








Through innovation we want to change the perspective in the imaging space.
We want to put the control back in the hands of the decision makers.



We understand our customers goals and we are developing a clear pathway to measurable savings.
855.401.4888
















































































DIRECTOR’S CUT
Six new CPT codes under “Magnetic Resonance Safety Implant/Foreign Body Procedures” went into effect January 1.
40
COVER STORY
Medical imaging devices are expensive to repair and require a great deal of precision to function appropriately. 14 44


RISING STAR
UT Southwestern University Hospital Operations Manager Kristi Schkade’s Hodgkin’s Lymphoma diagnosis sparked an interest in imaging.


Check out the latest imaging news including women’s imaging, awards and VR.
Technological advancements, such as improved image quality, reduced radiation exposure, and enhanced system mobility, are significantly contributing to the widespread use of C-arms.


Addressing the demand for skilled imaging service engineers requires a multifaceted strategy that balances recruitment, retention and internal development.
President
Vice
Kristin
Vice
Senior
Art
Digital
Cindy
Accounting




When her accounting career didn’t add up, Samantha Palensky examined the equation and found a solution.
Samantha Palensky, R.T. (R) (N), CNMT, MHA, radiology operations manager with Nebraska Medicine, explains that the decision to pursue a career in radiology resulted in more benefits than she ever imagined.
“I began my career with an initial focus on accounting, but after a few years of pursuing this field, I realized it was not the right path for me,” Palensky recalls. “Seeking a change, I transitioned into radiology, enrolling in the University of Nebraska Medical Center’s radiologic technology program in Omaha. At the time, I was unaware of the many opportunities this career could provide, but looking back, I am incredibly grateful for the direction it has taken me.”
After completing her training as a radiologic technologist, Palensky pursued a specialty in nuclear medicine technology.
“I spent 9 years working as a nuclear medicine technologist at Nebraska Medicine, during which I also earned a master’s degree in healthcare administration. This academic achievement sparked a desire for more, and I began exploring leadership roles that would allow me to leverage my healthcare background and administrative training,” she shares.
Nine years ago, she made the transition into management as a radiology operations manager, focusing specifically on CT and MRI.
“This role has allowed me to combine my clinical expertise with my passion for leadership, and I continue to be driven by the challenge of improving operations and enhancing patient care within the radiology department,” Palensky says.
When asked to describe her greatest accomplishment, Palensky has a two-part answer.
“My greatest accomplishment is earning my master’s degree and successfully growing my department’s volumes to meet increasing demands over the past eight years,” she says.
One aspect of an imaging career, especially in leadership, are the never-ending shifts.
“Imaging is constantly advancing and evolving, and staying at the forefront of these changes is a daily responsibility in healthcare,” Palensky says. “Keeping up with new technologies, workflows, and staffing models is always a top priority for me. During my time at Nebraska Medicine, I have benefited from the endless opportunities provided by working at an academic medical center, where we are continuously striving to advance imaging practices.”
When it comes to leadership, Palensky stresses the need to be open minded and understand that continuing education is a vital aspect of assisting others and helping the team achieve goals.
“I view leadership as an ongoing learning process. My role is to facilitate the support needed for my staff’s ideas and improvements, but ultimately, they are the ones who must implement and follow the policies,” she says. “I believe in listening first to understand their perspectives, then offering insights and asking questions to help drive progress within my departments and support the professional growth of my staff.”
“My staff members are amazing and our patients at Nebraska Medicine are genuinely thankful for their expertise, bedside manner and willingness to assist them along their healthcare journey,” she adds.
Her leadership approach is influenced by her mentors.
“My mentors are not imaging professionals but come from the nursing field. They provide me with valuable perspectives on healthcare and encourage me to adopt practices that align with those followed by nursing professionals. They also challenge me to push the envelope and think outside the box to find solutions,” Palensky says.
“Key lessons I’ve learned include the importance of standardizing processes to facilitate staff mobility across multiple locations, clarifying roles to improve understanding of how radiology impacts the organization, and how to effectively communicate to gain visibility with senior leadership,” she adds.
Switching from accounting to radiology has proven to be a wise decision for Palensky. It is a decision that continues to pay dividends.
“I love my job because of the variety of daily activities and challenges involved in running multi-location departments and managing people,” she says.
Away from work, Palensky shares that she has been happily married for 17 years. She has three children, including a 12-year-old son and two daughters ages 9 and 4. She also has a black lab. •

1. What is the last book you read? “The Mind Gym”
2. Favorite movie? “Step Brothers”
3. Who are your mentors? Marcy Saniuk, Michelle Freeman and Rebecca Duchman
4. What is one thing you do every morning to start your day? Exercise and meditate
5. Best advice you ever received? Don’t say no immediately, even if you know the answer is no. State that you will investigate it and then provide the answer, that way the other person feels as though you put the thought and effort into the question.
6. Who has had the biggest influence on your life? My family
7. What are your hobbies? Watching my kids pursue their passions in sports and life; watching movies
8. What is your perfect meal? Breakfast any time of day – eggs, potatoes, avocado and bacon with a salad

BY MATT SKOUFALOS
After you’ve visited 82 different countries in the world – and you’re counting down the next 100 you have yet to tour – it might be easy to feel like you’ve seen nearly everything there is to see. But for globetrotter Bryan Henderson, travel represents a lifelong pursuit upon which the sun has yet to set, no matter where on the planet he’s viewing it.
Growing up in a household with two working parents, Henderson and his siblings spent a lot of time with their retired grandparents. Henderson described his grandparents as “travelholics,” noting that his grandfather, Charles Ziel, had filled four passports with customs stamps, and was on his fifth at the time of his passing.
“He’d been to 100 countries, and my goal is to surpass that,” Henderson said.
Henderson had a good head start simply due to growing up in South Florida during the 1980s and 1990s. Cruises routinely departed from ports in Miami, Ft. Lauderdale and Cape Canaveral, and the Ziels taught him the trick of calling a week before the ship left to jump aboard at a reduced rate. This method would send them on three or four cruises a year, anywhere from a few days to a few weeks. Henderson was hooked.
“We loved it,” he said. “We had the best of times. You’ve got almost 30 different countries right in the Caribbean; by the time I got a driver license, I had been to all of them.”
Today, Henderson can say that he’s been to every country in Europe, all of South America except Guyana, and he’s heading back out to Asia next. He’s already seen Australia, China, Hong
Kong, Bali, and Japan, where the 6-feet-4-inches tall medical imaging director needed to kneel in the shower to wash his hair. Henderson had the opposite experience in the Czech Republic, where one of the things he appreciated was that “everyone was my height.”
In the Middle East, Henderson has been to Dubai, Abu Dhabi, Qatar, Jordan, Oman, Israel and Saudi Arabia. He’s been to Egypt, Morocco, and Tunisia in Africa and is planning to take his nephew on an African safari next year, after the teen graduates high school.
Crossing his seventh and final continent, Antarctica, off the list last year required complex preparations. The only two ways to visit the continent are with a research permit or on a cruise ship from South America. Sailing out of Chile through Glacier Alley in Patagonia was “absolutely beautiful,” Henderson said, as the vessel traveled on through Tierra Del Fuego in Argentina, and then south, crossing the turbulent Drake Passage.
The four stops in Antarctica didn’t make land – “There’s nothing really to see on land” he said – but they did offer a spectacular view of 30-feet tall ice cliffs, and an opportunity to navigate the intra-glacial channels on smaller boats.
“I’ve completed more than 400 scuba dives as a certified rescue diver and I had no idea that freezing water attracted so much wildlife,” Henderson said. “Orcas, whales, seals and five species of penguins; I’ve never seen so much wildlife in the ocean.”
A tour of Europe revealed the breadth of its history to Henderson. He was particularly fascinated by the old architecture and sites of antiquity in and around the Mediterranean and Baltic Seas.

“I thought that most of the Roman empire was solely in the country of Italy, and I hadn’t realized how much the remnants of their legacy were all over Europe,” he said. “We once chartered a yacht in the Adriatic Sea, and there was a massive Roman coliseum right on the coast of Pula, Croatia.”
On one cruise from Rome to Dubai, a 22-day jaunt through the Suez Canal and into the Red Sea, Henderson traveled through routes going into the Arabian Sea that the captain noted were frequented by Somali pirates. As he passed through the “high-risk area,” the cruise ship turned off all its lights so that it would appear to be a freighter, and passengers were told to lock their balcony doors. The cruise ship was escorted by an armed all-black companion boat, and moved through the passage without incident.
Henderson’s constant companion on these journeys is Anica, his wife of 20 years. Early in their courtship, each had disclosed that they weren’t really looking to become parents. When he asked, “What is your passion?” and she replied, “Traveling,” Henderson said, “This is going to work out great.”
“We had a list of the places that we had both already been to, which then left the entire rest of the world as something that we could explore together,” he said. “The most fun we have is sitting down and planning our next adventure.”

“It’s just going to make the entire world seem smaller,” he said. “It allows people to come together and communicate. I don’t think a language barrier should be a reason not to travel.”
Henderson’s top travel tip is to seek out local pubs or restaurants in which to spend time speaking with local people to learn about things that aren’t on tourist websites. Henderson always travels with a detailed itinerary, but is prepared to do anything off-the-cuff as opportunities present themselves.
“People are way friendlier than you’ll read about in the news,” he said. “They’re going to tell you things that aren’t known to tourists, and they are usually more than happy to inform you about the many wonders of their country.”
“I’ve been on the Autobahn where there’s no speed limit, I’ve been to jungles where there are no police, and I’ve been to beaches where there’s no clothing.”
The couple will spend Valentine’s Day 2025 in an over-water bungalow in the Maldives, and then some time in Dubai and Singapore as well. Henderson speaks English, Spanish, and German; and Anica, whose family is from France and Spain, speaks about seven languages. That’s useful for communicating across the globe, but new conversational mobile applications make it a lot easier for those who are less fluent in their nonnative tongues.

“As an American, we think we’re the freest country in the world, but we’re not,” Henderson said. “I’ve been on the Autobahn where there’s no speed limit, I’ve been to jungles where there are no police, and I’ve been to beaches where there’s no clothing.”
“In Japan, we stayed in a house that didn’t even have a lock in the front door because they don’t have crime in that area of Yokohama,” he said. “It boggles my mind how Americans think.”
With about 100 countries left to see on the planet, Henderson’s top remaining destinations include the Northern Lights in Iceland and scuba diving in the South Pacific. Along the way, he enjoys expanding his palate with new dishes and cultural flavors from different global cuisines.
“The two things you need to travel are money and time, and we never know how much we’re going to have at any given moment,” he said. “Your money will return, but your time won’t. Surprisingly enough, there’s a lot of beauty in other countries, and most of it is absolutely free.” •


UT Southwestern University Hospital Operations Manager Kristi Schkade, RT (R), (CT), (MR), says her interest in imaging began when she was diagnosed with Hodgkin’s Lymphoma.
ICE Magazine recently interviewed her to find out more about her journey and her goals for the future.
Q: WHERE DID YOU GROW UP?
A: I was born and raised in San Angelo, Texas, which is a vibrant city located in the heart of West Texas, known for its rich history and unique blend of culture. It is home to the Concho River, which flows through the city, offering scenic views and outdoor recreational opportunities. The city is also famous for its Fort Concho National Historic Landmark, a well-preserved military outpost that played a key role in the region’s frontier history.
Q: WHERE DID YOU RECEIVE YOUR IMAGING TRAINING/ EDUCATION?
A: I completed my education at the Howard College Radiologic Technology program in San Angelo, earning an associate of applied science degree. Shortly after graduating, I began my career at Shannon Medical Center in the X-ray department. Over the course of my eight
years there, I steadily advanced my skills and expertise, gaining experience in interventional radiology (IR), computed tomography (CT), and magnetic resonance imaging (MRI).
Q: HOW DID YOU FIRST DECIDE TO START WORKING IN IMAGING?
A: While completing my bachelor’s in business, I was diagnosed with Hodgkin’s Lymphoma. As a patient undergoing X-rays, CT, and PET CT scans, my interest in radiology was sparked. After finishing my bachelor’s degree, I began taking prerequisite classes for the radiologic technologist.
Q: WHAT IS THE MOST REWARDING ASPECT OF YOUR JOB?
A: The most rewarding part of my job is helping patients by providing a positive experience, lending a listening ear, or even just successfully placing their IV on the first try. I enjoy building connections with patients and empathizing with what they are going through. Additionally, I find fulfillment in improving my co-workers’ experiences, whether it’s by enhancing workflow processes or coaching and developing employees.
Q: WHAT DO YOU LIKE MOST ABOUT YOUR POSITION?
A: I appreciate the variety and dynamic nature of my position. Each day presents new challenges and opportunities, whether it’s coordinating staffing, optimizing workflows, or actively participating in CT and MRI scans. I value the collaborative environment, working closely with my colleagues to provide the best care possible. Being directly involved in patient care is incredibly fulfilling and allows me to make a tangible impact on patients’ health and well-being. I am drawn to the collaborative nature of the imaging field. In my current role, I work alongside technicians and other leaders in the organization to deliver comprehensive care to patients and that is something I find very appealing.
Q: WHAT INTERESTS YOU THE MOST ABOUT THE IMAGING FIELD?
A: First would be the constant advancements and technological innovations in the imaging field fascinate me. The rapid evolution of imaging techniques and equipment opens up new possibilities for diagnosis and treatment, making it an exciting area to work in. Secondly, I am passionate about patient care, and the imaging field plays a crucial role in diagnosing
and monitoring various medical conditions. The ability to provide accurate and timely imaging results directly impacts patient outcomes, which is incredibly rewarding.
Q: WHAT HAS BEEN YOUR GREATEST ACCOMPLISHMENT IN YOUR FIELD THUS FAR?
A: My greatest accomplishments thus far include working at the top-ranked hospital in the DFW area, where I advanced from a frontline employee to supervisor and then to manager within just three years. During this time, I successfully completed a clinical ladder program and led a process improvement project that resulted in significant changes, ultimately enhancing patient care and outcomes.
Q: WHAT GOALS DO YOU HAVE FOR YOURSELF IN THE NEXT 5 YEARS?
A: I want to continue my education and start pursuing a master’s in healthcare or business administration. I want to continue pouring into the employees to create a team of diversity, innovation, fostering a culture that embraces challenges, strives for excellence, and continuously seeks creative solutions to drive success.•
FAVORITE HOBBY: Traveling
FAVORITE SHOW: “Game of Thrones”
FAVORITE FOOD: Mexican cuisine, chips and salsa
FAVORITE VACATION SPOT: Beach vacation
1 THING ON YOUR BUCKET LIST: Take a trip to Greece and Italy

Ultrasound equipment failure can be catastrophic.

