
A report into the first 1000 days of life in marginalised groups in the United Kingdom
April 2022
Introduction
Dame Lorna Muirhead, Commission ChairPoverty and its dire effects prevents people from having the life many of us take for granted, and those wide ranging detrimental effects are well documented in this report.
Since we are all born unknowing, we rely totally on those who care for us to feed, love and nurture us; to keep us safe, to educate us and give us aspirations for the future so that we have a chance of becoming thriving citizens. If those caring things had not been done, we may have been prevented from reaching our potential. In turn, we may have children of our own and raise them as we have been raised so, whether positive or negative, the cycle is repeated. Any one of us could have been born into poverty to parents whose energy is largely subsumed with just keeping their head above water and not able to pay attention to child development. There is great need to break this cycle by parenting the parent.
Nonetheless, things are not all bleak. We live in a society which gives attention to such matters, however inadequate those efforts are. Hopefully, reports like this give policy makers a steer to the way forward.
Commissioners were indebted to those who need the assistance of the services provided, who took the time to tell us about their lives. They were also greatly impressed by the enthusiasm and commitment which resource-starved professionals demonstrated in their endeavour to do their best for those families for whom they are responsible. The do have a sense of frustration about lack of staff and money, but as the poet William Morris writes, they are not ''beaten by the muddle". The service users are also thanked for their faceto-face contribution in helping us compile this report.
Acknowledgements
Liverpool John Moores University thanks wholeheartedly all of the commissioners, who with an already busy workload, contributed their time and effort so generously.
We also offer our thanks to everyone who came forward to provide evidence for us. Some informants were well prepared in advance, others heard about us through publicity on local radio and television and others still just dropped in to see what was going on. We appreciate the health and social care staff as well as those from the third sector, who took some time out from busy jobs to tell us what was happening on the ground. Special thanks are offered to the service users who described some very difficult personal situations for themselves, in the hope of making things better for others in similar conditions. We hope we have been able to represent your voices well. and we are happy to donate 50% FOC, so £27.50 per unit for half of
Executive summary
Liverpool Health Commission had its genesis in autumn 2018 as a tool to help implement the university’s strategic vision of being a pioneering, modern civic university delivering solutions to the challenges of the 21st century. The Liverpool Health Commission’s aims were to conduct an independent investigation and critical analysis of current experiences in the first 1000 days of life in marginalised groups and to make grounded contributions to debates at national level that will seek to assist policymakers at all levels who are searching for meaningful, practical solutions to the problems and challenges facing the population and health sector across the UK in the 21st century. We established that the main focus of the commission would be on poverty as it is that which underpins many of the disadvantaged groups we discussed The commission consisted of 12 commissioners, as well as a chair and an academic lead. It was formally launched in May 2019. with hearings initially in six locations around the UK, each of which had high levels of child poverty from November 2019, until September 2020. As well as ensuring a geographic spread the commission chose to avoid places which had been the subject of other recent major inquiries.
The final choices therefore were:
Morecambe, a former seaside resort in north-west England; Middlesbrough in north-east England, a previously heavily industrialised town, was a centre for iron and steel works and shipbuilding; Clacton-on Sea, in south-east England, originally a stone age settlement and a popular seaside resort in the early 20th century Derry/Londonderry, the second largest city in Northern Ireland that lies very close to the border with the Republic of Ireland; Neath/Port Talbot in south Wales located about 10 miles to the east of Swansea with an industrial past is similar to that of Middlesbrough, but economically it also has a large rural population stretching up a number of valleys; Lanarkshire in south-west Scotland comprising north and south Lanarkshire counties is an inland area which was dominated by coal mining and associated iron and steel works until the 1980s; Merseyside was the final area to be considered, after all other evidence had been collected because it was the “home” of the commission.
Located in north-west England, it is a port area which was extensively bombed in World War II. It has subsequently been amongst the most impoverished areas of England. Its health outcomes and life expectancy are significantly worse than the whole of England.
The main report was drafted in February 2021 and findings from around the UK were used to inform the final week of evidence gathering in the Merseyside area in September 2021.
A critical overview of the existing literature was conducted to inform the commission’s approach drawing on relevant reports from all four UK countries as well as international agencies such as those of the United Nations. Initial contact was made with each area through the local council offices where officers responsible for child health services in the area agreed to support the project by assisting with provision of venues and providing further contacts in the health and council services as well as voluntary sectors and service user groups. We did not attempt to speak to managers but rather we chose to engage with people providing the hands-on services as well as those receiving them.
Findings
• Finance:
o Difficulties have been experienced by people who are not made aware of eligibility for certain benefit and who are struggling to make ends meet.
o The introduction of universal credit and subsequent changes to it have caused considerable confusion amongst both service providers and users.
• Housing
o Homelessness, housing provision and temporary accommodation are often inadequate for families with children in the first 1000 days of life
o Landlords are frequently not held accountable for their actions
• Local service provision
o Families struggle to maintain a good diet because of a lack of nearby providers of nutritious and affordable food.
o The reduction in Children’s Centres has led to social isolation as many families cannot afford the cost of public transport to their nearest centres
o Public transport is often inadequate especially in, though not limited to, rural areas
• Mental health
o Intergenerational cycles of poor mental health are being perpetuated
o Mothers suffering from mental health problems face difficulties in seeking help to reach out for help and there are insufficient trained carers to meet their needs
o Early detection and prompt management of infant mental health problems is rarely possible
• Infant nutrition
o As well as cultural resistance to breastfeeding public attitudes prevent some women from trying to breastfeed their babies
o Inaccurate information is often spread about breastfeeding on social media sites and bottle feeding still advertised on television
• Particular vulnerable groups
o Refugees and other migrants are frequently separated from their cultural groups and are unable to communicate and so obtain essential services.
o Babies who have been hospitalised do not always receive follow up services
• Overall
o Families who are drug/alcohol dependent are not always recognised and appropriate action taken in regard to their babies
o Domestic abuse is widespread with affected families not always able to remove themselves from danger
o Conflicting advice is often received from different agencies
o The involvement of multiple professionals can preclude the establishment of trusting relationships between service users and providers
Recommendations
1. Noting the often repeated mismatch between the wishes of professionals to use education to improve families’ circumstances and the ability of the families to respond, further exploration of more effective interventions is merited;
2. Community participation, and involvement of voluntary agencies should be maximised to tailor support and services around the individual needs of families.
3. Joint agency working remains a significant challenge to achieve and should be addressed as a matter of urgency to improve support for service users and outcomes.
4. Communication methods between staff and service users should be reviewed to ensure they are empathetic, effective and appropriate to meet needs.
5. Mobile services such as those provided in some rural areas bring services to the more remote communities. They could be used in urban areas where transport and access are barriers to service users.
6. Family focused approaches would ensure that awareness of the needs in the first 1000 days is not simply the responsibility of the mother. Families and extended families could be included in being supported to care for the baby
7. Policy changes are required to offer universal, long-term, appropriate support to families in need in the first 1000 days.
Conclusion
By interviewing front-line staff and service users the commission was able to understand their actual lived experiences. Many of the findings reflected failings that had been perpetuated over many years, which have been reported in a number of earlier reports and academic articles. However, the commission also found largely unreported successes throughout the country, which merit inter regional-sharing and adaptation to different settings and which are discussed later in this report. It is encouraging to see such initiatives, which, with sufficient and sustainable funding and support can benefit the future
generations. Although across the UK there is a policy commitment to improve child health outcomes it is evident that urgent action is needed to reduce poverty with much more investment and service development to achieve the desired goals.
A view from a community leader
Les Nicoll BEM Essex Fire and Rescue Service
I am a Community Builder for Essex Fire and rescue service (ECFRS), serving over 50 years as a firefighter and community worker.
Last Sunday I had a weekend with my children and grandchildren celebrating my 70th Birthday. Most of my time was spent being a Pirate, a ghost, a monster, a bank robber, a wrestler and a trampoline for my four beautiful boisterous Granddaughters. exaggerating my skills, making them scream and squeal, feeding their varied imaginations. Each of them healthy, well educated, able to relate to each other and enjoy adult company. Each of them, planned, anticipated, conceived out of love to parents who whilst not rich certainly all had jobs owned nice houses in good parts of the town. From conception each of these girls had all received good quality food, fresh vegetables, were not allowed sweets sugary drinks or exposure to cigarette smoke. Parents paid for them to go to nursery school, meeting and interacting with other children. Spending much happy time with loving adult family members.
My Role in the ECFRS involves me working in a very different environment. I spend a great deal of time working in Britain’s most deprived town. In an area of around 1,000 homes each tiny ex holiday lets, creating a shanty town, with more that 60% of its population receiving benefits. There is no heart to the village, Schools are a bus ride away, likewise Doctors, the nearest large supermarket is over 3 miles away, no football teams, no clubs, very large dependency on alcohol, drugs, foodbank donations, derelict buildings, rubbish strewn streets, running with vermin, slum landlords. Poor infrastructure, third and fourth generation poverty and unemployment. Two or three underfunded charities working incredibly hard swimming against the tide trying to make a difference. No money, no food, no help no opportunity, no way out. We continue to watch TV documentaries about this and other poor areas, read countless articles, with a not in my backyard amusement and interest, like the people Visiting Bedlam in the 19th century.
Would my/our grandchildren growing up in this environment thrive? Would they be as healthy? Would their imagination and social skills be as developed? Would their education offer limitless opportunities? We all know the answer.
Those of us reading this report are either already or are potentially people in power, with intelligence, influence people living my life and even better.
Will you nod your head and agree with some of the conclusions in this large and very well researched report? Will you quote some of the statements in your speeches, use them in your newspaper, working reports, university dissertation? We could of course use our privilege, our power, our time, and intelligence to make a difference? BUT WILL WE?
Chapter One: Liverpool Health Commission
Introduction
Liverpool Health Commission had its genesis in autumn 2018 as a tool to help implement the university’s strategic vision of being “a pioneering, modern civic university delivering solutions to the challenges of the 21st century” and its stated belief “in the power of sharing expertise, and of people coming together with a common purpose” (Liverpool John Moores University 2017) The Liverpool Health Commission was to be tasked with carrying out an independent investigation and analysis of particular public health or health care policy issues with the goal of making practical and realistic recommendations. Its broader aim was to make grounded contributions to debates at national level that will assist policymakers at all levels, who are seeking meaningful solutions to the harsh challenges facing public health and health care in the UK in the 21st Century.
The topic of marginalised women and children in the first 1,000 days of life (the time from conception to the end of the second year of infancy) was selected as the first commission by the executive leadership team Although there has been attention focused on the first 1000 days for several years by policy makers, we were concerned to explore not only what problems existed in this period of life but how those marginalised people had benefitted from some of the policy changes in recent years. Not only was this considered appropriate for the City of Liverpool due to its high levels of deprivation, but was also considered to be of wider national interest because its consequences are known to impact negatively on human growth and development at the crucial stages of early life.
Commission focus
As stated above, the first commission focuses on the topic of marginalised women and children in the first 1,000 days of life. In present times, taking this period to start from conception may be controversial, but by so doing it presents a unique window of opportunity. It is during the approximately 270 days from conception to birth that foundations for optimum health, growth, and neurodevelopment across the lifespan are established (United Nations 2017) Despite the majority of pregnant women in the UK seeking advice in the first trimester of pregnancy, it is often women from the many marginalised groups in our society who cannot or do not seek antenatal care or advice, and whose children may not benefit from the most optimal start in life
Large regional variations of poverty and infant morbidity and mortality exist within the UK. A recent KPMG report for the Liverpool Health Partnership
highlighted the harsh differences between the north and south of England and a recommendation was made for urgent academic work in four key areas, the leading one of which was identified as maternal and child health (Liverpool Health Partners 2017) Similar disparities are also found across Wales, Scotland and Northern Ireland. Maternal and child health concerns are therefore a key priority at different levels of health and social care across the UK. The causes and effects of the disparities are manifold and likely to vary across different parts of the country. They may include alcohol and drug dependency, a disproportionate number of migrants, people who only have a basic level of the English language or an above average teenage pregnancy rate. Such a list is not exhaustive but a catalyst for the start of the commission’s working life. Thus the Liverpool Health Commission focuses on this important area which has profound relevance regionally and nationally. Additionally, it addresses the United Nations Sustainable Development Goals 1-5, all of which are directly related to women and children’s health, bringing this topic into the dimension of global good health and the right to health (United Nations 2015).
Commission aims
The aims of the Liverpool Health Commission were:
• to conduct an independent investigation and critical analysis of current experiences in the first 1000 days of life in marginalised groups;
• to make grounded contributions to debates at national level that will seek to assist policymakers at all levels who are searching for meaningful, practical solutions to the problems and challenges facing the population and health sector across the UK in the 21st century.
Commission structure
The commission consisted of 12 commissioners, as well as a chair and an academic lead. The 12 commissioners were appointed by the LJMU ViceChancellor and all have held executive-level roles in public or professional bodies or come from a relevant professional or academic field (see Appendix 1)
Inquiry timeline
The commission was formally launched in May 2019. The opening hearing took place in November 2019, with the others (see chapter 3) following fairly quickly thereafter. The penultimate hearing was due to take place in April 2020 but was postponed because of Covid-19 and was finally held in September 2020 via Microsoft Teams. More information on the gathering of evidence and its analysis may be found in Chapter Three. The main report was drafted in
February 2021 and findings from around the UK were used to inform the final questions used to gather evidence in the Merseyside area in September 2021.
Inquiry report
This chapter has introduced the report. Chapter Two outlines key literature which has underpinned the commission’s work and places a strong emphasis on grey literature primarily from the UK, but also from international reports such as those issued by UN agencies and major charities. Chapter Three provides a detailed overview of how the commission collected its evidence and fulfilled its aims as well as outlining some of the limitations. Chapters Four –Nine synthesise findings from each locality visited by the commission and Chapter Ten offers concluding remarks. Appendix 2 reports on the schedule of visits.
Chapter Two: context of the commission
Introduction
A critical overview of the existing literature was conducted to inform the commission’s approach. It is beyond the scope of this report to synthesise and critically evaluate the numerous academic articles on the first 1,000 days of life published in peer reviewed journals. Instead, key reports from the United Nations, which have shaped initiatives in the UK, were reviewed as well as UK specific reports from a range of sources and are discussed in relation to the work of the commission.
United Nations reports
The United Nations’ (UN) Sustainable Development Goals were launched in 2015, following approval by the UN General Assembly (A/RES/70/1a). This collection of 17 goals are intended to be a global blueprint to be achieved by 2030 (United Nations 2015). While most could be considered by the commission, goal number 10 which aims to eliminate inequalities, is the most relevant to this commission’s work.
Before the term “first 1,000 (1,001) days” became popularised, the World Health Organisation (WHO) published a comprehensive report on essential nutrients for the developing child (World Health Organisation 2013). It highlighted interventions for pregnant women such as daily supplementation with iron and folic acid, intermittent iron and folic acid supplementation, vitamin A and calcium supplementation and reaching optimal iodine nutrition for non-anaemic pregnant women. Aimed at the global community, these recommendations apply to UK based pregnant women, particularly those disadvantaged by a sub optimal diet. The report discusses nutritional care and support for pregnant women during emergencies, a topic that has re-emerged during the Covid-19 pandemic. It also discusses nutrition of children in the first six months of extrauterine life and, drawing on evidence from several systematic reviews and previous UN reports, promotes a policy of six months exclusive breastfeeding. This remains an area in which the UK’s performance is poor and has been discussed at all commission hearings.
Launched in January 2017, the UNICEF publication “Early moments matter” catalysed the “first 1,000 days” initiatives throughout the world (United Nations 2017). Like the above WHO report, it focused on breastfeeding. However it also highlighted issues such as paid parental leave, high quality, accessible child services and grants for all families with children i.e. family friendly policies. Different countries have used this report as a springboard for developing their own policies in different ways. The UK’s response mainly
focused around the “Baby Friendly Initiative” which, since 1994, has been promoting breastfeeding in an effort to increase the currently poor rates throughout the country (UNICEF United Kingdom 2021).
This initiative works with public services to provide families with effective infant feeding support, enabling them to make an informed choice about feeding, get breastfeeding off to a good start, overcome challenges and feed their babies responsively. It includes giving information about skin- to-skin contact, understanding their babies’ cues, how to respond to them and implementing safe sleeping practices.
However, UNICEF UK cautions that offering effective support to parents is only possible when practitioners have sufficient knowledge and skills. When practitioners lack this knowledge and offer conflicting information, they can discourage mothers so undermining confidence in their parenting decisions. Research has found gaps in knowledge, skills and attitudes of health practitioners, resulting in poor provision of information and support to mothers (Maxwell 2019).
As well as knowledge about breastfeeding, UNICEF UK authors report that health professionals need the skills to communicate with mothers in unambiguous, beneficial, appropriate and non-judgemental ways.
A study on access and barriers to provision of maternal health published by the European Parliament (European Parliament 2019) suggested that the major barriers to provision of sexual and reproductive health services are (pp. 33-37):
• language and communication with health professionals;
• health professionals’ lack of experience in dealing with ‘difference’;
• structural inequalities;
• organisational barriers;
• culture and faith;
• mental health,
• fear and social stigma.
While this study refers to the EU Member States, including the UK at that time, in their totality, the same barriers are still to be seen in the UK and have been to the fore during the commission’s lifespan.
Reports from the UK
Turning to relevant reports from the UK, the devolution of various responsibilities from the Westminster parliament to Northern Ireland, Scotland and Wales means many health -related reports discussed are specific to one of the four nations. The Rowntree Reports on poverty are an exception and will now be considered in detail before moving on to other relevant reports.
The (Joseph Rowntree Foundations 2017) detailed report on poverty in the UK showed that consistent poverty rates are highest among families with young children (p. 3). A third of children lived in poverty from the beginning of the 21st century, falling by 15% from the period between 1994/95 and 2004/05 to 28% of children. The child poverty level fell to its lowest (27%) in 2011/12 but began to rise again after that, reaching 30% in 2015/16.
The 2021 report (Joseph Rowntree Foundation 2021) states that 14.5 million people in the UK were living below the poverty line before the onset of coronavirus, equating to more than one in five people. They provide details of overall trends in the different countries (p. 18):
• England: poverty levels have worsened, raising from 21.3% in 2011/122013/14 to 22.3%. Within England, London has the highest poverty rate, which is broadly stable over time. All other regions show a flat or worsening position except the East Midlands.
• Wales: poverty levels have experienced very little change, albeit rising marginally from 22.7% in 2011–12 - 2013/14 to 22.8%.
• Scotland: lower levels of poverty (currently 19.2%) worsening from 17.8% in 2011/12 to 2013/14).
• Northern Ireland: poverty levels have improved, lowering from 20.8% in 2011–12 - 2013/14 to 19%.
While the 2021 report primarily focused on “in-work poverty”, this undoubtedly affects children. The authors note the steady increase in child poverty, with children constituting a vulnerable group disproportionately likely to be pulled into poverty. The authors continue by observing that vulnerable groups already struggling to stay afloat have borne the brunt of COVID-19’s economic and health impacts. Particularly relevant to the commission’s work, these include:
• part-time workers, low-paid workers and workers in sectors such as accommodation and food services where there are much higher rates of inwork poverty;
• Black, Asian and minority ethnic households;
• lone parents – mostly women, many of whom work in hard-hit sectors –who are more reliant on local jobs and more likely to have struggled with childcare during lockdown.
Low-income families with children have been particularly affected by COVID19. Research carried out on behalf of the Joseph Rowntree Foundation and Save the Children (Maddison 2020) found that six in ten families with children in receipt of either Universal Credit or Child Tax Credit have had to borrow money since the beginning of the pandemic. Many of these families have relied on not only on formal lending such as credit cards, loans or overdrafts
but also payday loans. According to (Porter 2020), families who receive benefits are twice as likely to have borrowed money from family and friends as families who do not.
Lone parents continue to have the highest in-work poverty level of all family types and are disproportionately affected by barriers that prevent them escaping in-work poverty. They are more likely to be women, working in a lowwage sector, working fewer hours, and restricted by childcare and transport. The pandemic is likely to have had a big impact on people in this group because of the sectors in which they work, and their ability to work depends on childcare, which may have been unavailable during the national pandemic restrictions In-work poverty is also higher for black, Asian and minority ethnic workers than white workers, and is highest for Pakistani and Bangladeshi workers (Joseph Rowntree Foundation 2021). Consequently, ethnic minority families have also been hit hard by COVID-19. Compared with white families, they are more likely to have experienced an income loss and to have cut back on essential spending (Maddison 2020).
Another relevant recent UK wide initiative is that of the Royal Foundation. The Foundation commissioned a large study in 2019 to investigate attitudes surrounding child-rearing from conception to five years in all four UK nations. It comprised a “face to face” study of 3733 parents followed by two online surveys, a qualitative study of a sub-sample of 40 parents drawn from the face to face survey and an ethnographic report of 12 families and four community leaders. Their main conclusions are clustered into three key areas (p. 47):
1. The importance of promoting education and dissemination of evidence on the primacy of the early years to parents, parents of the future and the whole of society.
2. The need to cultivate and sustain more support networks for parents to enhance their mental health and wellbeing.
3. The need to encourage society as a whole to be more supportive of parents, carers and families in the early years.
Perhaps the most significant finding - related to the first of these themes - was that very few participants recognised or understood the importance of the brain’s development in the first 1,000 days and the impact this would have on the whole life of the child. The need for trust to be established between parents and service providers was a further key finding, one of relevance to the present commission’s work (The Royal Foundation 2020).
Another UK wide charity, the WAVE Trust, focuses on tackling the root causes of trauma related to adverse childhood experiences (ACEs), which are endemic in society. WAVE’s most recent report (WAVE Trust 2018) reviews global
systemic and methodological approaches taken to protect children from the threat of severe and multiple disadvantages caused by ACEs. While targeting the age group from 2-18, rather than the first 1000 days, some of their seven key messages are relevant to the present commission’s work as these identify the systems which are most likely to bring about improvements in the services for the most disadvantaged children and young people. One of these key messages states “parental dysfunction is a major cause of childhood ACEs; levels of youth and adult dysfunction are higher in the UK than other western European countries” (p. 16). It particularly targets teenage parents and recommends that services focus efforts on the disadvantaged wards that have ten times the levels of teen births found in the non-disadvantaged.
The final key message from the Trust states that “a national shift to a userfocused, trauma-informed care system characterised by ACE-awareness, followed by adoption of a pedagogical approach across all aspects of children and family services, would protect against severe, multiple disadvantage” (p. 5). WAVE recommend flat organisational structures such as already implemented in parts of Wales and Scotland as they have been effective in improving inter-agency collaboration, streamlining and simplifying working and reporting methods and replacing traditional silo cultures with effective approaches.
England
In 2009, the Government launched the Healthy Child Programme (HCP), with the aim of improving outcomes and reducing inequalities through a combination of universal provision and targeted support. The HCP is central to the delivery of preventative and early intervention services for children and families in England. Since its inception, there have been several key reports that directly address its work. The Marmot review (Marmot 2010), which focuses on reducing health inequalities in England, reported that its centre point was a “life course perspective” noting that “disadvantage starts before birth and accumulates throughout life” (p. 20). Drawing on evidence from previous reports, academic papers, statistical data and interviews, the review urged that action to reduce health inequalities had to start before birth and be followed throughout the child’s lifetime, as that is the only way in which the close links between early disadvantage and poor outcomes are able to be broken. For this reason, the committee recommended that giving every child the best start in life be its highest priority recommendation. A follow up was published in 2019, in which the recommendations for the best start in life were very similar ie:
• Increase levels of spending on early years and as a minimum meet the OECD average and ensure allocation of funding is proportionately higher for more deprived areas.
• Reduce levels of child poverty to 10 percent – level with the lowest rates in Europe.
• Improve availability and quality of early years services, including Children’s Centres, in all regions of England.
• Increase pay and qualification requirements for the childcare workforce (Institue for Health Equity 2019)
The Marmot review set in train a series of actions and has formed the basis for subsequent reviews of the first 1,000 days, all of which acknowledge the critical importance of this time. The major examples are presented below.
In 2014 a cross party manifesto (Leadsom, Field et al. 2014) stated that:
“[pregnancy] can also be a chance to affect great change, as pregnancy and the birth of a baby is a critical ‘window of opportunity’ when parents are especially receptive to offers of advice and support” (p. 5).
The manifesto noted that maternal stress is likely to affect the fetus or baby negatively, therefore, ensuring that the brain achieves its optimum development and nurturing during the peak period of growth in the first 1,001 days is crucially important and enables babies to achieve the best start in life. They further note the vital need for good bonding that will lead to better and longer lasting attachment between the baby and its primary caregiver(s). Since Bowlby’s work in the 1960s on attachment (Bowlby 1969), successive studies have shown that a baby’s social and emotional development is strongly affected by the quality of the attachment (Zeanah, Berlin et al. 2011)
At the time of the report’s publication, Leadsom et al noted that babies are disproportionately vulnerable to abuse and neglect than older children. They estimated that 26% of babies (198,000) in the UK were living within complex family situations of heightened risk where there are problems such as substance misuse, mental illness or domestic violence, with 36% of serious case reviews involving a baby under one.
The report’s main recommendation was that the best chance to turn the effects of negative factors around occurs during the first 1,001 critical days. They stated that every child deserves an equal opportunity to lead a healthy and fulfilling life, and with the right kind of early intervention there is every opportunity for secure parent infant attachments to be developed. They further noted that, in accordance with attachment theory, at least one loving, sensitive and responsive relationship between a baby and an adult caregiver teaches the baby to believe that the world is a good place and reduces the risk of them facing disruptive issues in later life. The final recommendation of the
manifesto states that, it is imperative that how children are raised is guided and influenced by the attachment principle and its evidence. However, attachment was a theme that informed the work of (The All Party Parliamentary Group for Conception to Age 2 2015) Their report states that groundwork for good citizenship occurs in the first 1,001 days as “ A society which fails to deliver it generates enormous problems” (p. 3). Its main focus is perinatal mental health and it notes that the cost of omitting to deal adequately with perinatal mental health and child maltreatment are high, closely linked and largely avoidable. Furthermore, the authors also stress the vicious circle where one generation of drug abusers, for example, passes the problem to the next generation, meaning the resultant social disruption, inequality, mental and physical health problems and cost perpetuate and multiply.
The report outlines two main aims:
1. Creating children who at the end of their first 1,001 days have the social and emotional resources which constitute a strong foundation for good citizenship.
2. Preventing high intergenerational transmission of disadvantage, inequality, dysfunction and child maltreatment.
It then outlines nine recommendations with potential approaches that could be taken to achieve them emphasising the importance of an inter-agency working and a national strategy, under the supervision of a Minister for Families and the Best Start in Life:
A more recent cross-party report led by Sarah Wollaston (Committee 2019) focused specifically on the first 1,000 days of life. Its data were collected in 2018 and comprised 86 written submissions, 80 posts on an onIine forum, three sessions of oral evidence taking, three focus groups and a one site visit to Blackpool. Both the written submissions and oral evidence were provided from health service providers and third sector organisations. The organisation chosen for the online forum was Mumsnet, a popular choice for mothers experiencing difficulties, from which the commission heard directly from parents about their experiences of pregnancy and early parenthood, as well as the services they used during this time. While aims of this commission were broadly similar to that of the present one, our focus has been more aimed at collecting evidence from the people providing hands on services and those who receive them.
As well as acknowledging the first 1,000 days of life as a critical phase during which the foundations of a child’s development are laid, the cross-party report
(Committee 2019) noted that exposure to stresses or adversity during this period can result in a child falling behind their peers developmentally. Thus, they conclude that intervening more actively in the first 1,000 days of a child’s life can improve children’s health, development, life chances and make a fairer, more prosperous society.
The committee focused on a broad definition of health, noting that enhancing the ability of services to support and empower parents and families to take care of themselves and their children is vital, but not sufficient. Other stressors such as poverty, poor housing and unstable employment also act against the ability of parents and families to create a safe, healthy and nurturing environment for their children. Its findings noted significant variations in the way local areas prioritise and support families in the first 1,000 days. Similarly, it found significant variation in staffing numbers, skills and the level of contact with families within the health services.
The committee also pointed out that improvements in service provision will only provide a ‘sticking plaster’ if they are not targeting the conditions in which some of this country’s poorest children live. As with previous reports, the government was urged “to lead by developing a long-term, cross-government strategy for the first 1,000 days of life, setting demanding goals to reduce adverse childhood experiences, improve school readiness and reduce infant mortality and child poverty” (p. 3) They expand on this by saying that the government should “coordinate the work of multiple departments and agencies; provide strategic direction to local areas and hold them to account; and ensure the issue remains a priority and continues to attract resources” (p. 27). They go even further by recommending that the Minister for the Cabinet Office should be given responsibility to lead the strategy’s development and implementation across government, with the support of a small centralised delivery team thereby placing it at the highest level of government.
Ten years after its inception, the committee called for the Healthy Child Programme to be revised, improved and given greater impetus, recommending that it begin before conception to come into line with the first 1,000 days initiatives. This would involve extending home visits by Health Visitors beyond the age of 2½ years, becoming more family focused, and ensuring that children, parents and families experience continuity of care during this critical period. Such an approach would also identify children and families who need targeted support earlier. In many cases women seek help during pregnancy even if they are not registered with a GP, so this time may offer such an opportunity.
The most recent report comes from the UK government’s commission, chaired by Andrea Leadsom, into the first 1001 days. The aim of the review was “to
improve the health and development of babies in England” (H.M. Government 2021) p. 7. The review comprised a questionnaire, to which there were 3,614 responses and virtual visits to London, Essex, Devon, Leeds, Manchester and Newcastle on Tyne. Additional information was collected through engaging with the online platform “Mumsnet” and a twitter feed.
1. The major focus of the review was to ascertain how families could be better supported. Two major themes were identified: each with three action areas. Ensuring families have access to the services they need comprised: Seamless support for families: a coherent joined up Start for Life offer available to all families, a welcoming hub for families: Family Hubs as a place for families to access
2. Start for Life services and the information families need when they need it: designing digital, virtual and telephone offers around the needs of the family. Ensuring the Start for Life system is working together to give families the support they need included: an empowered Start for Life workforce: developing a modern skilled workforce to meet the changing needs of families, continually improving the Start for Life offer: improving data, evaluation, outcomes and proportionate inspection and leadership for change: ensuring local and national accountability and building the economic case.
Scotland
The Scottish government’s “early years framework” (Scottish Government 2009) drew on evidence from several relevant disciplines to inform its policy of giving all children the best start in life. The framework defined early years as pre-birth to the eighth birthday. The report acknowledged that while early intervention has relevance to a wide range of social policies, it is in the earliest years that the best opportunities often arise. The four principles of early intervention the authors identified were:
1. all children should have the same outcomes and the same opportunities;
2. children at risk of not achieving those outcomes should be identified and steps taken to prevent that risk materialising;
3. where the risk has materialised, effective action must be taken;
4. the government’s agencies should work to help parents, families and communities to develop their own solutions, using accessible, high quality public services when required.
The report acknowledged that its ambitions could not be achieved without change and identified 10 elements of transformational change, all of which are relevant to the present commission’s work. The authors also put a renewed
focus on zero to three as the period of a child's development that shapes future outcomes.
A secondary analysis of data from the Scottish Household Survey (Barens and Lord 2012) used seven key indicators to define disadvantage as experiencing low income, “worklessness”, no educational qualifications, overcrowding, ill health, mental health problems and a poor neighbourhood. These criteria are of interest to the present commission. This report indicated that at the time of reporting there were approximately 24,000 households with children who had four or more of the seven listed disadvantages, the majority being in the south-west of the country.
A follow up report published by the government in 2019 formed phase one of the wider study ‘Scottish Study of Early Learning and Childcare’ (Scottish Government 2020). This report investigates whether increasing the hours of government funded early learning and childcare for children aged three to five (and some eligible two-year-olds) improves outcomes for children and parents, particularly those who at risk of disadvantage. The data showed that a majority of two-year-old children attending day-care did not have the crucial life skills and qualities they need if they are to grow up being healthy and valued members of society.
Other reports in Scotland mainly focus on regional initiatives but the maternalinfant survey (Scottish Government, 2017) investigated Scotland’s position in relation to achieving optimal health and nutrition for mothers and infants prior to, during and after birth. The report acknowledged that the diet and nutritional status of mothers before and during pregnancy and the subsequent nourishment received by infants is associated with the long-term health of the population. It additionally recognised the increasing importance of maternal preconception health and the influence this has on the likelihood of an infant later developing chronic diseases later in life. The survey was carried out at approximately 20 weeks of pregnancy, at eight-12 weeks and eight-12 months after giving birth. Its aims were primarily to investigate the adjustments women made to their diet prior to and during pregnancy, their plans for infant feeding and how they actually fed them. Additionally, they were asked about the “Healthy Start” programme and how they would use their vouchers. As each time point surveyed involved a different cohort of women it was not possible to form a longitudinal picture.
Wales
A national consultation by the Welsh Assembly on the first 1,000 days took place from 2016-2017. Several of the submissions made to the inquiry provide a wide ranging picture of the situation. Both NHS Confederation (Welsh NHS
Confederation 2016) and Public Health Wales (Public Health Wales 2016) note the inequalities throughout the country and the difference in outcomes for babies born in the highest and lowest social classes.
The NHS Confederation report particularly comments on the effectiveness of the “Flying Start” programme in the health boards where it is available. Conversely, Public Health Wales takes a broader approach, highlighting the prevention of adverse childhood experiences through provision of universally accessible preventative health services. In terms of possible solutions, it referenced the “triple p”, (Positive Parenting Programme) in Ireland that is delivered to three to seven year olds with good results, and recommended that the evaluation tools used could be replicated in areas of Wales which have adopted the Flying Start and/or Families First programmes.
Wales has had a focus on early years policy for many years and revised its Healthy Child programme in recent years (Welsh Government 2020). This programme has three levels of health prevention activity for the first 1000 days of life: universal, enhanced and intensive. The key health professional is the Health Visitor who interacts with the family from early pregnancy until the child is of school age at whatever level is necessary.
The current programme of the Welsh Government (Welsh Government 2021) highlights substantial work on improving services for children especially those that are ‘looked after’. It includes funding childcare for more families where parents are in education and training, continuing to support the flagship Flying Start programmes, preventing families breaking up by funding advocacy services for parents whose children are at risk of coming into care. They also seek to provide additional specialist support for children with complex needs who may be on the edge of care, explore radical reform of current services for looked after children and care leavers, eliminate private profit from the care of looked after children, fund regional residential services for children with complex needs ensuring their needs are met as close to home as possible and in Wales wherever practicable and strengthen public bodies in their role as ‘corporate parent’.
Northern Ireland
Amongst the recommendations from a 2013 research based paper (Perry 2013) two are of immediate relevance to the present commission:
• The fragmentation of responsibility for early years provision and childcare across departments and arm’s-length bodies;
• Areas of overlap in Learning to Learn and Towards a Childcare Strategy and the extent of joint working on these policies.
A later briefing paper emphasises the need for improved maternal health as well child health services (Perry 2016).
The current “Sure Start” programme offered in 38 localities of Northern Ireland supports children in disadvantaged areas from pre- birth until four. Since its inception in 2016, three national evaluations have taken place, the most recent in 2020. The latest review initially asked for areas to nominate themselves on the basis of their positive outcomes and, from the nominations, selected projects representative of a cross section of geographical areas, size and range of lead and accountable bodies and Child Care Partnerships for inclusion. A small inspection team then visited the sites and identified strengths and weaknesses of each site (Education and Training Inspectorate (Northern Ireland 2020).
Relevant key strengths were identified as a more consistent and effective culture of reflection and self-evaluation, the positive impact of the services and programmes, the highly effective practitioners, from varying professional disciplines and effective inter-disciplinary team collaboration and sharing of information to identify and follow up on the needs of families and children at the earliest stage.
A well-established charity, “Early Years”, is also active in the country, promoting high quality care for children up to 18 years. Their 2019 annual report show the charity, as well as being active in providing early childhood education, has a strong advocacy and lobbying role, with its basis in the UN Charter for the Rights of the Child. It acts as the lead partner in six of the Sure Start Programmes ensuring a link between education and health (Early Years 2019).
Conclusion
In an area where there have been many active partners involved with service delivery as well as numerous academic researchers at work, there are a plethora of publications. We have chosen to give some background from those we consider to be most relevant in informing the approach adopted by the present commission.
Chapter Three: The Liverpool Health Commission’s approach
Introduction
Informed by the numerous reports on the first 1001 days, the Liverpool Health Commission set out to explore current experiences in local areas to inform decision makers locally and nationally.
Refining the topic of investigation
After discussion by the Commissioners, it was agreed that we could never have an exhaustive list of marginalised groups, so we decided to leave the question open as to what constituted “disadvantage”. We concluded that the main focus of the commission would be on poverty as it is that which underpins many of the disadvantaged groups we discussed (Joseph Rowntree Foundations 2017). Following these discussions, as stated in chapter 1 the aims are:
• To conduct an independent investigation and critical analysis of the significant health area of the first 1000 days of life in marginalised groups;
• To make grounded contributions to debates at national level that will seek to assist policymakers at all levels who are searching for meaningful, practical solutions to the harsh problems and challenges facing the health sector across the UK in the 21st century.
Locations for collection of evidence
The areas of multiple deprivation in the UK and areas with high levels of child poverty were sought using data from the Child Poverty Map of the UK report (End Child Poverty, 2016). The most recent map is shown in Fig 1 below showing that areas which the commission visited are still amongst those most deprived in the UK.

