A step in the right direction Podiatry Review
SUMMER ISSUE Volume: 78 No: 3 Jul/Aug/Sep 2021 The Institute of Chiropodists and Podiatrists FREE 5 Page CPD Article The Venous Foot Pump: Modelling its function in gait Pages 19 - 23 Are Podiatry On-line Consultations a Good Idea? Paramedics Column Gary Strong chats to Tony Stone Pages 28-29 Pages 32-36 The impact of anti-cancer treatment on feet Part 2b Pages 24-27
The Institute of Chiropodists and Podiatrists News
Podiatry Review
Annual Subscription £20 UK /£30 Overseas
Published by
The Institute of Chiropodists and Podiatrists
150 Lord Street
Southport
Merseyside PR9 0NP
Tel: 01704 546141
Email: secretary@iocp.org.uk Website: www.iocp.org.uk
Editor: Andrew Williams, MInstChP, CFPodM

Academic Editor: Martin Harvey, PGCert, BSc, MInstChP, MCPodS
Academic Advisor: David M Holland, BSc, CSci, FFPM - RCPS(Glasg).
Volume: 78 No: 3 ISSN 1756-3291
Academic Review Team
Ms B Wright, MSc BSc (Hons), PGCE PGDip, FInstChP
Mr S Miah, CFPodM, MInstChP
Mr A Williams, MInstChP, CFPodM
Media and Publicity Contact: Doctor Bharti Rajput, MBE PhD
Email: media@iocp.org.uk
Medicines and Procedures Panel (MaPP)


Chair: Gaynor Wooldridge, MInstChP, CFPodM
Andrew Williams, MInstChP, CFPodM
Abid Ali, CFPodM, BSc, MInstChP
Somuz Miah, CFPodM, MInstChP
Martin Harvey, PGCert, BSc, MInstChP, MCPodS
Podiatry Review
Summer Jul/Aug/Sep 2021
Contents
© The
and
Disclaimer: The
and
expressed
and they
CONTACTS 4 IOCP Contacts 5 Editorial ARTICLES 8 President’s Address 10-11 Venn Healthcare 12-13 Obituary:
14 2021 Mid
Diary 15-17 Footnotes:
Practitioner News 24-27 Are Podiatry On-line Consultations a
Idea? 28-29 Paramedic Column 31 Dr B’s Business Box 32-36 The
LEARNING 19-23 5 page CPD articleThe Venous Foot Pump: Modelling its function in gait NEWS 38 Classified Adverts 39 Diary of Events 24-27 28-29 32-36 @IOCP_Chiropody @IOCPChiropody Podiatry Review Summer Issue 2021 | 3
Institute of Chiropodists
Podiatrists
Editor and the Institute of Chiropodists
Podiatrists accept no responsibility for any opinions
in the articles published in the journal,
do not accept any responsibility for any discrepancies in the information published. No part of this publication may be reproduced, stored in a retrieval system or transmitted in any form or by any means, electronic, mechanical, photocopying or otherwise, without the prior written permission of the publishers.
Vincent J Denvir
Wales
Foothealth
Good
impact of anti-cancer treatment on feet Part 2b
IOCP Contacts
President:
Executive Committee
Mrs L Pearson, FInstChP, BSc Pod Med
Chair Executive Committee: Mr M Harvey, PGCert, BSc, MInstChP, MCPodS
Vice-Chair Executive Committee: Mr A Ali, CFPodM, BSc, MInstChP, BSc
Chair Board of Education: Mr A Williams, BSc(Hons), CFPodM, FFPM RCPS(Glasgow)
Vice-Chair Board of Education: Ms B Wright, MSc BSc (Hons), PGCE PGDip, FInstChP
Chair Board of Ethics: Ms B Wright, MSc BSc (Hons), PGCE PGDip, FInstChP
Honorary Treasurer/Regional Director (Midlands): Mr S Miah, CFPodM, BSc (PodM), MInstChP
Regional Director (Scotland): Mrs H Jephcote, MInstChP
Regional Director (England North): Mrs C McCartney, MInstChP
Regional Director (England Midlands): Mr D Ayres, MInstChP
Academic Advisor: David M Holland, BSc, CSci, FFPM-RCPS(Glasgow)
Company Secretary: Miss A J Burnett-Hurst, HonFInstChP
Standing Orders Committee: Mr M Franklin, MInstChP
Branch Secretary Contacts
Branch Secretary Telephone Email
Birmingham & the Shires
(Acting secretary of)
Kate Harrison 01789 612959 kathrynharrison87@gmail.com
Cheshire & North Wales Michele Allison 07766 700027 missminou@hotmail.co.uk
Essex Beverley Wright 01702 460890 solespirits@hotmail.com
Leeds Caroline McCartney 07583 934468 hello@chiropodyandfoothealth.co.uk
Irish Janette Pegley-Reed 00353 8627 31371 jpegleyreed@gmail.com
Leicester & Northants Ian Fenton 07718 700 641 fenton303@ntlworld.com
London Sarah Bowen 07790 717833 footwoman@gmail.com
North West Alison Marsden 01772 623180 alison.marsden@hotmail.com
Nottingham Valerie Dunsworth 0115 931 3492 adunsworth@btinternet.com
Sheffield Helen Rawse 07789 025022 hrawse@live.co.uk
South Wales & Monmouth Esther Danahar 01656 740772 estherdanahar@yahoo.co.uk
South Coast Brenda Griffin 07894 454 711 brendagriffin2018@gmail.com
Scottish John Stott 0780 135 6485 jls@stottland.com
Wolverhampton David Collett 01785 716607 djcollett@hotmail.co.uk
4 | www.iocp.org.uk CONTACTS
Dear Colleagues
“Now is the winter of our discontent made glorious summer”. By the time you read this, hopefully the major effects of the Covid crisis will be in the past and we will, once again, be living a semblance of normal life. From the professional viewpoint those of us volunteering to work with vaccination teams as well as, I am sure, the majority of our members who have been looking after elderly and/or ill relatives and neighbours, will be once more taking up our professional duties. In this journal, an excellent piece by David Tollafield reviews telemedicine and how podiatry can play its part. This follows the ‘how to’ article by Dr Bharti Rajput in the Spring volume and points the way of the future. Inevitably, changes have occurred concerning the delivery of care to our patients. A case in point is the shortage of phenol, caused by an international scarcity of the chemical along with acetone, both of which are the active ingredients of many glues and resins. According to the laws of supply and demand, when demand increases and supply decreases, the result is a rise in price. Some of those colleagues involved in nail surgery have been in touch with Head Office to ask how to address the issue. It is an object lesson to all of us that we should be aware of, and be knowledgeable in alternative treatments. In the case of onychocryptosis there are many different therapies available including sodium hydroxide (chemical), potential cautery (electrolysis), direct cautery (electrocautery), direct cautery (electrosurgery), direct cautery (laser) and incisional surgery (Winograd/Frost etc.). All these techniques have their place and all have their drawbacks. Sodium Hydroxide requires flushing with aescetic acid following the procedure; electrolysis, electrocautery, electrosurgery and laser require equipment of varying expense and incisional surgery requires to be carried out in a ‘clean’ room. As the majority of the Institute members are engaged in solo practice the purchase of equipment which might only be used infrequently raises the spectre of cost/benefit. However, it may well be worthwhile speaking to members of your branch to arrange for group purchase or lease. Indeed, since all the techniques mentioned above require local anaesthetic induction, two members working together might not only be financially advantageous but reduce the pressure on the individual practitioner and allow a ‘list’ of patients to be treated. It may also be worthwhile speaking to larger local G.P. practices to see what facilities they have available and are willing to rent out.

Collaboration is an excellent method of working since no practitioner is all knowing and each member has some knowledge to share. In addition, isolation is not conducive to wellbeing since we all suffer from professional frustration from time to time and working with colleagues can definitely be helpful in this regard. As far as more advanced techniques such as incisional nail surgery are concerned, the Institute already runs a course on those procedures and help is always at hand. If you wish to undertake courses on the other techniques mentioned above, then just contact Head Office and provided there exists sufficient interest such courses will be arranged. If you feel that your branch members would benefit from lectures on the above subjects, then again, let Head Office know and they will put you in touch with colleagues who have the appropriate skills.
Winter is over and sunny uplands are ahead. We can take pride in our duties as we are almost unique in having the ability to consult a patient who is in pain and know that when they leave, they will do so in comfort. However, the world has changed and now is the time to embrace new challenges and new methods of working.
W J Liggins MA; BSc (Hons); FInstChP; FPodA. Dean of the College of Podatric

Surgeons
Guidelines for new and established authors
Content of your article should be Podiatry or foot health-related. Podiatry Review is mostly in easy-to-read format, and articles for submission should reflect this. CPD Certificates are issued for Case Studies and Articles. Please ensure that your name and title (ie - FHP, Podiatrist, or other) are included with your article. Please proof-read and spell-check your article before submission.
It would be helpful to the Editorial Committee if you could reference any books or Papers mentioned in your article. If you are not sure how to do this we are happy to assist.
Podiatry Review Summer Issue 2021 | 5 Editorial
Dear Members and loyal ‘Review Readers’
As you know, as an organisation we have a long history of supporting professional education at all practice levels in podiatry, chiropody and foot health that dates back to our founding years in the 1930s. Our Licentiate and Diploma courses in Chiropody were highly regarded in the days before the statutory regulation of Chiropody and Podiatry, whilst in more recent years we have provided various types of postgraduate training that has proved enormously popular in subjects as diverse as steroid therapy, advanced regional anaesthesia, platelet-rich plasma, dermal fillers and botulinum toxin in the feet and associated structures.
Currently, the Institute is one of the board members of the Foot Health Consortium that has been set up by NHS Health Education England to take forward the concept of a structured learning framework in Foot Health that will help to address both the subject of the training standard of the (currently) unregulated FHP workforce, as well as the shortage of student recruitment into University podiatry courses by looking to establish a nationally agreed education framework for the FHP workforce. Such an education and recognised qualification framework is hoped to establish opportunities for level 3, 4 and 5 FHP’s being recognised as able to provide support in the NHS workforce, as well as being an entry ‘staircase’ into University education for those who wish to ultimately complete degree training to gain HCPC registration as a Podiatrist.
In line with our commitment to current and future education development we have recruited a highly skilled fulltime education officer to the team at Head Office. I am therefore delighted to introduce Samantha (Sam) Connolly who joined the team in April. I have asked Sam to introduce herself and her brief CV follows this welcome. There are exciting times ahead in our profession, and I know that you will join me in welcoming Sam and supporting her efforts as she takes us forward into that future!
Samantha Connelly, Education Officer at The Institute of Chiropodists and Podiatrists
Known as Sam, I am a qualified tutor in Further Education and has worked within FE for 13 years both as a tutor and a personal tutor. I also have a BSc (hons) degree in Business and Management along with a Foundation degree in Business Information Systems.

I have been in Education and Training for the last 21 years and I cannot think of a better profession than to help and support others to achieve their ambitions. I understand the barriers to learning and also how to motivate learners. I am highly skilled in meeting targets and deadlines and in mentoring and supporting learners. I am committed to Education and Learning and Development and have always looked to further my own knowledge as I believe we can always learn. I have always strived to ensure that every learner maximises their true potential and achieves their goal.
I have coordinated two projects that promoted apprenticeships across Lancashire and built up a network and both apprentices and employers in order to support the project and reach out to all organisations and Schools across Lancashire. Recently I was Learning and Development Coordinator for a port. I developed all of the tracking and monitoring systems and worked with the tutors in the creation of training manuals and all training documentation in line with Health and safety and quality standards. I enjoy developing systems and I am highly skilled at ensuring quality processes are in place to ensure quality of provision.
I am looking forward to this new chapter in my career with the Institute of Chiropodists and Podiatrists and in supporting and assisting all of our learners and members in their further development.
I am an animal lover and have 3 cats and one dog. I enjoy spending time with my family and friends. I have just become a first-time grandparent and looking forward to the joys and challenges that it will bring to my life.
6 | www.iocp.org.uk ARTICLE


Podiatry Review Summer Issue 2021 | 7
President’s Address 2021
Dear Members, Directors and Fellows, my very warmest welcome to this the 66th Annual General Meeting of the Institute of Chiropodists and Podiatrists.
After yet another unprecedented year, many of us, including myself have experienced a variety of changes in our working lives. Some colleagues have taken early retirement, whilst others have elected for a complete change of tack, embarking on a new challenge that they may have wanted for some time.
During the pandemic there have been numerous inspirational people who have put their own problems and daily difficulties aside in order to help others, a lesson which is really humbling.
Many members and people’s, “just by chance”, meetings continue to be a great source of inspiration. One such person is Podiatrist Alice Murray (CH035907), who initially trained in Durham and qualified from the University of Salford. Due to personal experience of losing a parent through complications from Diabetes, this lady has made it her mission to set up a clinic in her family’s home town in Narobi (Kenya). The clinic will be housing a Diabetologist, Tissue Viability Nurse, a Chiropractor, also an internal medicine Dr and a Physiotherapist.
This dream will become a reality on 1st June this year, and now is one of three Podiatrists registered in Kenya. Any donations of Equipment, podiatry related goods or monetary donations will be most welcome. As with most countries it’s the people who cannot afford healthcare that tend to suffer the most.
Alice would be happy to welcome anyone (after Covid restrictions cease) and show interested parties the clinic and to see what they are trying to achieve for themselves. Currently staying in the Mount Kenya region called Nanyuki, well known for where the British Army Barracks are stationed, Alice has already contacted their Medical Officer in order to offer treatment to the Soldiers.
I must state I have received full and direct permission from Alice Murray to pass on her contact email: almurray62@gmail.com. I would like to wish Alice and her team all the very best for the immediate and long-term future.
I would also like us to remember our members that have passed away during the last 12 months, whilst we remember their hard work and dedication and character they brought to the organisation.
This March saw the opening of the CORU register for our colleagues in Southern Ireland. Wishing them a smooth and successful conclusion.
There have been, and still are, an abundance of quality online courses. To be fair, I am probably one of the most “technically challenged” practitioners, alas that won’t stop me trying to improve my skills in that area.
Very well done to all the Branches/Regions who have regular zoom meetings to keep members in the loop and giving each other a sense of being part of an organisation that isn’t afraid of change or adversity, we embrace it and look for the positives in it. This indicates we are a strong organisation willing to adapt and “step up to the challenge.”
I am happy to report that we are now working partners with the Motor Neurone Disease Association in order to broaden ours and our affected patients’ knowledge and understanding.
Thank you to all of my colleagues on the Executive Committee for all of their hard work and contributions throughout the year. Also, to Jill, Julie and all the staff at Head office for their continued work.
Finally, thank you to you, the members, for your continued support and input. As we look forward to the year ahead, relaxed restrictions and hopefully to seeing you in person in the near future.
Linda Pearson President, The Institute of Chiropodists and Podiatrists
8 | www.iocp.org.uk ARTICLE

