Department of Ophthalmology











































































New York Eye and Ear Infirmary of Mount Sinai (NYEE) made significant strides in the fields of science and technology over the past year, particularly in pursuit of cutting-edge approaches to early detection and treatment of diseases like glaucoma, macular degeneration, and diabetic retinopathy. We also began preparing for a more active international presence with other global partners to spread our extensive training and surgical capabilities to regions of the world in critical need of those resources.
We are tremendously proud of the progress we made. Foremost, in July 2023, we launched the Center for Ophthalmic Artificial Intelligence and Human Health (COAIHH) to bring the vast, transformative power of artificial intelligence (AI) and big data to the way we practice ophthalmology on both patient and population scales. The new Center, described more fully in this report, is the first of its kind in New York and one of the first in the nation. It will team up with the Windreich Department of Artificial Intelligence and Human Health at the Icahn School of Medicine at Mount Sinai to push the boundaries of research, clinical practice, and education of the next generation of computer scientists and ophthalmologists grounded in AI.
It’s hard to overstate the impact artificial intelligence and machine learning will have on ophthalmology and on NYEE. Clearly, our role in advancing new AI-driven technologies through COAIHH will put us in a position of growing prominence and power within a major

academic health system like Mount Sinai. Ultimately, the beneficiaries of that reordering will be patients. From our AI and machine learning-driven initiatives will flow exciting new applications that could reveal, from a standard fundus photograph linked to a trained algorithm, an undiagnosed ophthalmic condition, or a vascular or neurologic disease that those images are also uniquely equipped to capture.
At the same time, AI promises to shift the focus of health care from individual patients to global populations. NYEE plans to play a meaningful role in that evolution through advanced training platforms able to reach ophthalmic specialists in parts of the world where their services are sparse or nonexistent. A model for that enterprise has emerged over the past year through the tireless work of one of our highly skilled oculoplastic surgeons, Harsha S. Reddy, MD. Granted an extended sabbatical by NYEE and Mount Sinai, Dr. Reddy designed, developed, and rolled out a robust online curriculum to prepare physicians to perform oculoplastic surgery in Rwanda— an African nation without a single specialist in that desperately needed field.
While NYEE faculty members have often shared their skills with physicians in developing nations, we are now looking to grow those singular efforts into a more formal program in sync with our mission—and that of Mount
Sinai—to care for patients and educate physicians internationally. Dr. Reddy is helping to promote that outreach by building relationships and vetting sites where our institution can truly make a difference.


We continue to make a difference, of course, in the lives of patients closer to home, especially as a site for handling some of the most complex surgical cases. We describe several in this report, including one involving a patient with Marfan syndrome complicated by dislocated lenses in both eyes, which required our surgeons to employ a special technique for attaching a secondary lens to the sclera. Also noteworthy is that one of those surgeons was a highly valued member of our voluntary teaching faculty who commits time each week to impart his extensive knowledge and skills to our residents and fellows.
Our Ocular Oncology Service is one of a few locations in New York City to offer intra-arterial chemotherapy to treat retinoblastoma. As described in the report, this advanced minimally invasive and chemotherapeutic approach proved to be life changing for a pediatric patient, resulting in eye salvage and vision preservation.

We also moved the needle this past year in the field of research, a core strength of NYEE, through two published studies with important implications for
large-scale screening of age-related macular degeneration (AMD). Led by our Director of Biomolecular Retinal Imaging, R. Theodore Smith, MD, PhD, the researchers reported that subretinal drusenoid deposits in the eye can be linked to high-risk vascular disease elsewhere in the body, potentially setting the stage for ophthalmologists, cardiologists, and primary care physicians to cross-test for life-threatening heart disease as well as AMD. No less significant is the work we’ve begun to genotype consenting patients in Mount Sinai’s Bio Me ® BioBank and assign each a risk score for glaucoma based on their genetic construct. The results to date have been very promising, according to Louis R. Pasquale, MD, who is leading the research, and could evolve into a powerful predictive tool to target populations for glaucoma and early intervention.
Initiatives like these underscore our resolve to stay ahead of the technology and science curve so we can continue to ensure that our patients experience outcomes informed by the groundbreaking work of our researchers and clinicians. That we may now be able to broaden our hospital’s reach for the first time to much larger populations is not only a source of great excitement, but a validation of why many of us at NYEE chose to enter the field of ophthalmology.

Artificial intelligence (AI) and data science are about to reconfigure the field of ophthalmology, and New York
Eye and Ear Infirmary of Mount Sinai (NYEE) is poised to help lead that revolution through the launch in July of the Center for Ophthalmic Artificial Intelligence and Human Health, the first of its kind in New York and one of the first in the country.


























The Center is a partnership between NYEE and the Windreich Department of Artificial Intelligence and Human Health at the Icahn School of Medicine at Mount Sinai, which are committed to breakthroughs in AI-driven diagnostic and clinical care of eye disease that can benefit patients personally as well as on a much broader population scale.




























“Ophthalmology is in a unique position among all medical specialties to drive AI through its advanced imaging capabilities, which provide a window on not just ocular diseases like glaucoma, diabetic retinopathy, and macular degeneration, but systemic conditions such as cardiovascular, neurologic, and renal vascular disease,” says James C. Tsai, MD, President of NYEE and inaugural Director of the Center. “Our new Center plans to take full advantage of that strength by pursuing innovative



technologies that can lead to early detection and intervention of disease, thereby preventing vision loss and even heart attacks and stroke.”







The potential impact locally and globally of this new research, clinical, and educational endeavor is as boundless as AI itself. “Artificial intelligence could truly democratize access to health care by deploying in underprivileged areas advanced systems we’ve built at Mount Sinai to show which patients are at risk for disease from simple fundus photographs of their retinas taken in local doctors’ offices,” observes Thomas Fuchs, Dr.sc, Dean of Artificial Intelligence and Human Health at Icahn Mount Sinai. “This ability to get a better holistic view of the patient is not futuristic. It’s very real.”




Indeed, the infrastructure for such a system is currently being piloted at seven primary care sites within the Mount Sinai Health System. As part of NYEE’s teleretina program, they employ fundus cameras to provide non-mydriatic images of the back of the eye of patients during annual physical exams—images that are sent securely to NYEE retina specialists for reading. Once the system is transitioned to an advanced AI algorithm, real-time, on-site interpretation of these photos would be possible, potentially flagging a wide range of undiagnosed ocular and systemic problems. From this on-site feedback could flow immediate patient referrals to appropriate specialists.
Another innovative program in place at Mount Sinai Morningside and Mount Sinai West hospitals is tele-consult, which provides for rapid diagnosis and triage of patients with eye emergencies by linking ER physicians via sophisticated telemedicine platforms to off-site ophthalmologists from NYEE. Incorporating AI into the image interpretation could give tele-consults a bold new dimension in terms of even faster and more comprehensive diagnoses that far exceed the capabilities of the human eye.
Big data is the coin of the unfolding AI realm, and researchers under the Center’s umbrella will be particularly gifted thanks to the trove of dataembedded images from NYEE patients, as well as from genotyping data residing at Mount Sinai. That information will be critical to the development and training of computer algorithms by data scientists, which in turn will provide the key to countless transformative applications in areas like detecting and monitoring disease, and patient response to treatment. “We have fantastic databases of accumulated patient information that will enable us to learn how different trends and factors cause disease progression, and through that knowledge hopefully be able to intervene early in the disease process,” explains Alon Harris, PhD, Vice Chair of International Research and Academic Affairs at Icahn Mount Sinai, and Co-Director of the Center.







That discovery is well underway. NYEE scientists, for example, have integrated AI and mathematical modeling to better understand the risk factors and pathophysiology of glaucoma. By analyzing new-onset visual field loss patterns from more than 2,500 affected eyes, a research team has gained insights into why certain populations are at greater risk for glaucomainduced blindness. Another team developed unique models for detecting age-related macular degeneration (AMD) at early, intermediate, and advanced stages using an ensemble of deep-learning screening methods and AMD-specific algorithms.

















One exciting application waiting in the wings is the use of AI-driven ChatGPT to provide counseling to patients seeking answers to commonly asked questions about diseases like open-angle glaucoma. A carefully trained natural language processing program could provide the initial response, and if a patient felt more information was needed, they would be referred to a physician. Another intriguing application being eyed by scientists





at NYEE: Using natural language processing to review the recorded voices of patients over the years from telemedicine emergency interactions, and from that archived information, develop an algorithm that could determine which patients need to be seen immediately by an ophthalmologist, and which can safely wait.


For Louis R. Pasquale, MD, Co-Director of the Center, the promise of applications like these underscores the value of the new Center in recruiting and training future leaders in technologically advanced eye care and research. “We believe that having a fellowship in AI will be important to attracting the next generation of leaders, particularly computer scientists,” he says, “and we’ll be ready to partner with them to undertake projects that merge their highly specialized skills with the robust data sets available to them at NYEE and Mount Sinai.”

Concludes Dr. Pasquale, who is Deputy Chair for Research, and Director of the Mount Sinai/New York Eye and Ear (NYEE) Eye and Vision Research Institute at Icahn Mount Sinai: “There’s so much data we’re now leaving on the table, and through the new Center for Ophthalmic Artificial Intelligence and Human Health, we’ll finally be able to leverage it to the enormous benefit of our patients and the physicians who provide their specialized care.”










