Prepzyme® Forever Wet creates a long lasting moisture barrier. As seen here, instrument remains wet to the touch for days after application.






Prepzyme® Forever Wet creates a long lasting moisture barrier. As seen here, instrument remains wet to the touch for days after application.

The latest breakthrough in enzymatic pre-cleaning sprays, Prepzyme®
Forever Wet’s unique humectant properties form a moist coating over the instruments that lasts for days.

•The humectant formulation creates a moisture retention barrier which keeps soiled instruments and scopes moist for a prolonged period of time – unlike a GEL which HAS NO MOISTURE RETENTION properties
•Operating room safe, non-aerosol, multi-tiered enzymatic spray helps prevent bio-burden from drying on the surface of soiled instruments and scopes
•Ideal for transporting soiled instruments that may sit for an extended period of time
•Reduces tray weight during transport compared to liquid presoaks
•Soiled sharps are visible through humectant
• Decreases spills and potential cross-contamination

Have you heard of UltraSAFE? UltraSAFE addresses the common issues associated with formalin exposure to create a safer, standardized, and cost-effective solution to the challenges Perioperative Nurses face daily. We all know by now that formalin is carcinogenic and bad for our health. We also know that formalin is the accepted standard and is not going anywhere, which is why it is critical that you advocate for your health to ensure you can manage specimens in the safest way possible. That means ZERO EXPOSURE and complete automation. UltraSAFE offers exactly that. Say goodbye to manual filling and costly spills and take the guesswork out of documentation. With UltraSAFE, time to fixation, weight of specimen, and formalin quantity are recorded on a printed label to ensure the integrity of each specimen. The future is safe; UltraSAFE.

Milestone offers a professional development activity for any perioperative team members who participate in specimen management.








OR TODAY | Summer 2024


The global patient warming devices market is expected to reach $3.2 billion by 2030.

No matter the goal, a stronger core and hips will be foundational throughout one’s life.
LEVERAGING AI TO PROMOTE YOUR PERIOPERATIVE ORGANIZATION
AI can boost evidence-based practices and assist with marketing.

Diet has a huge effect on the brain and one’s mental wellbeing, even protecting against dementia.
OR Today (Vol. 24, Issue #7) Summer 2024 is published quarterly by MD Publishing, 1015 Tyrone Rd., Ste. 120, Tyrone, GA 30290. POSTMASTER: See address changes to OR Today at 1015 Tyrone Rd., Ste. 120, Tyrone, GA 30290. For subscription information visit www.ortoday.com. The information and opinions expressed in the articles and advertisements herein are those of the writer and/or advertiser, and not necessarily those of the publisher. Reproduction in whole or in part without written permission is prohibited. © 2024


PUBLISHER
John M. Krieg john@mdpublishing.com
VICE PRESIDENT
Kristin Leavoy kristin@mdpublishing.com
VICE
Jayme McKelvey jayme@mdpublishing.com
EDITOR
John Wallace editor@mdpublishing.com
ART DEPARTMENT
Karlee Gower
Taylor Hayes Kameryn King
ACCOUNT EXECUTIVES
Megan Cabot
Emily Hise
DIGITAL SERVICES
Cindy Galindo
Kennedy Krieg EVENTS
Kristin Leavoy
ACCOUNTING
Diane Costea
WEBINARS
Linda Hasluem
EDITORIAL BOARD
Vangie Dennis, MSN, RN, CNOR, CMLSO Assistant Vice President, Perioperative Services, AnMed
Justin Fontenot, DNP, RN, NEA-BC, FAADN Associate Professor, Tulane University School of Medicine, New Orleans, LA
Natalie Lind, Education Director for the Healthcare Sterile Processing Association, HSPA
Pat Thornton, MSM, RN, CNOR Perioperative Consultant, RNFA Dermatology Institute
Dawn Whiteside, DNP, MSN, RN, CNOR, NPD-BC, RNFA, Director of Education, CCI
Julie Williamson, BA Director of Communications, HSPA


Hospeco Brands Group (HBG) has completed integration of Ontario-based Innocore. HBG acquired Innocore a year ago, and all existing operations have continued under the Innocore name. Effective immediately, Innocore’s legacy go-to-market teams and activities, including sales, customer support, and marketing, will fall under the Hospeco Brands Group (HBG) name, ready to continue serving Innocore customers.
HBG is a United States-based, full line manufacturer of wiping solutions, personal care, odor control, cleanroom, safety and specialty products to serve building management, industrial and manufacturing, food service, education, health care and life sciences, hospitality and wellness, and a myriad of other markets. The integration ensures Canadian customers benefit from the strength and scale of a large global manufacturer with all the expertise and agility of a single-category provider.
Innocore, now Hospeco Brands Group, is well-known as a leading manufacturer of premoistened, non-woven, surface and
personal wipes, and other hand care products in Canada. The Touch Point brand in the United States and Certainty brand in Canada are now fully integrated into the HBG Signature Bundle of products. The integration complements HBG’s already-robust wipes offering and expands the company’s North American footprint in the wipes market.
Innocore’s legacy management team will now lead all Hospeco Brands Group Canadian business, strengthening the focus and support of this important market. Existing customers will experience no changes in salesperson, pricing or customer support.
Earlier this year, in February, HBG opened a new 58,000-square-foot warehouse next to the legacy Innocore manufacturing facility in Woodstock, Ontario, expanding its Canadian footprint and readiness to serve a growing Canadian customer base.
For more information, visit hospecobrands.com/brands/ formative-brands/innocore.
Hologic Inc. has signed a definitive agreement to acquire Endomagnetics Ltd (Endomag), a privately held developer of breast cancer surgery technologies, for approximately $310 million, subject to working capital and other customary closing adjustments.
“Endomag’s suite of solutions complements our existing breast surgery portfolio and will provide surgeons and radiologists with an expanded range of options to meet the individual needs of more patients undergoing critical breast cancer procedures,” said Erik Anderson, President of Breast and Skeletal Health Solutions at Hologic. “With a global footprint and a similar commitment to women’s health, we are excited about the potential of welcoming the Endomag team and our future opportunities together to increase access to these technologies and better serve patients across the breast health continuum of care.”
Endomag, which is based in Cambridge, United Kingdom, develops and sells breast surgery localization and lymphatic tracing technologies. Its products
include the Magseed® marker for magnetic tissue localization before surgery, the Magtrace® lymphatic tracing injectable for breast cancer staging and the Sentimag® platform, which supports both localization and lymphatic tracing.
“We are delighted to attract the strength and focus of Hologic to power the next phase of our growth,” said Eric Mayes, CEO of Endomag. “Our team is encouraged by our cultural alignment and the potential to strengthen a broader portfolio of solutions to improve women’s health globally.”
Endomag generated approximately $35 million of revenue in calendar 2023. The acquisition is expected to be slightly dilutive to Hologic’s non-GAAP earnings per share in fiscal 2024, break even in 2025 and accretive thereafter.
Completion of the acquisition is subject to customary closing conditions, including regulatory approvals.

The Association for Professionals in Infection Control and Epidemiology recently announced the publication of the Infection Preventionist (IP) Career Development and Advancement Guide.
Developed by the APIC Professional Development Committee, the new guide serves as a comprehensive resource to facilitate recruitment, retention, and promotion of IPs in the changing field of infection prevention and control (IPC) and establishes a framework for implementing the APIC Competency Model to develop and advance IPs.
Due to the pandemic and other market forces, the IPC field is expanding, presenting additional career opportunities in health care settings as well as public health, research, education, and consulting practice settings, highlighting the need for trained and competent IPs. At the same time, 40% of current IPs are approaching retirement age and will soon be leaving the field, creating an urgency to grow the
profession.
APIC’s new guide defines career stages, paths, and ladders, and provides templates and tools to develop job descriptions, competency assessments, training, and professional development plans. It provides direction for career entry and progression to ensure the continuing development and growth of a skilled IPC workforce.
“This is a crucial resource for our profession,” said Tania Bubb, Ph.D., RN, CIC, FAPIC, 2024 APIC president. “We know that competent and knowledgeable IPs are critical to optimize the efficacy of IPC programs. Investing in the growth and development of IPs by providing avenues to enter the field and meet career goals will help to address the IPC demands of the future.”
For more information, visit apic.org.



