

2023 Annual Quality and Patient Safety Report
Department of Medicine
Icahn School of Medicine at Mount Sinai Mount Sinai Health System
Mount Sinai Beth Israel Division Quality Champions
Clinical Immunology: Songhui Ma, MD
Endocrinology: Daniel Donovan, MD; Olga Kozachenko, NP-C
Gastroenterology: Custon Tafadzwa Nyabanga, MD
General Medicine: Desiree Chow, MD
Hospital Medicine: Dahlia Rizk, DO, MPH
Quality Improvement Peer Review Committee: Patricia Dharapak, MD
Infectious Diseases: Tessa Gomez, MD
Nephrology: Elliot Charen, MD
Pulmonary, Critical Care and Sleep Medicine: David Steiger, MD; Lina Miyakawa, MD
Rheumatology: Latoya Freeman-Beman, MD
The Mount Sinai Hospital Division Quality Champions
Clinical Immunology: Eugene Choo, MD*
Endocrinology: David Lam, MD; Nirali Shah, MD
Gastroenterology: Christopher Cao, MD; David Greenwald, MD
General Medicine: Nikita Barai, MD; Kelsey Bryant, MD; Kyle Koster, MD
Hospital Medicine: Anne Linker, MD
Quality Improvement Peer Review Committee: Aveena Kochar, MD
Infectious Diseases: Rachel Chasan, MD
Liver Diseases: Ritu Agarwal, MD
Nephrology: Joji Tokita, MD
Pulmonary, Critical Care, and Sleep Medicine: Jing Wang, MD; Timothy Harkin, MD
Rheumatology: Wendy Weiwei Chi, MD
Mount Sinai Morningside and Mount Sinai West Division Quality Champions
Endocrinology: Ilana Ramer Bass, MD
Gastroenterology: Tina Park, MD
General Medicine: Heather Viola, DO
Hospital Medicine (MSM): Brian Markoff, MD; Faye Reiff-Pasarew, MD
Quality Improvement Peer Review Committee: Lindsey Fox, MD
Hospital Medicine (MSW): Shantheri Shenoy, MD
Quality Improvement Peer Review Committee: Irina Zaretsky, MD
Infectious Diseases: Rahul Gaikwad, MD
Nephrology: Ruchika Batwara, MD
Pulmonary, Critical Care, and Sleep Medicine: Janet Shapiro, MD; David Steiger, MD
Rheumatology: Kristaq Koci, MD
Introduction
Dear Colleagues,
On behalf of the Office of Quality and Patient Safety for the Department of Medicine, I am pleased to present our 2023 annual report. This report captures our efforts and achievements in enhancing the quality of care and ensuring patient safety for our hospitalized and ambulatory patients throughout the Mount Sinai Health System (MSHS).
Thanks to the dedicated hospital Quality Leads, Division Champions, and my fabulous team of quality professionals and analysts, we have made significant strides in strategic areas that include priority safety goals for the MSHS as well as dozens of innovative performance improvement and quality projects. Key highlights are described below:
Quality Improvement (QI) Initiatives: Our team has supported dozens of QI initiatives aimed at enhancing patient care processes and outcomes. These initiatives have resulted in measurable improvements in areas related to Safe Transitions in Care, Medication Reconciliation, Inpatient Mobility, CLABSI Reduction, Enhanced Home Oxygen Education at Discharge, and many others.
Patient Safety Culture: We have worked diligently to foster a culture of safety throughout the MSHS by encouraging increased reporting of adverse events and near misses. The Quality Team reviews DOM SafetyNet Reports and contacts quality leads at each site to investigate and learn from these events in real-time. In some instances, education, counseling, or change in a process, has reduced the risk that the same event could happen again in the next 24 hours. In addition to SafetyNet Review, faculty from the Division of Hospital Medicine participate in Mortality Review of all deaths to determine if the death was expected. Peer Review Committees examine cases where the reviewer recognizes a concern or opportunity for improvement and the committee identifies best practices to mitigate future events.
Data-Driven Improvement: Our Quality Analysts are experts in extracting data from Premier, Epic, and Vizient. Through our robust data-gathering and analysis efforts, we have provided our Champions with actionable data to drive quality and safety initiatives. Data dissemination has been instrumental in identifying areas for improvement and monitoring progress over time. In 2023, MSHS made a commitment to collect and include extensive patient demographic information on the Tableau Dashboards. This has allowed us to provide reliable race, ethnicity, and language data to the Champions. In 2024, we will be diving deeper into this data to uncover disparities that will lead to new focused projects in alignment with the MSHS Advancing Equity in Quality initiative.
Partnerships and Collaboration: We maintain a strong partnership with hospital quality leadership across the MSHS, which has been effective in implementing interdisciplinary approaches to address complex quality and patient safety challenges. We look forward to continuing our partnerships with the hospital CMOs and the MSHS Office of Quality and Regulatory Affairs.
In closing, I extend my sincere gratitude to each member of my team, as well as our partners and stakeholders, for their unwavering dedication and commitment to quality and patient safety.
Respectfully,
Beth Raucher, MD, SM Professor of Medicine

Clinical Immunology
Mount Sinai Beth Israel
Division Quality Champion: Songhui Ma, MD

In 2023, the Division of Allergy and Clinical Immunology at Mount Sinai Beth Israel started two new quality improvement projects.
The first project focused on the topic of penicillin allergy with the goal of identifying all appropriate patients for delabeling (i.e., removing penicillin allergy from the patient’s medical record). The first aim was to risk stratify all patients seen in the allergy practice with a label of penicillin allergy by history of allergic reaction. The second aim identified appropriate patients for delabeling with penicillin skin testing and challenge. To facilitate the second objective, a procedure room staffed by nursing and supervised by the allergy physician was created. A team of nurses was trained in penicillin allergy challenge testing as well as recognition and management of anaphylaxis. To minimize scheduling errors, procedure visits were built into Epic and appointment confirmations were performed by the allergy secretary and written pre-visit instructions were provided to patients. Limitations included lack of physician time to address incidental concerns, as well as lack of staffing and exam room space within the clinic. Patient factors included anxiety regarding a potentially severe reaction to penicillin and the belief that penicillin evaluation was either unnecessary or nonurgent, as well as difficulty with scheduling and competing personal/work commitments.
Patients Labeled Penicillin Allergic (N=64)
Delabeled (i.e., penicillin allergy removed from medical record)
Evaluation with penicillin testing/challenge recommended
Other
In the first six months of 2023, penicillin allergy was addressed in 64 patients. Evaluation with penicillin testing and challenge was performed in 34 percent and recommended in an additional 52 percent Overall, 34 percent of patients were delabeled, either by history or by testing and challenge.
The second project was to counsel and offer smoking cessation resources to all patients with active tobacco use The Division is currently reviewing preliminary data on patients seen in the allergy clinic who have a documented social history of tobacco use and determining which of those patients were appropriately counseled on smoking cessation. Gaps identified in providing education and resources will continue to be addressed in 2024.
The Mount Sinai Hospital
Division Quality Champion: Eugene
Choo, MD

In 2023, the Division of Allergy and Clinical Immunology at The Mount Sinai Hospital focused efforts to improve its performance across two quality projects. The team plans to continue both projects into 2024.
The first quality project was to increase influenza vaccination rates in patients with reported or documented egg allergy who refuse the vaccine due to their allergy. The team identified patients with an egg allergy documented in EPIC in a six-month time period (February 15, 2023 to August 15, 2023) who visited the Allergy and Immunology clinics at Faculty Practice Associates (FPA) and Center for Advanced Medicine (CAM). Patients were then filtered by vaccination status documented in EPIC from the previous influenza season (2022-2023). Epic charts of patients without documented vaccination status were reviewed to determine if they received an influenza vaccine outside of the Mount Sinai Health System and if egg allergy played a part in their refusal to receive an influenza vaccine in the past.
**CDC estimated that the overall flu vaccination rate for eligible individuals (>6 months) for 2021-2022 was 51.4%
The overall flu vaccination rate (36.8 percent) for the past season in this population of egg-allergic patients was below the typical reported national average rate of 51.4 percent by the Centers for Disease Control and Prevention, and much of that difference was explained by their misconceptions
about vaccination and egg allergy. In 2024, the division plans to include all primary care practices and conduct provider education regarding ability to get vaccinated with an egg allergy.
The objective of the second quality project was to increase the rate at which Allergy and Immunology providers address a reported penicillin (PCN) allergy through counseling and education, and testing, among new patients at FPA and CAM. The long -term goal is to increase the rate at which a penicillin allergy is tested for and appropriately de-labeled. The team identified all new patients to the Allergy and Immunology FPA and CAM over a one -year period who had a documented penicillin allergy. The rate at whi ch the documented penicillin allergy was addressed either through counseling and education, or plan for future testing, or scheduled testing was determined.
Interventions included reminders during monthly Allergy and Immunology Division meetings about addressing and documenting penicillin allergy with all new patient encounters. In addition, an EPIC dotphrase was created and distributed among the division in order to increase ease of appropriate documentation and of planning an appropriate intervention plan (utilizing the validated risk stratification tool of the PEN-FAST score). In 2024, additional interventions are planned to include MyChart messages to patients and placement of posters in Allergy and Immunology clinics to remind patients if they have a penicillin allergy to discuss it with providers. Eventually, the goal is to expand education to increase awareness of the need to address penicillin allergy in other clinical settings (e.g., primary care and infectious disease). Ultimately, the Division plans to expand this project to the inpatient setting as well (potentially with beta lactam protocols) as detailed during Allergy and Immunology Division Ground Rounds on December 8, 2023, by PGY-4 fellow Faris Jaber, MD.
Endocrinology
Mount Sinai Beth Israel
Division Quality Champions:
Daniel Donovan, MD
Olga Kozachenko, NP-C

In 2023, the Division of Endocrinology at Mount Sinai Beth Israel continued its focus on three quality improvement goals.
The first quality initiative was to reduce hemoglobin A1C (HbA1C) levels in its diabetic patients
The Division approached this goal in two ways. First, the Division worked to reduce the HbA1C
New Patients with Documented Penicillin Allergy Presenting to FPA and CAM (141) (August 1, 2022-July 31, 2022)
level by 1 percent in all diabetic patients seen by its clinic providers. Second, the Division worked to increase the percentage of its diabetic patients with an HbA1C level less than 9 percent
Control is based on data from the year 2022
Previously identified challenges to achieving this metric included health literacy, preferred language, and patient adherence to diet, medications, and physical activity. In 2023, the Division’s Certified Diabetes Educators (CDE) remained instrumental in addressing these challenges. As an extension to the physician visit, they educated patients and emphasized best practices in managing the disease and its complications. The team also employed continuous glucose monitoring (CGM) to improve patient motivation and knowledge of how food affects blood sugar. Providers also insured quarterly patient visits (at minimum) and scheduled monthly appointments for those who were less adherent and could benefit from closer monitoring.
The Division also employed a patient language interpreter service to improve its outreach and care of non-English speaking patients. As a result of these continued multifaceted interventions, even more patients achieved the Division’s goal in 2023. In particular, 89.4 percent of patients met the goals of HbA1C decrease of 1 percent or HbA1C <9 percent in 2023 compared to 84.4 percent in 2022. In 2024, the Division will continue to work on this initiative.
The Division also focused on increasing the number of diabetic patients with a yearly dilated eye exam in accordance with ADA guidelines. Routine dilated eye exams are key to the early detection of diabetes-related eye diseases, including ones that can cause blindness.
The Division continued previous bundled interventions to achieve this metric. In particular, patients were educated on the importance of completing yearly eye exams and reminded to bring their external retinal exam report to their Mount Sinai appointment for review and documentation. During team meetings, providers were also reminded of the importance of documentation. Referring to our own ophthalmology service at Union Square also facilitated obtaining reports of eye examinations. In 2023, the Division observed a further increase in the rate of eye exam completion to 87 percent compared to 82 percent in 2022.
Diabetic Patients with HbA1C Checked
Hga1c <9% Goal Control
Finally, the Division continued its goal to improve the number of diabetic patients with a yearly foot exam in accordance with ADA guidelines. As with eye exams, the Division found that not all physicians documented foot exams when completed. In 2023, the Division continued to have patients remove their shoes at the beginning of each in-person appointment to encourage and facilitate the exam. Providers were reminded about the importance of foot exam documentation during provider team meetings and encouraged to refer patients to the podiatry service at Union Square.
Control is based on data from the year 2022
The rate of foot exam completion increased from 65.3 percent in 2022 to 77.8 percent in 2023. In 2024, the Division will continue efforts to improve compliance with this metric.
The Mount Sinai Hospital Division Quality Champions:
David Lam, MD
Nirali Shah, MD


In 2023, the Division was the proud recipient of the T1D Exchange Quality Improvement Collaborative Outstanding Adult Team Award. This award is given to “a well-rounded, highly engaged adult team with diverse team roles that demonstrates a working knowledge of QI methodologies in a clinical setting.” The Mount Sinai Diabetes Center at The Mount Sinai Hospital is a member of the T1D Exchange Quality Collaborative (T1DX-QI). This collaborative comprises 52 endocrinology practices nationwide, caring for more than 80,000 people living with type 1 diabetes. As a part of the collaborative, projects are undertaken by multiple sites with adaptation and supervision of the initiative executed by the local site.
In 2021, the Division initiated a quality improvement project to increase preconception counseling for women with diabetes by creating the “Preconception Counseling and Reproductive Education Program for People with Diabetes (PREPP’d)” program. Since 2009, there
Diabetic Patients with Foot Cream
Diabetic patients who had foot cream Goal Control
have been more than 6,000 pregnancies affected by diabetes at the Mount Sinai Health System. Women with elevated glucose during pregnancy are at risk of adverse pregnancy outcomes, and early planning and discussion of glucose goals are critical. Pre-intervention planning included identification of 439 patients at the The Mount Sinai Hospital campus (189 patients at the 17 E 102nd Street hospital-based clinic and 250 patients at the 5 E 98th Street FPA practice) who would potentially be eligible for counseling given their ages and pre-existing diabetes diagnoses.
The PREPP’d program included interventions focused on clinicians as well as patients both at the 17 E 102nd Street Diabetes Clinic (The Mount Sinai Hospital) and the 440 W 114th Street Endocrinology and Diabetes Clinic (Mount Sinai Morningside). To improve knowledge of preconception counseling, a pre-intervention baseline knowledge survey was administered to clinicians followed by educational lectures. In addition, resources were provided to clinicians to assist in documentation of patient counseling. Resources developed were based on existing American Diabetes Association standards of care and counseling topics included prioritizing history on reproductive health, pre-pregnancy planning specific to diabetes care and management, as well as diabetes goals during pregnancy. For patients with reproductive potential and a prior diagnosis of diabetes, a pre-intervention baseline knowledge assessment was administered with the intention to administer the same assessment six months–one year after the intervention.
In 2023, the Division continued its efforts to identify patients of reproductive potential and also continued to train clinicians. Previously, pre-intervention data was presented at the Endocrine Society annual meeting (ENDO 2022) and in 2023, post-intervention data was collected. Postintervention surveys were collected from 30 patients and 16 clinicians with results indicating an increase in both patient and clinician knowledge pertaining to diabetes and pregnancy (See Table 1). This data was accepted for poster presentation at the American Diabetes Association’s 83rd Scientific Sessions (San Diego, CA).
In 2022, the Division began a quality-improvement project focusing on ensuring patients living with type 1 diabetes, and using an insulin pump for their management, had an active backup prescription for long-acting insulin. Patients with type 1 diabetes require continuous insulin therapy to maintain glucose levels within a target range and avoid diabetic ketoacidosis (DKA), a
Table 1. Pre- and
Data
diabetes emergency. For patients who use multiple-dose injections of insulin, a long-acting insulin and a separate short-acting insulin before meals are used. For patients who use an insulin pump, only short-acting insulin is used; the pump constantly infuses insulin to “replace” the long-acting insulin. However, in the event of an insulin pump malfunction, this constant infusion ceases, placing the patient in danger of DKA. If the patient does not have a back-up long-acting insulin readily available, it also often leads to increased anxiety for the patient as they urgently emergently contact their provider seeking back-up treatment.
The Division identified patient, clinician, and system-level barriers as contributors to this quality issue. Patients are often unaware if they have back-up insulin that is unexpired and their insurance formulary coverage changes frequently. Clinicians often forget to ask their patients and lack resources to readily identify patients who lack back-up insulin. From a system perspective, the identification of patients using an insulin pump, at a practice level, is difficult due to how durable medical equipment use is documented within the electronic health record, therefore limiting quality reporting.
To date, the project has completed two PDSA cycles and, in 2023, initiated its third intervention and PDSA cycle. The first PDSA cycle incorporated back-up insulin assessment during the medical assistant (MA) pre-visit planning process. During the pre-visit planning process, patients with pumps had specific ICD-10 diagnosis codes added to their problem list and were asked if they had back-up insulin. MAs sent providers messages to alert them of patients who did not have back-up insulin. The second PDSA cycle involved prominent signs in exam rooms to prompt patients and providers to discuss the need for back-up insulin to decrease reliance on the medical assistant. With each PDSA cycle, there has been an increase in patients with back-up insulin prescribed, from a baseline of 32 percent to 69 percent at the end of PDSA cycle (See Table 2).
In 2023, with the successful increase in accurate ICD-10 coding to identify patients with insulin pumps, the Division initiated its third PDSA cycle, seeking a more automated reminder process. Patients with scheduled appointments and the appropriate ICD-10 code were identified through EPIC reporting and received a MyChart message before their visit, reminding them to check if they had back-up insulin at home and, if they did not, to ask their provider at their upcoming visit.
A third quality improvement project undertaken by the Division in 2023 focused on the implementation of a workflow to decrease the number of Patient Medical Advice Requests (i.e., MyChart messages) received by providers. The burden of the electronic health record system is frequently cited as a source of burn-out and dissatisfaction. Despite a large proportion of MyChart messages being non-clinical and administrative in nature, these messages are first received by
Table 2. Insulin Pump Users with Back-up Insulin Prescribed by PDSA Cycles
clinical providers. With the support of Mount Sinai’s Digital and Technology Partners, a MyChart pool was created that consisted of medical administrative assistant (MAA) staff already within the Division. A workflow was created for the administrative team to triage new MyChart messages to providers based on content and provide an opportunity to obtain necessary information by the staff before arriving in the provider’s inbox (see Figure 1). In addition to training, MAs were provided message templates for common message themes to improve efficiency and standardization of communication.
The workflow was put into place May 2023. At baseline, among the 20 providers with a total of 67 patient sessions, a median of 15.5 new MyChart messages were received per provider per day. Following implementation of the workflow, the median number of new messages received by providers was reduced by 30 percent to 11 new messages per day per provider. Notably, since implementation there has been a consistent decline of the number of MyChart messages received per provider, attributed to increased comfort by non-clinical staff and refinement in the workflow (see Figure 2). In 2024, the Division plans to continue to refine the workflow and include a layer of clinical triage for providers with a high volume of clinical sessions.

Figure 1 – MyChart message workflow with integration of MAA triage based on message content
Figure 2 – Median new MyChart messages received per provider per day for providers at FPA Endocrinology at 5 E 98th Street

Mount Sinai Morningside
Mount Sinai West
Division Quality Champion: Ilana Ramer Bass, MD

The Division of endocrinology at Mount Sinai Morningside and West initiated several quality projects in 2023. The first initiative was to implement a virtual diabetes self-management and support group. The target patient population for the support group is English-speaking, patients with type 2 diabetes mellitus, with no cognitive impairment. Patients must also have access to MyChart and be agreeable to a group setting. The benefits of using telehealth to conduct the support group include the elimination of transport barriers and cost and ultimately improve the noshow rate. The aim of this project was to utilize diabetes group education and support classes to improve HbA1C by 0.5 percent and to promote healthful lifestyle changes that result in at least one measurable behavior change (e.g., increase physical activity, eat balanced diet)
The diabetes self-management group meets bi-weekly and prior to the class the patient’s HbA1C and behavior goals are reviewed. During the group session, the patient creates at least one SMART (Specific, Measurable, Achievable, Relevant, and Time-bound). At the next session, the patient reviews their SMART goal and discusses whether the goal was met and as a group any barriers are discussed, or new goals are created. After six months, each patient receives a phone call to assess progress on their behavioral goal and to collect a final HbA1C
Patient Recruitment Flyer for the Diabetes Self-Management Support Group


In 2023, three sessions were offered that focused on an overview of diabetes management, monitoring, and nutrition. Demographic information for the patient participants is presented below.
Table 1. Patient demographics for diabetes self-management and support group (Q2-Q4 2023) (N=8)
Ten patients were referred to participate in the group. Eight patients attended on average and patients attended two sessions each. The average A1C prior to the start of the self-management group was 8.4 percent compared to 7.5 percent after the group session. Two patients met the goal of 0.5 percent reduction in A1C and three remained with an A1C of less than 7 percent (A1C was less than 7 percent for these patients at the start of the group sessions). All of the patients met the behavior goal initially, and 75 percent kept the goal at the end of the group sessions. Enrollment in the self-management group is ongoing and will continue in 2024.
The Division also sought to improve pre-operative diabetes control in patients undergoing elective surgery who see a primary care provider (PCP) at Mount Sinai. Uncontrolled diabetes poses many peri-/post-operative complications including infections, ileus, acute renal failure, and prolonged length of stay. The target patient population for this intervention is patients who have a
PCP at the Faculty Practice Associates with type 2 diabetes mellitus who are scheduled for surgery. Although this project is in the planning phase, the Division will utilize a visit with a nurse practitioner and certified diabetes educator and continuous glucose monitoring technology to improve diabetes control as measured by serum fructosamine before a scheduled surgery. The goal is to increase the number of patients who achieve a fructosamine of less than 325 (~A1C 8 percent) by 25 percent The Division is currently collecting baseline metrics and will continue this project in 2024.
Gastroenterology
Mount Sinai Beth Israel
Division Quality Champions:
Custon Tafadzwa (Taf) Nyabanga, MD

The Division of gastroenterology at Mount Sinai Beth Israel worked on several quality initiatives in 2023.
The first quality initiative was a focus on decreasing the no-show and cancellation rates for endoscopy. Common reasons for no-show and cancellation were identified, including patientinitiated cancellation or refusal, insurance or financial issues, patient not correctly prepared (e.g., not NPO), availability of escort, and change in patient condition (e.g., needing additional work-up with labs or consultant input). The baseline no-show and cancellation rate in 2022 was 24 percent, which was successfully decreased to 19 percent between January-June of 2023 through serial outreach phone calls from the MSDUS clinic coordinators at seven days, five days, and three days before the scheduled procedure.
To further address the no-show and cancellation rates, the Division changed the process for reminding patients. In May 2023, the outreach process was revised where the clinic coordinator called the patient 10 days before the procedure and a nurse called the patient five days before the procedure. Despite these efforts, the no-show and cancellation rate between July-December of 2023 increased to 22 percent. The Division also observed that use of GLP-1 agonists now adds to the reasons for procedure cancellation. The GI Division at all sites are investigating the impact of increased GLP-1 agonist use on cancellation rate and will continue with the initiative to decrease no-show and cancellation rates for endoscopy in 2024.
colonoscopy have a repeat procedure within one year. The Division will also shift future quality initiatives to the outpatient setting, and ensure a safe transition of care for patients after hospitalbased endoscopy services at MSBI transition to other sites.
The Mount Sinai Hospital
Division Quality Champions:
Christopher Cao, MD
David Greenwald, MD


In 2023, the MSH Division of Gastroenterology engaged in several new quality initiatives.
The first of these initiatives involved quality measures related to endoscopy. Indicators of a thorough examination during a colonoscopy include cecal intubation rate (CIR), adenoma detection rate (ADR), scope withdrawal time (SWT), and percentage of colonoscopies with adequate bowel prep as measured by the Boston Bowel Prep Score (BBPS).
CIR is defined as the percentage of colonoscopies in which the cecum was successfully intubated. The national benchmark is a goal rate of 90 percent of all colonoscopies and 95 percent of all screening colonoscopies. In the most recent quarter, the Division’s mean CIR was 97 percent, exceeding the recommended national benchmark.
An additional indicator of thorough examination is adenoma detection rate (ADR). The goal is detection of adenoma in 25 percent of patients – 30 percent in males and 20 percent in females –undergoing average risk colon cancer screening. The current ADR of the division is 39 percent, which exceeds this goal.
Rate of Cecal Intubation
Cecal Intubation Rate
Cecal Intubation Rate Goal
Fishbone Diagram of Root Causes of Inadequate Inpatient Colonoscopy Preparation












Different patients with different risk factors for poor prep (e.g.,comorbidities, poor prior prep, old age)

Pt not able to finish prep
Night time: prep v sleep






Some patients will just fail prep Inability

Scheduling issues

Failure to order additional prep when

In response, the Division developed an EPIC order set for inpatient colonoscopy bowel prep to facilitate improved interdisciplinary communication and documentation of bowel prep quality, dietary orders, patient education, and other patient “opt-in” decisions. The Division conducted house staff education on the importance of quality bowel prep and a health equity analysis of bowel prep outcome by age and preferred language.
The Division also continued to work on an initiative to increase compliance with Centers for Medicare & Medicaid Services (CMS) recommendations for appropriate follow-up intervals for normal colonoscopies in average risk patients (OP-29) and colonoscopy interval for patients with a history of adenomatous polyps (OP-30). OP-29 and OP-30 are CMS metrics that impact the hospital’s star rating.
To improve performance for OP-29, the team regularly pulls reports of non-compliant documentation with the goal of amending documentation 30-days post-procedure to become compliant. The Division also provides feedback to non-compliant physicians to educate them about follow-up interval and documentation standards. Through these interventions, the OP-29 compliance rate continues to increase. Like OP-29, OP-30 relies on appropriate documentation in Provation, an EMR software that captures follow-up intervals. Provider education in 2024 will focus on appropriate documentation to improve OP-29 and OP-30.
The third project involved capsule endoscopy training and reporting process improvements. A new training curriculum on capsule endoscopy for GI fellows was designed, reflecting the importance of video capsule endoscopy as a diagnostic tool in gastroenterology. In addition, after analysis of a process map, changes were implemented to expedite the reading of capsule studies, especially inpatient exams.