When your ultrasound equipment is down, so is your business. Don’t miss our Solutionist Series videos on Ultrasound Equipment Support where you’ll learn how to service your equipment, keep your business up and running and lower your total cost of ownership.
In this 10-episode virtual training course on the Philips Epiq ultrasound platform, Larry Nguyen, Summit Imaging’s Founder and CIO, identifies common failures and provides solutions for:
• Image quality — 2D grayscale, color, continuous wave or pulsed wave
• Power subsystem — power module and power regulator board
• External interfaces — control panel, touch panel, trackball, monitor and external IO
• Transducer types and applications — Doppler, linear, curved, endo-cavity and more.
• Transducer parts — a breakdown of standard and TEE
• Transducer parts and operational failures — from lens failure to cut or creased cords to CW noise and error codes

Larry Nguyen addresses lots more in our 10-episode Solutionist Series, so be sure to tune in.




FUJIFILM Healthcare Americas Corporation, a leading provider of diagnostic and enterprise imaging solutions, has announced that its ASPIRE Cristalle Acquisition Workflow System (AWS), the workstation that is used in conjunction with the company’s 3D mammography system, has been granted a Risk Management Framework (RMF) and Authority to Operate (ATO) on U.S. Department of Defense (DoD) networks.
The three-year ATO was awarded to Fujifilm for its ASPIRE Cristalle AWS version 9.x. The ASPIRE Cristalle AWS controls the exposure unit to acquire and process mammographic images. With this user-friendly, secure workstation, the operator can acquire and view the patient’s image(s) in as few as five seconds. With ASPIRE Cristalle AWS, organizations within the DoD network will be able to securely acquire and access patients’ mammography images.
The DoD’s RMF provides a process that integrates security and risk management activities into the system development life cycle. The risk-based approach to security control selection and specification considers effectiveness, efficiency, and constraints due to applicable laws, directives, executive orders, policies, standards, and regulations.
“This prestigious designation from the U.S. government attests to Fujifilm’s commitment to delivering advanced solutions in women’s health that meet the most rigorous security standards,” says Henry Izawa, president and chief executive officer, FUJIFILM Healthcare America Corporation. “We are honored to have earned the ATO for our ASPIRE Cristalle AWS-technology which will optimize the end user’s workflow and will ultimately benefit physicians and patients throughout the Military Health System.”
If your heart rate increases each time you hear the word “injection,” you’re not alone. Every 1 in 4 adults has a fear of needles — a fear that most attribute to an experience they had when they were children.
For kids who visit the hospital frequently, anxiety around even routine procedures might interfere with each visit and even lead to long-term trauma.
Children’s Hospital Los Angeles’ Interventional Radiology team – one of the most universally visited specialties at the hospital – is working to minimize negative medical experiences using virtual reality (VR) technology. In August, they hired Phoenix Hunt, CHLA’s first embedded hospital VR technologist, to guide and support patients through their procedures using specially designed, procedure-specific VR games.
“In most health care contexts, VR has been used to support patients as a relaxation tool,” explains Joseph Miller, MD, MS, director of interventional radiology.
“We’re applying these same types of technologies to pediatrics in a novel way to minimize anxiety, pain, and discomfort and even reduce anesthesia use.”
helps detach their anxieties from what they’re feeling and experiencing in the real world.”
This phenomenon has been studied extensively by CHLA’s Biobehavioral Pain Lab, led by Jeffrey Gold, Ph.D., whose research seeks to enhance the standard of care for anxious patients beyond administering medication to ease fear.
“VR can help dampen the brain’s pain receptors,” Hunt says. “Your body is so distracted with other stimuli that it kind of forgets to feel that anxiety or pain that you’d be noticing previously.”
“What we were missing was not so much the technology itself,” says Miller, reflecting on the early days of conceiving the program. “It was the person to help apply the technology in an individualized fashion.”

Most interventional radiology procedures only take a few minutes, but the prep time and setup are much more complex.
“A patient who just needs something to ease the anxiety and discomfort of the procedure ends up having to go without eating all night so we can administer anesthesia in the morning,” explains Miller.
As the medications leave the patient’s system, it can take several hours to fully recover. “That’s a lot logistically for the patient – and for their family and care team – for what is ultimately a five-minute procedure,” he adds. “Our goal is to reduce that footprint for everybody.”
“When you put a headset on somebody in a health care setting, it can transform their mind and immerse them in a completely different environment,” explains Hunt. “It
That’s where Hunt came in.
Hunt studied virtual-reality game design at Savannah College of Art and Design and was drawn to VR applications in health care. “I was perfectly good at designing video games, but I realized I wanted to work in the clinical setting as soon as I started connecting with patients,” he explains.
“The more positive
experiences I helped foster, the more I thought, ‘This is what I want to do for the rest of my life.’”
As Miller and the team finalized their vision for the VR technologist position, it became clear that CHLA would effectively create the blueprint for future U.S. hospitals. “We’ve yet to encounter another hospital using VR to get patients through procedures with an embedded VR technologist,” Miller says.
The role is made possible by the financial support of the nonprofit Child’s Play, which assists hospitals across the country in a variety of technology adoption initiatives.
It just so happened that the job posting coincided perfectly with Hunt’s post-grad career search. He joined the team in August, and they treated their first patient using VR a month later. •
Koning Health commends RadSite’s recent announcement to include a dedicated breast specialty in its Cone Beam CT (CBCT) Imaging Standards. This progressive step underscores the critical need for high-quality imaging standards in the diagnosis and management of breast cancer, an area where innovation and precision are paramount.
As the manufacturer of the FDA-approved Vera Scan, the world’s first and only commercially available 3D breast imaging device using CBCT technology, Koning Health has been at the forefront of advancing breast cancer detection. The Vera Scan offers unmatched clarity, patient comfort, and the elimination of painful breast compression, setting a new benchmark in breast imaging.
RadSite’s decision to establish robust imaging standards for breast applications in CBCT aligns with Koning’s commitment to transforming breast cancer screening and diagnostic protocols.
“Koning Health strongly supports the efforts of RadSite to raise the bar in imaging standards,” said David Georges, president of Koning US. “Establishing a dedicated breast specialty for Cone Beam CT imaging not only recognizes the unique capabilities of this technology but also ensures that patients receive the highest level of care and accuracy in breast cancer diagnostics.”
RadSite’s expanded standards mark a significant step for facilities utilizing CBCT technology for breast imaging, offering an opportunity to pursue accreditation through RadSite’s comprehensive medical CBCT accreditation programs, approved by CMS. These programs ensure that
imaging providers adhere to rigorous clinical performance and safety standards, while also meeting private payer requirements. RadSite’s accreditation has become a hallmark of excellence in imaging quality and care, with many large outpatient imaging providers transitioning to its programs.
While RadSite’s CBCT Imaging Standards provide a robust framework for quality assurance, imaging providers must also adhere to any state-specific regulations, which may in some cases be more stringent. Nevertheless, RadSite’s leadership in creating these specialty-specific standards is a critical advancement in ensuring consistent and high-quality imaging across the healthcare landscape.
The addition of breast-specific standards to RadSite’s CBCT Imaging Standards is a vital step toward fostering broader adoption of innovative imaging solutions like the Vera Scan. These standards provide a framework for ensuring consistent, highquality imaging while promoting patient safety and clinical efficacy.
The Joint Commission and Kaiser Permanente have announced Zuckerberg San Francisco General Hospital and Trauma Center (ZSFG) as the recipient of the 2024 Bernard J. Tyson National Award for Excellence in Pursuit of Healthcare Equity. This prestigious award, established in honor of late Kaiser Permanente Chairman and CEO Bernard J. Tyson, honors a healthcare organization for its efforts that achieved a measurable, sustained reduction in one or more healthcare disparities.
The award recognizes ZSFG, a safety net hospital and San Francisco’s only Level 1 trauma center, for its achievements under the initiative Reducing Racial
Disparities for African American Patients with Heart Failure. The improvement team’s efforts significantly improved care for all patients with heart failure at ZSFG.
Clinicians at ZSFG identified heart failure as a leading cause of hospitalization for Black/African American patients. Additionally, many heart failure patients who were readmitted also had co-occurring substance use disorders.
The Tyson Award selection panel commends ZSFG’s work, affirming its approach to addressing broad, systemlevel structural changes, educating staff and reducing silos among specialists.

A recent study by the Harvey L. Neiman Health Policy Institute demonstrates that mobile mammography is generally used by women otherwise unlikely to be screened, and thus is complementary to facility-based mammography rather than a substitute for it. Hence, mobile mammography could feasibly increase breast cancer screening rates, especially in traditionally underserved communities. This study, published in Clinical Breast Cancer, was based on 2.6 million women with Medicare fee-for-service insurance during the 2004-2021 period.
Breast cancer is the second leading cause of cancer deaths among women in the United States, making early detection an important step in reducing preventable morbidity and mortality. However, women can face significant hurdles when trying to access facilities that offer mammograms.
“Women of color in rural and underserved communities face substantial barriers to accessing breast cancer screening services. Mobile mammography is an innovative and practical solution to address this disparity in cancer care and deliver life-saving screenings and early detection to ensure these women get the critical care they need,” explained Dr. Bhavika Patel, professor of radiology, chair of research and clinical breast radiologist at the Mayo Clinic Arizona. “In fact, our past work examining trends in screening adherence among indigenous women in the western U.S. showed that rurality and community income play a significant role in declining rates of mammography utilization. We wanted to understand how mobile mammography might offer a way to increase screening rates among those who may not otherwise get breast cancer screening.”
The researchers found that less than half (49.5%) of the women in the study had a mammogram at some point during the 17-year study period. Among those with
a mammogram, only 0.4% utilized mobile mammography. This group tended to be younger and non-white, with fewer comorbidities, living in rural and lower income communities. Heat maps of beneficiary density for mobile and facility-based mammography usage demonstrated the complementary nature of mobile mammography; mobile mammography usage covered rural areas where facilitybased mammography did not.
“After controlling for various patient factors, we found that American Indian or Alaska Native women were 453% more likely to have mobile mammography than white women. Likewise, women in rural areas or in communities with below average incomes were 210% and 41% more likely to have mobile mammography than urban women or those in above-average-income communities, respectively.” said Dr. Eric Christensen, research director at the Neiman Institute. “Indigenous women also had the lowest rate of screening mammography usage among minority racial and ethnic groups. Hence, our findings suggest that mobile mammography may be particularly helpful in increasing breast cancer screening among these women and other underserved groups.”
“Our results show that mobile mammography is not cannibalizing facility-based mammography; it provides additive access to breast cancer screening. What’s more, it reaches women who might not otherwise get screened, and thus presents a complementary approach to facility-based mammography that may reduce access disparities and increase early detection of breast cancer,” said Casey Pelzl, senior economic and health services analyst at HPI and lead researcher on the study. “The low breast cancer screening rate among Medicare beneficiaries, and especially among those women residing in rural and impoverished areas, should catalyze efforts to promote screening access and adherence, particular for the traditionally underserved.”
Unlock your engineering team’s full potential with our in-depth, hands-on training courses at our state-of-the-art Center of Technical Excellence facility in


C-Arm Hologic & Orthoscan Family
OEC 9800/6800/9900
OEC Elite CFD inclusive Miniview Elite
Arcadis -Avantic/Orbic/Varic
Basic Principles of MRI Imaging
GE Excite Product Family
GE Innova x100
GE Innova IGS/Discovery
Siemens Axiom Artis
Siemens Artis Zee Cath Lab
Basic Principles of CT
GE CT 5X-7X, Brightspeed and Optima/Rev-EVO
Siemens Emotion 6/16 - Perspective CT
Siemens Sensation 10/16/40/64
Siemens Definition AS
Siemens Go Series CT
GE Definium, Optima, Discovery X-Ray
GE Precision 500D
GE Proteus
Siemens Multix Fusion
Siemens Ysio
Siemens Luminos Agile Max
Basic Ultrasound/PM
GE Logiq 9/Vivid 7 UL
GE Logiq E9/Vivid E9 UL
GE Logiq-Voluson Midrange Training (P7/P9/S8/E8/F6/F8
Voluson S6/S8/P8/S10/P6)
VIRTUAL - GE Logiq P3, P5, P6, A5
VIRTUAL -GE Laptops with Venue 40/50
GE Vivid E80/E90/E95 & Logiq E10
GE Vivid Midrange Training (S60/S70/S5/S6/T9/T8)
GE Voluson E6/E8/ E10
Siemens S1000-S3000 SC2000/ Antares UL
Siemens Sequoia II UL (New Version)
Siemens Mid-Range UL (X700,X300, X150, NX3, G40)
Sonosite Family (VIRTUAL)
Samsung Family
Toshiba Aplio - Xario (Aplio 300-400/i600-900/Xario 100200/A450-A550)

Wh
ile PartsSource was founded as an ecommerce parts provider in 2001, its true mission began in 2014 when Phil Settimi, MSE, MD, joined as president and CEO. His time spent with customers revealed the extreme inefficiencies plaguing biomedical and imaging technicians. He found technicians were spending many hours searching for replacement parts and waiting weeks for purchase approvals while procedural rooms sat offline, and critical assets were clinically unavailable. The industry was suffering from supplier stock-outs, logistical failures, high dead-on-arrival rates, and poor master data management.
“These problems were causing dramatic financial and operational impacts for our customers,” PartsSource Inc. Vice President and General Manager-Imaging Francis Vonder Haar said. “This deep customer insight resulted in the creation of a new software solution dedicated to the needs of clinical engineering teams. This software is purpose-built for the specialized workflow and procurement needs of the medical device supply chain, ensuring that customers have access to the highest-quality, lowest-cost, and most reliable supply options. With the launch of PartsSource PRO®, we became a trusted partner to Healthcare Technology Management (HTM) leaders and teams across the country.”
“In recent years, PartsSource has worked to understand the unique needs of the imaging industry and has improved our systems to best serve those priorities,” he added. “The needs are best summed up as ready-to-ship-inventory, speed, and knowledge. PartsSource has built a reliable, in-stock supply of key imaging parts, ensuring availability precisely when they are needed. Our PRO Imaging team provides a rapid, high touch, seamless approach, allowing parts to be quickly deployed to customers, meeting the speed needed to keep mission-critical imaging assets online. With the addition of the Radiological Service Training Institute (RSTI), PartsSource helps improve the quality of diagnostic imaging services required to keep clients current on the latest technology and best practices in the imaging industry.”
Today, over 1,600 hospitals across the United States rely on PartsSource PRO to continuously improve quality, costs and productivity within clinical engineering and supply chain teams.

