THINK ABOUT THE FUTURE
Succession Planning in Radiology

Interventional Radiology PAGE 32




















Succession Planning in Radiology

Interventional Radiology PAGE 32




















A haphazard training approach is risky and can seriously compromise patient safety and operational efficiency.
COVER STORY
Succession planning is an important aspect of an imaging department to maintain an efficient workflow and continued growth.


RISING STAR
Sgt. Jacob Loya is radiology specialist at Bayne-Jones Army Community Hospital who earned his radiologic technician credentials in 2024.


The latest imaging news for radiology directors and imaging leaders.
Find out more about some of the latest and greatest interventional radiology devices.

No matter how charming or creative the leader’s style, certain foundational elements must be in place for any team to thrive.
President
Vice
Kristin
Vice
Group
Jason
Kristin
Cindy

Through innovation we want to change the perspective in the imaging space.
We want to put the control back in the hands of the decision makers.



We understand our customers goals and we are developing a clear pathway to measurable savings.



BY ARLEEN BANDARRAE
Th e recent redesign of UCSF Health imaging operations created a new chief imaging officer role and eight new director positions to support regional and programmatic expansion of imaging services.
Tosca Bridges, recently named interim director, imaging operations – adult hospital, recently completed her early morning rounds at the UCSF Helen Diller Medical Center at Parnassus Heights.
Full of energy and her characteristic optimism, Bridges briskly observed that “Radiology has grown by leaps and bounds in recent years, and we are seeing great demand for imaging at UCSF.”
Bridges is enthusiastic about her new position and considers
it an extension of her previous roles in diagnostic radiology –as a technologist, an educator, and a regulatory compliance and safety leader – but on a larger scale.
Bridges first came to UCSF as a traveling technologist in 2002, working at UCSF on and off for five years, before gaining more experience in education with roles at Stanford and John Muir Health. In 2022, she returned to UCSF as chief manager of diagnostic radiology, leading a team responsible for 250,000 imaging exams each year in collaboration with many different service lines.
“I have come full circle – from starting as a dark room tech, to a radiologic technologist performing direct patient care, to a radiology clinical instructor and educator teaching radiation safety and various courses to surgeons, technologists and
students,” said Bridges. “I have experienced every aspect of radiology, and that gives me a unique perspective and helps me understand what leadership looks like at every level.”
Growing up in Mississippi, she worked as a dark room technician in college, processing film for technologists while she completed her studies. At 25-years-old, she set out to be a traveling technologist. She had never been on an airplane before, so she hopped in her car and drove all over the country.
“My dad gave me the motivation,” she said. “I was a daddy’s girl. He taught me everything I know, including how to drive and he raised me to be independent and to take care of myself.”
Today, as the main point of contact for imaging operations for the adult hospitals, Bridges collaborates with the radiology operations committee, perioperative triad collaboration and procedural areas to ensure that inpatient imaging operations run smoothly, and patients are getting the care they need.
Bridges has oversight of all imaging modality units – diagnostic radiology, MRI, CT, and ultrasound, interventional radiology, molecular imaging & therapeutics, and mammography – at UCSF’s Parnassus, Mission Bay, and Mount Zion adult hospitals. Bridges works closely with modality unit managers and supervisors at each site to ensure timely patient access to imaging, meet quality and safety goals, hire new technologists, lead in-service and cross-training efforts, and participate in the selection of new imaging equipment.
A key aspect of Bridges’ recent work includes her collaboration with the RadiationSafety Committee, Faculty Modality Chief Kimberly Kallianos, MD (CT), and Diagnostic Medical Physics Director Michael
1. What is the last book you read? Or, what book are you reading currently? Last book: “Multipliers: How the Best Leaders Make Everyone Smarter” by Liz Wiseman
Current Book: “A Financial Bestiary” by Ramin Charles Nakisa
2. Favorite movie? “Coming to America”
3. What is something most of your coworkers don’t know about you? I’m a private person who loves fishing and country living.
Hoff, Ph.D., for their work to revise patient shielding guidelines. Bridges also continues to work closely with Abdominal Imaging and Ultrasound Chief Dr. Zhen Jane Wang in driving fluoroscopy initiatives.
Bridges describes her leadership style as that of a servant leader.
“I understand the staff and where they’re coming from because I’ve come from there too,” she said.
Journaling since childhood, Bridges stays introspective, often reflecting on how to be her best self, while absorbing key learnings from the many leadership books she enjoys reading. Her regular yoga practice helps to maintain her high spirits in part by “twisting herself into a pretzel” to release tension she says.
“When life gets difficult, there’s always a silver lining,” said Bridges, brimming with positivity. She recalled taking care of her father when he struggled with dementia, alongside her mom – an experience that brought them closer together.
“We’re like sisters now,” she said, knowing her father would be very happy to see how close they are now.
Family has always been a shining light of inspiration in her life.
“My very classy, runway-ready grandmother taught me how to be my authentic self. If she could see me now, she would be very, very proud,” said Bridges.
Today, Bridges describes herself as grateful, invigorated, confident in who she is, and open to learning. She is a winning combination for success, as she plays a vital role in ushering in the next generation of imaging innovation and expansion of radiology services.
“In this role, I get to use all of my unique experiences and I am having a great time doing it!” said Bridges. •
4. Who is your mentor? Jeff Freymuth & Steven Cloyes
5. What is one thing you do every morning to start your day? Meditation practice
6. Best advice you ever received? Always be true to myself
7. Who has had the biggest influence on your life? My mother & father
8. What would your superpower be? X-ray vision (of course)
9. What are your hobbies? Yoga, shopping, wine tasting
10. What is your perfect meal? My mother’s home cooked cubed steak & gravy, rice, and butter beans.

BY JEAN GRAVES
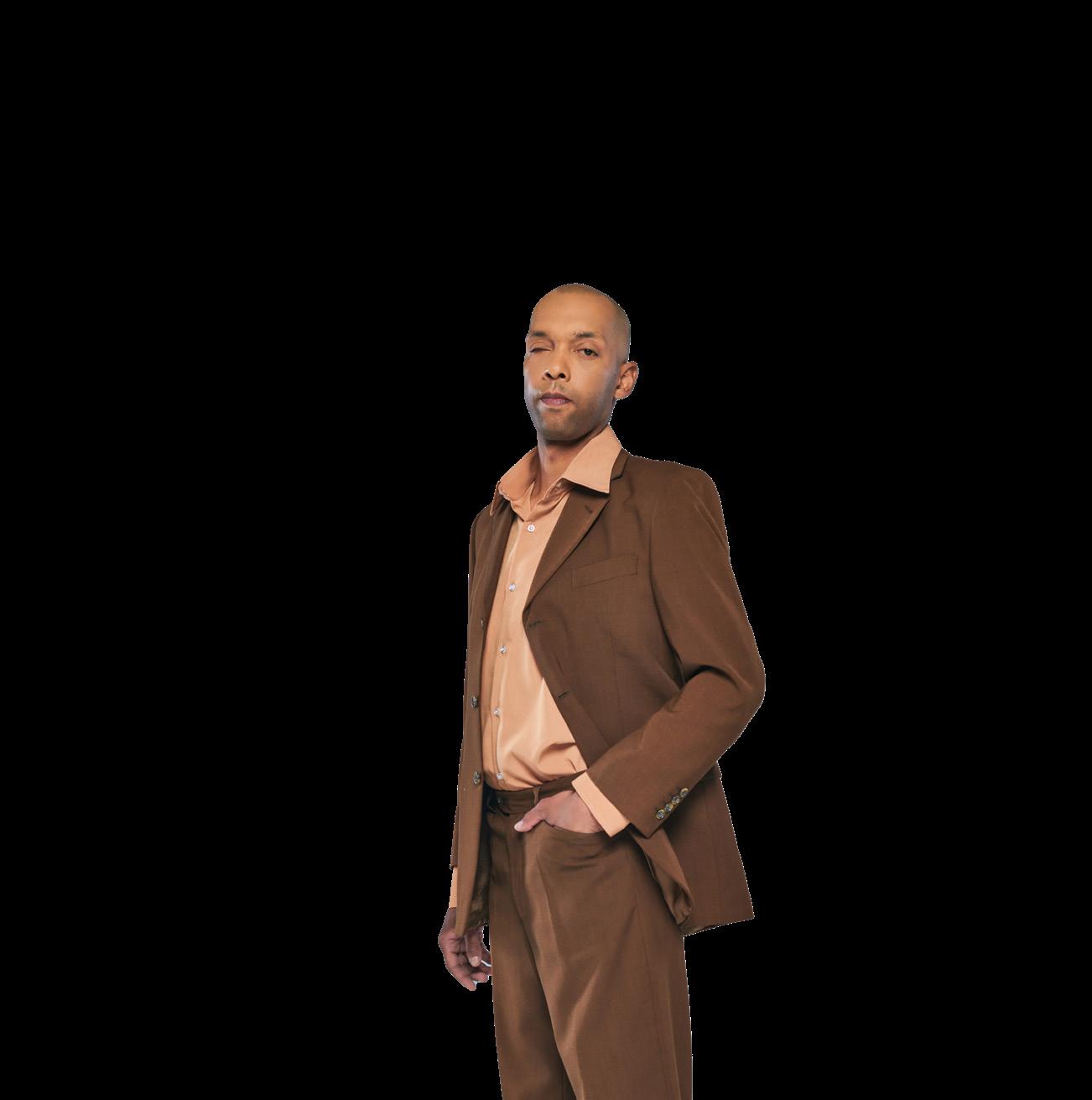
FO RT JOHNSON, La. | Sgt. Jacob Loya, radiology specialist at Bayne-Jones Army Community Hospital, passed the American Registry of Radiologic Technologists examination and earned his radiologic technician credentials in Shreveport, Louisiana.
ARRT is the world’s largest organization offering credentials in medical imagining, interventional procedures and radiation therapy. The organization certifies and registers technologists in a variety of disciplines through the oversight and administration of education, ethics and examination requirements.
Loya said after basic training, he spent six months in the classroom followed by another six-month clinical rotation to become a radiology specialist.
“Civilian radiology technologists earn a college degree, then challenge the registry to become certified, but military rad techs don’t earn a degree during our advanced individual training and are not required to earn the ARRT credentials to work at military treatment facilities,” he said.
The ARRT requires registry applicants to have an associate degree or higher from a regionally accredited college or university along with the successful completion of an educational program that demonstrates competencies in didactic coursework and clinical procedures.
Loya said earning his associate degree and challenging
the registry has been his goal since he graduated from advanced individual training.
“I chose to tackle the registry after I earned my degree from Northwestern State University,” he said. “I wanted to gain a new skill and show that I am knowledgeable and can provide the proper care to our patients. It is very important to me because I want my patients to know they are getting the best care available.”
Loya said challenging the registry and earning the ARRT credentials enhance his credibility with his patients as a professionally certified radiology technologist.

Command Sgt. Maj. Larry White, senior enlisted advisor, said he is proud of Loya and emphasized that BJACH soldiers strive for excellence, accept opportunities to excel and take pride in their profession every day.
“Sgt. Loya’s accomplishment is a testament to his professionalism as a noncommissioned officer,” he said. “He is not only proficient in his craft but has taken the necessary steps to ensure he provides top notch care to our soldiers, family members and beneficiaries. This is an example of how the soldiers at BJACH exemplify our motto: ‘We Provide the Best.’ ”
Loya said he didn’t pass the exam the first time, but that was a learning experience too.
“I knew the importance of earning the AART credential for my future in this field,” he said. “Continuing to challenge the registry has been rewarding. After I failed the first time, I could have given up, but I am resilient. I never lost focus on becoming a registered tech. Sometimes life happens, you don’t always get the results you want, but it’s important to never give up in pursuit of your goals.”
White said this accomplishment means a lot for the radiology department and their patients.
“Our patients can rest assured that Army Medicine is serious about providing care that rivals any civilian treatment facility in the world,” he said. “The radiology department at BJACH benefits from the accomplishments of our teammates because it exemplifies their dedication to professional excellence.”
Loya said all active-duty radiology specialists plan to challenge the registry.
“Being one of the few people to actually successfully challenge the registry shows soldiers it is possible by setting and sticking to goals,” he said. “The hardest thing is making it a priority when life happens. I hope I can be an example to my fellow soldiers that it is possible for them to do it too.”
Loya plans to make a career of the Army and is focused on earning his bachelor’s degree and earning the computed tomography (CT) credentials.
“My short-term goal is to get promoted to staff sergeant,” he said. “This summer I will be heading to San Antonio as an instructor for new radiology specialists. I hope I can inspire the next generation to challenge the registry when they get to their first duty station.”
Loya said he loves being a rad tech.
“I like working with patients,” he said. “Knowing I am part of the diagnostic process for our patients is very rewarding. Talking to patients and helping them determine the root cause of their issues is something I really enjoy. I always try to make a positive impact on my patients.”
Loya said he will continue pursuing credentialing in all the different modalities in the radiology field.
White said the BJACH radiology department consistently wins the Joint Outpatient Experience Survey (JOES) ancillary satisfaction award for their dedicated professionalism and customer service. •
BY FAMILY FEATURES
From a regenerative bath to that first cup of coffee, early morning rituals have the power to heal, restore and fuel. They can leave you feeling accomplished, empowered and ready to take on the day. How you spend your hours from 5-9 each day can ensure you’re well prepared to tackle whatever your 9-5 throws your way.
Establishing a well-planned and consistent routine removes the guesswork and makes it easy to accomplish more during these essential hours that set the stage for the day ahead. Get a jumpstart on your day with these tips to make the most of your morning routine.
Just as no two people are exactly alike, your morning routine should reflect your unique needs. Some people need these early hours to ease out of sleep and gradually work toward a busy day while others jump out of bed ready to set the day in motion. Decide what you can realistically accomplish in your waking hours before you hit the office and plan a sequence that makes sense for you and your family. When you have a steady routine in place, it’s typically easier to keep up with habits like early morning workouts, and on days when your energy is lagging, you can shift into autopilot and still get everything done.