Harsha S. Reddy, MD, has a passion for global ophthalmology that has led him to countries as distant as India, Nepal, and Ethiopia— devoting his personal time to serving on medical trips. When New York Eye and Ear Infirmary of Mount Sinai (NYEE) recently granted him an extended sabbatical leave to spread his considerable knowledge and skills in oculoplastics and orbital reconstructive surgery to Rwanda, an east-central African country devoid of that desperately needed specialty, he leapt at the opportunity.

In just a brief period, his impact and footprint are already visible. “Very few people have the professional and cultural commitment of Harsha to build something of the magnitude he has, and see it through to completion,” says Hunter Cherwek, MD, Vice President of Clinical Services and Technologies at Orbis International, a global nonprofit that trains, mentors, and inspires eye care professionals in places with the greatest need for them. “I love the fact we’ve been able to globalize his incredible teaching skills so that those who need them the most can truly benefit.”
Dr. Reddy, Director of the Ophthalmology Residency Program at NYEE, is a volunteer faculty member for Orbis, part of a global force of more than 400 medical experts from more than 30 countries who share their skills with local eye care teams. In that role, Dr. Reddy designed a blended learning curriculum for Orbis that consists of digital instruction on Cybersight—Orbis’ telemedicine platform, which offers eye care teams around the globe free virtual access to world-leading ophthalmic training developed by international medical experts—as well as on-site reinforcement and follow-up training.
The curriculum he designed, edited, and refined in collaboration with Cybersight experts consists of four modules covering the majority of oculoplastic soft tissue surgery through 800 slides and hundreds of photos, images, and videos. This online resource, designed to be a practical manual to bring surgeons-in-training to the functional level of an early-stage oculoplastics fellow, is now available free to ophthalmologists in low- and middle-income countries.

Content development, though, is only part of Dr. Reddy’s ambitious agenda. He spent a month as a visiting faculty member at the Rwanda International Institute of Ophthalmology delivering hands-on instruction encompassing wet lab, lectures, and actual surgeries. “I’d spend mornings doing didactics with the trainees,
and afternoons doing wet labs and live surgery at their side, often meeting with them individually to assess their skills,” Dr. Reddy recalls. “The goal was not to teach the complex surgeries right away, but to start with basics like suturing and offer them tips on how to improve their fundamental techniques. I loved working with the trainees who were hungry to learn and extremely motivated.”
There could hardly be a greater need for the skill set Dr. Reddy was eager to impart. Rwanda, a country of breathtaking scenery just south of the Equator, has not a single oculoplastic surgeon to serve 14.5 million people. “Having no specialists makes it very difficult to teach this subspecialty to residents,” says Dr. Ciku Mathenge, Director and Co-Founder of the Rwanda International Institute of Ophthalmology (RIIO), a nonprofit eye care organization that provides training, research, and community services in the region. “We have a lot of trauma cases that need reconstruction, many lid and conjunctival mass problems, orbital tumors that no one has the skills to fix, and a growing demand for correction of age-related lid problems.” Looking back at her experience with Dr. Reddy and the Cybersight initiative, Dr. Mathenge is quick to acknowledge, “Dr. Reddy filled a huge gap for us, and his teaching impacted the knowledge and skills of not just trainees, but also the faculty. I personally learned two new procedures from him.”
What could Dr. Reddy’s contribution mean for patients?
“With good oculoplastic training, we will be able to graduate more comprehensively trained surgeons who will be able to provide basic oculoplastic care in the district hospitals,” explains Dr. Mathenge, whose legacy includes transforming a public eye clinic in Kenya into one of the best-run facilities in the region. “For a patient with conjunctival squamous cell carcinoma or a child with retinoblastoma who needs an enucleation, professional care and management could mean life instead of death. For a child with a disfiguring condition, it could mean being able to attend school, rather than hiding at home.”
I love the fact we’ve been able to globalize his incredible teaching skills so that those who need them the most can truly benefit.
—Hunter Cherwek, MD
Which is precisely the reason Dr. Reddy remains unswervingly devoted to global outreach, despite a hectic schedule at NYEE, where he leads the nation’s largest residency program and has an active clinical and surgical schedule as Director of Oculoplastic, Orbital, and Reconstructive Surgery, and Director of the Department of Ophthalmology at Mount Sinai Beth Israel. “There is so much need, and we’re just scratching the surface in terms of what can and needs to be done,” he reflects. “We’ve made a good start. Nothing this comprehensive for beginning or intermediate oculoplastics distance learning exists anywhere in the world.”
(1), (7) and (9): Rwanda is known for its abundant wildlife and natural beauty.




(2): Dr. Mathenge performing an eye screening on a patient.

(3): Dr. Reddy with trainees in the OR.


(4): A female patient at the Rwanda Diabetes Association clinic for a diabetic retinopathy screening.
(5): Dr. Reddy conducting a wet lab demonstration for trainees.
(6): Cybersight Library on an iPad.

(8): A male patient getting an eye exam at the RIIO-Kibagabaga Community Eye Clinic.

At the same time, Dr. Reddy’s sabbatical and carefully curated Orbis project could potentially be a building block for a global education program spearheaded by both NYEE and Orbis International. Characteristically, Dr. Reddy signals his eagerness to take on the challenge.
“The goal is to develop a global health presence within our Department of Ophthalmology,” he states, “and I envision our own residents becoming involved in this outreach in a culturally sensitive way, where they benefit from learning how ophthalmology operates in other parts of the world.”
If Meenakashi Gupta, MD, Assistant Professor of Ophthalmology at the Icahn School of Medicine at Mount Sinai, has her way, the retina will become as critical a vital sign in annual physical exams of patients as temperature, blood pressure, pulse, and respirations.

And for good reason. A teleretinal screening program launched by New York Eye and Ear Infirmary of Mount Sinai (NYEE) in 2016 under her co-direction, now in place at seven primary care sites across the Mount Sinai Health System, has uncovered growing numbers of previously undiagnosed cases of diabetic retinopathy and other pathologies—particularly glaucoma and age-related macular degeneration—in patients undergoing their physicals. According to a review of the model program from 2018 to 2022, nearly 15 percent of the 1,313 images taken in six participating doctors’ offices showed various stages of diabetic retinopathy. Moreover, 12.3 percent of those images also showed clinically significant macular edema, 9.8 percent showed glaucoma, and 8.1 percent revealed maculopathy.
“We are expanding teleretinal imaging throughout the Health System based on its success to date,” says Dr. Gupta, a vitreoretinal surgeon and Co-Director of Teleretinal Imaging. “When our imaging detects diabetic retinopathy, macular degeneration, or an optic nerve concerning for glaucoma, we notify the patient’s primary care doctor with recommendations for follow-up with an ophthalmologist.”
As of August 1, 2023, the teleretinal screening program, which provides for fundus cameras operated by trained medical personnel at each participating site, has evaluated more than 3,500 patients. The nonmydriatic images taken of the back of the eye are then securely transmitted to Dr. Gupta for later reading. While the program was originally targeted at diabetic patients at high risk for diabetic retinopathy, its lens is now widening to include other ocular disorders.
“As the program progresses,” reports Dr. Gupta, “we are finding there is much more pathology that we are able to capture, and hopefully at a stage where early intervention can prevent the patient’s condition from worsening.”
Beyond the growing caseload, what Dr. Gupta finds encouraging is the positive reception the program has received from the primary care community. “Providers are coming to us and requesting the program for their offices,” she notes. “An additional 30 sites could be onboarded in the near future across the metropolitan area.”

Another exciting prospect on the horizon for teleretinal imaging is artificial intelligence (AI). This unfolding technology has the potential to transform the program by using its algorithmic power to interpret fundus photographs at the point of care, providing immediate
feedback to both providers and patients. The huge advantage is that if an abnormality is detected, an appointment with an ophthalmic specialist can be arranged before the patient leaves the office and is potentially lost to the system.
At present, AI only has Food and Drug Administration approval for use in diagnosing diabetic retinopathy. Technology needs to catch up to what the trained human eye can do. The ideal scenario for Dr. Gupta would be development of an algorithm with diagnostic ability to capture multiple pathologies.
“AI will definitely have a role in this program,” she advises. “We are now setting up the framework for that to happen, but we do not want to rush into it. We want to make sure we are using AI in the most responsible way for our patients.”
Alon Harris, PhD, FARVO, has a passion for uncovering the various causes of glaucoma that has led him to turn his investigative lens on such off-thebeaten-track domains as vascularity, disc hemorrhage, blood pressure, and low perfusion pressure. His latest study, supporting low intracranial pressure (ICP) as a potential player in the pathophysiology of normal-tension glaucoma, has major implications for the development of biomarkers that could potentially fl ag the disease well before it advances and robs patients of their sight.
Though not the first to link reduced ICP to the development and progression of glaucoma, Dr. Harris, Professor of Ophthalmology, and Artificial Intelligence and Human Health, at the Icahn School of Medicine at Mount Sinai, is one of the first to show its correlation to visual field zones through noninvasive measurement in humans. To that end, his work is helping to dispel controversy over the relationship between ICP and changes within the visual field, the long-held standard for glaucoma testing.
“The fact that high intraocular pressure (IOP) is the only approved indication for treating glaucoma doesn’t negate the fact that other risk factors are at play, such as ICP, which represents an opposing pressure to IOP on the optic nerve,” explains Dr. Harris, senior author of the study published in the January 2023 issue of Diagnostics. “My lab has been exploring these alternative risk factors to show that glaucoma is a multifactorial disease, bringing us closer to treatments tailored to individual patients.”