Podiatry Review Summer Issue 2021 | 9
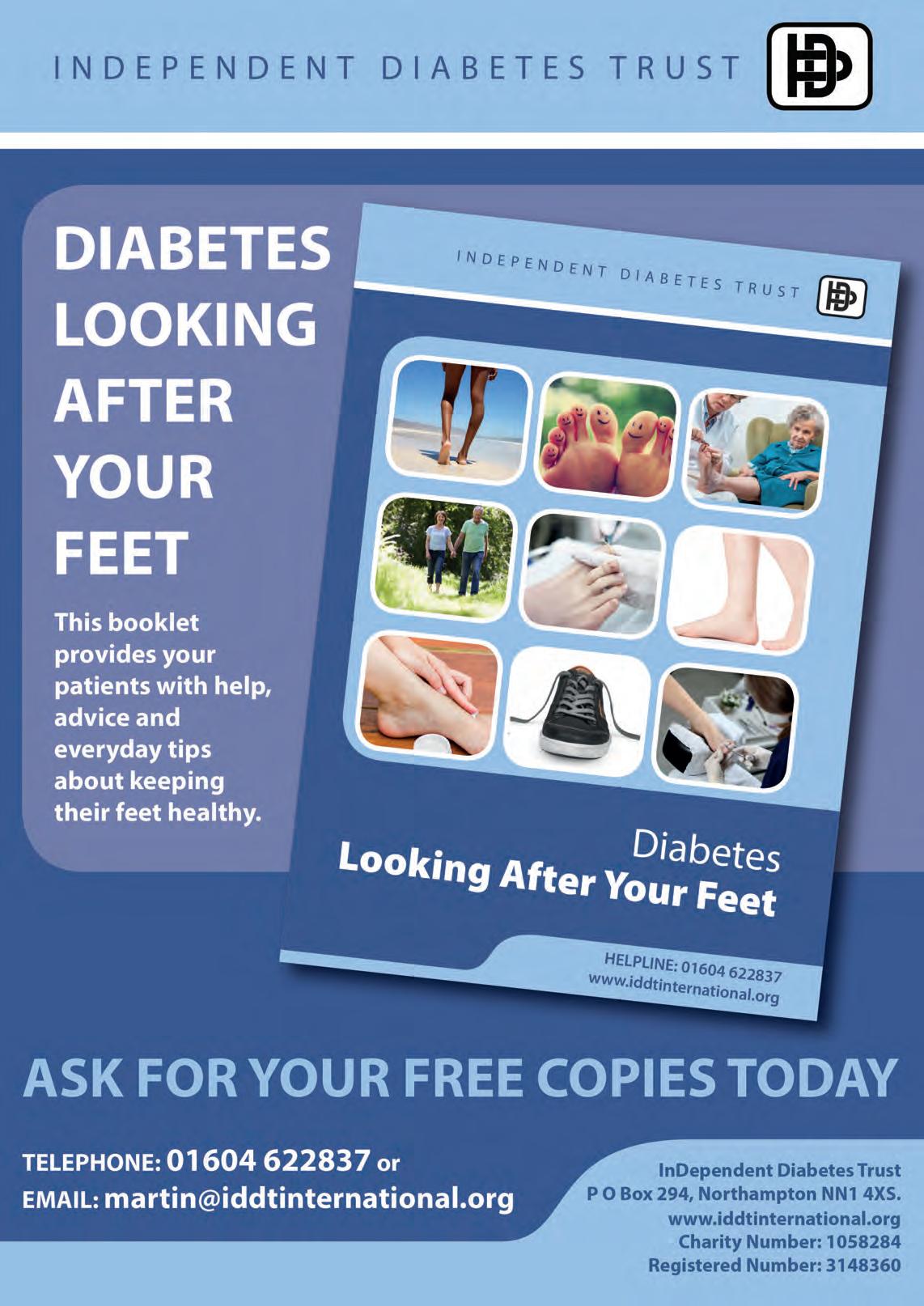
Expanding your treatment options

Shockwave Therapy (ESWT) has become increasingly popular in recent years, a valuable non-invasive tool for many podiatrists treating multiple pathologies from Plantar Fasciitis to Achilles Tendinopathy. The vast majority of clinicians in the UK, use radial shockwave, which is well evidenced and offers excellent results for patients. The benefits of radial shockwave are outstanding and many clinics choose to start with radial shockwaves. However, there are certain pathologies it cannot treat, this is where focused shockwave therapy expands treatment possibilities. Focused shockwaves are fast impulse/high energy density waves that are able to penetrate deeper into the tissues. Focused shockwaves deliver all of the power to a designated treatment depth of up to 12cm. Practitioners are able target an exact point with complete precision, making it ideal for treatments that require targeting tissue at a deeper level; such as close to bone, calcifications or delayed / non unions. Patients who are unable to tolerate radial treatments for acute injuries will also benefit from focused shockwaves.


EMTT® - The novel anti-inflammatory technology that’s got MSK specialists excited! Magnetiloth EMTT® is a novel technology that uses high energy magnetic fields for regeneration and rehabilitation at a cellular level. EMTT must not be confused with Pulsed electromagnetic field therapy (PEMF), EMTT is 40% stronger than PEMF, with a much higher oscillation and greater treatment depth of up to 18cm. In contrast to Shockwave Therapy, which initiates a pro-inflammatory response, EMTT® has an anti-inflammatory response, reducing pain and inflammation in acute pain presentation, irritable flare ups, neuropathic pain, diffused pain, degenerative pathologies such as Osteo Arthritis. In these cases, shockwave therapy would not be tolerated well, whereas EMTT® is tolerated, even with the most painful conditions such as rheumatic patients. EMTT® is not a replacement for Shockwave, far from it, these two devices treat very different conditions. It is an excellent tool to add to your current shockwave service or as a stand-alone treatment. Early adopters of the novel technology have described it as a ‘game changer’ for chronic pain and arthritis patients are loving it.
Accelerated healing through natural responses

10 | www.iocp.org.uk ARTICLE ADVERTORIAL(continued)
Radial Shockwaves Common Indications Plantar Fasciitis Myofascial Pain Syndrome Chronic Tendinopathies Larger treatment areas/ muscle groups EMTT Common Indications Degenerative Pathologies Acute Pain Diffuse Pain Focused Shockwave Common Indications Insertional Tendinopathies / Deep-Seated Tendons Bone stress Injuries / Stress Fractures / Non-unions Osteoarthritis Spinal Facet Joint Pain / Coccydynia Carpal Tunnel Syndrome Morton’s Neuroma Wound Healing Men’s Health Evidenced based practical learning Venn Healthcare run regular CPD events and are excited to be offering the UK’s first full day practical course dedicated to focused shockwave therapy. The Storz Medical range of shockwave systems have devices suitable for all clinics and provide access to regular online learning and a huge data base of clinical resources. For more info email info@vennhealthcare.com
complimentary technologies for MSK Pathologies


Podiatry Review Summer Issue 2021 | 11 -
3
Vincent J Denvir 1929-2021 :

Proud spokesman for the Chiropody profession
Vince was born in the east end of Glasgow and was proud of his Glaswegian roots. He was educated at St Agnes’ primary school, Lambhill and then St Mungo’s High School. His father was the janitor of St Thomas’ school in Riddrie where Vince was an alter-boy in the nearby church which meant he was often called at the last minute to help with church services. He was a keen footballer and played for St Mungo’s as a schoolboy and as a former pupil.
He was conscripted to national service in the RAF in 1947 and spent 2 enjoyable years as an instrument mechanic posted to Wiltshire for training and then at Edzel in Angus. It was from his posting in Wiltshire that he wrote to the Glasgow Foot Hospital, School of Chiropody in 1949 to ask if he could be considered for a place to study the new and exciting profession of Chiropody. His letter was received sympathetically by the Principal Mr J McBain Stewart (MBE), who boasted that the school had “…rather advanced ideas of what full training should be for the chiropodist who aims at making the profession both congenial and lucrative…”. This clearly attracted his attention and he gladly accepted a place and studied with enormous enthusiasm and commitment. In typical style he kept many of the documents outlining the course syllabus which remain in good condition to this day as a unique record of what constituted chiropody training in the early 1950’s. (see supplemental files on website). It was there that he met Pat McQuony, a teacher at the school, who remained a great lifelong friend and colleague until his untimely death at the age of 58.
After graduating with his diploma in chiropody he first worked at the Co-operative shoe and leather emporium in Glasgow. He was an enthusiastic teacher and was delighted to be appointed as a lecturer at the Glasgow foot hospital in 1954 where he worked for the next 6 years with Pat McQuony. He grasped his next great challenge in Stirling in 1960 when he was invited to set up the first child-school foot health service by the medical officer for health, Dr E. Neil Reid. Initially he travelled back and forth in a Ford Anglia, with only 3 forward gears and no reverse, between Glasgow and Stirling but within a year had moved with his young family to Bannockburn near Stirling. Spurred on by the newly formed NHS, he was given great support and encouragement to develop child foot health services which he did over the next 10 years. His personal enthusiasm and eye for detail helped create many novel ideas around children’s footwear and foot health education in schools (opposite)
He was a keen photographer and took hundreds of pictures of children’s feet and used these to give lectures at the Glasgow School of Chiropody throughout the 1970’s. He also gave regular talks about foot health in local schools, Mother’s clubs and community halls. He wrote a paper on the development of the child foot health service in Stirling which was published in 1971 and remains listed in major publication databases


12 | www.iocp.org.uk OBITUARY
(Denvir, V. J. “A school foot health service after 10 years.” Community Medicine 126.14 (1971): 185-9.). Information from this report was used in the “Children’s Footwear” Report of the Committee appointed by the Chancellor of the Exchequer (Cmnd 5243, March 1973) “examining the relationship between footwear prices and foot abnormalities in children” (left).

He was a very active member of the Society of Chiropodists and was on the committee for many years becoming Chairman of the Glasgow Branch in 1968. He kept almost all of the original conference programs starting in 1954 (see picture below) with names of attendees at the conference dinners. These lists provide a fabulous record of key people contributing to the development of Chiropody services in the UK between 1950 and 1980. A selection of these are included on the website as supplemental files. He chaired sessions and spoke at many of these meetings.

He was a fastidious collector of information. He made detailed measurements of hundreds of children’s feet recorded on punch-cards, the pinnacle of data collection in the 1960’s. Sadly his plans to follow these children up in order to see how these early measurements influenced their adult foot health never came to fruition but it was a visionary plan well ahead of its time.
He was an advisor and contributed to a parliamentary report on child foot health in 1970. He became the Chief Chiropodist for NHS Forth Valley in 1980 when his focus switched from education and patient care to service management. In typical style he applied himself diligently and with an eye for detail to create a high quality chiropody service for the people of Forth Valley.
He succeeded in persuading many self-employed practitioners to become NHS employees thus bolstering a growing service. He became an active member of the Association of Chief Chiropody Officers (ACCO) and went on to organise its annual meeting at Stirling Castle in the early 1980’s which was a great success. After guiding his service through several NHS reorganisations, he finally retired in 1992 and was replaced by a trusted successor, Joyce Brown. He spent his retirement playing golf, repairing all kinds of electrical and mechanical objects, travelling, tending to his beloved roses and caring for his grandchildren.
He remained fit and well until his late 80’s when he sadly developed Alzheimer’s disease. He died peacefully in his sleep at the age of 91. He is predeceased by his loving wife Veronica (Ronnie) and leaves 4 sons, 11 grandchildren and one great grandson.
He should be remembered as being deeply proud of his professional life at an important time in the history of chiropody as it developed high professional standards and became increasingly recognised as a key part of adult and children health services in the UK.
Martin Denvir

Podiatry Review Summer Issue 2021 | 13
Mid Wales Diary
By David Holland BSc, CSci, FFPM-RCPS(Glasg). Chartered Scientist and Podiatry Expert Witness.

The current situation with Covid has been a disaster for many Foot Health businesses. How can you make a living if patients won’t come to you, or you can’t go to them? Things are easing this year, but of course it can take years to build back lost income.
I have vivid memories of my Sunderland Chiropody Practice income stream drying up in the mid-80s – similar, in a way, to the problems experienced by those delivering Foot Health through Covid today. In 1984 the Miners’ Strike hit the coalfields and mining villages of the North-East of England. The film “Billy Elliot” portrayed just some of the hardships of the mining communities at that time. The knock-on effect on shops, pubs, hairdressers, and Chiropodists (we were all Chiropodists then) was drastic and immediate. In my case I left the Practice to my business partner and moved on – back eventually into the NHS where I worked as a Senior 1 Chiropodist at a Project in Jarrow.
Thankfully Covid has not affected my current practice, which is medicolegal. I deal with Solicitors and Barristers by email, phone, or video-conferencing, and moved over to assessing clients by video-link in March 2020.


