotriene receptor antagonist
5. Ketotifen
2. Cromolyn sodium
3. Aspirin
4. Ketotifen
Prevention: VIT, Rush desensitization, omalizumab
Denosumab, interferon-α inhibitor, cytoreductive agent; vertebroplasty/kyphoplasty
1. NCCN. Systemic Mastocytosis 1.2024. 2023. https://www.nccn.org/professionals/physician_gls/pdf/mastocytosis.pdf; 2. Pardanani A. Am J Hematol. 2023;98:1097-1116; 3. Mesa RA, et al. Cancer. 2022;128(20):3691-3699.
H1R, histamine H1 receptor; H2R, histamine H2 receptor; IM, intramuscular; VIT, venom immunotherapy.
than one-half of patients take ≥3 prescription medications and ≥3 OTC medications. 3
More
Treatment of Mediator-Induced Symptoms Related to MC Activation
Additional Considerations Indication(s)
Insect VIT

Omalizumaba
Epinephrine and other emergency drugs used for anaphylaxis
Honeybee, yellow jacket, wasp, or fire ant venom allergy
Avapritinib
Multiresistant MCA symptoms, therapy-refractory MCAS, confirmed IgE-dependent allergy in high-risk patients (prophylaxis)
Anaphylaxis (MCA event)
Adults with ISM
Clinical Trial Selective KIT inhibitor
FDA, US Food and Drug Administration.
aOmalizumab is not FDA approved for SM or recurrent anaphylaxis. Omalizumab is FDA approved to treat moderate to severe persistent allergic asthma, nasal polyps in adults, and chronic urticaria. Adapted from Valent P, et al. J Allergy Clin Immunol Pract. 2022;10(8):1999-2012.
Tyrosine Kinase Inhibitors1

• 3 categories of KIT inhibitors:
1. Inhibit only wild-type (WT) or non-codon D816V mutations: imatinib (also inhibits ABL, FLT3, PDGFRA, PDGFRB, CSFR1)
2. Inhibit both WT and D816V: midostaurina
3. Selective inhibition: avapritinib,b elenestinib, bezuclastinib
• There can be overlap in inhibition (eg, avapritinib inhibits KIT and PDGFRA mutants) 2

Preliminary reports suggest TKIs are effective in reducing or preventing anaphylaxis.
aNot indicated for nonadvanced disease and utility limited by gastrointestinal toxicity; bAvapritinib is the only TKI currently FDA approved to treat ISM. 1. Akin C. Immunol Allergy Clin North Am. 2023;43:743-750; 2. Trullas-Jimeno
ESMO Open. 2021;6(3):100159.
ABL,
Abelson murine leukemia viral oncogene homolog 1; FLT3, FMS-like tyrosine kinase 3; PDGFRB, platelet-derived growth factor receptor
β;
CSFR1, colony-stimulating factor 1 receptor.
A, et al.

Considerations for the Use of
Targeted Therapies
• Currently, targeted therapies are available only through specialty pharmacies1
• There is a risk of bleeding and thromboembolism associated with TKIs
– Risk varies depending on the therapy
• A subset of patients with ISM (with other non-KIT mutations) show faster progression and would benefit more from earlier treatment with targeted therapy3




1. Blueprint Medicines. https://www.ayvakithcp.com/AYVAKIT_Product_Pricing_Sheet_HCP.pdf; 2. Deb S, et al. Cancer Med. 2020;9(1):313-323; 3. Muñoz-González JI, et al. Blood. 2019;134(5):456-468.
Omalizumab Use in Nonadvanced SM

