






























































This column is a continuation of last month’s with more tips on how to be cyber-ready.
Revenue cycle management (RCM) is a vital element of practice management and an often-overlooked component of it.

This month’s Rising Star is Keck Medicine of USC/ Norris Cancer Center of USC Manager of Imaging Services, Serage M. Rahima.



Catch up on the latest news from around the diagnostic imaging world.



A look at some of the top POCUS and mobile ultrasound imaging devices available in the United States.
Intangible skills, such as emotional intelligence, are important for everyone, but especially for managers and leaders.




Matthew A. Mauro, M.D., was named president of the Radiological Society of North America (RSNA) Board of Directors in November at the 2023 annual meeting.
Mauro is president of University of North Carolina (UNC) Faculty Physicians and senior physician executive of UNC Health Care System Revenue Cycle. He is the James H. Scatliff Distinguished Professor of Radiology, as well as a professor of surgery at the UNC School of Medicine in Chapel Hill. He has been a faculty member at UNC since 1982.
Mauro received his medical degree in 1977 from Cornell University Medical College in New York. He completed his residency training in 1980 at the UNC School of Medicine and was chief resident during his last year. Between 1980 and
1982, Mauro completed fellowships in diagnostic and vascular radiology at UNC and abdominal and interventional radiology at the Mallinckrodt Institute of Radiology at the Washington University School of Medicine in St. Louis.
As RSNA president, Mauro will support RSNA’s mission by shepherding the Society through the evolving health care landscape and advancing the field of radiology through dissemination of high-quality research and education.
“The health care landscape is rapidly changing as we enter our post-pandemic environment,” Mauro said. “In addition to technical and scientific advances, we can anticipate changes to our health care delivery systems, labor management and patient expectations. The RSNA will maintain our position as the great convener for all those who interact with our

members to advance the fields of diagnostic radiology, interventional radiology, radiation oncology and medical physics. I am honored to have the privilege of serving as president of the RSNA.”
A prolific researcher, Mauro has published over 150 journal articles and numerous book chapters. He has co-authored five books. His textbook, “Image-Guided Interventions,” serves as a standard reference in the field. Mauro has given dozens of scientific research presentations nationally and internationally and has been an invited lecturer or visiting professor at over 200 institutions and meetings worldwide. He has served as principal or co-investigator on numerous funded grants, including several grants focused on diagnostic atherosclerosis imaging and treatment of complex pathology of the descending thoracic aorta.
A dedicated RSNA volunteer, Mauro served on the Scientific Program Committee beginning in 2005, and as chair from 2009 to 2013. He served on the Public Information Advisors Network from 2002 to 2011. Mauro is a regular faculty member for annual meeting
educational courses and was the associate editor of Radiology from 2002 to 2007. He has served on the RSNA Research & Education (R&E) Foundation Public Relations Committee and the Corporate Giving Subcommittee, and as an R&E Foundation grant reviewer. He currently serves on the R&E Foundation’s Board of Directors. Mauro joined the RSNA Board of Directors in 2015, serving as Liaison for Education.
Mauro has worked extensively with the Society of Interventional Radiology (SIR), where he was on the board of directors from 1996 to 2000, serving as president during his last year. With SIR, he served on the Executive Council from 1994 to 2000 and from 2002 to 2006. He was on the Scientific Program Committee from 2000 to 2002, served on the Steering Committee for the World Conference on Interventional Oncology in 2005 and held many other positions between 1992 and 2006.
Mauro has served on a number of editorial boards, including Clinical Imaging, Applied Radiology, American Journal of Roentgenology and Seminars in Interventional Radiology, among others. He has
been a manuscript reviewer for several journals. Mauro has been a book reviewer for “Gastrointestinal Radiology,” “Journal of Vascular and Interventional Radiology,” “Investigative Radiology” and “Academic Radiology.”
Since 2020, Mauro has been the RSNA Representative to the Academy for Radiology & Biomedical Imaging Research Executive Committee. He was past president of the Southeastern Angiographic Society, where he served on the Board of Directors from 2012 to 2018. Mauro has served on the American Heart Association’s Scientific Sessions Program Committee, as well as the Executive Committee, and he served on the Board of Chancellors of the American College of Radiology from 2003 to 2009. At the American Board of Radiology (ABR), Mauro served on the Board of Governors from 2015 to 2018 and on the Executive Committee from 2013 to 2015. He was trustee from 2006 to 2015.
He was awarded the gold medal by SIR in 2014. The ABR has presented Mauro with both the Distinguished Service Award and the Lifetime Service Award. •
“The health care landscape is rapidly changing as we enter our post-pandemic environment” - MATTHEW A. MAURO
Making sense of a year’s worth of paperwork and clutter can take some serious time, especially as many people have been working from home more than normal, but getting organized can help you tackle home management tasks more efficiently. Making the office a priority can reduce frustration when it comes to spending additional time in your office while working from home.

These five tips can help get you started:
1. Make sure you have furniture that can adequately store your stuff, including plenty of space for files, reference books and computer equipment. Pieces need not be costly to be functional and there are plenty of attractive options available online and at both small and major retailers.
2. Arrange the space with its intended use and your own work style in mind. For example, if you don’t need ample space to spread out over a large, flat work area, eliminate that space – it’s simply an invitation for clutter.
3. Place items you rely on frequently, such as a
calculator or ruler, within arm’s reach so they can easily be put away between uses. Capture these items in containers and bins to keep the space looking neat and free of clutter.
4. Establish a filing system that lets you keep track of important papers you need to keep of and have a shredder handy to help you discard any sensitive documents. Whether you alphabetize, color code or use some other method, group paperwork into segments for categories for easy access in the future.
5. Tangled cords can make even the most organized spaces look messy, and they may pose a fire or tripping hazard. Get control of your cords by storing devices you don’t use regularly and securing the remaining cords with twist ties or clips. Remember to use a surge-protected power strip to minimize the chance of damage should a power surge occur.
Find more tips to make your workspace tidy and organized at eLivingtoday.com. •
Share your RAD IDEA via an email to editor@mdpublishing.com.



