





Prepzyme® Forever Wet creates a long lasting moisture barrier. As seen here, instrument remains wet to the touch for days after application.








Prepzyme® Forever Wet creates a long lasting moisture barrier. As seen here, instrument remains wet to the touch for days after application.

The latest breakthrough in enzymatic pre-cleaning sprays, Prepzyme®
Forever Wet’s unique humectant properties form a moist coating over the instruments that lasts for days.

•The humectant formulation creates a moisture retention barrier which keeps soiled instruments and scopes moist for a prolonged period of time – unlike a GEL which HAS NO MOISTURE RETENTION properties
•Operating room safe, non-aerosol, multi-tiered enzymatic spray helps prevent bio-burden from drying on the surface of soiled instruments and scopes
•Ideal for transporting soiled instruments that may sit for an extended period of time
•Reduces tray weight during transport compared to liquid presoaks
•Soiled sharps are visible through humectant
• Decreases spills and potential cross-contamination



• Enclosed and vented dispensing chamber for complete operator and specimen safety
• Built-in scale for automatic specimen weighing
• Programmed maximum and minimum formalin levels for correct ratio
• Printed labels with customizable fields for complete documentation
• One-way valve lids for automatic filling and formalin fume protection
• Easy to use touchscreen with on-board tutorial videos for training


OR TODAY | Spring 2025


The global surgical equipment market is estimated to reach $32.5 billion by 2030.

Ruhof is dedicated to the research, development and manufacturing of stateof-the-art products for cleaning and reprocessing surgical instruments and scopes.
AORN’s new and updated Guidelines for Perioperative Practice in 2025 are the gold standard in evidence-based recommendations to deliver safe perioperative patient.

Gratitude and resentment – one makes you stronger while the other eats you from the inside. But you choose which one wins.
OR Today (Vol. 25, Issue #2) Spring 2025 is published quarterly by MD Publishing, 1155 Senoia Road, Ste. 200 Tyrone, GA 30290. POSTMASTER: See address changes to OR Today at 1155 Senoia Road, Ste. 200 Tyrone, GA 30290. For subscription information visit www.ortoday.com. The information and opinions expressed in the articles and advertisements herein are those of the writer and/or advertiser, and not necessarily those of the publisher. Reproduction in whole or in part without written permission is prohibited. © 2025


PUBLISHER
John M. Krieg
john@mdpublishing.com
VICE PRESIDENT
Kristin Leavoy kristin@mdpublishing.com
VICE PRESIDENT OF BUSINESS DEVELOPMENT
Jayme McKelvey jayme@mdpublishing.com
EDITOR
John Wallace editor@mdpublishing.com
ART DEPARTMENT
Karlee Gower
Taylor Hayes
Alicia Brown
ACCOUNT EXECUTIVES
Megan Cabot
Emily Hise
DIGITAL SERVICES
Cindy Galindo
Kennedy Krieg
EVENTS
Kristin Leavoy
ACCOUNTING
Diane Costea
WEBINARS
Linda Hasluem
EDITORIAL BOARD
Vangie Dennis, MSN, RN, CNOR, CMLSO Assistant Vice President, Perioperative Services, AnMed
Justin Fontenot, DNP, RN, NEA-BC, FAADN Associate Professor, Tulane University School of Medicine, New Orleans, LA
Natalie Lind, Education Director for the Healthcare Sterile Processing Association, HSPA
Pat Thornton, MSM, RN, CNOR Perioperative Consultant, RNFA Dermatology Institute
Dawn Whiteside, DNP, MSN, RN, CNOR, NPD-BC, RNFA, Director of Education, CCI
Julie Williamson, BA Director of Communications, HSPA
ChloraPrep™

Did you know? BD ChloraPrep™ Skin Prep is the only 2% CHG/70% IPA fully sterile surgical skin antiseptic in the US with demonstrated persistence of at least 7 days.1,2 Choose BD ChloraPrep™ Skin Prep and have peace of mind knowing that you are covered with persistent protection.
Why is persistence important?
Limits bacteria on the skin and helps minimize entry into a surgical incision after application
Healing takes time
Re-epithelialization can take up to two weeks3
Dressing
Changes can occur between 2–7 days
Recommended by numerous clinical guidelines4–10

Follow the QR Code to discover the difference of unmatched experience on proven performance.
BD ChloraPrep™ Skin Prep demonstrates at least PERSISTENCE1,2

1. Beausoleil C, Comstock SL, Werner D, Li L, Eby JM, Zook EC. Antimicrobial persistence of two alcoholic preoperative skin preparation solutions. Degala, et al. United States Patent 9,078,934. July 14, 2015. 3. desJardins-Park HE, Mascharak S, Chinta MS, Wan DC, Longaker MT. The Spectrum of Scarring in Craniofacial Wound Repair. Front Physiol. 2019 Mar 29;10:322 4. CDC, Berríos-Torres SI, Umscheid CA, et al. Centers for Disease Control and Prevention Guideline for the Prevention of Surgical Site Infection, 2017. JAMA Surg. 2017;152(8):784-791. 5. WHO. Global Guidelines for the Prevention of Surgical Site Infection, second edition. WHO Guidelines Approved by the Guidelines Review Committee. 2018. 6. Lok CE, Huber TS, Lee T, et al. KDOQI Clinical Practice Guideline for Vascular Access: 2019 Update. American Journal of Kidney Diseases. 2020;75(4):S1-S164. 7. Ling ML, Apisarnthanarak A, Abbas A, et al. APSIC guidelines for the prevention of surgical site infections. Antimicrob Resist Infect Control. 2019;8(1):174. 8. Ling ML, Apisarnthanarak A, Jaggi N, et al. APSIC guide for prevention of Central Line Associated Bloodstream Infections (CLABSI). Antimicrob Resist Infect Control. 2016;5(1):16. 9. NICE. Healthcare-associated infections: prevention and control in primary and community care. In: National Institute for Health and Care Excellence (UK) 10. O'Grady NP, Alexander M, Burns LA, et al. Guidelines for the prevention of intravascular catheter-related infections. Clin Infect Dis. 2011;52(9):e162-193.
By Dawn Whiteside
A s spring begins, familiar phrases such as “April showers bring May flowers,” “Don’t forget to smell the roses,” and “Breathe big” remind us of an often-overlooked aspect of patient care – complementary and holistic care. Nursing plays a crucial role in implementing evidence-based practices to enhance the health and wellbeing of individuals (ANA, 2025).
The American Holistic Nurses Association (AHNA) defines holistic care as interventions that support the whole person – body, mind, emotions, and spirit (AHNA, 2017). To support this approach, the Association of periOperative Registered Nurses (AORN) has published the Complementary Care Guideline for Recommended Practices, ensuring that surgical patients have access to holistic wellness options. According to AORN, “optimal perioperative nursing practice promotes patient well-being, and implementing patient-centered complementary care interventions can improve the perioperative experience for patients, their families, and healthcare workers, as well as reduce healthcare costs” (AORN, 2025). Integrating a holistic approach begins with assessment. Understanding
a patient’s values, health beliefs, and past healthcare experiences is crucial for implementing complementary care options (AORN, 2025). One key aspect of preoperative education is evaluating whether a patient takes herbs or supplements, as certain substances must be discontinued before surgery to prevent adverse reactions. This preoperative discussion also presents an opportunity to determine whether complementary care interventions might be beneficial or welcomed. For example, patients who regularly take vitamins or supplements may be more receptive to complementary therapies. Additionally, for individuals with a history of postoperative nausea and vomiting, ginger could serve as a complementary adjunct to traditional anti-nausea medications.
Music therapy is a well-recognized complementary intervention that helps reduce postoperative pain. While opioid medications remain the firstline treatment for moderate to severe pain, concerns related to the opioid epidemic have led to limitations on prescription duration and dosage. Incorporating music therapy into postoperative pain management has shown promising results. Research indicates that music with a tempo of 60-80 beats per minute is particularly
effective in reducing postoperative pain (Ferguson et al., 2024). Allowing patients to select their preferred genre while ensuring the volume does not disturb others – preferably through the use of headphones – enhances the effectiveness of this intervention (AORN, 2025; Ferguson et al., 2024).
Aromatherapy is another nonpharmacological method for reducing pain and stress. Lavender, in particular, is widely recognized for its sedative, antidepressant, relaxing, and antiemetic properties, with minimal toxicity risk (Silva et al., 2024). Postoperative pain is often exacerbated by sleep deprivation, physiological stress, and inflammation (Silva et al., 2024). A randomized controlled trial (RCT) involving cardiac surgery patients found that those who wore lavender oil-infused ceramic necklaces for 30-minute intervals experienced improved vital signs, including lower mean blood pressure and respiratory rate, as well as better sleep (Silva et al., 2024). Additionally, neroli oil, which has citrus overtones, has been shown to lower systolic blood pressure, though it did not significantly impact patients’ perceived anxiety or pain levels (AORN, 2025).
Guided imagery (GI) is another effective complementary intervention for reducing preoperative anxiety and

postoperative pain. Recommended for both adult and pediatric patients, GI has been shown to shorten the length of stay in the post-anesthesia care unit (AORN, 2025). This technique involves generating or recalling mental images and using verbal suggestions, such as storytelling, drawing, or dream interpretation (Pinto et al., 2024). Pre-recorded GI sessions may guide patients through progressive muscle relaxation and deep breathing exercises, helping to reduce stress, pain, anxiety, heart rate, blood pressure, and overall psychological distress (Pinto et al., 2024).
Scientific research on complementary and integrative health approaches continues to expand, supported by the National
Center for Complementary and Integrative Health (NCCIH). As part of the U.S. Department of Health and Human Services, the NCCIH investigates the safety, efficacy, and benefits of complementary care in improving healthcare outcomes (NCCIH, 2025). Perioperative patient care should encompass all possible strategies to optimize outcomes. When used appropriately and with patient consent, complementary care interventions can reduce stress and anxiety, alleviate pain, and ultimately enhance the overall patient experience. So, remember to “breathe big” and leave room to grow your practice by including complementary care interventions.

– Dawn Whiteside, DNP, MSN-Ed, RN, CNOR, NPDBC, RNFA is the Director of Education and Professional Development of the Competency & Credentialing Institute. Dr. Whiteside has over 35 years of experience as a perioperative nurse in many roles including circulator, scrub, first assistant, team leader, charge nurse, manager, and educator. She serves on the ABSNC Board of Directors as well as the editorial board for OR Today. As an educator, Dr. Whiteside is passionate about developing educational materials for all members of the perioperative team.
References
American Holistic Nurses Association [AHNA]. (2017). Position Statement: Position on the Role of Nurses in the Practice of Complementary & Integrative Health Approaches (CIHA). https:// www.ahna.org/Portals/66/Docs/ Committees/Corrected%20Position%20 Statment%20on%20the%20Role%20of%20 Nurses%20in%20the%20Practice%20 of%20Complementary%20%20 Integrative%20Health%20Approaches%20 (CIHA)%202016.pdf?ver=HNAu5c6jHUDiJCXgifuZg%3d%3d. Accessed February 12, 2025.
American Nurses Association [ANA].
(2025). Code of ethics for nurses with interpretive statements. https://www. nursingworld.org/our-certifications/anacode-of-ethics/ Ferguson, T., Taylor, C., Phillips, K., & Shannon, G. (2024). Music Listening: An Evidence-Based Approach to Managing Postoperative Pain. MEDSURG Nursing, 33(2), 73–78. https://doi. org/10.62116/MSJ.2024.33.2.73
Guideline for complementary care. In: Guidelines for Perioperative Practice. Denver, CO: AORN, Inc; 2025. National Center for Complementary and Integrative Health. (2025). About NCCIH. https://www.nccih.nih.gov/about
Pinto, B. M., Tavares, I., & Pozza, D. H. (2024). Enhancing Chronic NonCancer Pain Management: A Systematic Review of Mindfulness Therapies and Guided Imagery Interventions. Medicina (1010660X), 60(5), 686. https://doi. org/10.3390/medicina60050686
Silva, L. C. de M. A., dos Santos, K. V. G., dos Santos, J. J. de S., Camara, R. P. de P. O. A., Bezerra e Silva, S. Y., Silva, H. M. M. D., Ribeiro, K. R. B., Dantas, D. V., & Dantas, R. A. N. (2024). Efficacy of aromatherapy with Lavandula angustifolia oil on postoperative pain after cardiac surgery: A randomized clinical trial. EXPLORE, 20(6). https://doi. org/10.1016/j.explore.2024.103034

