MEDICAL IMAGING AND THE QUADRUPLE AIM
PAGE 30
PRODUCT
FOCUS ULTRASOUND SYSTEMS PAGE 25















PAGE 30
FOCUS ULTRASOUND SYSTEMS PAGE 25















Kenneth Saltrick, President of Engineering Services in Twinsburg, Ohio, knows from his long experience that C-arm machines themselves are absolute workhorses.
For customers looking to blend the gap between expensive OEM and unreliable used assemblies, WE have your solution.
Our complete repair contains a new cable assembly, utilizing all OEM cable and components with a harvested plate and connector housing as they are proprietary items. These completely repaired products will have a significant cost savings with build quality above new OEM products and carry a warranty of 180 days, which is untouchable in the market.


Phase 1: MRI Safety
Phase 2: MRI Fundamentals
Phase 3: Operational & Clinical Principles of MRI
Phase 4: MRI Service Essentials

Phase 5: System OS - syngo Classic or Native
Phase 6: System Courses
Aera/Skyra Avanto/Espree
Our 2023 Imaging Training Academy course matrix has been designed to give you a complete overview of what an individual would need to become an expert on any medical imaging system. We offer training solutions that will help take your career to the next level! No matter what stage of yourcareer, you can sign up for any course on this matrix.
Not sure what course to take? Call us today for your free assessment and speak to one of our National Technical Support engineers or Instructors to learn what course would be best for you!
Phase 1: X-Ray Safety
Phase 2: CT Fundamentals
Phase 3: Operational & Clinical Principles of CT
Phase 4: CT Service Essentials
Phase 5: System OS - syngo Classic or Native
Phase 6: System Courses
Definition (AS, Flash, DS) E-Line (Scope, Emotion, Perspective) Sensation Somatom Go
Phase 1: X-Ray Safety
Phase 2: RF Fundamentals
Phase 3: Operational & Clinical Principles of X-Ray
Phase 4: RF Service Essentials
Phase 5: System OS - Fluoro Spot Compact
Phase 6: System Courses
Cios-Alpha-Fusion Luminos Agile Multix Top Pro
Uroskop Omnia Ysio/Ysio Max
Phase 1: NM Safetv
Phase 2: NM Fundamentals
Phase 3: Operational & Clinical Principles of NM
Phase 4: NM Service Essentials
Phase 5: System OS - e.Soft
To learn more, check out our Training Page located on our website or contact our Sales Team today!
Phase 6: System Courses
e.Cam Symbia
Phase 1: X-Ray Safety
Phase 2: Angio Fundamentals
Phase 3: Operational & Clinical Principles of X-Rav
Phase 4: Angio Service Essentials
Phase 5: System OS - syngo Classic or Native
Phase 6: System Courses
Artis Zee/Artis Zee Max Pheno Icono Q/Q.Zen
877.604.6583 / 920.757.6583 training@technicalprospects.com www.technicalprospects.com
Phase 1: Electrical Safety
Phase 2: Ultrasound Fundamentals
Phase 3: Operational & Clinical Principles of US
Phase 4: Ultrasound Service Essentials
Phase 5: System OS - syngo Classic or Native
Phase 6: System Courses
Acuson Sequoia


















When is an open-door policy not an open-door policy?
In 2017, calls from the world of health care resulted in the idea of a Quadruple Aim system, one that would incorporate an additional goal that varied according to the institution proposing it.

Rachel Ammons is “a dedicated imaging professional who routinely goes above and beyond to help out in the radiology department.”


Catch up on the latest news from around the diagnostic imaging world.

A look at some of the top ultrasound systems and a booming market.


AHRA President Brenda DeBastiani shares updates on the organization.
We deliver an inside advantage you can’t get elsewhere:
We deliver an inside advantage you can’t get elsewhere:
• Int er nal su ppl y c hai n su ppo rti n g hund re ds of ul tras ound pro b es a nd MRI c oil s
• Int er nal su ppl y c hai n su ppo rti n g hund re ds of ul tras ound pro b es a nd MRI c oil s
• Engi n eer in g ex pe r tise in cl ud es tra nsd u cer
• Engi n eer in g ex pe r tise in cl ud es tra nsd u cer ar r ay s, pl as ti c m oldin g, 3 D pri n ti n g, ca bl e harne ss fabrica ti on , a nd pr ec ision len s es
ar r ay s, pl as ti c m oldin g, 3 D pri n ti n g, ca bl e harne ss fabrica ti on , a nd pr ec ision len s es
• Repair proc e sses info rme d by ou r le gacy in FD A reg is tere d ma nuf act uri n g
• Repair proc e sses info rme d by ou r le gacy in FD A reg is tere d ma nuf act uri n g
MORE R EAS ONS THAN E VER T O EVER T O INSIST ON INNOVATUS IMAGING IN SIDE! Get the inside scoop at booth 400 at MDExpo this April
MORE R EAS ONS THAN E VER T O EVER T O INSIST ON INNOVATUS IMAGING IN SIDE! Get the inside scoop at booth 400 at MDExpo this April
@
@
customercare@innovatusimaging.com
customercare@innovatusimaging.com
844.687.5100
844.687.5100
innovatusimaging.com
innovatusimaging.com


Debra M. Schultz is the twin sister of last month’s In Focus feature and worthy of her own article as the Senior Training Developer/Subject Matter Expert for the U.S. Army Radiology Specialist Program MOS 68P.
She holds a bachelor’s in general studies from Texas Woman’s University (TWU) as well as Master of Science in Health Science: Healthcare Management. She is currently a Sergeant First Class in the United States Army.
Schultz and her sister, Laurie Fross, were nominated by VA Puget Sound Health Care System Health Systems Specialist-Strategic Planner John Beall.
“I just think it would be a cool, feel-good story of a family duo serving the country while also being part of our imaging community and two of the nicest people I have ever met,” Beall said.
“I have two sisters and a brother. I am incredibly close with my twin sister, Laurie, and we talk every day. She is my confidant and best friend.
I am a single mom to an amazing young man, Jordan, who is almost
9. Unfortunately, both of my parents have passed away,” Schultz explained.
Schultz began her Army career after earning a bachelor’s degree.

“I joined the Army in June 2005 as an X-ray tech; I was working as a student athletic trainer at TWU. I wanted to join the Army since I graduated high school, however my dad pushed me to get a college degree,” she explained. “I still wanted to join the Army – especially after 9/11 – so after college graduation I decided to join the Army. I wanted to stay in the medical/health care field as I did with athletic training. I enjoyed taking care of the athletes and radiology seemed like a field I would be interested in.”
“I loved learning about the human body in my undergrad with all of the kinesiology studies, so X-ray seemed like a good job,” Schultz added.
When asked about her greatest accomplishment, Schultz answered in a way that highlights the importance of family.
“My greatest accomplishment is two-fold. Being a parent has been one of the greatest accomplishments I have had. Not just being a parent, but proving that I can be a leader in the Army and doing so
successfully as a single parent. I have an amazing village to help me care for my son, to include my sister Laurie, who has travelled down to San Antonio to help care for him while I continue to serve in the Army,” Schultz said.
“Additionally, serving in the military and affecting hundreds of people has been an amazing accomplishment. I currently sit in an instructor role as the senior training developer, but throughout my career, I have been able to affect so many soldiers and officers through developing relationships, being a mentor, friend and just listening. I learned that to be a great leader, I have to also be a great follower and a great peer. Watching the soldiers I have worked with ‘grow up’ throughout the Army and see their accomplishments is what motivates me to keep putting on the uniform every day,” she added.
Another reason she puts on the uniform every day is because she loves her job.
“I love my job because I have the ability to affect people on a level that is not just at the surface. Those that I have come across throughout my career, take what I have taught them or mentored them on and pass it on to their soldiers and the cyclical effects of that has only improved the radiology program in the Army. I have had the privilege to be mentored by some amazing people and
sharing that information, guiding soldiers, and seeing the improvements that have been made make it worthwhile,” Schultz said.
When asked to share more about her leadership style, Schultz explained that she tries to get to know everyone on her team and listen to their feedback.
“When I am approaching leadership, the first step I take is to get to know everyone I will be working with. While there are titles and positions of leadership, we all work together to achieve whatever end state we have established,” she said. “I feel it is incredibly important for me, as a leader, to earn the respect and confidence of my team, be transparent with them, know my own weaknesses and strengths and act more as a peer than a leader. I’ll be the first one in the room to admit I don’t know something, and I always ask a ton of questions.”
The art of asking questions has paid dividends thanks to some great mentors who have assisted Schultz with her imaging career.
“SFC Eddie Perales is one of my mentors. He is a senior radiology technologist, but above all an amazing human being. SFC Perales showed me the tools to reach my potential. He ‘showed me doors’ that I chose to walk through which skyrocketed my career. I trust his opinion and he never backs down from
1. What is the last book you read? Or, what book are you reading currently? I’m currently reading the Lean Six Sigma Pocket Book and the Five Love Languages of Children. The first book is towards my goals of what I want to do when I get out of the military and the second is so I can better understand my son’s love language so I ensure I am filling his tank every day. Having him take the love language quiz really opened my eyes to what he wants from me as his parent and I’m loving this new journey we are on.
2. Favorite movie? “Shawshank Redemption”
3. What is something most of your coworkers don’t know about you? That I grew up in a broken household with lots of childhood trauma
telling me the truth. He never let me back down from a challenge yet guided me towards the finish line,” she said.
“Major Jordan Gammons is another mentor of mine. I first met her as my company commander in 2013 at Fort Stewart, Georgia and she has been an amazing leader to confide in. Major Gammons assisted me as a mentor and leader through the passing of my father and the challenge of military demands as a new mother,” Schultz added. “Major Gammons has always supported my dreams and gives me amazing advice.”
“The hardest lesson that I learned in the military and as an adult is to put myself in uncomfortable situations. However, being uncomfortable has provided me the most amazing growth and success throughout my career,” she added.
When asked what she would want to share or pass on to the next leader, Schultz reminds everyone that we are all alike.
“I think it’s important to remember to be humble, self-aware, transparent, and always admit when we’ve made mistakes,” she said. “We’re human, but we can’t forget that there are thousands of other humans around us most likely going through the exact same challenges we are.” •
4. Who is your mentor? SFC Eddie Perales
5. What is one thing you do every morning to start your day? Look at positive affirmations that I have taped to my bathroom mirror
6. Best advice you ever received? Slow down and enjoy the moments you are in because you will never get them back and time is the most valuable thing you can give to anyone.
7. Who has had the biggest influence on your life? My father
8. What would your superpower be? I don’t want a superpower. I don’t like being in the center of attention and if I can help change people’s lives by being a role model or an ear to listen, then I’m content.
9. What are your hobbies? Baking, swimming, cycling, reading, playing with my son
10. What is your perfect meal? The company that comes with the meal is what makes it perfect.
Cap your imaging parts expenses.
WHAT IS A CAPITATED PARTS COVERAGE (CPC)?
• Unlimited coverage of all parts and X-ray tubes
• Certified Pre-Owned Glassware
• Includes Technical Support and System Training
• Forward Stocking
WHAT ARE THE BENEFITS TO OUR CUSTOMERS?
• Cap risk on parts expenses
• Improved access to parts & tubes
• Faster access to critical parts with our forward stocking locations
Under our unique Capitated Parts Coverage (CPC), you will have unlimited parts and glass coverage for your imaging equipment. You will also receive premium access to our technical support team and technical training classes.
Call us today to learn more.