Pre-capsule study



Capsule study
Post-capsule study


































































Third-year gastroenterology fellows began reading inpatient and outpatient capsules in August 2022 and logged all capsules read as well as their indication, date of notification by endoscopy staff of capsule completion, date of fellow report, and date of finalization. A hashtag was also created (# Capsule Endoscopy) to expedite notification of fellows by endoscopy staff when capsule studies were completed and ready for review.
As of December 2022, the fellows read 63 studies. Average times were 1.2 days from capsule study to notification, 0.7 days from notification to fellow report, and 2.7 days from fellow report to finalization. These data are being compared to historical data as well as continually monitored and reported to improve performance.
The Division has been working on improving rates of cancelled procedures due to Glucagon-LikePeptide-1 Receptor Agonists (GLP-1 RA). GLP-1 RA have risen in popularity given their weight loss effects achieved through delaying gastric emptying and increasing satiety. A theoretical risk of GLP-1 RA includes that of gastric retention and aspiration during endoscopies. Anesthesia guidelines have recommended holding GLP-1 RA for one dose prior to endoscopy, and MSH policy has been adjusted to holding GLP-1 RA for two doses prior to endoscopy. This guideline change has resulted in an increased risk of endoscopy cancellations in the past year. In the second half of 2023, 24 percent of patients taking a GLP-1 RA experienced a procedural cancellation. A fishbone and process map were created to identify reasons for cancellation of outpatient procedures due to GLP-1 RA.
Patient presents with indications for capsule study
GI consulted for inpatient capsule study
GI team evaluates patient, confirms need for inpatient capsule
GI team communicates plan with primary team front line provider for capsule study
Primary team orders capsule study
Patient fasts and undergoes necessary bowel preparation
Inadequate fasting/bowel preparation
Patient ingests capsule
Patient in endoscopy suite, EGD and colonoscopy unremarkable
Patient requires further endoscopic evaluation
Patient resumes eating too quickly or no evidence of capsule passing Interferes with study
Nurse confirms that patient has passed capsule and completed procedure
Nurse informs primary team of capsule completion
Capsule passes through digestive tract while capturing data
Endoscopy staff is notified of capsule completion
GI reading team is notified of capsule completion
Capsule study is read
Study report is finalized
Final study report is uploaded to Epic
GI team notifies primary team/patient of results
Primary team sees results directly on Epic
Subsequent interventions (e.g., endoscopic evaluation) can be arranged based on capsule findings
Capsule study delayed
MEASUREMENT



Patients with risk factors & many comorbidities

Patient anxiety about EGD

Reminders from coordinators about appt

Multidisciplinary teams coordinating EGD
Seasonal (i e. Holidays & frequent hospitalizations



Non-adherence to CLD (day before) or NPO (day of)
Anesthesia/sedatives







Patient education on diet & holding medications





An emergent case may come in, delaying the schedule
Difficult anatomy

Financial/insurance burden on patients

Not enough staffing

Scheduling issues













Cancellation of outpatient EGD




In response to this high cancellation rate, the Division is planning to instruct endoscopy staff to reach out to patients three weeks prior to their procedure to remind them to hold their GLP-1 RA as per MSH guidelines. This will be performed through implementation of an EPIC alert system notifying endoscopy staff of patients who are actively taking a GLP-1 RA.
Another ongoing project in the Division was the creation of a Celiac Disease (CeD) health maintenance EMR order set. CeD is associated with higher rates of osteopenia/osteoporosis due to malabsorption and pneumococcal infection. Patients with CeD should undergo dual X-ray absorptiometry (DEXA) within one year of diagnosis and be offered pneumococcal vaccine (PCV). In 2022, only 18 percent of CeD patients have undergone DEXA and 29 percent of patients have had PCV at MSH. The Division created a process map and expects to develop an order set for patients with newly diagnosed CeD to increase rates of DEXA and PCV at MSH.
Patient presents with concern for


Positive serologies?







Referred to GI for endoscopy
Positive histology?






Pre-diagnosis of CeD


Post-diagnosis of CeD






Finally, the Division continued to promote clinical pathways designed to improve outcomes by standardizing care. Pathways have been completed and are now live in Epic for upper and lower GI bleeding, acute ulcerative colitis, acute pancreatitis, percutaneous endoscopy gastrostomy (PEG), and colon cancer screening.
Upper GI Bleed Pathway

Lower GI Bleed Pathway

celiac disease
Celiac serologies checked
Celiac excluded
Celiac excluded
Celiac Disease Confirmed
Patient follows up with PCP Patient follows up with GI
Healthcare maintenance discussed?
DEXA and PCV ordered
DEXA and PCV performed?
For each of these pathways, the team has worked with Mount Sinai’s EPIC reporting and data warehouse teams to create robust reports. As these pathways are introduced, the Division is now able to monitor their usage and track their impact on key process and outcome measures. Faculty and voluntary IBD doctors who specialize had an hour-long seminar to update on the inpatient severe UC guidelines as well as discuss focus areas for research and quality.
The Division’s goal for the upcoming year is to increase utilization of the developed clinical pathways.
Mount Sinai Morningside
Mount
Sinai West
Division Quality Champions: Tina Park, MD

In 2023, the Division of Gastroenterology at Mount Sinai Morningside and West continued working on the quality improvement initiative of adequate bowel preparation quality for screening colonoscopies. Suboptimal bowel prep may hinder detection of polyps, thereby decreasing effectiveness of screening colonoscopy. The American Society for Gastrointestinal Endoscopy/American College of Gastroenterology (ASGE/ACG) task force recommends the rate of screening colonoscopies with inadequate bowel prep to be less than 15 percent. Therefore, target adequate bowel prep quality was set at ≥ 85 percent
The baseline rate of adequate bowel prep in 2016 prior to intervention was 72 percent. With the standardization of bowel prep instructions across all sites, focus on patient education at each practice, and implementation of split dosing prep, the rate of adequate bowel prep for screening colonoscopies improved to 80-87 percent by 2020-2022. The rate of adequate bowel prep appears to have decreased somewhat to 75 percent in 2023. The reasons for this decrease are unclear, however the decrease may be attributable to patients declining the diet the day prior to the procedure and/or noncompliance with the completion of the bowel prep in the advised timeline. *Data was not collected in 2019 or 2021
Adequate Bowel Prep Quality
In 2024, the Division plans to focus on patient education at faculty practice and clinics. The Division will continue to pursue further improvements in bowel prep quality with interventions, including the use of extended bowel prep for patients with history of poor bowel prep in the past, and improved distribution of prep instructions to the patients. Instruction distribution will be via handout during the office visit or, for non-office patients, via email, mail, or MyChart message, as appropriate. Instructions are also available on the Mount Sinai website so they can be easily accessed by staff and patients.
The second quality improvement project, led by Dr. Emily Seltzer and Dr. Priya Simoes, sought to improve percutaneous endoscopic gastrostomy (PEG) tube placement workflow and outcomes. Appropriate utilization of PEG tubes requires careful evaluation of the patient by both the primary team and the gastrointestinal consultants. Failure to appropriately select and evaluate patients prior to PEG consults may result in delay in PEG placement, increased length of stay, and procedure complications.
The goal of this study was to develop a standardized workflow for appropriate consultation. Implementation of a standardized pathway was completed in two phases from September 1, 2022 to August 30, 2023. The first phase involved a comprehensive lecture on PEG tubes given to medicine residents and advanced practice providers. Covered topics included appropriate indications and contraindications, pre-procedure optimization, placement technique, and associated procedure risks.
The second phase included rollout of a PEG-related checklist in the electronic medical record for primary teams to use before calling a PEG consult (Figure 1). The primary outcome measured was time between initial consult and PEG tube placement. Secondary outcomes included patient length of stay (LOS), 30-day complication rate after PEG, and 30-day mortality. Outcomes in preintervention groups were compared to those in the post-intervention group.


A total of 227 patients (116 pre- and 111 post-intervention) underwent PEG tube placement (Table 1). Post-intervention, the checklist was utilized in 69.4 percent of cases. Compared to preintervention, time between consult and placement decreased in those where the checklist was used (5.30 vs. 4.69 days). The most common reasons for delay occurred less frequently post-intervention (infection: 17.2 percent vs 9.1 percent, goals of care issues: 8.6 percent vs 5.2 percent, and anticoagulation: 6.0 percent vs. 5.2 percent). Similarly, average LOS decreased from 57.33 to 47.62 days. In post-intervention checklist-utilized patients, PEG tube complications occurred less frequently (17.2 percent vs 9.1 percent) and fewer patients died from any cause, 30-days postprocedure (11.2 percent vs. 10.4 percent).
The findings of this quality-of-care study provides compelling evidence that introducing a preconsult checklist, complemented by education initiatives, enhances patient selection and optimization for PEG tube placement (see table below). A reduction in time from consult to procedure was noted. There was also a decrease in LOS, complication rates, and mortality rates 30-day post procedure; however, it is unknown if this is from the intervention alone. Future endeavors involve expanding educational initiatives and optimizing patient care across other departments and institutions.

General Medicine
Mount Sinai Beth Israel
Division Quality Champion:
Desiree Chow, MD

In 2023, General Medical Associates (GMA) at Mount Sinai Beth Israel continued to work on improving the quality measures identified by Mount Sinai Health Partners Clinically Integrated Network. These measures include diabetes control, diabetic retinopathy and nephropathy screening, hypertension control, colorectal cancer screening, and depression screening.
To improve the retinopathy screening rate for diabetic patients the Division partnered with the ophthalmologists co-located in the same building. The shared electronic medical record allowed providers to view retinopathy screening findings easily and surpass the system goal of 74 percent.
With regards to the aim of increasing the nephropathy screening rate among diabetic patients, the Division focused more effort on changing how the quality measure is defined and decreased the rate to 63 percent in the second quarter of 2022. To address this, the medical office staff pended orders for microalbumin in patients with a best practice alert. The medical office staff also instructed patients to collect urine samples during rooming to avoid missing an opportunity. While the screening rate did not meet the target, staff continue to be encouraged to distribute urine sample cups and pend orders.
Rate of Retinopathy Screening Among Patients Ages 18-75 with Diabetes
Rate of Nephropathy Screening Among Patients Ages 18-75 with Diabetes
The Division was able to achieve further improvements in the percentage of patients with uncontrolled diabetes through continued collaboration with the embedded clinical pharmacist and diabetes educator. During weekly team huddles with the care management team, patients with uncontrolled diabetes and upcoming appointments were discussed to review care plans. The clinical pharmacist also recently started accepting referrals for remote patient monitoring for diabetes.
To increase the rate of colorectal cancer screening, GMA continued the previous quality project of having the medical office staff pend Cologuard orders for patients due for screening and having nurses remind those with open orders to submit the kits. For patients interested in colonoscopy, direct referrals were continued. By quarter 3 of 2023, the target of 72 percent was surpassed
Percent of Patients Ages 45-75 with Colonoscopy within 10 years, Sigmoidoscopy within 5 years, Cologuard within 3 years, or Fecal occult blood testing within 1 year
The Division was able to improve hypertension control through multiple interventions, including having providers repeat elevated readings and document home recordings. The Division continues to refer to the remote patient monitoring program as nursing provides outreach to patients with uncontrolled blood pressure to review medications and home blood pressure readings in between visits. In addition, a nursing-led hypertension clinic to facilitate prompt follow-up of patients initiated on antihypertensive medication was established.
Percent of Patients Ages 18-85 with a Diagnosis of Hypertension with Last Recorded Blood Pressure <140/90
For the last CIN metric of improving the rate of depression screening and follow-up, the medical office staff continued to perform PHQ-2 screening on all patients during rooming. A laminated PHQ-9 was given to patients to complete if PHQ-2 screening was positive. Providers transcribed the results into EPIC and selected a management plan. Overall PHQ-2 screening and follow up PHQ-9 rates have improved. The Division will continue to work on improving documentation of a follow-up plan.
Patients Ages >18 with PHQ2 Depression Screening in the Last Year and Follow-up
PHQ2 Screening PHQ9 Completed Follow up selected
In addition to the CIN quality measures, the Division initiated an interdisciplinary quality improvement project that aimed to improve transitions of care from inpatient medicine floors to outpatient care at GMA in 2022. The project was presented at the 2023 Society of General Internal Medicine (SGIM) Mid-Atlantic Regional poster session.

For 2024, the Division will continue to build on the improvements made this year. A major goal will be to develop workflows around the Mount Sinai Health System hypertension dashboard.
The Mount Sinai Hospital
Division Quality Champions:
Nikita Barai, MD
Kelsey Bryant, MD
Kyle Koster, MD



In 2023, Internal Medicine Associates (IMA) focused on evaluating and refining team-based care processes for chronic disease management, adherence to age-appropriate cancer screening, and transitions of care.
Chronic Disease Management
Hypertension
The Division continues its focus on achieving blood pressure (BP) control. Multifaceted efforts include standardization of the workflow for BP checks in office and at home, as well as a cuttingedge remote patient monitoring program. IMA’s interdisciplinary, team-based approach to this challenge is represented in the workflow diagram below.
Internal Medicine Associates Hypertension Pathway


Hypertension Dashboard and SmartSet
Blood pressure is a dynamic measurement, and in contrast to quality metrics that are measured with the completion of a specific test (e.g., diabetic nephropathy or retinopathy screening), patients with hypertension move in and out of the numerator for “control” because this metric is calculated based on the last ambulatory measurement in the system. Without real-time data about patients changing control status, it is difficult to address control at a population level. After much effort at the system level, the hypertension dashboard went live in EPIC in the summer of 2023. Efforts are underway to train attending and resident providers at IMA on the use of the population health tools available in the hypertension dashboard to improve proactive management and appropriate referrals to existing care pathways within IMA. An EPIC smartset was also created with input from a working group led by Dr. Barai.
The hypertension dashboard can be used by all team members and workflows are in development to refine best uses. At present, front desk staff reach out to patients whose last ambulatory blood pressure is considered uncontrolled (>140/90 mmHg) AND have an average ambulatory blood pressure >150/90 without an upcoming primary care provider (PCP) appointment and not enrolled in the remote patient monitoring program to bring them back into care with their PCP or our hypertension specialty clinic.
In 2023, one hypertension related abstract was presented at SGIM and one oral presentation was given. Blood Pressure Control Fluctuation and Quality Standards Stacy Tsai, MD; Nikita Barai, MD; Kyle Koster, MD; Mary B. Fishman, MD; Kelsey B. Bryant, MD MPH, MS; Presented at SGIM May 2023 by Stacy Tsai, MD
A total of 8,363 patients had a diagnosis of hypertension (HTN) in October 2022. The HTN control rate decreased from 69.3 percent in September to 68.3 percent in October. In this one-month period, 642 patients lost their controlled status and 555 patients gained blood pressure control. Of patients who were considered “lost control” of HTN, a subset of 360 encounters were reviewed. The mean blood pressure (BP) of those who lost their control status was 150/83 mmHg. Some 73.9 percent of these BP readings occurred outside of the PCP office. Of those that occurred in a PCP office, 89.4 percent addressed BP control with the patient during the visit. Of the charts
reviewed, 245 patients had a subsequent BP recorded; 57.6 percent of these repeat BP readings were at goal.
Clinical Update in Cardiovascular Risk Factors
Dr. Bryant collaborated with four faculty members from external institutions to create a clinical update in cardiovascular disease risk factors, which was presented at SGIM 2023 in Colorado. Approximately 300 attendees participated. Dr. Bryant contributed her expertise in hypertension as part of the triad of diabetes, hyperlipidemia, and hypertension, as three modifiable risk factors for cardiovascular disease.
Home Blood Pressure Monitor Campaign
Home blood pressure monitor access continues through a partnership with Integra (a benefits manager) by creating a closed loop feedback process to track orders.

Hypertension: Blood Pressure Control (<140/90)
Diabetes
In 2023, IMA continued to use a team-based model of care involving certified diabetes educators and a dedicated high A1C clinic staffed by our internal medicine interns.
Diabetes Control: HbA1C > 9
15.2%15.1%15.6%15.4%15.4%14.8%14.8%15.1%14.8%14.5%14.2%13.5%13.9%13.5%13.5%13.4%13.4%13.2%13.3%13.4%13.2%12.7%12.7%12.6%12.3%
Dec2021Jan2022Feb2022Mar2022Apr2022May2022Jun2022Jul2022Aug2022Sep2022Oct2022Nov2022Dec2022Jan2023Feb2023Mar2023Apr2023May2023Jun2023Jul2023Aug2023Sep2023Oct2023Nov2023Dec2023
DM HbA1c Poor Control (PCMH measure) Goal
In May 2022, the proportion of patients with uncontrolled HbA1C > 9 reached the target goal of less than 15 percent This trend has persisted and continues to decline to 12.3 percent as of December 2023. While the quality target is <15 percent, we have adjusted our internal goal to <10 percent as we continue to strive to provide the highest quality of care.
Diabetes: Eye Exam
Dec2021Jan2022Feb2022Mar2022Apr2022May2022Jun2022Jul2022Aug2022Sep2022Oct2022Nov2022Dec2022Jan2023Feb2023Mar2023Apr2023May2023Jun2023Jul2023Aug2023Sep2023Oct2023Nov2023Dec2023
DM Eye Exam: HM Goal
IMA continues to offer diabetic eye exams using an on-site retinal camera. This resource has improved access to screening on the same day as PCP visit, and the rates of completion have increased substantially since 2021. In 2023, the Division partnered with the ophthalmology department, which proactively reaches out to patients with abnormal retinal scans to bring them in for dilated eye exams and treatment of their diagnosed conditions.
Diabetes: Medical Attention for Nephropathy
Dec2021Jan2022Feb2022Mar2022Apr2022May2022Jun2022Jul2022Aug2022Sep2022Oct2022Nov2022Dec2022Jan2023Feb2023Mar2023Apr2023May2023Jun2023Jul2023Aug2023Sep2023Oct2023Nov2023Dec2023
In 2023, the Division continued to prioritize nephropathy screening in patients with diabetes. In the fall of 2023, a new workflow empowering medical assistants to identify patients with an open care gap for nephropathy screening and provide the patient with a urine cup and pend the order for completion was piloted. Continued improvement in the completion rate is expected
Cancer Screening
Colorectal Cancer Screening
IMA continues to improve colorectal cancer screening (CRCS) rates. Ongoing faculty and resident education has helped raise awareness of stool-based screening, and stool DNA testing now accounts for the majority of new orders for CRCS Direct access colonoscopy. A dedicated patient navigator has helped to improve access to colonoscopy. System-level improvements such as the opening of a new Medicaid-certified site will further enhance colonoscopy access for patients in 2024. Further improvement will focus on patients preferring noninvasive testing, which has been limited by provider education, patient awareness, logistical challenges with kit delivery and return, and patient comprehension and retention of kit instructions.
Dr. Kyle Koster obtained a grant in fall 2022 from ExactSciences, the manufacturer of the stoolbased test Cologuard, with guidance and support from colleagues in Gastroenterology (Dr. Steve Itzkowitz, Dr. Pascale White, and Lina Jandorf), other DGIM faculty (Dr. Nikita Barai), and residents (Dr. Zachary Stauber and Dr. Edward Cytryn) to improve patient education on the Cologuard test and improve successful kit delivery and return. The main barrier the grant addressed was poor return rates of kits, which are mailed to the patient upon ordering and require the patient to follow instructions at home and mail the kit back.
DM Nephropathy Goal
The grant was used to fund two interventions: a dedicated patient navigator and video-based instruction at the point of order. iPads were rolled out in each firm in fall 2022 to allow providers to play an instructional video while patients wait for labs or preceptor review. This intervention did not enhance kit return rates in a post-hoc analysis, however. The navigator started in January 2023, and kit return rate within 90 days improved from 57 percent to 67 percent. This improvement has persisted throughout 2023, and MSH has committed to funding the position through 2024. Dr. Cytryn and Dr. Koster presented this work at a poster session at the American College of Gastroenterology annual meeting in Vancouver in October 2023. The Division intends to submit this work for publication, as well.
Despite improvement in screening rates, the number of downstream colonoscopies from IMA alone (additional positive tests attributable to navigation and the rate at which those patients complete a follow-up colonoscopy) are not large enough to sustain this initiative. Therefore, the program is expanding to support other practices to enhance the value of this initiative and strive for cost-effectiveness. The division plans to present this work at meetings in 2024 and publish the results as well.
Dr. Koster and others, including Dr. Minal Kale (IMA attending) and Dr. Ishaan Dharia (rising chief resident) also obtained approval from the Quality Improvement Committee to pursue a MyChartbased initiative to further improve CRCS rates. Patients due for CRCS will receive an educational message that includes a comparison of colonoscopy and Cologuard and allow the patient to respond to an EPIC message pool to request an order without seeing their PCP first. If ineffective, the Division will bulk-order Cologuard for patients due for CRCS. Analysis will be led by Dr. Dharia with intent to present at meetings and publish the results.
Dec2021Jan2022Feb2022Mar2022Apr2022May2022Jun2022Jul2022Aug2022Sep2022Oct2022Nov2022Dec2022Jan2023Feb2023Mar2023Apr2023May2023Jun2023Jul2023Aug2023Sep2023Oct2023Nov2023Dec2023
Colorectal Screening Goal
Breast Cancer Screening
IMA continues to improve breast cancer screening rates. Improvement in 2023 was enhanced by increased access to testing, including the opening of new sites for mammography. Patients in value-based contracts are also actively approached to schedule mammograms.
Colorectal Cancer Screening
Breast Cancer Screening
80.5%79.4%79.4%79.7%80.2%80.0%80.1%80.9%81.0%81.3%81.3%81.8%81.8%81.6%80.8%80.9%80.8%80.8%80.3%80.1%80.2%80.2%80.2%80.2%80.4%
Dec2021Jan2022Feb2022Mar2022Apr2022May2022Jun2022Jul2022Aug2022Sep2022Oct2022Nov2022Dec2022Jan2023Feb2023Mar2023Apr2023May2023Jun2023Jul2023Aug2023Sep2023Oct2023Nov2023Dec2023
Mammography (PCMH Measure) Goal
Cervical Cancer Screening
Cervical cancer screening rates remain challenging primarily due to issues around access to screening. IMA appointment access does not easily permit addressing cervical cancer screening exams during primary care appointments given that appointments usually need to address multiple chronic conditions in a short period of time. In addition, wait times for both gynecology and IMA’s well-woman clinic are several months, and many patients have few other options for gynecology care.
In 2023, new providers were hired (four faculty and one NP), allowing for additional sessions dedicated to cervical cancer screening exams at IMA. MSH Gynecology also onboarded new providers in Q4 2022, improving access for patients. Since early 2023, screening rates have steadily increased. The Division will continue to examine access to screening and assess provision of dedicated cervical cancer screening visits to serve the patient population in 2024.
Cervical Cancer Screening
62.2%61.8%61.3%60.9%60.6%60.2%59.8%60.1%60.0%60.1%59.7%59.3%59.6%59.8%59.6%59.9%60.7%61.3%62.4%62.8%62.9%63.3%63.1%62.8%63.4%
Dec2021Jan2022Feb2022Mar2022Apr2022May2022Jun2022Jul2022Aug2022Sep2022Oct2022Nov2022Dec2022Jan2023Feb2023Mar2023Apr2023May2023Jun2023Jul2023Aug2023Sep2023Oct2023Nov2023Dec2023
Cervical Cancer Screening Goal
Ambulatory Quality Dashboard
In addition to the Hypertension Quality Dashboard described above, a more comprehensive quality dashboard is under construction to provide real-time data at the system, department, clinic, and provider level. The dashboard includes population outreach tools such as batch messaging for patients with open care caps and batch ordering for various cancer screenings. As of December 2023, the dashboard is being piloted by early adopters and will be built into quality improvement workflows to improve efficiency in 2024.
Transitions of Care
IMA has a complex patient population with a high chronic disease burden and many psychosocial barriers to cost-effective care. Continuous efforts are underway to improve transitions of care for patients to steer utilization toward more cost-effective and lower-risk sites of care. The following initiatives are aimed at improving transitions of care.
LPN-based Discharge Follow-up
To prevent recurrent emergency department (ED) visits and hospital admissions prior to 2022, Licensed Practical Nurses (LPNs) called patients following discharge to review medications and schedule follow-up. In 2022, this process was enhanced with standardized documentation via EPIC dot phrases and training from the Transitions of Care Center (TOCC). In 2023, reporting was developed to better monitor reach and impact on 30-day post-discharge readmissions and ED visits. Reach has remained limited by staffing shortages. In 2024, the Division will continue to monitor and evaluate the program to assess impact.
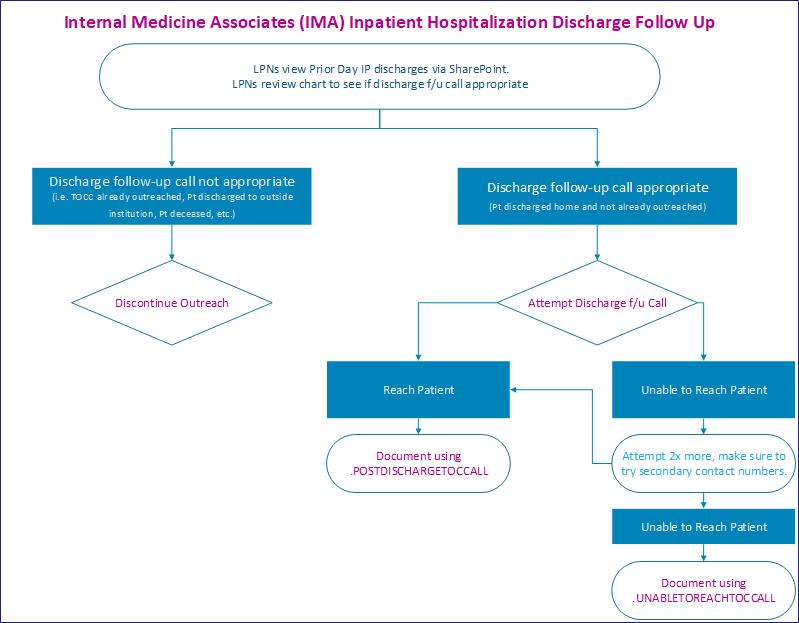
Unsuccessful call made by IMA LPN in 2 business days Successful call made by IMA LPN in 2 business days
Emergency Department Follow-up for High-Risk Patients
In 2022, IMA began a new process in which high-risk patients (defined as having either a last A1C > 8 and/or a last BP > 140/90 and/or 2+ ED visits in the last six months and/or two or more hospital admissions in the last six months) with no future IMA appointment are contacted by front desk staff to schedule follow-up. Reach rate has remained acceptable and show rate is on par with the IMA average. Beginning in late 2023, the process was expanded to all high-risk Medicare ACO patients who do not have follow-up scheduled within 14 days.

Data Reflects 05/02/2022 – 10/21/2023
NP Outreach for Discharge and ED Follow-up
In addition, IMA piloted NP-based outreach in response to a Q3-4 initiative with Healthfirst to followup all patients within seven days of hospital discharge and to follow-up patients with multiple chronic medical conditions within seven days of an ED encounter (these quality measures are known as MRP and FMC, respectively). The reach rate was excellent and the 2023 approach will be adjusted pending review of impact, cost-effectiveness, and available NP time in 2024. The goal is to scale successful work to all IMA patients as resources allow.


