THE NO SURPRISES ACT
PAGE 34
PAGE 29
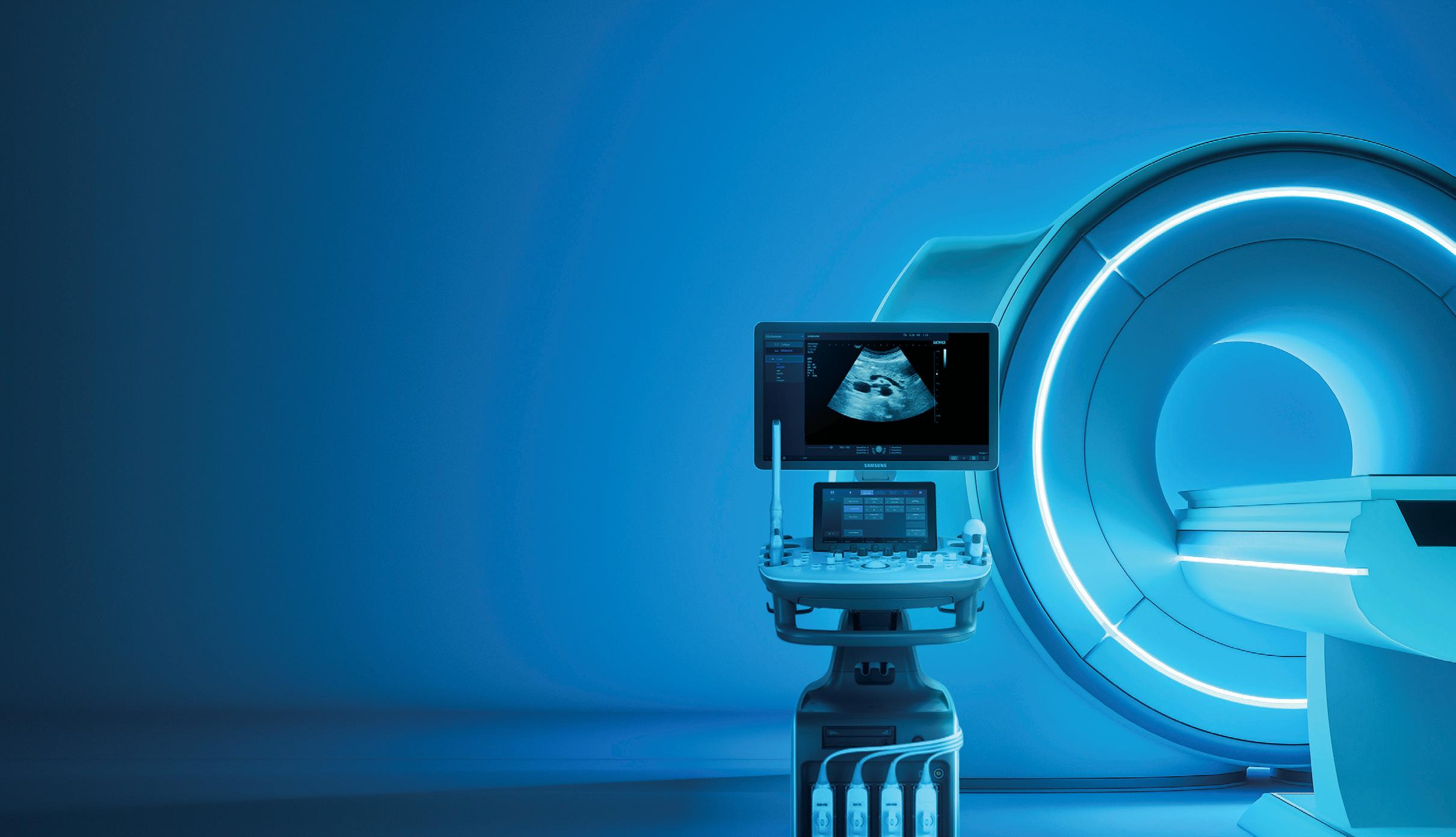
PRODUCT FOCUS: MRI

CORPORATE PROFILE PAGE 38
GUIDE TO AHRA
PAGE 54















PAGE 34
PAGE 29
PRODUCT FOCUS: MRI

CORPORATE PROFILE PAGE 38
GUIDE TO AHRA
PAGE 54














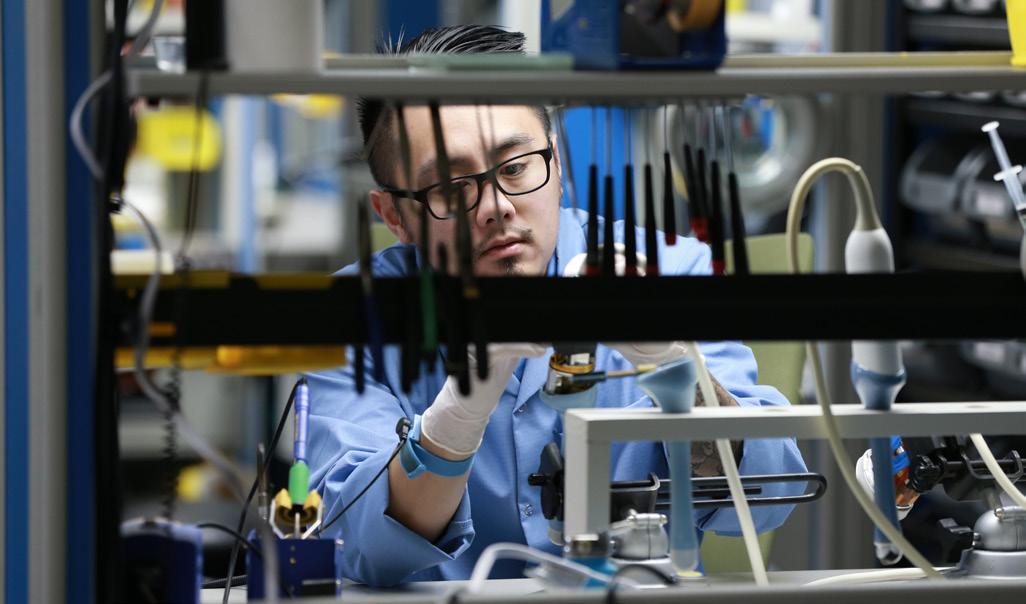
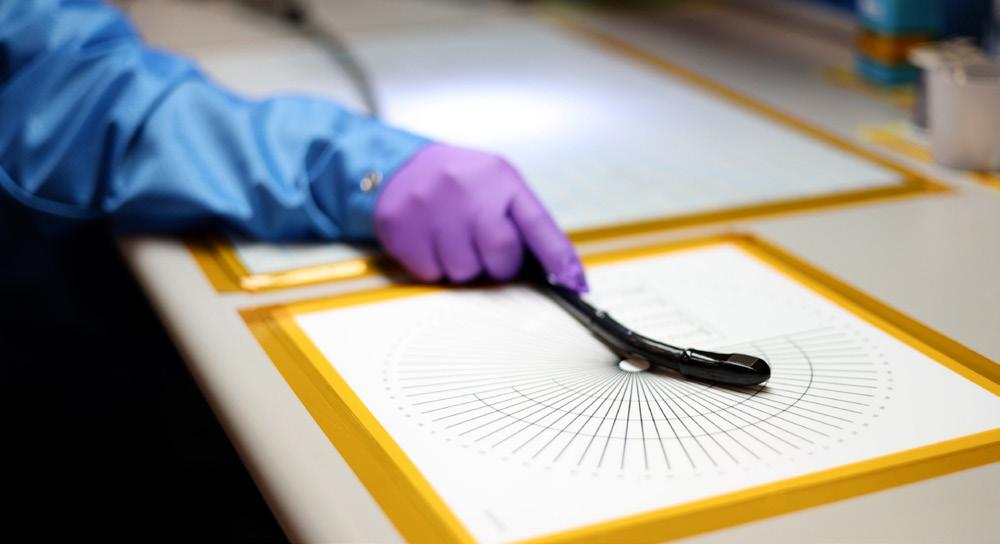
DOs:
Do carry a coil with 2 hands
Do store coils in a position where they are fully supported by a solid surface

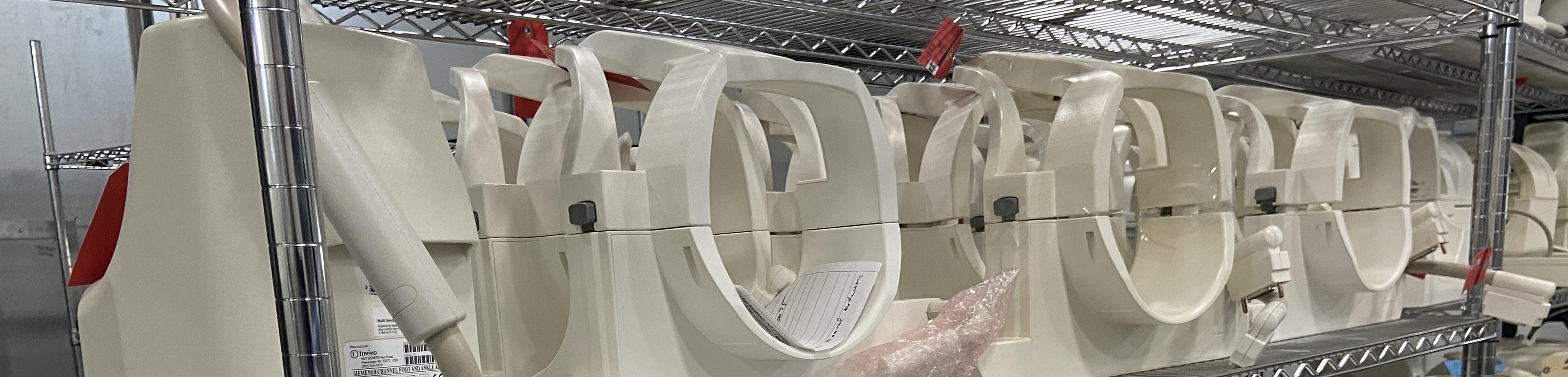
DON’Ts:
Do not carry, lift, or position a coil by using the cable or connector
Do not carry by the anterior bridge trusting the latching mechanism to hold the posterior section
Do not clean out a coil connector with common household cleaners
Do not store coils by standing them against a wall or hanging on stands support rails, or hooks
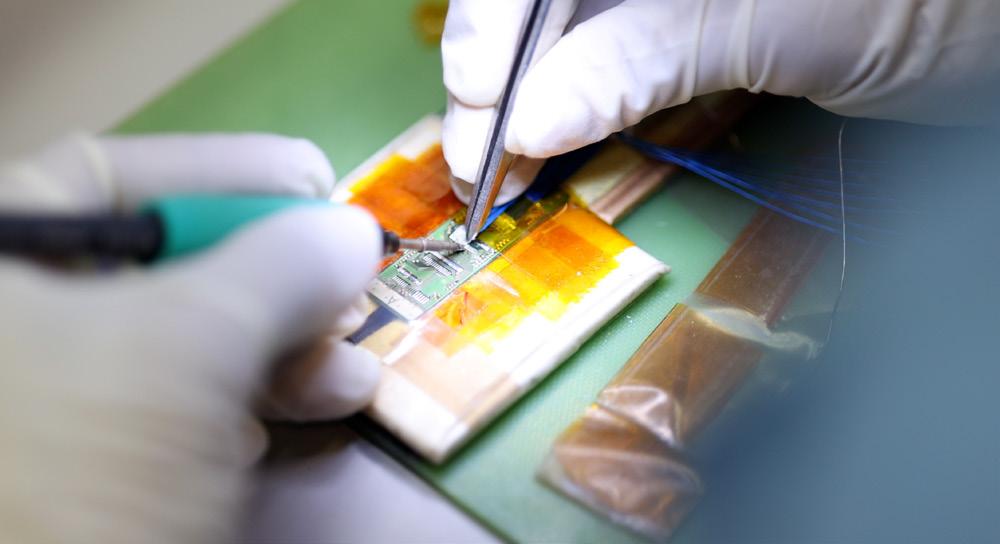
Our team of experts is here to help with your coils! We specialize in Siemens 1.5T and 3T coils and Tim style coils with an average turnaround time of 5 to 7 business days!
Capabilities include, but are not limited to:
• Complete diagnostics and repair of coils to the original manufacturer’s specifications
• Full electrical and mechanical rebuilds to improve and enhance performance
• Cosmetic refurbishment to a “like brand new” appearance
• Aesthetic touch-ups to the rigid or foam housings so that the coil is safe to use

• Abilities to repair not only the coil, but also the socket groups on the table side connector
• Provide 3D printed coil connectors or Balun cover replacements on Siemens coils

Additional offerings include:
• Use of an onsite MRI Scanner for QA/ SNR testing for 1.5T Siemens Tim
• Loaner program or exchange program
We have an extensive coil inventory covering most Siemens Avanto, Espree, Trio, and Symphony type coils. Our inventory contains the most popular models, Siemens Avanto Head, Body, Neck and Spine coils!
877.604.6583 / 920.757.6583
sales@technicalprospects.com
technicalprospects.com















DIRECTOR’S CUT
First-hand report and tips regarding an ACR survey.