Note: After housing costs. Map and data use 2019 local authority boundaries. Reprinted from UK Poverty 2022. By Joseph Rowntree Foundation, 2022. Copyright 2022 by Joseph Rowntree Foundation. Reprinted with permission.
Other factors to be taken into consideration were to have sites have a geographic spread and to avoid places which had been the subject of other recent major inquiries. The final choices therefore were:
• Morecambe, a former seaside resort in north-west England which catered mainly to families from Yorkshire, who took advantage of the rail links
developed in the mid 19th century to link the county with the new harbour. Its decline as a holiday destination began in the late 20th century when its two piers were damaged and demolished and new attractions failed due to poor financial planning. Its current population of about 35,000 comprises mainly retired people and young families approximately 15% of whom are considered to be living in poverty. It is a predominantly white town with only 5% of the population being of black or other minority ethnic groups. A few services for women, children and families are provided in the town of Morecambe for its residents and those of nearby villages but the majority of them are based in the nearby county town of Lancaster. An ambitious plan for regeneration of the area primarily through tourism but including digital health and liveability plans was launched in 2017, but due to Covid, much of it is currently on hold. Maternal and child health services are provided by Morecambe Bay NHS Trust, which was subject to an inquiry into maternity services in 2016 and continues to be under CQC scrutiny.
Figure 2 Morecambe Bay Action Plan
Reprinted from Costal Community team draft 2017-22(Morecambe Bay Coastal Community Team 2017)