Science has increasingly focused on IOP and, more specifically, the translaminar pressure differential (TPD)— the difference between IOP and ICP—as having a key mechanistic role in glaucoma. The New York Eye and Ear Infirmary of Mount Sinai-led team, which included scientists from the Lithuanian University of Health Sciences, found statistically significant correlations between ICP, TPD, and visual field parameters. These results supported their hypothesis that, in addition to elevated IOP, decreased ICP
could also account for earlier and deeper defects in the nasal visual field zone, where evidence of glaucoma is often first detectable. This pressure differential may lead to the injury of retinal ganglion cells, whose loss or degeneration is a hallmark of glaucoma.
“What makes our project unique is coupling ICP with the average pattern deviation scores of the visual field zones, particularly nasal, in normal-tension glaucoma,” notes Dr. Harris. “This becomes important when you consider that patients with normal-tension glaucoma don’t necessarily have elevated IOP. Therefore, if their ICP is found to be low, we could start to aggressively treat them to lower their IOP, knowing there is an interplay between the two pressures.”
Dr. Harris, who is also Vice Chair of International Research at The Mount Sinai Hospital, acknowledges that a biomarker for normal-tension glaucoma is on his lab’s radar. It will draw on advanced mathematical modeling and machine learning as part of a strategy to identify modifiable risk factors beyond IOP.
“In some patients there is a genetic predisposition to glaucoma, which makes them more prone to factors related to vascularity and perhaps ICP,” says Dr. Harris, who was among the first to show that low blood pressure and perfusion pressure are risk factors for glaucoma. “We’re now looking at these factors in combination with genetic screening to determine how they interact with one another to help us predict disease progression and the most effective treatment for glaucoma on a patient-by-patient basis.”
No physician would advise patients to take up cigarette smoking. But some curious anomalies exist in the medical literature: For example, smoking is associated with a reduced risk of Parkinson’s disease. And despite all the free radicals and carcinogens in cigarette smoke, it is hard to find evidence that smoking is adversely associated with glaucoma. Some studies even hint at an inverse relation between smoking and primary open-angle glaucoma (POAG).
One such recent study was conducted by a New York Eye and Ear Infirmary of Mount Sinai (NYEE) team led by Louis R. Pasquale, MD, Deputy Chair for Research, and Director of the Mount Sinai/New York Eye and Ear (NYEE) Eye and Vision Research Institute at the Icahn School of Medicine at Mount Sinai. For the first time, scientists took a genetic approach to describing the relationship between tobacco smoking and glaucoma to gain new insights into a disease whose pathogenesis is still largely unknown.
“We used publicly available genetic data sets to answer the question: Is there a shared genetic architecture between smoking and glaucoma-related traits?” says Dr. Pasquale, senior author of the study published in the February 2023 issue of Translational Vision Science & Technology. “We found a modest inverse relationship between the genes that predispose someone to smoke and clinically determined open-angle glaucoma (OAG) and intraocular pressure (IOP). It’s a finding no one wants to believe because of the bias that smoking should be bad for glaucoma.”
Tobacco smoking is a known risk factor for age-related cataract formation, thyroid eye disease, and age-related macular degeneration. But prior observational studies have shown conflicting evidence of a relationship between smoking and OAG. One such investigation showed an inverse trend, approaching statistical significance, between increased packyears of smoking and incident POAG, though findings from the American Academy of Ophthalmology Intelligent Research in Sight Registry suggested that smokers had higher IOP than individuals who had never smoked.
The NYEE study, which analyzed large sets of data from European participants in the Rotterdam Study, sheds new light on the smoking-glaucoma conundrum. The growing body of genetic research has uncovered genes that can reliably predict smoking addiction. A locus on chromosome 15 encodes a nicotinic acetylcholine receptor that is strongly linked to heavy smoking and nicotine dependence. Interestingly, pilocarpine, an acetylcholine receptor agonist, is one of the first drugs used to treat glaucoma.

After creating a genetic risk score to determine propensity for smoking and analyzing this score in relation to the measured IOP and diagnosed glaucoma, NYEE researchers found a consistent pattern of inverse associations between genetically predicted smoking and glaucoma, and between smoking and IOP levels.
While smoking cessation remains an important ocular and systemic health goal, the study suggests that the inverse relationship between smoking and glaucoma noted in some studies may be mediated by genetic loci that predispose people to smoke in the first place.
But could the shared genetic architecture between smoking and glaucoma reveal new drug targets for the disease? Pointing to one smoking-cessation agent’s, Wellbutrin, association with a reduced risk of glaucoma in two prior studies, Dr. Pasquale plans to probe the shared genes between smoking and glaucoma to see if they might yield clues to other glaucoma therapies.



The team developed two powerful new tools for in vivo delivery of neuronal factors to reprogram glial cells in the retina or the brain after other studies showed the ineffectiveness of a gene transfer approach once deemed highly promising by the field.
Under the leadership of Bo Chen, PhD, Professor of Ophthalmology, and Director of the Ocular Stem Cell Program at the Icahn School of Medicine at Mount Sinai, NYEE has been in the vanguard of the gene transfer therapy movement, which is different from the equally robust field of stem cell transplantation into the host.
His team, fueled by a $2 million grant from the McGraw Family Foundation, was among the first to demonstrate how adeno-associated viruses (AAVs) could be used to deliver neuronal factors to glial cells—including astrocytes in the brain and Müller glia in the retina—to reprogram those cells into neurons. Mouse model studies have shown that glia-to-neuron conversion can replenish lost neurons, repair damaged neural circuits, and, ultimately, restore functionality.
A major hitch recently developed, however, in this otherwise encouraging picture. Several studies found serious deficiencies in the use of AAV-mediated delivery of Neurod1. The problem was that neuron generation through this transcription factor was not originating in the glial cells, as it should have, but in the neurons themselves due to “leaky expression” by the AAV, and that this failure was not just common to Neurod1, but to other reprogramming factors.
“The danger is not only that AAV-mediated neuronal leakage can lead to misinterpretation of the data from glia-to-neuron conversion, but worse, it can drastically decrease reprogramming efficiency,” notes Dr. Chen. “That’s why it became of paramount importance for us to develop AAV-based gene transfer tools for highly specific delivery of neuronal programming factors that would enable us to study glia-derived neurogenesis without leaky expression into neurons.”
As described in the March 2023 issue of eBioMedicine , while Dr. Chen and his team found that leakage cannot be completely eliminated, the two new AAVdriven gene transfer systems they developed have proven to be extremely versatile and effective. They are able to deliver a range of programming factors, and combinations of factors, to glial cells in the retina and brain, with significantly reduced leakage. What’s more, these tools are widely available to the scientific community.
“Our latest research has given us valuable insights into how to make gene transfer therapy work more effectively, and we’re already using these new tools to improve programming efficiency in our new studies,” says Dr. Chen. “At the same time, we’re helping to advance the entire field of glia reprogramming and are more confident than ever that this work will eventually lead to the restoration of neural function in the retina and brain of humans.”
In July, Dr. Chen carried that buoyant message to his peers in China, where he was invited to address the 16th Annual Meeting of the Chinese Neuroscience Society. Present at that conference were noted scientists from China, Japan, and South Korea, as well as other academic institutions around the world.
Retinal regeneration of glial cells to potentially restore vision in people with glaucoma, macular degeneration, and other degenerative disorders is a red-hot field, and new findings from Mount Sinai/New York Eye and Ear (NYEE) Eye and Vision Research Institute scientists are helping to fuel that research.
Ophthalmologists have long agonized over how best to identify early warning signs of glaucoma, knowing they could provide the elusive key to diagnosing and derailing the progression to vision loss from the obstinate disease that afflicts more than 80 million people globally.
A new study from New York Eye and Ear Infirmary of Mount Sinai (NYEE) offers considerable hope. Researchers showed that measuring changes to flavoprotein fluorescence (FPF) in the optic nerve of people at various stages of glaucoma could set the stage for a critical new prognostic tool to potentially head off glaucoma before it can cause cell loss and structural damage to the optic nerve—damage that remains irreversible.
Mitochondria—the energy powerhouses of cells— produce FPF when they are stressed, and recent studies have suggested that dysfunction of mitochondrial proteins may be at the mechanistic root of glaucoma. Tellingly, FPF levels are elevated in people with glaucoma, especially in its early stages, and recede when mitochondrial oxidative stress is relieved by medication or surgery.
“The better we become at identifying early or ongoing degeneration to the optic nerve, the more proactive we can become at implementing protective therapy,” says Richard B. Rosen, MD, Vice Chair and Director of Ophthalmology Research at NYEE, and senior author of the study, published in the July/ August 2022 issue of Ophthalmology Glaucoma
“Our study is the first to show that FPF may be an important objective measure for predicting glaucoma progression at an early stage, compared to measuring structural damage at the optic nerve head after it’s occurred.”
Glaucoma is a group of optic neuropathies characterized by the degeneration and loss of retinal ganglion cells. Early diagnosis remains key to preventing progression and blindness since patients typically remain asymptomatic until late in the disease process, after irreversible damage has set in. Starting intervention early has been shown to improve treatment efficacy and long-term outcomes.
Flavoprotein fluorescence, for its part, could serve as an important biomarker and valuable supplement to intraocular pressure (IOP), retinal nerve fiber layer thickness, and visual field integrity, the standard parameters for detecting glaucoma. FPF could have particular utility for identifying disease status in patients without elevated IOP. This category includes the many patients with normal- or low-tension glaucoma who have pressures that fall within the normal range.
For their cross-sectional study, NYEE researchers used the OcuMet Beacon, a fundus camera with special filters that isolate fluorescence, to image and analyze 86 eyes, 50 with primary open-angle glaucoma and 36 with no disease. “Our findings showed the presence of mitochondrial dysfunction at the optic nerve head rim of eyes with glaucomatous damage, and that the degree of FPF corresponds to disease severity,” explains Dr. Rosen. “That suggests that FPF could serve as a reliable metabolic marker of disease status. Moreover, because the technology we used provides a quick and noninvasive snapshot of the eye, it could
potentially be a way to monitor the patient’s response to therapy over time, and to characterize the efficacy of neuroprotective therapies for glaucoma.”












