
THE TOTAL PACKAGE HAS ARRIVED.







Enhance your engineer’s skills and embark on a journey of technical expertise with our comprehensive training program on the Siemens Somatom Go CT.
DirectMed Imaging’s Somatom Go course is a 10 Day, 60-hour integrated training course. Week 1 is virtual using our Interactive Virtual Training Academy (IVTA), Week 2 is in person at our state-of-the-art training facility in Appleton, WI. Students will engage in discussion, lectures, and labs center on the core principles of operation, configuration, troubleshooting, and repair for all primary system components.
Our Somatom Go course expands upon the knowledge gain in DirectMed Imaging’s CT Fundamental and Syngo Native courses, unlocking the full potential of your service organization through our dedicated training program.
Your engineer also will learn both the OEM and ISO perspective and will acquire essential skills in performing preventative maintenance, optimizing system performance and ensuring the longevity of your equipment while earning valuable ACI Continuing Education Units (CEUs).
Our courses are taught by expert instructors with real-world insight leveraging over 165 years of imaging experience and are ready to teach your engineers the intricacies of the Somatom Go CT Platfrom. Our smaller class size assures a more effective hands-on learning environment for your engineer.
Contact our sales team today for dates and to reserve your seat for our upcoming course.
All courses are AAMI Certified and provide continuing education units.
Our AAMI certified instructors bring a wealth of knowledge and field experience to guide your engineer to excellence.



39
It is important to tell a story when we communicate to our teams. If we can weave important information into a story, we will have more impactful communication.
COVER STORY
Growing concerns regarding carbon emissions driven by human activity continue to contribute to global health challenges posed by climate change, the field of health care is taking steps to address its role.

14

Brandy Easa was nominated as a Rising Star by University Hospitals Radiology Director Michelle Dossa.


Catch up on the latest news from around the diagnostic imaging world.
ICE highlights products available to help imaging leaders reach asset management goals.

A coach or a mentor provides huge benefits and are highly recommended.





Martha Henderson is the manager of radiology services with Mercy Ships. She has a CT tech background. She holds several certifications and degrees, including MSc, BSc Diagnostic Radiography, PG Cert in CT (British). She works on MV Global Mercy (NGO Hospital Ship).
Her imaging journey started in Scotland.
“Growing up in the Highlands of Scotland, living and working in small communities has always been part of me. A friend’s mother was a radiographer, and she would show us different X-rays and the fractures identified,” Henderson recalls about her youth. “I was curious and fascinated that it was possible to learn more about the human body in this way. I graduated in 2008 and
have worked in remote and rural hospitals in Scotland. This prepared me for working with Mercy Ships as it taught me adaptability and provided a varied foundation of clinical experiences and pathology.”
She says her greatest accomplishment was taking a leap of faith.
“Taking the first step into international work in 2012. I always knew my path would take me into the humanitarian setting, however as a CT technologist I was not exactly sure how that would unfold,” Henderson said. “Often, surgical and medical missions rely on nurses and doctors. Finding Mercy Ships – and knowing they had a full radiology department onboard their ship – I found my calling. The organization now has two hospital ships and I feel incredibly honored to have set up the radiology equipment and services onboard.”
“Earlier this year, I completed my master’s in applied global health with a focus on global radiology service delivery. I feel incredibly grateful that my experiences allow me to raise the radiology profile amongst the conversation of global surgery,” she added.
Work does not feel like a job for Henderson because she loves what she does.
“Daily, I get to interact with patients from West Africa and learn about their culture and family. Volunteering on a hospital ship, you get to work alongside colleagues from around the world, to learn from their training and experiences really grows you as a professional,” she said. “Also knowing that radiology is a profession that can take you around the world and provide the opportunity for you to use your skills in many different countries and locations.”
“As the manager, I am responsible for ensuring we have highly trained CT techs who volunteer onboard, who provide CT and X-ray examinations for the patients who come onboard. This role also allows me to interact with many different radiology vendors and those collaborations are extremely rewarding,” she added.
Henderson explained that her approach to leadership is centered on helping others.
“I have learned in a humanitarian setting, that delivering health care is a complex, multifaceted system, working with colleagues who view the world from a different perspective. There are often layers we do not see, and its important to understand that communication can be difficult,” she said. “Setting a vision for where you see a service going is important, however that must be balanced with involving your team and making space for them to own the project they are working on, and to develop areas where they see improvement.”
Her leadership style was formed with influence from those who came before her.
“Some of the humblest leaders I have worked with demonstrate a willingness to empower their colleagues. To trust their judgment and experience, yet to remain open to provide advice or suggestions when needed,” Henderson said. “I feel the most effective mentors, allow you to provide your own solution to a problem that has arisen, rather than being the one who always has the answer.” •
1. What is the last book you read? Or, what book are you reading currently? I always go back and enjoying reading “To Kill A Mockingbird.” I find it incredibly powerful with its themes of injustice and empathy for others.
2. Favorite movie? “Salmon fishing in the Yemen” While a bit unique in storyline, the landscape filming is beautiful to watch. It is inspiring to see what can be possible, yet one must consider the cultural and political setting in which this occurs. Yet, it is a heartwarming film.
3. What is one thing you do every morning to start your day? But first coffee. Then, I usually read the to-do list from the day before and number the items in importance to help guide my day.
4. Best advice you ever received? “When you are being asked to do something that has never been done before, you can’t look around at others. Have the confidence to go forward and trust your own experience and calling.”
5. Who has had the biggest influence on your life?
Dr. Gary Parker is the head of our maxillofacial surgical program. He has dedicated 36 years (and counting) to providing free surgeries to patients with disfiguring benign facial tumors. Through his skill and dedication, patient lives are transformed. It is a privilege to support him and his surgical team.
6. What would your superpower be? Working internationally, involves a lot of travel. While I do enjoy sailing with our ship to a new country, I would love the ability to teleport. To arrive where I need to be without spending hours in airports.
7. What is your perfect meal? When I am home in Scotland, fresh seafood from the local fish shop is always a delight.

With spring cleaning in full swing, out with the old and in with the good. It’s the perfect chance to shake things up with the team.
Let’s tackle any lingering issues, especially within the team, head-on and ditch them for good!
Consider making a conscious effort to set some “new” ground rules together with your team, for example, no condoning tardiness, or engaging in gossip, ranting and raving with negativity, really anything you want to ditch in the past!
Make it official. Declare a “Clean Slate Day” at your next team meeting and cultivate a better work environment through this reset. What do you think? Ready for a fresh start for all? Here are some ideas to get you started.
Encourage open and honest communication. Implement a rule where issues are addressed directly with the person involved rather than discussing them behind their back.
Introduce a rule where team members commit to avoiding negative talk about colleagues, projects or the organization. Encourage constructive criticism and solution-oriented discussions instead.
Implement a weekly or monthly gratitude session where
team members express appreciation for each other’s efforts. This can help shift the negative focus as well as the underappreciated feelings.
Introduce a solution-oriented approach. Shift the focus from dwelling on problems to finding solutions. Encourage team members to come with proposed solutions when presenting challenges during discussions rather than complaining about the situation.
Launch awareness campaigns to reinforce the organization’s commitment to a bully-free workplace. This can include posters, newsletters, and workshops to remind employees of the importance of respectful behavior.
By advocating for a collective commitment to new ground rules, this Rad Idea encourages teams to confront lingering issues directly, paving the way for a fresh start.
The establishment of clear communication guidelines, a no-negative talk policy, gratitude practices, and a solution-oriented approach are integral components of this transformative initiative. These measures not only address specific behaviors that can undermine teamwork but also actively promote constructive and positive interactions within the team •
Share your RAD IDEA via an email to editor@mdpublishing.com.
Medilab Global Corporation was established in Miami, Florida, in 1995. Medilab Global served customers by selling and buying used medical imaging equipment globally. Clients included hospitals, distributors, imaging centers and private medical practices. Medilab Global specializes in selling used and refurbished medical imaging, surgical, laboratory equipment, and parts. The company also repairs and maintains any of the equipment it sells.
Medilab Global Director of Marketing Melissa Henao-Acosta recently told ICE Magazine more about this growing company.
Q: CAN YOU TELL US A LITTLE ABOUT YOUR COMPANY?
A: We’re a medical imaging equipment company that provides high quality pre-owned imaging equipment, parts and service to the health care industry worldwide. Carrying a variety of imaging such as CT scanners, MRI, C arms, mammo units, bone densitometers, X-rays and more. We have established one of the largest networks of dealers and certified engineers for every modality. We have also developed key business partners to provide complete solutions to our customers, by providing products and services that span the project life cycle. Our number one position is to deliver excellent customer service to our vendors and customers with exceptional communication and support.

Q: HOW DOES YOUR COMPANY STAND OUT IN THE IMAGING SPACE?
A: As a family-owned business, we know the impact medical equipment has on the life of the patient. We have seen over the years how medical products have been part of the recovery of our own family, neighbors, friends and buyers. We know that quality, honesty, medical knowledge and good customer service makes the difference to our buyers and consequently to the patient. Our goal is to reflect our values, knowledge, professionalism, excellence and customer service towards everything we sell and do.
Q: WHAT IS ON THE HORIZON FOR YOUR COMPANY?
A: Our aspiration is to attain a global reach, signifying the expansion of our presence internationally to offer essential medical imaging equipment and services to the health care industry and to also foster the growth of our brand.
Q: IS THERE ANYTHING ELSE YOU WOULD LIKE ICE MAGAZINE READERS TO KNOW?
A: We would like everyone to know that we are always here to help you find any pre-owned medical imaging equipment. We are in Miami, Florida, and ship worldwide. We really value making our customers happy with our products and technical services. Whatever it is you are looking for, don’t ever hesitate to reach out to us. •
For more information, www.medilabglobal.com.

