A step in the right direction Podiatry Review The Institute of Chiropodists and Podiatrists News SUMMER ISSUE Volume: 79 No: 3 Jul/Aug/Sep 2022 The Institute of Chiropodists and Podiatrists FREE 4 Page CPD Article Principles of Gait: Understand the Priciples of the Acceleration Lever System Primary Care Conference + Irish AGM & Conference Pages 21-24 Pages 8-9 Pages 30-34 Pages 36-37 COVID Toes: An Update Medical Honey: the taste of sweet success? Pages 12 -14 AiM - the Foot Part 2 NEW! Lower Limb Skin Surgery Course in Partnership with The Association of Surgeons in Primary Care Page 10

Editor: Andrew Williams, MInstChP, CFPodM
Academic Editor: Martin Harvey, PGCert, BSc, MInstChP, MCPodS
Academic Advisor: David M Holland, CSci, CBiol, FFPM-RCPS(Glasg)
Academic Review Team
Ms B Wright, MSc BSc (Hons), PGCE PGDip, FInstChP
Mr S Miah, CFPodM, MInstChP
Mr A Williams, MInstChP, CFPodM
Media and Publicity Contact: Doctor Bharti Rajput, MBE PhD Email: media@iocp.org.uk

Medicines and Procedures Panel (MaPP)
Chair: Gaynor Wooldridge, MInstChP, CFPodM
Andrew Williams, MInstChP, CFPodM
Abid Ali, CFPodM, BSc, MInstChP
Somuz Miah, CFPodM, MInstChP
Martin Harvey, PGCert, BSc, MInstChP, MCPodS
Contents Podiatry Review Summer Jul/Aug/Sep 2022
Review
Subscription £20
/
Podiatry
Volume: 79 No: 3 ISSN 1756-3291 Annual
UK
£30 Overseas Published by The Institute of Chiropodists and Podiatrists 150 Lord Street Southport Merseyside PR9 0NP Tel: 01704 546141 Email: info@iocp.org.uk Website: www.iocp.org.uk
© The Institute of Chiropodists and Podiatrists Disclaimer: The Editor and the Institute of Chiropodists and Podiatrists accept no responsibility for any opinions expressed in the articles published in the journal, and they do not accept any responsibility for any discrepancies in the information published. No part of this publication may be reproduced, stored in a retrieval system or transmitted in any form or by any means, electronic, mechanical, photocopying or otherwise, without the prior written permission of the publishers. CONTACTS 4 IOCP Contacts 5 Editorial ARTICLES 6 5 minutes with your CEO 7 IoCP & Melanoma UK partnership 8-9 Primary Care Conference & Irish AGM 11 Benefits of Shockwave Therapy 12-14 Medical Honey: the sweet taste of success? 15-17 Footnotes: Foothealth Practitioner News 18-19 Platelet Rich Plasma (PRP) 20 2022 Mid Wales Diary 21-24 4 page CPD articlePrinciples of Gait: Understand the Principles of the Acceleration Lever System 25 Understanding the Human Foot: Book review 26-27 College of Paramedics: CPD thoughts 30-34 AiM -the Foot Part 2 35 The International Podiatry Pilot Programme 36-37 COVID Toes - An Update 41 Obituary: Mary Marsh COURSES 10 Acupuncture, Laser therapy & Lower Limb Skin Surgery NEWS 40 Branch News 42 Classified Adverts 43 Diary of Events 12-14 @IOCP_Chiropody @IOCPChiropody Podiatry Review Summer Issue 2022 | 3 8-9 18-19
IOCP Contacts
Executive Committee
President: Mrs C McCartney, MInstChP
Chair Executive Committee: Mr M Harvey, PGCert, BSc, MInstChP, MCPodS
Vice-Chair Executive Committee: Mr A Ali, CFPodM, BSc, MInstChP, BSc
Chair Board of Education: Mr A Williams, BSc(Hons), CFPodM, FFPM RCPS(Glasgow)
Vice-Chair Board of Education: Ms B Wright, MSc BSc (Hons), PGCE PGDip, FInstChP
Chair Board of Ethics: Ms B Wright, MSc BSc (Hons), PGCE PGDip, FInstChP
Honorary Treasurer: Mr S Miah, CFPodM, BSc (PodM), MInstChP
Regional Director (Ireland): Mr S Preston, MInstChP
Regional Director (Scotland): Mrs H Jephcote, MInstChP
Regional Director (England North): Mrs C McCartney, MInstChP
Regional Director (England Midlands): Mr W J Liggins, MA, BSc(Hons), FCPS, FInstChP
Regional Director (England South): Ms B Wright, MSc BSc (Hons), PGCE PGDip, FInstChP
Regional Director (Wales): Mrs L Pearson, FInstChP, BSc Pod Med`
Academic Advisor: David M Holland, CSci, CBiol, FFPM-RCPS(Glasg)
Medicines and Procedures Panel (MaPP): Gaynor Wooldridge, MinstChP, CFPodM
Chief Executive Officer: Mr Anthony Hubbard, CSci CChem FRSC
Company Secretary: Miss A J Burnett-Hurst, HonFInstChP Standing Orders Committee: Mr M Franklin, MInstChP
Branch Secretary Telephone Email
4 | www.iocp.org.uk CONTACTS
& the Shires Kate Harrison 01789 262365 kathrynharrison87@gmail.com Cheshire & North Wales Michele Allison 07766 700027
Essex Beverley Wright 01702 460890 solespirits@hotmail.com Irish Janette Pegley-Reed 00353 8627 31371 jpegleyreed@gmail.com Leeds and North East Caroline McCartney 07583 934468
Sarah Bowen 07790 717833
North West Alison Marsden 01772 623180
Helen Rawse 07789 025022 hrawse@live.co.uk
Wales & Monmouth Esther Danahar 01656 740772
John Stott 0780 135 6485
Collett 01785 716607
(Acting secretary of)
Birmingham
missminou@hotmail.co.uk
hello@chiropodyandfoothealth.co.uk London
footwoman@gmail.com
alison.marsden@hotmail.com Sheffield
South
estherdanahar@yahoo.co.uk Scottish
jls@stottland.com Wolverhampton David
djcollett@hotmail.co.uk Branch Secretary Contacts
Dear Colleagues
Welcome to the summer issue of the Podiatry Review. Where to startso far what a busy year this has been for myself from opening my third clinic to getting elected as the new IoCP President 2022 - 2024!
On the 11th May, myself and our Leeds & North East Branch Chair Anne Mcintosh attended the Primary Care Show event at the NEC Birmingham. The Primary Care Show is made up of trade stands, lectures and speakers plus offers valuable networking opportunities and is a fantastic way to refresh and update your knowledge and skills!
Martin Harvey, our IoCP Chair, did a fabulous lecture at the Primary Care Show on ‘Trigger Points in the Lower Limb, Myofacial Pain and Dysfunction’ which was a full house!
The Institute’s 67th Annual General Meeting was held on the evening of Wednesday 12th May at the Arden Hotel Birmingham. Voting for the position of President had been carried out by a postal ballot on a one member one vote basis. My branch had nominated myself as the potential new President so I was completely overwhelmed when I was declared by Martin as now holding the elected position! My thanks to all members who voted for myself and to Bill Liggins and of course Linda Pearson who has served as President from 2014 - 2022 for their kind words of support. The AGM evening ended with drinks and food it was great to catch up and socialise with peers and head office staff after having only seen virtually over the last few years.
Our WhatsApp group, which I formed for our Leeds & North East Branch during the first lockdown, is still used on a daily basis by 32 members and has proved invaluable in building up relationships and interactions as well as some much needed friendly banter!
Our Leeds & NE Branch have held a number of meetings so far this year at St Mary’s Social Club in Batley, Leeds including a talk on Wounds, Wound Healing and Dressings given by our member Helen Beaumont-Waters.
In March myself along with Kirsty Warne and Afni Shah-Hamilton created the Institute’s first ever business club… aptly named ‘Step Ahead Business Club’. We will be running a quarterly interactive webinar event so members have the chance to ask and discuss the topic of the night. We had some very positive feedback from our first meeting and welcome any suggestions for future meetings.
And lastly Kirsty and I are currently organising a CPD day event in Leeds in October which we will be sending out information about shortly!
I’m looking forward to the rest of the year ahead and hope together we can grow an even better future for the IoCP and College of Foot Health.
Caroline McCartney, President & England North Regional Director

Guidelines for new and established authors
Content of your article should be Podiatry or foot health-related. Podiatry Review is mostly in easy-to-read format, and articles for submission should reflect this. CPD Certificates are issued for Case Studies and Articles. Please ensure that your name and title (ie - FHP, Podiatrist, or other) are included with your article. Please proof-read and spell-check your article before submission. It would be helpful to the Editorial Committee if you could reference any books or Papers mentioned in your article. If you are not sure how to do this we are happy to assist.

Podiatry Review Summer Issue 2022 | 5
Editorial
Chief Executive Officer Anthony Hubbard CSci CChem FRSC
I would like to congratulate Caroline McCartney on being elected to the role of President of the IoCP, to thank Linda Pearson for her contribution as our previous President and to thank Bill Liggins for accepting the nomination for the role and standing in the election. I would also like to thank all of you who took the time to vote for your chosen candidate in the election. It really is good to see people willing to stand for office and to see our democratic process being engaged by so many of you.
It has been great to learn all about the workings at the office, to attend the Primary Care and Public Health event at the NEC, to attend an AGM and to get down to driving improved activities for 2022 and beyond.

It has been good to meet with a lot of our members, old and new, to get an understanding of what they want from
their organisation and also to have members come forward to volunteer as mentors and tutors to support the growth in educational knowledge and to support business development of other members. I am still looking to increase our tutor base and if that is something that may be of interest to you, please get in touch with me directly at anthony@iocp.org.uk
I also had a very enjoyable visit to our island of Ireland conference in May; what a great event with some great speakers that was well attended by members and we had some non-members enrolling for the education too. We will be looking to hold more regional meetings as a way to deliver CPD, to allow networking and so that you can meet members from our Executive and staff to discuss IoCP matters.
We have also announced new working partnerships with the Association
of Surgeons in Primary Care, who will be delivering our new minor surgery courses and with Melanoma UK who we are working with to raise the awareness of the issues with skin cancer and to provide podiatric dermatology training for our members. It is a very exciting time to be able to enhance the learning and support that we are providing to our members in making a difference to both themselves as individuals and to the patients whom they are providing information and services to.
We have also launched our Step Ahead Business Club that had a great turn out for its inaugural meeting and second meeting with Jenny Tobin of Advanced Accountancy. We hope to see you at our next meeting!
Enjoy the summer and stay safe in the sun!
Your Charity of the Quarter Nominations
As we expand our partnerships and collaborations with other professional bodies and charities we would like to encourage members of both the Institute of Chiropodists and Podiatrists and the College of Foot Health to nominate their favourite charity, so we can show our support to their work and commitment in raising awareness of health related conditions and diseases. The Nominated Charity will be promoted by our organisation for the next quarter featuring in our journal and online.
Please nominate your charity by either writing to Head Office at: The Institute of Chiropodists and Podiatrists, 150 Lord Street, Southport, Merseyside PR9 0NP
or by email to julie@iocp.org.uk with the subject ‘Nominated Charity’, please include details of your chosen charity, a reason why you have nominated them, please also include your photo as nominee, as this will appear alongside the Charity Nomination Page in our October issue.
The final date for nominations to be received is 5th August, after this date a charity will be chosen at random for the next quarter starting in the October issue.
The winning charity would be contacted to let them know that they have been nominated as our charity of the quarter, for their logo and information, and we will publish their information along with a link to where members and subscribers of Podiatry Review can donate to.
6 | www.iocp.org.uk ARTICLE
Just a half-year in the role & it seems that I have been here a lifetime!
IoCP announce partnership with Melanoma UK



We were delighted to announce our partnership with Melanoma UK during Skin Cancer Awareness month in May. The intention of this partnership is to raise awareness of melanoma, not only during May but throughout the course of the year and your careers, for podiatrists and foot health practitioners to identify lesions of concern, and to give guidance through information and services available to both healthcare professionals and their patients.
Melanoma UK is the leading melanoma patient support organisation in the UK who are active in their participation in health technology appraisal meetings (NICE and SMC), presenting clinically validated information on their website, authoring publications from their Melanoma UK digital registry and who have developed and regularly engage with their very own panel of medical experts.
Melanoma is the deadliest form of skin cancer and is the 5th most common cancer in the UK. By 2025 it is projected that 19,513 people in the UK are expected to be diagnosed with melanoma and according to the World Health Organisation approximately 3,119 of these people are expected to die from melanoma that year.




As podiatrists and foot health professionals we see a 3rd of a person’s body each and every working day. It is important that we have an understanding of troublesome lesions and that we can identify those which could prove lethal to our patients. This partnership is the beginning of a journey to educate our profession, offer greater care to our patients, and an opportunity to work together to help reduce these daunting figures.
What better way to introduce you to melanoma on the lower limb than a highly-informative webinar on acral and subungual melanoma with Professor Christian Aldridge (Melanoma UK Medical Advisor) and Ms Kei Hutchinson (Associate lecturer In podiatry at Cardiff Uni) on Acral and Subungual Melanoma which can be found at https://www.melanomauk.org.uk/ acral-and-subungual-melanoma.
Together with Melanoma UK we aim to bring you further information, news and education around skin cancers and melanoma throughout the course of the year.
Anthony Hubbard, CEO IoCP: “I am delighted that we are in partnership with Melanoma UK. Melanoma UK are passionate about supporting patients and their families during the very difficult times faced upon diagnosis. They also actively promote education and awareness of melanoma to help to drive the early detection of the disease, which makes so much difference to the outcomes.
They have long-standing support from a large network of medical professionals who work in research, education, medical and surgical disciplines, as well as those who provide patient support after diagnosis. We are proud to be working alongside Melanoma UK, who will be supporting the IoCP in podiatric dermatology education, whilst we support them in driving their early detection awareness across our membership for the benefit of our patients.”
Podiatry Review Summer Issue 2022 | 7
For more information on melanoma and the great work and resources
50 60 70 80 90 100110 120 130 140 150 160 170 180 190 200 210 10mm 8mm 6mm 5mm 4mm 3mm When borders are irregular, ragged, blurred When there is no uniform pigmentation When greater than 6mm but could be smaller Changes to a mole’s appearance When one half doesn’t match the other REMEMBER THE ABCDE OF MELANOMA
available from Melanoma UK visit www.melanomauk.org.
Primary Care Conference and Exhibition



Our first major event since 2019 and the global pandemic. Arriving unsure of exactly what to expect in terms of overall delegate numbers and visitors to our stand, the event did not disappoint! For 2 days COVID was pushed to our subconscious as we interacted with many members, colleagues, trade and healthcare peers.
2022Launching our new minor surgery course in partnership with the Association of Surgeons in Primary Care, as well as our Class 4 Laser Therapy CPD course, all of our board members were on hand to discuss and answer any questions, including Gaynor Wooldridge who had numerous conversations about the benefits of Manuka Honey for wound care (followed by an exceptional article in this review!) and Martin Harvey who’s lecture on the main conference program ‘Trigger Points in the Lower Limb, Myofacial Pain and Dysfunction’ was very well attended.
Thank you to all who took the time to meet us and share their feedback. We were overwhelmed with enquiries from fellow organisations and trade partners about developing relationships to benefit our organisation and our members. Our team are busy working through this information and we hope to bring you further news in the coming months.
Ireland AGM & Conference