Vonder Haar recently shared more details about the company with ICE Magazine.
Q: WHAT ARE SOME ADVANTAGES THAT YOUR COMPANY
Vonder Haar: PartsSource was the first to market with our clinical resource management platform for healthcare, PartsSource PRO. In addition to this enterprise solution, PartsSource offers unique differentiators including our Evidence-Based PRECISION Procurement® Engine, Formulary Management for Enterprise Preferences, Peer-Based Benchmarks & Analytics, and Community-Based Purchasing Power.
PartsSource is committed to being the preferred partner for every imaging professional, offering a single-source solution for all your imaging equipment repair needs. Whether you are looking for CT, PET/CT, MR, cath/angio, mammography, ultrasound, nuclear medicine, or X-ray parts, glass, accessories, or supplies, PartsSource has you covered. Our robust platform maximizes patient throughput with instant access to over 300,000 imaging parts via an easy-to-use online ordering portal. We stock over 60,000 imaging parts, all ready for immediate shipment. We provide OEM original and non-new part repair and replacement solutions and proudly carry imaging parts from all major OEMs, including Siemens, Philips, and GE. With the most comprehensive catalog in the industry, our online marketplace is a one-stop shop for your imaging needs. PartsSource allows you to buy with confidence, save money, and earn rewards. New for 2025, PartsSource is also enhancing our imaging solutions by including RSTI training with every parts purchase as part of our 2025 Imaging Rewards Program.
Q: WHAT ARE SOME CHALLENGES THAT YOUR COMPANY FACED LAST YEAR?
Vonder Haar: In 2024, the industry faced a considerable number of challenges, including cost pressure, aging equipment, staffing shortages, high cost of downtime, and increasing regulatory compliance. PartsSource has worked hard to help clients overcome these obstacles, responding with instant quoting of in-stock inventory and real-time visibility on 60,000 SKUs, market best parts pricing on aftermarket imaging parts, extended
warranties on select parts, tailored forward-stocking options aligned to your assets/region, proactive stocking of strategic parts tailored to asset list, the nation’s largest pool of in-stock OEM new imaging replacement parts, and access to 300+ imaging OEMs and aftermarket suppliers to better ensure that imaging providers have the solutions needed to keep their mission-critical equipment operational.
Q: CAN YOU EXPLAIN THE COMPANY’S CORE COMPETENCIES AND UNIQUE SELLING POINTS?
Vonder Haar: PartsSource delivers a rapid, personalized parts ordering experience. We understand the importance of confidently meeting your replacement part needs. That is why we have invested in an entirely new approach designed to deliver unmatched speed, value, and assurance every time you turn to PartsSource for a replacement part.
PartsSource is also uniquely capable of assisting our clients with knowledge and training. The Radiological Service Training Institute (RSTI) provides end-to-end solutions including training, parts, service support, and technical support. Together, we are expanding the selection of training courses and investing in the latest technology to provide students with unparalleled hands-on learning opportunities.
Q: WHAT PRODUCT OR SERVICE THAT YOUR COMPANY OFFERS ARE YOU MOST EXCITED ABOUT RIGHT NOW?
Vonder Haar: We are very excited to offer strategic stocking of critical imaging parts, particularly high-end imaging glassware, including CT and cath/angio tubes, and flat panel detectors. Because these parts are mission-critical, PartsSource is able to strengthen supply chain reliability and resiliency for our customers. In 2025, we ensure that these parts can be delivered quickly to improve uptime for our clients.
Q: WHAT IS ON THE HORIZON FOR YOUR COMPANY?
Vonder Haar: PartsSource will continue to deliver on our commitment to being the preferred partner to every healthcare provider by consistently innovating proactive solutions that optimize medical equipment uptime, streamline procurement, and improve patient care. This includes increased investments in broader and deeper stock of parts for solving urgent needs in the industry. We are also working to solve the ongoing imaging labor problems, including a SkillBridge and apprentice training program through RSTI. PartsSource, with a network of over 5,000 service engineers, now offers a comprehensive solution for your imaging service needs, including contract and time-and-material support. We have made recent investments in technology and stock levels that allow us to forward deploy mission-critical imaging parts at a customer’s location in branded PartsSource lockers. These lockers will be stocked with parts that have been deemed mission-critical to each operation and can be accessed quickly and conveniently when failures occur, ensuring that key assets remain operational.
Q: CAN YOU SHARE SUCCESS STORY?
Vonder Haar: Earlier this year, a hospital reached out to us in crisis when a hard-down CT system had forced their hospital to go
on divert. Their situation was urgent: the CT tube had failed, and they needed a replacement immediately. In less than 14 hours, we identified the failed tube, located the correct replacement, delivered it to the site, and installed it. The hospital was taken off divert and back to providing lifesaving care. We are incredibly proud that PartsSource played a critical role in diagnosing and resolving the issue so quickly.
Q: WHAT ARE SOME RECENT CHANGES TO THE COMPANY?
Vonder Haar: At RSTI, we have worked hard to improve and increase our training options, with multiple new courses available in 2025. These new courses include Philips Azurion 8.2 Cath Lab with Flexvision, GE IGS (Cath Lab with LDM Large Monitor), Siemens Definition CT, Philips Ingenuity 128 CT, GE Pristina (3D Tomo Mammography), Philips Veradius C-Arm, OEC Elite Mini, and Hologic Horizon Bone Densitometry.
Q: CAN YOU TELL ME ABOUT THE PARTSSOURCE EMPLOYEES?
Vonder Haar: PartsSource employees are driven by a strong sense of purpose, focused on ensuring healthcare is always available to patients, which motivates them to work collaboratively and innovate to solve complex customer challenges within the healthcare industry. Our dedicated PRO Imaging team averages over 20 years of imaging experience per specialist. RSTI, celebrating its 40th anniversary, has cultivated a specialized and highly experienced team, with our dedicated personnel and expert instructors setting the standard for excellence in the industry. We continue to invest in the next generation of imaging leaders as the company grows.
Q: WHAT IS PARTSSOURCE’S MISSION STATEMENT?
Vonder Haar: The PartsSource purpose is raising the quality, availability, and affordability of healthcare, ensuring healthcare is always on for patients. PartsSource was founded on the idea that an evidence-based, data-driven approach to the healthcare supply chain can unlock better delivery, lower costs, and enhance clinical outcomes. This is especially true for diagnostic imaging equipment, where clinicians rely on this vital equipment to perform their mission-critical work. Driven by this purpose, PartsSource is rapidly expanding our diagnostic imaging solution set to better support healthcare professionals and enhance patient care.
Q: IS THERE ANYTHING ELSE YOU WANT READERS TO KNOW ABOUT PARTSSOURCE?
Vonder Haar: It is important for people to know that, though PartsSource has been around for over 23 years, we are rapidly improving and evolving, especially when it comes to addressing the needs of the imaging industry. We have been hard at work adding technical support to our solutions, and our imaging team is specialized and growing, with a renewed focus. We are committed to solving problems in partnership with all medical imaging professionals and we look forward to working with you this year and into the future. •
For more information visit www.partssource.com.
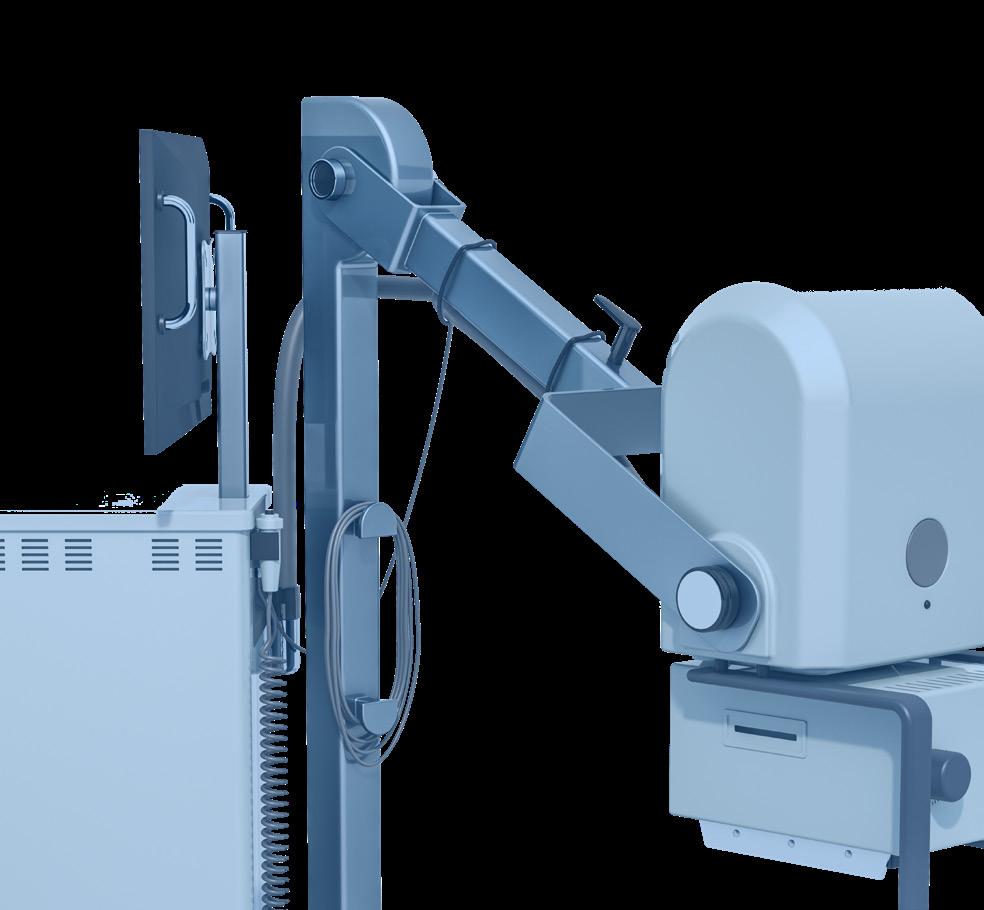
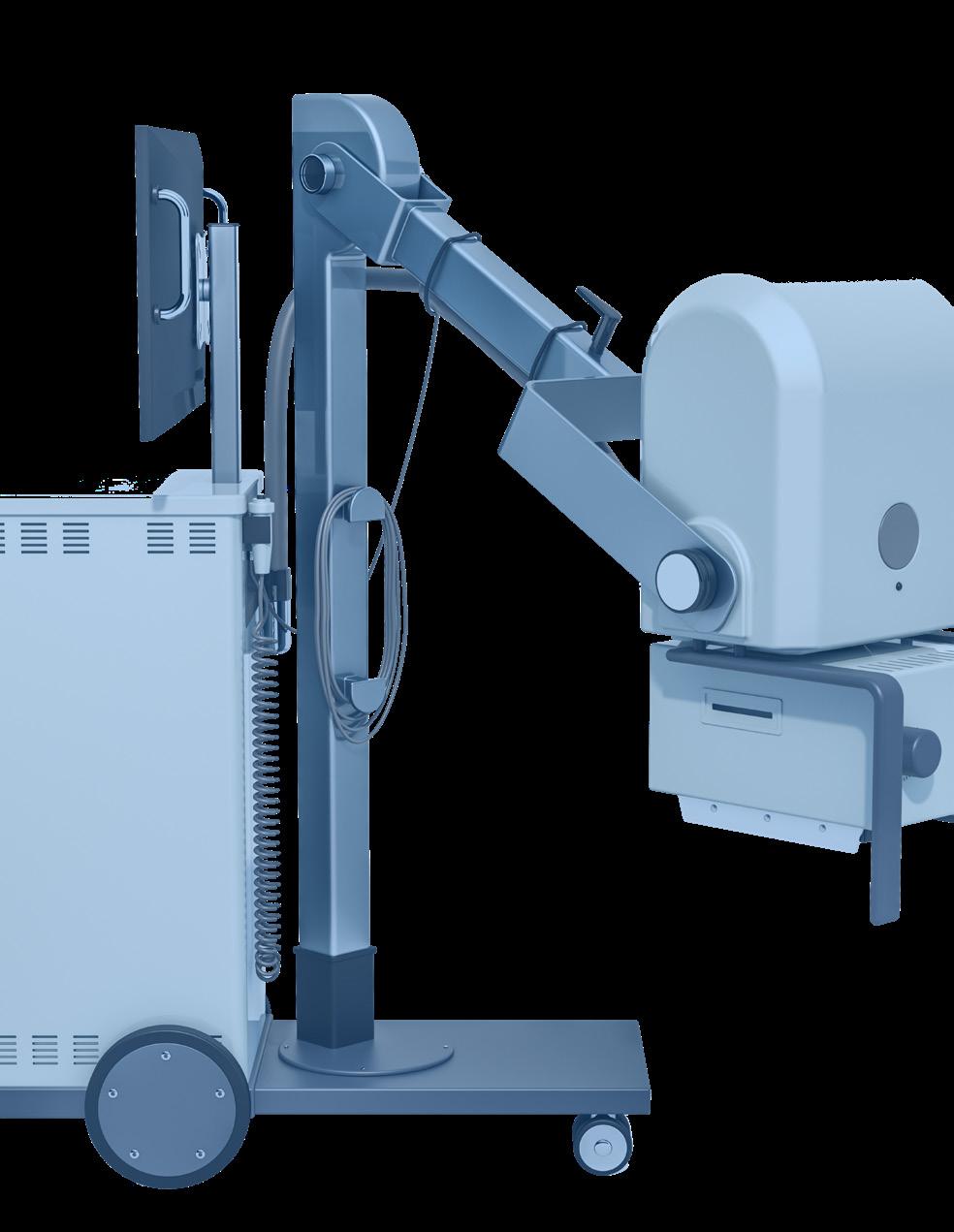
C-arm imaging is a medical imaging technique that uses X-rays to produce real-time images of an individual’s internal structures. C-arms are used in a variety of procedures, including orthopedic procedures, cardiac and angiography studies, therapeutic studies, pain management, emergency procedures, urology and gastroenterology.
ICE Magazine Editor John Wallace reached out to several healthcare systems seeking input from subject matter experts on C-arms for this Director’s Circle article. Participants are:
• Ashley Adams, MHI, BSRT(R)(VI), perioperative and procedural imaging manager, The Ohio State Wexner Medical Center
• Tosca Bridges, M.S., R.T.(R)(CT)(QM), director radiology clinical operations adult services (interim), The University of California San Francisco
• Jill Jones, associate director of medical imaging, Banner Imaging outpatient clinics in Arizona
• Edward Richards, radiology supervisor for surgery, University Hospitals of Cleveland.
Q: WHAT KEY FACTORS INFLUENCED YOUR DECISION TO SELECT YOUR CURRENT C-ARM MODELS?
Adams: We take an approach that ensures we have a balance of performance, usability and ongoing support by focusing on three key factors.
• Image Quality and Functionality: Ensuring the equipment delivers high-resolution images and meets the functional requirements for a wide range of procedures is a top priority.
• Ease of Use: It’s essential that the equipment is userfriendly, allowing radiology technologists to operate it efficiently and confidently.
• Service Agreement and Training: A comprehensive service agreement is critical to addressing any equipment issues promptly. Additionally, the training provided by the vendor as part of the purchase is a significant factor, as it ensures the team is well-prepared to use the equipment effectively.
Bridges: There are several key factors that influenced UCSF Medical Center’s decision to select the GE OEC Elite CFD model as our standardized fleet imaging instrument. The quality of imaging was the most important consideration in selecting the GE OEC CFD. The mobile viewing station for the GE consisted of a monitor-viewstation (MVS) equipped with a 4K (3840 X 2160) or 8,294,400-pixel resolution monitor. With a dynamic large FOV CMOS field detector (31x31 cm or 21x21 cm), the 1548 x 1524 pixels is able produce the highest quality images for trauma orthopedics, neuro spine, urology, and vascular imaging, just to name a few services.
A second consideration was the large arc depth of the “C” (33-inch depth) on the C-arm which allowed for uninhibited RAO/LAO or CRA/CAU movements to image the patient anatomy. The arc depth was a strong consideration also because many cases use arm boards for radial/brachial IV access or the arms are placed in “superman” pose as to not superimpose the arms in the field-of-view. Having the large arc depth allowed for unfettered angulation of the C-arm on larger habitus patients, patients with difficult anatomy or pathology, or suites with room constraints on the anesthesia cart placement.
A third consideration was the X-ray tube configuration of the GE system versus the other three vendors. The GE OEC CFD has a split-block configuration where the