• Anti-IgE monoclonal antibody approved to treat chronic spontaneous urticaria, chronic rhinosinusitis with nasal polyps, and moderate to severe persistent asthma1
• Effective on all vasomotor symptoms, including those secondary to anaphylaxis, and gastrointestinal and urinary symptoms2
• Safety and efficacy study of omalizumab in SM (2018)3:
– Demonstrated significant reduction in symptoms and patient-reported QoL:
• 38.5% complete symptom control
• 23% major response, 23% partial response
– Most effective for recurrent anaphylaxis and skin symptoms, less for GI, musculoskeletal, and neuropsychiatric
– No significant changes in tryptase levels or KIT D816V VAF
– No SAEs
SAE, serious adverse event.
aN=14 adult patients with SM who received omalizumab for a median duration of 17 months. 1. FDA. 2023. https://www.accessdata.fda.gov/drugsatfda_docs/label/2023/103976s5242lbl.pdf; 2. Buonomo A, et al. Mediterr J Hematol Infect Dis. 2022;14(1):e2022040; 3. Broesby-Olsen S, et al. Allergy. 2018;73(1):230-238.
Avapritinib Met Primary Endpoint in Patients With ISM Phase 2 PIONEER Trial
Avapritinib Targets the KIT
Receptor on the MC1,2 Avapritinib Significantly
Improved TSS Score3

MRGPRX2

aP=0.003.
















C3a, C5a KIT IgE


















Avapritinib
Avapritinib1







BSC, best supportive care; C, complement; TSS, total symptom score. N=212 adults with confirmed ISM with inadequately controlled symptoms (TSS ≥28) despite receiving BSC with ≥2 antimediator drugs were randomly assigned 2:1 to receive 25 mg avapritinib orally daily + BSC (n=141) or placebo + BSC (n=71) for 24 weeks. Patients could then continue to an open-label extension in which they received 25 mg avapritinib orally daily for up to 5 years.
1. Figure adapted from Castells M, Akin C. Nat Med. 2021;27(12):2081-2082; 2. Nicolosi M, et al. Medicina (Kaunas). 2021;57(11):1135; 3. Gotlib J, et al. NEJM Evid. 2023;2(6):EVIDoa2200339.
TSS Score Change -9.2 -15.6a -18 -16 -14 -12 -10 -8 -6 -4 -2 0
Placebo
IgG Tryptase Histamine

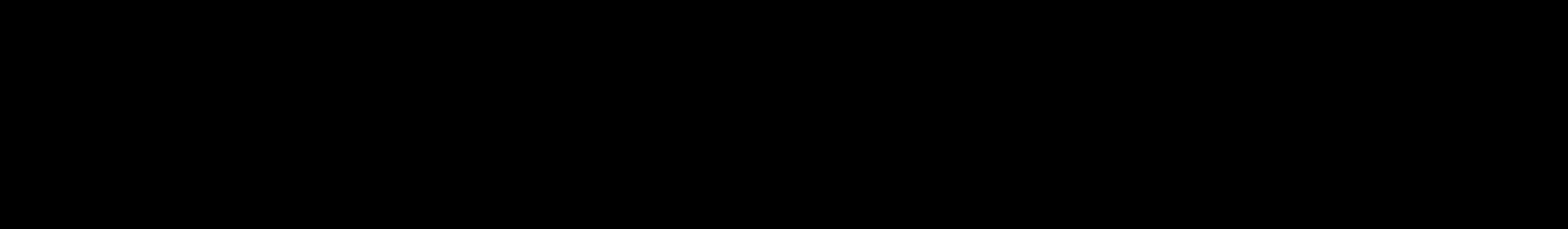
Avapritinib Met Key Secondary Endpoints in Patients With ISM Phase 2 PIONEER Trial
Avapritinib Significantly Improved Clinical Markers and Symptoms
Avapritinib Improved on a 30% Reduction in Symptoms vs Placebo