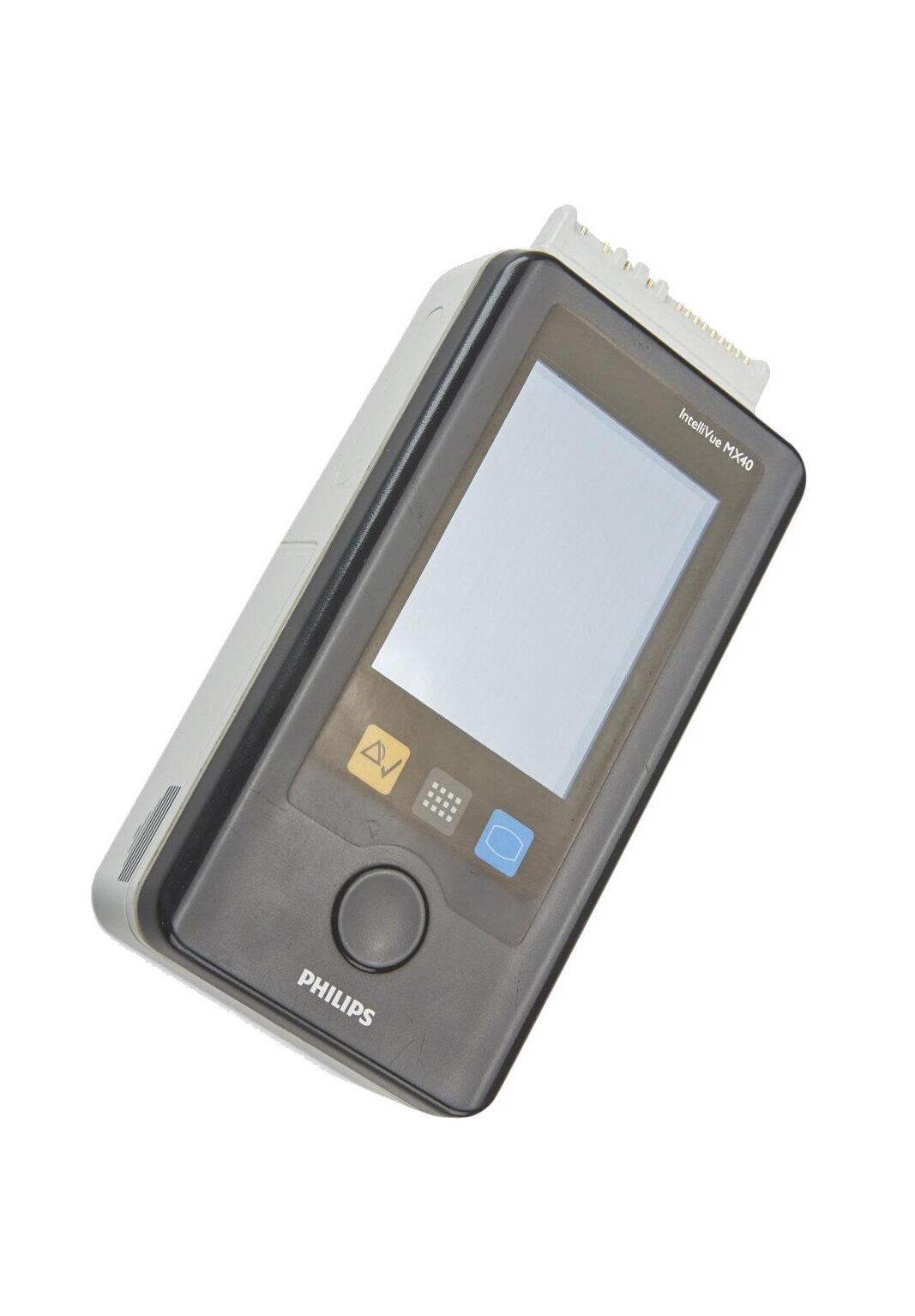
GE HealthCare has received 510(k) clearance from the United States Food and Drug Administration (FDA) for its Portrait VSM vital signs monitor that can provide clinicians with an accurate view of patient vital signs to support timely clinical decisions. As the next evolution of the DINAMAP legacy, Portrait VSM utilizes the SuperSTAT non-invasive blood pressure algorithm to provide precise and accurate measurement readings. Through its wireless connectivity and seamless EMR integration, the portable vital signs monitor was designed with the user workflows in mind, offering customized Early Warning Scores (EWS) and enabling care teams to focus on taking care of their patients by automating routine tasks.
Building on GE HealthCare’s family of Portrait monitoring solutions, Portrait VSM can connect with the latest iteration of the Portrait Mobile wireless and wearable continuous monitoring solution to seamlessly integrate patient data in one unified workflow, while ensuring patient mobility. Through a single click of the barcode scanner, Portrait VSM automatically imports the patient demographic data and a snapshot of the patient’s continuously monitored data - respiratory rate, oxygen saturation and pulse rate - from Portrait Mobile. This workflow streamlines the process of clinical rounding and reduces the steps needed to capture and chart a complete set of vital sign measurements.
A connected workflow and EMR integration can help enable accurate vital sign charting and eliminate the delay from manual data entry to support clinicians in making timely and confident treatment decisions. The uninterrupted flow of data and continuous measurement of vital signs, enabled by Portrait Mobile, can also help clinicians detect patient decline as it is happening, enabling timely intervention before a patient deteriorates.
Patients’ vital signs are typically measured by traditional spot check methods every 4-6 hours, which can cause early signs of patient deterioration to be missed. Undetected patient deterioration, particularly post-surgery, can lead to hazardous yet preventable consequences, with 30-day mortality after surgery representing the 3rd leading cause of death globally.3
To optimize patient care, Portrait VSM brings together standard spot check capability with continuous patient monitoring through its connectivity to Portrait Mobile.
“We remain focused on tackling healthcare’s biggest challenges and driving further efficiencies for care teams through new patient monitoring technology. To help ease the way to more confident care, Portrait VSM offers the clinical performance and capabilities that care teams can trust, so they can spend more valuable time with their patients,” said Neal Sandy, general manager, monitoring solutions, GE HealthCare. “With the addition of Portrait VSM, we are excited about this next step for the Portrait Ecosystem that was designed to support the right level of patient monitoring in observational care through a single, unified workflow.”
GE HealthCare’s Reimagining Better Health study highlighted the burden of inputting and accessing data manually, with nearly half of clinicians reporting that medical technologies at their facilities do not seamlessly integrate with each other.* Portrait VSM offers workflow efficiencies and capabilities to support hospitals and care teams in navigating current challenges they’re facing. Healthcare systems can incorporate and customize EWS protocols into the monitor view to help clinicians recognize the early signs of deterioration in patients and make timely interventions, while limiting manual calculations and transcription. To enable simplified rounding and help avoid delayed measurements, the Round Advisor feature also helps care teams manage and prioritize spot checks for multiple patients by assigning and tracking a sequence of care.
Built on a well-established history of clinical advancements, GE HealthCare’s FlexAcuity monitoring solutions are engineered to adapt to rapidly changing patient needs. GE HealthCare’s technology has been recognized globally for its design, receiving the iF Design Gold Award for Product Design in 2022 for Portrait Mobile and an iF Design Award in 2023 for CARESCAPE Canvas.
Diversey, a Solenis company, has added Oxivir Three 64 to its leading Oxivir product line. Oxivir Three 64 is a one-step hospital disinfectant cleaner that is bactericidal, virucidal and fungicidal all in three minutes at a 1:64 dilution. With more than 70 disinfectant claims, it now leads Diversey’s concentrate lineup of Accelerated Hydrogen Peroxide (AHP) dilution control products, making it fast, effective, responsible and sustainable.
Oxivir Three 64 in use has the best possible safety rating (category IV). Designed for health care environments, the solution is tough enough to clean and disinfect surfaces and equipment in one pass while being gentle on staff and surfaces. It is nonirritating to skin and eyes, requires no personal protective equipment and is compatible with most common health care surfaces and equipment.
In addition to being effective as a one-step, multi-surface, multipurpose disinfectant cleaner, Oxivir Three 64 is an EPA-approved soft surface sanitizer.

“The new Oxivir Three 64 formula raises the bar when it comes to efficacy and speed for our concentrates,” said Larinda Becker, executive director of infection prevention North America. “Health care staff can increase speed and effectiveness with a one-step disinfectant cleaner that is potent against a broad spectrum of pathogens in just three minutes.”
For more information, visit sdfhc.com, contact 800-558-2332 or visit Diversey.com.


Freestyle Partners LLC has announced the results of an in-hospital disinfection study using first-of-its-kind handheld Filtered Far UV-C devices to demonstrate the effective, rapid reduction of healthcare-acquired infection-causing pathogens from certain high-touch clinical surfaces. The study may help to address a major in-hospital challenge of disinfecting high-touch clinical surfaces that often cannot be disinfected by traditional manual methods.
Reducing healthcare-acquired infections (HAIs) is an ongoing and critical need within the global healthcare network. In U.S. healthcare facilities alone, 1.7 million patients contract HAIs annually and HAIs cause 99,000 deaths every year. Surface pathogens can persist for days to months and studies show that 50% of surfaces in healthcare environments do not receive adequate levels of disinfection during manual chemical cleaning. Yearly expenses for the U.S. healthcare system to combat HAIs are estimated between $28-$33 billion.
The study, led by researchers at The University of Texas MD Anderson Cancer Center, showed a statistically significant reduction of surface pathogens known to cause HAIs with the use of the Freestyle Partners handheld Filtered Far UV-C devices on most surfaces tested in clinical work areas of hematologic malignancy and stem cell units in and around patient care areas.
The device has proven effective in preclinical and clinical studies and offers the advantage of ‘no-touch’ disinfection when manual methods are not optimal. The results of the efficacy study work have been accepted and will be presented at several global infectious disease conferences including The Society for
Healthcare Epidemiology of America (SHEA), The European Society of Clinical Microbiology and Infectious Diseases (ESCMID Global) and The International Immunocompromised Host Society (ICHS).
This study continued to validate the highly effective and rapid reduction of harmful pathogens on most high touch surfaces. The devices used implemented patented functionality that enables proper use and achieved desired efficacy.
Filtered Far UV-C is a human-safe, breakthrough disinfection technology that utilizes invisible germicidal light to kill pathogens – viruses, bacteria, spores, fungi –and works in seconds when used in a handheld format, without 2–10-minute wet dwell times required by chemical disinfectants to achieve necessary efficacy.
“This study provides further real-world data on the efficacy of handheld Filtered Far UV-C devices to reduce surface pathogens which we hope could ultimately improve patient care and tackle the tremendous expenses healthcare institutions face in fighting HAIs,” said Jennifer Rosen, co-founder of Freestyle Partners, LLC.
Freestyle Partners, LLC has worked with scientists, technologists, and engineers within the Filtered Far UV-C space to develop prototypes, conduct lab testing, and publish peer-reviewed research on both the efficacy and safety of handheld Filtered Far UV-C devices.
For more evidence-based and peer-reviewed papers in scientific journals that support the efficacy, safety and use of Filtered Far UV-C, visit: freestylepartnersllc.com/the-science.



“No Scrubs” Required –Nothin’ but TLC for Periop!
Periop ConneCT, a premier event for perioperative RNs, CSTs, and SPD professionals in Connecticut and Northeast region, is proud to have the support of ORToday magazine in planning its annual conference October 25-26 in New Haven, Connecticut. Perioperative professionals are invited to attend for CE-accredited education, exhibits with leading vendors, and great networking events.
Periop ConneCT is also excited to introduce poster presentations for this year’s conference. Posters will be on display during exhibit hall hours and will provide attendees with an opportunity to earn additional CE credit. If you are interested in sharing your ideas and work with Periop ConneCT attendees, you can do so with a poster presentation. To submit a poster presentation, visit periopconnect.com/submit-a-posterpresentation The deadline for submissions is August 30, 2024.
Education at the 2024 Periop ConneCT include two keynote addresses. The morning keynote is “What Can You Do To Diminish Implicit Bias?” by Darlene B. Murdock, MSN, BBA, RN, CNOR, CSSM, Clinical Staff RN IV, Memorial Hermann Hospital-Texas Medical Center Research has shown that health care professionals’ biases can lead to disparities in health care. This presentation aims to raise awareness among health care professionals about implicit bias and how it can impact the quality of care they provide. The presenter will share personal stories, engage participants in an exercise to explore their initial thoughts when specific individuals walk into the OR, analyze a case scenario, and lastly provide some strategies to diminish implicit bias.
The afternoon keynote is “Integrity Check: Challenge ‘This Is How We’ve Always Done It’” by Sarah B. Cruz, CSPDT, CRCST, CIS, CHL, Quality Education Program Development Coordinator, The Bone & Joint Institute, Hartford Healthcare. “This is how we’ve always done it.” If you haven’t heard that phrase yet, don’t worry you will. Whether you’ve been on the receiving end or the utterer of it, it’s time to take an honest assessment of why this phrase lingers throughout professional history. Through integrity check, we look to understand the

who, what, when, where, and why of “this is how we have always done it.” This halting phrase is daunting to any professional. Let’s work together to inspire innovation and challenge it for our own professional development and healthcare industry growth!
The educational sessions also cover a wide variety of topics including clinical aromatherapy, joint infections, workplace violence, pain management, incivility, guinging students in the OR and more.
Early bird registration is $75 (valid until 8/31/24). Registration includes full registration and admission to all events, education and exhibits for the duration of the conference. It also includes access to on-demand online education for the event.
Student registration is $30 and requires registration with a university-issued email address.
Regular registration is $100 (after early bird registration expires on 8/31/24). It includes full registration and admission to all events, education and exhibits for the duration of the conference. It also includes access to on-demand online education for the event.
Onsite registration is $125.
ORToday.com Periop ConneCT is offering a limited number of scholarships to attend its annual conference on October 25-26 free of charge. If you find yourself in financial hardship and unable to cover the cost of registration please complete the application the link below to be considered for one of the scholarships. Visit periopconnect.com/scholarships to apply.
“No Scrubs” Required – Nothin’ but TLC for Periop! Come prepared to attend a ’90s celebration like no other! We want to treat you to some TLC with delicious food, an open bar and great music! “No scrubs” required for this event, but if you are heading straight from work, no problem, come as you are!
For more information, visit periopconnect.com.

