Learning Objectives

• Discuss SM pathophysiology, including implications for potential clinical presentations and new targeted therapies
• Evaluate patients with nonadvanced SM to characterize symptoms, disease burdens, and results from ancillary testing
• Discuss recent clinical trial evidence for new targeted treatment options in nonadvanced SM
• Individualize ongoing therapeutic regimens for nonadvanced SM based on symptomatology, patient-reported outcomes, and shared clinical decision making
SM, systemic mastocytosis.
DIAGNOSING NONADVANCED SM
 Patricia Lugar, MD, MS
Patricia Lugar, MD, MS
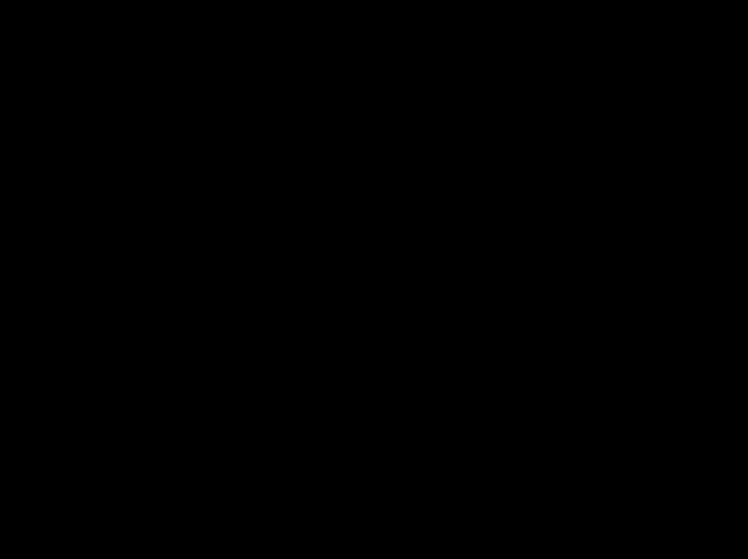
Clinical Characteristics of Nonadvanced SM

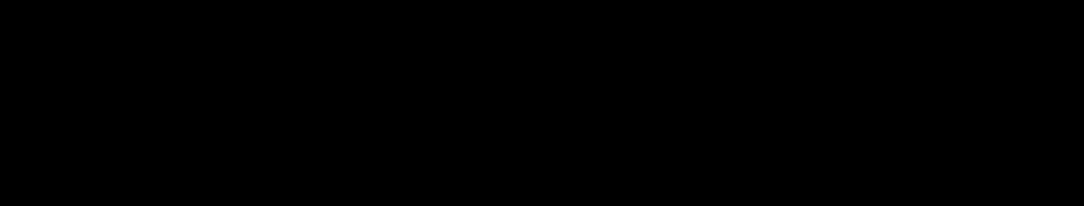
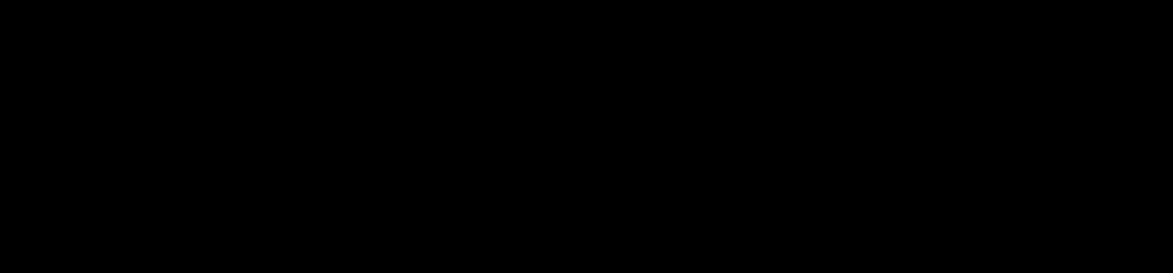
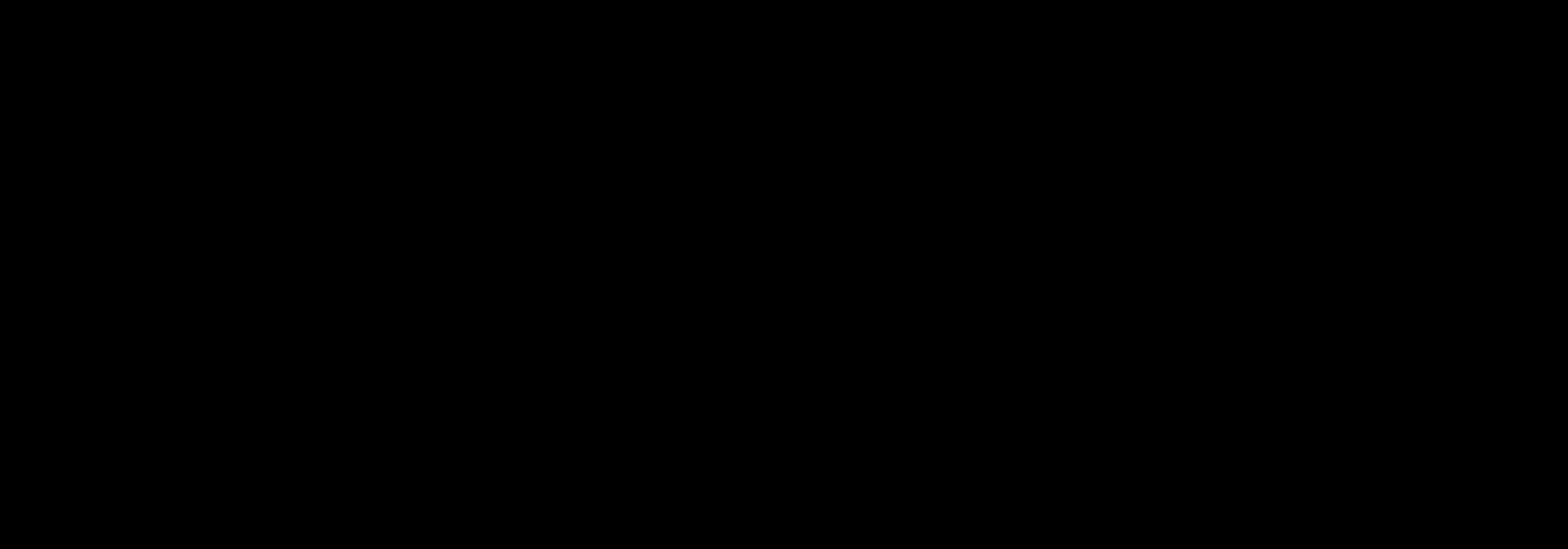
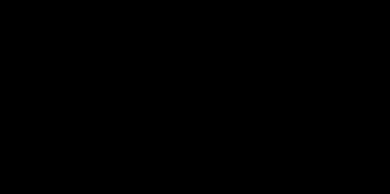
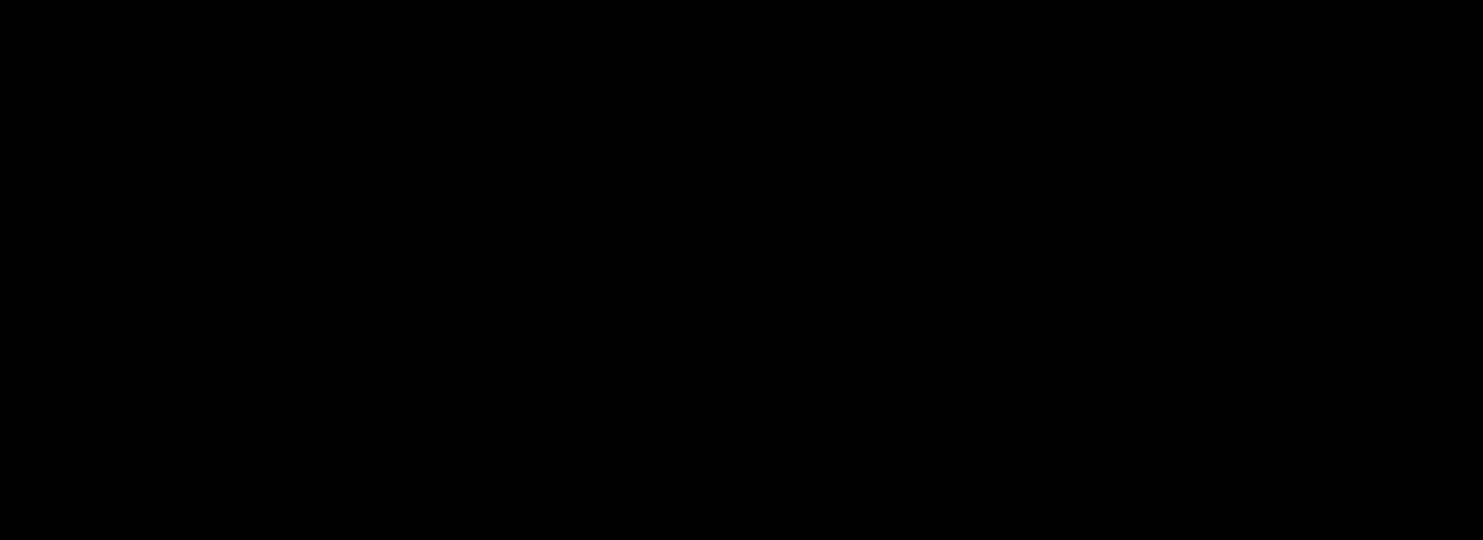
Patients, %
BMM, bone marrow mastocytosis; GI, gastrointestinal; ISM, Indolent SM; MC, mast cell(s); MPCM, maculopapular cutaneous mastoc ytosis; SSM, smoldering SM. Pardanani A, et al. Blood. 2010;115(1):150-151.
% Patient-Reported Signs and Symptoms by SM Subtype
0 0 0 14 78 19 86 72 72 55 68 41 45 18 23 50 77 64 64 10 11 13 15 21 36 67 69 78 85 0 10 20 30 40 50 60 70 80 90 100 Hepatomegaly Splenomegaly Lymphadenopathy Constitutional symptoms Idiopathic/recurrent anaphylaxis Musculoskeletal symptoms
MC mediator-related symptoms GI symptoms Cutaneous symptoms Urticaria pigmentosa/MPCM ISM (n=101) SSM (n=22) BMM (n=36)
Other
Clinical Characteristics of Nonadvanced SM
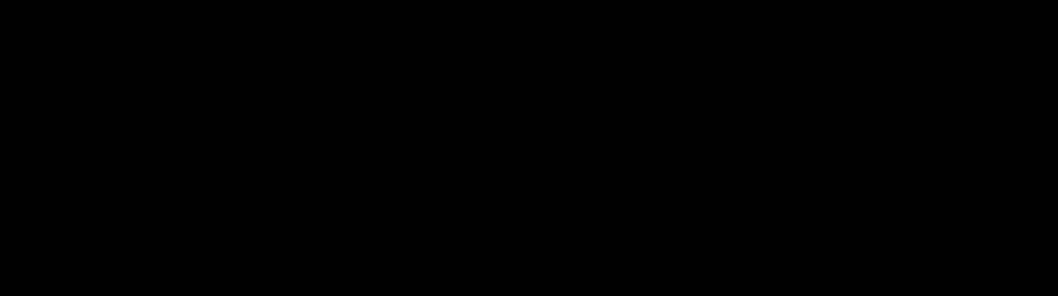
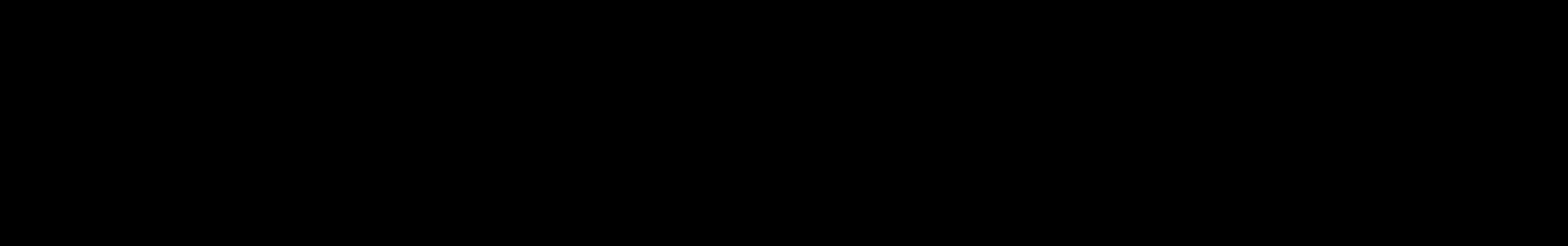
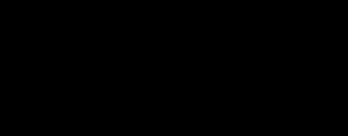
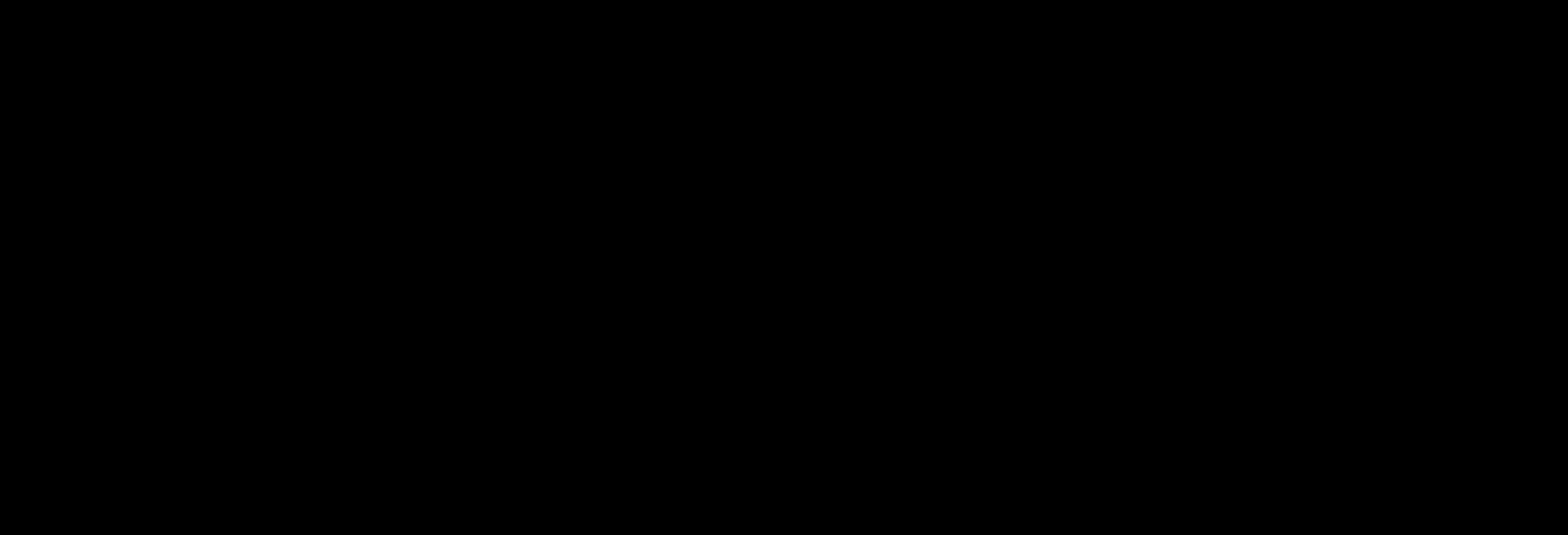
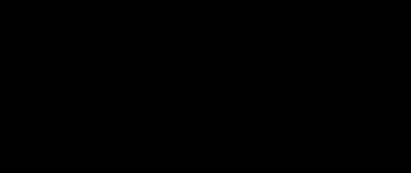
Most Bothersome Symptoms
Anaphylactic episodes