stomach a full meal, look for alternatives to give your system a morning boost, such as a protein-rich smoothie early and a more substantial snack later in the morning.
ENJOY A MINDFUL MOMENT
The way you end each day influences how you start the next one. Going to bed on time, avoiding screen time before you turn out the lights and creating a comfortable sleep environment are all keys to restful sleep. However, managing your sleep doesn’t end once you reach dreamland; your wake-up routine is also an essential aspect of a healthy sleep schedule. One of the biggest detriments to quality sleep is hitting snooze to delay your day. Just a few more minutes easily becomes 20, 30 or more and none of that time is quality rest, so you’re not really gaining anything.
Countless studies affirm the importance of a well-rounded breakfast. Researchers have found good nutrition provides fuel to help give you energy, promote clearer thinking and problem solving, improve mood and memory, and more. If you can’t
Making time to relax or do something you enjoy can set a positive tone for the day. You might savor a few quiet moments over a cup of coffee or spend quality time with a pet. Early morning light and nature sounds can provide calming background for meditation, or you might simply use the time to organize your to-do list so you feel better prepared to tackle the day.
CREATE A REJUVENATING SPACE
No matter your routine, the bathroom is central to it. You can start the day with a more positive outlook when you get ready in a space that’s equal parts functional and beautiful. With stunning design, innovative features that make life easier, environmentally conscious performance and do-it-yourself installation ease, the Aspirations Collection from American Standard provides a full suite of bathroom products to start your day right. Find more ideas and inspiration for making the most out of every morning at americanstandard.com. •
Share your RAD IDEA via an email to editor@mdpublishing.com.


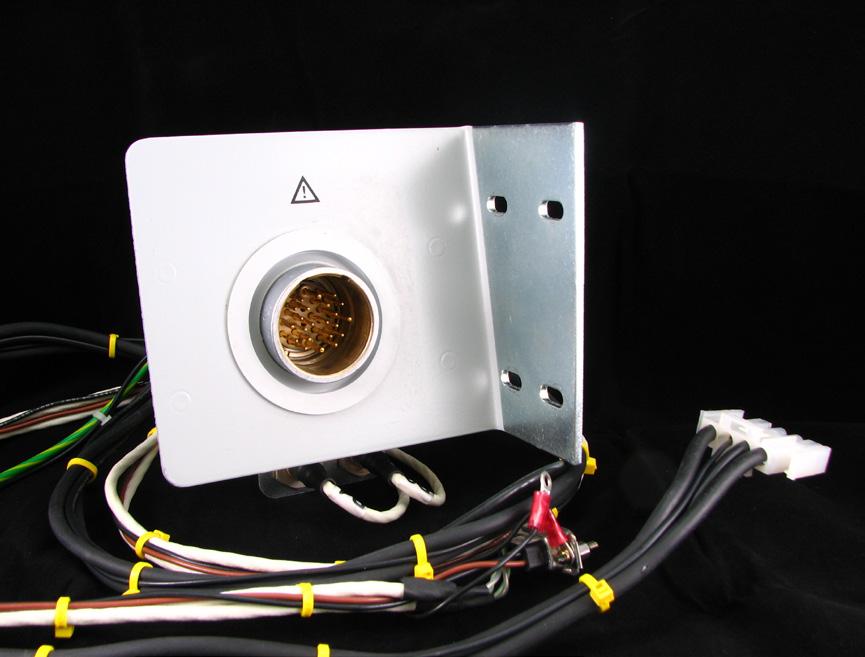
Kenneth Saltrick, President of Engineering Services in Twinsburg, Ohio, knows from his long experience that C-arm machines themselves are absolute workhorses.
For customers looking to blend the gap between expensive OEM and unreliable used assemblies, WE have your solution.
Our complete repair contains a new cable assembly, utilizing all OEM cable and components with a harvested plate and connector housing as they are proprietary items. These completely repaired products will have a significant cost savings with build quality above new OEM products and carry a warranty of 180 days, which is untouchable in the market.

BY MATT SKOUFALOS
In an effort to evaluate new learning models for radiology students in academic settings across the globe, radiologists in Kingston, Ontario, Canada and Nairobi, Kenya are partnering on a fouryear research project integrating distance learning, teleradiology and virtual reality.
Radiologist Omar Islam has headed the radiology department at Queens University in Kingston, Ontario, Canada, since 2019. In 2020, Islam’s department sought to establish a partnership with a sister department of Diagnostic Imaging and Radiation Medicine at the University of Nairobi in Kenya.
They called it the Global Health International Education Exchange and Visiting Professorship, and it was funded by a grant from the United Kingdom Association of Commonwealth Universities. Learners on both sides of the Atlantic would share in joint teaching and grand round sessions delivered remotely, a research project, and an in-person, visiting professorship – initially deferred by the novel coronavirus (COVID-19) pandemic.
“They’re our sister department on two sites, separated by thousands of miles,” Islam said. “Since 2021, we have shared at least four rounds at various intervals each year, taking turns. The most common is our monthly grand rounds: they do up to three and we do nine a year.”
During the pandemic, organizers focused on the online educational exchange, from which emerged a docket of rounds and other learning programs. The grant project, ongoing currently, explores diagnostic imaging lectures delivered through virtual reality (VR).
Islam believes the study represents the first of its kind in the world to evaluate the use of VR devices for medical education. Such an approach represents a departure from distance-learning instructional models like Zoom calls, PowerPoint presentations,
and self-guided learning modules. The research will evaluate, through surveys, testing, and learning feedback, whether the virtual approach is helpful, different, or better than other contemporary learning methods.
“Medical education is best delivered in a one-on-one format, ideally with the person right next to you, so you can have a nice dialogue as it’s discussed,” Islam said. “We use the VR headsets to transport the educator and the learner into the same room in cyberspace.”
“They’re in the same room, in a live format, viewing imaging cases and discussing the cases back and forth, bringing that thousands of miles distance between them down to zero,” he added.
Professors and learners take turns donning the equipment, and their fields of vision are projected onto a screen for the rest of the residents to view. The professor wears the VR headset for an hour, and then the learners take turns with the other headset, reviewing medical cases, and answering questions.
Participating in the learning study are 58 residents in Nairobi, who will complete 12 rounds per year over the four-year study period. Topics are developed from curriculum established by the Royal College of Canada curriculum and the technology partner in the research is a Saskatoon, Saskatchewan-based VR headset manufacturer called Luxsonic.
Much of the initial feedback has been positive, with the major exception of technical glitches related to the instability and speed limitations of the Kenyan Internet. In 2020, Queens paid to establish a Wi-Fi network at the University of Nairobi, and the Canadian team is still “trying to up the speed of the Internet on their end,” Islam said.
“That’s one of the negatives; the other issue has been the use of the joystick and the goggles,” he said. “It’s heavy, so that’s one thing; not everybody is used to that. Some of our younger radiologists who play video games are really into it,

but some are not.”
“In terms of the actual delivery of content, the ability to interact on a live basis thousands of miles away has been much more enriching than looking at a slide in a didactic lecture,” Islam said.
The VR format also allows students to scroll through an image database live, alongside the professor, and manipulate the images in the virtual space. That’s a massive departure from the learning environment in Kenya, where there is no PACS system, and patients control the physical films of their own imaging studies.
“The learners can manipulate those images that pop up on the screen just as if they were sitting next to us in front of a radiology monitor in our office,” Islam said. “That’s been the differentiating feature over other methods.”
“In Nairobi, the films are owned by the patient, so when the images are done, they
take the films and go, and there’s nothing left back unless the physicians are able to snag a copy, or take screenshot images with their phones,” he said.
“Obviously, the quality is not the same, and you can’t screenshot thousands of images, so they have limited electronic imaging libraries. When you’re doing educational sessions with VR goggles, you’re now in the electronic PACS world.”
As the research teams evaluate both the quality of the education and the educational medium, Islam said that he’s found the VR tools revitalized his approach to the classroom.
“I’ve done one of the sessions so far, and it was really neat,” he said. “It brought back the joy in teaching. I’ve been doing this for 24 years now, and after a while, it becomes semi-automatic. This method is new and hopefully engaging for everyone.”
“The ability to do different methods

of educational exchange through being transported into this virtual world was really neat, and there was no loss in quality of images and no loss of sound.”
Last year, Islam had the opportunity to visit the Kenyan students through the visiting professorship program, spending a week teaching and evaluating residents in person that he had only met previously in the virtual education setting.
“Medicine is kind of a global language,” Islam said. “We developed really strong bonds with the faculty and the students. They are smart, and very keen to learn, and get better, and support their patients and their country.”
“They enjoy what they do, and want to do more, which made it a really fun trip and a good way to establish bonds over shared goals of improving radiology,” he added. •