Come experience everything Arizona and Colorado have to offer. Life doesn’t get much better than 300 days of sunshine, hiking, biking, lakes, rivers, and so much more. We invite you to our out patient imaging centers where your feedback and life work balance are valued.






apply today at bannerhealth.com/careers

This month’s Rising Star is Keck Medicine of USC/Norris Cancer Center of USC Manager of Imaging Services Serage M. Rahima, ARMRIT, LEAN Six Sigma Yellow Belt, CRA. He earned a Bachelor of Arts from Governors State University and is pursuing an EMHA at USC Sol Price School of Public Policy.

ICE Magazine recently found out more about this future leader.
Q: WHERE DID YOU GROW UP?
A: I was born and raised in Chicago, Illinois, and moved to Southern California in 2018
Q: WHERE DID YOU RECEIVE YOUR IMAGING TRAINING/EDUCATION?
A: I am a certified MRI technologist by ARMRIT and went to Aquarius School of Science in Des Plaines, Illinois, and most recently I have also earned my Certified Radiology Administrator (CRA) from AHRA.
Q: HOW DID YOU FIRST DECIDE TO START WORKING IN IMAGING?
A: My father was diagnosed with Stage 4 colon cancer in 2009. At the time, I was in retail and my father was hoping all of his children would pursue something in the field of medicine. I saw how big of a role imaging played in his care and treatment and I told him that I would pursue a path in radiology. My father passed away two
Serage M. Rahima is a manager of imaging services who hopes to one day earn an AHRA Fellowship and become a director of imaging.
days after the start of my radiology program. My final promise to him was that I would finish what I started and leave a legacy.
Q: WHY DID YOU CHOOSE TO GET INTO THIS FIELD?
A: Radiology is personal to me. Throughout my father’s battle with cancer, I was very fortunate to witness him being cared for by some of the most compassionate and dedicated health care professionals. It resonated with me and inspired me. I saw how much of an impact even the simple things like a smile or kind greeting had on somebody like my father who was fighting for his life. I wanted to have that same kind of effect on patients. It has shaped how I view every single one of my patients … like they are my family. I treat and care for them in the same manner that I wanted him to be treated.
Q: WHAT DO YOU LIKE MOST ABOUT YOUR POSITION?
A: As a manager, I love being a team leader and having my staff enjoy what they do. I value each and every one of their efforts and contributions and I never let them forget that. My staff know that I am always available for them. I always tell them that I view them as my co-workers who work with me and not for me. I need to do my part as a leader to help and support them in any way I can. I am truly humbled and blessed to be in my position. I also love interacting with our patients and being able to bring a smile to their faces whenever possible. Like I said, radiology is personal to me, so any time I can impact a patient’s day in a positive way, I live for those moments. It’s such a gratifying feeling when they share how your kindness has helped them through some of the darkest and scariest times of their lives.
Q: WHAT INTERESTS YOU THE MOST ABOUT THE IMAGING FIELD?
A: I am amazed at how far imaging technology has come and now with developments like artificial intelligence that allows for automatic detection and immediate notification of abnormalities, it’s going to allow providers to treat patients faster and save more lives.
participating in creating an MRI protocol for non-conditional pacemakers. These are patients who otherwise would not have been able to have an MRI due to the nature of their device being incapable of being imaged safely in an MRI scanner. We worked with EP cardiology, the MRI guru himself Frank Shellock and our renowned radiologists to create a program and protocol to allow these patients to have an MRI safely under the supervision of cardiology. It has impacted the quality of care for so many of our patients.
Q: WHAT GOALS DO YOU HAVE FOR YOURSELF IN THE NEXT 5 YEARS?
A: After I complete my Masters of Executive Health Administration, I am hoping to earn my fellowship from AHRA and one day be a director of imaging if the opportunity presents itself. •
FAVORITE HOBBY:
Q:
A: I have had the privilege of working alongside some of the brightest minds in medicine at Keck Medicine of USC. If I had to choose one, I would say it was
As the vice president of community health equity at the UAB Health System in Birmingham, Alabama, Verlon Salley spends his days assessing and managing health equity concerns, and working to address disparities in clinical data and processes within the system.
But long before he rose to his current position in one of the most prominent academic medical systems in the state of Alabama, Salley was trying to work his way up through a long line of pit bosses and barbecue chefs within the crowded ranks of the family cook-outs.
Growing up in South Florida, Salley’s childhood was punctuated by weekly get-togethers that, for the size of his family, could have doubled as reunions. His parents grew up on the same street in households of 11 children each, and Sunday was reserved for whole-family gatherings.
“It was such a big family and there were so many grill masters – and some who thought they were grill masters – that we used to have contests,” Salley said. “Bring your best meat and cook it on the grill. I was nowhere near the top 10 of people who could get on the grill, so I was like, ‘Let me create something that has my presence on the grill.’ ”
Salley’s contribution to that careful hierarchy became a sweet and spicy dry rub that landed especially well with his Uncle Carl, who encouraged him to develop it into an all-purpose sauce. His aunt, who’d
worked in a high-school cafeteria, told him about how the cooks there made their own barbecue sauce from scratch. To that basic recipe, Salley incorporated influences from his own culinary experiences, and blended them into a balance that keeps the flavors from overpowering one other. He purchases his spices in bulk and prepares his sauce in a commercial kitchen near his home.
“My recipe comes from my family and people who helped me,” he said. “Every place I’ve been had an influence of food. In South Florida, barbecue is big, so there’s cumin. Caribbean people are big in South Florida, so that’s where the curry comes in; and then there’s spicy flavors. And for me, cinnamon was the only spice that I liked personally that brought out the flavor in every other spice.”
After experimenting with his recipe and soliciting feedback from some family members, Uncle Carl more than any of them offered useful insight into how to dial in the flavors, and became the namesake for the sauce. Salley put his image on the label, called it Uncle Carl’s All-Purpose Sauce, and for the next decade-and-a-half, gave away “probably thousands of bottles of sauce.”