As a large health care system with both academic and community hospitals, we have always had our “go-to” radiologists and technologists to lean on. Anytime we had a questions about protocol, practice, or equipment, we would turn to these individuals. However, we consistently heard from both professional and technical teams that there was a need to place structure around these groups of “go-tos.” Academic and community teams often practiced in different circles with different workflows and that was problematic. A need for standardization by modality regardless of location and need for modality education were opportunities highlighted in our efforts to function as one system. This feedback resulted in developing Modality Triads.
While the name is a little deceiving, as there are often more than three individuals in each Triad, these small groups of academic and community radiologists, technologists and physicists provide the clinical and technical expertise to ensure each modality has a team guiding clinical practice across our system. In addition to these three components, our Triads also consist of radiology managers, team leads and our radiology IT team. We have one radiology manager assigned to each Triad who holds them together by facilitating meetings, ensuring questions posed to the Triad are answered/projects move along, escalating issues as needed, and tracking the work done. Our team leads are techs identified as on-site points of contact who receive updates and communications from the Triads and are responsible for disseminating this information to their on-site teams. In addition, they (as well as anyone in radiology) can reach out to the Triads when issues or questions come up locally. And finally, Radiology IT is engaged as a close partner with each Triad as many projects or workflows require IT participation.

Over the course of this first year, our Modality Triads have been developed with an accompanying SOP that guides their roles and responsibilities. Over time, the Triads have become
more defined. We anticipate their continued growth and participation in many upcoming initiatives.
Important things to consider/lessons learned when developing/implementing Triads:
• Be intentional when selecting team members – consider participation based on structure and ensure physics and IT participation.
• Don’t prescribe meeting cadence or communication as each Triad may have different needs. We wanted our teams to perform based on what was needed for their particular modality. We only have prescribed meetings to meet regulatory compliance, i.e. CT protocol review.
• Have a tool for tracking work performed. Having a tracking tool at the start will help the Triads stay organized. Some modalities were inundated from the moment they were created. This tracking tool would have been very helpful.
• Communicate initially and send reminders that Triads are out there. It is important to remind all radiology teams our Triads exist and how they can be reached. Outlook distribution lists were a helpful tool to make communication easy. Take every opportunity to engage the Triads with decision-making, developing SOPs/workflows, equipment reviews, education. If they are out of site, they will be out of mind.
• Leadership support and follow up is critical. As we are rounding our first anniversary of our Triads, we are taking time to meet with the Triad managers to review this year and prepare for 2023. We want to ensure they have what they need, how we can improve what they do, and how they are best supported.
Celebrate! The Triads have taken on additional responsibilities and have provided support and guidance for our entire radiology service line. We need to recognize their efforts and celebrate their successes. Use communication tools such as your department newsletter to recognize their work. •
Madison Hospital Radiologic Technologist Rachel Ammons, ARRT, is this month’s Rising Star. The Alabama native grew up in Springville before attending college at Southern Union State Community College in the small town of Wadley.

Ammons was nominated for this article by Madison Hospital Director of Imaging and Cardiopulmonary Vaughn Eason.
“Rachel is a dedicated imaging professional who routinely goes above and beyond to help out in the radiology department at Madison Hospital. During staffing shortages, she has eagerly stepped up to work long hours and she mentors staff and students with ease,” Eason wrote in his nomination. “Rachel has inspired leadership to develop a career mentorship and professional development program to help imaging professionals achieve their goals.”
ICE found out more about this Rising Star in a recent interview.
Q: WHERE DID YOU GROW UP? OR, WHERE ARE YOU FROM?
A: Springville, Alabama
Q: WHERE DID YOU RECEIVE YOUR IMAGING TRAINING/ EDUCATION? WHAT DEGREES/CERTIFICATIONS DO YOU HAVE?
A: Southern Union State Community College; ARRT certified.
Q: HOW DID YOU FIRST DECIDE TO START WORKING IN IMAGING?
A: I have always been interested in the medical field and once I took anatomy, I realized everything about bones fascinated me.
Q: WHY DID YOU CHOOSE TO GET INTO THIS FIELD?
A: I love to help people and taking X-rays is interesting to me.

Q: WHAT DO YOU LIKE MOST ABOUT YOUR POSITION?
A: The challenge of taking different X-rays all the time.
Q: WHAT INTERESTS YOU THE MOST ABOUT THE IMAGING FIELD?
A: Broken bones and unique stories on how it happened.
Q: WHAT HAS BEEN YOUR GREATEST ACCOMPLISHMENT IN YOUR FIELD THUS FAR?
A: I am the clinical instructor for radiology students.
Q: WHAT GOALS DO YOU HAVE FOR YOURSELF IN THE NEXT 5 YEARS?
A: To further my education and get my bachelor’s degree. •
FAVORITE HOBBY: Running
FAVORITE SHOW: “The Office”
FAVORITE FOOD: All things breakfast related.
FAVORITE VACATION SPOT: Anywhere at the beach
1 THING ON YOUR BUCKET LIST: To go to the Maldives one day and stay in an over-the-water bungalow.
SOMETHING YOUR CO-WORKERS DON’T KNOW ABOUT YOU: I have been stung by a scorpion.
When Jason Szmania first enrolled in a karate class, he was a middle-schooler whose parents wanted him and his brother to have something to keep them out of trouble until they were old enough for high school sports. Szmania enjoyed it well enough, but by the time football and wrestling came around, martial arts had fallen by the wayside.
In hindsight, he regretted not completing his training, but never gave as much thought to going back for a black belt despite his appreciation of the discipline. It wasn’t until almost 20 years ago, when a dojo opened up down the road from his workplace in Elyria, Ohio, where Szmania was a clinical coordinator for nuclear medicine, that he found his way back.
“One of my nuclear students told me about a dojo that had opened up,” he said. “We were going together, and then he dropped out, but I kept going. I really wanted to go back to just keep active and get in shape.”
“It was a great experience I began as a youth,” he said. “I wished I’d continued that then. The class that we were going to, it was a mix of everything – stand-up fighting, wrestling, throws – that perfectly evolved into a hapkido class. I thought it might be a good thing to unwind after a long week or a stressful day. It teaches you to improve your focus.”
Despite the years that had passed between his introduction to martial arts and his reconnection to it, Szmania set himself back on the path he’d left behind as a teen pretty quickly. Not only did he earn a first-degree black belt in hapkido, but Szmania kept going all the way to his fourth-degree black belt, the mastery level. Between each successive degree, which is awarded only after a test, there are years of group study and individual training. Last year, his school surprised him with a
fifth-degree presentation, an honor reserved only for a master of exceptional polish. Szmania described it as “a humbling experience” that acknowledged his years of commitment.
“Some folks have to go overseas to get that level,” he said; “I never was out to get to this level. Now I’m just thrilled that I can continue and help teach folks.”
Szmania continues to help train new students at his school, Tiger Martial Arts of LaGrange, Ohio, in grappling, jiujitsu, and hapkido, a form that combines joint locks, throws, grappling, and striking. Every weekend, he teaches two classes, usually grappling or jiujitsu; hapkido is typically by invitation only, which Szmania said is a safety consideration.
“Hapkido means ‘the art of power in coordination,’ ” Szmania said. “It’s a big brother to tae kwon do. Besides the kicking and punching, you’re putting in joint locks, ground work, and grappling. It’s one of the original mixed martial arts.”
“[Because of its intensity], we want to make sure that we’re getting the right students in there that can handle this type of teaching,” he said. “You’re only as good as the partner that you’re working with. Your partner can really help you out a lot, especially as you’re learning to throw others. We want to teach the proper techniques and the safety aspects.”
After nearly 20 years of experience in the martial arts, Szmania said he’s come to enjoy teaching as much as he did practicing the forms as a student. It squares with his lifelong love of learning, and affords a chance for him to impart lessons not only about the disciplines he’s teaching, but also the mindset that corresponds with it: of adaptation, adjustment and acclimation to new modes of being.

“As a student, the biggest thing I try to take away is showing respect while you’re learning,” Szmania said. “Really try to focus on trying to do the proper techniques and understanding the meaning of what’s going on in the class.”
“In teaching, you become the person that a lot of folks will look to,” he said. “You’ve got to be able to think out-
side the box. Sometimes people aren’t as flexible as they once were in their younger days; you’ve got to come up with different avenues to get to that endpoint. Don’t say no; there’s always a way to solve the problem.”

In finding his form as an instructor, Szmania leans on the work done by his predecessors, some of whom helped with a first draft of a hapkido manual that he still uses today. Last month, he had the honor to test a master who wrote that manual with another elder master from his school. Opportunities such as these were beyond his imagination when Szmania first resumed his martial arts classes.

“I’m really glad I went back,” he said. “Out of all my hobbies, this is one of my favorites. When you come home, and you’re pooped out, or you’ve got sore muscles, you feel just rejuvenated. I’ve learned a lot just going through this.”
“You start off at that white belt level, and you’re seeking all the knowledge, and trying to pick the brains of everyone there,” Szmania said. “You start to evolve, and you keep on learning. Now, teaching, you learn to adapt your teach-
ing styles to the students you have; you have to be creative.”
Creativity and patience are equally valuable in Szmania’s role as a martial arts instructor as they are in his leadership role as radiology manager at University Hospitals Samaritan Medical Center of Ashland, Ohio. Both positions demand a significant degree of concentration and coordination, the ability to communicate complicated information across a team of individuals, and a dedication to precise outcomes.