aP<0.001; bP=0.005; cP=0.009.
N=212 adults with confirmed ISM with inadequately controlled symptoms (TSS ≥28) despite receiving BSC with ≥2 antimediator drugs were randomly assigned 2:1 to receive 25 mg avapritinib orally daily + BSC (n=141) or placebo + BSC (n=71) for 24 weeks. Patients could then continue to an open-label extension in which they received 25 mg avapritinib orally daily for up to 5 years. Gotlib J, et al. NEJM Evid. 2023;2(6):EVIDoa2200339.
Patients Achieving ≥50% Reduction, % 0 23 6 10 54 53 68 25 0 10 20 30 40 50 60 70 80 Serum tryptase BM MC aggregates KIT D816 VAF Reduction in TSS score Placebo Avapritinib KIT a b a 30 45 0 10 20 30 40 50 60 70 80 Reduction in TSS score Patients Achieving ≥30% Reduction, % a c
Avapritinib Treatment for ISM
• Avapritinib was approved by the FDA for use in adult patients with ISM in May 2023
– Not recommended for patients with platelet count <50 × 109/L
• 25 mg orally once daily on an empty stomach
– (ASM: 200mg orally once daily)
• Avoid coadministration with strong and moderate CYP3A inhibitors and inducers
• AEs: peripheral and periorbital edema, dizziness, flushing, photosensitivity
• To date, increased bleeding has not been reported in patients with ISM who are taking avapritinib
– Ensure patient does not have a history of intracranial hemorrhage before prescribing
• Monitoring: lab monitoring (CMP, CBC/Diff) and visit at 3 and 6 months after starting medication, then every 6 months
AE, adverse event; CYP, cytochrome P450. Drugs@FDA. https://www.accessdata.fda.gov/drugsatfda_docs/label/2023/212608s013lbl.pdf.



Lirentelimab

Siglec-8


MRGPRX2

Investigational Agents in Nonadvanced SM
MC1,2
Investigational Therapies




IgG




C3a, C5a KIT IgE







Tryptase








Therapeutic Target Investigational Agent Phase of Development
Bezuclastinib
Elenestinib

Bezuclastinib2,3 Phase 2 (Summit)




Masitinib

KIT

Elenestinib3 Phase 2/3 (HARBOR)


Histamine




IL-6

Sarilumab
Masitinib2 Phase 3
IL-6 Receptor Sarilumab2 Phase 2
Siglec-8 Lirentelimab4 Phase 1
IL-6, interleukin 6; siglec-8, sialic acid-binding immunoglobulin-like lectin-8.
1. Figure adapted from Castells M, Akin C. Nat Med. 2021;27(12):2081-2082; 2. Nicolosi M, et al. Medicina (Kaunas). 2021;57(11):1135; 3. Akin C, et al. Blood. 2022;140(suppl 1):6838-6839; 4. Siebenhaar F, et al. Br J Dermatol. 2023;189(5):511-519.

Elenestinib
Phase 2/3 HARBOR Trial Part 1 (ISM)
• Does not penetrate CNS
• Selectively inhibits KIT D816V while preferentially sparing WT KIT
• Primary endpoints: safety, PK, PD
– Well tolerated at all dose levels for median 35 weeks
– No treatment-related SAEs or AEs that led to drug discontinuation
• All AEs grade 3 or less
• Part 2 (initiation anticipated 2024)
Significant Dose-Dependent Improvements After 12 Weeks of Elenestinib
Secondary Endpoints
CNS, central nervous system; PD, pharmacodynamics; PK, pharmacokinetics.
aN=39 adult patients with ISM per WHO criteria with moderate to severe symptoms (ISM-SAF TSS ≥28), who were randomly assigned to receive BSC + oral elenestinib 25mg (n=10), 50mg (n=10), 100 mg (n=9) or BSC + placebo (n=10) once daily. N=86 additional open-label PK cohorts enrolled in parallel; bISM-SAF results are from the blinded portion of part 1.
Tashi T, et al. Blood. 2023;142(suppl 1):76.
Mean % Change From Baselinea Tryptase Level KIT D816V VAF BM MCs ISM-SAF TSSb 25 mg -15.4 -37.5 -22.6 -28.5 50 mg -50.9 -70.4 -28.1 -31.8 100mg -68.4 -77 -57.9 -33.6 Placebo +3.3 -2.5 -20.0 -22.2
Bezuclastinib
Summit Phase 2 (ISM and SSM) Part 1a Topline Results
• Minimal CNS penetration1
• High selectivity: does not inhibit PDGFRA, PDGFRB, FLT3, CSFR12
• Primary endpoints: safety, PK, MC biomarkers, symptom improvement at 12 weeks1
– No treatment-related SAEs; majority of TEAEs in patients on 100 to 200 mg once daily were low grade and reversible
– No bleeding

