SOLVING KENTUCKY’S GREATEST HEALTH CHALLENGES

WITH A GROWING NUMBER OF TRAINEES ACROSS THE STATE AND OPPORTUNITIES FOR GROUNDBREAKING RESEARCH, THE UK COLLEGE OF MEDICINE HAS DEMONSTRATED WHAT'S WILDLY POSSIBLE.


WITH A GROWING NUMBER OF TRAINEES ACROSS THE STATE AND OPPORTUNITIES FOR GROUNDBREAKING RESEARCH, THE UK COLLEGE OF MEDICINE HAS DEMONSTRATED WHAT'S WILDLY POSSIBLE.
SUMMER INTERNSHIP EXPOSES STUDENTS TO CAREERS IN INDUSTRY
PAGE 04
A YEAR OF GROUNDBREAKING RESEARCH PAGE 14
UK TRAINEES CONNECT WITH THOUSANDS OF PATIENTS AROUND THE WORLD PAGE 18
200+ NEW MEDICAL STUDENTS ACROSS 4 CAMPUSES PAGE 24
Message from leadership
Quick news
Integrated Biomedical Sciences summer internship exposes students to careers in industry, higher education
Cover Story: Strength in Numbers
A year of groundbreaking research
Alliance Research Initiative
UK trainees connect with thousands of patients around the world
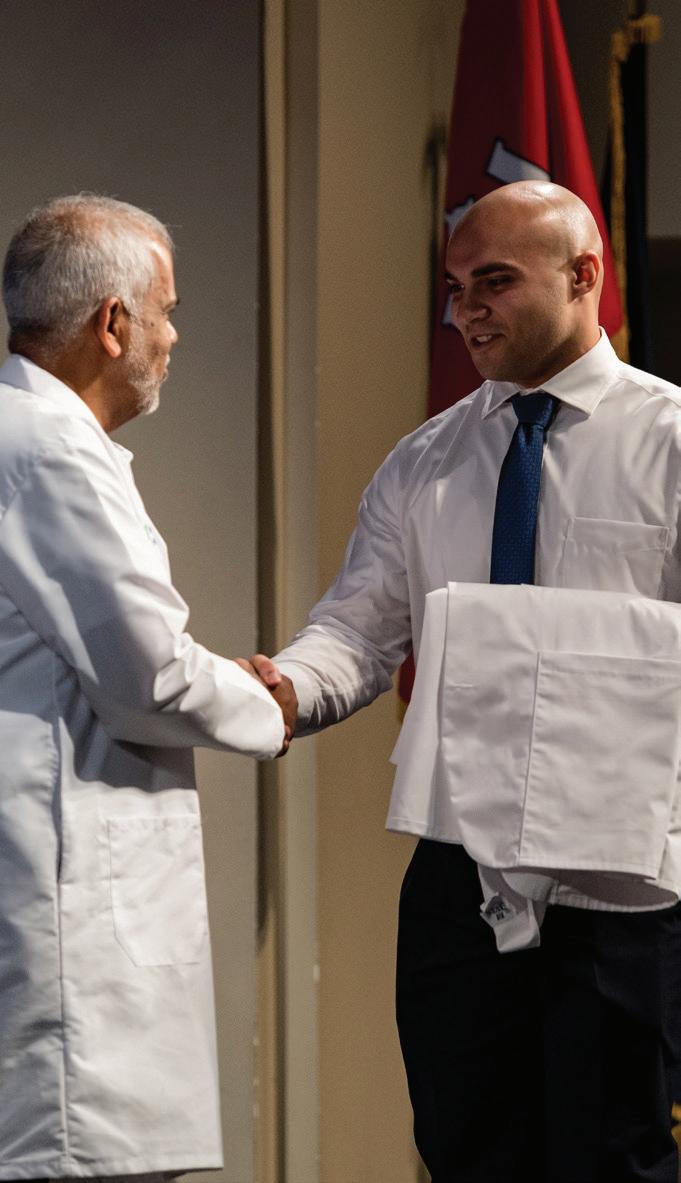
Marking a milestone
White coat ceremony gallery
Gifts that resonate through time MVPE