COVER STORY
The No Surprises Act is likely to be felt most deeply in the delivery of emergency care and medical imaging.
RISING STAR
Anna Meiners is the radiology manager at the UC Health Drake Center in Cincinnati, Ohio.


Catch up on the latest news from around the diagnostic imaging world.
A look at some of the top MRI options.


Three items to consider when you want to attract and retain quality employees.




How did plasma physics research turn into a successful radiology career? It is an easy question to answer for University Hospitals Cleveland Medical Center Chief Medical Physicist and Senior Staff Scientist Dave Jordan, MS, Ph . D. , DABR, DABMP, DABSNM, MRSE (MRSC), FACR, FAAPM. He is also a professor of radiology at Case Western Reserve University.
“I was introduced to medical physics by a fellow nuclear engineering graduate student when I was working on research in plasma physics. I had studied electromagnetic fields and radiation measurements and had a lot of hands-on experience with strong magnets and devices like particle accelerators,” Jordan explained. “This turned out to translate well to X-ray,
nuclear medicine and MRI.”
It also translated into a career that Jordan loves.
“There is a tremendous variety in my day-to-day work. I have days that are mostly meetings, ‘quiet’ office days working on projects, a fair number of administrative and management duties, and I still get out in the field plenty, where I get to do handson work with imaging equipment, catch up face-to-face with our front-line radiology teams and teach residents,” he says when asked why he loves his job.
Among his many accomplishments, helping others is what stands out in his mind.
“Starting a medical physics residency program and seeing our trainees go on to successful careers in medical physics will probably always be at the top of this list for me. There are not enough of these programs today, so there is a critical need, and it’s humbling to see the talent and the drive that students have
Dave Jordan loves his job and being able to help others.
to excel in this field,” Jordan said when asked about his greatest achievement.
The ability to provide guidance to talented students is another rewarding aspect of his day.
“Everyone has challenges in their work where they need something they don’t have, whether that’s a skill, knowledge, authority, resources, contacts or something else that a leader needs to provide. I’m usually trying to figure out what that is, and then provide what I can both to solve the short-term problem and to equip the person to succeed on their own in similar situations in the future, if I can,” Jordan said.
Appropriately, Jordan received some guidance from mentors during his career.
“My journey as a mentee has been a bit unusual; after graduate school I’ve had many different mentors, most shorter-term and focused on very narrow areas
or topics. I wasn’t ‘under anyone’s wing’ long-term, so to speak. But everyone I’ve worked with has modeled generosity with their time, attention and advice, so I’ve tried to do that as a mentor myself,” Jordan explained. “I currently mentor several medical physics residents as well as my employees who are working to advance their careers, so I try to remember what I didn’t know that would’ve been helpful when I was at their stage and guide them from what I know now.”
Away from work, Jordan enjoys spending time with extended family near home and all over the country.
“I’m a proud husband and a proud dad to a second grader and a kindergartener, and our senior rescue dog (chow-husky mix) is actually in charge of the household. We’re lucky to have my parents nearby and a wonderful extended family across the country to visit when we can,” Jordan said. •
1. What is the last book you read? “The System: The Glory and Scandal of Big-Time College Football”
2. Favorite movie? “Star Wars”
3. What is something most of your coworkers don’t know about you? I do actually sleep.
4. Who is your mentor? Jason Theadore is my business mentor, and Claudia Kraly and Himanshu Pandya (both now retired) taught me so much about the business of health care and how to navigate a big health system. Dr. Ray Muzic, a fellow radiology faculty member at Case Western Reserve, is my scientific and academic mentor.
5. What is one thing you do every morning to start your day? I make or pick up the biggest coffee I can, with plenty of cream and sugar, and scan my digital calendar and task list to plan out the day on a page in a paper notebook.
6. Best advice you ever received? Write everything down.
7. Who has had the biggest influence on your life? My parents
8. What would your superpower be? Invisibility. In physics we have the Heisenberg uncertainty principle – when you observe or measure something, you actually change it. There are so many situations where your presence can affect what you are seeing and hearing, so I think a lot about what it would be like to make a “pure” observation, whether that’s a business meeting or the sounds of bugs and birds on a walk through the woods.
9. What are your hobbies? Going to live theater with my wife, Lego and Play-Doh projects with my kids, and reading. Hoping to add travel, golf and playing guitar back to the list as the kids get older and the pandemic (hopefully) continues to wind down.
10. What is your perfect meal? Anything with plenty of cheese.
Are you overwhelmed with multiple tasks and feeling like there is not enough time in the day? This was my experience, which prompted me to consider ways to automate certain aspects of my operation. One area where we were falling short was onboarding new employees. I felt I made employees question their employment choice based on how erratic and terrible this process was.
While this is a crucial process, it was disorganized and caused a negative experience for our new hires. To address this, we evaluated our options. Delegating tasks was not a viable solution due to our current resource constraints. That’s when the idea of automation struck us as the perfect solution to streamline and improve this process. What a Rad Idea!
Automating the new employee onboarding process is an excellent way for leaders to streamline and ensure that all new hires have the information and resources they need to succeed in their new roles. Without automation, the onboarding process is inefficient, time-consuming and lacks standardization. Also, it is chaotic, especially since it is not tracked well and often. New employees may not complete all the necessary training or have all the required policies and procedures they need. This can lead to some HR processes being out of compliance. And, we know what a kick in the gut is when TJC requests HR records only to realize we don’t have them!
One idea for automating the process is to create an online onboarding portal that new hires can access as soon as they are hired. This eliminates the reliance on people to support this process. Your staff can be freed up to do the critical clinical work.
The portal should include all the necessary information and resources that new hires need to get started, such as company policies, benefits information, job descriptions and contact information for key staff members. Additionally, the portal should include interactive modules, such as quizzes and checklists, that new hires can complete to ensure they understand and comply with company policies and procedures.
Another critical component of the portal should be a messaging system that allows new hires to communicate with their managers and other key staff members. This messaging system can answer new hires’ questions and provide feedback and support as they navigate their new roles. Don’t wor-
ry about losing the human touch, as automation can be set up to allow for continuous communication and connection.
• Email reminders: Set up automated email reminders sent to new hires at specific intervals, reminding them to complete particular tasks or paperwork. These emails can be triggered based on the new hire’s start date or can be set up to be sent at specific intervals after the start date.
• Text message reminders: Similar to email reminders, text message reminders can be set up to be sent at specific intervals to remind new hires to complete specific tasks or paperwork. This can be useful for new hires who may not have regular access to email.
• Calendar invites: Automatically schedule calendar invites for new hires, reminding them of important deadlines and tasks they need to complete. These invites can be set to recur at specific intervals or dates.
• Task management software: Use task management software like Trello, Asana, etc., to assign tasks to new hires and set due dates for completion. This will allow new hires to see all their tasks in one place and track their progress.
• Reminder in the onboarding portal: Include a reminder in the onboarding portal that new hires can see when they log in. This can be a simple message or a list of tasks that need to be completed.
Personalized reminders: Use a personalized approach by assigning a mentor or a team member to follow up with new hires and remind them of the tasks they need to complete.
Imaging leaders can also use the onboarding portal to track the progress of new hires, ensuring that all necessary information and resources have been reviewed and all tasks have been completed. This allows leaders to identify and address any issues that may arise during the onboarding process and support new hires as needed, instead of finding out during a TJC inspection!
Overall, automating the new employee onboarding process can save precious time and resources while ensuring that new hires have the information and support they need to succeed in their new roles.
Onboarding is one of the most critical elements in ensuring that employees have a positive experience and will ultimately remain with the company. Hence, we need to have a well-established and sustainable onboarding process. •





Anna Meiners, MBA, RT(R)(CT), is the radiology manager at the UC Health Drake Center in Cincinnati, Ohio. This month’s rising star is a Cincinnati native pleased to be able to give back to her hometown community. ICE recently learned more about Meiners in a question-and-answer session.

Q: WHERE DID YOU RECEIVE YOUR IMAGING TRAINING/EDUCATION?
A: I graduated from UC Blue Ash with my associate’s and bachelor’s degrees in radiology and then received my MBA from Indiana Wesleyan University.
Q: HOW DID YOU FIRST DECIDE TO START WORKING IN IMAGING?
A: I knew early on I wanted to work in health care, but I wasn’t sure exactly what I wanted to do. When I was a junior in high school, I had a conversation with one of the seniors that was going into radiology. I thought back on my own personal experiences in radiology when I broke my arm three different times as a child and decided that was the field I wanted to pursue.
Q: WHY DID YOU CHOOSE TO GET INTO THIS FIELD?
A: My personal experience is what brought me to radiology, but I quickly learned I knew very little about radiology as a whole. The world of radiology is an expansive field that is ever-changing. It is simply astonishing the different ways we can care for patients within the realm of radiology.
Q: WHAT DO YOU LIKE MOST ABOUT YOUR POSITION?
A: As a manager, I thoroughly enjoy being part of a solution to a problem. There is nothing that makes me feel more accomplished professionally than creating solutions that positively impact both patients and staff.
Q: WHAT INTERESTS YOU THE MOST ABOUT THE IMAGING FIELD?
A: I have always said that radiology encounters almost every patient within a hospital, whether it be inpatient, outpatient or patients coming through the ER. We, as imaging professionals, have the knowledge it takes to run the equipment that allows phy -
sicians to diagnose, monitor or perform treatment. One of my favorite metaphors I’ve seen regarding imaging professionals is “We are the eyes of medicine, and without us, all would be blind.”
Q: WHAT HAS BEEN YOUR GREATEST ACCOMPLISHMENT IN YOUR FIELD THUS FAR?
A: Looking back over the years, I would say my greatest accomplishment was building a successful mobile mammography program from scratch. From the refurbishments of the coach, to building my team, scheduling of events, to the success stories where cancer was found early simply because we took the screenings to women versus women having to take time out of their day to come to us. We created an environment that made it convenient for women.
Q: WHAT GOALS DO YOU HAVE FOR YOURSELF IN THE NEXT 5 YEARS?
A: My goal is to become a radiology director. I intend to continue learning and expanding my knowledge in radiology overall with a focus on the operations/business side of the field. •
FAVORITE HOBBY: Cheering on the Cincinnati Bengals!
FAVORITE SHOW: “Ted Lasso”
FAVORITE FOOD: Indian or Asian
FAVORITE VACATION SPOT: Exuma Bay, Bahamas
1 THING ON YOUR BUCKET LIST: Travel to Scotland
SOMETHING YOUR CO-WORKERS DON’T KNOW ABOUT YOU: I was homeschooled from 3rd-10th grade and my mom put me in to Irish dancing for PE classes.
Andrew Sandstedt has always been an artist, but it took some time for him to take his talents into the professional sphere. As a teenager, he’d considered pursuing an arts degree after high school; his parents convinced him to get a business degree instead. When Sandstedt would see his classmates clutching their art portfolios on campus, he’d think, “Well, maybe someday,” and redirect his focus to his schoolwork.
“In art, like anything you do with life, there’s all kinds of paths that build on each other and move you forward,” Sandstedt said. And so his passions continued to reveal themselves in the novel interludes of his day. Murals that Sandstedt had painted in his children’s bedrooms circulated at a baby shower, where an interior decorator took notice of his work.
She hired him on for a few commissions, and as job cuts came through the ad department at his newspaper job, Sandstedt took on more painting work to pick up the slack. Eventually, he spun off his own painting business, which ran from 2005 until 2018, delivering services like finishing, plastering, and mural arts, typically in high-end residential and some commercial settings.
“I had a lot of repeat business from people who I had worked for, and then worked with a woodworker, and stayed busy,” Sandstedt said.
After a divorce, however, Sandstedt needed full-time work. He had picked up a bit of welding instruction some years earlier, learning from the shop foreman at his father’s machining company on his lunch break. When he
landed at the Holt, Michigan headquarters of Block Imaging, his skills were put to use as mechanical team lead, installing and de-installing medical imaging equipment at various sites across the country.
Neither did Sandstedt back-burner his artistic interests. When some friends at Friendland Industries, a metal processing plant in the Old Town district of Lansing, Michigan had an idea to showcase metal artists in town, Sandstedt put his welding acumen to use supporting an event they called ScrapFest.
“You have an hour to come in and pick up to 500 pounds of scrap, and then build something in a week,” Sandstedt said. “It was a fun thing, and then every year, I just kept doing it; coming back, and growing, and learning more about metalworking, and loving that art form.”
In 2023, ScrapFest will celebrate its 13th iteration; in that time, Sandstedt’s artworks have taken home two first-place wins, two second-place wins, and a people’s choice win. His pieces have also set the post-competition auction record three years in a row. After a time, he was recruited to craft the trophies for the ScrapFest winners, which led to a new line of business making custom metalwork trophies for events throughout the Old Town community – beard-growing competitions, business awards, and sports tournaments, to name a few. Sandstedt has even created trophies for in-house chili and basketball contests at Block Imaging.
“I’m going to make art until the day I die; I’m not just going to retire and do nothing,” Sandstedt said. “That’s why I love working at a place like Block that gives me the opportunity. My job lets me do a lot of things in life that the art might not let me do. Having a job that lets me take vacations and pay all my bills allows me to go make what I want to make.”