Our Irish branch held their very first conference and AGM on 21st May. This was the first opportunity for members, new and old, to meet and network in quite some time! CPD lectures included Tendinopathy management with Olgas Jones, Rearfoot pathologies with Sean Savage, Chairside treatments for tendinopathy with Claire Rooney and Marketing and Branding by Lorcan O’Donaile.
The event was highly successful and feedback from members and non-members alike, has been extremely positive. A huge congratulations and thank you to our wonderful branch team particularly Regional Director Stephen Preston and the amazing Janette Pegley-Reed who organised and managed the event, and to all of the wonderful speakers mentioned above. An extended thank you to Julie, Damon and Anthony from Head Office for joining the event. Our Irish branch are looking forward to their next big event on the 22nd of October, 2022.
8 | www.iocp.org.uk ARTICLE
Sian Parker-Perry
Lewis Stuttard
IoCP AWARDS

Student of the Year Awarded to Sian Parker-Perry Student Endeavour Award Awarded to Patricia Radford
The Basham Literary Prize 2021 / 2022 Awarded to both Afni Shah-Hamilton & Andrew Horwood
Academic Fellowship Awarded to Afni Shah-Hamilton

Consultant Fellowship Awarded to Afni Shah-Hamilton and Abid Hussain



Honorary Consultant Fellowship Awarded to Lewis Stuttard


Podiatry Review Summer Issue 2022 | 9
Afni Shah-Hamilton
Patricia Radford
Abid Hussain
COURSES
These courses are all approved and certified by The Institute of Chiropodists and Podiatrists
Podiatric Acupuncture Course



Date: 10th and 11th September 2022
Time: 9am until 5pm –two full days
Venue: IoCP Training Centre, Southport PR9 0NP
Tutors: David Lintonbon, DO PG Cert Clin Ed and Somuz Miah,CFPodM, BSc (PodM), Cert HTox, Dip Sp.I, PGC IP, MFPM RCPS (Glasg)
Cost: Members £450 Non-members £495
All students receive a box of acupuncture needles to take home with them
How will you benefit from Podiatric Acupuncture Training?
Podiatrists may use acupuncture to treat alone or in combination with other modalities, symptoms associated with musculoskeletal disorders, neurological disorders and circulatory disorders.
See more www.iocp.org.uk/course/podiatric_ acupuncture_course
Laser Therapy Course
Date: 24th September 2022
Time: 9am until 5pm
Venue: The Wiggin Training Centre at Sir Robert Peel Hospital, Mile Oak, Tamworth B78 3NG
Tutors: Somuz Miah, Abid Ali & Kirsten Sinclair
Cost: Members £225 Non-members £295
About the Course
To understand the basic principles and applications in the use of the most modern and up to date class 4 lasers. How they work, what they do, and how to practically use the technology in the treatment of a variety of condition for podiatry.
You will understand all the contraindications of when to, and when not to, use laser as well as health and safety, consenting and record keeping.
See more www.iocp.org.uk/course/class-4-lasertherapy
Lower Limb Skin Surgery Course in partnership with the Association of Surgeons in Primary Care (ASPC)

This course is designed to educate podiatrists on all aspects and considerations for minor surgery, from lesion recognition to legal requirements, through to performing minor surgery. There are 2 parts to the course.
WHO CAN APPLY
Part 2
Delegates wishing to carry out full thickness excisions of the epidermis and dermis and any non-malignant lesion or cutaneous benign neoplasm therein or thereon, and which necessitate closure by sutures or applied external skin closures such as ‘steristrips’ or similar (or any combination thereof) should first demonstrate their ability to perform such excision, closure, and any necessary haemostasis ‘in vivo’ to the satisfaction of an IOCP tutor, or other suitable mentor recognised by the IoCP.

Tutors: Dr. Soon Lim & Martin Harvey September intakes Thursday 22nd &
ABOUT THE ASPC
The ASPC are a dynamic and evolving organisation who exist to provide support, training and professional development for providers of Primary Care Surgery in the UK. The ASPC are affiliated with the Association of Surgeons of Great Britain and Ireland and have links with the Royal College of General Practitioners, the Association of Surgeons in Training, the British Association of day surgery and the PCSA, (ASPC sister organisation in the Republic of Ireland).
These affiliations establish the ASPC as being at the forefront of minor surgery within the community.
Course places are limited For further info phone 01704 546141 or email: info@iocp.org.uk Go to www.iocp.org.uk/courses-events/ to book your place
| www.iocp.org.uk
10
HCPC registered podiatrists with POM-A / POM-S & LA certificate
Part 1 of the course comprises 3 stages: • Online learning modules • Interactive cohort learning via Zoom - 1 day live session • Practical - a full 1 day workshop
COSTS FOR PART
£995 for
members & £1,200
COSTS
Mentorship £250
1
IoCP
non-members.
FOR PART 2
Thursday 29th September

Podiatry Review Summer Issue 2022 | 11
Products & Procedures under the microscope
With Gaynor Wooldridge Chair of the Medicines and Procedures Panel (MaPP) at the Institute of Chiropodists and Podiatrists
Introduction
Bees are incredible. Honey bees (Apis Mellifera) are nature’s chemists. They are able to change the watery sugar collected as nectar (83% water), into the supersaturated power food that we know as honey (18% water). If we were to perform this magical action of super saturation, we would need 181 components, including heat, enzymes and other chemicals to achieve our goal (Riddle, 2016).
In this article, we will discuss a brief history of the use of honey, by humans, for it’s medicinal, it’s biological and it’s activities on wound healing; we will also assess how we, as podiatrists, can incorporate medical honey into our management of foot ulcers (including diabetic wounds), acute and chronic wounds (superficial or deep), and post surgical wounds that present either in clinic or a domiciliary environment.
The History of Honey as a Medicine
Honey has been used by humans since ancient times. Geiling (2013) reports that modern archaeologists excavating ancient Egyptian tombs have often discovered unexpected pots of honey still preserved, and cave paintings dating from Stone Age (approximately 8000 years ago), depict a man climbing a cliff face on rope ladders to harvest honey (Topal et al. 2021, fig 1). It was the Egyptians, however, who almost certainly were the first people to apply honey to wounds. Honey, grease (animal fat to form a barrier) and lint (vegetable fibre to drain the wound) were the main components of the most common plaster used by the Egyptians, with honey used as an effective antibacterial. (Shah, 2011).
et al, 2008). Minden-Birkenmaier and Bowlin (2018) scrutinised the plethora of in vitro and in vivo evidence that demonstrated that honey debrides wounds, kills bacteria, penetrates biofilm, lowers wound pH, reduces chronic inflammation and promotes fibroblast infiltration.


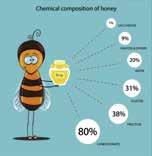
So what exactly is honey that makes it so special?
FIG.2
FIG.1
“The god Re wept, and the tears from his eyes fell on the ground and turned into a bee”
From an acient Egyptian papyrus

The first human beekeepers were foragers of wild honey, and not keepers of bees. Domesticated beekeeping became a common practice starting around 2,500 BC, again in Egypt and possibly earlier in China.
The use of honey in wound management has enjoyed a resurgence over the past few years, after falling out of favour in the 1940s (Clardy et al. 2009). This is largely due to the growing problem of antibiotic-resistant bacteria, and the combined difficulties in the management of chronic wounds that may become infected with methicillin-resistant Staphylococcus aureus or Pseudomonas (Lay-flurrie
The chemical make-up of honey (C6H12O6) is primarily sugar. Sugars contain very little water in their natural state (hygroscopic), but they can suck in moisture if left unsealed (Avarez-Suarex et al. 2014); very few bacteria or microorganisms can survive in this sort of environment. It is also extremely acidic, with a pH between 3 and 4.5, which kills off almost any bacteria and organisms that may attempt to colonise it (Nolan et al. 2019). An acidic pH also encourages blood to release oxygen, vital for wound healing, and reduces the presence of proteases that can impair wound healing (Du Toit and Page, 2009).
Sugar has an osmotic effect. The sugar naturally present in honey draws water out of damaged tissues, reducing swelling and encouraging the flow of lymph to enable wound healing. Sugar also draws water out of bacterial cells, preventing them from multiplying (Nair et al. 2020). Honey has been shown to also have an antibacterial effect on colonised wounds, such as methicillin-resistant Staphylococcus aureus (MRSA) and vancomycin resistant Enterococci (VRE) (Molan and Rhodes, 2015).
12 | www.iocp.org.uk ARTICLE
Medical Honey:
the taste of sweet success?
Lets get back to the bees, those scientists in the natural world, and where it all begins! Honey starts with nectar. Honey is a viscous substance with a very low water content, whereas flora nectar is approximately 80%. Bees are able to change the complex sugars found in nectar, into simple sugars by producing invertase, an enzyme in their salivary glands; this process is known as hydrolysis (Riddle, 2016).
ACTIVITY
Place
The goal of successful wound care must be to initially remove any offending insult, and then provide the best environment in order to facilitate good wound healing. Controlling the bacterial load of a wound is one of the most important aspects of ensuring an optimal level of healing (Jull et al. 2008).
Leave both overnight Remove both, dry potatoes and weigh
What does this tell us about osmosis?
A second enzyme, glucose oxidase, found in their “honey stomach” or crop, mixes with the nectar. This is then broken down into two by-products: gluconic acid and hydrogen peroxide (Jones, 2009). This mixture is regurgitated into the cells of the hive, and the bees remove most of the moisture by flapping their wings to dry out the honey substance (Topal et al. 2021).
Minden-Birkenmaier and Bowlin (2018) discussed how the production of gluconic acid results in the lowering of the pH of honey, and hydrogen peroxide enhances its bactericidal efficacy. This low pH of honey enables a series of events, allowing tissue repair to occur.
A reduction in protease activity in the wound site

An increase in oxygen release from haemoglobin
The stimulation of fibroblast and macrophage activity
The production of hydrogen peroxide also stimulates vascular endothelial growth factor (VEGF) and sterilises the wound (Molan and Rhodes, 2015).
The current potential of honey in wound care

A wound can result from either an external or internal insult. Following trauma, healing can be delayed for many varied reasons, and inadequate circulation often robs tissues of necessary nutrients, and potentiates pro-inflammatory cytokines; this can lead to tissue necrosis (Mustoe, 2004). The process of wound healing is classically divided into 4 stages: haemostasis (seconds to minutes), inflammation (3-5 days), proliferation (4-14 days) and remodelling (8 days to one year). There can be a significant overlap of these stages (Janis et al. 2010).
Tashkandi’s review of honey in wound healing (2021) concluded that medical honey is a promising wound healing agent, with a broad spectrum of antimicrobial activity and no known resistant pathogens. They also found that it was effective against clinical bacteria and fungal isolates, plus their associated biofilm. It was shown to be safe and cost effective. Cooper et al. (2011) also investigated the role of medical honey (Activon, Advancis Medical) and in vitro biofilm of MSSA, MRSA and VRE, and found that they could be prevented and inhibited at concentrations above 10%; these concentrations are available to use within clinical practice.
Our role in wound management
The role of the podiatrist and foot health practitioner within wound healing is an essential one. We are often the first to recognise the presence, or the impending formation, of a wound. More than 60% of non traumatic amputations occur in people with diabetes (Bell, 2009). We are all aware that prolonged chronicity of wounds is usually related to bacterial colonisation. This can 3 progress to the bacterial resistance of systemic and topical microbial agents, or the development of the dreaded biofilm. Our job as health professionals usually involves debridement of non-viable tissue and bacterial biofilms, followed by the application of an appropriate dressing. These are commonly a standard dry dressing, a highly absorbent dressing such as an alginate, or a hydrocolloid (Rossi and Morrazzo, 2021). This procedure often fails, which has lead to an interest in alternative treatment approaches, and a renewed interest in honey (Nair et al. 2020).
FIG.3
Honey-based products show excellent compatibility with tissue cell cultures when compared to silver dressings (Du Toit and Page, 2009).
Fig. 3 A granuloma treated with medical honey (one application) left in situ for one week.
Podiatry Review Summer Issue 2022 | 13
a piece of potato in 100mls of water
Place a piece of potato in 100mls of water with 2 tablespoons of honey
Products & Procedures under the microscope
(continued)
With an increasing number of wounds, decreasing budgets and reduced resource availability, as well as an NHS crisis post COVID, wound care services are under increasing pressure. As front line care providers, and often the potential ‘gatekeepers’, it is important that we provide a robust delivery of care, and pathways to ensure our patients have the best access to optimum medical interventions.
With the appropriate skills and knowledge it has been shown that podiatrists and foot health practitioners can greatly improve patient outcomes (Kivi, Dwyer and Lance, 2016). The ability for patients to attend primary care practices for dressing changes can be difficult for a number of reasons. Within our clinical environment, the possibility of a patient returning home with a simple, and effective, dressing routine, is definitely exciting and food for thought!
REFERENCES
Avarez-Suarex, JM. 2014. The composition and biological activity of honey: a focus on maunka honey. Foods 3(3): 420-432 Bell, DP. 2009. The role of podiatry in wound management. J Am Col Certif Wound Spec 1(3): 78-79 Clardy, J et al. 2009. The natural history of antibiotics. Curr Bios 19: R437-R441 Cooper, R et al. 2011. Inhibition of biofilms through the use of manuka honey. Wounds UK. Vol 1 No. 1 Du Toit, DF and Page, BJ. 2009. An in vitro evaluation of the cell toxicity of honey and silver dressings. J Wound Care 18: 383-389 Geiling, N. 2013. The science behind honey’s eternal shelf life. Smithsonian Magazine Janis, JE et Al. 2010. A practical guide to wound healing. Plast Reconstr Surg 125(6): 230e-44e Jones, R. 2009. Honey and healing through the ages. Journal of Api/Product and API/Medical Science 1(1): 2-5 Jull, AB et al. 2008. Honey as a topical treatment to wounds. Cochrane Database. September Rev 4: CD006083 Kivi, K, Dwyer, C and Lance, B. 2016. Honey of a wound: the use of medical honey to heal diabetic foot ulcers in a low resource environment. Wound Care Canada Vol 14, No 3 Lay-flurrie, K. 2008. Honey in wound care: effects, clinical application and patient benefit. BR J Nurs June 12-25 Minden-Birkenmaier, BA and Bowlin, GL. 2018. Honey based templates in wound healing and tissue engineering. Bioeng 5(2): 46 Minden-Birkenmaier, BA. 2018. Resurgence in clinical use of honey as a topical wound management. Bioengineering 5(2): 46 Molan, PC, and Rhodes, T. 2015. Honey: a biologic wound dressing. Wounds: a Ompendiim of clinical Research in Practice 27(6): 141-151 Molan, PC. 2011. The evidence and the rationale for the use of honey. Wound Pract Res 19: 204-220 Molan, PC. 2002. Reintroducing honey in the management of wounds and ulcers: theory and practice. Ostomy Wound Manag 48: 28-40 Mustoe, T. 2004. Understanding chronic wounds: a unifying hypothesis on the pathogenesis and implications for therapy. Am J Surj 187(5A): 655-705 Nair, HKR et al. 2020. Medical grade honey kills antibiotic resistant bacteria and prevents amputation in diabetics with infected ulcers: a prospective case series. Antibiotics 9: 529 Nolan, VC et al. 2019. Dissecting the antimicrobial composition of honey. Antibiotics 8(4): 251 Riddle, S. 2016. The chemistry of honey. Bee Culture Magazine Rossi, M and Morrazzo, P. 2021. The potential of honeybee products for biomaterial applications. Biometrics 6:6 Shah, JB. 2011. The history of wound care. J Am Col Certif Wound Spec 3(3): 65-66 Tashkandi, H. 2021. Honey in wound healing: an updated review. Open life Sci 16(1): 1092-1100 Topal, E et al. 2021. Traces of honeybees, API tourism and beekeeping: from past to present. Sustainability 13/21

FIGURES
Fig 1 Stone Age cave painting depicting a man on a ladder, foraging for honey. Found in the “cave of the spider” (cuava de la arana), Valencia, Spain. Shutterstock free image.
Fig 2 The Chemical Composition of Honey. Rybakova, image 6231260. Vectorstock free image. www.vectorstock.com/royaltyfree-vector-chemical-composition-of-honey-vector Accessed 23/5/22
Fig 3 Granuloma at nail sulcus, treated with Activon medical honey. Before and after photos. Permission to use given by patient.
GLOSSARY
Re or Ra The ancient Egyptian deity of the sun
MSSA methicillin-susceptible Staphylococcus aureus
MRSA methicillin-resistant Staphylococcus aureus
VRE vancomycin resistant Enterococcus
With thanks to Advancis Medical, manufacturers of Activon Manuka Honey https://uk.advancismedical.com


14 | www.iocp.org.uk
Footnotes
Foot Health Practitioners News - Issue 10



Hi Everybody.
It’s that time of year again. The sun’s out. The temperature is rising, and people are starting to wear sandals… has anyone else noticed that at this time of year we change occupations, we lose the title Foot Health Practitioner and become Magicians!
People who have neglected their feet all winter, suddenly expect us to turn them beach ready in one treatment.