“Chipper” Griffith III, MD, MSPH Dean, UK College of Medicine

There is strength in numbers, and the proof is in the past year. Our latest statistics demonstrate what I see every day at the University of Kentucky College of Medicine.
To start, our research teams achieved record-setting numbers this year. The College of Medicine received nearly $226 million in funding, our second-highest total recorded. We also saw our highest-ever number of grants awarded (954!) and a growing number of principal investigators (359). These exciting developments are a result of the hard work of our faculty, staff, and trainees, as well as continued investment in research that has grown under the leadership of Vice Dean for Research Becky Dutch, PhD. The Office of Research now supports a faculty and staff research awards program, a faculty research leaders program, the clinicianscientist program, the FORWARRD workforce advancement initiative, and the Research Professionals Network.
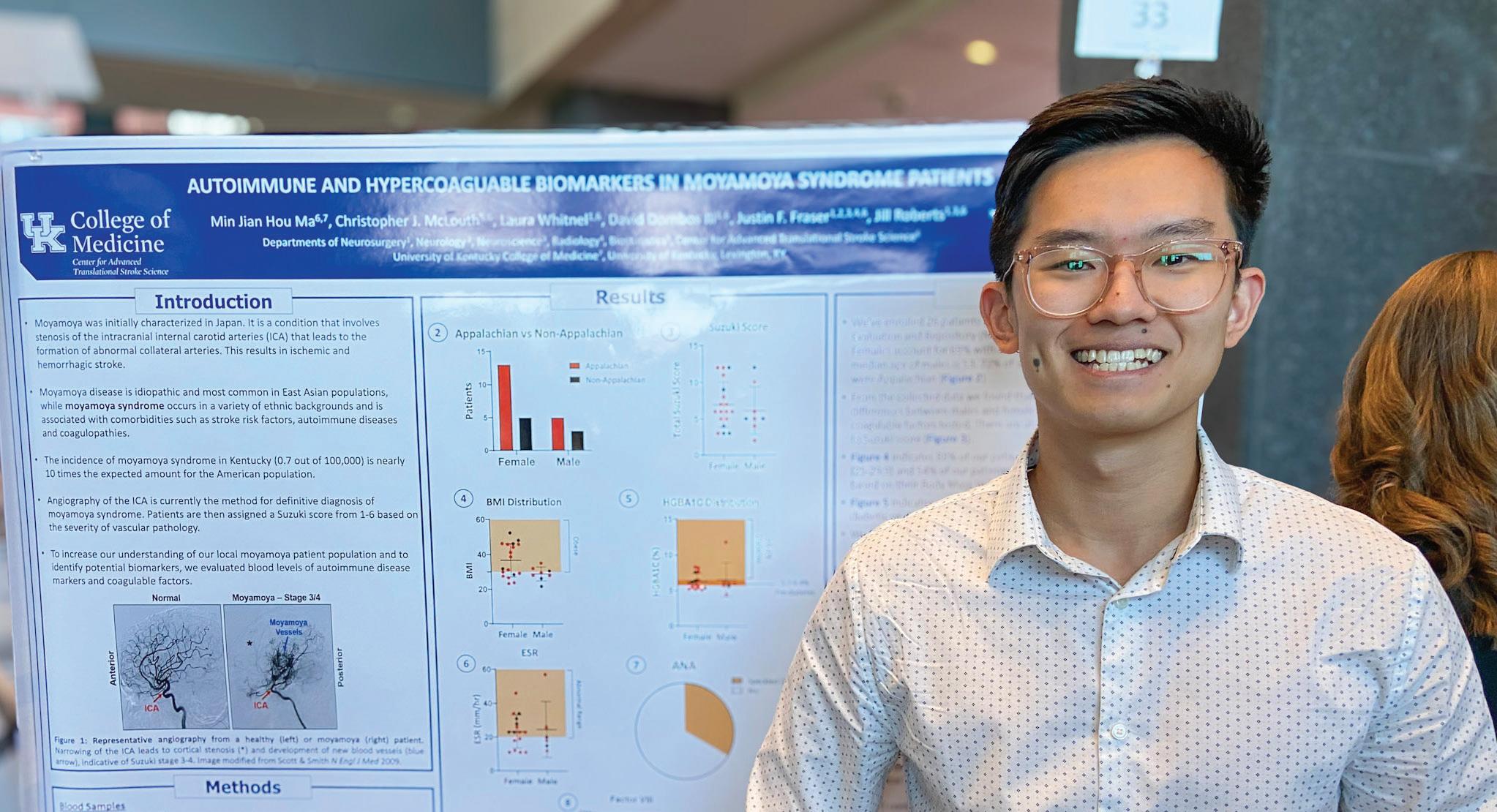
Our strength in numbers is felt across our four campuses. We are now one college offering exceptional undergraduate medical education in Bowling Green, Lexington, Morehead, and Northern Kentucky. We graduated 195 students this past spring across our sites. Of the Class of 2024, 73 students matched into a Kentucky residency program, 59 matched at the University of Kentucky, and 81 matched into a primary care specialty. The Michael D. Rankin MD Health Education Building will allow us to train even more medical students and keep this momentum moving forward.
We know training in Kentucky is a major factor in keeping physicians here to address the state’s physician shortage. The graduate medical education offerings here provide top-notch continued training including 77 programs accredited by the Accreditation Council for Graduate Medical Education (ACGME) across four sites: Bowling Green, Hazard, Lexington, and Morehead.
Our trainee numbers are powerful. With nearly 300 graduate students, 930+ residents and fellows, and 800+ medical students, the UK College of Medicine is bolstering our workforce of doctors, scientists, and health care leaders.
Of course, how can I forget the more than 1,400 faculty and 1,200 staff helping make this possible every day – and the growing alumni community inspiring our trainees to achieve greatness. The strengths of the individuals in our community allow the college to propel forward.
The UK College of Medicine is a growing academic medical center, and the strength is shown in our numbers. They convey an exciting preview of what can be accomplished in Kentucky, for Kentucky and beyond.
More than 2,000 learners across biomedical, medical, and graduate medical education.
195 graduating medical students in Spring 2024, with 42% of the class matching into a primary care specialty.
77 ACGME-accredited residency and fellowship programs. Nearly $226 million in total research funding.
954 active awards, our highest-ever recorded total.


The UK College of Medicine is excited to announce that Caroline R. Paul, MD, has been appointed the new associate dean of the Bowling Green Campus.
Dr. Paul’s extensive experience includes leadership roles in developing and implementing medical education programs, mentoring faculty, teaching, and contributing to medical research and scholarship.
She joins the UK College of Medicine from NYU Grossman School of Medicine and NYU Langone Health, where she was a general pediatrician, as well as an associate professor and co-director of faculty development in the NYU Department of Pediatrics. She also served as a medical education researcher in the NYU Institute for Innovations in Medical Education. Before her tenure at NYU, Dr. Paul was an associate professor at the University of Wisconsin School of Medicine and Public Health and faculty pediatrician at the University of Wisconsin Health West Clinic.
As the associate dean, Dr. Paul will be responsible for the overall leadership, implementation, and management of the Bowling Green Campus. She will work closely with leadership, faculty, staff, community stakeholders, and health systems to support all aspects of the medical education program. Her role includes supporting and mentoring students, ensuring optimal curriculum delivery, managing the recruitment and development of teaching faculty, and maintaining strong relationships with regional stakeholders.
As our college welcomes Dr. Paul to the Bowling Green Campus, we would like to recognize Todd Cheever, MD, our inaugural Bowling Green Campus dean, who paved the way for our regional site’s success. Dr. Cheever remains a vital part of the UK College of Medicine as the division chief for academic medical education.
The UK College of Medicine congratulates three trainees in the Office of Biomedical Education who were selected to join the 2024-2025 Scientist Mentoring and Diversity Program (SMDP) cohort.
The SMDP is a program under the International Center for Professional Development for undergraduate, graduate, and PhD students, as well as postdoctoral researchers. As part of the program, Dr. Smith, Aguzzoli-Heberle, and Obaleye will receive one year of mentoring from an industry executive and exposure to working in medical and biotech industries.


In 1964, the UK College of Medicine graduated its first class of medical students and sent off 32 doctors into the health care field to make a difference for patients in Kentucky.
In April 2024, the college celebrated the inaugural class with a spring reunion celebration.









































































The UK College of Medicine Integrated Biomedical Sciences (IBS) is an undifferentiated first-year core curriculum that serves as the entry point for a doctoral program in one of six basic science departments. All incoming doctoral students take the same courses during their first year and complete a variety of lab rotations before choosing their area of focus.


In 2024, under the leadership of Beth Garvy, PhD, senior associate dean for biomedical education, the Office of Biomedical Education launched a new innovative initiative aimed at enriching the education and career trajectories of its first-year students—a summer internship program.
Following their IBS year, 19 students completed four-week summer internships relevant to their unique scholarly interests. Diane Lally, PhD, director of trainee development for the Office of Biomedical Education, was integral to the development of the internship program. She worked closely with students to understand their interests and find diverse experiential learning opportunities across 10 partnering sites at UK and within the community.
“This internship happens at the end of that first year, just before they join their new labs,” noted Dr. Lally. “It helps them refine their career goals before starting the next step of their training.”
The structure of the internship program is managed in collaboration with UK’s Stuckert Career Center, ensuring comprehensive support for students. The program provides a holistic framework for personal and professional development, including structured assignments, regular reflections, and mentorship and networking opportunities.
“Soft skills were a major learning outcome for our students, skills they don’t necessarily get to practice in their regular coursework,” shared Dr. Lally.
After earning her undergraduate and master’s degrees in biomedicine in Brazil, Marilia Martins Manta was drawn to the UK College of Medicine for its unique IBS year, grateful that it “allows students to rotate through different departments before choosing a degree focus.” Manta spent her summer gaining insights into pharmaceutical development at Kindeva Drug Delivery, a contract development and manufacturing organization that works on the fabrication of important and life-saving products at UK’s Coldstream Research Campus.
“Heading into the last week of my internship I can say for certain that it was very important for my decision of career choice,” shared Manta. “I haven’t decided if I want to pursue industry or academia just yet, but I know I want to keep doing bench research.”
Susana Munoz Gil, originally from Colombia, also delved into industry dynamics through an internship at TruDiagnostic. “I was able to experience what a day in industry might look like,” Munoz reflects, “and was fascinated by the experiments I conducted. It felt like
The program not only exposes students to diverse career paths but also fosters essential skills like communication, critical for professional success.