Sandstedt’s artist philosophy is “creativity within confines.” He enjoys the logical exercises of making art within the limitations of found objects, or a commissioned assignment, and expressing himself there.





“Sometimes people have such an open end to what they’re supposed to do that it limits them,” he said. “They can have so many options it’s hard to pick one.
“I always talk about the movie ‘Apollo 13,’ ” Sandstedt said. “Things go bad, and they have to fix the problem to get to Earth. They dump a box on the table and say, ‘Here’s what we have. How do we use this material to make it work?’ That’s why I love the challenge of using repurposed and reclaimed stuff: it forces you to completely think in a different way.”
Sandstedt doesn’t believe he will ever fully retire from working his weekday job, but he does intend to focus more on custom work, and eventually, a gallery show of his portfolio. He would like to design some furniture with his sons, a mechanic, a machinist, and a woodworker, respectively; he’d love to place one of his pieces in a sculpture park. But whatever form his work takes, it’s most important to Sandstedt that he continues to grow as an artist.
“People ask me, ‘What’s the best piece of art you’ve made?’ ” he said. “Well, I haven’t made it yet, but you can
see the growth every year. The stuff I made when I was 25, versus 35, versus 45, it gets better all the time.”
“All these people that I admire, I always look at these big pieces and think, ‘How old was this artist when they made this?’ ” Sandstedt said. “It takes a while to hone in on what you’re good at, and get better and better. To be a master craftsman, you’re always learning, you’re always doing, you’re always teaching. I look at my nephews and sons who are in their early to mid 20s, and the deception of social media makes it look so easy for everybody to hit this stride full-tilt.”
As a working artist, Sandstedt also finds himself becoming an ambassador for the fine arts among friends and guests to his home. His walls and shelves are lined with original artworks from local artists, and when people ask him, “Where’d you get this?” he’s able to reinforce the connections that link the arts with their patrons.
“There’s some things that face-to-face interactions do,” Sandstedt said. “You’re not going to create this feel by something you’ve bought at Hobby Lobby or Target that’s been screen-printed and mass-produced.”
“When you communicate your craft to people, no matter what you do; when it’s original, and someone’s been developing and pouring themselves into it, it has an intangible X-factor that you can’t explain,” he said. •
Butterfly Network Inc. has received 510(k) clearance for a AI-enabled Auto B-line Counter that may simplify how health care professionals evaluate adults with suspected diminished lung function and can potentially accelerate their ability to make informed treatment decisions at the point of care.
Butterfly’s Auto B-line Counter leverages deep learning technology to produce a B-line count from just a six second ultrasound clip – a drastic change from traditionally manual, subjective counting processes to more consistent interpretation of B-lines. B-lines on an ultrasound scan appear as bright, vertical lines that indicate wetness in the lungs and are associated with pulmonary air-space disease, such as congestive heart failure, chronic obstructive pulmonary disease, pneumonia and COVID-19.
“Our goal at Butterfly is to give healthcare practitioners, and eventually consumers, a real time full color, annotated, window into the human body. Applying AI to make ultrasound easier to use is core to Butterfly and will enable powerful ultrasound to be in the palm of more clinician’s hands, across specialities, to monitor, assess, and prescribe treatments in a more informed way,” said Dr. Jonathan Rothberg, Butterfly Network’s founder and interim chief executive officer. “Our AI-enabled Auto B-line Counter empowers providers to assess lung conditions faster and with more confidence – and in turn, will aid in earlier detection, diagnosis, and
treatment of cardiovascular diseases, a leading cause of death globally, taking nearly 18 million lives each year.”
Butterfly’s Auto B-line Counter algorithm utilizes the state-of-the-art instant percent counting method that assigns numbers to confluent B-lines by the percentage of rib space occupied in addition to counting discrete B-lines – a technique that has been found to be more reliable than incumbent individual line counting methods, according to a press release. With it, trained providers can simply place the probe and receive a reliable number count right on their screen.
To develop and train its AI algorithms, Butterfly uniquely utilizes its secure Butterfly Cloud to access over 3.5 million de-identified ultrasound cines. These data inputs come from hundreds of sites across all 50 states in the U.S., offering potential for a broad and diverse range of age, gender, body mass index, ethnicity, and race. Continuing its credo to democratize healthcare by making medical imaging accessible to everyone around the world, Butterfly leverages this cloud data, in part, with the aim of creating more representative technology that the company believes will help bridge the divide in health technology experienced across diverse populations.
The company anticipates that the AI-enabled Auto B-line Counter will launch early summer in the United States.
The Medical Imaging & Technology Alliance (MITA) has announced that Paola Wisner, M.S., vice president of global research and development for Hologic’s Breast and Skeletal Health Solutions Division, will join the MITA Board of Directors.

Wisner, who has more than 20 years of professional experience in medical technology research and development, has led transformational company-wide initiatives to build a strong innovative culture, deliver sustainable growth, and to improve speed-to-market through organization, continuous improvement, and quality.
Prior to Hologic, Wisner worked at Hollister Incorporated, Medtronic’s Spinal and Biologics Business Unit, at the Dobelle Institute for Artificial Vision, and at Columbia University’s Biomechanics Laboratory.
“I am honored to represent Hologic and serve on the MITA Board of Directors,” Wisner said. “I look forward to collaborating with MITA staff, committees and board members to collectively advocate for the medical imaging industry and health care providers as we can continue to develop exceptional technologies and products that enable healthier lives for patients around the world.”
In addition to her professional experience, Wisner is passionate about education serving on the Board of Managers for Columbia Engineering Alumni Association and Chicago’s Metro Advancement Council at Midtown Educational Foundation. Through her public and private sector experience, she seeks to broaden access to high quality education by supporting innovation, reducing barriers to entry and building strong communities.
“Paola’s leadership, experience building partnerships that have delivered results across a portfolio of medical technology research initiatives, and educational track record make her an ideal fit for MITA’s Board of Directors,” said Patrick Hope, MITA’s executive director. “On behalf of MITA and all its members, we welcome her to the board of directors and extend our appreciation for her commitment to the value medical imaging delivers patients and providers.”


Come experience everything Arizona and Colorado have to offer. Life doesn’t get much better than 300 days of sunshine, hiking, biking, lakes, rivers, and so much more. We invite you to our out patient imaging centers where your feedback and life work balance are valued.






GE HealthCare recently announced that the next-generation bkActiv is available for guiding urology, colorectal and pelvic floor surgical procedures. The flagship intraoperative ultrasound imaging system, developed by BK Medical – a subsidiary of GE HealthCare – was designed to deliver high-performance ultrasound guidance with a simplified, intuitive user experience for surgeons.
“The bkActiv’s automatic no-touch autogain and advanced algorithms provide unmatched image quality, enabling confident decision making during surgical procedures. The system allows for minimal user interaction so that surgeons can focus on their patients,” according to a news release.
“By expanding the bkActiv system, we are giving physicians the tools they need to provide precise treatment with the ability to see fine details in image guidance, which ultimately may allow for better outcomes for people who require urology, colorectal and pelvic floor procedures,” said Urvi Vyas, general manager, surgical visualization & guidance, ultrasound at GE HealthCare, “We are proud to be the trusted partner for surgeons around the world given our long history of leadership in imaging and innovation.”
The bkActiv is a high-performance imaging system that allows for detailed, real-time surgical visualization, refined through decades of research, real-world use and extensive user feedback, the release states.
“With this addition, the bkActiv now supports next-level image quality of the prostate, kidney, and bladder, and has sensitive color doppler to visualize and measure the speed and direction of blood flow during the most complex surgical procedures. Combined with the new advanced portfolio of specialized, sterilizable transducers, needle guides, and procedure packs, the solution is designed to assist surgeons from simple procedures, such as biopsies, to the most advanced robotic surgeries,” the release reads.
The system’s features are designed with the physician in mind, and include:
• Intuitive design with True-Sense touch technology and Smart Button that allow surgeons to operate the system with one hand for full control during the procedure
• Advanced transducer portfolio including robotic and laparoscopic transducers
• Adjustable monitor mounted on a flexible arm that allows for optimal image viewing with landscape or portrait mode
• Easy integration into a crowded operating room due to its minimal system footprint



Royal Philips has announced the availability of Philips HealthSuite Imaging on Amazon Web Services (AWS). Additionally, Philips and AWS will build on their relationship, advancing AI in health care by applying foundation models using Amazon Bedrock to accelerate the development of cloudbased generative AI applications that will provide clinical decision support, help enable more accurate diagnoses and automate administrative tasks.
The availability of Philips HealthSuite Imaging on AWS is a new addition to Philips’ broad capabilities in enterprise informatics, enabling improved image access speeds, reliability and data orchestration for radiologists and clinicians across the entire imaging workflow – from diagnosis to therapy selection, treatment and follow-up. Clinicians will be able to access the latest innovations from any location, and health care organizations can reduce costs previously invested in on-premises hardware or data centers to host their image management platform.
Philips can help clinicians manage growing
workloads amidst staff shortages and speed time to diagnosis and treatment, enhancing patient outcomes. Philips HealthSuite Imaging will use Amazon HealthLake Imaging to increase scale, deliver fast time to first image, enable easy re-use of images for machine learning and research, and reduce medical imaging costs.
Philips will also use Amazon Bedrock as part of its efforts to develop generative AI applications to advance PACS image processing capabilities and simplify clinical workflows and voice recognition. Amazon Bedrock will enable Philips to develop machine learning-based applications quickly and reduce model development costs versus building foundational models (FMs) from scratch or running multiple task-specific model development efforts.
Philips and AWS provide migration expertise and planning services, total-cost-of-ownership analysis and cybersecurity technical expertise to enable an easy migration from on-premises to cloud-based solutions for customers.
The health care system is a substantial contributor to greenhouse gas emissions, and radiology’s role in the health care system presents an opportunity to lead low-carbon, sustainable initiatives in workplaces and communities, according to a special report published in Radiology , a journal of the Radiological Society of North America (RSNA).
The special report addresses the importance of climate change to radiologists and the medical imaging community, including the impact on human health and health equity, the contribution of health care and medical imaging to the climate crisis, and the impetus to build a more sustainable future.
“The focus is on actions and opportunities to address climate change in our role as radiologists and to link our actions with their impact and expected outcome,” said the report’s senior author Kate Hanneman, M.D., M.P.H., associate professor in the department of medical imaging at the University of Toronto and sustainability lead at University Medical Imaging Toronto in Toronto, Canada. “Because radiologists are adept at managing rapid technological change, we are ideally positioned to lead these initiatives within our departments, health care systems and communities.”
Climate change occurs due to increasing carbon dioxide (CO2) and other greenhouse gases in Earth’s upper atmosphere. Due to its large size and its intensive use of resources, the global health care system emits more than 2 gigatons of CO2 equivalent annually and accounts for 5 to 8.5% of total greenhouse gas emissions in developed nations.
While the majority of greenhouse gases emitted by the health care sector come from manufacturing, transporting, using and disposing of purchased goods, the sources of emissions from individual specialties differ. For diagnostic radiology, most emissions come from the production of medical imaging equipment and the energy needed to power it. Overall, medical imaging is estimated to account for 1% of global greenhouse gas emissions.
Although the dangers of climate change have been known for decades, health care has been slow
to address its substantial carbon footprint. However, there is a growing movement to align health care’s environmental practices with its core mission to minimize harm and protect public health.
“The harmful health effects of climate change disproportionately impact those already vulnerable due to social, environmental and public health factors,” Hanneman said. “Groups most likely to be harmed are those already experiencing health inequities due to age, race, culture, sex/gender, socioeconomic status, geographic location and chronic illness.”
As the focus on sustainability increases, radiologists are well positioned to play a leading role in pushing for greener health care. As experts in technology, radiologists can innovate more sustainable methods of care, such as finding new applications for telemedicine and telecommuting, reducing energy-intense imaging sequences that do not add clinical value, and scheduling patients more efficiently to minimize idle time for equipment. As key players in the purchasing process, radiologists can prioritize the energy efficiency of equipment in their purchasing decisions and work with vendors to improve the sustainability of their products.
The report outlines a framework for environmentally sustainable health systems that can be applied in radiology departments. First, reduce demand for health care services by supporting policies and programs that promote public health, including screening. Second, match the supply of health services to the demand; for example, by ensuring the appropriate use of imaging. Finally, reduce emissions from the provision of necessary care.
The authors also offer several toolkits highlighting actions institutions, organizations and individuals can take to address climate change.
“On the current trajectory of greenhouse gas emissions, climate change will become the defining narrative of human health,” Hanneman said. “Mitigating emissions offers the opportunity for a future in which local and global populations not only survive but thrive.”