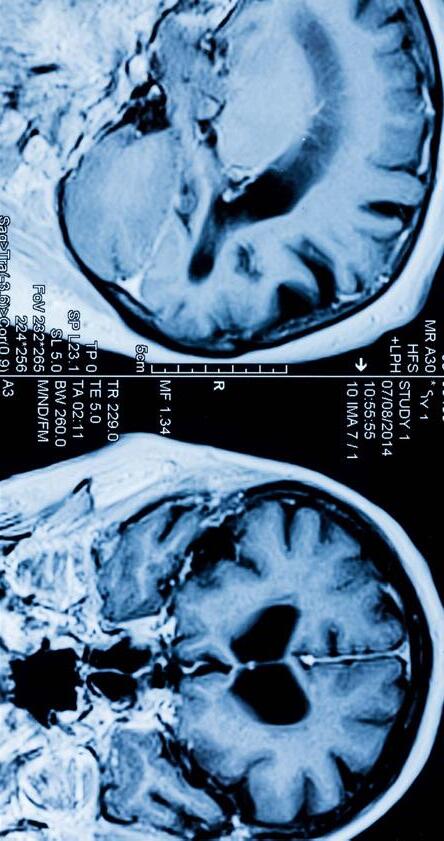











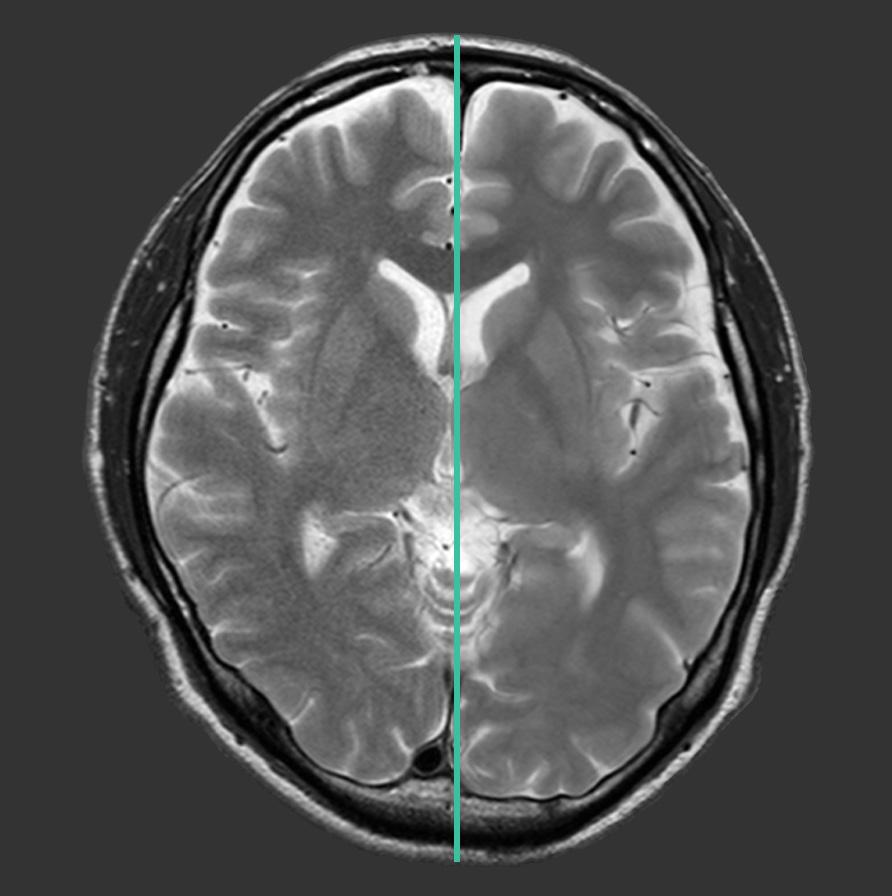
Fujifilm Healthcare Americas Corporation recently launched Version 10 (v10) suite of innovations for Echelon Synergy 1.5T MRI system. Echelon Synergy v10 deploys several cutting-edge technologies, including Synergy DLR Clear, Synergy Vision with StillShot and automated scanning process enhancements.
A recent study found 15-20% of MRI scans require rescan due to patient motion. Synergy Vision, now available for Echelon Synergy MRI, combines multiple in-bore cameras with StillShot artificial intelligence (AI) to mitigate the impact of motion artifacts. StillShot applies AI to correct motion-compromised raw data, referencing real time motion tracking collected during the scan.
Instead of repeating the acquisition, motion can be corrected, providing clearer, more diagnostic images. StillShot helps to streamline workflow for the technologist and provide a better experience for the patient.
The ”Gibbs” or “truncation” artifact has long been an image quality issue with MRI. Radiologists dealt with it or were compelled to call for longer scan time sequences to address it. Synergy v10 brings DLR Clear, a new AI based algorithm to address the truncation artifact, producing images with mitigated artifact without a scan time extension.
“Radial scanning in MRI serves as a common approach to address patient motion, but the technique faced challenges in certain circumstances from unique artifacts. Fujifilm’s v10 software enhancement was designed to help address these challenges,” said Shawn Etheridge, executive director,
modality solutions marketing for Fujifilm Healthcare Americas Corporation. “With v10, technologists can now apply our RADAR radial sequence with our iterative iRCM IP-Recon processing to mitigate spike artifacts, resulting in clear, high-quality images with reduced motion artifact”.
Deep Learning enhanced AutoPose for breast, hip and spine application are added with Echelon Synergy’s v10. AutoPose automatic slice selection, combined with expansion to whole body application for the AutoSet automated table movement capability, and AutoStart automatic scan start on door closure, can save operator steps, enable reduced total exam times, and allow technologists to better focus on patients.
Fujifilm will provide v10 software standard features to current customers at no charge.

Shared Medical Services Inc. (SMS) and Nebraska Medicine have announced the deployment of the Philips Mobile MR 5300 BlueSeal magnet. The MR 5300 with BlueSeal technology is designed to provide revolutionary, helium-free MR imaging capabilities in a mobile format, increasing access to care with advanced medical diagnostics for communities in both rural and urban areas. Philips was the first company to introduce helium-free operations in MR scanners in 2018, with nearly 2 million liters of helium saved.
“We’re excited to partner with Philips and Nebraska Medicine to deploy the first Mobile MR 5300 in the U.S.,” said Maureen Kenney, president of Shared Medical Services. “Introducing heliumfree MR technology into the SMS fleet presents a significant opportunity. The streamlined operations, combined with maintaining the highest level of diagnostic confidence, create a true win-win scenario.”
Philips, a global leader in health technology, developed the MR 5300 with the latest in AI technology and sustainability in mind, delivering a better patient and staff experience that is also better for the environment. Philips BlueSeal technology only uses 7 liters of helium, without the need for refills. The addition of Smart Workflow AI-technology dramatically reduces the steps needed to complete an MR exam – it offers guided patient set-up in under a minute and technology that accelerates MR scans by up to 50%.
“Our system provides superior image quality in a compact, mobile footprint, helping to increase diagnostic confidence for clinicians while expanding quality access and better care to more patients,” said Ioannis Panagiotelis, Ph.D., global business leader of MR at Philips. “The MR 5300 can simplify and automate the most complex clinical and operational tasks, increasing uptime, and ultimately lead to a better staff experience. In turn, this allows them to focus on what matters most – the patient.”
Nebraska Medicine, a nationally recognized health system, will be the first to bring the Mobile MR 5300 into its clinical operations. Samantha Palensky, radiology operations manager at Nebraska Medicine, highlighted the immediate impact on patient services, saying, “We’re excited to be partnering with Shared Medical Services on our new MRI mobile, the MR 5300, providing cutting-edge services to increase our patient capacity and decrease the pressure on our current MRI magnets in-house.”
She added, “We were excited to work with SMS as they were able to meet our demand for a quick turnaround of the new Philips MR, giving us continuity across all of our magnets for our technologists, thus increasing patient satisfaction and capacity for patients to have their scans done sooner.”
On October 25, 2024, the U.S. Copyright Office released the report “Section 1201 Rulemaking: Ninth Triennial Proceeding to Determine Exemptions to the Prohibition on Circumvention to coincide with the Federal Register’s public inspection copy of the final rule in the Section 1201 proceeding, which took effect on October 28, 2024.
Nathan Proctor, the senior director of the U.S. PIRG Campaign for the Right to Repair, shared his thoughts on the report. Proctor writes:
“Despite significant opposition from the medical device manufacturers, it is still legal to bypass technological protection measures in order to fix medical equipment.
Companies that make products from tablets to tractors sometimes use a quirk in copyright law to deny us the right to repair our own devices, or take them to the servicing vendor of our choice 17 U.S.C. § 1201 (known as ‘Section 1201’) is designed to protect copyrighted works from piracy and makes it a crime to bypass a digital lock set up to protect copyrighted content like music, video games or movies. But some manufacturers have exploited that provision to lock consumers into their own expensive, inaccessible repair services, by locking repair functions, too.
These digital locks turn fixing your phone, computer, tractor or medical equipment into copyright infringement subject to civil and criminal penalties.
There is a limited escape valve to this rule, however. Every three years, the Copyright Office reviews exemption requests to make certain types of circumvention permissible under the law. Over the years, the Copyright Office has granted exemptions to all manner of repair activities, concluding that repair is not a violation of copyright. This is important because medical device manufacturers have claimed 1201 violations when non-OEM servicers have bypassed locks in order to service equipment.
Three years ago, the Copyright Office added repair of medical devices to the list of exempted activities under Section 1201. Medical device trade groups opposed this exemption, and even sued to remove the authority of the Copyright Office to issue exemptions (the case was dismissed, but an appeal is pending). The Register of Copyrights noted in the rulemaking that the manufacturers and trade groups have failed to address a reasonable theory as to why the exemption should be rescinded, or that repair of a product is not fair use.”
We have a mission: Self perform on every aspect of our business. Specialize on specific modalities: Pet CT, CT & NucMed. Focus in a key geographic region.


Registration is now open for the 2025 Imaging Community Exchange (ICE) scheduled for February 22-24 in Orlando, Florida. Sign up today at AttendICE.com.
ICE 2025 boasts top-flight educational sessions, a large exhibit hall, networking events and more. Among the additional features are a leadership summit, keynote presentations and a reverse expo.
The conference begins Saturday, February 22 with Leadership Summit events. The Leadership Summit is by invitation only.
The next day features educational sessions starting at 9:30 a.m.

The ICE Break Networking Lunch starts at noon followed by the third educational session time slot at 1:30 p.m.
The first keynote address “The Secrets to Time Management Magic” by Fred Moore starts at 2:45 p.m. followed by the Exhibit Hall Grand Opening from 4-6 p.m. Monday, February 24 has 4 educational time slots. The conference concludes with a signature event – the Margaritaville Finale Party at 5 p.m.
For more information, visit AttendICE.com
Siemens Healthineers has received Food and Drug Administration clearance for two new features in its syngo.PET Cortical Analysis software application that use positron emission tomography (PET) to measure protein deposits in the brain associated with Alzheimer’s disease.
The first new feature, Centiloid scoring, standardizes the quantification of brain-amyloid plaque in PET scans across three commercially available beta-amyloid PET radiopharmaceuticals used to diagnose Alzheimer’s disease.
The other new feature, tau PET quantification, assesses and quantifies the distribution and density of tau protein tangles in the brain from a PET image acquired using the radiopharmaceutical flortaucipir.
Alzheimer’s disease is characterized by the accumulation of both beta-amyloid plaques and tau protein tangles in the brain. Deposits of beta-amyloid and tau occur in different regions and at different rates in the aging brain. Together, these pathologies lead to neurodegeneration, which results in cognitive and clinical decline in individuals with Alzheimer’s disease.
“The ability to quantify the buildup of amyloid plaque and tau protein in the brains of Alzheimer’s disease patients can provide clinicians with important diagnostic and staging information pertaining to the disease,” said Martin Cordell, Ph.D., director of product life cycle management at Siemens Healthineers Molecular Imaging. “The addition of Centiloid scoring and tau PET quantification features to our syngo.PET Cortical Analysis software fortifies our integrated and comprehensive portfolio for detection, diagnosis, monitoring, and follow-
up related to Alzheimer’s disease.”
Centiloid scoring for beta-amyloid PET is relevant in the diagnosis, patient management, and design of clinical trials of Alzheimer’s disease-modifying therapies. The new Centiloid scoring feature from Siemens Healthineers uses a 100-point scale to standardize beta-amyloid plaque PET measurements and enable clinicians to compare results from different PET scanners and tracers. The need to standardize beta-amyloid plaque measurements obtained via PET has increased dramatically with the FDA approval of new therapeutic drugs for Alzheimer’s disease. These drugs are designed to reduce cognitive and functional decline in adult patients with mild cognitive impairment or mild dementia due to Alzheimer’s disease by removing beta-amyloid from the brain.
Tau deposits have been shown to closely correlate with concurrent cognitive performance in individuals with Alzheimer’s disease. The new tau PET quantification feature from Siemens Healthineers uses Braak staging, a six-stage progressional model that classifies the progression of tau pathology in the brain and correlates closely with levels of cognitive impairment, with later stages associated with worse cognitive and clinical symptoms. Tau PET has played an important role in recent amyloid-directed drug trials with respect to patient stratification, drug management, and assessment of treatment response. Given tau’s close association with disease severity, several investigational tautargeted therapies are in different phases of clinical development. Tau PET quantification also has a major role to play in those trials.
GE HealthCare recently announced the launch of the Versana Premier, the latest release within the Versana ultrasound family of reliable, affordable, easy-to-use, and versatile ultrasound systems. Versana Premier offers automation and AI-enabled productivity tools to improve workflow and clinical features designed to enhance clinical efficiency and accuracy, all while delivering an effortless user experience and helping clinicians best meet their patient needs. The Versana Premier is designed to meet the multi-purpose needs of health care professionals across diverse clinical specialties and care areas, including general practice, OBGYN, musculoskeletal (MSK) and cardiology.
“The rising demand for imaging has driven the increasing use of ultrasound in primary care. Ultrasound is emerging as a key tool in these clinical settings, enabling accelerated diagnoses and improving patient outcomes and satisfaction,” said Phil Rackliffe, president and CEO of ultrasound and image guided therapies, GE HealthCare. “Versana Premier is equipped with advanced automated workflow and productivity tools, including educational resources, that can support these clinicians who are often the frontline of disease identification and diagnosis for their patients.”
With advanced features that are intuitive and innovative, Versana Premier empowers clinicians to deliver high-quality care and accurately make decisions to reach a diagnosis with the greatest of ease. Powered by VisionBoost Architecture and accompanied by high-quality probes, including XDclear technology, firstclass display technology and new imaging engine, Versana Premier provides exceptional image quality with faster speed. Users can also optimize images while scanning with Whizz, which continuously optimizes
imaging in real time, and adjust color display with Whizz Color Flow. Other features to support clinicians in clinical decisions include OBGYN imaging tools, like Whizz RenderLive and V-Live 2.0, to capture 3D/4D imaging to clearly follow the baby’s development.
With its enhanced ergonomics, automated tools, service and support, the latest release of Versana Premier offers advanced features for simplified diagnostics and guaranteed time savings.iii Clinicians can experience up to a 38% faster workflow with Whizz clinical features available on the system. Furthermore, AI-powered Whizz LabeI can automate labeling of the right kidney, gallbladder and liver, and the new Whizz Follicle can assist with volume calculations and measurements.
“Versana Premier is remarkably user-friendly and image quality in B-Mode is easy to optimize, making it possible to create amazing images,” said Dr. Martin Altersberger, Director of Echo Laboratory, State Hospital Steyr, Austria. “The ultrasound system integrates advanced functions with optimized image quality and educational resources, which can be used in various settings. It can, therefore, adequately support clinicians in a wide range of assessments and diagnoses.”
Versana Premier is the highest-tier ultrasound system in the budgetfriendly Versana ultrasound family, powered with smart clinical features and streamlined workflow tools to enhance efficiency and provide optimal care to a wide range of patients every day – all with effortless productivity in mind. Versana Premier is available in key countries around the globe. In the United States, Versana Premier is 510(k) cleared by the U.S. Food and Drug Administration and is currently commercially available, with shipments beginning later this month.