• Middlesbrough in north-east England, a previously heavily industrialised town, was a centre for iron and steel works and shipbuilding. As such it was an attractive area for inward migration, mostly from elsewhere in the UK, seeking manual work. In the second half of the 20th century most of this work disappeared, leaving an above average unemployment particularly amongst second and third generations descended from these immigrants. The main employers now are the James Cook University NHS Trust and Teesside University. Despite these two large employers, figure 3 depicts high numbers of unemployment and low numbers of employment in Middlesbrough from July 2020-June 2021 thus indicating high levels of income deprivation.
Employment and Unemployment (Jul 2020-Jun 2021)
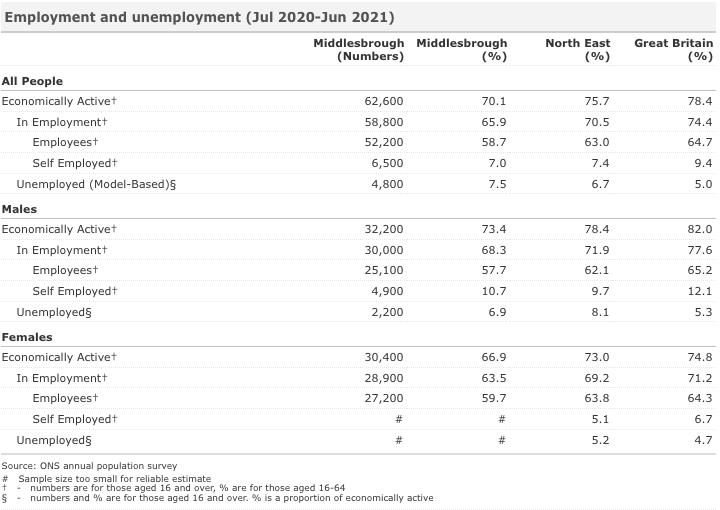
Note: For Middlesbrough. Reprinted from Labour Market Profile- Middlesbrough. By nomis Official Labour Market Statistics, n.d, www.nomisweb.co.uk/reports/lmp/la/1946157060/report.aspx#tabempunemp Copyright n.d. by Crown Copyright Reprinted with permission.
• Clacton-on Sea, in south-east England, was originally a stone age settlement and continued to thrive in Roman and medieval times. It became a popular
seaside resort in the early 20th century as it was in easy commuting distance from London by rail. It reached its peak in the decade following World War II. Now it remains popular for day visitors. Figure 4 indicates the positive economic impact tourism has had on the district of Tendring and the number of full time jobs tourism has brought to the area. Despite this, Clacton-on Sea is still considered a deprived area, and Jaywick which lies on Clacton-on Sea’s outskirts is consistently ranked one of the most deprived areas of the UK. It has a small maternity unit and many community services delivered jointly by the Tendring District Council, Essex County Council and Colchester NHS Trust.

Note: Reprinted from Tourism Strategy for Tendring 2021-2026 . By Tendring District Council, n.d. https://tdcdemocracy.tendringdc.gov.uk/documents/s33219A8%20Appendix%20Draft%20Tourism %20Strategy%202021%202026.pdf. Copyright 2022 by Tendring District Council. Reprinted with permission.
• Derry/Londonderry lies in the west of Northern Ireland and is its second largest city. It lies very close to the border with the Republic of Ireland. Its strategic location has seen its continued use as a port for several centuries. It was also a major centre for textile manufacturing until the 1970s and a small remnant of this remains. The “Troubles” of the late 20th century are thought to have originated here with widespread violence from the 1970s until the 1990s. Even after the Good Friday agreement some sectarian violence lingered but with
considerable investment by local, national and UK governments and international companies leading to employment it is considered a safe and stable place. Despite this, figure 5 outlines that there were low employment rates in the Derry City and Strabane District council from 2009-2018. Thus, indicating high levels of income deprivation. It has a major maternity unit at Altnagelvin NHS Trust and provides services to the surrounding communities.

Note: DCSDC is an abbreviation of Derry City and Strabane District Council Reprinted from Employment. By Derry City and Strabane District Council, n.d.
https://www.derrystrabane.com/getmedia/99ea2a21-86a1-4e4a -bc6a -0e006dc5bb4a/AEmployment-280619.pdf
• Neath/Port Talbot is an area in south Wales located about 10 miles to the east of Swansea and stretches from the south coast to the border of the Brecon Beacons national park in the hills. Its industrial past is similar to that of Middlesbrough, but economically it also has a large rural population stretching up a number of valleys. Its main employer remains the steel works although the workforce now numbers less than 50% of what it was in its heyday. The town houses a small maternity unit, with the main university hospital located in Swansea. A large number of community services are provided for the rural population. One such service is the Flying Start Health Visitors. Figure 6 outlines the number Flying Start Health Visitors allocated to under fours in Neath Port Talbot. It also indicates the high number of under fours that cannot access this service because of where they reside, despite living in income deprivation.

Note: Reprinted from Y 1000 Diwrnod Cyntaf yng Nghastell-nedd Port Talbot/The First 1000 Days in Neath Port Talbot By CymruWellWales, 2017. https://www.derrystrabane.com/getmedia/99ea2a2186a1-4e4a -bc6a-0e006dc5bb4a/A-Employment-280619.pdf
• Lanarkshire is located in south-west Scotland with the health board providing services for both the north and south Lanarkshire counties. It is an inland area which was dominated by coal mining and associated iron and steel works until the 1980s, with the major steel works at Ravenscraig closing in the early 1990s with approximately 10,000 job losses. Unemployment is still high in both North and South Lanarkshire, as depicted in figures 7 and 8 The University of the West of Scotland has one campus in the area. The major maternity and child services are located at Wishaw General Hospital, though the Lanarkshire Area Health Board have satellite services at its other hospitals and a large community-based service.
7
Percentage of Unemployed Individuals in South Lanarkshire
Note: Individuals aged 16-74 in 2011. Reprinted from South Lanarkshire: 2011 overview. By Scotland’s Census, https://www.scotlandscensus.gov.uk/search-the-census#/explore/snapshot Copyright n.d by Crown
Copyright. Reprinted with permission.
8
Percentage of Unemployed individuals in North Lanarkshire

Note: Individuals aged 16-74 in 2011. Reprinted from North Lanarkshire: 2011 overview. By Scotland’s Census, https://www.scotlandscensus.gov.uk/search-the-census#/explore/snapshot Copyright n.d by Crown
Copyright. Reprinted with permission.
• Merseyside was the final area to be considered because it was the “home” of the commission. Located in north-west England, it is a port area which was extensively bombed in World War II. It has subsequently been amongst the most impoverished areas of England. Its health outcomes and life expectancy are significantly worse than the whole of England as depicted in figure 9.
Women and children’s health services are provided by several maternity hospitals of which Liverpool Women’s Hospital is the largest with approximately 9,000 births per year and offering many specialist services. The main children’s hospital, Alder Hey, is a regional trauma centre with in-patient facilities for 300 children. Many community and third sector services are also found in the region.
Note: Liverpool 2019, Reprinted from Liverpool, Local Authority Health Profile 2019 By Public Health England, 2020. https://fingertips.phe.org.uk/static-reports/health-profiles/2019/e08000012.html?area-name=liverpool. Copyright n.d. by Crown Copyright Reprinted with permission.

Collecting evidence

Initial contact was made with each area through the local council offices where officers responsible for child health services in the area agreed to support the project by assisting with provision of venues and providing further contacts in the health and council services as well as voluntary sectors and service user groups. There was no initial attempt made to seek out specific organisations, rather to see who would come forward and from there to use a snowball technique to gain further participants. A complete list of participants and organisations providing evidence is located in Appendix 3.
Each visit lasted from between 1.5-2.5 days and sessions with individuals lasted from 20 minutes to 1.5 hours. An open process was initially adopted where those giving evidence were asked to talk about the strengths and weaknesses of the service they provided or received. By the third session an outline of questions used to frame semi-structured interviews was generated from the initial sessions. When the final focus groups were held in Liverpool the questions were very targeted having been generated from the commission’s earlier findings (see Appendices 4 & 5). Publicity was given to the project via local and regional radio and television networks in all locations.
Analysis
As the participants in each venue varied, there has been no attempt to quantify responses. Rather, we have undertaken a qualitative, thematic analysis using an inductive approach (Braun and Clark 2013). All analysis was undertaken manually. Each transcript was read and main themes highlighted. Themes from individuals were then compared within each visit and commissioners who had been involved asked to review and amend them if necessary. Finally, the themes were merged from each site and integrated into one common whole. This inevitably means that something that is particularly important in one single area has been omitted from the data synthesis chapter.
Chapter Four: Findings
This chapter together with those immediately following it takes the reader through the main findings of the commission. Each of these chapters presents some quotes to illustrate the breadth of evidence gathered. The subthemes in each chapter provide some insight into both positive and negative iniatives reported to commissioners. Recommendations are made at the conclusion of each chapter.
Finance
This chapter discusses the financial issues that were raised by staff as significant issues for service users. These factors include Universal Credit, service user budgeting capacity, benefits eligibility awareness, working culture and the perpetuation of a benefits culture.
Universal Credit
Respondents suggested that Universal Credit has been a “nightmare” as "There's a six-week wait." So, if you're a family that's relying on money and have a six-week wait, what are they meant to do for six weeks?” A recent survey of universal credit claimants supports this statement as figure 10 indicates that the majority of claimants surveyed on the Trade Union Congress website were unable to cope with a five week wait.
10
Universal Credit Claimants – Were You Able to Cope With the Five-Week Wait?

