Leading Change in the Nursing Profession











The latest breakthrough in enzymatic pre-cleaning sprays, Prepzyme® Forever Wet’s unique humectant properties form a moist coating over the instruments that lasts for days.

•The humectant formulation creates a moisture retention barrier which keeps soiled instruments and scopes moist for a prolonged period of time – unlike a GEL which HAS NO MOISTURE RETENTION properties
•Operating room safe, non-aerosol, multi-tiered enzymatic spray helps prevent bio-burden from drying on the surface of soiled instruments and scopes
•Ideal for transporting soiled instruments that may sit for an extended period of time
•Reduces tray weight during transport compared to liquid presoaks
•Soiled sharps are visible through humectant
• Decreases spills and potential cross-contamination













When the ultrasonic cleaner is supplying sufficient energy and condi�ons are correct, SonoCheck™ will change color. Problems such as insufficient energy, overloading, water level, improper temperature and degassing will increase the �me needed for the color change. In the case of major problems the SonoCheck™ will not change color at all.
Reveal the hidden areas of instruments with TOSI® - the easy to use blood soil device that directly correlates to the cleaning challenge of surgical instruments. TOSI® is the first device to provide a consistent, repeatable, and reliable method for evalua�ng the cleaning effec�veness of the automated instrument washer.
The LumCheck™ is designed as an independent check on the cleaning performance of pulse-flow lumen washers. Embedded on the stainless steel plate is a specially formulated blood soil which includes the toughest components of blood to clean.
Go beyond what you can see with all-in-one detec�on kits for blood or protein residue. HemoCheck™ is simple to interpret and indicates blood residue down to 0.1μg. The ProChek-II™ measures for residual protein on surfaces down to 0.1μg.






PUBLISHER
John M. Krieg john@mdpublishing.com
VICE PRESIDENT
Kristin Leavoy kristin@mdpublishing.com
VICE PRESIDENT OF SALES
Jayme McKelvey jayme@mdpublishing.com
EDITOR
John Wallace editor@mdpublishing.com
ART DEPARTMENT
Karlee Gower
Taylor Hayes
Kameryn King
ACCOUNT EXECUTIVES
Megan Cabot
Emily Hise
DIGITAL SERVICES
Cindy Galindo
Kennedy Krieg
EVENTS
Kristin Leavoy
ACCOUNTING
Diane Costea
WEBINARS
Linda Hasluem
EDITORIAL BOARD
Vangie Dennis, MSN, RN, CNOR, CMLSO Assistant Vice President, Perioperative Services, AnMed
Justin Fontenot, DNP, RN, NEA-BC, FAADN Associate Professor, Tulane University School of Medicine, New Orleans, LA
Natalie Lind, Education Director for the Healthcare Sterile Processing Association, HSPA
Pat Thornton, MSM, RN, CNOR Perioperative Consultant, RNFA Dermatology Institute
Dawn Whiteside, DNP, MSN, RN, CNOR, NPD-BC, RNFA, Director of Education, CCI
Julie Williamson, BA Director of Communications, HSPA



Getinge’s Servo ventilators received a boost into the future. With the launch of Servo TwinView, medical teams can access and analyze near real-time data from the ventilators, without having to step inside the sensitive environment in the intensive care unit (ICU).
As the health care sector strains with increasing demands and evolving challenges, the need for innovative digital solutions is growing more than ever, offering scalable and efficient ways to enhance patient care. Global medtech company Getinge continues to place a high priority on developing and providing cutting-edge digital solutions, as well as adding digital capabilities to existing products, to meet the complexities of the modern health care landscape.
“We are constantly working on expanding our offering of digital solutions to support and enhance high acuity care workflows,” says Elin Frostehav, President Acute Care Therapies at Getinge. “Our latest innovation, Servo TwinView, is a virtual twin to our renown ventilators, and first to benefit from it are the Servou and Servo-n models. Servo TwinView provides medical staff with near real-time view of the data displayed on the ventilator screen, without having to access the actual ventilator in the ICU.”
While viewing the ventilator data remotely, experts can provide a second opinion and support the staff who are working inside the ICU.
“The ICU is a sensitive environment with patients that are often critically ill, recovering from major surgeries, experiencing organ failure, severe trauma, or facing other complex medical issues. Servo TwinView opens the possibility to follow therapies without disturbing these patients and their relatives, explains Cecilia Sjöstedt, Vice President Critical Care at Getinge. “It enables hospitals to increase effectiveness of daily routines such as rounding and handover, supporting onboarding and training away from the patient room, potentially improving workflow and thereby freeing up time and costly clinical resources.”
An extensive prestudy, including end-user involvement, provided Getinge with valuable input in the development of the Servo TwinView. Substantial focus was spent to ensure that sharing of information was made easy and to enable colleagues to view and analyze the data on computers, smart phones, and tablets, in a secure way.
“This virtual twin of the physical ventilator is connected via Wi-Fi and the data is handled according to the individual hospital’s policies. We have put a lot of efforts into optimizing cyber security for this solution,” says Elin. “We hope Servo TwinView will become a great tool for many hospitals around the world, assisting them in their digital transformation journeys.”
The Accreditation Association for Ambulatory Health Care (AAAHC) releases its Certification Handbook for Advanced Orthopaedics (AOC), v43. Leveraging the previously released handbook updates to the Ambulatory Accreditation (AMB) and Medicare Deemed Status (MDS) accreditation programs, the new edition provides the most current information and guidance for surgery centers seeking to demonstrate their commitment to ongoing quality improvement and industry best practices in orthopaedic surgery.
The three-year specialty AOC program, originally launched in 2018, focuses on patient outcomes and aligns seamlessly with the AAAHC Certificate of Accreditation for Ambulatory or Medicare Deemed Status program. An expert panel of professionals in orthopaedic and complex spine procedures created the AOC program to provide a comprehensive focus on transitions of care from pre-assessment through discharge and rehabilitation. Organizations may seek certification for total joint, complex spine, or a combination of both services.
Like the latest v43 handbooks, the updates reflect and integrate 1095 Engage, AAAHC’s new Accreditation Management System (AMS) into the program with AOC Standards organized by Category, and each Category groups similar concepts to facilitate compliance.
“Ambulatory surgery organizations already accredited by AAAHC will realize additional benefits with the AAAHC AOC program,” said Noel Adachi, MBA, president and CEO of AAAHC. “AOC elevates the status of organizations having a dedicated core team of clinicians with an expertise in orthopaedics. Through an assessment of evidence-based clinical practice Standards and guidelines, ultimately, the AOC program assesses an organizational infrastructure that promotes excellence.”
Changes from previous Advanced Orthopaedic Certification Standards include guidance to support understanding of community needs assessment, as well as clarification of on-call physicians and examples of training hours. For ease of review and implementation, the v43 handbook contains a crosswalk identifying all changes from the previous versions.
“Committed to advancing health care, AAAHC remains dedicated to updating our resources with the latest industry best practices, ensuring organizations are prepared for surveys on a daily basis,” said David Shapiro, MD, Immediate Past Board Chair for AAAHC. “Whether providers are seeking accreditation to meet regulatory obligations or using it as a mechanism to enhance organizational performance and quality, the new handbooks feature expert-guided updates in our Standards, serving as a pertinent resource for your quality improvement journey.”
AAAHC released an educational webinar entitled Your Successful Transition to AAAHC v43 Standards on February 5 that is specifically designed for organizations currently participating in the AAAHC Advanced Orthopaedic Certification program or those seeking this certification. The goals of this webinar are to increase awareness and help facilities align their survey preparation and ongoing compliance activities with the newly developed Standards. Standards included in v43 will take effect April 3.
For more information, visit www.aaahc.org.
Surgeons who routinely change surgical gloves and instruments are incurring similar costs to those using the same equipment, a new study has found.
The economic evaluation funded by the UK’s National Institute for Health and Care Research (NIHR) follows a clinical trial conducted at 80 hospitals in Benin, Ghana, India, Mexico, Nigeria, Rwanda, and South Africa which established that routine change of gloves and instruments reduces surgical site infections (SSIs) by 13%.
The evaluation, published by the Lancet Global Health, serves as a follow-up to a clinical trial to assess the economic implications of implementing the findings from the trial. It compares the costs and SSIs associated with routine change of gloves and instruments versus current surgical practice of not changing them.
Among the seven low- and middle-income countries that took part in the ChEETAh clinical trial, the economic evaluation calculated that on average the cost of the intervention of $259.92 compared with $261.10 for current practice of reusing gloves and instruments.
Lead author Mwayi Kachapila, a health economist from the University of Birmingham, said, “It is very important for health care programs to be both effective and cost-effective. SSIs are associated with high treatment costs especially in low- and middle-income countries (LMICs) and this intervention will go a long way to reduce the cost burden to patients, health care systems and societies. Lowering SSIs not only minimizes patient recovery time but also significantly alleviates financial burdens, especially in LMICs where patients often bear the cost of their treatment. Additionally, this initiative aids in freeing up hospital bed space.”

Seventy years after North Shore University Hospital (NSUH) first opened its doors, the Level I trauma center and quaternary care teaching hospital today announced the completion of the Petrocelli Surgical Pavilion, a landmark decades-long project that will transform health care in the region. The $560 million, 288,000-squarefoot tower will complement nationally recognized cardiac, neurosurgery and transplant programs.
This investment by Northwell Health, New York State’s largest health care provider, represents one of the most significant projects of its kind in the New York Metro area and is an affirmation of its commitment to the communities that it serves. About 40 percent of all patients at NSUH come from Queens while another 5 percent travel more than 100 miles to seek care there.
“This is a proud moment for health care in the region. The Petrocelli Surgical Pavilion has been part of Northwell Health’s master plan for more than a decade,” said Michael Dowling, president and CEO of Northwell. “It took guile and determination to see this massive project through to completion. It took the belief of so many Town, County and State officials, along with the vision of countless donors, to help make it a reality. I want to personally thank everyone who made this investment in the health and longevity of New Yorkers possible. It is a true achievement.”
New York-based Skanska USA broke ground on the
capital project in April 2020, which was made possible, in part, through a significant gift from Attilio and Beverly Petrocelli.
The Petrocelli Pavilion will feature 18 operating rooms (ORs), including three hybrid rooms with advanced imaging, along with 132 intensive care rooms (ICUs). Hybrid ORs combine a traditional OR with an image-guided interventional suite, allowing for highly complex, advanced surgical procedures. This project will upgrade and expand the critical care capabilities of NSUH to ensure ever more exceptional care. Following a period of intensive staff training in the new surgical tower, patients will relocate to new critical care units and surgeries will begin later this month.
“What this surgical tower does is unlock the full potential and resources of New York’s largest health system to provide the most complex care possible to Long Island and New York City residents,” said Jon Sendach, executive director of NSUH and deputy regional executive director of Northwell’s Central Region. “North Shore University Hospital has made tremendous strides from its roots as a small community hospital. The North Shore team was already performing at a high level; we were only constrained by space. Now our world-class medical experts have state-of-the-art ORs and ICUs to do even more.”
For
Advances in healthcare technology continue to drive patient monitoring technology into the future; however, alarm sounds have remained similar, if not unchanged, for many years. Until now. Royal Philips, has received 510(k) clearance for its latest IntelliVue patient monitor software, which features the longanticipated availability of several new solutions, including the award-winning Philips Sounds alarm package, making it available in the USA and more than 200 countries worldwide.
Noise in hospitals can impact the quality of life and health of patients, their families and their care providers. In the average ICU, patient monitors account for up to 82% of alarm tones with up to 350 alarms per patient every day. While alarms function to gain attention, over time the sheer number of them can wear down caregivers and contribute to the anxiety of patients and their families. To help drive alarm management strategies toward a more peaceful, healing environment for patients and caregivers alike, Philips has applied a fresh perspective to acute patient monitor alarm sounds by collaborating with clinicians and world-leading sound experts.
“While alarms in acute care settings must be effective, they
should be sensible, informative, and respectful of the surrounding environment and the people in it,” says Christoph Pedain, business leader, hospital patient monitoring, Philips. “Throughout the process, we asked for input from care providers, administrators, patients and their families who are exposed to these alarms regularly and leveraged powerful data to help improve the experience overall.”
The IntelliVue alarm evolution involved a significant research investment to capture and implement input from care providers and patients in alarm-heavy environments. Together, Philips and the sound design group SenSound worked to soften and round the alarm tones and adjust alarm intervals to more gently signal status or request action using a more soothing – yet still impactful – set of alarm sounds. These changes are designed to help improve the patient and caregiver experience. Philips’ new patient monitoring sounds have been proven to reduce alarm noise by up to 66 percent.
Additional noteworthy capabilities within the new IntelliVue software update, including Philips Visual Patient Avatar, are now available in the USA and more than 200 countries worldwide.