“Working in a hospital sometimes you can have several different things thrown at you,” he said. “What are your priorities?”
“I think the biggest thing I’ve learned is patience, and really taking that time to listen and grasp the knowledge that you’re being given,” Szmania said. “A lot of folks will take it in different ways, just like at work. You might be given an idea, and have four or five different solutions. Sometimes it’s trial and error. [On the mat], you might try to move on someone, and they might lock you up and tap you out real quick. You try to learn from those mistakes.” •
GE HealthCare has entered into an agreement to acquire IMACTIS, an innovator in the rapidly growing field of computed tomography (CT) interventional guidance across an array of care areas. IMACTIS is a France-based company that was founded in 2009 by Stephane Lavallee and Lionel Carrat, who created CT-Navigation, an ergonomic universal solution that provides stereotactic needle guidance, enabling intuitive pre-planning and continuous control throughout a wide range of procedures, from diagnosis to treatment.
“We’re thrilled to take this step in strengthening our interventional guidance offering for patients and customers,” said Jan Makela, president and CEO of imaging, GE HealthCare. “The IMACTIS CT-Navigation system is designed to improve workflow for interventional radiologists and hospitals by increasing procedural accuracy,
while helping to reduce procedure time and radiation dose for patients and physicians. It is an innovative navigation solution for image-guided percutaneous procedures that aims for better patient outcomes, by reducing variability for simple and complex procedures and improving reproducibility.”
“The timing to join GE HealthCare is perfect,” said Pierre Olivier, president and CEO of IMACTIS. “Our solution, which is already deployed in leading health care systems in Europe and the U.S., is ready to scale and become a standard of care, thanks to GE HealthCare’s market access. Our product development team also sees significant opportunities to integrate our hardware and software into GE HealthCare solutions and make the workflow of the interventional radiologists and oncologists even simpler and faster.”•


The Diagnostic Ultra-portable X-ray for Space (DUXS) program achieved liftoff late last year by successfully obtaining medical diagnostic radiographic images in zero-gravity (Zero-G) conditions – including a re-creation of one of the first X-ray images ever taken by Nobel Prize winner Wilhelm Conrad Röntgen. The purpose of this study was to prove successful X-ray imaging is possible in a zero-gravity environment and show that existing equipment can produce diagnostic images in both zero-gravity and Low Earth Orbit (LEO).
The DUXS program is a partnership between industry and academia aiming to improve medical diagnostic capabilities in the final frontier and beyond. True weightlessness, which was required for this study, was accomplished by reserving space in a multi-parabolic flight provided by Zero Gravity Corporation (Zero-G) in G-FORCE ONE, a specially modified Boeing 727. During the flight, highly trained pilots perform a series of parabolas, between 24,000 and 32,000 feet which provides 20 to 30 seconds of Zero-G per parabola.
This flight’s imaging team consisted of four members. Sheyna Gifford, MD, MPH, MBA, MS, focuses her research on preventative medicine, rehabilitation and parastronautics. David Lerner, MD, is a researcher from the University of Washington specializing in radiology, as well as remote and aerospace medicine. These two researchers partnered with MinXray Inc., a leading global supplier of portable, compact digital imaging equipment. Vice President of
Marketing and Sales Jeanne Walter supplied MinXray’s Impact Battery-Powered Portable Digital Radiography System. Director of Global Sales Mike Cairnie took the images during the Zero-G flight. These images included a radiographic image of Gifford’s hand, which mirrored the first X-ray ever taken of Röntgen’s wife’s hand back in 1895 and provided the first conclusive evidence that medical-quality diagnostic X-rays can be quickly and simply obtained in microgravity.
Successful acquisition of radiographic images mid-flight helped identify the complexities that exist when imaging in Zero-G conditions and potential solutions for those problems. Establishing the single inertial frame between all components and participants, which is required for the system to capture quality diagnostic images, was a variable examined by the team during the pre-flight preparation. Several methods of stabilizing the X-ray generator, patient and digital detector together were developed and even modified during the actual flight as the testing progressed.
A line pair phantom was used to establish image quality compared to images acquired in normal earth gravity. Additional images of a patient’s hand, elbow, knee and thorax were acquired. The equipment functioned perfectly in the zero-gravity environment with diagnostic quality radiographs acquired comparable to those obtained in normal earth gravity. •
For more information, visit minxray.com.
MinXray in Action - Sheyna Gifford (l) and Mike Cairnie (r) at Zero-G. (Photo credit: Steve Boxall/Zero Gravity)AHRA: The Association for Medical Imaging Management appointed Nancy Green, CAE, FASAE, as interim chief executive officer of AHRA. Green brings vast association and nonprofit leadership experience, including serving as interim CEO for the American Industrial Hygiene Association, chief global learning and strategy officer at ASIS International, and most recently as ASAE’s chief operating officer.
AHRA President Brenda DeBastiani said, “AHRA is thrilled to bring in an association leader with the extensive knowledge and experience Nancy has to help us drive our strategic initiatives forward and deliver value for our members while we continue the search for a permanent CEO.”
“From the first conversation, it was clear that AHRA leadership and staff have a strong commitment to growing the organization and building member value. I look forward to partnering with this passionate team to define and achieve success for the future.” •

Ralph J. Basile, vice president of Healthmark Industries, has started his two-year term on the ASTM International board of directors.
ASTM International’s board is made of 25 leaders from a variety of companies, associations, universities, government bodies and other organizations around the world.
Through his work at Healthmark, Basile helps develop and market products to aid health care facilities in delivering safe and ready-to-use medical devices.
Basile joined ASTM International in 2004 and has participated in multiple committees. He is active in the committee on primary barrier packing (F02). He also serves on the executive subcommittee (F02.90) through his position as the subcommittee chair on liaisons (F02.80).
Additionally, Basile co-chairs a task group on the cleanliness of medical devices (F04.15.17) and is the technical contact for the development of multiple standards of the committee on medical and surgical materials and devices (F04) related to cleaning methods for reusable medical devices. •
ASG Superconductors (ASG) and Siemens Healthineers signed a partnership agreement to synergistically develop UHF MRI systems of unprecedented dependability for ground-breaking brain research.
The first project under the partnership shall be the delivery of a 10.5T MRI system to a University in China. The magnet will be built and comprehensively tested at ASG’s premises in Genova. Upon its arrival in Hefei, Siemens Healthineers is responsible for the integration and installation of the system.
“In the past, customers looking for a system above 7T had to order the magnet and the electrical integration separately,” says Arthur Kaindl, head of magnetic resonance at Siemens Healthineers. “With the new partnership, we are happy to offer these UHF systems on a turnkey basis for the first time. This will lead to a tremendous improvement in project execution for our customers and take a decisive step towards pushing the limits of MRI beyond 7T.”•



Bayer recently announced the acquisition of the global strategic imaging AI platform and solutions provider Blackford Analysis Ltd. The acquisition is part of Bayer’s strategy to drive innovation in radiology, including the development and adoption of AI within the clinical workflow, with the goal to ultimately improve patient care and advance Bayer’s position in digital medical imaging.
“Adding Blackford and its AI technology to our radiology portfolio secures Bayer an excellent position in the fastest growing segment within the overall global radiology industry,” said Stefan Oelrich, member of the board of management, Bayer AG and president of Bayer’s pharmaceutical division. “This acquisition complements our comprehensive radiology portfolio and nourishes our engagement to drive innovation in digital health. We are pleased to join forces with Blackford and their exceptional team to optimally utilize our combined expertise in healthcare technology with the aim to deliver true value to radiologists and their teams for the benefit of their patients.”
Blackford, which has a presence in the United Kingdom and the United States, provides infrastructure and access to a rich clinical application (ClinApp) ecosystem focused on imaging and analytics. The acquisition follows a development and license agreement between both companies in 2020 that laid the foundation for Bayer’s recently launched medical imaging platform, Calantic Digital Solutions. Building on technology from Blackford and adding additional workflow and analytics components, Calantic Digital Solutions delivers access to applications, including those enabled by AI, for medical imaging.
Blackford will continue to operate as an independent organization on an arm’s length basis to preserve its entrepreneurial culture as an essential pillar for nurturing successful innovation. The company will remain accountable to advance its technology, channel partnerships and ClinApp portfolio while benefiting from the experience, infrastructure and reach of Bayer as a global pharmaceutical company. The acquisition is expected to close later this year, pending the satisfaction of customary closing conditions. •


Radon Medical Imaging has acquired Premier Imaging Medical System – a provider of maintenance services and sales for new, used and refurbished imaging and biomedical equipment. This acquisition reinforces Radon’s strategy to be an industry leader in the medical imaging market, strengthens its business by providing access to new solutions and technology and further expands its geographic footprint.
For more than 30 years, Premier has specialized in selling, servicing and repairing imaging equipment, including fluoroscopy, C-arm, X-ray and other modalities, and provides biomedical equipment engineering services. Premier has deep and proprietary expertise in dynamic flat panel fluoroscopy technology updates for
GE Advantx, Legacy and Precision 500 analog fluoroscopy machines and has served numerous surgery centers, hospitals and other third-party independent service organizations in the southeast region of the U.S.
“We’ve been partnering with Premier for more than 20 years and are thrilled to formalize our relationship and officially welcome them to the Radon family,” said Anthony Border, CEO at Radon. “Robin West has been a fantastic leader who has helped build Premier’s reputation for delivering high-quality products, and his team of engineers are some of the best in the industry. We’re proud to have them on board for this next step on our journey.” •
The Joint Commission announced it is elevating Leadership (LD) Standard LD.04.03.08 – which addresses health care disparities as a quality and safety priority – to a new National Patient Safety Goal (NPSG) for all critical access hospitals and hospitals, as well as some ambulatory care organizations and behavioral health care and human services organizations that provide certain services, effective July 1, 2023.
Current requirements for Joint Commission-accredited organizations will not change. The intent behind the standard and associated elements of performance will remain the same; however, they will now be stated as NPSG Goal 16. The purpose of NPSGs is to improve patient safety – focusing on significant problems in health care and specific actions to prevent and solve them.
Accredited health care organizations will still be required to:
• Identify an individual to lead activities to improve
health care equity.
• Assess patients’ health-related social needs.
• Analyze quality and safety data to identify disparities.
• Develop an action plan to improve health care equity.
• Act when the organization does not meet the goals in its action plan.
• Inform key stakeholders about progress to improve health care equity.
Following the implementation of NPSG Goal 16, Standard LD.04.03.08 will be deleted.
Information on the research used to develop the requirements, including rationales and references, are available in R3 Report, Issue 38: National Patient Safety Goal to Improve Health Care Equity. Additionally, the new NPSG is posted on The Joint Commission’s Prepublication Standards page until July 1. •

