PAGE 24 DECEMBER 2022 LIFE IN AND OUT OF THE OR 21 MARKET ANALYSIS Carts, Cabinets Markets Expected to Grow 28 SPOTLIGHT ON Terry Jones, Ph.D, RN 20 CCI Changes in Perioperative Leadership 38 SCRAPBOOK Georgia Council of periOperative Registered Nurses


Can’t get to that tray of dirty surgical instruments? NO WORRIES! GET WET STAY WET FOR 72 HOURS For More Information and GENEROUS FREE SAMPLES 1-800-537-8463 • WWW.RUHOF.COM 393 Sagamore Avenue, Mineola, New York 11501 Tel: 516-294-5888 • Fax: 516-248-6456 An ISO Registered Firm Ruhof’s Prepzyme Forever Wet Pre-treatment an enzymatic pre-treatment humectant spray, will keep your instruments and rigid scopes moist for up to 72 hours - preventing organic debris from drying and hardening, making cleaning easier! Copyright ©2020 Ruhof Corporation
Prepzyme® Forever Wet creates a long lasting moisture barrier. As seen here, instrument remains wet to the touch for days after application.
INSTRUMENT TRANSPORT
HUMECTANT SPRAY
The latest breakthrough in enzymatic pre-cleaning sprays, Prepzyme® Forever Wet’s unique humectant properties form a moist coating over the instruments that lasts for days.
• The humectant formulation creates a moisture retention barrier which keeps soiled instruments and rigid scopes moist for a prolonged period of time – unlike a GEL which HAS NO MOISTURE RETENTION properties
• Operating room safe, non-aerosol, multi-tiered enzymatic spray helps prevent bio-burden from drying on the surface of soiled instruments and scopes

• Ideal for transporting soiled instruments that may sit for an extended period of time

• Reduces tray weight during transport compared to liquid presoaks

• Soiled sharps are visible through humectant
• Decreases spills and potential cross-contamination
Prepzyme® Forever Wet
AD-63 112320















ENVIRON-MATE® DM6000 SERIES CALL US BEFORE YOU BUILD OR REMODEL! 800-201-3060 Utility/SPD DM6000-2 Endoscopy Systems require plumbing most conveniently installed during new construction or remodeling. Eliminate staff exposure Reduce turnaround time y Screw top minimizes risk of C. Diff. 30” PROMETHEAN ISLAND® 4400 FLOOR MAT • Collect fluids before they reach the floor • Accurately measure spilled irrigation fluids • Reduce post-op clean-up/turnaround time Pays for itself in one year! Save canister & solidifier costs Check cost saving on our website Use the DM6000 for your project! • Surgery, endoscopy, SPD • Requires vacuum, electrical & drain ELIMINATE THESE! 46” Optional Fluid Totalizer DM6000-2A Arthroscopy Urology FM99 FILTER/MANIFOLD PROVIDES 4 CONNECTIONS FOR SCOPE, SHAVER AND FLUID COLLECTORS. 500CC CAPACITY! P.O. BOX 60 • GALENA, ILLINOIS 61036 PH: (815) 624-3010 • FAX: (815) 624-3011 www.mdtechnologiesinc.com
HMARK.COM
800.521.6224

25lb. Weight Capacity
SOLUTIONS
CARE
INTELLIGENT
FOR INSTRUMENT
& INFECTION CONTROL
for post-procedure transportation of contaminated instruments
procedure areas
the decontamination area Conveniently Transport Contaminated Instruments with the Disposable SST Tray System Manufactured from 100% Recycled Plastic Clear for Easy Identi cation Printed with Biohazard Symbol Reliable for Safe Transport
|
For more of Healthmark’s protection equipment solutions, including a full line of protective attire, visit hmark.com Designed
from
to
21 MARKET ANALYSIS
Mordor Intelligence reports that the medical carts market is expected to reach $1.8 billion by 2027.




OR
(Vol.
FOCUS
SURGICAL SMOKE UPDATE

More and more states are considering protecting patients and health care professionals from surgical smoke in the operating room.
#12)
24
OR TODAY | December 2022
Today
22, Issue
December 2022 is published monthly by MD Publishing, 1015 Tyrone Rd., Ste. 120, Tyrone, GA 30290. POSTMASTER: See address changes to OR Today at 1015 Tyrone Rd., Ste. 120, Tyrone, GA 30290. For subscription information visit www.ortoday.com. The information and opinions expressed in the articles and adver tisements herein are those of the writer and/or advertiser, and not necessarily those of the publisher. Reproduction in whole or in part without written permission is prohibited. © 2022 38 SCRAPBOOK The Georgia Council of periOperative Registered Nurses teamed up with OR Today for the second consecutive year to host its annual meeting. 22 PRODUCT
A look at medical carts and cabinets from some of the top perioperative suppliers.
6 OR TODAY | December 2022 WWW.ORTODAY.COM
contents features





INDUSTRY INSIGHTS 8 News & Notes 14 HSPA: Revised Guideline for Processing Flexible Endoscopes: Key changes for SP staff 16 AAMI Roundup 18 The Joint Commission: Assessing Life Safety Compliance 20 CCI: Changes in Perioperative Leadership IN THE OR 21 Market Analysis: Carts, Cabinets Markets Expected to Grow 22 Product Focus OUT OF THE OR 28 Spotlight On: Terry Jones 30 Health 31 Fitness 32 EQ Factor 34 Nutrition 37 Georgia Council Meeting 38 Scrapbook 40 Recipe 42 Index MD PUBLISHING | OR TODAY MAGAZINE 1015 Tyrone Rd., Ste. 120 Tyrone, GA 30290 800.906.3373 | Fax: 770.632.9090 Email: info@mdpublishing.com www.mdpublishing.com PROUD SUPPORTERS OF 28 SPOTLIGHT ON Terry Jones, Ph.D, RN 40 RECIPE OF THE MONTH Sumac-Crusted Filet Mignon with Honey-Lemon Glazed Carrots and Garlic Mashed Potatoes contents features PUBLISHER
M. Krieg john@mdpublishing.com VICE PRESIDENT Kristin Leavoy
EDITOR John Wallace editor@mdpublishing.com ART DEPARTMENT Karlee Gower Taylor Hayes Kameryn Johnson ACCOUNT EXECUTIVES Jayme McKelvey Megan Cabot Emily Hise DIGITAL SERVICES Cindy Galindo Kennedy Krieg EVENTS Kristin Leavoy ACCOUNTING Diane Costea WEBINARS Linda Hasluem
BOARD Hank Balch, President & Founder, Beyond Clean
Dennis, MSN, RN, CNOR, CMLSO, Assistant Vice President, Perioperative Services with AnMed Health System
A.
OR Dx + Rx Solutions for Surgical Safety
34 NUTRITION A Ferment Built for Winter December 2022 | OR TODAY 7 WWW.ORTODAY.COM
John
kristin@mdpublishing.com
EDITORIAL
Vangie
Sharon
McNamara, Perioperative Consultant,
Julie Mower, Nurse Manager, Education Development, Competency and Credentialing Institute David Taylor, President, Resolute Advisory Group, LLC Elizabeth Vane, Health Science Teacher, Health Careers High School
INDUSTRY INSIGHTS
Study Looks at a Better Solution for Surgical Site Dressings
DrySee, a medical technology company dedicated to improving wound care, created the first patented wound dressing that will change colors to indicate it should be changed. DrySee was the focus of a new clinical study published in the September issue of Journal of Wound Care . Results concluded that com pared to gauze or a 3M Tegaderm + Pad transparent film dressing, 75% of patients preferred the Dry See wound dressing. The DrySee dressing also had a greater wear time and patients reported that it stayed in place better during activities.
DrySee wound coverings have many uses, but the study was acutely focused on the potential to reduce surgical site infections (SSIs). According to the CDC, SSIs have an estimated annual cost of $3.3 billion and they are the leading cause of rehospitalization follow ing a surgery.
DrySee’s liquid indicating, waterproof bandages provide a secure, waterproof covering for low exudate wounds. If water or other liquids make their way into the bandage, the gauze barrier around the perimeter of the bandage will turn from a light blue to a dark blue

color. The color change alerts the user to change the bandage, knowing that the perimeter seal is broken. If liquid passes through the second adhesive ring and reaches the wound site, or if the wound seeps fluid or exudate, the internal gauze pad will turn a dark blue color, alerting that a bandage change is necessary.
“Showering and other daily living activities after a surgery can dislodge a wound dressing, but patients may not notice that the wound site has been exposed to potential contaminants that could lead to an infec tion,” said DrySee CEO Brad Greer. “DrySee wound dressings make it simple for patients to know, with a visual cue, if their wound is secure, and this technol ogy could radically change the health care system for the better. Not only can it help reduce unneces sary costs and hospital stays, DrySee dressings could improve patient quality of life and could even poten tially help prevent mortalities caused by surgical site infections.”
DrySee liquid indicating bandages are waterproof, sterile, disposable, breathable, non-latex, made in the USA and are available in three sizes.
news
& notes
8 OR TODAY | December 2022 WWW.ORTODAY.COM
Lazurite, Minnetronix Medical Make New Wireless Surgical Camera a Reality
































Lazurite and Minnetronix Medical have announced that the ArthroFree Wireless Surgical Camera System has achieved its final major milestone on the way to market: its first successful human use and the completion of its transfer to manufacturing. ArthroFree is the first wireless surgical camera system to receive FDA market clearance for arthroscopy and general endoscopy.
Lazurite, a developer of medical devices, worked with orthopedic surgeon Dr. Laith Jazrawi at NYU Langone Orthopedic Center to perform the first surgery using the ArthroFree wireless camera on September 13. In the coming weeks, additional surgeries will be performed at NYU Langone and other leading orthopedic centers us ing the system, which enables real-time, high-quality im ages without the intrusion of cords. Minnetronix scaled the manufacturing of ArthroFree from early pilot builds to market-ready production at its expanded new product introduction facility.
The camera is another “first” from the Minnetronix optics team, which specializes in designing, developing, manufacturing and commercializing complex optical systems. The Minnetronix team was integral to reducing
latency and enhancing image quality for the ArthroFree System, including development of an innovative image signal processing chain, the path an image takes to travel from initial capture on a sensor to a screen. Minnetronix also aided in development of the device’s light engine and mastered the production of its complex handpiece, increasing production speed and efficiency by develop ing a modular strategy of batch assembling subassemblies and finishing assembly inside a clean room.
news
Visit ort.touchpointmed.com or call 800 947 3901 to learn about TouchPoint Medical’s carts and workstations. POWERFUL ANESTHESIA CARTS The complete system for managing your anesthesia supplies. Coming soon with new intelligent features including enhanced security and inventory control. Support Multiple Workflows Improve Productivity Trusted Security Options
INDUSTRY INSIGHTS
& notes
December 2022 | OR TODAY 9 WWW.ORTODAY.COM
Stryker Launches Q Guidance System with Spine Guidance Software