The new house project is coming along well. My office is finished, and is pretty much self-contained, with shredder, photocopier, desktop PC, various laptops, phone, and internet. It is also a very nice space to work from – thanks to Alison my wife, who spent an age plotting and scheming (as she would say) and doing much of the hard physical work to ensure the finished article. Final verdict? It’s brilliant!
The house, really a large, modern cottage, is
called Wyvern. A Wyvern is a mythical two-legged dragon – think Game of Thrones dragons you won’t be too far out. Wyverns have some historical significance in Wales. Welsh hero Owain Glyndwr (1359-1415) carried a Wyvern emblem into battle.

Neither of us liked the name initially but can you change a house-name safely? Certainly it is considered very back luck to change the name of a boat. The name of the house – Wyvern – will probably stay.
On buying or hiring equipment for your Practice in 1978 my business Partner and I bought two dust-extracting drills – unheard-of luxury for most Chiropodists at that time. In the 1980s a published research paper emphasised the potential dangers of nail dust pathogens. I do wonder about that research paper. My father was a Chiropodist and was busy seeing patients from 1952 until 1991. He used a drill on nearly every patient – without dust extraction. For a man who also smoked 80 a day until he was well into his 50s he made a remarkable job of keeping his lungs healthy – he died aged 86 – not from any respiratory condition.
14 | www.iocp.org.uk ARTICLE
Footnotes
Foot Health Practitioners News - Issue 6

WELCOME BACK TO FOOTNOTES!
Dear Colleagues,
A number of our members and other readers of the ‘Review’ have asked if we could again incorporate the quarterly ‘Footnotes’ newsletter within the Review, so that its content is available to a wider audience than just the members of the College of Foot Health for whom it was originally designed.

As you will be aware, the Institute founded the College of Foot Health for the benefit of practitioners who have trained and qualified via the Institutes own Foot Health Practitioner course. Our course and membership of the College of Foot Health, was designed to set a benchmark for ethical practice, an appropriate level of training, meaningful indemnity insurance for public protection and responsible standards in the currently unregulated sector of Foot Health Practice, which sector has grown substantially in recent times.
In 2019 the Institute was invited by NHS Health Education England, along with other podiatry organisations, to sit on the leaders group of the Foot Health Consortium. This industry leaders’ consortium, chaired by Professor Beverley Harden, National AHP lead and Deputy Allied Chief Health Professions Officer, was set up in response to dropping recruitment levels into the registered sector, both NHS and Private, as well as the dramatic growth in the unregistered sector.
You, like myself, will be aware that the lack of a common level of education, scopes of practice, standards and ethics in the unregistered sector is an area that is long overdue for addressing. Whilst some FHP training courses are, as with the Institute’s, ethical, appropriate and fit for purpose, many are not and this is what the work of the consortium is designed to address. Decent FHP training, together with responsible support from ethical and professional organisations such as the Institute, can produce individuals who can safely and responsibly practice routine and general non-surgical/medical footcare. Additionally, by giving such individuals routes into further education they can aspire to progress through academic levels 4, 5 and 6 to ultimately gain degrees awarded by approved Universities and thereby qualify as Podiatrists should they so choose to follow the extra years of education.
In recent times it has become apparent that many podiatry practices are following the model of dental practices, who now almost invariably include hygienists, by having suitably qualified assistant practitioners as part of the treatment team and the NHS has for some time employed podiatry assistants in support of the registered workforce. This makes it all the more important for podiatry to have a clear understanding of the benefits that appropriately trained FHPs can bring to our industry mix be that as associates or with their own independent practices. Hence the renewed inclusion of Footnotes to help all parties to have a clear understanding of how the FHP sector operates and is evolving.
Martin Harvey, Chair Executive Committee Podiatrist Independent Prescriber
Podiatry Review Summer Issue 2021 | 15
Hi Everybody




I hope that you are all well, and your businesses are finally getting back to normal. Now that we are once again nearly out of lockdown, I thought that things would resume very quickly. This is not quite true.





































































































































































































I have just taken part in a Covid friendly First Aid Course, it was very surreal. We were not allowed to touch anybody else and had to abide by the covid rules.
Try putting yourself in the recovery position! Bandage your own leg. Put your own arm in a sling. You never know it may come in useful someday…
I hope everyone has a long hot summer, with lots of time spent with friends and family.












Best regards, Ian











Tea Tree and Skin Preparations











































































I am always asked about skin preparations, especially as many practitioners still love the old favourites, they have used from their training days. For example, Savlon, where we covered the base of our spray bottle and added water to make a lovely smelling skin prep. Of course, you cannot buy that same Savlon any longer, with the lovely aroma, but there are some very good commercial skin preparations from the chiropody/ podiatry trade houses that are cheap and good to use, such as chlorohexidine gluconate products. And like any good skin preparation, they also disinfect, kill bacteria, and reduce the risk of spreading germs, including COVID-19. Then I have been asked about tea tree oil as a skin preparation. Well, you may ask, and you might be right in thinking it will make a good skin preparation, and safer than other chemical skin preparations as it is ‘natural’, and kills bacteria, fungus, etc. This I am afraid is not always the case with tea tree oil or indeed many other essential oils.
Tea tree oil will not be miscible, which means it will not dissolve in water, unless you add some soap or detergent, and other ingredients that transforms it into a solution. This then will no longer render the preparation natural; but will make it into a very effective bathroom/ kitchen cleaner. Tea tree oil can be a good disinfectant for the bathroom and kitchen, but I would not advise it to be used as a regular skin preparation.
Although anecdotally it seems to work quite well as a treatment for nail conditions and has been used effectively to control athlete’s foot, where tea tree oil should be diluted in a carrier oil base. It can be used neat using only one drop on the nail, but the toxicity levels and chance of it reacting on a patient will gradually build up over time. Tea tree oil itself is particularly harsh on the skin and is not a good option for children, the elderly, and vulnerable patients. This is important, because it is dependent on the quantities that are used i.e., measured drops or percentage of tea tree oil in the solution.

















16 | www.iocp.org.uk
The commercial cosmetic products such as shampoos and bath oils that contain tea tree oil use a concentration of less than 1% dilution, which is considered safe, because tea tree oil and its properties denature when mixed with other chemicals. Problems do occur with larger quantities of tea tree oil dilution when made up into a solution of a lot of different, or harsh chemicals; whereby, it can cause dermatitis and reactions to skin, especially over prolonged use.
A 2012 study by Larson & Jacob in Dermatitis. 2012 JanFeb;23(1):48-9. doi: 10.1097/DER.0b013e31823e202d. The study’s abstract indicates that although:






Tea tree oil is an increasingly popular ingredient in a variety of household and cosmetic products, including shampoos, massage oils, skin and nail creams, and laundry detergents. Known for its potential antiseptic properties, it has been shown to be active against a variety of bacteria, fungi, viruses, and mites. The oil is extracted from the leaves of the tea tree via steam distillation. This essential oil possesses a sharp camphoraceous odour followed by a menthol-like cooling sensation. Most commonly an ingredient in topical products, it is used at a concentration of 5% to 10%. Even at this concentration, it has been reported to induce contact sensitization and allergic contact dermatitis reactions. In 1999, tea tree oil was added to the North American Contact Dermatitis Group screening panel. The latest prevalence rates suggest that 1.4% of patients referred for patch testing had a positive reaction to tea tree oil.
In the abstract of an older study in Australas J Dermatol. 2007 May;48(2):83-7. Rutherford, T; Nixon, R; Tam, M and Tate, B of The Skin and Cancer Foundation, Melbourne, Victoria, Australia


Tea tree oil use is increasing, with considerable interest in it being a ‘natural’ antimicrobial. It is found in many commercially available skin and hair care products in Australia. We retrospectively reviewed our patch test data at the Skin and Cancer Foundation Victoria over a 4.5year period and identified 41 cases of positive reactions to oxidized tea tree oil of 2320 people patch-tested, giving a prevalence of 1.8%. The tea tree oil reaction was deemed relevant to the presenting dermatitis in 17 of 41 (41%) patients. Of those with positive reactions, 27 of 41 (66%) recalled prior use of tea tree oil and eight of 41 (20%) specified prior application of neat (100%) tea tree oil. Tea tree oil allergic contact dermatitis is underreported in the literature but is sufficiently common in Australia to warrant inclusion of tea tree oil, at a concentration of 10% in petrolatum, in standard patchtest series. Given tea tree oil from freshly opened tea tree oil products elicits no or weak reactions, oxidized tea tree oil should be used for patch testing. Personally, as both a qualified aromatherapist and podiatrist for over 20+ years, I would not use tea tree oil as a skin preparation/ disinfectant for the feet. I would always recommend a patch test in case there is a reaction to any patient. Particularly, as I have heard and seen the results of
many reactions, allergies and burns caused by the misuse of tea tree oil. It is hard to mix in water, being an oil, it will sit on the top of the water and not mix/ dissolve so the concentration of the oil will be greater when the solution is almost finished or at the bottom of the spray bottle, which is when it can cause the most damage. Most irritations of tea tree oil are because high concentrations are used, and as already mentioned when used neat can have dermal reactions. Although, nails seem to fair ok, if a fungus or other microbial factor is present.
Most reactions will occur, because the oxidation products in the oil occur when the oils are aged or improperly stored, and especially in animals where paralysis and death can and does occur. There have been no deaths associated with humans, but as dogs and cats have more semi-permeable skin and a larger surface area than humans, it is more easily absorbed and will affect the animals’ nervous systems, etc. It does, however, affect the growing organs of children and can have a detrimental effect on the elderly and vulnerable people.
The storage of tea tree oil products is also very important and should be stored in a dark, glass bottle or containers, as tea tree oil is readily absorbed into plastic. If containers used for other purposes, it could cross contaminate products. Tea tree is known to rapidly degrade if it is exposed to air, light, and heat.
Other studies such as in the New England Journal of Medicine has stated that repeated use of tea tree oil may disrupt hormonal function and it has been revealed that boys have been warned against using hair oils and gels containing tea tree oil after three cases were found to have boys growing breasts. The growth of breasts disappeared when the boys stopped using the oils and gels. Whereby, US researchers believed tea tree oils may have hormone disrupters.
It is probably not what you wanted to hear, but the truth of the matter is that tea tree oil is a very aggressive oil that can dry out the skin and form blisters or rash. In addition, given the many studies produced in recent years and a great deal of them from Australia where tea tree oil is produced, it would be far safer not to use tea tree oil as a skin prep/ disinfectant for patient’s feet. If you have used tea tree oil as a skin preparation over the years without patients having the external, obvious signs of an allergic or dermatological reaction. It could be the unseen factors on the individuals body systems, i.e., growing organs in children, contribution to respiratory, nervous, skin, and other systemic problems in the infirmed and elderly that could be the real issue with using tea tree oil.
My suggestion is that practitioners please do not use tea tree as a skin disinfectant. As a household cleaner yes, and as an infrequent treatment for nail and fungal problems, but then only with extreme caution!
Take care, keep safe and well, best wishes.
Beverley Wright Vice Chairperson, Board
of Education
Podiatry Review Summer Issue 2021 | 17
Podiatrist all set for a new adventure
Alice Murray (CH035907) graduated from the university of Salford as a Podiatrist in 2020.
On 1st June this year she will be opening a podiatry practice within a multi-disciplinary clinic. Other team members include a Diabetologist, a Tissue Viability Nurse, a Chiropractor (also a Functional Medicine Doctor) and a Physiotherapist. Alice has recently gained registration to practice in Kenya.

The clinic’s location is in Nanyuki (Near the British Army Barracks), which is near her home and will be the only podiatry practice outside Nairobi. Alice is the third podiatrist in Kenya, the other two are based in Nairobi.
Anyone wishing to see what goes on first hand and help with donating their time by working at the Clinic alongside Alice and her team should contact her directly by email. Please also contact Alice if you want to know more about what she is aiming to achieve:
Almurray62@gmail.com
+254 722 153 771 (WhatsApp)
Sadly, Alice lost a parent from complications due to Diabetes, which stimulated an interest in Podiatry and led her to gaining this qualification. Alice also has a diagnosis of type 2 diabetes. This made her determined to help to prevent this happening to others and this will be one of the main foci of her practice.
In addition to working within her clinic, Alice will be carrying out work in the wider community, including voluntary work with poorer members of the community.
Alice has been able to raise funding for a Podiatry Chair and enough equipment to begin practice, but this has been financially difficult. Podiatry supplies and equipment are unavailable in Kenya and must be imported.
Donations of Podiatry equipment, related goods or monetary will be gratefully appreciated.
Linda Pearson, BSc.Pod.Med. F.Inst.Ch.P. President

18 | www.iocp.org.uk ARTICLE
The Venous Foot Pump: Modelling its function in gait
By Andy Horwood Independent Clinical Gait Analyst, Researcher, & Lecturer Product Designer Healthystep Ltd Visiting Lecturer & Fellow Staffordshire University
INTRODUCTION
Venous return involves internal forces of the cardiovascular system and external forces derived from breathing, muscle contraction and gait. The venous foot pump is important in lower limb health, and systemic wellbeing. Its interaction with cardiovascular disease must be considered during patient management.