In a move poised to significantly elevate standards within sterile processing, Crothall Healthcare (Crothall), a leading provider of sterile processing and support services, and Ascendco Health (Ascendco), a leading health technology innovator, announced a partnership that will bring forth a new era for instrument tracking and overall sterile processing quality within health care facilities across the nation.
Together, Crothall and Ascendco are revolutionizing efficiency and safety in SPD departments by combining Crothall’s expertise in data-driven processes and Ascendco’s cutting-edge instrument tracking technology to empower SPD professionals with the tools and knowledge necessary to achieve the highest levels of efficiency, accuracy, and patient safety.
“This partnership represents a significant leap forward for Sterile Processing,” expressed Afif Escheik, BA, a-IPC, CHL, CER, CIS, CRCST, CST, regional director of operations at Crothall Healthcare. “Ascendco’s dedication to technological advancements perfectly complements Crothall’s expertise in implementing best practices. Together, we can make a profound impact on patient safety and the overall quality of surgical services.”
Through a rigorous, data-driven approach, Crothall has achieved a remarkable record in sterile processing that has yielded an audit compliance improvement of approximately 90%, process errors reduction by up to 50%, and productivity gains of up to 62%. These industry-leading achievements, coupled with Ascendco’s innovative technology, promise to propel sterile processing practices to new heights making a significant impact on patient safety and quality of service.
Ascendco’s Sonar Tracking System, the industry’s most comprehensive and effective platform for surgical device management, will be a cornerstone of this partnership. Sonar’s ability to meticulously track instruments throughout the entire surgical workflow provides invaluable data and insights, optimizing instrument efficiency and minimizing the risk of errors.
As a result of Ascendco’s Sonar platform, sterile processing departments have reduced immediate use steam sterilization (IUSS) rates by up to 10%, sterile return rates by up to 25%, and return to decontamination rates by up to 5%. These metrics are indicators for improved workflow efficiency, better inventory management, enhanced quality assurance, and improved cleaning and decontamination processes.
“We are delighted to join forces with Crothall Healthcare, a renowned leader in the sterile processing domain,” said Brian Reed, CEO of Ascendco Health. “Their unwavering commitment to quality aligns perfectly with our mission to revolutionize sterile processing. Together, we will empower sterile processing professionals and Crothall workers with the tools they need to ensure all products going into the operating room are ready for use.”
The collaborative efforts of Crothall and Ascendco will culminate in the development of industry-leading protocols and analytics designed to empower sterile processing technicians with the knowledge and tools to consistently deliver exceptional results. This will ensure that sterile processing departments across the country can operate at the peak of efficiency and quality, ultimately safeguarding patient well-being.
Healthmark o ers the TEMP-USB-TH and TEMP-USB-TP to help you monitor the temperature and humidity of your department with ease

TEMP-USB-TP
• Features dual temperature probes which can gather over 250,000 readings (-40 to 257ºF)
• Perfect for measuring the temperature of sinks, ultrasonic baths, warming cabinets, refrigerators and other applications where a probe is needed to measure the temperature.
• Measures over 250,000 temperatures and humidity readings ranging from -22 to 176ºF
• Measures 0 to 100% relative humidity

hmark.com | 800.521.6224 | healthmark@hmark.com

For more of Healthmark’s innovative temperature monitoring solutions for instrument reprocessing & safety, visit
hmark.com
You don’t have to work in health care to be familiar with the Change Healthcare ransomware attack that occurred earlier this year. That hack caused billing disruptions across the country and inspired congress to convene hearings to begin exploring how the breach occurred and what steps to take to prevent comparable attacks in the future.
What you might not know, says Dr. Paul Alcock, chief information security officer for Surgical Information Systems and adjunct professor of cybersecurity at New York University, North Carolina State University and the University of Central Florida, is that although attacks on large companies make headlines, cybersecurity breaches are much more prevalent in small and medium-sized businesses. Also, the number one industry targeted by those attacks is health care.
Alcock and I recently sat down together to record an episode of ASCA’s Advancing Surgical Care Podcast titled “Cybersecurity for Surgery Centers.” Although most of ASCA’s podcast listeners work in surgery centers, health care professionals in many settings can benefit from the advice Alcock shares. Anyone can listen for free using a link on ASCA’s website (www.ascassociation.org/cyber-podcast) or the podcast
hosting platform of their choice. I encourage everyone reading this column to take time to listen to this valuable 12-minute program.
One reason health care entities are especially vulnerable to cybersecurity hacks, Alcock says, is the interconnectedness of the health care ecosystem. The dependence health care entities have on third-party vendors for critical business functions is another. One reason small businesses are often targeted, he adds, is that they tend to believe that because they are small, adversaries are not concerned with their data when, in fact, the opposite is true.
No matter what controls a facility puts in place, Alcock concedes, some level of risk remains. Since that risk can never be eliminated entirely, he encourages organizations to reduce it as much as possible. As a beginning, he recommends some practical, low-cost solutions that organizations can use to frustrate potential attackers enough that they will move on to their next target. Those include:
• identify any obvious vulnerabilities by starting with an internal risk assessment (he mentions some free resources that can help and talks about when hiring professional assistance makes sense);
• evaluate your business relationships with your thirdparty vendors from an IT
perspective;
• determine what data might interest your adversaries most and how they might attack, then look for security gaps that should be addressed;
• implement strong password management policies;
• leverage multi-factor authentication;
• update and patch your systems regularly;
• deploy some antivirus protections;
• train your employees; and
• invest a little time and money on the front end that could save you a great deal of time, money and energy on the back end.
Organizations with greater financial resources, he says, can create a more robust cybersecurity program that incorporates more advanced technologies, expertise and processes.
If a hacker does manage to break through your defenses, Alcock says, your reputation and future viability will largely depend on how well you respond. To help, Alcock recommends preparing an incident response plan well before any attack occurs, having a cyber insurance policy in place, ensuring quick access to a third-party consultant that can help with a response if one becomes necessary and more.
When it comes to cybersecurity, Alcock says, there is no endgame. Because the threat landscape is always
evolving and “the bad guys” are always trying new tactics, facilities that want to remain protected need to constantly review the protections they already have in place and make sure they remain relevant.
In a whitepaper titled “The State of Ransomware 2024,” cybersecurity company Sophos reports that high ransom demands are no longer limited to high-revenue organizations and expectations of payouts of $1 million or more have become commonplace. In fact, the average ask among 1,701 organizations that had their data encrypted and contributed data to the report was $4,321,880. Also, according to that report, other recovery costs associated with attacks typically exceed $1 million and average $2.73 million across businesses of all sizes. Health care entities of all shapes and sizes need to protect themselves from that
kind of risk. I encourage you to listen to Alcock’s advice and make sure that cybersecurity is a top priority in your facility today.
Before I sign off, I have one reminder on an entirely separate matter specifically targeted to ASCs. As I have pointed out in this column before, beginning in 2025, as part of Medicare’s ASC Quality Reporting Program, ASCs must conduct the Outpatient and Ambulatory Surgery Consumer Assessment of Healthcare Providers and Systems (OAS CAHPS) Survey or face reduced Medicare reimbursement rates in 2027 and beyond. ASCs cannot administer these surveys on their own, but at last count, only about a quarter of Medicare-certified ASCs had authorized a Medicare-approved vendor to conduct the survey in their facility. Survey vendors have informed
ASCA that they do not have the capacity to sign up all the ASCs that are not already administering this survey at the same time, and ASCs that are already participating have indicated that while setup can take many weeks or more, making certain an ASC achieves the high scores it deserves can take even longer.
I encourage every ASC that participates in Medicare’s ASC Quality Reporting Program to start now to select a vendor and begin administering this survey as soon as possible. Delaying any longer could cause your facility to be noncompliant in 2025. If you don’t know where to begin, visit ASCA’s website (www.ascassociation. org/prepare-oas-cahps) for help.
– Bill Prentice, ASCA CEO

n the constantly changing landscape of health care, it is crucial to acknowledge and cultivate excellence in nursing. The Competency & Credentialing Institute (CCI) is dedicated to this aim through its prestigious award programs: CNOR Strong and TrueNorth. These programs go beyond mere recognition; they are designed to promote a culture of innovation, continuing education, and excellence in the perioperative nursing profession through certification.
I
Studies have shown that nurses who have obtained the CNOR credential are more confident in their clinical practice. They have validated their specialized knowledge in perioperative nursing and placed a higher value on a culture of safety (Wright, et. al., 2021). A team of CNOR-certified nurses who have mastered the standards of perioperative practice, fostered a culture of professionalism, and demonstrated improved outcomes in surgical patients (Boyle, et. al., 2014) are what we refer to as CNOR Strong at CCI.
The CNOR Strong program highlights the facilities and health systems where at least 50 percent of eligible perioperative nursing staff are
CNOR-certified but also consistently recognizes and rewards nurses who become CNOR-certified or maintain their certification. This initiative began in 2016 and celebrates the dedication, expertise, and commitment to delivering top-notch patient care. Those interested in becoming a CNOR Strong awardee should continue to promote certification and advocate with leadership to support nurses interested in becoming certified to help attain the fifty percent certification requirement.
CNOR Strong is not only an award; it is a recognition of the exacting standards that these nurses and facilities uphold every day, ensuring the safety and well-being of their patients throughout the perioperative journey. An average of 150 recognitions are granted during each award cycle.
CCI’s TrueNorth Award, which was launched in 2013, celebrates facilities that prioritize certification as a guiding principle for their perioperative nurses. Strong leadership and organizational support for certification are often crucial in a nurse’s decision to obtain and maintain certifications (Wright, et. al., 2024) and are essential factors for recipients of this award. TrueNorth awardees and nominated facilities set outstanding standards of excellence in perioperative certification, emphasizing the signifi-
cance of continuous learning, proficient practice, and promoting excellence and patient safety. Every year, the TrueNorth award is given to a single winner who receives funding for a celebratory reception, an award presentation by CCI leadership, and access to professional development activities at no cost.
To be eligible for this award, facilities must submit a comprehensive application that outlines how they acknowledge and incentivize certified nurses. The application must also provide proof of the positive impact certification has on patient outcomes and staff performance. We highly recommend that applicants take the time to prepare their information in advance before transferring it into the application. This not only allows for a thorough review of spelling, grammar, and word count, but also ensures that applicants can easily organize and adjust their information as needed. Additionally, utilizing bullet points can make the information more streamlined and easier to understand. Taking these small steps can make a substantial difference in the success of your application.
CNOR Strong and TrueNorth are programs that aim to empower nurses and acknowledge their contribution to the health care landscape. These programs inspire nurses to push the boundaries of their practice, driving innovation
and improvement in patient care. Each of these programs accepts nominations yearly, and self-nomination of a facility or system is encouraged. The application period for CNOR Strong opens on November 1 and closes on December 31. TrueNorth nominations are accepted beginning October 1, with the window closing on November 30. Innovation is crucial to healthcare, and CNOR Strong and TrueNorth fosters a culture of innovation within the perioperative nursing profession. Award recipients often represent the forefront of innovative ideas and practices, pushing the boundaries of what is possible in the field. By recognizing and celebrating their achievements, CCI aims to boost nurses’ morale and confidence while encouraging them to embrace innovation

in their own practice, ultimately benefiting patients and sharing their learnings with colleagues.
The impact of CNOR Strong and TrueNorth extends far beyond individual recognition for facilities or health systems. These programs have a ripple effect throughout the nursing community, inspiring others to aim for excellence. By showcasing the exemplary work of certificants, CCI not only honors their achievements but also sets a high standard for the profession, driving continuous improvement and raising the bar for patient care everywhere.
1. Wright, M. I., Polivka, B., PhD., R.N., F.A.A.N., & Abusalem, S., PhD., R.N. (2021). An examination of factors that predict the perioperative cul -
ture of safety: The official voice of perioperative nursing. AORN Journal, 113(5), 465-475. doi: https://doi. org/10.1002/aorn.13373
2. Boyle, D.K., Cramer, E., Potter, C., Gatua, M.W. and Stobinski, J.X. (2014), The Relationship Between Direct-Care RN Specialty Certification and Surgical Patient Outcomes. AORN Journal, 100: 511528. doi: https://doi.org/10.1016/j. aorn.2014.04.018
3. Wright, M.I., Sha, S., Hall, L.A. and Hessler, B. (2024), Factors in the Perioperative Nurses’ Work Environment That Predict Work Engagement. AORN J, 119: e1-e12. doi: https://doi.org/10.1002/aorn.14095

– Melissa McKewen is the director of marketing and business development at CCI.