Stryker has unveiled its Q Guidance System for spine applications. The system combines new optical track ing options provided by a redesigned, state-of-the-art camera with sophisticated algorithms of the newly launched Spine Guidance Software to deliver more surgical planning and navigation capability than ever before. When used with the Q Guidance System, the Spine Guidance Software is intended as a planning and intraoperative guidance system to enable open or percutaneous computer-assisted surgery and is the first spine navigation software to receive FDA clearance for use with pediatric patients 13 and older.
“The Q Guidance System offers cutting-edge track ing options with its 4th generation FP8000 camera, and Spine Guidance Software allows for advanced planning and computer-assisted execution,” said Rob bie Robinson, president of the spine division. “With the addition of the Q Guidance System, customers now have access to a robust solution that includes imaging, guidance and instruments and is fully inte grated and designed to meet complex customer needs. In the years to come, our goal is to use the versatility of this system to help advance our technologies across multiple specialties including cranial, spine, ENT and orthopedics.”
Q Guidance offers surgeons numerous benefits, ac cording to a press release, including:
• A proprietary camera: The Q Guidance System features a fourth generation FP8000 camera that offers unmatched speeds and the flexibility of multiple opti cal tracking methods, including full-spectrum active/ passive hybrid optical tracking. It is the only guidance system with proprietary active technology and a noninvasive patient tracker, SpineMask.
• Image processing: Spine Guidance Software features completely redesigned applications, semiautomatic and automatic processing features, gesture recognition and broad compatibility with various types of image sets.
• Spine Guidance Software: Spine Guidance Software is designed to help surgeons optimize their workflow, minimize their time in the OR and address complex clinical decisions and techniques intraopera
tively. Its computational power is designed to support the spine product and software roadmap. The inten tion is to develop and release new technologies within the Q ecosystem.
“In my experience, Spine Guidance Software truly simplifies preoperative planning, navigation and ex ecution,” said Stephen George, M.D., director of spine surgery, Nicklaus Children’s Hospital. “From what I have seen, the Q Guidance System is a powerful platform that has provided reliability and performance in a solution that is conveniently scalable to a wide ar ray of surgical procedures, ranging from a single level fusion to a multi-level deformity correction. When used with the Airo TruCT scanner, Spine Guidance Software is designed to minimize time spent intra operatively planning, thanks to its auto segmentation capability, while also allowing us the benefit of being able to image the patient in the surgical position. Its intuitive and customizable software enables us to con figure the system to fit our preferences.”
INDUSTRY INSIGHTS news & notes
10 OR TODAY | December 2022 WWW.ORTODAY.COM
Olympus Launches Thunderbeat Energy Device for Open Surgery

Olympus Corporation (Olympus) has announced the release of the Thunderbeat Open Fine Jaw Type X surgical energy device for open surgery. With a new thermal shield, the Thunderbeat Open Fine Jaw Type X surgical energy device is designed to support safer procedures. The device is available commercially in Japan. The commercial launch of the product in Europe, the U.S., and South Korea is ex pected this year, with continued launches in other countries and regions following.
This device is part of Olympus’ Thunderbeat portfolio of hybrid energy devices that deliver both ultrasonic and bipolar energy simultaneously for tissue management, including hemostatic cutting and dissection, in laparoscopic surgery and open surgery. The Thunderbeat hybrid devices eliminate the need for multiple instruments during the sur gery, contributing to efficiency in the operating room and reduced operation time.
“This latest addition to our differentiated Thunderbeat line of products continues to deliver on Olympus’ com mitment to offering hospitals a full portfolio of advanced
news & notes
energy devices providing best-in-class functionality for numerous procedures and specialties in minimally invasive and open surgery,” said Phil Roy, global vice president and general manager of the surgical devices business unit.
The Thunderbeat Open Fine Jaw Type X device is designed for open surgical procedures that require delicate and fine tissue dissection, such as in thyroidectomy or radi cal neck dissection. The new thermal shield improves the thermal profile on the grasping surface, which reduces the risk of unintended heat damage to nearby tissue, nerves and other structures. The jaw design maintains a finely curved tip for precise dissection and enhanced visibility during use.
INDUSTRY
INSIGHTS
MEDICAL EQUIPMENT 1 . 80 0 .G E T.S O M A ( 1 . 80 0 . 48 3 . 766 2 ) W W W.S O M AT E CH N O L O G Y C O M FOR EVERY DEPARTMENT QUOTES IN LESS THAN 24 HOURS December 2022 | OR TODAY 11 WWW.ORTODAY.COM
Study Includes Baptist Health, LeanTaaS Collaboration
LeanTaaS Inc. has announced its inclusion in a Gartner case study along with Baptist Health, a not-for-profit integrated delivery network in Jacksonville, Florida.
The recently published “Case Study: Take an AI-Based Approach to Operating Room Scheduling and Utiliza tion” (Gartner, Barry Runyon, August 2022) states that “effective OR scheduling optimization can improve case throughput, OR capacity and utilization, clinician satisfaction and retention, patient experience measures and health care provider revenue.”
According to a previous Gartner report, “[Health care providers] recognize and understand well the value of optimizing patient flow and managing capac ity. Managing patient throughput and the utilization of facilities, staff, and materials are persistent hospital operational and strategic priorities that underlie most cost-optimization initiatives,” states the November 2021 report on “Emerging Technologies and Trends Impact Radar: The Real-Time Health System” (Gart ner, Gregg Pessin, Barry Runyon, et al.). The “Hype Cycle for Healthcare Providers” report from July 2022 continues that “monitoring and managing patient flow and capacity are persistent health care provider chal lenges, and optimizing the use of facilities, staff, and equipment remains a healthcare provider operational priority” (Gartner, Andrew Myers, Mike Jones, et al.).
As a large, complex, and busy integrated delivery network with 5 hospitals, 74 operating rooms, and ap proximately 47,000 surgeries annually, Baptist Health wanted to increase the utilization of its OR suites. Its existing OR scheduling software lacked predic
tive capabilities and clinician engagement features, so surgeons had difficulty finding and reserving ORs even when prime time utilization was low. Leadership also wanted to improve data on utilization and equipment needs before making important decisions on capital requests for new facilities and robotic equipment. To ad dress these challenges, Baptist Health worked with Lean TaaS to implement a predictive and prescriptive analytics platform that optimizes access to scarce OR capacity.
“Engaging LeanTaaS was an important step in improving OR utilization throughout Baptist Health hospitals,” said Amy Cate Huveldt, vice president of performance excellence, Baptist Health, Jacksonville. “We received real, worthwhile results from our in vestment in LeanTaaS and alignment of people and processes. Improving our OR operations translates to surgical growth, engaged providers, and improved patient care, all of which are helping us achieve our organizational goals.”
“We have a truly collaborative relationship with Baptist Health, and we’re thrilled to see iQueue for Operating Rooms featured as a use case in a Gartner Case Study,” said Ashley Walsh, vice president, client services, iQueue for Operating Rooms. “We’re continu ously working to provide our health system customers with the capacity optimization solutions they need, and it’s that clear access to valuable, actionable data that improves both the patient and provider experi ence. Baptist Health is proof that an investment in operational excellence is a win for clinicians, patients and the bottom line.”
news
INDUSTRY INSIGHTS
& notes
12 OR TODAY | December 2022 WWW.ORTODAY.COM

ONE CLICK. EARN CE’s. When you join us for a FREE webinar. OR Today has been approved and is licensed to be a Continuing Education Provider with the California Board of Registered Nurses, License #16623. CBSPD CE credits when applicable. ORTODAYWEBINARS.LIVE THURSDAYS AT 2PM ET WEBINAR ARCHIVES ONLINE WEBINAR SERIES
INDUSTRY INSIGHTS
HSPA
Revised Guideline for Processing Flexible Endoscopes: Key changes for SP staff
By Susan Klacik
The Association of periOperative Registered Nurses (AORN) released its updated Guideline for Processing Flexible Endoscopes. The revised guideline adds 10 new topics that provide more detailed guidance and delivers best practices for all stages of flexible endoscope processing based on a review of extensive evidence-based research. This article provides an abbreviated summary of some of those updates.
that processed items are free of viable microbes, and packaging systems protect the integrity of the sterilized contents until the package is opened for use while permitting the aseptic delivery of the contents.
Point-of-use treatment, leak testing
Sterilization versus HLD
The revised guideline separates steriliza tion and high-level disinfection (HLD) into separate sections. Similar to ANSI/ AAMI ST91:2021 Flexible and semi-rig id endoscope processing in health care facilities, the updated AORN guideline recommends sterilizing reusable flexible endoscopes that have a manufacturer validation for sterilization whenever possible. This recommendation is also consistent with the Spaulding Clas sification system that labels items, such as flexible endoscopes, which come in contact with non-intact skin or mucous membranes as semi-critical devices and are recommended to be processed by sterilization. Not every flexible endo scope can undergo sterilization accord ing to its manufacturer’s instructions for use (IFU); however, the sterilization recommendation notes that sterilization provides the highest level of assurance
If a liquid chemical sterilization (LCS) system will be used to sterilize an endoscope for a critical procedure, the endoscope should be immediately transported to the point of use in a closed processing container. Endoscopes used for a semi-critical procedure and are processed in a LCS system may be processed in the same manner as those that receive HLD. If process ing flexible endoscopes using HLD, it is recommended to use a compatible FDA-cleared AER in accordance with the manufacturer’s IFU. This recom mendation includes verifying that all connections are correctly connected and then monitoring the cycle using all rec ommended monitoring tools. If manual HLD is performed, it is recommended to process endoscopes with a compat ible FDA-cleared high-level disinfectant in accordance with the manufacturer’s IFU and the AORN Guideline for Man ual Chemical High-Level Disinfection. Using an automated process for HLD is recommended instead of a manual pro cess because automated processes may be more efficient and reduce personnel exposure to high-level disinfectants. It is recommended to have flexible endo scopes reprocessed in the same manner across all processing locations and shifts, including weekends.
Transport to the decontamination area now includes a hand-over process from the transporter to decontamina tion personnel and a list of information that should accompany the endoscope. The list should include the time that point-of-use treatment was completed; whether that treatment began imme diately after use of the endoscope (and, if not, the time that endoscope use was completed); and whether the endoscope was kept moist until point-of-use treat ment could be performed.
Leak testing is a critically important aspect of flexible endoscope processing, and verification of the leak tester’s pres sure accuracy or calibration of automatic leak testers ensures that the leak tester is producing the correct pressure. A new recommendation was added to verify the pressure of the leak tester in accordance with the manufacturer’s IFU. When using an AER that has a mechanical leak test, it is also recom mended that the leak test performed by the AER be considered as an adjunct to leak testing performed before manual cleaning. Note: Mechanical leak testing in an AER is not a substitute for leak testing performed before manual clean ing as recommended in the endoscope manufacturer’s IFU.
Cleaning, inspection, CV, drying and storage
The previous version of the guideline had a conditional recommendation that internal channels may be inspected with a borescope; however, the new version
14 OR TODAY | December 2022 WWW.ORTODAY.COM
recommends using a clean borescope to visually inspect accessible channels of flexible endoscopes before steriliza tion or HLD. Health care organiza tions should identify high-risk flexible endoscopes, including duodenoscopes, bronchoscopes, ureteroscopes and cys toscopes, and these high-risk endoscopes should undergo CV testing after each use, and the results of those tests should be recorded.
Thorough drying of flexible endo scopes is necessary because any moisture remaining on the surfaces of an endo scope can facilitate microbial growth and biofilm formation during storage. It is recommended to perform drying even when using an AER with an air purge cycle or extended dry time feature. It is also recommended to dry all accessible channels for at least 10 minutes; if vis ible moisture is still present, extend the dry time until visible moisture is no lon ger observed. The guideline also features a conditional recommendation that a compatible automated drying system, such as a drying cabinet with pressureregulated, HEPA-filtered air, may be used to dry endoscope channels. To help determine endoscope storage time, a new conditional recommendation was added on conducting a storage time risk assessment. A list of considerations perti nent to the storage time risk assessment is included. Further, new recommendations were provided regarding how to trans port endoscopes, which type of container to use, and how to properly clean and disinfect the container.
Water bottles, prions and data capture Water and irrigation bottles can be a source of endoscope contamination. It is recommended to label the water bottle with its contents and the date the bottle was filled or opened. Evidence has shown that simethicone may be difficult
to remove from water bottles, tubing and endoscope channels; therefore, it is not recommended to add simethicone to water or irrigation bottles.
There has been concern regarding the use of flexible endoscopes on pa tients with suspected prion disease (e.g., Creutzfeldt-Jakob Disease). Evidence shows that flexible endoscopes may be used on patients who are at an increased risk for prion diseases as long as the devices are processed using standard procedures for cleaning and sterilization or HLD.
The record keeping topic has been expanded and new recommendations now call for recording leak testing, CV and borescope inspection. Specific record-keeping recommendations are provided for AER or LCS processors. It is recommended to record all repairs and maintenance for all endoscopes and endoscope accessories, processing equip ment, water filtration systems (e.g., filter changes) and storage cabinets.
Leadership, quality control recommendations
Leaders are responsible for the safe working conditions and process manage ment, so they must be knowledgeable about sterilization and HLD and con firm that endoscope processing is being performed to the latest standards and regulations. Education is a critical part of endoscope processing. The revised guideline includes education recommen dations for personnel at the point of use who handle flexible endoscopes. A list of specific activities in which point-ofuse personnel should receive education and competency verification is included in the guideline. A conditional recom mendation has been added to consider increasing the frequency of competency verification for endoscopes that are used infrequently. Note: Flexible endoscopes are not just used in surgery and endos
copy settings. A new recommendation now includes education and compe tency verification for all who handle and process endoscopes, regardless of the location.
The revised guideline recommends a systems approach to quality assurance and performance improvement to help prevent endoscope processing errors. It lists several important systems that should be reviewed, such as providing adequate resources (e.g., time, per sonnel, inventory, space), prioritizing worker safety and ergonomics, standard izing processes among departments and establishing systems to improve trace ability. Audits are an important part of a quality system and can identify problem areas, assist in evaluating and improving the quality of endoscope processing and formulate plans for corrective actions.
Another recommendation was added to evaluate water quality and water fil tration systems at established times and after major maintenance to the water supply system. Other recommendations pertain to preventative maintenance for flexible endoscopes and equipment used in their processing. It is a regulatory re quirement that health care organizations report any suspected device-related serious injury or death to the FDA and the manufacturer (or only to the FDA if the manufacturer is unknown). A conditional requirement is also included in the revised guideline that states that a health care facility may report any device malfunction to the FDA.
The revised AORN Guideline for Processing Flexible Endoscopes has been updated in the eGuidelines Plus at https://www.aorn.org/eguidelinesplus. The 2023 print version will be available for purchase at www.aorn.org.
– Susan Klacik, BS, CRCST, CIS, CHL, ACE, FCS, is a HSPA clinical educator.
December 2022 | OR TODAY 15 WWW.ORTODAY.COM
AAMI Roundup
Mary K. Logan Grant Awarded to Novel
Sterility Assurance Research
The AAMI Foundation has named the 2022 recipients of the Mary K. Logan Research Award Program – a team of researchers who are investigating consistent methods for directly linking the efficacy of medical device sterile process ing practices to patient safety. The project, What Counts in Sterile Processing Departments: Measur ing Defects and Responses, has earned an award in the amount of $52,685, paid to Penn State Uni versity (PSU), where the research team is based.
“The overall objective of this project is to determine how SPDs approach measurement of process es, defects, and outcomes, which factors they feel most impact their effectiveness, and gather such information from SPDs across the country,” said Jessica Williams, as sociate professor at PSU. “Despite processing millions of instruments each year and being an essential component of accreditation, these departments are often taken for granted by hospital administration, health care providers and even health services researchers unless something goes wrong, like delayed surgeries or infection outbreaks traced to unclean instruments.”
At the center of the team’s hypothesis is an understanding that even high-performing sterile pro cessing departments (SPDs) may have different strategies to ensure they are effectively preventing patient infection. And despite ef forts from standards developers like AAMI to bring end-user experts to gether for information sharing, the socio-economic factors that influ ence a department’s best practices remain difficult to account for.
“While there is ample research and [manufacturer-provided in structions for use] about specific cleaning, sterilization, and disinfec tion technologies and processes, there is relatively little about the human and organizational side of SPDs,” said Williams.
The researchers aim to survey up to 10 directors from high-per forming sterile processing depart ments in an initial survey, follow ing up with in-depth analysis and a large-scale (~300 participants) cross-sectional survey of responses, human factors, and patient safety, among other factors. By looking at common strategies and best prac tices among SPDs for measuring and responding to defects in their processes, the work will help estab lish clear benchmarks for responsi ble departments and future studies.
“We believe our results will be used practically by SPDs who are eager to learn from peers,” Wil liams concluded. “We also expect that our results will be used by researchers studying patient safety, as our data will provide an essential first step of describing the current landscape of SPD defect measure ment as well as showing prelimi nary pathways through which SPD matters for patient safety.”
AAMI Partners with AmbiFi to Offer CuttingEdge Medical Process Support Tool