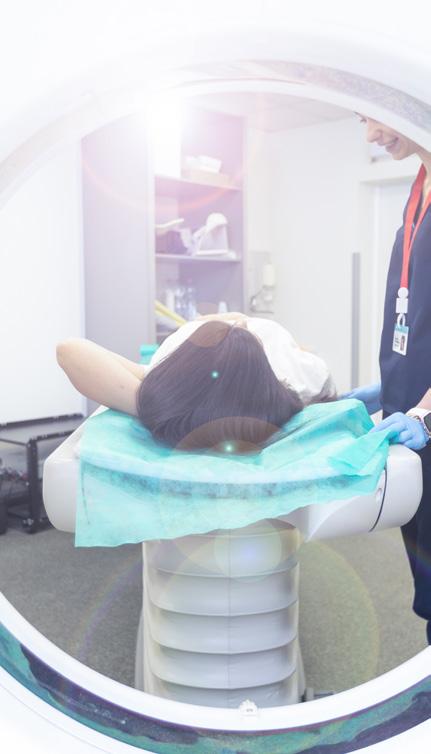
In terventional radiology (IR) departments diagnose and treat disease. IR professionals treat a wide range of conditions in the body by inserting various small devices, such as catheters or wires from outside the body. X-ray and imaging methods, such as CT and ultrasound help guide the radiologist. Interventional radiology can be used instead of surgery for many conditions. In some cases, it can eliminate the need for hospitalization.
ICE Magazine reached out to leaders in diagnostic imaging and IR to find out more about the modality and to share those insights. Participants in this month’s Director’s Circle article on interventional radiology are:
• Michelle Bourns, RT(R), interventional radiology manager, Parkland Health;
• Ken Gleeson, MBA, RT (R) (VI), system manager, interventional radiology, University Hospitals; and
• Alpana Patel Camilli, BS, CRA, (R) (CT), manager, interventional radiology and neuroendovascular surgery, UCSF.
Q: HOW DO YOU ASSESS AND INTEGRATE NEW TECHNOLOGIES OR TECHNIQUES INTO YOUR PRACTICE?
Bourns: New devices and methods are trending in the interventional radiology world. Our physicians and technologist stay current by attending conferences and completing hands-on workshops. Often these workshops are hosted directly within our IR department to allow maximum exposure to our frontline staff that may not have the opportunity to attend outside conferences. This also allows physicians to fully test and evaluate devices before they are used in clinical practice.
Gleeson: Technology moves so quickly in health care it
seems there is always something new on the horizon. When deciding whether to invest in new technologies, it is best to follow a tried-and-true method that includes the following steps:
• Thoroughly assessing what is needed, what problems will be solved and what the benefits are to patients and staff.
• Compare the options available – contact vendors, setup demonstrations, decide which option is best.
• Plan for implementation including staff education and training.
• Track and evaluate outcomes.
• Re-assess and adjust.
Patel Camilli: At UCSF Health, we systematically assess and integrate new technologies by prioritizing cuttingedge solutions that elevate patient care and address complex cases. With the recent acquisitions innovative ablation units, we are enhancing our precision treatment capabilities, especially for patients with challenging tumor presentations. We also stand ready to deploy advanced techniques, such as histotripsy, HIFU, LIFU ensuring our patients benefit from noninvasive, high-impact therapies. By the time patients reach UCSF, they have often exhausted conventional options – our approach focuses on offering innovative, minimally invasive alternatives tailored to deliver better outcomes
Q: HOW CAN INTERVENTIONAL RADIOLOGY BETTER COLLABORATE WITH OTHER SPECIALTIES TO IMPROVE PATIENT CARE?
Bourns: Working closely with other specialties allow for a more comprehensive approach for treatment. IR is part of a larger treatment team that includes oncology, cardiology, vascular surgery and urology – to name a


few. Creating process improvement committees, task forces and multidisciplinary tumor boards provide a platform to showcase advanced techniques utilized in IR. A great example of collaborative care in IR would be a patient receiving treatment for neuro aneurysm coiling procedure then proceeding to OR for an aneurysm clipping procedure. Another example would be a patient with liver cancer receiving chemoembolization in the IR suite then systemic therapy from the oncologist. The multidisciplinary approach can decrease length of stay and provide better patient outcomes.
Gleeson: Interventional radiology can better collaborate with other specialties by taking part in team meetings, providing education to referring physicians as to what treatment options offered by IR may be right for their patients and by getting involved in shared clinical trial and research opportunities. Ideally, interventional radiology would develop and distribute evidence-based referral guidelines that could be shared with physicians across the various specialties. Sharing of an electronic medical record (EMR) helps ease communication between physicians and ensures everyone has access to the same information.
Patel Camilli: Interventional radiology at UCSF actively fosters cross-specialty collaboration through structured partnerships with oncology, neurology, hepatology and cardiology. By participating in multidisciplinary conferences, including tumor boards, we streamline complex case management, ensuring every specialty aligns on the best course of action. Our IR suite also integrates scheduling with these specialties, reducing bottlenecks and ensuring procedures are performed with urgency. We are committed to demonstrating the unique value of IR, educating referring physicians, and offering advanced tools to complement traditional treatment pathways.

Q: WHAT CHALLENGES DO YOU SEE IN TRAINING THE NEXT GENERATION OF INTERVENTIONAL RADIOLOGISTS?
Bourns: The interventional radiologist is a resource for many specialties to seek advice and support for treatment plans for low- and high-acuity patients. The field of IR continues to evolve with technology, imaging techniques and medical devices. Physicians need to train on the latest technology to provide the best of care. This advancement of technology comes with a price and can be challenging for any organization to financially support the advancement in real time. The team must balance providing the best outcomes with older traditional techniques, while trying to keep pace with emerging technologies both educationally and financially.
Gleeson: One of the biggest challenges on training the next generation of interventional radiologists is the nationwide shortage of IR attendings. This forces the existing IR attendings to be spread thinly across coverage areas within their health systems, potentially making them less available to mentor their Fellows and Residents. This also contributes to physician burnout which affects the training experience of future IR physicians. Another challenge is the migration of several types of interventional procedures away from IR such as PE thrombectomies, peripheral artery disease interventions and other procedures that will limit the future IR physicians exposure to the full range of procedures needed for comprehensive training.
Patel Camilli: One of the biggest challenges in training future interventional radiologists lies in balancing the demands of clinical service with hands-on learning, especially as procedures become more specialized. Exposure to complex, high-acuity cases is essential, but it demands a structured learning environment to ensure both quality care and trainee competency. Additionally, future radiologists need advanced communication skills to effectively manage multidisciplinary teams and
provide empathetic care to patients who have already undergone multiple interventions. Rapid technological advances require a dynamic training curriculum to keep trainees fluent in both new technologies and evolving clinical protocols.
Q: WHAT BEST PRACTICES HAVE YOU IMPLEMENTED TO IMPROVE THE OPERATIONAL EFFICIENCY OF YOUR INTERVENTIONAL RADIOLOGY SUITE?
Bourns: Improving operational efficiency in IR is very important not only for high-quality patient care but for frontline job satisfaction. Three areas we focused on were:
• On-time starts
• Room turnaround time
• Employee engagement
We improved on-time starts 25% by standardizing orders, establishing tasks for providers and streamlining the preoperative process. We improved turnaround time 50% by working with clinical engineering to optimize the timing for equipment repairs and partnering with EVS to improve communication and reduce redundancies in the cleaning process. We improved employee engagement scores to the top decile by increasing frequency of one on ones, established daily multidisciplinary team huddles, and involved the team in goal setting.
Gleeson: Best practices applied to operational efficiency in IR suites would include the required use of a robust electronic medical record that provides critical data. This data can then be used to create benchmarks and KPIs to help find optimal workflows by identifying opportunities and deficiencies. Analysis of correct data helped to improve staffing of techs and nurses in the procedural areas as well as the pre- and postprocedural area. The use of “wearable” communication devices dramatically improved the efficiency of communications between team members. The implementation of a pre-procedure brief prior to each case helped reduce “wrong site, wrong side” situations and ensured that any special tools or equipment were available before beginning the procedure.
Patel Camilli: We have implemented standardized workflows, lean protocols, and real-time monitoring of performance metrics to ensure our IR suites operate at peak efficiency. With cross-training initiatives for both body and neuro IR, we’ve optimized staffing across campuses to adapt seamlessly to fluctuating caseloads. The adoption of specific treatment units/equipment allow us to streamline high-precision tumor ablation procedures, minimizing downtime and maximizing
throughput. Daily team huddles and predictive analytics tools ensure we proactively address scheduling, labor, and resource challenges, reducing delays and enhancing patient flow.
Q: WHAT OTHER INSIGHTS CAN YOU SHARE WITH ICE MAGAZINE REGARDING INTERVENTIONAL RADIOLOGY?
Bourns: Like many health care professions, IR has faced shortages. Burnout with IR technologist can be a real concern. The expectations set for an IR technologist can be overwhelming and intimidating. As leaders, we can be proactive and prevent this from occurring. Allowing flexible scheduling between the team gives some control back to the individual. We work hard to provide our team a psychologically safe environment where they feel empowered to speak up when they have concerns. We ensure they feel confident in their skills set by providing personalized training utilizing flow models.
Gleeson: Interventional radiology has come a long way from its beginnings, appearing as a cornerstone of modern, minimally invasive medicine. With its expanding role in oncology, neurology, and beyond, as well as its ability to integrate with innovative technologies like AI and robotics, IR is poised to continue playing an increasingly pivotal role in patient care. As the field adapts to these innovations, the next generation of interventional radiologists, administrators, IR techs and IR nurses will need to embrace both technical proficiency and interdisciplinary collaboration to continue improving patient outcomes in the future.
Patel Camilli: At UCSF, we are redefining the role of interventional radiology by embracing cutting-edge technologies that enable us to treat patients beyond the limits of traditional approaches. Our IR program emphasizes patient-centered care by focusing on outcomes that matter – reduced recovery times, fewer complications and highly personalized treatment plans. We recognize that innovation is not just about technology but also about leadership, which is why we invest in developing future IR leaders who can seamlessly blend clinical expertise with operational excellence. With a commitment to remaining at the forefront of precision medicine, UCSF IR continues to set new standards, ensuring our patients receive the best possible care when they need it most and our goal is to be just in time! •
“I LOVE THE CONTENT THAT ICE PRODUCES.”
- AUDREY HARRIS, IMAGING EDUCATOR, CHILDREN’S OF ALABAMA
“I TRUST AND ENJOY THE CONTENT FROM ICE.”
- HEATHER GRAVES, RADIOLOGY MANAGER, WAYNE COUNTY HOSPITAL
“I PARTICIPATE IN THESE WEBINARS TO ENRICH MY PROFESSIONAL KNOWLEDGE AND TO BE ABLE TO SHARE THE NEWS IN THE FIELD WITH MY STUDENTS.”
- CALIN CORCIOVA, ASSOCIATE PROFESSOR, MEDICAL BIOENGINEERING FACULTY
“THEY ALWAYS PRESENT USEFUL INFORMATION.”
-KATHRYN HALL, AUDITING MANAGER, STAR MEDICAL AUDITING


STAFF REPORT

The global interventional radiology products market is expected to reach $23.9 billion by 2024, according to a Globe Newswire report. Future Market Insights is the source for the report that also states that by 2034, the market is projected to reach $48.8 billion, rising at a 7.4% CAGR. A dynamic industry that has seen substantial growth in recent years, interventional radiology (IR) is one of the most rapidly evolving fields. The advancements in technology and the development of innovative techniques have significantly influenced the future.
The report also states that innovations in technology are expected to shape the future of IR. A number of emerging technologies are poised to significantly impact the field of technology, including augmented reality, robotics, virtual reality and artificial intelligence (AI). Interventional radiologists can benefit from these technologies through enhanced procedural accuracy, improved patient outcomes and expanded scope of practice.
Innovations in IR will improve efficiency and effectiveness in the future as new procedures and techniques are developed. Several techniques may improve patient outcomes, including endovascular repair, embolotherapy and interventional oncology, according to the report.
“Imaging technologies greatly enhance the guidance of interventional procedures. Imaging technologies will continue to advance in IR, including MRI machines, ultrasound equipment, angiography systems, CT scanners and fluoroscopy equipment.
Through these technologies, image quality will continue to improve, procedural planning will be enhanced, and real-time guidance will be enabled during interventions,” the report states.
“Interventional radiology is expanding its scope of practice. Interventional radiologists are researching new applications and therapeutic approaches and improving existing procedures and techniques,” it adds. “A wider range of medical conditions will be addressed by interventional radiologists, and minimally invasive surgery will be offered as an alternative to traditional surgery.”
Global Market Insights (GMI) reports that the “interventional radiology market size was valued at $28.1 billion in 2023 and is expected to exhibit growth at a CAGR of 5% from 2024 to 2032. The rising prevalence of chronic disease worldwide and increasing demand for minimally invasive procedures are significantly driving the market growth.”
Mordor Intelligence reports that “the interventional radiology market size is estimated at $26.96 billion in 2024, and is expected to reach $35.92 billion by 2029, growing at a CAGR of 5.90% during the forecast period (2024-2029).”
Mordor Intelligence’s report explained its prediction.
“The driving factor of the market is the rising trend of minimally invasive procedures, owing to the cost-effective solutions and lesser hospital stays. With the help of minimally invasive techniques, patients are treated quickly and are usually discharged from the hospital on the same day. Most of these processes require imaging technology,” Mordor Intelligence states. •