The Physiology of Blood Vessels and Haemodynamics
Systemic blood leaves the left side of the heart to enter large elastic-walled arteries. These divide into medium sized arteries, which in turn divide into arterioles. As arterioles enter tissues, they divide into countless microscopic vessels called capillaries, where exchanges of nutrients and waste occur between blood vessels and tissues. Before leaving the tissues, the capillaries unite to form venules, which in turn unite to form progressively larger veins, returning blood to the right side of the heart (Fig. 1). Blood pressure averages 90 mmHg in the proximal aorta, but returns to the heart at pressure close to 0 mmHg (Lie et al, 1989; Lee et al, 2013).
Figure 1 Schematics of the cardiovascular system (left) and capillary exchange (right). Images www.healthystep.co.uk


Podiatry Review Summer Issue 2021 | 19 CPD 5 page article
The Anatomy and Biomechanics of Arteries
Arteries are lined with simple squamous epithelial cells overlaid with elastic tissue, a layer of elastic fibres within smooth muscle, and an outer layer composed of elastic and collagen fibres. Sometimes a further elastic layer separates the middle layers from the external coating. Collagen fibres wind around the artery in two helices with opposite pitch (Murphy, 2014), giving arteries heart pump-linked elasticity (storing potential energy) and recoil (applying force through kinetic energy). When the ventricles eject blood, the arteries expand to accommodate the extra blood, and as the ventricles relax, the vessels recoil, pumping blood forward. Smooth muscle only controls stiffness and compliance of the artery wall in response to demands (Liu et al, 1989).
Large arteries (aorta, common carotid, vertebral, and common iliac arteries) are termed elastic arteries. They are thin walled, have little smooth muscle, but containing many elastic fibres. Medium sized arteries feed blood to tissues from the large vessels to the arterioles. Arterioles have little elastic tissue, but extensive smooth muscle that plays a key role in controlling blood flow and pressure, through vasoconstriction and dilatation. Capillaries are extensive in metabolic tissues such as skeletal muscle, nerves, kidneys, lungs, and liver. Few are found in tendons and ligaments, and usually none are present in cartilage and epidermis. Capillaries are composed of a single layer of endothelial cells on a basement membrane to allow blood-tissue gas and nutrient exchange to take place.
Venous Anatomy
At rest, around 60% of blood volume is within veins and venules, but this reduces under sympathetic nerve impulses that constrict veins, releasing more blood for skeletal muscle during exercise. Venules unite and drain capillaries after nutrient/waste exchange is complete. Blood pressure entering venules, is around 16mmHg, decreasing towards the heart. Veins’ walls are extremely thin compared to the arteries, although the connective tissue outer layer is thicker. Unlike arteries, they are not subjected to high pressures, and as a consequence are stiffer and less elastic. Veins contain bicuspid valves that prevent reflux of blood to help overcome the effects of gravity (Meissner, 2005).
There are three groups of veins: superficial veins running close to the skin, deep veins running deeper within the muscles and body tissues, and the perforating veins that link the superficial and deep veins together. The superficial veins drain through perforating veins towards the deep veins. Valves in the perforating veins orientate to prevent blood flowing back towards the superficial veins and are most common in the lower limbs (Meissner, 2005). In the foot, deep veins flow towards the superficial veins with reversed orientated valves (Bojsen-Møller, 1999; Meissner, 2005; Ricci et al, 2014).
Blood moves via hydrostatic pressure (Lee et al, 2013), where fluid flows from areas of high-pressure (arteries) towards areas of low-pressure. Tissue fluid enters blood via osmotic pressure, which draws fluid out of the interstitial spaces (Fig. 1). Fluid balance can be disturbed through increasing blood hydrostatic pressures due to cardiac failure, vein valve dysfunction, or blood clots. Protein
loss from burns, malnutrition, or liver and kidney disease will change the osmotic blood pressure, keeping fluid in tissues. Excess interstitial fluid is called oedema. Blockage or damage to the lymphatics can results in extremely disfiguring severe local oedema.
To avoid leg oedema, gravity must be overcome. The valves of the veins prevent reflux towards the feet but efficient venous blood flow requires three other mechanisms. Changes in thorax and abdomen pressures during breathing create a respiratory pump action. During inspiration, the diaphragm moves downward decreasing pressure in the thoracic body cavity, while it increasing pressure in the abdomen. Blood is pulled towards the lower chest cavity pressure superiorly. On expiration, the valves prevent the blood flowing back, as the pressures reverse (Takata and Robotham, 1992; Miller et al, 2005). Muscle activity creates skeletal muscle pumps, moving blood as muscles contact. Ground reaction forces (GRF) on the foot during stance and gait create a foot pump. These techniques and hydrodynamic flow rely on healthy functional vein valves (Horwood, 2019).
Venous Return from the Lower Limbs
Lower limb deep veins exist in pairs (venae comitantes), and are more complicated and variable than their corresponding arteries, with which they share their name (Meissner, 2005; Ricci et al, 2014; Ricci, 2015). Superficial veins (e.g. great and small saphenous) run above the deep fascia, linked to the deep veins by an average of 64 perforated veins between the ankle and the groin (Meissner, 2005). This allows blood to flow by aspiration into the deep veins (Ricci, 2015). Within the deep veins of the calf lie intramuscular venous sinuses that act as collecting sites for the muscular pump of the calf.
Muscular pumps work by compressing stiff vein walls running through the muscles and their fascial compartments, producing integrated flow out of the lower limbs (Meissner 2005; Ricci et al, 2014; Ricci, 2015). On contraction, muscles tighten the fascia and compress the veins raising pressures within the muscle compartment. Proximal valves open and blood is milked into the next section of vein towards the heart, with the valves preventing reflux on muscle relaxation (Fig. 2). This creates volumetric pumps which can reach pressures of over 200 mmHg in the calf, making it the most powerful lower limb venous pump (Meissner, 2005; Ricci, 2015).

20 | www.iocp.org.uk CPD 5 page article The
gait (continued)
Venous Foot Pump: Modelling its function in
Figure 2 A schematic of the muscle pump function. Image www.healthystep.co.uk.
The Foot and Calf Pump in Venous Return


Gait biomechanics and cardiovascular physiology meet directly in the action of the foot pump (Horwood, 2019). Blood pools in the plantar vault (arch) and heel when the leg is vertical and non-weightbearing (Gardner and Fox, 1983), thus tending to gather blood when sitting. Having perforating veins valves that shut towards the deep veins and open towards the superficial ones, means blood runs from deep to superficial in the foot (Bojsen-Møller, 1999; Meissner, 2005; Ricci et al, 2014). In the plantar heel, the veins mainly run transversely. Hence on heel loading, the blood is squeezed towards the sides of the foot and not towards the forefoot (Bojsen-Møller, 1999).

The plantar surface of the foot deforms under GRF during gait, allowing the heel and forefoot to be used as ‘compression pumps’, expelling blood into calf veins in concert with the action of plantar intrinsic muscles pumping (Broderick et al, 2010; Corley et al, 2010). GRFs acting on deep plantar veins at each step works like a hydraulic pump, with the valves in the perforating veins preventing reflux to the deep foot veins on offloading (Horwood, 2019). Each stroke of the foot and calf pump in ‘static’ weightbearing on the foot is estimated to move approximately 33ml blood into the popliteal vein at the knee, around 20% of this flow arising from the veins passing the ankle (Broderick et al, 2010). Higher gait forces likely increase this (Ricci et al, 2014), causing blood pressure in the superficial and deep veins of the leg to rise abruptly with each step (Bojsen-Møller, 1999). The foot, calf, and thigh muscle pumps overcome gravity induced pressures of around 90 mmHg in standing, and around 20 mmHg during walking (Reeder et al, 2013). Any failure in any one of these pumps through valve dysfunction or vein obstruction will cause a compromise in venous return.
plantar foot at heel strike may even have a small effect on the mechanical behaviour of the plantar fat pad (Aerts et al, 1995; Gefen et al, 2001; Weijers et al, 2005). Heel strike initiates the passive foot pump as its venous plexus is compressed (Fig. 4), driving the blood to the heel margins through the transversely orientated heel veins, up towards the foot and calf’s superficial veins (Horwood, 2019).
Figure 4 The foot pump at heel strike. Image www.heathystep.co.uk.
Image www.healthystep.co.uk.
Ankle motion help propel blood during the stance phase (Ricci, 2015). Ankle dorsiflexion (under eccentric calf muscle contraction) draws blood out of the superficial veins via those perforating the fascial envelope, taking blood to the deep calf veins, to propel it up the leg (Gardner and Fox, 1983; Ricci, 2015). The foot and calf venous pumps can therefore be modelled together, providing distinct periods of passive and active component activity during gait (Horwood, 2019). During swing phase, the foot is nonweightbearing, permitting gravity and swing centrifugal forces (Fig. 3) to temporarily pool venous blood in the feet (Horwood, 2019). The presence of blood pooling in the
At forefoot contact, the forefoot venous plexus undergoes compression, driving blood flow towards the superficial and proximal veins of the midfoot (Fig. 5). This process is aided by natural motions of pronation, increasing soft tissue compression by enlargement of the surface contact area (Horwood and Chockalingam, 2017; Horwood, 2019). During single-limb support phase, blood pumping continues under the GRF-body weight induced foot compression, until activation of the triceps surae and other ankle plantarflexors initiate engagement of the skeletal calf muscle pump (Horwood, 2019). This activity continues through late midstance in concert with active plantar foot intrinsic muscles (Horwood, 2019). Despite decreasing compression on the heel, increasing compression of the forefoot maintains compression pumping (Horwood, 2019). With foot vault lowering, the foot stiffens (Bjelopetrovich and Barrios, 2016) facilitating and improving propulsion energetics producing a large forefoot GRF (Cunningham et al, 2010; Usherwood et al, 2012).

Figure 5 The foot pump at midstance. Image www.healthystep.co.uk.
At heel lift (Fig. 5), plantarflexion power expresses shortening calf muscle fascicle length, maintaining muscle pumping and generating high GRF compression forces on the forefoot. The offloaded heel’s venous plexus may start to refill again in readiness for the next heel strike.
Podiatry Review Summer Issue 2021 | 21
Figure 3 Centrifugal and gravitational forces pooling blood in feet during swing phase.
The Venous Foot Pump: Modelling its function in gait (continued)
Active muscular pumping from the plantar intrinsic muscles will continue until the forefoot is unloaded (Horwood, 2019).
Dysfunction of Venous Return
Figure 6 The foot pump during terminal stance. Image www.healthystep.co.uk.


Gait perturbations may influence venous return, for patterns of foot compliance and stiffening are likely to be significant in driving the active and passive elements of the foot pump (Horwood, 2019). There could be conflicts between the mechanisms of the foot and calf pumps function that prevent harmonious unifunctional lower limb pumping, while the foot pump efficiency itself may have implications in therapy for leg ulcers that use foot-free bandaging (Reeder et al, 2013; Ricci, 2015).
Deficient venous return (venous reflux) can lead to chronic venous insufficiency. This can result from blockage of veins (such as a blood clot/thrombus), valve malfunction, or failures of the respiratory musculature, skeletal muscles, and/or foot pumps. Most venous reflux affects superficial and perforating veins, but sometimes just deep veins or all three vein-types are affected (Labropoulos et al, 1996). Leg veins dysfunction causes aching, foot-ankle swelling, skin changes, and ulcers (Labropoulos et al, 1996), which can be mild or incapacitating (Brandjes et al, 1997; Reeder et al, 2013). Skin changes, including discolouration from venous eczema, varicose veins, and itchy thrombophlebitis. Left untreated, venous reflux can increase the risk of serious infections in the feet and legs. Blood clots can form in sluggish flow of veins, causing thrombosis, causing local damage at the thrombus site. Blood clots risks breaking up in loose clumps that can then flow to small arteries in the lungs or the brain to block them. This can result in pulmonary embolism and strokes.
Fig 7 The activity of the foot and calf pumps in venous return during gait. Image www.healthystep.co.uk.

22 | www.iocp.org.uk
CPD 5 page article
The foot may also suffer from valve incompetence. Gardner and Fox (1983) reported a case of intravascular thrombi in the foot presenting clinically as plantar heel pain. It is unknown how common a phenomenon this is because the foot is not examined routinely for thrombus at post-mortem. Deep vein thrombosis (DVT) or venous thromboembolism (VTE) is common in the calf. A hot red swollen (painful) calf without a significant known injury event should be considered a DVT until proven otherwise, requiring urgent intervention. Even in seemly healthy individuals, long periods of sitting and inactivity are associated with emboli formation especially after surgery (Assareh et al, 2014) but also during long-distance flying (Hughes et al, 2003). Around 60% of people who develop a DVT go on to develop post-thrombotic syndrome within 24 months, developing leg swelling, pain, and ulceration (Brandjes et al, 1997).
Clinical Solutions
Graduated compression stockings influence venous return pressures. They apply gradually decreasing pressure the higher they go up the leg (hence the name ‘graduated’). Compression stockings reduce the risk of developing more serious post-thrombotic syndrome after a DVT by around 50% (Brandjes et al, 1997; Prandoni et al, 2004). They also improve venous ulcer healing rates (Reeder et al, 2013; Nelson and Bell-Syer, 2014). Compression hosiery is a well-proven biomechanical treatment in venous disease (Rabe et al, 2018). Combining compression stocking and lower limb exercises, including regular walking, can help manage venous insufficiency through biomechanical principles (Horwood, 2019).
Figure 8 Modern ‘foot pump friendly’ graduated compression hosiery avoids toe compression restricting intrinsic foot muscle activity. Images www.healthystep.co.uk.

REFERENCES:
Aerts P, Ker RF, De Clercq D, Ilsley DW, Alexander RM. (1995). The mechanical properties of the human heel pad: a paradox resolved. Journal of Biomechanics. 28(11): 1299-1308.
Assareh H, Chen J, Ou L, Hollis SJ, Hillman K, Flabouris A. (2014). Rate of venous thromboembolism among surgical patients in Australian hospitals: a multicentre retrospective cohort study. BMJ Open. 4(10): e005502.
Bjelopetrovich A, Barrios JA. (2016). Effects of incremental ambulatoryrange loading on arch height index parameters. Journal of Biomechanics. 49(14): 3555-3558.
Bojsen-Møller F. (1999). Biomechanics of the heel pad and plantar aponeurosis. (Chapter 9.) In: Disorders of the Heel, Rearfoot, and Ankle. [Eds.: Ranawat CS, Positano RG.] Philadelphia: Churchill Livingstone. pp. 137-143.
Brandjes DPM, Büller HR, Heijboer H, Huisman MV, de Rijk M, Jagt H, et al. (1997). Randomised trial of effect of compression stockings in patients with symptomatic proximal-vein thrombosis. The Lancet. 349(9054): 759-762.
Broderick BJ, Corley GJ, Quondamatteo F, Breen PP, Serrador J, ÓLaighin G. (2010). Venous emptying of the foot: influences of weight bearing, toe curls, electrical stimulation, passive compression, and posture. Journal of Applied Physiology. 109(4): 1045-1052.