•
Part 2: 24-week treatment (open)
100% of treated patients achieved ≥50% reduction in serum tryptase, KIT D816V VAF, BM MC burden within 12 weeks. 1
TEAE, treatment-emergent adverse event.
N=54 adult patients with ISM or SSM per 2016 WHO criteria with moderate to severe symptoms (on ≥2 antimediator therapies), who were randomly assigned 1:1:1 to BSC + placebo or BSC + oral bezuclastinib once daily: part 1A, n=20, 100 mg, 200 mg; part 1B, n=34, 100 mg, 150 mg for 12 weeks, followed by open-label extension (N=18).
1. Bose P, et al. Blood. 2023;142(suppl 1):77; 2. Akin C. Immunol Allergy Clin North Am. 2023;43:743-750.

Suboptimal Identification and Delayed Diagnoses Increase
Overall Patient Burden
• Delayed diagnosis due to the rarity of SM and the broad spectrum of signs and symptoms that are shared by other, more-common disorders1,2
– Puts patients at risk of life-threatening anaphylaxis, organ dysfunction, and severe osteoporosis
• Prior to diagnosis, patients had seen an average of 6 HCPs3


The median time from symptom onset to diagnosis of nonadvanced SM is 9 years.3


1. Ungerstedt J, et al. Cancers (Basel). 2022;14(16)3942; 2. Mikkelsen CS, et al. Dermatol Reports. 2014;6(1):5199; 3. Mesa RA, et al. Cancer. 2022;128(20):3691-3699.

Nonadvanced SM Has Significant Impacts on Daily Life and Employment

Were you limited in pursuing your hobbies or other leisure time activities?
Has your physical condition or medical treatment interfered with your family life? 63%
Has your physical condition or medical treatment interfered with your social activities?
aN=88 patients with ISM and 13 patients with SSM completed this survey thinking about their symptoms and disease over the prior week; bN=56 patients with nonadvanced SM. 1. Jennings SV, et al. Immunol Allergy Clin North Am. 2018;38(3):505-525; 2. Mesa RA, et al. Cancer. 2022;128(20):3691-3699.
SM-related employment changes2,b:
• 54% have reduced work hours
• 27% voluntarily quit
• 16% were terminated
30 50 31 58 35 58 48 58 22 8 32 8 25 8 22 8 0 10 20 30 40 50 60 70 80 ISM SSM ISM SSM ISM SSM ISM SSM Quite a bit Very much 52% 58% 66% 60% 66% 70% 66%
Patients, % 1,a
Were you limited in doing either your work or other daily activities?
Multidisciplinary Management of Nonadvanced SM
• The presence of multisystemic symptom manifestations requires multidisciplinary collaboration between:
– Allergy/Immunology
– Dermatology
– Gastroenterology
– Hematology/Oncology
– Primary care
– Rheumatology
– Endocrinology
– Psychiatry

Zanotti R, et al. Cancers (Basel). 2021;13(24):6380; Valent P, et al. Int J Mol Sci. 2019;20(12):2976.

Routine Monitoring

• Patients with stable SSMa should be monitored every 6 months and those with stable ISMa every 12 months, for changes in:
– Serum tryptase level
– CBC/Diff
– CMP
– Weight
– Physical examination, including skin/lesions
• Regression of MPCM lesions does not correlate with changes in underlying ISM
– QoL/Symptom burden: ability to participate in daily activities, ability to eat, respiratory symptoms under control, sleep
• Use MSAF or MQLQ
• DEXA scan every 1 to 3 years for patients with osteopenia/osteoporosis
If laboratory results or symptoms change, therapeutic adjustment should be considered.
aPatients with unstable SSM or ISM should be seen more frequently until stabilized.
Brockow K, et al. Arch Dermatol. 2002;138(6):785-790; NCCN. Systemic Mastocytosis 1.2024. 2023. https://www.nccn.org/professionals/physician_gls/pdf/mastocytosis.pdf.



