Dubin Breast Center
The Mount Sinai Hospital
1176 Fifth Avenue
First Floor
New York, NY 10029
We would like to welcome you to the Dubin Breast Center at Mount Sinai.
This extraordinary facility provides a seamless, supportive and multidisciplinary approach to breast cancer care. Your care will be provided by a group of outstanding physicians and health care practitioners providing comprehensive care in prevention, genetics, diagnosis, treatment and survivorship. In addition, there are nutritional and psychological services, social workers as well integrative medicine such as acupuncture, massage and yoga. Finally, there are clinical trials that seek to evaluate new treatments or approaches so that we can continually make improvements on today’s best treatments.
We have developed a Cancer Risk Evaluation (CaRE) Program, for women who have never had breast cancer but are at increased risk for developing breast cancer due to their family history or other factors. The CaRE program provides guidance and surveillance with the goal of early detection of breast cancer, and counseling regarding options for prevention and risk reduction.
As part of our Survivorship Program, there are primary care physicians with special expertise in breast cancer embedded right in our practices. These physicians may assist in your survivorship care.
Mount Sinai and the Dubin Breast Center strive to deliver outstanding, compassionate and personalized care. We hope you will agree that your experience supports your treatment, recovery and your path to optimal health and wellness.
Elisa R. Port, MD, FACS Director, Dubin Breast Center Chief, Breast Surgery, Mount Sinai Health System Professor, Surgery
In this Packet
Medical
Support
Nutrition and Lifestyle
Getting
1.
2.
Services 3.
4.
Around
Medical
Information on medicine, procedures, and what to expect.
Medications
It is UNSAFE to take the following medications before surgery because they can cause bleeding problems:
Anti-platelet medications generally need to be stopped one week prior to surgery (Plavix, Effient, Coumadin, Enoxaparin/Lovenox). Your surgeon will advise you specifically.
Medicines Containing Aspirin: Stop 10 Days Before Surgery
A A/D®
Alka Seltzer®
Anacin®
Analgesic Caplets®
Arthritis Foundation Pain Reliever®
Arthritis Pain Formula
Arthritis Strength Bufferin
ASA Enseals®
ASA Suppositories®
Ascriptin
Aspergum®
Aspirin
Aspirin Norwich Regular Strength
Asprimox®
Axotal®
Azdone®
B Bayer® (most formulations)
BC® Powder and Cold Formulations
Bufferin® (most formulations
Bufferts II®
Buffex®
C Cama® Arthritis Pain Reliever
COPE®
D Darvon® Compound 65
Dasin®
Dolprin®3
E Easprin®
Ecotrin (most formulations)
Empirin® Aspirin (most formulations)
Epromate®
Equagesic Tablets
Equazine®
Excedrin® Extra-Strength Analgesic Tablets and Caplets
Excedrin® Migraine
F Fiogesic®
Fiorgen PF®
Fiorinal® (most formulations)
Fiortal®
G Gelpirin®
Genprin®
Gensan®
H Headrin®
Heartline®
I lsollyl®
L Lanoprinal®
Lortab® ASA Tablets
M Macrainin®
Magnaprin®
Marnal®
Maximum Strength Arthritis Pain
Formula Momentum®
N Norgesic Forte® (most formulations)
O Orphengesic®
P Painaid®
Panasal®
Percodan® Tablets
Persistan®
Pravigard®
R Rhinocaps®
Robaxisal® Tablets
Roxiprim®
S Saleto®
Salocol®
Sine-Off® Sinus Medicine
Tablets-Aspirin Formula
Sodol®
Soma® Compound Tablets
Soma® Compound with Codeine Tablets
St. Joseph® Adult Chewable Aspirin
Supac®
Suprin®
Synalgos® —DC Capsules
T Talwin® Compound
Tenol-Plus®
Trigesic®
Tri-pain®
U Un-aspirin®
Ursinus®
V Vanquish” Analgesic Caplets
W Wesprin” Buffered
Z Zee-Seltzer®
ZORprin®
Medicines Containing Vitamin E: Stop 10 Days Before Surgery
• All Multivitamins
• Amino-Opt-E
• Aquasol E
• Aquavit
• d’alpha E
• E-10001U Softgels
• E-400 IU
• E-complex-600
• Vita-Plus E
Herbal Supplements, Powders and Pills: Stop 7 Days Before Surgery
Herbal supplements can interact with other medications by increasing or lowering your blood pressure, causing bleeding problems, or altering the effects of anesthesia or sedatives. *This is not a complete list. ALL herbal medications and dietary supplements should be stopped 7 days before surgery.
Examples of these medications are:
• Acai Berry
• Garlic
• Ginseng
• Turmeric
• Echinacea
• Ginkgo Biloba
• St. John’s Wort
• Valerian
• Fish Oils
• Omega 3’s
• Omega 6’s
Non-steroidal Anti-inflammatory Medications: Stop 2 Days Before Surgery
A Actron Caplets
B Bayer® Select Pain Relief Formula Caplets
C Children’s Motrin®
None of the above medications should be taken during the immediate post op phase. Your health care provider will instruct you when it’s safe to resume these medications. This is usually after your post op visit or 7-14 days after surgery.
Medications
Altran®
Arthrotec®
Advil Migraine® Advil® Aleve®
Anaprox DS® Ansaid®
ClinorilV D Daypro® Diclofenac E Etodolac® F Feldene® Flurbiprofen
Genpril® I lbuprin® Ibuprofen lndocin® lndomethacin K Ketoprofen Ketorolac L Lodine® M Meclofenamate Mefenamic Acid Meloxicam Menadol® Midol® IB Mobic® Motrin®
N Nabumetone Nalfon® Naprosyn® Naproxen Nuprin® O Orudis®KT Oxaprozin P PediaCare Fever® Piroxicam Ponstel® R Relafen® S Saleto200® Sulindac T Toradol® V Voltaren®
G
1B
Medications
Medicines that are SAFE to take up to the day of surgery are the acetaminophen medications. These medications do not increase your risk of bleeding. Do not take more than 4,000 mg in 24 hours. Very high doses can damage your liver. (No more than 3,000 mg if you are elderly)
Medicines Containing Acetaminophen:
A Acephen
Aceta® with Codeine
Acetaminophen with Codeine
Arthritis Pain Formula® Aspirin-Free
Aspirin-Free Anacin®
B Bayer® non-aspirin
D Darvocet-N 100®
Datril®
Di-Gesic®
E Esgic®
Excedrin P.M.®
F Fiorcet®
L Lorcet®
Lortab®
N Naldegesic®
Norco®
P Panadol® Percocet®
R Repan Roxicet®
T Talacen®
Tempra®
Tylenol®
Tylenol® with Codeine No.3
V Vanquish®
Vicodin®
W Wygesic®
Z Zydone®
Pain Control and Medication
You have been prescribed a narcotic analgesic for pain control after your surgery. Our goal is to minimize your pain so that you can heal quickly and get back to the things you enjoy. Your pain should not interfere with sleeping, eating, grooming, or taking care of yourself. We want you to be up and about, going for walks, and visiting with friends and family. Proper pain management will help you do this.
A few facts you should know about narcotic analgesics:
• You should NOT drive your car or operate dangerous machinery while taking narcotics. People are often less alert when taking this medicine.
• You should take this medicine before you have extreme pain so that it will work most effectively.
• This medication may upset your stomach or make you nauseous. This is a normal side effect and does not mean you have an allergy. It is best to take this medicine on a full stomach.