Clarius Mobile Health recently introduced a new accessory that enables all-day scanning with any of its 10 third-generation portable ultrasound scanners. The new Clarius Power Fan HD3 provides continuous power supply and cooling, enabling clinicians to scan without interruption, which is a first for handheld ultrasound systems. It’s available now for new and current users.
“Until now, having to recharge batteries and cool handheld ultrasound systems between scanning sessions has been required for every handheld ultrasound device. We’re excited to conquer this common industry challenge with the Clarius Power Fan HD3,” says Kris Dickie, vice president of research and development at Clarius. “With image quality and performance that now rivals compact ultrasound systems, clinicians are using Clarius handheld scanners for a range of applications
beyond point-of-care exams, including for longer, more comprehensive examinations and education purposes. The ability to provide unlimited scanning is an exciting breakthrough for using handhelds in every setting.”
Other handheld ultrasound systems typically start running hot after 20 to 30 minutes and can run on battery power for 1 to 2 hours with recharge times ranging from 75 minutes up to five hours for fully recharged batteries. With the new Power Fan, Clarius HD3 is the only handheld ultrasound system that enables 24/7 ultrasound scanning. Clinicians can snap the Power Fan onto the scanner to keep it cool and plug the Power Fan into a portable battery pack or outlet to keep the scanner running continuously.
The Clarius Power Fan is available now for current and new users of Clarius HD3 scanners. •


Come experience everything Arizona and Colorado have to offer. Life doesn’t get much better than 300 days of sunshine, hiking, biking, lakes, rivers, and so much more. We invite you to our out patient imaging centers where your feedback and life work balance are valued.






Diagnostic ultrasound devices are used in detecting fetal abnormalities during pregnancy. Since these devices can generate scans that allow medical professionals to provide the appropriate treatment, hospitals and clinics are increasingly adopting diagnostic ultrasound products.
The New Yorker recently ran an article that discussed how the “handheld ultrasound will replace the stethoscope.” The author explored how technological and clinical advancements are pushing ultrasound systems into new areas and that could impact the use of the ever-present stethoscope. The article pointed out that handheld ultrasounds are small, low-cost, no-radiation, accurate, flexible, point-of-care accessible devices. Furthermore, new advances in training, adoption, telemedicine and AI could make ultrasound a go-to device for a broad range of clinical settings. It even explored the option of having ultrasound in the homes of patients.
Grand View Research reports that the ultrasound market will continue to grow in the 2020s.
“The global ultrasound device market size was valued at $7.9 billion in 2021 and is anticipated to expand at a CAGR of 4.5% from 2022 to 2030,” according to Grand View Research. “The rise in the adoption of ultrasound devices for diagnostic imaging and treatment, coupled with the increasing incidences of chronic and lifestyle-related disorders, is expected to boost the market growth. In addition, the rising demand for minimally invasive surgery and technological advancements in ultrasound imaging technology are some of the key factors driving the market. Ultrasound is considered one of the most valuable diagnostic tools in medical imaging due to the fact that it is fast and less expensive. In addition, it is safer than other imaging technologies as it does not utilize ionizing radiation and magnetic field.”

The global diagnostic ultrasound market value is set to exceed $10 billion by 2030, according to a new research report by Global Market Insights Inc.
Growing birth rates across certain nations such as Russia, Germany, China and India will increase the deployment of novel diagnostic and treatment alternatives in health care.
The diagnostic ultrasound market from the 2D technology segment was worth $2.5 billion in 2021. 2D ultrasound scans provide black and white internal images and are commonly used during pregnancy check-ups, to detect cysts, tumors, or polyps in organs and diagnose fetus health. The images made using 2D ultrasound technology are radiation-free and provide a real-time, live view of the pelvis using high-frequency sound waves. With such favorable clinical applications, the use of this diagnostic ultrasound technology will increase significantly over the forthcoming years.
The general imaging segment was valued at more than $2.5 billion in 2021. Diagnostic ultrasound is increasingly used for examining the kidneys, abdomen, gall bladder, liver, pancreas and spleen. Pathbreaking technological advancements in the development of ultrasound systems will also bolster the usage of this technology across a variety of clinical applications, states the report.
The hospital segment accounted for over 49.5% share of the diagnostic ultrasound market in 2021. Hospitals are adopting novel diagnostic technologies such as ultrasound imaging to provide an effective diagnosis for complex diseases. These establishments also serve emergency patients who require urgent scanning to determine a diagnosis. Anesthesiologists use ultrasounds during surgeries to visualize targeted structures such as blood vessels, the heart, lungs and other organs.
The Latin America diagnostic ultrasound market is expected to depict 3% CAGR between 2022-2030. This is due to the growing awareness about early diagnosis in health care organizations such as hospitals. The general population is showing an increasing propensity for routine diagnosis which enables them to avoid future treatment complications. This in turn, will augment the demand for advanced diagnostic systems such as ultrasounds for early diagnosis applications across the Latin American region. •
STAFF REPORTThe global ultrasound system market is expected to experience significant growth in the coming years.
The Hologic SuperSonic MACH ultrasound system is designed to help improve efficiency and diagnostic accuracy. This high-performance system features exceptional imaging as it reduces speckle regardless of tissue density and offers improved lesion conspicuity. The SuperSonic MACH 40 system also boasts Shearwave PL.U.S Elastography for realtime tissue stiffness evaluation, Angio PL.U.S imaging for microvascular flow assessment, Needle PL.U.S imaging for enhanced needle visibility during biopsies, and 3D Ultrasound imaging for the breast. The system’s SonicPad Touchpad offers users an intuitive and ergonomic experience while helping to improve workflow by reducing a user’s movement and examination time.

The RS85 Prestige ultrasound system is revolutionized with novel diagnostic features and advanced intelligence technologies to assist sonographers and other health care professionals to diagnose with confidence and ease. Designed for scanning performance, the system delivers consistent image clarity, depth of penetration and sensitivity to perfusion of blood flow. At the core of the image quality is Crystal Architecture, which combines advanced beamforming (CrystalBeam), sophisticated image processing (CrystalPure) and advanced S-Vue Transducers to produce clear, uniform, highresolution images. The RS85 Prestige is empowering ultrasound professionals with diagnostic confidence on even the most challenging of patients.
The Sonosite LX is FUJIFILM Sonosite’s latest, premium point-of-care ultrasound (POCUS) system. The system’s large 21.3-inch clinical display extends, rotates and tilts to accommodate the varied clinical environments at the bedside, and its proprietary advanced image clarity is designed to enable greater diagnostic and procedural confidence. The system’s small footprint and adjustable display foster collaboration, allowing for real-time image and information sharing with the patient, clinicians and other hospital staff.

FUJIFILM Sonosite’s newly designed T8-3 transoesophageal transducer is compatible with the Sonosite LX and is designed to assist clinicians in using transoesophageal ultrasound (TOU) at the point of care.
*Disclaimer: Products are listed in no particular order.

The ACUSON Redwood ultrasound system, CV Edition 1, delivers detailed image quality, advanced technologies and greater workflow efficiency. Sharing a transducer portfolio with the ACUSON Sequoia, the system includes a dedicated cardiology platform with AI-powered 2 applications, stress echo, cardiac strain, 2D TEE transducer and adult and pediatric imaging. From improved sensitivity of our latest single-crystal transducer technology to next generation coherent image formation (CIF), and Siemens Healthineers exclusive color flash suppression technology, ACUSON Redwood delivers imaging with confidence. Its lightweight portability, hibernate mode, and rear-handle system make it easy to move around, bringing precision imaging to more patients.
1. CV Edition refers to a configuration that combines available cardiovascular options on the ACUSON Redwood ultrasound system.
2. AI-powered measurement tools consist of software applications leveraging machine learning-based Artificial Intelligence to achieve the intended outcome including eSie Measure and eSie Left Heart.







First Call Parts has been providing customers with quality replacement imaging parts since 2009. We pride ourselves in developing a top-notch reputation in the imaging industry as delivering the best in diagnostic imaging replacement parts. We specialize in the sale of refurbished/tested and used, Philips, Siemens, and GE in the Cath/Angio, R/F, and RAD modalities.

At RENOVO, we value knowledge, reliability, and integrity in our employees. If you are interested in being a part of a team that is committed to making a difference in healthcare equipment maintenance and healthcare asset and technology management, we invite you to apply for one of the open positions. We are always looking for talented, passionate, hard-working people to join our team.




The InterMed Group is a healthcare technology management company meeting the needs of our customers for over 20 years. InterMed sells and services medical equipment for our customers across the country and is growing quickly. As a result, InterMed is looking for an Imaging Field Service Engineer to perform repairs and preventive maintenance. This individual would be responsible for maintaining, inspecting and repairing imaging equipment for our accounts in the area and must be willing to travel for work.
Every day across central Pennsylvania, the people of WellSpan Health work together to support this non-profit mission of service—one patient, one community, one unique health care need at a time. We also collaborate with community leaders, area residents and other health care providers to make sure that inpatient, outpatient, home health and physician services are located where they can do the most good for our neighbors.

MXR Imaging, Inc. is the largest independent distributor of imaging sales and service in the U.S. As an industry leader, we provide a wide variety of New and Platinum Certified Pre-Owned imaging equipment. Additionally, we offer service support, legacy equipment assistance, equipment relocation, Mobile rentals, parts, training, and radiology consumable/durable goods to the healthcare market. MXR possesses an extensive imaging portfolio.