GE HealthCare’s Allia Platform represents the culmination of a multi-year collaboration with interventionalists and surgeons aimed at enhancing user experience, improving workflow efficiency, and increasing the adoption of advanced image guidance in daily practice. Designed to be a trusted assistant for image guided therapies – the Allia Platform features a robotic gantry with a smaller footprint than previous versions and other features to enhance user experience and improve workflow integration and efficiency. With just one click, users can access all of their essential functions to make it their own personalized workplace that meets the operator’s specific needs and
*Disclaimer: Products are listed in no particular order.

preferences in the interventional or hybrid operating room. Similarly, with the redesigned C-arm making the controls more accessible, it enables an optimized ergonomic setup for the user’s clinical needs, even in complex working positions at the head, neck or left side.
To further advance interventional innovation in image guided therapy, GE HealthCare also continues to expand its offerings of solutions that utilize digitization and artificial intelligence (AI) to help clinicians deliver precision care. The company’s ASSIST imaging software helps users easily access and use augmented reality to help precisely plan, guide and assess sophisticated interventional procedures with greater precision and dose efficiency. Embo ASSIST AI is the latest addition to the suite of ASSIST solution offerings designed to automatically segment vascular structures to facilitate embolization workflow planning, as well as help clinicians visualize and anticipate the destination of potential injections to support their embolization strategy thanks to AI-based simulation.

3The ARTIS icono ceiling, a ceiling-mounted angiography system from Siemens Healthineers, provides imaging guidance for a wide range of routine and advanced interventional radiology and cardiovascular procedures. Its design flexibility combines with intelligent workflows and advanced positioning accuracy. The system’s rotational capabilities and simplified C-arm cabling enable superfast cone beam computed tomography (CT) data acquisitions for reduced motion artifacts and less patient contrast dose. The new Xpand feature¹ enables transverse movement of the C-arm at the push of a button, permitting easier positioning for radial access and allowing the user to move the C-arm out of the way when direct patient care is required. Predefined Case
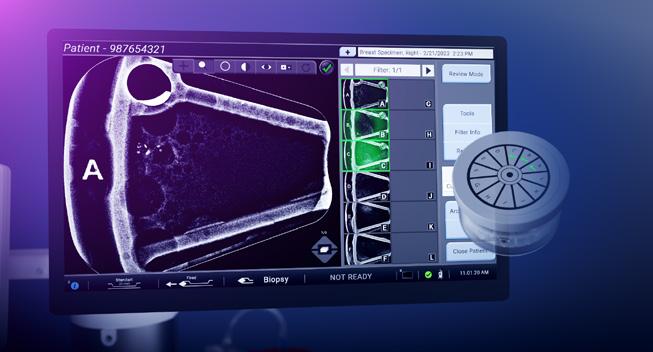
Hologic Brevera breast biopsy system revolutionizes the breast biopsy process by simplifying it into three easy steps, potentially saving up to 12 minutes per procedure.1 This innovation integrates tissue acquisition, imaging, verification, and sample preparation into one seamless process, streamlining the entire procedure. This allows providers to quickly access crucial information at the point of care. Equipped with CorLumina imaging technology, Brevera system empowers physicians to make swift, informed decisions while staying close to the patient. Remarkably, over 92% of patients surveyed found the biopsy experience with the Brevera technology to be faster than expected, highlighting its efficiency.2 Brevera biopsy system can deliver critical information at the point of care about the sample’s acquisition and imaging in as little as 8 seconds per core3, ensuring that both providers and patients benefit from faster, yet uncompromised, quality of care.
References
1. Hologic, Inc. 2021 - Brevera Pulse Wave 3. Physicians surveyed identified 12 minutes average time savings. Actual savings may vary.
2. Data on file. Hologic, Inc. 2019. A Prospective, Block Stratified Clinical Trial to Evaluate the Performance and Operation of the Brevera Breast Biopsy System (NCT03300206) Survey of 201 Medical Professionals.
3. VER-11549-001 Hologic Data on File. Brevera Reusable Driver Functionality Verification Report.

Flows permit precise intraoperative guidance and excellent clinical outcomes with minimal user interaction, faster system positioning, and low patient radiation dose. The new OPTIQ exposure control uses a contrast-based technique that is supported by intelligent, self-adjusting algorithms. OPTIQ automatically considers the source to image distance (SID), collimation settings, grid status, and patient thickness; it also determines and applies the optimal combination of the five available radiation exposure parameters and the detector dose as an additional variable. This exposure control is designed to achieve the requested contrast-to-noise ratio while prioritizing dose reduction.
¹ 510(k)-pending
BY MATT SKOUFALOS

For all the complexities associated with working in the radiology space, the business of administrative duties can often be a secondary consideration to operational needs. In the January 2017 issue of the Journal of the American College of Radiology E. Michael Donner, III, et al, describe these challenges in “Succession Planning and Management: The Backbone of the Radiology Group’s Future.”
“All too frequently, leadership in radiology groups defaults to those willing to do it,” the authors note. “Leadership vacuums commonly exist, and a specific focus on leadership identification and development is not emphasized because clinical work drives the group.”
Part of that is attributable to the notion that, “when entering medicine, most future physicians do not anticipate that they must be adept at business leadership activities,” they write. But compounding the issue are their observations that “most radiology practices do not have comprehensive succession plans,” and that “the current replacement process for a radiology practice leader is all too often an individual reluctantly agreeing to accept the responsibility.”
Rather than letting these considerations fall by the wayside until they necessitate an emergent response, the authors note that the American College of Radiology (ACR) Commission on Human Resources recommends succession planning as a necessity for all practices and offer some guidance on how to follow through with it in a formal, transparent way.
Michelle Nocera, director of radiology academic market at University Hospitals of Cleveland Ohio, said that succession planning became a topic of conversation one day when she realized that, if there were some circumstance by which she were unable to report for work, she’d have no idea who would be called upon to take her place.
“You never want to get in a situation where nobody knows what’s going on to the point that the company is suffering because you’re stuck,” Nocera said. “In my own training in leadership, as a manager and as a director, I have always been one to teach at least a couple people, if not everyone on my team, how and why I’m doing certain things.”
Beyond identifying for a long-term or permanent replacement, succession planning pays dividends in a variety of temporary circumstances as well. Nocera spoke plainly about the need for employees to be able to take paid time off (PTO) without worrying or wondering whether their absence for any length would cause problems for their colleagues, or delay projects.
The best way to achieve this, she said, is for organizations to commit to a process of continuous improvement, both institutionally and interpersonally. In her current position, Nocera said every employee both evaluates and is evaluated by their managers and direct supervisors in a 360-degree process to identify whether they would be
capable of advancement, and if not, how they might improve their performance to better ready them for subsequent opportunities.
“I evaluate all the people who report to me,” Nocera said. “I can review those people every year and say, ‘Are they ready for the next step in their career? If they’re not ready, what can I do to help make them successful and get them ready?’ That then becomes a topic of conversation at our reviews.”
Even for institutional “lifers,” as Nocera describes her own perspective on her current place of employment, there’s always an opportunity to continue to develop professionally and learn new skills and techniques. Advancement isn’t mandatory – plenty of people are happy in their current roles in addition to being well-suited to them – but committing to a process of continuous professional development affords every employee the opportunity to be supported in their own individual growth.
“Sometimes it’s hard for some people to stay in a role and not continue to advance,” Nocera said. “Some of those roles aren’t out there, and workers have to go somewhere else. But I also have a number of people who like where they’re at and what they do, and we just continue growing them. To come to work every day knowing that you love your job – that is the plan.”
A key component of helping employees continue to grow professionally involves developing clearly defined roles, responsibilities and expectations. Nocera spoke about the need “to map everything out, be very detailed, and share what I’m doing” with the employees to whom she reports and those who report to her. By way of example, she meets with a department manager to keep them in the know about director-level conversations that would affect the way that manager might work or might lead their employees.
“A lot of times, you might hear in your employee engagement series that staff don’t feel like they’re considered in decisions made higher up, so I try to have that dialogue to bring them in and fold them into that.”
“In radiology, we’re hands-on,” Nocera said. “That’s how our brains work. We have to be doing things to interact and remember. It is a continuous process developing an employee.”
In settings where there’s no structured process in place for employee development or for succession planning, Nocera recommends striking up a conversation with human resources or with institutional leadership to ask them whether there are any plans to create such channels, or opportunities to build them within the organization.
“Start with human resources and see whether they have any type of organizational development and management leadership programs,” Nocera said, “and if not, work with them to create leadership programs.”
Once such programs have been created, there’s additional work to be done to spread the word about them within the organization, she said. Peer evaluation systems, co-