• Narcotics can constipate you. While you are taking narcotics you should increase your fruit and vegetable intake, consume eight 8-ounce glasses of fluids every 24 hours and eat 25 to 35 grams of fiber a day. Do not drink caffeinated beverages. Take a 20 minute walk twice a day. If you become constipated, contact your doctor’s office and speak to the nurse.
• This medication may be habit forming. When you miss a dose do not take double doses or extra doses to make up for the missed dose. Take this medicine as prescribed.
• If your narcotic contains acetaminophen (Vicodin, Lortab, Lorcet, Percocet), avoid other forms of acetaminophen (Tylenol®) while taking this medicine. Taking more than 4 grams (4,000 mg) of acetaminophen in 24 hours is not recommended (3,000 mg if you are elderly). If you’ve been told not to take acetaminophen, contact your doctor’s office.
• Avoid alcohol at this time.
If you feel that your pain is not well controlled, contact your doctor’s office and speak to your Nurse Practitioner or Physician Assistant.
Breast Reconstruction
As of January 1, 2011, New York State law requires that every patient undergoing breast surgery in the state of New York receive breast reconstruction and insurance information.
Breast Reconstruction
After a mastectomy, a woman might choose to wear a breast form ( prosthesis ) that fits in her bra or a specially designed bra with a breast form built into it, have her breast reconstructed by a plastic surgeon, or do neither. Some women choose to get body art tattooed over their mastectomy scars. Others opt not to have a breast form, tattoo, or reconstructed breast. This is a highly personal decision. Discuss your options with your plastic surgeon to help you decide the best option for your comfort and appearance.
If you have a mastectomy, there are different types of breast reconstruction available. It is important to know that a rebuilt breast will not have natural feelings or functions; but the surgery can give you a result that looks like a breast. If you think that you want breast reconstruction, it is important to discuss reconstruction with your surgeon before your mastectomy and ask for a referral to an experienced plastic surgeon. Many women start reconstruction at the same time as their mastectomy; some wait several months or even years.
Breast reconstruction—surgery to “rebuild” a breast—is an option for anyone who has lost a breast because of cancer. New York State law requires health insurance policies that provide medical and surgical coverage to pay for reconstruction and for surgery to the other breast to achieve a good match. Required payment for breast reconstruction does not apply to self-insured health plans or to some plans paid for by out-of-state employers.
If you have questions about legislation on breast reconstruction or other insurance legislation, call the New York State Insurance Department at 1-800-342-3736.
If you are considering breast reconstruction surgery, this section gives information on the types of surgeries available.
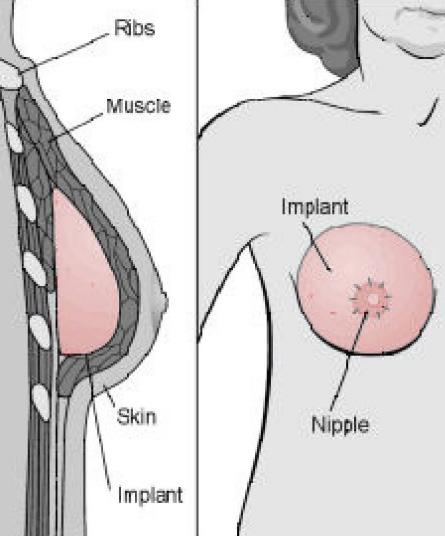
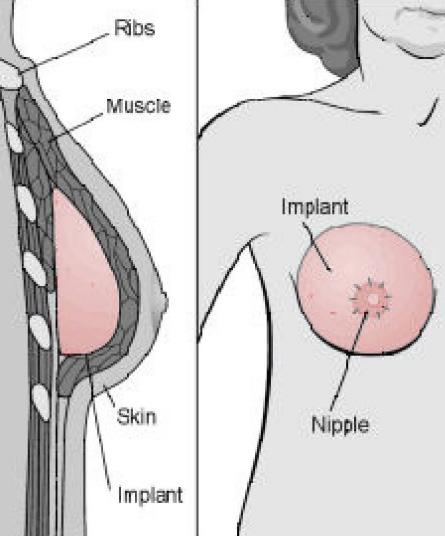
Reconstruction with Implants
Implants are plastic sacs filled with silicone (a type of liquid plastic) or saline (salt water). The sacs are placed under your skin behind your chest muscle. Implants may not last a lifetime, and you may need more surgery to replace them later. Sometimes saline implants “crinkle” at the top, or can shift with time, but many women don’t find these changes troubling enough to have the implant replaced.
The Food and Drug Administration (FDA) has studied the safety of silicone breast implants and the immune system for several years; the most recent research shows that these implants do not cause immune system problems. The FDA approved two kinds of silicone implants for breast reconstruction surgery in 2006. If you are thinking about having silicone implants, you may want to talk with your surgeon about the FDA findings and whether silicone implants are an option for you.
Breast Reconstruction
Breast Reconstruction with Implants
Possible Side Effects of Reconstruction with Implants
People who have had reconstruction with implants sometimes have pain, infection, or rupture (breaking) of the implant. Additionally, some people may not be happy with how the results look, or scarring could form around the implant over time, making the reconstructed breast look less attractive.
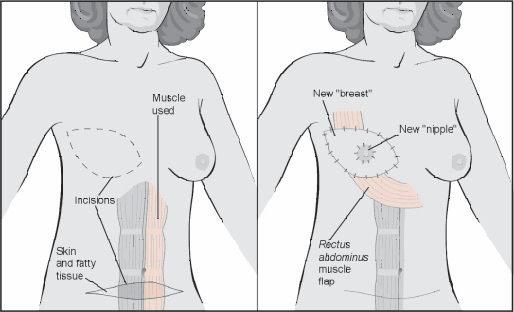
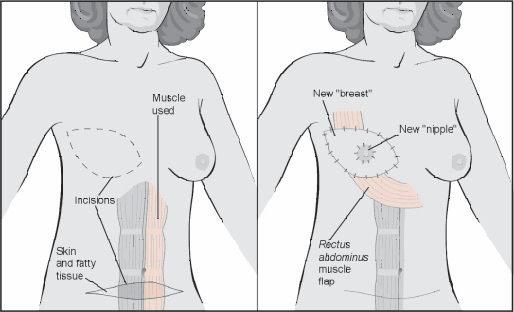
Reconstruction with Tissue Flaps
Tissue flap surgeries use muscle, fat, skin, and blood vessels moved from another part of the body to rebuild the breast. This tissue can be taken from the:
• Lower stomach area (known as TRAM Flap or DIEP Flap )
• Back
• Buttocks
These surgeries also sometimes use an implant to make the new breast match the opposite breast. A woman starting this process should know that it often requires more than one surgery. Extra steps may include adding a nipple, surgery on the opposite breast to create a good match, and perfecting the shape of the rebuilt breast.
Breast Reconstruction with Tissue Flaps
Possible Side Effects of Reconstruction with Tissue Flaps
These surgeries leave scars in two places: one where the tissue was taken from and one on the new breast. The scars may fade over time and may never go away completely. There also might be muscle weakness where the tissue was taken, differences in the size and shape of the breasts, or poor blood supply to the new breast. Choosing a plastic surgeon that has been trained in this surgery and has performed it successfully on many other women can reduce the risks.
From the New York State Department of Health nyhealth.gov
Support Services
Information on mental and physical health support groups
Breast Health Resource Program
Compassionate and informed support for individuals coping with breast cancer.
The Mount Sinai Breast Health Resource Program offers a flexible appointment schedule to best meet your needs. We are able to meet with patients and their families at our office, physician’s offices, or on the Mount Sinai campus.
The Mount Sinai Breast Health Resource Program is funded through generous gifts from individuals, corporations, and foundations. All programs and services are provided free of charge. To help us continue our patient care, contributions are greatly appreciated.
The Mount Sinai Breast Health Resource Program is a service of The Mount Sinai Hospital and an affiliate of the Dubin Breast Center of The Tisch Cancer Institute.
Mount Sinai Breast Health Resource Program
19 East 98th Street, Suite 4F
New York, NY 10029
T 212-241-7748
F 646-537-8927
To learn more about the Mount Sinai Breast Health Resource Program or to schedule an appointment, please call 212-241-7748
Young Women Connect