Agiliti is a nationwide company of passionate medical equipment management experts who believe every interaction has the power to change a life. Our industry-leading commitment to quality and team of expert technicians helps ensure clinicians have access to patient-ready equipment needed for patient care. Make an impact in healthcare and grow your career with Team Agiliti!

Intermountain Health is a leading nonprofit organization and health system that provides high-quality care to our patients and communities in Utah, Idaho, Nevada, Colorado, Montana, Wyoming, and Kansas. We are a team of more than 59,000 caregivers with a shared goal: to make a difference in our communities by putting our patients and families first, believing that fully engaged employees are the foundation of exceptional patient care. We value diversity and offer promising career opportunities with great benefits to those who share this goal.

Do you want to work in healthcare? Would you like to make a difference in the lives of patients and their families? Do you enjoy a new challenge every day? If you are skilled at servicing medical equipment in a clinical setting, we hope you will join our team!
Associated Imaging Services has been offering nuclear medicine and ultrasound solutions to our customers since 1990. We specialize in the sales and service of new and refurbished nuclear medicine cameras and ultrasound systems throughout Kansas, Oklahoma, Texas, and the surrounding areas.
 BY MATT SKOUFALOS
BY MATT SKOUFALOS
In 2007, the Institute for Healthcare Improvement (IHI) debuted its performance optimization framework for health care organizations, the Triple Aim. It is anchored in the acknowledgment that health care simultaneously faces spiraling costs, novel challenges, and questions of accessibility to broad segments of America. IHI proposed a framework encapsulating these concerns within a trio of responses, or aims: enhancing patient experience, improving population health and reducing costs.
Ten years later, IHI President and CEO Derek Feeley responded to calls from the world of health care to expand that framework into a Quadruple Aim system, one that would incorporate an additional goal that varied according to the institution proposing it.
“For many organizations, the fourth aim is attaining joy in work,” Feeley wrote then. “For others, it’s pursuing health equity. Some organizations highlight other priorities. The Military Health System, for example, has added readiness as their fourth aim.”
Feeley had no objections to institutions expanding their performance improvement aims, provided that work results in measurable action, keeps the focus on patients and doesn’t
undercut the already elusive goals of the initial three aims.
“Feel free to interpret the Triple Aim in a way that makes sense for you and your organization and what you need to achieve but do so in a way that is deliberate and strategic,” he wrote. “Whether you choose to work on the Triple Aim or the Quadruple Aim, understand that you can’t ignore joy in work or equity and expect to secure Triple Aim outcomes.”
In the time since the response to the triple aim ostensibly was expanded, many organizations have embraced health equity and addressing staff burnout as critical to health system optimization, leading to the emergent citation of a Quintuple Aim structure by early 2022. However-many-pronged the attack on systemic challenges a health care institution employs, its achievement requires clarity of approach and consistency of execution.
Dr. Cheryl Petersilge, CEO and founder of the Chagrin Falls, Ohio-based enterprise imaging consultancy Vidagos, said that the idea of achieving the quadruple aim (or triple or quintuple aim), as it applies to the medical imaging space, involves establishing continuity across the many segments of a health care organization that typically operate independently from one another.
“If you think about total quality assurance and imaging, you’ve heard of the comprehensive longitudinal medical record and continuity along the continuum of care,” Petersilge said. “One way you optimize medical decision-making is by making sure all the information is available to the provider at the time they’re making the decision. That’s what improving the patient experience is all about.”
“Images have been extremely siloed,” she continued. “They haven’t been accessible to providers outside of their office space. You’re either making medical decisions without the information, or you’re delaying care. It should be that all of the information is available at the time and location of care, whether it’s generated in your institution or not.”
Electronic medical records (EMR) and electronic health records (EHR) can help facilitate that information delivery and access, if implemented and overseen properly, Petersilge said. As a co-chair of the Society of Imaging Informatics in Medicine (SIIM) Enterprise Imaging Community, she not only appreciates the distinction between the two, but emphasizes that a medical imaging ecosystem is a peer system to EMR, and not subordinate to it. That’s a critical distinction when departments vie for consideration in an enterprise health care structure.
“If you look at both, there’s way more volume of data in the imaging record than there is in the EMR,” Petersilge said. “What medical specialty touches the greatest number of patients? It’s radiology, the big gorilla of enterprise imaging. So why would you consider that record to be an ancillary system? For a radiologist, and now many other imaging professionals, it is imaging system first: you’re paying for those tools, maximize the use of those tools for the imaging professional.”
Rather than working to fit the functionality of specialty imaging modalities and their respective software clients into an EMR-driven workflow, Petersilge argued that working within
a modern enterprise imaging structure provides the opportunity for much more sophisticated, imaging-specific processes. These systems set the foundation for workflow automation, as well as the incorporation of imaging-specific AI, and help to support the transition from free text information to discrete data. Doing so will ultimately support overarching institutional goals like those in the quadruple aim, ensuring that patients are best served by optimizing the workflows of the imaging specialists and better utilizing the information they generate.
“You should look at the two systems and say, ‘Which one offers the better functionality for my imaging professional?’” Petersilge said. “That, to me, is huge. One of the areas I focus in on is re-thinking how you search for and access these studies when you’re perusing the electronic record.”
By the same token, she points out that institutions can leverage the patient data that they already have on file to begin to understand and address population health goals. Although not every patient on file will have undergone a medical imaging study, a trove of information among those who have nonetheless exists, which could help project and analyze broader health trends and even pre-clinical disease states.
Better and more seamless information-sharing across departments and institutions also improves the quality of life for health care professionals. Clinicians who can readily access and analyze imaging studies remotely enjoy an experience superior to those who must compile patient information from different data sources. (“Thirty percent of CDs don’t open,” Petersilge pointed out). Smoother data sharing and access also helps to reduce imaging costs by eliminating redundant or inappropriate imaging, and can support offsite care centers when properly networked and centralized.
“If you consolidate them, you can have one central team that can manage all those imaging systems, and standardize so you have workflows that can come off the shelf,” Petersilge said. “It becomes much easier to handle existing modalities, deploy new pieces of equipment and integrate new modalities as they are introduced into the workplace.”
Centralizing supports for medical imaging teams isn’t only important for managing distributed locations or interdepartmental communication; it can also help coordinate remote employees, of which Petersilge points out there are more than ever
in a post-COVID (novel coronavirus) work environment.
“Within radiology, many departments went completely remote during COVID; many are preserving at least a portion of their workforce as remote,” she said. “With the radiologist shortages, that’s new. It allows you to retain staff, and for the staff to be more mobile and thus achieve greater work satisfaction.”
Enterprise imaging can also be structured in such a way as to reduce costs while supporting a flexible workforce, particularly by centralizing equipment management and support, Petersilge said.
“If ophthalmology has been managing its own equipment, or goes directly to the vendor, bring them into the enterprise imaging fold,” she said. “They get benefit of IT professionals to help them. I have seen a couple organizations that have been working without an image management system, and it’s a pain point for organizations: they can’t see all the images at once; they can’t see the images in the office with a patient.”
Finally, Petersilge said that in order to truly understand how to analyze and manage these concepts requires moving the health care system to a value-based structure that “really embraces wellness over episodic care” with incentives that lead toward rewarding those outcomes.
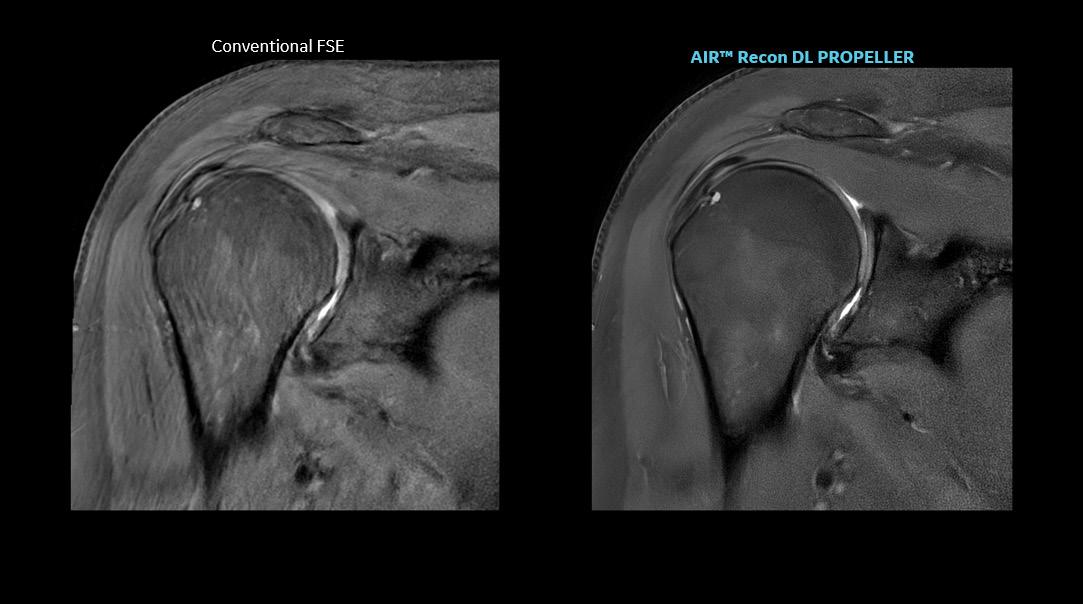
Loannis Panagiotelis, chief marketing officer for MR at GE HealthCare, said that his company has endeavored to address patient access to medical imaging and system productivity by increasing adoption of technological solutions that enable shorter scan times and sharpen image technology. AIR Recon DL, a deep-learning-based image reconstruction algorithm, removes image noise and artifacts from scans, leveraging raw image data to scan patients faster without compromising image quality.
Panagiotelis claimed the technology, which has been years in development, can sharpen images by as much as 60 percent and cut scan time in half.
Panagiotelis said. “We made [AIR Recon DL] available for all our systems – entry-level, mainstream, higher, new systems, legacy systems – and for all anatomies. That has been a grand success.”
Panagiotelis said that the improvements to throughput and efficacy of imaging that AIR Recon DL supports have expanded the reach of MR into studies that formerly were believed to be too complicated or time-consuming for the modality, including prostate screening, musculoskeletal imaging, and gerontological studies.
“It’s become simple and accurate, and that’s why this is taking off,” he said. “It becomes easy for the people to go and have these examinations. We believe it is impactful, but at the same time we are not compromising the procedure. The sharpness of these images is increasing because of the ability to combine
To date, GE HealthCare has sold more than 3,000 AIR Recon DL licenses, and installed some 2,000 systems; as of December 2022, the technology already had been used to scan about 5.5 million patients. With that level of adoption, Panagiotelis believes more patients will benefit from its advantages sufficient to address scanning backlogs, patient discomfort in the imaging suite, and even help make radiologists more comfortable during reads.
“We made sure that as many people as possible can benefit,”
studies with new types of contrast without compromising the overall duration of the scan.”