Abdominal/ stomach pain
Diarrhea/ loose stools
Fatigue
Patients can experience up to 14 different symptoms during the course of their illness.
Mesa RA, et al. Cancer. 2022;128(20):3691-3699.

18% 16% 13% 11% 0% 2% 4% 6% 8% 10% 12% 14% 16% 18% 20%
Patients, %
Diagnostic Algorithm for SM1
• Suspected MC activation-associated symptoms
OR
• Anaphylaxis
AND/OR
• Increased serum tryptase level (no mastocytosis in the skin, B- or Cfindings, or abnormal blood counts)
OR • Biopsy-proven adult onset mastocytosis in the skin
• Evaluation for SM

– BM biopsy or biopsy of organ with suspected extracutaneous involvement
– High sensitivity molecular testing for KIT D816V; if needed, additional KIT gene sequencing
– MC immunophenotyping using flow cytometry and/or immunohistochemistry
– Screen for FIP1L1-PDGFRA if eosinophilia is present and KIT D816V is negative
BM, bone marrow; FIP1L1-PDGFRA, factor interacting with PAPOLA and CPSF1-platelet derived growth factor receptor α.
1. National Comprehensive Cancer Network (NCCN). https://www.nccn.org/professionals/physician_gls/pdf/mastocytosis.pdf. Accessed December 19, 2022.
• CBC/Diff
• Serum tryptase
• CMP
SM Testing Standard of Care
• Blood smear
• BM aspirate smear
• BM biopsy
Laboratory Morphology
• FISH FIPIL1-PDGFRA, if eosinophilia present

• HαT
• High-sensitivity mutation analysis (ddPCR, ASO-qPCR) or qPCR for KIT D816V
• Myeloid gene panel (NGS)