AAMI has announced a strategic partnership with AmbiFi, an ad vanced software as a service (SaaS) performance support company. Ambifi provides mobile-first, real-time, hands-free, support for complex procedures while ensuring real-time process documentation and benchmarking.
“We continue to leverage proven technologies to better serve our members and stakeholders,” noted AAMI President and CEO Pamela Arora. “The cognitive load on all health care professionals continues to challenge the safe and effective use of health technology. AAMI is expanding its offerings to include AmbiFi’s revolutionary moment-ofneed performance support. Ambifi has the potential to transform the
INDUSTRY INSIGHTS AAMI
16 OR TODAY | December 2022 WWW.ORTODAY.COM
execution of complex medical device processes, enabling greater consistency, quality and transpar ency.”


Headquartered in Pittsburgh, Pennsylvania, AmbiFi leverages am bient computing and performance science to empower experts to easily transform industry standards, guidelines, procedural documenta tion and expertise into ambient intelligent copilots, called “ambiis.” Deployable on secure mobile devic es, including smartphones, tablets and smart glasses, these copilots may provide guidance and support during the execution of high-stakes processes, such as the processing of medical devices or even the train ing of surgeons.
“AmbiFi is a proven platform
that launched in the aviation indus try and is now used by thousands of pilots globally. After pivoting to health care, they have proven their platform across a wide range of clinical use cases,” said Robert Burroughs, senior vice president of education at AMMI. “Our goal is to bring this powerful capability to our many stakeholders. Given the incredible breadth and complexity of process that must be executed throughout a medical device’s life cycle, this tool has the potential to be transformative.”
As a part of the strategic part nership between AAMI and Am biFi, AAMI has adopted the AmbiFi platform and will leverage AAMI content and subject matter ex pertise to develop medical device,
sterile processing and healthcare technology ambiis for use by AAMI members and stakeholders. In ad dition, AAMI will work directly with medical device manufacturers, healthcare delivery organizations, and independent service organiza tions and educators to develop cus tom solutions utilizing the AmbiFi platform.
“AAMI is the de facto world leader driving the safe and effec tive use of healthcare technology via their standards and education,” said James Sharpe, cofounder of AmbiFi. “We can’t wait to see what they can do with the AmbiFi plat form at their disposal, and we look forward to working together closely to support AAMI members and stakeholders.”
www.cchangesurgical.com Protected Until Use. Automatically. Expert Slush Every Case. Automatically. SLUSH SLUSH Surgi SLUSH TM Fifteen consecutive evaluating teams just switched to SurgiSLUSH™ The Intersection of Smart & Simple SLUSH NEWS December 2022 | OR TODAY 17 WWW.ORTODAY.COM
INDUSTRY INSIGHTS
Joint Comission
Assessing Life Safety Compliance
By James Kendig, field director, The Joint Commission
A ssessing and preparing for a successful Joint Commission Life Safety Code survey within a surgical setting does not have to be a laborious or anxiety-producing event. With proper planning and prior knowledge of processes, ambulatory surgical centers (ASCs) can easily prepare for a successful survey.
Below is basic information, divided by process, to help ASC staff prepare for a suc cessful survey:
• Keep a flashlight available to help view spaces above the drop ceiling.
• Provide surveyors with a ladder that expands to easily reach an ambula tory facility’s ceiling. Most ladders are sold with a rating, so review weight requirements prior to purchase. Rou tinely, a ladder with a rating of Type 1 (250 lb. capacity) or Type 1A (300 lb. capacity) is sufficient.
Select inspection vendor
Selecting a vendor for inspection, testing and maintenance activities is an important step prior to the survey process. The inspection vendor must be knowledgeable about systems they are inspecting, testing and maintaining and should be up to date on related National Fire Protection Association (NFPA) require ments and Joint Commission standards.
The inspection vendor is also responsible for thoroughly understanding Joint Commis sion requirements. So, providing them with a copy of the standards manual and becoming familiar with standards and requirements is an important step before document review during survey.
Additionally, identifying a staff member to serve as a standards manual expert to enforce its requirements within a health care facility helps to successfully complete the document review. Larger organizations may
receive standards enforcement support from their corporate offices; however, stand-alone facilities require staff to personally become familiar with standards, elements of perfor mance and how they are organized within the standards manuals.
Keep current with updated code require ments
Specific NFPA codes are found in the Life Safety Code 101 document (2012 edi tion) in Chapter 2 “Referenced Publica tions.” Chapter 2 is a valuable reference for scenarios that involve multiple versions of updated codes. For example, in the chapter “Evaluating a Sprinkler System,” it notes that the 2010 edition of NFPA 13 and the 2011 edition of NFPA 25 are used. Another example notes that NFPA uses the 2010 edi tion of NFPA 10 related to fire extinguishers.
It is imperative to keep up with current codes used, since NFPA codes get updated approximately every three years. Errone ously using an earlier or later edition of the code may result in edits that would impact the inspection testing and maintenance of the various systems. Additionally, various versions of NFPA codes may add, delete or even edit certain sections. So, make sure the vendor is using the appropriate code to com plete inspection, testing, and maintenance activities (they are found in Chapter 2 of the Life Safety Code 101-2012).
Determine if the health care organization has CMS “deemed status”
Centers for Medicare and Medicaid Services (CMS) adopted the NFPA 101-2012 edition of the Life Safety Code on July 5, 2012, for deemed health care organizations. In simple terms, “deemed status” demonstrates that a health care organization not only meets but exceeds expecta tions for a particular area of expertise.
Deemed status is given by CMS or through an accredited agency. Health care
organizations that achieve accreditation through a Joint Commission “deemed status” survey are determined to meet or exceed Medicare and Medicaid requirements. So, a health care organization with “deemed status” would not be subject to the Medicare survey and certification process because it has already been surveyed by an accrediting organization.
Pass document review, inspection, testing and equipment maintenance
On the day of survey, Joint Commission surveyors typically arrive early, so it is im portant to be ready to greet them as early as 7:30-7:45 a.m. After introductions, the Life Safety Code surveyor completes a document review to specifically focus on inspection, testing and maintenance of a facility’s fire sprinkler system, fire alarm system, genera tor and related medical gases. It is wise to reference The Joint Commission’s Survey Activity Guide (SAG) for additional details of document review.
Typically, the Life Safety Code surveyor asks three introductory questions to orient themselves to an ASC:
1. What type of fire stop does the health care organization use? (This is followed up with review of train ing for use.)
2. Are there any prohibitions or safeguards when accessing the inter stitial spaces above the ceiling?
3. What does the health care organiza tion use for high-level disinfection? (This is asked to determine appro priate air exchanges for a specific product.)
Observe fire panels and pumps
Joint Commission surveyors observe an ASC’s fire panels to assure they are in work ing order. Additionally, they assess a facility’s generator to ensure it is in good condition
18 OR TODAY | December 2022 WWW.ORTODAY.COM
and that it is equipped with an emergency light. Surveyors also ensure a remote emer gency “power off” indicator is located a safe distance away from the generator.
A fire pump is less likely to be used unless the surveyed facility is an expansive or a multistory building. In these cases, community water pressure is commonly used to support the approved automatic sprinkler system.