magic.” Her internship at TruDiagnostic not only provided technical insights but also affirmed her passion for scientific exploration in an industry setting.
For Samantha Radomski, the internship was a “transformative experience.” She spent her summer working closely with Hollie Swanson, PhD, professor of pharmacology and nutritional sciences, assisting with the Summer Undergraduate Research in Environmental Science (SURES) program. Radomski’s involvement extended beyond routine tasks— she led workshops and conducted informational interviews with participants, embodying the internship’s goal of hands-on learning and experiential professional development.
“This internship has already played a large role in shaping my career goals and affirming what I will find fulfilling as a career,” shared Radomski.

This internship has already played a large role in shaping my career goals and affirming what I will find fulfilling as a career.”
Joshua Moses echoes similar sentiments, having “found his niche” in science communication through an internship with the college’s Office of Strategic Communications. “The biggest impact that this internship has had on me is that it showed me that I can do this career,” said Moses. “And I am pretty good at it.”
“Placing a biomedical PhD student on a marketing and communications team might seem unconventional, but Josh’s internship underscores the importance of scientists enhancing their communication skills to talk about the impactful work they’re doing,” shared Jorge Castorena, director of marketing. “It was inspiring to see how this opportunity not only helped Josh to grow, but also how our team benefited from his perspective as a scientist.”

For Radomski, the timing of the experience could not have been better. “This internship has been beneficial in both content and timing,” noted Radomski. “Because it’s at the end of my first year, I feel I have a renewed sense of confidence in my goals and am more committed to taking advantage of opportunities available.”
As the internship program continues to evolve, Dr. Lally and her team remain committed to enhancing students’ readiness for what lies ahead. “Our goal is for students to feel prepared both academically and professionally upon graduation,” shared Dr. Lally, underscoring the office’s broader mission of nurturing well-rounded biomedical professionals.
“This internship is just one piece of our career exploration efforts,” said Dr. Lally. “We provide year-round support through seminars, research days, as well as more practical lessons around updating CVs and LinkedIn profiles.”
Through mentorship, exposure to diverse career pathways, and practical experiences like the internship, IBS students are equipped with invaluable skills and insights, empowering them to chart their paths with confidence and purpose in the growing field of biomedical sciences.






STRENGTH IN NUMBERS
300+
biomedical trainees in UK graduate and certificate programs.
15 different areas of study at different levels across
6 basic science departments.
19 biomedical student participants in the inaugural IBS summer internship program.






























As we work to expand and enhance our care, training, and research across the state, we remain committed to our mission of improving the health and wellness of Kentuckians and beyond.
We utilize an integrated curriculum across all campuses, providing high-quality education to develop the next generation of health care leaders. Lectures are shared to all campuses via live stream and further enhanced by local faculty providing on-site teaching when appropriate. Our regional sites provide a more intimate approach to education and training with smaller class sizes, but students are exposed to the same curriculum regardless of location. Students are supported through our academic partners Morehead State, Northern Kentucky University, and Western Kentucky University.
During their clinical years, our medical students, as well as our residents and fellows, train alongside experienced physicians at leading health care institutions across the state including UK HealthCare, the Lexington VA Medical Center, Med Center Health in Bowling Green, St. Elizabeth Healthcare in Northern Kentucky, and St. Claire HealthCare, now under the UK HealthCare umbrella, in Morehead.
By training more students in Kentucky for Kentucky, UK is preparing more physicians to serve our communities and advance health care.
Here are some of those success stories.
5,500+ MD alumni serving communities in Kentucky and across the globe