Phenotype Genetics
• Flow cytometry (CD2, CD25, CD34, CD117, CD30 [optional])
• Immunohistochemistry (tryptase, CD25, CD117, CD30 [optional])
ASO-qPCR, allele-specific oligonucleotide-quantitative PCR, CBC/Diff, complete blood count with differential; CMP, comprehensive metabolic panel; ddPCR, droplet digital PCR; FISH, fluorescence in situ hybridization; HαT, hereditary α tryptasemia; NGS, next-generation sequencing; PCR, polymerase chain reaction; qPCR, quantitative PCR. Adapted from NCCN Guidelines. Systemic Mastocytosis Version 2.2022. https://www.nccn.org/professionals/physician_gls/pdf/mast ocytosis.pdf. Accessed January 3, 2023.
Differential Diagnoses
• Hereditary α Tryptasemia (HαT)
– Due to multiplication of TPSAB1 which increases basal serum tryptase levels (>8 ng/mL)1,2

– Symptoms consistent with MC activation, including abdominal pain and bloating, anaphylaxis, brain fog, flushing, urticaria3
– KIT D816V negative, no evidence of MC aggregates or markers of MC activation in bone marrow biopsy3
– Patients do not have elevated MC urinary metabolites as seen with SM3
• Other Conditions to Consider4-6
– Cardiovascular: Coronary hypersensitivitya, labile hypertension, orthostatic hypotension, paroxysmal arrhythmias
– Digestive: Adverse food reactiona, celiac disease, gastroesophageal reflux disease, gluten enteropathy, IBS
– Endocrinological: Fibromyalgia, carcinoid syndrome, insulinoma, parathyroid/thyroid carcinoma, pheochromocytoma, thyroxicosis
– Immunological: Autoinflammatory disordersa, familial hyper-IgE syndrome, vasculitisa
– Neurological: Anxiety, chronic fatigue syndrome, depression, headaches/migraines, hyperventilation, multiple sclerosis, panic attacks, postural orthostatic tachycardia syndrome, seizure disorder, somatization disorder, stroke
– Skina: Angioedema, atopic dermatitis, chronic urticaria, scleroderma
aLocalized MC activation can occur. IBS, irritable bowel syndrome; IgE, immunoglobulin E. 1. Lyons JJ, et al. Nat Genet. 2016;48(12):1564–1569; 2. Lyons JJ. Immunol Allergy Clin North Am. 2018;38(3):483-495; 3. Giannetti MP, et al. J Allergy Clin Immunol. 2022;150(5):12251227; 4. Scherber RM,
2019;7(4):1097-1106.
Borate U. Br J Haematol. 2018;180(1):11-23; 5. Theoharides TC, et al. N Engl J Med. 2015;373(2):163-172; 6. Castells M, Butterfield J. J Allergy Clin Immunol Pract.
Decision to Perform BM Biopsy in an Adult With Suspected SM
Perform
• Serum tryptase













• CBC/Diff
• High-sensitivity assay for KIT D816V mutational analysis on peripheral blood (if available)
YES Does the patient have skin lesions consistent with MPCM/UP? NO YES
Does the patient experience presyncope, syncope, signs of recurrent mediatorrelated symptoms, anaphylaxis, unexplained osteoporosis?
Perform high-sensitivity assay for D816V KIT mutational analysis on peripheral blood (if available)
BM biopsy may be needed in the future. Continue to monitor patient.
MPCM/UP, maculopapular cutaneous mastocytosis/urticaria pigmentosa. Figure adapted from Zanotti R, et al. J Clin Med. 2021;10(7):1420.
Perform BM biopsy NO Is tryptase >20 ng/mL? SM not likely YES NO
Perform BM biopsy Mutation not detected or not available Mutation detected
BMM
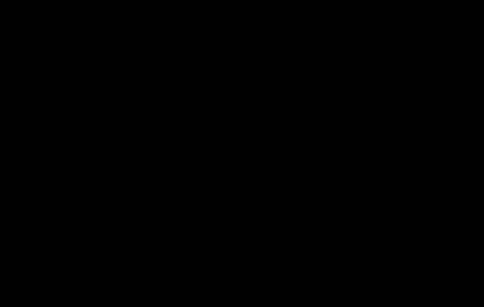
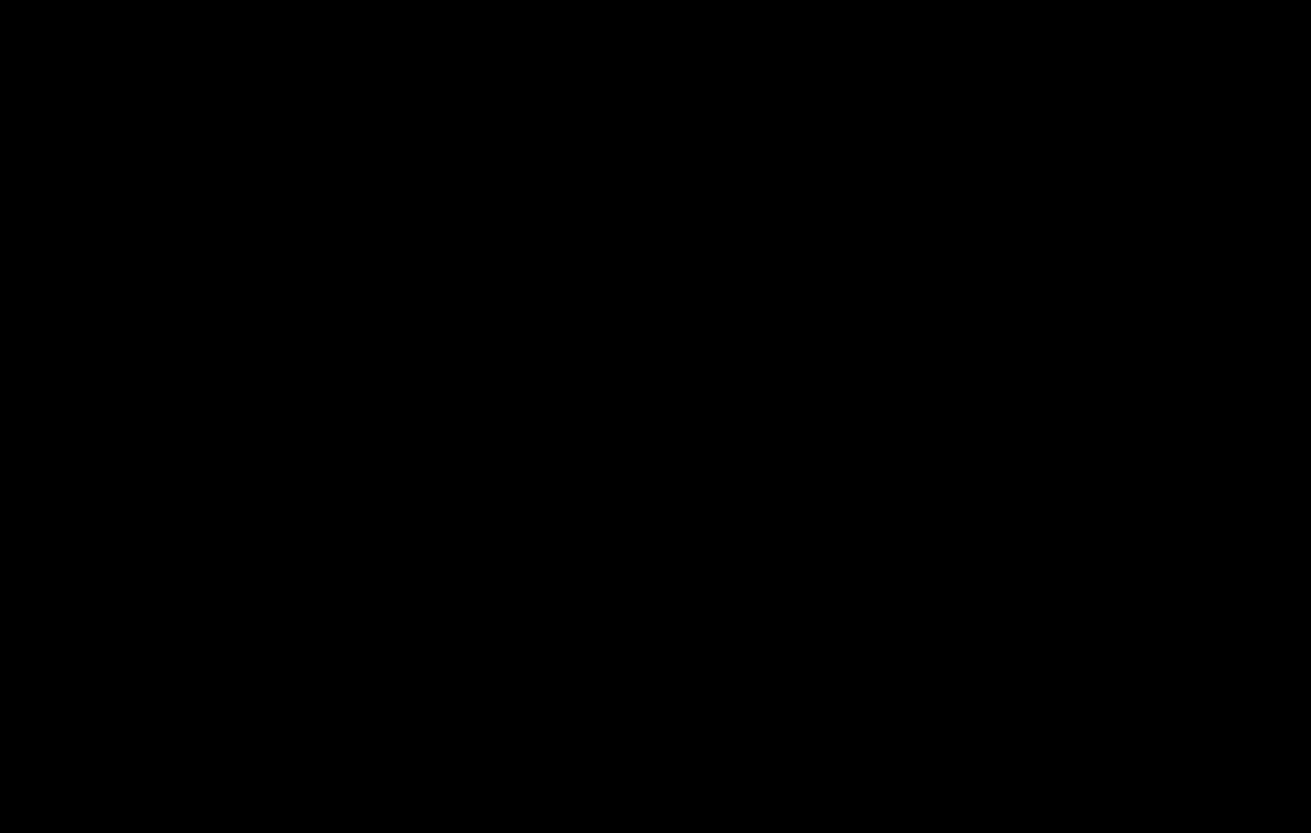
Classifying Subtypes of SM 2022 WHO Criteria

No additional findings
• Absence of skin lesions
• Serum tryptase <125 ng/mL
ISM
No additional findings
≥2 B-findings
• Biopsy BM MC ≥30% or serum tryptase >200 ng/mL
SM diagnostic criteria met
≥20% mast cells on BM aspirate smear
MCLa
SSM ASM
• KIT D816V with VAF >10% in BM cells or peripheral blood leukocytes
• BM hypercellularity or dysmyelopoiesis
• Organomegaly (without organ impairments)
≥1 C-finding
• Cytopenias present (ANC <1.0x109/L, hemoglobin <10 g/dL, or platelets <100x109/L)
• Hepatomegaly with portal hypertension/ascites
• Splenomegaly with hypersplenism
• Osteolysis that may be associated with osteoporosis and pathologic fractures
• Malabsorption with weight loss
aB- and C-findings possible.
WHO criteria for associated hematologic neoplasm met
SM-AHNa













• SM-acute myeloid leukemia
• SM-myelodysplastic syndrome
• SM-myeloproliferative neoplasm
• SM-chronic myelomonocytic leukemia
ANC, absolute neutrophil count; ASM, aggressive SM; BMM, bone marrow mastocytosis; ISM, Indolent SM; MC, mast cell(s); MCL, m ast cell leukemia; MPCM, maculopapular cutaneous mastocytosis; SSM, smoldering SM; SM-AHN, systemic mastocytosis with associated hematologic neoplasm; VAF, variant allele fraction; WHO, World Health Organization.
Figure adapted from Mannelli F. Ann Hematol. 2021;100(2):337-344; Khoury JD, et al. Leukeumia. 2022;36(7):1703-1719; Zanotti R, et al. Leukemia. 2022;36(2):516-524.
+
Potential Predictors
of Poor Prognosis in SM
• Disease subtype1
• Number and severity of cytopenia(s)1
• Basal serum tryptase level1
• Higher allele burden (VAF) of KIT D816V in peripheral blood1
• >60 years of age2
• Elevated serum alkaline phosphatase (>100 U/L)2
• Other genetic mutations are associated with progression to advanced SM3
–
Epigenetic regulators: ASXL1, DNMT3, EZH2, TET2
–
Transcription factors: RUNX1