Complete building tour, emergency manage ment session and report review







During a survey building tour, the Joint Commission surveyor focuses on NFPA code requirements as well as air pressure and relative humidity requirements within a building’s surgical areas. Remember, relative humidity is addressed in CMS memo S&C: 13-25-LSC & ASC. ASCs are not subject to all the same Life Safety Code (LSC) requirements as hospitals, but are required,


consistent with 42 CFR 416.44(a)(1), to maintain relative humidity (RH) in operat ing rooms in accordance with nationally accepted guidelines.

After completing document review and a building tour, it is time to complete an emergency management session to assess a facility’s compliance with ambulatory requirements. This overview takes approxi mately one hour and covers emergency event drills, staff training and responses dur ing an emergency drill or actual event.
Once the emergency management session is complete, the Life Safety Code surveyor and clinical surveyor, if present, exit the survey to conduct a preliminary report review. Remember, however, that the report is not considered final until it is reviewed and approved at The Joint Commission’s central office. For this reason, version control of documents is vital.
Conclusion
Joint Commission surveyors work onsite with ASC staff to ensure they are prepared for a successful survey. During survey, staff should feel free to ask the Life Safety Code surveyor questions to better understand the survey processes. Additionally, it is important to obtain answers to any questions regarding code requirements. Joint Commission sur veyors are present during survey to guide staff so that health care organizations, including ambulatory facilities, earn the Joint Commis sion Gold Seal of Approval, indicating that their facility meets The Joint Commission’s rigorous performance standards in delivering care and is committed to the highest level of health care quality and safety.
– James Kendig is field director at The Joint Commission.
OPERATING ROOM SOLUTIONS SURGICAL TABLE PADS - CASTERS - MAYO STANDS OPERATING ROOM SOLUTIONS 800.323.4282 www.ALCOSales.com ALCO has your solution! Surgical Table Pads Mayo Stands Casters Problem? Pro-Tek Standard Integra-Gel Extra Large Top! AL-85454 Thumb Operated! AL-81948 » Waterfall edge construction » Fluid & stain resistant » X-ray permeable » Antimicrobial » Latex-free No More Rusty Casters! X December 2022 | OR TODAY 19 WWW.ORTODAY.COM
INDUSTRY INSIGHTS Joint Comission
INDUSTRY INSIGHTS CCI
Changes in Perioperative Leadership
By James X. Stobinski
A s I have mentioned in previous columns, the Competency and Credentialing Institute (CCI) nurses teach an introduction to the operating room course at Edgewood College in Madison Wisconsin. In a recent class, my long-time friend Stephanie Davis presented to our class on the topic of the business aspect of perioperative nursing. I was surprised to hear that the revenue from surgery is shrinking as a percentage of total hospital revenue. She stated that OR revenue is now less than 50% of total revenue where previously that ratio had been 60-70%. This decrease represents a foundational shift in health care operations and reflects changing patterns of reimbursement.
From an overall perspective, this is part of a larger transition to a value-based system of care. Payers in the American health care system are increasingly ne gotiating for better pricing for surgical care. Bundled payments for the entire episode of surgical care are becoming increasingly common and perioperative staff must be aggressive in controlling expenses. The net result of all these changes is that perioperative leaders must develop new skill sets. Financial management has always been promi nent for perioperative leaders, but the level of financial acumen needed is
increasing rapidly. CCI is aware of the nature of the work of perioperative leaders from the job analysis work done in support of our certification exams. From these studies we know that financial management, operational management and strategic manage ment are significant portions of the work of leading in surgical services. All these areas require varying degrees of financial acumen.
The publication OR Manager con ducts an annual survey of periopera tive leaders to track trends. In previous years, we have heard of an impending wave of perioperative nurse leader retirements. From the 2022 survey it appears that surge is now happening. The age of the respondents and the reported years of experience has mark edly shifted, generally the respondents are younger, earlier in their career and educated at a higher level. Of the 2022 respondents, 91% had baccalaureate level education or higher as their high est educational attainment and only 4% reported a diploma of nursing. The departure or retirement of experienced nurse leaders has driven down the average age, opening opportunities for nurses earlier in their career.
When I first began working in the OR in the early 1980s the route to perioperative leadership was much dif ferent. The role of perioperative nurse leaders and managers was not as well delineated. It was assumed that peri operative leaders must be OR nurses
and that these nurses were required to have strong clinical skills. Job analysis findings from the CCI now demon strate that perioperative nurse leader ship is a separate and distinct role with little overlap with perioperative clinical skills. From the 2022 survey results, we also see that 23% of the perioperative leaders are not nurses. Increasingly, we are seeing non-nurses in surgery leader ship roles as supply chain and financial analysis gain in importance.
I do not see these findings as a temporary aberration. We are amid long-term foundational change in the business of how surgery is done. Hospi tal-based ORs will concentrate on more complex cases which cannot be done in an ambulatory setting but, more importantly, the skill sets for periopera tive leaders will continue to evolve. Financial expertise, the ability to work in intradisciplinary teams and higher levels of formal education and creden tials will become the rule. For those aspiring to leadership roles, including nurses, there are great opportunities. Flexibility, an innovative nature and a willingness to adapt as surgical care continues to evolve will be key.
– James X. Stobinski, Ph.D., RN, CNOR, CNAMB, CSSM(E), is CEO of the Compe tency and Credentialing Institute (CCI).
References: Saver, S. (2022). Survey: Some improvement in satisfaction, but stagnant compensation. OR Manager, (38)10. (Pp 1, 5-9). S.
20 OR TODAY | December 2022 WWW.ORTODAY.COM
IN THE OR market analysis
Carts, Cabinets Markets Expected to Grow
Staff report
The global surgical case carts market was estimated to be $326.28 million in 2021, according to ReportLinker. It is expected to reach $530.53 million by 2027, registering a compound annual growth rate (CAGR) of 8.32% during the forecast period 20222027.
A report from Grand View Research states that the U.S. medical carts market size was valued at $662 million in 2020 and is expected to expand at a compound annual growth rate (CAGR) of 11.8% from 2021 to 2028.
An increasing incidence of musculo skeletal injuries (MSI) among caregivers, growing demand for mobile computer carts in the critical surgical procedures, rapid increase in the volume of hospitals and urgent care centers, and growing admissions as well as an increase in adop tion of the electronic medical records in hospitals are a few factors driving the U.S. medical carts market growth, according to the report.
Due to the high number of patients infected with COVID-19 admitted to health care facilities across the country, there has been a significant increase in the deployment of medical carts, the report added. This has triggered a sudden surge in the market for medical carts in the U.S., creating infinite prospects for market play ers. For instance, in April 2020 Midwest Products & Engineering introduced its Emergency Response Cart to address ventilator workflow challenges associated with COVID-19 patients who require immediate treatment. Similarly, in March 2020, the firm ramped up its manufactur ing of medical carts to assist patient care during the COVID-19 pandemic.
A growing clinical need to help nurs
ing staff is expected to propel the market over the forecast period.
“Numerous injuries necessitate surgical correction, as there is an increase in mus culoskeletal ailments,” according to the report. “Nurses, doctors, and other medical experts can assess a patient’s status and respond in real-time with emergency and nonemergency equipment in hand. Furthermore, most of these medical carts feature locking mechanisms to ensure that only experts have access to prescrip tions and other equipment. As health care facilities employ more physicians and their support staff, they need a range of medical carts, comprising those used for medi cal procedures, anesthesia, transporting equipment, surgery, data entry (features electronic equipment) and emergencies. A protected medication cart integrated with a tablet PC is more suitable than using separate medication and computer carts on the surgical floor while saving space and cost in medical facilities. As critical care units have limited floor space and require intense patient care, demand for medical carts is likely to increase over the forecast period.”
Mordor Intelligence reports that the medical carts market is estimated to be $1.2 billion in 2021. It is expected to reach $1.8 billion by 2027, registering a CAGR of 7.78% over the forecast period (2022-2027).
As COVID-19 infection is widespread globally, patient care requirements have increased, and personal protection and medical equipment, including medical carts, are in high demand. As there is a huge inflow of patients across the world, there is an immense need to decrease the spread of infection. Handheld diagnostics are one of the critical paths of infectionspreading tools that must be taken care of. Hence, the usage of medical carts is likely to increase during the pandemic to safely
administer medications and other neces sary needs to patients and health care pro fessionals. For instance, in February 2021, Ergotron and Ingram Micro collaborated to donate medical carts to help in the novel coronavirus outbreak.
The major factors attributing to the increased adoption of medical carts in re cent years are a rise in health care facilities, increased health care burden necessitating technological advancements and a surge in patient care. Moreover, the reduction in la bor costs and the adoption of automation is likely to drive the growth of the medical carts market throughout the forecast period. In December 2021, the AMiS30EP pole cart was the newest addition to Advantech’s AMiS product line, which is a prominent provider of medical computer systems and services. Depending on the application, this product can be supplied with a variety of monitors and devices. As a result of these technical breakthroughs, the market is likely to expand in the near future. Moreover, in August 2021, the new Trio mobile computing workstation from Capsa Healthcare has been released. Cap sa’s Trio point-of-care platform mobilizes electronic health records and supports efficient and precise drug management. As a result of these developments, the market is likely to expand in the near future.
DataIntelo reports that the global medical cabinets market was estimated to be $8.11 billion in 2019. It is expected to grow at a CAGR of 4.7% from 2022 to 2030.
Medical cabinets are furniture specifi cally designed to store medical supplies and equipment. They come in a variety of shapes and sizes and can be either station ary or mobile. Some cabinets have hangtype shelves, which allow for the vertical storage of items.

December 2022 | OR TODAY 21 WWW.ORTODAY.COM
Capsa Healthcare Avalo Med/Surg Cart

The Avalo Series Med/Surg Cart is designed to provide organized and secure access to medications and supplies, while supporting the latest technology solutions and moni toring equipment. Avalo carts feature durable, high-impact panels, a lightweight design for easy maneuverability and smooth surfaces for easy cleaning. The Med/Surg cart is available in a range of heights and drawer configurations, with customizable drawer divider kits to provide optimal organization and visibility of supplies. A choice of lock systems ensures security, and a wide selection of optional accessories support an efficient workflow.

CIVCO Ultrasound Probe Storage Cabinet
CIVCO’s Ultrasound Probe Storage Cabinet provides a safe and clean environment for disin fected ultrasound probes. A fan draws air through a replaceable HEPA filter for continuous clean air flow using positive pressure. The system’s special ty shelves protect delicate probes from damage and vertical suspension facilitates drying. A 2022 study uncovered a very low risk of pathogenic bacterium growth on ultrasound probes 30 days after high-level disinfection when stored in the CIVCO Storage Cabinet.
For more information, visit civco.com
IN THE OR product focus
22 OR TODAY | December 2022 WWW.ORTODAY.COM
IN THE OR product focus
Healthmark HushKarts
Healthmark HushKarts are designed for quiet mobility with one-piece, double-wall polyethylene construction. There are no creaking bolts and no rattling metal with rubber-cushioned 4-inch sealed bearing casters designed for convenient storage. Each HushKart offers three shelves with slip resis tant surfaces and raised edges. They are ideal for use as surgical case carts, and for use by pharmacy, respiratory and CSD. Designed for easy cleaning, the carts are cart-washer washable. Polyethylene will not rust, corrode, dent or peel. One-piece seam less construction eliminates hard-to-clean grooves and crevices. The carts are available in three colors, establish a color-coding system to fit your needs. Choose a color (slate blue, dark brown, coffee beige) to coordinate with the décor.