We are dedicated to educating the next generation of compassionate, highly skilled physicians and scientists, with special emphasis on training more physicians to serve in rural areas.
With this goal in mind, the College of Medicine launched its Rural Physician Leadership Program (RPLP) in 2009. The RPLP is an educational program based in Morehead, Ky., designed to train future physicians and health care leaders to provide high-quality, compassionate care in rural settings. RPLP students complete their first two years of medical school at our Lexington campus before relocating to our Morehead Campus to develop clinical competencies and complete their medical education.
According to AAMC data from UK College of Medicine graduates from 2010-2015, the college ranks at the 96th percentile for graduates that go into rural areas of practice.
The RPLP is currently able to accept 12 new students each year. The demand for physicians, however, is higher than ever in the Commonwealth where some counties have no practicing physicians at all.
To address the ongoing physician shortage and the varied health care needs of rural populations, the College of Medicine has launched a new scholarly concentration in rural medicine available to students at all our campuses.
“When we announced it, we had relatively even interest from all the campuses,” shared Rebecca Todd, MD, associate dean for the Rural Physician Leadership Program (RPLP).
“I think that shows that medical students across Kentucky are interested in giving back to their communities.”
The scholarly concentration aims to equip medical students with specialized skills and insights crucial for serving rural communities. It also allows students to graduate with distinction, showcasing their commitment to serving rural populations.
“We wanted students to be able to celebrate that rural medicine was a dedicated interest of theirs,” Dr. Todd said.
The rural health concentration is open to any medical specialty. “Whether you want to pursue endocrinology, cardiology, surgery, or something else—the focus remains on rural health needs,” noted Dr. Todd.
Students apply to the concentration during their first year of medical school and complete clinical immersions in rural settings in the
following years. The program also emphasizes community involvement and development of leadership skills. Students are also expected to complete an additional rotation through the Area Health Education Center (AHEC) Program, beyond the standard AHEC requirements for graduation. Through this partnership, learners are able to gain invaluable clinical experience by shadowing physicians throughout rural Kentucky.
Colt Kendall, a Harrison County, Ky., native and second-year student at our Lexington campus, was eager to pursue this concentration because he hopes to return home to practice after finishing his medical training. He spent his summer completing a family medicine rotation at hishome hospital.
“I’ve absolutely loved this experience and it has only cemented my desire to return home to practice,” he shared.
Cydney Sampson, a second-year medical student at our Bowling Green Campus, shared that “pursuing this concentration has allowed me to shadow a physician and witness firsthand the challenges that those serving and living in rural areas must overcome.”
Shadowing a psychiatrist in Bowling Green, Sampson has been able to learn more about the specialty and gain a greater appreciation for its application in a rural setting.
“The need for mental health services is universal and Kentucky is no exception, especially given the prevalence of substance use in our state,” Sampson said. “With so
For as long as I’ve yearned to be a physician,
I’ve known I wanted to serve the Appalachian community.”
“This experience has made me even more certain that a rural area is where I want to be,” shared Kendall. “The relationships between patient and provider I got to see make me so excited to form my own relationships as a health care provider in the future.”
The scholarly concentration is still in its pilot phase, but looking ahead, Dr. Todd is optimistic about the program’s impact. “Ultimately we hope to increase the number of physicians practicing in rural Kentucky. By engaging students early into their careers, we hope to encourage their passion and foster long-term commitments to these communities.”
facilities – we are primed to accomplish this goal.
“Even though I’m at a regional campus, the College of Medicine has made access to the main campus and the various research projects they have to offer easy,” shared Logan Elliot, a fourth-year student in Bowling Green. “In addition to research opportunities, the college has fostered this excellent environment of collaboration between clinical departments and regional campus students, allowing us to easily rotate with, and learn from, attending physicians in Lexington.”
many of our counties facing barriers to basic health care access, psychiatric care is even more rare.”
For Brian Carter, an RPLP student, the summer shadowing experience offered clinical insight and a renewed sense of confidence. While shadowing a neurologist at St. Claire Regional Medical Center, Carter saw patients dealing with stroke, epilepsy, dementia, headaches, Parkinson’s disease, and more. Even though these conditions are typically covered by the first-year neurology unit, he shared, “making a diagnosis and creating a treatment plan with patients was a very different experience.”
“For as long as I’ve yearned to be a physician, I’ve known I wanted to serve the Appalachian community,” shared Carter. “The opportunities provided through the scholarly concentration continue to reinforce that decision.”
At the UK College of Medicine, we embrace our responsibility to drive the change and the discovery required to improve health and wellness across the state. As a recognized leader in biomedical research, we focus on innovative, transformative, and collaborative discoveries from the bench to the bedside. Through this approach, the institution is training our learners to become physicians who align evidence-based practice with the delivery of advanced clinical care.
Our objective is to advance transformative research through collaboration and innovation – leading to scientific impact and improved health for all. With faculty among the best in the nation – in the classroom, in the clinical setting, and in labs and research
Elliot worked with Sanford Archer, MD, professor of otolaryngology, and Logan Fluty, MD, a resident in the department. “When I met Dr. Fluty, I expressed interest in helping with ENT research,” shared Elliot. “He reached out immediately to share projects I could jump into.”
He shares that both mentors have offered continuous support throughout this process and were “readily available to answer any questions or to discuss what was going on.” Their guidance has not only facilitated Elliot’s academic growth but also nurtured his ability to conduct clinical research.
The number of students matching in Kentucky more than doubled from 2018 to 2024.

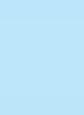
Justin Ma, a third-year medical student at our Bowling Green Campus, was inspired to pursue medicine after witnessing his father experience a stroke during childhood. He recalls the effect the event had on his family, noting “it opened my eyes to how someone’s health could not only impact their own wellbeing, but also really affect the people around them.”
Ma has been conducting neuroscience research under the mentorship of Jill Roberts, PhD, assistant professor of neurosurgery and neuroscience, and Justin Fraser, MD, associate professor of cerebrovascular, endovascular, and skull base surgery, both of whom call Lexington home.
During the summer between his M1 and M2 years, Ma was able to travel to Lexington and continue his research in person in the lab alongside Dr. Roberts.
Meghan Urhan Walker, also a third-year student in Bowling Green and PSMRF recipient, was drawn to research and science to enhance rural care. At a young age, her father was diagnosed with cancer and had to travel hours away from their rural home of Paducah, Ky. for treatment. The long commutes to distant hospitals for specialized care inspired Walker to become the physician her parents needed when she was younger.
Much of Dr. Roberts’ research focuses on Moyamoya, a disease most commonly found in East Asian populations. Moyamoya Syndrome, its non-idiopathic counterpart, is abnormally prevalent in Appalachia. Under the guidance of Drs. Roberts and Frazer, Ma has been working to identify biomarkers crucial for early detection and management.
“Dr. Roberts has been very understanding of my schedule as a medical student and has been very proactive about finding ways that I can help out from Bowling Green,” he shared. “She has given me many opportunities to learn new lab skills and is always supportive of me presenting at local conferences.”
Ma’s research experience was further enhanced by the Center for Clinical and Translational Science’s Professional Student Mentored Research Fellowship (PSMRF).
4 medical education campuses across the Commonwealth.
“When applying for medical school, I wanted to attend a school that would help me become more than just a physician; I wanted to be a rural physician,” shared Walker.
Under the mentorship of Martha Tillson, PhD, a research scientist with UK’s Center on Drug and Alcohol Research (CDAR), and Michele Staton, PhD, professor of behavioral science and faculty associate of CDAR, Walker’s passion for rural health has continued to flourish. Their guidance has been instrumental in her growth as a researcher, from learning basic research skills to presenting her findings at conferences, including the Kentucky Rural Health Association’s annual meeting.
“Despite the distance between Lexington and Bowling Green, they were always accessible for me to ask questions, receive feedback, and teach me new things,” expressed Walker. “Through Zoom, we had regular meetings and were able to work through statistics as if I was in the room.”
Her research project focused on health care disparities among incarcerated women with opioid use disorder. This project, part of the National Institute on Drug Abuse (NIDA)funded Justice Community Opioid Innovation Network, highlighted how health care
It opened my eyes to how someone’s health could not only impact their own well-being, but also really affect the people around them.”
utilization patterns correlate with county health rankings and physician-to-population ratios. Walker’s findings underscore the critical need for tailored health care policies to address the specific needs of vulnerable populations.
“In Bowling Green, I’ve been given opportunities to learn from physicians in rural areas, work with faculty who research health disparities, and attend classes that focus on being aware of patients’ external circumstances,” shared Walker. “Because of this, I feel that no matter the specialty I choose, I will be prepared to return home to western Kentucky and be the best rural physician I can be for my patients.”
“English or Español?” Whitney Weinschenk, a third-year medical student at our Northern Kentucky Campus, said asking that simple question elicited sighs of relief from some attendees at a community baby shower in Florence, Ky.
Weinschenk volunteered at the event alongside staff and providers from St. Elizabeth Healthcare, the UK College of Medicine’s clinical partner in the region. The community shower hosted more than 400 attendees, many of whom speak Spanish or French as their primary language.
Weinschenk, who handed out blankets during the event, was able to practice her Spanishspeaking skills and offer bilingual assistance to those in need. For Weinschenk, this was another stepping stone toward her goal of providing language-concordant care to her future patients.
Providing accessible and languageconcordant care to future patients is also the goal of Luis Comas Marrero, a second-year student at our Northern Kentucky Campus and president of its Latino Health and Culture Alliance (LHCA) student organization.
The mission of LHCA is to minimize the disparities faced by the local Spanish-speaking population by encouraging bilingual students to shadow physicians working with Latino and/or Hispanic patients. “It’s also culturally enriching for the medical students who may encounter cultures and perspectives they may not have seen before,” shared Marrero.
Students in Lexington share a similar passion for serving their community. The Lexington Latino Health Advocacy Association (LLHAA), a student organization in Lexington, was established to provide health care education, access, and opportunity to the local LatinX community. LLHAA students regularly volunteer at local clinics and participate in outreach activities that benefit Lexington’s Spanish-speaking population.
Knowing her students’ drive for compassionate care, Holly Danneman, MD, associate dean of the Northern Kentucky Campus advocated that the college provide students, faculty, staff, and trainees across all four campuses with free access to CanopyLearn, an online medical Spanish program.
CanopyLearn, a medical Spanish e-learning program, has been a useful tool for students,
as well as faculty, staff, and trainees, who want to learn Spanish or increase their language proficiency. Designed specifically for health care professionals, it includes 40 hours of instructional content broken down into simple 15-minute modules. There are 36 total lessons spanning three levels with multiple learning modes. The interactive modules are intended to provide a more holistic active learning experience and include grammar, pronunciation, and vocabulary for 36 medical specialties.
CanopyLearn is meant to be an e-learning tool. It is not an assessment or certification service or meant to take the place of interpretation services. The program does, however, allow students to learn medical terminology, brush up on their conversation skills, and follow along with the interpreter during clinical encounters. This can also help create a more inclusive environment for patients outside of the exam room, particularly if students are able to communicate and assist with tasks like wayfinding if a patient or their families need help navigating the hospital system.
“Having this course has been nice because I don’t get to practice Spanish in my daily life,” shared Weinschenk. “I try and log on to CanopyLearn for 15 minutes every day. It’s really nice because it’s more than just medical terms—you start from the beginning, learning actual Spanish conversation skills, too.”
According to recent data, nearly 8% of households in Lexington speak Spanish
Wherever you go, you’re going to need to communicate with other people.”
as their primary language. In Northern Kentucky, that statistic rises to almost 12%. “Wherever you go, you’re going to need to communicate with other people. Speaking the same language as our patients will help put them at ease and build a stronger rapport,” said Weinschenk.
UK can train
1,000+ medical students at once with the addition of the Michael D. Rankin MD Health Education Building.