A support and wellness group for young women who have been diagnosed with breast cancer.
For more information, please reach out to your clinical care team.
5:30 – 6:30
drop-in support group
First Thursday of each month |
pm Virtual
Dubin Schmoozin
Wednesdays | 11 am – 12 pm
Virtual drop-in support group
Knit, crochet, and experiment with craft projects while socializing with other women who are coping with breast cancer.

Beginners are welcome. Materials and instructions will be provided. If you have a project that you’re working on, feel free to bring it!
For more information, please reach out to your clinical care team.
Oncology Massage Therapy Services
Therapeutic oncology massage can be helpful in relieving stress and anxiety, as well as easing muscle tension during breast cancer treatment. Other benefits may include reduced pain and fatigue, decreased anxiety, reduced nausea, improved sleep, and a greater sense of wellbeing.
Our goal is to provide relaxation, support, and stress management.
Licensed Massage Therapists are available at the Dubin Breast Center to provide our patients with massage therapy services prior to, during, or after scheduled medical visits. Sessions are between 10-30 minutes and are provided at no additional cost.

Massage services include:
• Foot Reflexology
• Hand, Shoulder, and Neck Massage
• Relaxation Techniques
– Guided Meditation
– Breathing Exercises
– Reiki
Due to the popularity of the massage program, sessions will be offered at the availability of the therapist’s schedule and medical clearance.
The Dubin Breast Center massage therapy team is comprised of experienced New York State Licensed Massage Therapists (LMT) and Nationally Board Certified Reflexologists (NBCR) with advanced training in Oncology Hospital-Based Massage.
For more information, please reach out to your clinical care team.
Talking to Children
It is natural for parents to have concerns about their children when diagnosed with cancer. It is understandable to want to protect your children from worrying about you. Children are often better able to cope with a parent’s illness if they are given information early, clearly, and honestly. Parents know their own children best. The following communication guidelines might help as you prepare to talk to your children.

• Prepare yourself. Understand the medical information before you tell your children.
• Plan with whom and where you will talk. It is important that your children get information from a consistent source. It will enable them to come back to you or another trusted adult about future questions or concerns. Find a location that is safe, comfortable and quiet.
• Set the tone. What you say is just as important as how you say it. Even if you are sad, anxious, or frightened, try to project a calm, comforting, and positive tone. Children may feel overwhelmed if you seem overly anxious or emotional. Children tend to take their cues from their parents.
• Communicate on their level. If you have children of different ages, you might choose to speak to them separately or if you choose to speak together, gear the discussion towards the younger child and offer further explanation to the older ones individually.
• Be brief. Share information a little at a time to avoid overload. Remember this is an ongoing discussion not just a one-time conversation. It is often helpful to explain as you go. If you need testing followed by surgery followed by chemotherapy, talk about one thing at a time to help your child process the information.
• Be honest and hopeful. Simple and more general explanations will allow a greater opportunity for discussion. Offer a realistic, but hopeful assessment of the situation.
• Maintain routines. Maintaining the same sense of structure you always have is likely to reassure your children. Acknowledge that some things will be different. Let them know of changes in advance. It’s also important to have consistent and familiar caregivers.
• Reassure them. Your child needs to know that whatever happens, they will be okay. Your goal is not to make them think that everything is normal but rather to reassure them that even if something is hard and difficult, that they will be okay.
• Ask and listen. Encourage your child to express their feelings and ask questions. Explore the children’s reaction on a regular basis as their feelings can change as much as the situation at hand. If your child is quiet ask them if they have any thoughts about your upcoming test/procedure/consult, etc.
Talking to Children
The following are some age-specific tips for talking to your children.
• Under age 3: Even kids this young can sense a change. Use words in their vocabulary like, “Mommy has a boo-boo,” or “Mommy needs medicine,” to help them make sense of what is going on.
• Preschool aged 3-5: At this age children tend to focus on concrete changes in you or in their environment. For example, “Remember when Daddy had his knee surgery? I’ll be pretty sore like he was, but after a few days things will be back to normal.” At this age, they tend to have magical thinking and believe their behaviors or thoughts gave you the cancer and that those behaviors or thoughts can take it away. Be sure to tell them that they did not cause the cancer and that cancer is not contagious. Keep the conversation brief and revisit when asked.
• Children 6-10: Children at this age begin to develop a more realistic understanding of sickness and cancer. The older they get, the more detailed explanations they may require. They also have a broader perspective, and can put illness into context.
• Teenagers: Adolescents can understand the concept of sickness the way adults do. But their ability to cope with the information varies. Teenagers are egocentric and tend to focus on themselves and on how your illness affects them. Be sure to let them know that, for the most part, they will be able to maintain their activities and interests. Teenagers have access to the internet and information is readily available to them. They may also be concerned about their own risk of developing breast cancer in the future. Talk to your MD/RN to understand their risk.
• All Children: Always explore your child’s feelings. Ask them what they are thinking and how they are feeling. Let them know it’s okay to be angry, confused, or scared. Remind them that they can always talk to you or other caregivers about their concerns.