–
Signaling molecules: CBL, JAK2, KRAS, NRAS
– Splicing factors: SRSF2, SF3B1, U2AF1
ASXL1, ASXL transcriptional regulator 1; DNMT3A, DNA methyltransferase 3α; EZH2, enhancer of zeste 2 polycomb repressive complex 2 subunit; TET2, tet methylcytosine dioxygenase 2; RUNX1, RUNX family transcription factor 1 ; CBL, Cbl proto-oncogene; JAK2, Janus kinase 2; KRAS, KRAS proto-oncogene, GTPase; NRAS, NRAS proto-oncogene, GTPase; SRSF2, serine and arginine rich splicing factor 2; SF3B1, splicing factor 3b subunit 1; U2AF1, U2 small nuclear RNA auxiliary factor 1. 1. Valent P, et al. J Allergy Clin Immunol Pract. 2022;10(8):1999-2012; 2. Reiter A, et al. Blood. 2020;135(16):1365-1376; 3. Monaldi C, et al. Mediterr J Hematol Infect Dis. 2021;13:e2021046.
Nonadvanced SM Subtype Risk of Progression1 BMM Very Low ISM Low SSM Intermediate
Diagnosing Nonadvanced SM Clinical Pearls
þ Familiarize yourself with typical and atypical clinical presentations of SM
þ Conduct a thorough physical exam, including the skin, when there is a high suspicion of index for SM

þ Determine baseline serum tryptase levels è KIT D816V mutation analysis è BM biopsy to confirm SM







QoL Assessment Tools for Nonadvanced SM
HRQoL, health-related quality of life; QoL, quality of life.
1. Van Anrooij B, et al. Allergy. 2016;71(11):1585-1593;

2021;16(1):414.
2. Siebenhaar F, et al. Allergy. 2016;71(6):869-877;
2018;73(7):1489-1496;
• QoL: Mastocytosis Quality-of-Life Questionnaire (MQLQ)1 • HRQoL: Mastocytosis Quality of Life Questionnaire (MC-QoL)2 • Symptom Assessment – Mastocytosis Symptom Assessment Form (MSAF)1 – Mastocytosis Activity Score (MAS)3 – ISM Symptom Assessment Form (ISM-SAF)4
3. Siebenhaar F, et al. Allergy.
4. Taylor F, et al. Orphanet J Rare Dis.
TREATMENT STRATEGIES FOR NONADVANCED SM

 Anne Maitland, MD, PhD
Anne Maitland, MD, PhD
Treatment Considerations for Nonadvanced SM
Counsel patient and monitor for signs and symptoms of disease:

• CBC/Diff, CMP, KIT D816V
• Bone DEXA
• Total IgE and insect venom IgE panel
• Rescue and prevention plans for anaphylaxis
Counsel patient and monitor response vs progression
Restage in case of no adequate response or progression






Continue treatment if adequate response without progression

Referral to specialized center with expertise in SM.
DEXA, dual-energy X-ray absorptiometry; MCA, mast cell activation. Adapted from NCCN Guidelines. Systemic Mastocytosis Version 2.2022. https://www.nccn.org/professionals/physician_gls/pdf/mast ocytosis.pdf. Accessed January 3, 2023. Asymptomatic Symptomatic Observation Treat MCA symptoms with anti-MC/anti-MC mediator drug therapy or clinical trial
Symptom-Directed Treatment Strategies
Symptom
Pruritus, flushing
First Line
Additional Options

H1R antagonist
Abdominal pain, cramping, diarrhea, heartburn, nausea, vomiting
Headache, cognitive impairment, depression
H2R antagonist
H2R antagonist, LT/PG inhibitors, PUVA, omalizumab, cromolyn ointment
Proton pump inhibitor, cromolyn, ondansetron/olanzapine
H1R and H2R antagonist
Tricyclic agents, cromolyn
Hypotensive episodes
Epinephrine IM (acutely), supine positioning
Chronic H1R and H2R antagonists, LT/PG inhibitors, CS-A, omalizumab, MC cytoreductive agents
Osteoporosis
Bisphosphonate
Denosumab, interferon-α inhibitor, cytoreductive agent
Cromolyn, cromolyn sodium; CS -A, cyclosporin A; IM, intramuscular; LT/PG, leukotriene/prostaglandin; PUVA, psolaren plus ultravi olet A. Scherber RM, Borate U. Br
Haematol. 2018;180(1):11-23; Courtesy of Lawrence Schwartz, MD, PhD.
J
Stepwise Approach to Treat Mediator-Induced Symptoms Related to MC Activation
Basic Management Indication(s)
• Avoidance of any triggers
• Basic therapy with histamine receptor blockade (H1 and H2 receptor blockade)
Additional therapies and measures
• Add a proton pump inhibitor to H2 receptor blocker
• Add cromolyn sodium
• Referral to allergy/immunology specialist; add ketotifen, aspirin, or a leukotriene receptor antagonist (eg, montelukast, zafirlukast)
• Add corticosteroids

Additional specific therapies
• Insect venom immunotherapy
• Omalizumaba therapy
• Epinephrine and other emergency drugs used in anaphylaxis
• Midostaurin or avapritinib
Prophylaxis against MC activation events, including anaphylaxis
Prophylaxis against anaphylaxis, mediator-related symptoms
Gastrointestinal symptoms not controlled by H2 receptor blocker
Refractory skin or gastrointestinal symptoms
Refractory flushing, tachycardia, hypotension, or bone pain
Refractory allergic symptoms, anaphylaxis, MCAS
Honeybee, yellow jacket, wasp, or fire ant venom allergy
Multiresistant MC activation symptoms, therapy-refractory MCAS, confirmed IgE-dependent allergy in high-risk patients (prophylaxis)
Anaphylaxis (MC activation event)
MCAS in patients with advanced or refractory nonadvanced SM (reducing target cells and releasability)
aOmalizumab is not FDA-approved for SM or recurrent anaphylaxis. Omalizumab is FDA-approved to treat moderate-to-severe persistent allergic asthma, nasal polyps in adults, and chronic urticaria.
FDA, US Food and Drug Administration; LTE4, leukotriene E4; MCAS, MC activation syndrome; PGF2, prostaglandin F2. Valent P, et al. J Allergy Clin Immunol Pract. 2022;10(8):1999-2012
Other Management Strategies
Reduce
osteoporosis/osteopenia
Bone mineral density assessment; calcium & vitamin D supplementation, bisphosphonates, denosumab, interferon-α, vertebroplasty/kyphoplasty
Perioperative management
Consult with anesthesia and surgical teams, review prior anesthetic records, use “safer” agents
Clinical Trial
Selective mutant KIT inhibitor (eg, avapritinib)
Pardanani A. Am J Hematol. 2021;96(4):508-525.