By Madelyn Jo May, RN, CNS, DNP
F or more than 25 years, articles about patient safety have referenced the 1999 Institute of Medicine (IOM) report, To Err is Human: Building a Safer Health System. This report’s main conclusion was that most medical errors were not the result of individual recklessness. Instead, faulty systems, conditions, and/or processes lead people to make, or fail to prevent, mistakes.
Since that report, health care has grown in complexity and sophistication. Pharmaceuticals, robotics, electronic documentation, and AI are just a few areas that have advanced the range of viable treatment options.
So why is this report – a quarter century old – still used as the benchmark?
Despite the evolution of care, our adverse event rate has remained largely unchanged. A recent study of adverse events associated with surgical care¹ identified adverse events in 38% of perioperative cases with 49.3% related to surgical procedures. For surgeons, nurses, and techs, this percentage should be sobering. Even for errors related to “faulty
systems, conditions, and/or processes,” improvement is the responsibility of individuals and teams striving to do better for their patients.
The time-out: Consistency vs. complacency
Many organizations focus on the surgical time-out as a single perioperative event – a brief, deliberate, and structured pause taken by the surgical team immediately before an incision. It can become so rote as to lose its focus as a critical feature of patient safety.
Complacency is a very real threat when we strive for process consistency. Over time, routine procedures become mechanical, and individuals fail to recognize the importance of each step in a process. Surgical teams are not immune to these pitfalls of familiarity. Well-worn practices can lead to skipping steps, rushing through the process, or treating a time-out as a quick check rather than a critical safety measure. Regular training, active team engagement, and variations in approach will break through mindless repetition and reinvigorate your staff.
Perioperative care encompasses three phases: preoperative, intraoperative,
and postoperative. Similarly, the time-out process can be divided into distinct moments during surgical care: before anesthesia, before incision, and before the patient leaves the OR. In fact, the World Health Organization’s Surgical Safety Checklist², divides 19 items among those phases.
By reframing the time-out as a series of opportunities for the surgical team to stop and ensure that corresponding aspects of safe surgical care have been addressed, each pause can increase awareness, mitigate risk, and combat complacency.
You can use a PDSA quality framework to execute your training.
Plan – Step back to evaluate your time-out process. Review each element of your checklist. Be sure you understand why it is there and when it is most important. Then add time-out review as a frequent agenda item for education sessions
Do – Implement the training and vary your approach to keep the content fresh. Here are some suggestions:
1. Emphasize the what and the why. Review the items on your checklist and engage discussion about potential patient safety risks when an element is omitted. Review roles and responsibilities during a time-
out to ensure that the whole team has a stake in the process.
2. Emphasize the what and the when. Set the idea that a distinct timeout will begin each perioperative phase. Recreate the journey of a patient undergoing a standard procedure and ask staff to identify the appropriate places to pause and check in. Suggest errors that could occur and celebrate “great catches” when the team can tie potential mistakes to time-out items. Or mix up your checklist items and have the team reorder it based on the patient journey.
3. Emphasize the who and the how. Conduct a mock time-out and assign someone (preferably a surgeon or other leader) to make deliberate errors. This should help train team members to speak up. Normalize looking out for each other. In a culture of safety, every voice is valued.
Or switch roles for the scenario so that individuals see the process from another point of view and remain attentive.
Study – Conduct audits of real time-outs and seek feedback. You can assign varying team members to review how time-outs are conducted in their cases. Fresh eyes on the process can identify opportunities for improvement.
Act – Share results. When discrepancies in the process are shared, ownership of solutions is amplified. If it feels important to the group, engagement increases, and behavior changes. The goal is to keep your timeout process dynamic and purposeful.
The implementation of checklists and time-outs is widely associated with improved patient safety. It is not enough to implement the surgical timeout process, but to also ensure its consistent and effective execution. Finding ways to re-engage surgical
team members in a purposeful surgical timeout is critical to preventing adverse events and improving patient outcomes.

– Madelyn Jo May is a full-time RN surveyor for ACHC’s Hospital Accreditation Programs. She has 33 years of experience in acute care, having served as director of quality, safety & regulatory compliance and as CNO. Her passion for patient safety drives her to advocate for better practices, ensuring every patient receives the highest standard of care.
1. https://www.bmj.com/content/387/ bmj-2024-080480
2 https://iris.who.int/bitstream/ handle/10665/44186/9789241598590_ eng_Checklist. pdf?sequence=2&isAllowed=y


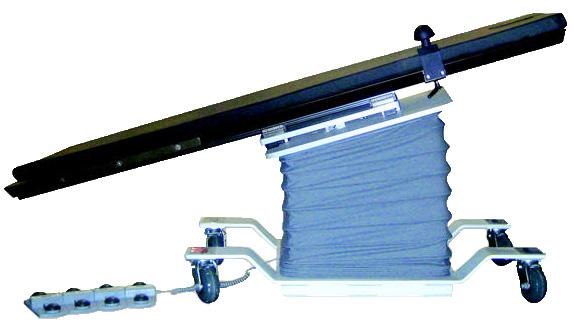
Soma Tech Intl was founded over 30 years ago with a mission to make healthcare more affordable by providing highquality refurbished medical equipment at an affordable cost. Over the years, Soma has built one of the largest inventories in the industry, backed by their ISO 13485:2016 certification, commitment to quality, and strong customer loyalty.
Soma Tech Intl Sales Director Ashish “Ash” Dhammam recently shared more information about this industry-leading company.
Q: What are some advantages that your company has over the competition?
Ash: Our advantages over our competition include our extensive refurbishment process, large inventory, strong warranty support, and field service, all complemented by a growing and repeat customer base. Soma offers cost-effective solutions to many hospitals and surgical centers without compromising on quality or patient safety, guaranteeing these facilities get the best return on their capital equipment investment.
Q: Can you explain your company’s core competencies and unique selling points?
Ash: Soma understands the critical importance of quality in the healthcare industry. Thus, we prioritize delivering trustworthy, top-tier equipment. When you request a quote, our team responds within 24 business hours, ensuring your needs are met promptly. Once an order for refurbished equipment is placed, our in-house team of skilled and certified biomedical engineers get to work. Our engineers specialize in specific types of equipment, ensuring each unit undergoes thorough testing and inspection.
Soma strongly focuses on quality control, ensuring that each product meets OEM standards. This is achieved through continuous investment in training, expanding our infrastructure, and optimizing our operations. With a large inventory, including dedicated stock for parts and long-term equipment support, we are prepared to meet your needs efficiently. Additionally, we strictly adhere to the ISO 13485:2016 standard, continuously improving our practices year after year to maintain the highest levels of quality and compliance.
We are committed to transparency with our customers, providing a unique engineering testing report with every piece
of equipment. This report proves that the unit has passed all necessary tests and is entirely patient-ready, meeting the highest safety and reliability standards. Whether seeking affordable equipment or expert service, Soma Tech Intl is dedicated to supporting the healthcare community with dependable, cost-effective solutions.
Q: What additions to Soma Tech Intl’s inventory and services are you most excited about right now?
Ash: Soma Tech Intl is expanding its offerings to serve healthcare facilities better. We now have a category of quickship items, providing same-day shipping on select products like EKG machines, stirrups, orthopedic accessories, carts, and patient monitors. This helps customers get the equipment they need without delays. We’re also focusing on highdemand specialties such as ophthalmic surgical equipment, surgical power tools, and OB/GYN equipment for obstetric and gynecological procedures, along with growing our specialty rentals portfolio. Additionally, we now offer brand-new power-assist surgical table stirrups and a universal spinal frame compatible with general surgical tables, Jackson tables, and other spinal tables. These products improve patient positioning and surgical precision while offering a more cost-effective alternative to name-brand options.

Q: What is on the horizon for your company?
Ash: Soma Tech Intl just finished the first stage in completing a 100,000 sq. ft. expansion, allowing us to significantly increase our inventory and better serve our customers faster. While the expansion is already enabling us to stock more equipment and meet growing demand, once completed, it will be a state-of-theart facility designed to enhance operations, streamline processes, and improve overall efficiency. The facility’s operations portion will begin taking shape this summer and should be complete by the end of the year. This investment reflects our commitment to continuous growth, ensuring we remain a leading provider of high-quality refurbished medical equipment while providing faster turnaround times and greater service reliability.
Q: Can you share how Soma Tech Intl has built long-term customer trust and provided critical support in urgent situations?
Ash: Soma Tech has consistently been the company of choice for capital equipment for many ASCs and hospitals nationwide. Our customers often come to us through word of mouth, a testament to the trust we’ve built over the years. We’ve repeatedly stepped in to provide critical equipment when facilities face urgent needs, whether due to sudden breakdowns, unexpected patient surges, or supply chain delays. Our ability to quickly deliver high-quality, patientready equipment has helped healthcare providers continue operations without disruption. Many of these customers remain with us for the long term, relying on our expertise, reliability,
and commitment to supporting their equipment needs.
Q: Can you describe your company’s facility?
Ash: Soma’s main headquarters is located in Bloomfield, Connecticut, and serves as the hub for our specialized biomedical engineering departments. These teams are dedicated to refurbishing a wide range of medical equipment, including ultrasounds, ventilators, anesthesia machines, X-rays, surgical tables, infusion pumps, and more. Our facility also houses a dedicated cosmetics department responsible for cleaning, sanding, and repainting equipment to restore it to like-new condition. Additionally, we have a large warehouse for storing equipment and office spaces for all other departments.
Our ongoing expansion significantly increases our technical department, warehouse capacity, and office space to enhance productivity and support our continued growth. Beyond our headquarters, we also operate micro repair shops within 20 miles of our main facility, allowing for more specialized service and faster turnaround times. In addition, we are expanding operations into Florida and the Upper Midwest with a focus on patient transport. Soma also has a small operation in the Pacific Northwest dedicated to sterile processing department equipment. These strategic expansions allow us to better serve healthcare facilities across the nation.
Q: How has Soma Tech Intl’s team contributed to the company’s longterm success and strong workplace culture?
Ash: Our success over the past 30+ years
is driven by our dedicated team—from expert biomeds to sales and customer service staff. Their expertise and commitment ensure that we provide exceptional service and reliable equipment. Many of our employees have been with the company for decades, bringing years of industry experience and knowledge that directly benefit our customers. We also take pride in fostering a supportive and collaborative work environment, where teamwork and shared expertise drive innovation and long-term success.
Q: Is there anything else you want readers to know about your company?
Ash: Soma Tech Intl is committed to giving back by actively donating medical equipment and supplies through the Rodos Foundation. Our efforts focus on improving surgical pediatric care and women’s health in underdeveloped countries, particularly in many African nations. Recent efforts include providing ultrasound equipment to healthcare facilities in Sierra Leone to support maternal and pediatric care. Over the years, we have also helped establish a small hospital with a NICU in Haiti, ensuring access to critical neonatal care. Currently, we are working on two projects in South America and India, furthering our mission to enhance pediatric healthcare. Through these initiatives, we strive to make a lasting impact on communities in need.
Scan QR code to visit Soma Tech Intl’s website.
W hat do the sterilization and sterility assurance fields have in common with a Clint Eastwood movie? Right now, the fields have “a lot of good, some bad, and some ugly.”
That’s according to Dr. William Rutala, director of the Statewide Program for Infection Control and Epidemiology and professor of medicine at the University of North Carolina. At the 2025 edition of the KILMER conference, Rutala took a wide-lens view of his field. Drawing on his decades of experience and more than 700 scientific publications, he discussed new sterilization technologies, surface disinfection, endoscope sterilization, ethylene oxide, and more.
The Good: Where Sterilization Science Succeeds
Rutala believes the field has “much better guidelines than we did many years ago.” Not only have groups like AORN and AAMI increasingly produced useful guidance documents, but guidelines from agencies like the FDA have also evolved. Yet implementing
manufacturer instructions for use (IFUs) remains challenging.
Right now, surgical instruments receive a Spaulding classification of “critical.” Overall, infections are rare, as surgical instruments have an enormous margin of safety. About 90% of reusable medical devices are sterilized using steam, and heat-resistant devices are usually processed using ethylene oxide (EO), vaporized hydrogen peroxide (VHP), and hydrogen peroxide gas plasma (HPGP).
Rutala also touted the importance of studies that “assess the robustness of sterilization technologies.” He cited several that focused on how proteins and salts impact sterilization. For example, one study of “dirty or non-cleaned instruments” applied steam, EO, and HPGP to instruments contaminated with bacteria and dried blood. Researchers found that steam was by far the most effective, followed by EO and HPGP.
Monitoring capabilities for physical, chemical, and biological parameters have also improved dramatically. Since the 1970s, the “read-out time” for assessing biological indicators has been reduced from days to minutes.
Environmental contamination and controls also belong in the “good” category. But despite awareness that environmental factors lead to healthcare-associated infections (HAIs), “we know our rooms are not adequately cleaned.” The issue? The field has “excellent products” but “very poor practices.” Further, “there are no specific regulations or professional organizational guidelines for microbiological control of surfaces.”
For instance, low-level disinfectants are “very effective against bacteria.” Yet the next patient in the room may be infected if pathogens are not removed from nearby surfaces. In response to these risks, “we have implemented supplemental disinfection technologies,” including the no-touch approach to room decontamination. Continuous room decontamination technologies, such as Far UV-C light paired with motion detectors, show promise but require more study.
The Bad: Room for Improvement
Rutala placed three items in the “bad” category. First, until November of 2024, no FDA-cleared standard defined when an instrument was clean.