For more information or to talk with a Social Worker, please call the Breast Health Resource Center/Dubin Breast Center at 212-241-7748 or email
DubinSocialWork@mountsinai.o rg
Nutrition and Lifestyle
Information and tips on diet and lifestyle
Nutrition and Lifestyle

Dealing with breast cancer and its treatments can be physically and mentally demanding. While just getting through this time may be your top priority, there are actions that you can take to feel and function at your best. As with most behavior changes, you may find it easier to adjust if you incorporate new habits slowly and in small increments. Any change towards a healthier lifestyle will have benefits, and small changes over time will add up to great rewards.

Maintain or become a healthy weight
As Americans have begun to eat more and move less, being overweight or obese in this country is common. Vanity aside, maintaining or becoming a healthy weight can reduce your risk for a number of diseases. In healthcare, we use a formula called the body mass index or “BMI,” which indicates how healthy your weight is based on your height. To determine if you are an appropriate weight, ask one of your health practitioners where you fall on the BMI scale or use an online BMI calculator. If you are overweight, the idea of weight loss can be quite daunting. Make small, short-term goals, and be sure to reward yourself along the way. Keep in mind that even a small loss toward your ideal weight can have great health benefits. Every bit counts! Your nutritionist can help you set goals and determine the best methods for sustainable weight management. If you are undergoing cancer treatment, make sure to ask your doctor if this is a good time to start a weight loss program.
Eat a plant-based diet
Eating well can make a big impact in your health and wellness as you go through the stages of cancer treatment and recovery. The American Institute for Cancer Research recommends eating a “plant-based” diet that includes a low intake of saturated fats. A plant-based diet does not necessarily mean a vegan or vegetarian diet. Rather, it encourages making the base of your meals plant-based with whole grains, vegetables, legumes, fruit, nuts, and seeds. Processed foods and animal foods, such as meat or dairy products, can contain high amounts of fats that have negative health consequences. To follow a plant-based diet, avoid using meat, dairy products, and processed foods as the centerpieces of your meals and start to think of these foods as condiments or side dishes. When choosing animal foods, generally opt for low-fat dairy products, lean cuts of meat, and fish. You can start by making a few plant-based meals or snacks per week and expanding your intake of plant foods over time.
Nutrition and Lifestyle
Increase beneficial foods and nutrients
Fiber: Eating a plant-based diet may make it easier for you to increase your intake of dietary fiber. Fiber is found naturally in whole grains, fruit, vegetables, legumes, nuts, and seeds. Its benefits include increased satiety (the feeling of being full), increased ease of weight management, helping to control blood sugar levels, and regulating digestion. To reap the greatest benefit from your foods, try to eat them in their “whole” state. Choose whole grain products instead of refined (e.g., quinoa instead of white rice) and consume whole fruits and vegetables instead of juices. Your goal for fiber intake should be about 25-30 grams per day. For more information on fiber, see the “Fiber Facts” handout.
Healthy fats: Replacing saturated and trans-fats in the diet (found in cuts of meat, dairy products, and processed foods) with unsaturated fats (found in fatty fish and plant foods such as oils, nuts, seeds, and avocados) can result in improved heart health and reduced risk for some cancers. Consistently consume moderate amounts of these fats with vegetable-rich meals to regulate blood sugar levels, increase feelings of satiety, and improve taste sensations. Fats are known to be “energy-dense,” meaning small portions are high in calories. Be mindful of your serving sizes when you begin to add these foods to your diet. In the traditional Mediterranean diet, the unsaturated fats of olive oil, fatty fish, nuts, and seeds are a major component, and some studies have shown a lower risk for breast cancer and other chronic diseases in women who follow this diet.
Vegetables: The fiber, vitamins, and minerals of vegetables make them excellent food choices. Additionally, many vegetables are very low in calories, so eating them can help you manage your weight. However, be aware that not all vegetables are created equally! Cruciferous vegetables, such as broccoli, cauliflower, and brussel sprouts have gained a reputation for being especially healthy for women with breast cancer.
On the other hand, starchy vegetables such as corn, peas, and potatoes are high in carbohydrate content and contain more calories than non-starchy vegetables such as asparagus or carrots. Starchy vegetables should be included only moderately in your diet.

Fiber Facts
Nutrition and Your Health

Post-operative constipation is quite common, even if you typically have regular bowel movements. The combination of anesthesia, pain medications, changes to your diet, fluid intake, and physical activity that occur before, during, and after surgery often contribute to postoperative bloating and constipation.
The good news is that eating fiber-rich foods and staying on top of fluid intake can help ease these symptoms and promote regularity. Increasing these fiber-rich foods slowly over the course of a few weeks post-surgery is a great way to ease your body back into a normal eating pattern and prevent constipation and its symptoms from getting worse. Follow these tips to get started:
• Drink plenty of fluids. Fluids help the body process added fiber without discomfort. Aim for at least 8–10 cups (8 ounces = 1 cup) per day, and always have a reusable, BPA-free water bottle nearby to sip from throughout the day.
• Choose whole grains. Try brown rice, quinoa, farro, freekah, millet, whole wheat pasta, and whole grain breads as opposed to the “white” versions.
• Read nutrition labels. Look for 100% whole wheat, rye, oats, corn, barley, etc. as the first ingredients on packaged foods such as breads, cereals, and pastas and look for at least 3–4 grams of fiber per serving.
• Cook with beans, legumes, and peas. Choose dried or canned (just make sure you rinse them!), and add to soups, stews, chilis, or try a cold bean salad. No matter how you use them, colorful vegetables are a perfect accompaniment.
• Choose fresh fruit and vegetables instead of juices. Juices are stripped of fiber during processing and can also contain a ton of sugar. Stick with fresh, whole fruits and vegetables as much as possible, and make sure to eat the peels or skins (if edible).