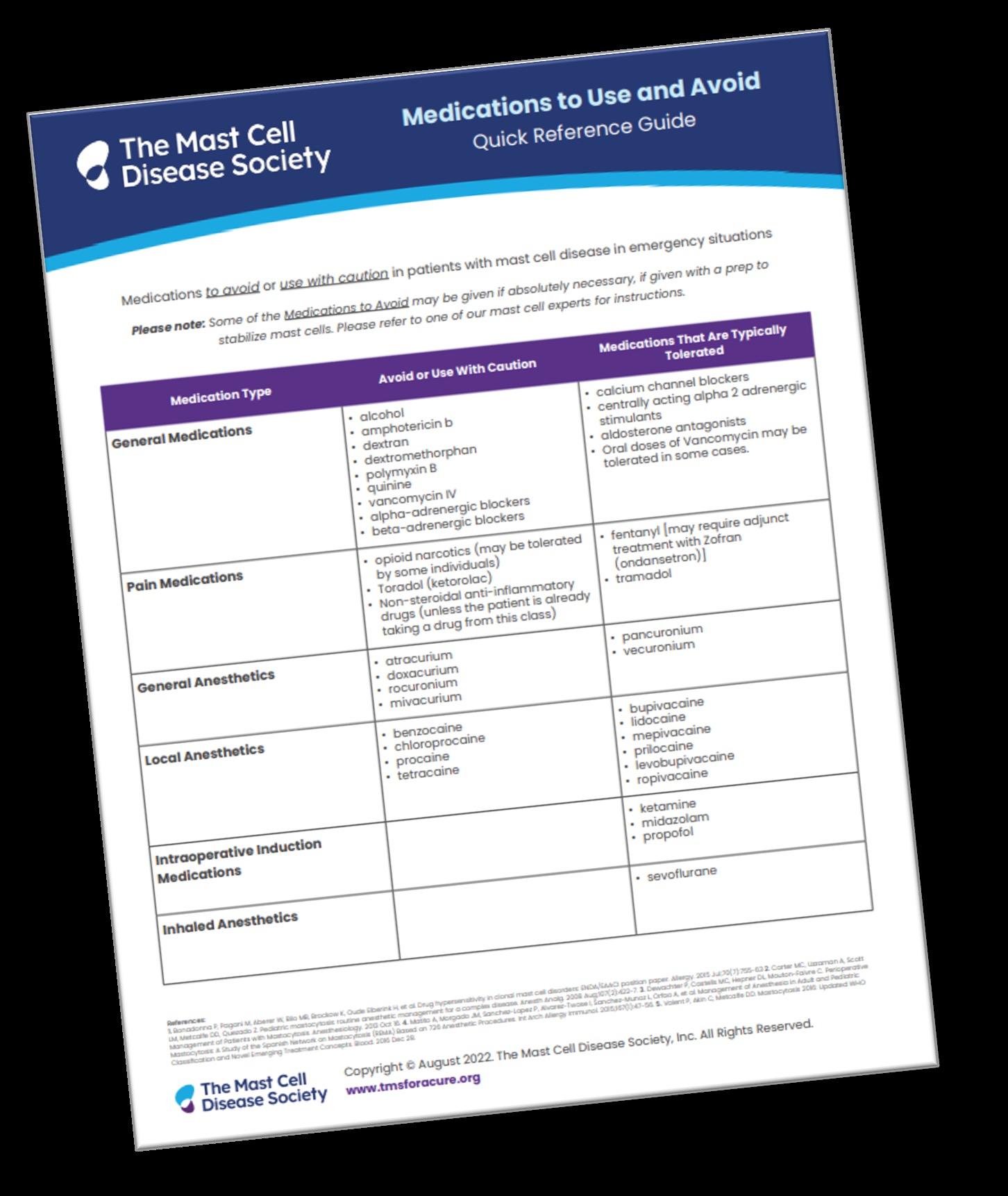
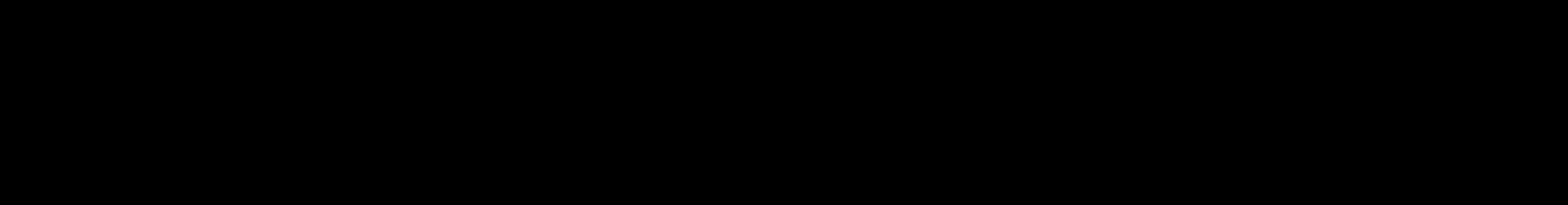
Medications to Be Avoided
Medication Type
General Medications
Avoid or Use With Caution
• Alcohol
• Amphotericin b
• Dextran
• Dextromethorphan
• Polymyxin B
Pain Medications
• Opioid narcotics (may be tolerated by some individuals)
• Ketorolac
General Anesthetics
• Atracurium
• Doxacurium
Local Anesthetics
• Benzocaine
• Chloroprocaine
Intraoperative Induction Medications
Inhaled Anesthetics
Medications That Are Typically Tolerated
• Quinine
• Vancomycin IV

• Alpha-adrenergic blockers
• Beta-adrenergic blockers
• Nonsteroidal anti-inflammatory drugs (unless the patient is already taking a drug from this class)
• Rocuronium
• Mivacurium
• Procaine
• Tetracaine
• Calcium channel blockers
• Centrally acting alpha 2 adrenergic stimulants
• Aldosterone antagonists
• Oral doses of vancomycin
• Fentanyl (may require adjunct treatment with ondansetron)
• Tramadol
• Pancuronium
• Vecuronium
• Bupivacaine
• Lidocaine
• Levobupivacaine
• Ketamine
• Midazolam
• Propofol
• Sevoflurane
• Mepivacaine
• Prilocaine
• Ropivacaine
https://tmsforacure.org/wp-content/uploads/TMS_Full-Patient-Guide_2022.pdf Accessed January 18, 2023.
IV, intravenous. The Mast Cell Disease Society (TMS). 2022.
Overcoming the Challenges Associated With Treating Nonadvanced SM


• Currently approved nonadvanced SM treatments do not include KIT mutation-directed therapy

ISM/SSM patients with higher risk of progression and/or with symptoms refractory to current treatments have limited options unless they develop C-findings
• However, promising targeted therapies are on the horizon
•
Therapeutic Targets and Investigational
Cell1,2

Cytokines
IgE and IgG, immunoglobulins; IL-6, interleukin 6; PDGFRα, platelet-derived growth factor receptor alpha; SCF, stem cell factor.

1. Figure adapted from Castells M, Akin C. Nat Med. 2021;27(12):2081-2082;
2. Nicolosi M, et al. Medicina (Kaunas). 2021;57(11):1135;
3. Akin C, et al. 64th Annual ASH Conference 2022. Poster 3041; 4. www.clinicaltrials.gov.
5. Espinosa E, et al. Clin Immunol. 2018;194:75-79.
Therapeutic Target Investigational Agents Phase of Development KIT Avapritinib2 Phase 2 sNDA submitted Bezuclastinib2,3 Phase 2 Elenestinib (BLU-263)2 Phase 2/3 Masitinib2 Phase 3 Midostaurin2 IL-6 Receptor Sarilumab2 Phase 2 Tryptase/
Hydroxychloroquine5 Phase
2/3
Agents in Nonadvanced SM
Investigational Therapies4
Mast
Midostaurin Inhibits Kinase Activity of Mutant and Wild-Type KIT
• Open-label phase 2 trial of midostaurin treatment for nonadvanced SM
• Primary endpoint: symptomatic response rate according to MSAF score: average 38% reduction in symptom severity that lasted through week 24 (P<0.01) • Secondary endpoint: disease-specific quality of life measured using MQLQ: median 29% improvement (P<0.001)
N=20 patients with ISM refractory to antihistamine treatment, monitored for 24 weeks. van Anrooij B, et al. J Allergy Clin Immunol. 2018;142(3):1006-1008.

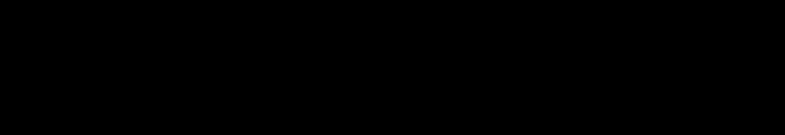
Midostaurin Has Clinical Benefit in ISM/SSM
Retrospective review of Mayo Clinic Experience
MC skin lesion improvement
MC mediator symptom improvement

BM MC decrease Serum tryptase level decrease
N=13, ISM n=11, SSM n=2 patients monitored up to 46 months. Treatment discontinued in 6 patients (46%) due to complete respon se (1), adverse effects (1), no response (2) and adverse effects-suboptimal response (2).
Farrukh F, et al. Am J Hematol. 2022;97(4):E138-E140.
44% 62% 50% 82% 0% 10% 20% 30% 40% 50% 60% 70% 80% 90%
Patients Demonstrating
Some tolerability issues due to gastrointestinal adverse effects resulting in dose reductions but no concomitant loss of response.
Response, %
PIONEER Trial
A 3-Part, Phase 2 Study of Avapritinib in ISM
• Enrollment: Patients with confirmed ISM who have moderate-to-severe symptoms despite receiving ≥2 best supportive care (BSC) medications
• Study design
– Part 1: Dose escalation
Primary endpoint
Determination of recommended phase 2 dose
Secondary endpoints
– Part 2: Pivotal efficacy
Randomized 2:1
Avapritinib 25 mg QD + BSC (n=141)





Placebo QD + BSC (n=71)
• ISM-SAF TSS
–
Bone pain
–
Abdominal pain
–
Rollover
Avapritinib 25 mg QD + BSC
Long-term safety and efficacy
Pharmacokinetics, safety, changes in mast cell burden, and patient-reported outcomes
Primary endpoint
Mean change in TSS
Key secondary endpoints
Rollover
Avapritinib 25 mg QD + BSC
Long-term safety and efficacy
Proportions of patients achieving >30% and >50% TSS reduction; >50% reduction in serum tryptase, bone marrow MC burden, and blood KIT D816V VAF; safety
– Part 3: Patients who complete PIONEER part 1 or part 2 will be eligible to enter an open-label extension (rollover) to evaluate the long-term safety and efficacy of avapritinib 25 mg QD