Research is a vital pillar of our mission at the University of Kentucky College of Medicine. It helps us bring important health care solutions to the bedside and provide optimal care to patients that need it.
The Office of Research has invested significantly into infrastructure helping research teams thrive while creating new opportunities to recognize important contributions of our faculty and staff. Recent successes include a research awards program, a faculty research leadership program, the clinician-scientist program, the FORWARRD initiative, and the Research Professionals Network.
Additionally, the college invested in grant writing support infrastructure and has continued to support research incentives, pilot awards, and the continuation of the Alliance Research Initiative that provides seed funding for interdisciplinary teams investigating health challenges impacting Kentucky and beyond.
In fiscal year 2024, the UK College of Medicine saw the results of those investments, as well as a reflection of our faculty, staff, and learners who help make these achievements possible. We saw growth in multiple fields, continuing trends observed over the past decade of tracking these statistics.
On the next page, you will read about one of our research alliances finding innovative solutions to health care challenges.

STRENGTH IN NUMBERS
Nearly $226 million in total research funding, a 6.6% increase over the previous fiscal year’s awards and the second highest total ever recorded for our college
In Aug. 2020, the College of Medicine Office of Research launched 18 Alliance Research Initiative teams from each of the five research priority areas— substance use disorder, cardiovascular, diabetes and obesity, neuroscience, and cancer— and other important emerging areas of science. Since then, some alliances have completed their research projects or transitioned to larger funding mechanisms due to their success and several new alliances have been added to the active roster.
One of the new alliances is the mHealth Application Modernization and Mobilization Alliance (MAMMA). mHealth, also called mobile health, refers to the utilization of mobile devices to aid in health care delivery. Established in 2023, MAMMA has been making significant strides in the realm of mobile health application research, leveraging the power of technology to conduct social and biomedical research via smartphone apps.
The overarching goal of MAMMA is to help researchers successfully integrate mobile technologies into their research methodologies, leveraging the power of technology to reach broader audiences, enhance data collection, and better inform patient care.
Mikhail Koffarnus, PhD, an associate professor of family and community medicine, and Carolyn Lauckner, PhD, an associate professor of behavioral science and in the Center for Health Equity
954 total grants awarded, our highest-ever number recorded
The College of Medicine represented 46% of the University’s sponsored project awards, with 7 out of the top 12 highest funded individual units 359 principal investigators leading groundbreaking studies

Transformation (CHET), serve as co-directors of the alliance. They support a large team of interdisciplinary researchers from the Colleges of Medicine, Health Sciences, Arts and Sciences, Fine Arts, Law, and Agriculture, Food, and Environment.
“One of the values of this alliance is bringing everybody together to share their expertise on this common problem,” shared Dr. Koffarnus. “Without it, these individuals normally wouldn’t interact because they’re in completely different parts of the University.”
Monthly meetings serve as a cornerstone for knowledge sharing and collaboration within the alliance. These sessions provide a platform for researchers to present their progress, seek feedback, and discuss common challenges, such as regulatory hurdles, buying cell phones, or navigating data privacy concerns.
Since its inception, the alliance has sponsored four impactful pilot studies, each addressing different health challenges through innovative mobile solutions.
One of MAMMA’s first pilot awardees was Yuyao Sun, MD, a clinical neurologist, who developed a project using a mobile app to track fat mass in patients with amyotrophic lateral sclerosis (ALS). The app, connected to a Bluetooth smart scale, allows for remote monitoring of patient’s symptoms that are critical for disease management between regular doctor visits.
“She developed this idea in response to a need that she saw in her practice,” said Dr. Lauckner. “It’s really patient-responsive.”
Another alliance project, led by Jami Warren, PhD, associate professor in the College of Health Sciences, targets Postural Orthostatic Tachycardia Syndrome (POTS) patients by utilizing an app connected to a smartwatch to monitor and track their symptoms. By empowering patients with quantifiable data, the app enhances their ability to manage and communicate symptoms effectively with health care providers, which could potentially accelerate their diagnosis and treatment.