While those observations are currently hypotheses, Dr. Rosen hopes to give them substance through his ongoing research with an even more advanced version of OcuMet Beacon, developed by



OcuSciences, Inc. “Through this imaging technique, we might be able to say to a patient, ‘Your FPF is up, so we need to add neuroprotective agents, or we may need to start you on therapies to reduce your pressure, even though it’s now considered normal,’” he elaborates. “This is a very exciting prospect, because for the first time, it would enable us to intervene before, and not after, the fact.”












































 Dr. Smith
Dr. Smith
As New York Eye and Ear Infirmary of Mount Sinai (NYEE) increasingly focuses on ocular health at the population level, no research takes on greater importance than that of R. Theodore Smith, MD, PhD, Professor of Ophthalmology at the Icahn School of Medicine at Mount Sinai, who has established an indelible pathway between high-risk cardiovascular disease and age-related macular degeneration (AMD).
By expanding that knowledge in two recently published studies, Dr. Smith hopes to set the stage for large-scale screening programs that could involve ophthalmologists, cardiologists, and primary care physicians cross-testing for potentially life-threatening heart disease as well as AMD, the leading cause of blindness.
“Screening for vascular diseases through inexpensive retinal imaging could make a significant contribution to public health and save lives,” says Dr. Smith, Director of Biomolecular Retinal Imaging at NYEE. “Likewise, screening patients with known cardiac abnormalities for unrecognized AMD could lead to early diagnosis and potentially sight-saving treatment.”
Dr. Smith’s latest findings demonstrate that two distinct disease pathways—drusen beneath the retinal pigment epithelium and subretinal drusenoid deposits (SDDs) above it—may contribute to early AMD, but that only a single pathway identified on retinal imaging, SDD, can be linked to high-risk vascular disease. In one of those studies, published in November 2022 in BMJ Open Ophthalmology , Dr. Smith’s team looks at a larger patient population than in previous studies to identify specific forms of heart disease—including cardiac valve and myocardial defects, and stroke/transient ischemic attack—that are associated with SDDs.
“What these diseases have in common is diminished circulation, or blood flow, to the eye,” explains Dr. Smith, the study’s senior author. “The carotid artery is a good example. We’ve demonstrated how a plaque obstruction to flow in the carotid artery produces SDDs on the same side of the blockage—a strong proof of principle that reduced blood flow to the eye is the cause of SDDs. In addition to ocular damage, the plaque blockage can also cause stroke.”
These breakthrough findings were presented by Dr. Smith at the American Society of Retina Specialists’ annual meeting at the end of July. Another discovery from his body of work—done in collaboration with the stroke and cardiovascular medical teams at Mount Sinai—was that a heart valve defect (such as mitral or aortic) could also result in reduced cardiac output and restricted blood flow to the eye, along with the formation of SDDs. This is the first known association of cardiac valve disease and AMD.
In the second study, which appeared in January 2023 in the journal Eye, the team further elucidated the separate drusen and subretinal drusenoid deposit pathways through quantitative autofluorescence, a powerful indicator and classifier of outer retinal pathology. Using ultra-sensitive detectors to study 18 patients with the “dry” form of advanced AMD, scientists learned that the dim fluorescent light emitted in the advanced stages caused by SDDs was consistently twice as bright as those caused by drusen. Combined with prior research, this discovery provides conclusive evidence that two different disease processes occur in AMD, one driven by drusen and the other by SDDs. The drusen process leads to darker fluorescence in the advanced stage, while the SDD process leads to brighter fluorescence, the study reported.
“The good news for patients and ophthalmologists is that both forms of AMD can be identified through standard retinal imaging,” notes Dr. Smith. “That could make it feasible to put an optical coherence tomography machine in a primary care clinic and quickly and inexpensively learn if a patient has drusen or SDDs—critical knowledge for the treatment of AMD. If the scan shows SDDs, the patient could also be warned by the physician that they may have an undetected and potentially life-threatening heart condition that needs to be evaluated and treated. This is particularly important information for women and underserved populations whose cardiac symptoms are frequently ignored.”
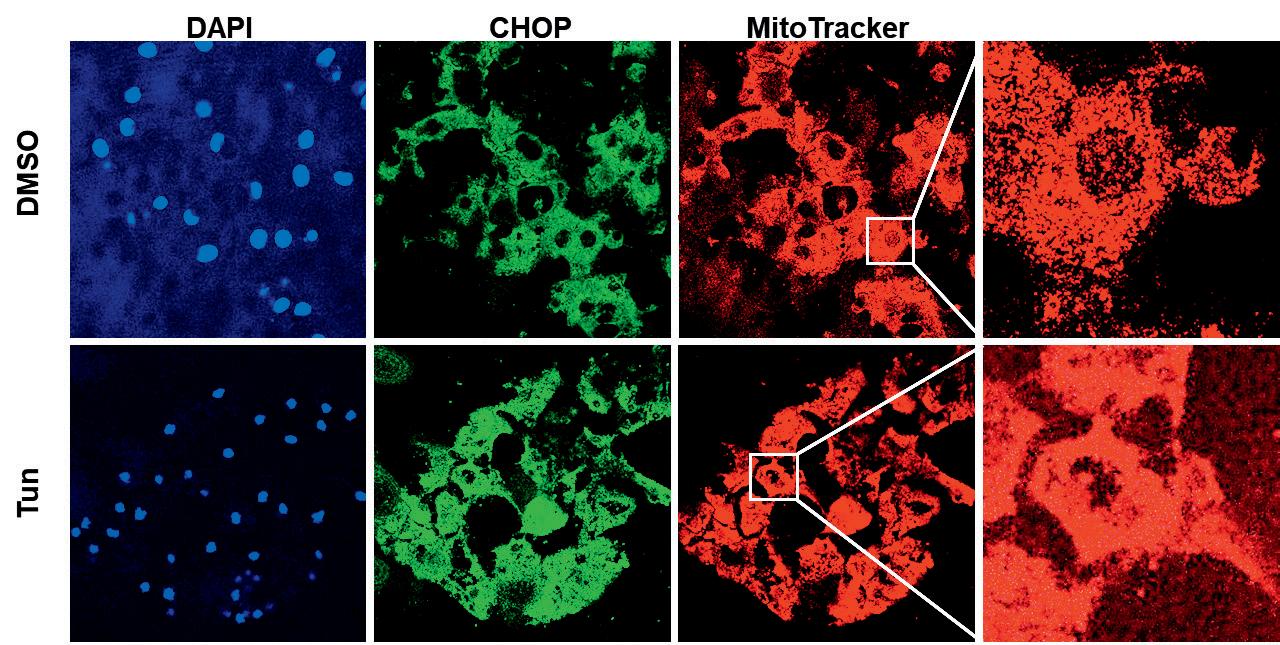
Common across an array of cor neal diseases is a littleunderstood phenomenon known as “crosstalk” that occurs between two organelles within the cells: the endoplasmic reticulum (ER) and the mitochondria. The way these components respond to intracellular stress could be pivotal to the death of corneal endothelial cells and a major contributor to such ocular pathologies as Fuchs’ endothelial corneal dystrophy (FECD), which affects 4 percent of the population in this country over 40, as well as age-related macular degeneration, retinitis pigmentosa, glaucoma, and diabetes retinopathy.
A team of scientists from the Mount Sinai/New York Eye and Ear (NYEE) Eye and Vision Research Institute is starting to shed valuable light on the pathophysiology of the ERmitochondrial interaction, with implications for not just ocular but neurodegenerative, cardiovascular, and metabolic diseases where crosstalk has also been reported. As part of its ongoing research, the team described for the first time the three proteinsignaling pathways that are activated when ER stress disrupts mitochondrial bioenergetics, resulting in corneal endothelial cell apoptosis.
“We’re moving the field ahead by demonstrating through our models the impact of endoplasmic reticulum stress on mitochondrial dysfunction, and how intraorganellar crosstalk between the two can mediate corneal stress levels,” says senior author Varun Kumar, PhD, Assistant Professor of Ophthalmology, and Pharmacological Sciences, at the Icahn School of Medicine at Mount Sinai. “We plan to screen drugs that target both the ER and the mitochondria, possibly through the inhibition of one of their pro-apoptotic pathways. This pathway has been studied in the past in other diseases, but limited studies about their crosstalk are available for ocular disorders.”
In a separate but related study, the Kumar lab is investigating the potential use of an existing Food and Drug Administrationapproved drug for uveal-type disorders as an ER stress inhibitor, along with several other compounds in phase 1 clinical studies.
Fuchs’ endothelial corneal dystrophy is an age-related disorder with a higher incidence in females. Currently, it is attributed to oxidant-antioxidant imbalance in the cells, along with the independent contribution of mitochondrial or ER stress and genetic factors. The only treatment for FECD is corneal transplantation, a major surgical intervention.
In their investigation, Mount Sinai/NYEE researchers learned that immortalized human corneal endothelial cell line F35T had significantly high induction of pro-apoptotic ER stress markers compared to normal control immortalized human corneal endothelial cell line HCEnC-21T. Treatment of HCEnC-
21T with tunicamycin (an ER stress inducer) activated three major ER stress pathways (PERK-eIF2-CHOP, IRE1-XBP1, and ATF6), disrupted mitochondrial ATP production and oxygen consumption, and induced mitochondrial fragmentation. These effects on mitochondria contributed to corneal endothelial cell death, explains Dr. Kumar, whose interdisciplinary lab draws on a wide range of Mount Sinai resources, including tissue banking and high-throughput screening of potential drug candidates.