Nausea
–
Spots –
Itching –
Flushing
–
Fatigue –
Dizziness
–
Brain fog –
Headache –
Diarrhea severity
Mean TSS 53/110
TSS, total symptom severity; QD, once daily. Akin C, et al. Blood. 2020;136(suppl 1):41-42; Akin C, et al. American Academy of Allergy Asthma & Immunology (AAAAI) Annual Meeting; February 24-27, 2023. Abstract 151; Castells M, et al. AAAAI Annual Meeting; February 24-27, 2023. Abstract 627; ClinicalTrials.gov. https://clinicaltrials.gov/ct2/show/NCT03731260.
Randomized 1:1:1:1 Avapritinib
Avapritinib
mg QD + BSC
Avapritinib
mg QD
25 mg QD + BSC (n=10)
50
(n=10)
100
+ BSC (n=10) Placebo QD + BSC (n=9)
Efficacy and Safety of Avapritinib in ISM
Phase 2 PIONEER Trial, Part 1
ISM-SAF TSS1
• At 16 weeks, patients treated with avapritinib 25 mg QD had clinically meaningful improvements in1
–
Total symptom severity
– QoL, as measured by MC-QoL

–
Bone marrow MC burden, serum tryptase, and blood KIT D816V allele fraction
• Avapritinib had a favorable safety profile and was well-tolerated across all doses1
In June 2021, avapritinib was FDA-approved for the treatment of advanced SM in adults.2
N=39 adults with confirmed ISM who have moderate-to-severe symptoms despite receiving ≥2 BSC medications were randomized to either 25 mg, 50 mg, or 100 mg avapritinib QD + BSC or placebo for 16 weeks.
BSC, best supportive care.
1. Akin C, et al. American Society of Hematology Virtual Conference; December 5-8, 2020. Abstract 1248; 2. FDA. 2021. https://www.accessdata.fda.gov/drugsatfda_docs/label/2021/212608s007lbl.pdf.
Weeks Mean Change From Baseline, % -50 0 4 8 16 -30 -10 0 10 Placebo (n=9) Avapritinib 25 mg (n=10) Avapritinib
mg (n=10) Avapritinib 100 mg (n=10) -20 -40 12
50
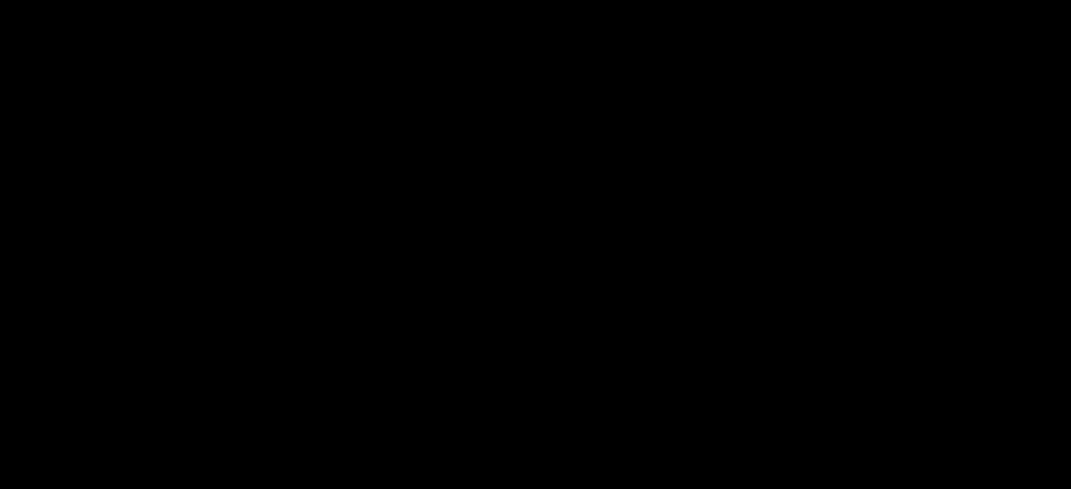
Avapritinib Met Primary Endpoint in Patients With ISM Phase 2 PIONEER Trial


P=0.003. N=212 adults with confirmed ISM with inadequately controlled symptoms despite receiving BSC, n=141 received 25 mg avapritinib QD + BSC or n=71 placebo + BSC for 24 weeks. Akin C, et al. American Academy of Allergy Asthma & Immunology (AAAAI) Annual Meeting; February 24 -27, 2023. Abstract 151; Castells M, et al. AAAAI Annual Meeting; February 2427, 2023. Abstract 627. TSS Score Change A Supplemental New Drug Application was accepted for priority review in January 2023. -15.6 -9.2 -18 -16 -14 -12 -10 -8 -6 -4 -2 0 Avapritinib Placebo
Avapritinib Met Key Secondary Endpoints in Patients With ISM Phase 2 PIONEER Trial
Overall adverse events and serious adverse events were lower in avapritinib vs placebo.
N=212

P<0.0001.
avapritinib QD + BSC or n=71 placebo + BSC
Castells M, et al. AAAAI Annual
February 24-27, 2023. Abstract
Patients Achieving ≥50% Reductions, % 54% 53% 68% 0% 23% 6% 0% 10% 20% 30% 40% 50% 60% 70% 80% Serum Tryptase Bone Marrow MC Aggregates KIT D816 VAF Avapritinib Placebo
adults with confirmed ISM with inadequately controlled symptoms despite receiving BSC, n=141 received 25 mg
for 24 weeks.
Meeting;
627.
KIT
Avapritinib Met Other Secondary Endpoints in Patients With ISM Phase
2 PIONEER Trial



-1.86 -5.87 -0.63 -2.64 -7 -6 -5 -4 -3 -2 -1 0 Spot severity Skin symptom domain Avapritinib Placebo
aP<0.0001, bP=0.0015. N=212 adults with confirmed ISM with inadequately controlled symptoms despite receiving BSC, n=141 received 25 mg avapritinib daily + BSC or n=71 placebo + BSC for 24 weeks. Maurer M, et al. AAAAI Annual Meeting; February 24-27, 2023. Abstract L69. ISMSAF Score Change a -22% -37% 86% -14% 10% -2% 0% -0.5% -60% -40% -20% 0% 20% 40% 60% 80% 100% MC burden Lesion surface area Lightened skin lesion color CD30+ MC in skin lesions Avapritinib Placebo Mean Change, % b
PATIENT-CENTERED MANAGEMENT OF NONADVANCED SM
 Patricia Lugar, MD, MS
Patricia Lugar, MD, MS
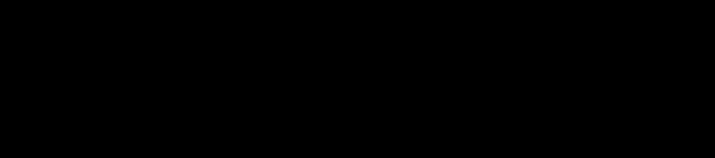
Suboptimal Identification and Delayed Diagnoses Increase Overall Patient Burden


• Delayed
due to the rarity of SM and the broad spectrum of signs and symptoms that are shared by other more common



Median time from symptom onset to diagnosis1
2,3
2
a median of 3 HCPs4 HCP, health care provider.
4. Jennings
Immunol
Clin
4 6 9.5 0 1 2 3 4 5 6 7 8 9 10 BMM ISM SSM Years
diagnosis
disorders
– Puts patients at risk of lifethreatening anaphylaxis, organ dysfunction, and severe osteoporosis
• Prior to diagnosis, patients saw
1. Van
Anrooij B, et al. Allergy.
2016;71(11):1585-1593; 2.
Ungerstedt J, et al. Cancers (Basel). 2022;14(16)3942;
3.
Mikkelsen CS, et al. Dermatol Reports. 2014;6(1):5199;
SV, et al.
Allergy
North Am. 2018;38(3):505-525.
Multidisciplinary Management of Nonadvanced SM


The presence of multisystemic manifestations of symptoms requires multidisciplinary collaboration between –
Allergy/Immunology
–
Dermatology
–
Gastroenterology
–
Hematology/Oncology
–
Primary care
–
Rheumatology
–
Endocrinology
–
Psychiatry
Zanotti R, et al. Cancers (Basel). 2021;13(24):6380; Valent P, et al. Int J Mol Sci. 2019;20(12):2976.
•
Routine Monitoring
• Patients with stablea SSM should be monitored every 6 months and those with stablea ISM every 12 months, for changes in1
– Serum tryptase levels