Previously, cleanliness was usually defined visually. According to Rutala, there should be a standard to address circumstances where sterilization fails. “We just shouldn’t have best available technology; we should have some standard that relates to the failure of our sterilization technology.” According to Rutala, a cleaning verification test should be, at a minimum, easy to perform, rapid, robust, accurate, safe for equipment, and evidence-based.
Second, there is no standardized test that measures the effectiveness of disinfection and sterilization technology against prions. CreutzfeldtJakob Disease (CJD), the most common form of prion disease in the U.S., can incubate for years and has a relatively rapid onset. Worse, these prions are resistant to disinfection and sterilization, strengthening the need for a standardized test. There are already two definitive cases where a medical instrument was responsible for a CJD infection.
Finally, there are no FDA-cleared sterilization technologies for use against prions. Rutala noted that existing guidelines on this issue can be controversial, as they are not
based on standardized testing and prionicidal data.
The Ugly: What Harms Patients
Issues with endoscopes are the bulk of the “ugly,” or “the very, very bad.” Per Rutala, endoscopes “always should have been … considered a critical instrument requiring sterilization” because of their complexity and high microbial load.
The transition to considering endoscopes as critical instruments has been gradual. In 2014, an article in JAMA recommended moving from disinfection to sterilization, and AAMI and AORN followed suit. Now, we have “FDA-cleared technologies for reprocessing useable endoscopes,” including sterilization modalities such as EO and HPGP.
A Word on Ethylene Oxide
Last, Rutala addressed ethylene oxide and concerns over “its role in public health and the fragility of the medical device supply chain.” Many medical devices would not be usable without it, and implementing the 2024 EPA rule could disrupt the supply chain. Public commitments to modality switching
are “easy to say,” but implementation is a very complex problem. So far, the transition from ethylene oxide to other sterilization technologies has been slow. In 2024, the Global Unique Device Identification Database (GUDID) indicated that the FDA had cleared nearly 56,000 individual medical devices for sterilization via EO. Potential alternatives lagged far behind.
The good, the bad, and the ugly can tell us a lot about hospital sterilization as well as industrial sterilization. Rutala’s keynote at the 2025 KILMER conference set the stage for the rest of the conference’s programming. Despite clear optimism about the field’s advancements, he did not shy away from enduring threats to patients. Speaking for sterilization scientists and professionals, he concluded his address to the medical device industry professionals in the room, saying, “we essentially have many of the same issues you do.”
Those interested in the slides from the keynote can access them at disinfectionandsterilization.org.

By James X. Stobinski, Ph.D, RN, CNOR, CSSM(E), CNAMB(E)
In late 2024 a remarkable success story unfolded as the CRNFA credential earned accreditation from the Accreditation Board for Specialty Nursing Certification (ABSNC).
The Certified Registered Nurse First Assistant (CRNFA) credential has existed since the mid1990s but was purchased by the National Assistant at Surgery Certification (NASC) company in late 2018. Achieving accreditation is a noteworthy achievement considering the challenges faced by both the Registered Nurse First Assistant (RNFA) community and NASC. In way of disclosure, I know the owners of NASC well and I have served as an unpaid consultant on the accreditation application.
The sale of the CRNFA certification to NASC, a for-profit company, was initially upsetting to the RNFA community. Collectively, RNFAs have faced numerous recent challenges to include changes in
reimbursement for assistants in surgery and the rapid increase in nurse practitioners in surgery. The sale of the credential to NASC was not well received by many in the community.
The CRNFA credential was originally an examination-based credential, the predominant model for nursing certifications. However, a long steady decline in testing volume and numbers of CRNFAs made maintaining valid examinations increasingly difficult. As the number of CRNFAs declined and interest in the credential fell the certification lost its long-held accredited status secondary to these test development challenges. The loss of accreditation was a blow to these nurses and lowered the status and recognition of the RNFA role.
The lack of accreditation also had practical implications for some CRNFAs to include surgical privileging, reimbursement and benefits such as bonuses for certification. Upon purchasing the
credential the NASC leadership recognized these issues and quickly began work on a remedy. The infusion of resources from NASC coupled with a fresh perspective on the process of certification opened an alternative route to regain accreditation – a portfolio-based certification.
In early 2019 NASC began the long, resource-intensive process of converting the CRNFA certification to a portfolio-based assessment requiring active engagement and documentation of reflective learning. Patel and Metersky inform us that, “Reflective practice is a cognitive skill that demands conscious effort to look at a situation with an awareness of own beliefs, values, and practice enabling nurses to learn from experiences, incorporate that learning in improving patient care outcomes.”¹
An assessment by portfolio requires a peer review process using validated scoring rubrics. This is a much different experience
than taking a certification examination. The CRNFA portfolio, “…documents the validation of the professional achievement of identified standards of practice by an individual registered nurse serving in the expanded role of the registered nurse first assistant (RNFA).”² It must be noted that an accredited portfolio is developed using many of the same processes as examination-based certifications. The key difference being in the manner of assessment.
To meet accreditation standards, NASC hired psychometricians with competency assessment experience to supervise the portfolio development process. Dr. Judith Hale, Ph.D., of Hale Associates led a group of dedicated, industrious volunteers in months of development and validation work to forge an industry-leading assessment process.³ The visionary leadership and resources of NASC



• Vent the left heart during cardiopulmonary bypass surgery
• Securely positioned by inflating a soft positioning balloon in the LV
• Ensure drainage of air, blood and debris
• Disposable for one time use
secured ABSNC for the CRNFA certification accreditation after 5+ years of work; a remarkable achievement.
The employment outlook for Registered Nurse First Assistants is promising as the overall volume of surgery continues to increase and more surgeries are shifted to the ambulatory setting. 4 As facilities search for cost-effective, proven strategies to increase efficiency and surgeon satisfaction RNFAs are well positioned. The accredited CRNFA credential provides a logical career path for RNFAs and satisfies facility requirements for certification. Those RNFAs now entering the role have far more professional development opportunities because of the efforts of NASC and its volunteers.
– James X. Stobinski, Ph.D., RN, CNOR, CSSM(E), CNAMB(E), is a senior perioperative consultant with the

• Keeps sterile tethered appliances on the surgical field from falling to the floor with 4 hook & loop closures
• Latex free self adhesive back for attachment to the surgical field
• Economical - Saves pre-op time
• Several sizes, configurations, colors
• Sterile shelf life 2 years
• New Users call for FREE SAMPLES



National Institute of First Assisting and a professor at Central Michigan University.
References
1. Patel, K. M., & Metersky, K. (2022). Reflective practice in nursing: A concept Analysis. International Journal of Nursing Knowledge, 33(3), 180–187. https:// doi.org/10.1111/2047-3095.12350
2. National Assistant at Surgery Certification. (2020). CRNFA certification. https:// nascertification.com/crnfa/ certification/
3. Hale Associates. (n.d.) About Judy Hale. Hale Associates Center. https://halecenter.org/about-judy
4. Brusie, C. (January 15, 2025).
15 Highest paying nursing jobs in 2025. American Society of Registered Nurses. https://www. asrn.org/journal-advancedpractice-nursing/3249-15-highestpaying-nursing-jobs-in-2025.html


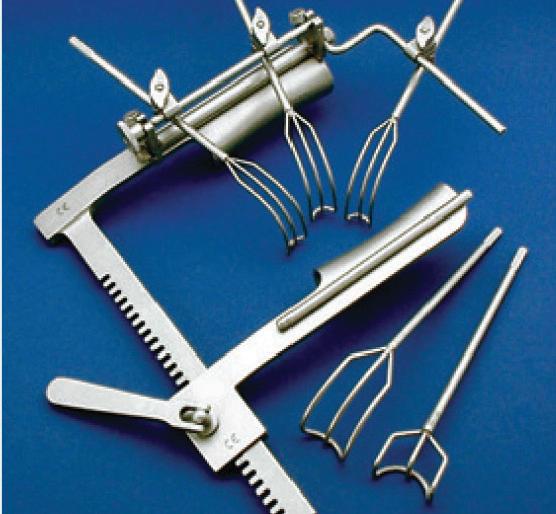
• Universal Self-retaining Heart Retractor
• Mitral Valve Repair or Replacement Surgery
• Exceptional Exposure for Right & Left Atrium Visit Kapp Surgical at www.KappSurgical.com


Agiliti, a leading manufacturer and provider of medical device solutions to the U.S. healthcare industry, recently announced the launch of Essentia, a versatile, multi-acuity bed frame designed to support a wide range of patients across different hospital settings. Essentia offers caregivers the flexibility to tailor care based on patient risk profiles and features proprietary safety capabilities –including the first-of-its-kind SlideRail – to help accelerate patient mobility and reduce risk to caregivers.
Essentia is the newest addition to an innovative portfolio of selfmanufactured beds and therapeutic support surfaces from Agiliti.
“The Essentia bed by Agiliti is tailor-made for more flexible and versatile patient care, backed by more than three decades of design innovation and clinical service expertise,” said Tom Leonard, CEO of Agiliti. “Its introduction builds on our long legacy of med-tech product and service solutions engineered to make sure caregivers are ready to meet the needs of every patient they serve.”
The bed’s SlideRail provides up to 39 inches of unobstructed egress space and flexes to three different positions for more support and security as patients exit or enter the bed. The adjustable handholds accommodate patient size and mobility and help reduce the burden and risk of injury to caregivers when moving or ambulating patients.
The on-bed, lighted SafeGlance icons provide caregivers a quick view of critical safety features, including the bed exit alarm, protocol timer, bed low height and brake status. Other features of the new Essentia bed include:
• 11.5” Deck Height: Essentia’s deck lowers to 11.5 inches from the floor – among the lowest of any multi-acuity bed frame available. Research shows that low bed height decreases the risk of serious injury from a fall. Combined with the SlideRail, these elements help hospitals minimize the risk of falls for a broad range of patients.
• RevTrend 20 with Weightbearing Footboard: Essentia introduces RevTrend 20, a 20-degree reverse Trendelenberg angle to support early mobility therapy. This unique feature allows patients to start weightbearing exercises sooner using the specially reinforced footboard.
• PowerBrake with AutoLock: With three locations on the bed, caregivers can set Essentia’s wheels to brake, steer or neutral with the press of a button. With AutoLock, the brakes activate after 60 seconds whenever the bed is plugged in, enhancing patient safety by keeping the bed from moving.
• MotionStop 360: 360-degree obstruction detection around the base of the bed frame will stop the bed from lowering if an object or obstruction is detected, helping prevent injuries or equipment damage.
• Powered Foot Extension: Caregivers and patients will appreciate the versatility of powered foot extension and the ability to customize the bed deck length from 80 to 88 inches with the push of a button.
• Support Surface Compatibility: A flat deck means Essentia is compatible with a wide range of support surfaces on the market, including more than a dozen Agiliti-manufactured foam and air options. Higher siderails mean even deeper air surfaces will meet safety standards for higher levels of patient acuity.
“We are thrilled to bring Essentia to the market and to offer caregivers a hospital bed that is specifically designed to help keep them safe and flex to the needs of the wide range of patients they serve,” said Tim McCarty, general manager of beds and therapeutic support surfaces at Agiliti. “The bed’s advanced capabilities will help patients get moving and out of the hospital faster.”
Beyond its capabilities as a manufacturer, Agiliti supports clinicians and patients with end-to-end medical device services and product offerings that help improve care outcomes and reduce costs for healthcare providers across the U.S.
Medline, the largest provider of medical-surgical products and supply chain solutions serving all points of care, today announced it has been awarded by the U.S. Department of Veterans Affairs (VA) 19 of a possible 20 delivery orders to support the Veterans Integrated Service Networks (VISNs) in administering high-quality care to veterans.
The agreement is to provide distribution of medicalsurgical products to the majority of VA Medical Centers (VAMC) in the Veterans Health Administration, America’s largest integrated healthcare system, and also encompasses distribution for Other Government Agencies (OGAs), including the Indian Health Service (IHS), Bureau of Prisons (BOP) and Health and Human Services (HHS).
The Veterans Health Administration (VHA) is a crucial provider of healthcare for veterans in the United States, with roughly 9 million veterans receiving care at more than 1,300 VA healthcare facilities across the country. The five-year contract aims to significantly improve efficiency and accuracy as part of the VA’s integrated supply chain improvement initiative. Medline’s best-in-class supply chain solutions, including its network of 45 distribution centers in the U.S. and an owned transportation fleet of 2,000-plus MedTrans trucks, will help ensure VA facilities receive reliable service.
“We believe Medline’s previous performance, competitive pricing and dedicated team were key factors for this award,” says Chris Powers, vice president of government services at Medline and a military veteran. “With every new relationship we forge, we keep the customer and their patients at the center of all we do, and we are honored to continue our work with the VA to serve our nation’s veterans.”
Newly awarded delivery orders and existing awards are estimated to be over $1 billion annually and will service over 90% of the Veterans Integrated Service Networks. Medline has extensive experience serving many federal and state government agencies, including the Centers for Disease Control and Prevention (CDC) and the Federal Emergency Management Agency (FEMA), state and local departments of health, hospitals and clinics, public schools and higher education institutions, medical examiners, law enforcement and emergency medical services (EMS), and the BOP. To support the needs of each agency, Medline has robust field-based representation and operational support, including contract compliance, dedicated customer service, logistics expertise, outcomes-based clinical programs, information systems and technology support.