Total Scope EndoCart carts
Total Scope’s subsidiary company, EndoCart, manu factures fully customizable endoscopy carts. The carts were developed by GI and surgical nurses as the safest and most efficient travel system for scopes. The company offers three different models with a wide variety of add-on accessories; therefore, they can tailor each cart to meet the needs of each facility’s environment. If your scopes travel between hospital or clinic floors, or scopes move to different departments on the same floor, EndoCart has a safe ergonomic cart solution. The carts will help keep the OR running at max efficiency.
*Pictured is the Deluxe EndoCart

December 2022 | OR TODAY 23 WWW.ORTODAY.COM
COVER STORY
SURGICAL SMOKE UPDATE

 BY DON SADLER
BY DON SADLER
24 OR TODAY | December 2022 WWW.ORTODAY.COM
Perioperative personnel have long known about the health hazards posed by surgical smoke in the operating room. It has been more than 30 years since researchers first documented that particulate matter in surgical smoke can pose dangers to nurses and others in the operating room (OR).
For many years, little was done to pro tect OR personnel from the dangers of surgical smoke. However, this is finally starting to change as a growing number of states are passing legisla tion designed to reduce the dangers of surgical smoke plume.
OSHA Alert … in the 1980s
The U.S. Occupational Safety and Health Administration (OSHA) first issued an alert about the health haz ards from surgical smoke way back in 1988. However, they didn’t follow up with any regulations requiring hos pitals and ASCs to limit or eliminate surgical smoke.
“Policy changes at the federal level can move slowly,” says Jennifer Pen nock, associate director, government affairs for the Association of periOper ative Registered Nurses (AORN). “So, our primary focus remains on the state level. We are seeing a positive response from our legislative outreach as many states seek to strengthen protections for health care workers and patients.”
According to Pennock, nine states have passed laws requiring hospitals and ASCs to use smoke evacuation systems to prevent human exposure to surgical smoke: Rhode Island, Colorado, Kentucky, Oregon, Illinois, Washington, Arizona, Georgia and Connecticut.
Surgical smoke legislation is pending in eight states – Utah, Iowa, Missouri, Arkansas, Ohio, West Virginia, Pennsylvania and New York. Also, the Texas Health and Human Services Commission is set to issue rules that would in clude provisions for surgical smoke evacuation for all operating rooms in the state, according to Pennock.
These laws require hospitals and ambulatory surgery centers (ASCs) to use smoke evacuation systems that prevent human exposure to surgical smoke. “Each year we build
“Legislators are incredibly worried about health care workers and are committed to the health and safety of the people dedicated to saving lives.”
-Jennifer Pennock
upon the momentum from the prior legislative sessions,” says Pennock.
“Legislators are incredibly wor ried about health care workers and are committed to the health and safety of the people dedicated to sav ing lives,” says Pennock. “They rec ognize that nurses and other health care workers are leaving their profes sions and want to make the changes needed to stabilize the workforce.”
As part of its advocacy efforts to effect changes for OR staff and patients, AORN launched a national petition drive last year urging OSHA to issue regulations requiring worker and patient protections from harmful surgical smoke.
Status of State Legislation
Kay Ball, Ph.D., RN, CNOR, CMLSO, FAAN, a perioperative consultant and adjunct professor at Otterbein University in Westerville, Ohio, has been performing research on the ef fects of surgical smoke on periopera tive personnel for more than a decade. She is optimistic about surgical smoke legislation passing in Ohio soon.
“We’re hoping to get some action during the legislative session after the midterm elections,” says Ball. “We want to get our legislation (SB161) out of the Senate Health Committee and on to the Senate floor for a vote, and then on to the House.
“If the legislation isn’t passed in this general assembly,” adds Ball, “it will be reintroduced after January 1 during the Ohio 135th General As sembly.”
In Georgia, SB573 was signed into law on May 9, 2022, thanks in large part to the work of a dedicated team of perioperative professionals led by Brenda Ulmer, RN, MN, CNOR. She started her efforts to get surgical smoke legislation passed in Georgia in 2019 after learning that the first two states in the nation (Rhode Island and Colorado) had passed surgical smoke laws.
“That’s when I decided Georgia should be the next state to pass legis lation to protect patients and health care workers from surgical smoke,” says Ulmer, who served as the Georgia Council Legislative Chair.
Beverly Kirchner, immediate past president of the Texas Collaboration of periOperative Registered Nurses (TCORN), has been spearheading ef forts the past several years to get surgical smoke legislation passed in Texas. After Senate Bill 429 failed to make it to committee last year, she and her team decided to go the regulatory route.
“The regulations are in draft format
COVER STORY
December 2022 | OR TODAY 25 WWW.ORTODAY.COM
and the Texas Department of Health is now reviewing comments received dur ing the comment period,” says Kirchner. “We will be notified if they change the wording of the regulations, which fol low the wording of Senate Bill 429.”
Pennock says that surgical smoke legislation is most successful in states with a strong group of grassroots advocates committed to working on policy advocacy for multiple years and through legisla tive sessions. “It’s important for AORN and the advocates to engage with stakeholders early in the pro cess,” says Pennock.

It’s also important to identify a strong bill sponsor in the House or Senate who will throw their politi cal influence into the success of the bill. “A strong bill sponsor can help all the stakeholders involved see the merits of the legislation,” says Pennock.
In Illinois, for example, Rebecca Vortman, clinical assistant profes sor of population health nursing science in the UIC College of Nursing, and Penny Smalley, an independent nurse consultant and director of education and regula tory affairs for the International Council on Surgical Plume, worked closely with the legislative sponsors of a surgical smoke bill that was passed in 2021.
Together, they built a grassroots coalition that was critical to getting the legislation across the finish line. The new law took effect on Janu ary 1, 2022, requiring hospitals and ASCs in the state to adopt policies to ensure surgical smoke plume
elimination with an appropriate evacuation system for every proce dure that generates surgical smoke due to the use of energy-based devices.
“We are so proud that we were two nurses who proved that our voices could be heard and that we could effectively lead the ad vocacy efforts needed to get this bipartisan bill passed through a grassroots effort,” says Vortman.
In addition to state legislation, regulatory bodies have also issued recommendations and guidelines regarding surgical smoke. This in cludes NIOSH, which recommends that a smoke evacuator be on at all times when airborne particles are produced during all surgical or other procedures.
However, this is only a recom mendation, not a requirement.
“State laws requiring surgical smoke evacuation policies pro vide a pathway for the accrediting organizations to enforce facility adherence to their own policies on surgical smoke evacuation through the organization’s accreditation processes,” says Pennock.
Damaging Effects of Surgical Smoke
Surgical smoke plume is formed when substances like tissue, blood and fluid are vaporized into a gaseous form. It is produced during most OR procedures when lasers and electrocautery devices are used to dissect tissue and stop bleeding. Numerous studies confirm that surgical smoke contains hazardous
chemicals, bacteria and live viruses.
“Most of what’s in surgical plume is 1.1 microns in size or smaller,” says Ball. “Any particles less than 10 microns can be irritat ing to lung tissue, and ultrafine par ticles can settle in alveoli, causing lung and air exchange problems.”
Vortman has performed research demonstrating the hazardous health consequences faced by OR person nel from prolonged exposure to surgical smoke, including eye and upper respiratory tract irritation. Surgical smoke plume also has mu tagenic and carcinogenic potential, according to Vortman’s research.
Other studies have shown that surgical smoke plume may con tain E. coli, MRSA, HPV, hepatitis viruses and HIV. There may also be SARS-CoV-2 and variants in surgi cal smoke plume, as well as toxic gases such as benzene, toluene, carbon monoxide, formaldehyde and hydrogen cyanide.
In addition, patients may be at risk from internal absorption of hazardous gasses and particulates in surgical plume.
Ball first performed research into the effects of surgical smoke on OR personnel in 2010 and then repeated parts of the research in 2020. “The results of the first study repeated 10 years later, which dem onstrates a profile for perioperative nurses,” she says.
When asked if they had respi ratory disorders or diseases, OR nurses in Ball’s study reported twice the incidences of respiratory problems compared to the general population. For example:
• 22.9% of OR nurses reported sinus infections and sinus problems compared to 11% of the general population.
• 10.9% of OR nurses reported asthma compared to 7.6% of the
COVER STORY 26 OR TODAY | December 2022 WWW.ORTODAY.COM
“A strong bill sponsor can help all the stakeholders involved see the merits of the legislation.”
-Jennifer Pennock
general population.
• 9% of OR nurses reported bronchitis compared to 3.4% in the general population.
• 24.2% of OR nurses reported allergies compared to 15% in the general population.
“Many research studies have shown the dangers of surgical smoke,” says Ball.
For example, AORN’s Guide line for Surgical Smoke Safety in cludes 223 references document ing the hazards of surgical smoke.
Ball also points to a study reported in the Journal of Clini cal Nursing in 2016. In this study, 49% of nurses and 58% of surgeons reported experiencing headaches, 40% of nurses and 42% of surgeons reported watery eyes, and 49% of nurses and 28% of surgeons reported coughing due to exposure to surgical smoke.
Sore throat, nausea, drowsiness, dizziness, sneezing, rhinitis and bad odors absorbed in the hair were also attributed to surgical smoke by nurses and surgeons in this study.
The Lowdown on Smoke Evacuation Technology
Many experts agree that using smoke evacuation technology is the most ef fective way to eliminate surgical smoke in the OR. “AORN and our members would like to see more widespread use of these devices,” says Pennock.
Julie Miller, MS, principal project engineer, device evaluation with ECRI, explains how smoke evacuator devices work: “A smoke evacuator is a suction source that incorporates ultra-high-effi ciency filters to remove smoke particles from the suctioned airstream at the surgical site.”
“The device uses high flows or high intake velocities to capture smoke at the nozzle, draw it through the tubing, pass it through the filters and recir
culate to room air,” adds Miller. “Most systems have variable flow control to tailor the capture for the given proce dure.”
According to Miller, the ULPA filters that most smoke evacuators use must demonstrate at least 99.999% efficiency for removing particles that are in the range of 0.12 micrometers in diameter, which is the most penetrating or difficult particle size for this filter grade to capture. “Surgical smoke is generally within this range,” she says.
“The size of the smoke particles generated, and the distance from the surgical site from which they captured smoke, can play a role in the efficiency of the device’s capacity for reducing surgical smoke,” adds Miller.
While using smoke evacuation devices might seem like a no-brainer, Miller says there are a few obstacles that may prevent some hospitals from using them. This includes concerns among some surgeons about their us ability.
“There’s a persistent belief that the smoke evac handpiece may be more cumbersome for surgeons than older designs,” says Miller. “But newer pencils exist that have integrated tub ing with encapsulation of the wire, as well as swiveling bases and extendable nozzles.”
Miller say there are also concerns about potentially disruptive noise caused by devices. “However, our evaluation of some portable evacuators showed an average operational noise of about 57 dB at max suction settings while the device is actively suctioning,” she says. “For reference, that’s about a normal conversational volume.”
There may also be cost concerns about using smoke evacuators. “The components needed for smoke evacua tion are more expensive per procedure than standard accessories,” says Miller. “For example, a standard ESU pencil and holster may cost about $2.50 while a smoke evacuation pencil with nozzle, tubing, holster and swiveling capabili ties may be closer to $25.”
Protecting the Perioperative Workforce
Part of Vortman’s motivation for advocating for surgical smoke leg islation is her concern for both the current and future perioperative workforce.
“If my daughter decides to pur sue a career in the operating room, I want to make sure she’s working in a safe environment,” says Vort man. “I don’t want her or any surgi cal team members to be exposed to the harmful contaminants of surgical smoke plume.”
AORN provides ongoing educa tion about surgical smoke, includ ing the AORN Go Clear program. “This is a comprehensive approach to protecting patient and worker safety by promoting a smoke-free environment wherever surgical smoke is generated,” says Pennock.
The AORN Go Clear Program includes all the tools and proto cols needed to start or enhance smoke evacuation practices. To learn more visit https://www. aorn.org/member_apps/Product/ Detail?productID=9709