“I’ve never advertised it,” he said. “It’s just a wordof-mouth thing; it’s not in stores.”
As an all-purpose sauce, Salley’s product was meant to be used by chefs preparing many different kinds of dishes, be they poultry, beef, pork or vegetables. It worked equally as well for Uncle Carl’s smoked turkey as it did for cousin Shawn’s ribs and pork shoulders.
“The sauce is good on everything,” Salley said. “I’ve
got a friend, Luz Randolph, who uses it on tofu, and another friend Arlisa Welch, who uses it on salads. My favorite is ribs, but it’s crazy how this sauce goes on any and every meat. I’ve never had anyone say they didn’t like it. Everything’s inspected, pH-balanced and tested.”
When the novel coronavirus (COVID-19) pandemic hit in 2020, things slowed down enough at work that Salley had the time to create an LLC and begin establishing Salley’s Sauces as a formal business. He researched food production and safety regulations, nutrition labels and trademarking. Friends worked with him on the label, advised him on the business, and have watched him grow the concept to its current form.
The first snag he hit in his trademark application came from fastfood chain restaurant Carl’s Jr., who challenged his use of the name Carl under its current spelling. Instead of spending his seed money in a
protracted legal battle, Salley added his own nickname to the label, and the product became Big Sal’s Sauce. Fortunately, none of the conversation about his naming conventions affected the composition of the sauce.
“I didn’t realize what this business was going to entail, but because I’m an executive, it didn’t faze me to jump through those hoops,” he said. “All those checks and balances that you learn being an executive, I’ve put that into this business.”
“The sauce has been perfected since 2007; it hasn’t changed at all,” Salley said. “What’s now about to take off is actually selling it outside of being online.”
Now that he’s supported his time-tested recipes with executive knowhow and a business and marketing plan, Salley is poised to field-test the business offline in 2023, bringing his products to farmers markets and festivals near
his Birmingham home, and seeing how far he can take it. His fervent wish is to establish his sauce business as a family-based business with which to establish a foothold in the market for his son to grow it in the future, should he choose to do so.

“I want to keep it solely proprietary, where my family does everything,” Salley said. “I would love to be able to pass this to my son. It would be up to him to take it wherever. I want this to be his vehicle and enhance his life; it could be his platform where he starts at a higher place than I did going into my college career.”
Whatever form the business takes – and regardless of the name on the bottle – Salley is confident that the time-tested recipe behind his sauces will continue to endure.
For more information about Verlon Salley’s homemade sauces, visit salleysauces.com. •





For the first time ever, the Imaging Conference & Expo (ICE) exhibit hall is sold out. Foyer booths remain available for companies wishing to reach the unique audience of dedicated imaging leaders.
It is an exciting time as more and more people are aware of the ICE community just as the COVID-19 pandemic has reached a point where in-person conferences are available.
The ICE 2023 Imaging Conference & Expo that is to run February 18-19, 2023, has been approved for 1.5 CEU credits upon completion of the course only. The CRES Study Group 2023 (Part I & II) that is to run February 17-18, 2023, has been approved for 7.5 CEU credits upon completion of the course only.
Registration is now open for ICE 2023. It is set for February 17-19 in Music City inside the recently renovated Renaissance Nashville Hotel. Registration – including free registration for hospital employees, students and active military – is available online at AttendICE.com. Walk-up registration will begin at noon on Friday, February 17, 2023, onsite at the Renaissance Nashville Hotel.