Corley GJ, Broderick BJ, Nestor SM, Breen PP, Grace PA, Quondamatteo F, et al. (2010). The anatomy and physiology of the venous foot pump. The Anatomical Record. 293(3): 370-378.
Cunningham CB, Schilling N, Anders C, Carrier DR. (2010). The influence of foot posture on the cost of transport in humans. Journal of Experimental Biology. 213(5): 790-797.
Gardner AMN, Fox RH. (1983). Venous pump of the human foot Preliminary report. Bristol Medico-Chirurgical Journal. 98(3): 109-112.
Gefen A, Megido-Ravid M, Itzchak Y. (2001). In vivo biomechanical behavior of the human heel pad during the stance phase of gait. Journal of Biomechanics. 34(12): 1661-1665.
Horwood AM, Chockalingam N. (2017). Defining excessive, over, or hyperpronation: A quandary. The Foot. 31: 49-55.
Horwood A. (2019). The biomechanical function of the foot pump in venous return from the lower extremity during the human gait cycle: An expansion of the gait model of the foot pump. Medical Hypotheses. 129: https://doi. org/10.1016/j.mehy.2019.05.006
Hughes RJ, Hopkins RJ, Hill S, Weatherall M, Van de Water N, Nowitz M, et al. (2003). Frequency of venous thromboembolism in low to moderate risk long distance air travellers: the New Zealand Air Traveller’s Thrombosis (NZATT) study. The Lancet. 362(9401): 2039-2044.
Labropoulos N, Touloupakis E, Giannoukas AD, Leon M, Katsamouris A, Nicolaides AN. (1996). Recurrent varicose veins: Investigation of the pattern and extent of reflux with color flow duplex scanning. Surgery. 119(4): 406-409.
Lee BK, Lee HY, Jeung KW, Jung YH, Lee GS. (2013). Estimation of central venous pressure using inferior vena caval pressure from femoral endovascular cooling catheter. American Journal of Emergency Medicine. 31(1): 240-243.
Liu ZR, Ting CT, Zhu SX, Yin FC. (1989). Aortic compliance in human hypertension. Hypertension. 14(2): 129-136.
Meissner MH. (2005). Lower extremity venous anatomy. Seminars in Interventional Radiology. 22(3): 147-156.
Miller JD, Pegelow DF, Jacques AJ, Dempsey JA. (2005). Skeletal muscle pump versus respiratory muscle pump: modulation of venous return from the locomotor limb in humans. Journal of Physiology. 563(3): 925-943.
Nelson EA, Bell-Syer SEM. (2014). Compression for preventing recurrence of venous ulcers. Cochrane Database of Systematic Reviews. 2014(9):CD002303.
https://doi.org/10.1002/14651858.CD002303.pub3
Prandoni P, Lensing AWA, Prins MH, Frulla M, Marchiori A, Bernardi E, et al. (2004). Below-knee elastic compression stockings to prevent the postthrombotic syndrome: a randomized, controlled trial. Annals of Internal Medicine. 141(4): 249-256.
Rabe E, Partsch H, Hafner J, Lattimer C, Mosti G, Neumann M, et al. (2018). Indications for medical compression stockings in venous and lymphatic disorders: An evidence-based consensus statement. Phlebology: The Journal of Venous Disease. 33(3): 163-184.
Reeder SWI, Maessen-Visch MB, Langendoen SI, de Roos K-P, Neumann HAM. (2013). The recalcitrant venous leg ulcer a never ending story? Phlebologie. 42(6): 332-339.
Ricci S, Moro L, Incalzi RA. (2014). The foot venous system: anatomy, physiology and relevance to clinical practice. Dermatologic Surgery. 40(3): 225-233.
Ricci S. (2015). The venous system of the foot: anatomy, physiology, and clinical aspects. Phlebolymphology. 22(2): 64-75.
Takata M, Robotham JL. (1992). Effects of inspiratory diaphragmatic descent on inferior vena canal venous return. Journal of Applied Physiology. 72(2): 597-607.
Usherwood JR, Channon AJ, Myatt JP, Rankin JW, Hubel TY. (2012). The human foot and heel-sole-toe walking strategy: a mechanism enabling an inverted pendular gait with low isometric muscle force? Journal of the Royal Society: Interface. 9(75): 2396-2402.
Weijers RE, Kessels AGH, Kemerink GJ. (2005). The damping properties of the venous plexus of the heel region of the foot during simulated heelstrike. Journal of Biomechanics. 38(12): 2423-2430.
Podiatry Review Summer Issue 2021 | 23
Are Podiatry On-Line Consultations a Good Idea?
David
The question Are podiatry on-line consultations a good idea? has not as yet had any great impact in our own press. Peter Russell posted his take on the ‘Remote GP’ in a recent Medscape article (2021) [1] . As reports have concerns about the impact on GP practices.
If these questions cannot be answered perhaps we can draw upon activities from other practices. This article follows on from my article providing advice - Giving advice on-line as a podiatrist [2]. The term video-conferencing (VC) is used specifically as part of tele-medicine and on-line consultations.
Of course on-line consultations might bring a range of different interpretation but we are really only at a technological junction where choosing tele-medicine over face to face contact is being raised for different purposes. Direct interfacing between two people forms the basis of VC and here many will be familiar with the benefits of ZOOM or MICROSOFT TEAMS. Tele-medicine is not new. Surgeons and specialists have used different forms for many decades. Consulting over patient images and results of tests has been common. As technology has improved so have the opportunities that tele-medicine brings.
“Between March and July [2020], NHS Digital estimated there were 102 million GP appointments, half of which were recorded as being over the phone or through video calls,’ writes Peter Russell.”[1]

Exploring on-line podiatry
“Foot health providers are not automatically sign-posted”
I wanted to look at the subject to raise the idea that there might be a place for VC in podiatry. Would it be called telepodiatry? It might be useful to look at the subject from a broad perspective. The precedent arises all the while access to the GP surgery provides a risk. This limits face to face contact with the GP. At present applying online, phoning the surgery or contacting NHS 111 all exist. The problem with NHS 111 (before the pandemic) was that ‘foot conditions’ tended to be
24 | www.iocp.org.uk ARTICLE
What do the two main organisations think? Is there enough data to reflect on performance to date in podiatry? Has Covid-19 made a difference to our attitudes?
R Tollafield
referred back to the GP. The main arena where recognition of good practice around foothealth is encompassed around the diabetic patient. Other areas of foot health don’t appear to be recognised and NHS111 will almost certainly use any other referral resource other than podiatry. And so it would appear that podiatry as first line foot health providers are not automatically sign-posted.
The Telephone Telephone consultations have certainly increased. As a patient I have participated in a skin assessment using photos I uploaded from my iPhone after speaking to a doctor. I went through the reception triage process first, then the GP phoned back. Speaking to a colleague before COVID, his view was certainly cool in responding positively about his ‘surgical’ practice and the idea of VC. So are there any positives?
Changing the shape of healthcare delivery
who don’t have access to services.” It becomes clear that she feels they are only seeing the tip of the iceberg and it comes down to being referred in a timely fashion. When asked about podiatric input she was very positive. As far as satisfaction ratings have been concerned these have come in at 98% for the remote service. For general podiatry and those who may not always deal with diabetic foot problems she believes upskilling and triaging patients using defined tools could be followed up with a VC with a patient in their home.
The Downside
Not everyone buys into the idea of telemedicine. In contrast with the positive overtures brought about by strong evidence in Scotland for well-defined areas of medicine, others take a different view. Overall rapport is not established partly because we cannot see each other. Loss of identity and warmth lead to less value than digitised video link. The Royal College of General Practitioners is far from in favour according to Professor Marshall. The loss of confidence or personal relationships can lead from lack of visual empathy. However there are those like Amjad Khan, director of postgraduate GP education for Scotland, who believes that such consultations are likely to stay.
Consultations by ’phone are shorter and cover fewer problems. Even when we could see GPs before Covid, one GP obsessed about only talking about one medical event or episode without an extended appointment. As patients we deemed this poor practice[5]. The question lies with overcoming these perceived weak trends and not seeing them as ‘factory led.’
Fiona Main (Diabetes Specialist Podiatrist) alongside Prof. Sandra MacRury conducting a remote foot consultation with a patient and podiatry colleague in the community.
If you wondered whether telemedicine was here to stay, my interview this month with Sandra MacRury, Professor in Clinical Diabetes and Head of Rural Health & Wellbeing, soon made it clear. Diabetes and podiatry are intimately linked in preventing amputations. “We’ve been running video conferencing consultations in our general diabetes service for many years”.
MacRury and her team have perfected a system whereby patients are visited by professionals, including podiatrists such as Fiona Main. [3,4] Using portable modems and tablets much of a consultation can be performed from a distance but importantly in the patient’s home. The whole process is designed as an integrated pathway. Visits can be linked back to clinics so that expertise can be offered and any cases, including ulcers can be managed and evaluated following treatment programmes.

“A few years ago we started thinking about how we could really improve equity of access for patients in rural areas with diabetic foot disease.” She points out the huge distances of hundreds of miles away. “It’s quite daunting for older people
Dr Roger Neighbour, a former RCGP president, who now lectures on consulting skills and general practice, warned of the dangers of evolving the system to the stage where the starting point was “digital until proven otherwise”. Neighbour considers that “we’re in danger of losing something very important... It behoves the old ones amongst us to make sure that the rising generation really do get to know and experience the reward and the fulfilment of doing face-to-face consultations, because once that’s lost, it’s lost forever.”
Research and making the case
The economic and social research council is part of UK Research and Innovation (UKRI) and is a large organisation looking at research on economic and social issues. Professor Trisha Greenhalgh and a team were awarded to look at the effectiveness of remote care during the COVID-19 pandemic in collaboration with the Nuffield Trust and University of Plymouth. “The thing about medicine is that it is governed not by hard and fast rules [and] standard operating procedures, but by professional maxims or rules of thumb, which apply in some but not all circumstances. But the question is, what are those rules of thumb, and how can we balance stipulating them explicitly, versus leaving scope for the 75% of patients who are
“It’s a skill and communication that podiatry is going to have to learn and develop”
Podiatry Review Summer Issue 2021 | 25
REFERENCES
(1 Russell, P. The Remote GP Consultation: No Turning Back? - Medscape - Feb 15, 2021. BMJ. 2020;368:m998. DOI: https://doi.org/10.1136/bmj.m998
(2) Tollafield DR Giving advice on-line as a podiatrist. 2020;February http://consultingfootpain.co.uk/giving-advice-on-line-as-a-podiatrist/
(3) Main,F, Zubala, A, Gorman, J, Jones, S, Jenny Hall,J, Macfarlane, D, MacRury,S. Technology-enabled remote management of diabetes foot disease and potential for reduction in associated health costs: a pilot study. Journal of Foot and Ankle Research (2021) 14:7 https://doi.org/10.1186/s13047-02000444-6
(4) MacRury,S, Stephen,K, Main,F, Gorman,J, Jones,S, Macfarlane,D. Amputations in People with Diabetes (RAPID): Evaluation of a New Care Pathway. Int. J. Environ. Res. Public Health 2018, 15, 999; doi:10.3390/ijerph15050999
(5) Tollafield, DR Communication with patients in Selling Foot Health as Podiatry 2020;26-27
(6) Greenhalgh T, Shaw S, Wherton J, et al. Real-World Implementation of Video Outpatient Consultations at Macro, Meso, and Micro Levels: Mixed- Method Study. J Med Internet Res 2018;20(4): e150. Available from: DOI: 10.2196/jmir.9897
(7) Royal College of General Practitioners. Guidelines https://www.rcgp.org.uk/policy/rcgp-policy-areas/-/media 2ED99A2DBEE424788E12D17FF73A55F. ashx
Bibliography
General Medical Council. Remote consultations. Available from: https://www.gmcuk.org/ethical-guidance/ethical-hub/ remote-consultations
NHSX. Information Governance. Available from: https://www.nhsx.nhs.uk/key-informationand-tools/informationgovernance- guidance
Health and Care Professions Council (HCPC). Information on providing online services. Available from: https://www.hcpcuk.org/registration/meeting-our-standards/informationon-providing-online- services/
What is Telemedicine? https://evisit.com/resources/what-is-telemedicine/
With special thanks to Professor Stuart Baird and Professor Sandra MacRury, Ms Fiona Main, The Royal College of Podiatry and the Institute of Chiropodists & Podiatrists, Phil Hendy, Plymouth University for sharing their views. The idea for this article has been influenced by the recent February 2021 Medscape article ‘No Turning Back’. This has been a podiatric reflective practice article written for 31/3/21and edited for Podiatry Review.
David Tollafield is a retired Consultant Podiatric Surgeon and now author and journalist in foot health medicine (www.consultingfootpain.co.uk). His latest book is Podiatrist on a Mission. The Genesis of a New Profession.