Another promising way the vision science team is attempting to understand and eventually harness the mechanisms of ER-mitochondria crosstalk is through the proteins of both organelles, along with their



signaling pathways. Specifically, they are examining the behavior of these proteins at the point of their connecting membranes—about which little is known by science—using animal models to isolate those structures for functional analysis.
“Focusing on these key membranes, which constitute more than half of the cellular content, is an exciting new direction for the field,” notes Dr. Kumar, who joined the Department of Ophthalmology in January 2022. “The hope is to use our findings to uncover new pharmacologic approaches to modulating the membranes—which would represent a huge advance for diseases like Fuchs’ dystrophy.”




Finding that none of the existing retinopexy choices for chandelier scleral buckling appealed to him, Richard B. Rosen, MD, Retina System Chief and Vice Chair, Director of Ophthalmology Research at New York Eye and Ear Infirmary of Mount Sinai (NYEE), came up with his own refinement.

“Cryotherapy disperses retinal pigment epithelial cells, promoting scar tissue, indirect ophthalmoscopic laser is often hampered by visibility during surgery, and conventional insertion of an endolaser is invasive and risks vitreous dragging and new tears,” he explains. “It boiled down to finding a simpler way to achieve retinal adhesion during detachment repairs.”
For Dr. Rosen, that involved on-the-spot modification of an available endolaser probe into a “Chandelier Laser.” This was accomplished by creating a depth-limiting sleeve from an 18-gauge angiocatheter—widely available in operating rooms—and enshrouding the endolaser probe tip to effectively shorten its reach. This would prevent the surgeon from inserting it too deeply into the vitreous cavity, where dragging the gel could cause retinal breaks.
Dr. Rosen deemed the 18-gauge sleeve the ideal size for this application because it easily slides on, gently clings to the shaft without slipping off while the laser is being manipulated, and is too big to penetrate deeper than intended.

“I wanted to avoid invading the vitreous, and a sleeve-
shortened EndoProbe® doesn’t permit the laser to enter any deeper than a conventional chandelier, which has been proven safe for illuminating scleral buckling procedures under the operating microscope,” he explains. “This method ensures the surgeon high-quality visualization, safe use of the laser, and the ability to complete the procedure entirely under the surgical microscope.”
In a pilot study reported in the May 2023 issue of Journal of VitreoRetinal Diseases, the first six patients operated on with the technique had successful outcomes following primary scleral buckling for retinal detachment repair. After two months, the retina remained attached in each patient without postsurgical complications.

The ideal patient, says Dr. Rosen, is a young individual with inferior retinal detachment where the lens is clear and there are no visibility issues. “For this type of patient, the procedure is lens-sparing and doesn’t accelerate cataract formation because it’s performed externally without significantly disturbing the vitreous or risking injury to the lens,” he notes.
The “Chandelier Laser” was well received by surgeons at a recent American Society of Retinal Specialists conference in Seattle, where Dr. Rosen presented it, and several of his colleagues at NYEE are starting to use it. “The method is simple, safe, and straightforward,” he emphasizes, “and ease of assembly of the plastic sleeve from 18-gauge angiocatheters commonly found in the operating room makes it readily available for surgeons to try.”
Even a technique that has been successfully employed since the 1950s and is considered a gold standard for ophthalmic surgery can be improved. Case in point: scleral buckling for retinal detachment repair.



is the secret sauce of successful surgery.—Richard Rosen, MD
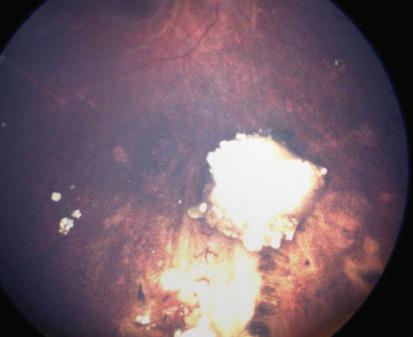
After diagnosing a three-year-old boy with unilateral retinoblastoma in the right eye, Ekaterina Semenova, MD, PhD, an ophthalmologist and surgeon with the Ocular Oncology Service at New York Eye and Ear Infirmary of Mount Sinai (NYEE), presented the mother with two options. One was removal of the cancerous eye, the other was preserving it by delivering a chemotherapeutic agent directly to the tumor site through intra-arterial chemotherapy (IAC).
There was little question in the mind of the mother or surgeon over which course to pursue. And in August 2022, NYEE teamed up with the Mount Sinai Pediatric Cerebrovascular Program to become one of the few institutions in the New York-metropolitan area to treat retinoblastoma, the most common type of eye cancer in young children.
“We now have in place a highly skilled multidisciplinary team to provide this specialized service, including ophthalmology, neuroendovascular surgery, pediatric oncology, radiology, and anesthesiology,” says Dr. Semenova, Assistant Professor of Ophthalmology at the Icahn School of Medicine at Mount Sinai, who proposed starting a retinoblastoma service after joining the department in October 2021, and received strong support from NYEE leadership. “We’re now treating our second patient and as people become more aware of this service, we believe the demand will grow.”
The success of the first young patient is cause for encouragement. Dr. Semenova, who led the multidisciplinary team, discovered the tumor (nearly 10 millimeters in thickness) arising in his retina, and recommended a two-part course of treatment. It consisted of intra-arterial chemotherapy done by Johanna Fifi, MD, a neuroendovascular surgeon and Professor of Neurosurgery, Neurology, and Radiology at Icahn Mount Sinai, to target the tumor, followed by a
series of intravitreal chemotherapy injections by Dr. Semenova to eliminate the tumor seeds floating in the vitreous.
“The child’s tumor was very large, which ruled out such alternative forms of eye-salvaging treatment as cryotherapy, thermotherapy, and plaque radiation therapy. External beam radiation is very rarely used now because it can cause secondary cancers and disfigurement of the face,” explains Dr. Semenova. “The field has been moving to intra-arterial chemotherapy over the past 15 years, and we judged it to be the most appropriate choice for this patient.”
Dr. Fifi delivered the first of three rounds of the chemotherapeutic agent melphalan, spaced a month apart, directly to the tumor site, working with a Mount Sinai neurointerventional team that included a pediatric anesthesiologist. This required gaining access through the femoral artery and snaking a microcatheter into the carotid and then the ophthalmic artery using X-ray guidance. “Because we were directly hitting the tumor, we could inject a lower dose of chemotherapy than if we used [conventional] intravenous chemotherapy, thus avoiding the use of multiple agents with greater toxicity,” notes Dr. Fifi, who is the Associate Director of the Cerebrovascular Center at Mount Sinai and Co-Director of the Pediatric Cerebrovascular Disorders Program at
Mount Sinai Kravis Children’s Hospital. “In the case of this young patient, the outcome was terrific. His tumor shrank with each treatment and was completely inactive after a few months.”
But intra-arterial chemotherapy alone was insufficient to eradicate the cancer. It left largely untouched the vitreous seeds, which threatened to grow within the gel inside the eye if not properly treated. This is where Dr. Semenova’s training and knowledge proved critical. Soon after Dr. Fifi completed her work, Dr. Semenova began a regimen of three intravitreal chemotherapy injections over several months, requiring use of a special technique to prevent cancerous cells from growing. “When I injected the chemotherapy, I performed cryotherapy at the same time around the needle to keep the tumor cells frozen in place when the instrument was withdrawn from the vitreous,” she says.

During Dr. Semenova’s examinations of the patient following the last procedure in February 2023, the success of the injections was clear. “The vitreous seeds were gone, along with the tumor, and a retinal detachment we initially found also disappeared,” she observes. And while the child’s sight out of the affected right eye was only 20/250—slightly worse than prior to surgery— there was a more significant outcome to be weighed. “We preserved the boy’s eye and his vision,” says Dr. Semenova. “And six months out, there is no sign of cancer. We look upon these as major successes.”



In the case of this young patient, the outcome was terrific. His tumor shrank with each treatment and was completely inactive after a few months.
—Johanna Fifi, MDFigure 3: X-ray showing delivery of intra-arterial chemotherapy agent. The red arrow is showing the microcatheter tip in place and blue arrow is pointing to dye in the ophthalmic artery.