Mount Sinai Morningside
Mount Sinai West
Division Quality Champion:
Heather Viola, DO

In 2023, the Division of General Medicine at Mount Sinai Morningside and West continued efforts to improve chronic disease management. Improving hypertension (HTN) control and depression screening rates were main priorities. Two new projects for the year focused on improving abdominal aortic aneurysm (AAA) screening rates among male patients with a history of tobacco smoking and liver fibrosis screening in the diabetic patient population.
The first focus was on improving blood pressure control, with the Division increasing its target metric from 70 percent to 75 percent of hypertensive patients having a last blood pressure (BP) on file of <140/90. BP control steadily increased since initiation of the project, from 62 percent in January 2022 to 70 percent by the end of October 2023 (reaching a peak of 71 percent at the end of August 2023). All three practice sites realized improvement throughout the past two years.
The Division developed a new strategy and workflow that was implemented in 2022. The efforts were continued into 2023 with a four-phase approach.
The first focused on provider education. Practice site champions were assigned and given the responsibility of consistently reminding providers during staff meetings about tools that were available to improve blood pressure management. Providers were educated to inquire about home blood pressure and, if taken the same day as the appointment, to enter the reading into the vitals portion of EPIC for both in-person and telehealth visits. Because home BP readings count toward the metric, this is especially helpful in the “white coat HTN” population. Additionally, providers were encouraged to utilize telehealth for patients checking their blood pressure at home to titrate their medication regimen. Providers were also educated to repeat BP at the end of the visit if the initial triage BP was high and to ensure vitals were updated in EPIC with the repeat value. Blood pressure visits were also scheduled with on-site clinical pharmacists and nurses in between provider office visits.
Another tool available to providers is the remote blood pressure monitoring program. The goal of this program is to coordinate with clinical pharmacists and patient care liaisons in a condition management program to help bridge the gap between provider office visits. The overarching goal is to better control BP to reduce future cardiovascular events and improve patient outcomes. This program allows providers to monitor patients’ BP from the comfort of their own homes with the coordination of a care team. In this four-part program, the physician first identifies appropriate patients and places a referral. Next, eligible patients are enrolled, introduced to their care team, and provided with and oriented to their BP monitoring devices. During the clinical management phase, pharmacists reach out via telehealth to monitor and manage BP. Frequency of telehealth visits varies by patient risk level. All treatment updates are shared with referring providers. Part four is the clinical maintenance phase in which patients have reached their clinical BP goal but are still actively followed monthly by the pharmacist.
The second phase of the new BP strategy focused on medical assistant (MA) education. Dr. Yeriko Santillan, the W. 147th Street site champion, conducted a BP measurement education session with clinical supervisors at the three sites. The clinical supervisors then re-educated their staff on proper blood pressure measurement techniques in hopes of standardizing the triage vital signs process. There have been periodic routine competence assessments to check in on MA BP practices.
The third phase was the development of a shared BP workflow that centered on MA engagement and pre-session huddles. Providers added a “last BP” column to their EPIC schedule headers so that it appeared on their schedule of patients for the day. MAs printed the session schedule and highlighted those identified with a last BP on file of >140/90. During the pre-session huddles, the MA told the provider which patients had a high last BP. This made both providers and MAs aware of any patients with uncontrolled hypertension on the schedule that day and allowed them to focus their efforts accordingly.
The fourth and final phase of the BP initiative included an increase in direct outreach to uncontrolled hypertensive patients with a goal of getting patients into the office for blood pressure follow-up visits with either a provider, registered nurse, or clinical pharmacist. Care teams consisting of nurses and population health team members conducted telephone outreach to patients to schedule appointments, discuss checking blood pressure at home, and discuss medication compliance. MyChart messages were sent to patients that could not be reached by phone. The outreach team was also educated on how to enter home vitals into the EPIC flowsheet. The Division saw an enormous improvement in blood pressure control this year with these efforts reaching a compliance of 70 percent collectively with plans to continue this workflow into 2024 to hopefully reach the new target of 75 percent
The next focus was on improving depression screening, a new department metric added in 2022. PHQ2 screening and documentation of a follow-up plan for those screening positive was tracked with a target compliance of 70 percent. The practices started the year under the target metric and ended the year with a compliance rate of 80 percent, indicating successful implementation of the efforts.
A multidisciplinary approach to improve depression screening was utilized. The care team, including providers, MAs, and social workers, was involved in the effort to improve depression
Percent of Hypertensive Patients with Last BP <140/90
Target
screening. The first focus was on provider education. Providers were educated during staff meetings and reminded to consistently complete the PHQ-9 and document the follow-up action taken (i.e., medication prescribed, therapy referral made, etc.) in the EPIC flowsheet once the MA notified the provider of a positive PHQ-2 screen during triage. MA supervisors also conducted MA education by consistently reminding all MAs to complete the PHQ-2 depression screen at all visits during rooming in an effort to standardize the triage. Social workers are also involved with the new behavioral health referral pathway.
Evidence has shown that mental health follow-up improves with personalized care coordination; patients are more likely to attend appointments and continue to follow-up with a psychiatrist if linkage to care occurs through their primary care provider (PCP). In light of this, the Division has initiated a new behavioral health (BH) referral pathway at the practice sites to utilize the social work (SW) and care management (CM) teams to directly link patients with psychiatry. The objectives behind the new referral pathway are to increase access to timely behavioral health care for patients referred from primary care, to provide patients with a liaison who can ensure adherence and engagement with behavioral health providers, and to track conditions for successful referral connections and recommend areas where additional capacity is needed.
The new behavioral health pathway starts with the PCP identifying a need and referring to SW/CM via a telephone encounter in EPIC. The SW checks for options for therapy/psychiatry within Mount Sinai, reaches out to partner coordinators to help link the patient to a mental health provider, and checks in periodically to ensure engagement with the BH provider. Smartphrase forms for SW documentation were developed to allow the population health team to track BH referrals and followup. A significant improvement in the depression screening rates over the past year was demonstrated with successful implementation of the new depression workflow and BH referral pathway.
Preventive Care and Screening: Clinical Depression and Follow-Up Plan
A new 2023 initiative focused on increasing the percentage of AA screening with ultrasound in the eligible patient population. Eligible patients included men aged 65-75 who have ever smoked. With the help of the population health team, an opportunity for improvement was identified. Prior to the initiation of the intervention, throughout 2022, 653 patients in the west side practices were eligible for AAA screening and only 29 of those had completed an AAA screen
1. FIB-4 score calculation performed on 10 percent% of the eligible population across the practice sites
2. Some 50 percent of patients with a FIB-4 score ≥ 2.67 are referred directly to liver clinic
3. And 50 percent of patients with indeterminate FIB-4 (>1.3 or < 2.67) are referred for fibroscan
Secondary outcome includes:
1. Percentage of identification of patients with significant liver fibrosis using the screening algorithm
At staff meetings, the Division reminded providers of the new workflow. Medical assistants and PCPs would identify diabetic patients on the daily schedules. The PCPs would then calculate the FIB-4 score prior to the visit utilizing the Smartphrase provided. PCPs referred to fibroscan or liver clinic according to the algorithm as shown below during the office visit.

Depicted below is the data thus far from November 2022 through the end of October 2023. The below two graphs show the percentage of eligible diabetic patients screened utilizing the FIB-4 index SmartPhrase. The goal was to reach 10 percent, depicted by the pink line. Both practices, depicted by the dark blue line, showed an improvement over the first year of the project starting out at 0 percent increasing to 11 percent for 2109 Broadway and 20 percent for 638 Columbus surpassing the target goal at both sites by the end of October. The bulk of provider education was done around early March 2023 when screening rates started to increase, highlighting the importance of remaining consistent with provider education to continue the efforts.
Unique Patients Newly and Ever Screened using FIB-4 SmartPhrase at 2109 Broadway
Percent of Patients Screened for FIB4
Percent Ever Screened Goal
Unique Patients Newly and Ever Screened using FIB-4 SmartPhrase at 638 Columbus
The graphs below depict the total number of diabetic patients screened with the FIB-4 index from November 2022 to October 2023 at both practice sites and how many of those required and received a referral based on the FIB-4 score. At 2109 Broadway, 78 out of the 185 patients screened with FIB-4, or 42 percent, required a fibroscan or a liver clinic referral while at 638 Columbus, 81 out of the 171 patients screened with FIB-4, or 47 percent, required a fibroscan or a liver clinic referral.
Unique Patients Screened Needing and Receiving Referrals to Fibroscan (FIB4 ≥ 1.3): November 2022 - October 2023
Unique Patients Screened Needing and Receiving Referrals to Liver (FIB4 ≥ 2.67):
-
2023 Screened Need Referral to Liver Received Referral to Liver
Approximately half of the total patients (159/356) screened across the two practice sites required either a fibroscan or direct liver clinic referral based on the screening algorithm, as shown below. And 102 of those 159 patients, or 64 percent, had the referral given to them. 92 out of those 102 patients accepted the referral made by the provider. 62 out of the remaining 92 patients, or 67 percent, completed the fibroscan test or liver clinic appointment.
Referral Cascade: November 2022-October 2023
The majority of patients who completed the referrals, 55 of the 62 or 89 percent, did not have any significant fibrosis as shown in the graph below. Some seven patients, or 11 percent, were found to have advanced fibrosis or cirrhosis. All of the fibroscan and liver clinic referral orders for these patients were placed at the time of the visit when the FIB-4 screening SmartPhrase was utilized indicating the importance of the new pathway. The FIB-4 score prompted the physician to make the referral that may not have been done otherwise showing that without this workflow, advanced
fibrosis would have been missed in some patients and appropriate linkage to care with a liver specialist would have been reduced
Fibrosis Staging from Fibroscan
No Fibrosis or <F3, FIB-4 Scores 1.3-2.95
Identified with Advanced Fibrosis (F3), FIB-4 Scores 1.3-6.19
Diagnosed with Cirrhosis (F4), FIB-4 Scores 3.89-4.97
The Division also continued the initiative to improve the rate of diabetic eye exam screening. The effort was multidisciplinary: medical assistants (MAs) completed pre-visit planning during their triage by pending referrals to ophthalmology, providers placed referrals to ophthalmology during both inperson and telehealth visits, and nurse practitioners completed direct telehealth outreach to patients. MA education was emphasized along with obtaining outside ophthalmology visit reports and entering those visit dates into the EPIC Health Maintenance tab. With these interventions in place, the division saw the diabetic retinopathy screening completion rate increase from 61 percent in 2021 to 72 percent in 2023, surpassing the goal of 71 percent.
Compliance Target
The Division continues to focus on breast cancer screening rates for women aged 50-74. By the end of 2023, all three practice sites had a compliance rate of 78 percent, surpassing the target of 75 percent. Several interventions helped the Division reach the target. MAs routinely ask for screening tests, including mammograms, during triage. If patients report receiving a mammogram, it is entered into the health care maintenance (HCM) portion of EPIC. If not done and the patient is due for screening, the MA pends an order for the provider to sign to ensure it is addressed during the visit. If the mammogram was done but the report is not in EPIC, the MA calls the radiology center
Diabetes Mellitus: Dilated Eye Exam
after triage to obtain the report. EPIC also began routinely capturing mammograms completed at MSHS and by claims in the HCM section.
In addition, the existing mammogram van initiative continued at all practice sites. The van sets up outside each of the three practice sites one to two times monthly. Providers have the capability to directly schedule their patients with the mammography van. This allows for easier access to mammogram scheduling and for an alternative screening location for patients with barriers preventing visits to the radiology center.
Breast Cancer Screening: Mammogram Women Age >49 and <75 Compliance Target
Another preventive care initiative aimed to increase the rate of colorectal cancer screening. Rates improved steadily throughout the year, from 70 percent of eligible patients early in the year to 73 percent compliance at year end, surpassing the metric goal of 72 percent Providers/NPs/RNs were encouraged to be more proactive in counseling patients about alternative screening tests to traditional colonoscopy for average risk patients, such as Cologuard and fecal occult blood testing (FOBT), as there was reluctance to attend procedures during the pandemic. This hesitancy has subsided throughout this year, helping to increase the compliance rate. In 2023, the west side practices have consistently been some of the highest utilizers of Cologuard in the Mount Sinai System.
The Division worked to improve the previously established collaboration with the Gastroenterology Division to facilitate direct colonoscopy referrals. Colonoscopy referrals are directly placed by primary care providers, bypassing a visit with the gastroenterologist. The gastroenterology scheduling coordinator reaches out to the patient directly to schedule an appointment and discuss the preparation for the procedure. The direct screening tool was updated to include 45-50 year olds, allowing this age category to be captured in the metric.
The division looks forward to continuing this great improvement into 2024 while continuing to offer Cologuard to average risk patients and to streamline the direct colonoscopy referral process with colleagues in gastroenterology.
Colorectal Cancer Screening
Another quality initiative continued the ongoing effort to decrease the percentage of diabetic patients with HbA1C >9 (indicating uncontrolled diabetes) The multidisciplinary team surpassed the HbA1C metric goal (below 18 percent) by year-end, with only 12 percent of patients having a last A1C of >9. The Division continued to utilize telehealth for patients checking blood glucose via finger sticks at home. Medication adjustments and dietary/medication adherence were both discussed via telehealth. There was also a coordinated effort by certified diabetes educators (CDEs) and clinical pharmacists on site to follow poorly controlled patients more closely, scheduling regular office visits in between provider visits. Utilization of point of care HbA1C testing during the visit was encouraged so medication changes could be made with the patient still there. The Division will continue to use telehealth to optimize diabetic management into 2024 as well as link the patients with CDEs and pharmacists to further reduce the number of patients with A1C of >9.
Diabetes Mellitus: Hemoglobin A1C Poor Control
Compliance Target
Finally, there is an ongoing project focused on reduction of emergency room utilization by patients who see the Division’s PCPs. The goals are to identify high-utilizer patients at each practice site (defined as two or more preventable emergency room visits or two or more inpatient
admissions), reduce unnecessary inpatient and emergency room utilization and total cost of care, and identify appropriate interventions or next steps to help reduce further utilization.
This project is coordinated by a multidisciplinary outreach team that includes the front desk, referral coordinators, social workers, RNs, and NPs. The interventions include care management referrals, specialist referrals, follow-up appointments with providers, education around accessing care (urgent care vs. emergency room), and education around resources (community paramedicine, meals on wheels, etc.). This work continued efforts started in 2022 by focusing on priority conditions that can lead to high utilization. Outreach was focused on patients in the diabetic, congestive heart failure, and chronic obstructive pulmonary disease, registries to help optimize their clinical picture as well as offer assistance with social needs in an effort to reduce hospital utilization.
In early 2023, initial data from the 2022 interventions was compiled. As depicted in the below graph, in Quartile 1 (baseline data prior to implementing interventions) there were 524 ER visits (blue line) and 345 IP admits (pink line). In Quartile 3 after implementing interventions, there was a significant 61 percent reduction in ER visits with only 204 and a 66 percent reduction in IP admissions with only 119. At 180 days in Quartile 4 there was an even further significant reduction in ER visits with only 171 ER visits and only 95 IP admissions. As implementation of these interventions and a focus on priority chronic conditions increases, the Division hopes to continue to see an associated decrease in avoidable emergency room utilization over the next year.
ED and IP Utilization at Baseline and 90 and 180 Days
ED Visits IP Admits
Hospital Medicine
Mount Sinai Beth Israel
Division Quality Champion:
Dahlia Rizk, DO, MPH

In 2023 the Division continued work on bundled efforts to improve hospital priority metrics.
Readmissions and Length of Stay (LOS)
Dahlia Rizk, DO, MPH; Kristine Favila, DO; Svetlana Chernyavsky, DO
The rate of readmissions for the Division increased from 8.6 percent (0.79 O/E) in 2022 to 9.8 percent (0.92 O/E) in 2023. While the O/E was just above the 0.86 target, the Division still maintained the second lowest readmission O/E in the health system. To intensify efforts to decrease readmission rates, the congestive heart failure (CHF) discharge checklist was enhanced and a post-discharge clinic at MSDUS was implemented. Utilization of the CHF pathway remained stable at 55 percent from 2022 to 2023 but the percentage of heart failure patients discharged on appropriate goal-directed medical therapies increased from 2022. Specifically, discharge prescriptions increased for aldosterone antagonists (17.4 percent to 25 percent), sacubitril/valsartan (36 percent to 50 percent), SGLT2 inhibitors (27 percent to 53 percent), and beta-blockers (93 percent to 95 percent). Readmissions subcommittees for CHF, chronic obstructive pulmonary disease, pneumonia, sepsis, and acute myocardial infarction, continued to meet monthly to discuss ongoing strategies to reduce readmissions in their respective areas.
In collaboration with the ambulatory practice, a post-discharge clinic opened in July 2023 to target patients at high risk for readmission who were recently discharged from the hospital. Since the start of the program in July 2023, 510 patients were made appointments at the post-discharge clinic and 169 showed (no-show rate of 6 percent). A decrease in readmissions was observed for those who had a follow-up appointment at the post-discharge clinic scheduled within seven days (11.85 percent with no appointment vs. 0.47 percent with an appointment) and within 14 days (10.9 percent with no appointment vs. 1.4 percent with an appointment).
(51)
Readmissions by Discharge Month
January 2023 to November 2023
Length of stay for patients discharged from the medicine service by hospitalists improved from 5.66 days in 2022 to 5.55 days in 2023, while the O/E increased from 1.41 to 1.45. The excess days per case for patients discharged from the medicine service by hospitalists increased from 1.9 in 2022 to 2.0 in 2023. Potential causes contributing to the excess day increase include service line changes and an increase in guardianship cases. The Division maintained several previous interventions to address length of stay and excess days including team huddles when the census was especially high (Zone Red) and biweekly multidisciplinary meetings involving case management, social work, physical therapy, nursing, and the chief medical officer, to identify and address discharge barriers in cases with long lengths of stay. In late 2023, a new initiative called the “complex discharge team” was started as a collaborative effort among social work, case management, and leadership, to identify difficult discharge candidates with the purpose of instituting early interventions to help combat excess days. More than 15 referrals have been made in the first three months of this initiative and the Division expects this to increase. In 2024, the Division will continue working on these initiatives and enhance existing strategies with the IT tools available through EPIC, including the “Discharge Today” tool, and evaluate the impact of the complex discharge team.
Central Hospitalist (CH) Role Continued Growth Toward Virtual Care: Throughput & Quality
Dahlia Rizk, DO, MPH
Throughput and Level Loading via Central Hospitalist
The Central Hospitalist (CH) role was launched in July 2022 to support the throughput, quality, and efficiency of inter-institutional transfers within the Mount Sinai Health System and from outside organizations. The role comprises a small group of senior hospitalists specially trained to assist with triaging appropriate cases and optimizing communication with the receiving teams. More than 1.5 years since inception, the CH role continues to demonstrate value with sustained gains in efficiency
in time to connection with clinical providers, as well as in support of the Clinical Command Center by optimizing the quality and safety of the patients being transferred. After the first year of the pilot, the CH role hours were expanded to further enhance the connection between transfer physician assistant (PA) team and the Command Center. The earlier start time helped to eliminate the backlog of cases at change of shift.
In 2023, an AI decision support tool was added to assist the CH role in identifying high -yield ED patients for level-loading transfer to another MSHS facility. Since implementation, level -loaded ED patients have benefited from a reduced overall LOS compared with those not level-loaded. On average, a reduction of 1.6 days was observed, specifically as a result of reduced ED dwell time. The AI decision support was also able to identify an additional 11 patients for transfer weekly from baseline.

Hospital at Home (HaH) referrals by CH
The next phase of the Central Hospitalist role was to incorporate use of the AI tool to support referrals for Hospital at Home (HaH). Algorithms for “Alternate Destinations” were created, which identified those most suitable for care at home by the HaH team via clinical and demographic prioritization. Since implementation in July 2023, there has been continued growth in the number of patients accepted to HaH, with an increasing percentage referred by Central Hospitalists. In January 2024, CH referrals to HaH became around-the-clock in order to facilitate earlier identification, approach, and review by the HaH team. This change further bolstered HaH admissions and allowed the HaH team to focus on the clinical care of patients admitted to their service. The expansion also led to the highest number of referrals to the HaH program to date, with the highest ratio of patients in the program directly stemming from CH team referrals at 48 percent when compared to other referral methodologies.
*Data and technology partnership Palantir and Command Center Leadership
Additional Division Projects
Implementing a Night Float Curriculum at a Small Academic Medical Center
Kristine Favila, DO; Dahlia Rizk, DO, MPH; Christopher Tricarico, MD; Kimberly Christophe, MD; Ian Yu, MD; Jessica Goldberg, MD, PGY2; William Wallach, MD
The Division established a novel night float educational initiative for the internal medicine trainees. The goal was to improve attending supervision and the trainee’s educational experience during the night float rotation. The initiative consisted of a 60- to 90-minute teaching session five-to-seven nights per week during night float rotation. Teaching sessions were case-based and included brief discussions of overnight admissions with real-time faculty feedback. The sessions were also a forum for residents to ask questions and solicit input on cross-coverage care, and for nocturnists to share additional educational pearls. Resident satisfaction was anonymously assessed through a nine-question survey and a separate GME survey. There were 28 responses from 105 residents (PGY1s-PGY3s) completing at least one week of night float. Of those surveyed, 100 percent felt more comfortable knowing that an attending was available overnight, 41 percent described session as “somewhat useful,” 38 percent described them as “useful,” and 10 percent described them as “very useful.” A GME survey showed a significant improvement from 65th percentile to above the 90th percentile for the question related to “supervision at night” after implementation of the night teaching program.
Improving the Perception of Workplace Safety With Proactive Rounding
Jeremy Quentzel, MD; Patrice Alexandre, MBA, MSN, RN; Steven Daoud, MHS, AE-C; Patricia Dharapak, MD
In response to an increased number of SafetyNet reports of incidents of patient agitation and aggression, the unit medical directors implemented a multidisciplinary quality improvement initiative to target workplace violence and improve the organizational perception of safety. The two-week intervention occurred in October 2023 and focused on the night shift (7 pm-7 am) given the inherent vulnerabilities stemming from fewer staff, visitors, and leadership present in the overnight hours. While security personnel already perform nightly rounds to confirm functionality of the unit’s panic button, the intervention involved proactive rounding by security twice a night, which included participation in informal huddles with the charge nurse. Proactive rounding aimed to increase the
Identification of patients with sepsis that have missed BPA
CH to contact frontline provider to reconcile missed opportunity
Monitor overall success of program in reducting sepsis morbidity & mortality
visibility of security presence for both staff and patients on the unit. The informal huddles also served as a forum for staff to escalate impending safety concerns.
Post-intervention anonymous surveys of security personnel found that 94 percent agreed/strongly agreed that proactive rounding was useful to reassure staff, and were willing to continue with the initiative, and 81 percent agreed/strongly agreed that increased security presence could reduce incidents of workplace violence. Similarly, post-intervention anonymous surveys of the unit staff found that 80 percent agreed/strongly agreed that increased security presence was reassuring and could reduce incidences of workplace violence. Allowing for the confounder of changing survey respondents, a reduction in the unit staff’s reports of feeling anxious/demoralized/stressed daily to a few times weekly was observed from 67 percent to 50 percent. The unit staff respondents also unanimously favored continuation of this initiative. The pilot demonstrated that partnering with security personnel, proactive rounding, and team huddles were feasible, favorably received, did not add cost, and could ease the perception of workplace violence. Next steps include expansion of the pilot to include the day shift and quantifying the impact of this intervention on frequency of workplace violence incidents. This work was competitively accepted as a quality/innovation abstract submission to the Society of Hospital Medicine, and will be presented at the 2024 national meeting.
Back to Basics: Rapid Response Training for the Academic Hospitalist
David Fruchter, MD; Kimberly Christophe, MD; Benjamin Felder, DO; Jessica Goldberg, MD; Dahlia Rizk, DO, MPH; Patricia Dharapak, MD
The hospitalist role has traditionally been within the hospital setting where a dedicated Rapid Response Team (RRT) and critical care support are available to respond to acute clinical events. While hospitalist involvement in RRT/Codes can vary by institution, the academic hospitalist is infrequently the RRT/Code team leader. As the hospitalist’s scope expands to new environments outside of the traditional hospital setting, forums for continued faculty development in this area are increasingly prudent. Simulation training is one such forum, which can lead to improvements in selfreported RRT performance.
In anticipation of the academic hospitalist group providing medicine co-management and RRT/basic life support (BLS) coverage without internal medicine trainee or critical care backup at the Mount Sinai Behavioral Health Center (MSBHC), a targeted behavioral health RRT curriculum with simulation training was developed. The aim was to standardize best practices in RRT management and familiarize faculty with the most common critical scenarios to expect.
The experience level among the 30+ faculty hospitalist group varies between 1-25 years postresidency training. An anonymous pre-intervention survey revealed that 46 percent of respondents disagreed/strongly disagreed when asked if they felt confident leading an RRT/Code while another 19 percent responded indifferently. Not surprisingly, respondents who were closer to residency training (<5 years since graduating) reported feeling more confident. The first intervention was a faculty educational conference to provide an overview of the indications and outcomes of past behavioral health RRTs at their institution and review the management of common RRT scenarios. The educational materials were also made available for independent review on a shared drive file. The second intervention was to offer elective in-person simulation RRT training.
Preliminary post-intervention survey data suggested that a faculty development conference to review the expectations and management of typical RRTs was an effective means of building RRT confidence, with 86 percent of respondents in agreement/strong agreement. All of the respondents
who attended the in-person simulation training agreed/strongly agreed that the training improved their RRT confidence. In-person simulation RRT training augmented the positive effect of the faculty didactic on RRT confidence. Both learning modalities appeared effective at increasing faculty confidence in leading an RRT regardless of experience level. Next steps include longitudinal surveys to assess the durability of self-reported RRT confidence and analyzing the impact of the RRT curriculum on clinical outcomes. This work was competitively accepted as an education/ innovation abstract submission to the Society of Hospital Medicine, and will be presented at the 2024 national meeting.
The Mount Sinai Hospital
Division Quality Champion: Anne Linker, MD
The Division of Hospital Medicine (DHM) at The Mount Sinai Hospital is active in many different aspects of quality improvement and patient safety, including length of stay, readmissions reduction, safety in transitions of care, hospital acquired infections, and patient satisfaction. MSH DHM is also part of the systemwide effort to expand the Mount Sinai at Home program and is proud to be a strong contributor to the enrollments in Rehabilitation at Home and Hospitalization at Home. The hospitalists are also active in multiple hospital-wide committees, including the Root Cause Analysis Committee, CRC, DOM Quality Improvement Committee, LOS/Readmissions Committee, MSHS Sepsis Committee, and the MSHS Pneumonia Committee.
Length of Stay
In 2023, DHM worked on several projects aimed at improving length of stay (LOS). The Division has worked to balance the rising census with efficient care coordination. Ongoing initiatives to target reduced LOS included the Discharge Acceleration at Sinai Hospital (DASH) program, which has been previously reported.
New projects in 2023 aimed to understand the impact of patients transferred from other facilities (interhospital transfer), to optimize the transfer process, and to optimize the coordination of bedside procedures for hospitalized patients through a new Procedural Service. A new “Phone-A-Friend” Program was also started, which provides real-time guidance and mentorship to faculty caring for complex patients.
Interhospital Transfer
Members of the quality team completed a retrospective review of interhospital transfers accepted to MSH from March 27, to June 30, 2023, with the goals of identifying indications for transfer and outcomes among patients transferred to MSH during that time period and understanding potential opportunities for improvement in the transfer process. The electronic medical record was reviewed for outcomes including patient LOS, time from transfer acceptance to patient arrival, consulting specialties, mortality, and risk of 30-day readmission. The team identified 103 patients meeting the
inclusion criteria. Most patients, 69 percent, were transferred from within the Mount Sinai Health System. And 71 percent were known to the health system in the two years prior to transfer. Approximately half of the patients were transferred for evaluation for a procedure, and approximately one-quarter were transferred for expert evaluation from a specialty service not available at the sending facility. Procedures included thrombectomy for VTE, vascular stenting, renal biopsies, among others. Some 78 percent of patients received the desired procedure, with an average time to procedure after arrival of 2.5 days. Average LOS, readmission, and mortality rates for these patients were higher than the average for hospital medicine patients during the same time period.
This work demonstrates potential areas of opportunity in optimizing the interhospital transfer process, including the screening process for transfer and the acceptance process by specialists, as 22 percent of patients did not receive the procedure for which they were transferred. The average 2.5-day delay from arrival to procedure also suggests potential for improvement in care coordination prior to procedure, particularly for those patients within the health system.
Improving Cost and Time Efficiency in Procedural Needs for Hospitalized Patients
Historically at MSH, DHM has been responsible for completing certain bedside procedures, including paracenteses and lumbar punctures (LPs). Due to the low volume of procedures, many faculty have little opportunity to perform these procedures and keep procedural skill sufficient to supervise procedures or maintain credentialing. In a needs assessment survey among hospitalists, of 26 respondents, only 26 percent reported feeling comfortable performing an LP and 58 percent reported comfort with paracentesis. Among those with 4+ years of experience, 0 percent felt comfortable performing an unsupervised LP. In addition, waiting for procedures such as an LP due to the need for another team (i.e., neurology) to assist has led to delays in patient care and longer LOS for some patients. As such, DHM established an On-Call Procedure Team (OPT) comprising five full-time hospitalists to perform LPs and paracenteses.
The OPT was implemented in April 2023. At the time of evaluation on November 17, the team had performed a total of 78 procedures, averaging 2.5 procedures per week. Most of the procedures were LPs (74 percent). Only 15 percent of LP attempts were unsuccessful, requiring radiology assistance, and 4 percent of LPs were traumatic. These rates are consistent with the literature, suggesting OPT members performed high-quality procedures. Most of the procedures, 54 percent, were requested on a resident teaching team and the OPT provided supervision of 27 different residents. This format has allowed for a cost-effective solution and has increased bandwidth for procedures, expedited procedure execution, and increased mentorship and training for residents in performing procedures.
Clinical Mentorship for Complex Cases: Phone-A-Friend Program
In 2023, MSH DHM created a new program called “Phone-A-Friend,” which serves as a peer resource for hospitalists to discuss challenging or complex patients, and to promote clinical development for less experienced hospitalists. A peer mentoring model was developed in which three senior hospitalists (SHs) with at least 10 years of clinical experience and administrative leadership experience were available to discuss complex cases. The SHs were available to discuss cases on a weekly 30-minute meeting through a video conferencing platform (though this was later changed to a shorter daily meeting on weekdays) and through a group email.
From implementation in February through October 2023, 58 cases were discussed with the SHs for an average of 6.4 cases per month. Most of the requests were for assistance in addressing discharge barriers (16), resource utilization (14), clinical decision-making (12), and patient or family conflict (5). More than half the cases (30) were escalated by hospitalists with three or fewer years of experience. A similar number of cases were discussed across the resident teaching teams (26) and primary attending teams (22). Thus far, 51 cases were reviewed for quality outcomes, demonstrating an average length of stay (LOS) of 26 days, median LOS of 14 days, and five cases in which the LOS was more than 90 days. There were nine deaths among these 51 patients for a mortality rate of 17.6 percent. During this same period, the overall mortality for patients on the hospitalist service was 2.7 percent. Hospitalists of all years escalated cases; however, hospitalists with less than three years of experience escalated the majority of the cases. The patients discussed had long lengths of stay and were sick, with higher mortality rates than our average patient. This format was effective in providing guidance to early career hospitalists caring for a complex patient population.
Readmissions
DHM is proud to continue ongoing work in transitions of care, with the goal of improving our readmissions (O/E 0.99 for 2023). There has been active work with several groups, including pulmonology and cardiology, to improve our COPD readmissions as well as CHF readmissions. DHM also provides a lecture series to the internal medicine residents during ambulatory blocks focused on improving communication and coordination of care during the transition that occurs at discharge from the hospital.
Medication Reconciliation Project
Medication reconciliation (MR) is foundational to patient safety during and after a hospital admission. Though MRs are consistently obtained at the point of admission, they may be incomplete due to missing information or not documented in the appropriate EHR tab. A QI intervention was conducted from July 31, to November 3, 2023, to increase the number of MR completed in the EHR tab. An online guide showing the workflow was created and distributed to all residents. Each week, a “Med Rec Monday” email was sent out to resident teaching teams with their current MR completion rates, along with a reminder of how to correctly complete and verify MRs. At the end of each two-week block, cookies were rewarded to the team with the highest percent of MR completion. The names of the winning team were publicized to the entire residency program.
In the three months leading up to the project, the average completion rate of MRs among admissions to GMTS was 39.5 percent. Over the entire course of the project, the MR completion rate was 62.4 percent on average.
Medication Reconciliation Completion Rate 2023
Figure 1. Percent of completed medication reconciliations per team, per block
DHM plans to continue building on this work to improve patient safety, with the overall goal of improving both HCAHPS scores related to medication teaching and hospital readmissions.
Voice Recognition Grant
MSH DHM spearheaded a collaborative internal ($43,500) grant from the Office of Well-Being and Resilience to pilot the use of 3M Modal Voice Recognition Software on the Hospital Medicine service at MSH, MSBI, and MSW. The pilot includes 27 participants, for whom data regarding use of voice recognition for documentation is being tracked. Due to participant turnover, 34 participants were included in the pilot over 18 months.
In total, voice recognition (VR) was used for 4,845 notes during the pilot period. Roughly half of those clinicians (18) who initially agreed to participate did not use VR at all and five were rare users (0.1 percent-5 percent of notes). Eight hospitalists used VR in at least 10 percent-30 percent of their notes and three utilized the technology more than 30 percent of the time. The highest utilizer employed VR in 49 percent of notes. Among regular users, VR was used most frequently for consult notes (31.3 percent), progress notes (25.6 percent), and H&Ps (20.0 percent). Event notes (0.7 percent) and discharge summaries (5.3 percent) were least likely to involve VR.
While turnover of participants during the pilot period confounded the qualitative assessments of workload and burnout perception over time, a survey of 16 of 25 participants at the pilot’s conclusion found that 88 percent moderately or strongly agreed that VR improved productivity, enhanced note-writing efficiency, and made their job easier. Eighty-one percent agreed or strongly agreed that VR reduced the amount of time spent documenting after work hours. Users also found that VR increased note comprehensiveness. Approximately 30 percent of respondents reported prior experience with VR technology. Not surprisingly, those with prior experience were more likely to perceive enhanced note-writing efficiency using VR.
Burnout was measured using the Maslach inventory in the beginning of the project October 2022 and again three months later. In the category of personal accomplishment, average scores were
← Incentive Intervention
need is identified. There have also been patient cases where the Hospital at Home team has called services for plumbing, decluttering, and pet control, for patients who were unable to complete these tasks on their own.
Central-Line Associated Bloodstream Infections (CLABSI)
DHM has taken an active role in interdisciplinary work to improve rates of catheter associated blood stream infection at MSH. This has included unit dyad (unit medical director and unit nurse manager) weekly rounding on our medicine units, partnership with hybrid units to ensure weekly rounding on patients who have central lines on non-medicine units, dedicated monitoring of CHG bathing on medicine units, and review of CLABSI efforts at monthly Dyad meeting with Quality leadership. Huddles also occur for frontline staff when a CLABSI occurs, in cooperation with Infection Prevention.
CLABSI Rate Number of Infections Total CLABSI Infection Rate
In addition, there have been dedicated efforts to improve awareness of which patients have central lines, the need for intravenous to PO conversion of common medications when possible, and documentation of central line duration as well as peripheral IV duration in daily progress notes. There was an improvement in CLABSI rates and MRSA rates compared to the prior years across units KCC4S, KCC5S, KCC5N, GP 10W, and GP9W. In 2003 the CLABSI SIR rate was 2.07 (compared to 2.95 in 2022) and MRSA SIR rate was 0.70 (compared to 1.49 in 2022).
Central Line Utilization Number of Device Days Utilization Rate
Hospital Total MRSA Rate (per 10,000 patient days) Infection Rate Number of Infections
High-Value Care
The Student High Value Care Curriculum is an active and expanding part of the DHM Quality Improvement efforts. In the past several years, the curriculum was expanded to create partnerships with several other divisions and departments. This curriculum mobilizes and empowers groups of
medical students, masters’ students, and nursing students to work together to solve real-world challenges and to decrease overuse of materials and services in the hospital.
In the 2022-2023 year the curriculum sponsored three projects. The first was a collaboration with Emergency Medicine focused on improving registration of correct preferred language in the Urgent Care Setting. The second was a collaboration with the Division of Infectious Diseases to improve awareness of appropriate use of procalcitonin testing to improving antibiotic stewardship. The third project was in collaboration with Obstetrics and Gynecology to improve rates of MMR vaccination in post-partum mothers. Data collection for all three projects is ongoing and will continue in 2024.
Care for Patients with Limited English Proficiency
Providing equitable care for patients of all backgrounds is a priority. In 2023, an interdisciplinary group led by DHM that included a medical student, colleague in language services, two nurse practitioners, and two attending physicians sought to understand the barriers to consistent use of interpretation services, and then designed a bedside tool for brief communication for patients with non-English language preference (NELP).
A survey of nurses (RNs) and patient care associates (PCAs) on two acute care units assessed modes of communication used with patients with NELP, perceived frequency of interpretation service use, and staff experience when communicating with patients with NELP. Survey responses, collaboration with the Language Services Department, frontline nursing/care assistant staff, patient and family member feedback were used to revise card content and design. The card included icons and captions and was translated into six languages, as well as English for non-verbal Englishspeaking patients.
Some 75 of113 staff members, 66.4 percent, responded to the survey: 55 nurses and 20 PCAs. A majority (n=66, 88 percent) reported baseline difficulty communicating with patients with NELP. 56 (75 percent) reported using telephone interpreter services; 42 (56 percent) reported using hand motions; and 49 (65 percent) reported using simplified English. Regarding average frequency of telephone interpreter use per shift: 46 percent reported 0-1, 46 percent reported 2-3, and 8 percent reported 4+ times. Many noted that the time required to call an interpreter and scarcity of video interpretation devices (one per unit) were barriers to consistent use of interpretation services.
In addition, 13 educational huddles were performed across 10 inpatient units. 14 interviews of patients/caregivers were conducted by an in-person interpreter. Translated statements regarding the patients’ right to formal interpretation and an icon to request an interpreter were added to the card. Interviews were sometimes limited due to patient fatigue or disorientation.
The team found that, though there was initial enthusiasm for the card, logistical challenges made it difficult to sustain use on most units. This work will lay the foundation for additional work to determine how best to assist patients with brief needs, where calling an interpreter is difficult for staff due to time pressure and other barriers.
EPIC Secure Chat Optimization
Members of DHM have been instrumental in our work to optimize asynchronous messaging in EPIC Secure Chat. A GME-wide survey was created to assess communication patterns among trainees, which showed that more than 50 percent of trainees feel secure chat is easy to use; however, more than 50 percent of trainees don’t optimally understand features within secure chat and more than 50
percent feel inappropriate messages are sent via secure chat. As a result, a system-wide workgroup with representation across service lines and roles was created and has presented at several committees with the aim of creating a unified culture surrounding secure chat, gathering support for Epic Secure Chat use, and identifying pain points within workflows.
Improving Mobility for Patients on the Medicine Service
A team of residents and medicine attendings also worked to optimize mobility of patients admitted to the medicine service, and this work subsequently spread to the health system as a whole. Several residents in the Healthcare Leadership Track worked with two attendings in DHM to identify barriers to regular mobilization of patients by staff and to develop adaptive methods to improve mobility. The medicine admission order set was adjusted to spread awareness that bedrest orders should be reserved for patients who are unsafe to mobilize. This team also performed an educational intervention for residents on the medicine teaching team to encourage earlier evaluation of patients who may benefit from physical therapy and to encourage appropriate request for skilled physical therapy, as opposed to a request for general mobilization of a patient. Data is still being collected to determine the impact on patient mobility.
Mount Sinai Morningside
Division Quality Champions:
Brian Markoff, MD
Faye Reiff-Pasarew, MD