generator is housed in the “C” separated by a highvoltage cable. A mono-block configuration houses the key components (X-ray tube anode, generator, and cable) in one tube housing. The difference is a split block has a smaller footprint, greater flexibility and ROM for positioning, and dissipates heat faster with active cooling. The Siemens Cios Alpha C-Arm does a splitblock configuration like the GE OEC CFD, however, the system footprint and IQ played a determining factor in our decision.
A fourth consideration, that may get overlooked in many purchasing decisions, is service for work orders and repair. At UCSF, we have purchased Philips, Ziehm, Siemens, and GE C-arms in the past five years and have had a chance to observe service call response and repair turnaround times. In our observation, we noticed better service and parts availability for repairs with GE C-arm systems compared to its competition. This can be due to more available local field-service-engineers or a parts depot in closer proximity. However, this consideration did play a significant role in our decision-making process on which vendor was the correct choice in an effort to standardize our fleet enterprise-wide.
A fifth consideration was the unit cost of each system and preferred discounts the vendor would provide to our large institution for a bulk purchase. UCSF did include other UC sites in our decision-making process, including UC Davis. This transparency and inclusion helped other sites decide on which product was also best for them and negotiate bulk purchases across the UC enterprise.
A sixth consideration was patient radiation dose and while this was hard to assess we did notice this was directly related to imaging quality (IQ) and available algorithms. GE had many options on its touch-userinterface that allowed us to reduce dose while maintaining IQ. This was more present during the actual on-site demos which allowed us to get feedback from surgeons in realtime on what was acceptable vs. ideal.
Jones: Currently we have several GE C-arms. We purchased these due to the familiarity of the technologist

UNIVERSITY HOSPITALS OF CLEVELAND

BANNER IMAGING OUTPATIENT CLINICS
with the equipment as most had worked on these types of units in the past. We did just recently purchase a Siemens C-arm. We purchased this due to the size of the unit for a more compact area as well as using several other Siemens products.
Richards: We went with GE OEC because they are very dependable and tech friendly. The C-arms we replaced were anywhere from 15 to 20 years old.
Adams: One of the primary challenges during the procurement process was coordinating the equipment delivery timeline to align with the approvals required from clinical engineering and radiation physics, ensuring a smooth and efficient implementation.
Bridges: During the procurement process we faced a host of challenges as we conducted an open-source vendor fair during COVID pandemic in 2020. During this timeframe, many projects at UCSF Medical Center were either delayed due to budgetary constraints or discontinued due to pandemic-related limitations. We formed a UCSF C-Arm Purchasing Committee in the summer of 2020 to include key stakeholders for their input and assessment of the vendors. Key stakeholders included radiology technologists, radiology leaders from multiple UCSF sites, surgeons from different disciplines, clinical technologies imaging (biomed), and our UCSF procurement team. Forming this team was time-consuming as much coordination was needed to include parties from different shifts and various UCSF medical sites. Upon formation of this committee, we had to dedicate time, in-between patient care and multiple other projects, to conduct research on each vendor to present a transparent comparison at each vendors product. We hosted four vendors (GE, Philips, Ziehm, and Siemens) in a virtual vendor fair (Aug./Sept. 2020) which required a presentation of product information to
all our stakeholders via zoom. Due to the pandemic, we could not host each vendor for on-site demos which may have limited our assessment of the capabilities of each C-arm. However, the UCSF C-Arm Purchasing Committee compiled a C-arm specification fact sheet and a vendor comparison PowerPoint for all stakeholders, pre-vendor virtual presentations, to make the process as transparent as possible. Post vendor presentations, we utilized Survey Monkey for an anonymous vote by our stakeholders to select two vendors for on-site demos. Upon that selection, we hosted two vendors in Oct./Nov. 2020, dedicating one week each, within our Parnassus OR. After the demos, we selected one vendor in Dec. 2020 to move forward as our standardized C-arm fleet vendor. This was a time-consuming process requiring coordination with our vendors, stakeholders, procurement team, and periop team. We utilized the demo to validate claims made by the vendors and to assess each system in a multitude of cases with different services.
Jones: We did not face any major issues during our procurement process. We went through the standard purchasing process to obtain PO and funds and then purchase our units.
Richards: There are many different challenges because we replaced all our C-arms, 14 in all within a two-month period. This ranged from getting approval from upper management, figuring out the different models that we needed, to coordinating delivery of three or four C-arms every couple of weeks.
Q: WHAT STRATEGIES HAVE YOU IMPLEMENTED TO MAXIMIZE C-ARM UTILIZATION?
Adams: To maximize C-arm utilization, we have implemented a targeted staffing model designed to align with the specific environments in which the C-arms are utilized. We also focus on resource stewardship by ensuring active utilization of equipment and systematically replacing underused units to enhance operational efficiency and optimize resource allocation.
Bridges: To maximize C-arm utilization within our OR we have set up several workflows. First, we work with our periop equipment utilization team to ensure that correct amount and type of C-arm is available for booking. We currently have 13 C-arms in our Parnassus OR which gives surgeons the ability to book their cases in the OR without fear of not having an instrument for imaging. Although our C-arms are the same model, we purchased different configurations to help best serve several different services. Our C-arm fleet consists of a motorized GE OEC CFD vascular C-arm, GE OEC CFD super “C” 21 cm flat detector, GE OEC CFD super “C” 31 cm flat detector, Philips Veradius Unity, and Ziehm 3D RFD Vision. Second,
we work with our periop charge nurses, POD managers, and periop triad to communicate any down equipment with approximate repair turnaround times. This helps utilize other C-arms, move start times for cases to ensure imaging instruments are available, or find alternatives in imaging to ensure cases can be performed. Our current fleet of C-arms is predominantly GE; however, we still utilize Philips Veradius Unity and Ziehm 3D RFD models within our fleet for specialized spine cases, urology, and/ or bronchoscopy navigation cases. Third, we work with other radiology modalities to help perform cases that require multiple forms of imaging. An example would be in CT where we perform Kyphoplasty cases that require the CT scanner and a mobile C-arm. Utilizing our C-arms for these procedures ensures we maximize utilization of our instruments and best serve our patients.
Jones: To maximize our C-arm use at our facilities, we must work closely with the radiologist and radiologist assistant to cover all of our facilities that offer C-arm procedures. On the days that we schedule procedures, we maximize the use of the physicians and assistants to get as many done as possible in our workday.
Richards: Every morning, we look at the schedule for that day to determine which cases will need the larger unit. Like, for instance, if we have a pelvic osteotomy, humerus rodding or other complicated case they will get the large C-arm and the smaller ones will be for simpler cases.
Q: ARE THERE ANY UPCOMING TRENDS IN C-ARM TECHNOLOGY THAT EXCITE YOU?
Adams: The advancements in 3D C-arm technology are really exciting, especially when you think about how they can be applied across different surgical specialties. The ability to provide real-time, high-resolution 3D imaging makes a huge difference in improving precision and outcomes for a variety of complex procedures.
Bridges: C-arm technology or trends that are potentially exciting include the improvement of 3D C-arm systems that allow for 3D spine and multiplanar reconstructions. UCSF Medical Center is a research facility and a teaching hospital; therefore, we perform many different types of cases utilizing navigation platforms (spine navigation using Brain Lab or Medtronic Stealth, and Bronchoscopy Ion). When using navigation platforms for precise instrumentation placement and/or revisions, the imaging software required to confirm placement of screws or needles is very important. The imaging technology of 3D systems allows us to image anatomy and hardware in multiple planes with low dose. This helps in the accuracy of hardware placement and increases patient care outcomes. Although 3D C-arm technology is still in its infancy regarding software and integration, the
technology could prove to help create better workflows at a lower cost than traditional imaging methods such as the Medtronic O-Arm.
Jones: Some upcoming trends in C-Arm technology are:
• Better imaging: Manufacturers are developing flat-panel detectors with higher resolution and contrast for clearer X-ray images.
• AI and machine learning: These technologies can help with image processing, reduce noise, and identify anatomical structures.
• Robotics: Robotic arms can help position C-arms more precisely, which can improve workflow and reduce strain on operators.
• More compact and maneuverable mobile C-arms: These C-arms can be used in tight spaces or during complex procedures.
• 3D imaging: This can improve procedure planning, intraoperative guidance, and reduce procedure time.
• Advanced software: Modern systems include software to assist with image processing and data management.
• Intuitive user interfaces: These interfaces can improve workflow efficiency and ease of use.
Richards: Last year, we also demoed a GE 3D C-arm for some ortho cases and it was amazing how clear the images had come out and the surgeons were very happy with the quality of the images too. I think this will be the trend of the future.
Q: WHAT ARE THE BIGGEST CHALLENGES YOU FACE REGARDING C-ARMS IN YOUR FACILITY?
Adams: One of the biggest challenges we face is the limited storage capacity for C-arm equipment, as well as securing dedicated space for performing routine preventive maintenance.
Bridges: The biggest challenges UCSF Medical Center faces regarding our C-arms is multifaceted and at times out of our control. First, like any large teaching/research facility, we face challenges of productivity and availability. For us to be productive as an institution our instruments need to be available for casework. It is not uncommon for our equipment to be down for several weeks as we wait on parts and/or service. This is probably due to the staffing of vendors and supply-chain-management issues regarding foreign-produced parts. Second, we face the challenge of making sure the user and end-user of the equipment is properly trained and proficient in understanding the proper utilization of instrument. This requires training and re-training of staff. Having poorly trained staff can cause harm to patients, improper use the of equipment, damage to the equipment and poor surgical procedure outcomes. Third, a challenge that most facilities don’t consider is proper storage space
for its inventory of C-arms. I imagine many facilities face issues regarding how to store equipment when not in use or when it needs to be serviced. UCSF does not have a large reservoir of space to park our fleet of C-arms. Therefore, we are in constant motion moving equipment around from OR suites back to a designated storage area with an accessible outlet for charging. Because C-arms consist of two large pieces, finding storage for 13 pieces of equipment is quite a challenge.
Jones: One of the biggest challenges with C-arm use in our outpatient facilities, is the radiologist or radiologist assistant coverage. Shortages in this field limit the number of days and procedures that we can offer our patients.
Richards: All the C-arms are wireless, which is great but sometimes there are areas in the OR where you can’t send your images. We just have to move them around until we get a signal.
Q:
Adams: We have implemented a quality check application that replaces paper-based processes, allowing radiology technologists to complete checks electronically and onthe-go. This innovation ensures that quality checks are performed consistently and efficiently daily, enhancing workflow.
Bridges: Some innovative uses or protocols that we have implemented is working with our navigation vendors for bronchoscopy to install software on our C-arms. This software is designed to make navigation for lung nodules much easier and more precise during a procedure. Another interesting innovation recently with C-arms has been the standardization of a small touchscreen user interface on the C-arm. Our radiologic technologists utilize this innovation to precisely position our equipment for specific anatomical imaging, to help measure vessels, and to mark areas proximal and distal for stenting or hardware pinning.
Jones: We are currently using our C-arms in the outpatient facilities for joint aspirations and injections and MRI and CT Arthrogram injections.
Richards: Currently, we are using the ROSA robot in conjunction with our C-arms for spine cases. The patients need to get a pre-op CT scan protocol that was put together with the surgeons, CT and the vendors which calls for 1mm cuts or smaller so that it can be used with the C-arm images and then converted over to the robot. •

A niche job board for the HTM and imaging communities
3300+ biomedical and imaging candidates
350+ open job opportunities throughout the United States
htmjobs@mdpublishing.com for posting inquiries
htmjobs.com to register today
Single-job postings to 12-month unlimited memberships

Featured Employers: Agiliti, Renovo Solutions, TRIMEDX, Erbe USA Incorporated, Middlesex Health, SP Associates, and more!