MAMMA awarded two additional pilot awards, co-sponsored by CHET, to projects utilizing mHealth applications to address health disparities.
Carrie Oser, PhD, a University Research Professor and the Di Silvestro Endowed Professor in Sociology, is working with MAMMA’s programmer to develop an app to support an intervention for people in recovery from substance use disorders who live in rural areas and may be experiencing challenges to their recovery. The app hopes to monitor symptoms, track social interactions, and help identify stressors that may trigger a return to use. It is especially beneficial to patients in rural areas who may lack regular access to supportive services or treatment.
Justin Huber, MD, an assistant professor of physical medicine and rehabilitation, was inspired to pursue his project after witnessing a need among his patients. With an emphasis on helping patients regain mobility following a stroke, Dr. Huber was already working with patients in his lab to capture clips of their movement on video to analyze their recovery progress using a custom algorithm. Now, with an mHealth application, he hopes to make that level of care more accessible to other providers and to his patients. Using smartphones, the ultimate goal is to allow patients to record their movements at home, allowing Dr. Huber to digitally track their symptoms and recovery progression.
“We’re hopeful that this could have a real impact,” shared Dr. Lauckner, “especially for rural patients who need rehabilitative services but may lack the means to come to the hospital frequently or have mobility issues that make traveling difficult.”
In addition to granting pilot funding awards, MAMMA offers recipients the invaluable resource of an in-house full-time application developer, Mitchell Embry, MA, to help develop and maintain their mobile health applications over time.
This innovative approach not only helps jumpstart researchers’ projects but also addresses a common barrier among physicians and biomedical researchers—access to coding and programming expertise—which is essential for developing effective and userfriendly mobile health interventions.
“Providing access to a full-time programmer for our researchers is basically unheard of,” shared Dr. Lauckner. “But it’s been absolutely invaluable to our alliance.”
Looking ahead, the alliance aims to not only expand its impact through ongoing and future research projects but also advocate for more streamlined regulatory pathways and sustainable funding models to support researchers interested in mobile health research.
“The MAMMA Alliance has made tremendous strides in a short time,” expressed Becky Dutch, PhD, vice dean for research. “They are opening up new avenues of research for faculty across campus.”
Dr. Dutch continued, “providing community, expertise, and access to an experienced programmer for those awarded pilots allow the alliance to rapidly jump-start a new research program, apply for new funding, and most importantly, work to improve health across the commonwealth and the nation”.
By championing these efforts, MAMMA is poised to support mobile health research innovation, ensuring that cutting-edge mHealth technologies benefit both researchers and the communities they serve.

We’re hopeful that this could have a real impact,
especially for rural patients who need rehabilitative services but may lack the means to come to the hospital frequently or have mobility issues that make traveling difficult.”


The University of Kentucky College of Medicine’s mission is to educate physicians and scientists who will positively impact care for patients in the Commonwealth and beyond.
Thanks to global health initiatives within the UK College of Medicine, residents and fellows are gaining invaluable experience in dozens of countries – helping thousands of patients while learning unique skills to enhance their practice of medicine.
Katherine McKinney, MD, senior associate dean for graduate medical education, praises her residents’ and fellows’ determination to implement these life-changing experiences into an already challenging training regimen.
“I’m always inspired by the interest that our UK residents and fellows have in global health outreach and travel, and the unique ‘service learning’ that transpires during these trips,” she said. “For those who’ve been able to do so, their consistent feedback has been that the learning and exposure to providing medical care in a different cultural setting yields incredible educational experience well worth figuring out how to make it happen!”
The “incredible faculty mentors” involved in global health initiatives, she added, have paved the way for UK residents and fellows to take on these fulfilling work and training experiences.
This story provides testimonials from some of the residents, faculty members, and alumni who are involved in global health initiatives at the UK College of Medicine. It is not an exhaustive list of the global health opportunities made possible through UK connections.
Fifth-year plastic surgery resident Evan Lynch, MD, PhD, joined Professor James Liau, MD, on a Global Smile Foundation medical mission to Ecuador, providing clinical and surgical treatment helping patients with cleft lip and cleft palate diagnoses.
Dr. Lynch said patients with these conditions face social isolation. For example, he met a family whose business suffered after the community learned of their child’s cleft lip. He added that the Global Smile Foundation sees patients from about 87% of the country, as well as from other countries. Some families drove seven to eight hours just to see their group’s medical
practice. Not to mention, the country was going through political unrest at the time.
“One patient said the rest of her family had fled to Colombia for fear of retribution, but she stayed back just to receive medical care for their child,” Dr. Lynch said. “You really see the stakes of the work we are doing. She was undergoing risk of personal harm just to get the care. As a provider, that really puts things into perspective.”
Dr. Liau, a plastic surgeon and faculty member in the UK College of Medicine Department of Surgery, has been going yearly to Ecuador with the Global Smiles Foundation since 2014, and he routinely brings a senior plastic surgery resident on global cleft care trips. Dr. Liau feels this opportunity provides residents like Dr. Lynch with invaluable perspectives on the impact surgery can have on patients and families, as well as a broader health care issues in developing nations.
William B. Inabnet, MD, MHA, the Johnston-Wright Endowed Professor and Chair of Surgery, is a strong advocate for faculty and residents building connections with health care facilities across the globe. He made global outreach one of his department’s pillars to measure success.
UK surgical faculty have traveled to at least nine countries to assist with medical care and provide training experience for residents. The department also made its first in-person visit to Zambia’s largest teaching hospital as part of the Lusaka Surgical Training Collaborative within the American College of Surgeons’ Health Outreach Program for Equity in Global Surgery (ACS H.O.P.E.).
Dr. Lynch said he noticed the surgery department’s passion for global health right away, adding that “Dr. Inabnet set the stage for faculty and resident involvement.” It is from this passion that the UK College of Medicine Department of Surgery helped fund Dr. Lynch’s travel to Ecuador and participation in the trip.
With fellowships around the corner, experience in Ecuador connected Dr. Lynch to seven surgeons from seven different health care institutions. “That’s seven new surgeons to bounce ideas off of, seven professional and personal connections,” Dr. Lynch said.
Dr. Lynch graduated from UK’s combined MD/PhD program. As a physician-scientist, one of his career goals is spreading the word about the importance of global health experiences through data collection and publications. “We need people who are effective communicators in that space, and I want to integrate that in my practice,” he said.
Paras Vora, MD, was part of the UK College of Medicine Department of Ophthalmology’s Global Ophthalmology (UK GO) residency track.
Dr. Vora’s family is from a small, rural town in India. “You saw some of the worst pathologies,” he said. A visit to his hometown during medical school – seeing doctors perform more than 40 cataract surgeries per day – inspired his interest in ophthalmology. He knew there was a need, and he saw firsthand how he could help others.
“When the patient takes their patch off and they can see again, there’s nothing like that in medicine,” Dr. Vora said. “Still, to this day, I have not found that gratification in anything else.”
While in residency at the UK College of Medicine, he joined ophthalmology faculty member Seema Capoor, MD, and the Hospital de la Familia Foundation for a two-week trip to provide eye care to a community in Guatemala. As a trainee, Dr. Vora provided support for cataract surgeries alongside a full-time attending.
He called the experience a “nice skills transfer,” with the physicians from different countries learning from one another.
For example, in the U.S., standard practice for cataract surgeries is phacoemulsification, a high-tech process breaking up the eye’s natural lens through small incisions to remove the cataract. Where Dr. Vora was in Guatemala, they used a more manual approach, which requires a larger incision but not a lot of equipment. “It’s ultimately a really helpful technique, especially for long-

term cataract patients,” Dr. Vora said. While recovery time is a bit longer for the manual process, the procedures take roughly the same amount of time.
Dr. Vora is continuing his ophthalmology education at the UK College of Medicine, this time through a vitreoretinal surgery fellowship. He said patient interactions during the Guatemala trip mirrored practice in rural areas of Kentucky, where there is also limited access to health care combined with burdening diseases.
“The skills you learn in Guatemala and those sorts of discussions are going to be very similar to when you’re in practice here,” Dr. Vora said. “You have to think clearly and quickly on your feet. How am I going to respect their fears? Their culture? Our part of the world is very distrustful of medicine.”
“We need to understand where they’re coming from, that’s really important.”