In 2023, the Division of Hospital Medicine at Mount Sinai Morningside embarked on new quality initiatives on opiate use disorder and advanced ongoing initiatives on laboratory stewardship, smoking cessation, and interdisciplinary rounding.
Laboratory Stewardship
Excessive laboratory testing can be painful, disturb sleep, decrease satisfaction, increase length of stay, increase transfusions, lead to venipuncture complications, and is labor intensive. Physician trainees often order extraneous labs due to a lack of understanding of what is necessary and fear of supervisor criticism. Electronic medical systems have simplified the ordering of lab tests, which can lead to recurrent ordering without much consideration.
The primary endpoint of this quality project was to reduce the number of common labs ordered on the inpatient medicine service per patient by 10 percent during six months. The process measure was the percent of patients with recurrent lab orders (labs ordered for multiple days), identified on a “recurrent labs” flag in the electronic health record (EHR). The team queried the EHR for the total numbers of the most common venous blood studies as the outcome measure (i.e., CBC, BMP, CMP, LFTs, PT/INR, APTT, Magnesium, Phosphorus, and T+S.). The project was divided into three phases: Phase 1 (January 3-20, 2023) established baseline data. Due to the low percentage of recurrent labs being ordered on the non-teaching service, the team focused on the teaching service. In Phase 2 (January 21-October 4, 2023), educational sessions were held for all providers,
the project team audited charts, provided feedback to providers, and distributed mouse pads that advertised the initiative with a QR link to an intranet site. The house staff was surveyed anonymously to assess barriers to reducing recurring lab orders. Phase 3 (starting from October 5, 2023 through the end of the year) broadened the aforementioned interventions to Mount Sinai West and introduced incentives for the teams.
Between January 3 and November 17, 10,144 charts were audited. The mean percentage of recurrent lab orders on the teaching service at Mount Sinai Morningside fell from 57 percent preimplementation to 42 percent and 17 percent in phases two and three, respectively. At MSW, the mean percentage of recurrent lab orders fell from 55 percent to 24 percent during phase 3. In the first six full months, the common lab orders per patient decreased by 14 percent at MSM over the prior year baseline, meeting the primary goal. The physician trainee survey during phase 2 revealed that the most significant barrier to reducing recurring lab orders was the additional workload that is required to check lab orders daily (87 percent), coupled with the concern over missing information (52 percent). The most frequently recommended approach to reduce recurring labs was to take the time to discuss lab orders collectively as a team during rounds.
An abstract was accepted for poster presentation to the Society of Hospital Medicine (SHM) 2024 conference.
Smoking Cessation With
Varenicline in Patients With Chronic Obstructive Pulmonary Disease
The Division of Hospital Medicine has continued its work with the Pulmonary Division to improve smoking cessation rates in COPD patients by initiating varenicline (Chantix) prior to discharge. The American Thoracic Society strongly recommends initiation of varenicline for smoking cessation, even in patients who are not ready to quit. Hospitalist initiation of varenicline takes advantage of the hospitalized patient’s forced abstinence from tobacco use, provides an opportunity for counseling on varenicline’s safety and efficacy, and decreases the barriers to initiation.
This project is a collaboration between the Pulmonary Division and the Division of Hospital Medicine at MSM/MSW/MSBI. The pulmonary division generates a daily EPIC list of patients admitted with COPD with active tobacco use and notifies the hospitalist teams. Hospitalists lead physician trainees and advanced practice practitioners in conducting varenicline counseling and initiation via an opt-out approach with the messaging “I’m going to give you a medicine that will change your relationship with nicotine.” Patients are discharged on varenicline and referred to a smoking-cessation clinic. After discharge, data is collected on smoking reduction and quit rates via chart review and phone calls.
Some 70 inpatients were prescribed varenicline between August 2022 and September 2023. Of the 60 patients for which there was data at six months, 22 percent had quit and 27 percent were smoking less. Of the 63 patients who were discharged with a prescription for varenicline, 36 percent had quit at six months and 32 percent were smoking less. This data compares favorably to self-reported tobacco abstinence at 12 months post hospital discharge, which has been noted to be 16 percent.
Future expansion of this project will be to additional hospitals within the Health System as well as to non-COPD patients who could most benefit from smoking cessation, such as cardiac patients.
An abstract was accepted for poster presentation to the Society of Hospital Medicine (SHM) 2024 conference.
Care Team Rounds
Throughput is a hospital priority. Decreasing length of stay (LOS) is essential to decongesting overcrowded hospitals and maintaining financial viability.
The team used the LEAN methodology of process improvement to perform a Value Stream Mapping exercise, which brought diverse clinical staff together to map the current state of inpatient throughput. The exercise identified efficient throughput delays each morning in the initiation of the clinical plan due to a lack of communication among the providers and the nurses (RNs), case managers (CM), and social workers (SW). A Kaizen (LEAN continuous improvement project) was then used to develop Care Team Rounds (CTR), an interdisciplinary working rounds on one of the medicine units with a geographically located teaching team. CTR combined the house staff presentations on the patients and discussion of plan of care with the attending with a report out by the RNs. CTR were also attended by the unit medical director, nurse manager, charge nurse, CM, and SW.
The primary aim was to reduce LOS over six months by 10 percent. The secondary aim was to improve patient communication as measured by the HCAHPS scores as well as to improve communication and workflow as reported by the care team. The non-nursing staff provided feedback via a survey tool. A qualitative analysis based on a focus group was used to assess the perspectives of the RNs.
CTR were trialed between March and November 2023. Though the initial length of stay (observed over expected) decreased from 1.97 to 1.35, it subsequently reverted to baseline. Overall, there was not a significant change in length of stay. The HCAHPS scores also did not indicate a significant trend, though the data was limited due to the low numbers of surveys on the unit and a delay in data reporting. In the survey of non-nursing staff, 40 percent said that CTR led to the initiation of the plan of care earlier in the day. And, 68 percent reported that the CTR improved communication with nursing. Overall, 65 percent wanted to return to the prior rounding workflow, 23 percent wanted to continue with CTR with changes, and 12 percent wanted to continue with CTR as it was. The main concerns from the attending physicians and residents were that there was insufficient time for teaching on these rounds. The main criticism from CM and SW was that too much time was spent on education that was not relevant to their roles. RN focus groups revealed that while CTR improved communication with SW and CM particularly regarding discharge planning, RNs felt the timing and length of CTR interfered with morning tasks. RNs reported that communication with providers did not change with CTR, and they continued to get information about the care plan from provider notes and through electronic communication (i.e., EPIC chat).
The inpatient medical service is challenging and requires balancing the needs of each team member with the need to expedite communication. Combining workflows expedites communication; however, it also leads to less efficient use of time. Future initiatives will use the lessons learned during this trial to strike the correct balance.
An abstract was accepted for poster to the Society of Hospital Medicine (SHM) 2024 conference.
Opiate Use Disorder
In 2023, the Division began a new quality initiative to address needs for patients with opiate use disorder (OUD). The Division is developing an order set and pathway along with training and
education that will support clinicians in managing opiate withdrawal via the Clinical Opiate Withdrawal Scale (COWS), pain management in patients with OUD, communication with patients with OUD, and transitions of care with respect to starting buprenorphine, methadone, and continuing pain management. In addition to measuring the use of the order set itself as a process measure, the Division will be measuring outcomes such as safety net incidences of workplace violence, naloxone administration, LOS, and readmissions.
Hospital Medicine (MSW)
Division Quality Champion:
Shantheri Shenoy, MD

Improving Medication Reconciliation Completion among Mount Sinai West General Medicine Teaching Teams
Medication reconciliation was added by The Joint Commission as a National Patient Safety Goal in 2005. Healthcare organizations are required to maintain accurate medication reconciliation information at transition points. Inadequate medication reconciliation can lead to poor patient outcomes, including readmissions. The goal of this project, led by Loren Barhold, PA, Chief Physician Assistant Hospital Medicine, was to improve medication reconciliation completion among MSW General Medicine teaching teams by 10 percent from August 1, 2023, to April 1, 2024. Baseline pre-intervention data showed a 55 percent medication reconciliation completion rate for inpatient General Medicine teaching teams at Mount Sinai West. Educational interventions for house staff, including a printed step-by-step guide on how to complete medication reconciliation, were distributed. A tutorial on how to interpret the medication reconciliation column was also conducted. In addition, safety data regarding medication discrepancies from inaccurate reconciliation is collected and shared with teams in a non-punitive way for feedback. Preliminary data from the first three months show an improvement in rates of medication reconciliation (see data below).
Percentage of Medication Reconciliations Completed Within 24 Hours by Teaching Team
Gold Silver Orange Purple
Improving Utilization of the Pneumonia Pathway for Inpatients at Mount Sinai West: A Care Standardization Initiative
The aim of this project, led by Fatma Abdel Qader, MD, was to increase utilization of the pneumonia pathway in Epic by 10 percent among inpatients. Baseline data for pathway utilization in patients admitted with pneumonia at Mount Sinai West is 2.6 percent for 2022 and 4 percent for 2023 YTD. The team has initiated educational interventions for house staff, hospital medicine faculty, and advance practice providers. Future interventions planned for 2024 include involvement of Unit Medical Directors and Unit Nurse Managers to remind care teams about the pathway during interdisciplinary rounds. The team is also focusing on involving clinical pharmacists in this initiative. Some of the other outcome measures this project intends to measure include: length of stay, mortality, and readmission rates for patients on the pneumonia pathway.
Increasing Naloxone Kit Distribution on the Inpatient Medicine Service
The aim of this project was to increase naloxone kit dispensing among patients at risk for opiate overdose admitted to the medicine service from 0 percent to 20 percent from October 2023 to March 2024, as this is a new initiative. Criteria for naloxone kit dispensing was established using guidelines from the New York City Department of Health and the Centers for Disease Control and Prevention. Baseline data obtained using ICD-10 codes suggested a total of 183 patients meeting criteria for a naloxone prescription over a three-month period on the General Medicine service at Mount Sinai West Hospital from January 2023 to March 2023. An algorithm detailing steps of naloxone kit dispensing was developed in collaboration with nursing and pharmacy. Large group educational sessions were conducted with the medicine residents, advanced practice providers, hospitalists, and nursing staff. Posters outlining prescribing protocols were created for each resident documentation room.
Ongoing interventions include chart reviews and reminder notifications to providers sent via secure Epic Chat. Preliminary data suggests a 53 percent increase in the number of kits offered from October to November 2023. Creation of a Best Practice Advisory in the electronic medical record for naloxone co-prescribing with high-dose opiates is planned as the next step to further aid in identification of at-risk patients.
Reducing Recurring Lab for Inpatients Admitted to Hospital Medicine at Mount Sinai West
The Division of Hospital Medicine at Mount Sinai West is collaborating with their colleagues at Mount Sinai Morningside on a project to reduce recurring labs for inpatients by 10 percent. The project was started in the fall of 2023 and is being spearheaded by Foram Parikh, MD, and Physician Assistant Nikta Athari
Interventions thus far have included educational sessions and rewarding the team with the lowest recurring labs with treats at the end of their two-week block. Preliminary data suggests a downward trend in the number of average recurring labs.
The Mount Sinai West Hospital Medicine team is also working on two other projects that will continue into 2024. The first involves improving utilization of intravenous iron in hospitalized patients with decompensated heart failure with reduced ejection fraction. This project is being led by Susan Lin, MD, in collaboration with cardiology and hematology teams. The project is in the initial stages of interventions and baseline data extraction.
Mount Sinai West Hospital Medicine is also working with social work and the patient relations team on a project titled the “Socially Complex Consult Initiative ” This project intends to bring together an interdisciplinary team to help providers in caring for patients who disagree with the recommended medical interventions to the point that it is no longer possible to care for the patient. In addition to having poor patient outcomes and increased length of stay, these scenarios can be emotionally and psychologically burdensome to the provider teams. The project was initiated in November 2023 and will measure the number of consults and time spent by the consult team as process measures, and length of stay and provider feedback as outcome measures.
Quality Improvement Peer Reviews (QIPR)
Mount Sinai Beth Israel
Division Quality Champion:
Patricia Dharapak, MD

The MSBI Quality Improvement Peer Review Committee (QIPRC) meets monthly to discuss the cases of patients who expired on the medicine service with the goal of improving care by identifying contributing circumstances and opportunities for improvement. Mortality cases are derived from the Quality Improvement Peer Review Trigger Tool (QIPRTT) and electronically assigned to reviewing faculty by the committee chair prior to each meeting. Each case is presented to the committee for discussion, after which the members determine whether the standard of care (SOC) was met through general consensus. If the SOC is met, the case will be closed. When the SOC is not met or met with room for improvement, corrective actions aligned with the identified contributing factors are implemented with the goal of preventing future similar occurrences.
There were 87 deaths on the medicine service through November 2023. The mortality rate was 1.2 percent with an O/E 0.66 (target = 1.0). To date, the committee reviewed 75 mortalities in 2023. As stipulated by the QIPRTT, seven cases receiving home hospice care at the time of admission were excluded from further review. Thirteen mortalities were transfers from other facilities. Forty-one percent of the mortalities reviewed were admitted to the ICU during their stay, palliative care was consulted in 75 percent of cases, and of those 73 percent were DNR and receiving comfort-based care at the time of expiration.
Death required further review
Death within 24 hours of Admission
The committee’s mortality SOC attributions were similar in 2023 to 2022. The committee consensus was that SOC was not met in four cases (6 percent), met with room for improvement in 14 cases (21 percent), and met in 50 (74 percent) cases.
For cases in which SOC was not met or met with opportunity for improvement, contributing factors were assigned. The most common contributing factors included delay in addressing abnormal test results (n=4) and treatment not monitored (n=3). For cases where the contributing factors were related to treatment, management, and diagnosis, efforts to improve quality of care were addressed through multidisciplinary peer learning case conferences, individual provider debrief, and through the resident quality improvement peer review curriculum.
Contributing Factors
Electronic Medical Record
Contributing Fall
Inappropriate treatment provided
Goals of care not documented
Hospital fall
Omission of care
Missed Diagnosis
Adverse drug event
Poor documentation
Hospital-acquired condition
Inappropriate medication dose
Delay address abnormal test
Treatment not monitored
Failure to escalate
Delay in diagnosis
Delay in Treatment
Three mortalities were referred to other divisions and departments for further review (i.e., pulmonary and critical care or nursing). The committee also referred two cases to SafetyNet, the Mount Sinai Health System reporting mechanism for safety events, near misses, or unsafe conditions.
In line with the health system’s mission to advance equity in quality initiatives and reviews, the committee began to examine preferred language in mortalities. In 2023, the preferred language of patients admitted to medicine was English, followed by Spanish and Chinese, which mirrored the preferred language of mortalities in the same time period. The existing literature suggests there is no significant difference in risk adjusted inpatient mortality between patients whose preferred language is English and those who preferred a non-English language. However, these studies typically excluded patients with missing language data from analysis. Within the health system, missing language data is specified in the electronic health record as either “Null,” “Language Not Listed,” “Need to Collect,” or “Unable to Communicate.” Using Tableau data, the committee observed that while patients with missing language data accounted for a small proportion (1.3 percent) of all inpatient medicine admissions across the health system in 2022, this group had a substantially higher crude and adjusted mortality rate when compared to those with a preferred language identified (Table 1). Within the missing language group, mortality differences were also observed (Table 2).
Table 1. Inpatient medicine metrics by preferred language2
*Missing Language includes: “Null’,” “Language Not Listed,” “Need to Collect,” and “Unable to Communicate”
Table 2. Inpatient medicine metrics by missing language sub-groups2
As meaningful equity analyses require accurate demographic information and inclusion of all populations, a sub-committee was formed to investigate this high mortality population. In 2022, there were 507 medicine admissions across the health system with language preference missing (includes “Null,” “Language Not Listed,” “Need to Collect,” or “Unable to Communicate”). After removal of duplicate admissions, 294 unique patients comprised the cohort.
Through targeted chart review for interpreter use or language documentation, the sub-committee was able to successfully re-classify the majority of this cohort as either English or non-English language preferred (Table 3). In the absence of corroborating chart documentation, some patients remained categorized as “unknown language.” In many cases, the initial categorization as missing language appeared to reflect severity of illness on presentation. Preliminary observations suggest that English was the most common language preference in the missing language cohort. The percentage of patients found to have a non-English preference was also observed to be higher in the charts reviewed from the missing language group than in the original sample (28 percent vs. 17 percent).
Table 3. Re-Classified Preferred Language after chart review
* Of 250 Unique Patients, 95 have been chart reviewed to date
Anticipated next steps after completion of chart review include assessing the impact of the reclassified missing language cohort on mortality rates and investigating the commonalities of this cohort to identify potentially actionable differences surrounding the hospitalization period. This work was competitively accepted as a quality/innovation abstract submission to the Society of Hospital Medicine and will be presented at the 2024 national meeting.
Lastly, in 2018 a resident Quality Improvement Peer Review curriculum was developed where trainees are invited to participate in peer reviews alongside the faculty committee. Prior to reviewing a case, residents attend a didactic session, which includes introduction to a framework for peer review and attribution of standards of care, and a review of different failure types and error subtypes. Paired with a faculty mentor, participating residents present their peer review findings at the meeting. In 2022, the curriculum became a required experience for all Internal Medicine PGY3s as it augments core skills required for internal medicine training (e.g., practice and systems-based learning and improvement) and provides an opportunity for individual reflection on providing care within a complex system. Since inception, the curriculum and committee continue to receive consistent positive feedback from trainees who have participated in peer reviews and committee discussions.
The Mount Sinai Hospital
Division Quality Champions:
Aveena Kochar, MD