The global fixed and mobile C-arms market size was estimated at $3.32 billion in 2024 and is expected to expand at a CAGR of 4.2% from 2025 to 2030, according to Grand View Research.
Factors contributing to industry growth, according to the Grand View Research report, include a rising number of surgical procedures, growing demand for minimally invasive surgeries, technological advancements, the increasing prevalence of chronic disorders, and the expanding global geriatric population. For instance, the WHO states that by 2030, one in six people globally will be aged 60 years or older.
Using C-arm systems in intraoperative procedures has become increasingly essential because they provide highresolution, real-time imaging that enhances surgical precision and patient outcomes. These systems are particularly valuable in complex procedures where accurate visualization of anatomical structures is essential. The growing adoption of minimally invasive surgeries, prioritizing smaller incisions, reduced recovery times, and lower risk of complications further drive growth in the fixed and mobile C-arms industry. These surgeries often require precise imaging guidance, so C-arm systems are important in operating rooms.
In addition, technological advancements, such as improved image quality, reduced radiation exposure, and enhanced system mobility, are significantly contributing to the widespread use of these systems, making them more efficient and accessible for various surgical applications. In March 2024, Siemens Healthineers introduced an advanced, automated, self-driving C-arm system designed for intraoperative imaging in surgery. The Cios Move features holonomic, omnidirectional wheels that enable precise maneuvering, even in confined spaces, and allow for easy and accurate positioning. The system can be moved to pre-set positions at the touch of a button using a remote control, significantly reducing the workload for technologists who previously had to adjust these positions manually.
The growing prevalence of chronic disorders is also contributing to the expansion of fixed and mobile C-arms industry, as these conditions frequently require advanced imaging for diagnosis, treatment planning, and surgical
interventions. Chronic disorders such as cardiovascular diseases, cancer, diabetes, orthopedic conditions like osteoporosis or arthritis, and neurological disorders like Parkinson’s disease or strokes often necessitate surgical procedures where precise intraoperative imaging is required.
Mordor Intelligence reports that the North America C-arm market size is estimated at $0.94 billion in 2025, and is expected to reach $1.19 billion by 2030, at a CAGR of 4.7% during the forecast period (2025-2030).
The healthcare system witnessed enormous challenges as a result of the COVID-19 pandemic. Several outpatient treatments were postponed or restricted during the COVID-19 pandemic to reduce the risk of viral transmission. Most chronic therapies were regarded as non-urgent. However, several imaging diagnostic technologies were widely available for COVID-19 diagnosis. The widespread use of diagnostic imaging technology during the COVID-19 pandemic significantly added to the market growth during the pandemic period.
Moreover, an article published in the Indian Journal of Radiology Imaging in January 2021 indicated a limitation in non-urgent imaging during the COVID-19 pandemic, which caused the rescheduling of mammograms, and other such screenings for diversion of the facility for COVID-19 care. Such postponement during the pandemic increased demand for imaging services. Currently, the market is regaining its growth pace owing to the normalization of the situation coupled with an increasing burden of injuries and road accidents.
The major factors driving the market growth in North America include the increasing geriatric population and the incidence of chronic diseases, and advancements in maneuverability and imaging capabilities. Moreover, the rising number of sports injury cases is expected to impact the North American C-arm market’s growth significantly.
Fortune Business Insights also predicts market growth.
“The global C-arms market size was valued at $1.95 billion in 2023, and is projected to grow from $2.03 billion in 2024 to $2.91 billion by 2032, exhibiting a CAGR of 4.6% during the forecast period. North America dominated the global market with a share of 53.33% in 2023,” according to Fortune Business Insights. •

*Disclaimer: Products are listed in no particular order.
The OEC 3D is a surgical imaging C-arm that provides precise 3D and 2D imaging to surgical suites while enabling efficient imaging every day. Based on GE HealthCare’s proven AW image fabric technology, the OEC 3D C-arm now enables surgeons to quickly capture and analyze 2D as well as precise 3D volumetric images with a C-arm, bringing CT-like images into the operating room. The OEC 3D continues to demonstrate versatility for every day procedures ranging from neuro-spine and orthopaedic trauma to interventional procedures including vascular, cardiac and pulmonary.
The Persona CS Mobile Fluoroscopy System is an advanced C-arm solution designed for rapid single unit positioning and is ideal for orthopedics, ASCs and pain management clinics. The system has a 5kW generator and a high resolution, 4K, 27-inch surgical viewing monitor with enhanced arm articulation. Users will experience advanced imaging clarity with a choice of 21 or 30cm Cesium Iodide (CsI) flat panel detector. With a dedicated radiography mode, removable grid and fluoroscopic imaging at up to 30 frames per second, Persona CS offers unsurpassed imaging performance in a compact footprint.
The Ciartic Move, a fully motorized mobile C-arm from Siemens Healthineers with self-driving capabilities, can accelerate and standardize 2D fluoroscopic and 3D conebeam computed tomography (CT) imaging for surgeons and operating room teams in hospitals and outpatient facilities. Designed for orthopedic, trauma, and spine surgery, the Ciartic Move also can be used in thoracic, vascular, cardiovascular, and general surgery, as well as urology and interventional pulmonology. Its self-driving capabilities automate imaging workflows, reducing the time, effort, and workforce capacity required to manually move and position the C-arm. Up to 12 procedurespecific positions can be stored and recalled at the touch of a button, along with related imaging parameters. Users can experience time savings of almost 50% during spine surgery and 55% during pelvic surgery compared with traditional mobile C-arms. A single user can fully operate the system remotely via a wireless control, even from within the sterile field. Its fully motorized chassis and touch-sense handles enable effortless maneuvering.


Hologic’s Fluoroscan InSight FD Mini C-arm imaging system is designed for easy positioning, flexibility and convenient mobility. The system features a rotating flat detector that is ideal for imaging long bones and, along with its collimator, enhances surgical positioning. The C-arm is designed with a forward tube source and has a 120-degree range of motion, both forward and backward, for excellent maneuverability and flexibility. Additionally, the Fluoroscan InSight FD Mini C-arm imaging system from Hologic offers a Low Dose Rate Option that enables the user to reduce dose rate while still providing clinically equivalent images. The unit also lowers scatter dose by 50% at 30 frames per second. The system can improve workflow as its customizable imaging parameters can be tailored to the preferences of individual surgeons.




“ICE Webinars always provide great timely information in a well planned format.”
- Nancy Godby, Director of Radiology, Cabell Huntington Hospital - Marshall Health Network
“I attend ICE webinars because of the variety of topics and presenters.”
- John Beall, Regional Director, United Imaging Healthcare
“I attend ICE Webinars to learn more about other imaging styles and get CE credits.”
- Amanda Brunson, Manager of CT and MR Imaging Services, MUSC Health Orangeburg
“I participate in these webinars to enrich my professional knowledge and to be able to share the news in the field with my students. “
- Calin Corciova, Associate Professor, Medical Bioengineering Faculty

“I attend ICE Webinars to learn more information related to radiology and imaging technology.”
- Krista Andrews, Imaging Manager, BSHW
... Since you are still flipping through this magazine, it simply means that you still have not found an honest, reliable, pre-owned imaging company that sells working systems.

Web: www.metropolismedical.com Well, Look No Further!
C-Arms • Bone Densitometers • CT • Mammography MRI • Nuclear Medicine • Radiographic Rooms R/F Rooms • Ultrasound • X-Ray

Tel: 718-371-6026
Fax: 718-371-6032
Email: info@metropolismedical.com



Medical Technology Management Institute (MTMI) began in 1989 when J. Ed Barnes, Ph.D., saw a need for continuing education for radiologic technologists. The company began with basic X-ray continuing education but soon branched out by adding cross training for its customers. MTMI had the first mammography training course to be accepted by the FDA to meet the MQSA requirement. MRI and CT training soon followed along with other modalities. Expansion continued with the addition of continuing education programs for physicists and physicians.
MTMI is celebrating 36 years in business in 2025 with 9,050 programs offered. Since its inception in 1989, 178,000 students have earned 1.82 million credits. MTMI President Brenda DeBastiani and Steve Cushman, Senior Director of Marketing, recently shared more information about the company and its plans for the future.
Q: WHAT IS THE MISSION AND VISION OF YOUR COMPANY?
A: The Medical Technology Management Institute is dedicated to providing quality continuing education, training in procedures and consulting services on advanced technology equipment in multiple imaging modalities within the medical community.
Q: CAN YOU DESCRIBE YOUR COMPANY’S CORE SERVICES OR PRODUCTS?
A: We provide world-class continuing education and training for medical imaging professionals with a specific focus on programs for technologists, mammographers, sonographers, dosimetrists, medical physicists and physicians.
Q: WHAT MAKES MTMI UNIQUE OR ESSENTIAL IN TODAY’S MARKET?
A: Our programs are taught by working clinical experts with national reputations in their field. What really sets MTMI apart is the breadth of our offering. We cover virtually every modality including radiography, mammography, computed tomography, magnetic resonance imaging, bone densitometry, ultrasound, PACS/imaging informatics, nuclear medicine and fluoroscopy. In addition, we deliver our programs in multiple formats to meet the busy lifestyles of today’s medical professionals. These convenient formats include live training, self-paced courses, webinars, on-demand videos and hands-on workshops.
Q: WHAT MILESTONES OR ACHIEVEMENTS HAS YOUR COMPANY REACHED?
A: Launching self-paced mammography and CT over the past 8 months has been a milestone for us! Also, we launched our first group of on-demand videos for medical physicists. All of those things have been “in the works” for quite some time.
Q: ARE THERE ANY RECENT AWARDS, RECOGNITIONS OR EXPANSIONS YOU CAN SHARE?
A: MTMI is well known in the industry for providing in-services just in time for MQSA or ACR violations or failures. Our industry experts provide additional training to mammographers or radiologists to ensure that their skills meet expectations, and their images pass inspections/accreditations.
Leadership and Team
Q: WHO ARE THE KEY FIGURES LEADING YOUR COMPANY?
A: Brenda DeBastiani is our president, and we have met several milestones with her leadership since her start in April of 2024.

She provides assistance in completing projects to ensure success, while truly caring about each employee.
Steve Cushman is the director of marketing, and he has been a key leader within the organization for over 10 years. His quiet leadership and positive personality shines wherever he goes. We have also relied on Steve for many things that are outside of the marketing scope because of his broad knowledge.
Miranda Melton, director of women’s imaging, is our key leader with mammography training, in-services and webinars. She is a respected expert in the mammography world. Her passion for taking care of patients is exceptional. When she provides instructions during webinars, in-services, or positioning workshops, the students naturally connect with her teaching style. They comment on how she can immediately improve their positioning techniques after watching them for just a couple minutes and how passionate she is about mammography. The Las Vegas Breast Imaging Conference, held annually, is one that you do not want to miss (scheduled October 4-5, 2025 this year). The lineup of speakers is being finalized as we speak, and Miranda will not disappoint!
A: Brenda DeBastiani, MBA, CRA, FAHRA, RT(R), has worked in imaging her entire career. She started out as a radiologic technologist and CT technologist for the first 15 years, supervisor for 12 years, and then director for 11 years. She worked in the hospital setting, while actively volunteering with the AHRA since 2004, where she volunteered on the design team, board of directors and was AHRA president 2022-2023. All of this experience prepared her for her role as MTMI President.
Steve Cushman, MBA is a veteran of the advertising industry. Early in his career, he spent 10 years as a consultant for McDonalds working with the new product development team in addition to leading a redesign of the drive-through experience. The following years, Steve drove strategic marketing initiatives for leading companies in agriculture, banking, higher education and healthcare. His initial contribution to MTMI was to introduce simulcasting of cross-training courses and transforming the continuing education program format from an in-person classroom setting to live webinars.
Miranda Melton, RT (R) (M), graduated from X-ray school in 1998 and was cross-trained into mammography. She admits that, at first, she was not good at it but had the opportunity to work with a positioning specialist who gave her tips to improve the quality of her work. Once Miranda saw the improvements, she got very excited about mammography. She was a stay-at-home mom for a bit, and when she came back to work, she began helping her coworkers to perfect their skills. After a 12-year stint in imaging management, Miranda joined MTMI. She first started with webinars and then came on full-time as the director of women’s imaging. She realized that she has always enjoyed teaching others, and that passion has grown. Students comment that Miranda has a soothing voice and creates a bubbly, upbeat atmosphere to learn. She engages her students and explains the concepts with good analogies and her own personal experiences or challenges that she has learned to overcome. Miranda shows students what joy mammography can bring to their lives.
Q: WHAT IS THE COMPANY CULTURE LIKE?
A: MTMI is truly a team-oriented environment. The staff is small and versatile. It’s a roll up your sleeves type of place.
Q: WHAT DIFFERENTIATES YOUR COMPANY FROM COMPETITORS IN YOUR INDUSTRY?
A: MTMI is a single source provider and can meet an institution’s every need because we offer programs for each staff discipline including technologists, sonographers, physicians and medical physicists. We have cross-training in every modality, this helps build flexible imaging teams to relieve the pressure of staff shortages and improve ROI. Our continuing education programs are offered in flexible webinar and on-demand formats to meet the unique needs of each employee. MTMI truly stands alone as the company that provides comprehensive imaging education. MTMI prides itself for being able to support imaging professionals through every step of their career from cross training to new modalities, meeting CE requirements and to developing leadership skills.
Q: WHAT’S YOUR UNIQUE SELLING PROPOSITION?
A: As many imaging leaders have already discovered, MTMI