Taken together, the myriad technological advances that work to improve operational efficiency, simplify ease of use of the imaging systems, reduce acquisition time, and enhance workflow “all brings the costs down,” Panagiotelis said. “We go over this process multiple times a year, collect customer feedback, and try to define our products to meet their needs. There are different customer segments, but increasing patient access, clarity of scans — everybody needs these things.”
Leveraging evolving technologies to improve holistic industry metrics like population health requires not only a deep understanding of the processes that underpin medical imaging systems themselves, but also an insight into the communities in which health care institutions operate, and the residents within them that they serve. Finding solutions to improve their specific needs “is really where the big effort is being made,” Panagiotelis said.
“There’s a lot of elements, a lot of effort that we need to take in order to bring the solutions to the market,” he said. “There are multiple elements of technology that we are trying to develop simultaneously that, in the future, may prove of particular benefit for patients in the field of psychiatry — fMRI, fiber tracking, neuroscience imaging. If MRI can enter this field, this will be a major breakthrough.”
“The things we’re trying to do today to make it easier and cheaper, include new techniques that make invisible pathologies visible,” Panagiotelis said. “We want to introduce an element of prognosis, not only an element of diagnosis.”
Dave Bennett, CEO of the Lake Success, New York-headquar-GE Healthcare states that 3D imaging provides for more clinical efficiency, allowing radiologists to eliminate the need for multiple 2D acquisitions—potentially leading to faster diagnosis.
“Health care is a constantly moving target with technology, but there are some core things at the bottom, and that’s the human experience, and how it crosses over everything from patients to clinicians to outcomes.”
tered interactive patient solutions developer pCare said that achieving optimal health outcomes hinges upon the recognition that the best patient care is achieved in a workplace that values staff wellness, too. Notwithstanding the extant labor issues in a landscape that is still defined largely by the impact of the novel coronavirus (COVID-19) pandemic on the business of health care, Bennett argues that stresses on the system as a whole can be distilled, in some respects, to stresses on individual professionals.
“How do we really tackle these sort of things and actually improve outcomes?” he said. “How do I focus on attending to their needs – physical, mental, professional and others – while keeping them engaged to focus on cost containment, patient engagement, improvement in outcomes?”
“On top of that, what’s most critical is the financial health of some of the largest health care organizations in the country,” Bennett said. “They’re really in financial jeopardy right now. We’ve seen an escalation in costs, largely labor, and the simple fact of supply and demand. You have a demand for a large number of skilled-trade health care professionals, and that supply is waning. The industry is challenged by those, and that’s why challenging burnout is critical.”
Losing veteran staffers also means depleting institutional memory when they take their years of experience with them upon departing, to say nothing of losing people who’ve learned how to manage staff, control costs, and reinforce institutional culture, to say nothing of the time investment required in training their replacements. However, Bennett argued that some of the stopgaps to addressing such issues, like digital innovation tools, can support the culture shifts that are necessary to optimize the patient experience, thereby supporting overall institutional goals.
“Health care is extremely conservative in its nature,” he said; “health care has to be cautious and take its time, almost to a fault. The speed with which we adopt these things is also an issue, and can have profound impact on organizations. We’re always looking for things that can be force multipliers; something that can be put in place to increase effectiveness.”
Bennett believes that remote technologies that have become more commonplace in the past decade – including advance patient registration, texting with practitioners, patient health portals – will accelerate further, from advanced adoption of telemedicine to increased delivery of virtual services, from rounding to patient navigation to staff intercommunication; all things that can be accomplished offsite as well as within a facility. Personalizing care to enhance the patient experience can also help health care staff to more seamlessly align their own experiences with institutional goals.
“The engineering of people is equally important,” Bennett said. “How does this technology fit into their workday? Is it doing things that are very critical? I hear all too often from health care professionals that this is a hard job. We need to be able to recognize that our staff is making this possible.”
“This digital transformation, and how it aligns with the four aims, is the ability to create mechanisms that go beyond patient satisfaction information, and how to use feedback to be able to recognize those staff for their great jobs,” he said. “We need to elevate our staff and let them know that we really care, they’re doing a fantastic job and they are really making a difference. Health care is a constantly moving target with technology, but there are some core things at the bottom, and that’s the human experience, and how it crosses over everything from patients to clinicians to outcomes.” •
Dave Bennett CEO of pCare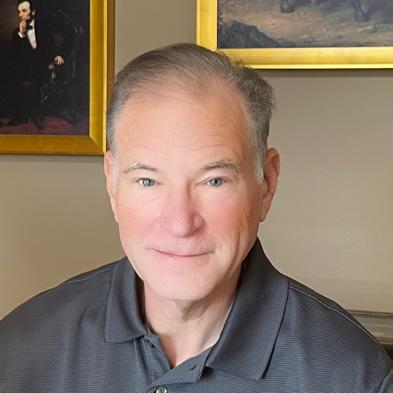
“This digital transformation, and how it aligns with the four aims, is the ability to create mechanisms that go beyond patient satisfaction information, and how to use feedback to be able to recognize those staff for their great jobs.”
Dr. Cheryl Petersilge CEO and Founder of Vidagos
“In order to truly understand how to analyze and manage these concepts requires moving the health care system to a value-based structure that ‘really embraces wellness over episodic care’ with incentives that lead toward rewarding those outcomes.”
Loannis Panagiotelis Chief Marketing Officer for MR at GE HealthCare
“The things we’re trying to do today to make it easier and cheaper, include new techniques that make invisible pathologies visible. We want to introduce an element of prognosis, not only an element of diagnosis.”
 AIR Coils are a technology in coils which are flexible, lightweight, and comfortable, enabling total freedom in coil positioning and handling during an MRI scan.
AIR Coils are a technology in coils which are flexible, lightweight, and comfortable, enabling total freedom in coil positioning and handling during an MRI scan.
The Association of American Medical Colleges (AAMC) does not only create curriculum to guide the future of medical education, but they have also begun to prepare medical schools and teaching hospitals to meet society’s evolving health needs. The AAMC is committed to equity, diversity and inclusion (DEI). They are developing strategic initiatives to cultivate a diverse and culturally prepared workforce, advance inclusion excellence, imbue equity-mindedness and enhance engagement with local communities (aamc.org).
Recently, I had the pleasure of witnessing a presentation by one of the AAMC’s leaders about “Advancing Racial Equity in Academic Medicine.” During this presentation, the presenter elaborated upon four crucial questions. These questions can be asked by any of us in reference to our own employer. Moreover, their downstream effect on the patients we care for.

The answer to the question relates directly to a narrative of your institution’s culture and how it exemplifies its core values. I am positive your employer has core value language around hiring competent staff that work to deliver high compassionate care. Take a good look at the racial demographics of your staff. Is your staffing racial representation made of the same racial makeup of the patients they are serving? If the answer is no … then why are they not represented in your organization’s culture? I am positive that every race of people has competent candidates that can exemplify your organization’s core value. Find them and hire them to improve your patients’ experience.
This relates to inclusion. As a nation, we have created a sense that there is always an “other” category. Should this exist in patient care? Why would one group get priority
of another, when the purpose of health care is to meet the care needs of the patient. Although this is the fundamental truth, there are incidents in history where a race of people have been experimented on and exploited (examples include Henrietta Lacks, Tuskegee Experiment, Vertus Hardiman). Situations like these have led some individuals to believe that they do not belong or can’t trust the medical system. Creating more inclusion strategies to employ diversity can be a step in the direction to help to resolve trust issues.
Even if we have embraced an idea of diversity and we have counteracted the dominant narrative on who should be included in our ranks, we have not really identified how we ensure that everyone is able to reach their own individual goals. We are just now beginning to ask those questions in health care organizations about what race, gender or type of individuals are being promoted and hired into leadership positions within our organizations. Do the hiring and promotion statistics show equity across all demographics? Trust me. I already know the answer to this, but I want you to ask it of your organizations.
There is a typical group that you may be thinking of – the board of directors, administration, payers. To counter this top-down approach, I want you to think of other groups we should be accountable to. They are our local communities, patients and staff. How can we hold true to our organization’s values if we are not true to hiring from within the cultures that exist in our immediate community? Therefore, guaranteeing we are serving our patients and including them in our vision. •
We understand that your future depends on quality education in a rapidly growing technological field. Our program offerings are designed to provide you with the skills and expertise needed for servicing today’s imaging modalities.


With one of the largest inventories in the industry, if we don’t have the part or device you’re looking for, we can help you source it from a variety of trusted partners around the globe.
We have engineers and installers on-board to make your purchase a priority. Whether it’s a full installation or de-installation, or technical troubleshooting, RSTI eXchange is Engineered for Life™



Our certified techs know our catalog and equipment like the backs of their hands. You’ll always get expert advice from the friendly and capable RSTI eXchange team.
 BY BRENDA DEBASTIANI AHRA REPORT
BY BRENDA DEBASTIANI AHRA REPORT
As AHRA President, over the past eight months I’ve had the opportunity to see things in the imaging realm from a new lens, and it has been enlightening and inspiring for me. The worldrenowned RSNA conference offered a wonderful opportunity to meet with AHRA corporate vendor partners to learn what they want to accomplish with us in 2023. Providing education to our members is our top priority, and we are so fortunate to have corporate partners willing and able to help us best meet our members’ needs. I look forward to continuing to build these relationships that are so valuable to the profession.
The AHRA Educational Foundation just kicked off its “$50 for 50” campaign in celebration of AHRA’s 50th anniversary this year. Last year, the AHRA Educational Foundation was able to provide over 30 scholarships valued at over $65K to our members because of the tax-deductible contributions from our AHRA family. Please keep in mind that donations are tax deductible and support a variety of scholarship opportunities. Please consider
giving, as your gift will be put to great use!
In an incredible gesture, we received a $25,000 donation from an anonymous donor. It will be earmarked for the Broadley scholarship, named after an AHRA founder, Louise Broadley. This act of generosity speaks volumes about how important this profession is!
In January, Nancy Green, CAE, FASAE, was appointed AHRA Interim CEO, and has been a great addition to the AHRA team. Bringing a wealth of knowledge and experience in the association field, Nancy has worked closely with the AHRA staff and Board of Directors on strategy, and how to best provide what members need and want.