Julia Fallon, MD, a retina fellow at New York Eye and Ear Infirmary of Mount Sinai (NYEE), likes to think of each surgery as a work of art, combining elements from her extensive surgical training in unique ways to meet the needs of each patient.

That mindset served her particularly well when she recently teamed up with volunteer faculty instructor Alexander Barash, MD, to perform surgery for the dislocated lenses in both eyes of a patient with Marfan syndrome (MFS), a serious complicating factor. “We had to treat his eyes differently than most secondary lens cases because his anatomy was so different,” Dr. Fallon explains. “We had to really think the case through and make important changes, like how far back in the eye to position the lens, as the surgery progressed. In addition, the removal of the displaced lens and surrounding vitreous gel had to be performed with extreme care due to the high risk of retinal detachment in patients with this connective tissue disorder.”
Perhaps the boldest stroke by these two highly skilled ophthalmologists was the decision to use a procedure known as the Yamane technique for scleral fixation of intraocular lenses. This eloquent surgical procedure was the perfect remedy for a patient whose lens implant could not be supported by the capsular bag, which had completely separated from its attachment to the wall of the eye as a result of the patient’s underlying condition. This technique, brought to NYEE about six years ago by Dr. Barash, indeed proved a masterstroke for the patient, Dean Klingler. Weeks after the completion of the second procedure on his left eye, he described the “miracle” of seeing for the first time road signs and other distant objects without the need for very thick glasses.
The ordeal began for Mr. Klingler, 57, on a Sunday morning in January 2023 when he woke up with blurry vision in his right eye. “It continued to get worse during the day,” he recalls, “and I finally walked over to the eye clinic at New York Eye and Ear, just four blocks from my apartment. Through providence or good luck, I wound up going to the best place in the field.”
Residents staffing the clinic found that the dislocated lens was blocking Mr. Klingler’s pupil, preventing
aqueous fluid circulation and drainage from the eye, which caused his intraocular pressure to be 60 mm/Hg, three times the normal amount and risking blindness if not urgently addressed. This was particularly troublesome when coupled with his MFS, a genetic condition that produces aberrant elastic fibers throughout the body, including in the aorta and the zonules—the suspensory ligaments attaching the lens within the eye, which become stretched out, and over time can rupture, leading to lens dislocation. Dr. Barash, who saw the patient during his repeat visits to the downtown clinic, sought to bring the pressure down with eye drops and oral medications. “Given the patient’s history of major heart surgery, we wanted to make sure he had appropriate clearance from his cardiologist before retinal surgery to ensure his safety,” says Dr. Barash, who maintains a private practice in Manhattan in addition to his volunteer work training residents and fellows at the Bendheim Family Retina Center at NYEE, as well as Elmhurst Hospital Center in Queens, a Mount Sinai affiliate.
For the first of the two surgeries on January 24, Dr. Barash asked Dr. Fallon, who was on duty that day, to assist. It was a fortuitous pairing since both had performed the Yamane technique many times, often together. The dislocated lens was removed with vitrectomy but there was no zonular support for a new intraocular lens. The Yamane technique was the ideal

option to fixate the new lens, as the sclera was thin in this long MFS eye, and suture-based fixation can erode through the sclera with time and cause the new lens to fall out of position. Similarly, the iris can also be thinned in patients with MFS and the lens would be similarly unstable affixed to the iris.


The Yamane technique, which requires considerable training, involves using a tiny corneal incision to insert the new lens. In order to affix the lens to the sclera to ensure its long-term stability, two 30-gauge needles housing the lens haptics were inserted through the sclera, creating a tunnel in which the haptic arms could rest. When the surgeons withdrew the needles, the haptics remained and became anchored in those scleral tunnels. The surgeons then cauterized the protruding ends of each haptic to fashion flanges that prevented the arms from slipping back into the eye.

While the surgery was a success, it was in a sense a tune-up for the analogous second operation six months later on the left eye. “I learn a little bit from each case, but probably more from this one because of the uniqueness of his anatomy,” acknowledges Dr. Fallon. The abnormal size and shape of Mr. Klingler’s eyes due
to the MFS meant that the normal anatomical structures were stretched and acted differently. That awareness served her and Dr. Barash well on the follow-up surgery when they revised critical aspects of the procedure, such as moving the intraocular lens back a half-millimeter from the 2.5 mm of the first. “We made a lot of adjustments,” confirms Dr. Barash, “because of the configuration of the eye where everything was floppy and worked differently.”
To the surgeons’ satisfaction, the second procedure was even smoother than the first. Validation came from the patient himself, whose intraocular pressure returned to normal in the following weeks, while his vision without glasses or contacts improved substantially to 20/30.
“I can’t believe how perfect my vision is now,” exclaims Mr. Klingler, a fundraiser for a nonprofit environmental organization. “There were certainly more than a few sleepless nights when I was wondering whether I would ever see well again. You could say I was lucky enough to find doctors at the top of their game.”

The American Academy of Ophthalmology reports that women represent about 30 percent of professionals in the field, a figure that signifies both challenge and opportunity for Women in Ophthalmology, a powerful collective of women ophthalmologists focused on cultivating the next generation of women leaders in their field.
“In general, we see gender inequality, especially in the surgical fields, but we’re fortunate in ophthalmology to be closing the gap,” says Nisha Chadha, MD, Associate Professor of Ophthalmology and Director of Medical Student Education, Icahn School of Medicine at Mount Sinai, and President since 2021 of the New York City group of Women in Ophthalmology. “We still have some way to go, though.”
As she further acknowledges, the pathway lies in greater voice and visibility, twin goals that have helped animate members of New York City Women in Ophthalmology (NYCWIO), including about a dozen faculty members, residents, and medical students from New York Eye and Ear Infirmary of Mount Sinai (NYEE). “We’re fortunate to be in a city that has so many amazing institutions and women in practice, and by bringing us together, we’re able to generate mentoring opportunities and help to recruit more women into our field,” Dr. Chadha asserts.
Monica Dweck, MD, Associate Professor of Ophthalmology at Icahn Mount Sinai and a founding member of NYCWIO 17 years ago, echoes that thought.
“It’s a chance for women ophthalmologists to network with other women from around the city, and that support system has been very helpful to us as we go through our careers,” she observes, adding that some individuals have secured fellowships and jobs through their association with the group.

Dr. Chadha sees recruiting more women to the field as the greatest accomplishment of the chapter, whose members include not just women from academic institutions across the city, but those in private practice as well as residents and medical students. “Our chapter is heavily focused on the recruitment of trainees and medical students, and on providing a network that empowers them to grow along whatever path they’ve chosen,” says Dr. Chadha. “They might not recognize the opportunities that are out there, so seeing women who have succeeded professionally can certainly be an inspiration to them.”
In addition to Drs. Chadha and Dweck, other NYEE faculty members on the board of NYCWIO are Tania Tai, MD, Vice Chair of Clinical Operations and Director of Microsurgical Education, Department of Ophthalmology; and Tamiesha Frempong, MD, MPH, Vice Chair of Diversity and Inclusion, Department of Ophthalmology, Icahn Mount Sinai, and Assistant Director of the Ophthalmology Residency Program at the Mount Sinai-affiliated Elmhurst Hospital in Queens.
NYEE is designated a “High Performing” Hospital for Ophthalmology by U.S. News & World Report® for 2023-2024
Industry clinical trials and federally funded clinical research projects

Dr. Chen is a recipient of the 2023 United Hospital Fund’s Excellence in Health Care Award, honoring extraordinary personal leadership to improve quality of care, patient safety, and patient experience. Dr. Chen joined the Icahn School of Medicine at Mount Sinai in 2021 as an Assistant Professor of Ophthalmology. She is the Director of the Comprehensive Ophthalmology Clinic, and an Associate Program Director for the Ophthalmology Residency at NYEE.
Mr. Loiacono is the newly appointed President of the Association of University Professors of Ophthalmology (AUPO), Administrators Council. Founded in 1966, AUPO has been the voice of academic ophthalmology, dedicated to research and education. As president, Mr. Loiacono, who has been a member of AUPO for more than a decade, will continue the legacy of advocating for ophthalmology administrators across the country. His first priorities are planning the annual meeting and working with the board of trustees on reimagining AUPO’s mission, vision, and strategy for the future. Mr. Loiacono is Vice President of Ophthalmology Services and Deputy Chair of Administration and Finance for the Department of Ophthalmology at NYEE and the Mount Sinai Health System.