Well, we all love a challenge don’t we…. Bring them on!
Last week I went to lunch with two retired Chiropodists. We had a lovely meal, and afterwards the conversation turned to the old days, I was amazed at some of the stories they told.
At the start of the day, they were issued one scalpel. This had to be sharpened on a stone, in between customers. It was kept in a jar of disinfectant to clean it. They used the same set of instruments for all their customers, these were also kept in the same disinfectant jar. No gloves were worn. Chiropodists were targeted not only for the number of customers they saw per day, but also for the number of accessories that they sold. These ranged from creams, toe props, to shoes and stockings.
They had 20 minutes per customer to complete this. If a customer did not rebook the next appointment, they had to be able to tell the store manager the reason why not. Makes me glad to be self-employed!
If there are any old school Chiropodists, Podiatrists, or Foot Health Practitioners out there who have any stories about days gone by, I would love to hear them.
I hope you all have a fantastic summer!
Best regards, Ian.
Some Historical Mysteries of the Foot
By Beverley Wright
It is interesting that over millions of years our feet have evolved and dramatize what we see today. More than four million years ago many of our ancestors lived in or among the trees to live, hunt and gather food. Early hominis had opposable big toes, like thumbs which allowed them to grasp branches with all four limbs.
It is thought by Morton (1935) that Australopithecus afarensis, which possessed a hindlimb adapted to terrestrial bipedalism, with a rigid ankle (Latimer et al, 1987: DeSilva, 2009) and an arched, nongrasping midfoot were tree climbers like our closest relatives, the apes. Not surprisingly the biological and adaptive significance of human climbing is still possible with the evolved modern human foot. Although, as climbing goes homo sapiens are more adaptive for activities in the central core of trees. However, there are many cultures today that are still competent tree climbers, especailly vertical climbing to gather fruits and honey, and evading dangerous animals and predators.
The foot’s most important tendon is named after the Greek hero Achilles. When Achilles was a baby, his mother tried to make him invulnerable by dipping him in the river Styx. But she held him by the heels, which remained unshielded (GreekMythology.com, 2021). It was there, in the back of his foot that was hit by a lethal arrow from his enemy, Paris, during the siege of Troy (Homer, 8th or 7th BCE).
According to popular legend the practice of foot binding emerged in the 11th Century China after Empress Taki was born with club
Podiatry Review Summer Issue 2022 | 15
feet. Her father issued an edict requiring all high-class woman to bind their feet so that no-one could discriminate against her. Small feet became a status symbol, mark of beauty, and a way to marry well. For centuries, Chinese women had their feet broken and bound to make them small and known as ‘lotus feet’.
In 1902, the Empress Dowager Cixi issued an anti-foot binding edict, but it was soon rescinded. However, following the founding of the People’s Republic of China in 1949, foot binding was completely abolished, and Chinese women today do not bind their feet (Preskar, 2021).
In medieval times walking in long pointy shoes was the height of fashion. The gait was much more toe focused, where men would walk like ballerinas, touching the ground with the toes and balls of the feet instead of the today’s common gait of walking with a heel strike first. Toe walking allowed individuals to put their toes down first to feel for any obstacles such as rocks, before placing their whole weight down, to lessen the chance of injury. In addition to developing good shapely calf muscles, which could be seen under the hosiery of the times. It was also very fashionable for young men to waggle their toes as a sign of appreciation to passing ladies. An early precursor of the wolf whistle (Victoria and Albert Museum, 2015).
The sensitive soles of the feet are vulnerable to more than just tickling. One medieval torture said to be used in France involved pouring salt water over the victim’s feet and then bringing in a goat to lick the salt-water off the feet with its rough tongue (Yamey, 2001).
Jack Daniels is famous for his sour-mash whiskey and distillery in Tennessee, USA; and for the way he supposedly died. It was said that when he couldn’t remember the combination of his safe, he kicked it in frustration and broke his toe. The toe became infected and later the toe was amputated, and then his foot due to blood-poisoning. Sepsis was said to have caused his death. Ironically, if he had just doused his toe in his own whiskey, the infection might never have occurred (Freeth, 2005).
Many early religions linked the soul to the sole, Sir James George Frazer (born January 1, 1854—died May 7, 1941). British anthropologist, folklorist, and classical scholar, reported in the Golden Bough that the followers of the Greek Philosopher Pythagoras were forbidden from piercing a man’s footprint with a nail or knife.

In 1991, Louis Hollis of Compton, California, had toenails that were on average more than 6 inches long. She holds the Guinness Book of World records the combined length of all ten

toenails was 220.98 cm (87 in). It was stated in the Guinness Book of World Records (2007): “She rarely wears shoes, but when she does, they must be open-toed and have at least 7.62 cm (3 in) thick soles to prevent her nails from dragging on the ground.”
Devendra Suthar a 46-year-old carpenter from Western India, holds the Guinness Book of Records for having 14 toes and 14 fingers, more than any other living person. He was born with polydactyly, which affects around one in every 700-to-1,000 births worldwide and occurs in the womb during the sixth or seventh week of pregnancy.

Jeison Orlando Rodríguez Hernández from Maracay, Venezuela has the Guinness World Record for the biggest feet on a living person, which are US size 26 feet. The 22-year-old has a right foot measuring 40.55 cm (1.33 ft) and his left foot has reached 40.47 cm (1.32 ft). This excludes cases of elephantiasis, and giantism (Guinness Book of World Records, 2018)

Footballers tend to have many metatarsal injuries, usually fractures such as Jones and/or March fractures. The ‘Jones’ fracture is a transverse fracture of the proximal metadiaphyseal junction of the fifth metatarsal bone involving the 4th-5th metatarsal articulation. The fracture is believed to occur because of significant adduction force to the forefoot with the ankle in plantar flexion (Theodorou et al, 2003).

 By Personalo at English Wikipedia.
By Personalo at English Wikipedia.
The ‘March’ fracture was derived in 1855 because of the effects of Prussian soldiers marching. The marching often caused stress fractures affecting one or more of the metatarsals of the foot. This occurred because of overuse and repetitive actions of the feet (Van Demark and McCarthy, 1946)
The foot has been a rich source of idioms, the Free Dictionary lists more than 276 examples, from ‘Put your best foot forward’ to ‘one foot in the grave’. It’s enough to make you fall head over heels (Free Dictionary, 2003-2022).
All
the best, Beverley
Chair of Ethics and Vice-Chair of Education
16 | www.iocp.org.uk Foot
News - continued
Health Practitioners
Please see page 20 for the References for this article










 Martin, Anthony & the Graduation Group
Yvonne Nelson
PremjidClays
Martin, Anthony & the Graduation Group
Yvonne Nelson
PremjidClays
Day MARCH 2022 The podiatry instrument packs given to students are sponsored by Heeley Surgical Podiatry Review Summer Issue 2022 | 17
Heather Holder
Graduation
Congratulations!
Richard Cortis Una Ennis
PLATELET RICH PLASMA (PRP): IoCP Guidelines

What is PRP?
PRP is derived from autologous blood, with concentrations of platelets above normal baseline levels; it also contains at least 7 growth factors. Normal blood contains approximately 6% platelets, but in PRP there is a concentration of around 94%. This translates to a powerful cocktail containing cytokines and growth factors. These stimulate cellular proliferation and tissue regeneration to dramatically accelerate healing.
Platelets are derived from the patients own blood (autologous), which reduces the chances of unpleasant side effects or infection, as long as sterile techniques are maintained throughout the procedure. It is advised that antiinflammatory medications are stopped prior to treatment to enable the PRP to work to maximum effect. Also, following injection, if pain relief is required, paracetamol is recommended if it is safe for the patient to take. If there is heat or swelling, an ice pack can be used to reduce inflammation.
Although blood is mainly plasma, it also contains a number of solid components ie. Red blood cells, white blood cells and platelets. Platelets are known for their importance in blood clotting. However, platelets are also rich in growth factors, which are extremely important in the healing of injuries.
PRP is plasma containing many more platelets than are typically found in blood. The concentrations of platelets, and therefore the concentration of growth factors, can be 5-10 times greater than usual.

Growth Factors in Platelets
Platelet derived growth factor (PDGF -aa, PDGF -bb, PDGF -ab)
Stimulates cell replication
Promotes angiogenesis
Promotes epithelialisation
Promotes granulation tissue formation
Transforming Growth Factor (TGF -B1, TGF B2)
Promotes formation of extracellular matrix
Promotes bone cell metabolism
Vascular Endothelial Growth Factor (VEGF)
Promotes angiogenesis
Epidermal Growth Factors (EGF)
Promotes cell differentiation and stimulates re-epithelialisation, angiogenesis and collagenase activity
Fibroblast Growth Factor (FGF)
Promotes proliferation of endothelial cells and fibroblasts Stimulation of angiogenesis
PRP in Podiatry Practice
Pain Management
The goal of PRP in pain management is to reduce or eliminate pain through healing. The platelets in PRP release growth factors that play a vital role in bone and soft tissue trauma.
Healing Soft Tissue Injuries
PRP injection is exceptionally effective in treating acute soft tissue injuries and chronic tendinopathies, such as Achilles’ tendon repair, acute ligament injury, muscle injury, meniscal repair and intra articular tissue repair.
Orthopaedic Healing
The platelets in PRP accelerate repair and strengthen damaged tissues naturally. By invoking the patients’ inflammatory response, PRP allows healing without significant risks of surgery, such as joint replacement or other invasive procedures.
• Plantar fasciitis, sports ligament injuries
• Achilles’ tendonitis, tendinopathies, chondromalacia atellae, ankle ligament injury, cartilage damage, degenerative arthritis etc
18 | www.iocp.org.uk ARTICLE
Whole blood Constituents 93% red blood cells 6% platelets 1% White blood cells
Types of PRP Collection
1. Gel Separator System
These tubes use osmosis to insure platelet concentrate gets captured in a gel layer, separated from WBCs and RBCs. The platelet count is lower than other systems but it is the most effective way to collect plasma that has a lower leucocyte count.
2. Buffy Coat System
Kits using buffy coat trap the WBC and platelets in a layer above a separated RBC layer. It produces a high platelet count, but the buffy coat traps the WBCs and a considerable leucocyte count as well.
3. Double Spin Buffy Coat
This means of collection is better able to filter other cell types away from the final product, increasing platelet recovery. It allows for the PRP sample to consist of almost pure, concentrated platelets remaining in a plasma layer, which is easily removed from the gathered RBCs below.
Single Spin
Single spin, such as Eclipse and Regenkit, rely on a soluble polymer to stratify blood elements. The polymer has a specific density between platelets and red blood cells. Upon centrifugation, the gel polymer creates a physical barrier which isolates red blood cells, creating a serum with low haematocrit levels (0%). The complete removal of red blood cells eliminates the potential for an inflammatory response which occurs when red blood cells are introduced outside of vascular pathways. Though RBCs are successfully eliminated, these single spin kits produce a serum with a platelet concentration less than whole blood and are also known as platelet poor plasma.
Dual Spin Kits
Dual spin centrifugation kits apply radial force to stratify blood elements and concentrate platelets up to 6.7 times that of whole blood. Blood is drawn in the presence of an anticoagulant, which prevents platelet activation during the mechanical stress of centrifugation.The sample is spun according to the manufacturer’s recommendations, and the resulting supernatant is collected for a second spin. The supernatant contains plasma, platelets, WBCs and a slight collection of RBCs. The second round of centrifugation is another opportunity for platelets still suspended in plasma to fall out of solution and result in a highly concentrated PRP.
Platelet Concentrations and Patient Outcomes
Single spin kits may have the appeal of a more streamlined process. Unfortunately, the polymer at the centre of the single spin process only targets platelets of a certain density. The exact polymer utilised is unknown, but the substance possibly has a specific density just above that of red blood cells, given the very low haemaocrit levels achieved. This process, therefore, will only capture platelets which correspond to the density of the polymer, whereas platelet density falls along a whole spectrum.
Successful PRP therapy harnesses the healing capacity of platelets by recirculating the cell fragments into damage tissue. Platelets are activated in the presence of calcium. Once activated, platelets re-granulate and start to release tiny, bioactive molecules known as growth factors.
Growth factors signal surrounding cells to increase migration and proliferation.
Anticoagulants
Silva, P et al. 2016. Platelet rich plasma obtained with different anti-coagulants and their effect of platelet numbers and mesenchymal stromal cells’ behaviour in vitro. Stem Cells International Vol 2016
Silva looked at sodium citrate (SC), ethylenecliaminetetracetic acid (EDTA) and anticoagulant citrate dextrose (ACD) during the process of obtaining PRP. Their results indicated that SC produced the highest platelet recovery and minimal change in mesenchymal stromal cell gene expression.
Sodium citrate 1 part SC to 9 parts while blood eg. 1ml SC : 9mls blood ACD A ACD A can be more uncomfortable injecting back into the tissues due to its acidity. Again, the ratio is 1:9
Both SC and ACD A are citrate based and utilise the ability to chelate ionised calcium present in blood to prevent coagulation, which forms non-ionised calcium citrate complex calcium ions.
Damaged joints would appear to activate the PRP due to the exposed collagen. Clinical outcomes appear to be very similar in ACD A and SC.
Turn down – Turn up Collection vs Single Spin vs Double Spin
Machado, Z.S. et al. 2019. Turn - down, turn – up: a simple and low cost protocol for preparing PRP.Clinics 74
A very interesting piece of research comparing single spin, double spin and a new, double spin technique using ACD A vacutainers.
Results
The results were very favourable: single spin increased platelet levels to 1.17 x greater than basal concentration. Double spin produced 3.09 x greater than basal concentration
Turn down – turn up increased platelet levels 4.07 x greater than basal concentration
Turn down – Turn up Protocol
1. Collect blood – 8.5mls blood with 1.5mls ACD
2. Centrifuge 200 x g for 15mins, cap of vacutainer facing down
3. Carefully remove tube from centrifuge and maintain in cap down position without turning
4. Carefully aspirate 3.5mls of haematic layer through rubber cap
5. Turn tube to upright (cap up)
6 Centrifuge at 1600 x g for 10 minutes
7. Aspirate 3.5mls of upper portion (PPP)
8. Aspirate 1-2 mls of PRP from lower portion of tube
Podiatry Review Summer Issue 2022 | 19
Mid Wales Diary
David Holland BSc(Hons) Pod-Med, CBiol, CSci, FFPM-RCPS(Glasg).