ICE is the only conference dedicated to imaging directors, radiology administrators and imaging engineers from hospital imaging departments, freestanding imaging centers and group practices. The first day of educational sessions kicks off on Saturday morning. Attendees can add to their knowledge while leading companies from throughout the nation set up their booths in the exhibit hall.
An ICE Break from noon to 1 p.m. gives everyone a
chance to stretch their legs before the afternoon educational sessions followed by the Exhibit Hall Grand Opening and Welcome Reception at 4:30 p.m. On Sunday, the classes start a little earlier with the first sessions set for 9 a.m. followed by an 11 a.m. round of classes. The exhibit hall will be open for two hours beginning at 12:30 p.m. with a free lunch served inside the hall.
Super Sessions cap off the educational offerings. The 90-minute presentations begin at 2:30 p.m. Everyone is invited to attend the Finale Party after the Super Sessions. This is an opportunity to celebrate the industry, catch up with friends and colleagues while also making new connections. ICE offers valuable CE credits and, keeping in line with successful conferences in the past, offers comprehensive educational opportunities for attendees.
Whether it’s invaluable continuing education, productive networking or the exclusive exhibit hall, attendees will have the perfect opportunity to enhance their careers and spend time with colleagues. As an added incentive, ICE conference admission is complimentary for all health care professionals, active members of the military and students.
ICE 2023 also features a CRES Study Group and Prep Class for an additional fee. The first session is Friday, August 17 from 1-5 p.m. The second session is slated for Saturday, February 18 from 8 a.m. to noon. • For more information, visit AttendICE.com.
FEBRUARY 17-19, 2023 • NASHVILLE, TNResearchers at the University of Wisconsin-Madison, the first U.S. clinical evaluation site for GE Healthcare’s industry-first silicon-based photon counting CTi, will begin human scanning using the device, which is engineered with Deep Silicon detectors with the goal of greatly enhancing imaging capabilities to help clinicians improve patient outcomes across oncology, cardiology, neurology and other clinical CT applications.
The collaboration comes nearly one year after GE Healthcare announced its first clinical evaluation site at Karolinska Institute and MedTechLabs in Sweden. Since then, the company has made rapid progress in enhancing the developing technology, building a new system prototype to include:
• A larger detector with the possible goal of enabling quicker scan times as well as expanding coverage;
of current indications by combining refined energy resolved data, high spatial resolution, reduced noise and improved soft tissue contrast. We are working with GE Healthcare by testing their novel photon counting solutions in human subjects to assess issues ranging from improving commonly encountered CT image quality limitations to evaluating whether previously out of reach clinical questions can now feasibly be answered.”
Photon counting CT could potentially advance the capabilities of CT, including the visualization of minute details of organ structures, improved tissue characterization, more accurate material density measurement (or quantification) and lower radiation dose.
• ECG-gated cardiac scan capabilities designed for coronary artery imaging; and
• Faster acquisition speed with the intent to reduce the likelihood of blurred images due to motion.
“Photon counting CT has promise to embody the best of CT imaging available to date,” explains Dr. Meghan G. Lubner, professor of radiology at the UW School of Medicine and Public Health. “This technology has the potential to expand the scope
GE Healthcare is pursuing a unique approach to photon counting CT, which may enable higher spatial and spectral resolution at the same time, thanks to several advantages provided by Deep Silicon detectors, including: the detector’s material purity, innovative geometric design, and true multi-bin technologies for high performance spectral imaging. As such, the research being done at UW-Madison will assist GE Healthcare in better understanding the heights of these unique capabilities. •
For more information, visit gehealthcare.com.

FUJIFILM Healthcare Americas Corporation recently announced the U.S. launch of the SCENARIA View Focus Edition Computed Tomography (CT) system, a premium scanner with an advanced Cardiac Motion Correction feature, called Cardio StillShot. The system is designed for routine and advanced clinical applications, including coronary computed tomography angiography (CCTA), interventional CT, extended coverage shuttle scanning for perfusion exams, and dual energy examinations. The system was showcased for the first time at the 2022 Radiological Society of North America (RSNA) annual meeting.
Fujifilm’s Cardio StillShot feature helps clinicians capture clear images of the heart – even on the most challenging heart rhythms by simultaneously acquiring two data sets in the scan. These data sets are then compared against each other to detect and correct motion. The final images have an effective temporal resolution of just 28 milliseconds, compared to 175 milliseconds
without Cardio StillShot.
“Providers need a powerful CT system that gives them the diagnostic confidence to make the right treatment decisions for their patients,” said Mark Silverman, director of marketing for CT, FUJIFILM Healthcare Americas Corporation. “Fujifilm’s SCENARIA View Focus Edition makes this possible through the convergence of high temporal resolution, enhanced workflow that reduce examination time, and advanced dose reduction capabilities.”
Fujifilm received FDA clearance for the SCENARIA View Focus Edition in April 2022. •

Canadian manufacturer KA Imaging is introduced its first mobile X-ray system at the 2022 RSNA meeting. The Reveal Mobi Lite is an integrated solution powered by patented SpectralDR technology, which makes is the world’s first mobile system with dual-energy capabilities.
Powered by the company’s patented SpectralDR technology, the Reveal Mobi Lite operates with the Reveal 35C detector, which is also sold as a retrofit solution. KA Imaging’s SpectralDR technology enables dual-energy subtraction, providing bone and tissue differentiation with a single standard X-ray exposure. It acquires three images simultaneously (DR, bone and soft tissue dual-energy X-ray images). The technology reduces patient dose due to the industry leading DQE of the Reveal 35C detector, and uses identical clinical techniques associated with state-of-the-art mobile DR X-ray, without disrupting existing workflows.
“Point-of-care X-ray has now changed forever because SpectralDR improves outcomes anywhere it is required,” said Amol Karnick, president and CEO of KA Imaging. The subtracted images aid the visualization of a number of conditions, including lung nodules, pneumonia, pnemothorax, confirming tips of lines and tubes, foreign surgical objects, visualing lateral spine and even coronary calcium.
Currently, the Reveal 35C is FDA cleared and available for sale in the United States of America. The Reveal Mobi Lite is not available for sale. •
Konica Minolta Healthcare Americas Inc. introduced its next-generation, compact point-of-care ultrasound system (POCUS), SONIMAGE MX1 Platinum, delivering incredible detail resolution for superior image quality. Clinicians can hand carry the SONIMAGE MX1 Platinum System wherever it is needed most – at the bedside, in an exam room or surgery suite. Konica Minolta introduced the new system at the 2022 Annual Meeting of the Radiological Society of North America (RSNA).
The MX1 Platinum System leverages an advanced imaging algorithm that achieves improved resolution of ultrasound images while maintaining optimum frame rates. This algorithm improves image quality of the color and grayscale modes, delivering speckle reduction and applying a smoothing effect to reduce graininess in the image. The exceptional image quality at the point-of-care can help clinicians make better informed diagnoses and facilitate accurate interventions, giving them confidence in what they are seeing to make immediate decisions that enhance patient care.