COVER STORY December 2022 | OR TODAY 27 WWW.ORTODAY.COM
“A smoke evacuator is a suction source that incorporates ultra-high-efficiency filters to remove smoke particles from the suctioned airstream at the surgical site.” -Julie Miller
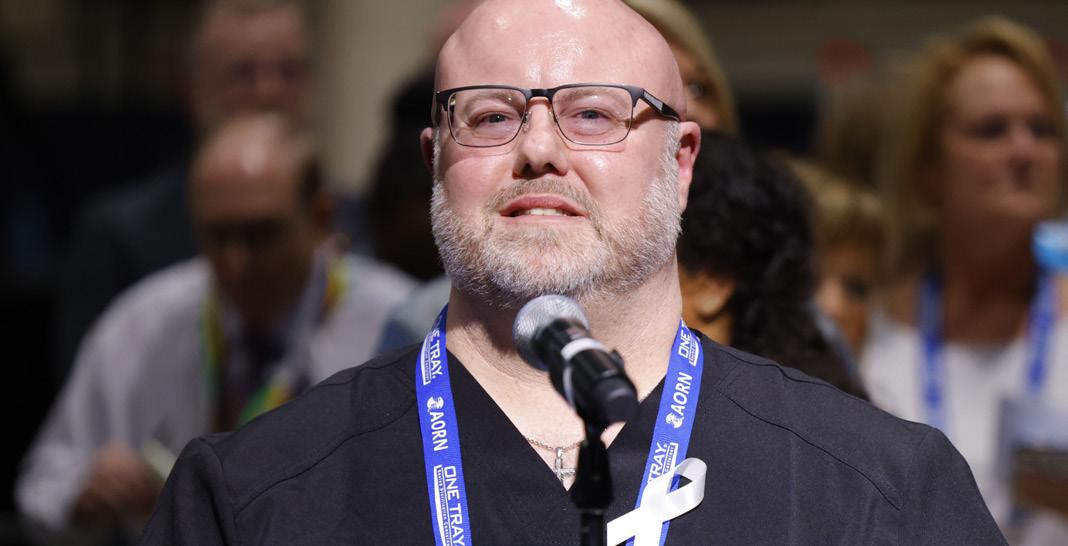
SPOTLIGHT ON:
Terry Jones, Ph.D. RN
By matt skoufalos
F or a seasoned nurse educator with several advanced degrees, Terry Jones doesn’t seem to remember the exact moment when she decided to pursue a career in nursing.

“It always seemed to be something that I wanted to do,” Jones said; “a bit of a calling, perhaps. It was some thing I was drawn to even before I understood what it fully entailed: the desire to be helpful, especially in those moments when people are struggling with health issues.”
Jones began her nursing career in the 1980s, attending nursing school at Marycrest College, the only bac calaureate program in Davenport, Iowa at the time. While attending nursing school, she availed herself of the opportunity to work as a nurse’s aide, which offered her work experi ence throughout the hospital in a variety of different areas.
That’s when Jones discovered her interest in critical care nurs ing; however, the specialty was just coming into its own at that point, and new graduates weren’t often permitted to work in critical care areas. So after graduation, when the time came for Jones to find a permanent position, she searched farther from home.
Finally, Jones landed on the Parkland Health and Hospital Sys tem in Dallas, Texas, which offered an internship curriculum for bacca laureate graduates who wanted to work in the critical care area. For a Midwesterner who’d never en countered the idea of a safety net hospital in Iowa, Jones confessed to experiencing “quite the culture shock, but in a good way.”
“I was drawn to it; drawn to the amount of need there was in that environment, and really learning what nursing was in that environ
ment,” she said. “And I stayed in that organization for 22 years be cause there were so many opportu nities for growth.”
Those opportunities expanded Jones’ understanding of the world of nursing, as she embraced the variety of options available to her in the field. Over the course of her time at Parkland, she worked in the ICU as a bedside nurse, and later took on roles in nursing education, management and research.
“We were one of the first hospi tals helping graduate nurses to get into the OR through a residency,” Jones recalled. “Then I served in an administrative capacity over re search, quality improvement, care coordination, and ended my stint there as the interim chief nursing officer. I really experienced health care through a variety of different lenses. I was always fascinated.”
While working at Parkland,
28 OR TODAY | December 2022 WWW.ORTODAY.COM
Jones also earned a master’s degree in nursing education from Texas Woman’s University and a Ph.D. from the University of Texas at Austin. She completed a second master’s degree in clinical sci ence from the University of Texas Southwestern Medical Center, and was recruited to work at the Uni versity of Texas at Austin as she decided to transition from bedside nursing work to nursing education. Since 2010, she’s worked full-time in academia. Today Jones is a tenured associate professor at the Virginia Commonwealth University School of Nursing in the Department of Adult Health Nursing and Nursing Systems.
“I loved my season at the bed side,” Jones said; “those are still some of my fondest memories of working directly with patients. There’s nothing better than being with patients and having that direct reinforcement of what you’re do ing; the immediate gratification of knowing that you helped someone.”
“I loved feeling like I made a difference in my patients’ lives,” she said. “Now I serve patients indi rectly by educating nurse managers, which was always appealing to me because I want every patient to have really good nursing care. To help other people learn to do that well is really important. Wherever I am, the patient is; if I have a seat at the boardroom, then I bring the patient with me.”
Jones also leverages the experi ence she’s cultivated throughout her decades in the field of nursing in the classroom environment. For as much as things have changed since she entered her career, Jones pointed out that “the human inter action between nurse and patient is very much the same.”
“People still experience pain,”
she said. “That space where we en ter with them into their suffering, and try to help and support them, and have empathy — those needs are the same. How we do that, and how much time we have to do all that is different, but the basic nurs ing need for care in the midst of suffering, I think that’s the same.”
“Currently, the health care system is more complex today than it’s ever been,” she said. “We have much more technology available. The immediate care environment is much different, the acuity of care is different, the length of stay is much shorter. We’ve tried to push so much care outside of the hospi tal. The amount of time for us to do teaching in the hospital is less and less, and it’s harder to teach patients when they’re acutely ill.”
been, she said. To her, that’s reason enough for professionals in the nursing field to embrace an atti tude of lifelong learning.
“You have to keep learning because our world keeps changing,” Jones said. “We have new technology, and treatment modalities, and ways of thinking. If you want to be as helpful as you can, you have to keep learning. When you do that, it’s been my expe rience that good things happen.”
As a veteran nurse and educator, Jones is still frequently contacted for advice from colleagues as well as prior students; by the time she left Parkland, she noted, “many of the administrators there were people that I hired.”
“Now after all these years hav ing been faculty, many students will continue to reach out,” Jones said. “It’s nice to be able to help build the next generation, and to share lessons learned so they can benefit from my experiences.”
“Sometimes all they need is to talk to someone else who under stands and lets them process out loud, and make connections when people are ready to move,” she said. “That’s one of the reasons I love teaching right now: to be able to help someone else not have to struggle in the same way that I struggled, to pay it forward.”
To Jones, those changes are also underscored by the emergence of a much larger team of special ized health care workers, including discharge nurses, health coordina tors and patient navigators. Today’s nurses interact with more people to get the job done, use more technol ogy over a shorter period of time, and treat patients who are in many ways more educated than they’ve
When she’s not working, Jones loves spending time in her gar den, and is very active within her church. Her interests include reading, music and traveling. She has been a frequent participant in nursing associations, from the Texas Nurses Association and the Texas Organization of Nurse Executives to the Academy of Medical Surgi cal Nurses. She was inducted as a fellow in the American Academy of Nursing in October 2022.
December 2022 | OR TODAY 29 WWW.ORTODAY.COM
“I loved feeling like I made a difference in my patients’ lives.”
OUT OF THE OR health
Vitamin D Supplementation May Help Depressive Symptoms
A n extensive meta-analysis suggests that vitamin D supplementation may alleviate depressive symptoms in adults with depression. Conducted by an international team of researchers, the meta-analysis includes dozens of studies from around the world.
Depressive symptoms cause a significant disease burden worldwide. The therapeutic efficacy of current anti depressants is often insufficient, which is why further ways to alleviate the symptoms of depression have been sought, for example, from nutritional research.
Vitamin D is believed to regulate central nervous system functions the disturbances of which have been associated with depression. In addition, cross-sectional studies have observed an association between depres sive symptoms and vitamin D deficiency. However, previous meta-analyses on the effects of vitamin D supplementation on depression have been inconclu sive. In a meta-analysis, results from several different studies are combined and analyzed statistically.
The new meta-analysis on the association of vita min D supplementation with depression is the largest one published so far, including results from 41 studies from around the world. These studies have investigat ed the efficacy of vitamin D in alleviating depressive symptoms in adults by randomized placebo-controlled
trials in different populations. The studies included those carried out in patients with depression, in the general population, and in people with various physi cal conditions. The results of the meta-analysis show that vitamin D supplementation is more effective than a placebo in alleviating depressive symptoms in people with depression. There were major differences in the vitamin D doses used, but typically the vitamin D supplement was 50-100 micrograms per day.
“Despite the broad scope of this meta-analysis, the certainty of evidence remains low due to the hetero geneity of the populations studied and due to the risk of bias associated with a large number of studies,” doctoral researcher and lead author Tuomas Mikola of the Institute of Clinical Medicine at the University of Eastern Finland says. The meta-analysis is part of Mikola’s Ph.D. thesis.
“These findings will encourage new, high-level clinical trials in patients with depression in order to shed more light on the possible role of vitamin D supplementation in the treatment of depression,” Mikola concludes.

The meta-analysis was carried out in international collaboration between Finnish, Australian and U.S. researchers.
For more information, visit tandfonline.com/doi/full/10.1 080/10408398.2022.2096560.
30 OR TODAY | December 2022 WWW.ORTODAY.COM
OUT OF THE OR fitness
Rotation for Better Posture
By miguel j. ortiz
There are many things people do to try and improve their posture, most of which are more reminders than actual actions.