soma@somatechnology.com (800) 438-7662
somatechnology.com
@Somatechintl
The Institute for Healthcare Improvement (IHI) and The DAISY Foundation have announced the recipients of the annual DAISY Award for Extraordinary Nurses in Patient Safety. The individual Honoree is Ashley Smith, BSN, RN, MEDSURG-BC, from Prisma Health Oconee Memorial Hospital in Seneca, South Carolina. The team award goes to the Adult Critical Care Nurses in the Intensive Care Units at Beth Israel Deaconess Medical Center in Boston, Massachusetts.
The DAISY Awards were presented at the 2025 IHI Patient Safety Congress. The DAISY Award for Extraordinary Nurses in Patient Safety celebrates nurses and clinical teams for their commitment to patient and workforce safety in the delivery of compassionate care for patients and families. More than 6,900 health care facilities and nursing schools across the US and in 43 countries and territories participate in the annual award program. All nurses and nurse-led teams from these DAISY partner organizations were eligible for the 2025 award.
“This year’s Honorees are particularly noteworthy for the actions they took that resulted in system-wide, and even nationwide, safety improvements,” said Patricia McGaffigan, RN, CPPS, Senior Advisor for Safety, IHI, and President, Certification Board for Professionals in Patient Safety. “These nurses are saving lives and shaping systems of safer care, and truly embody the spirit of The DAISY Award for Extraordinary Nurses in Patient Safety.”
“Partnering with IHI to honor nurses who have made an impact on patient and workplace safety is a thrill,” said Bonnie Barnes, FAAN, Co-founder, The DAISY Foundation. “This award aligns beautifully with The DAISY Foundation’s focus on compassionate care. There is nothing more compassionate than keeping patients safe from harm.”
• Ashley Smith, BSN, RN, MEDSURG-BC, Prisma Health Oconee Memorial Hospital (OMH), Seneca, South Carolina Ashley Smith’s colleagues know her to be a passionate advocate for patient safety with an unwavering commitment to improving patient outcomes. She has an extraordinary ability to identify safety risks. Prisma Health has a clinical operating system that empowers team members to readily improve the organization, and Ms. Smith has used this system to initiate many enterprise-wide solutions. In one such example, she streamlined the Electronic Health Record (EHR) system to significantly enhance workflow efficiency, allowing nurses to easily visualize patients’ fall risk status on the main screen. This advancement ensured quicker, more informed decision-making, directly benefiting patient care. In another example, Ms. Smith addressed the lack of integration between chair alarms and status boards, bridging this disconnect to create a safer care environment. Her efforts led to an impressive 20% reduction in fall rates on her unit, showcasing her ability to measurably improve patient safety. Both of these improvements impacted the
entire 18-hospital health system.
“Ashley Smith is a compassionate and empathetic trailblazer whose vision and tenacity have set a new benchmark for patient safety,” said Connie Spykerman, DNP, MBA, RN, NEA-BC, CNORe, Chief Nursing Officer, Prisma Health Oconee Memorial Hospital. “Her impact is invaluable, and her contributions have reshaped protocols and empowered teams to focus on safety. Her dedication to patient safety inspires us all. We are proud of her accomplishments, the culture at Prisma Health that fosters such commitment to excellence in care, and our clinical operating system that gives all of our team members the ability to improve our clinical systems.”
Smith’s influence extends to medication safety as well, and her leadership in ensuring safe care delivery has revolutionized workflows and added another layer of safety for patients across the organization. She frequently collaborates with her IT colleagues to improve systems to ensure clarity and precision in nursing actions. Her efforts have set standards for accuracy and safety and have transformed the care environment at Oconee Memorial Hospital and throughout the Prisma Health enterprise.
• Adult Critical Care Nurses, Intensive Care Units, Beth Israel Deaconess Medical Center, Boston, Massachusetts ICU nurses at Beth Israel Deaconess Medical Center consistently demonstrate their extraordinary commitment to patient safety, and one specific example resulted in a nationwide intravenous (IV) pump software recall. Nurses noticed that medication pumps were sounding an excess number of false occlusion alarms and interrupting the delivery of crucial medication. They utilized established communication vehicles and the patient safety reporting system to alert clinical and operational leaders. The nursing team assessed the situation, which quickly revealed that patient safety was at risk. The team collaborated with clinical engineering and the pump manufacturer to identify potential causes. It was discovered that the problem was related to a software upgrade, and that pumps by the same manufacturer deployed across the nation could be having the same issue. These actions led to a nationwide Class 1 recall, defined as a situation in which there is “reasonable probability” that patient exposure to a particular product “will cause serious adverse health consequences or death.”
“This is an extraordinary example of this team’s commitment to excellence through mitigation of patient safety risks,” said Pat Folcarelli, PhD, MA, RN, Chief Nursing Officer, Beth Israel Deaconess Medical Center. “It is a demonstration of how the staff is passionate about accountability for practice, and most importantly, how they use this passion to advocate for change.”
The ICU team received well-deserved recognition from the Food and Drug Administration (FDA), which noted their “outstanding contribution in promoting patient safety with medical devices.”
The number of U.S. product recalls remained high during 2024 with more than 3,200 events recorded for the second consecutive year. According to Sedgwick brand protection’s 2025 U.S. State of the Nation Recall Index report, the 3,232 recalls across five key industries represent the second-highest annual total in the past six years. Notably, 2023 and 2024 are the only consecutive years in the past decade in which U.S. recall events have exceeded 3,200. In contrast, the number of defective products recalled in 2024 fell to its lowest level since 2015, with 680.9 million units. This is a significant drop from the nearly 1.5 billion units that were recalled just two years earlier in 2022.
Sedgwick’s quarterly Index report analyzes recall data from the automotive, consumer product, food and drink, pharmaceutical, and medical device industries. This special edition not only includes Q4 events, but also provides a comprehensive year-in-review analysis of 2024 recall data and product safety trends. Multiple industries reached significant recall milestones in 2024. The consumer products sector experienced its second-highest recall total in the past eight years, while the medical device sector recorded a four-year high for recall events.








The new Gary C. Werths Building at Siteman Cancer Center on the Washington University Medical Campus realizes a bold vision for patient-centered, outpatient cancer care through the blending of state-of-the-art technology and robust amenities that support patients’ individual healing journeys.
To realize this ambitious vision, Lawrence Group partnered with Perkins Eastman to design the cutting-edge, 657,250-squarefoot facility, which officially opened on Sept. 30, 2024. The stateof-the-art cancer center serves patients of Siteman Cancer Center, based at Barnes-Jewish Hospital and Washington University School of Medicine in St. Louis, from throughout the region. The building’s advanced design supports the world-class medical team and research and will ensure healing outcomes for years to come – while leaving a bold mark on the urban fabric of St. Louis.
“Patients inspire everything we do,” said Siteman Director Timothy J. Eberlein, MD. “This facility expands on our 25-year history of leading-edge care and consolidates outpatient care to make visits easier for patients. We want every patient who walks through our doors to experience a supportive, calming and hopeful environment. This building was created with those goals in mind.”
Located near Forest Park in St. Louis, the Gary C. Werths Building is Siteman’s newest outpatient facility dedicated to multidisciplinary cancer care. About 75,000 people seek care each year at Siteman’s six locations for adult patients, with that number growing as more patients from around the country and beyond seek the expertise of WashU Medicine and BJC HealthCare cancer specialists and access to leading-edge clinical trials at Siteman.
This new model for cancer center design centralizes exam and specialty care spaces for an efficient patient experience, bringing together clinical services, including infusion therapy, clinical trials and diagnostic imaging, all under one roof to foster collaboration among multidisciplinary care teams.
The Gary C. Werths Building features 101 exam rooms, 88 private infusion rooms, and radiology and diagnostic imaging services, as well as nourishment stations, electric fireplaces, cozy seating and tables for playing games or crafting. A welcome desk, café, inviting lobby with seating, consultation spaces, information center/gift shop and retail pharmacy are located on the building’s first floor.


On April 5-8, 2025, perioperative nurses and health care professionals from around the world will come together for four days of dynamic learning, collaboration and inspiration. This year’s theme: Together We Rise, embodies the unity and collective commitment of perioperative professionals to elevate patient care and the art and science of surgical nursing.
AORN Global Surgical Conference & Expo is the world’s largest perioperative conference uniting nurses and leaders from around the world for four days filled with education, inspiring guest speakers, advanced research, hands-on workshops, networking and more.
• A Dynamic Four-Day Event covering a wide range of topics from specialized practices to broader healthcare issues. Hear from the top minds and leaders in the OR to discover the future of perioperative care.
• Engaging Educational Sessions with the opportunity to gain up to 200 contact hours with access to cutting edge evidence-based research.
• Hands-on Workshops and interactive experiences to improve your performance in and out of the operating room –ensuring you and your team can deliver the highest quality of care.
• Career Advancement with mentor opportunities, networking events, and increased visibility in the perioperative community.
Inspiring Speakers
Each day at AORN Expo offers a full schedule of educational and networking activities. Highlights include educational speaking sessions from some of the most innovative thinkers in health care and perioperative nursing, each offering unique insights into the future of nursing, health care and perioperative leadership.
EDUCATIONAL
AORN Expo 2025 will feature a plethora of the brightest and most innovative minds in perioperative care. Here’s a quick
look at what’s in store:
• Ruth Shumaker, RN, BSN, CNOR - “Are You a Perioperative or OR Nurse?”
• Louie Ang, DNP, MSN-Ed, RN, NPD-BC, CNOR-SURGOB - “To Infinity and Beyond: Advancing Perioperative Nursing through Technology”
• Marissa Tierney, RN, MSN, PCNS-BC, CCRN - “From Chaos to Control: The Power of a Code Team Response to Intraoperative Emergencies”
AORN’S COMPREHENSIVE EDUCATIONAL TRACKS
To meet the diverse needs of attendees, AORN Expo offers specialized education tracks designed to provide targeted learning experiences for nurses at every career stage:
• Leadership Summit: Gain full access to management-focused sessions and exclusive networking activities, along with all the benefits of the full conference.
• Ambulatory Hub: Gain access to specialized education sessions and networking opportunities tailored to outpatient surgery professionals.
• General Surgical Conference: Enjoy in-person access to all main conference education and activities, plus on-demand streaming for ultimate flexibility.
One of the most anticipated events at AORN Expo is the exhibit hall experience. As one of the largest surgical trade shows in the country AORN Expo sees upwards of 8,000 attendees every year.
Attendees can participate in product demos, learn about new solutions to critical challenges, and even earn additional contact hours through in-booth educational presentations. AORN Expo 2025 has been designed with multiple networking opportunities to ensure attendees can establish meaningful connections.
Whether you’re connecting with peers at a special reception, mingling in the first-time attendee lounge, or discussing ideas in the international lounge, networking is a vital part of the AORN Expo experience.Whether you’re connecting with peers at a special reception, mingling in the first-time attendee lounge, or discussing ideas in the international lounge, networking is a vital part of the AORN Expo experience.