Podiatry Review Summer Issue 2021 | 27
Gary Strong, MCPara, National CPD Lead, chats to… Tony Stone

MCPara, Head of Clinical Development (Emergency and Critical Care) at the College of Paramedics

Gary: Tony, thanks for taking some time to chat, this is a great way for me and our members to get to know you better. You were recently appointed to this new role…can you tell us what it’s all about?
Tony: Thank you Gary, it is great to chat to you. I started in this role at the beginning of the year – I cannot believe how quickly time has passed! The purpose of the role is to lead on all aspects of clinical development for members across the UK who are working in emergency and critical care settings. This will include development of educational activities, curriculum guidance and supporting relevant continuing professional development (CPD) opportunities. One of my biggest aims, working with colleagues and relevant stakeholders, is to create an approved national career development pathway for those who wish to specialise in critical care.
Gary: Tell us about your career to date.
Tony: Following a quarter life crisis in 2007, I retrained as a paramedic at the University of Hertfordshire. After graduation, I worked in the West Hertfordshire area where I undertook several roles as my experience grew. These included secondments as a rapid response vehicle (RRV) paramedic, clinical field operations trainer, education and training officer, in addition to a secondment in the ambulance control room, supporting triage of non-lifethreatening calls. In 2014, following a gruelling assessment and interview process, I was successful in joining Essex & Herts Air Ambulance (EHAAT) as one of their HEMS Critical Care Paramedics (CCP) a career achievement I am exceptionally proud of.
In 2017, EHAAT created their Patient Liaison Manager (PLM) role, following the success of the role at London’s Air Ambulance. I was thrilled to move into this role, along with one of my much-respected CCP colleagues, Adam Carr. Together, we developed an effective patient and family liaison service answering questions patients or families had about their pre-hospital journey, signposting them to appropriate support organisations (of which there are many) and learning about the patient or family pre-hospital experience and feeding this back into our governance process. I have no doubt that we have improved the postincident experience for many patients and their families, and I am glad that this role has now been developed by several HEMS and critical care services across the UK.
My role at the College is part-time so I am pleased that I can continue working at EHAAT, although now in a patient safety and quality role, as well as maintaining weekly clinical shifts.
Gary: Emergency and critical care includes a spectrum of different roles, I think. What can you tell us about the different opportunities available to paramedics working in this space?
Tony: Never has there been so many different opportunities for paramedics, and it is wonderful. It is impossible to list them all, but it includes pre-hospital roles (e.g. ambulance & RRV, specialist and advanced paramedic (critical care), HART, HEMS, BASICS etc.), in-hospital roles such as Advanced Clinical Practitioner (ACP) with credentialing opportunities currently through either the Royal College of Emergency Medicine (RCEM) or the Faculty of Intensive Care Medicine (FICM), not to mention retrieval and inter-hospital transfer services, expedition medicine and of course the Armed Forces. I am sure there are more, and this doesn’t even take into account the primary and urgent care roles Helen Beaumont-Waters (Head of Clinical Development Primary and Urgent Care) mentioned in the last issue of this magazine. It really is an exciting time to be a paramedic.
Gary: Emergency care is what many would regard as ‘traditional’ paramedic work. Yet now, for the average ambulance paramedic, it represents only a small amount of their workload, and many feel under-prepared. How can we deal with this challenge?
Tony: There is no doubt that core front-line 999 ambulance work has changed significantly over the years. Paramedics and ambulance service colleagues truly are a “Jack of all trades” and I have no doubt it is this adaptability that has paved the way for such rapid development of our profession. However, with often limited exposure to managing high acuity injury or illness, I understand why many members might feel under-prepared when they are tasked to such incidents. I feel that regularly embracing CPD and training opportunities (including physical scenariobased training), developing post-incident feedback systems and having consistent access to specialist or senior support will go some way to addressing this.

28 | www.iocp.org.uk
ARTICLE
Gary: Many new entrants to the profession have ambitions to work at what they regard as the ‘high end’ of practice. What would you say to students who are really keen to head towards a career in critical care?
Tony: As I previously mentioned, opportunities for paramedics both in and outside of ambulance services are increasing. I strongly believe that, regardless of how someone wishes to specialise in the future, a strong foundation of core paramedic experience is essential. Many (but I appreciate not all) students graduate in their early 20s – therefore have the potential for a 40-year paramedic career. I would strongly encourage students not to rush into specialist roles and to focus on developing their core paramedic skills; it is these skills that will enable someone to excel in a specialist role.
I think it is fair to say, critical care roles are often hugely competitive to get into. I would encourage those interested to grab as many different opportunities as possible (teaching, research etc.) to build their CV (with the caveat in my previous statement). Also look to become involved with your local air ambulance or BASICs scheme (or similar) many of which run training or governance days. Finally, it is important to develop your non-technical skills as these are often also tested during assessment stages for critical care roles. It is all about doing what you can to make yourself stand out from the many other applicants.
continue to improve teamwork, communication, and decision-making skills within our profession.
Gary: Emergency and critical care has always been a multidisciplinary affair. In my early years as a paramedic, I recall being very well supported by the West Midlands Care Team at larger incidents, working alongside doctors and nurses at scene. What are your thoughts on interprofessional collaboration, its benefits, and challenges?
Tony: Pre-hospital emergency and critical care should absolutely be a multidisciplinary environment. AHPs, nurses and doctors all bring unique qualities to patient care, just like the in-hospital setting. However, I think it is important that comprehensive training and education is delivered to prepare clinicians, regardless of profession, for the unique challenges of the pre-hospital environment.
It is fantastic to see rapidly expanding scope of practice, education opportunities, and governance from some employers of paramedics working in specialist or advanced roles. With regards to critical care, I am confident that, with time, we will see paramedics safely delivering procedures and interventions that are currently only provided by our doctor colleagues.

Gary: Tell us about your vision for your role. What can the College do to support the growth and development of paramedic practice in emergency and critical care?
Tony: I am truly delighted to have started in this new post this year and I’m looking forward to championing clinical development for paramedics who work in emergency and critical care settings.
Soon, I am to start a scoping exercise to investigate what pre-hospital paramedic-delivered critical care currently looks like across the UK. I am hoping this work, along with the feedback from the recent critical care workstream development survey will help the College go on to produce a nationally-agreed development framework for those working in critical care.
Gary: One of the challenges I have observed over the years is the need for critical care teams (e.g. air ambulance) and road crews to form a high performing team on scene, rapidly. I sense these days that a lot of the old communication barriers have been broken down, but I suspect there is still work to do on this. Can you comment?

Tony: Scenes which involve patients who are critically ill or injured are often stressful for all involved. I think it is this ‘stress’ that can sometimes cause communication to not be as effective as it could be. That said, training and awareness around CRM, human factors, hierarchy gradient and communication skills has greatly increased in recent years, and I do feel that the traditional perceived barriers between different pre-hospital teams have mostly been broken down. Everyone attending these challenging incidents wants the best outcome for the patient(s) and it is essential that all on scene work well together to deliver excellent prehospital care. Going forward, I feel it is vital to champion diversity within specialist teams as this will undoubtedly
My long-term vision is clearly defined, nationally agreed roles (training and education requirement, scope of practice etc.) for specialist, advanced and consultant paramedics in critical care. Maybe even one day we will have our registration annotated to reflect this.
Gary: Thank you Tony. It’s great having you on the team.
Podiatry Review Summer Issue 2021 | 29
PODARICK










NAILS IT!
Podarick can you help me? I recently heard that wearing lanyards and ID badges is a safety hazard and should be removed before driving, is this true?
Podarick says: Wearing lanyards while driving is a little-known hazard that employers and employees should be aware of. The UK police released a warning on the potential dangers of wearing a lanyard while driving. And for those wearing lanyards and ID badges to remove them when leaving work or going onto the next job for both safety and security reasons; and before starting any car journey, as it could reduce the risk of serious injuries.
In 2019 Dorset Police reported that drivers sustained serious injuries in several traffic accidents, because of their lanyards. The Police have advised people who wear lanyards, where possible to use breakaway lanyards that will unclip themselves if caught or stuck.
Dorset Police stated that “In one incident, a driver involved in a minor car accident was left with a collapsed lung when the force of the deployed airbag pushed the lanyard into the driver’s chest. Had the driver not been wearing their lanyard at the time, they would have likely walked away relatively unharmed.” “In another incident, an NHS worker was wearing a lanyard full of a set of keys for her medicine cabinets and lockers. This time the force of the airbags caused the keys to perforate the driver’s bowel. The injury resulted in a 6-week hospital stay, and 6 months off work.”
Driving is not the only situation where lanyards can pose a safety risk. A risk assessment should be used to assess whether lanyards and ID badges pose a safety risk to those who wear them in their occupations, so that a safer alternative can be considered. People working around machinery and large equipment should not wear lanyards due to the risk of them getting stuck and causing serious injury to the wearer. For example, a woman’s lanyard got caught in the conveyor belt she operated, and it pulled her in until she could not breathe. There are other examples with children and the elderly, which could cause serious harm or injury, so caution should be of the upmost importance.
Send your Nail Clippings to Podarick:

c/o The Institute of Chiropodists & Podiatrists 150 Lord Street, Southport, PR9 0NP


30 | www.iocp.org.uk
ARTICLE
It






































































Meet the Author



















Doctor Bharti (Doctor B) MBE PhD is a multi-award winning podiatrist who has is on a mission of making foot care wisdom viral. She is a regular author, speaker and contributor to the media on all matters feet, and is especially passionate about supporting Women in Business and serves as an ambassador to Women’s Enterprise Scotland. She was awarded the honour of an MBE in 2018 for services to Podiatry.

Follow Doctor B @thefootexpert on Instagram.
When I’ve read the online forums in the past few months, Podiatry and Foot Health Practices seem to have “toes coming out of their ears” and are experiencing a very busy period following the easing of lockdown restrictions. Whilst patients might have all sorts of foot problems, often what clinicians find most frustrating is dealing with phone calls and patient enquiries whilst also trying to provide their patients with the best care.

When business is booming, there’s perhaps no employee more valuable than your receptionist. Not only can they take tedious admin tasks off your plate, but they also provide a friendly face for patients visiting the practice and enable the clinician to focus on what they do best.
I’ve always believed that running a healthcare practice is a like playing a team sport. Like most teams we have the team manager, team captain, the players, and others who support the team to play at their best. What if I told you that in a healthcare practice that the receptionist is the most important hire you should make in your clinic, even more important than your clinicians!… stay with me, I’ll explain…
New patients and existing patient nurturing is vital to the success of our clinics and directly affects your bottom line. Whilst a ‘flashy’ website or striking décor may influence the overall patient experience it can never surpass an engaging interaction with a “caring and chatty” person behind the front desk.
First impressions really do matter and your receptionist defines the overall culture of your practice with a prospective patient who calls to schedule an appointment. Every new missed patient opportunity can cost your practice on average of £400-£1000 annually depending on your price structure… multiply that by 5 new patient enquiries not converted to a booking and it could see the numbers racking up quickly… therefore having your phone answered correctly is a huge responsibility. Moreover, surveys have confirmed that patients will find another provider if they have to deal with an unfriendly front desk member.
Thankfully, there are more options now than ever before to make that good first impression mainly divided between In-House and Virtual Receptionists.





































Hiring an in-house receptionist has been the traditional way of incorporating an administrative team to your clinic. Not only are they administrative superheroes but they can also assist with rebooking appointments, sterilising instruments, cleaning tasks, marketing support and much more depending on what you want. You must consider though that they require a living wage, breaks throughout the day, paid holidays and will only be able to answer one call at a time within your office hours plus the cost of office space and supplies. The key benefit to an in-house receptionist is having that person with whom your patients build up a rapport with over time when attending recurring appointments. If you don’t have the space in your clinic to accommodate an in-house receptionist, consider a virtual receptionist who can also get to know your business inside out. They too can provide informative customer service sometimes around the clock to prevent you from missing out on any new patient leads and can whilst nurturing your patient experience. The cost of a virtual receptionist is definitely lower with greater flexibility e.g. if you’ve got a slow day and don’t need someone to cover the phones, you can opt to answer them yourself. So in a nutshell, free yourself of administrative tasks and focus on treating your patients by hiring some reception support, not only will you see an increase in your patient numbers but you may even be able to find some work & life harmony. Until next time, may you achieve happiness with every step in life and business.

Podiatry Review Summer Issue 2021 | 31 Dr B’s Business Box
all
Every new missed patient opportunity can cost your practice on average of £400-£1000 annually
starts at the front desk
The Impact of anti-cancer treatment on feet
Podiatric Adverse Events: Part 2b Dermatological Effects
Afni Shah-Hamilton BSc MSc
Introduction
An increasing population now have ‘treatable but not curable cancers’. Whilst part 2a of this article focused on the neurological side effects of ‘anti-cancer’ treatments, this article discusses the four common dermatological events that can negatively impact the feet and legs as symptomatic podiatric adverse events (PAEs) are common in patients treated for cancer1. Radiotherapy, chemotherapy and targeted therapy are all known to cause these dermatological effects, many of which require podiatric treatment.
These dermatological PAEs have a negative effect on patients’ physical, functional, emotional, and social well-being2. They can be debilitating for someone already struggling with their anticancer treatment regime and a CancerCare survey identified that ‘nearly 80% [of patients] were concerned about the actual skin effects they experienced as a result of their treatment and how those side effects – namely irritation, rash and dryness- affected their quality of life’ 3 .
Publicising these issues (as set out in my previous article), recognising them in a clinical setting, and providing appropriate advice and treatment can be an invaluable part of supporting patients through this difficult time.
Four Dermatological Podiatric Adverse Events (PAEs)
The four main dermatological PAEs where podiatric-medical intervention is paramount 4 to avert the rapid development of complications associated with anticancer therapy are:

1 Xerosis
2 Hand-foot syndrome (HFS)
3 Hand-foot Skin Reactions (HFSR)
4 Nail toxicity, dystrophy, inflammation & infections
Whilst the first three conditions are skin related, they can all occur in conjunction with nail toxicity and dystrophy issues.
It is important to adapt treatment for cancer patients, both to reflect the specific nature of anticancer therapy and anticipate potential complications. By working in partnership with the patient and their cancer team, many problems can be minimised or avoided.