Also new is an extended battery life that enables a continuous two-hour scan time, so the MX1 Platinum System can be carried throughout the hospital or clinic without requiring a re-charge. A full suite of transducers is available
with MX1 Platinum System, including the L18-4 and HL184 wide-band frequency linear probes for musculoskeletal (MSK) and general imaging exams. The S4-2 phased array enables quick scans of the heart in perioperative situations, which allows clinicians to assess the patient pre- and post-surgery.
The combination of excellent image quality, powerful transducers and Konica Minolta’s Simple Needle Visualization (SNV) make the MX1 Platinum System an ideal POCUS unit for interventions. SNV highlights the advancing needle for greater visibility of the needle tip, shaft and injectate for more confident interventions or biologic injections. •
Advanced Veterinary Ultrasound (AVU), a division of Advanced Ultrasound Systems, and Draminski S.A., a manufacturer of quality point of care ultrasound (POCUS), have partnered to provide superb, feature-rich systems to the veterinary market, according to a news release. AVU is a leading provider of veterinary ultrasound equipment, probes, service and applications training.
Through the agreement, AVU is authorized to market, sell and service the line of portable ultrasound systems Draminski offers such as the Draminski Blue, iScan2 and iScan Mini systems.
“We are dedicated to advancing veterinarians and their businesses through excellent imaging products and services. Our partnership with Draminski enables us to offer outstanding veterinary ultrasound,” stated John Hryshchuk, president and CEO of AVU. “We are uniquely
positioned to be a veterinarian’s only ultrasound contact throughout the life of the product – we provide multibrand choices, the expertise to assist in the decision, the training for veterinary staff, technical support, service and after-warranty needs. We follow the practice as their complete care ultrasound vendor.”
Veterinary practices worldwide utilize ultrasound as their principle point-of-care imaging technology due to its portability as well as its non-invasive, non-radioactive, low-cost characteristics.
The AVU-Draminski veterinary solution delivers superior diagnostic imaging while providing empowerment through AVU’s expertise. AVU assists clients on a consultative level, matching technology with practice needs, helping clients through training, asset assessments and maintenance strategies. In this way, each AVU customer can attain the highest return for their investment. •
Radiaction Medical Ltd. has received an additional 510(k) clearance from the Food and Drug Administration (FDA) for its Radiation Shielding System, one that enables compatibility with the Siemens Artis family of fluoroscopy C-Arm machines.

The Shield System functions as an accessory to new and legacy C-arm models. Since its market debut in Spring 2022, the Radiaction Shield System stands alone as the only fully automated and integrated, head-to-toe shielding device that blocks radiation scatter at its source. Building upon its previous clearance with Toshiba Infinix-I systems, this latest authorization permits the Shield System to be used in a greater number of interventional cardiology and electrophysiology labs across the United States, expanding the availability of Radiaction’s potentially life-saving radiation shield to yet more physicians and staff.
Fluoroscopy-guided procedures have become a leading
source of occupational ionizing radiation exposure for health care providers. Currently available radiation protection solutions have limitations – leaving gaps in full body coverage, providing reduced protection to staff, and creating obstructions that can limit access to the patient. Radiaction’s technology blocks the threat of radiation exposure and eliminates these limitations. Clinical studies have shown that the Shield System can reduce radiation scatter to the entire interventional lab by over 90%, with even higher reductions to the heads and upper bodies of the treating physicians. •
GE Healthcare has announced an agreement with ulrich medical for a GE Healthcare branded contrast media injector in the U.S. The CT motion multi-dose syringeless injector, which delivers iodinated contrast media for computed tomography (CT) imaging procedures, reduces procedure setup time and increases patient throughput by eliminating time consuming preparation steps, while helping to optimize patient dosing and reduce wasted contrast media.

Recent research, led by Dushyant Sahani MD, professor and chair of radiology at the University of Washington and presented at the 2022 Radiological Society of North America (RSNA) Congress, demonstrates that when compared to a typical dual-syringe based injector using single or multi-dose vials, the CT motion may enable six additional patient CT exams each day in a busy emergency department, with up to three minutes saved per patient. The research, which analyzed over 6,000 patients who received Contrast Enhanced CT or CT Angiography, also shows CT Motion reduces cost from consumables and saves an average 30 mL of contrast per procedure.. •