• Talk to your doctor or dietitian about calcium and iron supplements. These could exacerbate constipation, and it’s helpful to inquire about smaller dosing if you’re taking these supplements.
• Move more. Regular physical activity can help decrease the amount of time it takes for food to move through the small intestine and helps promote regularity. After your surgery try walking 15–20 minutes a few times per day.
• Aim to consume 25–35 grams of fiber per day. Take inventory of approximately where you fall within this range now, and increase by 2–4 grams of fiber per week until you reach this range.
Fiber Facts
Fiber-Rich Foods
Whole grains
Brown rice
Whole wheat or rye bread
Oatmeal (old fashioned)
Quinoa
Beans and Legumes
Baked beans
Lentils
Black beans
Split peas
Kidney beans
White beans
Nuts and Seeds
Serving Size
Fiber Content
6
7
Whole wheat pasta Farro 1 cup cooked 1 slice 1 cup cooked 1 cup cooked 1 cup cooked 1 cup cooked 3.5 grams 2 grams 4 grams 5 grams
grams
grams
1
1
1
1
1
1
10
16
Peanuts 1 cup cooked
cup cooked
cup cooked
cup cooked
cup cooked
cup cooked
ounce
grams
grams 15 grams 16 grams 18 grams 19 grams 3 grams
Almonds Walnuts Pecans Pistachios Sunflower seeds Pumpkin seeds 1 ounce 1 ounce 1 ounce 1 ounce 1/4 cup 1/4 cup 3.5
2 grams 3 grams 3 grams 3 grams 1.5 grams
grams
Broccoli
(flesh
Pear Apple Orange Raspberries Blueberries Blackberries Strawberries 1 medium 1 medium 1 medium 1 cup 1 cup 1 cup 1 cup 6 grams 4 grams 4 grams 8
4
Vegetables Kale Cauliflower
Brussels sprouts Cabbage Potatoes (sweet, Russet) 1 cup cooked 1 cup cooked 1 cup cooked 1 cup cooked 1 cup cooked 1 medium
and skin) 3 grams 5 grams 5 grams 5 grams 4 grams 4 grams Fruits
grams
grams 8 grams 3 grams
Fiber Facts
Sample High-Fiber Diet
Breakfast
1–2 slices whole wheat or sprouted grain toast topped with 1 egg, 1/3 mashed avocado and tomato slices; Coffee or tea
Lunch Salad with kale, spinach mix (>2 cups raw), 1/3 cup roasted Brussels sprouts or broccoli, ½ cup quinoa, sliced radish, sliced cucumber, 2 tsp sunflower seeds, 3 ounces grilled chicken or tofu in a light olive oil/red wine vinegar dressing
Dinner
Snacks (1–2/day)
1–2 cups of vegetarian chili with 1 cup spinach added, topped with 2 tbsp 2% Greek yogurt, small whole wheat roll
1 apple with 1 tbsp nut butter or 1/4 cup almonds, 6 ounces 0% Greek yogurt, ½ cup berries, 1 cup baby carrots and sliced celery mix, 1–2 tbsp hummus, 1–2 cups steamed organic edamame
Constipation Relief Fruit Paste Recipe
For a natural solution to constipation, try 2–3 teaspoons of this recipe each day.
Ingredients
½ pound prunes
½ pound raisins or pitted dates
½ pound figs
2 ounces Senna tea leaves (found at health food stores)
½ cup lemon juice
Instructions
Boil 2 cups of water, add the tea leaves and let soak for five minutes. Strain the tea and pour 1 cup of the tea liquid into a large pot, discard the rest. Add the fruit to this pot and boil for five minutes. Remove from heat; add the lemon juice and stir. Allow the mixture to cool. In a mixer, blender or food processor, turn the fruit mixture into a smooth paste. Spoon it into jars or freezer containers and store in the refrigerator or freezer.
Note: This fruit paste does not freeze solid, but keeps well in the freezer for up to 3 months. It can be spread on toast, mixed in with oatmeal, blended into a shake, or eaten by itself.
Healthy Fats
Nutrition and Your Health
Replacing fats from animal-based and processed foods with those from plants and fish can result in reduced risk for heart disease, in addition to providing an array of other health benefits. Some excellent sources of fat include: oils, nuts and seeds, avocados, and salmon. A few are highlighted here:
Avocados are best known for their healthy, monounsaturated fats. They contain antioxidants and dietary fiber, as well as having anti -inflammatory and digestive properties. The nutrition and flavor of avocado is best preserved when eaten raw.

Extra virgin olive oil is the unrefined oil from the first olive pressing, and it is superior to other olive oils in both taste and health properties. Similar to avocados, extra virgin olive oil contains monounsaturated fats and has anti-inflammatory properties. It may also help to lower cholesterol and blood pressure along with reducing the risk for some cancers.

Walnuts are one of the only plant-based sources of the anti -inflammatory and heart healthy omega-3 fatty acids. Make sure to eat the flaky and slightly bitter skin of walnuts for optimal health benefits.
Salmon , like walnuts, is an excellent source of omega-3 fatty acids, aiding cardiovascular and inflammatory health systems. The specific types of fatty acid found in salmon (EPA and DHA) may provide benefits for cognition and protection against some types of cancer, including breast cancer.
Coconut oil was long thought to be a villain due to its saturated fat content. However, this plantbased oil has actually demonstrated heart healthy properties by raising HDL, “good cholesterol.” Coconut is also full of antioxidants and makes an excellent plant-based replacement for butter when baking.
Cruciferous Vegetables Nutrition


and Your Health
Cruciferous vegetables are often called the “super stars” of plant foods. They are packed with healthy nutrients and can be easily added to your diet.
Cruciferous Vegetables include: Arugula, bok choy, broccoli, brussel sprouts, cabbage, cauliflower, collard greens, kale, mustard greens, radish, rutabaga, turnip, and watercress. As a group, these vegetables are very high in vitamin A, vitamin C, folic acid (a B vitamin), and vitamin K. Some of these vitamins act as antioxidants, which can help to protect the body’s cells from damage. Cruciferous vegetables also tend to have high fiber and water contents, making them filling, low calorie foods that may also aid in digestion.
Phytochemicals are natural chemicals found in plant foods that have healthful effects. Some studies have found that the phytochemicals in cruciferous vegetables may help to defend against cancer.
Try to eat at least one serving of cruciferous vegetables per day; one serving is equal to ½ cup cooked vegetables or 1 cup raw.
Nutrition and Your Health
A Registered Dietitian is available at the Dubin Breast Center to provide our patients with individual counseling in the following areas:
• General wellness
• Weight management
• Side effect and symptom management
• Cooking and food preparation strategies
Meeting with a registered dietitian is a great opportunity to learn about how food plays a role in your health. During your nutrition consultation, your dietitian will work with you to create an individualized plan to help you feel and function at your best.
Nutrition consultations and follow-up visits are provided at no cost to all Dubin Breast Center patients. Please reach out to your clinical team for more information.