he “Global Surgical Equipment Market - Trends and Outlook” report from ResearchAndMarkets.com predicts continued growth.
The global surgical equipment market size is estimated at $19.8 billion in 2024 and is projected to post a CAGR of 8.6% during the forecast period 2024-2030 to reach $32.5 billion by 2030.
Surgical instruments can be categorized into sutures and staples, handheld devices, electrosurgical tools, and more advanced machinery like surgical robotics, endoscopic instruments, and powered tools. The applications of surgery equipment span many fields, including obstetrics, orthopedics, cardiovascular care, neurosurgery, plastic and reconstructive surgery, and specializations such as ophthalmology, ENT, urology, and general surgery.
The surgical equipment market growth is driven by the increasing incidence of chronic diseases, such as cardiovascular diseases, cancer, and diabetes, which result in a higher need for surgical procedures. The growing number of geriatric populations, who are more vulnerable to various health issues, also drives the demand for surgeries.
Innovations in technology, especially in minimally invasive surgery (MIS), serve as another catalyst for growth, as MIS provides advantages like quick recovery
times and a decreased likelihood of complications.
Moreover, increased awareness regarding the benefits of prompt surgical intervention, escalating healthcare expenditures, and enhanced healthcare systems in developing regions are promoting the demand for sophisticated surgical instruments. The rise in sportsrelated injuries, automobile accidents, and cosmetic surgery procedures additionally fuels market expansion. In addition, favorable government policies, foreign investment in the healthcare sector, and increasing disposable incomes are broadening access to surgical care worldwide, resulting in a larger volume of surgeries and, therefore, a greater need for surgical equipment.
North America dominated the global surgical equipment market in 2024, holding a 38.2% share due to a significant incidence of chronic diseases, an aging demographic, advanced healthcare systems, and an increasing demand for minimally invasive procedures and robust healthcare expenditures. The United States is particularly notable for its wellestablished hospitals, prominent industry players, and innovative medical devices that contribute to market growth.
In contrast, the Asia Pacific region is expected to experience the fastest growth rate with a CAGR of 9.5% during the forecast period 2024-2030, propelled by rising disposable incomes in nations
such as India, China, and Japan, as well as an upsurge in plastic, reconstructive, cardiovascular, and orthopedic surgeries. The rapid development of healthcare infrastructure, urbanization, and a rising elderly population further bolster the expansion of this regional market.
The surgical sutures and stapler was the largest segment of the surgical equipment market in 2024, with an estimated 42.3% market share, driven by its widespread application in wound closure. Sutures, which can be crafted from materials such as nylon or silk, and metal staplers, usually made of stainless steel or titanium, are chosen based on the nature of the surgery and patient requirements. Sutures may be absorbable, which breaks down naturally, or nonabsorbable, necessitating removal to avoid infection. Metal staplers are gaining popularity for their benefits, which include expedited healing and reduced infection rates.
On the other hand, the electrosurgical devices segment is projected to record the fastest CAGR of 9.1% from 2024 to 2030, fueled by the increasing preference for minimally invasive surgeries that result in quicker recoveries and shorter hospital admissions. These devices find applications across various specialties, including gastroenterology, gynecology, and dermatology, which further contributes to the expansion of the market.

IN THE OR product focus


The MHVC is a soft balloon-tipped catheter. It is inserted through the open left atrium during mitral valve surgery or through the right superior pulmonary vein on the beating heart and across the mitral valve into the left ventricle. Uniquely, the device is securely positioned and maintained in the LV by inflating a soft positioning balloon against the mitral annulus/valve. The balloon inflates, keeping the catheter tip below the mitral valve to ensure drainage of air, blood and debris from the left atrium and left ventricle. The MHVC consists of a flexible tube with a soft compliant balloon located on the distal portion of the tube with drainage holes both proximal and distal to the balloon. The catheter is provided with a tapered tip, a malleable stylet and depth markings to insure smooth insertion. Overall length is approximately 43.8 cm (17.25 in). The inflatable balloon is filled with sterile saline solution and holds the catheter in place at the desired location. Catheter 16 fr. O.D. (5.5 mm dia.) Supplied sterile, for one time use.
For more information visit KappSurgical.com.
Swann Morton scalpel handles are designed for precision and reliability in surgical procedures. Manufactured to ISO 13485, ISO 14001, and ISO 50001 standards, they ensure a precise fit with Swann Morton surgical blades, maintaining consistency in performance.
Over time, repeated use, sterilization, and handling can wear down handle fitment, affecting blade stability and surgical precision. A properly fitted blade is essential for maintaining control, and using a high-quality handle minimizes the risk of looseness or misalignment during critical procedures.

Swann Morton offers a variety of handle options to suit different surgical needs, including standard stainless steel, ergonomic stainless steel, and ergonomic plastic designs. The No. 3 or 5 fitment handles are compatible with blade sizes 6-16, while No. 4 or 6 fitment handles are used with blades 18-27. Swann Morton handles are also UDI compliant, the new requirement that identifies medical devices and is intended to improve patient safety.
Selecting the appropriate handle ensures a secure blade fit, supporting precision and consistency in surgical work.




The Olympus surgical energy portfolio includes the POWERSEAL Sealer/Divider 5mm Devices with three jaw designs each available in three shaft lengths: the POWERSEAL Straight Jaw, Double-action (SJDA); POWERSEAL Curved Jaw, Single-action (CJSA); and POWERSEAL Curved Jaw, Double-action (CJDA). The advanced bipolar surgical energy devices are designed to support procedural efficiency and surgeon comfort with a multifunctional feature set and carefully considered ergonomics. Each POWERSEAL design requires less squeeze force than competitor devices to close the jaws without sacrificing jaw force or sealing capability.
The POWERSEAL single-use devices provide surgeons with reliable sealing, dissection, and grasping capabilities in laparoscopic or open surgery and are designed for ease-of-use and comfort. The POWERSEAL devices are indicated
As one of the world’s largest suppliers in surgical instruments, Aesculap continues to raise the bar for how surgical instruments perform. Designed with the end user in mind, SQ.line Surgical Instrument enhancements go beyond performance in the OR. SQ.line Surgical Instruments are designed to offer improvements in ergonomics, sterilization capabilities, grip and repair. Featuring more than 200 patterns, SQ.line Surgical Instruments offer a complete solution to service basic instrumentation for spine and orthopaedic procedures.
for use in numerous surgical procedures including general surgery, gynecological, colorectal, bariatric, urological, thoracic, and vascular procedures. The POWERSEAL device is intended for single use only and has not been shown to be effective for tubal sterilization or tubal coagulation for sterilization procedures. Consult with a qualified professional prior to utilizing on patients who have electronic implants to avoid possible hazard.









I n 1976, Frank Bass and Bernard Esquenet teamed up to create The Ruhof Corporation. Frank Bass’s role in the company is one of sales, marketing and research while Bernard Esquenet is the chemist behind Ruhof’s success.
Prior to the launch of Ruhof, Frank recognized the need for hospitals to use more than simple dishwashing detergent in cleaning surgical instruments. Bernard had created cleaning solutions for the Navy, which were used to clean barnacles and other crustaceous marine residues from the heat exchangers and water evaporators of submarines and other naval vessels.
When Frank Bass approached him to develop cleaning solutions for hospital instruments, Esquenet realized that the enzymes he was using to eat away at the marine organism residues would also dissolve proteins off surgical instruments. Thus, Protozyme, the very first enzymatic cleaner for surgical instrumentation was born along with Surgistain, a product for refurbishing corroded stainless steel instruments.
Since then, Ruhof has dedicated itself to the research, development and manufacturing of state-of-theart products to ensure the complete cleaning and reprocessing of all surgical instruments and scopes.
Addressing the ever-increasing concern of cross contamination in hospitals, Ruhof’s research and development department revolutionized the cleaning industry with our multi-tiered enzymatic detergents and sponges, cleaning brushes, pre-treatment foams/sprays, cleaning verification products and more.
Additionally, the comprehensive ScopeValet line of endoscopy products supports the steps of the scope reprocessing cycle from bedside cleaning through to transport and storage. These GI offerings help endoscopy suites improve operating efficiencies while adhering to guidelines and protecting patients and staff alike.
Q: What are some advantages that your company has over the competition?
A: Ruhof Healthcare sells the only enzymatic detergent on the market (ENDOZIME BIO-CLEAN) clinically tested to pass the difficult ISO standard 15883 Annex F by dissolving bio fi lm and exposing underlying bacteria to high-level disinfectants or liquid chemical sterilants. Our products are of the highest quality available, and we offer the most complete line of surgical instrument cleaning, scope cleaning, and reprocessing supplies in the marketplace. In addition, the company is innovative, continually developing new products and technologies that clean, protect, comply, and verify to meet the needs of our customers.
Q. How have you been able to help with recent challenges faced by your customers?
A: Recent reports to the U.S. Food & Drug Administration (FDA) of processing errors with flexible endoscopes have brought much attention to the importance of this issue. In general, while flexible endoscopes are inherently difficult
to clean effectively due to their long narrow lumens and because they are used in highly contaminated areas of the body, the manual component of endoscope reprocessing appears to be the area most prone to error. As a
“We are always finding new solutions and new ways to help fight HAIs and to provide a safe work environment for patients and staff.”

result, revised guidelines from both the CDC and the AORN recommend the used of cleaning verification tests such as ATP bioluminescence, which has been shown to be both a rapid and effective method for assessing the efficacy of the cleaning process. Ruhof’s ATP Monitoring System, newly named the CleanRead Contamination Monitoring System is a quick, simple, and reliable method for verifying the effectiveness of
the cleaning and decontamination process for the outer surfaces and internal channels of scopes and cannulated instruments along with all non-critical facility surfaces. The CleanRead Contamination Monitoring System consists of a lightweight hand-held device, sampling tools – the CleanRead Surface ATP Detection Swab and Test InstruSponge – and easy to use software for tracking results. The system can also be used to test the efficacy of the cleaning process for the especially complex duodenoscope, an endoscope associated with outbreaks of Carbapenem-resistant Enterobacteriaceae (CRE) infections.
Q: Can you explain your company’s core competencies and unique selling points?
A: We are the only supplier of enzymatic detergents that manufactures its own product, guaranteeing consistency and quality. Ruhof is a registered ISO 14001 & ISO 13485 manufacturer, and we pride ourselves on the superior products we manufacture.
Q: What product or service that your company offers are you most excited about right now?
A: We’re excited to introduce a fresh brand identity for the ATP Complete 2 Contamination Monitoring System – now the CleanRead Contamination Monitoring System. This rebranding reflects our commitment to expanding beyond ATP testing to include protein testing and more. While users will continue to experience the same high-performing product, this change paves the way for future innovations. Our evolving product line includes the CleanRead ATP Test Swab, CleanRead Aqua ATP Detection Swab, and the CleanRead PRT Surface Protein Swab, with even more advancements on the horizon.
Q: Can you share some company success stories with our readers?
A: Ruhof often receives positive feedback from customers regarding cost savings. Perioperative and sterile processing professionals regularly tell us that they get better results and more cleaning efficacy using much less of our detergent than other brands. In addition, we receive many reports about product effectiveness. Recently a nurse contacted us about how Ruhof really “saved the day” for her. All other detergents failed to remove an unusual yellow/orange oily deposit from the scopes she was cleaning but our Endozime SLR enzymatic cleaner – which specializes in removing synthetic lipid residue – did the trick and she has been a loyal customer since.
Q: Can you highlight any future product plans?
A: While still in development Ruhof is working on a breakthrough
delivery system for Point-Of-Use Cleaning: A Portable Automatic Sprayer. The Sprayer quickly and easily applies Prepzyme Forever Wet – our multi-layered enzymatic humectant – over surgical instruments and scopes, prior to manual cleaning, to prevent the adhesion of bioburden. This automatic delivery system eliminates hard to use trigger sprayers and can cover an entire tray of instruments in half the time! Stay tuned for the arrival of this exciting product!
Q: How does Ruhof support customers?
A: Ruhof has a most knowledgeable and responsive customer service department and sales team ready to help our customers with questions, orders, troubleshooting, etc. Our user-friendly website and informative technical data sheets/ IFUs also provide support. We offer a program of free accredited continuing education for nurses and
CS/SPD techs, as we understand that ongoing education, training and mentoring are critical to the success of any clinical department. These CE opportunities are offered at national and local trade shows, as well as right on our website www.ruhof. com/pages/education.
Q: What is your company’s mission statement?
A: At Ruhof, we understand the importance of cleanliness in the healthcare fi eld and are guided by our commitment to excellence. We demonstrate this by offering reliable solutions and individualized service to help health care facilities meet and exceed their decontamination and infection prevention challenges. We are always fi nding new solutions and new ways to help fi ght HAIs and to provide a safe work environment for patients and staff. We value our customers as much as the patients that they care for.