– CBC/Diff
– CMP
– Weight – Physical examination, including skin/lesions3
• Regression of MPCM lesions does not correlate with changes in underlying ISM2
– QoL/symptom burden: ability to participate in daily activities, ability to eat, respiratory symptoms under control, sleep1,3
• DEXA scan every 1-3 years for patients with osteopenia/osteoporosis1
aPatients with unstable SSM and ISM should be seen more frequently until stabilized.
1. NCCN Guidelines. Systemic Mastocytosis Version 2.2022. https://www.nccn.org/professionals/physician_gls/pdf/mastocytosis.pdf. Accessed January 3, 2023; 2. Dr. Anne Maitland, personal communication; 3. Brockow K, et al. Arch Dermatol. 2002;138(6):785-790.
If laboratory results or symptoms change, therapeutic adjustment should be considered.
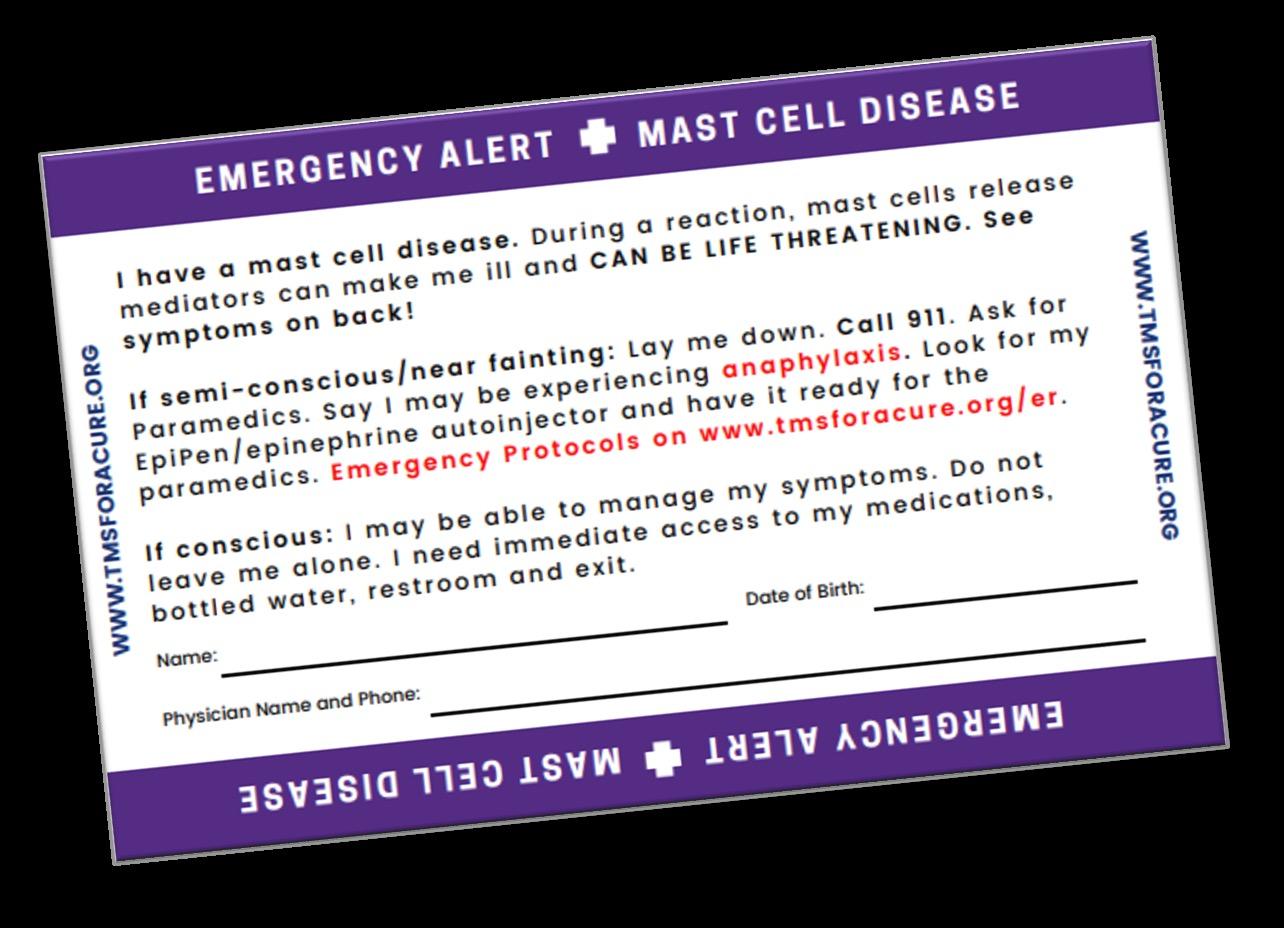
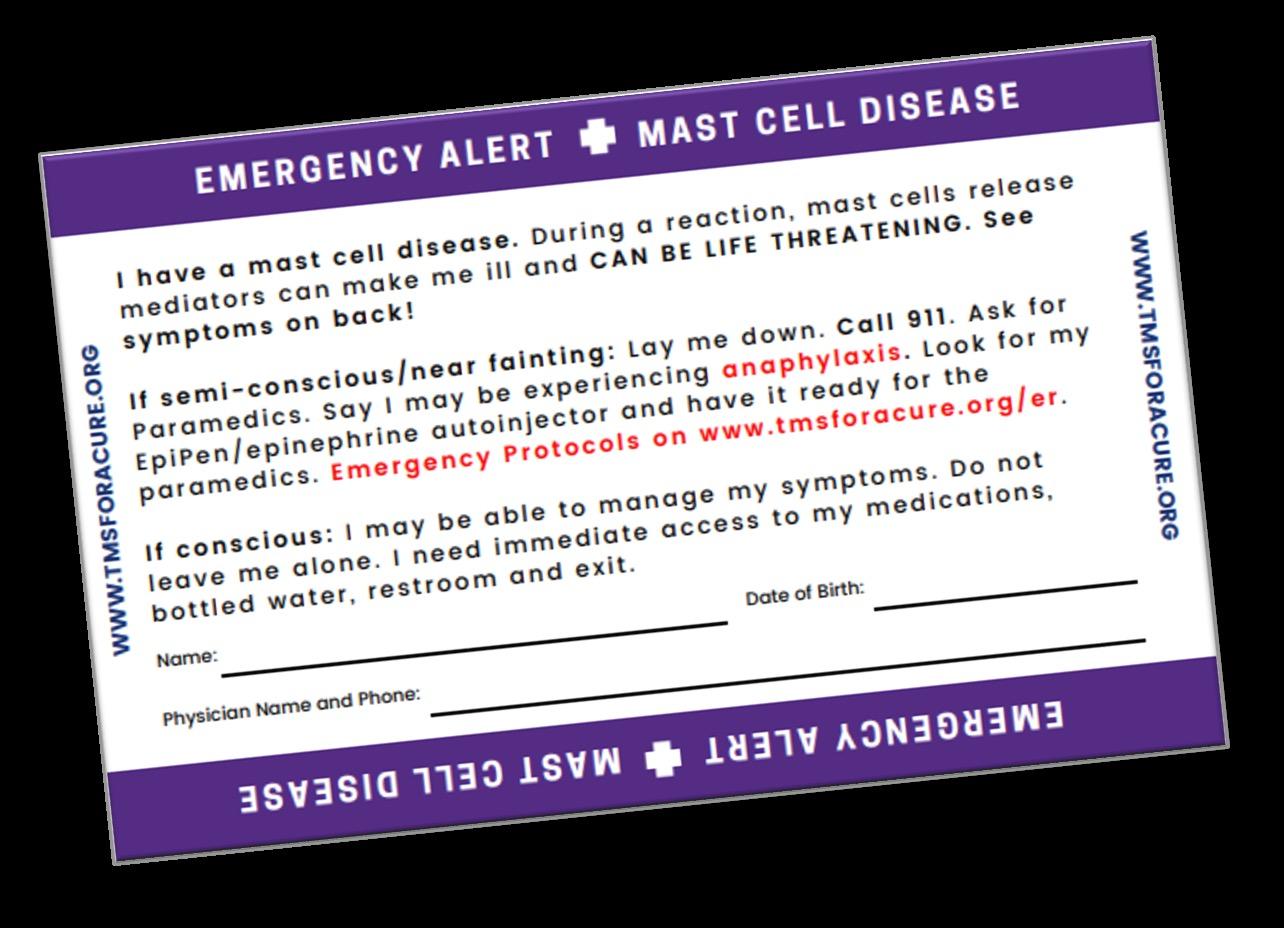
Patient Education Is Critical to Successful Management

• Trigger avoidance
–
Identifying potential triggers

Unpredictability of response •
–
Periprocedural precautions
Anaphylaxis Action Plan
–
Recognition –
Supine position
– How to administer epinephrine
–
Medical alert tag
• Medication adherence
• Finding support groups
•
2022.
TMS.
https://tmsforacure.org/.
Long-term Management of Anaphylaxis
• All SM patients should be trained in supine positioning
• All SM patients should be advised to carry 1 or 2 epinephrine autoinjectors to manage anaphylaxis
• Omalizumab, an anti-IgE mAb, has been shown to be effective for treating recurrent anaphylaxis1
• All SM patients should be assessed for venom allergy with skin and/or in vitro venom-specific IgE tests
– If positive, treat with VIT indefinitely2
• Omalizumaba may be considered if patient is not tolerating VIT3
– VIT benefits outweigh the risks in SM patients4
– If negative, retest after each sting
aOmalizumab is not FDA-approved for SM or recurrent anaphylaxis. VIT, venom immunotherapy.