The AHRA held CLIMB 2023 in San Diego, CA, February 24-26. This meeting focused on shared knowledge, leadership experiences at all levels, and had great support from exhibitors and sponsors. All of this with a waterfront view was true magic.
Next up is the 50th Anniversary Annual Meeting to be held July 9-12, 2023 in Indianapolis, Indiana.
I know AHRA members look forward to attending the annual meeting to learn what’s new, “recharge their batteries” and network with other imaging leaders.
I always walk away from the annual meeting with a renewed sense of purpose, a notebook full of notes about new information and a boost of energy.


In case you have never been to Indy, I want to share my experience. Last year in May 2022, I took a trip to Indy to do the “Indy Racing Experience.” You could not wipe the smile off of my face the entire day. Where else can you go 200 mph and get to listen to the roar of the race car up close and personal? All I can say is “WOW!” – this was an incredible experience. Indy offers great food and fun. There are multiple museums, beautiful architecture and lots of shopping opportunities nearby.
I hope that you can join us in Indy to celebrate our 50th anniversary. We have plans to honor our founders and past presidents, show appreciation to our current members and focus on our future.
The AHRA is well positioned to carry out future plans. We are excited about where we’ve been, where we are, and where we’re going as an organization. I believe that we are THE organization that imaging professionals need to belong to in order to receive the education and networking necessary to do the best job possible. The AHRA has allowed me opportunities to learn and grow, both personally and professionally, and that is a possibility for you, too! So volunteer, network, make new friends, and attend as many educational sessions as you can. Make yourself just a little bit vulnerable to learn new things, and I promise that you will not regret it.

If you have any questions or suggestions, please reach out to me! Brenda.DeBastiani@braverahealth.com •
 Brenda DeBastiani, AHRA President, MBA, CRA, FAHRA, RT(R), is director of imaging at Bravera Health Spring Hill.
Brenda DeBastiani, AHRA President, MBA, CRA, FAHRA, RT(R), is director of imaging at Bravera Health Spring Hill.
“I always walk away from the annual meeting with a renewed sense of purpose, a notebook full of notes about new information and a boost of energy.”
Tamponade is an unusual word. The radiologist was looking at the images, he said “I wish they would have told me he had tamponade.”
Cardiac tamponade happens when the fluid sac around your heart fills with blood or other fluid, putting pressure on your heart. Because of the pressure, your heart can’t fill up with blood, reducing how much blood your heart can pump and ultimately causing a drop in blood pressure. Trauma and certain diseases can cause cardiac tamponade. If not treated, it is always fatal.
What happens in cardiac tamponade?
Inside your chest, your heart is contained within a sac called the pericardium. The pericardium has two layers and holds your heart in place, and it also contains pericardial fluid. The fluid helps cushion your heart from outside force and stress.
The chambers of your heart must expand to fill up with blood before pumping blood out. Cardiac tamponade – which is sometimes called pericardial tamponade – happens when the pericardium fills with fluid (especially blood). Because the fluid has nowhere to go, your heart runs out of room and can’t expand enough to fill effectively.
What causes fluid to surround and compress the heart?
Several different types of injuries can cause cardiac tamponade. For example, it can happen with blunt trauma, such as a fall or a car crash, or penetrating trauma, like a stab wound from a knife.
It can also happen as a result of another injury, such as an aortic dissection. This happens when a tear forms in the wall of the aorta, a major artery in the center of your body. Blood can accumulate in between layers of the aorta’s walls and cause the artery to rupture, filling the pericardium with blood.
The AI system was trained to look for aortic dissection and aneurysms. We all knew that the large provider of reading services had AI that would find and diagnose AAA. This patient with tamponade presented in the emergency department and was quickly sent to CT for a AAA study.
The technologist responded quickly and sent the urgent message to the radiologist that the study was for AAA. This would mean the textual classification as an
AAA would elevate the study to the top of the worklist and result in a STAT interpretation.
The patient went down hill fast. The emergency department called the radiologist urging them to read the exam immediately. This call was not received by the radiologist. It was taken by a non-medically trained “facilitator” who took the doctor’s name and number with the promise to call them back.
The patient post CT scan was in the emergency department without an interpretation and died waiting for care.
The results of the study were provided two hours later. A loop of bowel had herniated into the heart area. This bowel was pushing on the heart and slowly causing the demise of the patient.
Why did the AI not save this patient?
Why did the CT technologist do everything right for the patient and still have to feel like she somehow let the patient die under her care? She entered the correct information to cause an urgent/immediate reading of the CT.
The answer is the AI is trained on the images on the CT screen not on the textual information.
If the image showed an AAA then the exam would be prioritized for immediate reading.
It did not!
Artificial intelligence answers the question correctly and tirelessly – if you ask it the right question and you understand its limitation and how to use it.
This is the challenge in imaging right now. We have it but are we doing it well? Has it been deployed well? Is there an ROI for solving this problem?
As this tamponade patient’s heart slowly failed because of the force the bowel loop was placing on it we should think about the failure of the system that was designed to help.
We should think about the expectation we have for AI in the future.
We should understand that to use AI in imaging we must know the opportunity and limitations.
We must ask the correct AI questions; patients lives depend on it. •
Mark Watts is an experienced imaging professional who founded an AI company called Zenlike.ai.

LOO


LOOKING LOOKING TO PURCHASE OR SELL? LOOK NO FURTHER.
213-276-8209
PMIMAGINGMGMT.COM GE • TOSHIBA • SIEMENS • PHILIPS


INTERIM SOLUTIONS. SUSTAINED SUCCESS.
� CT
� NUCMED

















� MAMMOGRAM

� IDEAL FOR UPGRADES AND PATIENT BACKLOG
� RELIABLE SOLUTIONS WITH KMG’S UPTIME GUARANTEE





































































































































































� PROJECT PLANNING & MANAGEMENT

� NEW OR USED SYSTEMS
� CONSTRUCTION & PERMITTING
� SYSTEM REMOVAL & INSTALLATION

� SUITE DESIGN & MODIFICATIONS
� STAFFING
KMG MOBILE SOLUTIONS KMG FIXED SOLUTIONS Mobile & Fixed In-House Imaging Solutions 3 3 0 . 5 2 8 .17 65 kingsmedical .com

Great Solutions. One Exceptional Company. ICEMAGAZINE 39 WWW.THEICECOMMUNITY.COM








Two




Every imaging leader I have met has mentioned their use of an open-door policy. I have supported this policy but realized a few years ago that an open door policy isn’t really an open-door policy in many cases.
Most people understand that an open-door policy is a management style that encourages employees to approach their leaders with any questions, concerns or ideas. This policy aims to create a welcoming and approachable environment that fosters open communication and encourages collaboration especially between the leader and the team member.
But the question remains, is an open-door policy an open-door policy, and are employees comfortable coming to your office? And the larger question is, how do you know your employees are comfortable using it? Are you making assumptions because you think you are approachable, and easy-going? Or, did you ask your employees for feedback on their comfort in using the policy and know without a doubt that your team is comfortable to have any type of conversations with you.
You may be the best imaging leader ever; however, you will need to understand the reasons why employees could be uncomfortable using your open door policy to determine whether you truly have an open-door policy. Here is a list of some reasons employees may not use your open-door policy.
The employee may fear that speaking up
could result in negative consequences, such as being passed over for promotions or given undesirable assignments or, worse case, losing their job. Especially in a non-union environment, this is highly possible.
An example of how speaking up could lead to fear of retaliation is if an employee brings up a concern about a coworker to their manager. The manager may see the employee as a “troublemaker” and start to treat them differently, such as giving them fewer desirable assignments or overlooking them for promotions. The employee may then be afraid to speak up again for fear of further negative consequences. This type of retaliation can create a toxic work environment where employees are scared to voice their concerns, leading to decreased morale, lower productivity and increased turnover.

Another example of how speaking up could lead to fear of retaliation is if an employee raises a concern about a specific project or policy to their manager. The manager may see the employee as challenging their authority and may respond by criticizing their work, or giving them a negative performance review, or simply being biased. This type of retaliation can make employees feel discouraged and unsupported, causing them to lose confidence in their abilities and become less engaged in their work.
Employees may feel unsure of their abilities or that their concerns are not significant enough to raise. Additionally,
employees may feel intimidated by the power dynamic between themselves and their leader, causing them to hesitate in approaching their leader with concerns or feedback. They may worry about the consequences of speaking up, such as criticism, retaliation or being seen as troublemakers.
Employees may not trust their leader to handle their concerns moderately or with confidentiality. Employees may feel that their leader does not have the skills, or the empathy to address their concerns and as such shy away from such conversations. For example, if an employee perceives their leader as uninterested or unresponsive to their concerns, they may feel that their leader is not capable or willing to address their needs, and they may be reluctant to approach them with further concerns.
Additionally, if employees do not feel that their leader has the capacity or resources to address their concerns, they may think it is not worth their time or effort to bring their concerns to their attention. This lack of support can lead to disengagement and frustration, making it less likely that employees will use an open-door policy.




Trust is a key factor in employees using an open-door policy. Unfortunately, there are many factors that erode trust, or prevent employees from building trust with leaders new to their position. Here are some reasons where employees may lack trust in their leaders which ultimately affects using an open-door policy.
The employee may have shared confidential information with a previous manager who betrayed their trust by sharing it with others, causing them to be hesitant to trust future managers with sensitive data. In addition, employees may also use rumors of
past employees, or their own observation of what transpires after an employee speaks up and then uses this as a measuring stick of trust and whether they should engage their leader.
Team members may have had negative experiences with previous managers and feel uncomfortable approaching you as their current manager. Negative past experiences can discourage employees from using an open-door policy and approaching their leader especially with sensitive conversations. These negative past experiences can create a sense of distrust and discomfort, making it difficult for employees to feel comfortable approaching their leader with concerns or feedback. Consequently, even though you can be the most compassionate and empathetic person with the active listening skills of the best communicator, an employee’s previous negative experiences
may affect how they use your opendoor policy. Some examples include:
• Disregarded concerns: The employee may have raised a concern to a previous manager who ignored or dismissed it, making the employee feel unvalued and unheard, and afraid to be burned again.