This year we wondered where our badgers were coming from. Badger burrows, or setts, are large, untidy, and quite recognisable, and we have none locally on this side of the river, apart from the sett beside the rugby club half a mile away. To reach our path the badgers from there would have to climb steps, negotiate a secure metal gate, and walk down a pavement, which seemed unlikely. Did they swim the river? They can swim, but don’t if they don’t have to.
The answer came when I saw, at night, what I thought was a badger on a walkway on top of a pipe which crossed the river. Alan, a neighbour, put up a wildlife camera, and sure enough - the badgers were using it as a thoroughfare. One video sequence showed a badger with a vixen about 15 feet behind waiting her turn to cross!


Various neighbours leave peanuts out for the badgers, or have bird feeders which attract them. We don’t. We moved our bird feeders after badgers insisted on digging up plants under it - night after night. Nice though the badgers are (in late Spring they bring the cubs to visit) for the sake of the garden we prefer that they stay on the other side of the hedge.
Haydn Kelly is a Podiatric Surgeon and Forensic Podiatrist. His creation forensic gait analysis first became admissible as expert evidence in the UK Courts at the Old Bailey in the year 2000. His book - Forensic Gait Analysis - is well worth a read. Forensic Podiatry, which includes gait analysis but also footprint analysis, is usually applied to Criminal Law, in the identification of suspects.
I’m a Forensic Podiatrist, but in Civil Law (Clinical Negligence, Personal Injury, and HCPC Hearings), where the application of forensic analysis is less obvious, but nevertheless useful in some cases, and vital in others. The Forensic Podiatrist can identify features of gait dysfunction on CCTV. Do they match with the
REFERENCES for page 16 FHP article
DeSilva,
Gavin Yamey (2001). “Torture: European Instruments of Torture and Capital Punishment from the Middle Ages to Present”. British Medical Journal. 323 (7308): 346. doi:10.1136/bmj.323.7308.346.
GreekMythology.com, The Editors of Website. “Achilles”. GreekMythology. com Website, 08 Apr. 2021, https://www.greekmythology.com/Myths/ Heroes/Achilles/achilles.html. [Accessed 16 May 2022].
Guinness World Records. 2007-2022. Available Online: https:// www.guinnessworldrecords.com/news/2007 and https://www. guinnessworldrecords.com/news/2018. [Accessed 16 May 2022].
Homer, (eighth or seventh century BCE). Iliad 9.252–53, 11.765–70, 19.326–27, Odyssey 11.509.
Latimer, B, Ohman, JC, Lovejoy, CO. Talocrural joint in African hominoids: Implications for Australopithecus afarensis. Am J Phys Anthropol 74, 155–175 (1987).
recorded injury? In clinical examination the Forensic Podiatrist has the opportunity to see, at close hand, if the symptomology matches the pathology on which the case is based.
Also, is the Claimant being completely honest? Some years ago, Haydn and I worked on an unusual Civil Law case together - he was instructed by the Defence, I by the Claimant. The case was Personal Injury-a Road traffic accident affecting both legs. The Claimant was in his 20s, and could not walk far. I examined him. His gait and endurance-level fitted with the injuries sustained in the accident. Poor chap seemed in a bad way. Haydn had reason to believe he was lying, and covert CCTV footage was ordered by the Defence. I reviewed the CCTV footage. It showed the Claimant, after coming out of his house, looking right and left, and proceeding to walk absolutely normally, twirling his walking stick as he did so. No special training in forensic gait analysis needed to identify blatant fraud! I imagine, although I don’t know, that he was prosecuted for Contempt of Court.
Morton, D. 1935. The Human Foot. New York: Columbia University Press. Personalo at English Wikipedia, CC BY-SA 3.0. Available Online: https:// commons.wikimedia.org/w/index.php?curid=50136438
Preskar, P. The Disturbing Tradition of Foot Binding in China: Probably the most painful thing done in the name of beauty. Article. Oct 30, 2021. Available Online: https://historyofyesterday.com/foot-binding-in-china10c676470d1. [Accessed 16 May 2022].
The Free Dictionary. 2003-2022. By Farlax Incorporated. Available Online: http://www.Idioms. thefreedictionary.com. [Accessed 16 May 2022].
Theodorou D, Theodorou S, Kakitsubata Y, Botte M, Resnick D. Fractures of Proximal Portion of Fifth Metatarsal Bone: Anatomic and Imaging Evidence of a Pathogenesis of Avulsion of the Plantar Aponeurosis and the Short Peroneal Muscle Tendon. Radiology. 2003;226(3):857-65.
Van Demark RE, McCarthy PV. March fracture. Radiology. 1946;46 (5): 496501.
Victoria and Albert Museum. 2015. Available at http://www.vam.ac.uk/ museum-life/getting-to-the-point-of-medieval-shoes. [Accessed 16 May 2022].
20 | www.iocp.org.uk ARTICLE
JM. Functional morphology of the ankle and the likelihood of climbing in early hominins. Proc Natl Acad Sci USA 106, 6567–6572 (2009). Freeth, N. 2005. Made in America: from Levis to Barbie to Google. St. Paul, MN: MBI.
Essentials of Biomechanics
Principles of gait: Understand the Principles of the Acceleration Lever System
By Andy Horwood Visiting Lecturer & Fellow Staffordshire University

INTRODUCTION
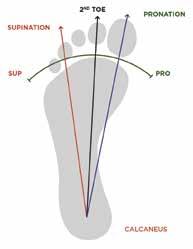
The foot must create cycles of compliance and stiffening throughout the stance phase of gait to safely manage its exposure to collision-induced energies. These forces derive from initial contact, full body weight loading, body weight transfer over the foot, and the application of acceleration power. Foot compliance allows energy dissipation (shock absorption), while stiffness permits energy storage followed by its release and application for locomotive power against the ground. Both properties require adaptable levels of elasticity to set differing foot flexibility during gait (see figure 1). Adaptability in the mechanical properties of a foot at any moment derives primarily from muscular activity and the gait speed, actions that both alter connective tissue tension and structural shape changes across the pedal anatomy. Together, these factors should set the foot up for terminal stance ankle plantarflexion power application to provide appropriate acceleration onto the next step
Figure 1: The cycles of foot compliance and stiffening occurring during stance phase are applied to impulses generated over a force-time curve. Paler areas indicating periods of compliance and darkening areas indicating increasing or decreasing stiffness across the foot vault. IHC = initial heel contact, HST = heel strike transient, IFFC = initial forefoot contact, FFL-LR = forefoot loading completed at loading response, HL = heel lift, and P-S = pre-swing. Vertical impulse peaks and troughs identified as F1, F2, and F3. Horizontal antero-posterior impulse peaks demonstrated by F4 and F5 peaks.

Image from the upcoming text ‘Origins and Principles of Clinical Biomechanics in Human Locomotion’, with permission of www.healthystep.co.uk.
The heel fat pad provides compliance at initial heel contact (IHC) during the heel strike transient (HST). Heel contact is followed by active foot stiffening across the vault (arch), which continues until initial forefoot contact (IFFC) when the foot starts to increase its compliance to dissipate the forefoot loading collision forces to the end of loading response (FFL-LR). The end of loading response creates the F1 vertical peak in vertical force as the foot reaches its foot-flat plantigrade posture. Throughout early midstance the foot remains compliant as muscle activity within the foot reduces to allow energy dissipation and increasing ground contact until the trough in vertical forces at F2. This compliance permits the foot to lengthen and widen by expressing linear-elastically during a period of lowering forces. However, towards the end of its stretching range, connective tissue becomes exponentially stiffened, thus demonstrating classic viscoelastic properties (Stolwijk et al, 2014; Bjelopetrovich and Barrios, 2016; Takabayashi et al, 2020). As late midstance progresses, the foot’s connective tissues become increasingly stiffened across the vault to a point of peak normal pronation as defined by Horwood and Chockalingam (2017), prior to heel lift (HL). The ability to create a large F3 peak of vertical force and the F5 peak of posterior force for acceleration, relies on the foot becoming a stiffened acceleration platform, thus reducing is ability to dissipate energy at the heel lift boundary. Pre-swing (P-S) is a period of increasing compliance readying the foot for swing phase. Note the F4 and F5 peaks of horizontal anteroposterior forces at the start and end of stance as the lower limb drives forces forwards into the ground, and then posteriorly into the ground behind the body.
Podiatry Review Summer Issue 2022 | 21 CPD 4 page article
Lever Systems within Human Lower Limbs
Lever systems are very simple machines that biology crudely uses to create motion at joints. They consist of point of motion (a fulcrum usually provide by a joint), a site of power application (an effort point provided by muscles), resistance (a load being moved, consisting of a certain region of body mass), and a beam (usually provided by a single long bone within land vertebrates) that is used to provide interaction between all these features (see figure 2). You will probably remember from your school days, that there are three lever systems based on where the fulcrum (pivot point), resistance (load), and effort are positioned in relation to each other. A class one system has the fulcrum in the middle, a class two has the resistance in the middle, and the class three has the effort in the middle (see figures 2, 3, and 4). The mechanical efficiency of any lever system is dictated by the distance the resistance is positioned from the fulcrum compared to the effort’s distance from the fulcrum
Figure 2: Components of a lever arm consist of a beam, a point of rotation known as the fulcrum (F), a resistance (R) being moved or resisted, and the effort (E) that apply the forces against the resistance. Each component is demonstrated here within a class two lever, where the effort is applied further away from the fulcrum than the resistance. Such an arrangement requires less effort force to move or resist the resistance force.
Image from the upcoming text ‘Origins and Principles of Clinical Biomechanics in Human Locomotion’, with permission of www.healthystep.co.uk.
A class one lever has the fulcrum in the middle, like a seesaw. This means either the effort and resistance can be the same distance from the fulcrum on opposing sides, or one can be nearer to the fulcrum than the other across the fulcrum. Whichever is further from the fulcrum has the mechanical advantage (see figure 3). Humans use crude class one lever systems around the hip concurrently with class three levers, but more for stabilisation of hip joints in the frontal plane rather than for significant sagittal plane joint motion. For large ranges of joint motion in the sagittal plane (flexions and extensions), class three levers are preferred. These place the resistance further away from the joint than the effort, so they are mechanically inefficient. The reason they are used in biology ties into concepts of muscle physiology costs. Changing muscle fibre length is metabolically expensive, especially when concentrically shortening them. Thus, reducing the amount of change necessary in muscle fibre length during locomotion overrides the mechanically efficiency of the lever system when it comes to gait energetics. Thus, applying the effort point of the quadriceps close to the knee via the patella and its tendon (ligament) means that the quadriceps only need to contract a little to create a large extension rotation of the knee that moves the foot and ankle a long way during late swing phase (see figure 4). This arrangement dramatically decreases the metabolic costs of power generation and motion, although it requires greater effort.

Figure 3: The distance that the effort (E arrows) and resistance (R) are positioned away from the fulcrum (F) affects the efficiency of a lever system. Here, within a class one lever system such as a seesaw [A], E and R can be equal distance from the fulcrum. If the effort force matches the resistance forces, the system is balance [B], but if E lies further from F than does the R [C], E has the advantage. The reverse is true in [D], where R is given the advantage by being further from F.

Image from the upcoming text ‘Origins and Principles of Clinical Biomechanics in Human Locomotion’, with permission of www.healthystep.co.uk.
The Type Two Lever Arm of Acceleration
There is only really one class two lever system used within the foot during gait (and it is arguable one). It is utilised during the action of initial heel lift. There is also another arguably class two lever system used at the hip via gluteus maximus resisting initial contact hip flexion that controls the drop of the upper body’s centre of mass (CoM) during loading response. This system also raises the CoM forwards by initiating hip extension in the sagittal plane at the start of midstance. However, it’s the one at heel lift that has the greatest influence on the foot ability to influence gait and its own healthy function.
At heel lift, effort is applied to the posterior surface of the calcaneus via the Achilles tendon enthesis. The resistance being moved is the mass of the lower limb needing to be lifted from the ground and tipped forward to follow the CoM of the, head, arms, and trunk.
22 | www.iocp.org.uk CPD 4 page article
Principles of Gait: (continued)
Figure 4: Muscle fibre length changes are metabolically expensive activities. During swing phase, tibialis anteriorinduced ankle dorsiflexion motion and large ranges of quadriceps-induced knee extension motion are achieved with only small muscle fibre length changes. This is because tendinous attachment points are located very close to the joint axis that they cross (A). If the quadriceps attached to the distal tibia (B), then extensive muscle fibre shortening would be required to bring about knee extension and such motion would be applied at a considerably slower rate.

Image from the upcoming text ‘Origins and Principles of Clinical Biomechanics in Human Locomotion’, with permission of www.healthystep.co.uk.
The trunk should already be positioned anterior to the foot before heel lift, being dragged forward behind the swing limb and falling forward under centrifugal and gravitational forces. Thus, the body’s CoM should not require heel lift power to continue to progress forwards and downwards. However, a powerful heel lift improves gait energetics.
The fulcrum at heel lift is not the ankle, for although the ankle undergoes plantarflexion motion at this time, the fulcrum point lies within the forefoot where the plantarflexion power is being applied to the ground. Ideally the fulcrum point should lie within the metatarsophalangeal (MTP) joints. Medial MTP joints make better fulcrums that lateral ones for reasons that will be discussed in later articles. If the foot functions efficiently, the resistance of the lower limb mass should lie between the effort (Achilles attachment) and the fulcrum (MTP joints), lying over the midfoot. This is much like the situation that occurs in emptying a wheelbarrow. Like a wheelbarrow (see figure 5), where the load lies within the barrow (or over the midfoot) dictates how easy it will be to tip the contents (resistance of body mass) forward over the fulcrum (MTP joins) and onto the next footstep during terminal stance. Obviously, the beam-like barrow must be ‘solid’ for the effort on the handles to move the load.
Summary
Although class three levers are preferred in biology, as they use minimal muscle fibre length changes to produce faster and greater ranges of motion for low metabolic costs, there are exceptions. These are when mechanical advantage potentially improves energetics over muscular metabolic costs because stabilisation is more important than motion, or power derives from other sources than active muscle fibre length changes. Class one levers within the lower limb are used for stabilising the hip within the frontal plane, particularly during single limb support. A biomechanically unusual class two lever system is used for heel lift at the starts of the acceleration phase of gait.
Figure 5: The classic example of a class two lever is the emptying a wheelbarrow, acting as a beam. Effort (E) is applied at the handle, the resistance (R) is within and above the barrow, and the fulcrum (F) is the wheel that is allowing the barrow to rotate. This arrangement can be used to represent the Achilles attachment as E, body mass being moved above the foot as R, with the length of the foot to the metatarsophalangeal joints providing the beam.