The MSH Quality Improvement Peer Review Committee evaluates all mortalities and morbidities, meeting monthly to pinpoint care quality issues. Before these meetings, cases are reviewed by house staff under faculty supervision or by faculty directly. Cases raising quality concerns are then escalated for in-depth committee review. Cases for review are also acquired through referrals from faculty, from Safety Net, or from The Mount Sinai Hospital’s serious adverse event (SAE) process. Even in cases where hospital-level review determines the care to meet standard of care, improvement areas are frequently identified in the departmental review. This interdisciplinary committee includes a wide range of healthcare professionals who, after discussing a case, vote on the standard of care (SOC) provided. If the SOC is deemed not to be met or met with room for improvement, strategies for patient safety and risk reduction are adopted to prevent recurrence. When provider errors are identified, the providers involved are counseled.
For cases with significant safety concerns or requiring interdepartmental involvement, the committee forwards them to the hospital leadership's SAE process for a comprehensive review to identify root causes and develop corrective actions, aiming to mitigate patient risks and prevent future incidents. Cases are often referred to various divisions for additional, in-depth review.
In 2023, the department reviewed 151 cases, representing an increase from 139 in 2022. Some 85 patients had DNR status after admission, up from 72 in 2022, and 35 had DNR status prior to admission, an increase from 31 in 2022, with 57 ICU stays (see graph below). The patient would have benefitted from Palliative Care consultation during the admission in 15 mortality cases in the past year
DNR After Admit DNR Prior to Admit Patient was Comfort Care
Palliative Care
Palliative Care should have been consulted
Patient transfer to other Facility
Hospice
Death required further review
Death within 24 hours of Admission
Of the 151 cases reviewed in 2023, 132 (87 percent) met the standard of care, compared to 128 (92 percent) in 2022 (below). In 2023, 15 cases (10 percent) met the SOC with an opportunity for improvement, while 18 (13 percent) did so in 2022. There were a total of nine cases that did not meet SOC; three of the patients died in medicine units. Of the remaining six, five expired in the MICU and one in the SICU within 48 hours of transfer from a medicine unit. The three cases below represent those that expired in a medicine unit. The standard of care was not scored in 1 percent of deaths in both 2022 and 2023, as these patients expired while in hospice care and did not necessitate further review.
*Six additional mortalities that occurred within 24-48 hours of transfer to an ICU where SOC were not met were also reviewed
Most common factors attributed to mortalities and adverse events were treatment delays (n=6), delay in addressing an abnormal test (n=4), hospital fall (n=4), failure to escalation (n=3), poor documentation (n=3), and undocumented care goals (n=3). Other factors included failure to escalate, missed diagnoses, lack of treatment monitoring, and adverse drug events.
Contributing Factors
Contributing Fall
Inappropriate treatment provided
Goals of care not documented
Hospital fall
Omission of care
Missed Diagnosis
Adverse drug event
Poor documentation
Hospital-acquired condition
Inappropriate medication dose
Delay address abnormal test
Treatment not monitored
Failure to escalate
Delay in diagnosis
Delay in Treatment
In 2023 there were many patient safety solutions that were implemented. The solutions addressed improvements in clinical care as well as improvements in workflow. Many of the cases are referred back to divisions for further review and creation of safety solutions. In 2023, referrals were made to the following departments: Radiology, Palliative Care, Rheumatology, Pulmonary, Rapid Response Team (RRT), Nursing, Emergency Department, Gastroenterology, Pulmonary Embolism Response Team (PERT), and the Critical Care division.
In addition, many of the cases where room for clinical improvement was identified were presented in Resident Quality Improvement conference as well as the Division of Hospital Medicine (DHM) QIPRC conference for further discussion and education to providers. During these case review presentations, opportunities for earlier diagnosis and strategies for improving a multidisciplinary approach to patient care with consultant involvement and coordination of care were discussed. Many of the cases discussed in the DOM QIPRC meeting uncover gaps in clinical care for patients in a specific topic area. For example, a case of delayed Clostridium difficile (C. diff.) diagnosis led to further education to the Division of Hospital Medicine providers on the topics of C. diff, utilization of the C. diff pathway to decrease Hospital Acquired Infection rates, and when to utilize Infectious Disease consultation service for c. diff. Other cases led to increased education of rheumatological emergencies, a topic less often clinically seen.
In 2023, several interventions were implemented to improve clinical workflows. For example, the documentation of patients being transferred to another Mount Sinai facility was standardized. There was also nursing education on when to call RRT and the appropriate use of Epic Secure Chat, the EMR’s secure messaging platform. A pathway was created for overnight escalation of critical events from the intern to the more senior resident, standardized documentation was created, and this was disseminated in the introduction of the block to the overnight senior and overnight interns.
To improve the documentation of DNR/DNI status, the medicine units purchased scanners for the purpose of scanning DNR/DNI documentation electronically into the medical record system and
designated DNR during their admission. And 20 patients had an ICU stay prior to expiration, and 13 patients who died were transfers from other facilities.
Disposition
Death within 24 hours of Admission
Death required further review
Hospice
Patient transfer to other Facility
Palliative Care should have been consulted
Palliative Care
ICU Stay
DNR After Admit
DNR Prior to Admit
Patient was Comfort Care
Total Mortality Case Reviews
After reviewing a case, the committee votes to determine whether standard of care was met, met with opportunity for improvement, or not met. In 2023, as the graph below depicts, the committee determined that standard of care was met in 65 of the cases reviewed, standard of care was met with opportunity for improvement in 10 cases, and standard of care was not met in one case. There were nine cases not scored because the patient died while in hospice care and therefore required no further review.
Standard of Care Designation
SOC Met with Oppurtunity for Improvement SOC Not Met
Scored (Hospice Patient) SOC Met
In cases where the SOC is not met or met with opportunities for improvement, corrective action plans are developed and implemented when appropriate. Cases with quality concerns that are not appropriate for the committee are referred to the hospital quality department for further review and discussion. The graph below shows the three most common contributing factors in 2023 were delay in treatment (n=4), delay in addressing abnormal test results (n=3), and inappropriate treatment program. Following this were delay in diagnosis (n=1), omission of care (n=2), hospital fall (n=2),
failure to escalate (n=1), treatment not monitored (n=1), missed diagnosis (n=1), and goals of care not documented (n=1).
Contributing Factors
Electronic Medical Record
Contributing Fall
Inappropriate treatment provided
Goals of care not documented
Hospital fall
Omission of care
Missed Diagnosis
Adverse drug event
Poor documentation
Hospital-acquired condition
Inappropriate medication dose
Delay address abnormal test
Treatment not monitored
Failure to escalate
There were several areas identified as opportunities for improvement. Medication reconciliation has been a recurrent theme over the past couple of years. Dr. Markoff and Eva Johansson are currently working on a project that aims to address the lack of timely completion of medication reconciliation on admission to the hospital. The charts of patients admitted to the medicine service are audited; care teams of patients whose charts lack a completed medication reconciliation at 48 hours after admission receive a targeted message and reminder to complete this task. Attending physicians are given feedback two-to-three times a week. The outcome measure is the number of medication reconciliations completed within 48 hours of admission.
A delay in obtaining radiologic studies overnight was identified via safety net as an area for improvement. A meeting was completing with radiology to improve the workflow. The first person to contact is the ED-tech, second the radiology resident on-call, and third is the supervisor. The phone numbers for these individuals were listed on a document that was circulated to the residents and advanced practice practitioners and the hospitalists.
A delay in timely performance of lumbar punctures was identified in two cases. Upon further review, a root cause was determined to be the lack of provider certification, both among the hospitalists and the neurologists. Dr. Markoff worked with Dr. Patterson from neurology to create a work-flow to determine who to contact first when a lumbar puncture is needed. There is also an initiative underway to enhance provider training to perform lumbar punctures
Opiate use disorder management has also been a recurrent theme. There have been many rapid responses requiring the use of Narcan, and many more unreported cases of a delay in the diagnosis of opiate withdrawal. The hospitalists plan to address the following issues: the delay in treatment and management of opioid withdrawal, the management of pain in patients with opioid use disorder, and issues involving transitions of care. The latter includes referrals for methadone
clinics, initiation of suboxone inpatient, and outpatient follow-up with appropriate clinics. Inclusion of Narcan kits on discharge will also be included. The process measures to be used include a COWS scoring system, use and creation of an opioid order set, the number of patients discharged on methadone, and the number of patients discharged with referrals to methadone or suboxone clinics. The outcome measures will include the LOS of patients with opiate use disorder, the number of SafetyNet submissions related to Narcan use and workplace violence.
HIV screening was identified as another area for improvement. The health educator team already attempts to screen all-comers in the ER, regardless of admission, for HIV and HCV. Those patients with altered mental status or who are on contact are not approached. A barrier to completion of HIV screening was the additional tube of blood required. Team discussed messaging the frontline provider currently caring for the patient and asking them to add-on the lab for the following day for admitted patients. Reaching out to the attending for those patients whose frontline providers have not responded was also discussed as a next step. The outcome measure will be comparing HIV screening completion pre and post intervention.
Lack of awareness of the SafetyNet tool was also addressed. The importance of SafetyNet reporting was discussed in patient safety lectures for the PGY-1 class and the PGY2-3 classes separately. The number of safety events reported before and after the lectures will be compared.
Mount Sinai West
Division Quality Champion:
Irina Zaretsky, MD

The Mount Sinai West Quality Improvement Peer Review (QIPR) Committee convenes monthly to deliberate on morbidity and mortality cases leading to death and/or significant adverse events. Each month, faculty members are tasked with reviewing cases beforehand. Cases identified with quality concerns and necessitating deeper examination are presented to the entire committee during the meeting for discussion. Opportunities for improvement are identified with corrective action plans developed and implemented as required by participants.
In 2023, faculty reviewed 142 cases, a rise from the 103 mortalities reviewed in 2022. Of the deceased patients, 65 percent (92) received comfort care, compared to 62 percent (64) in 2022. Thirty percent (43) had a "Do Not Resuscitate" (DNR) status prior to admission, while 48 percent (68) acquired DNR status after admission to the hospital. Twenty-eight percent (39) of these patients had an ICU stay before passing away. Eighty percent (114) had interactions with palliative care, and it was suggested that an additional 7 percent (10) could have benefited from palliative care intervention. Twenty-five percent (35) of the deceased patients were transfers from other facilities, 7 percent (10) were on hospice at the time of death, and 4 percent (six) passed away within 24 hours of admission. Ten of the patient deaths were deemed to necessitate further review.
Patient Disposition
Total Mortality Case Reviews
Patient was Comfort Care
DNR Prior to Admit
DNR After Admit
ICU Stay
Palliative Care
Palliative Care should have been consulted
Patient transfer to other Facility
Hospice
Death required further review
Death within 24 hours of Admission
Of the mortalities reviewed, 108 (81 percent) were English speakers, 13 (10 percent) were Spanish speakers, three (2 percent) spoke Cantonese, one (1 percent) spoke Albanian, and one (1 percent) spoke Haitian. Data for seven (5 percent) patients were not collected.
Language
English
Spanish
Need to Collect
Chinese
Haitian-Creole
Albanian
All cases are thoroughly discussed and voted on electronically to determine if the standard of care (SOC) was met, met with opportunity for improvement (OFI), or not met at the monthly QIPR meetings by the multidisciplinary team of clinicians.
As the graph above depicts, 78 percent of cases were deemed to have met SOC in 2023 compared to 86 percent in 2022. Standard of care was not met in 6 percent of cases for both years. And 6 percent of cases were scored as standard of care met with opportunity for improvement by the committee in 2023 as compared to 5 percent in 2022. Some 9 percent of cases were not scored in 2023 because these patients had a designation of hospice and therefore do not require further review and discussion compared to 3 percent in 2022.
Contributing factors to cases not meeting the standard of care included treatment delays (four), failure to escalate (two), hospital falls (two), and individual attributions such as lack of treatment monitoring, delayed abnormal test addressing, hospital-acquired conditions, undocumented care goals, and inappropriate treatment.
Inappropriate treatment provided Contributing Fall
Goals of care not documented
Hospital fall
Omission of care
Missed Diagnosis
Adverse drug event
Poor documentation
Hospital-acquired condition
Inappropriate medication dose
Delay address abnormal test
Following the identification of cases where the standard of care wasn't met, key areas for improvement were identified and addressed through specific actions:
• Improvement in stroke recognition: A quarterly neurology lecture series was implemented to improve recognition of an acute stroke and review indications for calling a stroke code
• Re-evaluation of IR consult processes: IR consult process is being re-evaluated to ensure there is appropriate follow-up after an initial consult
• Inclusion of symptomatic hypoglycemia in RRT criteria: RRT policy is undergoing revision with consideration being given to the inclusion of symptomatic hypoglycemia in the criteria
• Amendment of the COVID-19 pathway to include COVID-19-specific DVT prophylaxis: Current COVID-19 pathway is being revised to include appropriate DVT prophylaxis based on severity of COVID-19 infection, renal function, BMI, and risk of bleeding
Infectious Diseases
Mount Sinai Beth Israel
Division Quality Champion: Tessa Gomez, MD

In 2023, the Division of Infectious Diseases at Mount Sinai Beth Israel remained committed to increasing viral load suppression rates at the Peter Krueger Clinic (PKC). The ultimate goal of HIV treatment is viral load suppression, or the reduction of HIV viral load to an undetectable level. Key interventions by the Division were designed to increase patient adherence to their treatment regimen and follow-up appointments while educating patients about living with HIV/AIDS.
Weekly care gap reports are reviewed by the care team to identify unsuppressed patients with upcoming appointments and those without appointments. Care coordinators implement outreach to patients to schedule and/or provide appointment reminders, and also confirm that patients are taking their antiretroviral medications as prescribed. Education, community support, and obstacles to care are provided by nurses and social workers, when needed.
Standardized guidelines are regularly utilized by the team to manage patients with treatment failure, which is defined as having two consecutive unsuppressed viral loads or intermittent viremia. The following checklist guides the process for unsuppressed patients:
• Make sure that a resistance test is done to exclude resistance as a cause of non-suppression
• Assess for factors associated with treatment failure (e.g., resistance, substance misuse, unstable housing, mental health, side effects, insufficient insurance, treatment complexity, diversion)
• Connect patients to social services, mental health, and substance abuse treatment as clinically indicated
• Recommend and if accepted enroll patients in care coordination
• Arrange monthly follow-up appointments for six months to assess response
• Refills should not be provided for more than one month for patients with detectable viral loads
• Patient who failed to appropriately manage their treatment must be discussed at the monthly multidisciplinary meetings
• A list of patients lost to follow-up must be submitted to the NYC DOH Care Status Report to determine care status
The PKC care coordinators are crucial in increasing the identification of patients with mental health and/or substance use disorders. These patients were ultimately linked to care and those not linked were aggressively targeted. With the presence of on-site psychiatry and psychotherapy for evaluation of these patients, this has led to a steady but albeit gradual increase in patient appointments. These additions to the team facilitated linkage to mental health care and further augmented efforts to achieve and maintain viral load suppression at PKC.
PKC Workflow: Enhancing Viral Load Suppression
Provider identifies patients form the weekly care gap list provided by IAM Quality Data Team
During visit, the Provider educates importance of viral load suppression and schedules nurse visit in four weeks
Four weeks later, the Nurse sees the patient and smart phrases are utilized to document education, counseling, and barriers
Care Coordinator sends reminder call to all patients for all scheduled appointments, including rescheduling
Overall impact on rates of viral load suppression
The Division looked at a new population of unsuppressed patients from January 1, 2022, to December 31, 2022, and continued to apply workflows and processes, actively monitor patients with unsuppressed viral loads, and incorporate Smart Phrases in the EMR to make appointments for nurse visits. Through these interventions, by the third quarter of 2023, the team was able to achieve a 59 percent reduction in the number of PKC patients with unsuppressed viral loads (improved from 53 percent in the previous year), and has maintained an overall viral load suppression rate of 92 percent in 2023. The DOH benchmark for VL suppression is ≥90 percent
Active Patients with Last Viral Load in Past 12 Months Below 200
*Bottom 25%, Median, and Top 25% are NYS eHIVQual Benchmarks
To reduce the number of unsuppressed established PKC patients, the Division compares patient and provider adherence to the PKC treatment failure protocol for VL suppression based on ongoing intervention, which is reinforced to mitigate nonadherence.
For 2023, the clinic’s other quality project was aimed at improving cervical cancer screening rates in the presence of on-site gynecological (GYN) provider. Cervical cancer screening is of particular importance for patients with HIV infection. The incidence of cervical intraepithelial neoplasia (CIN) is four-to-five times higher in HIV patients than in non-HIV patients.
At PKC, from 2021 to mid-2023 there was an on-site GYN provider available for four screening sessions per month. The baseline cervical cancer screening rate at the end of the fourth quarter of 2021 was 67.5 percent, as compared to a benchmark of 76 percent.
The clinic aimed to improve cervical cancer screenings by increasing provider referrals to the colocated GYN provider through development of workflows that assign roles and responsibilities to key quality improvement tasks, as well as by implementing and monitoring the new processes to assess for areas for improvement.
PKC Workflow: Cervical Cancer Screening
CTMS Downtown Harlem IAM Jack Martin Morningside Peter Krueger Samuels
The clinic faced challenges and limitations that include a majority of patients not keeping their appointments despite receiving reminder phone calls, some patients being uncomfortable with a male gynecology provider, some insurances not covering services, and overstretched referrals to female providers. Despite these challenges, by the third quarter of 2023, the clinic had achieved a 73 percent cervical cancer screening rate through the interdisciplinary workflows and processes involving front desk staff, nursing staff, and care coordination.
Active Patients at Peter Krueger Eligible for Cervical Cancer Screening (N=182)
Completed Cervical Cytology in Past 5 Years
Due for Cervical Cytology
The data for PKC patients due for cervical cancer screening were also stratified by age and race for the review period. As the graph below indicates, 47 patients were overdue for cervical cancer screening by September 2023, of whom 20 (42 percent) were Black/African American; 24 (51 percent) were white (of which 65 percent identified as Hispanic). Overall, 80 percent of female patients who were still due for screening were 50 years old and above.
PKC Patients Due for Cervical Cancer Screening by Age
Number of Patients By Age
The next steps for the PKC clinic include conducting monthly provider meetings to address clinical care gaps that need to be fulfilled, providing incentives to patients (possibly care coordination funds), nursing counseling for no-show patients regarding the importance of cervical cancer screening in the HIV population, outreach to overdue patients to schedule a new appointment, and consideration of creating a focus group among women who are due for cervical cancer screening to identify perceived individual or systemic barriers to cervical cancer screening.
PKC embarked on another quality project in August 2023 aimed at increasing health care proxy (HCP) completion for HIV + established active patients 65 years and older in the past two years as a pilot study The goal is to outreach HIV established patients who are 65 years and older to complete HCP forms. Ultimately, the clinic goal is to outreach the rest of the HIV + population.
PKC Workflow: HCP Completion for Patients with HIV
IAM Quality team sends weekly health proxy care gap list for patients with an upcoming appointment with provider to relevant RN and provider
• Started gathering data in August 2023
HCP form is uploaded in EPIC under Ambulatory Advance Directives by front desk staff
countersigns the HCP form as a witness
• Baseline: N=222 65 years old and older, HIV + established active patients were identified in the past two years; data provided by Institute for Advanced Medicine Quality Improvement (QI) data team
• N=155/222 or 69 percent HIV + established active patients who are 65 years old and older do not have healthcare proxy documentation.
• The goal is to decrease the number of individuals who do not have an HCP to at least 50 percent in the next six months
• After obtaining the baseline numbers, the quality data team provided us with a weekly HCP care gap list so we (providers and assigned RN) can efficiently and systematically identify patients scheduled for each week and discuss HCP forms with them.
Percent of Patients with HIV with Completed HCP Forms
• The next step is to review the data in the next six months to see the progress
• Ongoing outreach to patients for completion of HCP by utilizing the healthcare proxy care gaps weekly list
In 2023, the Division also worked on a new quality initiative on the inpatient service. One fellow-led project aimed to assess the impact of the S. aureus nasal PCR screen on patterns of vancomycin use in pneumonia, and its clinical and cost impact at MSBI. MRSA nasal screening
completed by PCR testing results in hours, allowing for rapid de-escalation of anti-MRSA therapy (within 24 hours) reducing antibiotic utilization, laboratory monitoring, and costs. To introduce MRSA PCR testing, the Division worked with physician trainees to introduce MRSA PCR testing during noon conference, collaborated with nursing management for nursing education, and worked with EPIC to ensure results are released in a timely manner. The Division also wants to recognize the significant contribution, collaboration, and work put in by Microbiology and Laboratory Medicine as they helped to make the S.aureus nasal PCR available inpatient at MSBI.
As of the end of June, 103 patients (75.7 percent) received vancomycin for suspected community acquired pneumonia (CAP). Of those who received vancomycin for CAP, 54.6 percent did not have any noted risk factors for MRSA. MRSA nasal culture was obtained in 98 (72 percent) patients of whom seven (7 percent) patients had positive MRSA nasal culture. And 30-day all-cause mortality of 40/136 (29.4 percent) of whom 43 percent COVID, 78 percent in ICU, and 58 percent had required mechanical ventilation. Data suggests providers rely on microbiological data to de-escalate vancomycin when used empirically with mean duration of treatment ~2.5 days and mean amount of ~4.25gm vancomycin.
Ongoing efforts of this initiative include: limiting empiric vancomycin usage to those patients with CAP who have identified MRSA risk factors as suggested by ATS/IDSA guideline recommendations, and provider education on the importance of MRSA nasal swabs in aiding the de-escalation of vancomycin in patients with cultures and MRSA nasal swabs that do not show MRSA.
The Mount Sinai Hospital
Division
Quality Champion:
Rachel Chasan, MD

In 2023, The Mount Sinai Hospital’s Division of Infectious Diseases (ID) continued to expand on its quality initiatives. With increasing time from the height of the COVID-19 pandemic, the Division has been able to shift attention from inpatient COVID-19 care to other areas, including the ambulatory setting and antimicrobial stewardship efforts.
The Division continued work on two ongoing quality initiatives in 2023: improving the rate of HIV virologic suppression and improving the rate of COVID-19 vaccination. In addition, the Division developed a new initiative related to an antimicrobial stewardship app, which will launch in December 2023 as a pilot and more widely in January 2024. Finally, the second-year Infectious Diseases fellows each work on a quality initiative during their fellowship, which covers a broad range of ambulatory and inpatient ID issues.
HIV Virologic Suppression
HIV virologic suppression remains a major focus in ambulatory ID care at MSH. In 2020, due to the impact of the COVID-19 pandemic on ambulatory care, retaining patients in care and ensuring ongoing HIV virologic suppression was a major priority. The team focused on promoting patient
engagement and integrating telehealth visits into its operation. This involved a large-scale effort to enroll patients into MyChart to enable electronic communication and video visits. Ultimately, 86 percent of patients with HIV seen at the Jack Martin Fund Clinic (JMFC) in 2020 achieved virologic suppression, defined as having a viral load less than 200 copies per mL, which was slightly higher than in prior years.
In 2021 and 2022, a multidisciplinary team comprised of care coordinators, social workers, and front desk staff continued to work on retention in care as virologic suppression. A member of the team contacted patients who missed or were at risk of missing appointments, and a list of unsuppressed patients with upcoming appointments was generated and reviewed in the daily clinic huddle. While most visits were conducted in person, telehealth remained a strategy to engage patients when helpful to maintain retention, such as during major weather events, acute illness, or when issues with mobility and/or transportation are a barrier to onsite care. A Department of Health-funded (DOH) care coordination program continued to work on assisting patients in need of additional support, and retention in care rebounded to the pre-COVID rate. Due to the Division’s efforts, the virologic suppression rate continued to improve and rose to 87 percent in 2021 and 88 percent in 2022.
In 2023, the major development in ambulatory HIV care at MSH was the relocation of JMFC to the new Harlem Health Center, where the program consolidated with Mount Sinai Morningside, in late September. A working group was formed in the year prior to the move to ensure clear communication with patients and facilitate ongoing retention and virologic suppression. Communication has been conducted via letters mailed to patients, handouts on site in the clinic, as well as phone calls and mass EPIC MyChart message blasts. Patient retention since the move in late September at the new location is being monitored closely, and targeted outreach will be performed to patients who do not show to scheduled visits or those who are not scheduled for ongoing care. In addition, the clinic’s multidisciplinary team will continue to meet monthly to address challenging patients. Finally, the Jack Martin team, along with clinic leadership from across Institute for Advanced Medicine (IAM), continues to work on expanding the injectable antiretroviral treatment (ART) program, which is a desirable option for many patients with HIV.
The HIV virologic suppression rate among patients at the Jack Martin Fund clinic reached a goal of 90 percent by September 2023, and the goal will be to maintain this in the new practice location.
COVID-19 Vaccination
The Division started a new project in 2021 to increase the rate of patients vaccinated against COVID-19 at the JMFC. This was a multidisciplinary project, which evolved throughout 2021 and into 2022, and involved active outreach by nursing, providers, social work, and the care coordination team. Vaccination was encouraged by all team members, and patients were frequently sent from their appointments at the JMFC to the vaccine pod directly for vaccination. A report was created in April 2021 to track vaccination metrics, and this was distributed to providers to review their panels, target unvaccinated patients to facilitate vaccination, and reconcile vaccine data in the EMR. These multidisciplinary efforts led to the program reaching a goal of 80 percent vaccination with the primary COVID-19 vaccination series.
In 2022, the Division continued to focus on both ensuring patients had received their primary vaccine series and encouraging booster doses. As of February 2023, just more than 80 percent of patients at JMFC had been vaccinated with a primary series, while approximately 76 percent had received a booster dose. However, uptake of the Bivalent booster had been more challenging, with
only 27 percent of patients having received a dose of Bivalent booster. In the fall of 2023, the monovalent XBB-containing mRNA COVID-19 vaccines were recommended for all persons 6 months and older, and the Division began work to address barriers to vaccination and increase uptake. Nationwide, early distribution issues led to delays in access to the vaccine, but the vaccine is now available on-site in the ambulatory ID programs and efforts to increase uptake will continue in the 2023-2024 fall/winter season.
Antimicrobial Stewardship: Firstline app
The Division of Infectious Diseases began to focus on developing an app to support antimicrobial stewardship efforts in 2023, through a collaboration with Firstline and the DOHMH. The app will allow for easy dissemination of, and access to, institution specific ID guidance including treatment guidelines and detailed information on pathogens and antimicrobials. Firstline is an app first launched in 2014 that currently serves more than 300 hospitals and health systems. Use of the app has aided an increase in the number of providers using hospital guidelines and an increase in appropriateness of antimicrobial prescribing. The app can also allow for rapid communication on updates to guidelines as well as antimicrobial shortages. Content development for the Mount Sinai Health System specific version of Firstline has been ongoing for much of 2023, and the app will go live first in a pilot phase for the ID division in late 2023, with a plan for system wide launch and education in January 2024. The Division will plan to measure app uptake and usage, including by provider type, as an initial metric. Ultimately, the Division will also be able to measure guideline concordant care.