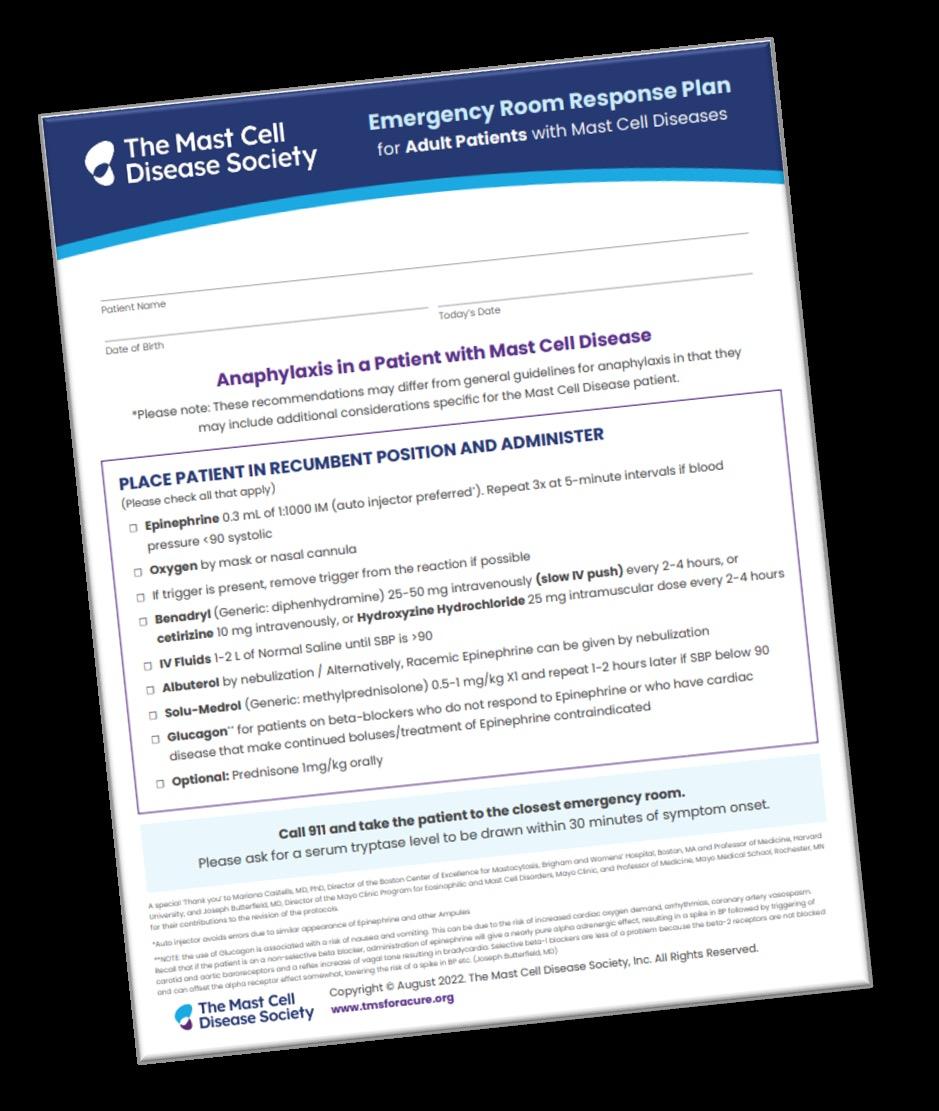
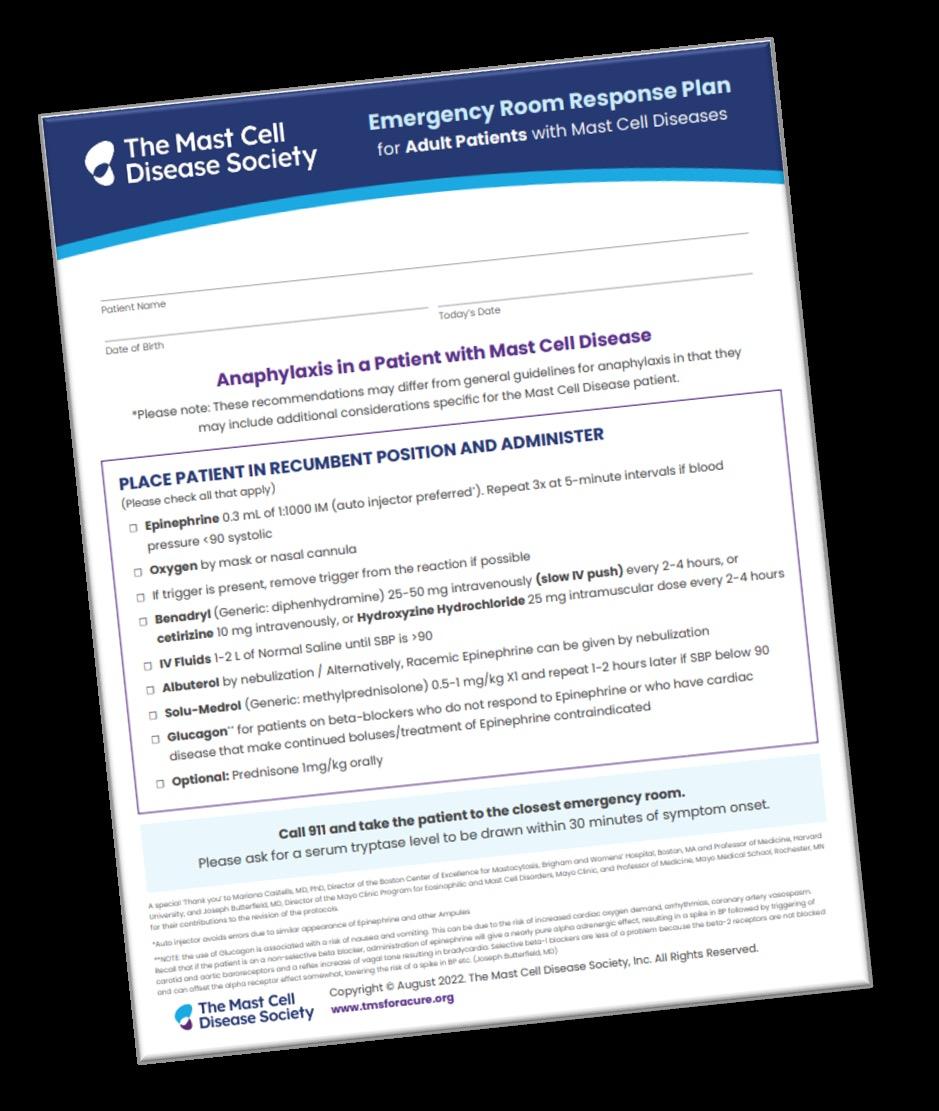
Anaphylaxis Management Is Critical to Successful Management1 • All patients with SM should be trained in supine positioning • All patients with SM should be advised to carry 1 or 2 epinephrine auto-injectors to manage anaphylaxis • Consider adding omalizumaba to treatment plan aOmalizumab is not FDA approved for SM or recurrent anaphylaxis. 1. Jendoubi F, et al. Clin Exp Allergy. 2020;50(6):654-661; 2. Valent P, et al. J Allergy Clin Immunol Pract. 2022;10(8):1999-2012. Classification Risk of Anaphylaxis2 BMM High ISM Intermediate SSM Intermediate Visit Our Clinical Resource Center at www.ExchangeCME.com/SMJeopardyResources.
Venom-Induced Anaphylaxis