Shoulder to Shoulder Global: 17 years. 43,000+ patients served.
Thomas Young, MD, the Jim and Suzanne Elliott and Family Professor of Pediatrics, has contributed greatly to the global health experiences of hundreds of trainees at UK. He founded Shoulder to Shoulder Global, an organization under the UK International Center working to improve health care in an underserved community of Ecuador.
Dr. Young said UK has had a connection with the country for over 50 years, having been “matched” by Partners of the Americas. “When I was looking for a site to do our first global health initiative, it made sense to tie to contacts we had in Ecuador,” he said.
Dr. Young’s first trip was in 2002, just with pediatricians. Now, each trip, he brings between 35-50 faculty and trainees from the colleges of Medicine, Arts and Sciences, Education, Dentistry, Health Sciences, Nursing, and Pharmacy. He runs three trips per year.
Shoulder to Shoulder Global brigades work to support sustained health care quality in the area. The organization helped establish a year-round active health center that has been open for 17 years.
“What you don’t want to do in short-term global health initiatives is go down for a week and disappear,” Dr. Young said. “Each of the trainees who go knows they are not only paying for their own housing, room and board, and medical supplies, but also to keep the clinic running because the clinic is who follows up on our patients.”
In addition, Dr. Young oversees the global health track within the UK College of Medicine Department of Pediatrics. It started 10 years ago and works “hand in hand”
with the Shoulder to Shoulder Global. At a given time, there are about 12-15 categorical pediatrics, med-peds, and triple-board residents involved. They join weeklong medical missions in their first two years of residency, then serve a month-long rotation in their third or fourth year.
Jonathan Barko, MD, joined Shoulder to Shoulder Global Brigades to Ecuador early into his residency training. Then last spring, just before graduating from UK’s internal medicine/pediatrics residency program, he completed a month-long “education- and service-focused” trip to Tanzania.
otolaryngology - head and neck surgery residency program.
While in residency, Dr. Noblitt connected with Matthew Bush, MD, PhD, MBA, chair for the UK College of Medicine Department of Otolaryngology and founder of the Kenya Outreach Program. Over the years Dr. Bush took several trips to Kenya to partner with the country’s flagship teaching hospital and only Ear, Nose and Throat (ENT) training program.
Although he never had the opportunity to travel to Kenya with Dr. Bush due to the COVID-19 pandemic, Dr. Noblitt was still inspired to serve that population. During school, he learned more about the PanAfrican Academy of Christian Surgeons (PAACS). The group is a U.S. faith-based organization that has developed surgical residency programs in 13 sites around Africa.

Dr. Barko served alongside an attending on the pediatric floor and pediatric ICU of the partnering hospital. He also worked alongside residents from Tanzania and helped to train their third-year medical students.
While there, Dr. Barko saw diseases he didn’t often see at UK, such as malaria and tuberculosis. The experience opened his mind to the variety of pathologies physicians treat. Along with developing an appreciation for more abundant U.S. health care resources, he also learned how lack of access to care can plague communities.
He recommends other physicians take advantage of these experiences. “There are so many opportunities to help other communities,” he said.
Bryce Noblitt, MD, always knew he had a calling to serve others. In 2012, he started medical school at the UK College of Medicine, and his vision started to take shape. Dr. Noblitt spent nine years at UK receiving this medical degree and completing the
Dr. Noblitt attended a PAACS conference and learned about an ENT department at AIC-Kijabe Hospital located in Kijabe, Kenya. AICKijabe was the only site that had an ENT program already established.
Following his residency, in the fall of 2022, he, his wife and three children packed up and moved to Kenya. Once they started to settle in, Dr. Noblitt began his work as a medical missionary at AIC-Kijabe Hospital in the ENT department as part of the postresidency program through Samaritan’s Purse.
The family has now been living overseas serving their new community for over a year with no return date penciled in. Three children have started school in town, and the family recently announced the birth of their fourth child.
Dr. Noblitt’s goal is to continue to learn, grow, stay strong in his faith, and provide the best care possible to all of his patients. “If you remember that and let that goal shape your career choices, then it leads to a more fulfilling career, and probably a more fun career.”
Follow the Noblitt family’s journey through their blog and YouTube channel at KenyaHear.org.
80,000+ miles traveled by residents and fellows on global health trips since July 2021

To donate to Shoulder to Shoulder, scan this QR code.

For more opportunities to donate to UK global health initiatives, email COMPhilanthropy@uky.edu.

Department of Behavioral Science celebrates
For 65 years, the department of behavioral science has engaged in transformative research and provided exceptional educational opportunities for learners. Founded in 1959 by William R. Willard, MD, the first dean of the College of Medicine, and Robert “Bob” Straus, PhD, the department was the first of its kind in the United States.
The decision to embrace behavioral science as a necessary discipline within medical education was unique for the time, but it has since become an established priority for the National Institutes of Health (NIH). At many medical institutions, behavioral scientists are scattered throughout clinical departments or placed in divisions within departments of psychiatry. As a freestanding basic science department at the UK College of Medicine, the department is an administratively independent academic teaching and research unit.
Dr. Straus, traveling by train, arrived at the University of Kentucky in 1956 as a member of the five-person team assembled by Dr. Willard. Their purpose was planning the construction and academic curriculum for what would become the UK College of Medicine. Dr. Straus would go on to serve as chair of the department of behavioral science for nearly 30 years. He was committed to recruiting faculty from a variety of behavioral and medical disciplines, recognizing the important role of multidisciplinary approaches to medicine and healing. That collaborative atmosphere contributes to the department’s strengths in education, service, and research through today, with several faculty holding joint appointments across the institution in disciplines such as sociology, anthropology, psychology, and social work, to name a few.