32 | www.iocp.org.uk ARTICLE
Why does it occur?
Xerosis
Xerosis (abnormally dry skin) can occur in patients who are receiving either targeted therapy, radiotherapy or chemotherapy5,6,7
The skin is unable to desquamate (shed) and retain hydration due to the impact of anticancer therapies on epidermal keratinocytes.
Many anticancer therapies, particularly those that treat various solid and haematologic tumours, target all rapid proliferation cells including epidermal keratinocytes. This leads to increased trans-epidermal water loss as the therapy lowers the rate of cell turnover. Given there are no oil glands in the soles of the feet, this exacerbates the problem further.
How does it present?
Patients will exhibit with generalised dry skin, erythema, itchiness and/or facial flushing. In my clinical experience, fissures on the lateral aspects of the soles and heels can arise and patients comment that their skin feels tight no matter what they put on it.

Hand-Foot Syndrome (HFS)
HFS, also known as PalmarPlanter Erthrodysesthesia (PPE), causes redness, swelling and pain on the soles of the feet and also on the palms. It is one of the most common adverse reactions to cytotoxic agents.
HFS is graded in severity, although there are a number of different classification systems for doing this. Depending on the grade, some protocols recommend reducing the dosages of some drugs.
Why does it occur?
There are two main theories as to why HFS occurs:
1 There is a greater concentration of keratinocytes in the palms and soles, and these are targeted by cytotoxic agents which focus on fast growing cells. The keratinocytes metabolise the drug quickly and produce a toxin, causing the skin reaction9.
2 There is a greater concentration of eccrine glands in the palms and soles, and the toxic drug is excreted onto the skin10
Either way, we know that HFS can result from more highly concentrated dosages or from low treatment doses over a prolonged period11.
All of the following drugs have been found to cause HFS: Anthracycline antibiotics Doxifluridine Methotrexate
Capecitabine
Doxorubicin Mitotane
Cyclophosphamide Cisplatin Paclitaxel
Floxuridine
Tegafur Cytarabine
Fluorouracil Vinorelbine Daunorubicin
Mercaptopurine Etoposide Docetaxel
Hydroxyurea (hydroxycarbamide)
How does it present?
Initial symptoms include
• Swelling (dysesthesia)
• Numbness
• Sense of tightness/stiffness
• Pain in the palms and/or soles
Two to four days later, this progresses into a burning pain, accompanied by oedema and bright, well defined, symmetrical erythema on the palms and soles. The patient’s palms and soles typically appear to have been stained in red paint and some patients may also see nail changes.

If untreated, skin lesions can progress to painful blistering, desquamated skin cells (flakiness), form crusts and ulceration. With each subsequent cycle of chemotherapy, the reaction will appear more quickly, more severely and can take longer to heal due to the patient’s compromised immunity. As the skin is painful to touch, analgesics may be recommended prior to treatment.

DID YOU KNOW?
HFS was first described in 1974 by Zuehlke and was associated with mitotane therapy for hypernephroma (tumour of the kidney)8 .
Hand-Foot Skin Reaction (HFSR)
An HFSR is distinct from, but related to, HFS. On the feet, these painful blisters can limit the patient’s mobility and their ability to weight bear properly and lead to an increased chance of a fall. Both HFS and HFSR can be particularly problematic for those patients with active lifestyles or where they are required to stand for long durations.
Why does it occur?
This may be due to increased leakage of the anticancer therapy through mechanical trauma of the skin.
How does it present?
HFSR occurs in areas of friction or pressure in the soles and palms within the first few weeks of anti-cancer treatment. The skin reactions appear as painful blisters, often on pressure points on the feet and develops into hyperkeratotic (callus) areas12
All of the following drugs can cause HFSR 13,14,15. :
Multikinase inhibitors
Sorafenib Sunitinib Axitinib
Regorafenib Pazopanib
Taxanes and Pyrimidine analogues
5-fluorouracil Capecitabine
Podiatry Review Summer Issue 2021 | 33
How can podiatrists help with Xerosis, HFS and HFSR?

Management of these conditions relies on the right intervention at the right time. Physical podiatric treatment is only a small part of this, with support, prevention, and selfcare all being key aspects. It is particularly important to take into account the patient’s lifestyle and how best to support them in maintaining key elements of their daily activities, as they are already managing significant disruption to their normal routines whilst undergoing anti-cancer treatment.
Education/Preparation
As noted previously, making patients more aware of the podiatric side effects of anti-cancer therapies and the support available, so that they can be prepared for them, can be of great help. Even less severe PAEs can generate disproportionate anxiety and distress in the midst of a cancer treatment programme.
Starting to regularly moisturise the feet prior to starting anti-cancer therapy helps by ensuring the skin is hydrated and combating the excessive desquamation of cells. A urea-based moisturiser can help prevent HFS and HFSR, or extend the time before first occurrence, and reduce symptoms16,17,18. Current thinking suggests 10-20% ureabased creams should be used and improvements can be seen within four weeks.
For my patients I typically recommend applying CCS heel balm two or three times daily, particularly after bathing. In my experience, other urea-based creams have been less successful and in some cases patients have complained of stinging, discomfort, pain and peeling. It may be that the CCS urea preparation reacts differently with the secreted anticancer agent and metabolites from the keratinocytes.
Other simple advice can also help – for example on hosiery and nutrition. Using bamboo fibre or rich cotton, seam-free socks helps improve comfort and reduce shearing. Bamboo fibre socks offer additional benefits through moisture and thermo regulation and are anti-bacterial (due to a bacteriostatic bio-agent Bamboo Kun). From a nutritional perspective, some treatments can cause a decrease in Vitamin C, E, B12 and Folic acid19 Vitamin B6 (Pyridoxine) has been useful in treating these conditions and alleviating HFS pain20,21.
For patients at higher risk of HFS or HFSR then educating them about PAEs and highlighting when they should seek urgent assistance can be valuable in getting the right podiatric treatment at the right time.
Podiatric intervention
Providing regular neurological, vascular and biomechanical assessments and good podiatric debridement and nail maintenance is key to preventing further painful complications such as open fissures, ulcerations and paronychia.
For my patients, I aim to schedule their six-weekly appointments two weeks after an IV treatment cycle is administered. This helps reduce the issues in painful weight bearing areas, manage xerosis and detect any neurological
changes. In an effort to minimise future issues, I regularly focus on neurology and footwear assessment. Neural disturbance may precipitate falls whilst footwear advice, insoles and exercises can help to avoid irritant trauma in the form of friction, heat, and pressure.
Self-care advice
Foot cooling22 and a cleansing regime23,24 are important, particularly for patients suffering from HFS or HFSR. Keeping feet cool helps to reduce swelling and stiffness in the foot and minimises the accumulation or leakage of the drug due to the vasoconstriction effects. Research has cited the use of frozen socks to prevent docetaxelinduced onycholysis and cutaneous toxicity of the foot and shown that wearing a frozen sock for 90 mins during drug administration reduces nail toxicity25.
I advise patients to wear refrigerated gel socks rather than frozen socks, as the mineral oil impregnated in the socks also improves the moisture content of the skin. Wearing the gel socks for 20 minutes, three times a day has reduced symptoms significantly, with improved healing times and skin integrity.
There are no specific guidelines on skin cleansing but research has shown it to be beneficial 26,27. It soothes skin irritation and sores, improves desquamation and is important in reducing the risks of infection. For my patients, I recommend regularly bathing the feet in a solution of lukewarm water containing a mixture of Epsom salt and normal table salt. This helps reduce inflammation whilst the magnesium content aids healing of the skin.
For Xerosis, patients should use ointments containing keratolytics (such as salicylic acid 6% with a urea base of 10%-40%) and cover the foot after administration. The need to avoid skin breakdown must be borne in mind in patients with thin and sensitive skin such as diabetic patients. I use Clearzal callus remover, which has delivered good results with close monitoring.
Nail toxicity, dystrophy, inflammation and infections
A large number of anticancer drugs impact the nails, although nails are typically only significantly affected after two months of the patient following a cancer treatment due to the slow growth rate of the nail plate (the drugs affect the kinetics of nail formation).
These PAEs can be extremely painful, severely impacting the quality of life of the patient. The fact that it is another visible sign of the anticancer treatment can also contribute to depression.
Symptoms can last many years after treatment and whilst they are usually reversible after discontinuation of the anti-cancer treatment, in my experience most patients still require ongoing podiatric care.
34 | www.iocp.org.uk ARTICLE (continued)
Why does it occur?
Anticancer drugs distort nail cell growth or the nail toxicity affects the nail fold and nail bed.
All of the following drugs can affect the nails28:
Arsenic Busulfan Cetuximab Cyclophosphamide Bleomycin Capecitabine Cisplatin Dacarbazine Dactinomycin Daunorubicin Docetaxel Doxorubicin Etoposide Fluorouracil Gefitinib
Hydroxyurea Idarubicin Imatinib Ixabepilone Melphalan Mercaptopurine Methotrexate Mitomycin Mitoxantrone Paclitaxel Pemetrexed Sorafenib Sunitinib Tegafur Topotecan Vincristine
Nail toxicity can be a particular problem for those receiving epidermal growth factor receptor inhibitors and taxanes. How does it present?
Cases can involve several, or in some cases all 20, nails.
The nail dystrophies include: Onychocryptosis Onycholysis Onychomadesis
Beau’s lines Mee’s lines Nail growth disruption Melanonychia Leukonychia Paronychia
Splinter haemorrhages Hypergranulation/ and Subungual haematoma periungual pyogenic granulomas
Taxane-associated Onychauxis/ acral erythema Onygryphosis Subungual ulcerations Fragile nail plate
As a result, patients may have increased difficulty in trimming nails and finding comfortable footwear.
How can podiatrists help?
In general, for those suffering from nail toxicity, timely and preventative podiatric actions can avoid disruption to the patient’s treatment cycle and maintain their mobility.
For all nail conditions, it is important to check footwear and hosiery for their impact on pressure areas. Also, the patient may have limited dexterity and mobility due to operations they have undergone during their treatment. As with HFS and HFSR, frozen sock therapy or use of gel socks has been found to significantly reduce nail toxicity, particularly in patients taking docetaxel29,30.
Providing good routine podiatric debridement and regular, effective sulcal management will help prevent further
painful complications such as onycholysis progressing to paronychia, ulcerations and secondary infections. Sulcal management of onycholysis should include removing onychophosis as well as smoothing the sulcal nail area.
For a number of cancer patients, particularly for those with paronychia, nail surgery may not be suitable due to comprised healing times and drug management issues. More frequent sulcal management is key. Nail packs with 1% povidone iodine/ dimethyl sulfoxide31 or bactigras may be needed to help alleviate pressure, whilst appropriate antibiotics coupled with very salty water footbaths can address unresolved infections (such as Staphylococcus aureus and Pseudomonas aeruginosa (found in more persistent cases))32 .
With onychomycosis it is important to choose the right topical antifungal as some fungal strains will be resistant or not designed to treat that type of fungus. For example, Terbinafine is effective against dermatophytes but less active against candida yeasts and non-dermatophytic moulds, whereas Itraconazole is effective against dermatophytes and candida yeast and some nondermatophytic mould. In cases of chronic paronychia, the yeast infection Candida albicans has been found.
Conclusion
There are multiple podiatric adverse events (PAEs) that commonly affect cancer patients although this remains relatively poorly publicised. Xerosis, HFS, HFSR and nail-related issues are all known dermatological side-effects of various anticancer treatments that can be managed or treated with suitable podiatric advice. There are also neurological PAEs such as peripheral neuropathy and autonomic neuropathy, as covered in part 2a of this article.
Greater awareness of PAEs could significantly help in limiting the negative impact – both through patients being mentally prepared for such issues and being aware of podiatric help being available.
By working more closely with the patient and their cancer unit, podiatrists can improve patients’ quality of life and even reduce the chances of patients not finishing their lifeenhancing anticancer therapy.
Podiatry Review Summer Issue 2021 | 35
REFERENCES
1 Lacouture M, Kopsky D, Lilker R, Damstra et al: Podiatric Adverse events and Foot Care in Cancer Patients and survivors. Nov/Dec 2018. Journal of American Podiatric Medical association Vol 108. No.6
2 HALEY AC, CALAHAN C, GANDHI M, WEST DP, RADEMAKER A, LACOUTURE ME. Skin Care management in cancer patients: an evaluation of quality of life and tolerability. Support Care Cancer 2011; 19:545-554
3 www.cancercare.org/press/releases/28-2008_05_27 Treatment side effects involving skin hamper quality of life for cancer patients, new survey shows.
4 Lacouture M, Kopsky D, Lilker R, Damstra et al: Podiatric Adverse events and Foot Care in Cancer Patients and survivors. Nov/Dec 2018. Journal of American Podiatric Medical association Vol 108. No.6
5 www.cancer.net/coping-with-cancer/physical-emotional-and-socialeffects-cancer/managing-physical-side-effects/skin-conditions
6 Lacouture M, Kopsky D, Lilker R, Damstra et al: Podiatric Adverse events and Foot Care in Cancer Patients and survivors. Nov/Dec 2018. Journal of American Podiatric Medical association Vol 108. No.6
7 HALEY AC, CALAHAN C, GANDHI M, WEST DP, RADEMAKER A, LACOUTURE ME. Skin Care management in cancer patients: an evaluation of quality of life and tolerability. Support Care Cancer 2011; 19:545-554
8 ZUEHLKE RL. Erythematous eruption of the palms and soles associated with mitotane therapy. Dermatologica 1974: 148(2): 90-92
9 ASGARI MM, HAGGERTY JG, MCNIFF JM, MILESTONE LM, SCHWARTZ PM. Expression and localization of thymine phosphorylase/ plateletderived endothelial cell growth factor in skin and cutaneous tumours. J Cutan Pathol 1999; 26 (2):287-294
10 MROZEK-ORLOWSKI ME, FRYE DK, SANBORN HM. Capecitabine: nursing implications of new oral chemotherapeutic agent. Oncol Nurs Forum 1999; 26 (4): 753-762
11 NAGORE E, INSA A, SANMARTIN O. Antineoplastic therapy-induced palmar plantar Erythrodysesthesia (“hand-foot”) syndrome. Am J Clin Derm 2000;1(4):225-234nt
12 GOMEZ P, LACOUTURE ME: Clinical presentation and management of hand-foot skin reaction associated with sorafenib in combination with cytotoxic thermotherapy: experience in breast cancer. Oncologist 16: 1508, 2011
13 LACOUTURE ME, REILLY LM, GERAMI P, ET AL: Hand foot skin reaction in cancer patients treated with the multikinase inhibitors sorafenib and sunitinib. Ann Oncol 19: 1955, 2008
14 LACOUTURE ME, WU S, ROBERT C, ET AL: Evolving strategies for the management of hand-foot skin reaction associated with the multi targeted kinase inhibitors sorafenib and sunitinib. Oncologist 13: 1001, 2008
15 ANDERSON R, JATOI A, ROBERT C, ET AL: search for evidence-based approaches for the prevention and palliation of hand-foot skin reaction (HFSR) caused by the multi-kinase inhibitors (MKIs). Oncologist 14: 291, 2009
16 REN Z, SHU K, KANF H, ET AL: Randomized controlled trial of the prophylactic effect of urea-based cream on sorafenib-associated hand-
foot skin reactions in patients with advanced hepatocellular carcinoma. J Clin Oncol 33: 894, 2015
17 LACOUTURE ME, WU S, ROBERT C, ET AL: Evolving strategies for the management of hand-foot skin reaction associated with the multi targeted kinase inhibitors sorafenib and sunitinib. Oncologist 13: 1001, 2008
18 HALEY AC, CALAHAN C, GANDHI M, WEST DP, RADEMAKER A, LACOUTURE ME. Skin Care management in cancer patients: an evaluation of quality of life and tolerability. Support Care Cancer 2011; 19:545-554
19 SCHREURS WH, ODINK J, EGGER RJ, WEDEL M, BRUNING PF: The influence of radiotherapy and chemotherapy of vitamin status of cancer patients. Int. J Vitam Nutr res 1985; 55 (4):425-432
20 NAGORE E, INSA A, SANMARTIN O. Antineoplastic therapy-induced palmar plantar Erythrodysesthesia (“hand-foot”) syndrome. Am J Clin Derm 2000;1(4):225-234nt
21 Vukelja SJ, Lombardo FA, James WD et al. Pyridoxine for palmar-plantar Erythrodysesthesia syndrome. Ann Intern Med 1989 Oct 15;111 (8):688-9
22 Zimmerman GC, Keeling JH, Lowry et al. Prevention of docetaxel-induced erythrodysesthesia with local hypothermia J Natl Cancer Inst 1994:86:557
23 MCQUESTION M. Evidence-based skin care management in radiation therapy. Semin Oncol nurs 2006 22(3):163-173
24 BOLDERSTON A, LLOYD N, WONG R et al. the prevention and management of acute skin reactions related to radiation therapy: a systematic review and practice guidelines. Support Cancer Care 2006 14 (8):802-817
25 SCOTTE F, BANU E, MEDIONI J, ET AL: Matched case-control phase 2 study to evaluate the use of a frozen sock to prevent docetaxel-induced onycholysis and cutaneous toxicity of the foot. Cancer 112: 1625, 2008
26 www.cancer.net/coping-with-cancer/physical-emotional-and-socialeffects-cancer/managing-physical-side-effects/skin-conditions
27 HALEY AC, CALAHAN C, GANDHI M, WEST DP, RADEMAKER A, LACOUTURE ME. Skin Care management in cancer patients: an evaluation of quality of life and tolerability. Support Care Cancer 2011; 19:545-55
28 GILBER P, HAIN A, PEEREBOOM V. Nail toxicity induced by cancer chemotherapy. J oncol Pharm Pract 2009; 15 :143-155
29 SCOTTE F, BANU E, MEDIONI J et al. Matched case-control phase 2 study to evaluate the use of a frozen sock to prevent docetaxel-induced onycholysis and cutaneous toxicity of the foot. Cancer 2008; 112:1625-31