• Unprofessional behavior: The employee may have encountered a previous manager who was inexperienced, disrespectful or unapproachable, making them reluctant to trust any future managers. Trust is so easy to break, and may take a while for someone to rebuild trust, even with a new manager.
• Unresolved conflicts/problems: The employee may have raised a concern or had a dispute with a previous manager that was not resolved, leaving a negative impression and causing the employee to feel discouraged to bring anything to the forefront. “What’s the point?” “Tried discussing and nothing never changes.”


• Unfair treatment: The employee may have experienced unfair treatment or discrimination from a previous manager, causing them to be hesitant to approach any future managers with concerns. They may be concerned of repercussions, or just don’t want any situation to impact their longevity and ultimately their salary at the organization. It is important for imaging leaders to know whether employees are comfortable using an open door policy and to understand the reasons why they may not. Reasons could be fear of retaliation, lack of trust, past negative experiences, or lack of confidence and support in their leaders. Imaging leaders, therefore, need to be aware of these factors and take steps to address them to create a welcoming and approachable environment where employees feel comfortable to communicate.
Stay tuned for the next article where I will help you discover how to create a welcoming environment and make your open-door policy truly effective. Don’t miss my next article! •
Ever been part of a course of instruction on listening? If not, you’re not alone. In more than three decades of working with teams, I can count on one finger the number of people who’ve taken a class on developing their listening skills.
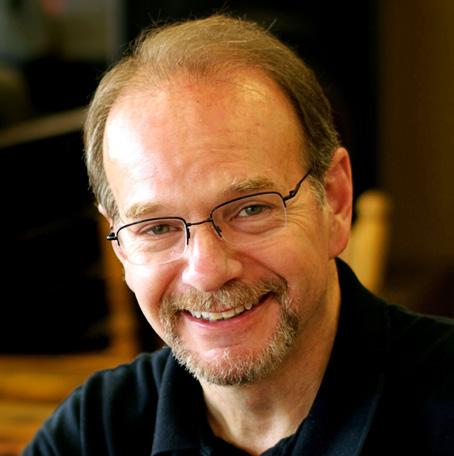
Time and again, people in management and leadership positions have told me they are good listeners. But, almost always, once these people are put in a position where they must actively listen to someone describe a workplace problem, they don’t do so well.

This is not something I’m inclined to criticize. After all, how can we expect people to do something if they’ve never been taught? And so, assuming that a majority of people reading this are similar to the groups I’ve worked with over the years, consider the following an “Introduction to the Art of Listening.”
Let’s start by doing a compare and contrast of hearing and listening.
Hearing is an ability to perceive sounds though vibrations that enter the ear. Providing a person’s ear canal is open, eardrums are intact and the cochlea and auditory nerves are functioning properly, a person should be able to hear sounds.
Listening goes beyond the ability to hear. Listening is a consciously learned
skill that involves comprehending, analyzing and interpreting meaning that come from the sounds we hear.
Hearing, by itself, is a subconscious, passive process, whereas listening is a conscious, active process.
We have no need to concentrate when it comes to hearing, and outside of turning off noisemaking devices or moving away from the source of a noise, we have little or no control over the sounds we hear.
On the other hand, purposeful concentration is required for listening, and it requires a heartfelt desire to understand the meaning and purpose of the information being conveyed.
Listening can and should occur with more than just ears because we can aid our listening by watching. The most reliable studies tell us that roughly 68 percent of communication is body language and 25 percent is voice tone. That leaves only 7 percent for words. This means that we can listen much better if we can observe a person’s body language.
Facial expressions offer much information to aid the listener in interpreting and analyzing.
Hand movements add nuance, too. Overall body posture is also informative.
Obviously, if we’re truly listening it means we’re not doing much talking. Also, as
we focus our attention on another person, we must seek to understand more than just the words we’re hearing. Effective listening requires that we actively seek to understand the thoughts and feelings that are behind the words of the person who is speaking to us.
When doing this, we often arrive at a subjective, educated guess, but it’s the starting point for helping the speaker know that we truly are listening. One question I always recommend a listener ask internally is, “What is this person thinking or feeling?” In other words, listening doesn’t involve only gathering the facts of what’s being said, but the person’s thoughts and/or feelings about it, too.
I cannot stress how incredibly difficult this step can be if the person speaking is bringing up a concern about you or saying something about your work or your team that is patently false. It is also extraordinarily difficult to do if someone is taking a position that runs 180 degrees counter to your value system. Our natural emotional response will be to defend ourselves or defend or correct false statements or defend something we value.
Listening in these situations calls for extreme amounts of control and patience.

A common human tendency is to “fix” things and move on. Add to that the fact that some of us process data in a matter-of-fact manner, believing that emotions are just muddy things that get in the way. But here’s the cold hard truth. All humans have emotions, regardless of how stoic they may appear, and emotions can be powerful drivers toward or away from any position.
This means that when one person is listening to another, it is easy to let our emotions get the best of us – to the point that we say things we regret later on.
To this I offer a trick that allows us to bear with the discomfort of feeling attacked if someone is saying something directed at us or our teams, and that trick comes out of Stephen Covey’s 7-Habits book: “Seek First to Understand, Then Be Understood.” Listening is “seeking first to understand.” It’s allowing someone else to be heard – to feel heard – first. The trick is knowing there are two parts, and that you will eventually get your turn to be heard in the second part.
To review: part one of the trick is listening to the other person (seeking first to understand), and the second part of the trick is knowing that you get to present your perspective next (then be understood). The downside is you don’t know how long it will take for the other person to feel truly heard. It could take 10 seconds. I could take 10 hours.
Regardless, think of the trick as exercising patience. Think of it as being mature as we follow solid principles of adult dialog.
Again, in no way is it easy to listen to someone if we’re in a hurry or being pressured or feeling attacked or lied about. But knowing that you will eventually get your turn to present your view of things can be what fills you with enough patience to listen, and listen deeply, all the way through until the other person truly feels heard.
After all, as a common maximum states, “People don’t care how much you know until they know how much you care.” And we show that we care by listening. Truly listening. Listening by conscious choice not only to another person’s words, but also to the thoughts and feelings behind the words, even if doing so is painful.
And that is the art of listening. •
Daniel Bobinski, who has a doctorate in theology, is a best-selling author and a popular speaker at conferences and retreats. For more than 30 years he’s been working with teams and individuals (1:1 coaching) to help them achieve excellence. He was also teaching Emotional Intelligence since before it was a thing. Reach him by email at DanielBobinski@protonmail.com or 208-375-7606.
As you may be aware, most of the content for what I write about here comes from “Internet research,” watching movies and shows on TV and live encounters with people. As I journey through my days, I often encounter some very common expressions that drive me nuts. I will tell you about them.

The first is “I want to …” as in “I want to thank you for everything you have done for me.” Why say it that way? I understand that the word expresses a need to thank, however if you really want to satisfy that need just say it. “I thank you for everything” actually communicates it way beyond the want. It’s as if the want is there but the actual expression of thanks is not. I want to thank you and I’m not really thanking you am I? I’m stopping short of the thanks.
Whenever I hear the “I want,” I always suspect that it is a cover up for not actually doing it. As if there is a hidden, alternate continuation to the phrase: “I want to tell you how much I appreciate you, but I won’t because I don’t.”
A follow up is when people say, “I can’t tell you how much I appreciate you.” Then, they move on. Is it because they can’t tell you since they don’t appreciate you at all? If they can tell you, why not just tell you.
“I can’t begin to describe how glad I am that I met you.” I don’t have the words to properly express my gratitude.” To me, these sound rather hollow and evasive. Is it that you are not glad to have met me, or have no or little gratitude and, are avoiding the truth?
“You never know” is another minor irritant to me. What does that even mean? Will the answer or solution never be available? You say something and instead of just
gently disagreeing and offering a reasoned rebuttal they throw out this nonsense. In my opinion this statement just means: “You’re point is too strong, I can’t think of anything relevant to say, so I will stop the conversation in its tracks.”
Note: Ruth asks, “Or does it mean that the recipient of a ‘You never know’ is too closed-minded to look deeper?” I should stop having her proofread my stuff.
I understand and accept that these expressions are entrenched in standard and even expected speech. I may be the only person that has issues with them. In my defense, I don’t really have a problem. I just tend to wonder about the meaning and intent which then interferes with the message itself. I’m spending valuable communication time thinking and wondering rather than actively listening.
While I’m at it, I also have meaning and intent questions when someone is talking and scratches their eye, or side of the nose, or rubs their chin. To me these are signs of discomfort with what they are saying or are about to say. I’m saying they are uncomfortable with the situation, not that they are fibbing. Pay attention and you will see this body language cue quite often, in real life of course. In movies, actors act as they are trained and will only show this when they want you to notice while the camera does a closeup to ensure you don’t miss it.
So, the bottom line is that I personally have quirks that interfere with good communication. I am aware of them and the consequences. And I can’t tell you how much I want to change. I want to tell you how much I appreciate you reading this and I can’t thank you enough for your support. •

































626 Holdings
p. 5
Advanced Health Education Center

p. 17
AllParts Medical



p. 47
Association of Medical Service Providers (AMSP)


p. 49
Banner Imaging
p. 23
CM Parts Plus

p. 43 Engineering Services

p. 3
HTMJobs.com

p. 28
ICE Webinars

p. 51
Imaging Academy
p. 2 Innovatus Imaging

p. 9
International X-Ray Brokers

p. 39 Isikel CET
p. 21
KEI Medical Imaging p. 37 KMG


p. 39
Maull Biomedical p. 47
Metropolis International p. 46

MW Imaging Corp. p. 44

PM Imaging Management p. 39

Ray-Pac®
Ray-Pac p. BC
Radiological Service Training Institute p. 35
Technical Prospects
p. 4
SOLUTIONS
TriImaging Solutions
p. 12 W7 Global, LLC.
p. 46

Register to view live webinars each month.


Watch recorded webinars on-demand.

ARRT Category A
CE credit is pending approval by the AHRA.