The metatarsophalangeal joints form the fulcrum of rotation.
The closer R (represented as the box in the lower image) is to the fulcrum (black star), and the further E is from the fulcrum the easier it is to tip the beam forward. The foot, if turned into a semistiffened beam can act as a type two lever for acceleration during heel lift, but muscular and connective tissue stiffening of the foot must occur for the foot to behave in a beam-like manner.
Image from the upcoming text ‘Origins and Principles of Clinical Biomechanics in Human Locomotion’, with permission of www.healthystep.co.uk.
This is probably possible because plantarflexion power is derived from elastic recoil from the energy stored within the Achilles tendon during late midstance, rather than via active muscular contraction within triceps surae. The lever system is debatably because it requires the foot to be semi-stiffened across the vault, which in turn necessitates activity of muscles such as tibialis posterior, peroneus longus, and other plantar extrinsic muscles and intrinsic muscles that are working on other lever systems at the same time (Ferris et al, 1995; Kokubo et al, 2012; Farris et al, 2019; 2020).
Thus, the effort required for stable, efficient heel lift involves more than the Achilles power alone.
Podiatry Review Summer Issue 2022 | 23
REFERENCES:
Bjelopetrovich A, Barrios JA. (2016). Effects of incremental ambulatory-range loading on arch height index parameters. Journal of Biomechanics. 49(14): 3555-3558.
Farris DJ, Kelly LA, Cresswell AG, Lichtwark GA. (2019). The functional importance of human foot muscles for bipedal locomotion. Proceedings of the National Academy of Sciences of the United States of America. 116(5): 1645-1650.
Farris DJ, Birch J, Kelly L. (2020). Foot stiffening during the push-off phase of human walking is linked to active muscle contraction, and not the windlass mechanism. Journal of the Royal Society: Interface. 17(168): 20200208.
Ferris L, Sharkey NA, Smith TS, Matthews DK. (1995). Influence of extrinsic plantar flexors on forefoot loading during heel rise. Foot & Ankle International. 16(8): 464-473.
Horwood AM, Chockalingam N. (2017). Defining excessive, over, or hyper-pronation: A quandary. The Foot. 31: 49-55.
Kokubo T, Hashimoto T, Nagura T, Nakamura T, Suda Y, Matsumoto H, et al. (2012). Effect of the posterior tibial and peroneus longus on the mechanical properties of the foot arch. Foot & Ankle International. 33(4): 320-325.
Stolwijk NM, Koenraadt KLM, Louwerens JWK, Grim D, Duysens J, Keijsers NLW. (2014). Foot lengthening and shortening during gait: A parameter to investigate foot function? Gait & Posture. 39(2): 773-777.
Takabayashi T, Edama M, Inai T, Nakamura E, Kubo M. (2020). Effect of gender and load conditions on foot arch height index and flexibility in Japanese youths. Journal of Foot & Ankle Surgery. 59(6): 1144-1147.

24 | www.iocp.org.uk
CPD 4 page article
Principles of Gait: (continued)
In the next issue: Essentials of Biomechanics, the complications of using the foot as a beam for a class two lever system are discussed.
Understanding the Human Foot - An illustrated Guide to Form and Function for Practitioners
 By James Earls MSc.
By James Earls MSc.
Published by Lotus Publishing, 2021. www.lotuspublishing.co.uk ISBN978-1-913088-26-2
Reviewed by Beverley Wright FInstChP, FHEA, MSc, MBA.
The author has trawled through the history of early homo sapiens and re-unearthed the origins of the anatomy of the human foot, its structure and function through its evolutionary stages.
The human foot opens a lot of intrigue and mystery, where the author makes the transition of the feet’s evolutionary history very interesting. Unlike some anatomy books that can be a mystery unto themselves, as the author remarks the frustration of not completely understanding anatomy and biomechanics from the many and various anatomy textbooks available. Luckily, this book reveals foot anatomy from the perceptions and findings of Dr Morton (1935) and the wildly held misconceptions of the ‘science story’ of the foot; to discover and comprehend the evolutionary processes of the human foot.
Fast forward a few million years, passing through evolution and the evolving foot. The shape of bone and other bone and soft tissue structures of the body that transitioned through time from our early ancestors the Australopithecus afarensis (tree climbing hominids), towards obligate bipedalism and human locomotion of the homo erectus and homo sapiens. It is hardly surprising, perhaps, that ‘each mammals foot has adapted to the ecology in which it is situated’ (p.185), which the author has eloquently stated within the pages of this exciting and informative treatise. The author manages to go deeper and deeper explaining the anatomy, foot structure, bones, soft tissues, and functions of the foot without it being a painful process for the individual to learn and understand foot and leg anatomy.
It is a complete guide to the anatomy and biomechanics of the foot. The wealth of colourful illustrations provides a deep insight, to support the evaluation and assessments of the foot. The books approach and the structure of the content is supporting the authors own learning style and the way he would have liked to have studied anatomy.
This is no dry tome; because of the inclusion of how to assess problematic structural and functional issues related to the foot and lower leg. Chapter eight is written by the author with Mark Parfitt-Jones, which draws together all the chapters on foot and leg anatomy. This provides a solid foundation for a greater understanding of the foot. The authors holistic approach considers the actions of the gait and how the bones and soft tissue elements of ligaments, extrinsic and intrinsic muscles of the foot and lower leg, have an impact on the body as a
whole. This allows for evaluation, application, and practical assessments, incorporated within this chapter.
Then chapter nine, written by Lucy Wintle, contributes an invaluable portrayal of corrective exercises for foot stabilisation, strengthening and mobilisation. Wintle’s depth of knowledge in functional anatomy, with two decades of experience in human movement; support the easily explained exercises, which are appropriately modelled and demonstrated by Wintle in the accompanying photographs.
The last chapter in this gem of a book, chapter ten’s ‘Designed for Life’, is dedicated to the shoes we wear that encompass the feet for the rituals of fashion, protection, running, and walking, etc. The importance of understanding footwear, the shoes anatomy, and right fit for the feet, including shoe lacing for the various foot types.
This book with over 130 references and other resources, describes in detail the wealth of information that has contributed to this treatise of anatomy and human locomotion. Overall, this is an excellent textbook, well written and easy to understand. It will certainly further health professionals, practitioners, and therapists’ knowledge and understanding of the anatomy and biomechanics of the foot. This paperback book can be found much cheaper online with the Kindle version also available, along with other books by the author.
AUTHORS PROFILE
JAMES EARLS, MSc., is a writer, lecturer, and bodywork practitioner specializing in functional movement and structural integration. He is the director of Born to Move, an education platform teaching real-life anatomy for movement and manual therapists, and he is popular presenter at conferences and workshops around the world.
Earls is the co-author, with Thomas Myers, of Fascial Release for Structural Balance and Born to Walk. He also writes regularly for professional magazines and journals; and has collaborated with many authors in the production of their titles.
Podiatry Review Summer Issue 2022 | 25
RRP £21.99 Paperback
James Earle has rendered an invaluable service with this superb book which should be essential reading for health professionals, practitioners, and therapists. I cannot recommend this highly enough.
CPD Thoughts: Whose responsibility is it?
Gary Strong MCPara, National CPD Lead, College of Paramedics, Chair of the CPD Together Group.

Stephanie Tempest Independent Consultant, Project Administrator for the CPD Together Group.

Last year, the College of Paramedics asked its members a question about continuing professional development (CPD): ‘Should the CPD you undertake be your responsibility, your employer’s responsibility or a mixture of you and your employer?’

At first glance, it might appear that the answer would be obvious. As we know, all regulated health and care professionals in the UK are accountable as individuals, one way or another, for their own CPD. The Health and Care Professions Council (HCPC) asks for evidence at the point of renewal of registration. The Nursing and Midwifery Council asks for evidence in support of revalidation. The General Medical Council requires evidence of regular CPD and reflection on learning. Why should paramedics be any different to anyone else? For all this, the range of responses to our question confirmed to us that there was indeed a variety of opinions within the profession.
Overall, 181 College members responded to the survey. For all the regulatory emphasis on individual accountability, over half of the respondents (n = 106) stated that CPD is a shared responsibility between the registrant and the employer. As the survey gathered qualitative rather than quantitative data, this gave members room to expand further, for example: ‘mixture of both but I think employers should provide regular training for staff within their role to ensure competencies are kept up; ‘mine to ensure I am compliant with HCPC, my employers to ensure they get the best out of me’. Just 28 respondents stated that CPD was solely their responsibility, and even here some pointed to the need for employers to provide support, in particular time, to engage in CPD activities.
The finding from the question within our paramedic community, that CPD is a shared responsibility, is an opinion broadly held across a wide range of health and care professions. Paramedics are not unique in viewing and seeking a more balanced and collaborative approach to CPD. Since 2018, the College has led work with around 20 different professions and trade unions to define and promote the importance of and responsibility for CPD at an individual level, by employers and the wider systems of policy makers, professional bodies and commissioners. The Principles for continuing professional development and lifelong learning in health and social care, known now by its shortened name CPD Together, set out five principles for CPD (see figure one), each of which can and should be understood and applied by health and care workers and their employees, and those who lead the commissioning and development of health and care services.
Figure one: the five principles for continuing professional development and lifelong learning in health and social care
Each of the five principles has a set of targeted statements focusing on the contributions of the individual registrant, the employer, and the wider system (see figure two for an example)

Figure two: An example of Principle 3 and the statements for the individual, the employer, and the wider system.

26 | www.iocp.org.uk ARTICLE
Dr
One strength of the CPD Together resource is the number of professions who contributed to and subsequently endorsed the messages, showing a strength of opinion in the need to understand CPD as a shared responsibility. Of equal, if not greater importance is the need to reinforce that CPD plays a vital role in supporting safe and effective practice, as learning must be of benefit to service users and/or improve the quality of service delivery.
Service pressures in and around the NHS and social care make it challenging for a new resource to be promoted effectively and gain acceptance. Yet three years after the initial publication, the multi-professional group that produced CPD Together remain as passionate as ever about the importance of access to and support for high quality CPD. Therefore, work has begun to refresh the look and feel of the resource, to provide supporting resources to promote its value and to engage in new conversations, like this one, to raise awareness of the CPD principles.
Our hope is that you will use the resource as an individual registrant e.g., in appraisals, supervision and when planning your own learning. We hope it will help you in discussions with your employer, or as an employer, to highlight the importance of continuing to develop as a professional. And we hope it places learning and development at the centre of the discussions on safe and effective practice.
Equally our desire is for a clear understanding of the importance of CPD to be accepted and built into policy by employers and higher-level decision makers. Commissioning of services must take into account the need for employees to be fit for the purpose for which they are employed, and that means they will need time and support for effective CPD which improves patient outcomes and enhances patient safety.

NHS employees can access CPD Together on the NHS Learning Hub https://learninghub.nhs.uk

Podiatry Review Summer Issue 2022 | 27

The Institute of Chiropodists and Podiatrists are proud to offer our members comprehensive, market leading support and unrivalled insurance packages, tailored to suit your needs! Including insurance to colleagues in the Republic of Ireland, we’ll never leave you stranded!
•
• Network through local member branches, situated throughout the United Kingdom and the Republic of Ireland for peer support and CPD events

• Access our confidential advice service, including advice from the IOCP medicines and procedures panel (MaPP) on the use of drugs and therapeutics as well as appropriate podiatric procedures.
Head to our website: www.iocp.org.uk or contact our team: info@iocp.org.uk
We’ve teamed up with Community, a modern trade union you can choose to opt into! Offering additional industry support, advice, and training.
Members also receive discounted rates on health plans from the Health and Medical Care Association (HMCA)

our
podiatry
member Run by members for the members! We are a truly democratic organisation where your voice is heard. We strongly believe in working together to build a stronger future for podiatry
Support
Join
growing
familybecome a
• Quarterly issues of Podiatry Review, contributing to your Professional Development
• Continuing Professional Development Support – Guidance and assistance with the members continuing professional development portfolio for HCPC audits & 20% discount on Elsevier academic books
• Business Support and special discounts from our trade and advice partners
• Access to the members area of the Institute website including a private discussion forum
• Member rates on all our CPD courses and access to our free CPD webinars!
Join the IOCP ‘Find a practitioner’ service to promote your business to members of the public finding the IOCP website through search engines.
PLUS… Podiatry Review Summer Issue 2022 | 29
Part 2 - The Foot
By Gary Ward Founder of Anatomy in Motion
AAnatomy in Motion (AiM) has allowed us to study the human foot in motion and connect it to the rest of the body. AiM has been expressed by many as breaking the mould of anatomical thinking by offering an alternative perspective and this, together with its key principles and laws of motion, was discussed in the previous article.
We now move on to AiM’s approach to observation of the foot, which will help simplify and enhance the understanding of biomechanics.
AiM adopts a structural approach where we choose to work on the structure and organisation of the bones and joints regardless of the symptoms. Pain symptoms will not normally be able to exist where optimal movement is present (e.g. if your pelvis is level and has optimum movement, lower back pain symptoms will not occur.)