The Medical Imaging & Technology Alliance (MITA) announced that GE Healthcare’s Jay Hill, chief technology officer, molecular imaging and computed tomography, will serve as MITA Board Chairman beginning January 1, 2023. Hill will succeed Michael Wendt, senior vice president of customer services, Siemens Healthineers, who will continue serving on the Board.
“It’s an honor to be elected Chair of MITA’s Board of Directors, and I’m looking forward to working with my colleagues to further demonstrate medical imaging’s unique value proposition to patient health,” Hill said. “Medical imaging technology – and the role of the people who invent
and maintain sophisticated equipment – are catalysts for better health care in our nation’s health care system. I’m proud to help lead MITA efforts as an advocate for this vital sector.”
“A key aspect of MITA policy effectiveness is member leadership and engagement,” said Patrick Hope, MITA executive director. “On behalf of the association and all its members, we extend a heartfelt thank you to Michael Wendt for his service and welcome incoming chairman Jay Hill. With a new Congress, we are eager to continue to advocate for policies bring value to patients and providers by supporting medical imaging.” •
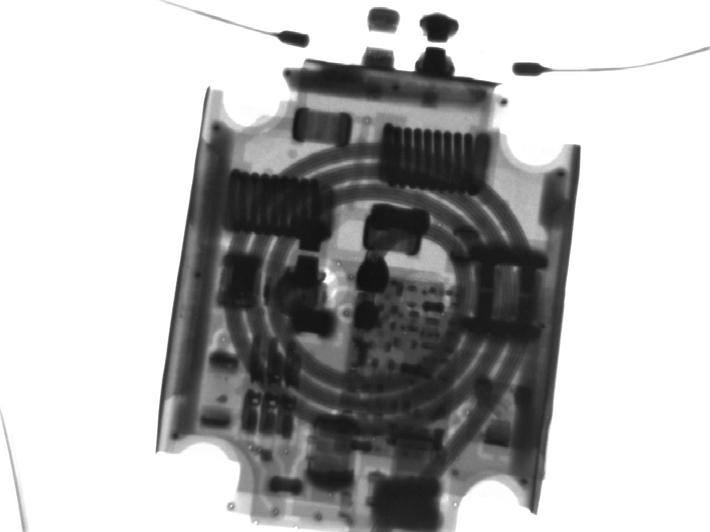
NeuroLogica Corp., a subsidiary of Samsung Electronics Co. Ltd., announced that its head-to-toe trauma imaging solution, the BodyTom 64 Point-of-Care Mobile Computed Tomography (CT) Scanner, has received 510(k) clearance from the U.S. Food and Drug Administration for commercial use in the United States.
“We’re thrilled to build off our expertise and elevate pointof-care imaging with our BodyTom 64, which can transform any room in a hospital into an advanced imaging suite,” said Jason Koshnitsky, senior director of global sales and marketing of NeuroLogica. “This full-body 64-slice CT scanner is an upgraded version of the BodyTom Elite CT scanner, providing enhanced functionality with the same high-resolution imaging capabilities.”
Based on customer feedback, the company designed the BodyTom 64 to enhance the user experience and improve clinical workflows through revisions to the software and the data acquisition system (DAS). Such revisions include incorporating Linux as the operating system and having the ability to generate up to 64 cross-sectional CT images of a patient’s body, versus the 32 images produced by the predicate BodyTom Elite.
With indications for pediatric and adult imaging, the BodyTom 64 is a multi-departmental imaging solution that can be utilized for various needs. •
For more information, visit NeuroLogica.com.
Block Imaging has announced the completion of CT tube repair and reload capabilities within their Block Imaging West facility in Ranch Cordova, California. The launch of this depot builds on its acquisition of Varex Imaging’s RHIT facility in 2021. Throughout the last year, Block Imaging has transformed the facility into a harvesting, component repair and forward stocking operation. The addition of the CT tube repair and reloading is just one of many ways the company plans to utilize the facility to expand and enhance services to the imaging industry.
Block Imaging President Jason Crawford remarked, “Our Block Imaging West facility has allowed us to provide West Coast customers with superior service due to its location. With the launch of CT tube repair and reloading as well as CT high voltage tank repair, we can provide additional value to health care providers everywhere. These services significantly drive down the total cost of ownership for CT assets as they mature by providing options for lower cost on-going maintenance.”
Block Imaging’s first replacement CT tubes will be for




the GE MX200 series CT tubes, used on certain models of GE’s Brightspeed, Discovery, Lightspeed, and Optima series CT systems. These tubes will also be compatible in fit, form, and function with the replacements manufactured by GE for the GE MX200 series, the Dunlee DA-200 series, the Varex MCS6074 model, and the Chronos AU200 series CT tubes.
Replacement CT tubes from Block Imaging will be fully repaired or reloaded and tested to OEM specifications. Reloaded models of the MX200 series CT tubes with new inserts will be available with a 12-month full replacement warranty. Repaired tubes will include a warranty commensurate with age and use.
“This exciting addition to Block Imaging’s capabilities represents years of experience and planning to establish the necessary processes to produce high-quality new and pre-owned CT tube housing assemblies. We are proud to be able to offer these services to our customers and look forward to the release of additional models and capabilities in the months to come.” Crawford added. •
The “Point-of-Care Ultrasound Device Market Research Report: By Type, Portability, Application - Global Industry Revenue Estimation and Demand Forecast to 2030” report has been added to ResearchAndMarkets.com’s offering.
The report states that the global point-of-care ultrasound devices market revenue is predicted to increase to $4.5 million by 2030 from $2.1 million in 2020, at a 7.9% CAGR between 2021 and 2030.