can save them money, make their lives easier, keep their staff current, improve patient care and avoid mistakes through continuous education. MTMI is flexible. We can provide imaging departments with in-service training on site, via live webinar and through specialized training created for each individual need. We provide what you need, when you need it!
Q: HOW HAS YOUR COMPANY ADAPTED TO RECENT INDUSTRY TRENDS OR CHALLENGES?
A: MTMI has aggressively invested in offering more programs in more formats. Cross-training for mammography and CT are now offered in three formats: In-person, live webinar and online self-paced. We are significantly increasing our on-demand programs with 25 new programs in 2025. Some of the new on-demand topics include our popular registry programs for mammography, CT, bone densitometry and interventional. MRI and breast ultrasound will be coming soon in addition to our first ever physicist on-demand programs. We are partnering with industry leaders like ScanLab to incorporate the latest innovation in imaging education, scanning simulation. In addition, we are listening to our customer’s requests for payment plan options which will launch in early 2025.
Q: HOW DOES YOUR COMPANY ENGAGE WITH THE COMMUNITY OR SUPPORT SOCIAL CAUSES?
A: Because MTMI is both local in Wauwatosa, WI, and remote across the country, each individual MTMI employee is encouraged to volunteer at their local level. In the imaging front, MTMI strongly supports the ASRT “Be Seen” Campaign, and we encourage all imaging technologists to raise the bar in educating others about the profession.
Q: HOW DO YOU INCORPORATE CUSTOMER FEEDBACK INTO YOUR PROCESSES?
A: MTMI thrives on student feedback. We survey every student at the completion of their program and review the input with instructors and leadership to incorporate continuous improvement. Each and every survey is read, and adjustments are made, where needed.
Q: WHAT ARE YOUR PLANS FOR THE COMPANY’S FUTURE?
A: Continued growth and innovation. We are listening to our
students who want more self-paced online programs. We are offering new programs in ultrasound, and more formats for medical physicists. We are also reaching out to the medical physicist assistants, as our medical physicist education also meets their needs.
Q: ARE THERE ANY EXCITING PROJECTS, PARTNERSHIPS OR EXPANSIONS ON THE HORIZON?
A: We already have MTMI videos imbedded in Densitas, teaching mammographers better positioning techniques. We already have ScanLab included to our CT and MRI courses, allowing the students 5 months of interactive, virtual scan time. As new opportunities arise, we are eager to partner to improve patient care and to improve our visibility.
Q: HOW DO YOU ENVISION YOUR INDUSTRY EVOLVING, AND HOW WILL YOUR COMPANY STAY AHEAD?
A: When COVID hit, our company moved from a total “inperson” education company to a virtual education company. We realized that many students needed that “in-person” educational experience to learn best, so it was brought back as soon as possible. Because we learned that many students appreciate the virtual experience, we left that in place. Self-paced is the new avenue, allowing students to access education when it is most convenient for them. Keeping our educational material updated to reference cutting edge technology has been implemented for 2025 courses, and we will continue to do that. We have to remain aware and responsive to our students’ needs. That will keep our company ahead.
Q: WHAT GOALS ARE YOU FOCUSED ON ACHIEVING IN THE NEXT 5-10 YEARS?
A: Consistent growth, expansion of physician programs, integration of the latest learning platforms
Q: WHAT DO YOU WISH MORE PEOPLE KNEW ABOUT YOUR COMPANY?
A: That we are a complete turn-key solution. That we offer inservices for ACR failures or MQSA violations, plus other modality in-services. That we are a leader in medical physicist continuing education.
Q: WHAT’S ONE SURPRISING OR FUN FACT ABOUT YOUR COMPANY THAT READERS MIGHT NOT KNOW?
A: That we train more mammographers than anyone else in North America.
Q: IS THERE ANYTHING ELSE YOU WOULD LIKE TO ADD?
A: MTMI has been around for over 35 years, and we have been great partners with technologists, physicians, providers, medical physicists and medical physicist assistants, athletic trainers, and physical therapists. We know who we are and what we specialize in. We want to continue partnering with each of you and meet your needs. Let us know how we can help!

Bone Densitometry Course
Mar 8 - 9 and May 3 - 4
Breast Ultrasound Course
Mar 21 - 23 and Apr 25 - 27
CT Training Course
New! Simulation Lab Included
Apr 28 - May 2 and Jul 28 - Aug 1
Initial Mammography Course
New! Online Self-Paced
Mar 10 - 14 and Apr 7 - 11
MRI Training Course
New! Simulation Lab Included May 12 - 16 and Sep 29 - Oct 3




4 - 5
MRSO Certificate Program
Apr 26 - 27 and Jun 28 - 29
MSK Ultrasound Course
Oct 10 - 12
PACS Administrator Course & Imaging Informatics
May 12 - 16 and Sep 15 - 19
Vascular Ultrasound Course
May 17-18 and Oct 10-11 See website for additional dates
Las Vegas Breast Imaging Conference
Oct 4 - 5





BY MATT SKOUFALOS
When Keith Hall joined the U.S. Army in 1999, he was a 19-year-old searching for opportunities that could help him find a stable career. What began as a six-year enlistment turned into a 21-year activeduty stint, in which Hall developed training in medical equipment repair, and then supported it with additional learning in imaging-specific skills. He was among the first participants in a training program with Philips that sent him to Cleveland for a year to become a subject matter expert in its CT equipment, and then into the Army global CT program for another five years before rounding out his career with another five years of leadership assignments.
Even with that lengthy background of classroom and field training and expertise, after Hall began his civilian career with Renovo at the University of Utah, he nonetheless needed to make adjustments upon being promoted to the company’s director of service for imaging for the western United States. Leadership skills are transferable, especially for someone with the ability to learn on the job, but there are always refinements to be made.
“There were things that I didn’t know or expect, but I feel like if you grow up and pay attention to your surroundings as you’re growing, you’ll have clues as to what your boss is doing,” Hall said. “I had a pretty easy transition because I had been preparing for growth and change for years. That may be the case for a lot of people looking to make the transition from biomed to imaging service leader.”
For professionals who come into the medical equipment repair field as a biomedical engineer, there’s no guarantee that their responsibilities will include medical imaging devices. Of the hundreds and thousands of technologies that are used to keep a healthcare system operating at peak efficiency, medical imaging devices are in a class unto themselves. They’re expensive to maintain and repair, and require a great deal of precision to function appropriately. Occasionally, the people who will be tasked with their oversight, or who assume those responsibilities as they climb organizational ranks, may not have the same familiarity with imaging equipment that technicians dedicated to their service do.
In circumstances such as those, healthcare technology managers can feel out of sorts, particularly for professionals who are used to having a strong command of their field. But with appropriate support and a plan for expanding their knowledge base, the transition can be managed effectively.
“I think the scope of the work is probably the biggest
differentiator between being a biomed and being a leader who came from biomed,” Hall said. “You’ve got to be able to understand overarching hospital business models from the C-suite perspective. Usually, they see biomed as something that costs them money; you need to be the ambassador that reinforces the idea that biomed is a revenue sustainer.”
Hall said he’s found success by developing the ability to split his focus among day-to-day, operational activities as well as long-term, strategic goals – not only those for the company, but those for staff and himself as an individual. Critically, the ability to verbalize those responsibilities and the processes that comprise the path to those goals involves developing strong written and verbal communication skills, as well as the ability to scale conversations up or down depending upon the audience.
“Most things that we do in our day to day jobs, regardless of what industry we work in, follow a process of some sort,” Hall said. “When I’m looking at fixing something, because something’s not going right, or I’m not getting the desired outcome, there is either a problem with the process, or there’s a problem with training or understanding. It’s the process, or it’s training, or it’s people.”
“When you understand that almost every problem can be broken down to the process, training, or the person, you can solve things so quickly,” he said.
Where biomeds may be generalists, imaging service engineers often are specifically focused on one or a limited handful of imaging modalities. They require a comprehensive understanding of the needs of the people they serve as well as of the equipment they service, its lifespan and the ability to maintain a current understanding of how to manage both.
Because the role of an imaging service manager is typically tailored to the specific requirements of the position in the context of the facility in which it’s housed, its focus can shift significantly depending on whether the manager is working in a single hospital, or supporting a broader regional, national or global team. That makes flexibility and mental agility critical skills in these contexts.
“Regardless of the environment, certain attributes remain consistent,” Hall said, “an understanding of inventory management and customer needs, the ability to evaluate resources, and developing effective service delivery models. Managers must also grasp the financial implications of downtime, as a non-functioning machine can lead to revenue loss for healthcare facilities. A successful imaging service manager communicates these insights to radiology directors

As James C. Hunter says in The Servant, ‘Perhaps we lead best by serving.’
and C-suite executives with urgency.”
Sometimes the skills that a strong imaging service leader needs aren’t always to be found within the organization itself. Hall recommends joining professional organizations, such as the Association for the Advancement of Medical Instrumentation (AAMI), following along with research provided by the Radiological Society of North America (RSNA), and seeking training from outside workshops and professional conferences. The Imaging Conference and Expo is set for February 22-24 in Orlando, Florida (AttendICE.com). Also, ICE Magazine offers webinars (ICEwebinars.live).
“Leadership needs to take a role in mentoring, and it doesn’t have to be within the organization,” he said. “I’ve mentored people who aren’t in Renovo; I’ve always fostered growth and development. The investment is in the people and their skill sets, and in our community.”
Eric Massey, regional director of operations field service in the healthcare technology solutions business at Crothall, spoke about the value of key mentors in helping to coach anyone moving into a management role. Massey, who worked as a biomed until 2010, said that when he was promoted into management, he was guided through his new role by leaders who took an interest in him and helped him network.
Among the benefits of working for a national service provider like Crothall, he said, is having access to a large support system of professionals who’ve often worked in various environments before joining the company. Their experience especially can be meaningful in helping younger and rising professionals work through the early days of a new job change.
“I had some really good mentors,” Massey said. “I would meet with them, and they would introduce me to people. Conferences are huge.”
Equally meaningful to developing the skill set of an imaging manager is the technical training required to do the job. Managers who oversee medical imaging and biomedical engineering staff may have different backgrounds, and Massey believes that the best way to make sure that someone with biomed experience understands an imaging oversight role is to get training in imaging devices.
“Going to an RSTI training or a Tri-Imaging training goes a long way to understanding the systems,” he said. “That’s what I did. It prepares you to communicate and understand those systems effectively.”
Although not every workplace is structured the same, Massey also thinks that specialization in job focus at the technical level should be mirrored by specialization at the management level above it.
“I think an imaging manager needs to be separate from the biomed manager because they’re two distinct areas,” Massey said. “Having people specific to imaging and understanding those modalities goes a long way to making sure that program runs efficiently. We need to train more imaging managers.”
When considering which employees to invite into management roles, Massey said he starts feeling out his best imaging engineers to plumb the depths of their knowledge, see how they communicate, and assess their technical background. Then, he considers which of those areas are strengths and which could use more polish, and connects them with opportunities to learn.
“I look for strong communication skills,” Massey said. “That’s one of your biggest challenges as an imaging manager: effectively communicating with the radiology director, being able to talk the customer through the repair, walking the customer through the repair process, and
reassuring them that we’re adhering to OEM procedures.”
“Everybody’s hot when these systems go down,” he said. “Does the customer trust and connect with the engineer? That’s when I know they’re ready to go out independently. If I see someone managing a program or a high-end imaging tech that radiology directors like, that’s what I look for.”
Shelby McCarty, imaging director of service for Midwest region for Renovo, agrees that the people who are best suited for management roles demonstrate strength in their ability to communicate with those around them, as well as serving their needs and leading people. Unlike other areas of leadership, where technical skills might be considered secondary facets of the job, McCarty said he believes they’re instrumental to having success as an imaging service manager. He differentiates between the management of things, “like a checkbook or inventory,” and the leadership of people.

“Leadership qualities are so much more important than management qualities,” McCarty said. “You must be able to build relationships and a network, or you won’t be successful. When I need help at a certain site, I call a local OEM service manager, and I get help only because we’ve developed a relationship. These relationships are usually built by trust through serving.”
“As James C. Hunter says in The Servant, ‘Perhaps we lead best by serving,’ McCarty said. “It’s the same thing you need as a field service engineer with your customer base: you develop the network and the relationship by serving, and that makes everything so much easier.”
In addition to building relationships, McCarty said strong leaders are able to check their own assumptions. The tactic of leading from the front doesn’t work without being able to balance the ability to follow input from others alongside your own instincts.
“In the industry, as you progress, there’s a fine line between ego and confidence,” he said. “Where the line gets drawn is where you’re self-aware enough to say that you’re not as good at something, and then go after those things. When I wanted to learn cath labs, I shadowed the main cath lab staff as a biomed. It’s that lifelong learning mentality and trying to get better at the things you’re passionate about that make you successful.”
Developing honesty and self-reflection about areas of personal strengths and weaknesses opens the door for a good leader to learn from those around them, McCarty said, and that’s a necessity when leadership roles carry responsibilities far different from those a biomed/imaging engineer may previously have mastered.
“Letting go of the technical side of things is something that is often hard for former imaging service engineers to let go of,” McCarty said, “but being truthful about yourself is key to growing. I consistently ask someone to show me how to do things more efficiently, how to better understand a financial statement better, or something as simple as tips for Microsoft Excel reports. You can learn something from everyone you meet.”
The process of evolving as a professional, adding new skills, and shoring up weaknesses helps imaging service managers not only to develop their own abilities but also to drive changes that make the work environment for the teams better that they oversee. This is particularly important, McCarty noted, as the field of healthcare technology management (HTM) sheds long-time professionals faster than it can necessarily replenish its workforce.
“To address this challenge, the HTM industry must become more innovative and proactive in developing effective training programs and recruitment strategies to engage the next generation of professionals,” he said. “It is crucial to cultivate a skilled workforce that can meet the growing demands and staffing needs expected in the near future, ensuring that we maintain a high standard of care within healthcare settings.” •

BY BETH ALLEN CRA, RT(R)(CT) DIRECTOR’S CUT
The MRI technologists that I have had the opportunity to get to know over the course of my career all agree on one thing: implant research is a very complex, time consuming, daunting task that gets more imposing every day, since the healthcare industry is implementing new devices continuously. There are patients that may have a retained foreign body that needs to be investigated, and the history may be sketchy at best. The risk of not performing the task with high attention to detail is a threat to the safety of both the patient and the technologist. Even if another tech is assigned to do the research, it is ultimately the responsibility of the performing technologist to review and sign off on the safety of executing the scan. Incomplete information can cause dissatisfaction for the patient, stress for the technologist due to schedule backup and fear of harm, as well as delays to patient care. Not completing research for these patients could deny them eligibility to have an MRI, potentially delaying diagnosis.
There is good news. This required extra work is being recognized with the approval of six new CPT codes under the heading of “Magnetic Resonance Safety Implant/Foreign Body Procedures” that went into effect January 1, 2025. As of this writing, we are still waiting on clear direction regarding how to implement the use of these codes and what
documentation will be required, but the fact that the codes have been created is a giant step in the right direction.
The intention of these codes is not that they would apply to every patient with an implant, but that they be utilized for the work required for complex implants or foreign bodies. There are plenty of those. It ultimately comes down to determining if it is safe to scan or not. Sometimes, it requires a team to make that determination, including technologists, physicists, physicians and device manufacturers to figure it all out.
In some cases, just finding out what the implant is may require a significant amount of time and research.
Several years ago, Banner Imaging identified the burden of this work on our front-line technologists. We implemented a task-oriented workflow through our RIS system that has been successful in centralizing the more complicated research required for scheduled patients ahead of time. This frees up the technologists scanning all day to focus on the patient in front of them, while an MRSO does the inquiry into these complicated cases. With these new CPT codes, it will help us to justify the extra resources needed to make our workflow even more robust. With 1 MRSO covering 27 scanners, we are going to need more help.
There is still quite a bit of information needed for us to take advantage of these codes within our system. I have plenty of questions, which I am confident we will get answers to, but I am grateful that we did the work ahead of time and have the structure to build upon.