This contrasts to other approaches to studying and treating anatomy, such as: Symptom based approach where solutions are provided for certain symptoms
Open chain (non-weight bearing) observations – i.e. assessing the patient whilst they are sitting in the chair in front of you.
Closed chain (weight bearing) observations - i.e looking at a patient in gait and stance positions.
Open chain and closed chain observations can show different ranges of motion, leading to confusion in how well structures are moving. AiM considers both aspects and any mixed messages become crystal clear when considering both isolated and integrated movement, for example when assessing a patient with hallux limitus.
This article will explore AiM’s approach to assessing pronation and supination and explain the dynamic potential between these two resting positions.
Key Principles
The foot has 26 bones and 33 joints all capable of moving in three dimensions. In order to maximise this potential, each joint must play its role in moving into a pronation and a supination shape. There are some key considerations when observing the foot in the closed chain to identify if it is a real possibility to achieve this optimal movement.
The Human Foot is a Tripod
The body can be viewed as being made up of a number of triangles and tripods. This can be seen in multiple relationships between bones, muscle and tendon shapes throughout the body. This occurs because the triangle is the most stable structure to achieve balance in nature.
The tripod of the foot creates a stable base for us to stand upon and is marked by three specific bones on the sole the calcaneus, the first metatarsal head and the fifth metatarsal head.
Without all three points at the base of this tripod being in contact with the ground, achieving a neutral foot is impossible.
In the absence of pressure in the first or fifth metatarsal head we can assume that pressure resides under the more central metatarsal heads, second and fourth (blue crosses

in the diagram) or (in the case of the first metatarsal) under the hallux. Clinical indicator: excessive points of callus around other metatarsal heads. Any such adjustment away from the optimal three points of contact is limiting to the foot’s movement potential and the patient will no longer be able to create the conditions required to pronate or supinate all of the bones in the foot.
An optimal tripod creates not only a stable base to stand on but also a broader pathway for the Centre of Pressure to pass through when we walk.
The less optimal the tripod, the narrower this pathway. This compromises the foot’s movement and subsequently the movement of the body as it passes up through the kinetic chain. Plantar pressure in stance and gait are therefore important not just to the foot but a crucial indicator of the whole body’s movement potential.
30 | www.iocp.org.uk ARTICLE
T T
Pronation and supination
Pronation and supination are the culminations of movement in three planes of motion (sagittal, frontal and transverse). Pronation occurs to lower the arches of the foot and create what is known as a mobile adaptor while supination forms a rigid lever as a result of the arches increasing in height.
Optimal movement of the foot is attained through the ability to both effectively pronate and supinate a foot. Pronation is therefore a critical and necessary part of the foot’s motion and without it a foot is unable to find its optimal rest position. Unfortunately, pronation has a bad reputation due to the tension it places in the system and the valgus alignment it inflicts upon the body. However, it’s important to state that only a foot that is stuck in pronation and unable to get out of it will suffer as a result of this tension. A foot that knows how to pronate and how to supinate out of that pronated position into a full rigid lever is in essence a healthy foot.
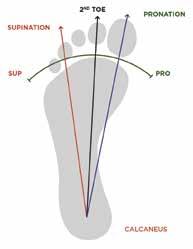
Three arches
TThe foot has three arches: the medial longitudinal arch (MLA), the lateral longitudinal arch (LLA) and the transverse arch (TA). The MLA is often used to assess a foot’s resting state and is the one most commonly referred to as the foot’s ‘arch’. Whilst we are often encouraged to view higher arches as superior, it is possible that a foot with a lower arch can still have the potential to move well. It is also possible for a high arched foot to be limited in range and this ultimately can be a problem for the body as a whole, for instance a cavoid foot.
One key piece of appreciation for the arches is that in a healthy moving foot, all three arches rise and fall together.
When the foot has access to its tripod and the three arches lower together, the foot bones are able to move into a pronation. Then when the three arches rise together, the foot bones are able to move into a supination.
When movement is compromised, medial pressure is exerted on the foot rather than nicely distributed between the three key points of contact.
A simple assessment to see if the foot is using its tripod properly:
When weight bearing, check to see if pressure is present under the first and fifth metatarsals by attempting to lift them off the ground
For example, in a healthy moving foot, never would the LLA rise as the MLA falls, as contact on the 5th metatarsal head would be lost. Clinical indicator: Excessive pressure/callus under the 1st MTPJ Likewise, when the first metatarsal is not in contact with the ground, sufficient plantarflexion of the first ray is compromised and a true supination cannot be achieved.
Clinical indicator: Hallux limitus / Hallux abducto-valgus (HAV)
Keystones
Like a roman arch, each of our three arches in the foot has a keystone and each keystone can be viewed as forming a triangle with each end of its arch. Its movement has a direct influence on the rest of the foot.
These three bones (talus, cuboid and second cuneiform) are useful to observe as the keystone’s position at rest or in motion is useful for determining its role in supporting the movement potential of the foot.
Talus
Observation of the talus can be utilised to quickly determine the resting state of the rearfoot. It’s the bone that connects the foot to the rest of the body.
In neutral it would ‘look along’ the line of the second metatarsal. When pronating it would rotate medially to the second metatarsal and when supinated it would rotate laterally toward the outer toes. It may also be everted at rest.
Cuboid
Narrower at the bottom than the top, the cuboid forms the central bone in the LLA and lateral border of the foot. It articulates between the calcaneus bone and the fifth metatarsal bone and performs a roll like action, flattening in a pronation and standing up tall “like a wall” in supination. Clinical indicator for restricted cuboid: Pain on the styloid process.
2nd Cuneiform
The second cuneiform sits in the middle of the foot at the top of the TA. Its triangular shape enables the narrowing of the foot as the foot supinates. During pronation the second cuneiform travels anterior and medially in space as it lowers to the floor and during supination it travels posterior and lateral in space as it rises upwards.
Bringing all of this together, if for example you see a resting foot that has a talus that is internally rotated, a cuboid that lies flat and a second cuneiform that lies anterior and medial to its neutral position you can see that it is pronated rather than in a neutral position. The more rigid a foot is whilst at rest, the less chance of achieving the necessary movements there are. The arch remains low, the tripod is compromised, tissues remain long and the potential for subsequent movement up the chain is limited. Clinical indicators of tissue stress: plantar fasciitis, morton’s neuroma, medial compartment syndrome, tibialis posterior dysfunction.
L
P Podiatry Review Summer Issue 2022 | 31
Finding centre in the foot
Centre is about the brain finding a rest position that allows movement equally in both directions. It is different to neutral as it implies the capacity to move to either side. It will vary from patient to patient (and over time) with true centre being the centre for a foot with optimised movement to both pronation and supination.
Any structure in the body, including the foot, must have an experience of its end ranges in order to find a central resting point between the two. Managed by the brain, the position of centre is chosen based on the bone, joint, muscle or structure’s experience of the edge of its movement potential.


True centre in the foot is only achievable when the tripod is optimised and the keystones are in the correct neutral position.
It is the experience of both pronation and supination that enables us to determine where our own centre is.
Treatment that allows the foot to access new joint motion will allow the brain to choose a new centre,
Sagittal plane foot motion (side view)
resulting in a change in resting muscle length. Even the most rigid of feet will have the potential to access new joint motion.
It’s important to recognise for example that a right rotated pelvis impacts the centre of each foot pronating the left foot and supinating the right foot (or presenting less pronated than the left).
Rearfoot, Forefoot and Phalanges
TThe next stage in using AiM to understand the motion of the foot and identify any restrictions is to use its Flow Motion ModelTM (FMM) to assess the foot in all three planes.
Within the FMM, the foot is divided into three sections, the rearfoot, the forefoot and the phalanges. The rearfoot includes the calcaneus and the talus, whilst the forefoot includes the midtarsal bones (excluding the cuboid) and the five long metatarsal bones.
To observe these sections, we break them down plane by plane. By understanding what should happen, we can then identify any restrictions in movement.
Pronation Supination
• The Calcaneus tilts forwards with the pressure moving anteriorly under the heel bone plantarflexion of the rearfoot bones.
• The lowering of the arch is representative of a forefoot dorsiflexion.
• As the rearfoot plantarflexes and the forefoot dorsiflexes, all three arches lower together.
• The second cuneiform is guided anteriorly.
• The articulation of the dorsiflexing metatarsals is to slide upwards inside the metatarsal phalangeal joints (MTPJ) and create a plantarflexion of the toes.
• This plantarflexion of the phalanges is insufficient for them to press down into the floor and lift the met heads up thus promoting the tripod.
The outcome of motion is that:
• The bones begin to open the joint spaces on the plantar surface.
• The foot becomes longer as where joints open, muscles lengthen.
• As the muscles contract from their lengthened position, the direction of movement in the bones is reversed.
• The plantar tissues pull the calcaneus toward the toes and the metatarsal heads back towards the heel bone causing a dorsiflexion of the rearfoot and a plantarflexion of the forefoot as the arch rises upwards, shortening the foot.
• The second cuneiform is guided posteriorly.
• This enables the distal part of the forefoot at the metatarsal heads to lower firmly into the ground, thus maintaining grounded contact of the tripod.
• The toes respond to the plantarflexing forefoot as the metatarsals slide downwards in the MTPJ facilitating a dorsiflexion of the toe.
• The result is an increase in arch height and a shorter rigid foot.
The outcome of motion is that:
• The bones begin to close the joint spaces on the plantar surface
• The foot becomes shorter as where joints close, muscles are contracting.
The act of lowering the arches is priming the tissue for contraction from an eccentrically loaded position in order to contract or spring back in the opposite supinatory direction. The resultant increase in arch height from the tissue contraction and closing of the joint spaces builds to create a full supination and the rigid lever that is used for optimum propulsion.
32 | www.iocp.org.uk ARTICLE (continued)
C
Pronation S plane Supination S plane Rearfoot Forefoot Phalanges Pronation PFX DFX PFX Supination DFX PFX DFX
Frontal plane foot motion (front view)
Pronation Supination
• The calcaneus tilts medially into eversion and encourages the pressure in the rearfoot to travel medial.
• Both the talus and the calcaneus move in the same direction of eversion, however the talus bone everts to a lesser degree than the calcaneus.
• The cuboid everts and flattens along with the calcaneal eversion.
• To avoid losing fifth metatarsal head contact as the weightbearing rearfoot everts, a forefoot inversion must occur to maintain the tripod.
• The inverted forefoot is akin to a varus forefoot which will look like a flat foot when placed on the floor.
• The phalanges move oppositely to the forefoot, enabling the nail bed to keep facing upwards to the sky and minimise frontal plane roll.
• Contraction of muscles such as posterior tibialis and soleus draws pressure to the lateral side of the calcaneus and inverts the rearfoot.
• The calcaneal inversion pushes the talus back up toward neutral and beyond.
• The cuboid inverts to stand “tall like a wall”.
• To avoid losing first metatarsal head contact as the rearfoot inverts, the forefoot must evert to maintain this critical contact point.
• The everted forefoot is akin to a valgus forefoot which forms a supinated foot when placed on the floor.
• The phalanges move oppositely to the forefoot, enabling the nail bed to keep facing upwards to the sky and minimise frontal plane roll.
Rearfoot eversion coupled with forefoot inversion with the tripod on the ground describes how the foot pronates in the frontal plane. The pronating foot is known as a mobile adaptor and you will notice how the foot spreads through the transverse arch.
Once again the lowering of the TA and the spreading of the forefoot is adding length to multiple tissues in the foot such as tibialis posterior, tibialis anterior, FHL and adductor hallucis. These tissues are then primed for contraction (you may recall AiM’s rule that muscles lengthen before they contract). The subsequent contraction is again to create the opposite shape in the foot. The outcome of this action raises the arches, coupled with the forefoot plantarflexion and forms the rigid lever as the foot shortens and narrows in supination.

Transverse plane foot motion (Top down view)
Pronation Supination
• The calcaneus internally rotates as the pressures move anterior and medial.
• The talus is guided forward and medially into the concave receptacle of the navicular bone and begins its internal rotation.
• The second cuneiform is guided medially
• Rear foot internal rotation (adduction) is met with forefoot abduction (external rotation) as the joints along the medial border of the foot are encouraged to open.
• Joints open on the medial border and close on the lateral border.
• The toes follow the forefoot as they rest on the ground fulfilling their role in the tripod.
• Contraction of muscles such as posterior tibialis and soleus draws pressure to the lateral side of the calcaneus and inverts the rearfoot.
• The calcaneal inversion pushes the talus back up toward neutral and beyond.
• The cuboid inverts to stand “tall like a wall”.
• To avoid losing first metatarsal head contact as the rearfoot inverts, the forefoot must evert to maintain this critical contact point.
• The everted forefoot is akin to a valgus forefoot which forms a supinated foot when placed on the floor.
• The phalanges move oppositely to the forefoot, enabling the nail bed to keep facing upwards to the sky and minimise frontal plane roll.
Forefoot Phalanges
AiM describes the talus as “The driver of the Bus” as it acts as a steering wheel in the transverse plane. The talus bone rotates internally and externally and has a knock on effect on the foot, the tibia and fibula and the rest of the body. Foot T plane
Tissues such as FHL, Flexor Hallucis Brevis and Extensor Hallucis Longus that run along the medial border are all lengthened in a pronation and contract back from their lengthened position to generate a supination in the transverse plane. The outcome of the supination is to close the joints on the medial border and facilitate an external rotation of the rearfoot and the leg to activate the extensor chain in the body.

Podiatry Review Summer Issue 2022 | 33
Pronation F plane
Rearfoot Forefoot Phalanges
Pronation EV INV EV
Supination INV EV INV
T-Plane Rearfoot
Pronation IR ABD Follows Forefoot ABD Supination XR ADD Follows
ADD
Forefoot
PRONATION SUPINATION
Rearfoot PFX EV IR DFX INV XR
Forefoot DFX INV ABD PFX EV ADD
Phalanges PFX EV ABD DFX INV ADD
Movement solutions
TThe AiM wedges were originally based on the concepts used when making orthotics; the orthotics original purpose was to help the foot gain access to a neutral position on its tripod.
The AiM methodology seeks to re-educate the foot to re-experience any of the joint motions detailed above that are absent from its day to day function while also encouraging access to the tripod on the ground.
To do this they use specifically designed wedges: to influence the bones in a direction of motion (eversion, inversion etc) to bring the ground up toward the first and fifth metatarsals in the absence of contact; and to relax the tissues and create the opportunity for new joint motion.
Increasing the foot’s contact area and directly influencing the foot’s motion in such a way encourages bones to move into positions they couldn’t previously access. This in turn enables the brain to establish a new centre in the foot, reorganising its resting position and dynamic potential.
Two foot shapes
There are only two optimal foot shapes that the foot should be able to access:
Pronation shape – mobile adaptor
· Foot lengthens and widens.
· Joints gap on the medial border and the plantar surface. Supination shape – Rigid Lever Foot shorted and narrows.
· Joints gap on the lateral border and dorsal surface.
Bringing this all together with a specific example, you will recall that the three keystones represent pivotal points in the three arches and together their resting position can be seen to determine the foot’s resting posture.
When the talus is internal, the cuboid lies flat and the second cuneiform is anterior and medial. The foot will be flatter and appear pronated. It will have limited access into further pronation and also into supination with reduced overall movement potential. This foot will not be in true pronation when you assess it in all three planes. Joints will be open on the base and along the medial border. There may be some compromise to some of the other joints, the whole foot may be everted (no opposition between forefoot and rearfoot) and the tripod sub-optimal.
To help rectify this, we need the talus to externally rotate back to centre, the cuboid to stand tall “like a wall” and the second cuneiform to travel in a posterior lateral direction. Together, this involves a supinatory motion requiring the muscles we have discussed to contract from their lengthen pronated state).
If muscles lengthen BEFORE they contract, in order to generate an unconscious supination in the foot, we need to first teach the flat foot to pronate well.