Brandy Easa is a rising star at University Hospitals.
Brandy Easa, MSN, RN, CRN, is the a ssistant n urse m anager of r adiology at University Hospitals St. John Medical Center. She was nominated as a Rising Star by Michelle Dossa, Ph.D., CRA, RT, radiology director at University Hospitals.
“We’d like to also submit for consideration our Radiology Assistant Nurse Manager Brandy Easa for your Rising Star column. Brandy supports our Radiology RN team as well as our intervention rad techs,” Dossa wrote.
ICE Magazine found out more about Easa in a recent interview.
Q: WHERE DID YOU GROW UP?
A: I grew up in Brook Park and Strongsville, Ohio
Q: WHERE DID YOU RECEIVE YOUR IMAGING TRAINING/EDUCATION?
A: I received my Diploma of Nursing from Fairview Hospital School of Nursing, and then my BSN and MSN through Cleveland State University. I also have my CRN – Certified Radiology Nurse.
Q: HOW DID YOU FIRST DECIDE TO START WORKING IN IMAGING?
A: I fell into IR. I had worked in many fields, and my last cath lab job required a cross-training to IR. When a full-time position opened up there I went and I never left. It is remarkable how much is done in IR and how little nurses are educated about this dynamic field in school.
Q: WHAT IS THE MOST REWARDING ASPECT OF YOUR JOB?
A: I never thought I would like being in management before I actually experienced it! I love watching things grow, be it people, places or ideas. Being part of growth is the best and most rewarding thing I do.
Q: WHAT DO YOU LIKE MOST ABOUT YOUR POSITION?
A: I would say seeing and being part of that growth and change. I love planning and developing workflows, bringing order out of disorder.
Q: WHAT INTERESTS YOU THE MOST ABOUT THE IMAGING FIELD?
A: I think it is remarkable to consider the continuum of care a patient receives in radiology. We see them in screening exams, diagnostic imaging, IR interventions, subsequent exams, and hopefully a successful resolution. The nursing aspect of this is where we can see that continuum best since radiology nurses touch every modality. Seeing our patients in the various areas and stages provides the patients with a familiar face during very personal and difficult struggles. Nursing is very different in radiology, but it allows for better relationships with patients where our skills and knowledge are at the forefront of what is cutting edge care.
Q: WHAT HAS BEEN YOUR GREATEST ACCOMPLISHMENT IN YOUR FIELD THUS FAR?
A: The IR department I originally came to was a very small venture. I have been able to watch it grow and become a hub of care for our region. We have brought on many new service lines and can provide state-of-the-art, outstanding patient care in a community setting. It has been very rewarding to see how far we have come and exciting to contemplate our future.
Q: WHAT GOALS DO YOU HAVE FOR YOURSELF IN THE NEXT 5 YEARS?
A: I would like to see us expand into markets where there appear to be IR “deserts” so that patients in these areas have access to high-level IR procedures. I would like to inspire my team to achieve certification so they can excel professionally. For my professional growth, I would like to try my hand at writing and presenting. •
FAVORITE HOBBY:
Making food. Any food, all food.
FAVORITE SHOW: Hard to say, but I am currently watching “The Bear” on Hulu.
FAVORITE FOOD: Things made with homemade dough – Danish, pastry, good bread.
FAVORITE VACATION SPOT: So far I am in love with Italy, but I want to travel more!
1 THING ON YOUR BUCKET LIST: Africa, specifically Kenya and Egypt
SOMETHING YOUR CO-WORKERS DON’T KNOW ABOUT YOU: I used to perform with a belly dance troupe.
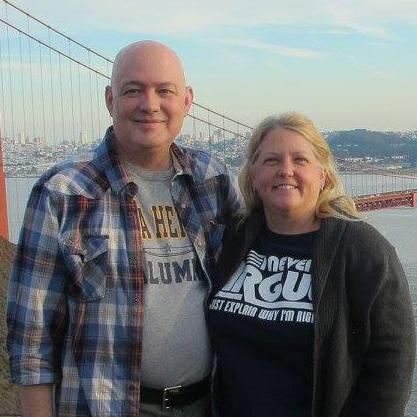
Larry Weinreich first became introduced to radiology in 1984 while serving in the U.S. Air Force. Throughout his eight-year USAF career, he worked with CT, X-ray, and interventional radiology systems as a technologist; after his active-duty career concluded, Weinreich continued as an RT in civilian imaging environments while also serving another 15 years as a medical liaison corpsman in the U.S. Navy reserves.
“Everywhere I went, they stuck me in front of an X-ray machine,” he joked.
As his civilian career wore on, Weinreich took on additional responsibilities, becoming a manager of imaging systems, and then a director of radiology, and eventually adding an educator’s role as a radiologic technology instructor at South Texas College in McAllen, Texas until the novel coronavirus (COVID-19) pandemic contracted the program.
Today, Weinreich is director of radiology at South Texas Health Systems, which includes imaging departments at the STHS Edinburg adult hospital, STHS children’s hospital, and six freestanding emergency rooms in McAllen, Edinburg, and the South Texas Valley.
“I like imaging because it’s different every day,” Weinreich said. “I get to solve problems, and make sure patients have a good stay. I like the people that I work with.”
When he’s not at any of the various locations under his supervision, Weinreich spends his evening and weekend off-hours developing Mellar Mercantile LLC,
the small online shopping business he operates with his wife, Melanie (Melanie + Larry = Mellar). At 59, he’s contemplating a future in which that enterprise gets his full attention in retirement. But together, the couple also has their hands full at present with a household of 17 adopted cats.
The orange cats are: Sunny, whose forepaws are bent at odd angles, and Beast; the tortoiseshells, Shelley and Sally; and Maine Coon mixes Oakley and Jack Dempsey. Rocky Marciano, a gray and white fellow, looked like he was starving when the Weinreichs met him, but never lost a fight scrapping for meals in the neighborhood.
Siren meows loud enough to let you know he wants attention, and so does mama cat Millie. Copper was named for her eyes; Wrinkles, for his wrinkly paws. Georgia was a mean kitten, so they named her after the Charlie Daniels Band song, “The Devil Went Down to Georgia,” but Rudy Valentino was so sweet and charming he was named for the iconically handsome silent film star.
“I’ve had cats most of my life,” Weinreich said. “I started rescuing cats when I was a kid living with my grandmother, who had about five or six cats of her own. When I found a kitten in the alleyway, she nursed it back to health, and kept it until it was a very old cat.
“I married my wife in 2009, and there were some neighborhood cats who were strays and feral, so we started TNR [a trap, neuter, and release program], fixing as many as we could,” he said. “They would show up pregnant, and we would find homes for some. Others had problems, and we kept them.”
With 17s come 17 heartbreaks, Melanie Weinreich
has said; although the couple’s fostering and care efforts have changed the fortunes of many wayward strays, it’s not always enough to save them. In moments like those, the Weinreichs comfort themselves by knowing that they’ve done what they can for those lives they’ve touched.
“I can’t stand to see animals in pain,” Larry Weinreich said; “I can’t stand to see them suffering, or lonely, or starving. If one of them’s around us and lost, we end up helping them. We keep far more than we’ve ever adopted out because I get attached to them, and we can’t give them up.
“They are part of the family,” he said. “They have all the emotions we do. I see love, I see jealousy. They have different personalities, likes and dislikes; some of them are pig-headed. They’re really thinking, living beings. The only difference is they can’t speak to us, and they don’t have thumbs.”
Of course the couple’s love of cats has poured over into their commercial operation. Among the most popular products for sale at Mellar Mercantile are its cat-themed, drop-ship coffees. With feline-related monikers like Caterwauler and Purrfect Brew, the Weinreichs have memorialized their housemates in the names of their coffee blends.
“‘Sunny Side Up’ is for my Sunny guy,” Weinreich said. “‘Tortitude’ is for Bear; ‘Maine Diet’ is for Jack Dempsey.”
Years ago, when the couple lived in Canyon Lake, and the local chamber of commerce was looking for someone to open a coffee shop in town, Larry contemplated starting one as a side business into which the Weinreichs might retire.
“I like coffee a lot,” he said; “I had wanted to open my own regular, walk-in, brick-and-mortar coffee shop, but it’s expensive, and I don’t know how to make the fancy drinks myself. So we got into drop-shipping.
“We incorporated as an LLC, got our EIN number from the IRS, and did something we never thought we were going to do together,” Weinreich said.
Today, the couple lives in McAllen, Texas, on the border of Mexico. Although they may still someday open a small coffee shop closer to home, they’re focused on growing the Mellar Mercantile brand online, expanding into imported arts and crafts from Africa and South America, and possibly expanding the inventory to include pet items. For now, the business is poised for slow, steady growth as it approaches its first six months of operation. And in the meantime, the Weinreich household hums with the low rumble of contented cats. •


 Sunny is one of Larry Weinreich’s favorite cats.
Eight Ball is one of the cats Larry Weinreich has rescued .
Sunny is one of Larry Weinreich’s favorite cats.
Eight Ball is one of the cats Larry Weinreich has rescued .
MMA fighters and an “atmospheric river” were no match for the annual Imaging Conference & Expo!
ICE 2024 stands out as one of the largest in the 10-year history of the event. The 10-year anniversary celebration added to the continuing education sessions, networking opportunities and a packed exhibit hall. In addition, the ICE18 Leadership Summit and Reverse Expo provided an extra boost to an already fun and exciting event.
Imaging leaders from throughout the nation checked into Hyatt Regency Irvine as some of the top MMA fighters checked out on Sunday before the signature Leadership Dinner. The dinner was a knockout as imaging thought leaders connected over common issues and personal stories.
The arrival of an atmospheric river did little to dampen the spirits of attendees and exhibitors with close to 400 people on hand for the first full day of the conference on Monday. Imaging leaders and service professionals took part in a special CRES Prep session as well as a variety of continuing education presentations.
The exhibit hall was the place to be later in the day with more than 60 companies on hand to share products and solutions that facilitate the many duties and responsibilities of the attendees.
Add an “amazing” keynote address and there is no doubt as to why everyone had positive feedback regarding ICE 2024.
ICE Magazine Group Publisher Megan Cabot was elated with the conference.
“Our annual ICE conference is always such a great event, but our 2024 event felt extra special this year,” she said. “The attendees and exhibitors that came to our show are top notch and I feel lucky to have them as colleagues and friends. If you’re a professional in the imaging industry make sure to put ICE on your schedule for conferences to attend in the years to come. The education and lifelong connections are worth it!”
“In speaking with an attendee after the event she said that she attends the ICE conference each year for the continuing education and vendor resources, but even more so for the
connections she makes with colleagues that often become lifelong friendships,” said MD Publishing Vice President Kristin Leavoy, CMP. “Hearing these words truly spoke to the uniqueness of the Imaging Conference & Expo and what sets our conference apart from others in the industry. We strive to help our attendees and exhibitors make connections that will serve them for years to come.”
Jessica Chambers, MHA, RT(R)(CT), Regional Service Line Director of Imaging with SSM Health St. Joseph Hospital-Lake St. Louis echoed Leavoy’s comments.
“I know I say this every time I’m asked about ICE, but the networking is most valuable thing for me,” Chambers said. “I forged genuine friendships with other great leaders that will continue to help me grow within my career. I also prefer this conference over others as it’s not so large that it becomes overwhelming, and you never have time to converse with people. While it’s great to see this continue to grow, it’s still sizable to be beneficial for me to get personal one on one time with the individuals I want to speak with.”
George Rozelle from GE HealthCare praised the quality of the attendees at the conference.
“Great attendees, I like the conference in particular because it is highly imaging focused which is right in our wheelhouse,” Rozelle said. “You have some of the key decision makers from the radiology department and the imaging departments. You have directors, you have administrators, and some of the technologists staff. It covers the gambit of administration down to who works on the machine.”
Phil Englert, vice president of medical device security with Health-ISAC Inc., shared his description of the conference.
“I would describe the ICE conference as insightful, educational and inspiring,” Englert said.
Shelby McCarty, an imaging supervisor from Trimedx, volunteered positive feedback after just one day at his first ever ICE.
“The vendor expo was great for me to be able to have points of contact and interface with those vendors that I can turn to and have different options for parts and service,” he said.
The next Imaging Conference & Expo is set for Orlando, Florida in February 2025. For more information, visit AttendICE.com. •
FUJIFILM Sonosite Inc. has announced the launch of Sonosite Voice Assist application, a first-of-its-kind voice command feature that enables proceduralists to control their Sonosite PX and Sonosite LX systems hands-free during sterile or clean procedures, including central venous access, peripheral nerve blocks, among many other intricate patient procedures. The Voice Assist is easily activated with a simple voice command, “Activate Voice,” whereby proceduralists are immediately able to control many of the critical functions hands-free during an exam.
FUJIFILM Sonosite’s Voice Assist feature allows users to freeze and save images, adjust gain settings, and add color flow all through the proceduralists voice command. The feature helps reduce health care provider costs and streamlines
workflow by eliminating the need for an assistant to be in the room to help complete an exam or procedure. Additionally, the hands-free operation allows the proceduralist to stay fully focused on the patient, contributing to a safer, more sterile environment.
“This groundbreaking advancement demonstrates FUJIFILM Sonosite’s commitment to not only enhancing its products but also improving patient care and empowering health care professionals to deliver the best possible medical services,” said Rich Fabian, chief executive officer and president of FUJIFILM Sonosite. “Performing ultrasound without having to touch and configure controls not only helps to maintain a sterile environment and enhance flexibility but makes performing an exam more accessible for every level of user.” •