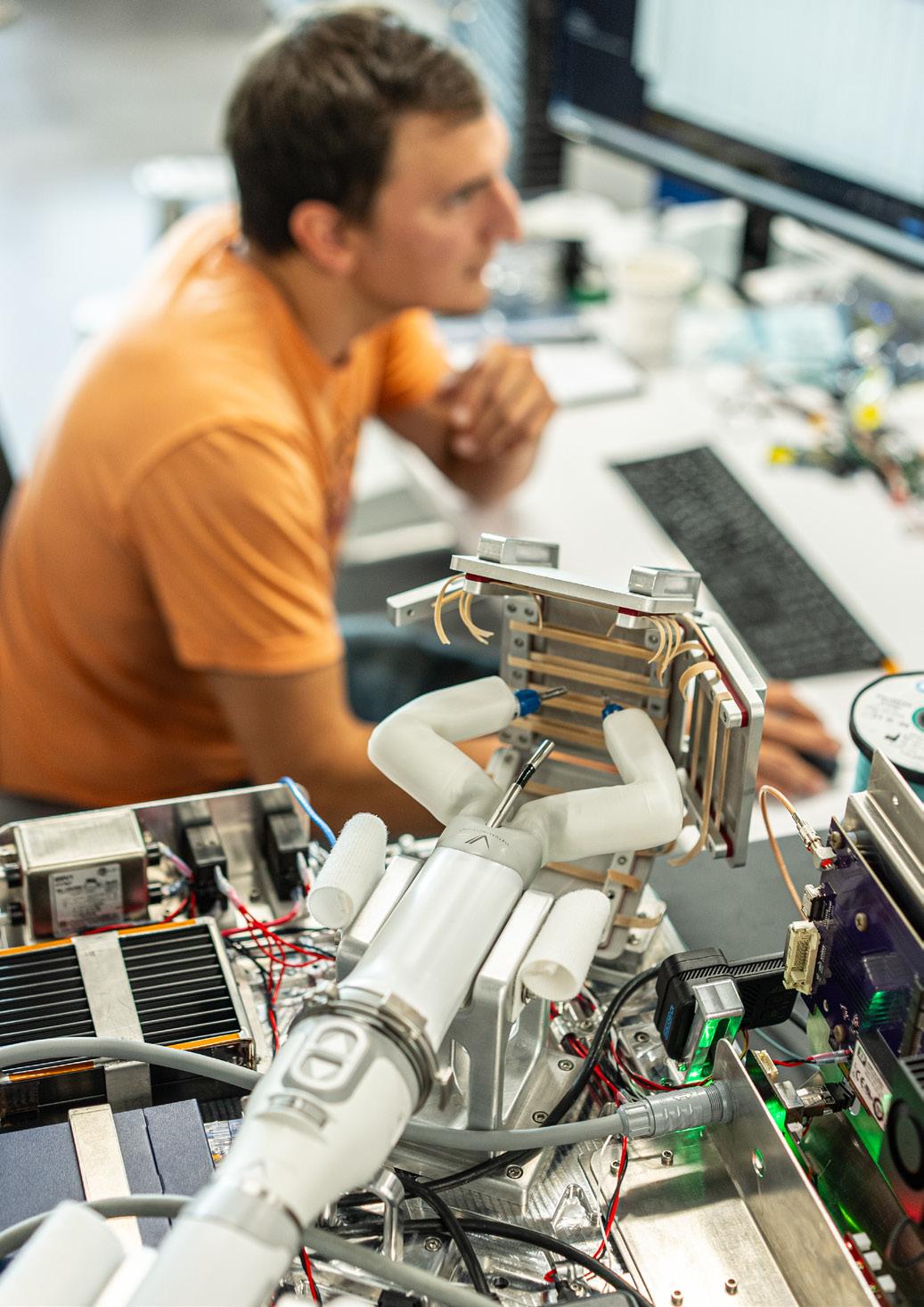
Virtual Incision Corporation, the developer of the MIRA Surgical System (MIRA), has announced that spaceMIRA is currently in transit to the International Space Station. The device is aboard a Northrop Grumman Cygnus cargo spacecraft carried by a SpaceX Falcon 9 rocket. The 2024 technology demonstration mission is driven by a grant awarded from the National Aeronautics and Space Administration (NASA) to the University of Nebraska through the Established Program to Competitive Research (EPSCoR) program.
Testing with spaceMIRA on the International Space Station will assess the impact of zero gravity when performing simulated surgical tasks. During a portion of the experiment, a surgeon operator at Virtual Incision’s headquarters in Lincoln, Nebraska, will utilize remote-controlled technology to direct the movements of the robot.
Learnings about remote surgery could potentially impact health care in space and across the globe. In the U.S. alone, one-third of counties do not currently have access to a local surgeon,1 and the shortage of surgeons could rise to more than 30,000 within the next 10 years.2 Remote surgery could serve as an option for these patients by enabling procedures to be performed from a distant location
The ideal device for these applications would be controlled by a surgeon through a console, enabling them to direct the movements of a camera and instruments inside a patient’s body. This type of technology, called robotic-assisted surgery (RAS), has been available for decades. While some exploratory work in remote surgery has been conducted, it is still typically performed with the surgeon in the same operating room as the patient.3 Although there are many complexities associated with remote operations, miniaturization of RAS could be a breakthrough by dramatically simplifying workflows at the site where the patient is located.
MIRA, the first miniaturized robotic-assisted surgery (miniRAS) device in development, is roughly 1,000 times lighter than existing technologies. As the only small form factor RAS device, it has the potential to make remote surgery more feasible by enabling transportation, storage, and setup time at an unprecedented scale. The University of Nebraska researchers leveraged MIRA’s unique design to create an iteration that enables pre-programmed as well as long-distance remote surgery operation modes.
“When we started this work at the University of Nebraska, we shared a collective vision that miniRAS could make robotic-assisted surgery available to any
patient, anytime, anywhere,” said Shane Farritor, Ph.D., co-founder and chief technology officer at Virtual Incision and professor of mechanical engineering at the University of Nebraska. “Exploring the use of miniRAS in extreme environments helps our teams understand how we can remove barriers for patients.”
“As thrilling as it is to have our technology in space, we expect the impact of this research will be most notable on Earth,” said John Murphy, president and CEO of Virtual Incision. “The introduction of miniRAS has the potential to revolutionize health care by making every operating room robot ready. We are taking a significant step by developing MIRA, an investigational device currently under review by the FDA. The testing with spaceMIRA will tell us more about the future potential of miniRAS as it might be applied to remote surgery applications.”
Apella, a health technology company, has announced an expanded collaboration to implement the company’s technology in all operating rooms across Houston Methodist.
Powered by ambient sensor technology and artificial intelligence, Apella provides new data and insights in real time to help surgical teams analyze the past, manage the present, and plan for the future. This increased efficiency ultimately allows for increased surgical volume and improves the quality of surgical services.
“Ambient technology is extremely important in shaping the way that we deliver care to our patients,” said Roberta Schwartz, executive vice president and chief innovation officer at Houston Methodist. “The data generated shows valuable insights that have al -
lowed for increased surgical volume in our operating rooms, helping us run our ORs more efficiently and enhance the overall patient experience.”
“Operating rooms are run in real time. Apella makes the operations in a surgical suite more efficient so that staff can focus on what really matters,” said David Schummers, CEO of Apella.
Houston Methodist is a leading health system in the U.S., with 3,265 beds and over 200 operating rooms (ORs). After beginning a successful pilot program in early 2023, Houston Methodist is expanding the program across all ORs and anesthesia locations in its system. With Apella, Houston Methodist has a 360-degree view of all operating rooms at once.












I recently had the opportunity to speak with long-time colleague Peter Graves. He is well known in perioperative nursing. He has worked extensively in health care associated industries. He also has experience in surgery research. Pete shared that he had recently been part of a team which had published, “A Review of the Evidence on the Role of Floors and Shoes in the Dissemination of Pathogens in a Healthcare Setting.” Our brief discussion spurred me to author this column. I would like to offer two thoughts which came to me after this conversation.
The first thought is that our specialty of perioperative nursing has many opportunities for further research. Consistent with current trends in nursing education, we have more nurses pursuing Doctor of Nursing Practice (DNP) degrees versus the researchfocused Ph.D. degree. “The Nursing Workforce Fact Sheet” from the American Association of Colleges of Nursing (AACN, 2023) informs us that as of 2022, “… 17.4% of … registered nurses held a master’s degree and 2.7% held a doctoral degree as their highest educational preparation.”
We do not have reliable data on the numbers of Ph.D.s in the perioperative specialty. I do feel confident in stating that we have less than what is needed to meet the opportunity for perioperative-related research. This brings me to the second main point of this article. While Ph.D.s may be needed on research teams, there are many opportunities for perioperative nurses to participate in research. A case in point is Peter’s career; his highest earned degree is a Bachelor of Science, and he has been a notable contributor to the advancement of surgery-related research. Our perioperative specialty can do much more in research. Our perspective is valuable and not all researchers need to be prepared at the doctoral level.
The reference citation for the article in which Pete was part of the team of authors follows below. This
literature review was published in the journal Surgical Infections. This points out the value of literature review articles in establishing the body of knowledge for surgical care and perioperative nursing, but also highlights the diversity of journals which may be suitable for perioperative-related articles. Not all journals are research centric as some are written for a broader audience. Perioperative nurse authors have many options. In the reference list, I document some of the recent journals which have published perioperative nursing content to include original research.
In example, the Journal of Perianesthesia Nursing (JOPAN) frequently publishes original research, and the editors are receptive to perioperative content. With a previous employer, I had the opportunity to write on professional development topics which are well-suited for the Journal of Continuing Education in Nursing. The International Journal of Nursing Studies is one of the top rated nursing journals in the world and they also publish perioperative research. A case in point is the work of the Australian researcher Brigid Gillespie with her publications on the PPCS-R instrument used specifically in perioperative nursing competency assessment. These are four suggestions for journals suitable for perioperative nursing content.
Perioperative nurses can also contribute to research efforts with volunteer service as a reviewer. I have volunteered in that service for the publication Perioperative Care and Operating Room Management (PCORM). This is an international, multidisciplinary journal which welcomes original research articles. My take home message is that there are many opportunities in perioperative nursing research and in publishing. If you, like my colleague Peter Graves, are motivated for this type of work I hope that you find the thoughts and suggestions I have presented this month to be useful.
To learn more about these updated guidance documents and other AORN guidelines for perioperative practice, visit https://aornguidelines.org/ guidelines?bookid=2260.
– James X. Stobinski, Ph.D., RN, CNOR, CNAMB(E), CSSM(E), is the director of education with the National Institute of First Assisting.
References
• American Association of Colleges of Nursing. (2023). Nursing Workforce Fact Sheet. https://www.aacnnursing. org/news-data/fact-sheets/nursing-workforce-fact-sheet
• Cramer, E, Stucky, C, Stobinski, JX, Wymer, J. & Boyle, D. (2022). Differences in Perioperative Nurse Job Satisfaction by Specialty Certification Status. Journal of Perianesthesia Nursing (JOPAN). DOI: 10.1016/j.jopan.2022.04.018
• Kinlaw, T., Stobinski, J.X. & Dunn, D. (2023). Using Innovation in Credentialing to Foster Meaningful Transitions to Practice and Support Continuing Professional Development. Journal of Continuing Education in Nursing. 54(9):413-420. doi: 10.3928/00220124-20230816-18. Epub 2023 Sep 1.
• Limper, H. M., Sier, A., Warye, K., Spencer, M., Graves, P., & Edmiston, C. E. (2024). A Review of the Evidence on the Role of Floors and Shoes in the Dissemination of Pathogens in a Healthcare Setting. Surgical Infections, 25(1), 46–55. https://doi.org/10.1089/sur.2023.194
• Maio, S. Stobinski, JX, & Brigid M. Gillespie, BM (2023). Psychometric evaluation of the United States-adapted Perceived Perioperative Competence Scale-Revised: A national survey, International Journal of Nursing Studies Advances, doi: https://doi.org/10.1016/j.ijnsa.2023.100173