Fellow Projects
Every ID fellow works on a quality-improvement project in the second year of Infectious Diseases fellowship at MSH. One project currently underway aims to address the transition to two-drug HIV regimens in the ambulatory setting. This is increasingly relevant with the growing number of twodrug ART options, including injectable cabotegravir and rilpivirine. These regimens are effective for HIV control and are well tolerated, but do not provide coverage for chronic hepatitis B, with which a significant number of patients with HIV are co-infected. A recently graduated second year ID fellow developed guidance on this transition, with consensus from stakeholders across the system from IAM and ID, and implemented an EPIC-based intervention to alert providers placing medication orders for two-drug ART regimens to remind them to check hepatitis B status. A current second-
Infectious Disease Screenings
In 2023, the Division also sought to assess the impact of the S. aureus nasal PCR screen on patterns of vancomycin use in pneumonia in the intensive care units. MRSA nasal screening completed by PCR testing results in hours, allowing for rapid de-escalation of anti-MRSA therapy (within 24 hours) reducing antibiotic utilization, laboratory monitoring, and costs. The Division educated providers on ordering MRSA nasal PCR swab when placing anti-MRSA agent (e.g., IV vancomycin) to treat for possible pneumonia. The Division also educated nurses and ICU staff on the process of collecting and sending the nasal swab for testing. IV vancomycin days of use per 1,000 patient days was tracked to determine if the intervention was successful in reducing vancomycin use. Post-intervention data showed there was less vancomycin use in each of the intensive care units, although the decrease cannot be attributed directly to this project as there were other simultaneous antimicrobial stewardship interventions.
Another initiative with the aim of reducing inappropriate antibiotic use, assesses the feasibility and utility of a clinical pathway to educate frontline providers about optimal communityacquired pneumonia (CAP) diagnosis and management. This project was conducted in collaboration with Infectious Diseases Society of America to implement a CAP algorithm derived from the 2019 CAP guidelines. The overarching goal was to reduce the overuse of anti-MRSA and anti-Pseudomonas aeruginosa agents for CAP management through education. Compared to the pre-implementation period, the overall usage of antibiotics decreased by 14 percent for antipseudomonal agents, driven by decrease in the usage of cefepime and meropenem usage decreased by 8.5 percent and 25.2 percent, respectively. The usage of gram-positive agents for MRSA increased compared to last year at MSW but decreased at MSM. Overall, the project was successful in decreasing the use of broad-spectrum antibiotics for CAP. There is room for improvement in the usage of anti-staph agents, especially vancomycin. In 2024 the Firstline app for antibiotic stewardship will be implemented systemwide and includes these CAP guidelines as well as other recommendations for appropriate use of antibiotics.
Liver Medicine
Liver Medicine
Division Quality Champion:
Ritu Agarwal, MD

In response to the high prevalence of chronic hepatitis C virus (HCV) and hepatitis B virus (HBV) infections affecting tens of thousands of people in New York City, Mount Sinai’s Division of Liver Diseases sought to enhance screening rates, subsequent linkage to care and treatment for patients who test positive.
Hepatitis C
To bolster screening rates and awareness, the Division of Liver Diseases continued various interventions throughout 2023. With the Center for Disease Control and Prevention's (CDC) shift in 2020 to recommend HCV screening for all adults, Mount Sinai adapted its screening practices through EPIC by updating the BPA alert, the health maintenance topic, and MyMountSinai notifications. The modified EPIC alerts now prompt providers to screen all adults for hepatitis C, and in MyMountSinai, all adult patients receive alerts prompting them to undergo screening, with notifications changing to "Not due" upon completion.
Additionally, the Liver Education and Action Program (LEAP) outreach team sends individual providers lists of screening-eligible patients before upcoming appointments and engages patients through MyMountSinai messages ahead of their visits. The outreach team also collaborated with the marketing department to promote HCV screening on social media platforms and monitors across the Mount Sinai Health System.
The Division also secured hospital leadership’s approval to update Mount Sinai’s HCV screening policy to reflect the CDC’s updated guidance and included recommendations on follow-up for patients who test positive. The updated policy can be found here: MSHS Hepatitis C Screening v.1 (policytech.com)
In 2023, as a result of all these efforts, HCV screening rates (newly screened patients/patients never screened) in primary care clinics continued to exceed the Division’s 20 percent goal. IMA’s screening rate increased from 25 percent in the third quarter of 2022 to 32 percent in the third quarter of 2023. During the same period, Mount Sinai Queens Family Health Associates’ screening rate increased from 33 percent to 35 percent. The screening rates at the Faculty Practice Associates and General Medicine Associates decreased slightly from 25 percent to 22 percent and from 31 percent to 25 percent, respectively. However, both still exceeded the 20 percent goal. At GMA, the decrease in the rate of screening is attributed to resident turnover in the summer, the new cohort received education in fall 2023 and HCV screening rates are expected to continue to improve. To ensure screening rates continue to improve the team will continue to distribute the list
of eligible patients to providers weekly. The Division’s goal to sustain HCV PCR order rates for Ab+ adults at 100 percent remained at 100 percent for 2022 – 2023.
HCV Screening Rates in Primary Care
To improve linkage to care, the LEAP team's patient navigators utilize a weekly EPIC report to identify HCV-positive patients, and conduct outreach to engage patients not already in HCV care. Navigators employ a comprehensive approach by making multiple phone attempts, sending physical letters or MyMountSinai messages, and reopening cases when patients re-engage. For reachable patients, they provide health education, schedule HCV evaluation appointments, offer reminders, and assist with insurance, transportation, and referrals. The Division also collaborates with the Emergency Department's HCV screening program. In 2023, 63 percent (n=323) of eligible HCV+ patients were linked to care (i.e., attended at least one appointment with an HCV provider), and navigators continue to engage an additional 17 percent (n=89), putting the Division on track to meet the 70 percent linkage goal for the year
HCV Navigation Outcomes for RNA+ Patients by Year
The Division also continued working on improving treatment continuum rates in Liver Medicine via care coordination for HCV+ adults. For patients enrolled into LEAP care coordination at the Institute for Liver Medicine in 2023, 82 percent (n=101) of eligible patients initiated treatment, exceeding the target of 76 percent. Many patients enrolled in 2023 are still in the process of completing treatment, so year-end data are pending. The following graph shows treatment initiation and completion rates over the past three years.
Treatment Continuum for Patients in LEAP HCV Care Coordination
Hepatitis B
In March 2023, the CDC revised its guidelines for HBV screening, transitioning from risk-factor based assessments to recommending universal one-time screening for adults. The World Health Organization (WHO) recommends screening in regions where prevalence is ≥ 2 percent. NYC presents a 2.9 percent HBV prevalence, with approximately 46 percent of individuals with HBV remaining undiagnosed. Anticipating the CDC's new guidelines, Mount Sinai’s Division of Liver Diseases proactively implemented universal one-time HBV screening for adults in primary care clinics in October 2022, becoming the first major health system in the United States to do so. Screening is supported by a new health maintenance topic in EPIC
The Division met with hospital leadership and management from population health, ambulatory care, electronic medical records (EMR) information technology, and laboratory teams, to secure buy-in, build the EMR modification, and disseminate provider education materials. The screening consists of three lab orders: HBsAg, anti-HBs, and anti-HBc, in alignment with updated CDC guidance. In response to primary care provider (PCP) concerns, several adjustments were made, including limiting the EMR alert to adults 18–79 years old rather than 18+, turning off patient-facing alerts, and creating a new EMR panel that includes all three labs in one order that is accessible directly from the health maintenance topic.
To complement the EMR alert, the Division conducted outreach to PCPs in three pilot clinics via presentations, feedback reports, broadcast and personalized emails, and a one page tip sheet that
Enrolled
Goal 4: Started Tx
Goal 5: Completed Tx/Cured
included division-developed smartphrases (see below) for providers to use to explain HBV screening lab results to patients via MyMountSinai messages.
HBsAg+ Refer to Liver in EPIC and email LEAP Patient Navigation Team (leap@mssm.edu or via EPIC P LEAP) .HepBPositiveMyChart
All Three Neg Vaccinate with 2 Dose Heplisav .HepBVaccinateMyChart
HBcAb+, HBsAg-, HBsAb+/-
Counsel patient cleared a past HBV infection. If immunosuppression is needed, they are at risk for HBV reactivation. Recommened LIVER referral beforehand: 212-241-7270 .HepBCoreMychart
HBsAb+, HBsAg-, HBcAb- Reassure patient they are immune. .HepBImmuneMyChart
Since implementation of the EMR alert (i.e., health maintenance topic), the average HBV screening rate has increased from 4 percent at baseline in September 2022 to 22 percent by September 2023 (exceeding Division target of 15 percent) across the pilot clinics that received the education (n=3) and from 3 percent to 15 percent in the clinics that did not (n=2).
Previously, Mount Sinai did not have a systemwide policy for HBV screening. While updating the HCV policy, LEAP leadership also secured hospital leadership’s approval to create a new HBV screening and vaccination policy to reflect the CDC and Advisory Committee on Immunization Practices’ updated guidance and included recommendations on follow-up for patients depending on their results. The new policy can be found here: MSHS Hepatitis B Screening and Immunization v.1 (policytech.com)
HBV Screening Rates in Primary Care
EMR Modification
LEAP patient navigators conducted patient outreach and navigation via phone, patient portal, and PCP engagement for patients who tested HBsAg+, with the goal of connecting them to liver care. From September 2022 to July 2023, the Division identified 284 HBsAg+ patients who were screened or had an encounter at one of the pilot clinics. Of these, 12 percent (n=34) were screened for the first time during this period and 41 percent (n=117) of these patients were not receiving guideline-concordant care for HBV even if they were aware of their diagnosis. LEAP linked 68 percent (n=79) of patients not in care to their first appointment, 11 percent (n=13) are still being followed by the patient navigators; and 21 percent (n=25) declined care or were lost to follow-up.
Patient Navigation Outcomes for HBsAg+ Patients
September 2022 - July 2023 (n=117)
Declined Linkage; 12; 10%
In Progress; 13; 11% Lost to Follow-Up; 13; 11%
Linked to Care; 79; 68%
For HBsAg+ patients who had a PCP but were not receiving HBV care, patient navigators messaged PCPs first to ensure alignment. Overall, PCPs welcomed the outreach efforts. PCPs helped us identify some of the reasons for the gap in HBV care:

P will continue its efforts to improve screening, linkage to care, and treatment rates for patients with chronic HBV and HCV. The Division will expand HBV navigation services to six additional Mount Sinai primary care clinics and further analyze barriers to care and possible
solutions for patients with hepatitis B. They also plan to continue to engage primary care providers around screening and to build community relationships to facilitate referrals.
The Division is also working on implementing HBsAg+ to hepatitis Delta virus (HDV) antibody reflex testing to improve HDV diagnosis rates.
Nephrology
Mount Sinai Beth Israel
Division Quality Champion: Elliot Charen, MD

The Division of Nephrology at Mount Sinai Beth Israel focused its efforts on increasing the percentage of patients without temporary catheters after 90 days on dialysis. Through education, the Division increased the percentage of patients without catheters by an average half a percentage point over the course of the year. This metric was confounded by the frequent influx of new patients with catheters and the departure of some patients with fistulas.
An ongoing Division goal is to decrease no-show rates for missed dialysis. The Dialysis Outcomes and Practice Patterns Study (DOPPS) indicated that missed hemodialysis treatments are associated with poor clinical outcomes. When one or more missed treatments occurred in a fourmonth period, hemodialysis patients were more likely to have worse laboratory measures, poorer health, and have higher rates of hospitalizations and mortality. Efforts to improve patient compliance with dialysis treatments were directed toward increasing communication and patient education. When nothing bad happens with a first missed treatment, the patient believes it is safe to miss more treatments. Continuous education is used to counteract this thought process.
Percent of Patients without Missed Dialysis Treatments
With these interventions, the Division was able to achieve an overall improvement in the percentage of patients without missed treatments.
The Division also continued to focus on decreasing 30-day readmissions for dialysis patients. By increasing education post-hospitalization and focusing on weight and fluid removal, an average additional half percentage reduction in 30-day readmissions was attained.
Finally, the Division collaborated with the critical care team on a resident-led quality initiative on the inpatient service to assess the effectiveness of the renal point of care ultrasound (POCUS) curriculum for trainees. The project aimed to assess the accuracy of resident-performed renal POCUS and its impact on the management of acute kidney injury. The Division is pleased to share that the project was presented at the American Thoracic Society (ATS) national meeting in Washington, D C , in May 2023.
The Mount Sinai Hospital
Division Quality Champion:
Joji Tokita, MD

Chronic Kidney Disease (CKD) Program
In 2023, the Mount Sinai Chronic Kidney Disease (CKD) Program expanded across the health system and is now active at more than 80 practices. CKD Program support includes engagement with a nurse practitioner for patient education, pharmacy review of medication lists with identification of opportunities for care optimization based on Kidney Disease Improving Global Outcomes (KDIGO) guidelines, and nutritional support provided by a CKD-focused dietitian. Scaling the program to encompass the large number of practices involved significant effort, including physician training and development of workflows for office staff. Clinicians continue to order KidneyIntelX tests on patients with type 2 diabetes (DM2) and early-stage CKD, and reports are available for more than 7,000 patients to date. Approximately 10 percent of the tested population has scored as high-risk and the team continues to work with the individual clinicians and practices in order to ensure an optimized clinical trajectory where possible.
In parallel to this work, a comprehensive CKD registry will provide detailed information on the size and status of the CKD population at Mount Sinai, including breakdown by stage as well as information about medication use (ACE/ARB, SGLT2, GLP1RA, MRA, etc.) and performance metrics (by provider and practice). Once finalized, this data will be shared with individual clinicians and ambulatory leadership for ongoing quality improvement purposes.
Availability of accurate and clinically relevant performance data is critical to ensuring improvements in long-term outcomes for this population. The first year of data from the Comprehensive CKD registry was presented at the American Diabetes Association Annual Meeting, including analysis of approximately 2,317 patients with at least 12 months of follow-up data. Key takeaways:
• Breakdown by risk score: High risk 11 percent, Intermediate risk 40 percent, Low risk 49 percent
• Post-test actions by risk score: High risk 50 percent, Intermediate risk 41.5 percent, Low risk 29 percent (actions include new prescription for SGLT2i, GLP-1 RA, or referral to specialist)
• Median HbA1C decreased from 8.2 percent pre- to 7.5 percent post-test in those scored as high risk (p<0.001)
• Median HbA1C decreased from 7.5 percent pre- to 7.3 percent post-test in those scores as Intermediate risk (p=0.001)
• The delta (post vs pre testing) in eGFR slopes was +2.5, +0.3, and +1.7ml/min/1.73m2/year for high, intermediate, and low, respectively).
Despite some of the successes observed with CKD program engagement, a number of challenges have been identified. Key among these include varying laboratory ordering practices (some pre and some post-visit, etc.), geographic challenges, lack of clinician familiarity with CKD and remote condition management in general, and, in some cases, reluctance to engage with the program. Concerted efforts are underway to resolve these issues, which are not entirely unexpected at large academic health systems. The team will be evaluating long-term outcomes in this patient population with the hope that improved compliance with standardized care will reduce CKD progression, lower cost of care, and improve quality of life.
Disclosure: KidneyIntelX is a commercially available New York State Department of Health approved predictive test that combines patient information and biomarker results. KidneyIntelX is based on technology developed by Mount Sinai faculty and licensed to Renalytix, Inc. Mount Sinai faculty and Mount Sinai have equity ownership in Renalytix, Inc.
Central Line-Associated Blood Stream Infection (CLABSI) Reduction Update: Nephrology
Despite significant long-term efforts to reduce the total number of inpatient CLABSIs, the incidence remains elevated. Central venous catheters (CVC) used for kidney replacement therapy (KRT), both tunneled and non-tunneled catheters, account for an important fraction of total inpatient CLABSI. In collaboration with hospital Infection Prevention, key interventions were implemented to reduce KRT-related line infections. These efforts included aggressive attempts to reduce total line days (no idle lines, etc.); use of arteriovenous fistula (AVF) as primary access wherever possible (now up to 73 percent at 117th Street, including AVG); use of standard line assessment form for dialysis patients when receiving hemodialysis (HD); a standardized approach to correct any observed deviations noted in status of line/dressing; use of a standardized line bundle for all dialysis patients; and strict adherence to portable and main reverse osmosis (RO) device/loop sampling and disinfection policy and procedure. All portable RO systems were replaced in 2022 and the main water treatment system was updated/replaced in 2023.
A detailed analysis of all 2023 CLABSI in lines used for KRT was performed. A total of 15 CLABSIs were identified in patients receiving KRT. And 12 out of the 15 CLABSIs were observed in patients treated “off-center,” who are generally sicker, in the ICU, or requiring special isolation.
Five cases were noted to have exit site concerns, such as dressing integrity, exit site bleeding, or skin breakdown.
In 2023 a corrective action plan was implemented to address the persistence of CLABSI, prioritizing aggressive measures to reduce the total number of inpatient line days. This has been one of the few successes as the CVC standardized utilization ratio (SUR) remains <1. Comprehensive audit of CVC dressing maintenance and access competency for all HD staff was conducted during the year and all staff participate in a quarterly audit of CVC care. Staff who interacted with a dialysis line in the 72 hours preceding a CLABSI event will be required to present a review at the monthly staff clinical quality meeting. Finally, close monitoring of patients with cirrhosis, coagulopathy, leukopenia, and immunocompromised status will continue, and lines noted to have flow concerns will be assessed and replaced if appropriate/feasible.
An overall reduction in dialysis CLABSI was observed in 2023 compared to 2022. It is unclear which measures directly impacted the outcome, however staff familiarity with and engagement in reduction efforts have improved during this time. The team aims to improve upon the performance in 2023 by continuing present interventions as well as making some adjustments in practice. In collaboration with the Vascular Access Service and colleagues in the Institute for Critical Care Medicine, the team will be changing catheter lock solution to heparin from saline (with the exception of patients who have contraindications to heparin). Lines that have recurrent flow issues will be replaced if standard measures are not successful in relieving arterial or venous pressure alarms. Outcome data on these measures will be reported in 2024.
End-Stage Renal Disease (ESRD) Quality Update
Clinical quality performance at the Mount Sinai Dialysis Center remains well above state and national averages. Overall performance on CMS Clinical Quality Indicators continues to exceed state and national averages. With respect to dialysis adequacy (measured by monthly Kt/V >1.2), Q1-3 2023 all met/exceeded 97 percent compliance. The clinic surpassed the national benchmark for management of hypercalcemia, and AV fistula and long-term catheter rates consistently outperform New York State and national averages.

Bloodstream infections remain a rare occurrence at 117th Street. The facility achieved a four-star rating in the annual dialysis facility compare report. A key challenge for 117th Street remains census management as the overall population has declined over the past three years, resulting in the closure of several shifts.
Dialysis Bloodstream Infections 2021-2023
Home Dialysis Programs: B1 Facility
Clinical quality performance of the Home Dialysis Programs has remained high despite numerous challenges during the COVID-19 pandemic. Peritoneal dialysis adequacy (measured by monthly Kt/V >1.7) was above 95 percent for the first three quarters of 2023.
Peritoneal Dialysis Adequacy (Kt/v >1.7)
Q3 2023
Q2 2023
Q1 2023
Q4 2022
Q3 2022
Q2 2022
Q1 2022
Q4 2021
Q3 2021
Q2 2021
Q1 2021
Like 117th Street, both units have seen a decline in census despite sustained efforts to ensure all patients in the CKD-ESRD transition period complete modality education and appropriate support in the decision-making process.

Pulmonary, Critical Care, and Sleep Medicine
Mount Sinai Beth Israel
Division Quality Champions:
Lina
Miyakawa, MD
David Steiger, MD


In 2023, the Division of Pulmonary and Critical Care Medicine at Mount Sinai Beth Israel (MSBI) and at the Respiratory Institute at Mount Sinai Downtown Union Square (MSDUS) continued collaborative efforts on various quality projects that encompassed both inpatient and outpatient practices.
Chronic Obstructive Pulmonary Disease Readmissions Reduction Program
Chronic obstructive pulmonary disease (COPD) is the third leading cause of 30-day readmissions among Medicare patients. Approximately 20 percent-22 percent of patients with COPD will be readmitted within 30 days. The Division is actively involved in a systemwide standardization of COPD Care initiative, which introduced a number of protocols and templates based on best practices and evidence-based data. The goal of the initiative is to optimize COPD management and improve the quality of care and safety of patients admitted with COPD. Identifying patients admitted with an acute exacerbation of COPD (AECOPD) in real-time facilitates the necessary multidisciplinary care of these patients to optimize their inpatient management and reduce the risk of a potential readmission. New criteria have been developed to identify patients admitted with AECOPD and capture them on a COPD list in EPIC. Patients will appear on this list when the “COPD Order Set” is used, a signed Pulmonary Consult Note is present, or when there is an admission diagnosis or hospital problem with a specific DRG code.
The Division, working closely with Oana Randolph, Associate Director of Clinical Integration at Mount Sinai Health System, launched a COPD Discharge Care Bundle whose aims include optimizing the safe transition of admitted patients with an acute exacerbation of COPD to the outpatient setting, and reducing avoidable readmissions. The bundle is activated for a COPD admission if the COPD order set has been used, a signed COPD consult note is present, or the patient appears on the EPIC COPD list. The patient then receives pulmonary consultation, spirometry testing (if not completed within the previous year), and comprehensive education regarding their diagnosis during the hospital stay. The patient also receives an inhaler regimen for discharge, a phone call within 72 hours of leaving the hospital, and a pulmonary outpatient clinic appointment within 7-14 days post discharge. The patient may also be referred for Pulmonary Rehabilitation, smoking cessation counseling, palliative or hospice care, or to the Remote Monitoring Program (below).
The COPD Discharge bundle played a major role in reducing COPD readmissions at MSBI. The COPD readmission rate to date was 14.8 percent (O/E 0.93) for 2023 compared to 16.9 percent for 2022, and 24 percent for 2021. In addition, the COPD mortality rate (in-patient and 30 day) has been 0 percent year to date 2023.
In 2023, other goals of the readmission program have been to analyze dashboard data to understand health disparities. In this regard, there has been an improvement in the precision of the data available in tableau that reports race and ethnicity. Additionally, patients characterized as high risk for readmission for AECOPD are being referred to a Remote Monitoring Program based at MSH that aims to detect early deterioration in the health status of enrolled high-risk COPD patients that can result in early intervention to optimize patient health and potentially prevent an in-hospital admission. As part of the “My Next Steps” initiative, educational material available for patients with COPD after an outpatient visit may help to reduce COPD readmissions by empowering patients to take further responsibility for “self-management,” including a focus on nutrition, exercise, and compliance with prescribed pharmacotherapy.
Pulmonary Embolism Response Team (PERT) Outcomes Data
The Division also sought to improve outcomes for patients with a pulmonary embolism (PE) through use of the Pulmonary Embolism Response Team (PERT). PERT is a multidisciplinary team of pulmonologists, cardiologists, cardiothoracic surgeons, and interventional radiologists who comanage patients with acute massive and submassive PE. The program provides an infrastructure to deliver rapid input from these experts to optimize and streamline treatment.
The PERT at MSBI, as well as Mount Sinai West and Morningside, work collaboratively, and patients who require specific advanced therapies for treatment of Intermediate or high-risk PE may be transferred to MSM or MSH. PERT was activated at MSBI, MSW, and MSM managing 78 patients in 2019, 88 patients in 2020, 47 patients in 2021, 82 patients in 2022, and 74 patients (January 1, 2023, to September 30, 2023). For each PERT activation, there was full and prompt engagement of all members of the PERT. The multidisciplinary team reached a consensus about acute PE management for each patient managed. The mean length of stay for acute PE patients managed by PERT was 7.45 days, and using the European Society of Cardiology (ESC classification) 8.11 percent PE patients were intermediate low risk, 52.7 percent were intermediate high risk, and 37.8 percent were high risk PE patients. Advanced therapies for the PERT managed patients in 2023 included catheter directed thrombolysis (4 percent), systemic thrombolytics (6.7 percent), catheter directed embolectomy (8.1 percent) and an inferior vena cava filter was placed in 6.7 percent patients.
Causes of 30-day mortality in 12.1 percent patients (n=9) included: high-risk PE (n=3), concurrent severe sepsis n=2, concurrent lung mass n=1, advanced COPD n=1 and patients with do not resuscitate directives. Major bleeding occurred in 8.1 percent patients (n=6) causes included lower GI bleed (n=1), uterine bleed secondary to fibroids (n=1), upper GI bleed in a patient with cirrhosis (n=1), bleeding from tracheostomy site (n=1) treated conservatively, and bleeding from a new
central line insertion site (n=1). The readmission rate at 30 days was 13.5 percent (n=10) where two patients were readmitted with new DVT or PE. Fifty-six (75.6 percent) acute PE patients managed by PERT followed up at either a Mount Sinai internal medicine or pulmonary outpatient clinic.
Aims for 2024 include establishing a multidisciplinary VTE clinic at MSM to address possible causes of acute PE management that may increase hospital length of stay for patients admitted with acute PE, improving outcome measures of patients managed by PERT, and continuing our systemwide PERT conferences where we review PERT outcomes data, discuss new literature pertaining to acute PE management, and share ongoing PE related research projects.
Inter-Hospital Transfer Acute PE Patients
Management options for acute PE have evolved in recent years with wider availability of advanced treatment modalities. Most institutions are not equipped or staffed for advanced PE care and patients often require transfer to centers with more comprehensive resources. An organized approach to the process of inter-hospital transfer (IHT) of critically ill PE patients to loco-regional expert PERT centers is still an unmet need. IHT has been previously studied for patients with acute trauma, ST-elevation MI, acute CVA. There is a paucity of data relating to outcomes of patients with acute PE who receive IHT.
The Division performed a retrospective review of consecutive patients diagnosed with acute PE from September 2021-June 2023 who received IHT as recommended by our systemwide PERT. The patients were referred from hospitals in the MSHS and from local nonaffiliated hospitals. Data from a total of 139 patients who received IHT were analyzed, including nine (6.5 percent) from “outof-system hospitals.” Sixty patients who received IHT were excluded due to incomplete data or the IHT occurred for non-PE diagnoses.
Presentation, Risk Stratification and Outcomes
Almost all IHT acute PE patients were classified as intermediate or high risk, and only 0.72 percent of patients transferred were at low risk. The survival rate was 94.2 percent. No patients died during IHT. A minority (33.8 percent) of IHT patients received advanced intervention at the
hospital where they were transferred. Of the 139 patients who received IHT, 66.25 percent received standard-of-care therapeutic anticoagulation, the remainder received advanced therapies that included catheter directed embolectomy 19.4 percent, 7.9 percent received systemic thrombolysis, 3.6 percent surgical embolectomy, and 2.9 percent catheter directed thrombolysis. All patients who received advanced therapies were at intermediate risk or high risk of mortality from an acute pulmonary embolism. The median time from PE presentation to intervention was 22.9 hours, and patients transferred from “out of system hospitals” suffered an increase time for transfer and for eventual intervention for acute PE management. Patients who suffered increased hypoxia during IHT were associated with increased use of advanced therapies at the destination hospital (OR 1.22, p = 0.03).
Association of Race With Outcomes for Patients With Acute PE Requiring IHT.
Race may influence the outcome of patients with acute PE requiring IHT for possible advanced management. A secondary objective of this initiative was to evaluate the associations between race and outcomes in acute PE patients requiring IHT. A retrospective chart review of 139 consecutive patients with acute PE treated in urban teaching hospitals in the Mount Sinai Health System from September 2021 to June 2023 who required IHT were reviewed and the association of race with specific outcomes was analyzed.
The Division found that Black patients received fewer catheter directed interventions (n = 42, p<0.001), suffered an increased in bleeding complications (p=0.028) and were less likely to followup after discharge (p=0.002). However, their rate of in-hospital mortality (p=0.209) or 30-day readmission (p=0.968) was not significantly different from those of other races.