The COVID-19 impact on the point-of-care ultrasound devices market has been negative due to the closure of manufacturing facilities. Moreover, almost all the health care resources were diverted to the fight against the pandemic, which is why most diagnostic imaging facilities were shut down, except for COVID patients.
The diagnostic bifurcation held the larger share in the POCUS devices market, on the basis of type, in the past. Such devices are being increasingly utilized for evaluating left ventricular systolic function and diagnosing severe mitral regurgitation, pericardial effusion, pleural effusion, pulmonary edema, and pneumothorax.
In the coming years, the portability segment of the point-of-care ultrasound devices market will be dominated by the trolley/cart-based bifurcation. These devices find widespread usage in hospitals as they can be easily taken from one place to another, such
as between radiology departments and emergency rooms (ER).
The highest CAGR in the POCUS devices market, under the application segment, will likely be seen in the emergency medicine category. As shifting the patient from the ER to the ultrasound ward can result in loss of valuable time, portable ultrasound devices are being used at the bedside to obtain immediate clinical information, increase efficiency, improve patient safety and decrease the risk of complications.
Europe has generated the highest revenue in the point-of-care ultrasound devices market till now because of the increasing chronic disease incidence, health care expenditure, and geriatric population and rapid technological advancements in radiology. The UN says that the region’s geriatric population will increase from 140.4 million in 2019 to 199.9 million by 2050, thus driving the volume of ultrasound procedures.
The Asia-Pacific (APAC) will be the fastest-growing POCUS devices market in the years to come owing to the rising demand for point-of-care treatment and diagnosis, increasing health care expenditure, and surging cases of lifestyle-associated and chronic diseases. Moreover, the aging population in Asia is set to reach 954.6 million by 2050 from 395.3 million in 2019, says the UN.
Fortune Business Insights also predicts market growth.
The global point of care ultrasound market is expected to eclipse 14% CAGR from 2020 to 2026, according to Fortune Business Insights. •
Apollo’s Enterprise Imaging solution, the Apollo Repository for Clinical Content or arcc, supports encounters-based point of care ultrasound (POCUS) imaging workflows. This strategy contributes to the ability for POCUS procedure reimbursements as a revenue stream by centralizing the images in the patient record, thus improving documentation for reimbursement claims of these procedures. Using arcc streamlines POCUS image capture and improves patient care. There is no need to wait for an order – imaging can occur immediately during care. This saves physicians’ time, reduces steps during the care process and provides staff efficiency gains in addition to generating revenue.


The quiet and powerful DRX-Revolution Mobile X-ray System – which delivered the industry’s first collapsible column – recently celebrated 10 years of providing quality medical imaging at the bedside. This mobile X-ray system continues to boost productivity while providing radiographers with an advanced set of features, including a smaller, lighter tube head and collimator; redesigned, more responsive display screens; functional LED lighting; and optional in-bin charging. Like its initial design, these new enhancements are based on feedback from X-ray technologists, radiology administrators and physicians, paving the way for improved workflow, patient care and clinical outcomes.
The ARIETTA 750 ultrasound system’s advanced beamformer and host of automated workflow tools enable sonographers and surgeons alike to image all patients quickly and efficiently. The system’s innovative imaging techniques, including Detective Flow Imaging, Carving Imaging, and eFocusing, combine to provide high-resolution, high-SNR imaging at any depth without the need to adjust focal zones. The ARIETTA 750 has many advanced and unique probes that fully cover the expanding range of procedures that benefit from ultrasound guidance.

At a time when clinicians need quick insights at the point of care, Vscan Air, a wireless, pocket-sized ultrasound device, can provide crystal clear image quality, whole-body scanning capabilities and intuitive software – all in the palm of the clinician’s hand. The Vscan Air offers:

• Crystal clear images for confidence in what clinicians see, where they need it.
• Dual-probe enables whole-body scanning with the flip of the wireless dual probe (for deep and shallow scanning) and a push of a button to capture images.
• Portability without compromise via the power of a high-performance ultrasound machine in a lightweight, wireless, pocket-sized solution.
• Redefining the patient experience and access to ultrasound technology – involving patients by sharing real-time images and send images as simple as see, snap, send.
The SOMATOM On.site portable head computed tomography scanner from Siemens Healthineers brings point-of-care neuroimaging to intensive care unit (ICU) patients to avoid risky and time-consuming transports, reduce the risk of complications, and improve workforce efficiency and staff utilization. The unique telescopic gantry design allows the radiation source to move away from the patient during scanning, while the base and front cover of the gantry remain stationary, which helps provide consistent image quality. The easily maneuverable system has an integrated drive camera that enables real-time viewing on the built-in Touch UI display. The integrated head holder and shoulder board accessories allow convenient patient positioning. Scan workflow is easy with myExam Companion powered by GO technologies, zero-click post-processing, and automatic wireless image transfer to PACS. Self-shielded telescopic gantry covers combined with radiation shields on the bore’s front and back reduce scatter radiation and allow the technologist to remain with the patient during image acquisition.







The Radiology Equipment Technician I (RADT I) performs scheduled maintenance and builds a knowledge base of a variety of common medical imaging devices & systems at multiple locations. Examples of these imaging devices & systems are; Portable radiographic, portable fluoroscopy, radiographic unit digital and conventional, radiographic/fluoroscopic digital & conventional Ultrasound, etc.


At RENOVO, we value knowledge, reliability, and integrity in our employees. If you are interested in being a part of a team that is committed to making
MIS provides asset management solutions for hospitals and imaging institutions nationwide. We combine 20 years of service experience with the industry’s most advanced asset-management software, raising the bar in theindustry to manage the increasing demands placed on diagnostic operations. With our contract management program, we make everything



Canon Medical Systems USA, Inc., a world leader in diagnostic imaging, is in search of qualified can-


life. Our industry-leading commitment to quality and team of expert technicians helps ensure clinicians have access to patient-ready equipment needed for patient care. Make an impact in healthcare and grow your career with Team Agiliti!

Field Service EngineerNuclear Medicine



patients and their families? Do you enjoy a new challenge every day? If you are skilled at servicing medical equipment in a clinical setting, we hope you will join our team!


For as much thought as goes into providing optimal patient experiences in health care from the perspectives of health outcomes and quality of care, management of revenue streams seldom seems to enter the conversation. Yet for its importance not only to the bottom line of any clinical operation, but also for its impact on patient satisfaction and total quality of experience, revenue cycle management (RCM) is a vital element of practice management and an often-overlooked component of it.