Dr. Pasquale received the 2023 Robert Ritch Award for Innovation and Excellence in Glaucoma from The Glaucoma Foundation in recognition of his outstanding work focused on the discovery of primary prevention strategies in open-angle glaucoma. He was also recognized in the International Glaucoma Review’s first global survey of Glaucoma Impact, which listed Dr. Pasquale fourth in the world based on Expertscape rankings. An internationally recognized leader in clinical ophthalmic research, Dr. Pasquale focuses his work on highlighting the environmental risk factors for exfoliation syndrome and uncovering the complex genetic architecture of primary open-angle glaucoma. Dr. Pasquale joined Mount Sinai in 2018. He is the Shelley and Steven Einhorn Distinguished Chair in Ophthalmology at NYEE, Chair of Ophthalmology at The Mount Sinai Hospital and Mount Sinai Queens, Deputy Chair for Research for the Department of Ophthalmology, Director of the Mount Sinai/New York Eye and Ear (NYEE) Eye and Vision Research Institute, and Co-Director of the Center for Ophthalmic Artificial Intelligence and Human Health at Icahn Mount Sinai.
The Macula Society recognized Dr. Rosen’s longstanding commitment and contributions to retinal research with the 2023 Paul Henkind Memorial Lecture and Award. An internationally renowned investigator and lecturer, he pursues research interests, including new treatments for macular degeneration and diabetic retinopathy, along with innovations in diagnostic retinal imaging and vitreoretinal surgical instrumentation. Dr. Rosen joined NYEE in 1989. He is the Vice Chair and Director of Ophthalmology Research at NYEE, Chief of the Retina Service for the Mount Sinai Health System, and the Belinda Bingham Pierce and Gerald G. Pierce, MD, Distinguished Chair of Ophthalmology, Icahn Mount Sinai.

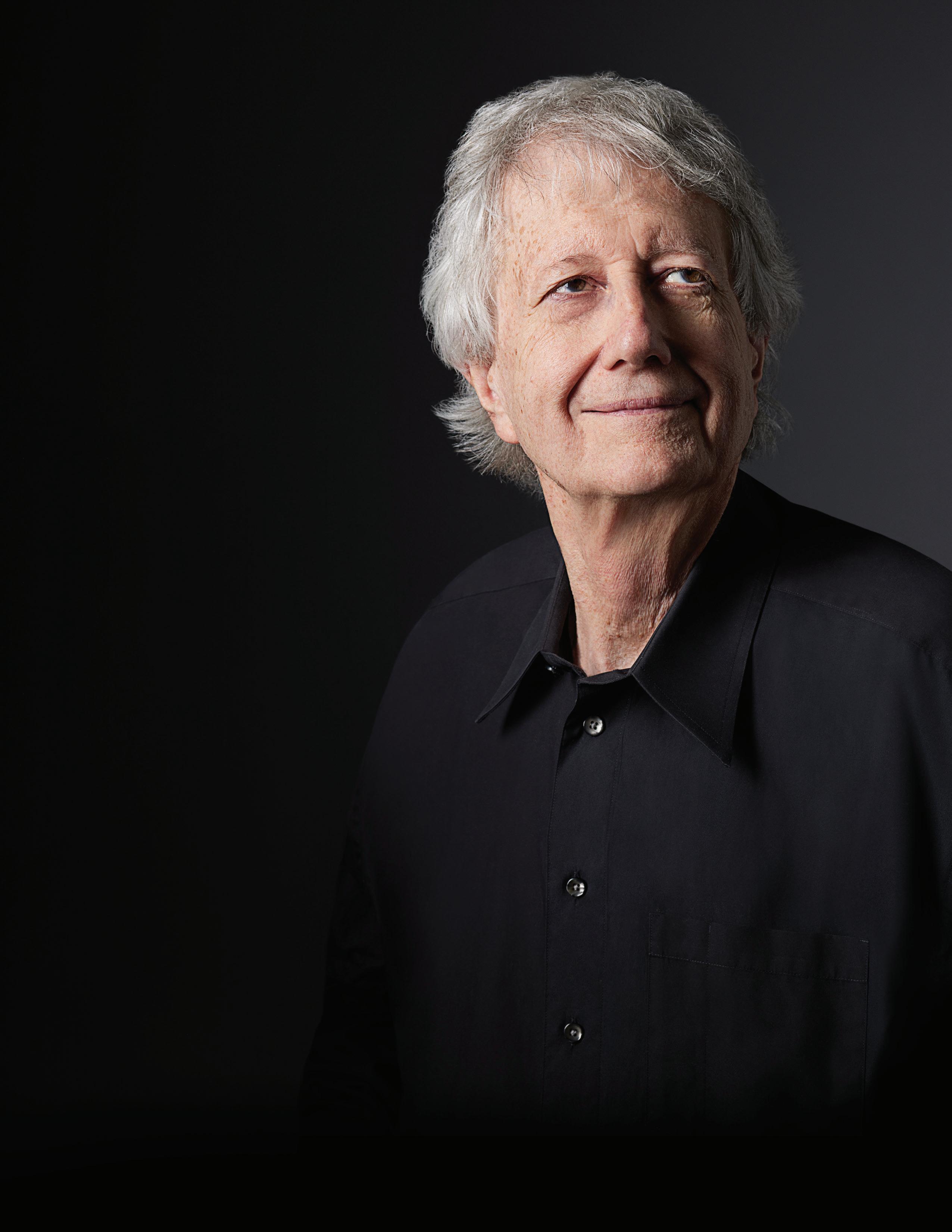
This year, the Department of Ophthalmology said goodbye to an outstanding physician who served Mount Sinai and the New York metropolitan region for 46 years. Dr. Friedman received his medical degree from NYU School of Medicine and continued his training in ophthalmology, followed by a fellowship in ophthalmic pathology at NYU. He was appointed Clinical Professor of Ophthalmology, and Pathology, at the Mount Sinai School of Medicine in 1977. A prolific lecturer at numerous national and international conferences, Dr. Friedman is an author or co-author of more than 200 articles and textbooks, held grants from the National Eye Institute, and was a participant in the Studies of Ocular Complications of AIDS Research Group. In addition to being a member of various ophthalmic societies, he served as president of the Eastern Ophthalmic Pathology Society in 1997 and the American Association of Ophthalmic Pathologists from 1992 to 1994.
We thank Dr. Friedman for his years of service and dedication to the field of ophthalmology, Mount Sinai, and the patients he served.

Dr. Wilkins joins the Department as Assistant Professor of Ophthalmology, Icahn Mount Sinai, with a focus on ocular immunology and uveitis. After completing his residency at Icahn Mount Sinai, Dr. Wilkins pursued dual fellowships in vitreoretinal surgery at NYEE and ocular immunology and uveitis at Wilmer Eye Institute/Johns Hopkins Hospital.