Carbapenem-Resistant Enterobacterales Hospital Acquired Infections
The MSBI ICU team completed an initiative to reduce Carbapenem-Resistant Enterobacterales (CRE) hospital acquired infections by implementing a prevention bundle. Hospital acquired infections (HAI) are detrimental to patient health and also contribute to multiple antibiotic resistant infections. CRE have limited treatment options and are associated with higher mortality rates. During the COVID-19 pandemic, CRE rates doubled in some studies, possibly due to higher rates of broad-spectrum antibiotic use. Many hospitals monitor Standardized Infection Ratio (SIR) to track the number of predicted infections compared to identified infections of HAI. Currently, a SIR does not exist for CRE, making it challenging to assess patient outbreaks and its relationship with antibiotic stewardship.
Using a multidisciplinary approach, the Division worked with Infection preventionists, nurse supervisors, physicians, advanced practice providers, and engineering to implement a prevention bundle. The bundle included weekly surveillance CRE detection rectal swabs with prompt isolation of identified CRE colonizers, and significant plumbing updates. Infection preventionists identified possible CRE reservoirs in ICU room sink drains, faucets, and handheld showers, which were either terminally cleaned or removed. Regular terminal cleaning and installation of splash guards to prevent patient contamination were also implemented.
In 2023, MSBI ICU successfully maintained a record of zero CRE infections. This represented a significant decrease from 2022 when eight ICU patients developed CRE infections. It is important to highlight that this study was conducted post-pandemic, and the improvement in antibiotic stewardship may be a contributing factor. As the roadmap for future pandemics is determined, exploring the implementation of SIR for CRE may help standardize the identification, tracking, and management of CRE colonization and infections.
Surveillence Swabs in 2023
CRE Rates in 2022 vs. 2023
Identification of Healthcare Agent 2023
The Division also aimed to improve the timing of tracheostomies in the ICU. MSHS Institute of Critical Care Medicine (ICCM) set a target to complete 90 percent% of indicated percutaneous tracheostomies before day 12 of mechanical ventilation. The potential advantages of earlier tracheostomy encompass improved patient comfort, reduced sedation requirements, better oral hygiene and pulmonary toileting, decreased ICU length of stay, enhanced speech, nutrition, and mobilization. Within the MSBI ICU, three trained intensivists perform percutaneous tracheostomies at the bedside.
In 2023, three additional physicians at MSBI ICU attended the ICCM Percutaneous Tracheostomy and Difficult Airway Course at MSH to further expand the team’s ability to perform tracheostomies when necessary. To achieve this objective, the ICU team directed efforts toward upstreaming palliative care, engaging in discussions with families earlier in the patient’s mechanical ventilation course. The strategy also involved utilizing Advance Care Planning (ACP) notes and optimizing EMR usage to ensure regular goals of care meetings for all ventilated patients. In 2022, 65 percent of tracheostomies (11 out of 17) were completed before day 12 of mechanical ventilation, and this was successfully improved upon in 2023, meeting the goal of 90 percent (18 out of 20 tracheostomies). Balancing measures, including mortality within 14 days after procedure and during hospitalization, were also monitored.
The previous initiative by the ICU team aimed at raising awareness about bias in pain perception among non-white patients had identified an area of improvement – the need to acknowledge patients’ preferred primary language. Achieving health equity requires a thorough understanding of existing disparities and inequities, and accurate REaL (race, ethnicity, and language) data collection is paramount in this process. To deliver truly equitable care, providers must be aware of and document the patient’s preferred language, and utilize the appropriate interpreter services. The team focused on increasing awareness regarding how to identify a patient’s primary language, aiming to educate ICU staff on the significance of using translator services. Emphasis was placed on the importance of avoiding communication in a secondary (weaker) language, which would fall short of optimal care. This awareness initiative not only addresses the complexities of the busy ICU workflow but also improves communication, and subsequently, patient care.
In collaboration with nursing leadership, strategies were implemented to reassess and re-document the primary language for each patient during their ICU admission. A “Language” column was introduced into each providers’ primary patient list within the EMR to enhance user-friendliness. Additionally, video-translator iPads were placed in each ICU room for patients whose primary language is not English.
Surveys were conducted before and after implementation. The pre-intervention survey revealed that only 14 percent of providers were “always” made aware of the patients’ primary language, which significantly improved to 72 percent post-intervention. Looking forward, the ICU team remains committed to ongoing efforts to enhance the equity of care for our patients.
Tracheostomy Before Day 12
Percent of Patients Assessed for Preferred Language in 2023
% pts assessed for preferred language
(% pts assessed for preferred language)
In response to a survey administered to fellows, the Division examined the ordering process for post-thoracentesis and post-bronchoscopy lab work (including cytology and pathology). The existing order set for post-thoracentesis was reviewed and reinforced to include additional necessary components. Additionally, a post-bronchoscopy order set was developed and is currently in the process of obtaining approval. Both initiatives were pursued to streamline the ordering process, with the overarching goal of enhancing efficiency.
Point-of-care ultrasound (POCUS) is widely accepted as an effective bedside tool in the emergency room and inpatient settings. Evidence on the role of POCUS in the outpatient setting is emerging. A new quality project to describe the current practice of POCUS in the Respiratory Institute was initiated. A survey indicated that 90 percent respondents thought POCUS was useful in the ambulatory setting but only 75 percent had ever performed POCUS in clinic. Time constraints were cited by 100 percent of respondents as a barrier to using POCUS in clinic, other concerns included the lack of patient gowns and availability of ultrasound when needed. Twenty-five exams were performed, with median exam time six minutes to perform a lung exam and 7.5 minutes for a limited echo. The most common clinical indications for which POCUS was performed was dyspnea (80 percent), cough (32 percent), and chest pain (24 percent). POCUS demonstrated strong concordance with chest X-ray and computed tomography (CT). This study demonstrated that lung and cardiac ultrasound were feasible to perform in a short period of time, however time constraints may prevent the appropriate use of POCUS in clinic. Further process improvements to the clinical workflow and education of clinicians on the median time to perform studies will be evaluated.
The Mount Sinai Hospital
Division Quality Champions:
Timothy Harkin, MD
Jing Wang, MD


In 2023, the Division of Pulmonary, Critical Care, and Sleep Medicine continued to work on quality initiatives spanning the outpatient and inpatient arenas.
The Division expanded the Chronic Obstructive Pulmonary Disease (COPD) program, which seeks to identify patients admitted with COPD exacerbation and track utilization of COPD resources with the goal of improving the care of hospitalized COPD patients and reducing COPD readmissions by building and optimizing MSHS COPD Resources:
• COPD dashboard, centralized EPIC patient list, and COPD order set to help identify patients admitted with COPD exacerbation and guide treatment recommendations for admitting providers
• Standardized COPD consult note template for effectively communicating to teams about the severity of disease, the need for adjustment of home medications, the establishment of a follow up plan that includes likely triggers and barriers to care, smoking-cessation recommendations, and discharge planning to ensure a safe transition to outpatient follow-up
• Pulmonary function testing, including inpatient spirometry
• Dedicated respiratory therapist to provide bedside education, review inhaler technique, perform bedside spirometry, and work to ensure close pulmonary follow-up and referral to Pulmonary Rehab
• COPD discharge bundle to optimize care transitions
• Registry of outpatients with COPD
• Focus on racial disparities in care utilization and outcomes
As of October 2023, the COPD readmission rate at MSH was 15.7 percent with an O/E of 0.87, both improved from 2022. There was growth in the utilization of the COPD pathway and respiratory therapy consult services.
The COPD discharge bundle formally started at MSH in the fall of 2023 and will focus on ensuring patients have an appropriate diagnosis at discharge, complete spirometry, and receive education (smoking-cessation counseling, COPD education, inhaler teaching) and have a scheduled pulmonary follow-up appointment. Discharge medication reconciliation along with post-discharge phone follow-up will also be included to facilitate care transition.
To further complement the above, the remote monitoring program (RMP) continued to follow COPD patients in 2023. Technology interventions can enhance self-management of COPD, increase smoking cessation, improve inhaler technique, and aid early recognition of exacerbations. Through this program, the remote monitoring team checks in regularly with patients and reaches out if patients exhibit out-of-range readings in vitals and symptoms. Education is provided to
patients on self-management strategies. There is also support for medication optimization, nutrition, stress management, and breathing techniques.
As of mid-October 2023, there were 12 actively enrolled patients in COPD-RMP. Three patients reached a total enrollment time of one year. Of this group, two patients had a reduced number of hospitalizations (from five in the preceding 12 months to three and two, respectively, since enrollment). The Division hopes to continue expanding utilization of remote patient monitoring in the coming year.
In 2023, the demand for sleep testing in the Mount Sinai Health System and in the community remained high. There remains a high prevalence of patients with obstructive sleep apnea (OSA), respiratory failure/hypoventilation, central sleep apnea (CSA), hypersomnia, insomnia, and neurodegenerative diseases in our patient population. Therefore, the sleep program aimed to continue efforts to improve access to sleep testing.
Since 2019, the Division has utilized the patient data and lab management system Compumedics Nexus360. The software is cloud-based, allowing for remote access and review of study results. The process to review studies and complete reports within seven days is now standardized.
The sleep lab, now spanning two floors at New York Eye and Ear Infirmary with a total capacity of 11 polysomnography studies per night, was successfully reaccredited by the American Academy of Sleep Medicine (AASM) in 2023. In collaboration with the Department of Pediatrics, a new dedicated pediatrics sleep lab was opened in Kravis Children’s Hospital, augmenting specialized full age spectrum sleep testing and care.
Additional sites were also added to the home sleep testing (HST) program across the Health System, further expanding capacity to provide this faster, and more convenient diagnostic tool in clinically appropriate patients. Through education and outreach, the referring network has expanded to include additional Mount Sinai practice sites in primary care, cardiology, ENT, and bariatric surgery. The sleep team worked with referral bases to develop more streamlined pathways for expedited testing and follow-up in patients undergoing surgery and procedures such as arrhythmia ablation. The program continues to use primarily disposable home sleep testing (HST) units and offers a direct ship option to patient homes when needed. A centralized SharePoint site is utilized for communication, aiding in referral tracking and quality assurance.
Each home testing location has a full-time technician to administer HSTs. The chief technician reeducates technicians in response to failed studies, and the team continues to work on improving education and training for patients on the use of home sleep testing devices. With these efforts, home study failure rates have remained consistently low. Furthermore, in continuation of work started as a prior year’s high-value care (HVC) project aiming to increase utilization of home sleep testing in the IMA primary care clinic, the group received a blue ribbon for its abstract at the 2023 Institute of Medical Education research day and presented the project at the DOM research day.
Some challenges to meeting the high demand for sleep testing have included ongoing faculty, technician, and support staff shortage (due to departures and illness) and lingering effects of global supply chain issues that led to delays in patients getting started on therapy. In an effort to counteract and overcome these challenges, the following interventions were continued: streamlining scheduler workflow through Epic referral work queues, optimizing third party vendor workflow to assist with prior authorization, centralizing the scheduling team, expanding scheduling staff and
sleep lab staffing to ensure a seven-day operation, ongoing tech education, ongoing recruitment of sleep clinical faculty, and optimizing centralized tracking of home sleep studies (while dispensing from multiple sites). Three physicians, three advanced practice practitioners, and one clinical nurse were added to the global sleep program over the course of the year.
With the above, the Division saw continued growth in overall sleep study volume and an overall downward trend in sleep study order to completion time Of the 5,000 home sleep studies completed in 2023, a diagnosis of obstructive sleep apnea (OSA) was confirmed in 3,457 (60 percent) cases. A majority of these patients are referred for follow-up with MSHS pulmonary/sleep consultants. Patients with “negative” home testing in whom clinical suspicion of OSA remains high typically go on the complete in-lab sleep testing, as recommended by diagnostic guidelines. In addition, in-lab testing can be utilized for evaluation of other sleep disorders, including complex sleep-related breathing disorders (central sleep apnea, hypoventilation/respiratory failure), parasomnias, hypersomnias, and sleep related movement disorders, which represented approximately 50 percent of testing indications in the lab in the past year.
To better capture patient satisfaction with the sleep testing process, the Division initiated patient surveys via Q-reviews following in-lab and home sleep study appointments. Patient experience with our sleep technicians and staff was consistently positive. Wait time scores aligned with ongoing efforts at access improvement. Any patient concerns were addressed through individual outreach, and the sleep team incorporated issues identified via feedback into regular safety and process improvement efforts.
Patient Satisfaction Q-Review Ratings
Nov 2023
Oct 2023
Sep 2023
Aug 2023
Jul 2023
Jun 2023
How well did the techonologist answer your questions?
How likely is it that you would recommend our facility to a friend or colleague?
How would you rate the registration staff (may have been on the phone)?
The environment was pleasant and comfortable.
Access to care was easy and convenient.
How would you rate the cleanliness at our practice?
How would you rate the technologist (professional performing the procedure)?
How would you rate the courtesy and friendliness of the staff?
How well were your tests and treatments explained to you?
How would you rate the ability to get an appointment when you needed it?
In the coming year, the Division plans to work on further improving wait times for scheduling a sleep study and access to sleep medicine consultation. To do so, the team will continue working on systems optimization, staffing, and standardizing and streamlining workflows and protocols as the sleep program grows. There will be further efforts to improve durable medical equipment (DME) management and facilitate better patient follow-up and treatment compliance monitoring, along with greater integration of sleep patient care via a multidisciplinary approach that now includes pulmonary/sleep, neurology, ear, nose, and throat specialists, and dental specialists in the Health System. Education for sleep lab technicians on complex sleep studies and titrations will also continue.
On the inpatient side, the Medical Intensive Care Unit (MICU) aimed to maintain tidal volume compliance in mechanically ventilated patients. There was consistent maintenance of
ventilator set tidal volume at <= 8 cc/kg (ideal body weight) at >90 percent in the MICU (average 97 percent compliance).
The MICU also embarked on an initiative to improve the accuracy and completeness of ethnic and racial designation in the electronic medical record (EMR). Greater than 16 percent of MICU patients in recent years had “other” and “unknown” race/ethnicity designations in the EMR. The MICU population also has a high proportion of Medicaid and Medicare insurance (27 percent and 49 percent, respectively, based on 2022 data). To improve accurate reporting of race and ethnicity information, MICU social workers will integrate demographic information collection into MICU registry for key demographic data as part of routine admission/evaluation data and nurses/physicians will administer a health literacy assessment using one of several validated health literacy tools. This project will add to the partnership with health system experts to create educational materials for patients and is part of ongoing efforts to improve inclusivity and equity of care for our patients.
Finally, the Division continued efforts to improve outcomes in patients undergoing bronchoscopy, especially in American Society of Anesthesiologists (ASA) physical status classification system (ASA) 3 & 4 level patients.
Bronchoscopy volume continued to grow with 2023 volume at 1,325 procedures total. The proportion of ASA 3 & 4 level patients represented 97 percent of all bronchoscopy cases performed. There was also addition of two ASA 5 & 6 level cases. The number of complications associated with 2023 bronchoscopies was 15 (1.1 percent), a sustained low rate compared with prior years. All cases with complications are reviewed and corrective actions implemented where appropriate.
Mount Sinai Morningside
Mount Sinai West
Division Quality Champions:
Janet Shapiro, MD
David Steiger, MD


The Medical Intensive Care Units at Mount Sinai Morningside and Mount Sinai West worked on several quality projects.
Respiratory Recovery. The Medical Intensive Care Units (MICUs) of MSM and MSW worked together to review the process for liberating patients from mechanical ventilation, as part of the work to reduce excess days. The group started by creating a process map to examine the process of sedation holds and breathing trials within the workflows of physicians, nurses, and respiratory therapists. The teams focused on the use of the respiratory recovery pathway that includes orders for spontaneous awakening and breathing trials. Use of the respiratory recovery pathway order increased by performing daily audits and reinforcing each team’s role and collaboration. The graph below illustrates orders for 2022 and 2023, with significant improvement in 2023. The rates of spontaneous awakening and breathing trials also improved.
Another initiative aimed at reducing excess days involved patients who undergo tracheostomy as they often have an extended MICU stay. Performing tracheostomy earlier in the hospital course may facilitate weaning from sedation and ventilator support, the transition from MICU to a stepdown unit, and discharge to a rehabilitation or nursing facility. Education about the importance of early tracheostomy and the training of several of our attending physicians in the performance of tracheostomy led to improvement in the rate of tracheostomy by ventilator day 12 from 40 percent to 80 percent

Mobility. The MSM MICU worked to improve progression of mobility for MICU patients. Improving mobility progression may improve physical function, reduce delirium, and potentially mitigate aspects of post-ICU syndrome. The MICU staff worked to improve documentation and increase patient mobilization by the following methods: education about documentation, inservices with Physical and Occupational therapists for nurses, and discussing and assigning a mobility goal by physicians during morning team rounds. Mobility progression was documented in 40 percent of patients in 2023, a marked improvement from 2022.

Formation of a Multidisciplinary Pressure Injury Prevention Team to Reduce Hospital
Acquired Pressure Injury (HAPI). The Medical-Surgical Intensive Care Unit (ICU) at MSW performed a quality improvement project focused on HAPI prevention. The multidisciplinary team was composed of a wound care specialist, ICU nurses, ICU physicians, a physical therapist, and a respiratory therapist. The team collaborated to increase awareness of HAPIs with a focus on the importance of screening, skin assessments, and preventive actions. In 2022, a total of 22 HAPIs were reported in the 8AE and 8AW Medical-Surgical ICUs. The team’s goal was to decrease HAPIs by 25 percent in 2023 compared to the previous year. From January to July of 2023, there has been a total of 12 HAPIs in the 8AE and 8AW Medical-Surgical ICUs, a decrease in HAPIs of 45 percent compared to 2022.
Diversity, Equity, and Inclusion (DEI). ICU patients may face discrimination and receive substandard care based on their race, ethnicity, gender, sexual identity, or socioeconomic background. The MICUs of MSW and MSM performed a joint DEI project using the resources of the MSW Center for Advanced Medical Simulation to raise awareness of racism and unconscious bias in the management of a critically ill patient. In 2022, core critical care simulation faculty underwent training on DEI and developed a case-based simulation curriculum. Faculty attended specific
training on debriefing a DEI simulation scenario. A standardized patient and simulation faculty directed the debriefings. The target was to have greater than 70 percent of critical care medicine faculty to be trained in the simulation lab; 90 percent of the MICU faculty at MSM and MSW underwent the simulation scenario. And 83 percent of faculty strongly agreed that the session increased their comfort level in handling a situation involving unconscious bias or structural racism.
Rheumatology
Mount Sinai Beth Israel
Division Quality Champion:
Latoya Freeman-Beman, MD

In 2023, the Division continued its efforts to increase annual tuberculosis (TB) screening rates in patients with Rheumatoid Arthritis (RA) on therapeutic biologics who are seen at MSBI Union Square (USQ)-Rheumatology. Biologic-treated RA patients are at a 31 percent increased risk of serious infections compared to conventional disease-modifying anti-rheumatic drugs (DMARDs), with reactivation TB typically occurring within 6-12 months of starting TNF inhibitors. As such, initial and annual screening for TB is paramount for patients on biologic therapy. The Division’s goal was to improve the rate of screening by 10 percent-20 percent.
MSBI Biologic Screening
January 2023-December 2023
January-23February-23 March-23 April-23 May-23 June-23 July-23 August-23September-23October-23November-23December-23
Previously manually pulled, extraction of available data on TB testing in patients with RA on biologics from the electronic health record is now automated. The baseline rate from the fourth quarter of 2022 was 59 percent. By the last quarter of 2023, the average rate was 57.9 percent Ongoing challenges include the cumbersome process of reviewing alternate data sources (e.g., labs, media, Care Everywhere) in patients without TB screening for confirmation of no other
occurrences and ensuring that on-boarding new faculty adopt use of a trackable EPIC smart phrase. Next steps in 2024 include quarterly faculty reminders for smart phrase usage, individual provider management of TB testing compliance, and reminders at system-level rheumatology faculty meetings.
A new quality initiative for the Division in 2023 involved adequate pain management, as assessed by general pain screening and post-procedure pain follow-up. The aim for general pain screening is to have a pain plan documented in 100 percent of patients with a pain score greater than 7. To improve this metric, the nurse manager will conduct monthly chart audits on patients with pain scores >7 for a pain plan documented by the treating physician. Compliance will be assessed monthly by the nurse manager and division QI lead. The aim for post-procedure pain follow-up is to have 100 percent of patients contacted within 48 hours of an in-office procedure to reassess their pain. To improve this metric, the Division plans to collaborate with nursing staff to ensure that a pain score call back is scheduled within 48 hours of a procedure in addition to use of an EPIC smartphrase. Both facets of the adequate pain management initiative will continue in 2024.
The Division also sought to improve vaccination rates for both influenza and pneumonia among patients with rheumatoid arthritis according to guidelines set by the Centers for Disease Control and Prevention. To improve vaccination rates, the division collaborated with nursing to ensure that all clinic nurses are trained to screen for and offer vaccination to eligible patients. Monthly audits are ongoing and will continue into 2024.
In 2024, the division will also focus on visit throughput as measured by the CGHCAHPS survey questions pertaining to “moving through the visit,” which reflects the degree to which the patient felt informed about delays and the patient’s experience of wait time at the office (time from arriving to leaving). The aim is to score above 90 percent by the end of 2024 from a baseline of 85 percent. To meet this goal, the Division plans to prioritize use of all exam rooms for in-person provider visits. Phlebotomy only visits will take place in infrequently used rooms such as isolation rooms, when available. Office staff will also be reminded to inform patients of any delays upon arrival.
The Mount Sinai Hospital
Quality

The The Mount Sinai Hospital Rheumatology Division sought to increase the rate of tuberculosis (TB) screening for patients on biologics, in accordance with a Centers for Disease Control and Prevention (CDC) recommendation to complete this screening before initiating biologics and annually while using anti-TNF medications. The Division continued two primary interventions to improve performance. The first entailed distribution of provider-specific scorecards quarterly to track performance and promote individual improvement. The second involved efforts to increase utilization of a health maintenance smartphrase that was added to EPIC in late 2020 that made it easier to view and document TB screening status.
Division
Champion: Wendy (Weiwei) Chi, MD
Tuberculosis Screening
These interventions have been successful, however improvement plateaued over the course of 2023. In 2024, the Division aims to continue improving screening rates to reach the goal of 90 percent for patients on biologics. In addition to the above measures, the Division plans to utilize reminders within EPIC to prompt providers to order the appropriate screening tests when needed.
The Division also sought to increase the rate of annual ophthalmologic exams for patients taking hydroxychloroquine (Plaquenil) to 90 percent. This is a critical measure because Plaquenil may cause irreversible retinal damage and early detection is the key to prevention. Unfortunately, the screening rate decreased to 52 percent in 2021. The Division attributes this decrease to challenges related to COVID-19, as patients had been more hesitant to attend routine screenings due to continued effects of the pandemic. In 2023, the Division continued to send individualized feedback to providers to reinvigorate efforts to improve this metric. Patient-directed reminder cards in English and Spanish were created in 2022 and continued to be distributed in the waiting room of the rheumatology clinic. These cards serve as another method for providers to be reminded to refer their patients on hydroxychloroquine for annual ophthalmologic exams and also provides a way for patients to be engaged in their own care.
The Division was able to improve the ophthalmologic screening rates to 65 percent over the course of 2023, and plans to continue its efforts to achieve a goal rate of 90 percent in 2024. In addition to continuing the above measures, new interventions will include adding signage in the exam rooms and having nurses incorporate documentation of last ophthalmology exam in patients on hydroxychloroquine as part of their medication review.
Additionally, in 2023, the Division continued a project to increase rates of pneumococcal vaccination for patients on biologics. Baseline rates of pneumococcal vaccination in 2021 were low, with only 23 percent of patients on biologic medications receiving any pneumococcal vaccine. The Division implemented a multidisciplinary intervention that involved providers generating lists of patients scheduled to be seen each week who have not yet received the vaccine and registered nurses reminding providers, both in person and through EPIC, about the vaccine for eligible patients at the time of the appointment.
Since these interventions were implemented in 2022, rates of pneumococcal vaccination have increased to 37 percent. The Division will continue these efforts in 2024 with the goal of increasing the rates to at least 50 percent by the end of the year.
Mount Sinai Morningside
Division Quality Champion:
Kristaq Koci, MD