mentorship programs, team-building efforts, and comparable processes help identify opportunities to develop leaders as well as areas of shortfall among other skilled employees. Cross-discipline training is another way for skill-building and talent evaluation to support institutional resilience and identify chances for streamlining workflow where possible.
“When you review your talent, you can see what knowledge and experiences are needed for professional development,” Nocera said. “I went through and talked to other leaders in different disciplines – people in the cancer center, people in respiratory therapy – because they have the same kind of information that we have.”
Nocera also recommended undergoing the process with the help of systems analysts or data teams that will be able to help develop and quantify their understanding of employee skill sets and opportunities to improve patient volumes, engagement scores, gaps in quality assurance, or any other key performance indicator that can help an organization and its members thrive.
“If your area doesn’t have the metrics to be able to see that, see if there’s somebody within that team that can help get you that data so that you can look at it daily or weekly,” Nocera said.
“The big thing out there right now is diversity, equity and inclusion (DEI) strategies; making sure that you’re broad in opportunity and access, and that the makeup of your leadership reflects the makeup of your workforce.”
Once that process is underway, the work of identifying
which employees will make the best new leaders for an institution can begin. Strong leadership qualities can include things like effective communication strategies, shrewd resource management, innovative approaches to jobrelated tasks, thoughtful conflict resolution, and the ability to translate a broad variety of employee perspectives into supportive actions that benefit the group as a whole.
“We want to make sure that we are always looking for different types of leadership,” Nocera said. “I want other people’s ideas and their types of leadership styles in the mix.”
When succession plans aren’t in place, sudden employee departures can be challenging to navigate. Nocera said she’s had the experience of joining a team whose leader retired without leaving any trace of their workflow behind. That loss of insight into daily processes is just one example of the withering of institutional memory that can occur when employees leave, and its effect can be cumulative across the workplace.
“In preserving institutional memory, I really like having that document that explains standard work,” Nocera said. “Document those things that we do every day, week, month, and keep it available. Write down the things that you have to do so that one, you don’t forget anything, and two, if it changes, it’s documented somewhere.”
Operating in the age of cloud-based storage offers an even easier opportunity for management teams to catalogue and share their work with anyone else in their organization for ease of access.
“If I left tomorrow, they could go on my OneDrive and see pretty much everything that’s happening,” Nocera said. “Building that institutional memory means really figuring out what’s going on every day instead of relying on individuals; creating resilient teams, so that if one person went away, that team still knows what’s going on.”
The value in that process extends beyond employee departure or illness, as well. Nocera knows she’s years away from her own retirement, but nonetheless doesn’t want to leave her coworkers in the lurch when she is ready to move on.
“I want to make sure that I leave my coworkers the ability to be successful,” she said, “ensuring that leadership remains headed in the right direction, and able to navigate change. Our industry is constantly changing, and we need to always be adaptable and creative to continue to live our mission, vision and values. We won’t be successful if the next generation of leaders aren’t able to understand what our organizational goals are.”
Nocera said the best way to certify that institutional priorities are met by various generations of leadership is to hard-wire it into institutional culture from the beginning. Succession planning involves consistent reinforcement of operational and long-term goals so that any time change occurs, everyone can remain in alignment with them.
Katherine A. Mohr, DBA, a consultant, speaker and educator, stresses the vital need for succession planning.
She believes it should always be a priority – kept “on a gentle simmer” – to ensure smooth transitions and prevent unexpected challenges. Continuous attention to this process prepares organizations for future changes.
“A great example of a successful succession plan occurred when I was transitioning out of one of my previous management roles,” Mohr said. “I had a specific person in mind to take my place; someone I had been closely monitoring and who stood out to me. It was one of my lead technologists, who consistently demonstrated exceptional skills and leadership potential.”
“During one of our casual check-ins, I decided to bring it up. As we chatted, and I asked her, ‘Are you ready for the next step in your leadership journey?’ she smiled and said, ‘Maybe in three to five years.’ I replied, ‘That’s perfect! I’m working towards a directorship, and if everything goes as planned, I’d love to mentor you into this role.’ ”
Mohr initiated a year-long process to enhance the technologist’s leadership skills, preparing her for the possibility of stepping into the leadership role. This process included tailored managerial training sessions, practical examples of daily departmental challenges, and ongoing support to build her confidence and expertise. After Mohr transitioned to a higher-level position at another institution, she committed to coaching the tech for an additional six weeks. This ensured a smoother transfer of knowledge and insights, allowing the department to thrive under its new leader.
“When I left my institution for a directorship, I ensured that I left a highly capable person in place, equipped with all the necessary tools for the job,” Mohr said. “I told my boss, ‘Give her a chance.’”
“It’s important to assess your team to identify individuals who are both interested and capable of taking on new responsibilities,” Mohr said. “You should start looking for these qualities in your team as soon as you assume a leadership role, regardless of where you are.”
“As a manager, I enjoy sharing my knowledge with my team,” she said. “I would never want to leave my department in a pickle where crucial information isn’t shared. Some people tend to hoard information because they believe it makes them more valuable; however, sharing our knowledge fosters a stronger team dynamic and helps everyone feel more confident in making autonomous decisions, even in the absence of a leader.”
As a consultant, Mohr has the opportunity to visit various institutions and identify potential leadership candidates based on their level of interest and current activities.
“You need to understand your staff and build from there,” she said. “Involve potential leaders in meetings, share departmental information with them, and watch how their leadership skills develop over time.”
“I strongly believe that implementing a clinical ladder process within a larger organization enhances employee engagement and fosters a sense of connection with leadership,” Mohr said. “In leadership roles, being open and
sharing information can cultivate a positive atmosphere, which can help mitigate negative feedback.”
By holding one-on-one meetings to discuss career goals, employees who may excel in leadership positions can be more easily identified. Understanding their aspirations, both professional and personal, enables leaders to assign tasks to their employees that support their growth into leadership roles.
“Giving employees a clearer understanding of the budget, the process for ordering supplies, and the locations to find new or replacement items when necessary encourages them to think more broadly and explore different options,” Mohr said. “A good leader consistently follows up after introducing these ideas; many leaders neglect this because they become too busy with other tasks, which undermines the example they are trying to set.”
Safeguarding institutional priorities begins with “hiring from within and mentoring upwards,” Mohr said. Organizations that practice this approach foster departmental and interdisciplinary cohesion and enhance record-keeping, which helps preserve institutional memory.
“I believe that when hiring someone for a leadership position, organizations should discuss succession planning on day one,” she said. “We need to share information continuously and document it so that it remains on everyone’s radar. Ultimately, this ensures the longevity of the institution.” •
For more information on this and more important topics, check out the upcoming educational sessions at the Imaging Conference & Expo at AttendICE.com/education/

A niche job board for the HTM and imaging communities
350+ open job opportunities
Single-job postings to 12-month unlimited memberships
3200+ biomedical and imaging candidates
htmjobs@mdpublishing.com
htmjobs.com

BY NICOLE DHANRAJ
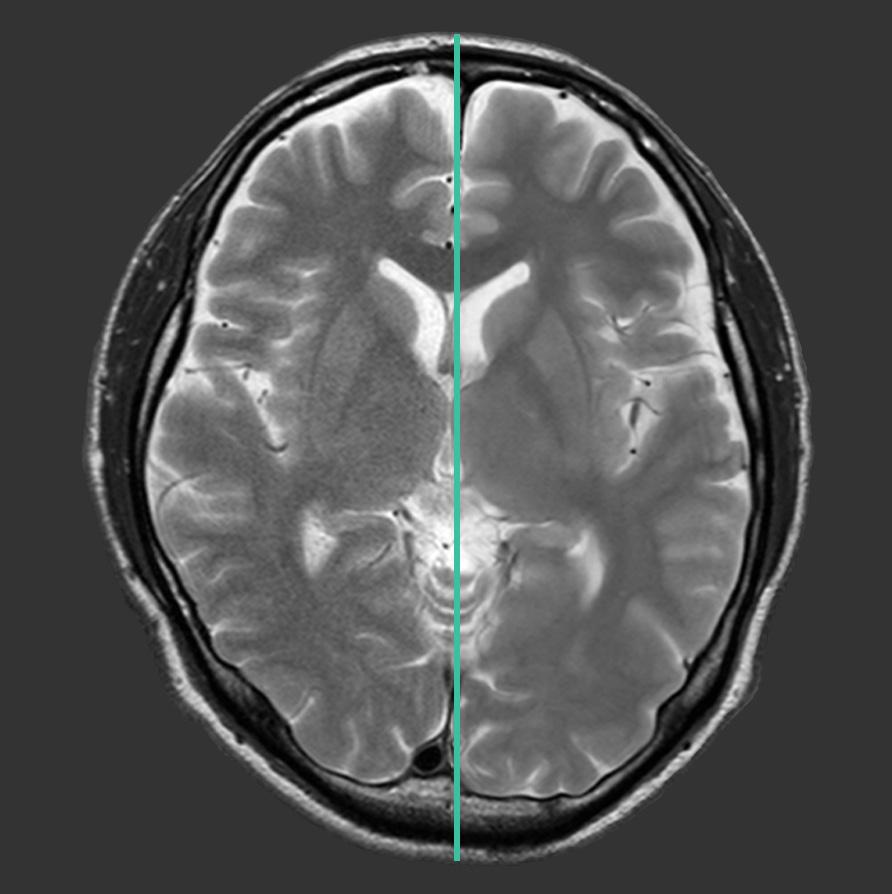
As an imaging leader, you’re familiar with the growing challenge of staffing shortages. The decision to bring in unlicensed MR technologists may seem like a practical solution, but it’s crucial to approach their training with care and precision.
From my own observations, I’ve seen firsthand the pitfalls of inadequate training and the dangers of expecting unlicensed staff to “wing it” in critical areas.
This article highlights why a haphazard training approach is not only risky but can seriously compromise patient safety and operational efficiency.
Integrating unlicensed MR technologists presents significant challenges that are exacerbated by inadequate training:
• Patient Safety: Insufficient training often means these technologists struggle with MRI physics and protocol adjustments. This can lead to incorrect parameter settings, resulting in poor image quality and potential risks to patient safety.
• Image Quality: Unlicensed technologists may produce subpar images without a solid grasp of MRI principles and anatomy, leading to misdiagnoses or unnecessary repeat scans. This lack of foundational knowledge impacts diagnostic accuracy and overall patient care.
• Equipment Integrity: Poorly trained technologists are more likely to mishandle MRI equipment, which can result in costly repairs and operational delays. Proper usage and maintenance ensure the longevity and efficiency of your equipment.
• Safety Protocols: Many unlicensed
technologists are unfamiliar with critical safety protocols, increasing the risk of accidents and adverse events. Comprehensive training ensures they are prepared to handle emergencies and adhere to safety standards.
• Training Overload: Trainers often lack the time or resources to provide in-depth instruction, leading to a situation where unlicensed staff may be left to “wing it” rather than receiving the thorough, handson training they need.
From my observations, cutting corners in training for unlicensed MR technologists is problematic for several reasons:
• Unlicensed technologists frequently do not fully grasp MRI physics or the nuances of protocol adjustments, leading to errors that affect patient safety and image quality.
• Insufficient training often means gaps in essential knowledge, such as anatomy and safety protocols, which can compromise the effectiveness of their work and increase the risk of errors.
• Inadequate training can lead to operational inefficiencies, including equipment misuse and a higher incidence of adverse events, which can impact both patient care and departmental efficiency.
ESSENTIAL ELEMENTS OF EFFECTIVE TRAINING
To prevent these issues, ensure your onsite training program includes:
• Your unlicensed techs need a strong grasp of MRI physics, safety principles, and anatomy. This knowledge is critical for performing their duties effectively and safely.
• Structured, supervised practice helps build confidence and competence. Unlicensed technologists must receive this guidance to avoid making costly mistakes.
• Training must cover emergency management protocols to ensure quick and effective responses when issues arise.
• Regular evaluations help track progress and address any gaps in knowledge or skills
• Providing opportunities for continuous learning helps technologists stay updated with the latest advancements and best practices.
As the leader of your department, your role is crucial:
• Invest in a well-developed training program that ensures all staff are adequately prepared.
• Make training a key part of your departmental budget and schedule, especially if you are using techs that are not formally trained.
• Actively engage with your team to understand their training needs and provide the necessary resources and support. Yes, operations are chaotic, but you must not overlook what they need.
MRI environments, we know are inherently complex and risky. The stakes are high, and the margin for error is minimal. Proper training, evaluation, and competency are not just optional – they are essential to ensure patient safety is never


compromised.
Unlicensed MR technologists can play a valuable role in alleviating staffing shortages, but this comes with the serious responsibility of ensuring they receive comprehensive and rigorous training.
Neglecting to ensure that our technologists receive proper, thorough training – assuming they’re adequately prepared or have enough time to learn – can introduce serious risks. These include compromised image quality, a higher likelihood of accidents and, most critically, potential patient harm.
As leaders in imaging, it is our duty to invest in robust training programs that provide unlicensed technologists with the foundational knowledge, practical skills and safety protocols they need.
Continuous evaluation and ongoing education are crucial to maintaining high standards of care and ensuring that all staff, licensed or unlicensed, are prepared to operate effectively and safely.
Let’s commit to excellence and ensure that our training programs reflect the seriousness of the MRI environment, ultimately protecting both our patients and our practice.
If you’re seeking guidance on developing or improving your training programs, please reach out.
I’m here to help you create a safer, more competent team and uphold the highest standards of patient care. •
Nicole Dhanraj, Ph.D., SHRM-SCP, PMP, GPHR, CPSS, CRA, R.T(R)(CT)(MR), is an experienced imaging director.
- New Windows 10 Platform with Dynamic Digital DR Panel
- Eliminates the OEM Saturn Windows 95 Platform
- Dose Reduction
- HIPAA Compliant, 510k approved.
- Fluoroscopy digital recording loops for MBS studies
- Upgrade Provided to your Proven R/F System in 4 days.
- Complete Refurbished Systems Available