PGY-4
Maria Castanos, MD
Elaine Han, MD
Kyle Hirabayashi, MD
Grant Hopping, MD
Jerry Hsu, MD
Sefy Paulose, MD
Gabriel Shakarov, MD
Daniel Vail, MD
Meena Zakher, MD
PGY-3
Aaron Brown, MD
Chih-Chiun Chang, MD
Ha Min Kim Chang, MD
Allen Costa, MD
Anthony Fam, MD
David Merriott, MD
Devayu Parikh, MD
Jackson Scharf, MD
Khushali Shah, MD
Davis Zhou, MD
PGY-2
Jennifer Drechsler, MD
Jose Omar Garcia, MD
Catalina Garzon Vargas, MD
Andy Huang, MD
Claire Kim, MD
Michael Lai, MD
Oscar Otero, MD
Yash Shah, MD
Benjamin Steren, MD
Amanda Wong, MD
Radames Rios-Gonzalez, MD (Glaucoma)
Julia Fallon, MD (Vitreo-Retina)
Andrew Jin, MD (Vitreo-Retina)
Neal Patel, MD (Vitreo-Retina)
Nilesh Raval, MD (Vitreo-Retina)
James C. Tsai, MD, MBA President, NYEE Chair, Department of Ophthalmology Director, COAIHH Icahn Mount Sinai and MSHS
Louis R. Pasquale, MD, FARVO Chair, Department of Ophthalmology, MSH and MSQ
Deputy Chair for Research, Director, Mount Sinai/NYEE Eye and Vision Research Institute and Co-Director, COAIHH, Icahn Mount Sinai
Paul A. Sidoti, MD Chair, Department of Ophthalmology, NYEE
Deputy Chair for Education, Department of Ophthalmology, Icahn Mount Sinai Chief, Glaucoma, MSHS
Mark Kupersmith, MD Vice Chair, Translational Ophthalmology Research, Icahn Mount Sinai Chief, Neuro-Ophthalmology, MSHS
Richard B. Rosen, MD, FARVO Vice Chair and Director of Ophthalmic Research, NYEE Chief, Retina Service, MSHS
Salvatore Loiacono Jr., MPA Deputy Chair, Finance and Administration, MSHS Vice President of Ophthalmology Services, NYEE
Elizabeth Sellman President and Chief Operating Officer, MSBI and NYEE
Tamiesha Frempong, MD, MPH Vice Chair, Diversity and Inclusion, Department of Ophthalmology, Icahn Mount Sinai
Sandra K. Masur, PhD
Vice Chair, Academic Development and Mentoring, Department of Ophthalmology, Icahn Mount Sinai
Anita Gupta, MD Vice Chair, Professional Development, Department of Ophthalmology, Icahn Mount Sinai
Alon Harris, PhD, FARVO Director, Ophthalmic Vascular Diagnostic and Research Program, MSH Vice Chair, International Research and Academic Affairs, Chair, Promotion and Tenure Committee, Department of Ophthalmology, and Co-Director, COAIHH, Icahn Mount Sinai
Gareth M. C. Lema, MD, PhD Vice Chair, Quality, Safety, and Experience, Department of Ophthalmology, NYEE
Tak Yee Tania Tai, MD Vice Chair, Clinical Operations, Department of Ophthalmology, NYEE
Gennady Landa, MD
Vice-Chair for Clinical Integration of Ophthalmology, Icahn Mount Sinai and MSHS Director, Retina, NYEE
Nisha Chadha, MD
Director, Medical Student Education, Department of Ophthalmology, Icahn Mount Sinai
Tsontcho A. Ianchulev, MD, MPH Director, Ophthalmic Innovation and Technology, NYEE
Sumayya Ahmad, MD Associate Director, Ophthalmology Residency Program, NYEE
Masako Chen, MD Associate Director, Ophthalmology Residency Program, NYEE
Avnish Deobhakta, MD Associate Director, Vitreo-Retinal Fellowship Program, NYEE
Tamiesha Frempong, MD, MPH Assistant Director, Ophthalmology Residency Program, NYEE
Meenakashi Gupta, MD Director, Resident and Fellow Wellness, Department of Ophthalmology, NYEE
Gautam Kamthan, MD Assistant Director, Ophthalmic Innovation and Technology, NYEE Associate Director, Cataract Surgical Training, NYEE
Gennady Landa, MD Associate Director, Vitreo-Retinal Fellowship Program, NYEE
Harsha S. Reddy, MD Director, Ophthalmology Residency Program, NYEE
Richard B. Rosen, MD, FARVO Director, Vitreo-Retinal Fellowship Program, NYEE
Tak Yee Tania Tai, MD Director, Microsurgical Education, Department of Ophthalmology, NYEE
Kateki Vinod, MD Director, Glaucoma Fellowship Program, NYEE
Angie E. Wen, MD Director, Cornea and External Diseases Fellowship Program, NYEE
CLINICAL
Cataract Surgery
Richard Koplin, MD Co-Director, Cataract Service, NYEE
Kira Manusis, MD Co-Director, Cataract Service, NYEE
Sumayya Ahmad, MD
Nisha Chadha, MD
Masako Chen, MD
Anita Gupta, MD
Tsontcho A. Ianchulev, MD, MPH
Gennady Landa, MD
Rachel H. Lee, MD
Neha Shaik, MD
Tak Yee Tania Tai, MD
Angie E. Wen, MD
Cornea, External Diseases, and Refractive Surgery
Anita Gupta, MD Director, Cornea and External Diseases, NYEE
Sumayya Ahmad, MD
Masako Chen, MD Kira Manusis, MD
Neha Shaik, MD Angie E. Wen, MD
Eye Trauma
John Aljian, MD Director, Anterior Segment Trauma Service, NYEE
Ronald C. Gentile, MD Director, Posterior Segment Trauma Service, NYEE
Harsha S. Reddy, MD Director, Oculoplastic Trauma Service, NYEE
Sumayya Ahmad, MD Masako Chen, MD
Mary-Abigail Craven, MD
Avnish Deobhakta, MD
Alberto G. Distefano, MD
Valerie I. Elmalem, MD
Robin N. Ginsburg, MD
Anita Gupta, MD
Meenakashi Gupta, MD
Gennady Landa, MD
Gareth M. C. Lema, MD, PhD
Kira Manusis, MD
Trisha Mor, MD
Richard B. Rosen, MD, FARVO
Neha Shaik, MD
Angie E. Wen, MD
Glaucoma
Paul A. Sidoti, MD Chief, Glaucoma, MSHS
Tak Yee Tania Tai, MD Director, Glaucoma Clinic, NYEE
Nisha Chadha, MD
Donna Gagliuso, MD
Tsontcho A. Ianchulev, MD, MPH
Paul S. Lee, MD
Rachel H. Lee, MD
Louis R. Pasquale, MD, FARVO
James C. Tsai, MD, MBA
Kateki Vinod, MD
Neuro-Ophthalmology
Mark Kupersmith, MD Chief, Neuro-Ophthalmology, MSHS
Rudrani Banik, MD Co-Director, Neuro-Ophthalmology Clinic, NYEE
Valerie I. Elmalem, MD Co-Director, Neuro-Ophthalmology Clinic, NYEE
Mary-Abigail Craven, MD
Alberto G. Distefano, MD
Ocular Oncology
Paul T. Finger, MD Director, Ocular Oncology, NYEE
Ekaterina Semenova, MD, PhD
Ophthalmic Pathology
Jodi Sassoon, MD Chair, Pathology, NYEE
Codrin E. Iacob, MD, FCAP
Oculoplastic, Orbital, and Reconstructive Surgery
Alberto G. Distefano, MD Director, Oculoplastic, Orbital, and Reconstructive Surgery, MSH
Harsha S. Reddy, MD Director, Oculoplastic, Orbital, and Reconstructive Surgery, NYEE Director, Department of Ophthalmology, MSBI
Mary-Abigail Craven, MD
Monica Dweck, MD
Valerie I. Elmalem, MD
Pediatric Ophthalmology and Strabismus
Tamiesha Frempong, MD, MPH
Thomas J. Quehl, MD
Edward Raab, MD
Primary Care Ophthalmology/Optometry
Masako Chen, MD Director, Comprehensive Ophthalmology Clinic, NYEE
Bessie Abraham, OD
Vivien Boniuk, MD
Christina Cherny, OD
Kristina Creadore, OD
Daniel Epshtein, OD
Karen Hendler-Goldberg, MD
Shreya Jayasimha, OD
Lisa Kingsly, OD
Leannza Tang, OD
Retina
Richard B. Rosen, MD, FARVO Chief, Retina, MSHS
Robin N. Ginsburg, MD Director, Retina, MSH
Gennady Landa, MD Director, Retina, NYEE
Nazanin Barzideh, MD
Avnish Deobhakta, MD
Meenakashi Gupta, MD
Gareth M. C. Lema, MD, PhD
Trisha Mor, MD
R. Theodore Smith, MD, PhD
Carl Wilkins, MD
Uveitis and Ocular Immunology
Varun K. Pawar, MD
Carl Wilkins, MD
Basic Science/Translational Research Faculty
Louis R. Pasquale, MD, FARVO Director, Mount Sinai/NYEE Eye and Vision Research Institute, Co-Director, COAIHH, Icahn Mount Sinai
Timothy A. Blenkinsop, PhD
Bo Chen, PhD
Yuen Ping Toco Chui, PhD
Alon Harris, PhD, FARVO
Varun Kumar, PhD Jun Lin, MD, PhD
Sandra Masur, PhD
Richard B. Rosen, MD
R. Theodore Smith, MD, PhD
Jose Mario Wolosin, PhD
Affiliated Leadership
Douglas F. Buxton, MD President, Jorge N. Buxton, MD, and Douglas F. Buxton, MD, Microsurgical Education Fund
Paul S. Lee, MD Chief, Department of Ophthalmology, James J. Peters VA Medical Center President, NYEE/MSH Department of Ophthalmology Alumni Association
Steven Agemy, MD
John Aljian, MD
Rudrani Banik, MD
Alexander Barash, MD
Brett Bielory, MD
Douglas F. Buxton, MD
Anais Carniciu, MD
Gaurav Chandra, MD
Elizabeth Fang, MD
Edmund Farris, MD
Paul T. Finger, MD
John Flanagan, MD
Donald Fox, MD
Seymour Fradin, MD
Ronald C. Gentile, MD
Robyn Horowitz, MD
Jimmy Hu, MD
Lawrence Jacobson, MD
Steven Kane, MD
Yogita Kashyap, MD
Stephen Kronenberg, MD
Kaushal Kulkarni, MD
Jessica Lee, MD
Kerline Marcelin, MD
Amy Mehta, MD
Jeffrey Nightingale, MD
Jai Parekh, MD
Deep Parikh, MD
Alexander Pinhas, MD
Aryeh Pollack, MD
Alexander Rabinovich, MD
Allen Rubin, MD
Edwin Schottenstein, MD
Jonathan Shapiro, MD
Glenn Silbert, MD
Mark Tannenbaum, MD
Theresa Tretter, MD
Cynthia Tung, MD
Eugene Weise, MD
Rebecca Weiss, MD
David Witzel, MD
Sze Wong, MD
Luna Xu, MD
Teaching Faculty at MSH
Alexander Barash, MD
James G. Chelnis, MD
Ben Cohen, MD
Peter Condax, MD
Stella Douros, MD
Jonathan Ligh, MD
Edward Marcus, MD
Emily Moriarty, MD
Joseph Podhorzer, MD
Ravi Raharkrishnan, MD
Alan Sheyman, MD
Teaching Faculty at VA Medical Center
Isaac Ezon, MD
Doris Herzfeld, MD
Paul S. Lee, MD
Gareth M. C. Lema, MD, PhD
Teddy Lyu, MD
Jonathan Schulhof, MD
Steven Teich, MD
Teaching Faculty at Elmhurst Hospital
Alexander Barash, MD
Robert Fischer, MD
Teddy Lyu, MD
Richard Most, MD
Michelle Rhee, MD
Andrew Schwartz, MD
Zinaria Williams, MD
Susan Zoltan, MD
COAIHH
Center for Ophthalmic Artificial Intelligence and Human Health
Icahn Mount Sinai
Icahn School of Medicine at Mount Sinai
MSHS
Mount Sinai Health System
MSH
The Mount Sinai Hospital
MSBI
Mount Sinai Beth Israel
MSM
Mount Sinai Morningside
MSQ
Mount Sinai Queens
MSW
Mount Sinai West
NYEE
New York Eye and Ear Infirmary of Mount Sinai






