Common themes include standing up straight, rolling your shoulders back or lift your head up. And, although these reminders are helpful considering our day-to-day lives involve a lot of sitting, they don’t promote the actual behavior of creating better posture. The best thing we can do are movements that will influence quality change and ensure stabilization creating the quality posture we are looking for. Without practicing rotation with stabilization, the body won’t be able to maintain the posture were looking for. Here are three moves that will help lengthen the body and help stabilize the core to help improve posture.
The first move is an elevated pigeon and lean. This movement starts from the base of the hips as it loosens up the glutes and lower back. When doing this movement, you want to try and bring the opposite shoulder to the opposite knee which begins a light rotation all the
way from your lower back to your shoulders. The idea is lengthening before you begin to strengthen. We can’t improve our posture until we have started to open up our back. This is a great exercise to start doing that. I recommend doing about 2-3 sets of 6-8 reps per side, holding the stretch for about 3-5 seconds once you’re in your deepest range of motion.
The second move is a half kneeling rotation and reach. This is where flexibility and strength begin to meet. This movement challenges your shoulder blades and stabilization. Being in a half kneeling position gives the lower extremities an added stretch while helping to stabilize the hips – making it easier to rotate. The idea is to press into the ground to stabilize the upper body while reaching to the ceiling with the opposite arm. This provides great rotation to help open up the core and strengthens the spine, shoulder blades and upper back simultaneously. We also want to make sure our head is following our top hand which helps loosen up the cervical spine or neck. I recommend doing 2-3 sets of 6-8 reps per side.
Our last movement is a half kneeling torso rotation. This exercise brings everything together as it challenges hip and core stabilization, while going through the torso rotation needed to dial in upper body posture. Sometimes I will have clients go through this exact drill against a wall to help with stability because many people will bend instead of rotate and that completely changes the movement. Whatever you do, try not to bend. Stay as upright as possible and allow the free moving arm to guide you through the rotation. This will strengthen your core as well as your shoulders, allowing the back to open up to help build better posture. Do 2-3 sets with 6-8 reps per side.
Have fun with your movements and take your time developing stronger ranges of motion daily.
- Miguel J. Ortiz is a personal trainer in Atlanta, Georgia. He is a Master Trainer for Pain-Free Performance and a Certified Nutritional Consultant with more than a de cade of professional experience. He can be found on Instagram at @migueljortiz. You can find videos of the exercises mentioned in this column at tinyurl.com/ORTfitness.
December 2022 | OR TODAY 31 WWW.ORTODAY.COM
OUT OF THE OR EQ Factor
Skills of Empathetic Listening
By Daniel Bobinski
A lmost everyone in America has learned how to write, and many schools require a speech class. Therefore, it’s a safe bet that pretty much everyone in your workplace have been taught how to speak and write. But how many people have taken classes on listening skills?
In my decades of working with teams, I can count on one hand the number of people who took a listening class.
Considering that communication is a two-way street, it’s vital that the people with whom we’re communicating feel heard. In recent months I’ve written about the importance of seeking the other person’s perspective on things before offering your own, but how we do that makes a huge impact on communication success.
More specifically, it’s one thing to think we’ve understood someone, but it’s something very different for the other person to truly feel understood. For that reason, let’s take this opportunity to discuss empathic listening.
The levels of listening
Most people practice different levels of listening throughout the week. Ignoring, pretending to listen, selectively listening and attentively listening. We use different levels for different occasions. In Stephen Covey’s book, “The 7 Habits of Highly Effective
People,” Covey underscores the importance of empathic listening. It’s a deeper level of listening that tunes in beyond a person’s words. It’s seeking to understand a person’s deeper thoughts and feelings about a matter.
Is empathic listening required all the time? Absolutely not. But if someone has a serious concern or there’s an important workplace issue that’s being addressed, we must drop all autobiographical listening, which is listening from our point of view, and practice empathic listening – seeking to grasp someone else’s deeper thoughts and feelings.
This doesn’t mean we need to agree with what’s being told to us, nor does it mean we need to feel the same way as the other person. Empathic listening is simply seeking to understand someone else at a deep level, then conveying that understanding in a non-judgmental and considerate way.
Think of yourself as an interpreter
If you’ve ever communicated through an interpreter, you probably have a grasp of empathic listening. You can’t understand the speaker, so you are automatically tuned in more to the person’s voice tone and body language. Your brain tunes into the speaker’s intensity levels and emotions. Then, when the interpreter conveys the actual words, you can merge the words with what you observed. You do this because you want to be sure you understand the true meaning of
the communication.
Empathic listening with people who speak your own language works much the same way. One good technique for empathic listening is to go beyond someone else’s words and ask yourself, “What is the person thinking? What is the person feeling?” Is the person angry? Eager? Elated? Concerned? Then, when an appropriate break arrives, you can say something like, “It sound like you’re concerned about ‘X,’” or, “You seem pretty excited about ‘Y.’” The idea is to deeply understand where the other person is coming from. Again, you don’t need to agree with it, but good communication involves understanding the other person’s thoughts and feelings about a matter and conveying that understanding in a non-critical way.
Daniel Bobinski, who has a doctorate in theology, is a bestselling author and a popular speaker at conferences and re treats. For more than 30 years he’s been working with teams and individuals (1:1 coaching) to help them achieve excellence. He was also teaching Emotional Intelligence since before it was a thing. Reach him by email at DanielBobinski@ protonmail.com or 208-375-7606.

32 OR TODAY | December 2022 WWW.ORTODAY.COM



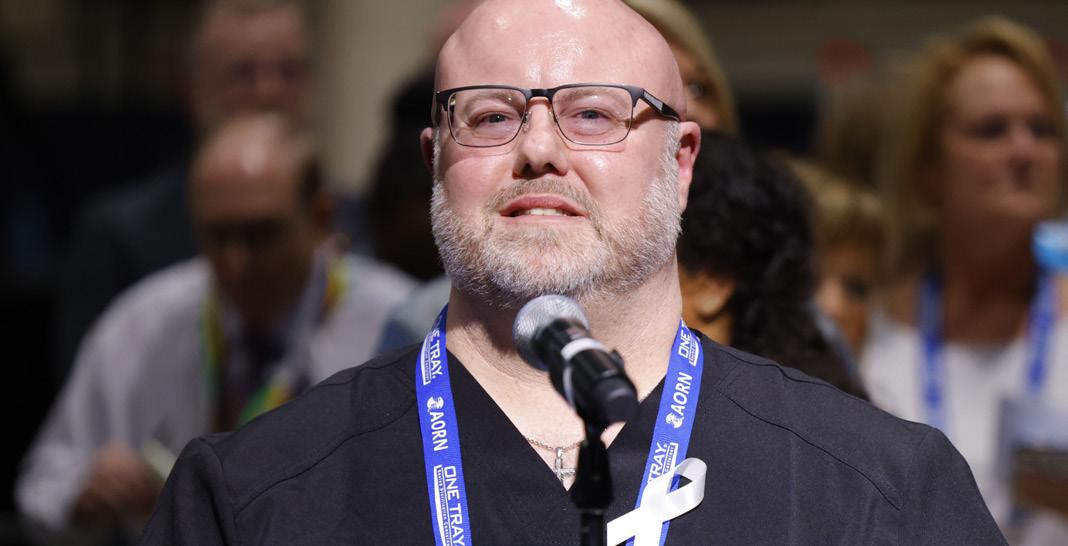


Get your contact hours, make lifelong connections, and re-energize with perioperative peers – all in one place. BOOK NOW. PAY LATER. CELEBRATION CONNECTIONS IMPACT INNOVATIONS HANDS-ON LEARNING INSPIRATION Change of plans? We got you. 100% Refunds Guaranteed BOOK WITH CONFIDENCE aorn.org/surgicalexpo S an A ntonio, T X Ap ril 1-4 , 2023
A Ferment Built for Winter
By KIRSTEN SERRANO
Recently, I taught a class about fermentation and told the group that fermentation is so easy that it seems like magic. Of course, there’s science behind the magic. The “magic” is actually industrious microbes getting to work. Naturally occurring microbes on the food and in the air convert carbohydrates into acid or alcohol – turning your cucumber into a pickle or your tea into kombucha, for example.
You have been benefiting from fermentation your whole life. In fact, humans have been using microbes to ferment foods since at least 7000 BC. You are probably eating fermented foods daily because fermented foods include beer, vanilla, coffee, cheese, chocolate, wine, yogurt, bread and much more. Fermentation preserves food, makes it more digestible, increases nutrient levels and
creates amazing flavors. However, not all foods that are fermented in their preparation contain live microbiotic cultures when we digest them.
What we didn’t know until just the past 20 years or so is how dependent we are on those live microbes for our health. Active, living fermented foods are full of microbes we call “probiotics.” These probiotic-rich foods help to populate our gut microbiome (the microbial life in your intestinal tract.) Our gut microbiome is responsible for digestion, most of our immune system and even make many of the neurotransmitters that run our brain! We can all benefit from eating more foods rich in active probiotics.
I have an easy and delicious way to enjoy a winter ferment and it deserves a spot alongside your winter meals. My family adds it to our Thanksgiving and Christmas meals. Regardless of whether you are a cranberry fan or not, I urge you to try fermenting them
in honey. All you need are fresh or frozen cranberries, honey and (optional) aromatics of your choice. You can choose to add ginger, orange (as sections with some peel or orange juice,) cinnamon sticks, star anise pods, cardamom pods, whole cloves, vanilla bean, etc.
With a ferment, thinking ahead is key. You want to give your ferment a minimum of 3-4 weeks fermentation time before serving. You can ferment it longer if you choose. You can store it for even longer – up to a year. One of the magical gifts of fermentation is its power of preservation.
Fermenting cranberries is a simple four-step process. First, prep your berries. You need to pierce their skins. Instead of painstakingly piercing each one, I use a fork to stab them en masse. Next, add your berries and aromatics to a glass or ceramic upright vessel. I use Mason jars and my favorite add-ins are slices of ginger, cinnamon sticks and a squeeze of orange juice. Cover with honey. You may need

34 OR TODAY | December 2022 WWW.ORTODAY.COM
OUT OF THE OR nutrition
OUT OF THE OR nutrition












to do that in stages – allowing honey to settle between berries before adding more. Leave some headspace at the top of the jar – an inch or so. Last, you need to cover them but do not add an airtight lid. The fermentation process produces gas and that needs to escape. The easiest options are to loosely put a lid on or cover with cloth and a rubber band. You can also buy inexpensive lids designed for fermentation that fit Mason jars. I highly recommend them.
Now, you can stand back and watch the magic. Leave your ferment out where you can keep track of it but not in bright light (avoid windows.) In a few days, you will start to see bubbles and that is how you know the magic is happening. You may even have some of the liquid honey run over the sides of the jar. That’s no big deal and even a sign of a healthy ferment. Just clean up what spills. The honey will become red from the berries and become runny. Once your ferment is done, you can enjoy them just as they are. I like to keep the ginger, remove the cinnamon sticks, and add them to a food processor with some fresh orange (add
some peel too!) and walnuts to make a chunky relish. Add as much of the liquefied honey as you like. Don’t throw out that runny honey. It’s teaming with healthy probiotics!
Once you have tried the honey fermentation process, expand your repertoire. Everything from peppers to other berries and even garlic can be fermented. Fermenting in honey will open the door to exploring more ferments.
Kirsten Serrano is a nutrition con sultant, chef, farmer, food literacy educator and the best-selling author of “Eat to Your Advantage.” You can find out more about her work at SmallWonderFood.com.