Appleton Area Health, in Minnesota, is the first to offer patients one of the most advanced X-ray systems. The KDR Flex Overhead X-ray System with Dynamic Digital Radiography (DDR) allows health care personnel to observe the bones and organs while in motion.

This new technology allows physicians and health care providers to observe the full range of joint motion to help evaluate suspected injuries. Physicians can now watch a patient’s motion of lungs and diaphragm during breathing to better analyze and diagnose suspected lung nodules, chronic obstructive pulmonary disease known as COPD, and interstitial lung disease to determine whether the diaphragm is paralyzed.
Dr. William Vandivier, medical director, Appleton Area Health, said, “If a picture is worth a thousand words, X-ray imaging in motion is worth millions more. With DDR, doctors can view a patient’s full range of motion in joints, extremities, neck and spine. This capability provides immediate information for diagnosis, surgical planning, and treatment follow-up, resulting in more individualized patient care.”
GE HealthCare is further advancing its precision care strategy with CT-Navigation, which offers clinicians detailed, real-time, 3D computed tomography (CT) images for stereotactic needle guidance across an array of care areas, including interventional and oncological procedures as well as biopsies, ablations, drainage, therapeutics and more.

Interventional radiology – and specifically interventional CT – plays a key role in the diagnosis and treatment of disease. Providing highly detailed images of internal structures – such as bones, organs, and tumors – CT-guided interventions can assist clinicians in performing minimally invasive procedures that guide stereotactic needles through the anatomy to biopsy or deliver treatment directly to affected tissue. As a result, interventionalists benefit from greater visibility and confidence in needle placement, while patients benefit from more accurate and precise care.
“Consistent and accurate ‘navigation’ through the body is key in delivering precision care,” explains Prof. Laura Crocetti, associate professor of radiology, division of interventional radiology, University of Pisa in Italy and deputy chairperson of the European Conference on Interventional Oncology (ECIO). “CT-Navigation is an intuitive technology that helps us achieve this by enabling clinicians to select and follow an out-of-plane trajectory for a safer path that avoids critical organs and reaches deep-located targets with impressive accuracy, while reducing procedure time and possibly radiation dose. Altogether, it helps us ensure better patient outcomes while expanding the boundaries of our practice.”
While many of today’s CT-guided solutions require
that interventionalists take multiple control scans and awkwardly position themselves and the needle inside the gantry of a CT system – increasing the risk of radiation exposure to the clinician – CT-Navigation enables a more comfortable and safe experience. Instead of working wholly within the CT system’s narrow bore, interventionalists using CT-Navigation can simply place a sensor on the patient inside the gantry. After scans are complete and the patient is removed from inside the system, interventionalists have full range of motion while navigating a needle more easily and safely through the patient’s anatomy using the placed sensor and detailed CT images.
“To achieve precision care, we must provide clinicians with the tools and insights they need to deliver the right treatment, at the right time, to the right patient,” explains Jean-Luc Procaccini, president and CEO, molecular imaging and computed tomography, GE HealthCare. “CT-Navigation does just that – acting as an anatomical GPS for interventionalists to use and care for patients with increased ease and accuracy. We are thrilled to now increase global access to this innovative solution and its many clinical benefits to healthcare systems around the world.”
CT-Navigation was developed by IMACTIS and became part of the GE HealthCare portfolio of solutions upon close of the previously announced acquisition of the France-based company.
It is the result of more than a decade spent studying provider needs and designing a navigation system to improve safety, increase accuracy and enhance the intervention workflow. •





RSTI is committed to improving the quality of diagnostic imaging service and helping students advance their careers through knowledge, education and hands-on, technical learning.

“Having completed Phase I: Principles to Servicing Diagnostic X-Ray Systems at RSTI was a large factor in getting selected for my current position with Mayo Clinic in the Medical Imaging Department.”
“RSTI teaches you how to work on a modality, not single machines…learning the theory then the process of how the machine works and how to service it gives you a good foundation and makes you ready for any model.”

COMPLETE SUPPORT PARTNERFOR OUR SERVICE CUSTOMER:


• Hands-On, Technical Training
• Imaging Parts Inventory – Tested and Ready to Ship!
• Service Support – Tube Installs, PMs, etc.
• Technical Support – Access to 174+ years of Instructor Technical Expertise

• Equipment Options – Including Mobiles
ISO 9001:2015 CERTIFIED (IQC CERTIFICATE NO. Q-1158)
The recent ICE webinar “The Power of Dedicated Breast CT: Why Healthcare Leaders Should Consider This Innovative Imaging Option” presented by Nicole Dhanraj, Ph.D., SHRM-SCP, GPHR, CPPS, CSSBB, PMP, CRA, R.T (R)(CT)(MR)(FAHRA), was eligible for 1 credit from the ACI. It is also approved for 1.0 Category A ARRT continuing education credit. AHRA ref: LEC12116 (expiration date: 4/30/2024).
Breast cancer diagnosis can be a complex and time-consuming process, often involving multiple imaging exams and follow-up appointments. Unfortunately, this can lead to reduced participation from women who want to avoid the discomfort and inconvenience of traditional screening methods.
In this webinar, Dhanraj explored how breast CT imaging can offer an adjunct imaging technique that can be used alongside mammography to provide a more comprehensive approach to breast cancer detection. She emphasized the benefits of dedicated breast CT technology, including improved workflow and patient outcomes. She helped attendees discover how breast CT imaging can positively impact a breast cancer diagnosis program and improve outcomes for patients.
Dhanraj provided additional insights via a question-and-answer session with webinar attendees.
One question was, “What is the cost versus standard mammo?” Another attendee asked how long it takes to do the CT scan and receive results from a biopsy. The complete Q&A is included in the on-demand recording of the webinar. It is available for free viewing at ICEwebinars.live.
Attendees provided feedback about the session via a survey that included the question, “Why do you join ICE webinars?”
“To learn the latest and most relevant information in imaging,” said Angela Harris, mammography care coordinator, Harris Health System.
“The content is always relevant and timely, very professional presentations,” added Nancy Godby, director of radiology, Cabell Huntington Hospital Inc.
“I received an email with this topic and although I am not clinical in nature, I enjoyed the topic and of course with a wife and two daughters it hit home. Also being a clinical equipment project manager and my wife being a cancer research nurse the topic was very relevant,” said Gerald McNeil, clinical equipment project manager, Northern Light Health.
For more information, visit ICEwebinars.live.

exams, according to Reportlinker.com.
According to a report published by Next Move Strategy Consulting, the magnetic resonance imaging (MRI) m arket generated $7.55 billion in 2022, and is projected to generate $12.19 billion by 2030, witnessing a CAGR of 6.2% from 2022 to 2030. The research offers a detailed analysis regarding drivers, restraints and opportunities to highlight changing market dynamics of the market. Moreover, the research provides an extensive analysis of major segments and their sub-segments to determine fastest-growing and highest revenue-generating segments.

A Reportlinker.com report on the magnetic resonance imaging market also predicts growth.
According to the World Health Organization (WHO), in 2021, various types of chronic diseases, such as cardiovascular diseases, cancer, chronic respiratory diseases, and diabetes, are responsible for approximately 17.9 million, 9.3 million, 3 million, and 1.5 million deaths, respectively. Also, the growing necessity and demand for innovative medical imaging technology to cater to the rise in injury, illness or congenital abnormalities in children fuels research and development activities globally. For instance, in March 2021, Philips announced a partnership with The Walt Disney Company to improve the health care experience of children. Philips partnered with European Hospitals for their first clinical research pilot program, which aimed at reducing fear and anxiety to improve children’s patient experience during MRI
“However, factors such as high cost of MRI systems and requirement of complex or high-tech infrastructure for installation and maintenance of these systems are restraining the growth of the market during the forecast period. On the contrary, integration of artificial intelligence (AI) in medical imaging including MRI by providing deep learning solutions for image acquisition, reconstruction and supporting clinical decision-making is expected to create ample opportunities for the market in the coming years,” the report adds.
The North America market is projected to hold the dominant share by 2030, Reportlinker states.
North America holds the largest market share of MRI market due to factors such as presence of a large pool of elderly population in countries such as the U.S. and Canada. The elderly population are prone to bone disorders and need MRI for the diagnosis and treatment of their medical condition. For instance, in July 2019, according to the United States Census Bureau, the total number of people 65 and older was 54.1 million in the country. Moreover, the presence of established health care systems in the region owing to the increased expenditure on health care by countries such as the U.S. and Canada enable public health care providers to adopt advanced MRI systems. These factors drive the growth of the MRI market. For instance, in 2021, according to the Center for Medicare & Medicaid Services (CMS), the U.S. Government spent $4.1 trillion in the health care sector to improve and maintain public health activities in the country, the report states.
In addition, a report from the The Insight Partners states that the pediatric MRI market could be worth $5.6 billion by 2028. •
The SIGNA PET/MR system performs PET and MR scans simultaneously, enabling customers to schedule a single study. The PET component boasts high sensitivity, offering lower radiation doses for radiation-sensitive patients like children, or faster scans with the same dose for patients who have difficulty remaining still for the duration of the scan. The pioneering Timeof-Flight PET technology provides crisp images, while Q.Clear reconstruction delivers 2x improvement in image quality. The system is also equipped with a premium 3.0T MR and AIR Recon DL, which enables reduced scan time without compromising image quality. Additionally, the SIGNA PET/MR is integrated with AIR coils, designed to reduce attenuation artifacts in PET images caused by the coils themselves. These soft, conformable, blanket-like coils are also faster to set up, helping to improve workflow and reducing technologist exposure to patients injected with radioactive isotopes. To address image artifacts caused by patient motion, MotionFree Brain¹ on PET and PROPELLER on MR are integrated motion correction technologies that can reduce image artifacts from non-compliant or subtly moving patients.
¹ MotionFree Brain is not yet CE marked. Not available for sale in all regions.

Fujifilm’s new ECHELON Synergy MRI 1.5 Tesla scanner is designed to provide its users with fast, effortless operation, streamlined workflow and enhanced patient experiences by combining powerful architecture and deep learning reconstruction with single-touch shortcuts and multiple on-gantry controls. The system’s SynergyDrive, which is powered by AI, is designed to deliver 50% scan time reductions from previous generations MRI and reduce image noise. The ECHELON Synergy has a 70cm wide bore and a 62 cm wide table to accommodate different patient sizes. The system will be available in the U.S. upon completion of regulatory requirements.


Swoop Portable MR Imaging System, the world’s first MR imaging system capable of providing neuroimaging at the point of care, can inform the timely diagnosis and treatment of acute conditions within a broad range of clinical settings.
A new breakthrough in 3.0T imaging is the MR 7700. With its XP gradient, it delivers on the clinical expectations of today, and helps to facilitate the most demanding research programs. It is the system of choice for advanced neuroscience and highest quality diffusion imaging, providing up to 35% higher signal. Combining imaging excellence with multi-nuclei integration, the system facilitates advanced workflows that accelerate exams and improve patient-centered productivity.
The MAGNETOM Free.Max MR scanner from Siemens Healthineers extends access to severely obese and claustrophobic patients with the first and only 80cm open-bore system, while offering every patient an improved experience. The most lightweight, compact whole-body MR scanner ever offered by Siemens Healthineers at under 3.5 tons and less than 80 inches high, scanner has a novel magnet design that requires less than 1 liter of helium, contributing to reduced infrastructure and total cost of ownership. Deep Resolve algorithms perform targeted denoising and employ deep learning to deliver sharper, higher-resolution images while reducing acquisition times. The myExam Companion workflow solution incorporates artificial intelligence to help the user navigate the examination more efficiently. The unique field strength of the MAGNETOM Free.Max enables new clinical applications that can improve implant imaging, reduce susceptibility challenges and present new opportunities in pulmonary imaging.
The 1.5T uMR 680 excels at patient comfort, high resolution imaging, and fast, quiet scanning. It’s designed with features to meet the demands of hospitals, including: a detachable table; SuperFlex blanket-style coils that conform to the patient; QScan for quiet imaging; EasySense touchless respiratory gating; uAI DeepRecon for high resolution and high signal deep learning reconstruction; uCS 2.0 (United Compressed Sensing) for fast 2D/3D/4D exams. Comes fully configured (all-in configurations) and features software upgrades for life to keep it modern throughout the entire life of the scanner with a service agreement.






Our focus at Medical Equipment Doctor is to partner with healthcare administrators to keep their budget and costs in check through providing top-level refurbished equipment sales, service, and rentals, for all their medical equipment needs. This has led our company to be recognized nationally as the affordable solution to purchasing brand new medical equipment.