Ultrahigh-spatial-resolution photon-counting detector CT improved assessment of coronary artery disease (CAD), allowing for reclassification to a lower disease category in 54% of patients, according to a new study published in Radiology , a journal of the Radiological Society of North America (RSNA). The technology has the potential to improve patient management and reduce unnecessary interventions.
Coronary CT angiography is a first-line test in the assessment of coronary artery disease. However, its diagnostic value is limited in patients with severe calcifications, or calcium buildup in the plaque of the coronary arteries.
Ultrahigh-spatial-resolution photon-counting detector CT (PCD-CT) improves image quality compared to conventional CT. Additionally, it provides better spatial resolution, or the ability to differentiate two adjacent structures as being distinct from one another.
“Our study provides a glimpse into the potential impact of performing coronary CT angiography using ultrahigh spatial resolution technology on risk reclassification and recommended downstream testing,” said study co-author Tilman Emrich, M.D., attending radiologist at the University Medical Center Mainz in Germany, and assistant professor of radiology at the Medical University of South Carolina in Charleston.
For the study, researchers evaluated coronary stenoses, or narrowing in the coronary arteries, in a vessel phantom (in-vitro) containing two different stenosis grades (25%, 50%), and retrospectively in 114 patients (in-vivo) who underwent ultrahigh-spatial-resolution cardiac PCD-CT for the evaluation of coronary artery disease. In-vitro values were compared to the phantom’s manufacturer specifications, and patient results were assessed regarding effects on coronary artery disease reporting and data system reclassification (CAD-RADS).
“The study used a combination of artificial vessel models and real-world patient data,” Emrich said. “It simulated three types of reconstructions from a single PCD-CT scan, resembling conventional CT, high-resolution, and ultrahigh-spatial-resolution
scans. Observers evaluated the severity of stenosis and generated CAD-RADS classifications, guiding further patient management decisions.”
In-vitro results demonstrated a reduced overestimation of the stenosis by ultrahigh-spatial-resolution scans by reducing the adverse effects of the calcifications on the image.
Results from the patients with suspected or diagnosed coronary artery disease confirmed a lower median degree of stenosis for calcified plaques (29% vs. 42%) with ultrahigh-spatial-resolution PCD-CT compared to standard CT. Ultrahigh-spatial-resolution often led to patients being reclassified to a lower CAD-RADS category. Of the 114 patients, 54% were given a lower CAD-RADS classification than they were originally assigned. The researchers found in-vitro quantification of the 193 coronary CT angiography-based stenoses was also more accurate using ultrahigh-spatial-resolution than standard resolution.
“We found that ultrahigh-spatial-resolution reconstructions resulted in significant changes in recommendations for over 50% of patients,” Emrich said. “The impact was particularly notable in cases with calcified plaques, where ultrahigh-spatial-resolution reduced the overestimation of stenosis.”
Emrich explained that ultrahigh-spatial-resolution may address the current limitations of conventional cardiac CT angiography by reducing the overestimation of stenosis due to calcium blooming, an effect which can cause small, high-density structures — such as calcifications — to appear larger than their true size.
“This could significantly alter recommendations for downstream testing, potentially leading to a reduction of unnecessary procedures (and their potential complications) and reduced healthcare costs,” he said.
No substantial benefits of ultrahigh-spatial-resolution were observed for mixed and non-calcified plaques.
“It is important to note that these findings are from a simulation study, and further validation is needed in real-world comparisons,” Emrich said. •

Butterfly Network Inc. has announced the commercial launch of its third-generation handheld point-of-care ultrasound (POCUS) system, Butterfly iQ3, which received FDA clearance last month. Butterfly iQ3 is powered by the company’s most advanced semiconductor chip with a data transfer rate that is double that of its predecessor. The result is unparalleled image quality and faster micro-beamforming for advanced 3D capabilities: iQ Slice and iQ Fan.
“Butterfly iQ3 is a pivotal moment in Butterfly’s trajectory, further validating the company’s initial hypothesis that semiconductor-based digital ultrasound is not only viable, but the future of all ultrasound,” said Joseph DeVivo, Butterfly Network’s president, chief executive officer, and board chairman. “With the introduction of iQ3, we’re witnessing a paradigm shift in ultrasound. iQ3 sets a new standard where digital image quality matches that of traditional handheld devices, and even certain carts. This device will attract more seasoned POCUS experts to choose Butterfly and support new learners to gain confidence and competency through artificial intelligence and advanced imaging tools.”
Butterfly iQ3 brings best-in-class, high-resolution image quality with twice the processing power compared to Butterfly iQ+ and a novel “no focus” rubber lens, enabling providers to intuitively identify anatomy, observe small structures, and ultimately, make more confident diagnostic decisions, according to a news release. In a blind survey distributed by third-party vendor, Intellisurvey, 475 clinicians across more than eight specialties compared Butterfly iQ3 images to GE
Vscan Air CL, with the majority across all categories ranking iQ3’s overall image quality better than that of GE Vscan Air CL.
Launching on Butterfly iQ3 are two new, advanced 3D imaging capabilities designed to make image capturing easier: iQ Slice and iQ Fan. These tools join Butterfly’s existing robust feature list of over 20 anatomical presets, six imaging modes (B-Mode, M-Mode, Color Doppler, Power Doppler, Pulsed-Wave Doppler, and Biplane Imaging) and collection of artificial intelligence (AI) and advanced imaging tools (e.g, Auto Bladder Volume Capture, Auto B-Line Counter, NeedleViz, and a rich set of Calculation tools).
Butterfly iQ Slice: The world’s first automated, sequential ultrasound capture mode on a handheld device, made uniquely possible by Butterfly’s proprietary Ultrasound-on-Chip technology. iQ Slice automatically steers the beam to scan an organ and capture up to 46 ultrasound slices at a time across a wide angle. The imaging mode is designed to make it easier and faster to acquire excellent images without skilled maneuvering. These files can either be immediately read and measured at the bedside by skilled scanners, or for those less experienced, can be sent to a specialist for further review – similar to the workflow of a CT or MRI.
Butterfly iQ Fan: A dedicated lung tool that further builds on the core iQ Slice technology to allow providers to benefit from real-time, back-and-forth virtual fanning, making it easier to visualize A-lines and other lung conditions. With iQ Fan the user no longer needs to manually fan the probe, and can just focus on analyzing the images. •
The Joint Commission has announced a voluntary Responsible Use of Health Data (RUHD) Certification program for U.S. hospitals and critical access hospitals, effective Jan. 1, 2024. Protecting patient privacy is a foundational element of a strong data use policy. The new certification will provide guidance and recognize health care organizations navigating the appropriate sensitivities needed to safely use data for purposes beyond clinical care, known as secondary use of data.
Secondary use of data includes quality and operations improvement, discovery, or algorithm and artificial intelligence development. The certification will provide an objective evaluation as to whether an organization is committed to utilizing best practices in its secondary use of data and promoting responsible use of data by demonstrating established protocols regarding transparency, limitations of use and patient engagement.
Nearly 85% of U.S. hospitals have the capability to export their patient data for reporting and analysis purposes, according to the Office of the National Coordinator for Health Information Technology. However, there is no standard approach to use de-identified data nor to validate best use practices. Organizations working toward standardization may help address the unmonitored handling of secondary health data.
“As more health care organizations are leveraging clinical data for secondary purposes, there have been increased calls to assure responsible data stewardship,” says Jonathan B. Perlin, MD, Ph.D., MSHA, MACP, FACMI, president and chief executive officer, The Joint Commission Enterprise. “The Joint Commission recognizes it can play an important role in validating that robust policies and procedures are in place to help protect, govern and accountably use secondary data. We believe our Responsible Use of Health Data Certification will help health care organizations use data responsibly to improve the safety, quality and equity of care, develop new technologies, and discover new
therapies benefitting all patients.”
RUHD Certification is based on principles adopted from the Health Evolution Forum’s “The Trust Framework for Accelerating Responsible Use of De-identified Data in Algorithm and Product Development.” The certification’s requirements cover these areas:
• De-identification process
• Data controls
• Limitations on use
• Algorithm validation
• Patient transparency
• Oversight structure
“On behalf of the industry leaders in the Health Evolution community, we are honored to inspire and serve as a catalyst for this important work. The principles established within the Trust Framework are more pertinent than ever for organizations engaging in cross-sector collaboration to propel a new generation of data-powered solutions as artificial intelligence forges a new frontier of innovation and discovery in healthcare,” says Richard Schwartz, CEO, Health Evolution. “The Health Evolution Forum developed the Trust Framework with the intention that its enduring principles will serve as the groundwork for industry-leading organizations and coalitions to build upon this effort and chart the path forward in an ever-evolving technology, regulatory and business environment. It is with deep appreciation that we recognize the significant work by the health care leaders in the Health Evolution community who contributed their time and expertise to develop the Trust Framework.
RUHD Certification will validate to patients and other stakeholders that an organization has policies and procedures in place to protect health record data. Hospitals achieving RUHD Certification will be recognized publicly for establishing an objective and rigorous process for meeting the necessary requirements.
Hospitals may immediately begin working toward RUHD Certification. •
GE HealthCare and MedQuest Associates, a leading owner, operator, and manager of outpatient diagnostic imaging facilities, recently announced a three-year collaboration to deliver excellence in patient care by providing access to innovative technologies from GE HealthCare and the infrastructure and resources from MedQuest that are needed to optimize multi-site outpatient imaging networks for success.
As the demand for imaging services grows, advancements in technology enable a broader range of services to be provided in ambulatory settings, which can help alleviate the burden on acute care hospitals. Innovative care models and emerging technologies in outpatient imaging are vital to boosting operational efficiency and expanding access, helping ensure top-tier patient care. MedQuest’s model of joint ventures with health systems, coupled with GE HealthCare’s innovative technologies, will help deploy emerging imaging solutions, including solutions to support theranostics, into the


ambulatory setting.
MedQuest CEO Jason Howard shared, “Our commitment to customer-centric care is at the center of everything we do. Building upon our more than 25-year history as a leader in outpatient imaging, our partnership with GE HealthCare will position us at the forefront of innovative care delivery and product line development, enhancing the level of care for our patients and health system partners.”
MedQuest will continue to broaden it’s ability to provide high-performing care in the outpatient imaging space with the addition of AI-enabled digital capabilities from GE HealthCare, including AIR Recon DL, AIR Touch Technology, Imaging Protocol Manager, Smart Subscription and Digital tools with Imaging 360. These innovative capabilities will help enable clinicians to provide improved outcomes for patients and deliver personalized, precise patient care, while improving radiology workflows and helping ease workloads for care teams. •
• One-year-old company with over 100 years of experience manufacturing and supplying X-ray tubes.
• High-quality components from IAE SpA, Europe’s premium X-ray tube manufacturer for 75 years.
Made in the USA with US and European components.
Contact us at:
X-Ray America, LLC
Email: info@X-RayAmerica.com
Phone: 1.854.999.6888
Global: IAE.it
US Headquarters: X-RayAmerica.com


The ICE webinar “Real Talk” presented by Janel Morgan, MSW, SHRM-CP, Prosci, was sponsored by RSTI. Since 1985, RSTI (Radiological Service Training Institute) has been providing the finest quality diagnostic imaging training. The session was approved for 1.0 ARRT Category A CE credit by the AHRA.
Morgan focused on how to have effective conversations, especially when it’s difficult. Indivdiuals face difficult conversations every day and handling them poorly impacts quality of life, productivity, success and relationships. This session provided simple tools to transform difficult conversations into effective, respectful conversations, or “real talk.”
Participants were able to increase their ability to bring to life the following elements of a real talk conversation:
• Being respectful, even if it’s uncomfortable in the moment
• Sharing their honest perspective
• Maintaining positive intent
• Taking action as a result of the conversation
• Improving the quality of their relationships
Attendees were also able to ask questions during a Q&A session.
The webinar was popular and received positive reviews. Tracy Moore, the radiology director at Peterson Regional Medical Center in Texas won an ICE gym bag.
Attendees were asked, “Why do you join ICE webinars?”
“The information is always very helpful,” said ElizaBeth Killingsworth, a radiation safety officer at UT Health East Texas.
“Quality leadership content,” said Dustin Ward, a radiology supervisor/MRSO at Saint Luke’s Health System.
“They are informative, well produced and I can usually watch at work,” shared Jeanie Brown, a multi-modality technologist at RAYUS Radiology.
“Relevant topics and excellent speakers. Bonus for the CE credits!” said Kathryn Hampton, an account manager, icometrixI.
“I participate in the webinars in order to gain knowledge and information necessary for my professional and personal development, and to be able to share them with my students,” said Calin Corciova, an associate professor at the University of Medicine and Pharmacy “Grigore T. Popa” Iasi.
For more information, visit ICEwebinars.live
 MELISSA HENAO-ACOSTA
DIRECTOR OF MARKETING
MELISSA HENAO-ACOSTA
DIRECTOR OF MARKETING
WHAT PRODUCT, SERVICE, OR SOLUTIONS DOES YOUR COMPANY PROVIDE TO THE INDUSTRY?
We’re a Medical Imaging Equipment Company that provides high quality pre-owned imaging equipment, parts and service to the healthcare industry world-wide. Carrying a variety of imaging such as CT Scanners, MRI, CARMs, Mammo Units, Bone Densitometers, X-Rays and more.
TELL US WHAT DIFFERENTIATES YOUR COMPANY FROM THE COMPETITION?
As a family-owned business, we know the impact medical equipment has on the life of the patient. We have seen over the years how medical products have been part of the recovery of our own family, neighbors, friends, and buyers. We know that quality, honesty, medical knowledge, and good customer service makes the difference to our buyers and consequently to the patient. Our goal is to reflect our values, knowledge, professionalism, excellence, and customer service towards everything we sell and do.
WHY DID YOU CHOOSE ICE FOR ADVERTISING?
We became intrigued by advertising with ICE due to its dedicated audience of imaging professionals, precisely the demographic we aim to target.
WHAT PRODUCT, SERVICE, OR SOLUTIONS DOES YOUR COMPANY PROVIDE TO THE INDUSTRY?
NCSI provides end to end equipment services and maintenance for nuclear medicine systems located at nuclear medicine sites around the globe.
TELL US WHAT DIFFERENTIATES YOUR COMPANY FROM THE COMPETITION?
42+ years of experience in this industry in a multivendor environment enables us to support nuclear medicine systems, cameras and components from many manufacturers.
WHY DID YOU CHOOSE ICE FOR ADVERTISING?
We are excited about ICE to provide exposure of our services to medical professionals, asset managers and other key stakeholders responsible for nuclear medicine.



is anticipated to drive market growth.
The health care asset management market is expected to register a compound annual growth rate (CAGR) of 30% from 20242029, according to Mordor Intelligence.
Health care asset management is a systematic and cost-effective strategy to plan, acquire, operate, and dispose of a health care organization’s equipment and physical assets. The primary factors that encourage adopting health care asset management in health care organizations are keeping track of medical devices, high operating costs, time savings, enhanced patient care, higher staff productivity, significant cost savings and intense maintenance.
Real-time location systems (RTLS) and radio frequency identification devices are crucial instruments for health care asset management (RFID). The increased demand for improving efficiency and the rising integration of cloud computing, electronic health records and other digital systems in hospitals are driving the market. However, low awareness and innovation in this sector in low- and middle-income countries is a significant challenge for the health care asset management industry.
Hospitals are increasingly adopting automated workflows and intelligent business analytics to ease the burden on their staff to improve workflow bottlenecks. Real-time location systems (RTLS) are poised to find widespread usage in health care asset management systems. The ability to manage multitasking involved in data capturing, integration, visualization and analysis to enhance reliability
Furthermore, the growing focus on existing assets’ effective management along with the workforce has propelled numerous medical facilities worldwide to adopt efficient management technologies and solutions of investments, therefore enlarging market growth of health care asset management.
In urgent circumstances, the patient’s state can change in a matter of seconds, and if the effectiveness of the operations is poor, the patient could perish. An additional driver of the asset management market in the health care system is the growing demand to increase hospital operational efficiency. However, the outdated health care infrastructure and worries over data privacy are a few factors that prevent using these technologies.
The availability of robust health care infrastructure has propelled the demand for hospital asset management solutions, as their immediate implementation is possible. The North America region has been one of the early adopters of IT infrastructure. According to Internet World Stats, the penetration stands at 89.4% of the population, which increases the deployment of asset management solutions in health care.
Moreover, North America accounts for more than 40% of the global pharmaceutical industry. Also, the growing awareness about the benefits of deploying asset management systems in health care can lead to increased demand for the market in the future.
Additionally, the market is expected to develop due to the rising usage of RTLS asset management and health care asset management with IoT for patient tracking, asset tracking, staff location and throughout. •
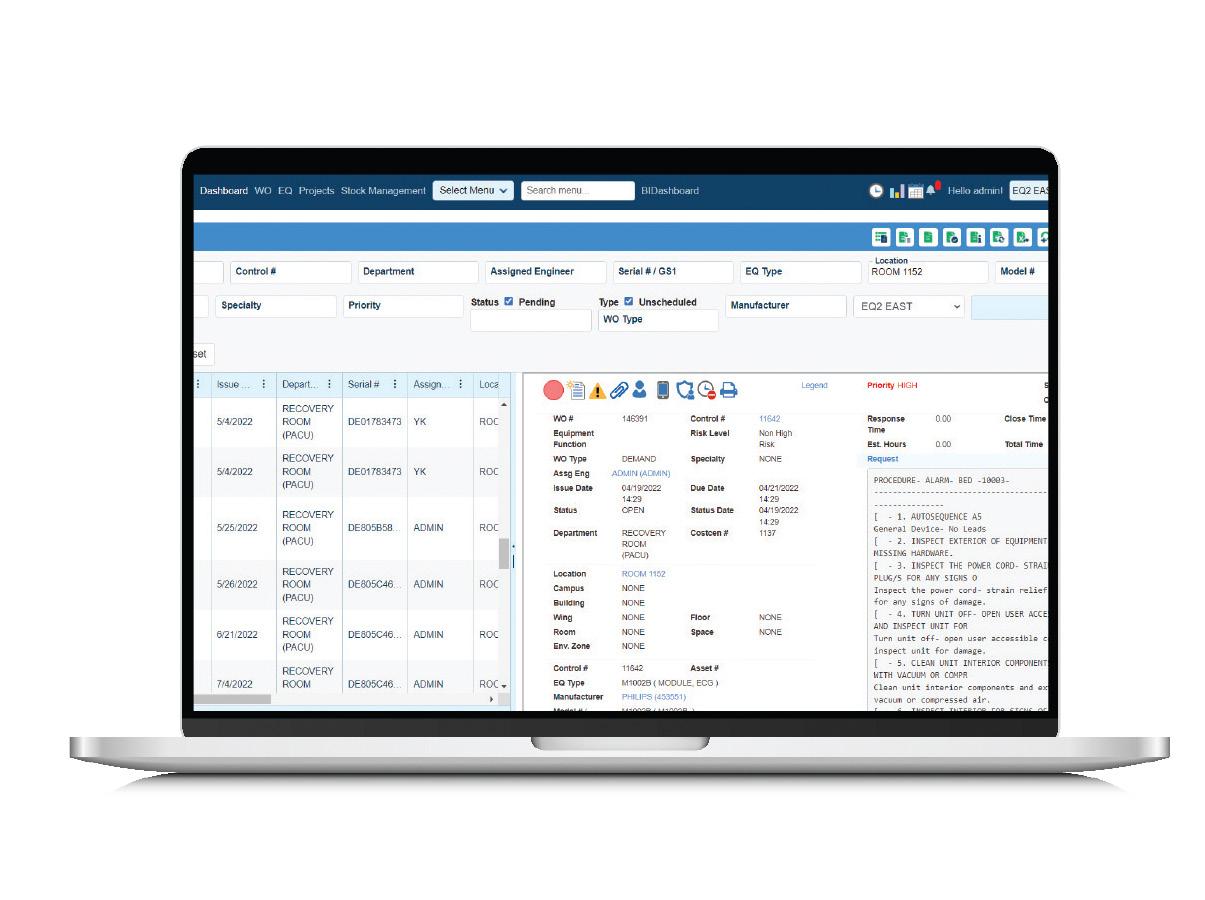
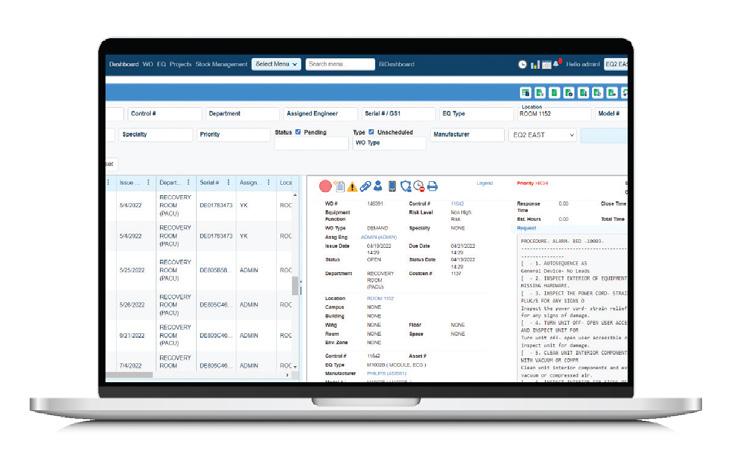
EQ2 and its product HEMS One are dedicated entirely to the needs of health care. HEMS One is a complete modern CMMS and asset management software product for HTM/Biomed, Imaging, Facilities, EVS, and IT departments and is the choice of some of the most prestigious health care organizations. Over 30 years of innovation and 100% U.S. based support team means you can be assured that your hospital will be using one of the best CMMS products available. Schedule your live demo of HEMS One today.

Unite your floor plans and enhance asset management with work orders and assets all on one convenient screen. CMS View from FSI gives you 24/7 access to integrated floor plans, equipment and work order records on any mobile device. Visualize locations of assets and work order icons on the floorplan, saving technicians an average of four minutes per asset/work order. Unlike paper-based programs, CMS View stores your critical asset, work order, and drawing data in one easy-to-access platform to give you insights and guide decision-making, boosting your team’s productivity with visibility into work order locations.
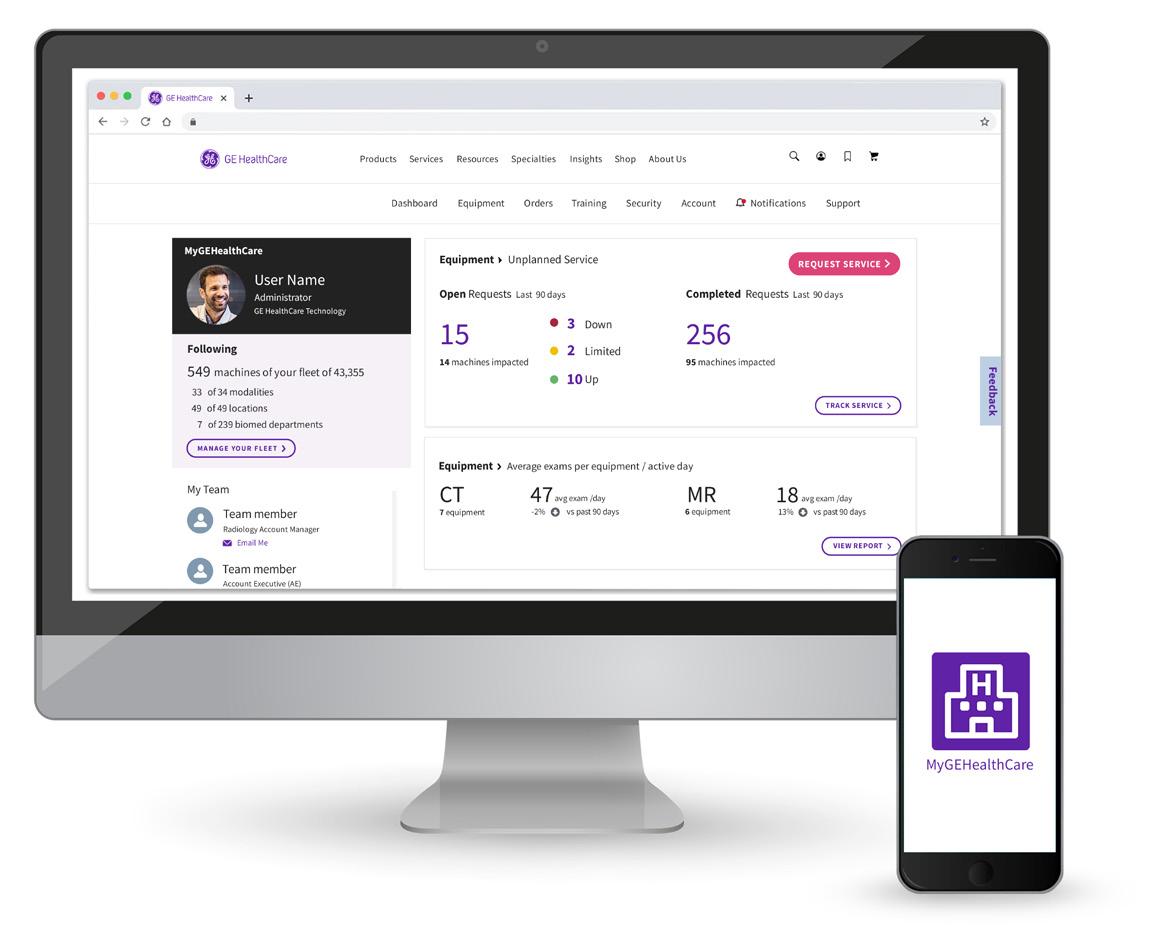
Your one-stop shop to easily manage equipment and personalize service support for your entire equipment fleet. MyGEHealthCare Experience is your online, hassle-free way to manage your equipment and fleet information. It’s your one-stop shop where you can get proactive insights and service that facilitate department-wide communication. The desktop experience of MyGEHealthCare Experience builds on mobile app to give comprehensive, full life-cycle support of any device. It’s a unified support experience that includes the useful features GE HealthCare customers have enjoyed for years, now delivered through a personalized dashboard and reports.

The Guardian Program from Siemens Healthineers improves the uptime of imaging systems through continuous real-time system monitoring, prediction mechanisms based on artificial intelligence, and proactive services that combine to identify problems and frequently correct malfunctions before they occur. With Guardian, all connected systems proactively relay data to the Siemens Healthineers Customer Care Center, where a dedicated expert monitors operations in real time, looking for even slight deviations from standard operating conditions. Upon discovering a potential issue, a Guardian Expert opens a service ticket for the affected system and/or contacts the customer with recommendations for immediate action (e.g., remote repairs or the scheduling of an on-site visit.)
Imaging leaders and experts replied to questions from ICE Magazine to share their asset management insights with readers this month. This Director’s Circle article is a companion piece to the Product Focus feature that highlights some tools and services that health care facilities can use in regards to the asset management of imaging equipment and devices.
Top-notch imaging leaders providing their thoughts and knowledge include members of the ICE18 Leadership Summit recently held in conjunction with the Imaging Conference and Expo (ICE) in Irvine, California. For more information about the ICE conference, visit AttendICE.com. Participating in the April 2024 Director’s Circle are:
• Jessica Chambers, MHA, RT(R)(CT), Regional Service Line Director of Imaging, SSM Health St. Joseph Hospital
• Michelle Dossa, Ph.D., CRA, RT(R), Radiology Director-West Market, University Hospitals of Cleveland
• Nancy Godby, MS-MHA, MA, RT(R)(M) ARRT, CHC, Director of Radiology, Cabell Huntington Hospital Inc.
• Katherine A. Mohr, DBA, MA, BS, CRA RT (R) (CT), Director, Sinai Hospital
Q: WHAT ARE THE AUTOMATION TOOLS YOU USE TO TRACK YOUR ASSET’S PERFORMANCE AND UTILIZATION?
Chambers: Currently we do not have a good source of truth for asset utilization, we are currently evaluating some solutions yet haven’t landed on one to invest in yet. I do track all imaging equipment on a replacement roadmap that we pull downtime hours from our biomed partners and age of equipment to help estimate replacement strategies.
Dossa: We are currently able to pull data from our EMR as well as use Power BI tools. We have a specific set of KPI based on engagement, quality, and finance that we track/re-
port for all of our imaging sites across our system. We develop system-wide S.M.A.R.T. goals each year that are tied to our organizational goals and our results are tracked and reported – some on a weekly basis while others are monthly.
Godby: I maintain an Excel spreadsheet listing all equipment/ assets and we receive monthly and quarterly reports of repairs made.
Mohr: TMS. We do not track utilization.
Q: HOW DO YOU INCORPORATE THESE METRICS INTO YOUR OVERALL DEPARTMENT GOALS?
Chambers: We track the appointment fill rates in our outpatient imaging departments to understand our capacity in these departments. Most of our other goals are around volume and NOI and due to the lack of utilization dashboards in our organization we are unable to form dedicated goals around utilization. If we are blocking appointments from down equipment, then it will have a direct impact on volume and net operating income therefore the asset itself is identified as a gap and we will use that data to assist us in escalation for replacement.
Dossa: This year, we have a team working on a green/red dashboard that will display our S.M.A.R.T. goals and KPI so we can track our performance. We build action plans around our results.
Godby: We utilize information for equipment planning and purchases.
Mohr: Uptime is tracked globally, not just for radiology devices.
Q: WHAT IS THE STRATEGY FOR MANAGING AGING EQUIPMENT, ESPECIALLY WHEN THERE ARE BUDGET CUTS?
Chambers: I have a 10-year roadmap forecasting when we will replace equipment. I work with each hospital VPO to deter-




mine the order in which we will ask to replace the equipment across the region. We are given a regional budget to spread across the seven hospitals and therefore it’s a collective effort to determine what we need to replace first. We still have quite a bit of aging equipment, so we are still in the catch-up phase. We hope with this more proactive strategy of replacing before the equipment is limping along, we will see better outcomes in the future.
Dossa: We have been working on a non-obsolescence plan with key equipment vendors. Our plan has helped us declare specific equipment configurations for each modality as well as prioritize replacements over the course of 10 years. We look forward to this planned structure vs. piece-by-piece replacements.
Godby: I include on my Excel sheet a future date for which I believe we need to begin to plan to replace each piece of equipment.
Mohr: We maintain service contracts or use an insurance program.
Q: AS AN IMAGING LEADER, WHICH DEPARTMENTS DO YOU WORK WITH WHEN IT COMES TO ASSET MANAGEMENT?
Chambers: Purchasing, since we have a pre-established equipment roadmap our purchasing team will use the estimated replacement numbers to negotiate pricing. Additionally, if I am transitioning vendors, I will connect with biomed to verify they are trained to service the equipment. If not, we will make sure their training is included in the equipment quotes. I have to work with IHT to perform a technical assessment on the equipment to verify it is safe for the network.
Dossa: Equipment replacement requires collaboration with many – radiologists, technologists, physics, radiology IT, research, ordering providers, HTM, vendor, facilities, finance, leadership, supply chain, strategy.
Godby: Materials management, contracting, risk management for contract reviews and each of our radiology leadership to determine how best to proceed.
Mohr: Clinical engineering.
Q: WHAT MODALITY WILL YOU BE REPLACING NEXT? WHAT FEATURES ARE A MUST-HAVE FOR THE NEW DEVICES?
Chambers: MRI. Our equipment is very out of date. We do not have a lot of the fast-scanning technologies within our scanner. We feel we can actually grow volume with a newer scanner as new technologies will allow us to shorten scan times.
Dossa: We hope to be adding a CT in an ED space. We are looking for cardiac and neuro capabilities in additional to the ability to perform more traditional ED exams, i.e. chest, abdomen, pelvis. We must have ease of use and fast reconstruction ability for our technologists to ensure quality throughput.
Godby: We do not have any plans for replacement for the next fiscal year.
Mohr: MRI, standard 1.5T with breast imaging capabilities.
Q: WHAT ELSE CAN YOU SHARE WITH ICE MAGAZINE READERS REGARDING ASSET MANAGEMENT?
Chambers: In the recent years, we really have changed our focus from a replacement of “broken” equipment mentality to a more forward-thinking proactive approach. The development and collaboration of the roadmap has really helped us with engaging the key stakeholders and keeping everyone updated on the progress of new equipment purchases. I would like to see us get to a point one day that we are able to replace equipment to keep up with technology versus using equipment far past its life expectancy and missing out on multiple generations of advanced technology.
Dossa: Have one source of truth when it comes to equipment inventory. We found that many had lists but did not always track the same information and/or accurate information. We found physics to have the most accurate inventory. From there, we touched each piece of equipment to validate information. Asset management is a team sport. Be sure to include all key stakeholders when developing and executing a plan. And, don’t be afraid to have those difficult conversations when needed around what may be needed and where in your health care system. Be smart about using capital assets. •
ST. JOSEPH HOSPITAL CABELL HUNTINGTON HOSPITAL INC. NANCY GODBY SINAI HOSPITAL KATHERINE A. MOHR• A niche job board for the HTM and imaging communities powered by TechNation.
• 2800+ actively looking biomedical and imaging professionals.
• Completely FREE and confidential registration and application process.
• The fastest growing HTM talent network in the country.
• 350+ open opportunities throughout the United States.
• A variety of posting options ranging from single-job postings to 12-month unlimited memberships.

htmjobs@mdpublishing.com for posting inquiries
htmjobs.com to register today





Amidst the overwhelming scientific evidence that carbon emissions driven by human activity continue to contribute to global health challenges posed by climate change, the field of health care is itself taking long overdue steps to address its role in the mechanisms at work therein.
“Health Care’s Climate Footprint,” a 2019 environmental policy paper from the international non-governmental agency Health Care Without Harm, provides some of the most comprehensive accounting of the scope of carbon emissions attributable to the business of health care across the planet.
According to the paper, the healthcare industry accounts for 4.4 percent of global carbon emissions. About 10 percent of the carbon emissions produced by the United States alone is attributed to health care, and the American health care system is the top C02 emitter “in both absolute and per capita terms,” at 546 million tons.
That same policy paper describes greenhouse gas emissions from health care as resulting from “energy consumption, transport, and product manufacture, use, and disposal,” in various ways. Direct emissions from health care facilities and their vehicle fleets comprise 17 percent of their global health care carbon footprint; they contribute another 12 percent via indirect emissions from purchased energy sources (electricity, steam, cooling, and heating). Health Care Without Harm attributes the re -
maining 71 percent to supply chain sources “through the production, transport, and disposal of goods and services” including “pharmaceuticals and other chemicals, food and agricultural products, medical devices, hospital equipment, and instruments.”
Finally, even when accounting for supply-chain emissions, 25 percent of all health care emissions “are generated outside of the country where the health care product is ultimately consumed,” according to the document. It also attributes the bulk of emissions from the health care industry to its consumption of fossil fuels, and notes that half of the global climate footprint from health care sources is a result of energy generation for and within the health care sector.
The research paper “Climate Change, Carbon Dioxide Emissions, and Medical Imaging Contribution,” written by Eugenio Picano, Cristina Mangia, and Antonello D’Andrea, and published by the J ournal of Clinical Medicine in 2022, posits that medical imaging accounts for approximately 1 percent of the global carbon health care footprint, based on “a conservative estimate of 10 billion medical examinations per year worldwide.”
Nearly every authoritative source on carbon emissions in general, as well as those relating to the health care industry in specific, agree that the work set before the largest institutions of the day lies in changing the courses of their environmental future in ways great and small. How that work might be achievable, and managing the changes that inherently will come
with it, now falls to decision-makers in the device manufacturing world and leading health care institutions as much as it falls to legislators and policymakers.
Vibhas Deshpande, vice president of sustainability innovation and strategic research at Siemens Healthineers, said that his company has put its commitment to sustainability front and center among organizational objectives, foremost by adding the word “sustainably” to its value statement last year – “We pioneer breakthroughs in health care. For everyone. Everywhere. Sustainably.” – and establishing key performance indicators for charting the change.
These KPI include a 90 percent reduction in its Scope I emissions (volume of greenhouse gas emissions directly controlled by the company) and Scope II emissions (volume of greenhouse gas emissions indirectly controlled by the company, including purchased energy) by 2030, before ultimately hitting net zero by 2050. Siemens Healthineers is also seeking to reduce its Scope III emissions (all indirect emissions not covered by Scopes I and II) 28 percent by 2030, and 90 percent by 2050.
“We are absolutely committing to this,” Deshpande said. “We need to help our customers who are downstream, so both of us benefit from a reduction in the carbon footprint.”
Reducing emissions at the institutional level means reducing power consumption at the imaging device level. Siemens Healthineers research collaborations with the Universities of Basel in Switzerland
and California at San Francisco (USCF) illustrated, respectively, how much electricity is required to power MR machines, and how much might be conserved by regulating it.
“In the University of Basel study, Dr. Elmar Merkle and colleagues showed that the annual consumption of three CT units and four MR scanners was equal to the annual energy consumption of a town of 850 people,” Deshpande said. “That’s the magnitude of the problem here.”
UCSF research revealed what could perhaps have been expected, which is that even merely turning the systems off when they’re not in use offers a significant reduction in power consumption.
“Most scanners are not in use overnight, but they’re still consuming energy because superconducting magnets need to be kept cool,” Deshpande said. “One way to reduce energy during non-operational hours is to cycle cooling. That saves a lot of energy; that’s an easy win to get.”
Similarly, Deshpande spoke about finding ways to manage energy demand from MR systems by using artificial intelligence (AI)-driven software optimization to help configure their operations. Newly available, AI-powered, lowmagnetic-field-strength scanners also may help conserve resources.
“We will always need to strike a balance between the benefits of these high magnetic fields – such as higher resolution and higher signal, to better understand some clinical problems – and the resources needed to manufacture, install and run this equipment,” Deshpande said.
“Cost-effectiveness comes down to what is the appropriate use of resources for each patient,” he said. “Imaging as a standalone
activity is energy-intensive, but if you look at the entire patient care pathway, the appropriate tests done at the right time can be valuable in reducing the entire cost of care in that patient’s life.”
For an original equipment manufacturer (OEM), contemplating that care pathway also motivates an internal analysis of the life cycle of an individual scanner, from materials sourcing to the manufacturing process, use of the technology in the field, and what happens when it’s retired.
Deshpande said Siemens Healthineers is trying to extend the useful life of its scanners through modular designs that are able to be upgraded at the customer site, and also by recycling those elements of its manufacture that are able to be recovered. The helium used in cooling MR magnets can be reclaimed from defunct scanners and reused in other processes. Newer Siemens Healthineers MR systems, like the MAGNETOM Free.Max, which is powered by a 0.55T magnet, use only a fraction of the helium demanded by legacy systems.
“It’s not only about when a machine is in use, but we really want to think holistically from the material supply to the end of life of the machine,” Deshpande said.
To that end, OEMs will be instrumental in the work that’s needed to build partnerships and policy guidance as the medical imaging space manages operational changes in pursuit of sustainability. Device manufacturers may be able to reduce the energy their imaging systems consume by helping their customers to manage infrastructure conditions onsite before they’re installed, Deshpande said, or by working with regulators to develop EnergyStar criteria for medical imaging devices. Customer and academic partnerships
provide key feedback and information that helps the next generation of technology function better and more efficiently.
“It really has to be a collaboration,” Deshpande said. “You can derive intelligence and drive changes by integrating information from the manufacturers, clinicians, and companies providing different products being used in the care pathway. I think we all believe that this is the right thing to do.”
Dr. Sean Woolen, director of prostate imaging at UCSF, who worked with Siemens Healthineers on MRI power conservation research, believes the pathway to greater sustainability in operational culture must be “framed in a winwin scenario” to generate buy-in from all parties involved. For example, saving on electricity consumption doesn’t only reduce the carbon footprint of a health care entity, it also cuts costs, which is important when green energy sources are a more expensive choice than their fossil-fuel-based alternatives.
“Some people will talk about the ultimate solution, which is having your hospital on fully clean energy,” Woolen said. “At UCSF, we have quite a bit of our hospitals on clean energy. But usually, the cleaner the energy, the more expensive the price. Being able to be more efficient with energy use saves money.”
Changing behavior in any context is both a critical piece of embracing sustainability culture and “one of the hardest things to do,” Woolen said. The most lasting improvements might be those that are folded into protocols or the background operations of new technologies. For instance, the three key insights from the MRI study – powering down equipment, shortening scanning times, and scanning on lower field strengths –
don’t achieve as much individually as realizing each improvement, let alone doing so at scale.
“We talk about performance gaps in health care all the time,” Woolen said. “You have some solutions that we know would make a huge impact on sustainable health care. How many institutions are following those practices so that we can close that gap?”
“Anything automated is going to be the easiest level of behavior change,” he said. “Figure out what the barriers are for technologists who don’t have the knowledge; why some of these simple solutions aren’t always happening. We should all be practicing at that same high level of evidence.”
Other imaging leaders believe some of the gains that can be won by managing power consumption on imaging devices can be further extended by similarly turning off PACS monitors and computers as well as office lights at the end of a shift.
A group out of Northwestern University is working with Siemens Healthineers to measure the power output associated with different pulse sequences during an imaging study, to see whether certain studies require more energy than others. The same researchers are also seeking ways to recycle some of the disposable materials con -

sumed in the imaging space, like iodine contrast agents and their packaging materials.
Dr. Katherine Maturen is the associate chair for ambulatory radiology and strategy at Michigan Medicine, and medical director of its East and Northeast Radiology Ambulatory Care Units in Ann Arbor, Michigan. Maturen and Woolen are collaborating on a comprehensive scoping review of medical imaging sustainability literature, synthesizing previous studies to develop a database of known values (such as the energy and carbon emissions associated with a single scan), and create a roadmap for future research.
Among hundreds of articles that have been published on the subject of radiology sustainability, Maturen noted that maybe only 50 articles are based on primary data collection efforts; most articles are commentaries and calls for action.
“Right now, there’s a lot of gaps in our quantitative knowledge; once we’ve resolved that, we can start to make broader statements,” she said.
Maturen agrees that it’s difficult to reconcile the impulse towards reducing energy consumption in medical imaging with the historic drive in the field to capture “the most high-definition, beautiful

images achievable.” It’s even more complicated to demonstrate a clear business directive in doing so, especially in a landscape of conflicting financial and cultural incentives.
“I think you have to make it practical to people,” Maturen said. “It has to be within the scope of what we can change. These issues are very high-level and seem out of reach to many practicing radiologists.”
“What other specialties are making headway on sustainability?” she said. “Anesthesia, because they’re literally using greenhouse gases. Some surgical specialties are doing well because they’re targeting waste, so they’re getting efficacy quickly.”
Maturen also rightly points out that the bottom line of the argument – reducing carbon emissions – takes precedence over the mechanisms by which people in the health care sector achieve it.
“The outcome we’re talking about is an ethical outcome,” she said. “It doesn’t matter why they make a sustainable change in practice – maybe because it is faster, less expensive or because they are personally concerned about the environment – it just matters that they do it. As sustainability becomes incorporated into practice, people’s attitudes will change over time.” •






Iread a leadership article a few years ago that laid out the reasons why it is important to tell a story when we communicate to our teams. We can tell them what to do. We can give them instructions on the steps required to accomplish a task and the reason we want the task performed. A list of instructions is difficult to pay attention to and information may not be retained. If we can weave important information into a story, we will have more impactful communication.
For instance, I recall the horrific story about an MRI safety incident that occurred over 20 years ago. An oxygen tank was brought into the scan room while a 6-year-old boy was being scanned. The tank launched into the bore of the magnet and killed the young patient. This event has been used since then to demonstrate the reason for strict MRI safety rules in and around Zone IV. We have signage on the door stating that the magnet is always on and warning of the danger inside, but those signs can be ignored. Especially, if people are distracted.
There are pictures of gurneys, IV poles and the like stuck to a magnet all over the Internet. Nothing gets the point across like sharing the details of this tragedy. Magnets are stronger, scans are faster, expectations for throughput are higher. When creating a workflow for our MRI team, safety must be the number one priority.
We have implemented mock code drills at our offices. This allows our teams to walk through an emergency scenario and think through what they would do. We let them ask questions and give suggestions. We perform a separate drill for MRI, since it has unique challenges. One of the main obstacles is to manage the MRI door while we are working to
quickly remove the patient from Zone IV.
We do a debriefing after each of these drills. We have many sites and each of them has unique layout, different clientele, and personnel with varying levels of experience. We have gotten very positive feedback from our team members, who appreciate the time dedicated to being prepared.
Being that we are ambulatory imaging, we do not have a code team that will be rushing to assist with our emergency. We call 911 and manage the situation until EMS arrives. This can feel like an eternity. Fortunately, these emergencies are not common, but they do happen and we need to be prepared.
By presenting these drills as stories for our teams to role play, we are providing them with details they are more likely to remember than just a list of things to do. Shortly after our first drill, an MRI patient had a seizure during a scan. The team stated they were able to stay calm and take care of the patient quickly and effectively just like they had practiced. They didn’t really do anything they had not done before, but they did not feel as stressed or anxious as they would have.
A story can be used to inspire, empower, express frustration or evoke change. It allows the listener to relate to details being expressed and have a better understanding of how and why something is being communicated. Our team members will have not just heard the story, they have learned from it and will be better able to execute the instruction.
The next story I have been asked to tell is about an outstanding, heartfelt patient experience. I have lots of those. The struggle will be to pick the best one.
Thanks for all you do. •
 BY MARK WATTS PACS/IT/AI
BY MARK WATTS PACS/IT/AI
The patient has not generated urine in three years,” the kidney transplant surgeon shouted into the phone. The patient was living due to the process of blood filtration via dialysis. This interaction with me was caused by my reminding him that radiology technologists have a scope of practice that did not allow them to remove indwelling catheters by policy at our institution.
“Just have the nurse do it!” This leads me to the key point of this article. The nursing scope of practice is broad and in high demand. The embodiment of this foundational participation in the providers of the most “care” in health care are nurses. If your imaging department has good nurses you truly know their value. If one nurse is freed up from tasks that could be performed by a capable level of care-appropriate substitute, that would help humanity.
The health care industry now stands at a crossroads, seeking innovative solutions to address staffing shortages, an inexperienced workforce and issues related to retention. Some estimates put the nursing shortage as high as 400,000 by 2025, greatly jeopardizing patient care and increasing the heavy toll on the nurses who remain in practice.
Virtual nursing, a concept that marries the strengths of traditional nursing models – primary nursing and team nursing – is emerging as a promising solution to address the challenges faced by health care organizations.
In this column, I will delve into the essence of virtual nursing and explore how adopting technology can revolutionize patient care and nursing practices, all while ensuring that nurse leaders are equipped to navigate this transformative journey. Importantly, this model has been shown to enhance nurse and patient satisfaction while improving financial and operational efficiencies for hospitals.
For decades, the nursing profession has predominantly relied on two models: primary nursing and team nursing. Primary
nursing designates a single nurse who assumes the primary responsibility for and coordination of a patient’s care, while team nursing involves a collaborative effort among multiple nurses, including non-licensed personnel. Each model has merits and limitations.
The need for immediate action to lessen the stress felt by nurses is evidenced in a recent study that spotlights the lack of engagement in the profession. The 2023 National Nursing Engagement Report found:
• Less than half of U.S. nurses say they are fully engaged at work.
• Another 14.4% say they are “unengaged.”
• Less than 40% of millennial nurses say they are fully engaged.
Compounding the problem is the heavy toll nurses report, especially those earlier in their careers. The American Nursing Association found about one-third of nurse respondents with less than 10 years of experience indicated being either not or not at all emotionally healthy.
It’s increasingly clear that to solve this problem, we can’t simply rely on replacing people with people – technology must be put in place to offset these shortages and automate tedious tasks that are adding stress and stealing joy from the practice of nursing.
Virtual nursing represents a paradigm shift in the nursing profession, combining the best elements of primary and team nursing to create a novel and effective approach to patient care. It’s a revolutionary concept that has gained significant traction in the health care industry, driven by its ability to provide a satisfying experience for nurses and patients.
Amidst the growing buzz surrounding virtual nursing, various voices and opinions vie for attention. Some claim expertise, while others offer individualized solutions. The noise in the health care arena can be deafening, making it essential to cut through the chatter and focus on the core issues that virtual nursing can address.
Virtual nursing provides a multifaceted solution to a range of pressing challenges. Moreover, virtual nursing programs enable experienced nurses to take on mentorship roles, fostering the professional growth of younger, less-experienced nurses.
Patients, including the elderly, benefit from the personalized one-on-one attention provided by virtual nurses, resulting in fewer incidents requiring higher levels of care and reducing the likelihood of injuries, including fall risk.
To implement virtual nursing effectively, health care leaders must decide on the approach that best suits their organization’s needs, whether that involves establishing a centralized command center focusing nurses on specific tasks or deploying the geographical model of virtual nursing with nurses onsite working both on the unit and in the virtual role. A flexible rotation system can serve as a potent retention tool, providing nurses with the opportunity to experience both primary and virtual nursing roles.
Health care providers – including nurses – can sometimes be slow to adopt new technologies. Clinicians like to see a clear roadmap of how to proceed, accompanied by clearly defined expected outcomes. With virtual nursing and AI platforms, there is no one-size-fits-all manual. We must stress that while outside the box, the customization of care models based on best practices is key to success.
One of the key advantages of virtual nursing is its potential to enhance existing workflows and identify areas where tasks can be reallocated or improved. Nursing leaders should encourage innovation and collaboration among their teams to ensure the program’s success. Involving nursing teams in developing the virtual care model and defining the role of the virtual nurse facilitates engagement.
According to the PRC study, nurses are more likely to be fully engaged if they believe they are active participants in de-
cision-making about their patients’ care and that their opinions are valued by leadership.
It’s crucial to emphasize that virtual nurses are not intended to replace traditional nursing staff but rather to complement and augment their efforts. The successful integration of virtual nursing requires clear collaboration and trust-building.
Virtual nursing offers a transformative path forward for health care organizations facing staffing challenges, retention issues, and the need for improved patient care. Nursing leaders must embrace this innovative approach by proactively seeking solutions and participating in the ongoing conversation about the integration of technology in health care.
While regulations surrounding virtual nursing and AI are expected to evolve, health care leaders should not wait for directives to be imposed upon them. Instead, they should actively engage in discussions to shape the regulatory landscape, removing the mystique surrounding AI and promoting the adoption of best practices and common-sense guidelines.
By committing to transparency, validation, and collaboration, nursing leaders can pave the way for the successful implementation of AI-powered virtual nursing programs, ultimately benefiting patients and the dedicated professionals who provide their care.
The transplant patient was being evaluated for a kidney transplant (he found a match) and an accurate evaluation of his vascular roadmap was part of the journey. During the three years he had not generated urine his bladder had shrunk from nonuse. Having a nurse available to handle these situations is helpful for imaging and is good medicine.
Virtual AI-assisted nursing may be the only way the nurses will be available. •
Mark Watts is an experienced imaging professional who founded an AI company called Zenlike.ai.
 EMOTIONAL INTELLIGENCE
BY DANIEL BOBINSKI
EMOTIONAL INTELLIGENCE
BY DANIEL BOBINSKI
oday, in 2024, Taylor Swift is one of the biggest pop stars in the world. In 2010, Swift was facing intense criticism about her singing voice. What did she do? She hired a vocal coach. People may still criticize her, but her move impacted her pocketbook tremendously. In 2010, Swift was worth $310 million. Today, she’s worth more than $740 million.
Beyoncé is another huge star, and not only did she start working with a voice coach at age 8, she still employs a coach to help her maintain and improve her singing skills.
The late Steve Jobs, founder of Apple, worked with a workplace coach and mentor for years, as did Google co-founder Larry Page. Current Google CEO Sundar Pichai also uses a workplace coach.
If you happen to be the entity running the universe, I’ll go out on a limb to say you don’t need a coach or a mentor. For everyone else, huge benefits abound in such relationships, and I recommend you look into them.
People often use the terms “coach” and “mentor” interchangeably, but distinct differences exist. Frankly, so long as you know what you’re expecting from the person helping you, it doesn’t matter what label you apply, but for our purposes here, let’s define a mentor as someone within your organization that’s been assigned to you. A mentor helps you develop relationships with key people and helps you improve specific skills. The overarching purpose of a mentoring relationship is shortening your learning curve so you can more quickly impact your company’s bottom line.
Mentors are usually more directive and instructive because the goal of a workplace mentor is to bring you up to speed quicker and operate with an organizational
focus.
Conversely, a coach operates with a personal focus. A coach is usually someone you choose to help you grow in areas you want to address, and you often have a say in setting the agenda. Traditionally, a coach works more like Socrates, asking questions to stimulate your critical thinking and facilitating growth in areas that are of interest to you.
Frankly, I’m not so much concerned about which type of relationship you establish or what term you use so long as you know what you want or need.
As an example of the importance of knowing what you want and what you’re getting, the HR manager for a company that makes golf equipment once called me to help address tension on her company’s leadership team. At the initial meeting, a senior vice president challenged my associate with “So, what do you guys know about golf clubs?” Without batting an eye, my associate responded, “Nothing. And we don’t want to know anything about golf clubs. We’re experts in workplace relationships.” The SVP thought we would be telling them how to make better golf equipment. Once he understood our role, things went fine.
Regardless of whether you get a coach or a mentor, benefits are abundant. Let’s explore some ways these relationships can help you.
1 . You’ll gain clarity. Perhaps you’ve heard the expression that you’re too close to something to see it? Take your chin, for example. It’s part of who you are, but you can’t see it without a mirror. Having another person point out that you’ve got a dab of whipped cream on your chin is quite helpful. Similarly, having someone provide an objective perspective on what they observe about you will be valuable information for becoming more effective.
2. You’ll have accountability. It’s too easy to put
personal or professional growth on the back burner, mainly because you rarely have a deadline for it. Because of that, being accountable to yourself for growth is not impossible, but it can be quite difficult. Having someone to whom you’re accountable helps you stay on track with those personal and professional development action items that are important, but rarely urgent.
3. Your growth map is custom tailored to you. You can – and should – read books and attend workshops on personal and professional development, but they will always be designed for the middle of the bell curve. In coaching and mentoring relationships, everything is customized to meet your individual needs. The extreme value of one-on-one dialog simply can’t happen in a workshop or by reading a book.
Here are some tips for getting the most from any personal or professional improvement endeavor you undertake.
First, be brutally honest. Not just with yourself, but with your mentor or coach. Our human nature tries to cover up weaknesses (what I call blind spots) so we can present ourselves in the best possible light. That’s good advice for companies building brand loyalty, but bad advice when you’re an individual trying to better yourself. You don’t go to a doctor for your annual checkup and say everything is fine when you know it’s not. If you want something to be better, you must be forthcoming
about it. A good coach or mentor knows how to create what I call an “emotionally safe environment,” allowing you to explore sensitive issues without condemnation.
Second, make personal or professional development a high priority. Going through the motions gets you nothing, because you’ll always get out of life what you put into it. Think of it this way: If you’re digging into a pile of gold, the more energy you use pushing down on the shovel, the more gold you’ll get on the shovel.
Third, expect change to take time. You’ve succeeded in the workplace all these years using techniques you picked up along the way, even if those techniques have left damage in your wake. Becoming a better leader often means changing the way you do things, and frankly, an aircraft carrier moving at high speed does not turn on a dime. Put forth the effort, but know improvements don’t happen overnight.
On a final note, if you hire someone to help you, choose to be serious about your growth. It pays off. One doctor I know who invested in himself and hired a coach said it was the best money he ever spent. •
Daniel Bobinski is author of the best-selling book, “Creating Passion-Driven Teams,” and president of Leadership Development, Inc. He’s been helping organizations of all shapes and sizes since 1989. Learn more at www. eqfactor.net or reach Daniel at 208-649-6400


Iheard someone say, “What does not kill you makes you stronger” and wondered exactly what that means and who first said it. Internet here I come to research it to death. Wait, what if it does kill me? I will not then be able to bore you with this column. Let’s see if it does in fact make me stronger.
First, this saying is apparently a modification of a quote from Friedrich Nietzsche, the late 19th century German philosopher. From my “research,” the actual quote is, “Out of life’s school of war: What does not destroy me, makes me stronger.” Although the difference may be slight, in my mind “kill” and “destroy” imply divergent paths. The intent may be that life’s slings and arrows, things that happen to us that may not be our fault, may actually improve our resilience. Even if they are our fault, resilience can be enhanced by each event.
So, what is resilience? According to apa.org, “Resilience is the process and outcome of successfully adapting to difficult or challenging life experiences, especially through mental, emotional, and behavioral flexibility and adjustment to external and internal demands.” Resilience reminds me of a quote from Stephen R. Covey, the author of “7 Habits of Highly Effective People.” He wrote, “It’s not what happens to us, but our response to what happens to us that hurts us.” So, we have response ability, we can choose how we respond to people and things.
Every day we successfully react, respond, accept, and reject, etc., incoming issues and challenges, maybe without conscious thought. The actions we take and internalize change us and prepare us for similar future events. We are improving our resilience.
So … resilience can and is learned, just like good communication and any other life skill. It is a product
of experiences and practice. Can we take steps to improve resilience other than by experience?
According to research, resilience is influenced by mental, emotional, behavioral flexibility, and how we view and engage with the world. Unless I have this all wrong, all this stuff so far is talking about our attitude, and attitude is mostly a choice. We can wake up and go forth looking for problems and to be offended; or we can go forth looking for ways to be happy and to be effective in dealing with the challenges and people we encounter. Having a well-defined value system goes a long way in dealing with these types of challenges.
But … what about those events that come close to destroying us? The tough ones are the physical events such as a deforming accident or emotional events such as the death of a loved one (which itself can be physically debilitating). These compel us toward the realization and eventually acceptance that we can never go back to normal. We can only move forward to a changed normal. The pain caused by the event may never fully dissolve, however through resilience we can evolve within the pain.
Another quote from Friedrich Nietzsche: “To live is to suffer, to survive is to find some meaning in the suffering.” Survival is the strength part of the quote from above. We can accept to be destroyed, or find meaning and strength in accepting what cannot be changed. You should only fight what can be changed and has meaning to you.
Wow, that’s all depressing stuff! However, I am stronger for the experience of the research and the attempt to make sense in the writing. You will be stronger by the experience of surviving to the end. •
Manny Roman, CRES, is association business operations manager at Association of Medical Service Providers.
MANNY ROMAN, CRES





When life, or the people in your life, push your limits, the emotional load may feel insurmountable. Making sense of the chaos in your life can allow you to rediscover peace and joy, but circumstances like a crisis can complicate the process of emotional healing.
“Almost nobody is trained on what to do with their emotions in times of crisis and stress, and most of us are never taught how to manage our emotions in normal times,” said Eric Paskel, who holds a master’s degree in clinical psychology and is a licensed marriage, family and child therapist. “If you’ve ever admired someone who was cool under pressure then you know it’s possible to emotionally survive, and even thrive, in a crisis.”
Paskel, an author and motivational speaker, has spent 34 years exploring how human beings can rise above their dysfunctional tendencies and control their emotions. He has developed a series of resources to help individuals prevent their emotions from owning them in a crisis, allow people to do more observing and less reacting and take decisive actions to help themselves and their loved ones.
Learn how to take charge of your emotional health with these practical and effective tips, adapted from Paskel’s Emotional Survival Kit, a free online video course on personal crisis management.
During a crisis is when personal growth is most possible. During adversity and crisis, there are always lessons to be learned and shared. Sometimes growth comes as the result of overcoming the pain of a crisis, but there are other sources of growth.
To accelerate your growth, begin by recognizing you need help then be willing to accept that help. It may come in the form of advice from a professional or it may be simply listening to the perspective of others with similar experiences.
A simple change in perspective like a crisis or a forced change, such as having to work from home, is both a challenge and an opportunity, although the challenges and benefits will likely be different for each individual person.
Some people will benefit from the isolation, which they’ll see as solitude. Some will be challenged by a noisy home while others will be thrilled to have the company of family or roommates all day. The key is to find a way to turn those challenges into gold.
Begin by identifying your challenges. Then find the silver lining. What are the benefits that come with these challenges? It may be that your rigorous travel schedule allows more time at home or that you’ve been able to tackle a long-standing list of lower-priority tasks. Then choose to focus on the positive and find ways to adapt to

1. Participants in the reverse expo made valuable connections.
2. Greg Bennick’s keynote address “Build a Better Now” awed those in attendance as he performed magic and juggled items while delivering an inspiring message. The keynote was sponsored by Equips.
Martha Sandoval
ICE
RSTI’s
6. An ICE attendee demos a piece of equipment at the Universal Diagnostic Solutions Inc. booth inside the exhibit hall.
7. ICE 2024 was filled with education, networking and fun! Several attendees enjoyed the balloon-filled “igloo” near the registration desk.
8. The ICE 10th Anniversary Party was very popular with exhibitors and attendees.
9. Alain Lengue from MultiMedical Systems is seen with Marshall Misouria from Rocky Mountain Regional VA Medical Center at the 2024 Imaging Conference & Expo in Irvine, California.
ICE























ICE Magazine connects with industry leaders to provide top-quality educational opportunities through its monthly webinar series