Note: Online Survey on the Trade Union Congress website from 19th May-20th of June 2020, Reprinted from Universal Credit and the impact of the five week wait for payment, By Trade Union Congress, 2020, https://www.tuc.org.uk/sites/default/files/202011/Universal%20credit%20and%20the%20five%20week%20wait%202020.pdf. Copyright 2022 by Trade Union Congress. Reprinted with permission.
Furthermore, increases in service user employment impacts their Universal Credit. For example, a health visitor reports: “I visited somebody this morning who’s had their Universal Credit cut by half because it’s been deemed that
Figure 12: Universal Credit claimants – Were you able to come with the five-week wait? (Trade Union Congress, 2020, p.8).
she’s fit enough to work and her money wasn’t great as it was and it’s gone down to like just under, well around £400 a month and it’s her and a baby. I mean, that is horrendous isn’t it” 1. In this circumstance staff explain that “It’s that fine balance of upskilling parents to a certain level but then not impacting on the money they’ve actually got to spend on their families” 2 .
Budgeting
Respondents highlighted how extreme family poverty is sometimes influenced by service user struggles with personal budgeting: “I've got one mum and she just lives on benefits, but she budgets it so well. You know, she just can do it, where other families just can't” 3. Issues with how professionals saw service user as managing their limited finances were also presented: Despite Family Solutions “going in to help them with budgeting and help them with bills and time to manage. She’s coming to us on a regular basis saying, “I haven’t got any money for food. I can’t feed my kids. So it’s really difficult because we can educate and educate and educate, actually unless they want to participate in that, it’s really hard”. She expressed concern that this is linked to a dependency culture. For example, regarding foodbanks she says we are “creating an issue because then you’re providing food for somebody on a regular basis”, however “We’ve had to do that because there’s a huge need for it” 4
Eligibility unawareness
A further problem is that service users are often unaware of the full extent of financial supports for which they are eligible or are prevented from applying due to psychological barriers of mental ill health. For example someone had “bailiffs banging on his door. He had a young child. And he’d gone into a spiral of depression, because he didn’t think he could get out of that” however “he had such bad anxiety that he had only ever applied for the housing benefit and one of his benefits he had not applied for” because it involved going in person to the job centre. With Home Start help this service user greatly improved in his mental health and gained about “£80 more to live on” and now has “the
1 Neath, fi3d3d14
2 Middlesbrough, fia7cc1e
3 Morecambe, fi03e99c
4 Clacton, fi2b104e
benefits he should have had, but he would never have had if we hadn’t have gone in” 5 .
Benefits’ culture
Problems of Universal Credit, budgeting, and eligibility unawareness feed into the perpetuation of pre-existing benefits’ cultures within communities. Confusion over what service users are entitled to is not restricted to service users themselves, but also staff, unable to keep track of all the changes may give wrong advice.
Respondents acknowledge the existence of a benefits, non-working culture which has been cyclically passed down through families across the generations. Individuals who have had a negative “experience at school, bullying problems, mental health problems” then “leave school early or with no qualifications and very much a low self-esteem or mental health problems. Then obviously they become parents and they've got no confidence in the workplace or no aspirations to work” 6. A voluntary worker says “We need to get the kids to aspire to move away, even if they move away a mile” however “what we're up against is, of course, that mum and dad are partying every weekend…The kids get dragged into this, so then we have children of eight and nine smoking, of 10 and 11 drinking alcohol, sexually active around 13 and 14, and that's because they're just following this trait” 7. This respondent felt that such examples within these communities influences young people’s educational attainment, teenage pregnancy, ill health, personal aspirations and ultimately financial hardship and dependency upon benefits, creating a cycle of generational poverty.
Working poverty
Hard working families often live in poverty because the government provision of 30-hours free childcare a week is determined by the availability offered by childcare providers. This may not match the hours of the mother’s job, so mothers “want to work these hours, but they can't fit the childcare in these hours and it just doesn't work. So, then they'll end up giving up work” 8. Some respondents argued that irrespective of whether one parent is working, both parents work or neither are working, they may be in equal need of financial
5 Clacton, fi07d21c
6 Morecambe, fie072b4
7 Clacton, fief656b
8 Morecambe, fi03e99c
support due to the combination of high childcare costs and low wages. The most likely scenario is “that there's only one parent that's there and they're trying to work. Then, actually, the local economy around here can be quite grey. It's not all payroll orientated” 9. This creates the situation where “We’ve got quite a few parents who are so proud, going out and doing work, but would be far better off, in some instances, on benefits and universal credit” 10, and the realities of working poverty deter many families from working.
Community participation
Recognising the extreme financial deprivation where “poor people don't buy clothes in the charity shop because they can't afford them” 11 but faced with a complete lack of funding respondents have found ways to help with little or no funding. These endeavours acknowledge that people within the community want to help and local charitable or health organisations want to offer support. “With the little charities that I run, I am never short of volunteers. I have loads of people” and “There are loads of these organisations around that are really working hard for the community, and they're run by absolutely wonderful people. Lovely people” 12. Social media was also highlighted as a tool for spreading the word about charitable ventures across the local community, saying “That's my tool. Facebook, by keeping it friendly, people help. If you're not slagging people off, if you're not complaining, if you use Facebook for the tool that it is, it's amazing” 13 .
Income maximisation and staff financial education
A pilot project in which Health Visitors were given additional skills to equip them to discuss financial situations was very successful in maximising serviceuser income and has received national recognition alongside increasing staff confidence in having difficult financial conversations. “Traditionally, health visitors always thought finances weren’t really in our bag” however by incorporating financial questions into health visitor assessments, supporting staff through this development and linking it to a Money Matters pathway, “in the first year of that programme in the first pilot working with 20 families, and in that partnership we managed to secure £100,000 for those 20 families”.
9 Morecambe, fie072b4
10 Middlesbrough, fia7cc1e
11 Liverpool group discussion
12 Clacton fief656b
13 Derry, fi4eb3d5
Such positive results were repeated a second year, showing this is a successful method for “maximising income and lifting some of these families out of poverty” 14 .
Recommendations
• Build on the strengths of community members by involving them in whatever activities possible;
• Ensure programmes are in place to keep health and social care professionals up to date with latest policies to help their clients;
• Have sufficient professional and voluntary help in place to assist community members to manage their financial situation.
Chapter Five: Housing
This chapter discusses a range of issues related to public and private accommodation - noted by stakeholders to have a negative impact upon the health of women and babies during the first 1,000 days - before outlining suggested solutions. Problems present in relation to home conditions, homelessness and inappropriate temporary accommodation, migration and statutory rehousing.
Home conditions
Home conditions drive many mental and physical health determinants seen across the seven localities, with some areas reporting people living in static caravans, chalets, wood houses or beach huts, some of appalling quality. It was reported that landlords buy properties cheaply and place tenants in them without maintaining them to liveable, safe standards. The huts, for example, are extremely small and draughty as they were built only for use as summer holiday homes. These have been noted as negatively impacting on infant development as they are damp, mouldy and “tiny, tiny, little places that they live in. So the amount of time that a child could even have the opportunity to crawl” 15 is very limited. Figure 11 displays the physical and social impact of poor home conditions on individuals/households and neighbourhoods.

Note: Reprinted from Housing and Public Health. By M. Shaw, 2004, Annual Review of Public Health 2004, 25, 397-418. Copyright 2022 by Annual Reviews Reprinted with permission.
Furthermore, tenants are often concerned about raising issues with landlords because “they don’t know how that’s going to affect their tenancy, whether that’s going to cause them to be evicted” 16. Indeed, a voluntary worker describes some tenants being frightened of private landlords as bullies who frighten their tenants. He reports that “there's one landlord who has 160 houses. He rules it with a rod of iron.” 17 . While poor home conditions do impact upon an infant’s development, social services sometimes receive inappropriate referrals for home conditions from health staff who do not understand the extreme poverty of the areas in which they work. One respondent noted that one particular family “are absolutely amazing, they meet all the needs of these children, but, health were complaining because of the conditions of the home. I can’t change that home and it’s because of poverty. It is. She works, she’s on maternity leave at the moment. He works intermittently, with an agency. They’re trying. They’re really trying” 18 .
Homelessness and temporary accommodation
Women and their babies may become homeless and require temporary accommodation due to circumstances such as eviction, poor mental health, fleeing domestic violence or being put out of their family home for becoming pregnant. Figure 12 displays the scale of the issue in England. As clarified by mental health nurses and health visitors, homelessness has a significant antenatal impact upon baby health due to “the stress, the impact of stress in pregnancy and the kind of baby genetics around that…and it is a really unsettling time where they don't know where they’re going to be living”. They say “there should be no rough sleeping at all, everyone should be accommodated. But the reality very often is some of the accommodation that people are offered, they don’t want to take up, and you can understand why”. Much of the accommodation offered is completely unsuitable, and “can be a roof over their head, but very often it’s not much of a home, it’s very cold, money’s tight, it does affect their nutrition” 19 .
16 Clacton, fi73d00d
17 Clacton, fief656b
18 Neath, fi7d080d
19 Lanarkshire, fi870adb
12
Homeless 0-2year Olds


Note: England 2014, Reprinted from An unstable start, all babies count, a spotlight on homelessness, NSPCC. By S. Hogg, A. Haynes, T. Baradon, C. Cuthbert, 2015, https://library.nspcc.org.uk/HeritageScripts/Hapi.dll/filetransfer/2015AnUnstableStartAllBabiesCountsp otlightOnHomelessness.pdf?filename=AA58F75CEDE68892A73FB681FE246B8371684F102152F0AA780A 14959D3BCE5767137B3B2A935011CBAEC3068664FF681AA6D2524E357BAB96C006752CCD756759AD7 7BD1E389823A55CFAAE74B2EE64F46C611AD1724BE1AC500B025490CCB1CD8D9D26B00674E723A731 951BB13FBE2976B714838E6BBB09A9FD539E6F7F27DD3EA0DC4386C6EDAC8F0E252527FCA6955013E8 6EE573EFCAE62FF1D24E6212CD57816E591540239CFA9857B1A6F20F4769801F7402B79F462D525C870 AD9350EF414632F9EE98FD015&DataSetName=LIVEDATA Copyright 2015, by NSPCC. Reprinted with permission.

Mothers with young babies can be placed into temporary accommodation without good health and social supports around them, miles from where their other children go to school. Regardless, they will be “expected to literally walk three miles. If you’ve got, say, a baby and a child at school, it’s just not… Most of us wouldn’t be able to sustain it or do it” and receive criticism when they do
not manage to get there. This results in service users avoiding the services, “because they’re just finding it a real struggle because of all the judgemental attitudes that they’re getting from a range of professionals, really: health, education” 20
Migration and statutory rehousing
When people voluntarily migrate because “you can get some really cheap accommodation” 21 many young, impoverished parents desperately seeking affordable housing are drawn to the area, increasing the number of babies. However, the facilities are often extremely poor in areas where rent is very cheap. However, “if you went and rented there, you’d be surrounded by all sorts of social issues and problems, and there are very few actual resources there to deal with any of those issues” 22 . An NHS Child Health Commissioner explains that South Lanarkshire, particularly Clydesdale, is “a net importer of young people from, not only outwith Lanarkshire but outwith Scotland” and that they are currently “seeing a growth in the private sector of residential houses being built for looked after and care experienced young people” 23 . One issue with the housing of young people moving from England to Scotland is that each country has different legislative frameworks. For example, while the local authority in England retains overall responsibility for their young people, Scotland is under “a directive from the government that any child or young person who becomes looked after must receive a health assessment within 28 days”. Lanarkshire’s receiving health board is “not necessarily notified of these young people, so there right away, within that 28-day window, we don't know that they're in our area” 24 and may not be able to give them necessary care.

20 Clacton, fi73d00d
21 Clacton, fi966b1a
22 Clacton, fi73d00d
23 Lanarkshire fid49f17
24 Lanarkshire fi870adb
Direct payment to landlords
When discussing the extreme financial deprivation respondents explained that with the introduction of Universal Credit, all housing benefit is paid directly to service users. While this is prima facie a positive and empowering initiative, staff say “it’s giving the power to the woman, but actually I think it’s better if some of it gets taken for rent and things that she’s going to have to pay” 25 . Service users in Liverpool who were receiving universal credit all reported that their rent was now being deducted first, reporting this as a positive move.
Quality community housing
Several respondents outlined positive psychological impact that high quality social housing has upon inhabitants: “The families who are in there, the outlook is so much different” because “if people have somewhere nice to live, most of them appreciate where they live and look after them” 26 . One respondent recommended “a scheme where you end up building houses but it’s the local community that build those houses” as a “community enterprise that uses local people, with their local skills, where they get paid, so you start to then increase the economy” 27 This housing association approach would circumvent the need for private landlords by making housing a community enterprise and reinvesting in the community by increasing job opportunities. Investing in the community to create housing would lift community spirits and develop residents’ skills while addressing a vital housing need.
Educating staff and service users
As reported parents can be misperceived by staff as negligent regarding the conditions of their home. Thus, staff should also be educated as to which conditions of the home may present important safeguarding risks to children, and which undesirable conditions (such as aesthetic factors) are a consequence of poverty but do not pose a health risk. Service users “don’t understand why they face aggression from people coming in saying, “You’ve got to do this, this and this”, and then “their emotions take over and they have conflicts with the social workers, or they deny compliance” 28 .
25 Clacton, fi880def
26 Morecambe, fi03e99c
27 Clacton, fi73d00d
28 Middlesbrough, fic36ed2
Recommendations
• Checks should be made on private landlords to ensure that properties are up to acceptable standards;
• Pregnant women and those with children under 2 years should be housed appropriately;
• There needs to be more coordination between services when families move out of area;
• Involve and utilise the skills of the local community when developing new housing areas
Chapter Six: The impact of local facilities and services
This chapter discusses issues concerning a broad range of issues such as educational programmes, parks and recreational facilities, hospitals and doctors’ surgeries etc together with the physical network that bind them together such as road and railway networks, telephone lines, bridges etc. All of these issues were found by the commission to have a significant impact upon women’s and babies’ difficulties accessing healthcare and often resulted in poorer health outcomes. Respondents acknowledged that these shortages are frequently a by-product of cuts in public spending and notably exacerbate existing challenges for societies’ most vulnerable groups. Suggested steps to alleviate the associated problems, as well as initiatives in implementation are presented below.
Local facilities
Most areas visited by the commission report extremely poor local facilities in some cases lacking a local supermarket and the most affordable supermarkets do not deliver and are furthest away. Thus, families depend upon corner shops where the prices are high, and products are limited. If workers are unaware of this type of contextual detail, they may refer families inappropriately and undermine service user self-esteem. For example, a family was flagged by a health visitor due to poor nutrition, as “they didn’t have the privilege then of fresh veg and fresh fruit [so] what they did was they brought frozen” 29 . In fact the health visitor seemed to be unaware of the nutritive value of frozen freshly picked vegetables.
Conversely some women are not referred because there is no service on offer in their local area, not because they do not need support. While “there are really good services in pockets of areas” which can take referrals from across the locality, poverty is so extreme that most families cannot afford to travel, meaning access is a postcode lottery” 30. A psychologist explains that lack of funding also affects her client base as her “waiting list is a year and a half for paediatric psychology and about 20% of that is children under two. If they have to wait a year and a half, they’ve doubled their age so we’ve missed the opportunity to intervene” 31 . When discussing the impact of poor funding, respondents explained that current services cannot operate effectively to meet people’s needs, and
29 Neath, fi7d080d
30 Derry, fif006f6
31 Derry, fibe69b4
numerous pilots have been stymied. For example, “we have a young parents’ project here where mummy goes and lives in a flat and there are staff downstairs. So, there are maybe 22 flats, but there’s no real specialist services that go in to that housing project, really. It used to be much more but then they lost funding”. The purpose of this project is to support parents who never had a secure attachment to their own parents, learn how to parent, while their babies are in a crèche five days a week, “so that they can be better parents than what their experience of parenting was”. They also explain that family support workers are “vital”, “really key” and “make a huge difference”, however “we don’t actually have any funding for any of them” 32 . A reduction in Children’s Centres, despite their immense popularity across the demographics, was consistently reported. Figure 13 highlights the scale of the issue in England from 2009-2017.
13
Total Children’s Centre Closures for each Local Authority, 2009-2017