BY MARK WATTS PACS/IT/AI
bdominal aortic aneurysms (AAAs) pose a significant health risk, with rupture often leading to fatal outcomes. Traditionally, clinical management and rupture risk assessments have heavily relied on measuring the aneurysm’s maximum diameter. However, this parameter alone is insufficient to capture the full complexity of rupture risk, as it does not account for the biomechanics or the structural properties of the aneurysmal wall. Recent advancements in artificial intelligence (AI) and machine learning (ML) are providing a more nuanced approach, integrating patient-specific biomechanical characteristics and structural integrity data to enhance rupture prediction. This article delves into the potential of AI in AAA rupture forecasting, exploring how biomechanical and structural analysis can augment the predictive capabilities beyond maximum diameter.
AAAs are localized enlargements of the abdominal aorta that can lead to life-threatening ruptures if left untreated. Traditionally, rupture risk has been associated with the aneurysm’s maximum diameter, with larger diameters suggesting greater rupture risk. However, studies have shown that ruptures can occur in aneurysms below critical diameter thresholds, highlighting the need for a more sophisticated predictive model.
In recent years, the field of medical imaging has witnessed an explosion in the application of AI to enhance diagnostic accuracy and treatment planning. This article examines how AI, coupled with biomechanics and structural analysis of the aneurysm wall, offers a promising pathway for improving rupture risk predictions and providing personalized care.
The maximum diameter threshold (often 5.5 cm for men and 5 cm for women) has been the primary criterion for determining surgical intervention. While simple and widely used, this threshold has limitations.
• Neglect of Wall Stress: The diameter alone does not account for variations in wall stress or structural strength.
• Patient-Specific Factors: Maximum diameter does not consider patient-specific variables such as tissue composition, biomechanical forces, or inflammatory status, which can impact rupture likelihood. These limitations highlight the need for a more comprehensive and personalized approach, incorporating biomechanical modeling and structural data.
Biomechanical analysis considers the forces exerted on the aneurysm wall and provides insights into how these forces impact the structural stability of the aneurysm. Key biomechanical factors include:
• Wall Stress and Strain: The stress on the aneurysmal wall can vary significantly across different sections. High-stress areas are more prone to rupture, even if the diameter is within safe limits.
• Intraluminal Thrombus (ILT): Many AAAs develop an ILT, which can act as a protective cushion but may also promote wall degradation over time. ILT thickness and distribution influence the aneurysm’s biomechanical profile.
• Blood Pressure: High blood pressure can increase wall stress, but the effect varies based on patient-specific anatomy and wall strength.
Analyzing these biomechanical aspects with traditional methods is challenging and time-intensive. However, AI models trained on large datasets can rapidly assess these parameters and predict rupture risks with high precision.
CHARACTERISTICS OF THE AAA WALL
The structural integrity of an aneurysmal wall is determined by various factors, including:
• Tissue Composition: Collagen and elastin are key structural proteins in the aortic wall. Degradation of these proteins weakens the wall and increases rupture risk.
• Histopathological Changes: Inflammation, calcification, and
neovascularization within the aneurysmal wall are indicators of tissue degradation and increased rupture susceptibility.
• Microstructural Anomalies: Microscopic examination of aneurysmal walls reveals fiber orientation, alignment, and density, which can impact the wall’s response to stress. By integrating structural characteristics into AI models, clinicians can better understand the interplay between tissue composition and biomechanical forces, leading to improved rupture predictions.
AI models can revolutionize AAA rupture prediction by integrating biomechanical, structural and clinical data to provide a holistic understanding of aneurysm stability. Key approaches include:
• Machine Learning Models for Rupture Prediction
ML algorithms, such as support vector machines, random forests, and neural networks, are capable of handling complex, high-dimensional datasets, making them well-suited for predicting AAA rupture. These models can be trained on historical AAA data, learning the relationships between biomechanical parameters, structural characteristics and rupture outcomes.
• Deep Learning for Image-Based Biomechanical Analysis
Deep learning, particularly convolutional neural networks (CNNs), has shown promise in medical imaging analysis. CNNs can analyze CT and MRI scans of AAAs to extract detailed information on wall thickness, ILT presence, and tissue composition. This data can then be fed into biomechanical models to predict wall stress distribution and identify rupture-prone areas.
• Integrating Multimodal Data
AI models that combine imaging data (for structural analysis), biomechanical simulations (for wall stress and strain), and patient demographics (for personalized risk) offer a comprehensive approach to rupture prediction. For example, multi-modal networks can take CT imaging data and combine it with blood pressure measurements, resulting in personalized biomechanical risk assessments.
Several studies have demonstrated the effectiveness of AIenhanced biomechanical models in predicting AAA rupture:
• Wall Stress Analysis Models: Researchers have used finite element analysis (FEA) models to simulate wall stress distributions. When integrated with ML algorithms, these models have accurately predicted rupture-prone AAAs, even in patients with diameters below the intervention threshold.
• Histological and Biomechanical Modeling: AI models trained on histological data (such as collagen and elastin density) and biomechanical parameters have shown high predictive accuracy, providing a better assessment of wall integrity than diameter alone.
• Personalized Rupture Risk Prediction: Machine learning models trained on patient-specific data (e.g., blood
pressure, genetic predisposition, lifestyle factors) have been used to predict rupture risk on an individual basis, allowing for more tailored treatment plans. These case studies underline the power of AI to go beyond static metrics, providing a dynamic and patient-specific risk assessment.
While AI has significant potential, there are challenges in implementing it for AAA rupture prediction in clinical practice:
• Data Limitations: AI models require large datasets to achieve accurate predictions. However, AAA rupture data can be limited, and access to comprehensive, multi-modal data remains a challenge.
• Interpretability: Many AI models, particularly deep learning prediction tools into existing clinical workflows without disrupting care delivery will be crucial. Models need to be user-friendly and accessible for non-specialists.
• Validation and Regulatory Approval: AI models require extensive validation across diverse populations before they can be widely adopted in clinical settings. Regulatory agencies are also in the early stages of establishing frameworks for AI tools in health care, making approval processes complex. Future research directions may focus on creating standardized datasets, improving model interpretability, and developing guidelines for integrating AI predictions with clinical decision-making.
AI has the potential to revolutionize AAA rupture prediction by moving beyond the limitations of maximum diameter and incorporating biomechanical and structural data. Through machine learning and deep learning, AI models can process vast amounts of complex data, including wall stress, tissue composition, and patient-specific characteristics, providing a personalized approach to risk assessment.
The integration of biomechanics and structural analysis into AI models allows for a more comprehensive understanding of AAA rupture risk, offering a safer and more efficient approach to clinical management. Although challenges remain, continued advancements in AI technology and collaborative research will likely pave the way for more accurate, patient-specific predictions and ultimately reduce the incidence of life-threatening aneurysm ruptures. •
Mark Watts is an experienced imaging professional who founded an AI company called Zenlike.ai.
For further reading, consult foundational studies on biomechanics in AAA rupture, recent publications on AI applications in radiology, and guidelines on integrating AI in clinical practice. Specific AI methodologies and case studies in AAA rupture prediction are well-documented in medical imaging and machine learning journals, which provide in-depth technical insights into model development and validation.
BY DANIEL BOBINSKI EMOTIONAL INTELLIGENCE
In many ways, building an effective team is a lot like baking a tasty desert. You have to get the recipe right. Sure, bakers can add their signature flourishes, but without the essential ingredients, even the fanciest design won’t compensate for bad taste if a key ingredient is missing. The same goes for team building. No matter how charming or creative the leader’s style, certain foundational elements must be in place for any team to thrive.
What follows are five ingredients every team needs, but before I get to those ingredients, let me underscore the necessity of ensuring you have the right people on your team. In his book, “Good to Great,” Jim Collins points out that your organization is like a bus. The leader drives the bus, and to be successful, the right people must be on the bus. Therefore, hiring correctly is fundamental.
But what if you inherit a team? If that’s the case, the leader must ensure that people are in the right seats on the bus. About 15 years ago I was called in to work with a team, and in short order, I realized that all the people were quite talented, but about a third of them were in the wrong jobs. This made the team less effective, because a third of them weren’t really passionate about what they were doing. Unfortunately, the team leader did not act on what I pointed out, and a year later he was replaced.
In other words, a fundamental understanding for any team is to not only have the right people on the bus, but also
have them sitting in the appropriate seats.
As for the five key ingredients below, don’t just skim over them. If you’re a team leader, ask yourself, “Am I truly providing these elements?” If you’re a member of a team but not the leader, ask yourself, “How can I help establish or reinforce these elements?”
This list is far from exhaustive, but I believe every team needs at least these five things to function at its best.
1. Honesty. This seems like a nobrainer, but I’ve lost count of how many employees tell me honesty is missing from their workplace. People need leaders and team members they can trust. This mean no half-truths, no sugarcoating, no bluffing your way through answers. If you don’t know something, be honest about it. Say something like, “I don’t know right now, but I’ll find out.”
Of course, if you say you’re going to find out, definitely do so and report back. Also, by all means, don’t lie. When – not if – a lie is found out, it’s game over for trust. From that point forward, anything you say will have a cloud over it. Leaders set the tone for honesty, but being honest is everyone’s responsibility. If you make honesty the norm for yourself, other people on your team are more likely to practice this principle.
2. Trust in Your Team Members. Assuming you have the right people on your team and they’re in the right positions, if they know their job, let them do it. So many employees tell me, “They train us, but when it’s time to make decisions, they don’t let us do what we were trained for.”
When you hire the right people and
give them the training and tools they need, trust them to get the job done. If you don’t, their passion will fizzle and they’ll do only the bare minimum. If you find you genuinely can’t trust your team, it may be time to ask some people to get off the bus. But while you’re at it, also review your hiring and training processes.
3. Mutual Respect. Long ago I was told, “Give what you want to get.” That’s especially true for respect. If you want your team to respect each other – and you – then you must first show respect to others.
Being respectful is not complicated. It starts with being polite instead of demanding. It means talking with people like they’re people, not subordinates or excess baggage. Listen to what people say and take their input seriously. Just because someone sits lower on the org chart doesn’t mean you can talk down to them. As the legendary advertising executive David Ogilvy put it, “If you treat people like dwarfs, you become a company of dwarfs. But treat them like giants, and you build a company of giants.”
4. Recognition. Everyone likes to be recognized. Some want public acknowledgement while others prefer it one-to-one. Either way, people want to know their input if valued. However, don’t stop at individual praise. Also be sure to celebrate the team as a whole. Both types of recognition are important.
5. Support. Teams cannot thrive without support. This goes beyond just saying, “I’ve got your back.” It means
showing both practical and emotional support. Are you giving your team members the tools and resources they need? Do they feel like you’re in their corner when things get tough? Without real support, weaknesses emerge, and over time those weaknesses become magnified. This is something teams must guard against, because cracks in a team’s foundation rarely show up overnight. They often grow slowly, over time, and can eventually cause major problems.
It’s also important for team members to support other team members. However, be sure that one person does not become the support system for the entire team. If something should happen to that person, the resulting gap can have a significantly negative impact on productivity.
Bottom line, if you’re leading a team, take time to reflect. Are the elements listed above truly in place, or do blind spots exist? It’s an important review, because when the basics are solid, then you can add your personal leadership flourishes and take things to the next level.•
Daniel Bobinski, who has a doctorate in theology, is a bestselling author and a popular speaker at conferences and retreats. For more than 30 years he’s been working with teams and individuals (1:1 coaching) to help them achieve excellence. He was also teaching Emotional Intelligence since before it was a thing. Reach him by email at DanielBobinski@ protonmail.com or 208-649-6400.
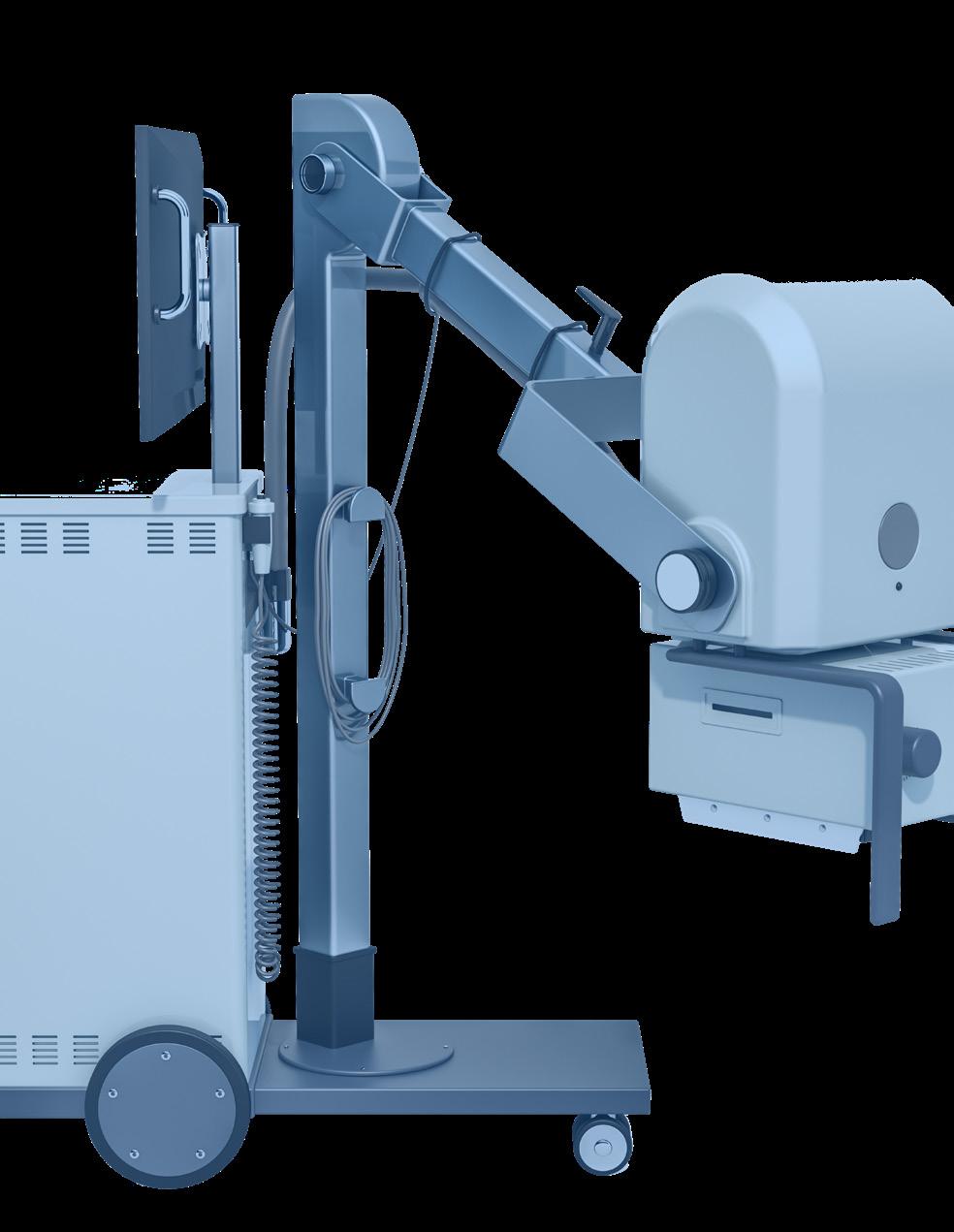
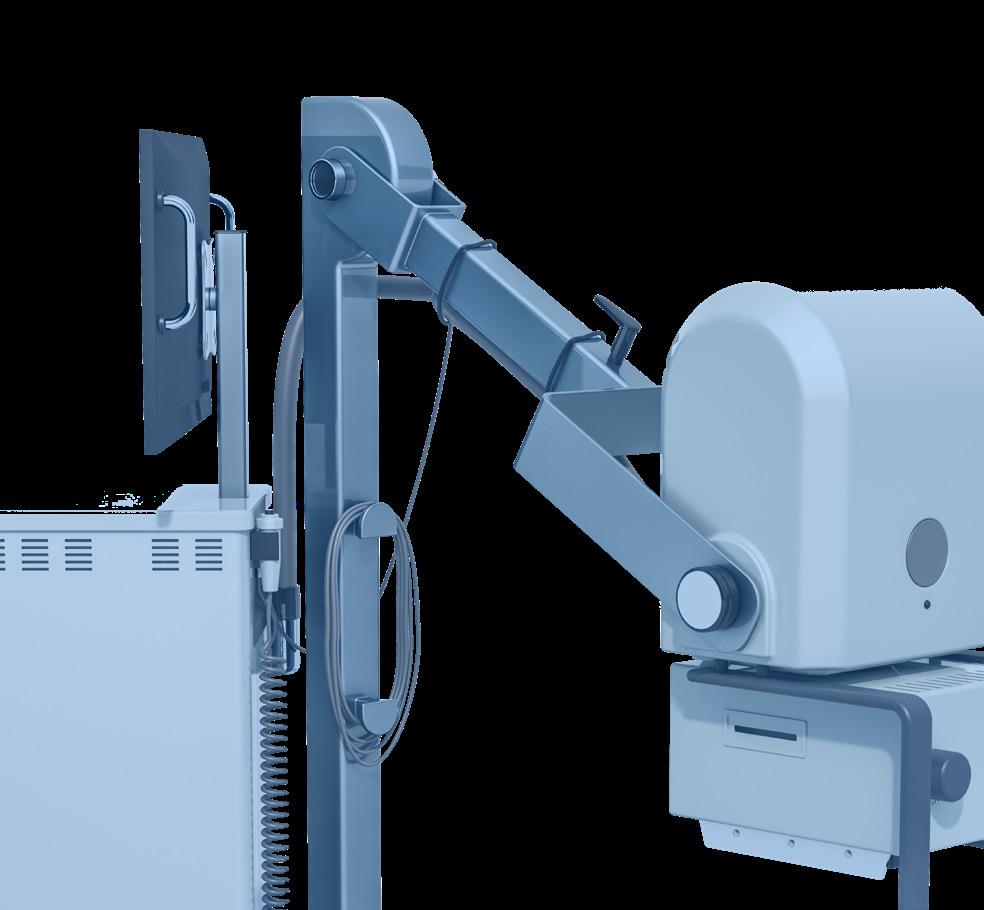