• Severe venom anaphylaxis is more prevalent in men, and is highly associated with HαT1,2
• Based on clinical history, patients with SM should be assessed for venom allergy with skin and/or in vitro venom-specific IgE tests
– If positive, treat with VIT indefinitely2
• Omalizumab may be considered if patient does not tolerate VIT3,a
– VIT benefits outweigh the risks in patients with SM4
aOmalizumab is not FDA-approved for SM or recurrent anaphylaxis.
1. Rueff F, et al. Allergol Select. 2017;1(1):53-58; 2. O’Connell MP, Lyons JJ. Curr Opin Allergy Clin Immunol. 2020;20(5):431-437; 2. Niedoszytko M, et al. Allergy. 2009;64(9):1237-1245; 3. Ricciardi L. Int J Immunopathol Pharmacol. 2016;29(4):726-728; 4. Jarkvist J, et al. Allergy. 2020;75(1):169-177.
Patient Education Is Critical to
Successful Management
• Trigger avoidance:
– Identifying potential triggers
– Unpredictability of response
• Periprocedural precautions
• Anaphylaxis action plan
• Emergency department response plan
• Medication adherence
• Support groups
TMS. https://tmsforacure.org/.


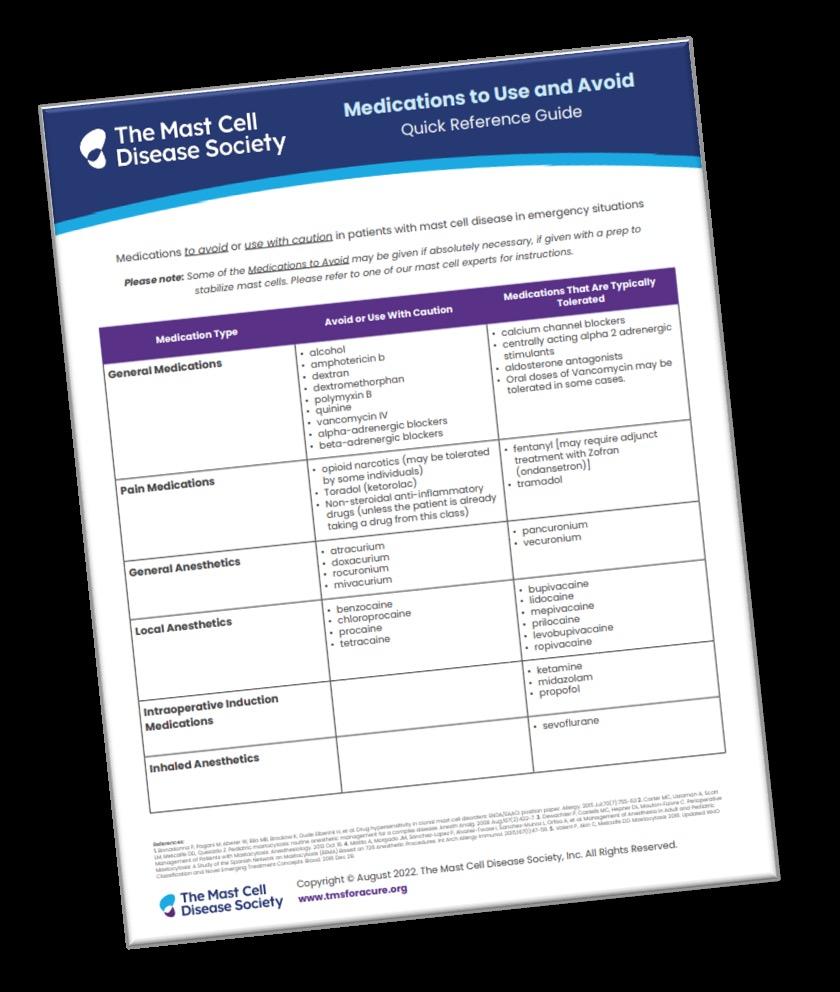
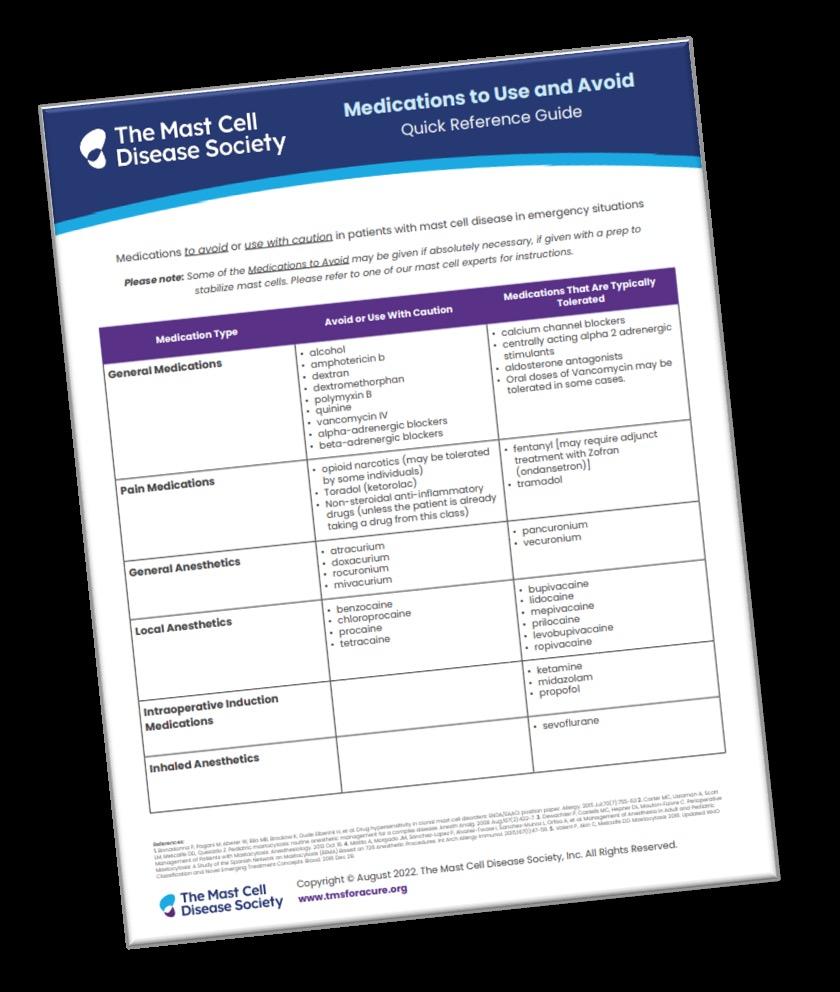
Medication Type
Medication Considerations in Patients With SM
Avoid or Use With Caution
• Alcohol
• Amphotericin B
General Medications