Eating During Cancer Treatment
General goals: to provide your body with enough calories, protein and nutrients to help repair and build body tissues and keep your energy levels up.
In general, a plant-based diet is recommended during treatment (and beyond!), which includes colorful fruits and vegetables, whole grains, healthy fats, and lean proteins. However, the foods you are able to eat will also depend on treatment side effects, and it’s important to remain flexible.
Q&A
Q. How should I eat if I have a decreased appetite?
A. Try eating small meals and snacks every few hours, rather than eating large meals. Make sure these snacks include a protein source whenever possible, which can be eggs, yogurt, cottage cheese, chicken, fish, turkey, nuts/nut butter, milk, tofu, etc. Try to take advantage of the times when you do have an appetite, and eat a larger meal. Keep favorite foods on hand if these are more appealing to you.
Q. How should I eat if I feel full quickly after eating?
A. Focus on having small meals and snacks throughout the day instead of large meals. Try to avoid drinking liquids during meals and instead, have them thirty minutes before or after. Avoid eating gas- producing and high-fiber foods, such as raw vegetables and fruits, beans, and whole grains, because they may make you feel full too quickly.

Q. How should I eat if I have nausea or vomiting?
A. Try to have small meals every few hours instead of large meals and stick with bland foods, such as toast, crackers, pretzels, yogurt, cream of wheat, potatoes, rice, or noodles. Sometimes, foods that are cold or room temperature may be easier to eat than foods that are hot. Make an effort to avoid greasy, spicy, high-fiber foods, and foods with strong odors; prioritize good hydration by sipping on fluids throughout the day. Ginger may help decrease nausea, and options to try include ginger tea, ginger beer, pickled ginger, ginger candies, and ginger snaps.
Q. How should I eat if I have diarrhea?
A. Make sure to drink plenty of fluids to prevent dehydration, such as water, diluted juices, broth, caffeine-free teas, and coconut water. Stick with foods that are low in fiber, such as mashed potatoes, yogurt, noodles, applesauce, toast, cottage cheese, rice, eggs, and cream of wheat. Avoid caffeine, raw fruits and vegetables, and if you are sensitive, limit dairy products as they can exacerbate diarrhea.
Q. How should I eat if I have constipation?
A. Make sure to focus on maintaining adequate hydration by drinking at least 10 cups of fluids daily. Include foods that naturally promote bowel regularity, such as prunes (stewed or dried), prune juice, grapes, figs, and papaya. In general, make sure to eat a diet high in fiber and include whole grains, fruits and vegetables, and beans into your meals daily. Regular exercise can also help promote bowel regularity.
Eating During Cancer Treatment
Q. How should I eat if I have mouth soreness or dryness?
A. Eat foods that are soft, moist, and/or blended, as these are easy to chew and swallow; and use liquids to make dry foods moist, such as gravy on bread and milk on dry cereal. Drink plenty of fluids and make sure to brush your teeth and rinse your mouth often to decrease pain and help your appetite. Special mouthwashes that may help are Biotene (over the counter) or Magic Mouthwash (prescription). For mouth soreness, avoid foods and drinks that are spicy, salty, tart, very hot, and very cold. For mouth dryness, eating sweet or tart foods and liquids, such as lemonade, hard candy, and popsicles, may help your mouth make more saliva.
Q. How should I eat if my sense of taste or smell changes?
A. Try different flavors such as tart, salty, or sweet to find foods that you can tolerate, and add seasonings such as herbs and spices to make foods taste better. Try having meats at room temperature or cold, and if you cannot or do not eat meats, choose other good protein sources. These include Greek yogurt, eggs, nuts, nut butters, cheese, milk, shakes, and tofu. Brush your teeth and rinse your mouth often and eat with plastic utensils to decrease metallic tastes in the mouth.
Q. How should I eat if I often feel tired?
A. Have foods on-hand that take little or no work to prepare, such as Greek yogurts, cheese sticks, peanut butter, crackers, boxed soups, frozen entrees, vegetables, and fruits. Do not be afraid to ask for help with food shopping and meal preparation from friends and family—more often than not, they are more than happy to help. When you’re feeling more energized, try to make batches of food that can be frozen and used for later. Make sure to drink plenty of fluids (at least 10 cups per day) and exercise regularly, which can help you feel more energized.
Q. How should I eat if I gain weight?
A. Try to make half of all your meals vegetables and fruits, which are naturally low in calories and high in nutrients and fiber. If you find yourself emotionally eating when you’re stressed, sad, or afraid, focus on other strategies to help you cope. This can be exercise, calling a friend or family member, meditation, reading, or joining in support group activities.
Q. Are there foods I should avoid?
A. People who are going through cancer treatment may have a hard time fighting infections and food poisoning. Make sure to wash all raw fruits and vegetables very well, and wash your hands before and after preparing foods. Cook meats and eggs very well, and avoid raw foods (sushi, smoked salmon, shellfish), salad bars, deli meats, unpasteurized juices, milk, and cheese where bacterial contamination can be more likely.
Q. Can I meet with a nutritionist?
A. Yes! Our registered dietitian is always available to meet with you in person, speak with you on the phone, or answer questions via email.
Nutrition and Lifestyle
Exercise
Physical activity can reduce the risk for breast cancer and improve breast cancer related outcomes, and greater benefits are associated with higher levels of exercise post-diagnosis. The possible reasons for this positive effect are related to the promotion of optimal immune, antiinflammatory, and metabolic functioning. Exercise can also help with the symptom or side effect management of many breast cancer treatments and can minimize bone loss.