Succeeding Dr. Straus, Thomas Garrity, PhD, and Carl Leukefeld, DSW, continued expanding upon the department’s complementary missions of education, research, and service during their respective tenures. Dr. Garrity’s 12-year tenure as chair saw the expansion of behavioral science training to encompass graduate students as well as medical students. Dr. Leukefeld, drawing on his experience at the NIH, significantly enhanced the department’s research capabilities, creating a robust infrastructure that bolstered faculty success in securing external grant funding.
Thomas Kelly, PhD, current chair of behavioral science, has inherited a department with impressive successes and hopes to maintain its momentum. Under his leadership, the department has continued to expand its educational reach by developing an undergraduate certificate program. Claire Clark, PhD, serves as director of graduate studies within the department and oversees the newly established program, aimed at providing a foundational understanding of behavioral science that be will effective as students transition to future careers in medicine.
“The work of our department is having an impact— an immediate impact,” Dr. Kelly said. “The research that we do is at the patient level, at the community level, and at the policy level.” The department also supports and partners with two prominent research centers within the college— the Center on Drug and Alcohol Research (CDAR) and the Center for Health Equity Transformation (CHET). These collaborations have not only advanced scientific knowledge but also address critical health challenges facing Kentucky and beyond.
“The UK College of Medicine was one of the first of a new generation of medical schools,” said Straus in a 2010 interview. “It was planned with special attention to the needs of its students, its patients, and the people of Kentucky, as well as to meeting the standards of academic and scientific excellence.”
As we celebrate the 65th anniversary of the department, and the establishment of the College of Medicine at-large, we are grateful to all who have contributed to its successes over the years. We look forward to all the department of behavioral science will continue to accomplish through its robust educational programs, transformative research initiatives, and its lasting impact on Kentuckians and beyond.

In 1959
the UK College of Medicine established the first behavioral science department in the world











K Phillips, MD, left the 1974 UK College of Medicine graduation ceremony with his degree in one hand and a brand-new doctor’s bag in the other. The bag was as full of tradition and meaning as it was of physician’s instruments. Gifted to the entire graduating class every year by a private company, it marked the entry into the world of medical practice.
Inside the bag were the basic tools of the trade: a Littmann stethoscope, a tuning fork, a reflex hammer, and a Welch Allyn otoscope/ophthalmoscope set—which Dr. Phillips uses to this day, 50 years after receiving the gift.
Dr. Phillips was sad to see the tradition disappear in the ensuing years. A bag and diagnostic instruments were expensive, and medical school graduates saddled with debt had been grateful to be free of yet another expense. But even more than that, it was gratifying to know that other people wanted to honor their achievement and their call to service.
Years later, a similar tradition was in jeopardy. The UK Medical Alumni Association had been purchasing the professional white coats that incoming students received at the annual White Coat Ceremony but couldn’t sustain the expense while also funding student scholarships.
This time, Dr. Phillips and his wife Faye saw an opportunity to save an important tradition that symbolized the beginning of so many medical careers. They started a fund that has paid for every white coat gifted to new UK medical students since 2010.
For Dr. Phillips, it was a way not only to contribute to the college that trained him, but also to pay forward a gift that never lost its resonance over decades of professional practice. In another 50 years, these white coats will be cherished mementos of the spirit of gratitude that lives on through the Phillips’ gift to new trainees.


To learn how you can contribute, so you can help support tradition please contact COMPhilanthropy@uky.edu
“Our family is forever grateful to the University of Kentucky College of Medicine for the wonderful education that I and one of our sons received. I was able to attend medical school when tuition was quite affordable and now look with shock at the very expensive education that our future physicians must endure. We certainly believe in the education of physicians to serve our Commonwealth and want the UK College of Medicine community to know our deep appreciation by sponsoring an endowed scholarship in our family’s name. Hopefully this will enable many men and women to achieve their goals and in turn encourage them to give back through their continued support down the road.”
– Al Hoskins, MD, MACP
To share your own notes of encouragement with incoming medical students, scan this QR code.

“I am filled with gratitude and deeply appreciative of my scholarship donor. I was once a little boy with a hefty dream of becoming a physician, and many obstacles crossed my path that I was not capable of resolving on my own. My success and achievements have been the result of kind, caring, and generous people like yourself who have helped a first-generation student like myself make my dream a reality. I have excelled in my first year and grown as a student, a friend, and a future physician. I have earned leadership and service roles, made valuable connections in the medical field, and become an even more curious learner in the past year, all because of you. Thank you!”
Cameron Coulter Class of 2027

The University of Kentucky College of Medicine is excited to share the winners of the third annual Mission, Vision, Pillar, and Enabler (MVPE) Awards.
The college honors this year’s award-winning faculty, staff, and learners who have made exceptional contributions to the overall mission, vision, and purpose of the college’s current strategic plan.
This strategy includes excellent education, patient-centered clinical care, transformative research, diversity and inclusion, community engagement, and enabling the successes of each.
Winners are listed below. Please join us in congratulating these incredible members of the UK College of Medicine community.
Mission
Christine Brainson, PhD
Associate Professor with Tenure, Toxicology and Cancer Biology
Aaron Chacon
PhD Candidate, Pharmacology and Nutritional Sciences
Leslie Justice
Graduate Medical Education Coordinator, Physical Medicine and Rehabilitation
Vision
Molly Bates, MD
Fourth-Year Resident, Neurology
Dong “Dan” Han, PsyD
Professor, Neurology, Neurosurgery, and Physical Medicine and Rehabilitation
Taylor Bradley Fourth-Year Medical Student
Jacklyn Brewer
Nurse Navigator
Sabrina Brewer
Administrative Operations Coordinator, Research
Claire Clark, PhD, MPH
Associate Professor, Behavioral Science
Misty Fenech
Health Education Coordinator Senior, Internal Medicine
Terry Hinds, PhD
Associate Professor, Pharmacology and Nutritional Sciences
Michelle Lofwall, MD
Professor, Behavioral Science and Psychiatry
Bell Alcohol and Addictions Chair
Colleen McMullen
Editorial Officer, Internal Medicine
Whitney Nipple Admissions Officer, Bowling Green Campus
Bryan Rone, MD Professor, Obstetrics and Gynecology
Parijat Sen, MD
Assistant Professor, Internal Medicine
Lillian Sims, PhD Lecturer, Behavioral Science
5,300+ members of the UK College of Medicine community
UK Medicine magazine is a publication of the UK College of Medicine.
For more information, write: University of Kentucky College of Medicine 780 Rose Street, MS 335E Lexington, KY 40536-0298
Editor: Audrey Kirby O’Gara, Communications Director, Email: Audrey.Kirby@uky.edu | Phone: 859-323-1143
Photography: Lily Wilder, UK College of Medicine Communications; Mark Mahan Photography; Clinton Lewis, Western Kentucky University, Morgan Ravenscraft, Mark Setters
Editorial: Charla Hamilton, Audrey Kirby O’Gara, UK College of Medicine Communications; Brandon Duncan, Contributor
Design: Jordan Gieselman, UK College of Medicine Communications
Copyright © 2024 University of Kentucky. All rights reserved.
An equal opportunity university. No part of this publication may be reproduced without written permission of UK College of Medicine.