Pain Medications
• Dextran
• Dextromethorphan
• Polymyxin B
• Opioid narcotics (may be tolerated by some individuals)
• Ketorolac
• Atracurium
General Anesthetics
Local Anesthetics
Intraoperative Induction Medications
• Doxacurium
• Benzocaine
• Chloroprocaine
• Quinine
• Vancomycin IV
• Alpha-adrenergic blockers
• Beta-adrenergic blockers
Medications That Are Typically Tolerated
• Calcium channel blockers
• Centrally acting alpha-2 adrenergic stimulants
• Aldosterone antagonists
• NSAIDs (unless the patient is already taking a drug from this class)
• Fentanyl (may require adjunctive treatment with ondansetron)
• Tramadol
• Rocuronium
• Mivacurium
• Procaine
• Tetracaine
• Pancuronium
• Vecuronium
• Bupivacaine
• Lidocaine
• Levobupivacaine
• Ketamine
• Midazolam
• Propofol
• Mepivacaine
• Prilocaine
• Ropivacaine
Inhaled Anesthetics
TMS. https://tmsforacure.org/wp-content/uploads/2023/03/TMS_Full-Patient-Guide_r6.pdf.
• Sevoflurane
Patient Resources and Action Plans








Systemic Mastocytosis, 2022
TMS provides multifaceted support to patients, families, and medical professionals through education, advocacy, and collaboration.
GARD helps patients find information, services, experts, financial aid, and support groups.
NORD is a patient advocacy organization committed to the identification, treatment, and cure of rare disorders through programs of education, advocacy, research, and patient services.
ECNM is a group dedicated to improving diseaserecognition, diagnosis, and therapy in patients with mastocytosis in Europe.

NCCN Guidelines for Patients®
Visit Our Clinical Resource Center at www.ExchangeCme.com/SMJeopardyResources.
Summary

• Nonadvanced SM has a complex pathophysiology and clinical presentation, necessitating multidisciplinary management
• High-sensitivity assays (ddPCR, ASOqPCR) are the most reliable for KIT D816V analysis, especially with a low VAF
• Traditional management of nonadvanced SM is largely preventive and symptom directed
• Avapritinib is FDA approved specifically to target the pathophysiology of ISM
– Other selective TKIs are under investigation and may soon provide additional therapeutic options
• Patient education (triggers, anaphylaxis, and ED action plans) are essential to minimizing the significant negative impact SM has on QoL and activities of daily living
ED, emergency department.