A community hospital patient preparing for elective orthopedic surgery was seen in the perioperative clinic. The pre-anesthesia evaluation with evidencebased treatment protocols included EKG testing and high sensitivity troponin labs based on the patient’s history and presentation. Test results were abnormal and warranted immediate action. Rather than the elective procedure, the patient was admitted for urgently needed open heart surgery.
An ASC included the STOP-Bang questionnaire in its pre-anesthesia evaluation to identify cases with undiagnosed obstructive sleep apnea (OSA). The anesthesia team refines its treatment and post-procedure monitoring plan for every patient with positive screening.¹
A pre-anesthesia evaluation is a CMS requirement for hospitals (at CFR §482.52(b)(1)) and ambulatory surgery centers (at CFR §416.42(a)(1)(ii)).
Specific requirements dictate who can complete the evaluation, when it must be completed, and what elements must be included. Hospitals and ASCs have the opportunity to go beyond meeting the
technical aspects of these requirements; they can use what is required as a springboard for a comprehensive, standardized approach to completing an evaluation of each pre-surgical patient that effectively manages risk for the patient and the organization.
Organizations that embrace both the letter and the spirit of the pre-anesthesia evaluation are doing more than complying with regulatory expectations. They are demonstrating a proactive culture of safety.
Some components of the assessment may be completed up to 30 days before the scheduled surgery. These elements must be reviewed and updated within 48 hours of the procedure, but the extended 30-day window of time affords the anesthesiologist, the proceduralist, and other members of the care team time to complete a thorough evaluation of the patient. Evidence-based risk assessment tools (like STOP-Bang) are widely available and can be included to further stratify overall perioperative risk of morbidity and mortality. As an accreditation organization, ACHC encourages clients to develop standardized assessment processes that include review of cardiac, respiratory and endocrine risks. The 30-day window allows for:
• Notation of anesthesia risk according to established standards of practice (e.g., ASA classification of risk).
• Identification of potential problems related to anesthesia administration, particularly those that may suggest a risk of complications or contraindications to the planned procedure (e.g., difficult airway, ongoing infection, limited intravascular access).
• Gathering and analyzing additional relevant data or information, as required by standard practice for anesthesia or organizational policy (e.g., stress tests, additional specialist consultation).
• Development of an individualized plan of care, including the type of medications used for induction, maintenance, and post-operative care.
• Meaningful discussion with the patient (or their representative) about the risks and benefits of anesthesia, using simple language in the patient’s preferred language.
Other opportunities include assessment of: cardiac risk, frailty, allergies and complicated medication regimes that may include anti-coagulants, blood pressure medications and insulin.² Risk stratification and standardized processes allow for appropriate recommendations for
additional testing such as a 12-Lead EKG and lab tests.³ During an early assessment, providers may learn that their patient has a cardiac history, but hasn’t followed-up with their cardiologist in years. Other patients with a history of diabetes may be identified as having elevated hemoglobin A1C indicating poor glucose control. These findings present opportunities for the anesthesia team to request additional evaluation by the specialists who manage these shared patients.
This approach to a comprehensive evaluation allows the anesthesiologist and their team an in-depth understanding of each patient’s overall health status and the opportunity to mitigate risk through pre-operative optimization and anesthesia plans that are tailored to each patient and their health status.
Then, because things change, another pre-anesthesia evaluation must be completed within 48 hours of the procedure. Elements that must be performed within this time frame include:
• A review of the patient’s medical history, including anesthesia and drug or material allergies or reactions.
An interview and examination of the patient, if possible, given the patient’s condition. 4
Once the patient assessment is complete, issues identified must be addressed. Outdated evaluations for critical health conditions must be considered. Many anesthesia teams manage perioperative clinics in which the surgeons or proceduralists defer the management of pre-procedural optimization to the clinic/anesthesia department.
This partnership approach supports standardization of the process and helps prevent confusion when multiple providers or departments are attempting to coordinate the clearance process. Under this structure, abnormal test results and outdated health assessments are identified and follow-up is coordinated through a central resource. Additional testing or other actions on abnormal results may lead to delays in the scheduled procedure date; coordinating further appointments and testing is not always feasible in a short period of time.
Finally, be sure to document updates to the status of the pre-anesthesia evaluation in the medical record. Documentation is always critical but especially important when information regarding test results and communication from providers is returned from a range of sources at different times. Coordination to verify all outstanding results and other pre-operative communications are accounted for ensures that no outstanding results are missed. Anesthesia should review all new results as part of the pre-anesthesia evaluation and incorporate them into the treatment plan.
Through the pre-anesthesia evaluation, the team managing the process has communicated with all key stakeholders, collaborated with the patient’s community-based physicians, and coordinated necessary testing and treatment plans.
Communicate the anesthesia plan to the surgeon and the patient. “Patient” education includes a patient’s support person and is ideally started well before the procedure
date with specific instructions to be followed prior to and after the procedure. Instructions, especially related to medications, should be reiterated multiple times and in verbal and written formats as opposed to being new information at the time of consent and discharge.
Yes, the pre-anesthesia evaluation is a requirement. It is clear, though, that organizations can approach it as a task list or look at it as a requirement that tremendously enhances patient safety. When embraced, the pre-anesthesia evaluation can optimize patient safety and improve outcomes for patients during the perioperative period.
Joshi GP, Ankichetty SP, Gan TJ, Chung F. Society for Ambulatory Anesthesia consensus statement on preoperative selection of adult patients with obstructive sleep apneascheduled for ambulatory surgery.
¹ Anesth Analg. 2012 Nov;115(5):1060-8. doi: 10.1213/ ANE.0b013e318269cfd7. Epub 2012 Aug 10. PMID: 22886843.
² Makary MA, Segev DL, Pronovost PJ, Syin D, Bandeen-Roche K, Patel P, Takenaga R, Devgan L, Holzmueller CG, Tian J, Fried LP. Frailty as a predictor of surgical outcomes in older patients. J Am Coll Surg. 2010 Jun;210(6):901-8. doi: 10.1016/j.jamcollsurg.2010.01.028. Epub 2010 Apr 28. PMID: 20510798.
³ Practice Advisory for Preanesthesia Evaluation: An Updated Report by the American Society of Anesthesiologists Task Force on Preanesthesia Evaluation. Anesthesiology 2012; 116:522–538 doi: https://doi.org/10.1097/ ALN.0b013e31823c1067
4 https://www.cms.gov/regulationsand-guidance/guidance/manuals/downloads/som107ap_a_hospitals.pdf















The Association of periOperative Registered Nurses (AORN) updated its “Guideline on Team Communications” and “Guideline for Safe Environment of Care,” both of which feature numerous recommendations that affect Sterile Processing (SP) areas and functions.
One noteworthy addition to the “Guideline on Team Communications” is the recommendation to establish an environment that promotes resiliency for the work environment and team members. Resiliency enables an individual or complex system to dynamically respond to unanticipated distractions, interruptions and disturbances to maintain a safe environment under conditions that could lead to failure. This description suits dynamic work in health care environments, such as surgery and the sterile processing department (SPD) where there are frequently unanticipated distractions, interruptions and disturbances. Some system factors can also enhance or promote resiliency in the surgical environment, which could improve employee capabilities and system performance. In surgery, for example, resiliency presents itself with the use of skills coaching to prompt team members about tasks to be completed, optimize workspace design and room setup for efficient positioning of people and equipment, and accurately use standardized communication tools such as “time out” protocols. In the SPD, resiliency can be practiced by standardizing workspaces and shift reports.
The “Guideline for Safe Environments of Care” provides recommendations for maintaining a safe environment of care for patients and perioperative personnel, including those working in SPDs and other areas where device processing is performed. The revised guidelines that apply to SP areas include programs for occupational slip, trip and fall prevention; latex, chemical and fire safety; waste management; and regulatory reporting.
Specific to slip, trip and fall prevention, the guideline recommends evaluating areas for environmental hazards, collecting and analyzing data on slip, trip and fall events, and providing education to alert employees about risks and how to mitigate them. AORN commonly incorporates checklists for error prevention, and this guideline uses them to evaluate the implementation of a slip, trip and fall prevention strategy. Health care facilities should have procedures in place for routine floor cleaning, spill man-
agement and reporting of slips, trips and falls, and the program should monitor trends and evaluate program effectiveness.
A new fire risk assessment and prevention algorithm was added to the “Environments of Care” guideline to help the perioperative and SP teams identify fire risks and direct appropriate intervention depending on the risks that are present. One area in which SP professionals play an integral role is evaluating electrosurgical unit safety and performing risk assessments.
As the “AORN Guideline for Electrosurgical Safety” recommends, electrosurgical devices with insulation should be inspected with an active electrode insulation integrity tester while preparing active electrodes for packaging during processing. This recommendation is also stated in ANSI/AAMI ST79:2017 & 2020 Amendments A1, A2, A3, A4 (Consolidated Text) Comprehensive guide to steam sterilization and sterility assurance in health care facilities; it states that instrumentation intended for use with electric current should be tested for integrity each time it is processed, following the instrument manufacturer’s written instructions for use (IFU) for inspection.
The updated “Environments of Care” guideline builds on the goal of providing a latex-safe environment and now recommends establishing a latex safety program to alleviate the risks associated with latex allergy and sensitivity for patients and personnel. Additionally, a chemical safety plan was added to the guideline to assist facilities in developing their own. The plan includes implementing safe practices for the storage, handling and disposal of chemicals to reduce the risk of accidental exposure.
Further, based on medical device reporting regulations, reporting of any suspected device-related serious injury or death has been upgraded to a regulatory requirement. A recommendation was added to the guideline to report device malfunction to the U.S. Food and Drug Administration (FDA), even if it did not result in patient harm. The FDA uses medical device reports to monitor device performance, detect potential devicerelated safety issues, and contribute to risk-benefit assessments of suspected device-associated deaths, serious injuries, or device malfunction.
To learn more about these updated guidance documents and other AORN guidelines for perioperative practice, visit https:// aornguidelines.org/guidelines?bookid=2260.

AAMI eXchange is back!
The 2024 edition of the conference will be held in Phoenix, Arizona from June 14-17, 2024. As always, AAMI eXchange is a must-attend event for anyone involved in health care.
We expect to host over 2,100 health technology professionals, and eXchange will feature over 165 exhibitors including leading manufacturers and service providers, over 10 hours of exhibit time including networking events on the expo hall floor, and more than 80 educational sessions and workshops offering content tailored to various technical fields and professional areas. Coming on the heels of AAMI eXchange 2023, held in Long Beach, California, AAMI eXchange 2024 is expected to exceed its previous editions.
If you work directly with medical devices or in a field that relates to health technology, AAMI eXchange is for you. Not only will attending allow you to make face-to-face connections with peers from across the country, but eXchange is a brilliant chance to hear from experts, discover new professional opportunities, and learn from the best.
Like previous years, eXchange24 will feature a wealth of training, educational sessions, and informative keynote sessions alongside the AAMI expo hall where attendees can view the latest and greatest in health technology.
In addition to several keynote sessions, eXchange will feature several concurrent symposiums. These include the Clinical Engineering Symposium presented by ACCE and an Industry Symposium presented by Palo Alto Networks.
A special thanks to this year’s sponsors, including Asimily, Crothall Healthcare, GE Healthcare, Ordr, Siemens Healthineers, Sodexo, TRIMEDX, and USCO Biomedical Services. The American College of Clinical Engineering is also acting as a contributing organization at eXchange24.
The eXchange expo hall will feature over 165 exhibitors from the medical device industry alongside other associations, trade press and more. Expo hall activities will include an AR/VR Theater, and exhibitor in-booth theaters from the Siemens Healthineers, STERIS Corp, TRIMEDX, Avante Health Solutions, and GE HealthCare. Also, Live @AAMI eXchange, sponsored by GE Healthcare, will be returning
this year, and AAMI staff will take the chance to cover the conference and dialog with AAMI Awards winners, eXchange24 attendees, and conference presenters on key issues related to healthcare technology management.
Training at eXchange24
Training at AAMI eXchange will cover a number of technical areas and is divided into several distinct tracks.
• Iot and AI Interoperability
Track, sponsored by Ordr: This track will feature experts like the Mayo Clinic’s Kurt Griggs and Axel Wirth of Medcrypt Inc. on the cutting-edge threats and challenges that medical devices face due to new tools like AI.
• Cybersecurity Track sponsored by Asimily: The Cybersecurity Track features experts like Jeff Hooper, Ph.D., of the Children’s National Medical Center, and Priyanka Upendra of Asimily, on issues such as FDA requirements, risk management, and more.
• Patient Safety Track: Taught by experts like ECRI’s Erin Sparnon and researchers from the University of Massachusetts Amherst, this track will address issues like AI in relation to health equity, human factors, and
new tools like smart pumps.
• Professional Development Track: This track will feature experts such as AAMI board member Heidi Horn, and individual sessions will address management best practices, dealing with career obstacles, job searching, and building leadership skills.
• Sterilization Track: The Sterilization Track is taught by experts such as Nupur Jain of Intuitive and Samuel Tobin of Nemours Children’s Health, and will include sessions on borescope inspections, cleaning robotic surgical instruments and more.
• Home Health Track: This track features experts from groups like the MITRE Corporation and the Mayo Clinic and will focus on issues such as cybersecurity and the inpatient digital experience.
• Equipment Management Track: This track will feature experts such as Russell Lang of Agiliti, Brian McLaughlin of Massachusetts General Hospital,
and will address medical equipment planning, realtime location services, service contracts and capital planning.
• VR/AR Track: This track will feature experts such as Richard Ludwig and Matthew Kwiatkowski of GE Healthcare, and will include sessions on video training in HTM, augmented reality surgical navigation and more.
• Regulatory Track: The Regulatory Track will feature speakers such as Scott Trevino of TRIMEDX, Binseng Wang of Sodexo, and others on regulatory compliance, and the tradeoffs of regulating medical device sorting.
In short, AAMI eXchange24 is set to be an excellent opportunity for training, learning and connecting with HTM professionals in your niche or further afield. Questions about registration, the expo hall, or other issues? Contact events@aami.org.


L eadership is the art of guiding and influencing others towards a common objective. The successful implementation of change within the health care system cannot be done by an individual nurse; it necessitates collaborative effort from the entire nursing community. In this collective pursuit, nurses must acknowledge and embrace the leader within themselves. Frequently, I encounter nurses who disassociate from leadership roles, stating, “I am not a leader; that is the manager’s responsibility.”
Overcoming this mindset is pivotal, as the primary obstacle to creating necessary changes to impact our environment and most importantly our patient care lies in the recognition that each nurse, irrespective of formal titles, possesses leadership qualities.
Leadership is a dynamic skill that can be cultivated and honed over time. Nurse leaders must create a foundation for developing and refining their own leadership skills, as well as seeking opportunities to access formal education and training. Formal leaders have a title or are in a position of authority that require others to follow their direction. Informal leaders do not have an official title or position
but do have influence over individuals because of their ability to motivate others with a demonstrated passion to lead. Any nurse can become an informal leader by being a role model to others, persistently advocating for evidence-based practice, and helping the organization achieve better outcomes (Competency and Credentialing Institute [CCI], 2021). Effective leaders have essential characteristics that include being a visionary, having the ability to clearly articulate desired goals, are passionate about the goal, can share and inspire passion in others, and are ethical in their actions (CCI, 2021). Effective nursing leaders are often role models within the unit they work. The passion for improving patient care, creating a healthy work environment and supporting others is palpable.
The Institute of Medicine’s (IOM) report (2011), “The Future of Nursing: Leading Change, Advancing Health,” discussed the need for nurses to lead change. Thirteen years later, it continues to be a key factor in health care and the nursing profession. The four key messages from the IOM report led to many recommendations related to advancing the role of nursing professionals as leaders within health care (IOM, 2011). To support the role of nurse as leader, the IOM report recommendations included expanding current opportunities for nurses to lead and collaborate with other members of the health care team, including physi-
cians, provide a seamless academic transition to increase the proportion of nurses with a baccalaureate degree, as well as double the number of nurses with a doctorate, and commit to lifelong learning (IOM, 2011). The latest Future of Nursing Report (2021), “The Future of Nursing 2020-2030: Charting a Path to Achieve Health Equity,” again calls on nurses and organizations to expand the leadership role of nurses.
Leadership development may come through experience, but it may also come through training or formal education. It is important for formal leaders and managers to support informal leaders in achieving growth within the leadership role. The challenge is then for formal leaders to seek out and better utilize the opportunities within and/or outside the organization to provide the training and education needed for their informal leaders to be successful. One way for organizations to seek resources is to partner with academic institutions. Academic partnerships may already be part of the organizations health care system as the host of nursing students to support clinical rotations. Additional resources may be available to advance the leadership skills of staff nurses. Many health care organizations offer tuition assistance or reimbursement that nurses have not considered using to support professional growth.
CCI has partnered with Edgewood
College in Madison, Wisconsin for several years. The nursing team at CCI teaches two 16-week electives for prelicensure nurses to experience perioperative nursing. The next collaborative effort between CCI and Edgewood College is a formal academic training program for perioperative leadership – The Perioperative Leadership Graduate Certificate course, set to debut in the fall of 2024. Tailored for practicing nurses who have already graduated, this course delves into key leadership domains, including communication, human resources, professionalism, operations, strategic management, and finances. These domains have been built based on the psychometrically validated job analysis for the Certified Surgical Services Manager (CSSM) credential offered by CCI. The perioperative leadership graduate certificate course provides an overview of how health care and leadership intersect and form the basis of quality outcomes and improving patient care services.
Recognizing that leadership is an inherent and vital characteristic of nursing, nurses find themselves in a unique position to instigate substantial positive change. As informal leaders inspire their peers through unwavering passion and commitment to fostering the change they envision for the future, the imperative is to proactively seek and leverage available resources for success. This proactive approach ensures that nurses not only contribute
to improving the overall work environment but also elevate the standards of practice for the benefit of their patients.

Dawn Whiteside, DNP, MSN-Ed, RN, CNOR, NPD-BC, RNFA is the Director of Education and Professional Development of the Competency & Credentialing Institute. Dr. Whiteside has over 35 years of experience as a perioperative nurse in many roles including circulator, scrub, first assistant, team leader, charge nurse, manager, and educator. She serves on the ABSNC Board of Directors as well as the editorial board for MD Publishing. As an educator, Dr. Whiteside is passionate about developing educational materials for all members of the perioperative team.
References:
• Competency and Credentialing Institute (CCI), 2021. CSSM Exam Prep Book, Second Edition.
• IOM (Institute of Medicine). 2011. The future of nursing: Leading change, advancing health. Washington, DC: The National Academies Press.
• National Academies of Sciences, Engineering, and Medicine. 2021. The future of nursing 2020–2030: Charting a path to achieve health equity. Washington, DC: The National Academies Press. https://doi. org/10.17226/25982.

Phone: (618) 476-3550
Toll Free: (877) 828-9975
Email: sales@macmedical com






Electro Lube™ anti-stick solution is clinically demonstrated to keep tissue from sticking to electrosurgical instrumentation during use, leading to less tim e spent on handbacks to remove eschar buildup during the procedur e. Electro Lube is packaged sterile, and ready to use. To obtain samples and schedule a product trial at y our facility, visit www.steris.com/healthcare.



A surgical instruments market overview and forecast for 2024-2030 by IndustryARC indicates growth in the coming years. IndustryARC is a provider of market research reports, custom consulting services, data analytics and industry analysis.
A forecast summary states that the surgical instruments market size is forecast to reach $35.8 billion by 2030, growing at a CAGR of 8.4% during the forecast period 2024-2030.
Surgical instruments are tools or equipment used for purposes such as cutting, dissecting, gripping, holding, dilating or expanding, suctioning, retracting, or suturing. These tools are utilized in a wide range of processes and operations. The majority of surgical tools are constructed of stainless steel. Other metals used in addition to stainless steel include titanium, chromium, vanadium and molybdenum. Surgical instruments are tools that allow surgeons to access the soft tissue, remove the bone, dissect and isolate the lesion, and remove or destroy the aberrant structures as a therapy. Increasing prevalence of chronic diseases such as cancer, blood disorder, autoimmune diseases, and other disease coupled with growing geriatric population are the major factors driving the growth of the market. Increasing cases of accidents and injuries are set to further enhance the overall market development of the surgical instruments market for the period 2024-2030.
The report: “Surgical Instruments
Market Forecast (2024-2030)” by Industry ARC, covers an in-depth analysis of several segments of the surgical instruments market.
Key takeaways from the report include:
• North America will dominate the surgical instruments market in 2030 owing to rising number of surgical centers. The surgical instruments market scope for different regions will be provided in the final report.
• Increasing number of surgical procedures are likely to aid the growth of the surgical instruments market.
• Strict government regulation is poised to create some hurdles for the surgical instruments market.
Handheld instruments held the largest share in the surgical instruments market in 2023 and is estimated to grow at a CAGR 7.1% during the forecast period 2024-2030. Forceps, retractors, dilators, graspers and scalpels are examples of handheld instruments. These surgical tools are normally made of high-quality stainless steel and are available in a variety of sizes and shapes that are ideal for certain operations. Handheld instruments are widely used during surgery. Handheld instruments are estimated to register a higher CAGR during the 2024-2030 forecast period.
Cardiology held the largest share among application segments in the surgical instruments market in 2023 and is estimated to grow at a CAGR 6.9% during the forecast period 2024-2030. Cardiovascular surgery is used to treat diseases and conditions of the heart and blood arteries throughout the body. Coronary
bypass surgery, aortic or mitral valve replacement or repair, and aneurysm repair are all common cardiovascular treatments. The increase in the number of coronary and percutaneous cardiology procedures, as well as the number of cardiology surgeries, is driving the growth of this segment.
North America dominated other geographic locations in the surgical instruments market report with a major share estimate of 34% in 2030. This is attributed to the increasing prevalence of chronic diseases such as cancer, blood disorders, autoimmune diseases and other disease in this region. Furthermore, rising health care expenditures and technological advancements are driving the growth of the market in this area.
Increasing incidence of road accidents across the globe is another factor that is increasing the growth of the surgical instruments market. According to the Centers for Disease Control and Prevention, each year around 1.2 million people are killed owing to road accidents around the world. Furthermore, growing adoption of minimally invasive surgery (MIS) instruments will also drive market growth. Thus, increasing the growth of the surgical instruments market during the forecast period 2024-2030.
Some of the leading companies in the surgical instruments market are Medtronic plc, Progressive Medical Inc., Scanlan International, Abbott Laboratories Inc., Boston Scientific Corporation, HOYA Corporation, Koninklijke Philips N.V., Biolitec AG, Stryker Corporation and Johnson & Johnson.
The Maxima Adson Tissue Forcep by Henry Schein is crafted from premium surgicalgrade German stainless steel, known for its performance qualities and durability compared to standard stainless steel. It can be used for general practice needs as well as for specialized procedures. With measurements of 4-3/4” length, the Maxima Adson Tissue Forcep has a nonlocking thumb handle and a straight, delicate pattern. It can hold and manipulate delicate tissue during surgical procedures, and its 1x2 teeth provide a firm grip on tissue in an atraumatic way. Because of its OR-grade stainless steel, the Maxima Adson Tissue Forcep can sustain multiple sterilizations, resulting in a longer shelf life for the product.
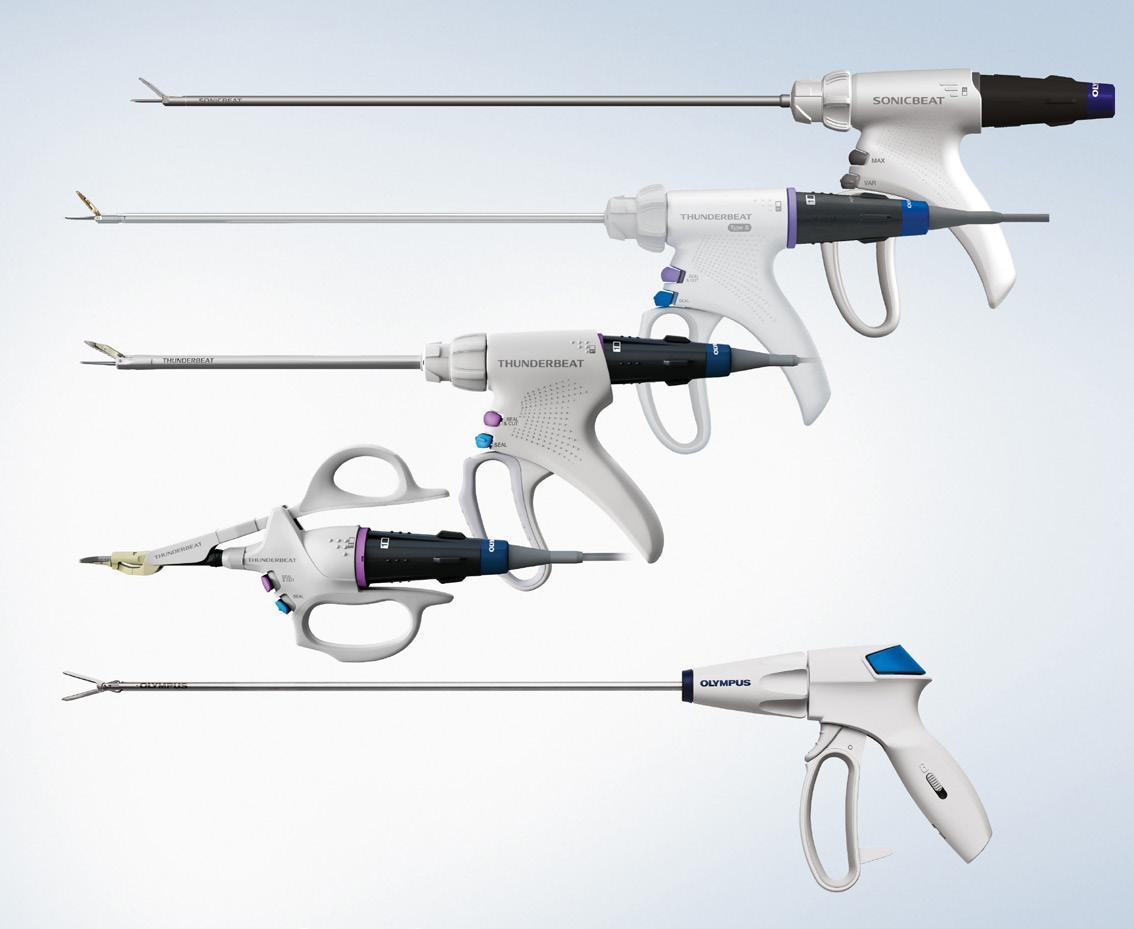

The Olympus surgical energy portfolio combines ultrasonic, advanced bipolar, hybrid and standard energies powered by a single surgical energy platform, the ESG-410, offering the user the power to choose which solutions best fit their surgical needs. The POWERSEAL portfolio includes advanced bipolar vessel sealers/dividers and is indicated for 7mm vessel sealing, including pulmonary vessels. The devices are designed for ergonomic comfort and versatility. The THUNDERBEAT portfolio offers unique hybrid energy, ultrasonic and advanced bipolar energy, in one device. This combination of technologies results in advanced hemostasis for vessels up to 7mm with efficient, precise tissue cutting. The SONICBEAT portfolio is an ultrasonic technology created for vessels up to 5mm and reduces the need for an additional grasper due to its wiper jaw design. With a choice in hybrid, advanced bipolar, ultrasonic, and standard powered surgical energy devices, the user can be equipped with the right tool, at the right time.



The MICHELER Heart Vent Catheter (MHVC) is FDA cleared K200289. The MHVC is a soft balloon-tipped catheter. It is inserted through the open left atrium during mitral valve surgery or through the right superior pulmonary vein on the beating heart and across the mitral valve into the left ventricle. Uniquely, the device is securely positioned and maintained in the LV by inflating a soft positioning balloon against the mitral annulus/valve. The balloon inflates, keeping the catheter tip below the mitral valve to ensure drainage of air, blood and debris from the left atrium and left ventricle. The MHVC consists of a flexible tube with a soft compliant balloon located on the distal portion of the tube with drainage holes both proximal and distal to the balloon. The catheter is provided with a tapered tip, a malleable stylet and depth markings to insure smooth insertion. Overall length is approximately 43.8 cm (17.25 in). The inflatable balloon is filled with sterile saline solution and holds the catheter in place at the desired location. Catheter 16 fr. O.D. (5.5 mm dia.) Supplied sterile, for one time use.
For more information, visit KappSurgical.com.

Lazurite’s ArthroFree System includes the first wireless camera with FDA clearance for arthroscopy and endoscopy. Free of cumbersome camera cables, ArthroFree lets surgeons work with maximum dexterity, precision and focus. Surgeons say they don’t have to constantly be moving cables around while operating, so they can focus on the task at hand and not on the equipment. Surgeons can also rest assured that ArthroFree’s connection to the surgical tower will be contamination-free, every time, guaranteed.

Paragon 28 Inc. has launched the Mister Tendon System which allows surgeons to perform a distal cut of the flexor hallucis longus (FHL) or flexor digitorum longus (FDL) tendon through a minimally invasive incision, harvesting a working length of tendon suitable for tendon transfer procedures. Use of this instrumentation through a minimally invasive approach, is designed to allow for better healing and quicker recovery time in flatfoot reconstruction. In addition to the harvester, an accessory dilator instrument is provided to help bluntly dissect soft tissue, improving harvester access without causing additional damage.
As a perioperative or SPD professional, you deal with many complex situations. That’s why the instruments your surgeons use should be highly functional, easy to use and easy on their hands. Snowden-Pencer Ergonomic Modular Laparoscopic Instruments are designed with surgeons for surgeons for the ideal balance of function, strength and design – with a focus on ergonomics, durability and flexibility. The instruments have a unique modular design, featuring over 125 jaw patterns, that offer thousands of combinations to meet the standards and needs of surgeons across multiple specialties. That’s the difference of ergonomics in surgeon-focused design.
For more information, visit steris.com/vmueller.

Stryker’s Blueprint Mixed Reality Guidance for shoulder arthroplasty offers surgeons a new tool to execute their pre-operative plan using 3D imaging to operate with more precision and consistency. Designed by a team of world-class surgeons, the system takes stereotaxic surgery – a three-dimensional surgical technique – to the next level and enables real-time visualization of implant positioning and surgical decision-making. Mixed reality guidance is designed to allow surgeons to deliver more precise surgical results with much less variability than surgery without guidance.


Introducing SQ.line KERRISON Bone Punches, Aesculap’s next generation of premium Kerrisons. This instrument is built to increase performance, with an ergonomic handle designed to reduce pressure points for comfortable use during surgical procedures. With an easy-to-clean design, this surgical instrument helps to enhance processing for your SPD team. SQ.line KERRISON Bone Punches offer a time-saving potential–compared to a leading competitor — with a fast and intuitive assembly and disassembly. Additional features and benefits of the SQ.line KERRISON Bone Punches are available at Neurosurgical Instruments (aesculapusa.com).

 By don sadler
By don sadler
Published in 2010, the “Future of Nursing Report: Leading Change, Advancing Health” explores how nurses’ roles, responsibilities and education need to change to meet the increased demands for health care and advance improvements in the nation’s complex health system.
One of the report’s key messages is the need to transform nursing leadership.
“Nurses should be full partners with physicians and other health professionals in redesigning health care in the United States,” says the report.
Transforming leadership translates more broadly to the health policy arena, where nurses should have a voice in health policy decision making.
“Nurses also should serve actively on advisory committees, commissions and boards where policy decisions are made to advance health systems to improve patient care,” states the report. “Yet a number of barriers prevent nurses from serving as full partners.”
Renae Battié, MN, RN, CNOR, FAAN, vice president of nursing for the Association of periOperative Registered Nurses (AORN), points out that the nursing code of ethics states that perioperative nurses are to collaborate with others in advancing the quality of health for all.
“Use of the title RN carries with it the individual’s responsibility to act in the public’s best interest and to promote social justice by advocating for patients,” says Battié. “To do this, perioperative nurses need to stay connected to broader nursing initiatives.”
One example is the affiliate ANA membership available to all AORN members. As an outcome of “The Future of Nursing Report,” AORN is also a member organization with Nurses on Boards and has more than 10,000 nurses serving on boards and actively matching nurses with needs. “This is an example of nursing being well-positioned for impact,” says Battié.
“Perioperative nurses need to engage with the nursing profession at large or we’ll be forgotten,” says David Wyatt, Ph.D., RN, NEA-BC, CNOR, FAORN, FAAN, chief nursing officer, University Hospital, UT Southwestern Medical Center, and AORN past president. “There’s a great opportunity now to shape the profession and ensure that we have a voice in where it is headed in the future.”
Wyatt says that AORN members have opportunities to serve on task forces and as subject matter experts with their ANA state nursing associations. “Reach out to your local chapter or the national headquarters to get involved,” he says.
“Many of the committees and board rooms in nursing where decisions are made do not have representation from perioperative nurses,” says Dawn Whiteside, DNP, MSNEd, RN, CNOR, NPD-BC, RNFA, director of education and professional development for Competency & Credentialing Institute (CCI). “So important decisions about patient care are being made without our expert input. Nurses are front-line caregivers so we need to have a seat at the table in order to influence change.”
Elaine D. Geroski, RN, MSN, CNOR, CSSM (E), assistant vice president of patient services at the WVU Medicine Grant Memorial Hospital, serves as the president of the CCI Board of Directors.
“Volunteer board service has helped me gain knowledge and network with other
nurses throughout the nation,” she says. “And by volunteering as a subject matter expert, I’m helping lead change to increase patient safety and compliance of standards.”
Geroski recalls her first committee volunteer experience. “I remember sitting across from a director of periop from a larger city and thinking, ‘How can I contribute from a smaller rural facility?’ ” she says. “But I learned that they prized diversity of regions, and I was probably picked based on my rural hospital’s location and size.”
Melissa R. Nosik, Ph.D., BCBA-D, ICE-CCP, SHRMSCP, CEO of the CCI, lists a number of reasons why she believes perioperative nurses should take an active role in leading change in the nursing profession by serving and volunteering:
• Quality improvement – As frontline caregivers, perioperative nurses are well-positioned to identify areas for improvement in clinical practice, workflow efficiency and patient safety. “Nurses’ involvement in leading change initiatives can drive quality improvement efforts and enhance the overall standard of care,” says Nosik.
• Specialized expertise – Firsthand experience in the operating room gives perioperative nurses valuable insights into the challenges and opportunities within health care delivery.
• Collaboration and interdisciplinary care – Effective perioperative care requires collaboration among various health care professionals including surgeons, anesthesiologists and support staff. “Nurses who lead change initiatives can foster a culture of collaboration and interdisciplinary teamwork, resulting in better coordinated and more comprehensive patient care,” says Nosik.
• Professional development – Taking a leadership role allows perioperative nurses to enhance their professional development and contribute to the advancement of the nursing profession. “By engaging in initiatives such as research, education and policy advocacy, nurses can elevate the status of perioperative nursing and promote continuous learning and growth,” says Nosik.
• Patient advocacy – By taking a leadership role, perioperative nurses can champion initiatives that prioritize patient-centered care and improve outcomes.
• Adaptation to evolving practices – The health care landscape is constantly evolving with advancements in technology, changes in health care policies and shifts in patient demographics. “Perioperative nurses who actively lead change initiatives can help their colleagues adapt to these changes and stay abreast of best practices in surgical care,” says Nosik.
Senator Gale Adcock (North Carolina State) is a family nurse practitioner and former chief health officer at global
software company SAS, where she led the onsite primary care practice. Over the past three decades, she has been appointed to four different health-related state boards and commissions by three different North Carolina governors.
“These experiences have helped me become more comfortable asking tough questions, offering a minority opinion and handling conflict,” she says.
Policymakers, both inside and outside your workplace, cannot be experts on every issue they face.
“When no one at the decision-making table represents the views of perioperative nurses, there’s a risk that poor or even failed policies will be enacted,” she says.
Adcock says that nurses’ voices have no impact when they’re confined to grousing in the locker room or staff lounge.
“If a perioperative nurse cannot be one of the policymakers, then it’s up to them to educate and influence those who are,” she says.
One of the best ways to actively lead change is to join national and state organizations that speak for perioperative nurses.
“Many of these are responsible for proposing, monitoring and lobbying for and against bills impacting the work that perioperative nurses do,” says Adcock. “They hire professional lobbyists to ensure that nurses’ perspectives are heard and considered by state lawmakers.”
Adcock also urges nurses to seek appointments to advisory boards and commissions from their local, state and federal officials. “Search the website of your county, city and governor for information about existing boards and commissions, any board-specific qualifications, and how and when to apply,” she says.
Brenda C. Ulmer, RN, MN, CNOR, has been spearheading the charge to get surgical smoke evacuation and filtration legislation passed in states around the nation. She started her efforts way back in 1996 as the chair of AORN’s first multidisciplinary round table discussions on surgical smoke. She served on AORN’s Smoke Task Force in 2006, which resulted in the AORN Smoke Position Statement and Smoke Tool Kit.
“Because of a personal health experience, I knew how bad breathing surgical smoke is and that physical symptoms take a long time to develop,” says Ulmer. “I felt that advocating for smoke evacuation was the right thing to do.”
According to Ulmer, in the 15 states that have passed laws on surgical smoke evacuation, everything started when a nurse or group of nurses contacted state legislators and said this is a workplace hazard that needs to change. “Addressing the issue at the state level has demonstrated that when we work together, we have the power to make significant practice changes,” she says. “Our voices can and should be heard.”
Ulmer urges nurses to get to know their local and state
legislators before they need to ask for something.
“In Georgia, we invited local politicians to one of our conferences, which allowed us to get to know them and they us,” she says. “We also partnered with our AST organization and with the Georgia Nurses Association.”
Nurses are rated as one of the most trusted professions year after year.
“This is something we can leverage as we publicly advocate for ourselves, our patients and safe working conditions,” says Ulmer.
Most perioperative nurses lead busy lives, both professionally and personally. One of the biggest challenges is simply finding the time and energy to volunteer and serve in ways that help lead change.
“I understand these real-life challenges, but I urge nurses to do whatever they can,” says Ulmer. “There is no shortage of situations where you can make a difference.”
Wyatt acknowledges that the time commitment to serving and volunteering is a legitimate consideration.
“I encourage nurses to figure out how they can engage based on their current season of life,” he says. “Service won’t look the same for everybody, but I believe there’s an obligation for nurses to contribute to the profession in whatever way they can.”
Another common challenge to service is obtaining support from your primary employer, including the scheduling flexibility to devote to volunteer service.
“I gained support by emphasizing the return on investment,” says Geroski. “Volunteering for service with the CCI has allowed me to attend AORN events free of charge. Otherwise, my small facilities could not afford to send me to these conferences.”
Some nurses hesitate to serve because they don’t think they have the knowledge or skills to contribute to a board or committee.
“This is completely wrong,” says Geroski. “Diversity is valued among the committees and boards I’ve served on. Believe in yourself and the knowledge you bring to the table. You know more than you think you do.”
Battié concurs.“Lots of nurses don’t see their experience as valuable,” she says. “But periop nurses advocate every day



for their patients when they can’t speak for themselves. That same voice can speak up as an advocate for improving health.”
Battié recommends starting out local – for example, serving on a school, church or professional board, like an AORN chapter.
“This will help you get used to the structure of board work and communications,” she says. “There are many resources for understanding how a board works and learning the language of a BOD.”
Ulmer says she sometimes hears nurses say, “Well, I’m just a nurse.”
“To me, this indicates that they think they have no power and can’t do anything except go to work and collect a check,” she says. “However, being a trusted professional gives nurses power that not all professions enjoy.”
From the outside, board service and advocacy can look mysterious and the process can be hard to understand.
“So, some nurses think service is only for those who are experienced in advocacy or active politically,” says Adcock “But this is far from the truth: Everyone starts somewhere, and every board member doesn’t have to have the same degree of prior board experience.”
Actively serving to lead change will not only benefit the nursing profession as a whole, but nurses themselves may benefit personally in many different ways. “For me, it’s the personal satisfaction of doing a good job,” says Ulmer.
“Being somewhat of a nerd, I instantly go to the knowledge that you gain, which is invaluable,” says Geroski. “Another benefit is making life-long friends whom you have so much in common with.”
Battié says these kinds of experiences help grow leadership skills and can open doors of opportunity for influence and impact. “They look great on resumes, too,” she says.
Wyatt says he has never been one to sit back and wait for others to lead the charge. “There aren’t enough nurses stepping up right now and using their voices to lead change,” he says. “Important decisions will be made with or without our input.”
Nurses can’t complain about where things are headed if they’re not willing to get involved, says Wyatt.
“The more of us who step up and engage, the more likely we are to have solutions that produce positive outcomes for our profession,” Wyatt adds.




F rom her early days volunteering as a middleschool candy striper in Clewiston, Florida, to establishing her own health care consulting company, Natalie Jones has enjoyed a rich career in nursing; one that has taken her across the United States and internationally, through various levels of academic achievement, and to the top levels of leadership in her field.
“I always had a desire and a passion for health care,” Jones said. “I would see nurses on the television and think, ‘I would like to be a nurse someday.’
” That passion was invigorated even more when she expressed her desires to her parents.
“My parents encouraged me to follow my dreams and always reassured me that nothing was impossible for me to achieve,” Jones said.
After graduating a year early from Clewiston High School, Jones pursued her passion, and was accepted into the nursing program at Palm Beach Junior College, in West Palm Beach, Florida. While completing nursing school, she joined John F. Kennedy (JFK) Medical Center in Lake Worth, Florida as


a patient care technician. When she had completed the nursing program in 1984, however, jobs in her chosen profession were scarce. Jones was hired as a graduate nurse, and then as a Registered Nurse on a medical-surgical unit after she completed her state board examination.
Jones gained exceptional experience in patient care on that unit, but her introduction to perioperative nursing came when a PACU nurse remarked that she would be great working in the operating room, and encouraged her to seek an opportunity in a new ambulatory center recently built by JFK Medical Center.
“She said, ‘You’d really be good. Talk to the director and see what openings they have,’ ” Jones recalled. “There were no openings in the operating room at the time, but I was offered a position in endoscopy. I thought, why not? Change is good and accepting the position in endoscopy would at least get my foot in the door.”
After only a week and a half of working in the endoscopy department, the only other nurse there at the time went on vacation, providing Jones the first of what would become many op-
portunities to oversee a perioperative department. But even after becoming the endoscopy charge nurse, Jones retained such an interest in the perioperative environment that she took every spare moment to go into the OR. Whether observing cases, learning to pick cases, wiping down the rooms in the mornings, or updating preference cards, Jones made it known that she would do anything she could do to begin transitioning into the OR.
“I learned how to scrub before I learned to circulate,” Jones said. “I was already assisting in the OR, by coming in in the morning, wiping down the rooms, spreading the cases around, and starting the sterilizers for the OR team in the morning, and I wasn’t even in the OR yet. I availed myself and committed any additional time that I had to learn the processes and to demonstrate my desire to become an OR Nurse. I continued to work hard, and was not ever satisfied with just the status quo,” she said.

Finally, Jones gained the attention of one of the top general surgeons at the facility, Dr. Charles Moore. Moore, whom she remembered for his dedication to patient care, tenacity, strong will and meticulous surgical technique, took note of Jones’ enthusiasm, and advocated on her behalf. He asked the perioperative director, “Why are you wasting her talent? Why don’t you teach her how to scrub? Put her in my room, and I’ll teach her.”
For Jones, this surgeon’s willingness to advocate on her behalf was the start of a rewarding and lasting nursing career in perioperative services.
Despite seeking alternative (advanced) positions as a charge nurse, or nurse manager in the OR, Jones ran into objections, obstacles and barriers over her lack of either additional experience or additional education. She went on to earn a Bachelor’s in Healthcare Administration at Florida Atlantic University in Boca Raton, and then a Master’s in Business Administration from Nova Southeastern University.
“In one of my first organizations, I was there for a very long time, trying to advance and get to the next level,” she said. “Here I am this young, eager, motivated, hair-on-fire, can-do-anything-in-the-world nurse, and kept getting all kinds of excuses. It all worked for me because it was a motivating factor for me to say, ‘Education will never be an Achilles’ heel again.’ ”
Besides a strong work ethic and the pursuit of higher education had always been instilled in her by her parents, who both held college degrees and worked as educators in the school system.
“I had to be self-motivated to work hard – not because anybody told me I needed to, but because I wanted to,” Jones said.
“I wanted to know more about leadership and the business of health care,” she said. “My leadership track was to become a chief operating officer (COO) or chief nursing officer
(CNO). I advanced from charge nurse to nurse manager to perioperative director to administrator, leading perioperative and cardiovascular services both nationally and internationally.”
Jones credits her high degree of self-motivation with providing her the resolve necessary to push herself into positions of greater opportunity. Eventually, she also realized that when she wasn’t finding them where she was, choices abounded elsewhere in the health care space if she was willing to branch out.
Jones eventually joined Palms West Hospital, where she became a manager of perioperative services, and developed experience with strategic planning, budgeting, equipment acquisition, physician and nursing recruitment, physician relations and patient safety. She parlayed that into a nurse manager position at Mercy Hospital in Miami, and eventually into a role as the director of surgical services at Parkway Medical Center. The chief nursing executive who opened the door for Jones to ascend to that position, Rhue LaMont, became a transformative mentor
“We had to perform, but there was nothing like being a first-time director and someone taking the time to make sure you succeed,” Jones said. “Rhue gave several of us the opportunity for directorship positions; she mentored us and supported us, and that experience was invaluable.”
With her confidence – and resume – bolstered, Jones began to move into interim management and leadership roles on a consultancy basis. She began traveling to Minnesota, Michigan, Washington State and eventually Dohar, Qatar in the Middle East. All the while, Jones felt more and more empowered in roles of increasing responsibility. Even if she began a contract with a three-month tenure, Jones never served less than a year and oftentimes a year-and-a-half in any role. Today, she remains a steadfast advocate of the opportunities available to contract nurses and
nursing leaders to serve health care organizations.
“They’re eager to have you there, and you make a difference,” Jones said. “I was so blessed in every aspect. You have to be easily adaptable and quick on your feet. You have to be able to effectively assess and evaluate the organizational landscape quickly. And my experience expanded so much – I got to see different hospitals, organizations, executive teams, and gain phenomenal experience.”
“You break out of the siloes,” she continued. “You see different parts of the world. Your knowledge base is expanded, and that knowledge that you take from one organization is beneficial to another organization. The most rewarding aspect for me with interim traveling was taking that skill and expertise onto your next organization.”
Jones further enhanced her experience and expertise, earning a doctorate in health administration, then going back to earn her BSN, and launching NBJ Healthcare, her selfdirected health care consultancy consulting company. Other accomplishments include serving as a member and an officer of Association of periOperative Registered Nursing Nurses (AORN) South Florida Chapter 1004, as a member of the Board of Directors for the Florida Council of periOperative Registered Nurses, and as a member of the AORN National Nominating Committee. In her current position as Associate Faculty for the Doctoral Health Administration Program at the University of Phoenix, Jones enjoys the opportunity to help cultivate future health care leaders.
When she’s not working, traveling or spending time with her husband, Gilbert, Jones says that she enjoys attending comedy shows, bowling, horseback riding and a good spa day. She and Gilbert are also active members of their church, Redemptive Life Palm Beach, in West Palm Beach Florida where they have served as faithful members for 25-plus years.

One of the many things I hear people say in the gym is that they don’t squat because it hurts their knees. Without realizing that they squat almost every day whether it’s sitting down, going up stairs, or picking something off the floor. You cannot escape it. You will need to squat. Instead I wish people worked more on how they squat instead of avoiding it, but that’s OK because that’s where I come in as a trainer.
After some time correcting form or properly showing people how to move better, it brings me great gratification knowing I helped improve someone’s movement pattern to elevate their life. I want to do the same for you. So, before we dive into some squat variations, I want to bring up a couple of key points that everyone should consider.
First, how is your ankle flexibility? If you have weak ankles or poor flexibility, please improve this as it will help with stability and squat depth. Second, do you understand how to properly brace
your core? When weight lifting you should never draw in the naval. You should be bracing at your core as if your preparing for impact. Third, understand that with all movements it’s not about how much you lift, it’s about how you lift it. Now, let’s get into some squat patterns.
Our first movement is the DB Goblet Squat, a classic squat that really helps keep the body centered since the weight is chest centered and forces the core to be heavily engaged. This exercise is great for recognizing if you’re actually bracing at your core appropriately. It can also be done with a KB, but there are several variations that make this exercise easier or harder. Keep in mind, if getting low or squatting in general makes you nervous, I suggest pulling out a chair and practice barely hitting your butt to the chair to control range of motion. If you really need practice bracing your core then sit all the way down, brace and then stand up.
The second exercise is the KB Sumo Squat. It requires decent hip mobility in order to drive the legs wide enough to be in a proper
position. You don’t need a super wide stance. It’s important to make sure the knee stays over the ankle complex, however if you begin this movement and see heavy internal rotation at the knee or an inability to keep the knees driving wide during the movement, then I would stick with the Goblet squat for now. Because of this wide stance, the glute and inner thigh focus will turn up, giving a burn in the legs that you might have been looking for.
Our last exercise is the most advanced It’s the DB RLESS, aka, Rear Leg Elevated Split Squat. Before attempting, please make sure you can complete the two squats explained above. This movement requires decent balance and hip stability. This exercise is basically a single leg squat with back leg support. I would say the front foot will need to have at least 80% of your weight because of the heavy isolation. Don’t be surprised as to how quickly the legs tire, especially if you’re saving this movement for the end of a workout.
Have fun with these movements, stay active and never stop improving.





I n a recent study of the brain’s waste drainage system, researchers from Washington University in St. Louis, collaborating with investigators at the National Institute of Neurological Disorders and Stroke (NINDS), a part of the National Institute of Health (NIH), discovered a direct connection between the brain and its tough protective covering, the dura mater.
These links may allow waste fluid to leave the brain while also exposing the brain to immune cells and other signals coming from the dura. This challenges the conventional wisdom which has suggested that the brain is cut off from its surroundings by a series of protective barriers, keeping it safe from dangerous chemicals and toxins lurking in the environment.
“Waste fluid moves from the brain into the body much like how sewage leaves our homes,” said NINDS’s Daniel S. Reich, M.D., Ph.D. “In this study, we asked the question of what happens once the ‘drain pipes’ leave the ‘house’ – in this case, the brain – and connect up with the city sewer system within the body.”
Reich’s group worked jointly with the lab of Jonathan Kipnis, Ph.D., a professor at Washington University in St. Louis.
Reich’s lab used high-resolution magnetic resonance imaging (MRI) to observe the connection between the brain and body’s lymphatic systems in humans. Meanwhile Kipnis’s group was independently using live-cell and other microscopic brain imaging
techniques to study these systems in mice.
Using MRI, the researchers scanned the brains of a group of healthy volunteers who had received injections of gadobutrol, a magnetic dye used to visualize disruptions in the blood brain barrier or other kinds of blood vessel damage. Large veins are known to pass through the arachnoid barrier carrying blood away from the brain, and these were clearly observed on the MRI scans. As the scan progressed, a ring of dye appeared around those large veins that slowly spread out over time, suggesting that fluid could make its way through the space around those large veins where they pass through the arachnoid barrier on their way into the dura.
Kipnis’s lab was making similar observations in mice. His group injected mice with light-emitting molecules. Like with the MRI experiments, fluid containing these light-emitting molecules was seen to slip through the arachnoid barrier where blood vessels passed through.
Together, the labs found a “cuff” of cells that surround blood vessels as they pass through the arachnoid space. These areas, which they called arachnoid cuff exit (ACE) points, appear to act as areas where fluid, molecules, and even some cells can pass from the brain into the dura and vice versa, without allowing complete mixing of the two fluids. In some disorders like Alzheimer’s disease, impaired waste clearance can cause disease-causing proteins to build up.
Continuing the sewer analogy, Kipnis explained the possible connection to ACE points.

“If your sink is clogged, you can remove water from the sink or fix the faucet, but ultimately you need to fix the drain,” he said. “In the brain, clogs at ACE points may prevent waste from leaving. If we can find a way to clean these clogs, its possible we can protect the brain.”
One implication of ACE points is that they are areas where the immune system can be exposed to and react to changes occurring in the brain. When mice in Kipnis’s lab were induced to have a disorder where the immune system attacks the myelin in their brain and spinal cord, immune cells could be seen around ACE points and even between the blood vessel wall and the cuff cells; this led over time to a breakdown of the ACE point itself. When the ability of immune cells to interact directly with ACE points was blocked, the severity of infection was reduced.
“The immune system uses molecules to communicate that cross from the brain into the dura mater,” said Kipnis. “This crossing needs to be tightly regulated, otherwise detrimental effects on brain function can occur.”
Reich and his team also observed an interesting connection between the participants’ age and the leakiness of ACE points. In older participants, more dye
A series of MRI images shows the movement of light-emitting molecules moving through the arachnoid barrier. Fluid containing light-emitting molecules was seen to slip through the arachnoid barrier where blood vessels passed through. (Photo credit NINDS)
leaked into the surrounding fluid and space around the blood vessels.
“This might point to a slow breakdown of the ACE points over the course of aging,” said Reich, “and this could be consequential in that the brain and immune system can now interact in ways that they’re not supposed to.”
The connection to aging and the disruption of a barrier separating the brain and immune system fits with what has been observed in aging mice and in autoimmune disorders like multiple sclerosis. This newfound link between the brain and immune system could also help explain why our risk for developing neurodegenerative diseases increases as we get older, but more research is needed to confirm this connection. This study was supported by the NINDS Intramural Research Program, the National Institute on Aging (AG034113, AG057496, AG078106), and the Cure Alzheimer’s Fund BEE Consortium.
Refe rence
• Smyth, LCD, et al. “Identification of direct connections between the dura and the brain.” Nature. February 7, 2024.
DOI: 10.1038/s41586-023-06993-7t




I n my most recent column, I wrote that fears are a source of obstacles that slow us down or stop our forward progress altogether. When we describe someone as lacking motivation, we’re using bad psychology, because the word motivation means “a reason to move,” and everyone already has reasons to move. What slows people down is either a lack of connection between their internal reasons to move with the goals and missions of the organization, or the presence of fear.
Solving the first problem, the lack of a connection, falls to a person’s supervisor. Rather than manipulate using intimidation, which leads to demoralization, supervisors do better by getting to know the interests of individual team members and then showing how those interests connect with the vision and mission of the organization. We’ll talk more about that in a future column. Today, I want to talk about fears.
Fears are normal and natural emotions that can be powerful in both positive and negative ways. On the positive side, fears can save our lives, such as not stepping out in front of a bus. On the negative side,
fears can cause us to avoid stepping out to accomplish great things.
Thus, if we’re experiencing procrastination or a lack of motivation, we should look within to see if unhealthy fears have become obstacles for us.
If we’ve determined that an unhealthy fear is leading to procrastination, that fear needs to be identified. I know a medical lab technician named Jo who was sometimes called on to do blood draws, but she hated doing them. Her heart rate would increase and she felt overwhelmed as soon as a blood draw was assigned.
Being that blood draws were part of her job, Jo started journaling in an effort to determine why she was so uncomfortable with them. She realized that as a child, she saw her mother wince in pain upon getting a needle stick, and that created a strong emotional impression. It seemed so simple, but the emotional imprint was strong. Fears can be like that.
Multiple ways exist for reducing or eliminating the impact of fears. Jo overcame her fear of blood draws by visiting the phlebotomy department on her day off and spending several hours watching the procedure over and over again. After several visits, Jo’s disdain for drawing blood disappeared.
Sometimes just talking about a fear will do the trick. Relaxation techniques can also work. Sometimes it’s necessary to talk with a professional counselor. But fears can also be rooted in fear of punishment. For example, if a supervisor criticizes employees easily, employees may fear stepping out to avoid the verbal lashing. Those situations often call for involvement from Human Resources.
Either way, once a fear is identified and strategies are established for minimizing or eliminating the fear, then forward progress becomes much easier.
To reiterate, it’s bad psychology to declare someone lacks motivation, because everyone has a reason to move, and we all move better when no obstacles exist in our path.
Daniel Bobinski, is author of the bestselling book, “Creating Passion-Driven Teams,” and president of Leadership Development, Inc. He’s been helping organizations of all shapes and sizes since 1989. Learn more at www.eqfactor.net or reach him at DanielBobinski@protonmail. com or 208-649-6400.


When talking about beauty and diet, radiant skin, full hair, and a certain youthful quality may come to mind. But beauty is so much more than that, and there are strategies for looking (and feeling!) good at any age.
Diet certainly plays a part in aging and beauty because many macroand micro-nutrients are vital in preventing premature aging. Macronutrients that support beauty are:
• Carbohydrates: Carbohydrates are the main source of energy for all the cells in the body. The key here is to get the majority of carbs from whole grains, fruits, and vegetables so that you get the energy for vitality, but you don’t get a big spike of blood sugar to throw the body out of balance.
• Fats: Lipids (another name for fats) are vital for youthful skin by keeping cells healthy, preventing moisture loss, and keeping skin moisturized and supple. The best types of fats for healthy skin are PUFAs, which include fats from fatty fish, walnuts, flaxseeds, chia seeds, and seaweed, and MUFAs, which include olives (including olive oil), avocados, and nuts.
• Protein: This vital macronutrient is important to the structure and function of all parts of the body including the skin, hair, and nails. Collagen is a form of protein that is abundant in skin and connective tissues, but it also can be consumed – often added to beverages like coffee or smoothies for a little boost. Collagen production requires vitamin C and adequate protein intake.
Choose these food categories that can support your beauty.
• Vitamin A foods: carrots, tomatoes, red peppers, melon, fish, eggs
• Vitamin C foods: sweet potatoes, red peppers, citrus fruits, strawberries, tomatoes
• Vitamin E foods: almonds, peanut butter, pumpkin, wheat germ oil, sunflower seeds
• Biotin foods: nuts, egg yolks, oats
• Selenium foods: Brazil nuts, seafood, broccoli, soybeans
Grace O is the creator of FoodTrients, a unique program for optimizing wellness and longevity. She is the author of three award-winning cookbooks. Her latest cookbook is “Anti-Aging Dishes from Around the World.” Learn more at Foodtrients.com/recipes/beauty.

Strawberries and almonds don’t just add beauty to this luxurious dessert, they support beautiful skin. Almonds deliver plenty of fiber, omega-3 fatty acids, and vitamin E. Strawberries are loaded with vitamin C and anthocyanins, which may help inhibit the growth of cancer cells and improve capillary function in the brain, eyes, and skin.
This almond cake recipe works well with glutenfree flour. I prefer the taste and texture of Cup4Cup
Ingredients (Serves 8)
• 3 eggs
• 1 tsp. pure vanilla extract (or seeds from 1 vanilla bean)
• ¼ cup honey
• ¾ cup vanilla or plain yogurt
• 1/3 cup monk fruit sweetener (I use Lakanto Golden) or brown sugar
• 3 Tbs. butter, melted and cooled
• 1 cup almond flour
• 1 cup coconut flour (or another cup of almond flour, if preferred)
• ½ cup all-purpose, gluten-free flour (I prefer Cup4Cup)
• 1/4 tsp. ground nutmeg
• 1 tsp. baking soda
• ½ tsp. baking powder
• ¾ tsp. salt
• Whipped Cream Topping (optional)
• 1 cup heavy cream
• 1 Tbs. Lakanto Monkfruit Sweetener (or sugar), plus ad -
flour. I also use monk fruit sweetener, which works beautifully as a sugar substitute. I recommend buying a brand that has been blended with erythritol so that you can replace it 1:1 with white sugar, like Lakanto, which makes both a classic variety and a Golden variety that substitutes for brown sugar. It’s available on Amazon, in Walmart, or in health-food stores. This cake is delicious even without the whipped-cream topping.
ditional to taste
• ½ Tbs. pure vanilla extract
• ½ cup mascarpone cheese
• Sea salt to taste
Garnish
• 2 cups sliced strawberries
• ¼ cup toasted sliced almonds
Procedure
1. Preheat oven to 325 degrees F.
2. Grease a 9-inch round pan and line the bottom with parchment paper.
3. In a medium bowl, whisk the eggs, and then whisk in the vanilla extract, honey, yogurt, sweetener or sugar, and butter.
4. In another bowl, sift together the flours, nutmeg, baking soda, baking powder, and salt. Slowly mix the dry ingredients into the bowl with the wet ingredients.
5. Pour the batter into the cake
pan and bake for 22-25 minutes or until a wooden toothpick inserted in the center of the cake comes out clean.
6. Set aside and cool completely. Then invert the pan onto a cooling rack.
7. Make the whipped-cream topping (if using): With a handheld electric or stand mixer, whip the heavy cream until it begins to thicken. Add the sugar and vanilla extract and continue to beat until fluffy. When nearly done, add the mascarpone and a pinch of salt and beat in until mixed. Add more sugar to taste.
8. Top the cake with the whipped cream (if using), leaving a 1-inch border uncovered.
9. Garnish with the strawberries and almonds and serve.
Gluten-Free if using gluten-free flour
Sugar-Free if using monk fruit sweetener
INGREDIENTS:
• 10 medjool dates, pitted
• 1/2 cup dried tart cherries
• 1/4 cup walnuts
• 2 tablespoons rolled oats
• 1/4 cup cocoa powder
• 1 tablespoon chia or hemp seeds (optional)
• 1/4 teaspoon salt
• 2 tablespoons peanut or almond butter
• 4 tablespoons tart cherry juice
• 1/4 cup mini chocolate chips
• cocoa powder (optional)
• melted chocolate (optional)

By family features

F or many, enjoying a small indulgence can serve as a reward for a job well done or a mood-boosting pick-me-up. In fact, mindful snacking is on-trend for a majority of consumers.
According to Mondelez International’s fourth annual State of Snacking Global Consumer Trends Study, 78% are choosing small indulgences to pamper themselves and 68% are checking nutrition labels on snacks.
With today’s changing palates and the growing demand for sour, less sweet foods and beverages, a superfruit like tart cherries can help snackers permissibly indulge without the guilt. Primarily grown on small family farms in the United States, Montmorency tart cherries – also referred to as sour cherries – are available year-round in dried, juice and juice concentrate, canned and frozen forms.
More than 110 scientific research studies show Montmorency tart cherries are a superfruit. In addition to their sweet-sour taste and unique nutri-
ent profile, research suggests tart cherries – one of the few natural food sources of melatonin – may help improve sleep, aid in exercise recovery, reduce inflammation, ease arthritis symptoms, improve gut health and promote heart health. In fact, in one study published in the “European Journal of Nutrition,” adults who drank Montmorency tart cherry juice slept about 40 minutes longer on average and had up to a 6% increase in sleep efficiency.
While increasingly featured in functional beverages and health-positioned foods, tart cherries can also add drool-worthy flavor to superfruit-infused snacks, such as these Tart Cherry Brownie Bites. Plus, using tart cherries as a favorite ingredient in recipes like these adds a health halo to sweets – reinforcing the trend of permissible indulgences.
As an ideal superfruit snack that makes snacking more satisfying, tart cherries provide delicious flavor and potential health benefits in recipes and beyond so you can savor the moment and cherish every bite.
Recipe courtesy of Hannah Zimmerman of Bite Sized Studio on behalf of the U.S. Tart Cherry Industry
Prep time: 10 minutes
Yield: 12 bites
1. In bowl of food processor, combine dates; dried tart cherries; walnuts; oats; cocoa powder; seeds, if desired; salt; and nut butter. Pulse 30-60 seconds until ingredients are ground into tiny pieces.
2. Add tart cherry juice in 1 tablespoon additions, pulsing mixture after each addition, until crumbly dough forms.
3. Transfer dough to bowl and fold in chocolate chips.
4. Roll dough into 12 balls. Serve plain or finish balls with dusting of cocoa powder or drizzle of melted chocolate, if desired.
OR Today is proud to have AORN Connecticut Chapter 0701’s support for the Periop ConneCT conference. The event will be held October 25-26, 2024 at the Omni New Haven Hotel at Yale in New Haven, Connecticut. Join perioperative professionals throughout Connecticut and the Northeast for CE-accredited education, exhibits with leading vendors, and great networking events. Visit our website to see education offered.













Everyone likes FREE stuff and we want to hear from our readers! It is a win-win for everyone involved. Please take a moment to tell us what you like about OR Today magazine.
You could win a $25 gift card! Simply go to ORToday.com/Contest and fill out the short form for your chance to win!


Quatisha Ashley SPS Technician at Hartford Healthcare
“OR Today is a magazine that provides perioperative and SPD professionals with up-to-date news and information about their profession. The magazine educates readers about new guidelines, techniques, and equipment, as well as practical information for career building, problemsolving, and overall wellbeing. It has been serving the perioperative community for over 20 years, offering valuable insights and resources to those in the field. It keeps me informed about developments in the operating room and sterile processing.”
–
Quatisha Ashley, SPS Technician at Hartford Healthcare
“It’s not easy to be a pioneer – but oh, is it fascinating!”
– Elizabeth Blackwell, MD, (the first woman in America to earn a medical degree)


UltraSAFE is an innovative instrument for large biospecimens which allows Perioperative Nurses to handle Pathology specimens in complete safety, with no exposure to formalin fumes. Through the one-way valve lid, UltraSAFE automatically dispenses formalin into specimen buckets utilizing an automatic injection system. The buckets are filled in an enclosed and vented chamber that eliminates operator exposure to formalin fumes. Formalin is dispensed based on specimen weight and specific lab guidelines. Time to fixation, weight of specimen, and exact formalin quantity are recorded on a printed label to ensure standardized documentation.

















I f you find yourself dreaming of sunshine, sand and sparkling pools, it may be time to start looking forward to your next vacation getaway. Get a jumpstart on building excitement for the journey ahead by beginning preparations early, which offers many benefits, including better rates and more time to research your options.
Start exploring ideas for a fun-filled trip with these tips from the travel experts at Funjet, which specializes in providing travelers with vacation packages to hundreds of destinations around the world:
Booking your vacation well in advance allows you to take advantage of the best deals at the most popular hotels and hottest travel dates. In addition, by being flexible with travel dates, families can save hundreds of dollars. Moving travel dates by a day or two can result in major savings, often even more than the discounts you can get on last-minute trips.
Deciding where you want to go is the first step, but with a literal world of possibilities, it can be difficult to narrow down your choices. One place you can find inspiration is by exploring the top travel destinations others are choosing. For example, the top 10 travel destinations booked with Funjet in 2023 include numerous international destinations. Las Vegas is the only U.S. city to make the top 10 list. Mexico is especially popular, with Cancun, Cozumel, Puerto Vallarta and San Jose Del Cabo. Others include Belize City, Belize; Liberia, Costa Rica; Montego Bay, Jamaica; Panama City, Panama; and Punta Cana, Dominican Republic.
Whether you prefer adults-only or family-friendly, luxury or budget-friendly, there’s a diverse range of all-inclusive resorts
to choose from. All-inclusives are known for their convenience and value. They offer hassle-free experiences with meals, drinks and often activities included. While many resorts in Mexico and the Caribbean islands are all-inclusive, be aware that smaller islands like Antigua may feature European planstyle hotels, where meals and drinks are not included.
An all-inclusive package usually encompasses a variety of activities and amenities curated to offer an enjoyable and costeffective vacation. Within these packages, guests often have the opportunity to access amenities such as swimming pools, engage in sports activities, participate in fitness classes and other entertaining experiences.
While all-inclusive resorts make tropical getaways stress-free and economical, it’s customary to express appreciation for exceptional service with tips. Resorts typically don’t require tipping, but guests commonly tip as a gesture of gratitude. When deciding to tip, families should consider modest amounts, like $1-5 per meal per person, and be mindful of different service levels as well as the convenience of using local currency. Having cash on hand makes it easier to tip as needed and ensure you have extra for souvenirs and other purchases.
Although most travelers believe it’s essential to stay connected, it’s a good idea to limit screen time so you can make the most of your vacation. Schedule a specific time, preferably in the morning, to address emails and online tasks then enjoy a worry-free rest of the day. While phones are often used to capture photos and videos or look up information about nearby attractions, putting away the screens means you’ll be able to enjoy the scenery, connect with loved ones and have a truly rejuvenating experience.
Find more tips and plan your next adventure at Funjet. com or call your local travel advisor.