S terile processing (SP) professionals must work toward excellence with every action and interaction they undertake. Unfortunately, significant time and attention go toward addressing challenges and disruptions, so the successes of the department aren’t always prioritized, shared or celebrated. The challenges SP professionals face each day can range from instrumentation and information technology (IT) to mechanical challenges and difficult personal interactions. Regardless of the challenge, the resolution must be swift and appropriate.
The key to tackling SP-related challenges lies in effective troubleshooting and assessment. This practice involves searching for the source of the problem and correcting it to make a process or practice whole or functional again. A wise question SP leaders can ask is: “What tools are being given to technicians to become better at troubleshooting?” Many times, SP leaders may face a challenging issue that technicians do not know how to address. Perhaps they did not know where or how to look for the answer, or instead of reporting it, maybe they simply assumed that the next person would address it. Does your staff make
the initial call for equipment repairs with the vendor or the facility’s biomedical engineering team, or do they report it to leadership?
Troubleshooting can be effective for addressing mechanical issues, departmental processes, and even personal interactions. Often, SP team members aren’t comfortable troubleshooting. Perhaps they believe they do not have the authority to troubleshoot, or that it is only the leader’s responsibility. That assumption can be detrimental to the department’s success. SP leaders should encourage every team member to speak up and bring their ideas and concerns to the forefront immediately.
There are several key troubleshooting steps that will have all team members identify problems and become part of the solution. Utilizing these tools will not immediately guarantee success, but continuing to work with them will help develop a clear path to success and problem mitigation.
Pinpoint the problem. The first step in problem solving is knowing a particular problem exists and determining its root cause. Some things occur that can just be a fluke, not a root cause. Start by asking questions about the problem and seeking answers to those questions. Once the questions uncover specific problems, address each problem before moving to the next. An example would be soiled in-
struments coming through the washerdisinfector. Are the soiled devices the result of poor manual cleaning, inadequate point-of-use treatment, a defect with the washer, or a combination of all these factors?
Consider this scenario: The technician in decontamination sees an instrument tray came from the operating room (OR). It was sprayed at the point of use and organized. The technician bypassed the manual cleaning and goes straight to the washer. The technician fails to realize that the conveyor taking the rack to the washer is jammed. The rack does not go immediately into the washer and is delayed for more than two hours before he notices it. And on this day, the washer has a blocked spray arm that is not producing the appropriate flow of water. We can also add that there was no hand-off communication to identify that this one-of-a-kind tray is needed for another case. The tray comes through the washer, and it is visibly unclean. As one can see, the answer is not always an obvious one.
Establish probable cause. The next step is creating a list of the probable causes or concerns. Break out the causes into various categories and reflect on each separately and in the order of the process, listing them from the highest concern to the lowest. It is prudent to have several people involved in all processes to gain per-
spective and capture all opportunities. Seek out the advice of someone who is doing the task routinely, even if they are less experienced. Often, leaders have years of experience but may no longer be experiencing the issues personally.
Again, using the previous scenario, consider the following:The technician makes the decision to skip manual cleaning.There was the fact that the conveyor did not activate as it should, and the washer spray arm was blocked. Additionally, the department did not know the tray would be needed for a later case. It is necessary to break down each challenge and troubleshoot each step.
Determine the action plan. Be sure to include all individuals necessary to help determine the plan of action. If it is necessary to include an outside vendor or an in-house IT or BME colleague, invite them to participate. Do not overlook others who can bring vital information to the team. Identify any specialty equipment or supplies to help achieve the desired outcome. Evaluate and rule out all possibilities that may be creating the challenges.
As we now know, the example scenario is truly multiple challenges wrapped into one. Breaking it into steps and reviewing each from the beginning is crucial to determine the best solution(s). Some may mistakenly stop at the point of the technician’s error with manual cleaning. It is advised, however, to follow the process to identify other outliers that could be contributing factors for the process failure.
Implement the plan. When determining the plan of action, one may find there are several options. The key is to implement one plan at a time. Implementing multiple changes at once could prove detrimental to the plan and outcomes. Successfully implementing a plan requires that each step be taken one at a time. If a failure still exists, reverse the steps to find the culprit. There may need to be an adjustment to a single step.
In continuing with the scenario example, it can be easy to immediately assumed the problem is limited to the technician not performing a critical step, but there are numerous other contributing challenges – the conveyor failure, the spray arm blockage and the communication oversight. If the leader stops at the technician’s mistake, they will never fully address the other challenges that be less obvious but no less egregious.
Document and share the findings. Once the problem, action plan and implementation strategy are identified and determined, it is vital to document the challenges, proposed solutions and findings. That information should then be shared with staff and others as needed (e.g., customers, infection preventionists, biomedical staff, executives). Establish an effective way to communicate the steps associated with troubleshooting the challenge. Consider laminating and posting the material in the department, or distributing it in an email for all stakeholders to access.
In our scenario, the leader found that the technician did skip a step
and that they can be easily coached or reviewed with a competency to assure the technician is aware of the oversight and understands the correct process.The conveyor and spray arm can be addressed by the service technician coming in to review the equipment and perform preventive maintenance.Again, the technician will be reminded of his responsibility for ensuring the conveyor is activated and working properly and that the spray arms inside the washer have movement and clear flow. Additionally, the issue of the tray not being identified as being needed later should be captured with possible updates to preference cards (review the interface of the preference card and the instrument tracking system if used).Another solution is to identify one-of-a-kind trays with a distinct color label.This serves as a visual reminder for all staff to prioritize those trays.
Learning troubleshooting techniques and practices is beneficial to the entire SP team, regardless of their position and experience level. The goal is to work as a team to identify problems earlier, proactively find the most effective solutions and document the process and results. Doing so helps contribute to greater outcomes for the patients as well as the SPD and the customers its serves.
– Tony Thurmond, CRCST, CIS, CHL, FCS, serves as sterile processing manager for Dayton Children’s Hospital. He is an HSPA Past-President and serves as an HSPA columnist.
Operating room surgeons and technicians trust STACOOL VEST to keep them cool during long and intense procedures.



The StaCool Vest™ is the most lightweight, comfortable body cooling system available. It uses highquality, durable materials and easily replaceable ThermoPaks to cool the body core efficiently.
Made from comfortable, breathable Airprene
Nontoxic and nonflammable ThermoPaks
Spandex sides for additional comfort and flexibility
Front zipper for easy dressing and removal
Lightweight – adult sizes are 5 to 5½ pounds with hydrated ThermoPaks
Wear under or over scrubs
Available in a wide range of sizes to fit any body type
Made in the USA

I recently wrote on the salient issue of nursing burnout and the staffing issues resulting from nurses leaving the profession. This month, I would like to turn to some very recent research on the reasons why health care professionals suffer burnout and leave employment. Linda Aiken and her co-authors in a study published in 2023 in the JAMA Health Forum state that, “Disruptions in the hospital clinical workforce threaten quality and safety of care and retention of health professionals.”1
Aiken and her team studied Magnet facilities and found that, “… hospitals characterized as having too few nurses and unfavorable work environments had higher rates of clinician burnout, turnover and unfavorable patient safety ratings.”1 Similar studies for clinicians in six European countries report comparable findings.2 In a study of the top factors for nurses ending health care employment in the years 2018-2021, 41% ended their employment for reasons other than a planned retirement.3 Of those respondents 22% cited burnout or emotional exhaustion and 18% cited insufficient staffing.3 These studies bring the consequences of unfavorable work environments and staffing shortfalls into sharp relief. Most notably, nurses younger than 30 cited emotional exhaustion (43%) and insufficient staffing (40%) as their reasons for leaving health care employment.
As Aiken and colleagues state, it is important to know which interventions the workers believe are effective in decreasing the contributing factors to burnout. A recent debate has centered on whether to build the resiliency of the workforce or
devote resources elsewhere. In these three studies doctors and nurses, when selecting from a list of potential interventions to improve the work environment, rated current popular options such as resiliency training, workplace champions and quiet places in the work setting as the least favored choices. These interventions, although popular with health care leadership, have not yet stemmed the tide of burnout and staff exits. We now come to a crucial choice. Do we stick to current methods which have not yet proven effective and are disliked by clinicians or try new approaches identified by the clinicians?
Nurses and doctors in these recent studies offer possible solutions to include better nurse staffing ratios, improved work environments which allow scheduled, uninterrupted breaks, no unscheduled work assignments, more clinician control over work assignments and additional resources devoted to supporting clinicians new to practice.1 This would entail markedly higher labor costs for nursing, but training more providers or placing more emphasis on recruiting will not solve this problem.
It is possible that staffing issues may reach a crisis point where regulatory bodies impose a solution such as mandatory staffing ratios as a condition of participation. Conspicuously, CMS has recently proposed staffing ratios for nursing homes.3 Large scale, systematic changes to the work environment are possible. One example, the changes in physician resident work hours in the early 2000s.
A common theme emerges from these three articles. A sizable portion of the respondents do not trust management to address legitimate safety concerns or create better work environments. In this first study nearly a third of the respondents said their values did not align with that of management.
If we accept that workforce shortages will inevitably cause safety and quality issues and worsen retention issues, we should be attentive to the responses from clinicians.1,2,3 Clinicians increasingly believe that facilities’ leaders have control over issues which negatively impact their work. The fundamental disconnect facility leaders either cannot or will not institute feasible, evidence-based solutions known to clinicians. The evidence, as manifested in prolonged staff shortages, is increasing and pizza parties and more resiliency training may not be enough to reverse the trend.
1. Aiken, L. H., Lasater, K. B., Sloane, D. M., Pogue, C. A., Fitzpatrick Rosenbaum, K. E., Muir, K. J., McHugh, M. D., & US Clinician Wellbeing Study Consortium (2023). Physician and Nurse WellBeing and Preferred Interventions to Address Burnout in Hospital Practice: Factors Associated With Turnover, Outcomes, and Patient Safety. JAMA Health Forum, 4(7), e231809. https://doi.org/10.1001/jamahealthforum.2023.1809
2. Aiken, L. H., Sermeus, W., McKee, M., Lasater, K. B., Sloane, D., Pogue, C. A., Kohnen, D., Dello, S., Maier, C. B. B., Drennan, J., McHugh, M. D., & Magnet4Europe Consortium (2024). Physician and nurse well-being, patient safety and recommendations for interventions: cross-sectional survey in hospitals in six European countries. BMJ open, 14(2), e079931. https://doi. org/10.1136/bmjopen-2023-079931
3. Muir, K. J., Porat-Dahlerbruch, J., Nikpour, J., Leep-Lazar, K., & Lasater, K. B. (2024). Top Factors in Nurses Ending Health Care Employment Between 2018 and 2021. JAMA network open, 7(4), e244121. https://doi.org/10.1001/ jamanetworkopen.2024.4121

– James X. Stobinski, Ph.D., RN, CNOR, CSSM(E), CNAMB(E)