The Division of Rheumatology’s main quality project focused on improving Shingrix vaccination in patients on Janus Kinase (JAK) inhibitors. Since 2017, Centers for Disease Control and Prevention guidelines have recommended vaccination against the virus that causes shingles (varicella zoster virus) for everyone 50 years or older, and for those 19 years or older if immunocompromised. JAK inhibitors, a class of immune modulating medications frequently prescribed in rheumatology practice, are associated with an increased risk of shingles compared to other antirheumatic drugs. Therefore, vaccination is especially important to reduce this risk.
Currently, the Shingrix vaccine is not available for direct administration at Mount Sinai Morningside and West rheumatology clinics, requiring patients to follow up with their primary care office or obtain it from their pharmacy. This presents an additional barrier to implementing and tracking shingles vaccination compliance when compared to the immunizations for influenza and pneumonia, both of which are offered on site for rheumatology patients. In addition, patients who obtain the vaccine from their pharmacy or from providers outside the Mount Sinai Health System may not have it reflected in their electronic medical record. To improve vaccination rates, providers were reminded about the recommendation and informational posters were printed and posted in clinics. This intervention in addition to the faculty’s diligence has led to a marked improvement in Shingrix vaccination rates for our immunosuppressed patients on JAK inhibitors as seen in Figure 1. From Figure 2 we see a discrepancy in vaccination rates particularly affecting the African-American population. Further areas of improvement will focus on improving the vaccination rate in this group of patients.
Dr. Koci and the Division of Rheumatology at MSMW would like to recognize and thank Internal Medicine resident Jin Feng, MD, for her contributions to this year’s quality improvement project pertaining to Shingrix vaccination.
Shingrix Vaccination Rate in Patients on JAK Inhibitors Stratified by Age
As seen in the figure above the overall vaccination rate improved from 22.2 percent to 39.19 percent, reaching our goal of more than 10 percent improvement.
Shingrix Vaccination Rate in Patients on JAK Inhibitors Stratified by Age
Quality Improvement Projects in Progress
Patients with connective tissue disease are frequently prescribed immunosuppressant medications that increase their baseline risk for developing infections. It is important that patients understand this risk so they can seek timely medical attention and temporarily stop taking the relevant medications, when appropriate. This education will have the anticipated effect of improving patient autonomy and morbidity overall.
The aim of this project is to improve patient understanding of immunosuppressant medications and infection risk in an outpatient rheumatology setting. The goal is to improve understanding of infection risk among rheumatology patients prescribed immunosuppressant medications by 15 percent
The clinic medical assistants handed an anonymous questionnaire to each patient and the patients returned the completed questionnaires in a box. The results of the survey showed that out of the patients who are on immunosuppressants, 57 percent know the medication lowers their immune system. Some 57 percent also endorsed knowing all the risks; however, the remaining patients surveyed did not feel sure about knowing the side effects. And 64 percent reported having received written information about the medication. Of those who had received written information, 72 percent correctly answered to stop the medication and notify the provider in case of infection. Of those who had not received written information, 60 percent elected to stop the medication in case of infection.
From the survey data, we concluded that written information should be offered to the patients as a higher percentage of patients who had received written information knew to stop the medication should there be an infection. In 2024, the Division will continue to encourage the providers in the clinic to provide written information to patients and continue to explicitly clarify what to do in case of infection.
Publications, Presentations, and Grants
MSBI Abstracts and Presentations
Hospital Medicine
Quentzel J, Alexandre P, Daoud S, Dharapak P. Improving the Perception of Workplace Safety with Proactive Rounding. Society of Hospital Medicine, April 2024. San Diego, CA. (poster)
Fruchter D, Christophe K, Felder B, Goldberg J, Rizk D, Dharapak P. Back to Basics: Rapid Response Training for the Academic Hospitalist Society of Hospital Medicine, April 2024. San Diego, CA. (poster)
Dharapak P, Dupont ME, Dempsey B, Yu I, Raucher B. Preferred Language and Inpatient Mortality: Every Voice Counts Society of Hospital Medicine, April 2024. San Diego, CA. (poster)
General Medicine
Chow D, Dharapak P, Loughney W, Cuervo CM, Cruz C. Improving Transitions of Care from Hospital to Primary Care. Mid-Atlantic Regional Society of General Internal Medicine, September 2023. New York, NY. (poster)
Garpestad C, Batista E, Weissman MA, Truglio J Taking off the Pressure: Improving Hypertension Management at East Harlem Federally Qualified Health Center. Society of General Internal Medicine Regional Conference, September 2023. New York, NY (oral)
Pathak N, Price C, Cruz CM, Weissman MA. Using DISC Personality Tests to Develop Leadership Skills in Internal Medicine Residents. Society of General Internal Medicine Regional Conference, September 2023. New York, NY (poster)
Nephrology
Ishisaka Y, Wang HY, Mitaka H, Charen E, Harbord N, Patrawalla P. Effectiveness of Training in Renal Pocus for Acute Kidney Injury: A Novel Curriculum for Internal Medicine Residents. American Journal of Respiratory and Critical Care Medicine 2023; 207:A3156. (poster)
Pulmonary
Bahk J, Dolan B, Sharma V, Sehmbhi M, Fung JY, Lee YI. Characteristics of Tracheostomized Patients: COVID-19 Vs Non-COVID-19. InB44. Frailty, Nutrition, and Prolonged Mechanical Ventilation. American Thoracic Society Annual International Conference, May 2023, Washington D.C. (poster)
Bahk J, Sharma V, Dolan B, Sehmbhi M, Fung JY, Lee YI. Clinical Outcomes of Tracheostomized Patients: COVID-19 Vs Non-COVID-19. InB44. Frailty, Nutrition, and Prolonged Mechanical Ventilation. (pp. A3400-A3400). American Thoracic Society Annual International Conference, May 2023, Washington DC. (poster)
Ishisaka Y, Mitaka H, Charen E, Harbord N, Patrawalla P. 1094: Utility Of Renal Ultrasound In Guiding Management Of Acute Kidney Injury. Critical Care Medicine 2023 1;51(1):543, Critical Care Congress, January 2023. San Francisco, CA. (poster)
Ishisaka Y, Salguero BD, Miyakawa L, Rothman A. Assessing Bias in Treatment of Empyema. American Thoracic Society Annual International Conference, May 2023, Washington DC. (poster)
Ishisaka Y, Watanabe A, So M, Steiger D, Aoi S, Kuno T. 869: Mortality And Bleeding Risks Of Interventions For High- And Intermediate-Risk Pulmonary Embolism. Critical Care Medicine 2023 51(1):427, Critical Care Congress, January 2023. San Francisco, CA. (poster)
Lim S, Miyakawa L, Filopei J, Dharapak P. Increasing Health Care Proxy Documentation in an Intensive Care Unit – A Quality Improvement Initiative. American College of Chest Physicians Annual Conference, October 2023, Honolulu, HI. (poster)
Salguero B, Lo Cascio CM, So M, Steiger D, Chaddha U. Cost Difference Analysis of Medical vs Surgical Thoracoscopy in a Single Center in the United States. American Association for Bronchology & Interventional Pulmonology. August 2023, Chicago, IL. (poster)
Sharma V, Bahk J, Dolan B, Sehmbhi M, Fung JY, Lee YI. Complications of Tracheostomies in the COVID-19 Era. InB44. Frailty, Nutrition, and Prolonged Mechanical Ventilation. 2023 May (pp. A3403-A3403). American Thoracic Society Annual International Conference, May 2023, Washington DC. (poster)
Sridhar P, Radhakrishnan DN, Patrawalla P, Kim B. Clinician experiences, feasibility, and outcomes of point-of-care ultrasound in a pulmonary clinic. American College of Chest Physicians Annual Conference, October 2023, Honolulu, HI. (poster)
Sridhar P, Singh A, Wang HY, Ehrlich M, Acquah SO, Steiger D. Analysis of Outcomes of Acute Pulmonary Embolism Patients Receiving Inter-hospital Transfer Managed by the Pulmonary Embolism Response Team. 2023 May (pp. A2009-A2009). American Thoracic Society Annual International Conference, May 2023, Washington DC. (poster)
Publications
General Medicine
Verma H, Hasegawa D, Tepper DL, Burger AP, Weissman MA. Patient Satisfaction with Telehealth at an Academic Medical Center Primary Care Clinic. Telemed J E Health. 2024 Jan;30(1):103-107. doi: 10.1089/tmj.2023.0158. Epub 2023 Jun 15. PMID: 37327015.
Kee, D; Verma, H; Tepper, DL, Hasegawa, D; Burger, AP, Weissman, MA. Patient Satisfaction with Telemedicine among Vulnerable Populations in an Urban Ambulatory Setting. Mayo Clinic Proceedings: Digital Health, March 2024, Volume 2, Issue1, 2024, Pages 8-17, ISSN 2949-7612, https://doi.org/10.1016/j.mcpdig.2023.11.004. Originally published online 2023 December. https://www.sciencedirect.com/science/article/pii/S2949761223000949
Li T M, Tepper D L, Burger A, Weissman MA. Internal Medicine Recruitment in the Social Media Age: Strategies to Target Residency Applicants Mayo Clinic Proceedings: Digital Health. Volume 1, Issue 2, June 2023, Pages 55-59 https://doi.org/10.1016/j.mcpdig.2023.02.001
Pulmonary
Alexander M, Ishisaka Y, Miyakawa L, Rothman A. Assessing Physician-Based Biases on the Decision to Place Indwelling Pleural Catheters. J Bronchology Interv Pulmonol. 2023 Apr 27.
Bahk J, Rehman A, Ho K, Narasimhan B, Ain Baloch N, Zhang J, Yip R, Lookstein R, Steiger D. Predictors of Pulmonary Embolism in hospitalized patients with COVID-19. Thrombosis Journal 2023, 21:72
Olazagasti C, Seetharamu N, Kohn N, Steiger D. Implementing physician education to increase lung cancer screening uptake. Lung Cancer Management. 2023 Feb;11(2):LMT55.
Singh A, Rana Y, Monfasani A, Filopei J, Zatakia J, Blackwell L, Steiger D. Late presentation of acute Pulmonary Embolism following outpatient treated COVID-19. 2023 International Journal of Clinical Studies and Case Reports. DOI: 10.46998/IJCMCR.2023.32.000796
Invited Lectures and Recognition
Presentations
“Colorectal Cancer Screening Updates” CHCANYS statewide clinical quality meeting, Virtual, 3/14/23
“Plenary Panel Discussion: Charting the Course for Sustainable and Equitable Telehealth Solutions: Key Perspectives for Today and Tomorrow” with Jasmine Bishop, Kevin Curtis, Danielle Louder; Northeast Regional Telehealth Conference, 9/19/23
Panelist, High School for Math, Science, and Engineering, Fireside Chat Series #1: “Math and Society” New York, NY (virtual), 10/25/23
Media
“What you Need to Know about Biologics” Facebook Live Series Episode #11 host with guest Dr. Songhui Ma, January 18, 2023 https://www.facebook.com/MountSinaiNYC/videos/the-use-ofbiologics-in-allergic-diseases/627204732498059/
“What you Need to Know about the Thyroid” Facebook Live Series Episode #12 host with guest Dr. Michael Via, February 28. 2023 https://www.facebook.com/MountSinaiNYC/videos/what-to-knowabout-thyroid-disease/557171359527603/
“What you Need to Know about Lung Cancer Screening” Facebook Live Series Episode #13 host with guest Dr. Lina Miyakawa, April 6, 2023 https://www.youtube.com/watch?v=hKTWnQeTscY
Quoted in “What medical dramas get right and wrong about hospital work” Becker’s Hospital Review April 14, 2023 https://www.beckershospitalreview.com/digital-marketing/what-medicaldramas-get-right-and-wrong-about-hospital-work.html
Quoted in “Food poisoning recently? Sick restaurant workers might be to blame, says CDC” by Shiv Sudhakar Fox News online, June 3, 2023. https://www.foxnews.com/lifestyle/food-poisoningrecently-sick-restaurant-workers-might-blame-cdc
Interviewed for “Men’s Health in the 20s, 30s, 40s, 50s and beyond” PIX11 News, June 14, 2023. https://pix11.com/video/health-tips-for-men-in-their-20s-30s-40s-and-50s-and-beyond/8733497/
“What you Need to Know about Hepatitis B and C” Facebook Live Series Episode #14 host with guest Dr. Vani George, July 14, 2023
https://www.facebook.com/mountsinainyc/videos/819686099669631/?refsrc=deprecated&_rdr
Quoted in “Air Travel Ailments: A Guide” By Gina Van Thomme, Paper Gown column, August 1, 2023, https://www.zocdoc.com/blog/air-travel-ailments-a-guide/
Quoted in “How to manage stomach flu symptoms at home” by Cheryl Solimini, CVS Online, October, 25, 2023, https://www.cvs.com/learn/health/cough-cold-flu/stomach-flu-symptoms
“Tips on Sleep” Facebook Live Series Episode #15 host with guest Dr. Boris Gilyadov, November 14, 2023 https://www.youtube.com/watch?v=bTJQG9B0xBQ
MSH Abstracts and Presentations
Division of General Internal Medicine
Cytyrn E, Stauber Z, Jaeckel K, Barai N, Fishman MB, Jandorf L, Itzkowitz SH, Koster KM. Improving colorectal cancer screening rates with multitarget stool DNA testing by implementing a comprehensive program of tailored patient navigation in an inner-city population. The American Journal of Gastroenterology. 118(10S): S240, October 2023.
Poster session presented at: “American College of Gastroenterology Annual Scientific Meeting”; October 2023; Vancouver, Canada.
Stacy Tsai, MD, Nikita Barai, MD, Kyle Koster, MD, Mary B. Fishman, MD, Kelsey B. Bryant, MD, MPH, MS, "Blood Pressure Control Fluctuation and Quality Standards" Abstracts from the 2023 Annual Meeting of the Society of General Internal Medicine. J GEN INTERN MED 38 (Suppl 2), 81–799 (2023). https://doi.org/10.1007/s11606-023-08226-z
Endocrinology
O’Malley G, Ogyaadu S, Levister C, Rioles N, Hardison H, Roberts A, Accacha S, GuttmanBauman I, Vendrame F, Basina M, Fallurin R, Levy C. “Reproductive health counseling in the T1D Exchange Quality Improvement Collaborative (T1DX-QI).” American Diabetes Association 83rd Scientific Sessions. Poster 1052-P, June 2023. San Diego Convention Center, San Diego, CA.
Wang AW, O’Malley, G, Levister C, Arasaratnam D, Rouviere M, Shah N, Lam D, Levy CJ. “Preconception counseling and Reproductive Education Program for People with Diabetes (PREPP’D) – An educational program for underserved women with diabetes ” ENDO 2022, June 2022. Atlanta, GA.
Hospital Medicine
Truong T, Schmer S, Dunn A. Assessing an Artificial Intelligence-Assisted Discharge Prediction Tool. Society of Hospital Medicine National Meeting, April 2024, San Diego, CA. (poster)
Knees M, Yu A, Keniston A, Peterson R, Schwatka N, Sakumoto M, Kochar A, Westergaard S, Burden M. Beyond Beepers: Navigating the Digital Shift in Hospital Communication. Society of Hospital Medicine National Meeting, April 2024, San Diego, CA. (poster)
Radja G, Dunn A, Varga A, Vincent R. Impact of Dynamic Lighting on Hospitalized Patients. Society of Hospital Medicine National Meeting, April 2024, San Diego, CA. (poster)
Hack B, Epstein J, Nguyen VT. Med Rec Mondays: Improving Medication Reconciliation Among Internal Medicine Residents. Society of Hospital Medicine National Meeting, April 2024, San Diego, CA. (poster)
Dharapak P, Chokshi K, Nguyen VT, Sawant A, Raucher B, Dunn A, Linker A. Utilizing Voice Recognition to Improve Practice Efficiency and Reduce Burnout. Society of Hospital Medicine National Meeting, April 2024, San Diego, CA. (poster)
Nguyen VT, Gabriel E, Reyna M, Gronowitz M. Phone-A-Friend: A Clinical Mentorship Model to Discuss Complex Cases. Society of Hospital Medicine National Meeting, April 2024, San Diego, CA. (poster)
Baek M, Nguyen VT, Dunn A. Fill in the Procedural Gap: An On-call Hospitalist Procedure Team. Society of Hospital Medicine National Meeting, April 2024, San Diego, CA. (poster)
Aoun R, Liu D, Zhang E, Soong B, Park S, Nguyen VT. Limiting Waste: Reducing Urine Culture Testing in Inpatients. Society of Hospital Medicine National Meeting, April 2024, San Diego, CA. (poster)
Plick N, Gabriel E, Nguyen VT. Indications and Outcomes of Interhospital Transfers to an Academic Center. Society of Hospital Medicine National Meeting, April 2024, San Diego, CA. (poster)
Nguyen VT, Perez L, Dunn A. Heavy Stuff: Discharge Density vs Length-of-Stay to Assess Performance. Society of Hospital Medicine National Meeting, April 2024, San Diego, CA. (poster)
Nissel A, Yu P, Dunn AS, McGreevy J, Reyna MA. More Patients than Beds: Maintaining Quality While Moving Patients. Society of Hospital Medicine National Meeting, April 2024, San Diego, CA. (poster)
Crecelius T, Linker AS, Gottenborg E, Kwan B, Keniston A, McBeth L, Martin SK. ‘Hitting Pause on Your Professional Development Is Not Neutral’ - Fellowship Program Directors' Perspectives on Hospitalist Gap Years." Alliance for Academic Internal Medicine Annual Conference, April, 2023. Austin, TX (poster winner, Award of Excellence for Research Poster)
Golec S, Epstein J, Linker AS, Nguyen VT. Click for Cookies: Improving Trainee EHR Use in Medication Reconciliation. Society of Hospital Medicine National Meeting, April 2023, Austin, TX. (poster winner of Conference Grant Award for resident travel to conference)
Gronowitz M, Das R, Linker AS, Truong T, Fiscaletti O. Get Moving! Assessing Internal Medicine
Physician Attitudes about Patient Mobility. Society of Hospital Medicine National Meeting, April 2023, Austin, TX. (poster winner of Conference Grant Award for resident travel to conference)
Kamat S, Gontzes A, Liu C, Dashevsky J, Floodstrand M, Linker AS. Click it before you stick it: A Student-Led Improvement Project. Society of Hospital Medicine National Meeting, April 2023, Austin, TX. (poster)
Crecelius T, Gottenborg E, Linker AS, Kwan B, Martin S. Fellowship Program Directors’ Perspectives on Hospitalist Gap Years. Society of Hospital Medicine National Meeting, April 2023, Austin, TX. (poster)
Kara A, Kangelaris K, Astik G, Keniston A, Schwatka N, Kulkarni S, Sakumoto M, Linker AS, Bowling GD, Radhakrishnan NS, Mathews B, Auerbach A, Burden M. Parental Leave in Hospital
Medicine: We Can Do Better. Society of Hospital Medicine National Meeting, April 2023, Austin, TX. (poster)
Narayanan M, Kara A, Mathews B, Astik G, Fletcher M, Burden M, Dhawan A, Linker AS, Jenkins A, Eniasivam A, Woodruff A, Sterken D, Readlynn J, Radhakrishnan N, Lee T. But what does inclusion look like? Insights from hospitalists. Society of Hospital Medicine National Meeting, April 2023, Austin, TX. (poster)
Igwe N, Ha JE, Linker AS, Raucher B, Dunn A, Nguyen VT. Assessing Vulnerabilities in Transitions for COVID-19 Patients Discharged on Oxygen. Society of Hospital Medicine National Meeting, April 2023, Austin, TX. (poster)
Kangelaris K, Astik G, Keniston A, Sakumoto M, Linker AS, Kulkarni S, Bowling G, Leykum L, Auerbach A, Schnipper J, Burden M. Necessary Evil: Multi-Institutional Rapid Qualitative Analysis of Jeopardy Systems. Society of Hospital Medicine National Meeting, April 2023, Austin, TX. (poster)
Limaye N, Matias W, Rozansky H, Neville B, Vise A, Gershanik E. Understanding Whether Patient Language Translates Into Disparities For Sepsis Outcomes. Society of Hospital Medicine National Meeting, April 2023, Austin, TX. (poster)
Kwon DY, Wang A, Park J, et al. Don’t Hesitate, Moms Vaccinate: Exploring Varicella and MMR Vaccination Rates in Postpartum Mothers. Poster presented at: 2023 Association of Clinicians for the Underserved Annual Conference. July 23-26, 2023; Washington, DC.
Kwon DY, Letchuman S, Aoun R, Linker AS. Improving Health Equity Through Student-Driven High-Value Care Initiatives. Poster presented at: 2023 Association of Clinicians for the Underserved Annual Conference. July 23-26, 2023; Washington, DC.
Letchuman S, Zhou A, Gyasi A, Yang A, Gallate Z, Delicce A, Aoun R, Linker AS, Fuller R. Improving Antibiotic Stewardship: Optimizing Procalcitonin Utilization in Patients Admitted with Respiratory Tract Infections. Poster presented at 2023 The Mount Sinai Hospital Department of Medicine Research Day. May 16, 2023; New York, NY.
Liver Medicine
Mageras A, Woods E, Collado F, Bhuiyan T, Romano C, Wyatt B, Roediger R, Dieterich DT, Results of a Universal Hepatitis B Screening and Linkage to Care Program in a Large, Urban Health System. AASLD The Liver Meeting, November 2023. Boston, MA. (poster)
Mageras A, Woods E, Wyatt B, Roediger R, Collado F, Bhuiyan T, Romano C, Dieterich DT, Improving Hepatitis B Screening and Linkage to Care Rates via the Electronic Medical Record, Provider Engagement, and Patient Navigation in a Large, Urban Health System. EASL International Liver Congress, June 2023. Vienna, Austria. https://www.natap.org/2023/EASL/EASL_148.htm. (poster)
Roediger R, Mageras A Universal Screening & Vaccination for Viral Hepatitis Elimination. Empire Liver Foundation, May 2023. https://empireliverfoundation.org/webinar-archive/. (webinar)
Peer-Reviewed Publications
Endocrinology
Fallurin, Reshmitha, Madeleine Rouviere, Grenye O’Malley, Susel Rodriguez Ortega, Ally Wang, Selassie J Ogyaadu, Camilla Levister, David W Lam, Nirali Shah, and Carol J. Levy. "143-LB: Preconception Counseling and Reproductive Education Program for Persons with Diabetes (PREPPD)." Diabetes 72, No. Supplement_1 (2023).
Hospital Medicine
Schwatka, NV, Keniston, A, Astik, G, Linker, A, Sakumoto, M, Bowling, G, Auerbach, A, Burden, M. Hospitalist Shared Leadership for Safety, Health, and Well-being at Work, United States, 20222023. American Journal of Public Health 114, 162_166. Accepted January 3, 2024, published online February 14, 2024.
Liu H, McCroskery S, Rajasekaran V, Linker AS, Poeran J, Truong TT. Racial Disparities in Documented Chief Complaints and Diagnoses in Sepsis Patients. J Intensive Care Med. 2023 Jul;38(7):630-634. doi: 10.1177/08850666231155397. Epub 2023 Feb 5. PMID: 36740933.
Shyu M, Golec S, Anderson J, Linker AS, Nguyen VT, Raucher B, Dunn A. Analyzing Monday discharges to identify lost opportunities for weekend discharge. Intern Med J. 2023 Apr;53(4):625628. doi: 10.1111/imj.16062. PMID: 37186364.
Busch JI, Keniston A, Astik GJ, Auerbach A, Kangelaris KN, Kulkarni SA, Leykum LK, Linker AS, Nieto K, Pierce RG, Sakumoto M, Burden M. Exploring the Impact of COVID-19 on Women Hospitalists: A Mixed-Gender Qualitative Analysis. J Gen Intern Med. 2023 Nov;38(14):3180-3187. doi: 10.1007/s11606-023-08371-5. Epub 2023 Aug 31. PMID: 37653202; PMCID: PMC10651559.
Banashefski B, Henson P, David N, Kok HT, Beerkens FJ, Shyu M, Linker AS, Tsega S, Dunn, AS, Fuller R. An interdisciplinary student-led multifaceted intervention addressing overuse of broadspectrum antibiotics for patients with low-risk penicillin allergies. Antimicrobial Resistance & Infection Control. 2023;12:34-40.
Yeshoua B, Bowman-Zamora C, Dullea J, Ditkowsky J, Shyu M, Zhao W, Shin JY, Linker AS, Tsega T, Dunn A, Shah M. Interventions to reduce repetitive ordering of low-value inpatient laboratory tests: a systematic review. BMJ Open Quality 2023;12:e002128. doi: 10.1136/bmjoq2022-002128
Linker, A.S. and Jones, C. Creating a path forward: Reimagining pathways to improve gender equity in authorship. J. Hosp. Med. 2023; 18: 283-284. https://doi.org/10.1002/jhm.13069
Kulkarni SA, Keniston A, Linker AS, et al. Building a thriving academic hospitalist workforce: A rapid qualitative analysis identifying key areas of focus in the field. J Hosp Med. 2023; 18: 329-336. doi:10.1002/jhm.13074
Linker, A.S., Jones, C.D. and Ruhnke, G.W. (2023), Can we build the plane while flying? Creative approaches to expand the research community in hospital medicine. J. Hosp. Med. 2023;18: 560561. https://doi.org/10.1002/jhm.13115
Cho HJ, Tsega S, Krouss M, Goetz C, Dunn AS, Di Capua J, Lee I, Linker AS, Makhni S, Korenstein D. Student High Value Care Initiative: a Longitudinal Model for Student-Led Implementation and Scholarship. J Gen Intern Med. 2023 Feb 24. doi: 10.1007/s11606-023-08100-y. Epub ahead of print. PMID: 36829048.
Haller MD, Cho HJ, Ahn J, Krouss M, Alaiev D, Yoon GH, Dunn AS, Fagan I. Initiative to reduce inappropriate venous thromboembolism prophylaxis in an 11-hospital safety net system: An electronic health records-based approach. J Hosp Med. 2023;18:502-508.
Dunn AS. Commentary on Caso, et al. in Heart. In AF, underdosing of DOACs was not linked to reduced bleeding. Ann Int Med. 2023;176:JC32.
Asgary R. Cancer care and treatment during homelessness. Accepted in Lancet Oncology, Volume 25, Issue 2, 2024. Pages e84-e90. https://doi.org/10.1016/S1470-2045(23)00567-3.
Molta M, Bowler ME, Asgary R. Epidemiology, Risk factors, and Strategies to Prevent and Manage Poisoning Due to Pharmaceuticals in Children in LMIC Countries; A Systematic Review. Accepted in Journal of Global Health, July 2023.
Bauder L, Giangobbe K, Asgary R. Barriers to effective health communication during epidemics and pandemics; a systematic review. Disaster Med Public Health Prep.2023 May19;17e395.
Asgary R, Beideck E, Naderi R, Schoenthaler A. SMS Texting for Uncontrolled Diabetes among Persons Experiencing Homelessness: Study Protocol, Contemporary Clini Trials. 2023 Mar 12;128:107149
Asgary R, Bauder L, Naderi R, Ogedegbe G. SMS text intervention for uncontrolled hypertension among hypertensive homeless adults in shelter clinics of New York City: protocol for a pragmatic randomized study. BMJ Open. 2023 Oct30;13(10):e073041
Rose McKeon Olson, Cody P. Nolan, Neha Limaye, Miriam Osei, Daniel Palazuelos; National Prevalence of Diabetes and Barriers to Care Among U.S. Farmworkers and Association With Migrant Worker Status. Diabetes Care 1 December 2023; 46 (12): 2188–2192. https://doi.org/10.2337/dc23-0960
Nephrology
Tokita J, Sinfield C, Donovan MJ, McNicholas T, Kattan M, Lam DW. 12-LB: Clinical Impact of Risk Profiling with KidneyIntelX on DKD Progression in a Large Integrated Health Care System. https://diabetesjournals.org/diabetes/article/72/Supplement_1/12-LB/150261/12-LB-Clinical-Impactof-Risk-Profiling-with
Conference Presentations
Hospital Medicine
Whinney C, Dunn AS, Mueller S, Dekhtyar J. Navigating Interhospital Transfers: Communicate and Triage for Success. Workshop, SHM Converge National Meeting 2023.
Linker AS, Astik G, Kulkarni S, Kangelaris K. Don’t be a Lone Ranger: Creative Ways to Expand Academic Opportunities Through Multi-Center Networks. Didactic Workshop, Early Career Hospitalist Track. SHM Converge National Meeting 2023.
Chokshi, K. Clinical ethics as an important space for reflective engagement with racism in medicine: Evaluating the role of patient race and primary language in clinical ethics consultation. American Society of Bioethics and Humanities, National Meeting, Baltimore, Maryland, October 2023.
Chokshi, K. Innovation in Collaborative Clinical Ethics Consultation: Panelist American Society of Bioethics and Humanities, National Meeting Baltimore, Maryland, October 2023
Chokshi, K. Group model ethics consultation as an adjunct to Advance Care Planning, American Society Bioethics and Humanities, National Meeting, Baltimore, Maryland, October 2023
Krouss M, Linker AS. Add Value: How to Lead Initiatives to Stop Doing Things We Do For No Reason – Workshop. 18th Annual Mid-Atlantic Hospital Medicine Symposium. New York, NY October 20-21, 2023.
Book Chapters
Asgary R, Williams A. Chapter (16), Pain and Torture: War’s Civilian survivors and refugees. Pain in Vulnerable Populations; edited by Paul Christo, Rollin Gallagher, Joanna Ktzman, and Kayode William. Oxford University Press, scheduled for Nov 2023
National & International Invited Speaker
Asgary R, Health Strategies to Improve Providers’ Competency and Quality of Cervical cancer Screening in Low-Resource Settings. Invited Lecturer, Webinar; Access to Care Seminar Series, American University of Armenia, Yerevan, Armenia, December 2023
Asgary R. Moral and psychological distress in humanitarian settings. Invited Lecturer, Delta Omega Webinar series. George Washington University, Washington D.C., April 2023
Dunn AS. Course Director, Mid-Atlantic Hospital Medicine Symposium. Oct 2023.
Nguyen VT. Course Co-Director, POCUS Course at MSW.
Regional Meetings
The Division of Hospital Medicine at Mount Sinai Health System, in affiliation with SHM and collaboration with ACP, hosted the 17th Annual Mid-Atlantic Hospital Medicine Symposium, “Mastering the Care of the Hospitalized Patient” on October 21-22, 2022.
Featured speakers from MSH DHM included: Andrew Dunn, Erin Gabriel, Dilan Jogendra, VinhTung Nguyen, Krishna Chokshi, and Michael Herscher.
MSH DHM Faculty also collaborated with other MSHS faculty in presenting a Mount Sinai Health System Point of Care Ultrasound for the Hospitalist Course. MSH DHM faculty included Vinh-Tung Nguyen, Teddy Holzer, and Michael Herscher.
Grants
$334,000 grant and $60,000 extension, McClung Foundation - Study impact of novel lighting system on sleep for hospitalized patients; PI – Andrew Dunn
$43,500, MSHS Office for Well-being and Resilience - Using voice recognition technology to improve wellness. PI: Anne Linker, Krishna Chokshi, Vinh-Tung Nguyen, Patricia Dharapak, Ashwin Sawant, Andrew Dunn, Beth Raucher.
Partner site in Achieving Diagnostic Excellence through Prevention and Teamwork (ADEPT) multicenter grant, funded through AHRQ. (Anne Linker and Aveena Kochar, site PI. Team members: Vinh-tung Nguyen, Tao Xu, Jeffrey Epstein, Samuel Hundert, Andrew Dunn.)
MSMW Abstracts and Presentations
Gastroenterology
Seltzer, ES, Park E, Arosemena PM, Varela, I, Neelam, A, Smith, M, Simoes, P. S1703 Reflections of a Newly Implemented Percutaneous Endoscopic Gastrostomy Tube Workflow. Official journal of the American College of Gastroenterology| ACG 118.10S (2023): S1271-S1272. (poster)
Hospital Medicine
Reiff-Pasarew FE, Keller K, Veldboom EJ, Pearson JM, Waite H. Care Team Round: Development of Interdisciplinary Working Rounds. Society of Hospital Medicine, April 2024. San Diego, CA. (poster)
Reiff-Pasarew FE, O’Sullivan M, Jurta J, Antretter JR. Inpatient Varenicline for Smoking Cessation in COPD Patients. Society of Hospital Medicine, April 2024. San Diego, CA. (poster)
Reiff-Pasarew FE, Hernandez K, Sadud S, Chernyk A, Shenoy S, Sing V, Parikh F, Anaraki NSA, Chen PL, Pearson JM, Dempsey B. Society for Hospital Medicine, April 2024. San Diego, CA. (poster)