We will have to implement a way to assure that we assign the correct code. There have been a few articles published that define the codes. They are segregated into work that is done to plan for the MRI ahead of time and work that is done the day of the exam. More than one code can be applied. I will be on the lookout for the information and instruction to use these codes, but I am overjoyed that they have been created.
Overall, this advancement now reimburses this necessary safety work. Across imaging, it gives value to the time
required to do the research and may assist in securing support to invest in our safety programs. Hopefully that will increase efficiency, safety and satisfaction for our patients and our MRI team members.
We are on the right track.
What took them so long?
Thanks for all you do! •
— Beth Allen CRA, RT(R)(CT), is the director of clinical operations with Banner Imaging.
We have a mission: Self perform on every aspect of our business. Specialize on specific modalities: Pet CT, CT & NucMed. Focus in a key geographic region.



BY MARK WATTS
For decades, radiologists were at the forefront of cardiac imaging, pioneering techniques and collaborating with cardiologists, physicists and engineers to develop modalities such as radiography, echocardiography and coronary arteriography.
Yet, paradoxically, radiologists now find themselves sidelined in a field they helped create. This shift reflects the aggressive expansion of cardiologists into cardiac imaging and radiologists’ retreat from the discipline.
The decline of radiologists’ involvement in cardiac imaging began in the 1970s when cardiologists, initially trained by radiologists, mastered coronary arteriography. Self-referral and unmet demand for cardiac imaging spurred cardiologists to claim greater control over these procedures, effectively excluding radiologists from cardiac catheterization laboratories. As radiologists withdrew, cardiologists embraced emerging imaging modalities such as echocardiography and nuclear medicine, which provided functional and quantitative insights critical for patient management.
Artificial intelligence (AI) now promises to redefine the roles of radiologists and cardiologists, offering challenges and opportunities. AI-powered tools are revolutionizing cardiac imaging by enabling faster image acquisition, precise quantification of cardiac function and automated detection
of subtle abnormalities. This shift favors a collaborative approach, as AI democratizes access to advanced imaging insights. Radiologists, equipped with expertise in imaging physics and AI integration, are uniquely positioned to reclaim their influence. Advanced modalities like CT and MR imaging have emerged as pivotal tools in cardiac imaging. These technologies offer high-resolution data essential for assessing myocardial function, evaluating coronary arteries and guiding interventional procedures. By leveraging AI, radiologists can enhance diagnostic accuracy and streamline workflows, reinforcing their value in multidisciplinary teams managing heart disease.
A critical factor in radiologists’ diminished role has been the erosion of specialized training programs in cardiac imaging. Most radiology residency programs now allocate minimal time to cardiac imaging, leaving radiologists underprepared to compete with cardiologists. However, renewed interest in cardiac imaging training offers hope. Programs emphasizing AI-driven techniques, such as automated plaque characterization and myocardial strain analysis, can reinvigorate the field and attract new talent.
The future of cardiac imaging depends on collaboration between radiologists and cardiologists. AI enables such partnerships by providing tools that transcend
traditional boundaries. For example, AI algorithms for image reconstruction and interpretation can support radiologists in producing high-quality diagnostic studies while enabling cardiologists to focus on clinical decision-making.
Moreover, AI facilitates the integration of multimodal imaging data, creating comprehensive cardiac assessments that combine the strengths of CT, MR, echocardiography and nuclear medicine. This holistic approach aligns with the broader goals of precision medicine, improving patient outcomes through personalized care pathways.
Radiologists oversee the majority of CT and MR scanners, placing them at the epicenter of cardiac imaging advancements. By adopting AI-driven workflows, radiologists can deliver cost-effective, noninvasive diagnostic solutions that rival traditional invasive methods. Additionally, radiologists’ expertise in managing large imaging datasets positions them to lead research in AI applications for cardiac imaging, such as predicting outcomes or identifying early markers of disease.
To regain a central role in cardiac imaging, radiologists must prioritize education, research and collaboration. Expanding training programs to include advanced cardiac imaging
techniques and AI applications is essential. Research funding for imaging innovations, particularly in molecular imaging and AI, can also catalyze progress.
The cardiology community’s historical success in securing funding from organizations like the National Institutes of Health and the American Heart Association serves as a model. Radiology departments must adopt a similar strategy, emphasizing the societal impact of cardiac imaging advancements.
The evolution of cardiac imaging reflects a broader transformation in healthcare, where interdisciplinary collaboration and technological innovation are paramount. Radiologists have an opportunity to reestablish their role by embracing AI, fostering partnerships with cardiologists and investing in the next generation of imaging specialists. With heart disease remaining a leading cause of mortality, radiologists’ contributions to improving diagnostic accuracy and patient care have never been more crucial.
This is not merely a reclamation of territory but a reinvention of radiology’s identity within cardiac care – a chance to redefine the field through innovation, expertise and collaboration. •
— Mark Watts is an experienced imaging professional who founded an AI company called Zenlike.ai.



In the fast-paced world of medical imaging, hospitals and healthcare facilities rely on highly trained professionals to maintain and service their imaging equipment. Properly functioning imaging devices are critical to delivering accurate diagnoses and effective treatments. But where do the technicians servicing these advanced systems get their training? Increasingly, third-party service training programs are filling this essential need—offering specialized, hands-on instruction that equips engineers with the skills to troubleshoot, maintain, and repair complex medical imaging systems.
As imaging equipment becomes more sophisticated, the need for advanced technical knowledge has grown. Thirdparty service training programs, such as those offered by the Radiological Service Training Institute (RSTI), bridge the gap between manufacturer training and the hands-on skills demanded in the field. These programs are designed to be comprehensive and practical, providing technicians with real-world experience on a variety of imaging systems, from X-rays to MRIs.
One of the standout benefits of third-party training is its focus on the independent service market. While original equipment manufacturers (OEMs) may limit their training to their own systems, third-party training programs cover a broader range of equipment, preparing technicians to service multiple brands and models. This
versatility not only enhances a technician’s capabilities but also provides hospitals with more cost-effective and flexible service options.
Hands-on experience is the cornerstone of effective technical training. At RSTI, for example, technicians are not just taught the theory behind imaging equipment; they actively disassemble, reassemble, and troubleshoot machines in a controlled environment. This type of immersive learning ensures that students leave the classroom with practical skills they can immediately apply in their work.
Training courses are tailored to meet the diverse needs of attendees, ranging from basic principles for beginners to advanced troubleshooting techniques for seasoned professionals. This approach enables technicians to stay current with industry developments and confidently handle the challenges of modern imaging equipment.
When RSTI first opened its doors in 1985, the concept of third-party training for medical imaging equipment was almost unheard of. At the time, most training was either manufacturer-driven or unavailable to independent technicians, leaving hospitals and healthcare facilities with limited options for servicing their critical imaging systems. Recognizing this gap, RSTI became a trailblazer in the field, offering technicians and organizations access to high-quality education that was both comprehensive and brand-agnostic. This groundbreaking approach not only empowered independent service providers but also laid the foundation for a thriving industry that now plays

a vital role in ensuring healthcare systems worldwide remain operational and cost-effective.
Since opening its doors in 1985, the Radiological Service Training Institute (RSTI) has been a leader in providing exceptional training for imaging service professionals. Over the years, RSTI has earned a reputation for its rigorous curriculum, experienced instructors, and commitment to advancing the careers of its students.
In 2025, RSTI will celebrate its 40th anniversary, marking four decades of dedication to empowering technicians and supporting the healthcare industry. From its humble beginnings, the institute has grown to become a trusted partner for independent service organizations, hospitals, and engineers worldwide.
As RSTI celebrates 40 years of excellence, its commitment to innovation and education remains unwavering. The institute continues to expand its offerings, incorporating the latest advancements in imaging technology and adapting to the evolving needs of the healthcare industry.
For technicians seeking to enhance their skills or
organizations looking to strengthen their in-house service capabilities, third-party training programs like those at RSTI provide a proven pathway to success. By combining hands-on technical instruction with decades of expertise, RSTI ensures that imaging equipment—and the patients it serves—receive the highest level of care.
In 2025, RSTI’s 40th anniversary will be more than a milestone; it will be a celebration of the countless professionals who have passed through its doors and gone on to make a difference in healthcare systems around the world.
Third-party service training plays an indispensable role in maintaining the reliability and performance of hospital imaging equipment. Institutions like the Radiological Service Training Institute not only deliver exceptional hands-on instruction but also build a legacy of excellence that spans decades. As RSTI looks forward to celebrating its 40th year, its mission remains clear: to empower technicians and elevate the standard of imaging service training.
If you’re ready to enhance your skills and join a legacy of excellence, consider RSTI—where hands-on learning meets real-world expertise. •

BY NICOLE DHANRAJ
Having a diverse workforce is critical to advancing innovation, collaboration and patient care in healthcare, particularly in radiology departments. Yet too often, our efforts become knee-jerk reactions – a scramble to recruit broadly from underserved populations without first reflecting on the specific gaps in our teams.
This lack of intentionality can lead to a workforce that appears diverse on the surface but fails to bring the varied perspectives necessary for optimal team performance and patient outcomes. To create lasting change, radiology managers must start with a strategic question: Who are we missing?
From Reaction to Strategy: Improving Diversity in Radiology
It’s tempting to approach diversity by focusing on the broad goal of representation. However, this reactive approach often misses the nuances of what makes a team truly diverse and inclusive. Instead of asking how to recruit more diverse candidates, radiology leaders should start by evaluating their existing team’s composition.
Ask yourself:
• Are most of your hires coming from the same universities or medical schools?
• Do your team members share similar socioeconomic backgrounds or come from the same geographic region?
• Is your leadership team dominated by individuals with shared cultural or professional experiences?
When everyone comes from the same mold, it creates an echo chamber that stifles innovation, limits cultural competency, and alienates patients whose backgrounds differ from those of your staff. Diversity isn’t just about meeting quotas – it’s about ensuring your team has the range of perspectives needed to serve your patient population effectively.
Understanding who is missing requires an honest assessment of your department’s blind spots. This involves more than counting demographics; it’s about identifying the perspectives and experiences absent from your team.
Consider the following areas:
• Are you prioritizing graduates from prestigious universities while overlooking candidates from community colleges or technical programs?
• Does your hiring pipeline draw from the same local region, potentially missing candidates with broader life experiences?
• Are there patient populations – such as immigrants or non-English speakers – whose unique needs aren’t reflected in your staff’s expertise?
Identifying these blind spots allows you to move beyond surface-level diversity and address the structural barriers that may prevent certain groups from joining your team.
Once you’ve identified your department’s gaps, recruitment can become a targeted, strategic effort to enrich your team.
Here are some actionable steps:
• Partner with historically Black colleges and universities (HBCUs), Hispanic-serving institutions (HSIs), and community colleges to connect with candidates from underrepresented backgrounds.
• Look for candidates who have worked in diverse settings, such as rural hospitals, urban clinics, or international healthcare environments, to bring fresh perspectives.
• Focus on hiring individuals who excel in cultural competency, adaptability, and patient communication – skills that enhance team dynamics and improve care delivery.

By tailoring recruitment efforts, you ensure that new hires don’t just meet diversity goals but contribute meaningfully to the team’s collective expertise and cultural awareness.
Addressing blind spots isn’t just about recruitment; it also requires dismantling internal practices that reinforce sameness.
For example:
• If your hiring committee is made up of individuals from similar backgrounds, it may unconsciously perpetuate biases. Including diverse perspectives in hiring decisions ensures a more inclusive process.
• Are promotions in your department based solely on technical skills? Consider recognizing contributions that enhance team
culture, improve patient care, and drive innovation.
Breaking the echo chamber requires ongoing effort to challenge the status quo and ensure every team member brings unique value to the department.
By shifting from reactive DEI efforts to a strategic focus on who is missing, radiology departments can build stronger teams that reflect the communities they serve.
The next time you consider diversity, pause and reflect: Are we addressing this strategically, or are we simply reacting?
The answer will shape your team’s ability to deliver exceptional care and drive meaningful change. •
— Nicole Dhanraj, Ph.D., SHRM-SCP, PMP, GPHR, CPSS, CRA, R.T(R)(CT)(MR), is an experienced imaging director.

Mako is a cutting-edge solution that revolutionizes your way of work with plug-and-play simplicity. It’s our most efficient and versatile meter, delivering the highest practical accuracy experienced with the industry’s broadest application range. Beyond the hills of spreadsheets, Ocean NextTM software awaits. Ocean NextTM gathers data from Mako in real-time so you can truly excel. Immerse yourself in a world of streamlined routines and complete traceability, Ocean NextTM.