For the cleaning verification of surgical instruments, endoscopes, and surfaces, CleanRead™ Handheld is a cloud-based cleaning monitoring system used to help hospitals and other healthcare organizations achieve optimal standardized cleaning levels.

• SMART HANDHELD MOBILE PLATFORM
• CLOUD-BASED
• WI-FI CONNECTIVITY
• INFINITE USERS & TEST POINTS
• CUSTOMIZABLE DASHBOARD
• RFID RE ADER / BARCODE READER
• USER FRIENDLY INTERFACE



• ENDO SCOPY
• STERILE PROCESSING
• OPERATING ROOM
• ENVIRONMENTAL SERVICES, etc.






Eliminate
Reduce turnaround time














By Don Sadler
The Association of periOperative Registered Nurses (AORN) has issued new and updated Guidelines for Perioperative Practice in 2025 that all perioperative personnel should be aware of. These guidelines are the gold standard in evidencebased recommendations to deliver safe perioperative patient care and achieve workplace safety.
How Are the Guidelines Drafted?
The Guidelines for Perioperative Practice are drafted by the AORN Guidelines
Advisory Board, which is comprised of a chairperson, at least eight perioperative nurse members and liaisons from other professional associations.
The first step in drafting the guidelines is a literature search. Next, the level and quality of each piece of evidence (both research and non-research) is appraised using AORN’s evidence-based appraisal tools, with an appraisal score of I-V and A, B or C assigned. Very low levels of evidence are not accepted.
The research is then translated into recommendations and the guidelines’ required elements are confirmed:
introduction, purpose, evidence review, recommendation (rating), glossary and references. Each recommendation is rated using AORN’s evidence rating model:
• Regulatory requirement
• Recommendation
• Conditional recommendation
• No recommendation
The draft guideline is posted on the AORN website for a 30-day public comment period. All submitted comments are reviewed and action is taken on each: accept, accept with modification or not accept. The draft is then amended in collaboration with the editor-in-chief
before the final draft is submitted to the Guidelines Advisory Board for final approval before the guideline is published. Each guideline is reviewed and updated on a five-year cycle.
Following is an overview of the new and updated AORN guidelines issued in 2025.
The Enhanced Recovery After Surgery (ERAS) guideline is a new guideline focused on how to implement this evidence-based model of care. “We believe that ERAS is the standard of care that should be implemented in all patients undergoing surgery,” says Lisa Spruce, DNP, RN, CNS-CP, EBP-C, CNOR, ACNS, ACNP, FAAN, AORN Senior Director of Evidence-Based Perioperative Practice.
According to Spruce, the ERAS guideline offers guidance on preoperative screening of patient risk factors, optimizing the patient’s health prior to surgery and comprehensive education for patients in an ERAS program.
“Preoperative preparation includes preparing the patient for surgery by appropriate fasting guidance, conducting risk assessments, implementing a surgical site infection prevention bundle, warming the patient, and preparing for multimodal pain management by strategically targeting various physiological pathways,” says Spruce. “Multimodal analgesia aims to optimize pain control while minimizing the adverse effects associated with narcotic pain medications.”
The most important recommendations in the postoperative period are encouraging early patient mobilization and early return to a normal diet. “If a patient happens to have an indwelling catheter or drain placed, it’s important to remove these as soon as possible,” says Spruce.
One common obstacle to ERAS program implementation is variation in care driven by physicians’ strong personal preferences. “If organizations base their protocols on the best available evidence, they shift the focus toward the patient’s well-being and away from historical provider preferences,” says Spruce.
According to Karen Reiter, national vice president of ASC operations for TriasMD,
ambulatory surgery centers (ASCs) started using ERAS before hospitals identified it as a tool for better patient outcomes.
“Our centers perform complex spine surgeries and all patients go home in less than 24 hours,” says Reiter “We train our team members to keep their eye on discharge – every decision they make is to work toward an earlier discharge. In complex cases, patients are managed almost like they’re in the ICU. They are not ‘tucked in and lights out’ unless there is a doctor’s order that they are staying overnight for observation or extended care.”
“Surgery is evolving. With this evolution, perioperative teams members must remain vigilant in maintaining a culture of sharps safety to protect ourselves and one another.”
Educating patients and their families “early and often” is the key to achieving successful patient outcomes with ERAS, says Reiter.
“Upon admission, the family is present for education, and expectations around mobilization and discharge are reemphasized at this time. A family member remains with the patient throughout the duration in the ASC,” Reiter adds.
Reiter stresses the importance of getting surgeons onboard with ERAS. “Surgeons have to understand that we are keeping their patients moving through,” she says.
Spruce believes that ERAS will lead to a number of patient benefits, including shorter hospital stays, fewer postoperative complications, faster recovery, reduced readmission rates, lower costs and higher levels of patient satisfaction.
“Research around ERAS is ongoing and I think we will see more pediatric and special populations research coming out, in addition to more specialty specific protocols,” says Spruce. “ERAS is growing
around the world so there’s a lot to learn about implementation efforts in other countries as well.”
According to Karen deKay, MSN, RN, EBP-C, CNOR, CIC, FAPIC, AORN
Senior Perioperative Practice Specialist, updates were made to the surgical attire guideline to determine what are the best practices for surgical attire in the perioperative setting, as well as how surgical attire influences other factors that can lead to better or worse patient outcomes.
deKay lists the following primary changes to the surgical attire guideline:
• Form an interdisciplinary team to determine circumstances that may require perioperative personnel to change surgical attire when returning to the OR or procedural area after being in other areas of the building or outside building for short periods of time.
• Form an interdisciplinary team to determine if lanyards will be used in the perioperative setting. If so, develop and implement a process and schedule for routine disinfection.
• Develop and implement staff education to increase compliance with cleaning and disinfection of stethoscopes, cell phones and personal communication devices.
• Perform frequent hand hygiene when handling communication devices throughout the workday.
“By implementing these guidelines, healthcare facilities can reduce the introduction of potential pathogens into the perioperative environment from surgical attire, stethoscopes and personal items,” says deKay. “This will minimize a patient’s exposure to microorganisms that can contribute to an SSI.”
These guidelines will also prevent the introduction of pathogenic organisms that may adhere to scrub apparel during the workday from being brought into public places or the homes of perioperative personnel, adds deKay.
New research on sharps injuries and changing regulatory requirements, along with advancements in safety devices, led
to a review and update of the sharps safety guideline.
“Sharps safety remains of particular importance to all members of the surgical team because everyone is at risk,” says Emily Jones, MSN, RN, CNOR, EBP-C, AORN Senior Perioperative Practice Specialist. “Unfortunately, the data show that sharps injuries continue to occur in the perioperative setting.”
The new elements in the updated guideline for sharps safety include a new section about creating and sustaining an organizational sharps safety program to support safety throughout the organization where all members have a role to play.
“Experts agree that the institution has a responsibility to be fully engaged in a culture of sharp safety,” says Jones. “Leaders can support a non-punitive environment that creates a psychologically safe atmosphere to improve reporting of sharps injuries.”
In addition, there are new recommendations related to the process of selecting sharps disposal containers. At a minimum, sharps disposal containers must be:
• Closable,
• Puncture resistant,
• Leak proof on the sides and bottom,
• Labeled according to OSHA biohazard labeling requirement,
• Easily accessible,

• Located as close as possible to the immediate work area,
• Maintained in an upright position throughout use, and
• Replaced at a frequency to reduce overfilling.
To overcome potential resistance to changing how sharps are handled in the operating room, Jones recommends that leaders include surgical staff members as part of an interdisciplinary team to identify achievable solutions toward sustaining change. “For example, leaders can involve direct care staff members during device evaluation, implementation of sharps safety initiatives or competency verification activities,” she says.
“We recognize that surgery is ever evolving,” Jones adds “With this evolution, perioperative team members must remain vigilant in maintaining a culture of sharps safety to protect ourselves and one another.”
Updates were made to the patient temperature management guideline to prevent inadvertent patient hypothermia. For example, a new section was added to support facilities and teams in developing a patient temperature management plan for how they are going to tackle the issue of periop normothermia that includes prevention of hypothermia and malignant hyperthermia.
“We also created a sample Periop Normothermia Bundle so facilities don’t have to reinvent the wheel and start from scratch if they don’t already have
this in place,” says Renae Wright, DNP, RN, CNOR, EBP-C, AORN Senior Perioperative Practice Specialist. “In addition, we revised the recommendation language around active warming, prewarming and passive insulation to reinforce that active warming is more effective than passive insulation for raising patient temperature and treating hypothermia.”
Two new recommendations were also added to this guideline: to implement intraoperative warming according to the patient temperature management (PTM) plan, and to continue warming into the postoperative period while minimizing interruptions to warming. “These were added because we saw in the literature that inconsistent intraop warming practices and lengthy pauses in warming contributed to hypothermia,” says Wright.
Wright notes that the incidence of periop hypothermia reported in the literature ranges between 2% to more than 80% among different patient populations, depending on the degree of warming measures implemented.
“High-quality evidence supports using one or more active warming methods to prevent and treat hypothermia,” says Wright. “Which type or combination of active warming methods is most effective is still unclear because there’s a lot of variation in study methodology and results.”
“Remember that the purpose of this guideline isn’t so much to educate and inform or dispel misconceptions, but to make recommendations for practice,” says Wright.

A review and update of the packaging for sterilization guideline was prompted by the need to incorporate ergonomic concerns about packaging defects caused by personnel discomfort, as well as concerns about the use of peel pouches and the presence of holes in sterilization wrap and filters.
“In addition, there is a growing body of evidence on the use of quality improvement initiatives to identify and remove underutilized instrumentation from sets,” says Amber Wood, MSN, RN, CNOR, CIC, EBP-C, FAPIC, AORN Senior Perioperative Practice Specialist. “The goal of the updated guideline is to guide perioperative teams on evaluating and using sterilization packaging systems in a manner that protects the integrity of the sterilized contents until delivery to the sterile field.”
When selecting and using packaging materials, perioperative teams should incorporate ergonomic features into the design of the sterile processing area.
“For example, work surfaces should be at a comfortable height, lighting should be adequate, anti-fatigue flooring or mats and adjustable seating (such as sit-stand stools) should be used, and there should be adequate space for the performance of tasks,” says Wood.
All single-use sterilization wrap and filters should be inspected for defects before use. “There is also new guidance for using quality improvement initiatives to identify and remove underutilized instrumentation from sets,” says Wood.
In addition, recommendations for the use of peel pouches were enhanced to emphasize the correct use of pouches. “This includes verifying that all seals are completely closed and smooth without gaps, folds, bubbles or wrinkles, and using heat sealers according to the manufacturer’s instructions for use,” says Wood.
The updated packaging for sterilization guideline is expected to highlight important recommendations to reduce the risk of packaging defects that could compromise the sterility of the package and increase patients’ risk for infection.
“As new sterilization technologies and materials are developed, this guideline will continue to evolve and update perioperative teams on the latest developments and evidence-based practices for selection and use of sterilization packaging systems,” says Wood.
A review and update of the sterilization guideline was prompted by the need to incorporate guidance for sterilizing devices produced by additive manufacturing (e.g., 3D printing), the practice of short-cycle sterilization, procedures for transportation of sterilized items between facilities, and updated recommendations for water quality monitoring in ANSI/AAMI ST108:2023.
According to Wood, the updated sterilization guideline is intended to help perioperative teams achieve more effective and reliable sterilization processes that will reduce the patient’s risk for infection.
The update adds a definition for short-

cycle sterilization: “A sterilization method for a wrapped or contained load that is sterilized in accordance with the device, sterilizer and packaging manufacturer’s instructions for use; includes a dry time; and is packaged in a sterile barrier that permits storage for use at a later time.”
“This addition was needed to address this as a commonly used term and practice in ophthalmology centers,” says Wood. “It aligns with the CMS definition.”
Wood says the updated sterilization guideline continues to stress the importance of using physical monitors and chemical and biological indicators to monitor sterilization processes. “We added a table based on a request during public comment to help readers quickly identify the recommended frequencies for routine sterilizer efficacy testing for various sterilization methods,” she says.
The update also adds a new recommendation, in alignment with ANSI/ AAMI ST108, for routinely monitoring the quality of water systems that supply steam generators (e.g., boilers). “This is important because the quality of the incoming water supply is a major factor influencing steam quality and purity,” says Wood.
To learn more about the Guidelines for Perioperative Practice, including purchase and subscription options, visit https://info. aorn.org/GuidelinesBook2025.