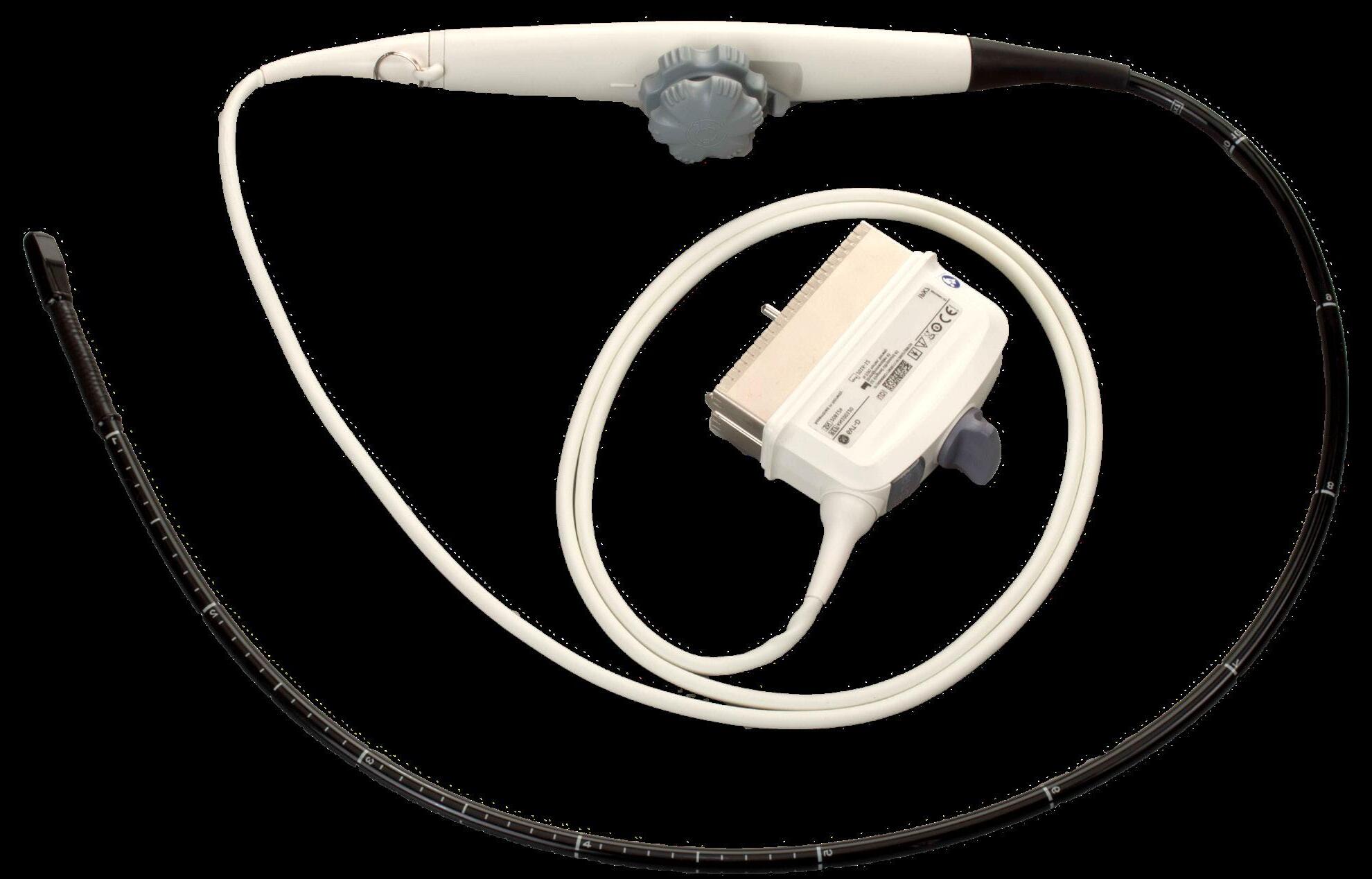
A t first impression, the idea of using a surgical instrument to inspect surgical instruments might sound silly. After all, aren’t there better tools for maintaining endoscopes and lumened instruments than…other scopes? Well, perhaps not. That’s at least according to a team of researchers who recently determined that borescopes are well-suited to visually inspect the tubes that transport liquids or gasses during a medical procedure.
To be clear, the use of borescopes to inspect the nooks and crannies of devices like endoscopes is nothing new. After all, what tool would be better suited to inspect the narrow channels of an endoscope – a kind of borescope specialized for inspecting the insides of a patient – than the kind designed for getting a camera into a tight space? However, the study, titled “Beyond Endoscopes: Pilot Study of Surgical Instrument Lumen Inspection,” aims to address a noted lack in information about using borescopes to inspect lumened instruments other than endo-
scopes, ensuring they’ve been properly cleaned and maintained before being sterilized for patient use. A lumen is a cavity or channel within a tubular device specifically designed to transport liquids, gasses, or even small surgical implants into a patient’s body.
“Our goal with this research was really to explore if borescope inspections can bring the same kind of value to inspection of surgical instrument lumen as they have with inspecting endoscope channels,” said Krystina Hopkins, research manager at Ofstead & Associates, who helped lead the study.
She emphasized the importance of examining whether borescope inspections could provide beneficial information for reprocessing professionals. Borescope inspections were systematically conducted on arthroscopic shaver handpieces and suction tubes that are regularly cleaned and sterilized.
Results from the study revealed unexpected complexity within instrument lumens, including common architectural features in devices that can lead to debris accumulation. Despite efforts to clean the instruments thoroughly, debris remained persistent in some devices, leading to the replacement of those instruments.
This underscores the challenges in cleaning instrument lumens and highlights the need for improved inspection and maintenance protocols, the authors noted.
Hopkins emphasized the importance of having a comprehensive plan in place to address findings from inspections, as unexpected issues are likely to arise. She also highlighted the need for industry-wide standards and guidelines to guide frontline personnel in conducting effective inspections and responding to findings.
Looking ahead, Hopkins mentioned plans for the “Lumens 2.0” study to expand on their findings and encouraged further research in the field. She emphasized the role of standards organizations like AAMI in developing guidance that can supplement current manufacturer instructions, ultimately enhancing patient safety and instrument reliability.
The study, launched by Cori L. Ofstead, MSPH, president and CEO of Ofstead & Associates, marks a significant step toward improving the quality and safety of surgical instrument processing through innovative inspection techniques and collaborative industry efforts.






t first impression, the idea of using a surgical instrument to inspect surgical instruments might sound silly. After all, aren’t there better tools for maintaining endoscopes and lumened instruments than … other scopes? Well, perhaps not. That’s at least according to a team of researchers who recently determined that borescopes are well-suited to visually inspect the tubes that transport liquids or gasses during a medical procedure.
A
Surgical settings strive to provide quality care but aren’t immune to adverse events with an associated risk of patient harm. Hospitals and ASCs know that QAPI is mandatory and comprehensive of all departments. Tracking, trending, measuring, monitoring – all familiar concepts. And yet, the Centers for Medicare and Medicaid released a quality and safety memo on March 9, 2023, noting that QAPI
Conditions of Participation deficiencies are the third most cited of the 24 CoPs for Medicare participating hospitals.1
Activate through Ownership
Regulatory agencies expect to see a well-designed and well-maintained quality program that addresses aspects of performance including processes of care, contracted services, and internal operations.
While the organization’s governing body ultimately ensures that a data driven program is in place,2 individuals
and teams can – and should – be engaged in identifying meaningful measurement goals (benchmarks) for the work they do. Offer guidelines for consideration when determining quality indicators:
• What is the established benchmark? Is it based on nationally-recognized standards of practice, or on the organization’s own history of performance?
• What is the sustainability time frame? If the benchmark is met consistently, do you increase the level of challenge or add a new metric?
• Who owns oversight of QAPI reporting? At the team/department level? At the organization level?
• How do the selected quality indicators demonstrate improved health outcomes or a reduction in medical errors?
Building individual ownership of quality is the best way to avoid the need for improvement based on an adverse event.
In addition to activating your quality proactively, consider QAPI data in adverse event analysis.
In the surgical setting, an adverse event, or worse, a “never event,” requires immediate investigation. Perhaps a piece of equipment failed, an incorrect dose of medication was given, or a wrong site procedure took place. Calling attention to the issue alone is not sufficient to drive sustainable improvement. Uncover the “why” and “how” by conducting a root cause analysis (RCA).
RCA is your key to a dynamic and effective QAPI response to an event.
Pinpoint the underlying factors or causes of the failure. Don’t hesitate to dig deep into “why.” Did someone miss scheduling preventive maintenance or performing a routine calibration? Did an employee miss an important step? Why? Lack of documentation? A communication error? Were instructions readily available? Is there a flaw in the training program?
Next comes the “how.” How will you fix it? Your goal is to avoid recurrence, so that the correction sticks. Use your RCA to choose the best single action – such as creating work instructions for maintaining each piece of surgical equipment, or refreshing staff education. Select the fewest number of actions that will create improvement. Throwing the kitchen sink at the problem means you’ll never know what was really effective.
The Agency for Healthcare Research and Quality (AHRQ) Patient Safety Network published a case study chronicling one procedure that encompassed two never events: wrong patient and wrong side.
“A first-year orthopedic surgery resident was consulted to aspirate fluid from the left ankle of a patient in the intensive care unit. The resident, accompanied by a second resident, approached the wrong patient, obtained consent from the patient’s wife via telephone, and inserted the needle into the patient’s right ankle. At this point, a third resident entered the room and stated that it was the incorrect patient. The procedure was immediately terminated, and the needle was with-

The “Patient Warming Devices-Global Strategic Business Report” has been added to ResearchAndMarkets.com’s offering. It predicts that the global patient warming devices market will reach $3.2 billion by 2030.
The global market for patient warming devices estimated at $2 billion in the year 2022, is projected to reach a revised size of $3.2 billion by 2030, growing at a CAGR of 5.9% over the analysis period 2022-2030.
Surface warming systems, one of the segments analyzed in the report, is projected to record 4.7% CAGR and reach $1.3 billion by the end of the analysis period. Growth in the intravascular warming systems segment is estimated at 7.2% CAGR for the next 8-year period.
The patient warming devices market in the U.S. is estimated at $715.9 million in the year 2022. China, the world’s second largest economy, is forecast to reach a projected market size of $451.9 million by the year 2030 trailing a CAGR of 8.1% over the analysis period 2022 to 2030.
Among the other noteworthy geographic markets are Japan and Canada, each forecast to grow at 4.2% and 5.5% respectively over the 2022-2030 period. Within Europe, Germany is forecast to grow at approximately 4.8% CAGR.
According to a report published by Growth Plus Reports, the global patient warming market is expected to reach
$2.98 billion by 2031 and to grow at a CAGR of 7.5% during the forecast period.
The global patient warming market is experiencing substantial growth, driven by the increasing prevalence of surgical procedures, growing awareness of the importance of maintaining normothermia during surgery, and technological advancements in patient warming devices. A comprehensive analysis of the market reveals a dynamic landscape dedicated to improving surgical outcomes, reducing the risk of perioperative complications, and enhancing patient comfort.
The global patient warming market features a competitive landscape with key players contributing to research, development and commercialization of patient warming devices.
While the patient warming market presents significant opportunities, challenges such as concerns about device efficacy, regulatory compliance, and the need for standardized warming protocols need to be addressed. However, ongoing research, technological advancements, and the potential for market expansion in emerging economies offer avenues for growth and innovation in patient warming solutions.
The global patient warming device market size was $4.0 billion in 2022 and is expected to register a revenue CAGR of 8% over the forecast period, according to a report by Reports and Data.
The market for patient warming devices is experiencing growth due to the
increasing incidence of chronic diseases such as cancer, diabetes, circulatory and heart conditions. Additionally, the global aging population is more susceptible to hypothermia. Therefore, the demand for patient warming devices is expected to rise over the forecast period.
Furthermore, the market revenue is growing due to the increasing adoption of advanced technologies including forced-air warming, conductive warming, and radiant warming. These cutting-edge technologies aim to enhance patient outcomes and improve warming efficiency. Additionally, there is a rising demand for disposable patient warming blankets and mattresses, driven by an increased focus on infection prevention and control measures in hospitals and other health care settings.
Moreover, the COVID-19 pandemic led to a higher number of critically ill patients, increasing the demand for patient warming equipment in hospitals and intensive care units. The pandemic has also spurred the development of innovative patient warming technologies designed to enhance patient comfort and reduce the risk of infection transmission.
Furthermore, government initiatives to improve patient care services and health care infrastructure in developing nations are contributing to market revenue growth.
Attune Medical’s ensoETM modulates and controls patient temperature through a single-use silicone tube inserted into the esophagus, similar to a standard gastric tube, and connected to an external heat exchange unit. Positioned in the esophagus, next to the heart and great vessels, water circulates inside the closed-loop system to efficiently warm or cool a patient. Unlike surface devices, the ensoETM’s internal placement won’t impede patient access during procedures in the OR, ER, ICU, or electrophysiology lab for various temperature management applications. The ensoETM works with existing heat exchangers and is the only device cleared for use in the esophagus for patient temperature modulation.
IN THE OR product focus


Baxter products featured at AORN 2023 included the commercial launch of a new conductive Baxter Patient Warming System designed to help achieve and maintain patient normothermia (body temperature within standard limits). The system eliminates the need for disposables, as the warming technology is built into the table pad, which can reach temperatures up to 40 degrees Celsius. In addition, reusable conductive warming blankets can reach temperatures of 43 degrees Celsius and provide an increased surface warming area to help quickly warm from above and below. The system is also air-free, which may reduce risks associated with forced air systems1 – such as contamination of the surgical site – and operates quietly. This warming solution can also be combined with WaffleGrip, a positioning accessory that helps keep the patient warm and secure in the steep Trendelenburg position, in which a patient is tilted head-down at up to a 45-degree angle. The Baxter Patient Warming System is compatible with its TS7000, TS7000dV and PST 500 surgical tables.
1 Mehta V. Comparison of forced air and conductive heating systems during outpatient orthopedic surgeries. Journal of Anesthesia and Surgery. 2018. https://doi.org/10.15436/2377-1364.18.1771.
MAC Medical’s Blanket & Fluid Warming Cabinets offer an unparalleled range of sizes and options ensuring the ideal customer solution. Available in single, dual, and triple chamber configurations accommodating blanket, intravenous fluids, and irrigation solution warming at different temperatures in each chamber. With Easy Log data recording and USB Data management standard on all models, documentation requirements are streamlined. Computer-controlled convection heating and fully insulated cabinetry supply consistent temperature management throughout. Manufactured in the USA, each MAC Medical Warming cabinet features a “Built to Last” warranty.