The wedges provide the tripod contact necessary to guide bones in the appropriate direction whilst weight bearing. This action of guiding the joints into pronation triggers a muscular response (Joints ACT: Muscles REACT). In particular, triggering an eccentric lengthening in the muscles required for foot supination.
The AIM wedges were originally based on the concepts used when making orthotics; the orthotics original purpose was to help the foot gain access to a neutral position on its tripod.
In essence, appropriate use of the wedges gives permission to the foot to move again. With a wider base: the foot is able to access more movement at individual joint there is an increased amount of opposition between the rearfoot and forefoot structures; and there is more awareness in the ligaments and tendons that span these joints, with a critical response in the soft tissue to the movement.
This experience of new movement is important to the body and brain’s perception of itself and is critical for its future progression.
Conclusion
In the first article a couple of AiM’s key rules were highlighted: ‘Muscles lengthen before they contract’ and ‘Joints ACT: muscles REACT’. We can now see how these rules play out in the foot. Additionally, there is a third key rule – “Everything orbits around centre”, the underlying concepts of which I touched on earlier.
Due to the corrected nature of the movement, all bones now enter their end range in three dimensions simultaneously and all of the tissues experience maximal length before contracting back from this lengthened position to form a supination and guiding the keystones back towards their neutral position. This lifts all three arches together while maintaining the tripod on the ground.
Once this has been established and the foot has more integrity on its tripod and more access to its movement, it is then possible to complete the experience of teaching the foot how to fully pronate and supinate, thus allowing it to reorganise itself into a new centre.
The interesting thing about working with a foot when weight-bearing is that you instantly get to see the knock on effect of movement in the foot throughout the kinetic chain. If two feet are not able to function the same, there will be structural adaptations throughout the body and the tension and compression changes that occur throughout the system are a hotbed for the provision of symptomatic problems.
The next article will discuss the knock on effect of the foot’s available motion to the rest of the body, how it influenced the development of the Flow Motion ModelTM and how, by using structure, AiM provides answers to the many symptoms we are confronted with in clinic every day.
I
S-Plane F-plane T-Plane S-plane F-plane T-plane
34 | www.iocp.org.uk ARTICLE (continued)
Bilateral forefoot tripod
The International Podiatry Pilot Programme
Podiatry International Update, interview with Gabrielle Choucri

Who are We?
Health Education England (HEE) exists to support the delivery of excellent healthcare and health improvement to the patients and public of England. They ensure the workforce of today and tomorrow has the right skills, values, and behaviours at the right time and right place. An essential element of this is to ensure an effective supply of AHP’s, supporting robust deployment and development of staff, whilst supporting retention across professions and geography. (This paragraph is taken from: www.hee.nhs.uk/our-work/ allied- health-professions/increase-capacity/ supporting- international-recruitment)
The Directorate of Global Health Partnerships (DGHP) within HEE has significant experience in the development of ethical International migratory pathways, most notably developing a highly successful model for the international recruitment of Registered Nurses which saw over 2,000 nurses joining the English NHS. International recruitment creates a rich, diverse, cultural and knowledge exchange-greatly benefitting the NHS workforce and local communities.
• Predicted Podiatry vacancies in 2025 would be double that of 2018-19- an increase from 7.0% to 14.8% (Unpublished data by Health Education England, HEE and NHS England and NHS Improvement, NHSEI)
• Supply and demand gap of over 1,000 vacancies by 2025 (Unpublished data)
• Multifactorial reasons: High retirement rates, low attrition, preference of Private practice over NHS? The Podiatry degree NO longer being fully NHS funded could have also caused a dip in the number of applicants. (However, there are now bursaries which may have improved application numbers).
• Of the 186 Podiatry graduates for the year 2020, less than half went on to work in the NHS (taken from Health Education England, Student Data Collection Dataset, June 2020 (unpublished).
There are initiatives that attempt to save the profession, including raising the professional profile of Podiatry which has been an ongoing theme in the Podiatry world. Podiatry contacts in Canada and
Australia strive to push the elevation of podiatry as a profession, by creating awareness about the Podiatrists skillset, to create awareness globally but also for the younger minds at school age, so that people know what Podiatry is alongside ‘being a vet, or a doctor’ and the great and varied career it can span and opportunities it could provide.
(The following journal backs up the workforce shortage for Podiatry:
https://jfootankleres.biomedcentral.com/ articles/10.1186/s13047-021-00470-y)
Initiatives in the UK?
• Return to work schemes
• Retention of existing staff- expanding scope of practice/creation of positions
• Apprenticeships with Universities and local NHS Trusts
• First contact point initiative within GP surgeries
• The Podiatry Career Framework
Despite these initiatives, there are still predicted gaps in years to come.
The quest to explore International waters: What did we do?
HEE, drawing on the expertise and with the support of numerous Podiatry professionals, including the Institute of Chiropodists & Podiatrists, the DVLA, the Health and Care Professionals Council and the Home office (Visa and & Immigration) studied global markets and international Higher Education Institutions to map educational standards and outcomes for podiatry against UK standards/ requirements. This step was fundamental for the successful and ethical selection of an international partner. (Choucri,2022)
Opportunities found?
As you may have guessed- the podiatry profession globally, is small, niche, complex but rich in potential and determination to succeed and remain strong. Countries still battle for official degree titles and scope of practice, causing complications, and therefore HCPC accreditation would not be possible, therefore they would not be able to legally practice here in the UK. Some countries have very low student numbers entering programmes and graduating; meaning it would be unethical to build migratory pathways with them.
However, here is what Spain could offer:
• 15 Spanish Universities provide 4-year Podiatry degrees similar to the UK. (HCPC have a record of accrediting Spanish Podiatrists)
• Over 600 Podiatry graduates in the year 2020
• Not an abundance of Podiatry job opportunities /full time work. Many graduates work in jobs that are not Podiatry, or are offered only a few days clinical work per week.
• There is no public health service provision of Podiatry in Spain, therefore the pilot programme would not drain Spain of much needed professionals.
• NHS experience and opportunities are attractive as they are rare in Spain.
• Upon returning to home country - the candidates will be able to provide enhanced, once in a lifetime gained experience, to deliver exceptional standard of care in their communities. (Spain are trying to implement Podiatry in their public health service)
• Ethical assurance: There is an oversupply of Podiatrists (that is, that Spain, trains more Podiatrists than their domestic services require)
The Proposal
From the research gathered to date, HEE was able to propose a pilot study, partnering with Spanish universities and their Spanish Podiatry governing body (Consejo General de Colegios Oficiales de Podólogos). The pilot study aims to: Recruit Newly Qualified Podiatrists from Spain into pre-agreed NHS Podiatry Trusts. Recruits will be employed initially on a 3-year contract, with sponsorship for a 3-year Tier II UK Visa provided by the employing Podiatry Trust. At the end of the initial 3-year contract the NHS Podiatry Trust will be able to offer a contract extension and Visa sponsorship extension if desired by both the Trust and the Podiatrist. (Choucri,2022)
NHS Trusts were invited to bid, detailing their workforce needs, experience of International recruitment, pastoral support, and information about their local areas and teams. Candidates were invited to apply and choose a preferred region including options of city/rural/seaside areas.
The pilot will be fully evaluated, and a report shared with stakeholders on completion. The evaluation report will include recommendations made for future recruitment practice and potential rollout.
Further details will be in the next issue!
Podiatry Review Summer Issue 2022 | 35
But wait - Why are we doing this? Here are the stats!
COVID Toes – An Update
Iain B Mcintosh
BA(Hons) MBChB, DGMRCP.MSSCh Former Chiropody Schools Inspector
SummaryDoctors and podiatrists were puzzled at the start of the pandemic when people began reporting swelling and redness of feet, which were often chilblain-like lesions, with the condition sometimes lasting for months. The condition remains controversial despite further research into the cause and effect with further evidence of causation required from larger studies. Patient history enquiries into changed footwear and behaviour during the pandemic and particularly during lockdown and quarantine are required. Identifying environmental and behavioural factors may direct treatment to conventional chilblain management, concentrating on advice and prevention rather than covid causation.
Chilblains form after intermittent or prolonged exposure to cold or damp air. The coldness causes blood vessels near the skin surface to constrict leading to decreased oxygenation and inflammation in those exposed areas. “COVID toe” was thought to be a side effect of the body switching into attack mode to fight off the virus with the immune system overreacting in its response. Lesions occur at any age, but affect children and teenagers more commonly. For some it is painless, but the rash can be extremely sore and itchy, with tender blisters and swelling.

A range of cutaneous manifestations have been described in association with SARS-CoV-2 infection during the COVID-19 pandemic [1]. Among them, chilblain-like lesions (CLL) have been occurring more frequently than expected. However, the link between SARS-CoV-2 infection and CLL is not well established. SARS-CoV-2 infection strongly triggers the expression of type
I interferon (IFN)-stimulated genes, which assist in the host’s antiviral protection. Diseases mediated by type I IFN, such as monogenic autoinflammatory interferonopathies or lupus erythematosus, are characterized by micro-angiopathy leading to clinical chilblains. SARS-CoV-2 infection seems to be associated with vascular skin symptoms and has been shown to damage capillary endothelium and disrupt the thrombo-protective state of endothelial cells, likely contributing to microvascular thrombosis. Moreover, the histopathological features of COVID-19-associated CLL include endothelial damage and features of micro-angiopathic damage [2-8]
An observational study was conducted during April 2020 in France.1 All patients referred with CLL seen during this period of the COVID-19 pandemic were included except patients with a history of chilblains or chilblain lupus. to study skin, blood endothelial and immune system activation in CLL in comparison with healthy controls and seasonal chilblains, excluding chilblain lupus. Researchers pinpointed the parts of the immune system that appear to be involved. Findings, reported an activation loop in the skin associated with endothelial alteration and immune infiltration of cytotoxic and type I IFN-polarized cells, leading to clinical manifestations. The conclusion was that chilblain-like lesions are characterized by immune cytotoxic infiltration, interferon polarization and endothelial alteration in the skin.
During the pandemic many often observational reports have offered circumstantial evidence pointing toward an association with SARS-CoV-2 infection, although the immunological and PCR data have been more limited, with only the minority of cases having
evidence of infection [1,4–8] and some studies having none whatsoever [2, 3]. Anecdotally, post pandemic cases are being diagnosed and managed differently from idiopathic chilblains due to this presumed relationship with SARSCoV-2.
Chilblain diagnoses have increased during the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) pandemic and attributed to viral infection and a subsequent robust antiviral immune response. As a result, providers have managed cases differently than idiopathic chilblains, which are associated with cold exposure. The relationship between pandemic chilblains and SARS-CoV-2 infection, however, remains unclear as most patients do not test positive for SARS-CoV-2–specific PCR or antibodies [2].
Recent research evidence from Yale University does not support the assumption that covid is a cause of increased chilblain-like lesions [9]. In this study, there was evidence of prior SARS-CoV-2 infection in the cohort with a temporal association in local infection rate and the co-occurrence of cases from the same household, as well as a substantial fraction reporting exposure (35%) to infected individuals and symptoms indicative of infection (35%). However, only (9.5%) patients with chilblain eruptions had evidence of a prior SARS-CoV-2 infection. None of the cases within households had evidence of infection. This number approximates to the regional seroprevalence of SARS-CoV-2 at the time (8.5%), indicating that this outcome could have been expected by chance. In this detailed study of a cohort of patients with chilblain eruptions presumed to be caused by SARS-CoV-2, researchers did not find evidence supporting an association with prior infection [2]
36 | www.iocp.org.uk ARTICLE
Their hypothesis was that an immune response from an abortive infection could not rule out covid, but other explanations of how the pandemic could have triggered the rise in cases should be considered in diagnosis. They suggested that people were not wearing socks and shoes when confined to the home during lockdown and when working from home. Once “covert toes” became a well-known phenomenon, people may have erroneously begun to attribute their chilblains to the condition. They postulated the increased incidence was attributable to altered behaviour during the pandemic with people not wearing socks or shoes at home during quarantine and pandemic restrictions. Home behaviour has changed remarkably since 2020 with the discarding of office clothing-wear and this may have extended to shoe and sock allegiance and closer proximity to radiator or fire encouraging chilblain appearance. This was a small study and further research with replication is needed to lend further support to the data. During the coronavirus disease pandemic, dermatologists observed an increase in pernio-like acral eruptions. Direct causality of pernio due to COVID-19 was not established in many cases because of inconsistent testing methods (often negative results) for severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). However, a form of COVID-19?associated pernio is probable because of increased
occurrence, frequently in young patients with no cold exposure or a history of pernio, and reports of skin biopsies with positive SARS-CoV-2 immunohistochemistry [10] .
Review of published literature suggests several unifying cutaneous and systemic mechanisms may explain COVID-19?associated pernio 11: SARSCoV-2 cell infection occurs through the cellular receptor angiotensinconverting enzyme 2 mediated by transmembrane protease serine 2, subsequently affecting the reninangiotensin-aldosterone system with an increase in the vasoconstricting, pro-inflammatory, and prothrombotic angiotensin II pathway. Severe acute respiratory syndrome coronavirus 2 cell infection triggers an immune response with robust IFN-I release in patients predisposed to COVID-19 associated pernio.
Age and sex discrepancies correlated with COVID-19 severity and manifestations, including pernio as a sign of mild disease, are likely explained by age-related immune and vascular differences influenced by sex hormones and genetics. These affect susceptibility to viral cellular infection, the renin-angiotensin-aldosterone system balance, and chilblains are the most common diagnosis to explain COVID toes. Affected patients present with erythema and swelling involving acral surfaces and consistent lymphocyte-rich histopathology,
Patient Management Advice
• Resist urge to scratch-this will further damage the skin.
• Use calamine lotion to soothe itching.
• Lanolin rubbed into the feet, will help retain body heat.
• Wear woollen or cotton socks.
• Keep whole body warm.
• Take paracetamol or ibuprofen to ease pain.
• Avoid cold or damp environment when possible.
• Wear warm, waterproof clothing, gloves, and thick socks in cold and damp environments.
• Rewarm affected skin gently, without massaging, rubbing, or applying direct heat.
• Keep affected skin dry and warm, but away from sources of heat.
fulfilling the diagnostic criteria. It remains essential to distinguish pernio from other cutaneous acral eruptions that can also be associated with COVID-19 and recognize any dermatologic findings potentially associated with SARS-CoV-2 infection, which are important cutaneous signs of COVID-19 severity [10] .
Attention was drawn in Podiatric Review in 2020 to a possible relationship between chilblains and covid infection at the start of the pandemic [11]. Two years and thousands of victims later despite much more research, there remains controversy about this clinical entity. Research studies have often been small and observational, and more studies are needed to justify conclusions.
Conclusion
Practitioners presented with chilblain cases should certainly consider a relationship with current or past covid infection, but not assume infection is the cause. They should extend patient history enquiries into changed footwear and behaviour during the pandemic and particularly during lockdown and quarantine. Identifying environmental and behavioural factors might direct treatment to conventional management of chilblains concentrating on advice and prevention. Nifedipine prescription may be appropriate in severe cases.
DO NOT
• Put feet or hands on a radiator or under the hot water to warm them up
• Smoke – narrows peripheral blood vessels
• Have drinks with caffeine in content
• Scratch or pick at affected skin
Podiatry Review Summer Issue 2022 | 37
Please see overleaf for the References for this article
REFERENCES
1 L. Frumholtz, J. D. Bouaziz,M. Battistella, J. Hadjadj,R. Chocron,D. Bengoufa Type I interferon response and vascular alteration in chilblain-like lesions during the COVID-19 outbreak*: 05 October 2021https://doi.org/10.1111/bjd.20707
2 C. Galván Casas et al., Classification of the cutaneous manifestations of COVID-19: A rapid prospective nationwide consensus study in Spain with 375 cases. Br. J. Dermatol. 183, 71–77 (2020).
3 E. Freeman et al; American Academy of Dermatology Ad Hoc Task Force on COVID-19, Pernio-like skin lesions associated with COVID-19: A case series of 318 patients from 8 countries. J. Am. Acad. Dermatol. 83, 486–492 (2020).
4 D. Fernandez-Nieto et al., Characterization of acute acral skin lesions in non-hospitalized patients: A case series of 132 patients during the COVID-19 outbreak. J. Am. Acad. Dermatol. 83, e61–e63 (2020).
5 E. E. Freeman et al., The spectrum of COVID-19-associated dermatologic manifestations: An international registry of 716 patients from 31 countries. J. Am. Acad. Dermatol. 83, 1118–1129 (2020).
6 C. Galván Casas et al., Classification of the cutaneous manifestations of COVID-19: A rapid prospective nationwide consensus study in Spain with 375 cases. Br. J. Dermatol. 183, 71–77 (2020).
7 V. Piccolo et al., Chilblain-like lesions during COVID-19 epidemic: A preliminary study on 63 patients. J. Eur. Acad. Dermatol. Venereol. 34, e291–e293 (2020).
8 A. Saenz Aguirre et al., Novel outbreak of acral lesions in times of COVID-19: A description of 74 cases from a tertiary university hospital in Spain. Clin. Exp. Dermatol. 45, 1065–1067 (2020).
9 Jeff R. Gehlhausen, Alicia J. Little, Christine J. Ko,Lack of association between pandemic chilblains and SARS-CoV-2 infection. February 25, 2022 | 119 (9) e2122090119 | https://doi.org/10.1073/pnas.2122090119
10 Mark A. Cappel, MD,a Jonathan A. Cappel, MD,b and David A. Wetter, MDc Pernio (Chilblains), SARS-CoV-2, and COVID Toes Unified Through Cutaneous and Systemic Mechanism Mayo Clin Proc. 2021 Apr; 96(4): 989–1005. online 2021 Jan doi: 10.1016/j.mayocp.2021.01.009
11 Mcintosh I Covid Toes Observational aberration or Clinical entity? Podiatry Review vol 77