December 2022 | OR TODAY 35 WWW.ORTODAY.COM
Need Pump Support? Trust the Experts. 753E 877.266.6897 aiv -inc.com NEW! Current Monitoring Dual-Rated Special Purpose Relocatable Power Tap

www.ORToday.com MAGAZINES SPECIAL OFFERS WEBINARS CONFERENCE UPDATES AND MORE! TAKE GOOD CARE: NURSES • SURGICAL TECHS • NURSE MANAGERS and get a first look at:
Periop Pros Praise Georgia Council Meeting

staff report
The Georgia Council of perioperative Registered Nurses teamed up with OR Today for the second consecutive year to host its annual meeting. It was held at the Atlanta Evergreen Lakeside Resort. The popularity of the meeting and positive feedback from attendees and exhibitors exceeded all expectations!
A sold-out exhibit hall featured 37 perioperative companies with almost 100 booth personnel on hand to answer questions and deliver insights regarding their products and solutions. In addition, 135 perioperative professionals from throughout the United States registered to attend. Some attendees traveled from California and Connecticut for the annual meeting after seeing the education and exhibits that would be at the event. Attendees also included several AORN board members and board member candidates. Sponsors Stryker, Aerobiotix and ConMed added to
the value of the annual meeting with networking events, door prizes and an outstanding keynote addresses. Attendees could earn up to 5.5 CE credits approved by OR Today, a licensed Continuing Education Provider with the State of California Board of Registered Nursing. License #16623
MD Publishing, the parent company of OR Today, enjoyed being able to help host the annual meeting and give back to the important perioperative professionals who sometimes go unnoticed. MD Publishing Vice President Kristin Leavoy, CMP, said it was a great event. She could not be happier after receiving overwhelmingly positive feedback from almost everyone who attended.
The Georgia Council of perioperative Registered Nurses Annual Meeting is quickly becoming a can’t miss event.
“I visited with more people today than I did all last week at the OR Manager conference,” shared Eric Brown from C Change Surgical.
“I met an attendee here at the conference who is placing an order that will cover the cost of our participation at the event and ensure that we return for years to come,” Skytron/Surgical Specialties of Georgia’s Matthew Nichols said.

“It had been a while since we have had fantastic face-to-face conversations with attendees and we will definitely be coming back next year,” said Michelle Daniels from Encompass Group.
Tracey Young, MSN, Registered Nurse, University of Pittsburgh Medical Center, attended the meeting. She has been working on her dissertation and after struggling to find additional information she made a connection at the meeting that will enable her to move forward. She will now be able to complete her dissertation.
“It is an absolute blessing, and I am so thankful to be here,” Young said.
For more information , visit gacouncilnurse.org.
December 2022 | OR TODAY 37 WWW.ORTODAY.COM
recap Georgia Council
SCRAPBOOK Georgia Council

SCRAPBOOK
he Georgia Council of perioperative Registered Nurses Annual Meeting powered by OR Today was held at the Atlanta Evergreen Lakeside Resort. The meeting featured a sold-out exhibit hall with 37 perioperative companies repre sented by almost 100 booth personnel to answer questions





and share insights regarding their products and solutions. In addition, 135 perioperative professionals from throughout the United States registered to attend. Some attendees traveled from as far away as California and Connecticut for the annual meeting. For more information, visit gacouncilnurse.org.

38 OR TODAY | December 2022 WWW.ORTODAY.COM
1 3 4 2 T 6 5 7
SCRAPBOOK Georgia Council
1. The Georgia Council was kicked off with a welcome reception and vendor networking event, sponsored by Stryker.
2. The exhibit hall was filled with exceptional booths representing companies from all over the country.
3. Attendees were given the opportunity to earn up to 5.5 CE credits over the course of 2 days.


4. Exhibitors jumped at the opportunity to interact with a record attendance at Georgia Council.


5. Guests settled in for the highly anticipated Keynote presentation, sponsored by Aerobitox.
6. OR Today’s Emily Hise pictured at the registration desk
where she helped check in over 130 attendees. 7. Skytron/Surgical Specialties of Georgia’s Mathew Nicols. 8. OR Today’s Kristin Leavoy after a quick interview with Tracey Young, MSN, Registered Nurse. 9. Attendees had the chance to enjoy some lunch in the exhibit hall sponsored by Stryker.
10. Erica Basora presenting about her journey to self-publishing night one.
11. Attendees getting to sit in on Surgical Smoke Implementation Plan to Effect Practice Change, Sponsored by CONMED.
December 2022 | OR TODAY 39 WWW.ORTODAY.COM
9 10 11 8
OUT OF THE OR recipe Recipe the
Garlic Mashed Potatoes: INGREDIENTS:
• 2 pounds russet potatoes, medium diced, skin on
• cold water
• 1 teaspoon kosher salt, plus 1 pinch, plus additional, to taste, divided
• 1/2 pound unsalted butter
• 4 cloves garlic, minced
• 1 cup heavy cream
• 1/2 teaspoon ground white pepper, plus additional, to taste, divided
Honey-Lemon Glazed Carrots:
INGREDIENTS:
• 2/3 cup honey
• 1/4 cup fresh-squeezed lemon juice
• 1/2 teaspoon sumac
• 1/4 teaspoon lemon zest
• 2 pinches kosher salt, plus additional, to taste, divided
• 1 pinch ground black pepper, plus additional, to taste, divided
• water
• 1 pound baby rainbow carrots
• 1/3 cup olive oil
• 1 tablespoon unsalted butter
Sumac-Crusted Filet Mignon:

INGREDIENTS:
• 4 Omaha Steaks Private Reserve Filet Mignons (7 ounces each)
• 2 tablespoons kosher salt
• 1 tablespoon sumac
• 2 teaspoons ground black pepper
• 1 teaspoon dried thyme leaves
• 1/3 cup grapeseed oil
• 3 tablespoons unsalted butter, divided
40 OR TODAY | December 2022 WWW.ORTODAY.COM
By family features
OUT OF THE OR recipe
Start a Holiday Tradition with Tender Steaks
reating traditions is a festive focal point for many families throughout the holiday season, and a timeless way to bring your nearest and dearest back year after year is with an exquisite meal.
C
With a combination of savory, salty and sweet bites, Sumac-Crusted Filet Mignon with Honey-Lemon Glazed Carrots and Garlic Mashed Potatoes provides a little something for everyone. At the center of this seasonal feast is tender, flavorful cuts of filet mignon, hand-cut by master butchers at Omaha Steaks to make your family’s holiday truly special.
To find more holiday recipe inspiration, visit OmahaSteaks.com/Blog.

Sumac-Crusted Filet Mignon with Honey-Lemon Glazed Carrots and Garlic Mashed Potatoes
Servings: 4
1. To make garlic mashed potatoes: Add potatoes to stockpot. Cover with cold water by about 1 inch and add 1 pinch salt. Turn on high heat and bring to boil 12-15 minutes, or until fork tender. Drain and place potatoes in large mixing bowl.
2. In saucepan over medium heat, melt butter. Add garlic and simmer 5 minutes. Add heavy cream, 1 teaspoon kosher salt and 1/2 teaspoon white pepper; bring to boil. When mixture boils, reduce to simmer 3 minutes then remove from heat.
3. Mash hot potatoes until most lumps are gone. Using hand mixer on low speed, slowly add butter and cream mixture until desired smoothness and taste.
4. Season with salt and white pepper, to taste.
5. To make honey-lemon glazed carrots: In small bowl, whisk honey, lemon juice, sumac, lemon zest, 1 pinch salt and 1 pinch pepper.
6. Preheat oven to 425 F.
7. Fill stockpot 2/3 full with water. Bring to boil and add 1 pinch salt. Blanch carrots in boiling water 5 minutes. Drain and shock with cold water. When cool enough to handle, halve carrots lengthwise.
8. In large saute pan over medium-high heat, add oil and butter.
9. Add carrots to pan, flat sides down, and season with salt and pepper, to taste. Sear until browned, about 2 minutes.
10. Flip carrots and season with salt and pepper, to taste. Add half of glaze to pan and glaze generously. Bake 3 minutes. Add remaining glaze to carrots and bake 2 minutes. Remove glazed carrots from oven.
11. To make sumac-crusted filet mignon: Thaw filet mignons in refrigerator overnight, pat dry with paper towels then bring to room temperature 30 minutes.
12. In small bowl, whisk kosher salt, sumac, black pepper and dried thyme. Season steaks on all sides.
13. In cast-iron pan over high heat, add grapeseed oil.
14. Place filets in pan and cook 4 minutes until browned and seared. Add 1 tablespoon butter to pan.
15. Flip filets and butter baste about 20 seconds. Cook filets 3 minutes for medium-rare.
16. Remove filets from pan and top each with 1/2 tablespoon butter. Rest steaks 7-8 minutes.
17. Place garlic mashed potatoes on plate and top with sumac-crusted filet mignon. Place honeylemon glazed carrots next to filet mignon and mashed potatoes.
December 2022 | OR TODAY 41 WWW.ORTODAY.COM
INDEX advertisers
ALPHABETICAL
AORN 33
AIV Inc. 35
ALCO Sales & Service Co. 19
C Change Surgical 17
CATEGORICAL
ANESTHESIA
Soma Technology 11 ASSOCIATION
AORN 33 C-ARM Soma Technology 11
CARDIAC PRODUCTS
C Change Surgical 17
CARTS/CABINETS
ALCO Sales & Service Co. 19 Cygnus Medical 44 Healthmark Industries Company, Inc. 5 TouchPoint Medical 9 CS/SPD
MD Technologies Inc. 4 Ruhof Corporation 2
DISINFECTION
Cygnus Medical 44 Ruhof Corporation 2
DISPOSABLES
ALCO Sales & Service Co. 19
ENDOSCOPY
Cygnus Medical 44
Healthmark Industries Company, Inc. 5 MD Technologies Inc. 4 Ruhof Corporation 2
FALL PREVENTION
ALCO Sales & Service Co. 19
FLUID MANAGEMENT
MD Technologies Inc. 4
Cygnus Medical 44
Healthmark Industries Company, Inc. 5
I.C. Medical, INC. 43 MD Technologies Inc. 4
OR Today Webinar Series 13
Ruhof Corporation 2 Soma Technology 11 TouchPoint Medical 9
GENERAL
AIV Inc. 35
HOSPITAL BEDS/PARTS
ALCO Sales & Service Co. 19 INFECTION CONTROL
ALCO Sales & Service Co. 19 Cygnus Medical 44 Healthmark Industries Company, Inc. 5 MD Technologies Inc. 4 Ruhof Corporation 2
INSTRUMENT STORAGE/TRANSPORT
Cygnus Medical 44 Ruhof Corporation 2
MONITORS
Soma Technology 11 ONLINE RESOURCE
OR Today Webinar Series 13 OR TABLES/BOOMS/ACCESSORIES
Soma Technology 11
OTHER
AIV Inc. 35
PATIENT MONITORING
AIV Inc. 35
POSITIONING PRODUCTS
Cygnus Medical 44
REPAIR SERVICES
Cygnus Medical 44 Soma Technology 11
REPROCESSING STATIONS MD Technologies Inc. 4
Ruhof Corporation 2 RESPIRATORY Soma Technology 11
SAFETY Healthmark Industries Company, Inc. 5 SINKS Ruhof Corporation 2
SMOKE EVACUATION
I.C. Medical, INC. 43
STERILIZATION
Cygnus Medical 44 Healthmark Industries Company, Inc. 5 MD Technologies Inc. 4
SURGICAL
MD Technologies Inc. 4 Soma Technology 11
SURGICAL INSTRUMENT/ACCESSORIES
C Change Surgical 17 Cygnus Medical 44 Healthmark Industries Company, Inc. 5
TELEMETRY AIV Inc. 35
TEMPERATURE MANAGEMENT
C Change Surgical 17 WASTE MANAGEMENT
MD Technologies Inc. 4
42 OR TODAY | December 2022 WWW.ORTODAY.COM










FREE PenEvac® SAMPLE REGISTER TODAY! www.icmedical.com/free-sample or call 623.780.0700 for a FREE DEMO. 623.780.0700 www.icmedical.com 30 30 years BUSINESS OVER Earn Two FREE CE Credits Online! FREE CEU Download Live & Virtual CE Presentations available upon request.








TM





























































































 BY DON SADLER
BY DON SADLER