Reprinted from Stop Start, Survival, decline or closure? Children’s centres in England, 2018, By G. Smith, K. Sylva, T. Smith, P. Sammons, A. Omonigho, 2018, https://www.suttontrust.com/wpcontent/uploads/2018/04/StopStart-FINAL.pdf
Figure 15: Total children’s centre closures for each local authority in England, 2009-2017 (Smith, Sylva, Smith, Sammons and Omonigho, 2018, p.15).
32 Middlesbrough fi1d7ffb
Furthermore, following their closure, one service-user said “Well, you won’t see me again because I can’t walk to it” 33 . They have lost valuable resources for both the staff and service users, as popular services and programmes such as a domestic abuse service drop-in and community freedom programmes were run from the Children’s Centres. They have also lost the capacity to “refer families for specific kinds of domestic abuse, targeted support”, and now families will only receive support if they reach the highest level of risk criteria, leaving those who need lower level and preventative support without. She concluded that this all means “It’s never going to break the cycle, is it? The children just grow up in that environment. The parents aren’t getting the outside voices to support them to know, to find another way, so there’s the intergenerational transmission. It just never gets broken” 34 . Another respondent explained that there is a severe lack of local services as “There are 7,000 people living here and there's no school”. Furthermore “there isn't anywhere where you can buy a loaf of bread or a pint of milk, so to go shopping, you have to get a taxi to Tesco three or four miles away. There is one tiny church. Otherwise, the nearest church is a couple of miles away. The doctor's is a couple of miles away”. As most families do not drive and “won't think about getting a train” with the nearest station 5 miles away, “it is just a forgotten island of poverty” 35 . Such cuts mean that GPs are seeing an influx of people who have Social Care involvement but have not been able to get needed support via this route due to the pressures on Social Care.
In addition, when discussing a developing multiagency pilot project which collaborates with the police to take a holistic, whole family trauma-informed approach to ACEs, the changes they are seeing in families “are quite significant” but “there is no money for this pilot project”. Funding cuts mean that the contracts for highly skilled and trained staff are only being renewed on a short-term basis for six months or so and paid in monthly arrears as “national HR department won't allow you to issue permanent contracts, when it's not guaranteed that your income is more than monthly”. This means “maintaining those specialist staff to be able to do this work is incredibly difficult” 36 as they do not know if their contract will be extended and must look for other jobs. She says “It is very unstable. More unstable than I've seen it in a long time” as
33 Morecambe, fi8efdb4
34 Morecambe, fi79d21c
35 Clacton, fief656b
36 Middlesbrough fi55b949
"We're existing on more than 50% of our contracts…being six months plus six months, or twelve months" 37 .
Physical networks
Several stakeholders highlight that families in rural, isolated areas cannot reach the services due to there being extremely poor public transport and most families do not drive. The extent of these families’ isolation caused by geographical location and poor infrastructure also creates challenges for the staff who provide home visits. They must juggle large caseloads of families across the county, and their ability to provide high quality home-visits is restricted by the time they must spend driving between hard-to-reach areas, as “if you’re up in the valleys we could have an half-an-hour drive up to one valley and then come back down another valley” 38 . The uptake of free nursery placements may also be low because parents cannot afford the bus fare to reach placement, or it takes more time to travel to the placement than the placement lasts. Similarly, many families cannot afford the travel expenses to get their children to dental appointments, particularly if they are travelling from very remote rural areas “They can’t afford to go. They can’t afford to get the taxi to the hospital, that’s 30 quid in a taxi” 39 . Similarly in Liverpool service users noted that while there was a good bus service they often could not afford to use it as “it costs over £12.00 to get us all into the city and back “[ a three mile journey] 40

37 Middlesbrough, fi55b949
38 Neath, fif1071a
39 Lanarkshire, fid2f9af
40 Liverpool fg002
This wide geographical dispersal also affects multiagency communication, information sharing and collaboration, as “other authorities are maybe a bit smaller and maybe it is a wee bit easier to manage and things. People have personal relationships with people within different agencies, and things like that” 41 . As articulated by a service user, “I would definitely invest in infrastructure. Also, just to be able to walk out, as a woman who’s just had a baby, I would like to be able to get on a bus that’s more regular or get on a train and I’d be able to visit friends, if you’re not able to drive or you can't afford to drive, or you live in a place that’s not accessible. So, I would be sorting out infrastructure first of all, so that people could be made available” 42 .
As one respondent conveys: “If they’re [the mothers] not getting any socialisation that’s bad for the babies as well. They do need to meet with people. I mean when I first took up the post with teenage pregnancy, there was a young mum who committed suicide because she had nobody”. She also explains the struggles service users face in accessing services due to poverty, as “It’s the actually getting to the hospital and bus fares, I mean especially my young mums who haven’t got any benefits. They’re not entitled to anything, many of them. How are they supposed to get to hospital for appointments?”, “Even to get to hospital it’s £5 or if you’re on universal credit, £5 is an awful lot of money when you’re on benefits” 43 .
Particularly vulnerable may be refugees, victims of domestic abuse, or those who suffer from illness or disability issues, as the distances they must travel for care can be a huge psychological, emotional and financial strain and many services are ill-equipped to alleviate this burden.
Local and mobile services
Local and accessible women’s centres are vital for children to get early socialisation because “it is very much stay at home and stay within your community. They can't afford the bus travel. They can't afford the leisure centres. They can't afford the day trips out here and everywhere so it becomes very isolating for the children” 44 .
Seeing every child and family regardless of their postcode means all issues will be detected and allows more targeted work to proceed with the families which really need it. “We follow the Healthy Child Programme, so every child gets
41 Lanarkshire, fi5fcb01
42 Derry, fi7bcc6d
43 Morecambe, fi8efdb4
44 Derry, fi04e1c7
their five mandated contacts. So we will be seeing every child” 45 This evidence suggests that services must be universally available to all to avoid families falling through the net by making sure the most vulnerable are always included, reducing the risk of stigmatisation.
Joint agency working
Joint agency working has led to restructuring with an examination of “things like what it meant for a young person who has had a life maybe in care, they had to go on and be a parent themselves, what that looks like for their child, what having a family nurse means in terms of keeping their child out of the care system. Or the other side of that is removing a child much earlier than it would normally be removed and in terms of the damage to the child and also the whole monetary thing about keeping children out of care, or bringing them into care and getting them foster parents quicker than would otherwise happen ” 46 . Another group explained that “since we’ve been brought in-house, into the local authority, that has improved because, obviously, we’re part of the team now so we’re involved more” 47. This happened following a boost of funding and greatly increased cohesion, cooperation and cross boundary working by increasing the service’s access to information.
Low-cost prevention
Professionals across the nation stress that it is important to focus on implementing early low-cost interventions which are preventative, to minimise the outspend on extremely high cost and much less effective ‘solutions’ down the line When “pulling back the years, the weeks and months to see what could have been better for that family that come to you at two, that child and that mum and the dad”, a health visitor says that problems for families will remain “a sea of problems, like a tsunami” and keep growing “If you don't look at the prevention…it's a no-brainer. It's too big a problem” . However, “With the correct interventions, well, sometimes, not always, but sometimes quite easy to fix at a low cost”. To support this argument, she examples how “off the top of my head”, it costs around “£4,000/£5,000 or something” for a family to have access to [our] service for “two and a half years of pregnancy”. “The research shows that the cost/benefit is massive in all that not going to the GP, hospital, healthcare…and then obviously social services, child protection, criminality,
45 Clacton, ficcb2f9
46 Derry, fibe69b4
47 Neath, fif1071a
probation, the prisons”. These outputs are “a massive, massive burden and a cost to the nation” which can be reduced “if you just put in that small amount of money early on” 48 .
Recommendations
• Introduction of more mobile services for health prevention and educational activities and also early childhood services;
• Expansion of low cost prevention activities;
• Utilise local centres for maternal/child activities and provide community organised transport;
• Encourage joint working between different agencies to group together services at times appropriate to the service users.
48 Morecambe, fie072b4
Chapter Seven: mental health
This chapter begins by conveying the magnitude of the problem of poor mental health in areas visited by the commission, as reported by stakeholders. It then explores how poor mental health can be transmitted across generations in cycles and how it prevents families from engaging with the services. Following this, it presents evidence that lack of low-level support and greater service demand than supply means staff are unsustainably targeting only highlevel need families, rather than implementing longer term preventative solutions. Next, it relays the findings that there are significant gaps in attention and provision surrounding infant mental health and parental bereavement. Finally, it lists the wide range of recommendations and successes communicated by stakeholders to address these issues.
The extent of mental health issues
In each locality visited by the commission, poor mental health was reported to be an extremely pressing issue “most of the families that we’re meeting with, like young mums are all suffering with anxieties” 49 . Midwives report “a surge in mental health[problems] in the area” as “a lot of our girls have poor mental health, a lot of them are on prescribed medications, probably their diets are not the best. So, their health and wellbeing- And a lot of them have really high levels of anxiety and stress, which impacts upon the health of their babies” 50
Intergenerational cycles of poor mental health
Respondents explained that many service users unknowingly perpetuate unhealthy and damaging behaviours which will negatively affect their relationship with their child and their child’s self-esteem. This is because they “don’t know any different about how you treat children because of the way that they have been brought up”. For example, “I’ve been out to visit women who are lovely, beautiful women but the language that they use around their baby from very early on is quite shocking”, “they don’t mean it in a harmful way” but “they have been brought up to believe that you speak to children, you know, “You're a little bugger,” blah-blah-blah, and it breaks my heart when people have just got a brand new baby that they are saying is lazy or is greedy or is naughty” 51. Health visitors also note that mental health issues caused by childhood trauma are an issue due to the prevalence of domestic incidents,
49 Clacton, fi07d21c
50 Lanarkshire, fi97ff4c
51 Clacton, fi880def
“And the thing is, that repeats, doesn’t it? So, that trauma can stay and it affects all aspects of their life, like employment and relationships. And that just repeats, doesn’t it? And that can then cause trauma for them, when they have their children. It’s just a cycle, isn’t there? And it is breaking that cycle” 52. They explain that “we’re on maybe the second or third generation of families who haven’t had a parenting example” 53 and question “If your mental health when you're 20 or 30 is a problem and you're having your own children from then…How do you interrupt that cycle?” 54 Will they be able to do it?” 55. Poor parental childhood experiences in this case feeds self-doubt about their own ability to parent, as they have had no clear model of how to do so well.
Challenges to engage and isolation
Respondents described the difficulties they face engaging with service users who have poor mental health as “when we get a referral, it might take six weeks to even get through the front door, even though we’ve had a conversation and they’ve said, “Yes. I’ll be in tomorrow.” You go, and you can’t get in. But you know they’re in there. You can hear the baby crying or the curtains twitching” 56. Such families may have “been given a leaflet or they’ve been in the centres” but are unable to take advantage of the services on offer and act upon information due to the anxieties which affect their confidence, understanding, or ability to engage. Groups that address mental health often do not work as families will not attend due to psychological barriers such as lacking confidence and anxiety, Staff say “we are looking at how it’s going to change, because it’s not working. And we have people on the waiting list who then don’t come” 57. While mental health problems contribute to service user isolation by preventing them from engaging with services, the converse is also true as isolation increases the risk of suffering mental health issues.
Poor mental health drives pregnancy
Respondents highlight that poor mental health derived from lack of opportunity and deprived upbringing can lead teenagers to aspire to become pregnant to gain a sense of achievement (Cook and Cameron 2015) and “a
52 Clacton, fif40d2b
53 Morecambe, 3
54 Morecambe, fie072b4
55 Lanarkshire, fic7eb7c
56 Clacton, fi07d21c
57 Clacton, fif40d2b
sense of being loved and things that they’ve never had”. They explain that “for young girls who don’t feel they can attain educationally, what more aspirational is there than to become a mum? Going back to thinking about teenage pregnancy but again we can say everything is higher out here. Actually, if you look at aspirations, whether that’s in employment or educational attainment, for them that’s their aspiration, a sense of achievement is pregnancy”. For many young women “where they have perhaps been in a family where they haven't felt loved or…they try and kind of compensate by having a baby” 58. This is especially common for looked-after young people, causing a high degree of issues as “these young women who are becoming pregnant and then don’t have support mechanisms to support them and then struggling obviously” 59 and are more likely to have their children removed into care, perpetuating the cycle.
Fighting fires
Stakeholders interviewed across the UK affirm that mental health services need more investment via increased funding, development, and staff training, to address the demand which outweighs the current support available. Figure 14 presents the lack of specialist community perinatal mental health teams in the UK in 2017, particularly in Scotland, Northern Ireland and Wales.
58 Clacton, fif40d2b
59 Clacton, Fi273827
14
Community Perinatal Mental Health Teams.
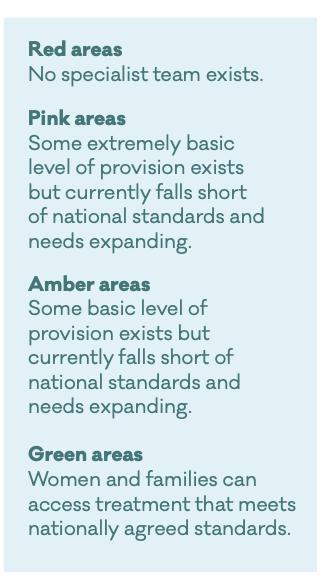

Note: UK 2017, Reprinted from Improving access to specialist perinatal mental health services. By Maternal Mental Health Alliance, n.d, https://www.suttontrust.com/wpcontent/uploads/2018/04/StopStart-FINAL.pdf
Furthermore, one respondent noted that if she had a magic wand she would wish for good provisions in perinatal mental health, as “What we don’t do well is mental health”. She explains that “We do have a perinatal mental health service, but it’s massively overstretched, hugely under-funded, and it’s just not good enough. Consequently, it’s people in crisis who are seen, which is just fighting fires all the time” and that “there’s no preventative stuff, and that’s a massive failing in my opinion because then that’s a knock-on thing” 60 . However, as the level of support required by families naturally fluctuates, “unfortunately, we do get a revolving door, really, of some families that come in at a later date, which is a shame really because I think some of these families they wouldn’t necessarily need a higher level of a child protection type of concern if they had that lower level longer term support” 61 Staff only have the capacity to act as a crisis team for mental health as “things are pretty much out of hand”, and if “families haven’t responded to that early intervention or they’ve had support and then, when that’s withdrawn” they will collapse
60 Neath, fi2a78e3
61 Neath, fif1071a
again 62 Addressing this problem and implementing change requires system change, one respondent noting that “we need to get better at earlier intervention, and consistent care” because at present “I think we sort of firefight. So, when there’s a crisis, we go in there, we give all these services. And then, once we start doing well, we pull everything back. And then we wonder why everything falls flat on its face” . Fire-fighting is neither a sustainable nor long-term solution, because “if we look at our cohort of mostly babies that are removed, when they're removed at birth, often the parents have had troubles themselves, growing up. So, whether it’s that they’ve been looked-after or they’ve had- you know, there’s been domestic violence or mental health [problems]”, and without early intervention or consistent low-level support, negative outcomes will keep repeating themselves. 63 .
Bereavement
In each place that we visited there is a lack of any tailored bereavement support for families “where there had been maybe multiple miscarriages or still birth or premature birth after the baby was born and even complications then for siblings are struggling, because they’ve expected a baby and they’re only small. They can’t understand why” 64. These issues are quite common and there is high unmet demand for support. When describing her mental health following a miscarriage, one service user says “I was disappointed and disheartened. I can’t explain myself. I couldn’t face anybody. I couldn’t even step out of my house. I was just in my bedroom. I didn’t even worry about having a drink or food, anything” 65 .
Infant mental health
The issue of infant mental health is mentioned in all areas of the UK visited. One respondent reported a “continuing lack of recognition or understanding, despite all the research and understanding about and focus on the early years, even at a government level to some extent in Scotland, about the potential for serious mental health disorders in infants”. He suggests several factors contribute to this, including “the denial and the pain of being aware of infant mental health difficulties and the pain of infants” or lack of understanding of “the idea that infants can have serious mental health disorders”, traditional
62 Neath, fi6e3093
63 Derry, fi76ed1d4
64 Derry, fi6f1276
65 Middlesbrough, fic36ed2
overfocus on mother which makes infants ‘invisible’ and the “absence of access for infants, to a large degree, to specialist mental health services” 66 .
Universal, long-term, low-level support
Acknowledging that mental health problems can affect anyone, staff at one Home Start convey that one of their main strengths is how they can offer universal support as “we don’t have a criteria of meeting certain benefit because disability, domestic abuse, postnatal depression doesn’t happen to a certain demographic of our society, it’s across the board. So, I’m really passionate that Home-Start doesn’t have that barrier”[3] . In similar vein, a health visitor in Derry says that their ‘Healthy Child, Healthy Future’ programme is universal, which is good as “there should be a facility for all mothers or all parents to have that level of intervention”. However, she also argues that “there are a lot who would choose not to have it if they felt they weren’t avoiding the service. But if they had the opportunity to dip in and dip out, I think there is a huge proportion that would choose that”. Allowing service users to have this flexibility would give staff the opportunity to focus their resources on families which really need support, as “there are a lot that need more that aren’t getting it”. She concludes “parents need to be able to dip in to the service as they need. They still need contact. But I don’t think they need the input that we are giving as a universal” 67
Education
In many areas visited by the commission, it was argued by stakeholders that parents, staff and children require more education about mental health to prevent the perpetuation of unhealthy behaviours. Some respondents argued that teaching people “antenatally a better way of looking after their children” is what is needed if “we’re going to break that cycle of the negativity of low self-esteem” 68. Others believed that parental education surrounding self-care and mental health is missing, as “they do do birthing classes. So, they do breastfeeding, bottle feeding, birth, but I think there needs to be more in terms of the importance of looking after yourself and that baby in the beginning, to make sure that when baby is born, that both you and baby are as fit as you can be. It’s a hard time, isn’t it?” 69 .
66 Lanarkshire fi5fcb01
67 Derry fi08d207
68 Clacton, fi880def
69 Neath, fi6e3093
End siloed working
Respondents argue that preventing the intergenerational cycle created when families with poor mental health have more children requires aligning “children’s and adult services more effectively so that we’re looking at the whole family approach to it. That is going to be a challenge going forward because we have worked separately” 70 . Another says “Where we need to improve, absolutely, is that [relationship between] adult services and children’s services, so it’s an adult presenting with adult mental health services but has children in the family. Are we connecting those up in terms of, “Okay, we’re working with the child, but mum or dad has got these needs, how are we working together?”. This may require a return to local community models of care and a “restructure of the clinical commissioning groups and the alliance to really look at shared governance arrangements, shared pooling of resources” 71 . The campaigns and messages must be linked together to avoid confusing service users.
Multidisciplinary-team hubs
The educational courses various centres offer have a huge positive impact upon service user confidence, as women start with no self-esteem and there is “a lot of reassurance needed and within a few weeks even you can see the change in them. Then they’re going out for tea and coffee, they’ve made friends, the big change in the parents as well as the children is great”. Staff are “in with social services so, if they see anything that they're worried about, they can help”. This includes facilitating contact with parents they think are struggling with mental health and “they’ve got, which I'm really proud of, a counsellor on their team who works through all the different things. Mum can come in and say, “Look, I'm really struggling with post-natal depression,” and she’s referred within a matter of weeks to the counsellor and they go through everything from CBT, she does reflexology and she does all that kind of stuff to help the mums” 72 .
Groups
All service providers reported that they have seen great results from the groups they offer (for service users whose mental health allows them to attend), as “parents really benefit from the groups anyway, but they establish
70 Clacton, fi273827
71 Clacton, fi273827
72 Derry, fi04e1c7
friendships and they get something socially out of it”. This fostering of social bonds tackles the poor mental health caused by isolation and the absence of support networks, as parents “support each other really well. It’s come from a group, but they really support each other well”. It gives them the opportunity to “discuss with other parents and reassure themselves as well, “I’m not on my own here.” And learn from other’s experiences, other people’s strategies… It helps, yes” 73 .
Relationship building
Building trust can often be a struggle because of service user poor mental health, adverse experiences with others in their “background and just a general mistrust of social services”. Many service users have “been brought up in a family environment where social services are bad, they come to take your children away” 74 . This pervasive mistrust and fear of the services is best countered over time by relationship building through transparent and open communication, listening to service user opinions and feelings, and advocating for them. One respondent explains that once a mother has had her child removed there needs to be “mental health first aid in the initial period but then there’s the addressing the issues that have lead them to this point” otherwise the mother will find herself in the same situation as “None of those circumstances have changed because the professionals follow the baby, not mum”. She points out that “From a cold hard financial point of view, the NHS is struggling. There’s a lot of time and resource goes into these vulnerable families where there is the very strong potential that that child is going to be removed again, that second, third, sometimes, fourth child is going to be removed. There’s a lot of drain on the resources for the local authority” 75 .
Recommendations
• Invest more in mental health services development, and staff training, to address the current demand;
• Put more programmes in place to prevent, detect and treat infant mental health problems;
• Acknowledge all forms of bereavement and ensure sufficiently trained professionals and volunteers are in place to deal with this;
73 Neath, fi7d080d
74 Neath fic49a15
75 Morecambe, fi8efdb4
• Build upon the success of existing multi-disciplinary team hubs to end siloes or duplicate services;
• Offer sufficient education programmes to address the needs of both service users and providers;
• Where possible provide continuity of care services so that consistent information is given to service users.
Chapter Eight: Infant nutrition
The main issue concerning infant nutrition discussed by stakeholders was the UK’s low breastfeeding rates. This chapter reiterates the importance of breastfeeding and discusses the factors which interviewees report obstruct healthy breastfeeding activity, alongside the ways they think these could be successfully overcome.
The importance of breastfeeding
Breastfeeding is a crucial element in protecting the baby against health difficulties even if the mother is suffering from health problems such as postnatal depression as depicted in figure 15.
The Benefits of Breastfeeding

Reprinted from Exclusive breastfeeding: why choose to breastfeed?, by Scottish Government, n.d. https://www.parentclub.scot/articles/exclusive-breastfeeding-why-choose-breastfeed. Copyright n.d. by Crown Copyright. Reprinted with permission.
A respondent reiterates this: “The mum that I've got that has got severe depression, believe you me her attachment with her baby is fantastic, mostly, I believe, because it's coming naturally because she's breastfeeding. She's still breastfeeding this eight-month-old. He's a happy, happy baby. She's in tears. She's in tears and been to the doctors for more antidepressants, but her baby is a happy baby” 76 .
A concerning message from some health professionals is that bottle-feeding presents extreme risks to both mother and infant: “If you bottle feed your child, it’s more likely to have gastric problems, respiratory problems. It’s more likely to be hospitalised in the first year of its life. You baby is more likely to get
76 Morecambe, fie072b4
childhood leukaemia if you bottle-feed it. Your baby when it grows up is more likely to have diabetes and obesity. And for you yourself, you’re more likely to get ovarian cancer or breast cancer if you don’t breastfeed” 77 . However, despite the extensive health and financial benefits of breastfeeding (particularly for women living in poverty), the commission heard that breastfeeding rates remain negligible in every area visited, evidence which aligns with the findings of UK based breastfeeding surveys discussed in Chapter 2. The reasons for this will be elaborated upon below.
Breastfeeding is difficult
Regarding practical difficulties, six months of exclusive responsive breastfeeding is incredibly challenging to execute in daily life. As one respondent, a midwife, health visitor and mother commented “it's a nightmare, and I've done it twice. It is really, really hard. It is really hard” 78 . Women often face difficulties getting the baby to latch. As a health visitor notes: “boy, you know, it was a struggle. I remember it took as long to get the baby latched on to the boob as it took my husband to fly from Edinburgh to Schiphol” 79. Physical struggles can in turn lead to further off-putting emotional struggles. Another practitioner highlighted that in rare cases physical barriers such as medication or breast surgery can completely contraindicate breastfeeding. Psychological barriers also occasionally prevent women from breastfeeding. Health professionals noted how “people who have experienced trauma breastfeeding can be a huge issue for them because they can reexperience the trauma”, and “a lot of public health nurses wouldn’t have an awareness of about how if you’ve been sexually abused or had the trauma then that can cause a really dangerous attachment with the kids” 80 .
Cultural resistance
Interviews with stakeholders provide anecdotal evidence revealing how deeply acceptance and encouragement of bottle-feeding is entrenched in UK culture. For example, a health visitor noted: “One of my colleagues … was chatting to a young mum and she said, ‘Oh, well, I'm going to feed the natural way,’ so she presumed she meant breastfeeding. She said, ‘Oh, that's good, have you got-‘ she said, "No, I'm bottle feeding." She said, ‘Well, that's not what 'natural'…’
77 Clacton, fi880def
78 Morecambe, fi7f9efb
79 Neath, fi3d3d14
80 Derry, fif006f6
and the girl said, ‘It is around here’” 81 Evidence found by the commission suggests that negative public attitudes towards breastfeeding, subliminal messaging promoting bottle-feeding and the spread of misinformation all feed into maintaining and perpetuating active social deterring of mothers from adopting the healthiest approach of responsive breastfeeding. These factors will now be discussed in turn.
Public attitudes
Social perceptions and attitudes towards the breast which frame it as pornographic have a wider impact upon women’s freedom and security to breastfeed their baby in public spaces with “people have said they go out to a café and they’re told to go and feed their baby in the toilet” 82. Children and Family Services staff in Lanarkshire explain that “We do not have dads in that group, and the reason that we do not have is we have found that if women are breastfeeding they are uncomfortable, for whatever reason, if males are in and around the group” 83 . This suggests that cultural sexual objectification of the breast within UK culture remains a strong force impacting on women’s willingness to breastfeed by creating an uncomfortable atmosphere. Similarly, migrants from cultural backgrounds where breastfeeding is the norm, doing so in front of men may remain inappropriate for other social, cultural or religious imperatives. Figure 16 supports these findings and indicates that there are negative attitudes and social perceptions towards breastfeeding as public commentary on web based sources presented breastfeeding in the UK as acceptable with discretion or not acceptable.
81 Middlesbrough, fi34ff85
8282 Neath, fi3d3d14
83 Lanarkshire, fiff21e3
Figure 16
Public Opinion of the Acceptability of Breastfeeding in Public

Note: by media outlet. Reprinted from UK views toward breastfeeding in public: An analysis of the public’s response to the Claridge’s incident, by C. Morris, G.A. Zarate de la Fuente, C.E. Williams, and C. Hirst, 2016, Journal of Human Lactation, 32(3),472-480. Copyright n.d. by SHURA. Reprinted with permission.
Subliminal messaging
A powerful factor which contributes to the normalisation of bottle-feeding in the UK is its presentation through media and advertising. Health visitors note that “You never see popstars or celebrities in the newspaper breastfeeding, it’s always the bottles, all the latest bottles that are out” 84. Others agree, stressing that “formula companies are very, very good at promoting their product and making lots and lots of money” 85 and subliminally spreading messages which contradict health recommendations to maximise profit.
Spread of misinformation
A recurring theme across locations is that health professionals must combat the pervasive and damaging influence of health advice and information derived from unreliable sources, which are trusted nevertheless by serviceusers. A health visitor explains that “one of our biggest things that we fight against is media, other families’ experiences. So, they’ll listen more to what they're reading – celebrities, everybody else – than listen to the safety advice that we’re giving” 86 . The power of combined cultural factors is reflected in feedback across the UK with healthcare professionals often dismissing the risks. A midwife reports of a
84 Neath, fi3d3d14
85 Morecambe, fie072b4
86 Clacton, fif40d2b
town that “they had a big Romanian population who were starting to bottlefeed their babies because they saw the local women” 87. Migrant populations which usually have a culture of breastfeeding are therefore at risk of losing this behaviour due to the pervasive influence of bottle-feeding culture across the UK. Challenging and changing breastfeeding behaviour will not be successful when pitched solely at the level of the mother-child relationship, but the wider cultural understanding and mindset must be addressed and adjusted alongside increasing confidence and trust in the advice of healthcare professionals.
Inadequate education
Midwives, health visitors and nurses all mention mothers’ lack of education surrounding breastfeeding is a factor contributing to the low rates of exclusive breastfeeding until six months. Mothers may not understand the wide ranging benefits of breastfeeding for themselves and their infant, the health risks of processed formula feeding, how breastfeeding supplies the best nutrition possible and the impossibility of ‘spoiling’ or ‘overfeeding’ their child via offering their breast at every cue. It is argued that “So many women actually even would try and initiate breastfeeding if they had the information, but they need that information antenatally” and unfortunately “often they're not getting that information antenatally. There are women who are choosing even not to give the first colostrum because they just don't know” 88. The importance of beginning this education early in the antenatal period was stressed, with suggesting education surrounding breastfeeding should begin in school through sex education. If the message is conveyed, it must be repeated and thoroughly implanted, although midwives report a lack of time and money to address deficiencies. Inadequate education affects staff as well as service users. Evidence found by the commission suggests that health and social care staff as well as politicians, local MPs and councillors lack awareness of the significance of the issue and the marketing power of companies advertising processed infant feeding substitutes.
Trained peer support workers
Evidence suggests that companion-like breastfeeding support from consistent faces - regardless of job title, would help improve breastfeeding rates. This is especially important in the early days of the postnatal period birth, as the gap between the prebirth and 10-14 days post birth mandated health visiting contact is too long and negatively impacts breastfeeding rates because many
87 Derry, fi2e74ad
88 Morecambe, fie072b4
parents give up during this period due to the lack of support and challenges of breastfeeding. The recommendation of further investment into breastfeeding peer supporters is backed up by reports that peer support workers have improved breastfeeding outcomes and “mums do tell us is really helpful just knowing that if they're struggling they can phone a buddy who will give them reassurance” 89 .
Delivery style
Education itself does not appear to be sufficient in increasing positive engagement. It must be coupled with an appealing and unprovocative delivery style and careful language. Professionals report that the Baby Friendly Initiative has positively evolved their approach and delivery style in a productive and constructive way, moving from “being very staunch, We are supporting breastfeeding, protecting breastfeeding, trying to promote it all the time” to acknowledging the real life constraints and saying, "No matter which feeding choice you choose, we want you to do that having been informed with the evidence, and when you make your choice we want to support you to do it in the most safe way." 90 They are emphasising woman’s empowerment and choice by educating staff and mothers regarding the options and how the infant brain builds and bringing about non-judgemental support for women who make the choice to formula feed so that infant development and motherbaby attachment bonding is still promoted to the highest degree possible. If a mother does decide against breastfeeding or has done so with previous children, care must be taken not to make her feel inadequate or guilty as “None of us are perfect and it's the hardest job in the world. All we're doing as health professionals is imparting that information to them and then listening and helping to support them, because it's hard work” 91 .
Policy changes
Importantly, health visitors and midwives in the English sites argue that the UK government needs fully to adopt and improve upon implementing the International Code of Marketing of Breast-Milk Substitutes. While the code has been implemented in most member countries, “Britain decided to make its own little version up called the infant feeding regulations” 92. This legislation
89 Lanarkshire, fid49f17
90 Neath fi3d3d14
91 Morecambe, fie072b4
92 Morecambe, fi7f9efb
named “The Infant Formula and Follow-on Formula Regulations” incorporates part, but not all, of the Code into law, as it only applies to formula for babies under six months.
Recommendations
• Introduce a complete ban on advertising of formula based milk products for babies;
• Ensure that each new mother has individual support in place to help her overcome difficulties associated with breast feeding;
• Develop resource packages for mothers regarding a network of locations within easy reach where they can be comfortable feeding their babies or expressing their breasts;
• Provide support materials for mothers who are unable to breast feed their babies.
Chapter Nine: Safeguarding vulnerable groups
In the areas visited by the commission, many vulnerable groups with additional or unique safeguarding needs – beyond those created by poverty - were discussed. These groups include (but are not restricted to refugees and migrants; premature and hospitalised infants; looked-after infants, children and young people; infants at risk of care; victims of domestic abuse; substance (including alcohol) misusers and persons with disabilities. This chapter briefly explains the health and social care challenges facing these groups as well as the respective recommendations to alleviate them.
Refugees, asylum seekers and migrants
Several issues facing vulnerable refugee mothers and their babies were raised. Refugee women “who are seeking asylum, who shouldn’t be chargeable”, have “been turned away, saying that they’re not eligible to receive care”, “been told upfront that they should be charged, even though, again, they shouldn’t be chargeable” or have “been erroneously charged”. In other cases, “people who have applied for Section 4, haven’t received Section 4 – through no fault of their own – have then been charged…They’re now found to be eligible for Section 4 and receiving it. They’ve still been told that they will receive that charge, regardless”. This incorrect healthcare charging is having “such a harmful impact on people” and is “all the time being more and more proven to be harmful”. Its consequences are that women become “too frightened to
COVID-19
Staff from the refugee resettlement team in Lanarkshire report “It has just been a nightmare with COVID, because I can’t go out to go see them, and they can’t go in. I am trying to do video calls with them on my phone. Then, try and get an appointment doing three-way calls with midwives and hospitals. It’s really, really difficult just now”. As hospitals increased restrictions “they would only let the women in. The husbands couldn’t go in either. It was the women on their own. Even their interpreting services right now, they are not using face-to-face interpreters. They are not even booking interpreters over the phone. They are using, kind of like, this machine right now for interpreting”. She says that clients feedback the machines are “okay” but “there is still a lot of confusion. They don’t really always know what is going on. It has been much more difficult”.
Lanarkshire, fi62ad07
access care”, “haven’t been receiving the care they need, or…There’s been a big delay in them accessing care” 93 .
Several suggestions for improving the situation for refugees, asylum seekers and migrants were made by respondents: “as a blanket, we would say that the charging regulations ought to be rolled back in. Or at least, if they are going to be maintained, Maternity Action at the moment have a judicial review pending, saying that maternity care, pregnant women, etc., should be exempt”. Secondly, Section 4 has not been implemented well and much suffering would be prevented “if only the Home Office may be allocated resources, allocated training, did something that meant that Section 4 was implemented in the way that the policy itself says”. Thirdly, accommodation standards need to be correctly implemented, as “the system for how properties are checked doesn’t seem to be working. So, it’s quite like soft-touch stuff that should all be happening but hasn’t been, to make sure that when housing providers are looking to move somebody because of transition, it’s that there are those rigorous checks in place to say that they are moving people into accommodation that is appropriate and is within the size regulations, that has the full inventory. All stuff that really is there and laid out in the contract, but just to make sure that it is happening” 94 . Premature and hospitalised infants Serious, often unrecognised long-term health implications of infant hospitalisation due to premature birth or surgery may impact “socially, emotionally, behaviourally on the child, but also on the whole family system”. The impact this can have on the child is highlighted in figure 17. After discharge from neonatal units is a crucial time parents begin to have difficulties and problems. For example, “when parents are discharged from the unit, mothers are more likely to have postnatal depression and posttraumatic stress disorder, but research that Leo's Trust did in England showed the emotional impact that having a premature baby can have, not only on the parents but on grandparents and babies as well”.
93 Middlesbrough, fi1d7ffb
94 Middlesbrough, fi1d7ffb
of Neo-natal Intensive Care Unit on Infant

Reprinted from, Infant medical trauma in the neonatal intensive care unit (IMTN), by A.L D'Agata, E.E Young, X.Cong, D.J Grasso, J.M McGrath, and P.L Forsythe, 2016, Advances in Neonatal Care, 16(4), 289-297. Copyright 2022, by The National Association of Neonatal Nurses. Reprinted with permission.
The needs of these families are “often just totally ignored” and if this issue is not recognised and changes implemented in “services and development policy in order to be able to meet that need”, children will continue to present with predictable (and avoidable) behavioural, social or emotional problems further down the line. 95 . Hospitalised infants often have “spiky profiles in terms of neurodevelopment” and are “the clumsy children or the children who are coming last in the class. The stakeholders’ response to this is ““Seriously? Take a good developmental history, that child has spent most of the first six months of its life in hospital. It’s had developmental interrupters, attachment interrupters because you can’t get the same experience of attachment when you’ve been in hospital, and that’s the reason for the difficulties you’re seeing because there’s been a difference in how the brain has developed.” Regarding interrupted process of attachment bonding, damaged parent-child relationship or parental mental health issues, “A lot of the relational impact is because of the experiences the parents have had and the trauma they’ve experienced, especially if there’s been early hospitalisation, they thought they were going to lose their child” .
“There are a lot of things we can do if we can just get in early. An awful lot of things can be done, especially in hospital, to improve the parent-child relationship [ by working] alongside our medical colleagues to provide nonmedical support. That's a listening ear. It's help for parents maybe to fill in a children in need application. We bring clothes and equipment to the parents as well. We also have a breast pump loan service”. However, “When babies are discharged, our work then really begins” to “offer support in families' homes” visiting “certain families, between one and eight weeks, to offer a listening ear, signposting to other services, and provide help in terms of moving out of the home so they don't become isolated but moving into our community services” 96
Looked-after infants, children and young people
A respondent reports “we have a real issue” with child trafficking and exploitation of children in care, as “unfortunately, our young people, especially in residential [facilities], who are looked-after, come together and introduce each other to these places and to, mostly men, sometimes women. But yes, it’s a real worry”. Despite sharing intelligence across Police, Health and Social Services regarding “where young people are going when they're running and where they're found…the reality is that young people will continue to go back” to the people and addresses known to be involved in these operations. Child
95 Derry, fiedc347
96 Derry, fibe69b4
exploitation and trafficking interlinks with drug use in looked after children, as one nurse relays how “I had a conversation with a wee girl the other day, she’s 14, and she loves drugs, loves taking drugs, that’s just the thing she wants to do. I said to her, “How do you pay for it?” She said, “I don’t have to pay for it.” And I said to her, “The debt will be called in at some point, and it may not be money that they're looking for.” But she just thinks they're her friends and they’ll look out for her. So, it’s very difficult” 97 .
She also raises how there is a big problem with fetal alcohol syndrome (FAS)in looked-after children, due to alcohol abuse in girls and young women who go on to have their children removed. Another respondent accounts the extremely high rates of FAS in foster children, where in terms of the numbers of infants with this disorder “it’s two to three times bigger than autism. So we know autism pathways exist, ADHD pathways exist, and this is also preventable. So we ought to be doing more, this one thousand days. It’s really important”. She believes of individuals with FAS, “70% or 80% go through the care system. So they’re society’s children and we know that they’re vulnerable, and we know outcomes are poor, poorer, than people who’ve been in the looked after system, generally” 98
More research needs to be done especially on FAS and staff need more training on it, as “it’s a really important thing to know. Because I think when you're trying to safety plan or teach these people about things like contraception or what would happen if they were to have a baby, you need to aim it correctly”. FAS affects the way people learn and communicate, and evidence suggests it is extremely common in looked after children
Infants at risk of becoming looked-after
Respondents say that the level of risk and caseload weight has increased over that past ten years, and this “changing in the thresholds as well for social working stuff has had a very detrimental effect” on both service users and the staff who “know they’re dealing with really dangerous stuff and they can’t give it the input and it’s going to blow up in the face anytime”. For example, “we had a child death not last year but the year before and that’s had a real huge eye opener for staff”. 99 .
For babies who are likely to be removed into permanent care, a specialist nurse for looked after children reports “we have a real issue with
97 Derry, fi76ed1d4
98 Middlesbrough, fi4dde45
99 Derry, fif006f6
accommodation. So, we have no mother and baby placements. We have some specialist foster placements, and that’s the ideal, where we put mother and babies, when we’re hoping that mum is going to be able to keep baby with her” 100. This lack of suitable placements lowers the likelihood of mother and child being able to remain together safely and increases the likelihood that the child will be moved around and placed into care, affecting the development of secure attachment and increasing the probability of future negative health. There is a pressing need for mother and baby units in the UK, as reported by one respondent in Neath who explains “We haven’t got a mother and baby unit in Wales. Again, that’s down to resource. You’re lucky if there’s a bed available because they are quite small units.” 101 Similarly another says “we need better mother and baby placements, because a lot of these women can do it, they're so capable, they just need the skills. They’ve never been taught how to parent, they’ve never been parented themselves”. Educating service users how to parent is crucial, as “we sit here with a list and say, “You have to do this, this and this, for you to keep your baby with you.” But we don’t really give them the tools or the help to- You know, you kind of have to go and do it yourself” “And we don’t also give them the chance, when they fall, to pick themselves back up again. You know, we’re very much time-driven – “You have to do this, you can’t mess up.”. However, if these are not available, concurrent planning is the next best thing for the baby as “if baby can’t go back, then it stays where it is” 102 .
100 Derry, fi76ed1d4
101 Neath, fiff4ade
102 Derry, fi76ed1d4
Domestic abuse
Respondents from each locality reported “Domestic abuse in this area is rife. It’s really high, really high and it’s just forever growing. We’ve got a massive problem with domestic abuse in this area. It’s horrible” 103 Figure 18 exemplifies this as it depicts the high level of potential domestic violence in Neath Port Talbot in 2015/2016. Moreover, if the service user has “been a victim of domestic violence, they seem to fall into that same sort of relationship again. And, instead of waiting for it to become really stable, and think, “Let’s get a house together,” they’ll just have a baby together. It’s almost like the baby is the commitment” 104. Thus, more children are born into families with a background of domestic abuse. Another notes one challenge is when they “get referrals from Social Care and the victim doesn't actually want to come into the service, but feels that they have to for part of the child-protection plan”. This may happen because victims of domestic abuse do not have a full understanding of what domestic abuse entails or its impact upon themselves and their children, and there is “an element of minimisation or maybe just not really understanding what they're affected by” or “they just don't think the children are affected by it, and that's a very common pattern”. When working with perpetrators of domestic abuse who have expressed a desire to change, staff say “it is a very delicate piece of work” because of associated risks. Challenging perpetrators and making them accept the impact of their behaviours “can be quite risky, so we have a safety worker which runs alongside that service, who checks in with the victim regularly to make sure that things aren't escalating as a result of our challenging and discussions throughout the groups”. Another challenge faced by staff is supporting victims in affluent areas, “which we find to be sometimes our most difficult
103 Clacton, fi2b104e
104 Clacton, fi966b1a

Note: Figures for 2015/2016. Reproduced from Neath Port Talbot Violence Against Women, Domestic Abuse and Sexual Violence Strategy 2016 - 2019. by Welsh Government, n.d. https://democracy.npt.gov.uk/documents/s27881/Draft%20VAWDASV %20Strategy.pdf
areas because of the lack of eyes on a family and the lack of services”. Within these communities, members of the public “don't mind fundraising for you, but they won't really accept that it's happening in their area. We find that with schools. We find that with GPs. We find that even on the local streets” 105 Specialist midwives act as key-contacts, coordinators, and try to “educate about adverse childhood experiences and the impact of that on families, and try and encourage people to not choose that for themselves, or to know that they have a choice, rather, not to choose it for themselves. But a lot of families don’t know that there are any choices, and they’re very limited anyway”. When women are referred to them, they “deal with all the social workers and all the horrible stuff, and they can, you know… They tell me all these horrible things that happen to them, and then that’s it. They don’t have to tell anybody else, because I’ll coordinate that for them” 106 .
The introduction of a routine domestic abuse enquiry pathway has “definitely made a difference” and “replicated the research. I think their disclosures rate increased by six times, and I think… I’m not sure whether ours has gone up that much, but ours has definitely increased since we introduced that” 107 Staff say that when asking about domestic abuse during routine enquiry, professionals must word their questions and explanations very carefully to help women disclose any abuse. For example, it is important to word questions “in such a way that she realises that domestic abuse just isn’t something physical, that it could be emotional, financial, psychological abuse, and maybe give
105 Middlesbrough, fi2006d8
106 Morecambe, fi79d21c
107 Morecambe, fi79d21c
some examples of what that could be, rather than just saying, “Are you suffering from domestic abuse?” 108 .
To work with child victims one must work with the whole family unit, as “if you can make those changes in that family before they have any more children, when they go on to have other children, then absolutely, those children will benefit from all of that work that has been done”. Due to the intergenerational transmission of abuse, “you can't pluck the child out of the context, do a bit of therapy and put them back, and everything is all hunky-dory”, thus teams must look at the experiences of the whole family for the best results 109 .
COVID-19
Staff from a refugee resettlement team report that COVID has also hindered safeguarding procedures, as the opportunities for picking up on the subtle signs of abuse or privacy necessary for disclosure are no longer available. Under normal circumstances “you would go in. You would have your booking appointments, and that would be face-to-face. They would get all the information. They would ask you things like, “Do you have problems with domestic abuse? Is there any kind of that in the household?”. However, “Right now they are doing these appointments over the phone, and they don’t know what’s there or who is there. The husbands could be there. The husbands could be abusing them, or there could be things that are going on, and they are not getting appropriate answers to these questions, because even if you are on the other end of a phone, you don’t know who else is in the room. There might be pressure there where they can’t answer the question appropriately”. Additionally, women locked into houses with their abuser are “getting pregnant. There is more pressure on pregnant women, and you know, domestic abuse when women are pregnant. I think this is an issue right now with pregnant women”. Lanarkshire, fi62ad07
Substance misusers
There were high levels of substance abuse within all the communities we visited. Figure 19 supports this as it indicates that there were higher numbers of drug-related acute hospital stays by individuals residing in the most deprived areas of Scotland in 2015/16. Therefore, it seems that deprivation and substance abuse go hand in hand.
108 Derry, fi2e74ad
109 Middlesbrough, fi55b949
Number of drug-related general acute hospital stays in Scotland in 2015/16 by deprivation

Reproduced from SPICe Briefing Drug Misuse, by SPICe, 2017, https://archive2021.parliament.scot/ResearchBriefingsAndFactsheets/S5/SB_17-22_Drug_Misuse.pdf
Copyright n.d. by Scottish Parliament. Reprinted with permission.
One respondent argues this is connected to the sense of hopelessness and despondency caused by poverty, when he explains “nobody moves [there] Everybody ends up [there]. There's no employment. There's lots of drugs, there's lots of alcohol, but worse than anything, there's no heart” 110 .
Community midwives note “we’re starting to see, unfortunately, more issues with drugs that we didn’t have” 111 previously. A specialist nurse says that for infants who are “going into a placement where we’re not quite sure if they're going to remain with mum”, the “difficulty in that phase [the first 1,000 days], we would find, for that cohort, is keeping babies and mums safe”. A main risk is that a lot of pregnant mothers are “engaging in really worrying things, like a lot of alcohol misuse, drug misuse, mental health, homelessness all those sorts of things. So, it’s very difficult. We try and safety-plan as best we can but, really, until we get baby delivered, that’s the difficult period”. She notes that many young people currently in care will continue to be the next generation of parents, however “we’re in quite a difficult time just now. I think there obviously always have been issues with drugs and alcohol and mental health, I don’t know if it seems especially awful just now…Legal highs are a major thing for us just now, and it just creates absolute chaos, it really does” 112 .
110 Clacton, fief656b
111 Derry, fi2e74ad
112 Derry, fi76ed1d4 Figure 19
Preventing and addressing substance abuse requires “educating mothers, the effect that that drug use is having on an unborn baby, because a lot of them haven’t seen a baby that’s withdrawing and haven’t seen the difficulties that they shouldn’t go through”. Also important is helping women to develop their own intrinsic motivation to change and develop their trust in the services. Some women do manage to change their behaviours “if they’re a person who wants to change to be able to care for their child, to have the family unit”, however in many cases the internal motivation is lacking because “they’re being dictated to or they’re saying, “To keep your child, you need to do this,” then it’s not always the best, you know?”. In addition to resentment leading to lack of compliance and engagement, the respondent reports that many women are disheartened from trying to change their behaviours due to mistrust of the services and the expectation that ““Oh well, you’re going to take my baby off me anyway. So, what’s the point? I may as well just do what I’ve got to do and don’t worry about how they can protect these happening to their children, going forward” through education 113 .
Persons with disabilities
Those who work with parents with learning disabilities appear to be thin on the ground with workload becoming particularly challenging. There is a clear gap in services for parents with learning disabilities, who could benefit from the provisions offered by Adult Services but very few meet the criteria. Thus, the needs and vulnerabilities within these families are not being well met or a lower level of care is provided, which a staff member says is “quite unfair, that just because they’re not open to adult services they still have vulnerabilities that we need to address as well”. Advocacy work is necessary for this population during meetings because “sometimes they feel a little bit under pressure during those meetings to ask questions in case they look a bit silly”. Therefore “if you go to any child protection conferences or any reviews then they have the advocates there for the parents to then explain what’s been discussed” and “after the meeting I would check out with them that they’ve understood everything and things like that as well” which makes them “feel more comfortable” 114 .
113 Lanarkshire, fi97ff4c
114 Neath, fif1071a
COVID
A respondent who supports youngsters with additional support needs, says the implementation of the 1140 hours project which increases nursery provision for children under the age of three in Scotland involved the opening of new nursery establishments and extensions to existing nurseries “to accommodate the increased capacity, if you like, that we need to find within early years to accommodate those children”. However, “There have been some hold ups due to COVID because, obviously, sites were shut down and just the way that building and planning works, people often have a slot for something and then they move onto other projects. So, there is a bit of an impact on that, and in terms of the implementation of 1140 hours we have been delayed”.
Lanarkshire, fi5fcb01
Autism Spectrum Disorder (ASD) is “one of our most common increasing neurodevelopmental issues that we have nationally as a real big crisis”. There is a particular “gap in our service delivery in terms of children aged 14 onwards who are NEETs [Not in Education, Employment, or Training], who have ASD, whether diagnosed or not, who have either been excluded from school or have excluded themselves from school and are just off-radar and then present in crisis somewhere further down the line. There is absolutely no support there whatsoever or there is no engagement with any of those mainstream services” 115 . Likewise, “ASD is a huge issue that has come up in 20% of all referrals say to family resource centres. It’s coming up all the time”. This need is unmet by the statutory services and the third sector “have to be very careful that we don’t fill a gap for statutory service because initially when we started there was…a lot of areas where ASD a lot of them they have no staff” 116 .
To tackle this, one area has developed an ASD connect service which utilises the relationships and partnerships that mental health voluntary sector organisations have with “schools and with the DWP, the much wider partners” as well as parents, to find these children and reconnect them into society Another reports that increasing numbers of infants presenting with the disorder could be reflective of what appears to be an increased public awareness of ASD. They say “There certainly is more awareness of ASD, and if you ask any therapist, they’ll say the numbers for ASD have significantly grown.
115 Clacton, Fi273827
116 Derry, fif006f6
We feel as if there is that, you know, because there’s more public awareness, families are coming and asking us, ‘Do you think my child has autism?’” 117
Recommendations
• Standard of accommodation for refugees/asylum seekers or those suffering from domestic abuse needs to be thoroughly checked before people are placed;
• Volunteers from the community should be encouraged to work with parents of children requiring hospitalisation to provide them with support and material goods where required;
• More investment is required to prevent children becoming looked after by ascertaining the key cause of the problem and providing appropriate support;
• Looked after children, especially those in residential facilities, require intensive support and education to improve outcomes;
• Routine domestic abuse inquiries should be instituted when women are attending ante natal and immediate post-natal services to ensure the safety of both mother and infant;
• Parents with disabilities must have appropriate specialist professional support backed up by well trained volunteers in addition to other professionals.
117 Lanarkshire, fie6285c
Chapter Ten: Conclusions and recommendations
The Liverpool Health Commission has visited seven localities with high areas of deprivation where its commissioners have heard evidence from those directly providing and receiving services that are pertinent to the first 1000 days in each locality. We did not attempt to speak to managers but rather we chose to engage with people providing the hands on services as well as those receiving them.
Our findings, however, as has been illustrated in the previous chapters, are consistent with those of the national and international reports we cited in Chapter Two, many of which had written or oral evidence presented to them by more senior personnel or parents who engaged with particular social media sites.
Findings
Our main findings are:
• Finance:
o Difficulties have been experienced by people who are not made aware of eligibility for certain benefit and who are struggling to make ends meet.
o The introduction of universal credit and subsequent changes to it have caused considerable confusion amongst both service providers and users.
• Housing
o Homelessness, housing provision and temporary accommodation are often inadequate for families with children in the first 1000 days of life
o Landlords are frequently not held accountable for their actions
• Local service provision
o Families struggle to maintain a good diet because of a lack of nearby providers of nutritious and affordable food.
o The reduction in Children’s Centres has led to social isolation as many families cannot afford the cost of public transport to their nearest centres
o Public transport is often inadequate especially in, though not limited to, rural areas
• Mental health
o Intergenerational cycles of poor mental health are being perpetuated
o Mothers suffering from mental health problems face difficulties in seeking help to reach out for help and there are insufficient trained carers to meet their nee
o Early detection and prompt management of infant mental health problems is rarely possible
• Infant nutrition
o As well as cultural resistance to breastfeeding public attitudes prevent some women from trying to breastfeed their babies
o Inaccurate information is often spread about breastfeeding on social media sites and bottle feeding still advertised on television
• Particular vulnerable groups
o Refugees and other migrants are frequently separated from their cultural groups and are unable to communicate and so obtain essential services.
o Babies who have been hospitalised do not always receive follow up services
o Families who are drug/alcohol dependent are not always recognised and appropriate action taken in regard to their babies
o Domestic abuse is widespread with affected families not always being able to remove themselves from danger
• Overall
o Conflicting advice is often received from different agencies
o The involvement of multiple professionals can preclude the establishment of trusting relationships between service users and providers
Recommendations
1. Community participation, and involvement of voluntary agencies should be maximised to tailor support and services around the individual needs of families.
2. Joint agency working remains a significant challenge to achieve and should be addressed as a matter of urgency to improve support for service users and outcomes.
3. Communication methods between staff and service users should be reviewed to ensure they are empathetic, effective and appropriate to meet needs.
4. Mobile services such as those provided in some rural areas bring services to the more remote communities. They could be used in urban areas where transport and access are barriers to service users.
5. Family focused approaches would ensure that awareness of the needs in the first 1000 days is not simply the responsibility of the mother. Families and extended families could be included in being supported to care for the baby
6. Policy changes are required to offer universal, long-term, appropriate support to families in need in the first 1000 days.
Recommendations
Recommendations have been made in the previous five chapters in relation to each of the major issues raised.
Overarching recommendations
1. Noting the often repeated mismatch between the wishes of professionals to use education to improve families’ circumstances and the ability of the families to respond, further exploration of more effective interventions is merited;
2. Community participation, and involvement of voluntary agencies should be maximised to tailor support and services around the individual needs of families.
3. Joint agency working remains a significant challenge to achieve and should be addressed as a matter of urgency to improve support for service users and outcomes.
4. Educating staff and service users so that services can be optimised. This may be through organisations who employ staff, but also in the third sector. In some cases, too much information is presented at once and in others insufficient is given. A middle-of-the-road, empathetic approach needs to be employed which would build relationships between services users and providers, and within communities.
5. Mobile services such as those provided in some rural areas bring services to the more remote communities. They could be rolled out in other areas.
6. Family focused approaches would ensure that awareness of the needs in the first 1000 days is not simply the responsibility of the mother. Families and extended families could be included in being supported to care for the baby
7. Policy changes are required to offer universal, long-term, low-level support to families in need in the first 1000 days.
Conclusion
By interviewing front-line staff and service users the commission was able to understand their actual lived experiences. Many of the findings reflected failings that had been perpetuated over many years, which have been reported in a number of earlier reports and academic articles. However, also it was encouraging to find largely unreported successes throughout the country, which merit inter regional-sharing and adaptation to different settings. It is encouraging to see such initiatives, which, with sufficient and sustainable funding and support can benefit the future generations. Although across the UK there is a policy commitment, to improve child health outcomes it is evident that much more investment and service development is needed to achieve the desired goals.
References
Annual Population Survey 2020/21. Edinburgh, APS Group Scotland. Care Quality Commission (2021). “University Hospitals of Morecambe Bay NHS Foundation Trust, Inspection report.” Retrieved 11 Jan 2022, from https://api.cqc.org.uk/public/v1/reports/3b80406d-f460-4a53-bc465a02451638ab?20211223165846
Barens, M. and C. Lord (2012). Multiple disadvantage in Scotland. Secondary analysis of the Scottish Household Survey dataset.
Bowlby, J. (1969). Attachment and loss. New York, Basic Books.
Braun, V. and V. Clark (2013). Successful qualitative research: A practical guide for beginners. London, Sage.
Committee, H. o. C. H. a. S. C. (2019). First 1000 days of life report. London. Cook, S. and T. Cameron (2015). "Social issues of teenage pregnancy." Obstetrics, gynaecolgy and reproductive medicine 25(9): 243-248.
Early Years (2019). Annual report 2018-9. Belfast, Early Years.
Education and Training Inspectorate (Northern Ireland (2020). an evaluation of imporving practice in Sure Start. Belfast, ETI.
European Parliament (2019). Access to maternal health and midwifery for vulnerable groups in the EU: 64.
H.M. Government (2021). The best start for life: a vision for the 1,001 critical days. London. Institue for Health Equity (2019). Health equity in England: the Marmot review 10 tears on Joseph Rowntree Foundation (2021). Annual poverty report. London, JRF. Joseph Rowntree Foundations (2017). UK poverty report. London, JRF.
Leadsom, A., F. Field, P. Burstow and C. Lucas (2014). The 1001 Critical Days: The Importance of the Conception to Age Two Period. .
Liverpool Health Partners (2017). Business plan 2018. Version 1.2.
Liverpool John Moores University. (2017). "Strategic Plan, Liverpool John Moores University, 2017-2222." Retrieved February 9, 2021, from https://www.ljmu.ac.uk/~/media/files/ljmu/public-information-documents/strategicplan/ljmu-strategic-plan-2017-2022.pdf?la=en
Maddison, F. (2020). A lifeline for our children. York and London: JRF and Save the Children. .
Marmot, M. (2010). Fair society, healthy lives.
Maxwell, C. (2019). A mixed methods study exploring UK mothers' experiences of bottle refusal by their breastfed baby PhD, Liverpool John Moores University. Morecambe Bay Coastal Community Team (2017). Coastal Community Team Draft Economic Plan 2017-2022.
Perry, C. (2013). Early years provision: Research and Information Service Research Paper. Belfast, Northern Ireland Assembly.
Perry, C. (2016). Early years and children’s services: a brief overview. Belfast, Northern Ireland Assembly.
Porter, I. (2020). Autumn Budget - why we must keep the £20 social security lifeline.
Public Health Wales. (2016). "Submission to National Enquiry on first 1000 days CYPE(5)-2917 – Paper 2." Retrieved 24 Feb 2021, 2021, from
https://business.senedd.wales/documents/s67718/CYPE5-29-17%20-%20Paper%202%20%20Public%20Health%20Wales%20%20Response%20to%20First%201000%20days%20consultation.pdf.
Scottish Government (2009). The Early Years Framework. Scottish Government. (2020). "Scottish Study of Early Learning and Childcare." Retrieved 23 Feb 2021, from https://scotcen.org.uk/our-research/research/scottish-study-of-earlylearning-and-childcare/.
The All Party Parliamentary Group for Conception to Age 2 (2015). Building great Britons. The Royal Foundation (2020). State of the nation: understanding public attitudes tot he early years
UNICEF United Kingdom. (2021). "The Baby Friendly Initiative - Early Moments Matter." Retrieved Feb 12, 2021, from https://www.unicef.org.uk/babyfriendly/early-momentsmatter/.
United Nations. (2015). "Sustainable Development Goals." Retrieved Feb 9, 2021, from https://sdgs.un.org/goals
United Nations. (2017). "Early Moments Matter." from https://www.unicef.org/earlymoments
WAVE Trust (2018). 'Age 2 to 18 - systems to protect children from severe disadvantage'. Welsh Government (2020). An overview of the Healthy Child Wales Programme. Welsh Government (2021). Welsh Government programme for 2021-2026 update. Welsh NHS Confederation. (2016). "Submission to national inquiry on First 1000 Days: CYPE(5)-29-17 – Paper 1." Retrieved 24 Feb 2021, 2021, from http://www.seneddtest.assembly.wales/documents/s67717/CYPE5-29%20-17%20%20Paper%201%20-%20Welsh%20NHS%20Confederation%20%20Response%20to%20First%201000%20days%20consultation.pdf.
World Health Organisation (2013). Essential nutrition actions. Geneva, WHO.
Zeanah, C., L. Berlin and N. Boris (2011). "Practitioner review: clinical applications of attachment theory and research for infants and young children." Journal of Child Psychology and Psychiatry 52(8): 819-833.
Appendix 1: Commissioners and University Staff
Commissioners
Dame Lorna Muirhead
Chair
Former president Royal College of Midwives and Former Lord Lieutenant, Liverpool
Ms Maggie O’Carroll Director, The Women’s Association
Dr Paul Hughes Director Addaction
Dr Colm O'Mahony
Sexual Health Consultant
Mr Neil Frackelton Chair SWACA
Dr Mary Packer
Obstetrician and Gynaecologist
Prof Vivian Hope Public Health Specialist
Dr Ruth Hussey
Former Chief Medical Officer, Wales
Prof Barbara Parfitt Professor Emeritus of Nursing
Dr Sue Thomas Chair, the Whitechapel Centre
Dr Urmi Das Consultant Paediatrician, Alder Hey Hospital
Mrs Janet Brennan Deputy Director of Nursing, Liverpool Women’s Hospital
Liverpool John Moores’ University Staff
Professor Valerie Fleming Academic Lead. Professor of Women’s Health
Dr Lorna Porcellato Reader, Public Health Institute
Ms Sarah Wolffe Research Assistant
Mr Gerry Diver
Project administrator (until November 2020)
Ms Becky Self PhD student/research assistant
Ms Jen Lovelady
Project administrator (from December 2020)
Appendix 2: Schedule of visits
Morecambe: 29/30 October 2019
Middlesbrough: 26/27 November 2019
Derry 15/16 January 2020
Clacton on Sea 11/12 February 2020
Neath/Port Talbot 17/18 March 2020
Lanarkshire (Microsoft Teams) 22-25 September 2020
Liverpool 1-2 September 2021
Appendix 3: Organisations giving evidence
Morecambe
Home start
Social Work
Specialist Midwives
Community Midwives
Royal Lancaster Hospital
Nursery Manager
Council
Health Visitors
*Service users
Middlesbrough
Community midwife team
Barnardo’s
Public Health (local Authority)
National literacy Trust Hub
Strong families
Middlesbrough Council
Fetal Alcohol Spectrum Disorder (NGO)
Harbour (NGO)
Maternity Voices’ Partnership
Asylum Matters
Health Visitors
*Service users
Derry
Paediatric Psychology Service, Western Trust
DCSDC
Health Visitors
Family Support Hubs
Women’s Centre
Action for Children
Specialist Health Visitors and Midwives, Western Trust
Child and Family Support team, Western Trust
Tiny Life
MACE trust
Community Midwifery Team
*Service users
Clacton on Sea
Community Builder
Essex Fire and rescue service
Child and Young Persons’ Transformation Programme
Family Solutions
Essex Council
ECFWS??
Extra- Support for Families
Jaywick Community Resource centre
Essex Child and Family Wellbeing Service
Home Start
Coastal Birthing Unit
Community Midwifery team
Sydney Health Hub
*Service Users
Neath/Port Talbot
Team around the family
FAST team
Flying start
Social Work
Community and Primary Care
Midwives
*Service users
Lanarkshire
Social work
Infant Mental Health
Alcohol & Drug Partnership
Health Improvement
Child Protection
South Lanarkshire Partnership
Educational Psychology
Health & Homeless
Cares
Early Years Education
South Lanarkshire Leisure & Culture
Fàs
Family Nurse Partnership
Speech & Language Therapy
FASD
Health Promotion
Child Health Commissioner
Refugee Resettlement Programme
Child Smile
Public Health Nutrition
Infant Feeding Development
Money Matters
Scottish Government
Social Work Family Centre
**Service users
Liverpool
***Service users
*In each area, service users approached us spontaneously thanks to publicity generated by local media. Additionally service users were part of delegations form a number of organisations.
** Because of Covid restrictions, the Lanarkshire meetings were online and thus no spontaneous approaches could be made. A member of the commission who lived locally was able to speak to some on other dates.
*** Sessions were specifically organised for service users
Appendix 4: guiding questions for sessions 3-6
1. What input do you (does your organisation) have to the -9 months – 2 year age group?
2. What is its particular contribution?
3. How does it dovetail with other organisations in the area?
4. How do people get to know about you?
5. What about vulnerable groups? Do you deal with a special group you would classify as such?
6. Can you give an example of a special initiative you have worked on?
7. What do you see as the biggest problems in the area with regard to this age group?
8. What other organisations are contributing especially to this age range?
9. How do you see the interface between public and voluntary sectors (and health and social services)?
10. What would you see as lacking in this area?
11. How could it be addressed?
12. If you had a blank slate, how would you propose to set up services that are relevant and inclusive?
Appendix 5: Questions for service users in final focus groups
Finance
Can you give us any examples of people you know who are working but struggle to make ends meet?
Do you know of anyone who is afraid that if they go into work, it could make their financial position worse as it would affect their benefit?
Has universal credit made things better or worse?
What is in place to help families to budget?
Have you come across people who don’t know they are eligible for some benefits?
What do you think about present assistance form the government for childcare?
Housing
Can anyone comment on the appropriateness of referrals in this area?
What about catering to the needs of pregnant homeless women or mothers?
Have you any experience of people moving to low cost rentals?
What do you think of the idea of payments being made directly to landlords out of someone’s benefit?
What do you think about the provision of community housing in this (or nearby) area?
Local services
What sort of access do you have to local supermarkets etc?
What services for people with young families are there?
Do you feel you can access essential services using public transport?
Is it easy to see the doctor/nurse/midwife?
If you need specialist medicals services where do you go?
Are there services for particular groups like refugees or teenage parents?
Do you feel that services should be post code driven or should the same services be available for all?
Mental health
How have you learned your parenting skills?
Do you know of services that are in place for people who may not have had a good parenting role model
What is in place to help isolated people learn to interact with other parents?
What would your advice be to teenagers who want to have a child?
What services exist locally for maternal/infant mental health?
Infant nutrition
How are the majority of babies fed in your experience in this area?
What do you think are the main barriers to breastfeeding?
Have you ever seen adverts on TV for bottle feeding? (should these be there?)
Have you seen any children suffering from fetal alcohol syndrome, due to their mothers drinking excessively during pregnancy?
Do you know what services are available?
General
What conflicting/confusing messages do you see or hear of people receiving?
What are the main barriers preventing you from receiving essential services? What experience do you have of people having to go to multiple agencies to receive help?
Do you think that health/social care professionals can easily engage with you?
Do they have enough knowledge to help people deal with their situations?
Have you experienced any pilot groups that work well but simply stop when the money runs out?
Ask about specific vulnerable groups that have been mentioned in the report e.g.
Refugees/forced migrants
Infants born prematurely or with medical problems.
Parents with disabilities
Looked after (or in danger of being looked after) infants
Victims of domestic abuse
Substance misusers
Finally, If you could make one recommendation to improve things, what would it be?