Podarick can you help me?
PODARICK NAILS
IT!
I would like to offer a foot bath service for client’s feet before a treatment. But I am not sure if it is safe to do so anymore. Would you have a solution to this or advice not to soak the feet at all?
Podarick says:
There is nothing better or more relaxing than bathing your feet in a bath or foot spa, not to mention there are a lot of health benefits. This is something that can be provided by pedicurists, or from a foot health practitioner, chiropodist, or podiatrist, but this will be up to the individual practitioner and the type of treatments they offer.
It has been observed that foot health professionals no longer provide foot baths as part of a treatment as they used to. For most practitioners it is time consuming when doing a 20-30-minute treatment. Although, it is not just the time involved for foot baths, more importantly it is the risk of cross infection. Many foot health practices do not offer foot bath services, because of not being able to disinfect the foot baths appropriately, due to the risk of cross infection.
Most health professionals provide medical procedures, where they adhere to high levels of hygiene. This means that all their equipment is either properly sterilised or disposable, so their patients are not put at risk from cross infections. If foot baths are used it is important that disposable foot bath liners are used for each patient, to ensure they do not pass on any infections or problems from a previous foot bath user. Then there is hot water, which if it comes from the tap, will contain some bacteria. Unless, using boiled water, which of course must be mixed correctly with cold water to avoid scalding your patient. Particularly, patients with diabetes or other foot neurological conditions, where it would make assessments difficult after a footbath. The skin softening effect may make it more likely to cause a risk of haems (cuts), especially if the skin became too waterlogged, while removing callous and corns.
It is not so much a common practice, as it once was, to do foot baths before a treatment. The use of skin preparations, such as preoperative skin antisepsis with chlorhexidine gluconate before any basic foot treatments are more regularly used. It decreases the risk of healthcare-associated bacteraemia and multidrugresistant organism transmission, which foot baths cannot do, but they do help soften skin and nails. It becomes the practitioner’s choice, along with a risk assessment on each patient that will determine the use of foot baths as part of a treatment.
Send your Nail Clippings to Podarick: email: info@iocp.org.uk
38 | www.iocp.org.uk ARTICLE (continued)
Podiatry Review Summer Issue 2022 | 39
CONGRATULATIONS!
I would like to congratulate the winner of this year’s Presidents Prize (2022) Mrs Janette Pegley-Reed. Thanking her for all her hard work in arranging and giving her time to organise meetings and seminars. I will be awarding the prize in person in October in Ireland.


In addition, I am happy to present two “Unofficial” Thank yous from me to Michele Allison and Michael Franklin, for their continued outstanding service, dedication and commitment to the IoCP.
Hi everybody. A tongue in cheek poem by Ian Fenton
How I love my patients
They’re such lovely folk They come and sit and talk to me We laugh and share a joke
How I love my patients
They tell me all their woes Just before they take a seat And show me all their toes.
Finally, I would like to wish
a very happy and welldeserved retirement. After a 30-year career in teaching languages, Valerie decided to change tack and ran a very successful practice for the past 20 years as well as holding the role of Chairman of the Sussex Branch. Congratulations and all the best for the future.
Linda Pearson, Past President
I guess by now I’ve seen most things Their corns and their hard skin But sometimes I think to myself Oh! Where do I begin?
How I love my patients
Most fill me with good cheer And now I’ve come to realise I chose the right career.
THANK YOU!
I could not be present at the AGM and was unable to thank personally and on behalf of all the members from the Cheshire, North Wales, Shropshire and Staffordshire Branch, our President for all her hard work and support while holding her position at the IoCP.
I remember when Linda came to the board in 2014. I believed then, she was the youngest President. Linda occupied this position for 8 years, the longest time of all presidents. Linda has always been most approachable, took her task to heart and served the IoCP with integrity.
We are honoured and pleased, that one of our branch members has been the President.
We wish Linda well and look forward to see her at our next meeting. Michèle Allison Chair and Phil Yeomans Vice Chair
How I love my patients
And the joy they sometimes bring But how I love them most of all When they make my till bell ring!
I hope you all have a good summer.
Regards Ian.
40 | www.iocp.org.uk BRANCH NEWS
Valerie Probert-Broster
Mary Marsh Reg.
CH18682
Mary trained as a Chiropodist in a class of six at the Scholl School of Chiropody in Islington, London in 1998. After qualifying she worked in the Milton Keynes area and later set up her own clinic in Harold, Bedfordshire.

When the HCPC was introduced, Mary applied and was accepted. She gained an excellent reputation both professionally and in the community. For example, she helped in raising money for Alzheimer’s by abseiling down the inside of the Northampton Lift tower.
She joined the Leicestershire Branch of the IoCP where she was a very valuable and popular member. She regularly attended meetings and also supported the AGM and Annual Dinner and Dance with colleagues around the country.
Unfortunately, she was diagnosed with breast cancer in August 2020 but carried on until it was no longer feasible. Sadly, having been given the all clear and planning a return to work, the cancer returned and she lost her battle with it and died in April this year. She will be sorely missed by her family, all those who knew her, and is a great loss to the Institute.
A Little note about Mary…

I met Mary in 1998 at Scholl School in Islington, we were both looking forward to starting a new career and adventure. We were a class of six but I guess because Mary and I lived fairly close we kept in touch and met regularly in Milton Keynes for shopping and lunch, obviously we talked feet but lots of other topics as well and always took our diaries to make the next meeting date.
Mary introduced me to our local goup “Leicester and Northants” and they met mostly in Kilsby, these meetings helped us make new friends and encouraged us to start our own clinics.
Over the years we both attended meetings at Kettering Foothealth Conference and Lutterworth AGMs. We also travelled to Southport together to attend the annual AGM and Dinner Dance which was a very sociable weekend. Mary was always good company and had a chat and a smile for everyone.
Life can throw up obstacles but Mary always stayed positive and smiled through the good and the difficult. During lock-down we met outside at Emberton Park and had our usual walk and chat, by this time Mary’s hair was growing back and again she was positive about the future and with Sue Forster giving her help and advice on the stages of recovery she stayed focused.
In May we were due to meet again and I was going to provide the lunch at her house as she was feeling tired but unfortunately this wasn’t to be, as she was taken ill and had to give up the fight!
I will miss her dearly as everyone who knew her will - Keep smiling Mary we will think of you often with love.
Ruth Rose
OBITUARY
David Ayres and the Leicester & Northants Branch Members
Podiatry Review Summer Issue 2022 | 41
Please note: all products advertised in the Podiatry Review and on the Website are accepted by the Institute of Chiropodists and Podiatrists on the basis of a commercial advertising service and purchasers should carry out their own assessment as to the suitability of such products for their own specific needs. Acceptance of the advertisement by the Institute does not imply our endorsement or approval of the product.
SVTS Chiropody Drill repair and sales
We offer an excellent competitive and efficient repair service for all makes of Podiatry/chiropody Nail drills. Berchtold, Hadewe, Suda, Footman, Podiacare, Podo Tronic and Podo Pro EVO-30,40&50 drills. We sell Berchtold S35/ S30, Hadewe, EVO 30,40.50 Dust Bags from £1.25 – £2 each. WE ALSO BUY UNWANTED DRILLS.
Unit 255 Stratford Workshops, Burford Road, London E15 2SP Contact us on 0208 5190044 or www.chiropodydrillrepair.co.uk
Chiropodist/ Podiatrist required in Heswall, Wirral
We are situated in Heswall, Wirral. We are a busy multi-discipline clinic in the heart of a thriving village.
Our clinic is exceptionally busy with five chiropodists and full-time reception staff. The position is offered with hours to suit applicant.
The successful candidate must be personable, not afraid of being busy and have great attention to detail. In return they can earn £200-300 per day. This is a self-employed position and payment is on a fee sharing basis.
Tel: 01513 429665 for further information
Hinckley, Leicestershire
We are looking for the right person to join our amazing team. This is an excellent opportunity to practice and develop your skills in a supportive environment.
This post will suit a Podiatrist with a good level of general skills, LA and POMS.
Full-time Employed (Part-time minimum 25 hours will also be considered). Based on Skills and Experience£27,000 to £36,000 (pro-rata if part-time). Up to £1000 towards CPD requirements annually.
The clinic specialises in the treatment of skin and nail conditions, such as Nail Surgery, Lacuna for Fungal nails, and Verrucae Treatments including Swift, Cryotherapy, Faulknor’s Needling and Electrosurgery. We also offer custom orthoses.
Our in-house services include Physiotherapy, Hearing Care, Counselling, Dermatology and Paediatric Medical and Surgical Services.
If you would like to be part of our work family, please contact Faye Vogiatzoglou on 07867784082 and/or forward your CV to contact@medipodclinics.com.
Podiatrists / Chiropodists required for busy clinics in the New Forest, Hampshire Situated in the idyllic location of the New Forest, with one of our clinics positioned within a mile from the Solent overlooking the Isle of Wight to the Eas. We have vacancies for enthusiastic candidates who enjoy variety in their role and attention to detail is a must.
We offer Podiatry, Biomechanics (custom orthotics using 3D scanning system), Verrucae Treatments (including Swift), Nail Reconstruction, Prende Wax Therapy Treatment.
We are extremely busy with Nail Surgeries, so experience in this area is particularly desirable. We offer a competitive salary (dependent upon experience), uniforms, free parking, company pension scheme and private healthcare scheme. There is no lone working as we have our customer service team at both sites. Whether you are looking for a full-time or part-time role, are experienced or newly qualified we would love to hear from you.
Please apply with an up-to-date C.V. to Christopher Gillingham at Chris@forestfootandhealth.com or contact me on 07890 614034 for further information.
42 | www.iocp.org.uk
ADVERTS
CLASSIFIED
Diabetic Foot Module Course 10th – 14th October 2022 At The Wellcome Collection Euston Road, London Intensive update course for specialist practitioners. For more information, please email diabeticfootmodule@gmail.com
DIARY OF EVENTS
JULY 2022
14 Sheffield Branch Meeting
At 7.30pm Via Zoom
Contact Helen on 07789 025022 or email hrawse@live.co.uk for further information
17 Wolverhampton Branch Meeting and AGM
At 10am at the Reading Rooms, Market Street, Penkridge, Staffs. ST19 5DH
Speaker to be arranged
Contact: David on 01785 716607 or email djcollett@hotmail.co.uk
27 London Branch Meeting
At 7.30pm Via Zoom
Contact Sarah on 07790 717833 or email footwoman@gmail.com
SEPTEMBER 2022
11 Cheshire, North Wales Branch Meeting
Venue TBC
Contact Michele Allison on 07766 700027 or email missminou@ hotmail.co.uk
21
Birmingham and the Shires Annual General Meeting
8pm at Willersey Village Hall, Willersey, WR12 7PJ
Autoclave Servicing Session, please contact Kate to book.
Contact Kate Harrison on 01789 262365

OCTOBER 2022
9 Wolverhampton Branch Meeting and AGM
10am at the Reading Rooms, Market St, Penkridge, 5DH Speaker to be arranged
Contact: David on 01785 716607 or email djcollett@hotmail.co.u
26
London Branch Meeting
7.30pm via Zoom.
Contact Sarah on 07790 717833 or email footwoman@gmail.com
NOVEMBER 2022
17 Sheffield Branch Meeting
At 7.30pm Via Zoom
Contact Helen on 07789 025022 or email hrawse@live.co.uk for further information
JANUARY 2023

8 Wolverhampton Branch Meeting & AGM
At 10am at the Reading Rooms, Market Street, Penkridge, Staffs. ST19 5DH
Contact: David on 01785 716607 or email djcollett@hotmail.co.uk
25 London AGM Meeting
At 7.30pm via Zoom.
Contact Sarah on 07790 717833 or email footwoman@gmail.com
Please email julie@iocp.org.uk with information about Branch Meetings whether face-to-face or via Zoom etc.

Keep your Branch members up to date so they can attend.
SOUTH WALES AND MONMOUTH BRANCH
Meetings are taking place via Zoom, members who would like details of the next meeting and wish to attend please contact Esther on 01656 740772 or email estherdanahar@ yahoo.co.uk
Podiatry Review Summer Issue 2022 | 43
advert
for more information
To place an
opposite or
please email julie@iocp.org.uk







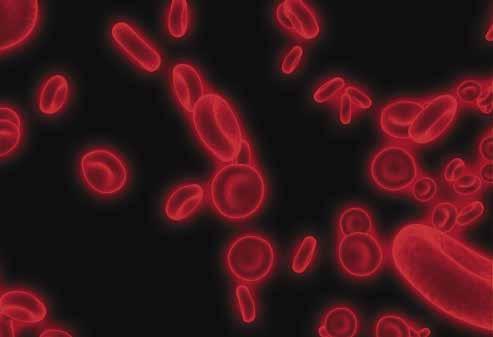


























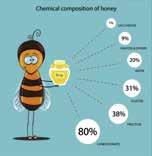














 By Personalo at English Wikipedia.
By Personalo at English Wikipedia.










 Martin, Anthony & the Graduation Group
Yvonne Nelson
PremjidClays
Martin, Anthony & the Graduation Group
Yvonne Nelson
PremjidClays













 By James Earls MSc.
By James Earls MSc.