We strongly recommend that you get at least 45-60 minutes of moderate to vigorous activity on most days of the week, and more is better. This activity does not need to be performed all at once, and it can be easily incorporated into your regular daily schedule. If you are crunched for time, you may find it easier to break up your exercise into 10-15 minute segments, 3-5 times per day. For basic health benefits, and especially if you have any physical limitations, you need only to perform moderate activity. Exercise to the point that you increase your energy level and not to the point of exhaustion.
Most importantly, exercise should be something that you find enjoyable. If you have never enjoyed going to the gym, there are plenty of alternatives... You can try a dance or yoga class or take a brisk walk with a friend. At Dubin, we offer two levels of walking groups that you are welcome to join.
Examples of enjoyable, low-impact exercises include:
• Swimming
• Water aerobics
• Bike riding
• Tennis
• Ice skating
• Roller skating or blading
• Pilates
• Aerobics
Limit your intake of alcohol
The way that alcohol affects health is complicated. Cardiovascular benefits from moderate red wine consumption have made alcohol popular in health media. However, there are no cancer benefits to drinking. In fact, even moderate alcohol intake is related to the development of many types of cancer. As little as two drinks per day for men and one drink per day for women can increase the risk for developing these diseases. A number of studies have seen a connection between alcohol and breast cancer, and the type of alcohol (e.g., red wine vs. whiskey) does not change this observation. The exact mechanism is unknown, but the relationship may be due to
Nutrition and Lifestyle
the effect of alcohol on hormone levels. Our recommendation is to have less than one drink every other day and to consider limiting intake to social events or special occasions. (One drink is equivalent to 12 oz beer, 5 oz wine, or 1½ oz 80-proof liquor.) Examine when, why, and how much you drink. You may find that drinking is a habit, that it serves emotional purposes, or that it simply heightens a dining experience. Think of positive behaviors that can serve as a substitute for some of your drinking. If you think that you may have an issue of alcohol abuse, there is no better time to pursue a lifestyle change. Inform one of your Dubin healthcare providers, and we will connect you with appropriate resources.
Smoking
Quitting smoking is the single best healthy lifestyle choice you can make for yourself. Smoking is directly related to lung disease and lung cancer. It also plays a role in the development of cardiovascular disease, stroke, and many kinds of cancer, including throat, esophageal, tongue, stomach, and bladder. Furthermore, it can contribute to other types of illness such as peptic ulcers and infertility. It can cause severe illness in people who don’t smoke through the inhalation of second-hand smoke, and can be particularly harmful for people having surgery by interfering with wound healing and increasing the risk of pneumonia.
• There are 4,800 chemicals in cigarettes including 69 which are known carcinogens.
• Nicotine is the addictive part of the cigarette and travels to the brain faster than medication delivered into a vein.
• Cessation of smoking often requires several attempts. Do not get discouraged if you quit and start again.
There are several resources available for smoking cessation:
• New York City has a hotline where you can get help. Call 311 and get free nicotine patches and gum.
• Call the American Lung Association for information and additional resources, or visit their “Stop Smoking” page online.
• The Mount Sinai Health System offers a few smoking cessation programs, please call 212-523-3606 for more information.
Stress Reduction:
Stress is defined as “your response to your environment.” This can be either good or bad. Good stress is often a motivator to get up in the morning and be engaged in our lives. It shows that a person is adapting to the world around them. It energizes us, allows us to be creative, solve problems, and learn.
Nutrition and Lifestyle
Bad stress leads to fatigue, frustration, and irrational problem solving. When people are confronted with a stress-inducing event, they respond initially with a drop in energy while the mind understands what is happening to them. Next, there is a surge in energy while the person adapts, either solving the problem or running away. Many people know this as the fight or flight response. If the issue cannot be resolved, cannot be resolved satisfactorily, or is continuing for a prolonged and unmanageable amount of time, the person becomes fatigued and exhausted and no longer functions well.
When a person is under stress, their:
• heart rate increases
• breathing becomes rapid
• pupils dilate
• muscles tense
• blood pressure increases
When a person is relieved of their stress everything returns to normal. When a person is under constant or uncontrolled stress, blood pressure, heart rate, and respirations all remain chronically elevated. This can lead to illnesses such as peptic ulcers, coronary artery disease, and mental fatigue.

We cannot always control the amount of stress we are under. A cancer diagnosis can keep us feeling stressed for a prolonged period of time; make us feel out of control, fearful, and sad. We can, however, control our stress response by learning to manage it and learning relaxation techniques. A reduction in stress, even for a short period of time, can help you feel more in control of your life and what is happening to you.
Techniques for Stress Reduction:
• Schedule time for yourself every day. Even 15 minutes in your favorite room with a cup of tea and a book can help induce the relaxation response.
• Quiet time is essential to your health, but others do better with friend-time or by socializing. Know what works and schedule it into your calendar.
• Mind-body activities such as yoga, tai chi, or meditation can slow your heart rate, relax your muscles, and reduce your breathing rate. Done regularly, the effects can be felt more readily and have a longer, sustaining effect on your health.
• Expend energy. A cardio class at the gym, riding your bike, or swimming laps can help you feel less anxious and sad. The increased blood flow to your brain can help you feel less flustered and make your thinking more clear.
• Cut back on your caffeine intake. This is adding stimulation to your anxiety. Green tea contains an amino acid that promotes a calming sensation. Herbal teas have similar effects.
Nutrition and Lifestyle
• De-clutter your home and work environment. The clutter is adding to your sense of loss of control and anxiety. Enlist the help of family and co-workers to clean off surfaces, file papers, and organize spaces.
A breast cancer diagnosis or the treatments that follow may serve as a particularly stressful time in your life. This is the time to pull together your emotional resources. Let friends and family members cook you meals and care for you, take on some of your chores, and listen to your fears. We have a variety of supportive resources at Dubin: massage therapists, psychologists, social workers, and a psychiatrist, who are all here to assist in your breast cancer care. Speak to someone on your health team to be connected with these services.
Managing Fatigue
Fatigue is the most common side effect of breast cancer treatment, and it is estimated that about 9 out of 10 people may experience this. Symptoms of fatigue include lack of energy, sleeping more than usual, feeling unable to do normal activities, putting less effort into appearance or self-care, feeling tired after sleeping, having difficulty concentrating, and having trouble finding words. Complementary approaches that have been found effective in reducing fatigue include: massage, acupuncture, meditation, reiki, tai chi, and yoga.
Tips for Managing Fatigue
• Exercise is an excellent treatment for fatigue, with plenty of research to support this. It’s recommended that you get a minimum of four hours per week of physical activity, but when you’re fatigued, set a goal of about 15 minutes of walking per day, and then gradually increase this time, as able. Other types of gentle exercise include yoga or tai chi.
• Eating too many refined carbohydrates such as white breads, pasta, white rice, and sugary desserts may sound particularly appetizing when you’re fatigued, but these foods will only increase feelings of lethargy.
• Eat a diet that is rich in vegetables and contains adequate amounts of fruit, legumes, fish, nuts, seeds, and oils.
• Fatigue may occasionally be related to certain vitamin or mineral deficiencies. Ask your doctor if you should be tested for any of these, or speak with your nutritionist about which foods contain these nutrients.
• Stay away from alcohol, coffee, caffeine, and nicotine in the evening to avoid disrupting sleep patterns.
• When you have the energy to cook, make a large batch of something, and freeze the excess in small containers. When you are too tired to cook, you can quickly heat up one of these.
• Keep a consistent schedule by going to bed at the same time each night and waking up at the same time each day, giving yourself about 8 hours of sleep in between. Early morning exercise may help to solidify your routine and provide additional energy, while strenuous exercise in the evening may keep you from falling asleep at night. Also, limit naps to 30 minutes to avoid grogginess.
• While you may not be able to keep up with your usual routine, be kind to yourself, and allow yourself to rest and recover adequately.
Nutrition and Lifestyle
Tips for better Sleep
• Do not overeat, especially after 6 pm, and eat meals at the same time every day.
• Reduce or eliminate caffeine intake, or stop caffeine intake early in the day. Caffeine can have a long lasting impact in our bodies, and can influence our ability to fall or stay asleep. Its effects may be subtle or seemingly unrelated to sleep difficulties. Chocolate contains caffeine and should be avoided in the evening.
• To avoid waking for urination, reduce your fluid intake after 5 pm, focusing on meeting your hydration needs earlier in the day.
• Get aerobic exercise early in the day and limit vigorous exercise in the evening. Body temperature plays a role in sleep, with cool temperatures promoting sleep and heat promoting waking. As exercise raises the body’s temperature, it may be difficult to fall asleep afterward.
• Attempt to get 15–30 minutes of morning sun exposure.
• Avoid napping, which may interfere with your sleep cycle.
• Dim lights and avoid “screens” in your area at least one hour before bed. Exposure to lights can reduce the production of melatonin, which is a hormone that promotes sleep.
• Go to sleep and wake up at the same time every day.
• Reduce noise and stimulating activity at least one hour before bed.
• Develop routine bedtime practices.
• Cool the temperature of your environment at least one hour before bed. 65 degrees is thought to be the optimal temperature for sleep.
• Consume herbal teas in the evening (chamomile, lemon balm, valerian, etc.).