At RENOVO, we value knowledge, reliability, and integrity in our employees. If you are interested in being a part of a team that is committed to making a difference in healthcare equipment maintenance and healthcare asset and technology management, we invite you to apply for one of the open positions. We are always looking for talented, passionate, hard-working people to join our team.



The InterMed Group is a healthcare technology management company meeting the needs of our customers for over 20 years. InterMed sells and services medical equipment for our customers across the country and is growing quickly. As a result, InterMed is looking for an Imaging Field Service Engineer to perform repairs and preventive maintenance. This individual would be responsible for maintaining, inspecting and repairing imaging equipment for our accounts in the area and must be willing to travel for work.
As one of the largest faith-based, nonprofit health systems in the U.S. we play a huge role in the communities we serve in the greater Dallas Fort Worth area. Our mission is “to improve the health of the people in the communities we serve” and we get it done every day. Imagine the power of 26,000+ team members with a singular focus and determination.
First Call Parts has been providing customers with quality replacement imaging parts since 2009. We pride ourselves in developing a top-notch reputation in the imaging industry as delivering the best in diagnostic imaging replacement parts. We specialize in the sale of refurbished/tested and used, Philips, Siemens, and GE in the Cath/Angio, R/F, and RAD modalities.

Agiliti is a nationwide company of passionate medical equipment management experts who believe every interaction has the power to change a life. Our industry-leading commitment to quality and team of expert technicians helps ensure clinicians have access to patient-ready equipment needed for patient care. Make an impact in healthcare and grow your career with Team Agiliti!


Universal Medical Resources’ operating principles are based on practicing the core values of Collaboration with the nuclear medicine community; embracing Diversity of ideas, beliefs, and practices; commitment to Excellence in producing the highest quality outcomes; and recognizing our Ethical Community through actions guided by fairness, trust, honesty, and integrity.

Do you want to work in healthcare? Would you like to make a difference in the lives of patients and their families? Do you enjoy a new challenge every day? If you are skilled at servicing medical equipment in a clinical setting, we hope you will join our team!
Associated Imaging Services has been offering nuclear medicine and ultrasound solutions to our customers since 1990. We specialize in the sales and service of new and refurbished nuclear medicine cameras and ultrasound systems throughout Kansas, Oklahoma, Texas, and the surrounding areas.


In a recent white paper, Tina Azar, vice president and market leader for global analytics firm EXL Health, reported that one in five medical claims and one in six hospitalizations can include a “surprise bill” or “balance billing” from an out-of-network physician. That these issues might present themselves during emergency care, when a patient may be least able to advocate for themselves, or answer insurance questions; or when receiving services from an ancillary provider at an in-network facility, at which a patient might reasonably believe its providers participate in their health insurance, is challenging enough. Compounding that fact, Azar wrote, is that surprise and balance billing are proving to be among the leading causes of medical debt in America.
That’s per an April 2021 study in the Journal of the American Medical Association, “Frequency and Costs of Out-of-Network Bills for Outpatient Laboratory Services
Among Privately Insured Patients,” which reported that “out-of-network outpatient laboratory services were five times more common than out-of-network emergency department visits, and 34 times more common than outof-network anesthesiology services, and are associated with substantial patient out-of-pocket costs.”
The “No Surprises Act,” embedded within the federal Consolidated Appropriations Act of 2021, is meant to curb this practice, banning surprise bills for most emergency services, out-of-network cost sharing, balance billing for out-of-network providers at an in-network visit, and up-front notice about billing procedures and complaint disputes.
The legislation also requires health care providers to notify their customers, “in clear and understandable language,” whether the provider from which they are seeking services participates in their insurance, the contracted rates and diagnostic codes for the procedure(s) they’re about to undertake, how to find this information if they’re working with an out-of-network provider, and “a good-faith estimate” of both the customer’s and insurer’s shares of their bill, as well as how much they’ve already been billed against their deductible.
In short, the law forces providers to generate and publicize their pricing structures so that customers have
a chance to make a more informed decision before consenting to care. For integrated hospital groups, it reflects a significant intersection of challenges related to staffing, revenue cycle work and compliance. In terms of lines of service, however, its impact is likely to be felt most deeply in the delivery of emergency care and medical imaging.
Angie Bush, system director of radiology services at the University of Texas Medical Branch in Galveston, Texas, said she believes the overall challenge of the law involves keeping radiology, still a revenue generator for many health care institutions, from becoming a commodity service.
“It’s going to change everything for us,” Bush said of the new law, “and interventional radiology is going to be hit the worst.”
Bush foresees a number of complications that could arise for radiology directors, revenue cycle teams, and practice administrators, simply as a function of unintended consequences. What happens, for example, when a referring physician orders the wrong exam? What happens when administrators develop a cost estimate, but other medical deductible payments in process have not yet hit the patient’s insurance?
“We could be off on our estimate simply because of what is still pending,” Bush said. “And what happens to radiology workflow when, instead of protocolling studies after the appointment is scheduled, we have to ask physicians to protocol before scheduling just so we can insure the CPT doesn’t change for the payment?”
Beyond all those wrinkles, Bush also described the lengthy process that must be completed before any potential cash prices can be calculated for those requesting them. It starts with determining the patient’s copay – which can change if that person carries insurance and has met their deductible – and even that’s contingent upon the timing of other medical bills that might have been incurred for routine procedures, ranging from laboratory exams to primary care copays.
“If more bills are issued to say that they met their deductible, it’s going to change, and that’s out of my control,” Bush said. “Say they have a $1,000 deductible, but to get that MRI order, they had to see a doctor. Did that doctor send his bills already? Maybe he ordered labs, or a test that was done somewhere else. These other pending payments may change what my estimate will be, not because the cost of my test changes, but because what
the patient is liable for varies based on other providers dropping their payments and the insurance company recognizing them.
“All of those bills that that patient paid could contribute to their deductible for the year, but if this person comes straight to imaging, we see that they have a $1,000 deductible,” she said. “If they have a deductible, we have to collect that deductible. If we find out that they met that deductible, then we have to reimburse it.”
“This is an error where a patient normally would be happy that they don’t have to pay as much, but we can only give the cash-pay price based on what is documented in the patient’s insurance at the time,” Bush said.
Quoting a cash-pay price for an interventional radiology (IR) procedure is even more complicated, Bush said, and many facilities are still developing their methodologies for doing so. Her institution is starting by compiling an average cost for the most common IR procedures, then ranking them by complexity, and basing a cash rate on those average costs, including any medications and supplies typically needed for the work. At some point, however, doctors will be left to guess as to whether a procedure for which they’re researching protocols is simple or complex, as best as they can surmise ahead of performing it.
“For MRI, CT and nuclear medicine, the big change is that we’re going to have to protocol that order to ensure that that is going to be the actual CPT code that we’re going to perform,” Bush said. “Currently, radiologists protocol exams for the next day; for a cash-pay rate, they have to protocol it before the cash-pay rate is given. Our rev-cycle would call our reading room assistant; the radiologist has to pull that order up, look at the history, and do the protocoling right then and there, so it will interrupt their reading cycle. They give that information to rev-cycle, and they can give a more accurate cash-pay rate.”
Even if those quotes are one-offs, the process of interrupting reading workflows to address providing them is time-consuming, and potentially yields inaccurate results. Bush pointed out that the copay an imaging facility may collect and what the procedure may cost will not always be the same. When that happens, determining who’s responsible for the difference could become an issue.
“I’m curious how this is going to play out,” she said. “If we over- or under-estimate, that’s considered a hit against this rule. We have to get within a certain percentage or dollar amount of accuracy, and any time we don’t get it, we may be penalized financially as an institution.”
“Our organization is a very strong, lean organization,”
Bush said. “Our leaders expect us to look beyond the superficial pain, and get to the root of the cause.”
“If the root of this law is to prevent people from going into debt because of medical expenses, this law isn’t the answer, it’s changing the culture of how we seek care. It’s the Band-Aid; it’s not the root,” she added.
Elyce Wolfgang, director of imaging services at WellSpan Health of York, Pennsylvania, an integrated health care system serving several counties in the south-central region of that state, said that, even as a health care professional herself, she occasionally has a difficult time interpreting her insurance benefits and costs. She hopes the impact of the no-surprises law ultimately will lead to greater pricing transparency for patients overall.
“When you think of someone who has zero health care background and experience, for them to interpret what their insurance actually covers versus in-network, out-of-network; it’s confusing,” Wolfgang said. “That’s where we struggle as a whole. How do we better explain this to people in a way that they can understand it, and it’s easy to understand?”
One of the ways in which Wolfgang believes that medical imaging could be tripped up by the constraints of the bill lies in some of the underlying structure of the industry in 2023. In an effort to maintain competitive pricing while also increasing patient access to services, many imaging institutions rely on teleradiology services for reviewing studies as well as ancillary services provided by specialists like anesthesiologists, which inadvertently could expose patients to out-of-network costs.
“It’s not like we have signage posted in the hospital that if you come in for a CT scan, the radiologist’s report is going to come from a third party,” Wolfgang said. “Obviously, we have credentialing to ensure safety, but you don’t know, as the patient – and even as the health care provider, I wouldn’t even know where to begin to inform the patient – that your test went to an outside radiologist.”
To ease customers into the work of calculating pricing prior to scheduling a service, or to avoid balance billing, facilities like WellSpan are coming up with pricing calculators that patients can use to estimate the anticipated costs of their visits.
“We have a price estimator tool where the patient can log into their chart, get an estimation for their study, and it links in their insurance,” Wolfgang said. “It will give a
“When you think of someone who has zero health care background and experience, for them to interpret what their insurance actually covers versus in-network, out-of-network; it’s confusing.”
- Elyce Wolfgang
pretty decent, pretty accurate estimation; what is doesn’t always take into consideration is have you met your deductible yet, and do you have coinsurance. Sometimes it pulls that, and sometimes it doesn’t. That information is only as good as the information the patient provides us.”
Despite attempts to capture accurate information, pricing can fluctuate for any number of reasons. Some studies, like mammograms, may be statutorily covered by insurance under state screening mandates; however, additional imaging that might be needed as a follow-up may not be. Some patients don’t understand the differences among copay, coinsurance, and deductibles, let alone how study pricing is determined; and Wolfgang believes that, beyond any of it, many patients will simply elect to receive care at the facilities where they are most comfortable, regardless of whether it’s the lowest out-of-pocket cost.
“I think the majority of patients are still going to ignore the price tag,” Wolfgang said. “Let’s say I’m familiar with my health system, and the CT that I get here is going to cost me $100 more than if I go somewhere else, but I love my doctors and my experience here. I’m willing to pay a little more out of pocket to stay here than go with another organization.”
“We’re headed in the right direction, but I just don’t think we’re there yet as an imaging industry,” she said. “I think we’re a while away from getting there, wherever ‘there’ may be.”
Dr. Howard P. Forman, MBA, FACR, is a professor of radiology and biomedical imaging, public health (health policy), management, and economics at Yale University. He believes that, although the no-surprises law reflects a greater effort to gain more price transparency overall, that is the responsibility of larger health care institute on the whole, and not specifically of the field of radiology.
“Nobody expects that full transparency will result in a dramatic transformation in anything,” Forman said. “There’s no certainty that it will result in greater positive change; there are even concerns that full transparency will result in higher prices. But we believe that perfect information al-
lows consumers to make better decisions, and it includes both price as well as the value of what they’re buying.”
To Forman, radiologists and practice owners must address both the consumer understanding gap in what services they’re buying when patients contract for them, as well as the options for selecting a practitioner or a facility, and the impacts to care and costs that are conferred with those decisions.



“There are a lot of people that have responsibility here,” he said. “In an ideal world, hospitals could contract for consummate services, and take responsibility for any costs that occur outside of the network that they are selling. If a hospital tells a patient when they roll into the ER that they are in the network, that hospital could figure out how to take responsibility for anyone who is not in network for that person, and then contract with people who are in network.”
“Radiologists are often hospital-based providers,” Forman continues. “If a radiologist is performing services for a hospital that is Company X, and the radiologist is not a provider for Company X, that seems like something that can be figured out ahead of time. Most of the cost of radiology is tied up in the technical component, and hospitals do have the ability to transmit current data on these things.”
As institutions approach questions of price transparency, Forman noted that the federal government, to date, has been more concerned with developing compliance with the law than achieving perfection. He described the attitude around enforcement as one of being “extremely understanding,” and offering plans for remediation rather than assessing financial and legal penalties as an incentive to getting everyone onboard. Once enforcement actions shift, however, and the consequences for failing to comply with the rules become more significant, facilities could be subjected to corrective action plans on strict timelines, with automatic fines incurred.
“No one’s saying that they have to be perfect; they just have to comply,” Forman said. “We all have to play our part.” •
Avante Health Solutions was created through the acquisition and successful integration of nine different companies that were viewed as “best in class” in their respective fields of service.
“Through calculated harmonization of these legacy organizations, Avante has created a holistic value proposition unrivaled in the biomedical support space,” Avante Health Solutions Vice President Enterprise and Strategic Accounts Dur Thomason said. “With broad capabilities and shared operational efficiencies, Avante Health Solutions can partner with our customers in every phase of the life cycle of medical equipment, from consultation and acquisition, installation and support, to service and disposition of assets.”
Thomason recently shared more information about the company with ICE magazine.
Thomason : As a comprehensive independent service organization, Avante is continuously innovating new repair technologies to drive down service costs without sacrificing quality or diagnostic deliverables. As part of that offering, Avante has created Remote Technology Solutions to empower our partners with a revolutionary brand-agnostic tool for service and support. This robust and proprietary technology utilizes predictive analytics that lead to service efficiencies, such as faster diagnosis and repair of equipment. Further, our Remote Technology Solutions helps customers prevent catastrophic equipment failures and avoid downtime.
Thomason : COVID and economic pressures certainly impacted the health care industry and service businesses. However, Avante’s size, scope of capabilities and innovations in repair and service mitigated many of the resulting challenges we faced. Avante services customers and patients in both human and animal health markets, operates in all 50 states domestically and 35 countries internationally. This provides Avante the ability to flex as market conditions and trends change. Additionally, with a team of 140 service engineers and nearly 40 customer service representatives, Avante is committed to providing a positive customer experience and maintains industryleading levels of customer satisfaction and referral rates.
Q: CAN YOU EXPLAIN YOUR COMPANY’S CORE COMPETENCIES AND UNIQUE SELLING POINTS?
Thomason : Avante Health Solutions is an industryleading provider of diagnostic imaging, medicalsurgical, patient monitoring and ultrasound equipment. In addition to these operating segments, we also provide rental equipment and solutions for animal health providers, international health care facilities and the U.S. federal government. As a comprehensive provider, we partner with our customers from consultation and installation to service, repair and ongoing technical support for the full life cycle of medical equipment.
Q: WHAT PRODUCT OR SERVICE THAT YOUR COMPANY OFFERS ARE YOU MOST EXCITED ABOUT RIGHT NOW?
Thomason : Avante’s proprietary Remote Technology
Solutions! This is an exciting suite of products that provides a real-time, cloud-based deliverable for a brand- and modality-indifferent solution for equipment management and support.
Q: WHAT IS ON THE HORIZON FOR YOUR COMPANY?
Thomason : We continue to explore new modalities and services that will round out our product and service commitment to our partners. As part of our consultative approach, we monitor the market and talk regularly with our customers to guide us to areas of need for both innovation and to fill support deficiencies in the marketplace. Based on that feedback, Avante will continue to evolve through both organic growth and acquisition.
Q: CAN YOU SHARE SOME COMPANY SUCCESS STORIES WITH OUR READERS – A TIME THAT YOU “SAVED THE DAY” FOR A CUSTOMER?
Thomason : From significant cost avoidances such as preventing an MRI quench to next flight out delivery of mission-critical cath and CT parts, our customers are routinely the superhero in patient care as our diagnostic imaging support teams support them in maximizing uptime and diagnostic volumes. However, whether it is the cost-effective repair of patient monitoring equipment or fulfilling guaranteed ultrasound uptime for a mother’s first look at her unborn child, our employees are committed to serve our customers and their respective health care communities as if the equipment serviced was treating or diagnosing a family member.

Q: CAN YOU PLEASE DESCRIBE YOUR FACILITY?
Thomason : Avante owns three strategically located state-of-the-art, ISO 13485 certified centers of


excellence from which our business units operate and warehouse our extensive inventory. In addition to these showcase locations, Avante utilizes a national network of operational warehouses and forward stocking depots to speed delivery of mission critical parts to our customers and maximize uptime performance.

Q: CAN YOU HIGHLIGHT ANY RECENT CHANGES TO YOUR COMPANY, INVENTORY, SERVICES, ETC.?
Thomason: In the past year, we have implemented several key leadership changes aimed at enhancing the strategic operations of our businesses Collectively, these individuals contribute over 100 years of health care industry knowledge.
Q: CAN YOU TELL ME ABOUT YOUR EMPLOYEES?
Thomason: Despite Avante’s size and numbering nearly 470 employees today, we maintain the family-based corporate culture that drew many of us to the legacy organizations years ago. This level of interpersonal commitment to each other and our positive impact on patient care motivates us to provide unparalleled comprehensive service and support for our customers. I am extremely fortunate that our leadership team has afforded me the opportunity to invest in and build a strategic accounts team responsible for all facets of Avante’s business. The strategic accounts team of Doug Katz, Chris Ackerman, Scott Boucher and Aline Ekizian are responsible for bringing unique enterprise solutions from all of Avante to all of our customers.
Q: WHAT IS YOUR COMPANY’S MISSION?
Thomason: Our mission is to support your mission. Avante Health Solutions is committed to moving health care forward by supplying value-based medical equipment solutions to our customers so that they can focus on patient care.


Q: IS THERE ANYTHING ELSE YOU WANT READERS TO KNOW ABOUT YOUR COMPANY?
Thomason: In addition to supporting our customers’ in their mission of patient care, Avante Health Solutions also prioritizes the growth and development of our employees. As a rapidly expanding company, we offer a wide range of career opportunities across various departments such as field service, technician, operations, and sale. We believe in investing in our employees, and provide ongoing training and support to ensure their success. Join us at Avante to advance your career and be a part of a team dedicated to making a positive impact on health care: avantehs.com/careers. •
For more information , visit avantehs.com.
Banner Imaging is accredited with the ACR as is required by CMS for outpatient facilities. This is an ongoing process since we always have a renewal due somewhere or a new piece of equipment being added. Our team has become very proficient at subm itting the application, gathering the required images and documents, and receiving approval.
I have seen questions about what to expect out of an ACR survey on the AHRA Forum. Most responses direct folks to the ACR website and the toolkit that is set up there. Everything necessary is laid out on the site, but sometimes it is nice to have a little bit more detail so I thought I would share our experience.

Recently, four of our centers were selected for a virtual accreditation survey. We felt prepared for this, as we have experienced several in-person surveys prior to the pandemic but decided this would be a great time to refine our information and educate other team members. Our modality managers handle the details of the ACR process, so site managers are not as up to speed on the requirements and the specifics of each modality in their center.
Things have changed a bit since the pandemic and a virtual survey is slightly different. Previously, we had all our site information in an ACR Toolkit physical binder, which we updated every 6
months. We began building an online toolkit in Teams about a year ago that includes all the required information for each of our sites but is all in one place. We were very happy we had already started this when we received notification that we were going to be surveyed, especially since it was at four sites.
The electronic binder is set up just like the physical binder with the tabs suggested on the ACR website. We have tech information split by modality instead of by site, which makes them all easier to manage. The same is true for radiologists and physicists. Our policies are listed in a spreadsheet with links to our policy software.
Being that the surveyor is not physically onsite, we were asked to present a video or PowerPoint presentation of our center. We provided a floor plan of our space to begin the presentation. It is important to include the waiting room and appropriate signage, including the notice to patients regarding the process to submit a complaint to the ACR. The surveyor also needs to see MRI zone signage, in use light for CT and hot lab signage. We presented pictures of our emergency kit and the daily log.
Our surveyor did a review of the physical space; policy and procedure review; personnel, physician and physicist credentials and continuing education; physicist reports; peer review, and daily QC logs. We then went through image verification for each modality. The
surveyor viewed PACS images to verify that specific information was included either on the screen or in the DICOM header.
We had the same surveyor for all our visits, but all were scheduled separately. She was very patient and easy to work with. She even allowed team members from all four sites to be included on the first survey so they could be prepared when it was their turn. This helped us immensely for the proceeding surveys since everyone knew what to expect. We also had the same point person navigate the toolkit for each of the surveys that had helped to build it. This allowed us to move from one section to the next quickly and efficiently.
If I was to give any advice, I would say be prepared by following the toolkit. Go into the survey seeking to understand areas that can be improved. Be friendly with your surveyor since this is a joint effort. Do whatever possible to make their job easier by knowing and understanding your information. Prepare ahead of time and have an internal mock survey to find anything that may have been missed before the real deal.
We did learn that we had not been good about updating contact information when we had a site manager change. The ACR uses this information to contact the site to set up the survey. We also will be updating personnel and physician information more frequently.

All in all, the experience was interesting and painless. I was so happy that we had prepared as a team, and I was proud of our performance. We will keep our toolkit up to date and should be ready for the next one. •

























































































































































































































































Only two things are certain, death and taxes. This article is written with a heavy heart. My brother called me to let me know my 42-year-old niece was told she may not make it through the weekend. I jumped on a plane and flew to their home. She was diagnosed with breast cancer at age 30, treatment and surgery and a cancer-free declaration. Chemo had leached her bone material. She suffered multiple spine fractures causing pain that required stabilization rods to be placed in her back.

Her six-month follow up checkup scans went from nothing noted to Stage 4 cancer in six months.
In 2016 researchers at Stanford University were able to train an AI system to accurately predict if a person would die in 3 to 12 months. This remarkable application is representative of the wide variety of roles that AI and deep learning will play in the upcoming years.
Palliative care usually involves providing relief for a patient’s pain, stress and other symptoms when the patient has a terminal diagnosis and no cure is expected. Knowing when such specific care is warranted may have beneficial effects for the patient, family and caregivers – and help determine when such care would be most effective. To create the Death Algorithm, the Stanford team used information from about 170,000 patients who had died from cancer, heart and neurological diseases. Various information from medical records – including a patient’s diagnosis, medical procedure, imaging scans codes and drugs prescribed were used to teach the AI system. Then, a deep neural net was trained, with various internal weights adjust -
ed for the neuron units. The deep neural net made use of input layers of 13,654 dimensions (codes for diagnoses and drugs).
In the end, 9 out of 10 people predicted to die within 3 to 12 months did die within this timeframe. Also, 95 percent of those whom the algorithm determined would outlast 12 months did live longer lives.
When I arrived at my brother’s home, I was greeted by a somber houseful. I chatted with my niece who was alert and able to ambulate. I reviewed her brain MRI results that documented 12 separate cancerous masses. She said her doctor had arranged hospice care. We spoke about how the use of hospice had changed over time and that this designation was just as much about “living well with cancer” in a pain free manner, with access to resources like home care.
She looked at me and said, “So, I could go to the beach?”
Lack of medical knowledge and modern health care practices can rob patients of the opportunity to bucket list a couple of memories. I know that I would want to know if I was living my last 12 months.
I can tell you that we enjoyed a flight of six flavors of Tillamook ice cream and more than one Ruby Red microbrew beer at the beach the next day. Life is short, hug the ones you love. •
 BY MELODY W. MULAIK
BY MELODY W. MULAIK
Positron emission tomography (PET) is a nuclear medicine study that creates cross-sectional tomographic (3D) images of the metabolic activity in the patient’s tissues. Cancers can cause abnormalities of blood flow or metabolism before structural changes are visible, and for this reason PET can often detect cancer at an earlier stage than CT or MRI. Even though there have not been many coding changes for PET scans imaging studies over the last few years, there have been new radiopharmaceuticals that have been granted approval and assigned Healthcare Procedure Coding System (HCPCS) codes. This expansion of radiopharmaceuticals may offer an opportunity to expand your services and subsequently your revenue.
As a reminder, Medicare’s National Coverage Determination (NCD 220.6.17 ¹) classifies oncologic scans as either initial treatment strategy or subsequent treatment strategy. A scan falls into the initial treatment strategy category when it is performed to determine the physician’s initial treatment strategy for a patient who has a cancer that is “biopsy proven or strongly suspected based on other diagnostic testing.” Scans performed for diagnosis and staging of cancer are considered initial treatment strategy scans. (“Staging” refers to the diagnostic work-up the physician performs to determine the extent of the patient’s cancer). Initial treatment strategy does not include scans performed for screening, which is the preventive evaluation of a patient without
signs or symptoms of disease. Medicare and other payers do not cover PET for screening.
According to the NCD, the patient’s physician must order the initial treatment strategy study for one of the following purposes: To determine whether the patient is a candidate for an invasive diagnostic or therapeutic procedure; To determine the optimal anatomic location for an invasive procedure; or To determine the anatomic extent of the tumor when the recommended anti-tumor treatment reasonably depends on the extent of the tumor.
The NCD allows for coverage of only one initial treatment strategy scan per cancer per patient. For example, if a patient has an initial treatment strategy scan for lung cancer, and several years later the patient is found to have colon cancer, an initial treatment strategy scan can be billed for the colon cancer. CMS Decision Memo CAG-00181R4 ² states watchful waiting is not considered an initial treatment regimen. This means a scan performed after a period of watchful waiting would be considered an initial treatment strategy scan rather than a subsequent treatment strategy scan. The Medicare NCD defines subsequent treatment strategy scans as those that are performed to guide subsequent management of anti-tumor treatment strategy after completion of initial anticancer therapy. Clinicians often refer to this as “restaging,” which is a re-evaluation of the cancer stage following completion of a course of treatment. Medicare does not cover studies performed for surveillance purposes in a patient with previously treated cancer who has no clinical evidence to suggest active disease. These studies are considered to be screening rather than subsequent treatment strategy scans.
The NCD allows for coverage of no more than 3 subsequent treatment strategy scans. In addition to the 3 subsequent treatment strategy scans covered under the NCD, Medicare Administrative Contractors (MACs) and Medicare Advantage plans have the authority to cover additional scans if desired.
The table below reflects the most frequently utilized HCPCS Level II codes for PET tracers. Several PET radiopharmaceuticals (A9591, A9595, A9596, A9602, and A9800) have pass-through status under the Outpatient Prospective Payment System. The facility specific HCPCS codes (e.g., A9593 – UCSF) are not included in the list.

C-11 choline is used to evaluate patients with biochemical recurrence of prostate cancer. This agent has a half-life of only 20 minutes, which means it must be produced at the same location where it is used rather than being transported from an off-site supplier. Medicare coverage of scans performed using choline C-11 is at the discretion of the individual MAC.
Gallium-68 dotatate (NETSPOT) is an oncologic radiopharmaceutical that received FDA approval in June 2016. It is used for evaluation of somatostatin receptor-positive neuroendocrine tumors. Fluciclovine F-18 (Axumin) is an oncologic radiopharmaceutical that received FDA approval in May 2016. It is used for patients with recurrent prostate cancer. Fluoroestradiol F18 (Cerianna) diagnostic agent used
for the detection of estrogen receptor (ER) positive lesions as an adjunct to biopsy in patients with recurrent or metastatic breast cancer. Copper CU 64 dotatate (Detectnet) is an oncologic radiopharmaceutical that received FDA approval in September 2020. It is used for the localization of somatostatin receptor positive neuroendocrine tumors (NETs) in adult patients.
PET scans are an excellent imaging tool to identify and stage most types of cancers and there is no indication this technology will be replaced with something new anytime soon. Continuing to look at your current offering and how it may be expanded could benefit your organization and the patients in your community. •
1. https://www.cms.gov/Regulations-and-Guidance/Guidance/Manuals/downloads/ ncd103c1_Part4.pdf
2. https://www.cms.gov/ medicare-coverage-database/ details/nca-decision-memo. aspx?NCAId=263
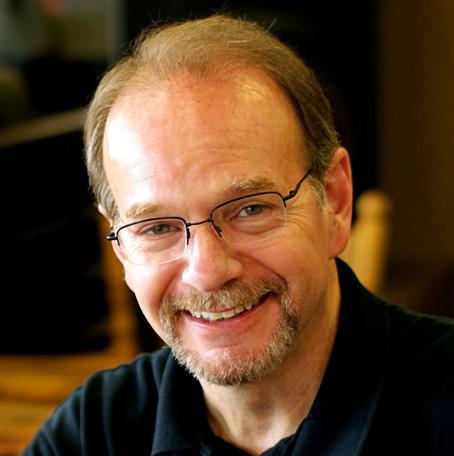
Beliefs and attitudes about the workplace have definitely changed over the years, and the people of today’s workforce look at labor and lifestyles much differently than the workforce of 30 years ago.
This became the topic of conversation during a recent phone call with an old colleague. This gentleman recently became a senior manager at a large company (you would know the company if I named it), and he told me that two of his main concerns are attracting good employees who are just entering the workforce and keeping the good ones he already has.
“The workplace has changed since you and I first started out,” he told me. “There’s a different work ethic these days.” I agreed. And, I thought if he wanted to create methods by which he could both attract and keep good employees, it was probably best if we started by identifying what contributed to an employee’s sense of engagement.
After some discussion, we settled on three main components.
• Employee commitment to the organization’s vision and mission
• Employee motivation and enthusiasm – one’s personal reasons for engaging with a unique job description
• Employee esprit de corps – the sense of camaraderie and unity that exists on a team
First up was having employees be committed to a vision and mission statement. It should go without saying, but if your organization doesn’t have those, then creating them will be a necessary first step. I’ve written in this space before about vision and mission statements, so if those are lacking where you work, let me encourage you to visit https://theicecommunity.com/ and search for vision and mission to get my take on those.
But assuming you already have them, a fundamental action for getting people committed to those statements is to talk about them regularly. That means you yourself need to know
them. It’s sad, but if I walk into any company and ask five people to tell me their organization’s vision and mission statements, I’m likely to get a blank look, a laugh, an “I don’t know,” or five completely different answers.
Bottom line here, if employee engagement is the goal, then employees need to know what they’re engaging. We should regularly talk about our company’s vision and mission to employees and help them understand how their work contributes to achieving those goals.
Next up is strengthening your employee’s motivation and enthusiasm. You’ve probably heard me say it before, but what slows people down is not a lack of motivation, but the presence of obstacles. That’s because the word “motivation” means “a reason to move,” and everyone already has a reason to move. What slows people down are obstacles. If we get rid of a person’s obstacles, each person’s own reason(s) to move will propel them forward.
The key here is to help each individual see how their personal reasons to move will result in fulfillment and the sense of a job well done when it comes to accomplishing the tasks required for a specific job. Know that telepathy doesn’t work here. Because we can’t read people’s minds, we need to interact with individual employees to learn more of who they are and what makes them tick.
One way to do this is to converse with people about their interests, attitudes and values. What do they like? Why? What interests them? What are their dreams and goals? It’s been said that people don’t care how much you know until they know how much you care. If you show genuine interest in people, they will know you care.
Notice the word “genuine.” This is one of the traits of a good manager. People are the focus here, not machines or systems, so if we want the people on our teams to engage, we first need to get to know the people working on our teams.
Then, as you get to know your team members, take some
one-on-one time to privately review each person’s job description with that person. Again, if you don’t have job descriptions, then creating those will be a prerequisite to this, but once you know what drives a person, find ways to connect their natural motivators to the requirements of the job.
You can even go beyond a person’s current job and show how their interests, attitudes and values connect to future opportunities within the company. Look for ways to connect company values with an individual’s values. I’m not saying invent things. Definitely be intellectually honest. It’s just that often times people aren’t shown how their personal values correlate to a company’s values. Identifying the similarities goes a long way to engaging and retaining good people.

You might be saying, “Wait, this takes a lot of time.” Absolutely it does. You won’t see it in many managerial job descriptions, but it’s part of a manager’s duty to learn the strengths, weaknesses and motivations of each person on a team. It’s still work. It’s just a different kind of work from what we think of as work.
Lastly, let’s touch on building a sense of camaraderie and unity on a team. Much could be addressed here, but two actions that stand out as essential are ensuring everyone understands the purpose of the team and also encouraging open communication among team members.
With regard to purpose, it’s easy to say, “Didn’t I cover that when I ensured each person understood the vision and mission and when I connected their natural motivations to their job descriptions?” The answer is both “yes,” and “no.” Those are individual efforts. Building esprit de corps means helping everyone on the team realize that everyone else on the team is also intimately aware of the team’s purpose and goals. It’s like designing an open book. It’s creating an open and ongoing dialog among team members.
Building esprit de corps also involves creating, projecting, encouraging and rewarding a can-do attitude. On teams where people are free to encourage and free to offer and receive feedback, esprit de corps is more easily established.
Like I told my friend, work on these things and you are more likely to attract and retain quality employees, no matter what their generation. •
Daniel Bobinski, who has a doctorate in theology, is a best-selling author and a popular speaker at conferences and retreats. For more than 30 years he’s been working with teams and individuals (1:1 coaching) to help them achieve excellence.




We live in a community with a homeowners association (HOA). We are mostly pleased with the way it is run. Property values are maintained by ensuring that everyone complies with the regulations we all agreed to upon purchasing the homes. We are personal friends with two of the board members so we hear probably more than we should about what is happening. One of these board members actually asks me for advice regarding handling people issues and sometimes takes my advice.
So, why am I boring you with this and what does that have to do with the title of this writing? Well, I have been involved in multiple discussions at meetings as well as more private conversations regarding the “violation” process. When someone is found to be in violation of a regulation, the management company sends a violation notice to the perpetrator. The recipient then is provided time to effect a correction and document the resolution. My objection is to the manner in which the violation is presented to the homeowner.
I contend that the present letter is somewhat insulting and implies that the violation was intentional. My first letter arrived before I even took possession of our home: You are in violation due to overgrown weeds in the front yard. The previous owner had vacated a few weeks prior to our move. We were very surprised at the tone of the letter – the presentation. I have been in multiple discussions regarding this presentation with multiple board members and homeowners. I propose that they change the presentation to change the perception.
I’m getting to the point, OK? When I conducted imaging service training to in-house biomed service personnel, I would highlight that their customers normally only saw them when something was wrong or broken. Their presence was attached to broken. I told them they should sometimes show up when nothing was broken to break this perception of broken-you, you-broken.
The saying that “Perception is Reality” is true, however, what determines perception? If we leave perception totally to the perceiver, what influence are we exerting? If what we see

determines where we sit, then let’s provide the chair so we can influence the perception. If we do a good job with the presentation, then we are providing the chair pointed in the direction we want.
Let’s use the violation letter from the management. If the only correspondence with the homeowners is the dreaded letter, how are we to perceive it when we see the envelope?
I’m telling you from experience that the first response is alway emotional, to anything. When we see the address, we immediately think, “Crap, what did we do, or not do now?” Letter means broken-me, me broken-means letter.
In my discussions with my friends on the board, the response is, “A violation is a violation, period. It should not be sugar-coated.” The word has such negative connotation. Look up the word in a thesaurus and the implication is that there was intent to violate.
I suggest that the letter be a critique sandwich. The negative “violation” should be sandwiched between positive items. For example, begin with the great and well-maintained community that we live in, then inform of the “discrepancy” found, then provide a reason to maintain the beauty and value of the community. Or some other sandwich which is less aggressive, that is until they refuse to correct the discrepancy, then get aggressive.
How is one to view an unveiled threat of fines and liens if not in a negative way. A good presentation may provide an alternate, less menacing perception and improve the perception of the HOA. I also suggested a monthly newsletter from the board in order to preclude the broken-me situation.
So, my advice to those of you who made it this far, is to evaluate how you present even good stuff. Prepare to answer 10 questions that your presentation may generate to ensure that you provide the chair you wish to provide. Presentation is 100% … Still.
By the way, my board member friends are unconvinced, so my presentation has been awful. My lovely Ruth says, “Stay out of it unless you are willing to run for the board.” My response is: I will run, but it will be away from the board. •

















As AHRA president, I have had the honor of watching our board of directors develop and implement a strategic plan that is both aspirational and achievable, to best meet the needs of the AHRA members. Keeping the AHRA members’ needs at the forefront of our minds has given us great focus on who we want to become, and how to best get there.
The AHRA Educational Foundation kicked off its “$50 for 50” campaign in celebration of AHRA’s 50th anniversary this year. So far, we have already raised close to $10,000 donated by just 13 members of the AHRA and Education Foundation Boards. Now how’s that for committed board members? Last year, the AHRA Educational Foundation was able to provide over 30 scholarships valued at over $65,000 to our members because of the tax-deductible contributions from our AHRA family. Please keep in mind that donations are tax deductible and support a variety of scholarship opportunities. Please consider giving at ahra.org/give50, as your gift will be put to great use!
Nancy Green, CAE, FASAE, interim CEO, has been a great addition to the AHRA team. She has brought a wealth of knowledge and experience from

the association world. She has been a breath of fresh air, challenging us to think bigger and beyond our comfort zone.
The AHRA 2023 Annual Meeting, where we’ll be celebrating our 50th year as an association, will be held July 9-12, 2023 in Indianapolis, Indiana. For me, the AHRA Annual Meeting is my “Super Bowl,” as I cannot wait to see the entire AHRA team together. I always walk away from the annual meeting with a renewed sense of purpose, a notebook full of notes and a boost of energy. I also always walk away with new AHRA friends and family. Indy offers great food and fun. There are multiple museums, beautiful architecture and lots of shopping opportunities nearby. You don’t want to miss this celebration! We have plans to honor our founders and past presidents, show appreciation to our current members focus on our bright future.
If you have any questions or suggestions, please reach out to me! You can email me at Brenda.DeBastiani@braverahealth.com. •

The AHRA 2023 Annual Meeting and Exposition is set to take place in Indianapolis, Indiana, from July 9-12, and promises to be a very special event, according to AHRA: The Association for Medical Imaging Management.




The gathering will bring together founders, past presidents, current and next-generation imaging leaders to celebrate the 50-year anniversary of AHRA. The premier event for imaging leaders at all levels, the conference affords broad networking opportunities, insights into health care trends and challenges, and dynamic educational sessions in two distinct conference tracks for aspiring and established leaders.
Set in the currently popular theme of a Hollywood “origin story”, the event will showcase AHRA’s historic beginnings, while also very much looking toward the future. There will be exciting discussions around debuting AHRA’s mentoring program, the expanded and more accessible 2023-2024 Leaders of Choice Program, and an exhibit hall showcasing cutting edge vendors in a close-up, hands-on setting. The AHRA Annual Meeting is the best way for imaging leaders to set themselves, and their organizations, up for success.
Additional half-day workshops are offered, including the Certified Radiology Administrator (CRA) Exam Workshop, designed to assist those pursuing the esteemed CRA designation.
“This event will be about creating new memories with all members of the AHRA community, as we celebrate 50 years of success and growth in medical imaging management,” said AHRA President Brenda DeBastiani, CRA, FAHRA. “I invite imaging and health care leaders to come and experience this
exceptional chance to learn and make meaningful, lasting connections with authentic, committed thought leaders. Join us in creating change and success that impacts the next 50 years in health care.”

AHRA 2023 will enable attendees to network with peers from across the nation and gain insight into health care services, tools and trends that will impact patients. Over the course of four days, they will have the opportunity to participate in educational breakout sessions and workshops. The training offered will enable attendees to hear from dynamic speakers in the medical imaging community and earn CE credits. Additionally, attendees can meet directly with vendors and identify ways to help their health care facility improve operational efficiency.
The education offered includes several areas of emphasis including tracts for established leaders and aspiring leaders. Workshops will be available focused on executive leadership, the CRA exam, inclusive excellence and disagreeable employees. •
For more information, scan the QR code.


Be sure to visit these exhibitors!
Advanced Health Education Center aheconline.com

Booth #829
Avante Health Solutions avantehs.com
Booth #328
Block Imaging blockimaging.com

Booth #320
Fresenius Kabi fresenius-kabi.com
Booth #114
ICE Magazine theicecommunity.com / attendice.com
Booth #1133
Injector Support and Service weareiss.com

Booth #931
KA Imaging kaimaging.com

Booth #329
KMG Medical Imaging kingsmedical.com

Booth #1228
Landauer & RaySafe landauer.com / raysafe.com

Booth #921
Medical Imaging Solutions wearemis.com


Booth #929
MXR Imaging-Booth mxrimaging.com
Booth #210
Probo Medical probomedical.com
Booth #1206

Radon Medical Imaging radonmedicalimaging.com






Booth #1021
Rapid Radiology, Inc. rapidrad.com






Booth #928
Richardson Healthcare rellhealthcare.com
Booth #832
RTI Group North America rtigroup.com


Booth #728
Sky Factory skyfactory.com
Booth #529 Sodexo
us.sodexo.com/industry/healthcare.html

Booth #1200
Summit Imaging mysummitimaging.com

Booth #831
Technical Prospects technicalprospects.com










Booth #730

Register to view live webinars each month.


Watch recorded webinars on-demand.

ARRT Category A
CE credit is pending approval by the AHRA.


DOs:
Do carry a coil with 2 hands
Do store coils in a position where they are fully supported by a solid surface

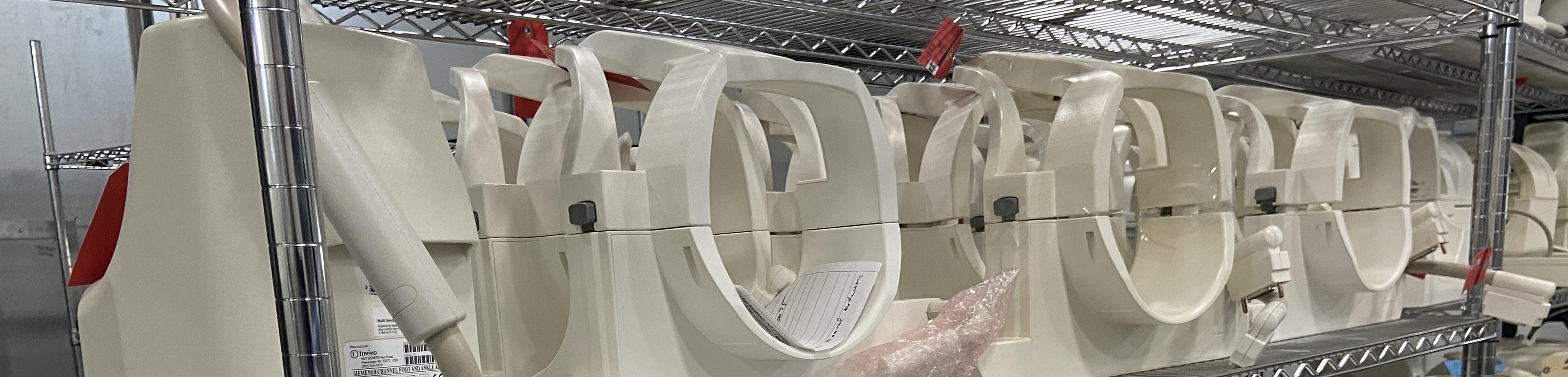
DON’Ts:
Do not carry, lift, or position a coil by using the cable or connector
Do not carry by the anterior bridge trusting the latching mechanism to hold the posterior section
Do not clean out a coil connector with common household cleaners
Do not store coils by standing them against a wall or hanging on stands support rails, or hooks
Our team of experts is here to help with your coils! We specialize in Siemens 1.5T and 3T coils and Tim style coils with an average turnaround time of 5 to 7 business days!
Capabilities include, but are not limited to:
• Complete diagnostics and repair of coils to the original manufacturer’s specifications
• Full electrical and mechanical rebuilds to improve and enhance performance
• Cosmetic refurbishment to a “like brand new” appearance
• Aesthetic touch-ups to the rigid or foam housings so that the coil is safe to use

• Abilities to repair not only the coil, but also the socket groups on the table side connector
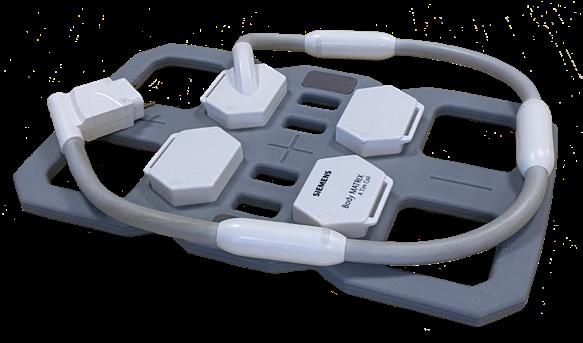
• Provide 3D printed coil connectors or Balun cover replacements on Siemens coils

Additional offerings include:
• Use of an onsite MRI Scanner for QA/ SNR testing for 1.5T Siemens Tim
• Loaner program or exchange program
We have an extensive coil inventory covering most Siemens Avanto, Espree, Trio, and Symphony type coils. Our inventory contains the most popular models, Siemens Avanto Head, Body, Neck and Spine coils!
877.604.6583 / 920.757.6583
sales@technicalprospects.com
technicalprospects.com
FEBRUARY 18-20, 2024


“I think it has been very well put together and very informative. I highly recommend it to anyone in the imaging field.”

You are invited to submit a proposal to share your experience and expertise with colleagues at ICE 2024 in Irvine, CA.



To submit a proposal, visit attendice.com/call-for-presenters.
DEADLINE: JUNE 30, 2023

– B. Wilson, TRIMEDX
IT ALL STARTS ONLINE
ICEWEBINARS .LIVE
1 2 3
REGISTER
Register to view live webinars each month.
WATCH Watch recorded webinars on-demand.



EARN
ARRT Category A CE credit is pending approval by the AHRA.







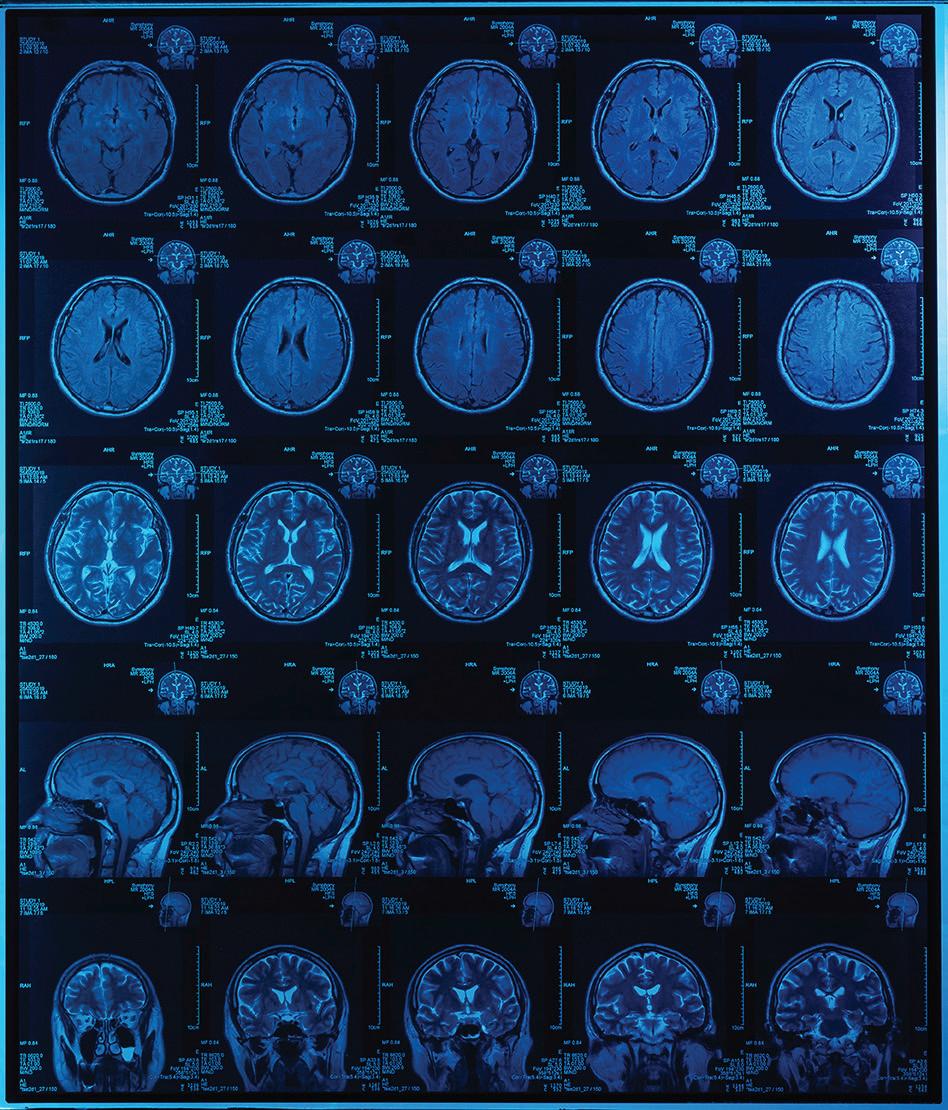
Down

1 Small jaw joint in front of the ear, abbr.
2 Damage physically
3 Linear accelerator, abbr.
4 C-____: x-ray image intensifier
5 Way in which something is done
6 _____ imaging: the combining of multiple hospitals or radiology departments into a single imaging system
7 Unwanted material on imaging equipment that can be removed using a wash liquid
10 Word describing location
11 Not often seen

12 Contrast material
13 Artery that supplies blood to the brain
15 French for “south”
17 It’s measured during cardiac computed tomography
19 Abnormality in which part of an organ is displaced and protrudes through the wall containing it
23 Cleaning bar
25 Template for protein synthesis
28 Take care of a bill
29 Acidity factor
626 Holdings
p. 5
Advanced Health Education Center

p. 64
AHRA
p. 67
AllParts Medical



p. 64
Avante Health Solutions
p. 38-41
Banner Imaging

p. 19
Brandywine Imaging
p. 43
Chronos Imaging, LLC


p. 25
CM Parts Plus

p. 49
Engineering Services
p. 3
HTTM
p. 44
HTMJobs.com
p. 32
ICE Webinars

p. 58, 62
Imaging Academy
p. 2

Innovatus Imaging

p. 9
KEI Medical Imaging


p. 52
KMG
p. 57
Maull Biomedical

p. 50
Metropolis International

p. 50
PM Imaging Management


p. 44
Radon Medical, LLC
p. 23
Ray-Pac®
Ray-Pac
p. 68
RSTI
p. 26
RTI Group North America
p. 21 Technical Prospects
p. 4, 59
SOLUTIONS
TriImaging Solutions
p. 13
W7 Global, LLC.
p. 52

AHRA's origin story began 50 years ago. Join your imaging peers this summer at the AHRA 2023 Annual Meeting and Exposition-- the pinnacle of our year-long celebration of the great strides made by AHRA and the medical imaging community over these past five decades.



The stage is set for a special look at AHRA's history, as well as today's challenges and successes, and a glimpse to what the future of imaging may hold.
Do not miss this memorable imaging event. After all, you're helping shape the next 50 years of healthcare!