SERVICE
BY ERIC MASSEY
The medical imaging equipment services market is projected to surge to $85 billion by 2031, according to Market Research Intellect, driven by advancements in technology such as AI integration and enhanced MRI, CT and ultrasound systems. These innovations bring new complexities, increasing the need for specialized maintenance to keep cutting-edge equipment performing reliably and ensuring high-quality patient care.
Our industry faces a critical challenge amid this technological evolution – a growing shortage of skilled imaging service engineers (ISEs) capable of diagnosing, maintaining
and repairing increasingly complex imaging devices. With many experienced ISEs approaching retirement, recruiting qualified professionals to fill these roles is becoming more difficult. At the same time, an aging population and continuous investment in new imaging equipment are driving hospitals to expand their fleets of advanced imaging technology.
The U.S. Bureau of Labor Statistics projects a 17% growth in job opportunities for medical equipment repairers between 2021 and 2031 – a field U.S. News & World Report recently ranked among the top seven healthcare jobs “you’ve never heard of.”
Could a solution to filling the growing talent gap in imaging technology already be within our reach?
Addressing the demand for skilled imaging service engineers requires a multifaceted strategy that balances recruitment, retention and internal development. To attract new talent, offering competitive incentives, signing bonuses and clear pathways for career advancement can be effective. Equally important is recognizing and developing the talent already within your teams. Initiatives such as structured recognition programs, opportunities for upskilling, and targeted training programs help retain top talent, close workforce gaps and strengthen workforce capabilities. By looking inward and identifying biomedical technicians who show the aptitude and interest in expanding their skills, we can offer targeted training to help them transition into imaging engineers. Through targeted training, these team members can expand their skill sets, helping to fill workforce gaps while ensuring continuity in service delivery. Additionally, it benefits our clients by helping hospitals manage costs more effectively, while enabling our teams to remain agile in meeting the evolving needs and unique equipment mix of each hospital or region, ensuring timely and reliable support.
Investing in the development of our most promising biomedical technicians, we tap into a resource that not only addresses staffing needs but enhances the way hospitals manage the service needs of their imaging equipment. BMETs bring unique insights, streamline operations and reduce the risks of external hires. Training BMETs for imaging roles offers unique advantages, including:
• Reduced learning curve and improved consistency: BMETs bring a strong technical foundation, positioning them to learn the complexities of imaging systems more quickly while ensuring a deeper understanding of hospital-specific equipment.
• Lower recruitment risk: Hospitals can avoid the risks associated with hiring external candidates who may not be a cultural fit or familiar with the hospital’s systems.
• Strategic workforce planning: It allows service support companies and hospitals to create a pipeline of skilled workers, preparing for retirements or staff shortages without the pressure of sourcing external talent.
• Increased staff engagement: Offering an alternate career path shows a commitment to professional development, which can boost engagement, loyalty and overall job satisfaction.
Crothall Healthcare’s Healthcare Technology Solutions developed and piloted a training program designed to help its BMETs transition into ISE roles addressing a critical industry talent gap while advancing career growth from within.
Transitioning to an entry-level ISE takes several months to a year to complete. Fortunately, Crothall has been able to
leverage its relationships with third-party national training centers to enroll its BMETs in comprehensive training programs offered by these companies.
Comprehensive training, combined with their commitment to mastering new skills, ensures hospitals receive a high level of service. Every BMET completes core foundational courses before advancing to equipmentspecific training tailored to the healthcare organization.
BMETs, like ISEs, often face high-pressure situations where they need to explain the impact of equipment issues and servicing needs in a way that’s clear and reassuring. At Crothall, we don’t just hone their technical skills – we help them build the confidence and communication skills needed to navigate tough conversations with empathy and professionalism.
By equipping teams with the skills to manage complex imaging equipment, hospitals can maintain consistent service levels, reduce delays in equipment availability and provide patients with uninterrupted access to the care they need.
Ensuring hospitals have highly skilled professionals repairing and servicing critical medical equipment will always be our industry’s top priority. At the same time, hospitals are seeking cost-effective ways to manage support services, allowing them to redirect savings toward patient care. One expense is the reliance on OEM service contracts, which often prove burdensome for health systems challenged with reducing costs.
These contracts can cost healthcare organizations millions of dollars annually. Some original equipment manufacturers charge nearly $1,000 per hour, with labor costs for a single equipment repair ranging from $5,000 to $30,000 – or more.
By proactively investing in our most promising BMETs and guiding them into imaging roles, we’re tackling two of the healthcare industry’s most pressing challenges: reducing costs and addressing workforce challenges – without compromising service quality. This approach not only helps hospitals reduce reliance on costly OEM contracts but also minimizes equipment downtime, ensuring patients have quicker access to accurate imaging results. Reliable service delivery supports timely diagnoses and treatments, ultimately improving the patient experience.
Tapping into the talent within your existing workforce can play a critical role in addressing workforce challenges. Whether advancing into imaging roles or excelling in their current positions, BMETs can contribute significantly to maintaining high-quality care and supporting a more sustainable future for the healthcare industry.
— Eric Massey is a Regional Director of Operations for Crothall Healthcare. To learn more about joining the Crothall team, contact Eric at eric.massey@crothall.com.

BY DANIEL BOBINSKI EMOTIONAL INTELLIGENCE
Imagine a workplace in which employees regularly perform at high levels because they feel safe sharing bold ideas and voicing concerns without fear of retribution. Now imagine what happens when such a culture doesn’t exist. In such places, innovative solutions are left unspoken and conflicts linger unresolved. When that happens, it’s easy for teamwork to weaken.
At question: “What conditions are needed for high-performance teams to exist?”
One company decided to crack the code to answer this question. They spared no expense, nor did they rush their work. In 2012, Google launched Project Aristotle, an ambitious $80 million, multi-year study. Their goal? Discover why some teams are successful while others struggle.
Google’s research team analyzed over 180 teams across the company and conducted hundreds of interviews. What did they discover? Traditional metrics such as IQ scores, years of experience, or even resources available to a team mattered far less than one foundational element: psychological safety.
In essence, psychological safety is a shared belief among team members that their environment is safe for interpersonal risk-taking. It’s the freedom to say, “I might be wrong,” or, “I disagree,” without a fear of reprisals or judgment.
The differences were significant. People on teams with high psychological safety were 76% more likely to share ideas, delivered 40% higher performance outcomes, and were 47% more likely to stay with the company. These findings should make CEOs and business leaders in all industries sit up and take notice.
In addition to psychological safety, Google’s researchers identified four additional dynamics that high-performing teams shared. Together, these five components can serve as a set of operating principles for leaders and organizations striving to create thriving teams. What follows is a brief overview of these five components.
Psychological Safety. As stated, this factor is the cornerstone of success. Team members need to feel safe to express themselves without fear of embarrassment or punishment. What Google also learned is that psychological safety doesn’t happen by accident. It’s built through deliberate actions by team leaders, who play a pivotal role by modeling vulnerability, such as admitting mistakes or acknowledging their own uncertainties.
The researchers found that humility is a key factor, and that small things can have a big impact. A phrase such as, “I might be wrong, but …” or, “My research thus far leads me to believe that …” lets other team members know that the leaders don’t think of themselves as infallible. In other words, effective team leaders let others see it’s OK to be human.
Another factor in creating psychological safety is called “conversational turn-taking.” It means people don’t let their teams be dominated by only a few voices. Instead, team members practice active listening and equal participation in team meetings is encouraged.
Dependability. Project Aristotle also found that teams excel when members reliably complete their tasks on time and meet expectations. That said, dependability isn’t just about meeting deadlines, it means creating a culture of accountability. Clear

expectations are established, and team members hold each other accountable for their commitments.
Bringing this component to reality could involve implementing a performance management system or leveraging tools such as work dashboards to keep everyone aligned.
Structure and Clarity. In addition to dependability, teams are more likely to thrive when their members have clearly defined roles, goals and plans. This means leaders must take the time to ensure team members know how their roles and goals support team objectives and how their work helps create a bigger picture. Without these in place, teams risk miscommunication, inefficiency, and reduced engagement, leading to subpar performance.
Interestingly, team members who are confident of their roles and understand their team’s objectives also feel more secure in their psychological safety.
Meaning. We’ve already stated that team members engage more when they know how their work aligns with their organization’s bigger picture, but they also engage more when they understand how their work aligns with their personal values.
This means team leaders need to connect with team members individually to learn what drives each person. It means looking past the paycheck. Some people are driven by helping others. Others are driven by gaining new knowledge. Some are driven by developing systems while others are driven by creating beneficial surroundings. Additional internal motivators exist, so it’s wise for team leaders to become students of the different motivators so they can connect individual employees with the team’s overarching goals.
That said, a straightforward technique is for leaders to ask questions such as “What about this work excites you?” or “How do you see this project contributing to your personal growth?”
Impact. Lastly, Project Aristotle found that teams are much more likely to perform better when members can see tangible
results from their work. Leaders can foster this by celebrating milestones, sharing client feedback, or highlighting the broader impact of a team’s efforts.
Additionally, by recognizing individual contributions, leaders reinforce the idea that individual efforts matter.
The joy of Project Aristotle is that the findings resonate far beyond Google. Implementing these five components into your teams can transform how your workplace functions, no matter the industry.
Just know that these five components don’t make teams cohesively warm and fuzzy; they make teams more effective. Project Aristotle found that teams operating strongly with these five principles experienced more conflicts than low-performing teams. The difference was that the high-performing teams had the tools to resolve conflicts quickly and thus move forward productively.
Finally, Google’s data also revealed that small changes lead to significant improvements. For example, implementing simple practices like starting team huddles with personal updates or acknowledging contributions led to a 23% improvement in team effectiveness within weeks.
With this information, perhaps it’s time for some key questions. Are you fostering psychological safety? Are roles and goals clear? Do your team members see meaning and impact in their work? Remember, teams with these five components in place delivered 40% higher performance outcomes than teams in which these components were missing. What can your teams do differently or better? •
— Daniel Bobinski, who has a doctorate in theology, is a bestselling author and a popular speaker at conferences and retreats. For more than 30 years he’s been working with teams and individuals (1:1 coaching) to help them achieve excellence. He was also teaching Emotional Intelligence since before it was a thing. Reach him by email at DanielBobinski@protonmail.com or 208-649-6400.

BY FAMILY FEATURES
The same risk factors that contribute to making heart disease the leading cause of death worldwide also impact the rising global prevalence of brain disease, including stroke, Alzheimer’s disease and dementia. The global death rate from Alzheimer’s disease and other dementias is increasing even more than the rate of heart disease death, according to the American Heart Association’s Heart Disease and Stroke Statistics 2022 Update.
Globally, more than 54 million people had Alzheimer’s disease and other dementias in 2020, a 37% increase since 2010 and 144% increase over the past 30 years (1990-2020). Additionally, more than 1.89 million deaths were attributed to Alzheimer’s disease and other dementias worldwide
in 2020, compared to nearly 9 million deaths from heart disease.
“The global rate of brain disease is quickly outpacing heart disease,” said Mitchell S.V. Elkind, M.D. M.S., FAHA, the past president of the American Heart Association (202021), a professor of neurology and epidemiology at Columbia University’s Vagelos College of Physicians and Surgeons and attending neurologist at New York-Presbyterian/Columbia University Irving Medical Center. “We are learning more about how some types of dementia are related to aging, and how some types are due to poor vascular health. It’s becoming more evident that reducing vascular disease risk factors can make a real difference in helping people live longer, healthier lives, free of heart disease and brain disease.”
According to the statistics update, people with midlife hypertension were five times more likely to experience impairment on global cognition and about twice as likely to experience reduced executive function, dementia and Alzheimer’s disease. The risk for dementia associated with heart failure was nearly two-fold.
Experts recommend maintaining a healthy weight, managing your blood pressure and following other hearthealthy lifestyle behaviors that can also support good brain health while studies show maintaining good vascular health is associated with healthy aging and retained cognitive function.
Optimal brain health includes the ability to perform tasks like movement, perception, learning and memory, communication, problem solving, judgment, decision making and emotion. Cognitive decline and dementia are often seen following stroke or cerebrovascular disease and indicate a decline in brain health.
Consider these steps to live a healthier lifestyle and protect your heart and brain health:
• Don’t smoke; avoid secondhand smoke.
• Reach and maintain a healthy weight. Be mindful of your eating habits; eat foods low in saturated fat, trans fat, sodium and added sugars.
• Be physically active. Start slowly and build up to at least 150 minutes of moderate physical activity (such as brisk walking) each week. As an alternative, you can do 75

Exceptional Value
Impressive Warranty


minutes of vigorous physical activity, or a combination of the two, to improve overall cardiovascular health.
• Get your blood pressure checked regularly and work with your health care team to manage it if it’s high.
• Have regular medical checkups and take your medicine as directed.
• Decrease your stress level and seek emotional support when needed.
Learn more about the relationship between heart health and brain health at heart.org. •
• One-year-old company with 67 years of experience manufacturing and supplying X-ray tubes.
• High-quality components from IAE SpA, Europe’s premium X-ray tube manufacturer for 75 years.
Made in the USA with US and European components.
For a product list and prices contact us at:
Email: info@X-RayAmerica.com
Phone: 1.854.999.6888
Global: IAE.it
US Headquarters: X-RayAmerica.com



















ACROSS
1 Impenetrable by x-rays or any other form of radiation
7 X-ray unit
8 Aka radionuclide scanning
10 Price tag
12 Test measuring the electrical activity of the heart, abbr.
14 Title holder
17 Current measurement
18 Primate
19 Chemical symbol for lead
20 Electrical resistance unit
21 Occurring every year
23 Additional amount
25 One ___ million, 2 words
26 The study and treatment of neoplasms

“Anyone can hold the helm when the sea is calm.”
–
29 CAT, for one
31 “___ was saying ...”, 2 words
32 Put in a new equipment to take over from older machines
35 Make a purchase
37 Total amount
38 Hydroelectric project
39 Pressure measurement, abbr.
40 Organ that acts as a blood filter
DOWN
1 Gradual reclosing of an artery after it has been widened through angioplasty
2 Version of MRI that creates color pictures of the paths of nerve fibers in the white matter of the brain, abbr.
3 Condition of reduced bone mass
4 Severe pain in the chest caused by inadequate blood flow to the hear
5 Stars and stripes land
6 Narrow beams of light or other forms of radiation
7 Resistivity in physics
9 Computer
11 Set of facts and figures systematically displayed
13 Very high frequency form of magnetic radiation, 2 words
15 Environmental watchdog agency, abbr.
16 Kidney related
19 Keystone State, for short
22 One of the choices when considering aging equipment
24 Abbr. on a business letter
27 X-ray image intensifiers, 2 words
28 Single unit
30 Original equipment maker, abbr.
33 Friend
34 Metal container
36 Raise
PM Imaging Managment pmimagingmgmt.com • 213-276-8209
Radon Medical radonmedicalimaging.com • 866-723-6698
843-767-8090





































































































































































































































































































































































Kenneth Saltrick, President of Engineering Services in Twinsburg, Ohio, knows from his long experience that C-arm machines themselves are absolute workhorses.
For customers looking to blend the gap between expensive OEM and unreliable used assemblies, WE have your solution. Our complete repair contains a new cable assembly, utilizing all OEM cable and components with a harvested plate and connector housing as they are proprietary items. These completely repaired products will have a significant cost savings with build quality above new OEM products and carry a warranty of 180 days, which is untouchable in the market.