1. Jendoubi F, et al. Clin Exp Allergy. 2020;50(6):654-661; 2. Niedoszytko M, et al. Allergy. 2009;64(9):1237-1245; 3. Ricciardi L. Int J Immunopathol Pharmacol. 2016;29(4):726-728; 4. Jarkvist J, et al. Allergy. 2020;75(1):169-177; 5. Valent P, et al. J Allergy Clin Immunol Pract. 2022;10(8):1999-2012. Risk of Anaphylaxis5 BMM High ISM Intermediate SSM Intermediate



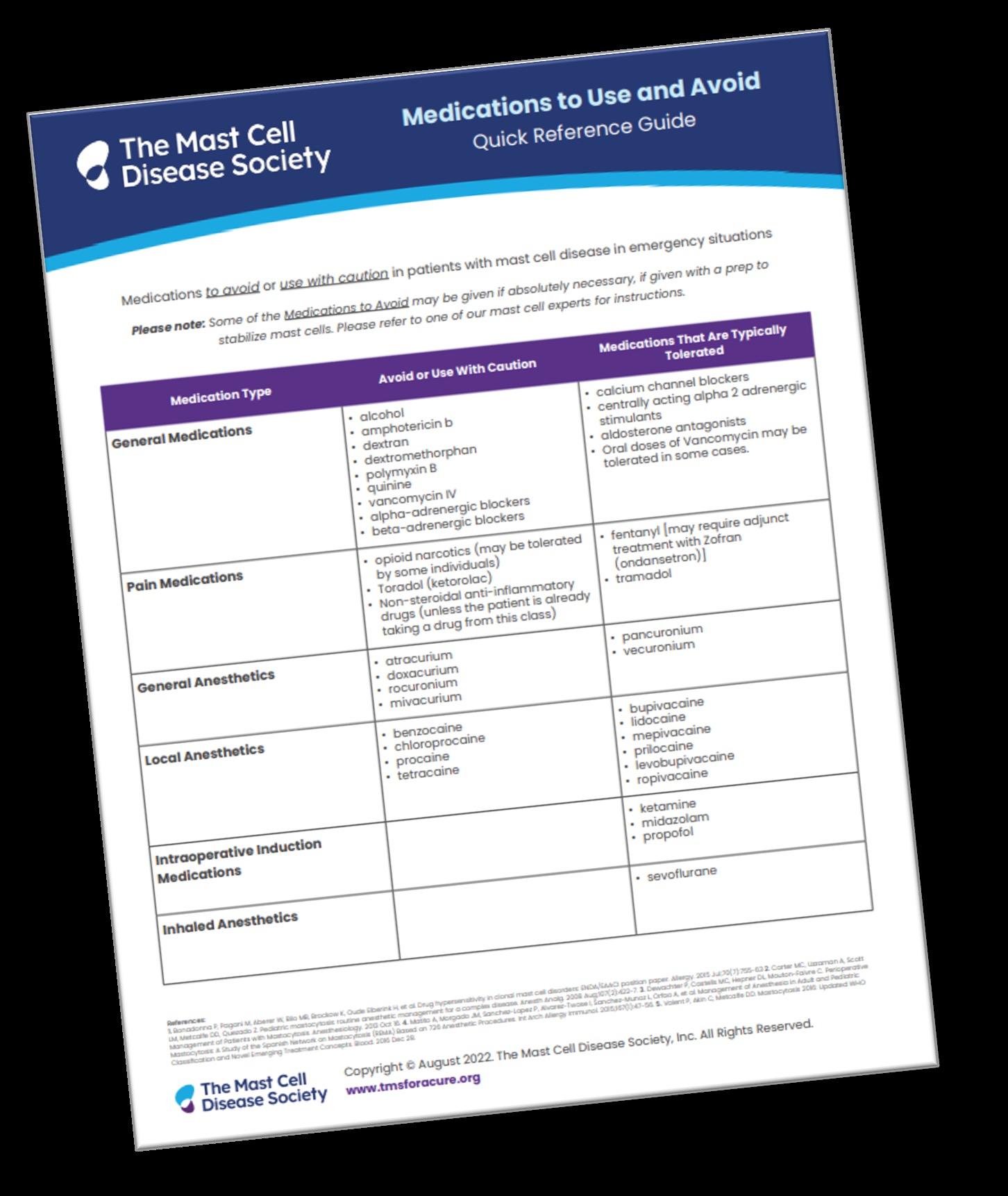
TMS. 2022. https://tmsforacure.org/.
Patient Action Plans
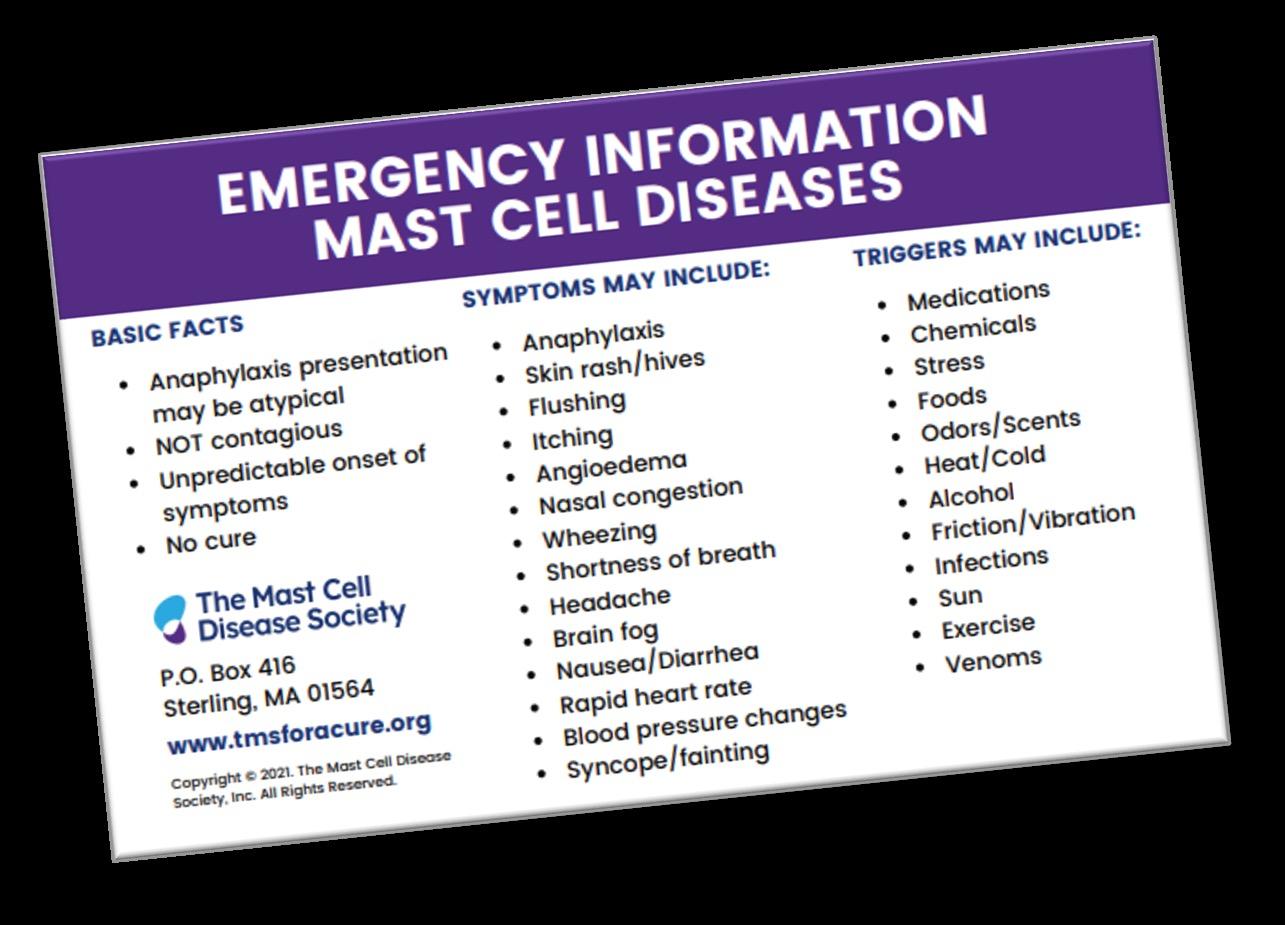
Patient Resources

NCCN Guidelines for Patients®

Systemic Mastocytosis, 2022
https://www.nccn.org/patientresources/patient-resources/guidelines-for-patients
The Mast Cell Disease Society (TMS) provides multifaceted support to patients, families, and medical professionals through education, advocacy, and collaboration.

https://tmsforacure.org/
GARD helps patients find information, services, experts, financial aid, and support groups.
https://rarediseases.info.nih.gov/

NORD is a patient advocacy organization committed to the identification, treatment, and cure of rare disorders through programs of education, advocacy, research, and patient services.
https://rarediseases.org/

Summary

Nonadvanced SM has a complex pathophysiology and clinical presentation, making identification and diagnosis difficult • Physical and/or neuropsychiatric symptoms disrupt daily activities and reduce quality of life • Disease management must be personalized and largely preventive and symptom-directed
Targeted agents are under investigation for treatment of nonadvanced SM and may soon provide therapeutic alternatives
• The multisystemic manifestations of nonadvanced SM necessitate multidisciplinary management
•
•