BY NICOLE DHANRAJ DEI
arginalization in health care – especially in radiology – goes beyond statistics; it’s a real challenge affecting patients’ access to essential imaging services.
Imagine a patient in pain, needing an MRI to diagnose a chronic condition but facing barriers based on geography, finances or cultural background.
For radiology leaders, addressing these barriers isn’t just about making patients feel welcome – it’s about saving lives by ensuring fair, timely access to imaging.
WHAT DOES MARGINALIZATION LOOK LIKE IN RADIOLOGY?
Marginalization in radiology occurs when patients encounter obstacles that others don’t: longer wait times, fewer referrals or lack of nearby imaging centers. These challenges can delay diagnoses, affecting outcomes for conditions where early detection is crucial, like cancer and cardiovascular disease.
As Dr. Martin Luther King Jr. once said, “Of all the forms of inequality, injustice in health is the most shocking and inhumane.” In radiology, this truth is clear – a lack of access to imaging can mean the difference between life and death.
THE REAL IMPACTS OF MARGINALIZATION IN RADIOLOGY
Take, for instance, a Black patient with persistent symptoms who is less likely to be referred for advanced imaging than a white patient with similar complaints.
Research suggests that biases – whether in clinical decisionmaking, financial resources or logistical challenges – can prevent
these patients from receiving the imaging they need.
In rural areas, patients may face hours of travel to the nearest imaging center, a major hurdle for those with limited transportation or work flexibility. By addressing these gaps, radiology managers can help ensure that quality care is accessible to all.
EFFECTIVE STRATEGIES RADIOLOGY LEADERS CAN IMPLEMENT TODAY
Creating a truly inclusive radiology department requires more than good intentions. The following steps offer practical and impactful ways for managers to make a difference:
• Data-Driven Equity: Using Analytics to Close Gaps
Radiology leaders can use data to uncover disparities in their department. Regularly reviewing referral rates, wait times, and follow-up appointments across demographics can highlight gaps in access and treatment. For instance, if Black or rural patients consistently have longer wait times, consider adjusting scheduling priorities or adding additional appointment slots for high-risk communities.
• Community Advisory Panels: Hearing from Those We Serve
Understanding patient experiences is vital. Establish a community advisory panel made up of patients and community leaders from marginalized backgrounds. Quarterly meetings with the panel can cover topics like accessibility, communication, and comfort during procedures, allowing for feedback that informs policies and improves outreach efforts.
• Collaborate with Public Health Organizations for Preventive Imaging
By partnering with public health organizations and local nonprofits, radiology leaders can extend their reach into underserved communities. Organizing “Radiology Days” at community centers, offering low-cost or free imaging like mobile mammograms or lung screenings, builds trust within communities and promotes preventive health.
• Leveraging AI Tools to Minimize Diagnostic Bias
Artificial intelligence (AI) can reduce diagnostic bias by analyzing patient data without preconceived notions, ensuring fair access to advanced imaging. Piloting AI-powered tools for referrals and diagnostics, and collaborating with IT to ensure they work effectively for diverse populations, can help maintain consistency across all groups.
• Introducing Sliding Scale or Subsidized Imaging Programs
Financial barriers prevent many patients from accessing necessary imaging. Establishing a sliding scale fee structure for high-cost services like MRIs or CT scans, with funding options through grants or community health initiatives, can make services more accessible for patients facing financial constraints.
• Diversity Mentorship Programs: Building a More Inclusive Workforce
A diverse radiology team fosters trust and understanding with patients from marginalized backgrounds. Developing a mentorship program for young professionals from underrepresented communities, in partnership with local universities, can enhance team diversity and cultural competence.
• Patient Navigation Programs for Supportive Follow-Up Care
After a scan, patients often need clear guidance on their results
and next steps. Establishing a patient navigation program that assists with scheduling follow-ups, explaining imaging results in simple terms, and helping patients access additional resources can improve outcomes, especially for those with limited health literacy.
• Form a Health Equity Quality Improvement (QI) Committee
A QI committee focused on health equity provides oversight of equity goals in the radiology department. Setting metrics specifically for health equity – like access to imaging types and diagnostic accuracy – alongside quarterly audits, allows for ongoing assessment and adjustments to improve fairness and accessibility.
Addressing marginalization in radiology is a gradual but essential journey. By implementing data analytics, AI tools and community partnerships, radiology departments can make strides toward a more inclusive environment.
Every small improvement, from patient navigation to affordable imaging, adds up to a big impact on patient care. This isn’t just about individual patients – it’s about fostering a health care system where everyone has the opportunity to access timely, quality imaging. With dedicated effort, we can ensure that diagnostic imaging becomes a bridge to better health outcomes for all, not just a select few. •
Nicole Dhanraj, Ph.D., SHRM-SCP, PMP, GPHR, CPSS, CRA, R.T(R)(CT)(MR), is an experienced imaging director.

IMAGING CONFERENCE & EXPO
FEBRUARY 22-24, 2025 • ORLANDO, FL
25 hours of accredited CE education
Exhibit hall featuring the latest technology, products and services
The opportunity to win great door prizes donated by exhibiting vendors.
Keynote address on The Secrets to Time Management Magic
The industry’s best networking events to connect and share best practices with other leading imaging professionals
Margaritaville at ICE Finale Party
Rosen Plaza Hotel







Technology applications in the fitness industry continue to build momentum as wearable technology, mobile exercise apps and data-driven training technology all appear in the top 10 of the 2025 ACSM Worldwide Fitness Trends. The report was published by the American College of Sports Medicine in its November/December issue of ACSM’s Health & Fitness Journal. Based on the annual survey of 2,000 clinicians, researchers and practitioners in the fitness industry, wearable technology was named the number one trend for 2025, followed by mobile exercise apps (#2) and exercise programs for older adults (#3).
“Digital technologies are becoming more critical to the way we design, deliver and evaluate health and fitness services,” said A’Naja Newsome, Ph.D., ACSM Certified Exercise Physiologist and co-author of 2025 ACSM Worldwide Fitness Trends: Future Directions of the Health and Fitness Industry.
“Wearable devices, mobile apps and data-driven training methods will create avenues for reaching new clientele and elevating fitness experiences. The exercise professional will need to be innovative in their approach to using technology while increasing client adherence and autonomy.”
Mobile exercise apps were next as the number two trend, continuing the focus on technology. One of the fastest risers on the trends list, mobile apps landed as the second biggest trend just two years after coming in at #20. In 2023, there were 850 million fitness app downloads by nearly 370 million
users. This popularity, along with complementing wearable technology, may have fueled the quick rise up the list.
Completing the Top 10 technology trifecta was data-driven training technology (#7), which made a significant jump from #18 in 2024 to the seventh spot in 2025. Benefits of datadriven training technology include better understanding of the physiological responses to an exercise stimulus in realtime, individualized coaching and instruction, even in a group setting where there may be various fitness levels, and the use of biofeedback (i.e., sleep, and heart rate variability) as critical components of training and recovery. Importantly, exercise professionals can use real-time data to tailor daily exercise sessions to account for acute and chronic conditions, which increases the safety of exercise for special populations.
“Clients desire instant feedback on their training so they can adjust or modify to maximize outcomes and reduce injury,” continued Newsome. “We are seeing this in individualized programming and in group-based classes.”
In addition to digital technology, two other trend categories formed in the Top 10: training modalities and fitness programming. exercise programs for older adults (#3), exercise for weight loss (#4) and exercise for mental health (#8) reflect strong trends toward programs designed for specific needs and populations.
Training modality trends were represented in the top 10 by traditional strength training (#5), high intensity interval training (#6) and functional fitness training (#9).
Of the top 10 trends, only health and wellness coaching (#10) was not included in the three dominant categories of digital technology, training modalities and targeted programs. •
Visit theicecommunity.com for the solution.
ACROSS
1 Technology that can reduce the radiation dose in CT scans and estimate radiation risks, goes with 10 across
8 Current measurement
10 See 1 across
11 Metric weights, abbr.
13 Auxiliary, for short
14 It can be measured on an EKG
17 Specialist dealing with the trachea, the pharynx and nasal cavities, abbr.
18 Road, for short
19 Place in water
20 St Louis arch state, abbr.
21 ___ morphology
22 Carry out
23 Unruly crowd
Quote of the Month:

24 Yttrium-90 agent used in radioimmunotherapy to treat non-Hodgkin’s lymphoma
26 Painter of limp watches
28 Aka 3D mammography
32 Good grades in exams
33 Materials such as barium and iodine
34 Where blood tests are done
2 Monoclonal antibody used in immunotherapy treatment of non-Hodgkin’s lymphoma
3 Down with the flu, e.g.
4 Copy
5 Like xenon and krypton
6 Didn’t have
7 Metal being used in contrast enhanced mammography
“Leadership is the capacity to translate vision into reality.”
– Warren Bennis
9 Very large
12 Narrowing of an opening or passageway in the body
14 Unit of frequency
15 Coast Guard rank, abbr.
16 It’s used to treat epilepsy
20 Grand ___ seizure
21 Broken arm mold
25 Nose related
27 Da Vinci’s Mona ____
28 What nurses are renowned for, abbr.
29 Medical survey demographic
30 Agreement word
31 24 in a day, abbr.
ImageOne

• $300 a month


• 1/6 page ad included in the marketplace

• Up to 5 categories in our ICEDEX
• Your company name, website and phone included in your ICEDEX listings

• Your company name in the alphabetical business index
• Appear in the print and digital magazine