For more information, visit www.macmedical.com.
Level-up: the established efficiency of the HotDog Patient Warming System is now enhanced by the Warming Mattress+Return Electrode. This integrated system combines electrosurgical grounding with premier underbody warming, promoting intraoperative safety and simplicity. The system uses airfree, conductive heating to provide uniform temperature distribution, utilizing reusable warming blankets and mattresses controlled by the HotDog Multiport Temperature Management Controller for precise thermal regulation. Distinguished by its environmental and economic benefits, the HotDog Patient Warming System is clinically proven to enhance patient normothermia, setting a higher standard in perioperative care.
For more information, visit www.augustinesurgical.com.


StaCool Industries’ StaCool Vest Core Body Cooling System keeps surgical teams cool, comfortable, and completely mobile so that they can focus completely on the task at hand during long procedures. Despite elevated ambient temperatures due to layers of sterile medical garb, the StaCool Vest maintains a consistent, comfortable core body temperature thanks to ThermoPaks in the front and back, which provide hours of cooling relief. This
unique design is self-contained, so wearers have freedom of movement with no hoses or bulky coolers. A thermal barrier is built in to ensure wearer does not get too cold. Micro-thin, highly breathable materials are easy to care for, providing wearers unsurpassed cooling comfort without compromising mobility. StaCool Vests are available in unisex sizes from XX-small to XXX-large, the Industrial Vests are fully adjustable to suit all body types and sizes. A spare set of ThermoPaks are included with each vest to extend cooling time and comfort.
For more information, visit www.stacoolvest.com.

Encompass offers passive and active warming solutions that follow patients throughout the perioperative journey. Encompass has paired an innovative new carbon veil active warming technology with Thermoflect’s proven passive warming to create the Nova Active Warming System. Combining active and passive patient warming is a more effective way to fight hypothermia.
For more information, visit www.encompassgroup.com.
 BY DON SADLER
BY DON SADLER

Artificial intelligence, or AI as it’s more commonly referred to, has come seemingly out of nowhere the past couple of years. Put simply, AI is technology that enables computers to simulate human intelligence and problem-solving capabilities. While it has only recently become a hot topic, the term “artificial intelligence” was actually coined in 1955 by a Stanford University professor.
One particular application of AI that has probably captured the most attention is ChatGPT. This technology uses large language models (LLMs) to allow users to enter prompts online and have human-like conversations to complete tasks such as composing articles, blogs, emails and social media posts. ChatGPT was launched less than two years ago by OpenAI, an artificial intelligence research company.
Marketing More Effectively with AI
Erica Basora, MSN, RN, NPD-BC, CNOR, is a perioperative nurse and nurse educator. She’s also an author and owner of That’s Love Publishing, a publishing company that produces children’s books, coloring books, journals and cookbooks, as well as a conference speaker and podcaster. And she’s the mother of two children.
In addition, Basora is a lifetime member of the Association of periOperative Registered Nurses (AORN) and a member of the Georgia Council of periOperative Registered Nurses.
“When I first heard about AI, I wanted to learn more about how I
could use it to leverage my time since I wear so many different hats,” says Basora. “My publishing company and the Georgia Council both have very small marketing budgets so I wanted to see if AI could help us market more effectively.”
While helping the Georgia Council plan and organize its annual conference last year, Basora decided to see if AI could help her promote the event and boost attendance. She used ChatGPT to create social media posts on LinkedIn starting 60 days before the conference.
“I looked at it as kind of an experiment to see if AI could help us boost awareness of the conference and ultimately the number of conference attendees,” she says.
Basora started tracking the number of conference signups once she began posting AI-generated content on LinkedIn. The numbers speak for themselves:
“AI is opening doors for new job duties like writing ChatGPT prompts and other creative ways to incorporate AI into content creation. Just because things are evolving doesn’t mean that employees are being displaced.”
- Erica Basora
• 70 days out from the conference: 10 registrations
• 60 days out from the conference: 19 registrations
• 49 days out from the conference: 48 registrations
• 38 days out from the conference: 68 registrations
• 23 days out from the conference: 82 registrations
• 0 days out from the conference: > 100 registrations
“There’s no question that using AI to create and schedule social media posts on LinkedIn helped us boost conference attendance,” says Basora. “This was really eye-opening for me because it was so easy and effective.”
Basora uses the term “the Art of Nursing” to describe the use of knowledge, skills, technology and compassion to provide patients with holistic care.
“In today’s digital age, nurses and health care organizations can harness the power of AI to promote their organizations and increase member engagement while preserving the Art of Nursing,” she says.
According to Basora, the intersection of the Art of Nursing and technology/ AI results in enhanced communication and marketing, advancements in patient care, remote monitoring and more personalized patient care.
“Marketing is simply any activity you engage in to promote your health care organization,” she says.
It includes the four Ps:
1. Product
2. Price
3. Place
4. Promotion

The most common marketing tools used by health care organizations typically include email, snail mail, newsletters, blogs and social media.
“So, the question becomes: Who in your organization is responsible for these marketing tasks?” says Basora. “Maybe it’s you, or maybe you have a volunteer, or maybe you need to hire a professional marketer. But can you really afford to do this?”
Basora encourages health care organizations to use AI to create a 30-day social media marketing plan to promote a meeting or conference.
“You can do this in five minutes,” she
posts for my organization’s annual conference. Write each post for LinkedIn discussing education.”
“Write a 30-day marketing plan for the nurse’s organization’s annual vendor fair. The target audience is operating room nurses who want to improve their practice, learn and have a good time at this year’s conference. Make the post engaging and convince individuals to attend. Each post should be written with emojis and hashtags for LinkedIn.”
How AI is Revolutionizing Marketing AI is revolutionizing marketing strategies by providing data-driven
addition, always be mindful to not place confidential information in ChatGPT.”
Here’s a mnemonic – START – for employing AI in content creation:
S - Specify how you want the AI to act.
T - Train the AI with data that will improve the relevance of the answer.
A - Add text that directs the software to deliver an expected outcome.
R - Review the output for relevance and crosscheck it for accuracy.
T - Track the results and determine if you have to make adjustments.
“Using AI allows perioperative professionals to leverage technology to increase our impact and smoothly transition into the digital age.
says. “Create the content using ChatGPT, find copyright-free images and videos at Pexel.com or Pixabay.com, and schedule the posts using Canva.com.”
Here are a few examples of ChatGPT prompts for creating social media posts to promote a meeting or conference:
“Write a ‘save the date’ LinkedIn post for the nurse’s organization’s annual vendor fair that will take place on (fill in the date) at (fill in the location.) Make the event sound fun and energetic and use emojis in the content.”
“Write 30 days of social media

insights and personalized customer experiences while optimizing ad targeting. “With AI you can streamline marketing processes, personalize content to audience segments and improve customer experiences,” says Basora.
AI is best used as a starting point for creating content.
“You should always change the prompts to use your own unique voice and regularly review and finetune the content, as well as research the output for accuracy so there’s no misinformation,” says Basora. “In
A few common myths have sprung up regarding the use of AI and ChatGPT. One of the biggest is that AI will eventually replace jobs currently being performed by humans.
“I don’t see this as job displacement at all,” says Basora. “Instead, AI is opening doors for new job duties like writing ChatGPT prompts and other creative ways to incorporate AI into content creation. Just because things are evolving doesn’t mean that employees are being displaced.”
Another myth is that AI-generated content lacks creativity. Basora counters this.
“While it’s true that the output from AI depends heavily on the input it receives, this actually highlights the importance of human creativity in guiding AI,” says Basora. “By effectively using prompts that reflect our unique voice and objectives, we can generate highly creative content that aligns closely with our goals.”
Yet another myth is that AI is too complicated and costly. “AI tools like ChatGPT are becoming more accessible and user-friendly,” says Basora. “The initial investment in learning how to use them can lead to significant time and cost savings in your marketing.”
According to Justin Fontenot, DNP, RN, NEA-BC, FAADN, AI could have major implications in the area of evidence-based practice.
“It takes an average of 15 years for new evidence to reach the bedside, while evidence-based practice uptake in clinical settings currently sits at just 50%,” says Fontenot. “This is a big concern for nurse leaders who are instrumental in advancing and sustaining evidencebased practice in clinical settings.”
Fontenot says that research-based
communities by letting them know how it improves patient safety and care.”
The impact of artificial intelligence on health care and in the operating room goes well beyond marketing and messaging, of course. However, Basora notes that integrating AI into perioperative marketing expands the reach of the perioperative department and contributes to the evolution of the Art of Nursing.
“Using AI allows perioperative professionals to leverage technology
This helps ensure that we continue to engage our members and foster a culture that delivers exceptional care to our patients and the community.” - Erica Basora
AI platforms such as Elicit can significantly speed the process of research translation in clinical practice.
There are also some ethical concerns about widespread use of AI and ChatGPT. Basora says it’s crucial to use AI ethically by ensuring that it augments human interaction, rather than replacing it.
“We also must be vigilant about the data sources used by AI to avoid biases that could affect the output,” she adds.

“Using AI to develop evidencebased practice permits automation of tasks that have previously been performed manually, which can speed the translation rate into clinical settings,” he says.
“AI tools can accomplish work that takes six months to perform manually in a couple of weeks,” says Fontenot. “This is a competitive advantage that health care organizations can market to their
to increase our impact and smoothly transition into the digital age,” says Barora. “This helps ensure that we continue to engage our members and foster a culture that delivers exceptional care to our patients and the community.”
Basora offers a free online course with guidance on how to market your organization using AI. Visit https://publishwithconfidence. com/ericabasoramarketingwithai to learn more.
We offer cooling vests and accessories to keep all members of the OR staff comfortably cool and focused when the operating room temperature is heated to AORN and Joint Commission recommendations! We have dedicated members of our team that are committed to helping you choose the perfect apparel for your OR room and staff.
The lightweight CoolOR® Circulating Water System keeps surgeons and staff cool and comfortable by continuously circulating cold water through tubing sewn within the vest. The surgical cooling vest system features a safe, water-tight cooling reservoir, quick-connect couplings, insulated water lines, attached wheels and a retractable handle.
Discreet pockets hold your choice of reusable cooling pack technologies. This is a cost-effective option that allows for freedom of movement while providing effective cooling.





UNLIKE OTHER PRODUCTS ON THE MARKET, CoolOR® IS FULLY STOCKED AND READY TO SHIP WITHOUT DELAY.
Are your surgeons feeling the heat in the operating room? Introducing the CoolOR® Circulating Water System, a game-changer in surgical comfort. Here’s why it’s a must-have for your team:
• CONTINUOUS COOLING
• WATER-TIGHT RESERVOIR
• QUICK-CONNECT COUPLINGS
• INSULATED WATER LINES
• PORTABILITY
CHOOSE COOLOR®: Because comfort matters, especially when lives are at stake. Contact us today to explore our high-quality water circulating systems and experience the difference firsthand!