CIRCULATING COOLING SYSTEMS FOR OPERATING ROOMS & MEDICAL FACILITIES

CoolOR® IS FULLY STOCKED AND READY TO SHIP WITHOUT DELAY.
Are your surgeons feeling the heat in the operating room?
The CoolOR® Circulating Water System is a game-changer in surgical comfort. Here’s why it’s a must-have for your team:
• CONTINUOUS COOLING
• WATER-TIGHT RESERVOIR
• QUICK-CONNECT COUPLINGS
• INSULATED WATER LINES
• PORTABILITY
Because comfort matters. Contact us today to explore our high-quality water circulating systems and experience the difference firsthand!



Two highly anticipated conferences for perioperative nurses are set to take place in 2025, offering education, networking, and an opportunity to connect with peers in the field.
Connect 2025: Elevating the Perioperative Experience
The Periop Connect 2025 conference will be held on October 11-12, 2025, at the Omni New Haven Hotel at Yale. This event will bring together leading experts and professionals from across the perioperative community to discuss the latest trends, challenges, and innovations in the field. Registration details will be available soon, and the Call for Presenters is now open. Those interested in presenting at the conference are encouraged to submit proposals at periopconnect.com/call-for-presenters. Attendees will have the opportunity to learn from renowned experts and network with other professionals, fostering growth and collaboration in the perioperative field. This conference aims to provide attendees with the tools and insights needed to continue improving patient care and advancing their careers.
The Southeast Councils of AORN will hold their 2025 conference on November 1-2, 2025, at the World Golf Village Renaissance in St. Augustine, Florida. Building on the success of their inaugural conference in 2024, this year’s event will celebrate “The Power of You: Circles of Care.” The 2024 conference saw groundbreaking achievements, including the merging of North and South Carolina Councils, the introduction of bills mandating the evacuation of surgical smoke in Florida and South Carolina, and the
selection of two Southeast nurses to receive Daisy Awards.
In 2025, the conference will continue to focus on the collective power of perioperative nurses. Attendees will explore the critical role nurses play in advocating for patients and their colleagues. The theme “Circles of Care” will highlight how perioperative nurses create safe, supportive environments for patients and each other, ensuring high-quality care through every procedure.
This year’s event will also mark the inclusion of Tennessee as the newest state joining the conference, further emphasizing the strength of collaboration. Organizers are aiming for an even larger turnout in 2025, with more exhibitors, attendees, and presentations. Registration details will be released closer to the event. For more information on both
and speaker opportunities, please visit the official event websites.
Periop Connect is a key gathering for perioperative professionals to share knowledge and collaborate on advancements in patient care. The conference offers cuttingedge education, networking opportunities, and practical resources for those working in the perioperative field.
The Southeast Councils of AORN brings together perioperative nurses from multiple states to enhance patient safety, foster collaboration, and advance the profession. The annual conference has become a key event for education and advocacy, empowering nurses to make a difference in their practices and
Date: October 11-12, 2025
Location: Omni New Haven Hotel New Haven, CT
Join perioperative professionals throughout Connecticut and the Northeast for CEaccredited education, exhibits with leading vendors, and great networking events.


Date: November 1-2, 2025
Location:
World Golf Village Renaissance St. Augustine, FL

This year’s event will celebrate “The Power of You: Circles of Care.” The conference will focus on the collective power of perioperative nurses. Attendees will explore the critical role nurses play in advocating for patients and their colleagues.

The operating room is one of the most dynamic and challenging work environments imaginable. As a result, most experienced perioperative nurses are used to dealing with unpredictability and change, as well as assuming new responsibilities and wearing lots of different hats.
This is even more pronounced at a critical access hospital. These were established in 1997 to provide service in rural areas where patients might otherwise have to drive long distances to receive emergency care.
Elaine Geroski is the assistant vice president of patient services and chief nursing officer at West Virginia University Medicine Grant Memorial Hospital, a critical access hospital in Petersburg, W.V.
“At a critical access hospital, you’re not limited to just one role,” Elaine says. “You have to wear multiple hats because the role requires extensive collaboration across all the units. This is

one of the things that I find so rewarding about my job.”
Elaine has been a perioperative nurse for the past two decades, working in a wide variety of different hospital environments. Her roles have included operating room and PACU RN, director of surgical services, senior director of perioperative services, operating room nurse educator, clinical manager, vice president of nursing, and director of workforce development.
Perioperative nursing was hard to break into 20 years ago because new nurses weren’t hired directly into the OR.
“You had to work as a floor nurse first,” she says. “I was working in a unit at a hospital that was being closed and they told us we could apply for any position except the OR. Well, I applied for the OR anyway – and I was accepted! I had a wonderful mentor who was willing to give me a chance, and I soon discovered that perioperative nursing was what I loved.”
Elaine believes that perioperative nursing requires more advanced
technology skills and the ability to solve problems quickly. “Sometimes you only have a split second to deal with issues that come up,” she says. “And you have to fix equipment on the fly because everybody else usually is scrubbed in and can’t scrub out.”
Perhaps the biggest thing that sets perioperative nursing apart is the fact that OR nurses are responsible for speaking up for patients who are under anesthesia and unable to speak for themselves.
“This is a special gift because OR patients will never know what you did to protect them,” Elaine says. “I think this is very rewarding, but if you want to hear accolades from patients, then perioperative nursing probably isn’t for you.”
Elaine encourages other perioperative nurses to speak up for patient safety.
“Don’t be afraid to ask questions if something doesn’t look quite right,” she says. “The power of the perioperative nurse can change a patient’s outcome.”
One of the biggest changes Elaine has seen over the past two decades in the
“The power of the perioperative nurse can change a patient’s outcome.”
OR is the respect that is shown to all members of the perioperative team.
“Disrespect and bad behavior simply aren’t tolerated in the OR anymore,” she says. “I once had a scope thrown at my head early in my career at a different organization, but things have changed since then. I don’t see this kind of thing happening anymore. Every surgeon I work with is civil and teamwork-oriented.”
When Elaine became a director of perioperative services, she says she noticed that some standards “weren’t being followed to a T. By properly implementing these standards, we saw a 75% reduction in surgical site infections. I wanted to do more so I got my CSSM certification, which enabled me to volunteer to be a part of the Competency & Credentialing Institute (CCI). In addition to my CNOR certification, I became one of the first 100 people credentialed to be a certified surgical services manager.”
Elaine applied for a position on the CCI board of directors and was elected in 2018. Then she was elected president of the CCI board in 2021, serving in this role for three years –the longest tenure of any CCI board president.
“Volunteering on the CCI board has been invaluable to my perioperative career,” she says. “I’ve learned so much about certifications and credentialing bodies. But the most valuable part has been the collaboration with other entities.”
During her last year as president, the CCI board focused on working closely with the Association of periOperative Registered Nurses (AORN) to make sure they were one unified voice.
“In the past, I didn’t think we
were representing ourselves as a united front,” she says. “But that has changed now, and I’m very proud of this.” Elaine says her time on the CCI board, including her three years as president, represents some of the most rewarding work of her career.
In recognition of all the accomplishments in her perioperative career, Elaine received the DAISY Nurse Leader Award in 2024. The DAISY Foundation was established in 1999 by Tena Barnes Carraher after her husband Patrick Barnes died from complications of the auto immune disease ITP. Tena and her family wanted to recognize the tremendous care and compassion Patrick’s nurses brought to him and their family during his illness.
Elaine is proud of her hospital’s five-star CMS rating for patient safety, nurse responsiveness and overall quality. In addition, WVU Medicine Grant Memorial Hospital was ranked #27 in the country by Money.com for delivering safe, high-quality patient care and patient experiences.
“I think this speaks volumes about every nurse, technician and provider in our facility,” she says.
To relax and unwind outside of work, Elaine refurnishes antique furniture.
“This is a real stress-reliever for me,” she says. “I’m constantly looking for pieces for my next project, which tends to clutter up my basement.”
Rather than sell refinished pieces, Elaine keeps them in her home. “It’s hard to let go of pieces after I’ve put so much time and effort into refinishing them,” she says. Before





By Family Features
Research conducted by YouGov on behalf of Siemens Healthineers¹ reveals Americans’ devotion to football fandom could put their heart health at risk. According to the survey, roughly 1 in 5 Americans (21%) would hesitate to leave a professional sporting event to go to the hospital if they suspected they were having a heart attack. Among American football fans, however, 28% would hesitate to leave a professional sporting event to go to the hospital if they suspected they were having a heart attack. This number only declined to 19% among football fans who themselves have already visited the ER with symptoms of a heart attack.
The survey of more than 1,000 U.S. adults sought to pulse check Americans’ worry about heart attacks, whether they would be interested in learning more about their risk of heart attacks, and the likelihood they would act on information about that risk.
The survey revealed that more than half of Americans (54%) have, or know someone who has, visited the emergency room with suspicions of a heart attack. When asked who they worry about having a heart attack within the next year, 49% indicated they are worried about a family member having a heart attack and 35% are worried about having a heart attack themselves. Yet, when it comes to attending professional sporting events, many of the devout football fans indicate they would leave their worry at the gates.
“Americans may not know the importance of acting quickly when heart attack symptoms begin. It’s important to seek help as soon as possible if you suspect you might be having a heart attack to minimize heart muscle damage – there can be severe consequences for waiting,” said Ian Lentnek, MD, cardiologist, and medical affairs director at Siemens Healthineers. “As blood flow to the heart is blocked, heart muscle tissue begins to die. Significant damage can occur in less than an hour, so don’t wait to seek medical attention if you suspect you might be having a heart attack.”
The survey also indicates Americans would welcome more information about their risk of having a heart attack. Just over two-thirds of Americans (67%) would want to know if they are at risk of
having a heart attack within the next year. Having information about their risk might also lead to behavior change: 75% of Americans agree that if they had information about their future heart attack risk, they’d be more compelled to make necessary lifestyle modifications to reduce their risk.
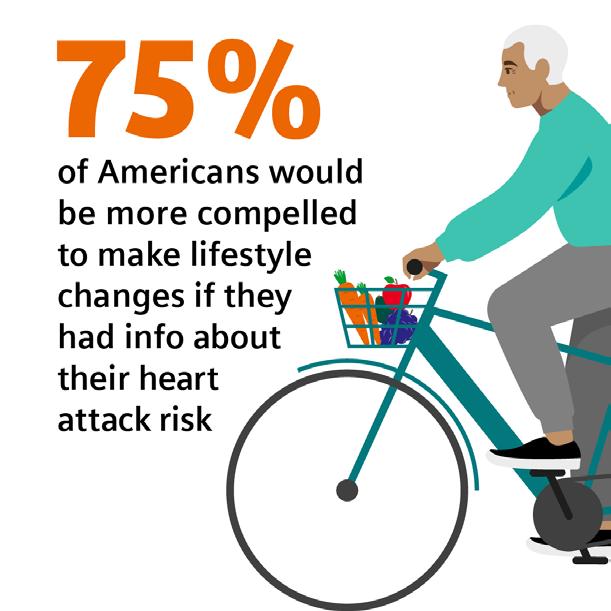
“These findings mirror Americans’ growing interest in having information about their health that they can act on,” said Lentnek. “The good news is this predictive risk assessment is possible. A blood test used in ERs across the country can help assess patients’ risk of cardiac events for up to a year. Offering patients data-backed information about their risk could improve how patients respond to clinician recommendations such as seeking immediate medical attention if they experience symptoms –chest pain or shortness of breath, for example.”
The test Lentnek refers to is the Atellica IM HighSensitivity Troponin I (TnIH) blood test, developed and manufactured by Siemens Healthineers. TnIH is part of the routine evaluation for patients presenting to the ER with
symptoms of a heart attack. It now can help patients who are not having a heart attack as the only high-sensitivity troponin I blood test available in the U.S. that can be used as a prognostication tool.² For patients, this means their test results can now also help assess their impending risk of a major cardiac event or death within the next 365 days.
1. All figures, unless otherwise stated, are from YouGov Plc. Total sample size was 1118 adults. Fieldwork was undertaken between 12th - 13th December 2024. The survey was carried out online. The figures have been weighted and are representative of all US adults (aged 18+).
2. Results now can be used as an aid in prognosis for 30-, 90-, 182-, and 365-day all-cause mortality and major adverse cardiac events (MACE) in patients presenting with signs and symptoms suggestive of acute coronary syndrome (ACS). This claim applies to the Atellica IM TnIH assay and is intended for U.S. audiences only.