30 GILBER P, HAIN A, PEEREBOOM V. Nail toxicity induced by cancer chemotherapy. J oncol Pharm Pract 2009; 15 :143-155
31 CAPRIOTTI K, CAPRIOTTI JA: Chemotherapy-associated paronychia treated with a dilute povidone-iodine/dimethyl sulfoxide preparation. Clin Cosmet Investig Dermatol 8: 489,2015
32 HOESLY FJ, BAKER SG, GUNAWARDANE ND, COTLIAR JA. Capecitabineinduced hand-foot syndrome Complicated by pseudomonal superinfection resulting in bacterial sepsis and death: case report and review of the literature. Arch Dermatol 2011; 147(12): 1418-1423
About the author
Afni Shah-Hamilton runs Tiptoe Foot Care, a private pain management and podiatry practice in Barnet, London. Afni graduated from University College London in Podiatry BSc (Hons) and completed her master’s degree at Kings College London. She currently sits on the Macmillan AHP advisory board and has previously been a member of the national patient safety campaign, Sign up to Safety, advisory group. Afni has worked for Southwark Foot Health Department in conjunction with Guy’s and King’s College Hospital as well as working for the Society of Chiropodists and Podiatrists (now the Royal College of Podiatry) as a Union Learn Fund Project Worker, promoting learning and development across the profession.
Afni has significant experience of dealing with high risk patients through her close relationships with oncologists and a local cancer charity. She is passionate about the role that podiatrists can play in improving the quality of life for both cancer sufferers and cancer survivors.

36 | www.iocp.org.uk
www.tiptoefootcare.com Twitter @tiptoefootcare
ARTICLE (continued)
Award of Consultant Fellowship of the IOCP
The Institute of Chiropodists and Podiatrists
Award
Submissions are invited from members or academic fellows of the Institute pursuant to granting them additional recognition as a Consultant Fellow of the Faculty of Podiatric Medicine of the Institute of Chiropodists and Podiatrists (CFPodM). This allows fellows to progress to further advanced training and practice indemnified by the IOCP.
Consultant Fellowship is a clinical award for senior members of the profession, recognising and demonstrating their seniority and an advanced scope of clinical practice. The minimum attainments of individuals seeking the award must be as follows:
• They must be current registrants of the Health and Care Professions Council, in good standing, at the time of application without pending disciplinary action.
• They must be current full members or academic fellows of the Institute of Chiropodists and Podiatrists with current IOCP Option 4 professional indemnity insurance.
• They must have a degree in Podiatry or Podiatric Medicine awarded by a UK university
• They must have Local Anaesthesia (POM-A) and Prescription Medicine (POM - S) annotations recorded on their HCPC registration entry OR have POM-A and Supplementary Prescribing/ Independent Prescribing recorded on their HCPC annotations.
• They must have a minimum of 12 years of clinical practice as a podiatrist.
• They must submit evidence of a pattern of continuing professional development throughout their career to date in subjects appropriate to podiatric medicine.
• They must submit a curriculum vitae, showing their journey through the profession to the date of application and this must demonstrate how they believe themselves to have a scope of practice that merits the title ‘advanced/Consultant’
• They must agree to submit a presentation/lecture to the IOCP Annual Conference demonstrating their advanced knowledge/ practice/research.
The award is via the agreement of the panel of the Consultant Fellowship board of the IOCP who will ensure that all of the minimum standards have been met. Applicants will also be required to successfully undertake an interview and provide two professional references including a statement/sponsor of support. Once the criteria has been met and the appropriate application paperwork submitted to the registered offices of the Institute, the award will then be formally issued upon payment of the nominal administration fee of £150.
Award of Academic Fellowship
The Institute of Chiropodists and Podiatrists
Award
Submissions are invited from members of the Institute pursuant to granting them additional recognition as an Academic Fellow of the Faculty of Podiatric Medicine of the Institute of Chiropodists and Podiatrists (FPodM).
Application is by way of completion of the appropriate paperwork and submission of a 5000 word dissertation containing previously unpublished material on a relevant podiatric subject that meets the approval of the Review Board of the Faculty of Fellows. Such dissertation is to be constructed on sound academic principles and be adequately referenced in an accepted academic style.
For members who have not previously published, the Board is happy to give informal and friendly guidance to members wishing to develop this interesting new area of their professional career. A nominal fee of £100 is payable to cover the necessary administration by Head Office. Certificates of Fellowship will be awarded to successful Fellows and their names recorded on the Roll of Fellows maintained by the Faculty.
Accepted dissertations will be published in Podiatry Review and be added to The Fellows Library which will be an electronic knowledge bank available online to registered members. Such activity is also held to be Continuing Professional Development (CPD) by the IOCP and is suggested as being suitable to record in the event of HCPC audit.
Applications will be accepted from current members who are HCPC registered, annotations such as POMs or LA are not a condition of application as this is an academic award open to all HCPC registered full members of the Institute.
For further information and an application form please contact Head Office by emailing secretary@iocp.org.uk.
Podiatry Review Summer Issue 2021 | 37
AWARDS
CLASSIFIED ADVERTS
Please note: all products advertised in the Podiatry Review and on the Website are accepted by the Institute of Chiropodists and Podiatrists on the basis of a commercial advertising service and purchasers should carry out their own assessment as to the suitability of such products for their own specific needs. Acceptance of the advertisement by the Institute does not imply our endorsement or approval of the product.
SVTS Chiropody Drill repair and sales
We offer an excellent competitive and efficient repair service for all makes of Podiatry/chiropody Nail drills. Berchtold, Hadewe, Suda, Footman, Podiacare, Podo Tronic and Podo Pro EVO-30,40&50 drills.
We sell Berchtold S35/ S30, Hadewe, EVO 30,40.50 Dust Bags from £1.25 – £2 each. WE ALSO BUY UNWANTED DRILLS.
Unit 255 Stratford Workshops, Burford Road, London E15 2SP Contact us on 0208 5190044 or www.chiropodydrillrepair.co.uk
Diabetic Foot Module Course – change of date In London 11th – 15th October 2021
Venue - The Wellcome Collection Euston Road Intensive update course for specialist practitioners. For more information, please email diabeticfootmodule@gmail.com
Chiropodist/ Podiatrist required in Heswall, Wirral
We are situated in Heswall, Wirral. We are a busy multi-discipline clinic in the heart of a thriving village.

Our clinic is exceptionally busy with five chiropodists and full-time reception staff. The position is offered with hours to suit applicant.
The successful candidate must be personable, not afraid of being busy and have great attention to detail. In return they can earn £200-300 per day.
This is a self-employed position and payment is on a fee sharing basis.
Tel: 01513 429665 for further information
Part time self-employed Chiropodist/ Podiatrist/ COFH trained FHP required in Coalville, Leicestershire
The FooT Centre requires a part time chiropodist/podiatrist or college of foot health trained FHP to join our friendly team in the very busy FooT centre clinic.
The ground floor clinic is based in Coalville, Leicestershire and has forecourt parking.
Equipment, instruments and all medicaments supplied This a self-employed 50/50 fee sharing position for one or two days a week.
Please contact Sue for more information on 07447 917 239 or email sue.iocp@ntlworld.com
38
| www.iocp.org.uk
To place an advert here or for more information please email
julie@iocp.org.uk
SOUTH WALES AND MONMOUTH BRANCH
Meetings are taking place via zoom, members who would like details of the next meeting and wish to attend please contact Esther on 01656 740772 or email estherdanahar@yahoo.co.uk
JULY 2021
4 Wolverhampton Branch Meeting
At 10am at the Reading Rooms, Market Street, Penkridge, Staffs. ST19 5DH
Contact: David on 01785 716607 or email djcollett@hotmail. co.uk
AUGUST 2021
5 Sheffield Branch Meeting
At 7.30pm Via Zoom
Contact Helen on 07789 025022 or email hrawse@live.co.uk for further information
SEPTEMBER 2021
20 London Branch Meeting
At 7.30pm Via Zoom
Contact: Sarah on 07790 717833 or email footwoman@gmail.com
26 Cheshire, North Wales Branch Meeting
At 10am at The Dene Hotel, Hoole Road, Chester
Contact: Michele on 07766 700027 or email missminou@ hotmail.co.uk
OCTOBER 2021
7 Birmingham and the Shires Branch Meeting
7.30pm Venue to be confirmed. Contact Kate Harrison on 01789 262365 for further information
10 Leicester and Northants Branch Meeting
At the Lutterworth Cricket Club - Branch meeting/Seminar/ Autoclave servicing in the morning
Contact: Ian on 07718 700641 or email fenton303@ntlworld.com
10 Wolverhampton Branch Meeting
At 10am at the Reading Rooms, Market Street, Penkridge, Staffs. ST19 5DH
Contact: David on 01785 716607 or email djcollett@hotmail.co.uk
NOVEMBER 2021
4 Sheffield Branch Meeting
At 7.30pm Via Zoom
Contact Helen on 07789 025022 or email hrawse@live.co.uk for further information
DECEMBER 2021
6 London Branch Meeting
At 7.30pm Via Zoom
Contact: Sarah on 07790 717833 or email footwoman@gmail.com
JANUARY 2022
9
Wolverhampton Branch Meeting & AGM
At 10am at the Reading Rooms, Market Street, Penkridge, Staffs. ST19 5DH
Contact: David on 01785 716607 or email djcollett@hotmail.co.uk
13 Birmingham and the Shires and Annual General Meeting
7.30pm Venue to be confirmed.
Contact Kate Harrison on 01789 262365 for further information
23 Leicester and Northants
Annual General Meeting via Zoom
At 10am via Zoom
Contact: Ian on 07718 700641 for further information
Podiatry Review Summer Issue 2021 | 39
DIARY OF EVENTS
Please email julie@iocp.org.uk with information about Branch Meetings whether face to face or via zoom etc. Keep your Branch members up to date so they can attend.