Alexis Chaudron took a circuitous route to begin her career as an OR nurse, but the twists and turns in her path have made it all the richer for the experiences.
Chaudron began her pursuit of a medical degree at Johns Hopkins University after high school, but changed her major from pre-med to public health as an undergraduate. Focusing on the opportunities of community and preventive health rather than just treating ailments had exposed Chaudron to the business and legal aspects of health care, and so she continued her studies at the graduate level, earning a master’s in healthcare administration at the University of North Carolina in Chapel Hill.
The UNC school of public health further refined Chaudron’s focus on preventive health with its emphasis upon quality and process improvement. From there, she went to work in health care consulting and at a group purchasing organization. Yet, as well-rounded as her resume became, Chaudron felt like she was still missing the experience of bedside care.
“It gave me a very different vantage point for looking at health care,” she said. “I still yearned for that patientprovider relationship, and went back to Johns Hopkins for nursing school.”
In the course of her studies, Chaudron fell and broke her arm, which she describes as a stroke of good fortune. Without another place for her to continue her studies,
Chaudron was assigned to the operating room in an observatory capacity to keep her clinical hours going.
“That truly is what started my career,” she said. “The OR is so fascinating. It was the first place that I got to interview patients, and have them get enough faith and trust in you to take care of them when they’re asleep on the table. I didn’t think there was anything more important than being a patient advocate for someone who can’t communicate for themselves. As someone who had been around the health care block, I felt I would be really good at it.”
After graduating, Chaudron’s first opportunity in the OR training program came at Georgetown University, where she said she received “comprehensive orientation in every surgery service line under the sun,” and settled on orthopedics.
“I entered the operating room with this different perspective because nursing was a second career for me,” Chaudron said. “I already had an eye for efficiency and quality; the OR basically put everything together for me. It was fascinating, and because of my background in health care admin and business, I went quickly through the ranks.”
In the operating room at MedStar Georgetown University Hospital, Chaudron developed first-hand knowledge of the administrative responsibilities that apply to the surgical space, which she leveraged into a promotion to nursing supervisor. Dealing with “all the sticky situations in the middle of the night” afforded her the opportunity to grow her knowledge base by exploring the whole-hospital picture. Whether she learned about patient flow, bed
placement, triaging patients, or delivering care, the various perspectives afforded her a different outlook from her clinical experiences in the OR. When Chaudron moved back to California to get a job as an evening charge nurse at a local community hospital, she was well equipped, both from leadership and theoretical perspectives.
“It was my first work outside of an academic institution, and a really great opportunity to flex my leadership muscles with a small team, and try to run the evening,” she said. “In any OR, the evening team is really a family with skeleton resources. You have to lean into each other and trust, because we have to work together as a team.”
From there, Chaudron earned her first managerial role at a hospital in the University of Southern California system, and then she took an opportunity as a nurse manager at the University of California Los Angeles (UCLA). It was the biggest facility she’d managed, but afforded her progressive leadership experience, a path to a directorship, and an expanded scope of responsibility from there.
“It helped hone my leadership voice and skills in terms of looking at things from the perspective of budget management planning, staff optimization and hours,” Chaudron said. “I got to learn a lot and was exposed to a lot very quickly.”
Since leaving UCLA, Chaudron began interim nursing work and has built a robust business as an expert medical witness. In those circumstances, she has been able to apply her theoretical and practical knowledge of nursing leadership and management to performance improvement for a variety of health care institutions, and has herself benefited from the educational opportunities they present.
“You can always do better the following day than you did the day before,” Chaudron said. “These situations have just given me so much opportunity to learn for myself and to help educate the team. It has certainly been eye-opening and cool to throw in all the experience I have had as a nurse of 14 years and see how much improvement I can do in a short time.”
Not one to rest on her laurels, Chaudron also recently completed her educational doctorate at Vanderbilt University, which will enable her to consider teaching and preparing the next generation of nurses. In a collection of advanced degrees, it’s the first that she has earned outside of medicine, and Chaudron hopes to leverage it in pursuit of nursing recruitment and continuing education.
“As a nurse, it is important for us to stay abreast of industry trends, equipment, and make things easier for the staff so there’s not as many barriers as I experienced,” she said. “As the focus continues to be on cost-effectiveness and process efficiency, I think it’s going to continue to tighten, and people need to be open-minded.”
When she’s not working, Chaudron enjoys destination hiking, and has traveled around the world to places as far-flung as Mount Kilimanjaro, the Swiss Alps, Chile and Japan. She also operates a medical travel company, Passport Surgical Partners, which helps connect patients with providers in Costa Rica and Colombia to access more affordable and timely medical, surgical and dental care.



B reast cancer mortality is significantly reduced when women regularly attend screening mammograms, according to research presented at the annual meeting of the Radiological Society of North America (RSNA).
Early detection of breast cancer, before symptoms are present, is key to survivability. According to the American Cancer Society, women between the ages of 45 and 54 should get mammograms every year. Women who are 55 years and older can switch to every other year or continue with annual mammograms. Skipping just one scheduled
mammogram could result in a more advanced breast cancer diagnosis, significantly impacting a patient’s chance of survival.
“The purpose of mammography is to detect breast cancer during the few years it can be seen on a mammogram, but before symptoms are apparent,” said study author Robert A. Smith, Ph.D., senior vice president and director of the American Cancer Society Center for Cancer Screening in Atlanta, Georgia. “If a woman unknowingly has breast cancer and misses or postpones her mammogram during this time when she has no symptoms, but her breast cancer is growing and perhaps spreading, then the window for early detection will be lost.”
Even though regular mammograms are an important factor in early breast cancer detection, there are still many barriers that restrict women from receiving this preventative care, including access and work or family obligations.
“It is challenging to keep track of your schedule, and in the U.S., many women do not receive reminders. Further, for all of us, the obligations of work and family compete with our scheduled health care,” Smith said.
Smith and colleagues sought to identify the exact impact of missing even one mammogram.
The researchers obtained women’s screening history from oncology centers throughout Sweden for a
period from 1992 to 2016. A total of 36,079 breast cancer patients were included in the study.
Using data from the Swedish Cause of Death Register, the researchers identified 4,564 breast cancer deaths among the patients included in the study.
The researchers then tracked all of the women’s participation in five or fewer most recent invitations for breast cancer screening prior to cancer diagnosis.
Women who attended all their invited screening mammograms had a survivability rate of over 80%. Women who didn’t participate in any screenings had a survival rate that ranged from 59.1% to 77.6%.
Women who attended all five screening mammograms saw a 72% reduction in the risk of dying from
breast cancer compared to women who didn’t participate in any screening mammograms. Even after conservative adjustment for potential self-selection factors, there was a highly significant 66% reduction in the risk of breast cancer death.
“Women who attended all five previous mammography examinations prior to a diagnosis of breast cancer were nearly three times less likely to die from breast cancer compared with women who had not attended any examinations, and each additional examination attended among the five previous examinations conferred an additive protective effect against dying from breast cancer,” Smith said.
The researchers stressed that imaging facilities should prioritize getting patients in for screening
at the earliest opportunity. This is especially important when women have to cancel their appointments. Facilities should reschedule these screening mammograms for the next earliest available appointment.
“These findings show that as much as possible, adherence to regular mammography screening is the very best insurance a woman has against being diagnosed with an advanced breast cancer that could be lifethreatening,” Smith said.
Co-authors are Stephen W. Duffy, M.Sc., Amy Ming-Fang Yen, Ph.D., László Tabár, M.D., Abbie Ting-Yu, Ph.D., Sam Li-Sheng Chen, Ph.D., Chen-Yant Hsu, M.D., Peter B. Dean, M.D., and Tony Hsiu-His Chen, Ph.D.









Pays for itself in one year!
Save canister & solidifier costs
Check cost saving on our website
Use the DM6000 for your project!
• Surgery, endoscopy, SPD
• Requires vacuum, electrical & drain





•
•






N o matter what your goal, having stronger hips and core will always be foundational throughout your life. Inactivity, for example, can cause a wide variety of issues in the hips. Over activity without quality recovery can to lead to the same issue. Having a quality sense of balance is important but also requires good foundational movement patterns.
Whether you’re a runner, strength training, turning 60 or playing sports, these next three exercises will be very beneficial in helping maintain healthy hips, a stronger core and ultimately a better feeling body. All you need is a wall and a mat and to get started.
The first movement is known as polishing the bowling ball. The analogy is that your hip is the ball. You want to take it through internal and external rotation while in a slightly balanced position. This movement will strengthen the ankle, knee and hip while also stretching and relaxing areas in the back because of the more mobile hip joint. When the hips are
compensating or over active in certain areas, it can tend to bother the back which can lead to a lot of discomfort. Doing two sets of at least 5-6 reps during warm up. It is also a good stretch to loosen up. This movement should be in your weekly routine.
The second movement is more core focused as we want to work our way up. It is called the Banded Deadbug and is a great way to work your core as well as protect your spine and neck. Most people don’t do crunches or certain core movements because it tends to bother the back. This is a great alternative. Segmenting the hips, while putting tension on the core in an isometric fashion, is a great way to improve functional movement patterns. It’s an exercise that will expose imbalances within your core and hips. It will also improve coordination. I recommend doing this in your warm up routine or as a core finisher when completing a training session.
The last exercise is focused on putting these two movements together. It requires balance and strength to challenge the hips and core. It is the Single-Leg Banded
Lateral Step. This is a simple foundational movement pattern that can progress with several variations depending on what your goal is, but it’s a great exercise you’ll find in many routines. Going back to a standing exercise that highlights more hip and glute work and challenges core stability really solidifies why these three exercises should be in everyone’s warm up routine at least once a week. I recommend hitting higher rep counts but moving slowly to challenge balance. Then move faster to challenge coordination, less reps for quickness and more reps for strength endurance.
Enjoy these three movements and know that implementing them more than three times a week is more than OK.
– Miguel J. Ortiz is a personal trainer in Atlanta, Georgia. He is a Master Trainer for Pain-Free Performance and a Certified Nutritional Consultant with more than a decade of professional experience. You can find videos of the exercises mentioned in this column on his YouTube channel at tinyurl.com/ ORTfitness.

L ots of people strive for positions of management or leadership. Some people are naturally inclined to do well in those roles, others must learn the skills. When someone exercises good management or leadership, chances are the workplace hums along pretty well. However, when someone in one of those positions lacks those skills, let’s just say things usually don’t go so well.
Such was the case when a friend of mine, whom we’ll call Robert, signed on to a new company. A few months back, Robert was asked to join the team of a start up to serve as director of production. Wisely, Robert asked for a job description, but none existed. “It will have to emerge,” the company founder said.
Since the company founder, whom we’ll call John, owned several businesses, Robert assumed John knew what he was doing, and he discarded his standard practice of taking a position only when a clear job description was provided. Suffice it to say Robert quickly regretted his decision. Robert recently shared what happened.
Onboarding was horrible. The new company already had five other employees when Robert was brought on. Robert figured John would introduce him to the other team members, but no introductions
took place. Robert knew one of the other employees already, but John made no effort to get Robert connected with the others. This frustrated Robert, because not only was he unclear about his own job responsibilities, he was unclear about what the other people were supposed to be doing to help the company meet its goals. No policies were explained. However, as Robert soon observed, that’s probably because policies and procedures were made up on the fly.
Micromanagement flourished. The owner, John, revealed his micromanagement tendencies in the very first week. Even though Robert had decades of experience in project management, John kept redirecting Robert’s decisions and acting as if Robert ought to be able to read John’s mind. Tasks would be delegated to Robert, but then John would step in, take back responsibility for the tasks and do them the way he wanted. Rather than receive training on what was expected, Robert was corrected and scoffed at.
Meetings were disorganized. Robert was accustomed to attending meetings where agendas existed and focus was maintained. Such meetings did not happen at John’s company. Meetings regularly ran long, despite John declaring that meetings needed to start and end on time. And, because no meeting agendas existed, conversations took many directions and
much time was wasted. The first meeting ended with John saying, “OK – we’re done.” After that, Robert stepped up at the end of each meeting to summarize what decisions were made and clarify the action items decided.
Communication fell flat. All employees of the company were told to communicate using an online app, but when Robert sent questions to John via the app, John would rarely answer. And even when he did, his answers were terse and unclear. Robert would have to text John to ask him to respond to the questions posed in the app, but even then, John would only respond occasionally.
It didn’t take long for Robert to feel frustrated. He’d always been recognized as a top performer in his previous places of employment, but now he felt he was being set up for failure. He didn’t feel valued. He didn’t feel productive. And, he didn’t see any hope of things turning around. Before his two-month anniversary with John’s company, Robert resigned.
This did not need to be. It was obvious from Robert’s past successes that he could have been a huge asset to John’s business, but John failed to create the conditions for similar success. Let’s go back through the reasons Robert left and discuss what John could have done differently.
When onboarding, by all means, even if it’s a rough draft, companies need to provide a list of tasks and duties required
for every position. Duties are general areas of responsibility; tasks are specific action items that someone is supposed to do. Additionally, ensure all new hires are introduced to their team members, including people from other departments who will interact with the new hire. Each person’s basic responsibilities should be explained. Research shows that a new employee’s attitude toward the company is set within 72 hours of starting. For employees to be fully engaged, managers or leaders need to connect with new hires multiple times during those first three days, answering questions and asking what can be done to help the new employee succeed.
Micromanaging is a most demoralizing management style. Training needs to occur, followed by good delegation. Three things need to be delegated: responsibility, authority and accountability. As a quick overview, being responsible to complete a task means one is duty-bound to do the work. John would delegate a task, but then, without telling anyone, he would
we’re on instagram!


do the work himself. Robert was shocked many times to discover a task he had been assigned was already completed by John, and all his efforts to accomplish his assignment were wasted.
Meetings need a clearly stated purpose and an agenda. Whoever is planning the meeting needs to think those things through, and then publish an agenda for how the meeting should flow to achieve that purpose. When those things happen, meetings are often more productive. It’s also important for whoever is leading the meeting to keep it on track.
Communication is key, and it must work for everyone. Lots of communication avenues exist these days, so care should be taken not to use too many methods or details get lost. Perhaps most important, rapid response and clarity need to be practiced. Managers and leaders cannot ignore questions from subordinates and expect those people to remain engaged and productive. Let me also add that “please” and “thank you” go a long way toward people feeling valued and respected.