• Do not lie in bed after night waking.
• Keys to an ideal sleep environment include: complete darkness, relaxing pillow, cool temperature, controlled noise, no computer or TV, and hidden or removed clocks.
• The bedroom should be for sleep or intimacy only. Do not read, work, or watch TV in bed.
Nutrition and Lifestyle
Summary
People who are successful in making changes understand some basic concepts. Find out what motivates you and use that to maintain your focus. Some people track their progress in a journal and others reward themselves at specific milestones such as being able to swim 10 laps or losing 5 pounds. Change is a process that takes time. If you can stick to a new routine for 30 days, research has shown that your likelihood of continuing with that behavior is strong. Start slowly and don’t overwhelm yourself. Don’t be hard on yourself if you are not successful. Simply recommit to your goal and start again. Pick something easy to begin with so that you are successful right away. Choose something you have always wanted to do.
Take advantage of the Dubin Breast Center resources and use this opportunity to do something really good for yourself.

Getting Around
Information on parking and navigating
Mount Sinai
6 P i Legend The Mount Sinai Hospital Ground Level Admissions–Pre-testing, Surgical and Procedural Registration, Family Waiting Area Take Guggenheim stairs or elevator to second floor Dubin Breast Center 1176 Fifth Avenue, First Floor Bookstore Chapel (first and second floor) Cashier ATM Machine Plaza Café Patient Services Center Rehabilitation Services and Clinics Ruttenberg Treatment Center Elevators Stairs Escalators Bus Stop Restrooms Parking Information/Security Lost? Call 212-241-6068 or 46068 from a house phone All buildings are wheelchair accessible. For Atran, please get directions. Food Subway (at 96th Street and Lexington Avenue) 1 2 3 4 5 6 Gift Shop 8 7 9 10 11 P P 6 i i i i i i 1 2 3 4 5 6 7 8 9 10 11 Central Park Fifth Avenue Madison Avenue East 98th Street East 101st Street East 102nd Street Klingenstein Pavilion (KP) 1176 1428 1425 1440 1450 1468 1470 35 5 10 17 3 East 101st Street 10 East 102nd Street Center for Advanced Medicine (CAM) 35 East 102nd Street Hess Center for Science and Medicine (HCSM) 5 19 Kravis Children’s Hospital Guggenheim Pavilion (GP) Annenberg Building Atran-Berg Icahn School of Medicine at Mount Sinai Faculty Practice Klingenstein Clinical Center (KCC) Atrium 1184 1190 3 Down to MC Level East Elevators West Elevators
Patients of the Dubin Breast Center may park vehicles at our garage, located one block from our office, at: 99th Street, between Park and Madison Avenues.
If this garage has no available spaces, patients can refer to the following nearby parking facilities, located within walking distance of the Dubin Breast Center.
Satellite Parking & Shuttle
Patients may also utilize parking and shuttle services at the Mount Sinai Hospital Parking Facility, located on the Northwest Corner of East 104th Street and Madison Avenue.
After parking, please retain your ticket to be stamped and paid for at the Dubin Breast Center registration desk. The shuttle from the garage to the Ruttenberg Treatment Center, Mount Sinai Radiation Oncology, and Dubin Breast Center, is available every 20 minutes.
• Shuttle Hours of Operation: Monday – Friday, 7:30 a.m.–7:30 p.m.
• Parking & Shuttle Cost: $20 per day
• Please note, Mount Sinai observes a no tipping policy.
For any questions or to report a concern about parking or shuttle service, please call 212-241-5661.
Name of Garage Address Phone Number Hours of Operation Distance Rate per Hour Rate per Day East 97th Parking Corp. 175 East 96th Street (Between Third Avenue and Lexington Avenue) 212-348-8361 24 Hours 0.4 mile $9.00 $26.00 Manhattan Parking 215 East 96th Street (Between Second and Third Avenue) 212-410-5270 24 Hours 0.5 mile $13.00 $30.00 99 pm LLC 1559 Lexington Avenue (Between East 99th Street and East 100th Street) 212-828-5282 24 Hours 0.6 mile $10.00 $18.00 Gallery Garage Corp. 40 East 94th Street (Between Madison Avenue and Park Avenue) 212-369-9304 24 Hours 0.6 mile $17.00 $35.00 Icon Parking Systems 182 East 95th Street (Between Third Avenue and Lexington Avenue) 212-289-9760 24 Hours 0.6 mile $12.00 $24.00 Majestic Car Parking 1199 Park Avenue (At East 94th Street between Park Avenue and Lexington Avenue) 212-534-9616 24 Hours 0.8 mile $15.00 $32.00 Lexington Garage Corp. 1501 Lexington Avenue (At East 97th Street between Third Avenue and Lexington Avenue) 212-987-0270 24 Hours 0.8 mile $12.00 $26.00 Parking
Sunday Monday Tuesday Wednesday Thursday Friday Saturday Month: