McGan Insulation Tester



Detect



















Detect
Test
Test




in
Next
it over the dark web.
as a point of
email,
TechNation (Vol. 13, Issue #11) November 2022 is published monthly by MD Publishing, 1015 Tyrone Rd., Ste. 120, Tyrone, GA 30290.
POSTMASTER: Send address changes to TechNation at 1015 Tyrone Rd., Ste. 120, Tyrone, GA 30290.
TechNation magazine is dedicated to providing medical equipment service professionals with comprehensive, reliable, information concerning medical equipment, parts, service and supplies. It is published monthly by MD Publishing, Inc. Subscriptions are available free of charge to qualified individuals within the United States. Publisher reserves the right to determine qualification for a free subscriptions. Every precaution is taken to ensure accuracy of content; however, the information, opinions, and statements expressed in the articles and advertisements herein are those of the writer and/or advertiser, and not necessarily those of the publisher.
PUBLISHER John M. Krieg
VICE PRESIDENT Kristin Leavoy
ACCOUNT Jayme McKelvey EXECUTIVES Megan Strand
ART DEPARTMENT Karlee Gower Taylor Powers Kameryn Johnson
EDITORIAL John Wallace
CONTRIBUTORS Roger Bowles K. Richard Douglas Jim Fedele Joie Marhefka Manny Roman Connor Walsh David Witt Steven J. Yelton
DIGITAL SERVICES Cindy Galindo Kennedy Krieg
EVENTS Kristin Leavoy
WEBINARS Linda Hasluem
HTMJOBS.COM Kristen Register Sydney Krieg
ACCOUNTING Diane Costea
EDITORIAL BOARD
Jim Fedele, CBET, Senior Director of Clinical Engineering, UPMC
Carol Davis-Smith, CCE, FACCE, AAMIF, Owner/ President of Carol Davis-Smith & Associates, LLC David Francoeur, CBET, CHTM, Service Zone Vice President Midwest Imaging - Siemens Healthineers Jennifer DeFrancesco, DHA, MS, CHTM, System Director, Clinical Engineering, Crothall Healthcare Rob Bundick, Director HTM & Biomedical Engineering, ProHealth Care
P.12 SPOTLIGHT p.12 Professional of the Month: Jason Head, CBET p.14 Company Showcase: Vizzia Technologies p.18 Department of the Month: The Atrium Health Clinical Engineering Department p.20 Shifting Gears: A Video Platform to Make Better Biomeds
P.24 INDUSTRY UPDATES p.24 News & Notes p.28 Ribbon Cutting: Maple Tree Biomedical p.30 AAMI Update p.32 ECRI Update
P.36 THE BENCH p.36 Biomed 101 p.39 Tools of the Trade p.40 Webinar Wednesday
P.61 EXPERT ADVICE p.61 Career Center p.62 [Sponsored] Innovatus p.66 The Future p.70 Cybersecurity P.76 BREAKROOM p.76 Did You Know? p.78 The Vault p.80 HTM Jobs p.82 Where in the World is Ben C.? p.90 HTM Strong p.86 Service Index p.89 Alphabetical Index
Like us on Facebook, www.facebook.com/TechNationMag
MD
800.906.3373
Email: info@mdpublishing.com www.mdpublishing.com
Proud supporters of



Children’s of Alabama is the num ber-one rated children’s hospital in Alabama, as ranked by U.S. News & World Report. The hospital receives high rankings within pediatric specialty services; ranking in the top 50 nationally in all 10 services areas, including cancer, cardiolo gy and heart surgery, diabetes and endo crinology, gastroenterology and gastroin testinal surgery, neonatology, nephrology, neurology and neurosurgery, orthopedics, pulmonology and urology.
In this center of excellence for pediatric care, the medical devices must be managed expertly.
Supervising the Biomedical Engineer ing Department at Children’s is Jason Head, CBET. Head has been a biomed for
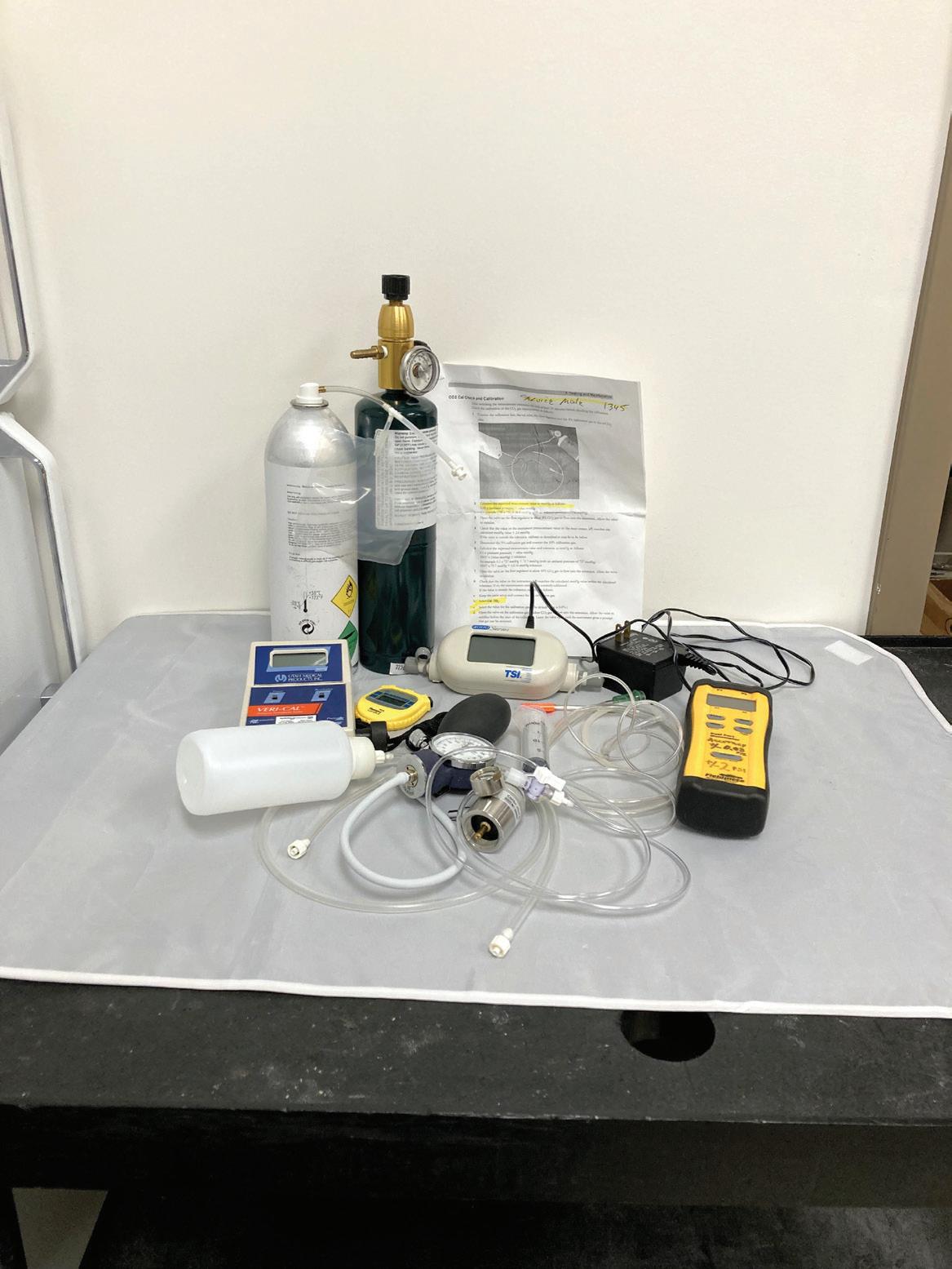
37 years and has been certified for a long time also.
“[I] have been a CBET since 1987 and took the test so long ago that I am grandfathered, so that I do not have to take the test again,” he says.
“I started out as a biomed tech at Schumpert Med Center. I have worked as a lead tech at East Alabama Medical Center, a field service rep for Datascope and Cobe/Gambro, a lead tech at Children’s Hospital of Alabama and am currently working as the biomed supervi sor at Children’s Hospital of Alabama,” Head adds.
Head’s acumen for electronics prompt ed an electronics course instructor at Jefferson State Community College to suggest a biomed training program.

“When I was in high school, I went to
the area ‘trade school,’ where I studied ‘radio and TV,’ which was a basic electronics course which prepared you to work on radio and TVs and industrial electronics. I excelled in this program and my teacher told me about a program called biomedical equipment technology at the University of Alabama at Birming ham, where they would teach me about medical electronics. I knew that I did not want to work on TVs for the rest of my life and that ended up being one of the smarter decisions I made,” Head says.
His specialty areas as a biomed are dialysis, the cardiovascular area, ECMO, physiological monitors and their associat ed networks.
Beyond the scope of a biomeds more
routine assignments are the larger projects that can come along periodically. Some of the most challenging can be new con struction projects or additions to existing facilities. Head has firsthand experience with this situation.
“In 2012, we opened a new 14-story facility in which we had to make sure that all of the new equipment was inventoried, checked and placed in the correct rooms,” Head says.
He says that they were implementing an RFID system in this new facility and he had to walk each area and name the IR and RF sensors so that they could track the equipment.
“We also had to rent transport monitors for the move of patients across three crosswalks from the old facility and the new facility that we did over the weekend. We also had to move existing equipment and set it up during the move, which included two intensive care areas, a step-down unit and a large ER with Level
1 trauma rooms. We had to do our day-to-day activities during the day and got the new facility ready after-hours and weekends, but we had the perfect group of guys and we pulled it off without any major issues,” Head adds.
More recent challenges are more in line with national trends. He says current issues include staffing, supply shortages and training new technicians.
Head does important work even when away from supervising biomeds on-thejob.
“I am also a firefighter/EMT in my hometown, am learning to play the banjo, and enjoy being with family and friends and following the Alabama Crimson Tide,” he says.
The family he mentions includes a long marriage.

“I have been married for almost 30 years to the prettiest and sweetest woman that I have ever met. We have three wonderful children and two grandchil
dren,” Head says.
He has some unselfish thoughts about his many years in the profession.
“I have enjoyed my time as a biomed and want to be able to leave it better than I found it by helping, and trying to teach the newer biomeds coming into the field what I have picked up in my journey,” Head says.
The pediatric patients at Children’s of Alabama can be confident that they have both the services of a world-class health organization along with expert biomeds, supervised by a conscientious professional.
FAVORITE BOOK: The Bible; “Black Hawk Down”
FAVORITE MOVIE: “Cool Hand Luke”, “Christmas Vacation”, “The Bridge on the River Kwai”
Jason Head, CBET, loves being able to support the health care needs of children as supervisor of the biomedical engineering department at Children’s of Alabama. When not at work, Head enjoys spending time with family and serving as a firefighter.

FAVORITE FOOD : Seafood, pizza
I can usually make people smile or laugh.
FAVORITE PART OF BEING A BIOMED?
Working with a great group of technicians. Meeting new people and having an opportunity to make their day a better day and the ability to serve the clinicians that help children get better and helping give children the opportunity to have a healthy and normal life.
WHAT’S ON MY BENCH : Bible, Diet Mt. Dew, Fluke multimeter, PicQuic screwdriver and an iPad.

Medical facility construction has shifted considerably in recent years. Now, there is a heightened sense of urgency to remodel, expand or build new clinics and hospitals to remain a health care provider of choice.
According to a 2022 hospital con struction survey conducted by the American Hospital Association, hospitals continue to invest in acute care facilities, with construction projects underway or in the planning stages increasing from 16% in 2021 to 23% in 2022.
Increasingly, these new state-of-the-art facilities are incorporating innovative healthcare technology management (HTM) solutions early in the design process that are implemented during the construction phase.

Vizzia Technologies is a recognized leader in the development of advanced real-time location systems (RTLS). Recently, several prominent health care providers have collaborated with Vizzia on their new hospital construc tion projects.
CHILDREN’S HEALTHCARE OF ATLANTA Vizzia participated in an extensive two-year national evaluation process to provide the industry’s most advanced RTLS asset management solutions to Children’s Healthcare of Atlanta.
Children’s selected the Vizzia InVIEW software platform to provide real-time data analytics to improve patient care and Vizzia’s enhanced Environmental Monitoring solution to protect patients and critical medical supplies, including vaccines. Vizzia also services Children’s Health of Orange County in California, a level 1 pediatric trauma center.
Children’s Healthcare of Atlanta is one of the largest pediatric clinical care providers in the country (1 million patient visits annually with 673 beds across three hospitals) and is consistently ranked among the top children’s hospitals by U.S. News & World Report.
Children’s new 70-acre medical campus features the Arthur M. Blank Hospital. The $1.5 billion health care project is the largest ever in the history of the state of Georgia. It includes a 9-story
hospital with more than 1.5 million square feet of space and a total of 446 beds. Also attached to the hospital will be an 11-story, 325,000-square-foot medical office building.
The RTLS technology that will be deployed and managed by Vizzia at Children’s is also used at other leading pediatric hospitals across the country, including: Boston Children’s, Children’s Colorado, Cincinnati Children’s, Chil dren’s Philadelphia, Stanford Children’s, Texas Children’s and St. Jude Children’s.
Grady initially selected Vizzia to optimize its legacy asset tracking system. The Vizzia professional services team conducted clinical interviews to discover use cases and performed an extensive audit to ensure maximum facility coverage.
Vizzia then delivered two powerful software modules of asset management and environmental monitoring to Grady. This enabled their biomedical engineering department to monitor thousands of
medical devices and clinical supplies in real-time across all facilities. Coupled with Vizzia’s fully managed solutions and on-site support team, they helped Grady to increase utilization rates of its devices and reduce staff time looking for clean supplies.
The Grady Health System in Atlanta, Georgia is one of the largest safety net health systems in the United States. Grady consists of the 953-bed Grady Memorial Hospital, six neigh borhood health centers, and the Marcus Stroke and Neuroscience Center. With its nationally acclaimed emergency medical services, Grady has the premier Level I trauma center in the metro Atlanta region and handles over 700,000 patient visits each year. Grady was named one of the nation’s “Most Wired” hospitals for the 8th year in a row and earned the HIMSS Analytics “Stage 7” designation.
Grady is building a new $227 million Center for Advanced Surgical Services (CASS) in downtown Atlanta. The expansion will increase Grady’s surgical clinic capacity by 45% and surgery capacity by 25%. This new 10-story, 577,000-square-foot facility will feature state-of-the-art technology. Based upon Vizzia’s proven RTLS solutions, Grady has awarded the company this major project.
Vizzia is also protecting Grady’s critical medical supplies, to include blood storage and COVID-19 vaccines. Real-time alerts let clini cians know if a refrigerator or freezer deviates from desired conditions to protect important and expensive products. Vizzia is the only RTLS provider to offer a fully managed service that provides live 24/7 customer service that proactively contacts clinicians to ensure alert resolution.
Piedmont had successfully partnered with Vizzia at its flagship hospital in Atlanta, saving hundreds of thousands of dollars by tracking equipment and right sizing its fleet. Biomedical engineering executives selected Vizzia as their systemwide platform for asset management. The impressive results included $2 million in savings, increased productivity by 90% and increased equipment utilization by more than 20%.

Piedmont Healthcare is the largest provider in Georgia serving 3.4 million patients (80% of the state’s population) across 1,400 locations including 22 hospitals.
The new Marcus Tower in Atlanta is a $603 million, 16-story hospital with 408 beds. Vizzia was selected early in the project and collaborated with the hospital to have a modern RTLS network in place when the hospital opened during the COVID-19 pandemic, four months early.
Vizzia operates an IOT Lab onsite at the University of New Mexico. The Lab serves as an objective testing ground to evaluate emerging wireless sensor technologies (i.e., Bluetooth, Infrared, RFID, Ultrasound, Ul tra-Wideband, and Wi-Fi). As Vizzia is hardware agnostic, they can recom mend which solution will work best in a specific health care facility.
The University of New Mexico School of Engineering is the highest-ranked engineering program in the state. It was ranked as one of the Top 100 engineering programs in the country by U.S. News & World Report in 2021.
For more information, visit vizziatech.com.








Headquartered in Macon, Georgia, Atrium Health Navicent is a leading health care provider in central and south Georgia. The nonprofit health sys tem was incorporated in 1994.
The Atrium Health Clinical Engineering Department is made up of a cohesive 13-member team.
The department includes Bobby Benjamin, Mica Buice, David Couch, Jacob Cruz, Ca’Ron Gordon, Chrystal Hinton, Eric Kemp, Jeannine Kieweg, Angelia King, Virgle Stroud, Russell Miller, Herman Yang, Supervisor Brad Litke and Manager Skip Nieland.

“We have a really good group of techs. We get along really well and work well together. We have a vast variety of backgrounds, but they all blend together to make a great team,” Litke says.
He says that the clinical engineering (CE) team services more than 50 Atrium Health Navicent facilities, including Atrium Health Navicent The Medical Center, central and south Georgia’s only Level I Trauma Center,
multiple hospitals, diagnostic centers, urgent care practices, medical offices, skilled nursing facilities and a senior life-plan community.
“Each technician is assigned an area of the health system in which they specialize. That means, they’ve gone to school and been trained on specific equipment and have worked on it for several years. For example, Chrystal Hinton is a respiratory specialist and primarily works on ventilators. Ca’Ron Gordon works in the cardiac department and cath labs. Angelia King stays scrubbed-out and works on OR equip ment. Eric Kemp maintains dialysis equipment in-house, which is a rare thing, because most health systems have to contract that service,” Litke says.
Having a specialist on staff has helped with network integration, along with support from IT.
“We are heavily integrated, thanks in great part to our integration systems analyst Russell Miller and our IT counterparts. About 3,200 pieces are connected to our EMR or PACS imaging system, including all bedside monitors,
telemetry, anesthesia, perfusion, dialysis, ventilators, lab analyzers, imaging equipment and ECGs,” Litke says.
With several in-house specialists, most of the equipment is serviced by the team, but there are exceptions.
“Service contracts are managed through a collaboration amongst the clinical engineering department, finance department and the department owning the equipment. So, we have traditional manufacturer’s contracts on some of our equipment,” Litke says.
He says that since the companies that make the robots in the OR don’t provide training on maintenance, they make use of a service contract. They also use contracts for equipment for which no one has been trained.
“We also have a program called EMMP, Equipment Maintenance Management Program, where we self-insure the equipment. It’s a collabo ration between us and the department needing the equipment maintained. We talk with them regarding the best way to maintain it, either through the manufacturer’s contract, through third-party vendors or
through training one of our staff on maintenance of the equipment. We determine the best avenue for getting the work done and keeping the costs as minimal as possible,” Litke explains. One of the team’s primary goals is cross training so that if a specialist goes on vacation, that equipment can be main tained with proficiency.
The team has taken on projects in addition to its other daily duties. These have included updating the EHR system, converting a monitoring system and helping acquire additional medical equip ment to meet the increased needs caused by the COVID-19 pandemic.

“Recent projects include helping with clinical equipment selection, installation and integration for the Atrium Health Navicent Beverly Knight Olson Chil dren’s Hospital expansion. This also included adding neonatal ICU and observation beds and outfitting six acute and 10 non-acute emergency exam rooms, two trauma bays and a full pediatric imaging suite,” Litke says.
He says that the CE team also participated in the conversion from Philips classic to Philips PIIC iX, and replaced 107 central and overview monitoring stations, multiple servers and network hardware.
“Our department additionally was
integral in the conversion from Cerner to the Epic electronic record management system across four hospitals (Atrium Health Navicent The Medical Center, Atrium Health Navicent Baldwin, Atrium Health Navicent Peach and Monroe County Hospital, an Atrium Health Navicent partner). We developed, mapped and verified network connec tions between patient monitoring systems, capsule integration servers and EPIC Bridges interface engines,” Litke says.
He says that the department also converted from Fetalink to the Obix Obstetric monitoring system, reconfig ured and updated barcodes on over 700 Alaris infusion devices and pointed all point-of-care units to a new Carefusion server.

“We worked with multiple vendors at the outbreak of the COVID-19 pandemic to acquire medical equipment necessary to supply a Georgia Emergency Manage ment Authority 24-bed mobile facility. We were able to wirelessly connect bedside monitors to a central station with a remote viewing station for the welfare and safety of both teammates and patients,” Litke says.
The team remains involved with the biomed community beyond work hours as well.
“We participate in the Georgia Biomed Instrumentation Society as
members and hold a position on the board. We receive training and education through the association on an annual basis. Also, the association creates an opportunity to share information with other biomeds and find out how they deal with certain issues,” Litke says.
He says that they are also on the advisory board for the local technical college’s electronics and biomed training program.
“There’s not a lot of awareness about the biomed technology field. We work with them to help maintain that program, so that we have a feeder system to train and develop biomed technicians. In addition, we attend the college’s job fairs to give presentations about what we do and the opportunities that exist for graduates. In fact, most of the people we’ve hired here have come from the local technical college,” Litke adds.
According to the health system, Atrium Health Navicent has made a concerted effort to build partnerships with local educational institutions to create career pipelines, enabling the health system to fill current jobs and help build a job-ready workforce for the future.
Part of Atrium Health Navicent’s suc cess strategy is vested in its CE depart ment, which keeps up to date on its ability to proficiently maintain the medical equipment inventory.

Twenty-seven years ago, social media did not exist. Although the term “social media” had been used sparingly around the same time, it had not yet entered the popular lexicon. From the mid-to-late 1990s, to the present day, the growth and utiliza tion of social media has exploded.
Users of social media number in the billions. On its own, Facebook has nearly 3 billion monthly active users. Not far behind Facebook is YouTube, the video sharing and social media platform, with 2.2 billion monthly active users.
Content creators who use YouTube are always hoping to attract subscrib ers and “likes.” If a YouTuber meets certain criteria, the channel can be “monetized.” This may be the icing on the cake for a platform that allows content creators to reach hundreds or thousands, or even millions, of viewers and subscribers.
Alongside all of the entertainment content found on YouTube, one of the primary benefits of the platform is that it is a great vehicle for informing.
Teaching, training and informing make up a sizable portion of You Tube’s video library.
One member of the biomed community who recognized this fact and has utilized YouTube for teaching and training is Justin Barbour. Barbour is something of a YouTube veteran with 550 videos under his belt and counting.

“I started my YouTube channel four years ago when I decided to video a training about isolated power systems. I didn’t want to repeat the training to other people in the future, so I created a channel and let YouTube host the training video. I emailed the link to the video to the hospital facilities department and they could train at their leisure,” Barbour explains.
Barbour says that he never intended to continue making videos, but the initial experiment went so well, that he continued with a couple of other topics.
“I thought the biomed community would laugh me into being unemploy able, but as time went on, I received many positive emails and video comments encouraging more content.
I have had to learn about speaking, recording/cameras, video editing, sound editing and marketing on my own. It’s been a journey,” Barbour says.
He says that each video starts with either a request from a viewer, a “Wow, you didn’t know about that” moment or a “I wish I would have known that” moment.
“Each day, I see enough content to make half a dozen videos and time is the only detractor from me constantly posting content. Some videos take lots of time to develop. The video on ‘Cardiac Output’ took over 14 hours of research, scripting, recording, audio editing, video editing, upload ing and then marketing/social media posting,” Barbour says.
“Over 14 hours to make a seven-anda-half-minute video. It’s a labor of love, because in that eight-minutes, the viewer will have acquired enough knowledge, at an accelerated rate, to make up for hours of book research. That’s the power of video content. We need to do more with less and I believe that training on YouTube is one of the easiest ways to accomplish that goal,” Barbour adds.
Another powerful capability of YouTube is its reach. One person, producing video content anywhere in the world, can reach a global audience.
“Most people think that repairs and training are an issue that affect the U.S. [only], but I have received emails from biomeds in almost every country in the world. This is a worldwide conflict which we can all help solve. I have developed several unique methods for attacking the YouTube and Google algorithms, which help me reach an unintended audience,” Barbour says.
He says that the real magic has been boots on the ground and meeting people at events, using LinkedIn, answering questions online, writing articles, public speaking and all other forms of self-marketing.


“You can’t simply post a video and it magically goes viral. Biomeds are a community who didn’t have much or any social media representation when I started this project. I had to carve out the process from scratch. This is why I’ve been a huge advocate for biomeds to start using social media. The more people who post their knowledge; the more people who will use tools like YouTube to be better at their craft,” Barbour says.
The channel and its content have led to more professional opportunities for Barbour.
“Since the start of this channel, I have been flown across the country several times to meet biomeds, attend company events, tour facilities, see new products before they hit the market and I have some sort of credence as a serious biomed. I have met hundreds of amazing people, and it all culminated to this moment, where I became the vice president of business development at FOBI Medical; a position that I surely would not have been considered for if I stopped making videos years ago,” Barbour says.
The channel spawns 10-20 daily emails or messages online regarding medical technology or asking Barbour for his thoughts on something. He splits up his day to balance out his online obligations with his work and family obligations.
“In the morning, I try to answer shorter reply emails; during lunch I try to respond to LinkedIn messages; and in the evenings I try to answer longer messages, because then I have more time to think about or research the answers. The key is balance, and that balance is getting harder to achieve as the channel gets larger,”
Barbour says.
Asked about what advice he has for others considering a biomed or technology YouTube or other social media channel, Barbour ticks off some important observations: You are not going to be famous. You are not going to get rich. It’s going to take years before you ever see a gain from your efforts. You need to watch what you say; it could affect your employ ability. Most medical facilities have policies against recording; be careful. Biomeds/clinical engineers are a very small group – maybe ~10,000 in the U.S. – your efforts are helping people around the whole world.
The work on this growing social media channel has been rewarding and Barbour is grateful for the channel and his career choice.
“I absolutely love this career, but I have a deeper admiration for the people who have supported me over these 19 years, to get me to this point,” he says.
Learn for yourself what has made the Better Biomed channel such a success: youtube.com/c/BetterBiomed




Probo Medical has acquired Mi Healthcare. Terms of the transaction were not disclosed.
Established in 1995, Mi Healthcare is a Liverpool, United Kingdom-based provider of medical imaging equipment and services to public and private health care facilities across the UK. Mi Healthcare’s team provides ultrasound and X-ray sales, rental and service solutions across the UK with offices in England and Scotland. Mi Healthcare is led by founder Tim Dickinson and CEO Mark Edwards.
With the acquisition of Mi Healthcare, Probo will extend the reach of its diagnostic imaging equipment sales, rentals and service capabilities throughout the UK. Mi Healthcare’s 25-year track record of quality in the diagnostic imaging sector have positioned it as a leading partner for Probo’s continued Europe an expansion, according to a press release.

“Our partnership with Probo will provide a deeper and more comprehensive solution set for our customers, as well as oppor tunities to best support our growing team,” said Dickinson.
Edwards said, “We have long known the Probo team, and we are excited for the future of bringing Mi Healthcare into the Probo family. The combination with Probo connects us to a significant platform that allows both organizations to grow faster together and brings a set of resources to our customers and employees that is unmatched in our sector.”
“Mi Healthcare is well-known in the UK market as a high-quality service provider for their customers with longstand ing relationships that evidence that commitment to quality,” said Michael Asmer, CEO of Probo. “As we look to harness the shared expertise and collaboration between our teams, we are excited at what this combination will bring to both Probo and Mi Healthcare’s customers.”
Probo Medical is backed by Avista Capital Partners, a leading New York-based private equity firm with more than 40 growth-oriented health care businesses globally.
maintain a device.
management and
community. A new
incidents
an original
manufac turer (OEM)

or other support
to
or
goal is to provide biomeds a place to share their experiences to help others as well as collect data regarding right to repair issues that can be shared within the industry and with regulatory organizations, including the FDA.






Share a right to repair issue today at 1technation.com/ right-to-repair-incident.


EQ2 LLC has released an additional Single Sign-On (SSO) service for the company’s “HEMS” CMMS software. Since its hospital clients have numerous applications their users frequently access, those clients want to limit the number of logons required to use these applications. SAML 2.0 (Cyber Ark, Shibboleth) is used by many hospitals and is now supported in HEMS. Other SSO services EQ2 HEMS
supports include: OpenID Connect (OIDC) (including Azure AD, CyberArk), ADFS with WS-Fed (including SecureAuth, and Windows ADFS).
Since HEMS is built on its own platform, EQ2 can support many different types of single sign-on services and will continue to add new ones as requested by new and existing clients.
The Joint Commission President and Chief Executive Officer Jonathan B. Perlin, MD, Ph.D., MSHA, MACP, FACMI, shared the following information on September 13, 2022.
“Today we announced the beginning of a review of all Joint Commission ‘above-and-beyond’ requirements, those that go beyond the Centers for Medicare & Medicaid Services (CMS) Conditions of Participation (CoPs) and are not on crosswalks to the CoPs.
During the COVID-19 public health emergency (PHE), CMS put many requirements on hold. As the PHE nears its end, CMS has been reviewing the waived requirements to determine whether some should be permanently retired. The Joint Commission will similarly address the necessity of our own unique requirements.
Specifically, we will review each requirement to answer:
• Does the requirement still address an important quality and safety issue?
• Is the requirement redundant?
• Are the time and resources needed to comply with the requirement commensurate with the estimated benefit to patient care and health outcomes?
In addition to a direct review of each requirement, we will conduct quantitative analyses of scoring patterns and tests for redundancy. Where necessary, we also will conduct literature and field reviews and engage experts within the field.
American health care still has a long way to go to fully recover from COVID-19 and to reach a new equilibrium – es pecially as we are now witnessing secondary effects from the pandemic. At The Joint Commission, we are committed to working with health care organizations and other stakehold ers to help address the many challenges health care is facing, as well as to making our own requirements as efficient and impactful on patient safety and quality as possible.”
For more information, visit jointcommission.org.
SOLUTIONS
Tri-Imaging Solutions recently appointed Rich Springer as senior vice president of operational excellence.
Springer has more than 30 years of executive experience as a strategic operating executive with extensive global experience working for medical diagnostic imaging, biotech and technology companies. His addition to the leadership team will enhance Tri-Imaging’s ability to empower its partners with dynamic solutions, according to a press release.
Prior to joining Tri-Imaging, Springer served as the president, enterprise solutions group for the Alpha Source Group, a healthcare technology services company. In that role, he worked with health care providers, ISO/asset management companies and medical device manufacturers to improve their performance and profitability. Preceding his time with Alpha Source Group, Springer built a successful 30-year career with leading health care organizations including GE Healthcare and Crothall Healthcare in a variety of executive operating and commercial roles.
“I’m honored to join the Tri-Imaging Solutions team.
There’s no question that Tri-Imaging Solutions’ innovative offerings have empowered our partners.” Springer said. “I am excited by this opportunity to help improve the compa ny’s operational performance and support the strategic vision to deliver a competitive advantage.”
“We couldn’t be more thrilled to have Rich step into this new role” said Eric Wright, president of Tri-Imaging Solutions. “His appointment comes at a crucial moment for our organization as we build upon our growth and drive innovation in the industry. We look forward to having him on our leadership team as we develop and drive overall strat egy for Tri-Imaging Solutions.”
Springer joins a seasoned team of executives at Tri-Imag ing Solutions, including Wright, Senior Vice President of Business Development Wanda Legate, Chief Financial Officer Bruce Maurer, Vice President of Operations John Drew and Vice President of Technical Services Josh Raines.
For more information, visit www.triimaging.com.






Maple Tree Biomedical LLC provides medical device inspection, maintenance and repair services. MTB services everything from physical therapy, anesthesia, audiometry, sterilization, laser, patient monitoring, laboratory and more.I work with independent clinics, surgery centers, labs and the odd veterinary center. MTB also assists hospitals when they are short staffed to help catch up on testing. Maple Tree Biomedical LLC Owner Andrew Whyte, BMET, recently shared more information about his company.”
A: Maple Tree Biomedical is a one-tech show. I handle every repair personally and I have a vested interest in the outcome. When my customers call or email, it doesn’t go to some answering service or a black hole email account. I will personally answer the phone or respond to the email and we will start working on a solution immediately. Repairs should be measured in hours, not weeks.
A: Maple Tree Biomedical has been cementing its place in this region and I hear from new customers weekly. I look forward to growing both territory and adding new employees in the near future.
A: I feel honored to have been featured in the TechNation’s July article 40 under 40. There are a handful of BMETs in the article and I was glad to be included. For more information, visit mapletreebiomed.com.



sponsored by

NOVEMBER 2 | PartsSource
Save the date for this live webinar. Participation is eligible for 1 CE credit from the ACI.



Save the date for this live webinar.
Participation is eligible for 1 CE credit from the ACI.
NOVEMBER

webinar. Participation
Save the date for this
from the
NOVEMBER
for 1
Save the date for this live webinar. Participation is
credit from the ACI.
1

The Association for the Advance ment of Medical Instrumentation (AAMI) has announced a strategic partnership with AmbiFi, an advanced software as a service (SaaS) perfor mance support company. Ambifi pro vides mobile-first, real-time, hands-free support for complex procedures while ensuring real-time process documenta tion and benchmarking.
on secure mobile devices, including smartphones, tablets, and smart glasses, these copilots provide guid ance and support during the execution of high-stakes processes.
AmbiFi platform.
“We continue to leverage proven technologies to better serve our members and stakeholders,” noted AAMI President and CEO Pamela Arora. “The cognitive load on all health care professionals continues to challenge the safe and effective use of health technology. AAMI is expanding its offerings to include AmbiFi’s revolutionary moment-of-need performance support. Ambifi has the potential to transform the execution of complex medical device processes, enabling greater consistency, quality and transparency.”
Headquartered in Pittsburgh, Pennsylvania, AmbiFi leverages ambient computing and performance science to empower experts to easily transform industry standards, guide lines, procedural documentation, and expertise into ambient intelligent copilots, called “ambiis.” Deployable
“AmbiFi is a proven platform that launched in the aviation industry and is now used by thousands of pilots globally. After pivoting to health care, they have proven their platform across a wide range of clinical use cases.” said Robert Burroughs, senior vice president of education at AMMI. “Our goal is to bring this powerful capability to our medical device stakeholders. Given the incredible breadth and complexi ty of process that must be executed throughout a medical device’s life cycle, this tool has the potential to be transformative.”
As a part of the strategic partner ship between AAMI and AmbiFi, AAMI has adopted the AmbiFi platform and will leverage AAMI content and subject matter expertise to develop medical device, sterile processing, and healthcare technology ambiis for use by AAMI members and stakeholders. In addition, AAMI will work directly with medical device manufacturers, healthcare delivery organizations, independent service organizations and educators to develop custom solutions utilizing the
“AAMI is the de facto world leader driving the safe and effective use of healthcare technology via their standards and education. We can’t wait to see what they can do with the AmbiFi platform at their disposal, and we look forward to working together closely to support AAMI members and stakeholders,” said James Sharpe, cofounder of AmbiFi.
When you think of the materials used to develop space stations, you may not predict a correlation to the health care industry. However, the 2022 Kilmer Fund’s $11,600 research grant recipients, Paulo Laranjeira, sterility assurance QA manager at Cordis US, and William Leiva, global scientific affairs manager at 3M Health Care, chose to explore an innovative new connection. In pursuit of reducing the carbon footprint of materials used in medical devices and increasing the antimicrobial properties of endoscopic tools, the researchers developed a polymer with copper particles, a common material utilized in space that also possesses inherent antimicro bial effects.
This was of particular importance,
as up to 1.6 infections can emerge per 100 endoscopic procedures, which is due in part to the difficulty in main taining the sterility of the lumen and tiny channels present in endo scopes. Although endoscopy remains an advantageous procedure in the medical community, with this high of an infection rate, reducing the microbial load is paramount.
“We are trying to bridge those efforts with these new technologies that I think are going to be in many ways revolutionary for the health care industry, the medical device industry and perhaps for others too,” Leiva said. “You’re not necessarily thinking about how to use this in the medical device industry … the industry in general lacks awareness that this technology is there. I think now the challenge is to demonstrate that it can be applicable to the biggest concerns that we have, at least in the endoscopy area.”
Laranjeira and Levia are the second recipients of the AAMI Foundation’s Kilmer Fund grant, which provides funding to individu als and groups seeking to advance the science of microbiological quality or sterility assurance through
collaborative research.
“The Kilmer Fund is a central part of the AAMI Foundation’s mission to support deserving healthcare technol ogy professionals through scholar ships, grants, and professional development recognition programs,” said Steve Campbell, executive director of the AAMI Foundation and chief operations officer of AAMI. “With patient safety as AAMI and the AAMI Foundation’s north star, we could not be happier to support this research.”
develop their own policies so they can reuse and recycle some of the devices.”
To balance these two consider ations, Laranjeira, Levia and their research team developed a Polylactic acid (PLA) polymer infused with copper particles via additive manufac turing efforts or 3D printing. By distributing a large number of these small copper particles evenly through out the polymer, they were able to increase the surface area in which the natural antimicrobial properties of copper are engaged, thus saving on costs and increasing effectiveness.

SETTING A SUSTAINABLE PRECEDENT Copper has long been utilized in space machinery for its inherent resistance to heat, among other benefits. Howev er, the metal has been far less explored by medical device manufacturers. With so many stakeholders in the health care industry, there are various factors to consider, such as sustain ability and cost.
“From the industry side, you cannot bring products that are going to be biodegradable if they are going to be 10 times more expensive,” Levia added. “From the hospital side or health care facilities, they have to
With the increase in waste pro duced during the pandemic, the need for sustainable materials such as the one being developed in the study, is of particular importance.
“The amount of waste is just insane – especially after the pandemic, so many disposable devices go to different waste streams, and most of them are not recyclable. Even though they can be, they are not currently,” Levia added.
Fortunately, with the recognition of the Kilmer Fund, the research has high potential to be recognized and imple mented in the medical device space.

When a caregiver or responder reaches for an automated external defibrillator (AED), they need the device to be functioning correctly. Someone’s life literally de pends on it. Routine visual and opera tional checks can go a long way toward ensuring the safety and effectiveness of AEDs; and some newer models include features that facilitate this process. ECRI’s testing of AEDs reveals which device features and deployment practices can be most effective.
Stand-alone automated and semiauto mated external defibrillators, often collectively referred to as AEDs, are used in emergency situations when a person suffers a cardiac arrest. AEDs analyze the person’s ECG and either deliver a shock automatically or prompt the user to do so if one is warranted. If a defibrillation shock is not appropriate, the AED will advise against a shock, and will guide the user to perform cardiopulmonary resuscitation (CPR) until medical assistance arrives.
The speed with which a defibrilla tor is deployed can be critical to a successful resuscitation attempt. Every minute that a patient goes without defibrillation decreases the likelihood of resuscitation. Every minute that a
patient goes without adequate circula tion increases the likelihood of tissue death, which can lead to poor neuro logical outcomes or damage to heart tissue. High-quality CPR can help provide some circulation and delay the onset of negative health effects, but it is insufficient on its own.
Reducing the time to the delivery of a defibrillation shock can greatly improve a patient’s chances of survival with a good outcome. For that reason, ECRI recommends paying careful attention to factors that can impact the time-to-shock when making AED purchasing and deployment decisions.
AEDs are intended for use by individ uals who have CPR training or basic life support (BLS) training, but who are not qualified to analyze a cardiac rhythm and recommend a shock. Typical users include medical profes sionals, targeted responders (like security guards, police officers, firefighters and designated volunteers) and bystanders who witness a cardiac arrest or other medical emergency and are able to locate an AED and respond. The core purpose of an AED is to speed the delivery of potentially life-saving therapy by making defibril lation easier for users who have not received advanced cardiac life support (ACLS) training.
AEDs are often used for public access defibrillation, and thus may be found in public spaces like schools, athletic facilities, shopping centers and conference centers. In hospitals and other health care settings, AEDs may be located in lobbies, parking areas, stand-alone sub-acute care facilities or other areas that may not be supported by a code team or that may be subject to long response times.
KEY PERFORMANCE CHARACTERISTICS Performance characteristics that affect the time-to-shock include the follow ing:
• Accuracy of ECG analysis. AEDs should have a high sensitivity and specificity for determining when a patient requires a defibrillation shock. Delivering a shock inappropri ately may cause pain to the patient and could trigger a lethal arrhythmia. Conversely, failure to deliver a shock when one is appropriate will increase the time to shock delivery and decrease the likelihood of resuscitation with a good outcome.
• Analysis time and charge time. Both the time required for the AED to analyze the patient’s ECG and the time required for the AED to charge to the
desired energy level factor into the time-to-shock. Minimizing the total hands-off time between the pause of CPR (to allow the device to analyze the rhythm) and the delivery of the shock (when warranted) can improve the chances of a successful resuscitation. Some AEDs allow the charging process to be initiated while CPR or rhythm analysis is ongoing; this feature can help reduce the hands-off time.
• Ease of use. The AED must be easy for the intended user population to operate, with clear instructions and con trols. The device should not contribute to delay of therapy due to user uncertainty. Many newer models even provide real-time CPR feedback and a metronome to improve adherence to CPR guidelines during the periods before and between shock delivery.
For best results, AEDs must be rapidly accessible and operational at all times. “The best defibrillator in the world is useless if it can’t be located or isn’t ready for use when it’s needed,” explains Mairead Smith, a principal project engineer in ECRI’s Device Evaluation group. Issues related to how a device is deployed and main
tained can have just as big an impact on the success of a resuscitation attempt.
AED placement. Ideally, an AED would be located so that most of the covered area will be within a 60- to 90-second walk for likely responders, including bystanders. Further, units should be placed in a central location where rescuers are likely to look, such as a lobby, a security desk, an elevator bank or near emergency phones. Additionally, a unit may be needed on each floor of the building: Rescuers are likely to search for an AED on their floor, without going up or down stairs or an elevator. Also, be sure to consider restrictions that could delay access to a patient or AED, such as locked doors that a rescuer may not be able to open.
Within a health care facility, AEDs should be considered for spaces that may not be easily covered by the code team. This might include outlying buildings and parking areas, for example.
AED maintenance. AEDs in the United States are equipped with automated self-tests, in which the AED assesses key functions like battery operation, electrical circuit status, ability to charge and, some times, the status of preconnected defibrillation electrodes. Notably, two of the three models included in ECRI’s August 2022 evaluation of AEDs can
transmit readiness statuses from these checks via Wi-Fi. This capability allows program managers to monitor readiness remotely.
“Remote monitoring reduces the need for in-person device checks, which can be very convenient when a device manager is responsible for multiple AEDs, especially if they’re located in separate buildings” ex plains ECRI’s Smith. “But you should still go around once in a while to make sure everything looks good in person.” ECRI recommends that health care facilities inspect each AED on at least a monthly basis to confirm that the device has passed its self-tests and is otherwise in good condition.
Downsides to keep in mind with Wi-Fi capabilities are that they can add to the cost of the unit and can shorten the battery life.
TO LEARN MORE . . .
Members of ECRI’s Capital Guide, Device Evaluation, and associated programs can access the following resources for making effective AED purchasing and deployment decisions: “Evaluation Background: Automated External Defibrillators (AEDs)“ (2022 Aug 11); “Placement of AEDs for Quick Access in Healthcare Environments” (2022 May 18); and “Sure to Shock: ECRI’s Defibrillator Checklists“ (2022 Feb 22). To learn more about membership, visit https:// www.ecri.org/solutions/device-evaluations, or contact ECRI by telephone at (610) 825-6000, ext. 5891, or by e-mail at clientservices@ecri.org.
To facilitate effective CPR, the Zoll AED 3 includes a sensor that assesses chest compressions, and the unit provides helpful on-screen diagrams and voice prompts.

The defibrillation pads for the Philips HeartStart FRx are applied to ECRI’s defibrillation analyzer, which is used to input various ECG rhythms and to measure the energy delivered by the AED.

Diagrams on the Stryker Lifepak CR2, along with detailed voice prompts, guide the user through the process. In step 2, the user pulls the ring to access the defibrillation pads.





Endo Technologies is a veteran-owned endoscopic repair company that specializes in Olympus large diam eter flexible scopes. Founded in 2001, our goal is to offer high-quality repairs at a lower cost to facilities than the OEM. With over 65+ combined years of experience, our simple no-cap service contracts, and staff training through pattern recognition, we are confident that we can provide superior service to our facilities. With our 30-day no cause out, you can cancel at any time, making us a risk free opportunity to cut unneces sary costs. In addition to our service, we also sell Certified Pre-Owned Olympus endoscopy equipment at a highly competitive price.

Endo Technologies strives to create a partnership with our customers and give feedback on the repairs that we see coming in. With open communication, we can isolate patterns and eliminate unnecessary repairs through training on proper procedures. We provide high-definition loaners, 180s and 190s, quick turnaround times and paid two-day shipping to take the stress out of endoscopic repairs so that you can focus on the procedures on hand.
For more information, visit endoti.com.

One thing that has fascinated me since entering the professional world is how the people at the top got to where they are. Most often, you don’t get the chance to interview a hospital president and ask them about their career path so you may see if that is shared on their LinkedIn profile. In my experience, executives don’t post the full breadth of their working life online, instead focusing on the past 5-10 years. It makes you wonder how they made that leap from graduate to executive.
While I am not an executive, I do aspire to be one someday (some may call me crazy for having such a dream) and thought to share my opinions and experiences that have paved the way for me to get there.
I worked as a frontline BMET for 10 years before changing my career trajectory towards leadership. I recognize that there are numerous paths to follow and there is not a “one size fits all” answer, but I stand by the decisions I made and am grateful for the opportunities I had. Those 10 years allowed me to develop the technical skills and begin my growth in professional communication – verbal, body language and articulate e-mails.
If you ever sit in a meeting with managers, directors or higher-level individuals, take note on how they present themselves; how they sit in their chairs and address the room
when speaking. More often than not, they are calm, confident and profes sional. While they may be shaking on the inside, they’ve learned to control their voice and body through repetition. Public speaking, whether in front of a room of 5 people or a crowd of 700 usually gets easier over time with practice. At least it has for me.
About 5 years into my BMET career, I pursued an MBA deciding that it would help me move into leadership sometime down the line. I believe it helped when I decided to transition into a clinical engineer role. I made this career move on the basis that knowing the other side of the HTM business (regulatory, contracts, project work, database administration) would prepare me to lead a team. Around the same time, I got involved with my regional HTM association in which I currently sit on the leadership board.
It was during this time that I felt
I had matured the most and stopped thinking like a tech and more like a leader. I began looking at problems as opportunities to be fixed instead of ignored. I began corresponding with directors and an occasional vice president with regularity which further honed my communication skills. I took note of how these leaders crafted their emails – specifi cally not making them lengthy, breaking up thoughts into para graphs, and using accurate spelling, grammar and punctuation.
One life lesson – long emails get skimmed at best. Keep them short and sweet if you want to get your message across.
Fast forward 16 months and I’ve solidified my position as an HTM supervisor – my first true leadership role. I went into the position trying to keep myself grounded – looking at all the decisions through the lens of a technician. Having been one so long (and relatively recently at the time), I knew where the pain points were and what was realistic to ask of my team. Retention, I found, is a daily challenge of any leader. If you let off the gas, it’s easy to slip and lose the trust, respect and coopera tion of your team leading to them seeking opportunities elsewhere.
I began to involve myself in everything I could – learning the ways of hospital operations outside the lens of HTM. I made friends with other site leaders and went out of my way to ask questions about

their work – how it’s done and why they do what they do. I wanted to expand my knowledge to everything because that’s what executives are expected to know. It helped that I had a “glass half full” and “can-do” attitude towards pretty much everything asked of me. Leaders are expected to get it done, not complain about the ask. Don’t get me wrong, I challenged decisions I didn’t agree with, but at the end of the day if it needed to get done, I got it done.
Fast forward another 16 months and I was promoted to a site manag er at one of the largest sites in my system. I continued my trend of remembering my biomed roots while learning more and more about the rest of the site and meeting other leaders. I prided myself on being a go-to resource for many things and keeping organized. It was around

this time I was introduced to Micro soft OneNote which replaced Excel as my note keeping tool of choice. Highly recommended if you can get past the short learning curve. If you plan to move into leadership, being adaptable and learning new things despite “this is how it’s always been done” is a must-have mentality! Those who cannot accept change are doomed to fail.
An opportunity to volunteer on a major conference planning commit tee presented itself to which I was thrilled to participate. This, again, introduced me to leaders throughout my organization and gave me the opportunity to participate and show what I bring to the table. Through this committee, I was introduced to a leader in a department outside of HTM that I found interesting. When a position opened up in that depart
ment, I applied and that brought me to where I am today.
If you’ve made it this far, my point is that networking and attitude play a role in moving up the corpo rate ladder. You need to be good at what you do and deliver on promises as well or people will see through you eventually. Don’t be afraid to branch out of your comfort zone, ask questions and take on new challenges.
Feel free to connect with me on LinkedIn or ask me questions directly: https://www.linkedin.com/ in/greg-czajka-chtm-6375301a/
– Greg Czajka is a support services opera tions director, operations and strategy for Advocate Aurora Health.
Note: The ideas in this column are those of the author and do not reflect my current or previous employer nor that of TechNation.






Interstate Batteries offers Pure Gel Sealed Lead-Acid (SLA) Batteries, providing a reliable and trusted power source to the medical mobility industry. Delivering quality performance, Interstate’s Pure Gel Mobility Batteries will power scooters and wheelchairs with reliable deep cycle batteries and can manage harsh conditions with twice the cycle life of a standard battery. With Interstate’s Gel Batteries, consumers can count on superior performance for their power wheelchairs, scooters or mobility aids with the convenience of longer battery life. In addition to offering quality Gel Batteries, Interstate offers the Interstate Advantage, which provides the mobil ity industry with an end-to-end battery program that includes local delivery, recycling services and expedited shipping.
Whether you are located in a remote location or have high cycle demands, customers can rely on Interstate’s Pure Gel Mobility batteries to provide the following benefits:
• Twice the cycle life of standard battery
• High current on demand for long service life
• Ideal for deep cyclic discharge use
• Superior performance at higher temperatures For more information, visit interstatebatteries.com/mobility.
The Webinar Wednesday series continues to deliver free continuing education credits to healthcare technology management (HTM) profes sionals around the world! One recent webinar explored medical device secu rity. Another presentation featured two experts on workflows and compliance.
The Webinar Wednesday presentation “Finding Your Phase of Medical Device Security with Nuvolo and Cynerio” was sponsored by Cynerio and eligible for 1 credit from the ACI.
Most health care environments contain thousands of OT, IoT and IoMT devices that vastly improve patient care. The devices also introduce significant new cybersecurity risks. Unfortunately, securing these devices with traditional IT approaches has become an unachievable challenge. In order to protect patients and the facilities providing care, new approach es and technologies must be adopted and integrated with in-place systems.
In the webinar, Chad Holmes, security evangelist at Cynerio, and Dustin Smith, executive solution consultant at Nuvolo, discussed common phases of securing connected devices in health care environ
ments, key activities in each phase and steps that can be taken to start improving cybersecurity practices immediately. From assessing risk to automating inventory, and finally improving monitoring and response activities, the session provided a clear roadmap for attendees.
The webinar also included a ques tion-and-answer segment where attendees could obtain additional expert insights. One question was about using a CMMS to improve security practices. The presenters said it is usually a rather quick process.
Another question asked about what steps can be taken when funding is not available.
The presenters suggested speaking with vendors because they can sometimes share solutions that other customers have used and are often willing to work with you to find a solution.
The complete question-and-answer session is available in the on-demand recording of the webinar at WebinarWednesday.live.
Attendees provided feedback about the webinar in a survey that included the question, “What does Webinar Wednesday provide the industry?”
“Great value and information on hot topics that apply to our HTM industry,” Manager Shannon Dingus said.
“The technologies at HTM evolve
rapidly and all HTMs learn these trends in a timely manner. The TechNation webinar series fills these gaps for HTMs,” said Tedd Koh, MET, Olive View UCLA Medical Center.
“Good general knowledge, lots of topics that explain what is happening in the field of health care,” said Glenn Fraser, CBET, Stanford Children’s Healthcare.
“These webinars give a lot of insight to facets of biomed support that are frequent ly overlooked by the engineering manage ment that is more interested in plumbing solutions than software security,” said David Green, system designer with Square One Industries.
The Webinar Wednesday session “Using Existing Tools to Strengthen Your Workflows and Compliance” was sponsored by Phoenix Data Systems. It was a popular session with 87 attendees for the live presenta tion. It was eligible for 1 credit from the ACI. An on-demand recording of the webinar is available at WebinarWednesday.live.
In the session, Mike Roggmann, CBET-R, LSSBB, project manager/ implementation lead at Phoenix Data Systems, discussed using existing tools to strengthen workflows and compliance.
Roggmann answered the following
questions during his presentation:
• What is a workflow?
• Why is this important?
• Where to start?
• What do workflow reviews mean for CMMS?
He also discussed the easiest ways to review if workflows are being followed and how to simplify continued monitoring to make it easy.
During a question-and-answer session, one attendee asked if there is a method for helping techs know about contracts and other work related to a device?
Roggmann said there are a couple of different ways a technician can achieve that with AIMS. He went on to discuss the different approaches to obtain that information.
He also discussed how to view PM completion and project productivity using AIMS.
An on-demand recording of the webinar, including the Q&A session, is available at WebinarWednesday.live.

Attendees provided feedback via a survey that included the question, “Why did you attend today’s webinar?”
“I will be able to use the information of the system to share with my biomed students at the college. They do need to know how the new CMMS system works,” said George Panyarachun, professor, Los Angeles Valley College.


“The webinar was recommended to attend for continuing education on our workflow and policies,” said Michelle Campuzano, office manager, Comprehensive Equipment Management Corporation in New York.



“Wanted to learn more about strong workflows, how to build, maintain and assess efficiency. To see how AIMS CMMS can help with workflows in a database,” shared Keith Waters, manager, clinical technology services in Oregon. For more information, visit WebinarWednesday.live.










Manage your medical devices, technicians, vendors, costs, and compliance in Nuvolo Connected Workplace for Healthcare. With powerful HTM Asset Management capabilities, our leading software solution includes:


→ Built-in automated workflows that empower your teams to work smarter, not harder.















→ Planned maintenance capabilities that let you easily schedule PMs and monitor completion and compliance in real time.







→ Contract management capabilities to connect your contracts with each covered device.


→ Ability to integrate with other applications and services—such as RTLS, cyber monitoring, recall & alert services, and so much more.

Interested in learning more? Check out the Nuvolo Connected Workplace for Healthcare solution today: nuvolo.com/industry/healthcare




Th e TechNation roundtable series continues this month with a look at asset tracking and real-time location systems (RTLS). Partici pants sharing their RTLS insights are ZulaFly Managing Partner Stephanie Andersen, Cox Prosight Product Director Jaiganesh Balasubramani an, Sonitor Technologies Inc. Chief Commercial Officer Matt Crane, Cognosos Director of Product Man agement Paula Dycaico, Medigate by Claroty Industry Principal-Healthcare Ty Greenhalgh, Capital i LLC Chief Operating Officer Shon McManus and Vizzia Technologies Chief Commercial Officer Dave Wiedman.
Stephanie Anderson Zulafly
ANDERSEN : There are a number of new RTLS technologies in the market today that are providing customers with cost-effective, easy-to-deploy systems along with very good location accuracy that they may not have seen in the past. Since integra tions with external solutions (EMR, CMMS, Nurse Call) is a niche for ZulaFly, the value add we bring is that not only are we hardware
agnostic, but we have integrated our solution with a number of RTLS technology vendors in the market today. ZulaFly also has the ability to consume data from multiple hard ware technologies deployed in a facility, to a single user interface; thus eliminating the need for “rip and replace.”

BALASUBRAMANIAN : RTLS technology is a vital part of any hospital’s infrastructure. Effective RTLS will help your hospital in its journey to become a leader in the health care industry. As such, it is important for
providers to consider which RTLS option is correct for their needs. WiFi-based RTLS technology utilizes pre-existing wireless access points to track assets. The primary benefit of a Wi-Fi-based system is that it uses a hospital’s pre-established infrastruc ture, eliminating the need for additional infrastructure costs. Infrared, or IR, RTLS technology is powered by technology that is like a television remote. A major benefit of IR is that it can be significantly more accurate than other RTLS technolo gies. Ultra-wideband is a radio-based form of RTLS technology that aims to provide short and stable tracking technology. The leading benefit of UWB RTLS technology, by far, is location precision. Ultrasound identi fication is a RTLS technology that utilizes simple, inexpensive badges and tags to transmit and communi cate locations using microphones. On average, ultrasound can track assets within 3-5 meters. Bluetooth tech nology is common across all sorts of devices. On top of ease of use, it’s far and away the most diverse form of RTLS technology. BLE provides asset tracking advantages like geofencing, zonal coverage, choke point cover age, and maintenance management — among a variety of others.
CRANE : Health care facilities can be some of the most complex environ ments. Choosing the right RTLS that future proofs a health care facility’s investment by allowing them to seamlessly expand from the simplest of use cases, such as asset tracking that may only require zone level accuracy, to the most demanding use cases, such as staff safety and workflow that require bed and or bay level accuracy, is an important and critical decision. RTLS solutions based on Wi-Fi and BLE are primar ily communication tools, not positioning tools. Signals from these technologies are inherently designed to efficiently travel through walls, glass and floors, and as a result can deliver predominantly zone level accuracy. This might be sufficient if a facility is solely interested in tracking or locating assets and not doing more advanced RTLS use cases such as asset utilization, inventory management, PAR level management, staff safety, rounding, nurse call automation, etc. But as we all know, health care facilities are looking to get the highest return on investment (ROI) from their RTLS. The best way to do this is by choos ing the right initial infrastructure from the beginning so that they can layer on additional use cases that
can deliver incremental value. Most, if not all of these use cases require a higher level of accuracy (room, bay, bed, etc). For these more advanced use cases, true positioning technolo gies are required. Ultrasound-based technology has proven, in side-byside comparisons, to deliver the most accurate and reliable positioning data down to room, bay and bed level, while also requiring the fewest number of devices. Ultrasound signals are reliably and consistently contained within walls, glass and floors and will not “hop” or “bounce” out of its location, unlike infrared (IR) and ultrawide band (UWB). These other technologies require significantly more devices to block and contain signals to try to mimic the accuracy ultrasound can deliver with a single device.
DYCAICO : In its simplest form, the differences in RTLS technology are as follows: there are highly accurate and expensive solutions, and ones that are more affordable but not accurate enough to measure any real efficiency improvements. The most significant similarity (and possibly only) between these two types of RTLS technology is that they both make it very difficult to produce a hard-dollar ROI. Luckily, advance ments in cloud, AI and machine learning have drastically helped reduce the accuracy versus afford ability tradeoff, enabling the next generation of RTLS technology to provide a highly accurate and ultra-lightweight solution, including a measurable, hard-dollar ROI.
GREENHALGH : Health care leaders invest in RTLS to gather data to forecast equipment requirements, identify trends in utilization, and op timize staff efficiency and patient safety. The Bluetooth Low Energy (BLE) and Wi-Fi technologies, which use Radio Frequency Identification (RFID) are not “Star Trek” level accuracy sometimes leaving “circles


of uncertainty.” However, RTLS can integrate with a medical device security platform (MDSP), like Medigate, to correlate network device location details with the RTLS data increasing the location accuracy within HDOs.
MCMANUS : RTLS technology has witnessed significant growth the past 10 years as it penetrates the manufacturing, health care, trans portation and government markets just to name a few. With growth comes opportunities for innovation, which drives competition; as such, consumers now have a variety of RTLS technologies to choose. Most people are familiar with the Active and Passive Radio Frequency Identi fication (RFID) typically used in supply chain logistics and container tracking. RFID is a proven technolo gy with global standards and a relatively strong signal with long read range capability. Some of the drawbacks are the size of the tags, especially with Active RFID due to the energy supply, and the physics behind RF – this can create interfer ence when not considered. Ul tra-Wideband (UWB) is becoming more popular due to the exceptional ly low power level coupled with the high transmission frequency. This
Jaiganesh Balasubramanian Cox Prosighttechnology is minimally impacted by metallic surfaces and can precisely track thousands of tags within a facility.
WIEDMAN : Manufacturers are contin uously developing new wireless technologies for multiple industries. Health care facilities represent a unique challenge, given the different infrastructure materials and clinical uses cases that are specific to each hospital. Vizzia operates an IOT Lab at the University of New Mexico. The lab serves as an objective testing ground to evaluate emerging sensor technologies (i.e., Bluetooth, Infra red, RFID, Ultrasound, Ultra-Wide band and Wi-Fi). As Vizzia is hardware agnostic, we can recom mend which solution will work best in a specific health care facility.
ANDERSEN : It’s important to find a system that allows the customer to create the fields with information they would like to see and gather data for. The ability for each facility to customize the information displayed within the dashboards not only creates shorter ramp-up time for staff, but also allows for a


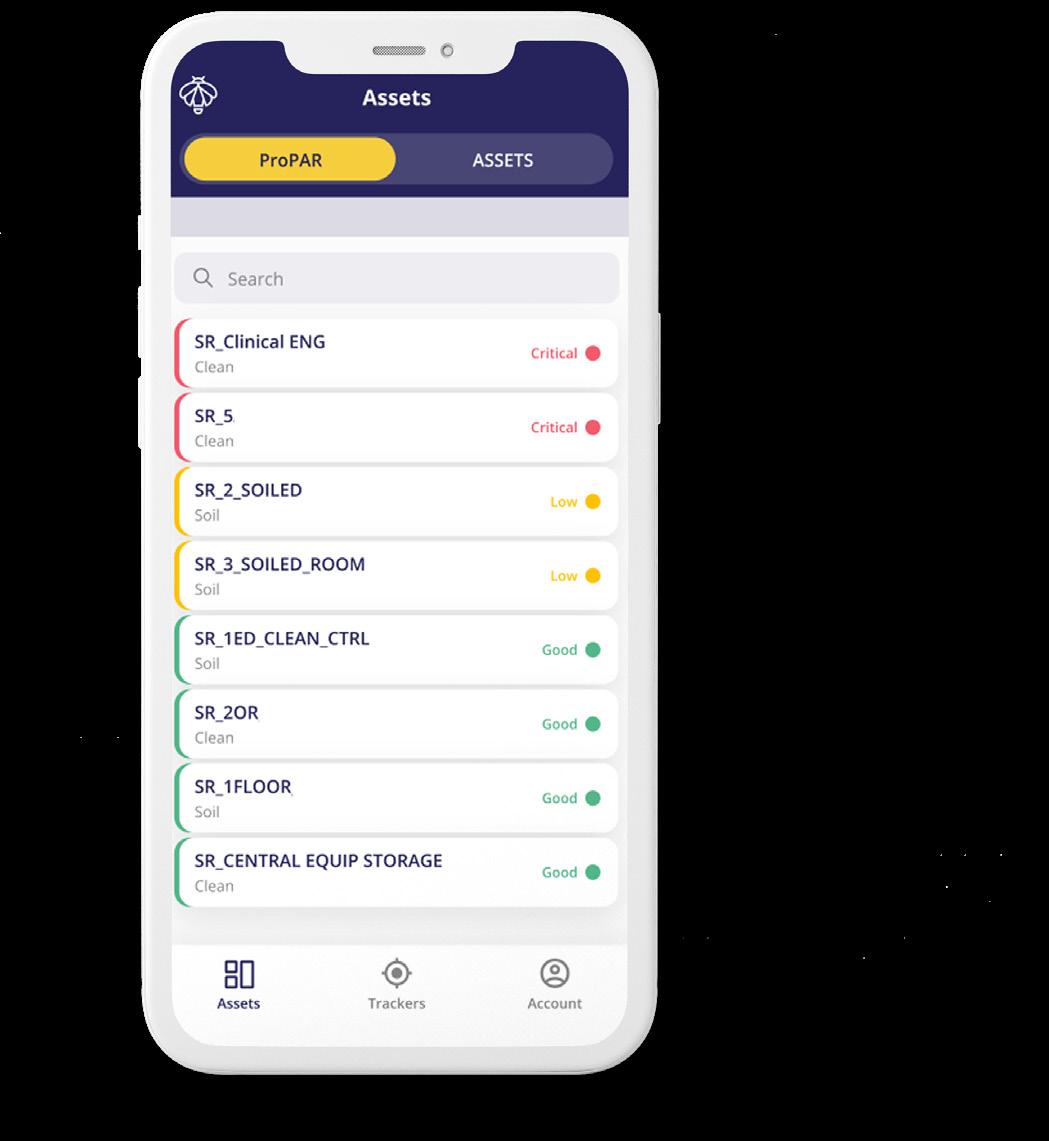
seamless integration to CMMS systems. The ideal solution will also provide options for multi-asset search and the ability to view those asset on maps. You will also want a solution that provides a mobile app for your users on the go. Reports on asset usage for reimbursement purposes should also be available as part of the standard solution.
BALASUBRAMANIAN : RTLS 2.0 as it’s been termed offers significant advantages and improvements over legacy RTLS solutions. RTLS 2.0 allows hospitals to deploy a platform solution and unlock several uses cases including asset tracking, staff duress and workflow, environmental monitoring, patient wandering/ elopement/workflow without the need to constantly add more infrastructure. The newest features include the ability to integrate with other health IT systems like asset management or EMR/EHR without significant cost hurdles eliminating the silos which exist in these systems today.
CRANE : Post-pandemic, there is a growing interest in three types of applications for RTLS – hand hygiene monitoring, contact tracing and infection control. The common theme among these emerging appli cations is to enable the health care enterprise to improve patient and staff safety while providing data to operational leaders that support process improvement regarding workflows in and around direct care areas.
DYCAICO : One of the newest and most impactful RTLS features is the enhanced real-time visibility of clean and soiled rooms. Now, RTLS solutions can self-report inventory levels. For example, if inventory falls below a set threshold, the RTLS system will automatically alert teams and provide room specific picklists to ensure PAR levels are always main
tained. Another notable feature is the ability to not only alert staff of equip ment loss in real-time, when the asset passes by an exit monitor, but also provide support for them by allowing them to use the mobile app to use “nearby” to locate the asset. For example, a wound vac passes by an exit monitor that leads to a soiled linen area. The exit monitor will send an alert by SMS message or email to a staff member. The staff member can go to the area and use the nearby function to locate the asset.
GREENHALGH : RTLS technology continues to evolve providing environmental services (EVS) for patient room and bathroom cleaning, automated reminders for cleaning, repair and preventative maintenance. Prioritizing tasks and notifications if temperatures drop in refrigerators or a door is left open is an example of how some hospitals used the technol ogy during COVID to protect vaccines.
MCMANUS : Some newer features integrate other facilities’ functions with RTLS. Some of these functions include integrating with the building management systems, like lighting
and HVAC systems. The newest features also include tags with accelerometers that can save on battery life and provide additional information when devices are moved.
WIEDMAN : Advanced data analytics and actionable reports have become table stakes for RTLS software. Biomeds, clinicians and the C-suite want a robust software solution that provides comprehensive visibility into a hospital’s assets.

ANDERSEN : There are a number of ways that an asset tracking system can provide a hard dollar ROI: asset utilization, PAR level on supply closets, notifications on rental equip ment when equipment is no longer in use, staff time saved when needing equipment and, most importantly, is understanding your facility spend prior to deploying an asset tracking system. This will become your benchmark to compare against moving forward. Utilizing historical asset location reports also assists with reimbursement of equipment usage that was used for specific procedures.
BALASUBRAMANIAN : Asset tracking systems can help reduce search time for equipment for nursing, clinical engineering and biomedical teams. Improvements translate into the various teams focus more on care, equipment maintenance and replen ishment. Asset tracking can help improve utilization of equipment, hence reducing yearly repurchasing of equipment not needed and reduction in rental costs. In addi tion, it can help reduce loss of equipment by alerting when equip ment leaves a building or has been left unattended. Asset tracking can help improve and automate various
determine whether a purchase is required, saving hospitals and health care facilities from unnecessarily renting equipment or purchasing assets. Moreover, exit monitors reduce the costs associated with loss and theft, while enterprise-wide insights save money by enhancing general processes and efficiencies.
Shon McManus Captal i LLCasset workflows including preventive maintenance, rental returns and replenishment.
CRANE : Studies conducted by Gartner and AMR Research found that on average, hospitals lose, can’t find or have stolen 20-30% of their mobile medical equipment (IV pumps, bladder scanners, wheelchairs, etc.) annually. An average inpatient hospital has 8-13 such assets per bed and the average asset cost is $5,000. If we take an average of 5 assets per bed, a 200-bed hospital will have approximately $5 million invested in clinical mobile asset inventory. With RTLS, a hospital can reduce lost and stolen assets, minimize the need for surplus inventory and eliminate the need for duplicate rental inventory by an average of 20%. For a 200-bed hospital, this could result in over $500,000 annually in savings. (Reference: sonitor.com/solu tion-briefs)
DYCAICO : RTLS gives teams a clear and comprehensive view of the utilization of any class of equipment, enabling evidence-based procure ment decisions that lead to meaning ful savings. Essentially, the data collected from RTLS helps staff
GREENHALGH : Many institutions suggest upwards of 50% of a techni cian’s time is spent searching for devices. This variable alone can often provide an adequate ROI for investing in an RTLS. Avoid unnec essary device purchases to replace mistakenly “lost” or “missing” devices. Combining MDSP data with RTLS data, users can support day-to-day operational workflows, such as preventative maintenance and recalls, by identifying the network location of the devices and pinpoint them on a map further supporting the business case for RTLS.
MCMANUS : The return on investment or cost savings associated with asset tracking systems inside a health care facility will be realized immediately, especially for larger facilities with tens of thousands of medical devices. First, accountability of the medical device – administrators no longer must worry about equipment being shoved into storage closets never to be found again … but needing to spend money to replace. Second, RTLS improves efficiency of service and maintenance of the medical device. Technicians will not spend countless hours (money) in search of the device; this will increase produc tivity and decrease downtime. Most importantly, mitigation of risk, which is ever prevalent when a “missing” life-saving medical device could not be serviced but finds its way onto a patient. The liability costs associated with an event like this could be unimaginable.
WIEDMAN : The benefits enjoyed by biomedical and supply chain leaders include: increased equipment utiliza tion to 75%; reduced equipment CAPEX; decreased rental fleet size; reduction in device shrinkage; and reduced PM and search time. I led a RTLS educational session at AAMI eXchange 2022, which profiled case studies of $10 million in savings from 8 prominent health care systems (Wake Forest Baptist; Adventist Health; Texas Health; CHRISTUS Health; Oregon Medi cal; Emory Healthcare; Providence Mission; and Piedmont Healthcare).
ANDERSEN : Security is a concern that should be taken very seriously when deploying any technology within a health care facility, ensuring solu tions are HIPAA and SOC2 compli ant. ZulaFly takes cybersecurity seriously regardless of the applica tion, whether it’s asset management, staff safety or patient workflow, that we are implementing for our customers.
BALASUBRAMANIAN : Cybersecurity should be an important consider ation when selecting asset tracking solutions. Some elements to consider include HIPAA, NIST and SOC 2 Compliance. This ensures that the solution being considered adheres to the most stringent requirements in health care for security, data protec tion, encryption and identity/access management.
CRANE : When thinking about cyber security, it’s all about identifying the weakest link within your system and unfortunately no system is complete ly immune. Sonitor does not store any critical patient or hospital sensitive data as we only capture and

transfer location data to our part ner’s application software. However, with regards to asset tracking, understanding the impact a breach might have can help you develop the appropriate safeguards. For example, if the location data of an asset is changed as a result of a breach, what impact would that have on hospital processes or workflows? If the assignment of an asset is changed, what effect would that have? At worst, this might disrupt flow and cause some inefficiencies.
DYCAICO : When considering RTLS technology, hospitals should look for a system that functions independent ly of Wi-Fi and other technology platforms that house PHI or protect ed information. Doing so will ensure that wireless networks don’t experi ence interference or unnecessarily heavy traffic and will eliminate potential access points for a cyberse curity incident.
GREENHALGH : Visibility is the corner stone to any cybersecurity program. You can’t protect what you can’t see. Device identification includes know
ing the make, model, serial number, MAC, IP address, OS version and the physical location of the device. Prioritizing risk and mitigation response times are often based on where a device is located, the ER versus an outpatient clinic. The same device with the same vulnerability but in different locations often have different risk levels and severity of impact. Knowing where every device that creates, stores, transmits or receives ePHI is a HIPAA security rule risk analysis requirement. The combination of an RTLS with an MDSP system can more accurately alert security operations when devices containing ePHI are lost or “walk out the door.”
MCMANUS : With any broadcasting or transmission technology there are always cybersecurity risks associated with use. Consumers must mitigate these risks by clearly defining their requirements, assessing the technolo gy that best meets their needs, and implementing all safeguards during installation of the RTLS. Consumers should not let the cybersecurity risk detract from the overwhelming benefits of an RTLS – understand the risk, mitigate the risk.
WIEDMAN : The Vizzia enterprise platform has been built from the ground up, specific to the unique needs of the health care industry. We are intentional in deploying ad vanced technologies and best practic es that address both infrastructure security and compliance regulations. Amazon Web Services (AWS) is our data hosting partner, which meets both HIPAA and HITRUST stan dards. We are also undergoing System and Organization Controls (SOC–2) compliance, as established by the American Institute of Certi fied Public Accountants (AICPA).
ANDERSEN: Start with the “musthave” functionality first, such as simply providing staff the ability to quickly locate equipment. From there, it’s easy to add-on PAR level, asset utilization, rental equipment dashboards, preventative mainte nance dates and so much more that can quickly provide a hard and soft dollar ROI. Since RTLS provides many use cases and applications, make sure to include multiple departments in RTLS conversations; security, biomed, supply chain, pharmacy and nursing to name a few. Buy-in from leadership will prove vital in a successful RTLS deployment.
BALASUBRAMANIAN : Some of the best practices when integrating RTLS into a health care facility include
• Formalize departmental owner ship and collaboration, ensuring buy-in and role definition among IT, clinical experts and nurses.
• Plan use cases early and have a clear understanding of how they’ll improve outcomes. This includes planning how to integrate the RTLS solution with existing workflows and other software solutions to achieve improved efficiency, cost savings and other outcomes
• Set up use and maintenance processes for RTLS, such as battery replacement, as well as badge and tag ordering and general equipment upkeep.
• Make smart use of vendors’ expertise. RTLS companies have the insights that can help organizations chart strategy or set up effective integration with other systems.
• Channel RTLS data into contin uous process improvement and workflow efficiencies. More
impactful outcomes require analyzing data, making changes and continuing to follow up on progress.
CRANE : Include clinical staff from the beginning and throughout the process. Ensure there is a well-de fined plan and ownership over maintenance and management of the system, whether it’s done in house or outsourced. For example, who and how will batteries in tags and devices be monitored and changed? Be transparent as to how reports and data will be used – make sure it focuses on value to caregiver/patient versus using information in a punitive way. Make sure to map out and understand what data sources will feed what applications. Is it one data source to one or one to many?
DYCAICO : First, it is best for health care facilities to understand and outline what they want from their RTLS. If that answer is simply to find equipment, then RTLS technolo gies like Wi-Fi or typical Bluetooth Low Energy (BLE) solutions may be the best fit. However, the true ROI of RTLS isn’t just in locating assets – it should be about supporting automation and producing action able insights to assist with critical decision-making and workflow enhancements.
GREENHALGH : Technicians having access to device locations can have tangential benefits for IT, who are often interrupted from their work to help find a wayward device. Work order management can also be positively impacted by an RTLS. The ability for clinicians to initiate a service request without interrupting their daily activities. Simply pushing a button can create a work order and pushing it again, when the BMET is finished with the service call,
updates the work order as complet ed. The time savings from automat ing this process are potentially significant.
MCMANUS : When integrating RTLS into a health care facility it is best to take a wholistic approach. This is Project Management 101, first you need to identify key stakeholders and get their buy-in. Next, outline the expected outcomes and goals you desire to achieve with the RTLS (some refer to this as KPIs). This will be specific to each facility and leadership team. Then we get into the nitty gritty, identify the number of devices, technology platforms and software that would require integra tion, degree of location accuracy required for the project, etc. All these steps should direct you to the RTLS system that best fits your facility’s needs.
WIEDMAN : Lessons learned from our 15-plus years of “go-live” experience with hospitals and clinics nation wide, have been published in a 15-page industry white paper. There are four key best-practices for HTM executives to utilize: 1) discover the top pain points in your hospital; 2) build a cross-functional steering committee; 3) select equipment and devices for tracking; and 4) identify KPIs to measure success up front.
EDITOR’S NOTE: This roundtable article was edit ed for length. Read the complete in-depth version online at 1TechNation.com/roundtable.
MedWrench is a product focused support network where medical professionals, purchasing administrators, manufacturers, dealers and industry experts can provide opinions, share ideas, and gather relevant information on medical technology and equipment. We want to say thank you for all of our users over the years. MedWrench wouldn’t be here if it wasn’t for our users!








Cybercrime cost Americans nearly $7 billion in 2021, substantially up from the $1.4 billion in losses in 2017. Micro soft reported an 1,100 percent increase in cyberattacks the week after the World Health Organization announced a global emergency be cause of COVID-19 in 2020. There are few people who have not been impacted.
Phishing scams led all types of Internet crimes in 2021; up nearly 40 percent. Cybercriminals have nearly perfected designing emails to resemble consumer companies, fooling unsuspecting victims. The criminal causes the victim to become an unknowing partner.
The victims of phishing scams and “non-payment” scams are most often people over the age of 50, who accounted for $3 billion of the 2021 losses. Those aged 60 and over filed 92,371 complaints in 2021 with the FBI.
Both personal email and busi ness email accounts have been targets of cybercriminals. More than $2 billion was stolen in 2021 through business email accounts.
The changes in the dynamics of the office; remote work and virtual meetings contributed to more online scams during the year.
It has become a routine feature
of modern-day life for a consumer to get a notification that their personal information has been compromised in a breach or that their email or other information was discovered on the “dark web” by an identity theft protection service.
Consumers have had to adapt to two-factor authentication and password management software to help protect themselves. Yet, the opportunities for criminals to mount an attack, compromise confidential information or spy on someone unnoticed has only increased with the increased onboarding of more “things” owned by the average person.

The Internet of Things (IoT) has exploded and the average “smart home” has numerous consumer products connected to the Internet. This is in addition to home net works, desktop computers, laptops, tablets and phones.
As a business segment, health care has been particularly vulnera ble and targeted by cybercriminals. Protected or personal health information (PHI) is a valuable commodity to cybercriminals who sell it over the dark web.
Millions of patients have been affected by this crime in recent years and it has cost health care organizations millions of dollars in compensation, penalty fees and

“The victims of phishing scams and “non-payment” scams are most often people over the age of 50, who accounted for $3 billion of the 2021 losses.”
reputation damage. Health care employees across the organiza tion must be trained to recog nize cybercrime and vulnerabili ties. Every weakness in the system, including email, must be addressed as a point of exposure for ePHI.
Medical devices are exposed to vulnerabilities throughout their life cycle. Some contain vulnerabilities at the point of installation and others are exposed years later. Attention to any existing vulnerability, or any new weakness that is created because of legacy software or any other reason, is essential to protecting the entire network and ePHI.
The importance of buttoning up any weaknesses in the system aren’t only to prevent a data breach, but also because con taining a breach can take time and expose more ePHI to hack ers. Knowledge of network security protocols has become an important talent in the biomed toolbox. It has also resulted in newer hybrid posi tions designed to address these threats.
Upgrades are important. Routine patching should be a habit. If one day a month is designated for patching, this will ascertain that it happens fre quently. Will the vendor be a partner during a data breach? This is a good pre-purchase question. Because imaging equipment contains an operating system, do you segregate these devices?
When purchasing new medi cal devices, it is best to know if the manufacturer is planning an upgrade a short time later.
The challenges for medical
configuration or solution design, but is anyone verifying this?
“A secure configuration may include aspects of the infrastruc ture in addition to the medical device configuration so it would require more than an HTM professional to perform this function,” Rubino says.
Any skipped steps during installation could provide an opportunity for hackers.
devices in the health care envi ronment increase exponentially every year as threats increase. Protection of PHI is fraught with the realities found within any equipment inventory. With budget constraints, some organizations are holding onto legacy devices.

“Ideally, an organization would have a documented secure configuration for all devices deployed within their environ ment. This is achievable when the overwhelming majority of the inventory comes from a small number of manufacturers and the organization has stan dardized on a few models. How ever, the typical medical device inventory is composed of poten tially hundreds of different manufacturer and model combi nations. Each combination may require its own consideration which should occur during the intake process, but what hap pens after the install,” says An thony Rubino, medical device network risk manager at Scripps Health in San Diego, California.
He says that there is some expectation the equipment was installed according to the secure
“A complete post-install verification of the secure config uration is time consuming and likely to be omitted. However, on occasion, unforeseen issues surface during install that cause a deviation from the secure configuration. Perhaps the medical device arrived without the latest operating system version or the dedicated VLAN is not routed through a firewall. Without a proper feedback process in place, the medical device may be improperly in stalled and potentially vulnera ble,” Rubino says.
After installation, every device should be carefully watched for any deviation in expected functioning. Some devices need to remain as a stand-alone.
“For setting up the device in the environment, by carefully monitoring its network activity, setting policies to get alerts on when there is a change in that behavior, health systems can track misconfigurations, unde sired changes in network topolo gy that could affect the device and any other issues and quickly move to fix and remediate them,” says Shankar Somasund aram, CEO and founder at Asimily in Mountain View, California.
One of the leading vulnerabil ities is unsupported legacy
Heidi Horn, MA, AAMIF VP at Nuvolosoftware that is found through out the health care industry.
“Networked medical devices with unsupported operating systems pose one of the biggest cyber risks. Unfortunately, it has been my observation when talking to health systems all over the world that most have no idea what operating system any of their equipment is running. You can’t protect what you don’t know about, so the first step is to get an accurate inventory of what equipment is networked, what each device’s IP and MAC address is, whether it stores and/ or transmits PHI, what operat ing system and upgrade version it’s running, and if it has antivi rus software or a firewall, etcetera,” says Heidi Horn, MA, AAMIF, vice president, industry solutions at Nuvolo.
She says that many hospitals are running passive monitoring software that can collect this information off the network, but if it’s not feeding back into their CMMS and matching to each applicable device, there’s no context to the data, and so it doesn’t do you much good.
“To add to the confusion, if a threat is identified by your cyber software, but only the IP address is known, you will have no way of knowing what or where the device is or who supports it. Therefore, it’s important for this data to be available in your CMMS,” Horn says.
Somasundaram agrees and singles out obsolete or outdated software as a concern.
“Health systems are having to deal with medical devices that are not kept up with updates, new versions, etcetera. This to be expected, since the software life cycles are accelerating continuously while medical devices are used in the environ ments for longer periods of time
as long as they are clinically viable. We have also seen cases where medical devices are not correctly configured in the network, and in some cases have been directly exposed to the network. In addition, as devices get de-commissioned improper disposal procedures mean ePHI could get exposed inadvertent ly,” he says.
Somasundaram says that the solution to the problem is not as complex as it seems. With the right approach, technology and processes; all of this can be addressed.

“First, for devices running outdated software and operating systems: Just because a device is running an outdated software does not mean that it is immedi ately a risk. A careful evaluation has to be done to understand whether there is a path to the device from an attacker. If there is a path, and if there is high impact of that device in the environment, then the attack vector can be mitigated by appropriate controls to ensure that the device can continue to be used as long as needed,” he says.
Rubino says that another
problem to address is, even if the device was installed properly according to the approved secure configuration, aspects of an organization’s environment change over time.
“Perhaps the original secure configuration includes security controls that have become obsolete. Regular reviews of the secure configuration or solution design should be part of every device security program,” he says.
Focusing on cabled devices attached to a network isn’t enough. The reality of connected devices today means that dozens or even hundreds of mobile devices can be connected through access points within the health care environment. These can include phones, tablets or other devices used for clinical purposes. It can also mean a number of non-medical devices.
Mobile devices owned by the health care facility can also present a risk.
“While aging networked devices pose the biggest risk, aging mobile devices that store PHI and lack cyber protection and/or are not tethered, also pose a major risk. I know of many examples where someone stole a mobile device like an ECG machine that had patient data on it, and the hospital had to go through a whole OIG investigation and pay fines. So, again, it’s important to have an inventory of those devices and ensure they’re properly protect ed,” Horn says.
Some health care organiza tions have had a breach occur as a result of a cellphone. Personal device strategies might include devices supplied by the institu tion. Also, telehealth may introduce new vulnerabilities.
Shankar Somasundaram CEO & Founder at Asimily
Devices taken out of service pose a real risk as well. Knowledge of what devices may contain per sonal information, or simply being aware of all devices in inventory, are both important.
“Not properly decommission ing a device, and documenting its proper disposal, creates a huge risk for an organiza tion. With the hospitals I have worked with over the years, on average, approximately four percent of devices due for a PM at any given time cannot be located and are ‘assumed’ to have been disposed of,” Horn says.
She says that HTM depart ments usually identify these devices in their CMMS as “lost” or “missing.”
“If any of those thousands of ‘lost’ devices stored PHI, and the hospital has no record of their proper disposal, that is a serious regulatory risk,” Horn adds.
The process for taking devices out of service should be
well-documented.
“For de-commissioning, health systems need to follow a methodical process and carefully track which devices have ePHI, follow proper de-commissioning processes including ensuring they are cleaned carefully before disposing them,” Somasundaram says.
Newer biomeds often have the advantage of cybersecurity training as a standard element in training. All members of the biomed department need to receive some training in this area.

“As I reflect on the topic and title of this article, it occurs to me that aging devices and aging HTM technicians have one major thing in common when it comes to cybersecurity – when they entered the hospital for the first-time years ago, cybersecuri ty was not a major concern. Because of this, many aging devices, as well as aging techni cians, are not prepared for the cyber threats that hospitals face
today. Fortunately, these gaps in knowledge (for the techs) and security protocols (for the equipment) can be improved with a little bit of effort,” Horn says.
Mitigating risk requires managing the risk profile of every device throughout its life cycle; from pre-procurement to de-commissioning.
“Finally, health systems can also get ahead of the problem by ensuring they are evaluating devices at procurement and deploying them in a secure way. Being able to then understand different risk profiles for differ ent configurations, understand ing which ones to go with and pros and cons of each can go a long way in ensuring that the right devices are acquired and deployed correctly,” Somasunda ram says.
“Not properly decommissioning a device, and documenting its proper disposal, creates a huge risk for an organization.” –Heidi Horn



Mention this ad for 10% OFF your next part or repair.

Scan the QR code and get an instant quote by using our free ultrasound probe evaluation tool.




























The topic of millennials in the work force has been in the news quite a bit lately, with one message coming through loud and clear: The demograph ic that will represent 75% of the global workforce in the next five years is not particularly loyal to their employers.
According to a survey by The Motley Fool, millennials accounted for 55% of those who changed career paths during the pandemic. And Gallup reports that 21% of millennials say they’ve changed jobs within the past year, more than three times the number of non-millennials who report the same. Those statistics made me wonder how companies can find and then retain this generation notorious for job-hopping. According to Anthony Reynolds, CEO of HireVue, there are four recruitment strategies that can help companies hire and retain millennials.
• Ensure your hiring is fair. “The bottom line is millennials care. They care about fairness and equality for all, and they want to work for socially responsible companies,” Reynolds says. “Plus, they care about equal pay among genders. Incorporating technology that is designed to mitigate bias into your hiring practices can help ensure your hiring is fairer and more transparent.”
• Measure for retention. What this means is to look for and fast-track candidates that possess “true skills that predict job performance” –
not just perfect resumes or degrees, Reynolds explains. Factors to look for include conscientiousness, emotional intelligence and problem-solving, he notes.
• Create a positive candidate experience. Millennials do their research when it comes to applying for jobs. And as Reynolds says, it’s easier than ever today for job seekers and current employees to weigh in about the company online. “In a candidate-driven market, you want to make sure your employee and candidate experiences are positive,” he stresses. “Take the necessary steps to create a positive candidate experience. Remember – if it’s not positive, candidates will go somewhere that is.”
• Think through your total compensation package. Millenni als look for jobs that offer a holistic package. “While salary is still a top priority, there are other factors as well,” says Reynolds, who cites ManPowerGroup’s research to show what these sought-after employees look for. “They found the top priorities for millennials are money (92%), security (87%), holidays/time off (86%), great people (80%), and flexible working conditions (79%).”
“Millennials want to work for companies that care about them as people – not just employees,” Reynolds says. “And it’s a
sentiment that impacts their overall engagement at work.”
Once you have millennials on board, it’s important to interact with them regularly in ways that make them feel engaged, according to Tabetha Sheaver, owner of Midwest business consultancy Plus Delta. She offers this advice:
Facilitate, encourage and enrich dialogue. That approach, Sheaver says, helps millennials gain a greater understand ing of where they stand in the organization. “It lets them know they can converse freely with management about not only their job but also about their hopes and aspirations,” she explains. “In other words, create a safe space for two-way conversations.”
Take time to explain how the company works and why. “What I am finding is millennials want leaders to take the time to explain their thinking, their ‘why’, and to clearly show them how to do what is being asked of them,” she says “Leaders have been doing the work they are doing typically for 15 to 20-plus years, but millennials haven’t; they need to learn. When millennials feel their leaders are investing in them, and care about their learning and development, they are more likely to stay.”
– Kathleen Furore is a Chicago-based writer and editor who has covered personal finance and other business-related topics for a variety of trade and consumer publications. You can email her your career questions at kfurore@yahoo.com.

We’re often asked, “What are the top repairs or service issues on MRI coils. Since so many have asked, independently of each other, we thought that it would be a great idea to share the content with TechNation readers. Coil life cy cle can be affected by several factors: Random electronic failures, general wear, premature wear and prevent able damage/trauma. Innovatus has amassed a large amount of failure analysis data after repairing almost 40,000 coils.
Based on data captured in the past two years – spanning over 3,600 coil repairs – over 34% of all coils present with mechanical damage due to preventable damage or trauma. An additional 18% possess failures related to preventable damage/ trauma. About 28% are related to general wear and less than 20% are actually failing because of random electronic component failures.

Simply stated, the majority of MRI coils sent to Innovatus have a root cause associated with physical, mechanical or preventable damage. Fifty-five percent is a very strong data point in that most service


contracts do not include failures related to preventable damage (or only allow for several preventable events). This means that many customers, who are paying a premi um to include coils on their magnet’s service contract, are paying upward of $50,000 or more, out-of-pocket, for an exchange coil from the OEM. One of the more frequently encountered points of failure is the system cable. Cable failures begin as intermittent issues that progress to hard failures, similar to any tethered device. Users typically begin to experience RF signal dropout, system ID failures and/or bias control voltage failures. The results
begin to present as image artifacts and ultimately QC failures. Al though system cables will become intermittent over time, most cable failures are related to one, or several, acute events that accelerate or exacerbate the cable’s natural life cycle.
Cable replacements from the OEM (if available) are extremely costly, with some approaching $15,000. A common strategy to address cable failures in the repair industry is to patch and splice an individual intermittent/broken wire. The reality of that approach is that, if one wire in the cable harness has become intermittent, the rest are
likely compromised and will most likely result in a latent failure. Innovatus’ preferred approach to cable failures is to rebuild the entire cable harness. This approach resets the cable’s life cycle and offers clients the longevity they expect.
Another common failure applies to flexible coils. Flex coils are designed to be draped across or wrapped around a region of interest. Embedded within the flexible areas of the coil is complex circuitry mounted to and connected by flexible copper traces. As you can guess, continued flexing will degrade and damage the flex circuits and is one of the more common points of failure on these types of coils.
Similar to cable failures, flex circuit failures begin as highly intermittent issues that progress into hard failures. Common to flex coil failures are stress fractures and tears in the flexible traces underneath the foam covering. Many times, there are no signs of physical damage to the foam, yet the underlying circuit ry has become compromised. That being said, a solid percentage of flex coils present with tears to the foam as well as the underlying circuitry due to compromised handling and transportation practices.
A common approach to repair flex circuit failures is to cut and fold-back the foam covering, bridge/ patch the broken flex circuit with copper material and then reseal the foam. In extreme cases, when there are many compromised areas, the entire flex area needs to be replaced and the entire coil needs to be re-foamed. Each repair provider has their own unique approach. Degrees of success and repair longevity are based on the materials and tech niques employed. Innovatus is confident in its approach, as coil repairs are warranted for six months.

There are several strategies for preventing and minimizing coil failures. Based on historical trends, the life cycle of most MRI coils is based upon the level of care and handling employed by end users.
One solid practice that can help to offset preventable damage is prop er cable routing practices and following the recommended process for connecting and disconnecting the coil from the magnet. To avoid opportunities for preventable damage, users may just need to pause for a second and look around.
Another best practice is to be sure that the coil is unplugged prior to lowering the table. Failing to do so may damage the coil, cable or connector and is traditionally not covered under the warranty or service contract.
Continuing with the last point, hasty actions are often the cause of much of the preventable damage seen, and most OEMs are very clear regarding patient placement practic es. For example, when using a flex coil, it’s important that technolo gists never attempt to adjust the position of the patient by moving the coil, as it may cause both physical and internal electro-mechanical damage. Also, flex coils should never be transported holding the foam section. The foam sections are
not designed to support the weight of the coil.
Establishing a well-communicat ed set of policies and best practices are the most effective methods of addressing failures within user control. These would span practices related to periodic inspection, proper storage, transportation, patient placement and cable routing practices as well as proper cleaning and disinfection processes.
A good strategy to compliment an MRI service contract is, if an MRI coil possesses any signs of physical damage, address that failure through repair versus the service contract. The result would reduce the costly out-of-pocket expense to a few thousand dollars.
Innovatus has repair capabilities on over 1,000 models of MRI coils. We have a solution for you. Latest breakthroughs include repairs to Philips fiber optic dStream coils and GE Air coils.
For more information , email at TedL@innovatusimaging.com or visit www.innovatusimaging.com/ultrasound.
-Ted Lucidi, CBET, is a clinical, tech nical and commercial specialist at Innovatus Imaging.



























As I write this column for the No vember 2022 issue, we are fully into the 2022 fall semester at Cincinnati State. This school year has started with a renewed interest in the healthcare technology management (HTM) field. Our program remains relatively small but solid for the past 30 years. We continue to wrestle with methods for increasing enrolment as we have cooperative education and full-time employers anxious to hire our students and graduates.
I recently had the opportunity to participate in a webinar hosted by AAMI. This webinar was titled “BMET Educators Share How to Teach Proper CMMS (Computerized Maintenance Management System) Data Entry.” This topic is one that we chose to feature in our HTM classes beginning this fall. We are adding software to our courses and students will learn more about this during their cooperative education assignments. A big thank you goes out to Heidi Horn and Nuvolo for providing software to educational institutions to allow us to teach “real-world” software in our laborato ries. We are excited to implement this software and enhance our coverage of the CMMS topic this year.
We found that this topic is very important to educators and hospital personnel. The webinar was very
well attended and many important questions were asked and answered.
The following link to the AAMI website has some additional resourc es on CMMS. AAMI website states, “Computerized maintenance man agement system (CMMS) software has become essential for healthcare technology management (HTM) program operations. Due to a lack of standardization in data collection, it has been all but impossible to assess their industry as a whole. That’s why six competing CMMS suppliers recently came together to standard ize how medical device information is configured. In the first phase of their work, they outlined an agreed-upon method for optimizing and standardizing failure codes. The second phase of the group’s work focused on defining and standardiz ing CMMS work order types.” aami. org/HTM/htm-resources
I feel that this is a good time to review some additional educational resources that I find useful for educators and HTM professionals looking to update or upgrade their competencies. We use these in our curriculum.
A resource that I find very useful is the “Core Competencies guide” from AAMI. The AAMI website states, “The intent of Core Compe tencies for the HTM Entry-level Technician: A Guide for Curriculum Development in Academic Institu
Steven J. Yelton, P.E.
tions is to provide academic institu tions/schools that offer technician training for the healthcare technolo gy management (HTM) profession with the following:
• a standard set of competen cies that graduates of techni cian training programs (certificate, diploma or degree) are expected to possess upon program completion; and
• recommended topics that a program curriculum should include in order for students to learn and possess the core competencies identified in this guide.
The competencies and topics in this guide are relevant to HTM technicians entering the workforce, and the topics reflect the knowledge and skills that entry-level techni cians are expected to perform successfully in entry level positions regardless of the employment organizations, e.g., hospitals, clinics, independent service organizations, military and manufacturers. This guide may also assist schools in preparing their graduates for professional certification, e.g., ACI certification exams.”
A PDF version of the “Core Competencies Guide” is available for free download from AAMI. https:// store.aami.org/s/store#/store/browse/ detail/a152E000006j64zQAA
Another resource that I use in the classroom and recommend to HTM professionals is the “HTM Career Planning Handbook.” The AAMI website states, “Career development is much more than getting a new job; it is about growing your skills and experience to advance in your career and be more valuable to your current and future employers. AAMI’s goal in creating AAMI’s Career Planning Handbook is to foster the development and advancement of its members. Many AAMI members work in institutions where they are part of a small staff of HTM professionals. Finding good guidance on career advancement can be challenging. This handbook provides you with tools you need to create meaningful career goals and chart the path to advancement. This guide also gives you the information you need to have conversations with your organization’s leaders on your future career objec tives.”
We find this guide to be very helpful to students it also, as the description says, provides tools to create meaning ful career goals and chart the path to advancement.
It is available at: https://store.aami.org/s/store#/store/ browse/detail/a152E000006j61QQAQ

These are just a few of the resources available to you from AAMI. Many others are available from different HTM organizations and societies. Please take advantage of resources made available by your local HTM group.
I also want to mention that AAMI membership is complementary to full-time HTM students and full time faculty.
– Steven J. Yelton, P.E., CHTM; is a Senior Consultant for HTM in Cincinnati, Ohio and is a Professor Emeritus at Cincinnati State Technical and Community College where he teaches biomedical instrumentation courses. He is the Immediate Past Chair of AAMI’s Board of Directors, a member of AAMI’s Foundation Board of Directors, Former chair of AAMI’s Technology Management Council (TMC) and Chair of AAMI’s HTAC Committee.









Imagine you are a defense or gov ernment agency, presented with a new wireless robot that allows for doctors from across the nation to perform surgery on patients. The technology is said to be the “next surgical robot of the future.” You are just about to ask for a quote for the product when the salesman mentions that the product is still in the process of becoming FIPS compliant.

Many hear those words when evaluating products, but never realize the complexity behind the letters or acronyms. Some may be asking “What does FIPS compliant mean?” or “Do I really need it to be FIPS compliant?” The answer to the second question is “Yes!” FIPS (140-2) stands for Federal Informa
tion Processing Standard and was developed by the National Institute of Science and Technology (NIST) to be the benchmark safety and cryp tography standard organizations must adhere to when protecting data. The FIPS standard is a require ment for all federal agencies that use cryptographic-based security systems to protect sensitive information in both computer and telecommunica tion systems (including voice sys tems) as defined in Section 5131 of the Information Technology Man agement Reform Act of 1996, Public Law 104-106 and the Federal Information Security Management Act of 2002, Public Law 107-347 (FISMA). It was implemented for third-party organizations working with the government to comply with the standards to protect Sensitive but Unclassified information (SBU). In
layman’s terms, the standard was built to validate that commercial cryptography algorithms are safe guarding sensitive information by encrypting and protecting the data.
There are a few areas an evaluator needs to know when reviewing the product. The first is to understand what a cryptographic module is, since it will be a key component for products that are FIPS compliant or FIPS validated. Let’s take the first word, cryptography. Although cryptography is not just encryption, we will focus on its use of encryp tion via keys and algorithms to protect the integrity of networks,

programs and data from attacks. A cryptographic module can be hardware, software, firmware or any combination of the three that implements some form of cryp tographic function (encryption, hashing, message authentication or key management) that implements encryption via algorithms or other methods. To receive FIPS compli ance, NIST and Communication Security Establishment Canada (CSEC) developed a Cryptographic Module Validation Program (CMVP) as defined by the International Orga nization for Standardization/ International Electrotechnical Commission (ISO/IEC). The pro gram will administer and evaluate the cryptography module to include the module’s level of security (1-lowest to 4-most stringent). When reviewing products, it is recommend ed to understand the data that will be involved with the product and review the level of encryption the system provides.
Next, let us review what the differ ence is between FIPS compliance and FIPS validation. FIPS compliant means some components of a product are validated, but the product has not been validated. FIPS validated means that a product has undergone and passed detailed conformance testing from a National Voluntary Laboratory Accreditation Program (NVLAP). Government agencies, especially for medical areas, commonly require 140-2 certification/validation. Due to the extensive documentation and validation that takes place for a
module to become certified, a FIPS certification may take months. It is important when evaluating products, to ask if the entire product is FIPS validated or what aspects are FIPS compliant. Do not forget that FIPS compliant does not mean the entire product is compliant.
Now, let us circle back to the wireless surgical robot scenario. When evaluating the wireless surgical robot, you should be focusing on identifying possible threats and determining if this product has the capabilities to protect your data. For those familiar with the CIA Triad, you know that when implementing a cybersecurity framework, you need to focus on maintaining confidentiality, integrity and availability. Despite any fire walls or encryptions that are imple mented, without a robust encryption from a FIPS validated system, the product has the possibility to allow other systems to read all traffic. Therefore, although the wireless surgical robot is a groundbreaking invention, it may be exposing your organization to more threatening cyberthreats. In this case, waiting for the system to become FIPS certified is the safer and more responsible approach. This decision will ensure that your network and data is always secure.
FIPS 140-3
So, what about FIPS 140-3? We have long awaited the time when FIPS 140-3 was going to be the standard for FIPS compliance. On September 21, 2021, CMVP stopped accepting FIPS 140-2 submissions for new validation certificates. Even though
the FIPS 140-2 submissions are no longer accepted, the module valida tions continue to be valid for five more years. This means that during your product evaluation, you can still consider products with FIPS 140-2 certifications. One thing to note is that by 2026, the certificates will all be moved to the historical list. There are not as many changes between 140-2 and 140-3; but now 140-3 aligns more with ISO/IEC 19790:2012(E) and ISO/IEC 24759:2017(E). If an update or change is made to the FIPS ISO/IEC standards that NIST does not feel is adequate for the security needs of the federal government, NIST will have the flexibility to adopt a different standard or create a revised standard controlled by NIST, to maintain the most secure posture possible.
You can obtain a FIPS certificate by contacting the medical device manufacturer (MDM) directly as part of your evaluation/prepurchase process or search for it on the CSRC Cryptographic Module Validation Program website (crc.nist.gov) by certificate number, vendor or module name. Keeping a copy of the FIPS certificate, making note of it in your medical device inventory and including it as part of your gover nance risk and compliance (GRC) policy will ensure you are further reducing risk of sensitive informa tion exposure and at the end of the day making your job easier to ensure that your medical devices are as secure as they can be.
– Nadia ElKaissi , CHTM, is the chief engineer at Charles George VA Medical Center.












M B I O M E D I C A L P A R T N E R S W I T H T O P I N D U S T R Y L E A D E R S A N D H O S P I T A L S A C R O S S T H E N A T I O N T O P R O V I D E T H E H I G H E S T Q U A L I T Y M E D I C A L E Q U I P M E N T F O R H O S P I T A L S , C L I N I C S A N D C O M P A N I E S A L I K E . L O C A T E D I N S A N T A A N A , C A L I F O R N I A , P M B I O M E D I C A L I S A D E P O T T O A S S I S T I N A L L I N D U S T R Y N E E D S A N D T H R I V E S T O P R OV I D E A C O M M O N G R O U N D F O R E N D U S E R B I O M E D I C A L E Q U I P M E N T































Do you consider yourself a history buff? Are you widely regarded among coworkers as an equipment aficionado? Here is your chance to prove it! Check out “The Vault” photo. Tell us what this medical device is and earn brag ging rights. Each person who submits a correct answer will be entered to win a $25 Amazon gift card. To submit your answer, visit 1TechNation. com/vault-november-2022. Good luck!
Send a photo of an old medical device to editor@mdpublishing.com and you could win a $25 Amazon gift card courtesy of TechNation !

Hand-wrist CPM machine






The Healthcare Technology Manager is a key member of many inter-hospital com mittees such as life safety, environment of care, capital acquisition, budgeting.
will have a well-established
relationship within the facility
customer satisfaction results and performance indicators being paramount.



Canon Medical Systems USA, Inc., a world leader in diagnostic imaging, is in search of qualified candidates to fill our open positions.



Medical Systems offers a competitive salary and benefits package, we support a diverse workplace and are an equal oppor tunity employer. We invite you to join and become part of our Canon family.
The Supervisor of Healthcare Technology Management (HTM) is responsible for the coordination of daily operations of one or more entities. Healthcare Technology Management staff are engaged in installing, inspecting, testing, monitoring, calibrating and repairing all OSF HealthCare patient care equipment.
The TRIMEDX Biomedical Engineering Intern gains on-the-job training by shadowing experienced clinical engineers, biomedical engineers, lab engineers, and radiology engineers under the close supervision of TRIMEDX management. In this po sition, you will perform preventative maintenance procedures, inventory validation, and have the opportunity to work alongside experienced techni cians in a real-time service environment.
InfuSystem is a growing healthcare service provider, specializing in medical devices and related products and services for patients in hospitals, clinics, ambulatory surgery centers, and other major service centers. We provide direct payer rentals, pump and consumable sales, and biomedical services and repair, serving all 50 states and Canada.
United Infusion honors to serve hospitals, nursing homes, home care agencies, surgery centers, testing labs, veterinary hospitals and practices, colleges, universi ties, and emergency medical centers.

Agiliti is a nationwide company of passionate medical equipment management experts who believe every interaction has the power to change a life. Our industry-leading commitment to quality and team of expert technicians helps ensure clinicians have access to patient-ready equipment needed for patient care.

Are you an independent go-getter that is mechanically inclined and that makes customer satisfaction and safety their top priorities? Come join our team, as a medical equipment installer!
Under the general direction of the Installation Proj ect Manager, you will provide complete equipment installation, in accordance with plans and specifi cations, including scheduling, delivery, installation, check-out, and final inspection of equipment
This position requires familiarity with many classes of medical imaging equipment and may perform maintenance on equipment outside these specialty areas. The Customer Support Engineer II/ III ensures regulatory compliance, assists in inventory, safe use and proper handling of medical Imaging equipment.
























828-396-6010
Bickford
800-795-3062
International,
Technologies, Inc.
800-609-9802
Biomedical, Inc
828-396-6010
of Biomedical
866-866-9027
Institute www.ecri.org
1-610-825-6000.
Medical www.probomedical.com
3174947872
855-401-4888
A.M. Bickford 75
74
ALCO Sales & Service Co. 72 Asset Services 4 Avante Health Solutions 57 BC Group International, Inc 92 Cadmet 79

41 Cognosos 23 College of Biomedical Equipment Technology 11 ECRI Institute 64 Elite Biomedical Solutions 37 Endo Technologies, Inc. 77 Engineering Services, KCS Inc 6

79
Excelitas Technologies 16 Healthmark Industries 7 HTM Jobs 80 Infusion Pump Repair 42 Injector Support and Service 22 Innovatus Imaging 8 Interpower 91
Medical Imaging
69 Lexicon MedParts
Life Spark Medical 25 Mammo.com 34 Maull Biomedical Training 60 Medigate 5 MedWrench 50 Multimedical Systems 27 Nuvolo 43
PM Biomedical 73 Probo Medical 58 Pronk Technologies, Inc. 2, 75 ReNew Biomedical 35 RepairMED 89 SakoMED 65 SalesMaker Carts 77 Siella Medical
51 Southeastern Biomedical, Inc 60 SPBS, Inc 41 Tri-Imaging Solutions 17 TruAsset, LLC 67 USOC Bio-Medical Services 3 Vizzia Technologies 38 Webinar Wednesday 29
Each month, TechNation magazine will feature photos from throughout the industry on this page. Be sure to tag your posts with #HTMStrong and check the magazine each month to see which photos are included and what is happening in the HTM community.







Interpower® hospital-grade replacement cords are manufactured well beyond minimum agency standards. Made in the U.S.A., Interpower NEMA 5-15, 5-20, 6-15, and 6-20 hospital-grade replacement cords provide correct amperages and voltages for medical devices—portable CT scanners, X-ray machines, medical-grade treadmills, ECMO machines, and ventilators—machines demanding AC power.

Interpower North American hospital-grade replacement cords come with NEMA hospital-grade plugs bearing the “green dot.” They are continually tested to surpass UL 817 (18.2.4.1) and C22.2 No. 21-14 requirements for hospital-grade power cords and cord sets.
Interpower cords and components are manufactured in accordance with Interpower’s product quality plan: hipot testing, continuity testing, ground testing, and inspections after each process. All cords provide the customer with the correct North American connections to the local mains power, which means our cords are ready to use right out of the box. In-stock cords ship the same day!