Most employees will work hard for an organization, but managers and leaders need to create conditions for success or those employees will leave for greener pastures.

Daniel Bobinski, who has a doctorate in theology, is a bestselling author and a popular speaker at conferences and retreats. For more than 30 years he’s been working with teams and individuals (1:1 coaching) to help them achieve excellence. He was also teaching Emotional Intelligence since before it was a thing. Reach him with questions at eqfactor.net or at 208-375-7606.

OUT OF THE OR nutrition

O ur diet has a huge effect on our brain and our mental wellbeing, even protecting against dementia. The brain is the hungriest organ in the body, consuming more than 20 percent of your body’s total energy haul. At the same time, our brain cells are irreplaceable. Unlike the rest of the body, where cells are continuously replaced, the vast majority of brain cells stay with us for our entire lives – which means they need extra care and nourishment.
So, what should be on the menu? Lots of the following on a daily basis:
• Fatty Acids: A specific kind of fats called polyunsaturated long-chain fatty acids, such as the famous omega-3s. Fatty fish – such as salmon, mackerel, anchovies, and sardines – are the best natural sources of the only kind of fat the brain needs throughout a lifetime.
• Glucose: A specific kind of carbohydrate called glucose. Glucose is the only energy source for the brain, so it’s crucial that the brain gets enough of it. Foods that are naturally rich in glucose and that at the same time contain enough fiber to stabilize your blood sugar levels are beetroot, kiwi fruit, whole grains, sweet potatoes, onions, and spring onions.
• Vitamins and minerals: All sorts of vitamins and minerals, especially those with antioxidant effects such as vitamin A, vitamin C, vitamin E, and selenium – but also iron, copper and zinc. Fruits and vegetables are the best natural sources of these: go for berries, oranges, grapefruit, and apples, which are sweet but have a low glycemic index. Leafy green or cruciferous vegetables (broccoli, cabbage, spinach, kale, dandelion greens) are also recommended
• Extra virgin olive oil: Last but not least, extra virgin olive oil is a brain must, as it is loaded with anti-aging nutrients such as omega-3s and vitamin E. Vitamin E is particularly important to protect ourselves against dementia.
– Grace O is the creator of FoodTrients, a unique program for optimizing wellness and longevity. She is the author of three awardwinning cookbooks. Her latest cookbook is “Anti-Aging Dishes from Around the World.” Learn more at FoodTrients.com/recipes/antiinflammatory.

It’s hard to beat this combination of eggs, celery, and turmeric for brain health. You can spread my egg salad on toast, eat it in a sandwich, or serve it on a bed of mixed greens. It’s delicious with sliced tomatoes or thinly sliced scallions. For extra antioxidant power, add a few teaspoons of minced parsley or watercress. I prefer the taste of eggs from freerange hens whose yolks get their bright yellow color from the marigolds and grubs they graze on.
Chef’s Note: To make shelling the eggs easier, add a splash of vinegar to the cooking water. If you’re serving this dish as a salad, refrigerate it first for a minimum of 2 hours.
Ingredients
• 6 eggs (organic, free-range, or Omega-3-enriched)
• ½ cup mayonnaise
• 2 Tbs. capers
• ¼ cup diced celery
• 1 tsp. turmeric powder
• 1 tsp. minced dill
• 1 tsp. minced chives
• Salt or salt substitute and freshly ground black pepper to taste
Instructions
Servings: 3-4
1. Place the eggs in a pot of cold water. Slowly bring the water to a boil over medium heat. Cover the pot, remove from the heat, and let the eggs sit for 7 minutes.
2. Drain the eggs and cool them in a bowl of water with ice.
3. In a separate bowl, mix the mayonnaise, herbs and spices.
4. Shell the eggs, then mash them with a fork or cut them into small cubes.
5. Fold the eggs into the seasoned mayonnaise.
• 1 cup whole milk
• 1/2 cup Premier Protein Strawberries & Cream Protein Shake
• 1/4 cup packed brown sugar
• 1/2 teaspoon salt
• 1 large egg, lightly beaten
• 2/3 cup creamy peanut butter
• 2 cups heavy whipping cream
• 2 teaspoons vanilla extract
• 1/2 cup sugar-free strawberry jelly
 By family features
By family features

OUT OF THE OR recipe
I
n a world of packed schedules and boring food, it can feel like doing the healthy thing means giving up some of what makes you happy – like treats and flavors you love. Choosing health shouldn’t mean restricting yourself; everyone deserves a treat now and again.
Try incorporating better-for-you ingredients into your favorite indulgences. Look for convenient, ready-to-use products, like Premier Protein High Protein Shakes, to help infuse the nutrition you need with the joy you deserve. With 30 grams of protein, 160 calories and 1 gram of sugar, the shakes make it easy to take the first step and keep that momentum going, adding nutrient-dense protein to nearly any recipe. In addition to a smooth, creamy texture, each shake delivers 24 vitamins and minerals including vitamins C and E, which help support a healthy immune system as part of a healthy diet and lifestyle. With 11 flavors – including strawberries & cream and chocolate – there’s an impossibly indulgent option for everyone to make a healthy life a happy endeavor through recipes like Peanut Butter Jelly Ice Cream.
Find more information and recipes at PremierProtein.com or on Instagram.
Peanut Butter Jelly Ice Cream Servings: 12
1. In large, heavy saucepan, heat milk, protein shake, brown sugar and salt until bubbles form around sides of pan. Whisk small amount of hot mixture into egg. Return to pan, whisking constantly.
2. Cook and stir over low heat until mixture thickens and coats back of spoon. Remove from heat; whisk in peanut butter. Quickly transfer to bowl; place in ice water and stir 2 minutes. Stir in cream and vanilla. Press wax paper onto surface of custard. Refrigerate several hours or overnight.
3. Fill cylinder of ice cream freezer 2/3 full; freeze according to manufacturer’s directions.
4. When ice cream is frozen, spoon into freezer container, layering with jelly; freeze 2-4 hours before serving.




 – Theodore Roosevelt
– Theodore Roosevelt
“OR Today magazine is a great place to find the latest news and industry trends for periop. You can find conferences, webinars, articles, and plenty of other useful information to keep up to date with best practices.”
– Matthew Avilla, UC Davis Health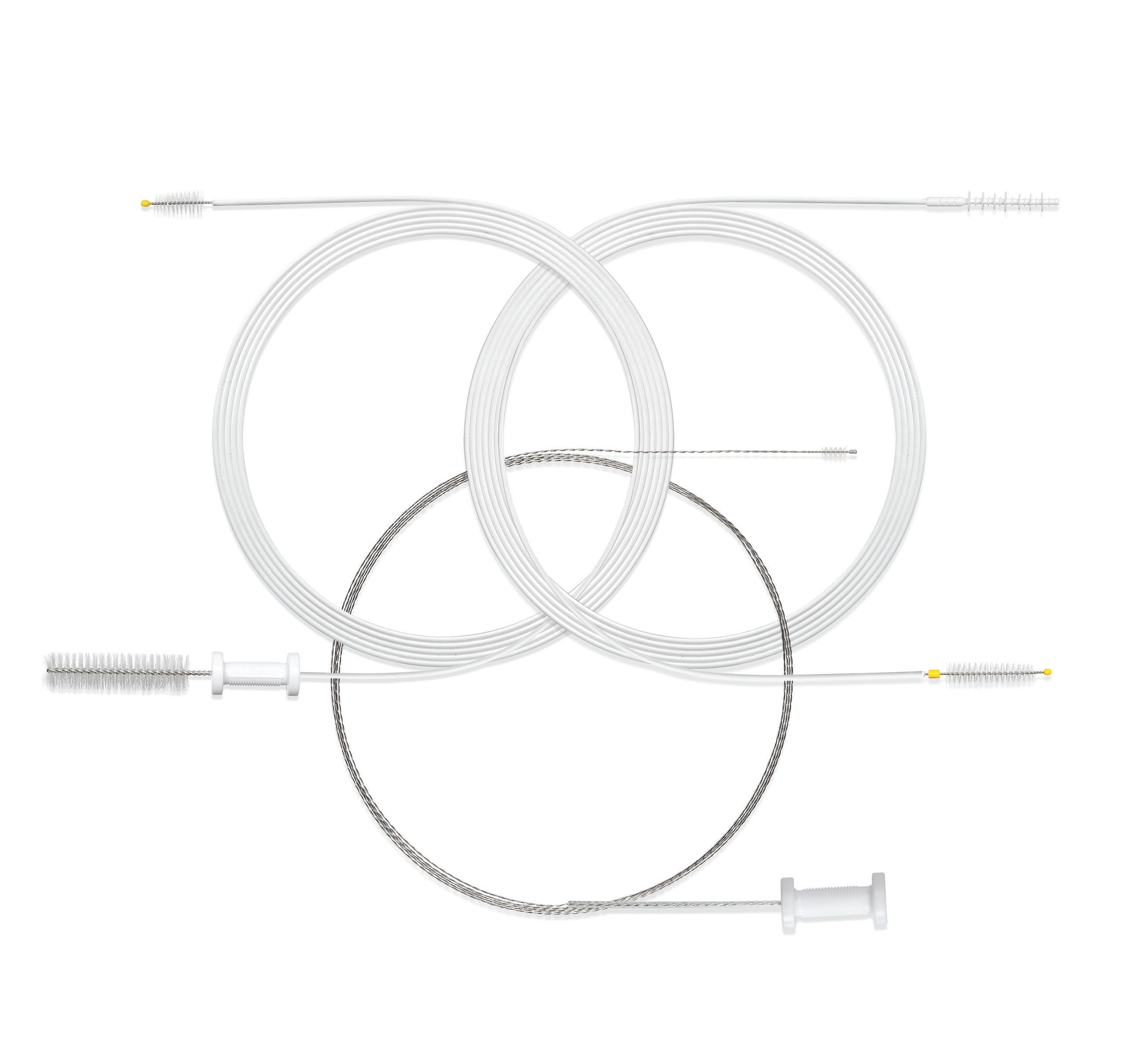
ENDOSCOPE REPROCESSING AND OUR SCOPE BRUSHES... A LOGICAL RELATIONSHIP
No doubt about it... cleaning and reprocessing flexible endoscopes is a detailed process. Manual cleaning, one of the vital steps for effective scope reprocessing, can be challenging if you don’t have the right tools. STERIS brushes are uniquely engineered to help you meet that challenge head on. Let us show you how our cleaning brushes make sense in your processes.

Scan the QR code to learn how our DuoSwift® Cleaning Brush outperforms competitors
 Double-Header Cleaning Brush
DuoSwift Combination Squeegee Brush
Small Wonder Cleaning Brush
Double-Header Cleaning Brush
DuoSwift Combination Squeegee Brush
Small Wonder Cleaning Brush