By Miguel J. Ortiz
The best exercise equipment you will find in any gym will always be your body. So, technically speaking, you may not need the gym. It depends on your goals, but the like-minded motivation and assistance from a fitness professional can help tremendously. Your body is an incredible tool, and you can learn a lot from it, if you’re paying attention.
So, what are some good movement patterns to do at home and how can we use them to help us with our goals? Let’s start with 7 basic movements patterns – squat, lunge, bend, rotate, gait, push and pull. Let’s look at how these movements assist in some quality workouts as well as help direct attention to some needed areas.
When you hear the word gait, that
means it’s a cyclical movement pattern, think cardio. Running, rowing, jump rope, bicycle riding, elliptical, swimming, etc. are all examples of gait movement patterns. This movement pattern is great for a warmup, general calisthenics, a long run or a cool down. It is a common goto for all exercise enthusiasts.
The squat is by far one of the most important movement patterns. So, do you know who has the best squats? Most people wouldn’t guess this, but children have the best squat pattern. Why? Because they learn to pick everything up using their legs. Bending over to pick things up only starts to occur when we get lazy or a lack of activity has started to become prevalent. We sit and use our legs every day, so this movement pattern is never something to ignore.
Next, let’s look at the lunge. Depending on the person, a lunge can
be a little advanced. You might need some assistance. If you are practicing lunges at home, you might want to start stationary or simply do a step-up. This can assist with future lunge patterns and more advanced movements as you progress.
Bend or hinge movements will cover two different categories. It is very important to understand how to separate the two. It’s perfectly fine for your back to bend, but take caution as you don’t want to be bending during heavy strength movements as injury may occur. Most of your other bend movements will happen during stretching, yoga, core, crunches, leg lifts and Pilates exercises.
Rotate is another movement pattern that will cover a lot of core exercises and the same concepts need to be applied when keeping the back straight. A good example would be a plank rotation or
a V-sit twist. Both exercises are in a stationary position, both require you to keep your back straight and deal with rotation.
Push and pull movements are next on the list. These are pretty self-explanatory as you are either pushing away or pulling something toward you. Push-ups, shoulder press (push) and triceps push downs are good push examples. Pull examples are pull-ups, bicep curls (pulls) and rows.
So, now that we reviewed all our movement patterns, let’s put them together and try a fun little home workout. I suggest three rounds of the following.
1. 20 air squats
2. 10 push-ups
3. 20 lunges
4. 20 leg lifts
5. 30 jumping jacks
6. 40 bicycle crunches
Have fun with your home workout and don’t be afraid to take these exercises outside. Want to mix it up with your normal jogging routine? Well, maybe you decide to do 5 pushups or 10 squats every 10 minutes of running and see what that will do to your workout.
Enjoy your body for its ability to be pushed to the limit and never doubt yourself. You will never know what you can accomplish until you try.
we’re on instagram!


OUT OF THE OR fitness





By Grace O

W e’re well into spring, so presumably your mood has already lifted from a couple of months ago. But it certainly makes sense that what you eat has lots to do with how you’re feeling about yourself and the world.
With longer hours of sunshine (which helps your body use vitamin D for bone health) and the bounty of spring fruits and vegetables available, it’s easy to avoid nutritional deficiencies that increase inflammation within the body, which can contribute to a number of maladies and diseases.
For example, there is evidence that depression can be caused by a low-level inflammatory disorder or a deficiency of certain nutrients. By making some lifestyle changes such as increasing exercise and avoiding sugar, highly processed foods, and simple carbohydrates, you can lift your mood and reduce inflammation
that can lead to chronic health issues such as heart disease, metabolic disorders, and even cancer.
Adding supplements to your regime, such as B-complex vitamins, and eating unsaturated omega-3 fats with a diet of antioxidant-rich foods like salmon, turmeric, green tea, leafy greens, and broccoli can give a boost to your health and outlook.
I’ve compiled a list of FoodTrients foods that can enhance not only your health but your moods and added information on what they do for your mind and body:
Salmon and shrimp – Excellent sources of protein and Omega-3 fatty acids to enhance brain health.
Tomatoes and watermelon – Their red color means they’re both full of lycopene, which helps prevent the formation of inflammatory compounds that can contribute to poor mood.
Chili peppers – Capsaicin in chilis helps reduce inflammation in the
body and brain.
Beets, spinach, edamame, beans, and lentils – These contain high levels of folate, which supports cognition and a good mood.
Garlic – Chromium and other compounds present in garlic act as natural mood stabilizers.
Fresh fruits and vegetables – Full of vitamins and minerals, the fiber in produce promotes good gut health and feelings of well-being.
The great news is that moodboosting foods feature in scores of delicious dishes that you’ll enjoy while doing your mind and body a favor. Here is a great warmer weather recipe to try that will enhance your mood.
– Grace O is the creator of FoodTrients, a unique program for optimizing wellness and longevity. She is the author of three awardwinning cookbooks. Her latest cookbook is “Anti-Aging Dishes from Around the World.” Learn more at FoodTrients.com/recipes/ anti-inflammatory.

The look of this dish alone is enough to make your eyes dilate with anticipated pleasure! The shrimp is a great source of protein and omega-3 fatty acids. The cabbage, a cruciferous vegetable, provides tryptophan and selenium, which relax your body and mind. Purple cabbage has 10 times the vitamin A of green cabbage. It also contains antioxidants, and a good amount of vitamin C. Mangoes are a superfood, containing over 20 different vitamins and minerals. ¾ cup of mango provides 50 percent of the RDA for vitamin C and a small but significant amount of your daily Vitamin A and vitamin B6.
Ingredients
For the Dressing:
• 3 Tbs. plus 1 tsp. rice wine vinegar
• 1 tsp. coconut aminos or tamari
• 1 tsp. soy sauce
• 2 tsp. pure maple syrup
• 1 tsp. grated fresh ginger
• 2 cloves garlic, grated or minced
• 1/2 tsp. Chinese 5-spice powder
• 1/8 tsp. sea salt
• 1/3 cup avocado oil
• 2 tsp. toasted sesame oil
For the Slaw and Shrimp:
• 2 mangoes, cut into chunks
• 6 radishes, thinly sliced
• 3 carrots, grated or peeled into ribbons
• 1/2 head purple cabbage, finely shredded
• 1/4 cup chopped fresh cilantro or Thai basil
• 2 tablespoons avocado oil
• 1 clove garlic, minced
• 1/2 tsp. Chinese 5-Spice powder
• 2 tsp. sesame seeds
• 1/4 tsp. sea salt
• 1/4 tsp. freshly ground pepper
• 1/2-3/4-pound large shrimp, peeled, deveined, tails left on
• 4 green onions, thinly sliced
1. Make the dressing: Whisk together the first eight ingredients (vinegar through salt). While whisking, slowly drizzle in oils until fully combined. Set aside.
2. In a large bowl, toss together mangoes, radishes, carrots, cabbage, and cilantro (or Thai basil). Drizzle with dressing, toss and allow vegetables to marinate for 20 minutes. Taste, and adjust seasoning.
3. In a medium bowl, whisk 2 Tbs. avocado oil, garlic, Chinese 5-spice powder, sesame seeds, 1/8 tsp. salt, and ¼ tsp. pepper. Add shrimp and toss to coat.
4. In a large skillet over medium-high heat, sauté shrimp for about 4 minutes or until cooked through. Divide slaw among serving plates, top with shrimp, and garnish with green onions and more sesame seeds.
– Grace O is the creator of FoodTrients, a unique program for optimizing wellness and longevity. She is the author of three award-winning cookbooks. Her latest cookbook is Anti-Aging Dishes from Around the World. You can find more age-defying recipes at Foodtrients.com/recipes. Recipes and photos reprinted with permission of FoodTrients.com.
• Butter
• 36 thawed tater tots
• 10 eggs
• 1/2 cup heavy whipping cream or half-and-half
• 1/2 cup shredded cheese
• 2 teaspoons garlic powder
• 2 teaspoons onion powder
• 1 package (2 1/2 ounces) real bacon pieces
• salt, to taste
• pepper, to taste

By family features

M ornings for many families involve hurried breakfasts and mad dashes out the door. These Egg Tot Muffins can help take that grab-and-go breakfast to the next level. High in protein and flavor, they are a good way to get rid of early morning brain fog. Plus, you can make them ahead of time so all you have to do is pop them in the microwave and enjoy on the go. Find more morning meal inspiration at Culinary.net.
Egg Tot Muffins Serves: 12
1. Heat oven to 350 F.
2. Grease muffin tin with butter. Place three tots in each muffin hole and smash down.
3. In bowl, whisk eggs, cream, cheese, garlic powder, onion powder and bacon pieces. Season with salt and pepper, to taste. Fill each muffin hole completely with mixture.
4. Place cookie sheet under muffin tin to contain messes and bake 20-25 minutes.
Breakfast is the most important meal of the day as it jumpstarts metabolism, boosts energy, and improves focus. A balanced morning meal supports health, curbs overeating, and sets the tone for a productive day.
By Daniel Bobinski, Th.D.
Life is usually a game of whack-a-mole. You handle one problem and two more pop up. Add the aspect of highpressure decisions and the stress gets real, creating what feels like an emotional minefield.
Two of the biggest players in this arena are gratitude and resentment. If you aren’t already aware, one makes you stronger while the other eats you from the inside. But the good news is you get to choose which one wins.
THE DANGER OF RESENTMENT
Let’s hear the bad news first. Resentment is a sneaky little emotion that creeps in when we feel slighted or unappreciated. It might start with some small event, such as someone else getting credit for our work or someone lashing out at us despite our best efforts. If we don’t forgive and move on, it’s easy to let those moments simmer and boil up to feelings of resentment.
The problem with resentment is that it doesn’t just sit quietly. Before long, it starts seeping into our conversations. This can lead us to being short with others or bitter about policies, and before we know it, we’re caught in a cycle of negativity that poisons our interactions and drains our motivations.
The real downer is that every moment we spend in resentment is one
less moment for us to enjoy peace of mind.
The gratitude antidote
You might not realize it, but there’s actually power in gratitude. Instead of dwelling on what went wrong, if we choose to be grateful for what went right and for whatever learning occurs, we actually gain benefits.
Research shows that gratitude improves our resilience, boosts our mental health and strengthens our abilities to be good collaborators. In other words, if we make a habit of recognizing and being thankful for the good going on around us, we train our brains to see opportunities for success and growth.
Imagine two professionals working the same grueling shift. One is consumed with frustration, saying things like, “I always get the toughest assignments,” or “No one ever appreciates what I do.” But the other says things like, “That was a tough case, but thankfully, we handled it well,” or “Despite the obstacles, the team really did a great job today.”
Same job. Same stress. Completely different attitudes.
Choosing gratitude
How can we make gratitude our default? Allow me to offer a few thoughts.
Pause and reflect. Before ending your
workday, take 30 seconds to identify at least one thing that went well and give thanks for it.
Acknowledge others. A daily “thank you” to a colleague builds bridges. Reframe challenges. Instead of saying, “Why do I always get the hard assignments?” try, “I’m glad I have the skills to handle tough situations.”
Bottom line, life will always resemble whack-a-mole, but what can change is our response. Resentment keeps us stuck, and even weighs us down. But having gratitude and being thankful helps us navigate challenges with a clear head, and that leads to peace of mind.
Daniel Bobinski, is a best-selling author and a popular speaker at conferences and retreats. For more than 30 years he’s been working with teams and individuals (1:1 coaching) to help them achieve excellence. He was also teaching Emotional Intelligence since before it was a thing. Reach him by email at DanielBobinski@protonmail.com or 208-649-6400.











































