In understanding the revenue cycle from a comprehensive perspective, Mario Pistilli, administrative director of imaging services at Children’s Hospital Los Angeles, said it’s important to recognize the breadth of patient and administrative experiences that RCM touches. It begins before a patient is ever seen, with the collection of demographic information, and concludes after services have been rendered, through final payment and disposition of the bill. However, before that bill is discharged, there are always opportunities for things to go sideways, and without clear understanding of how bills are being generated, and visibility into that process, any other efforts to improve RCM operations won’t take root.
In radiology departments, billing information might be an internalized component of a radiology information system (RIS), or it might originate from a separate process that’s managed independently. Such information will include identifying details about the patient, the procedures they’ve undergone – including the universal Current Procedural Terminology (CPT) code describing that service – and the time, place and provider related to it. When the process doesn’t go smoothly, then it’s a question of troubleshooting points of failure in the system, from missing documentation to mistyped data to incorrectly coded procedures. Any one of those issues can delay billing (and reimbursement), leading to the work of unpacking the process to see where it failed (or was failed by error). Sometimes those issues are on the coding side, sometimes they’re on the billing side, and sometimes they surface at another point along the way. But without knowing there’s a problem, issues can linger and persist until they’re impossible to ignore.
The way to address such concerns involves reporting processes that identify issues within the system – denials, missing documentation, coding errors – and what’s needed to resolve them regardless of the reason they emerge, Pistilli said. Implementing tracking metrics and a way to visualize and manage those data allows institutions to get a handle on RCM issues and how to resolve them. While automation and AI-powered processes can support some of that detective work, at some point, process improvement is reliant upon individual expertise to correct.
“I prefer to eliminate errors before I make them rather than spending this work, time, money, effort, to fix stuff after,” Pistilli said. “Let’s
get clean information in and a clean bill out the door in the first place. How do we stop that so we have less accounts to work on the back end? There’s process issues that the radiology director can control to really impact the revenue cycle, and it could be worth a lot of money,” he said.
Pistilli has dedicated one full-time employee exclusively to revenue cycle work, the better to identify any data trends before they hit reporting, as well as unpacking what might be behind them.
“I want to know why these things are in there, and not just fix the same problems month after month,” he said.
In some practice environments, intelligent revenue cycle automation and billing applications driven by artificial intelligence (AI) software offer an alternative to dedicating staff or management resources to investigating RCM issues. Amy Raymond, vice president of revenue cycle operations at healthcare AI developer AKASA of San Francisco, California, said that AI-powered RCM tools are no longer “nice-to-have technology” but have instead become “a mission-critical tool.”
“Many health systems and hospitals have already implemented automation and AI for their operations, or are looking to do so,” Raymond said.
According to an AKASA survey of nearly 400 CFOs and revenue cycle leaders at hospitals and health systems across the United States, some 78 percent of those polled “are currently using or are in the process of implementing automation in the revenue cycle,” she said.

Raymond reported that revenue cycle AI and automation processes are being sought to deal with “the most time-consuming, manual workflows,” including prior authorizations, claims denials, and to make up for staffing shortfalls. However, in order to successfully automate these processes, systems must be trained in which questions to ask and how to answer them.
“Just as a self-driving car can accel-
erate, brake, and turn based on what it encounters, revenue cycle automation solutions need to be capable of navigating complex workflows rife with edge cases and the unknown,” Raymond said. “This is why we believe in the power of automation combined with human experts in the loop as the way forward. When the system runs into a new challenge, it can flag down an RCM expert to complete the task in question, all while the automation watches and learns over time. This is a great way for revenue cycle departments to overcome the above-mentioned challenges and avoid common (human) errors that occur within the medical billing process.”
“If the system runs into outliers – for example, a payer changes requirements needed for a certain procedure without any heads up – rather than breaking or stopping work, our AI flags it to our revenue cycle experts, who resolve it in real-time while teaching the machines how to handle it correctly the next time it occurs,” Raymond said. “These more intelligent AI and machine learning solutions that leverage humans-in-the-loop, and can adapt to changes in real time with little to no maintenance, will be the future of revenue cycle automation.”
Raymond believes the future of automation in RCM will involve ever-tighter interrelationships between those AI-powered processes and human staffers with situational judgment and the expertise to appraise the circumstances of any issue in the cycle. As much as that evolution follows along with the cycle of technological development and process improvement, that relationship has also been driven increasingly by labor concerns brought on by the novel coronavirus (COVID-19) pandemic and the “Great Resignation” social trend that has followed it.
Some automated processes have been employed for a number of years, Raymond pointed out. These include robotic process automation (RPA), whereby a vendor-built bot (i.e., program) can be used to automate each step of a specific revenue cycle process; however, once those bots are constructed, they are often static, and can’t adapt to changes in things like payer portals or electronic healthcare records. AKASA seeks to distinguish itself from those fixed processes by leveraging AI and machine learning technologies supported by human revenue cycle experts to confront those shortfalls in the automation approach.
“The back office of health care is essential to keeping the doors of hospitals open by ensuring the bills are paid,” Raymond said “Yet, these revenue cycle teams were facing labor shortages like never before. COVID-19 has stretched hospitals and health care systems beyond the breaking point. And for all the new problems the pandemic has introduced, it has also shed a light on decades-old issues, where health care operations teams have historically been understaffed.”
The result of these circumstances has been that those staffers who have stuck with their roles have faced extra work and the burnout that come with it. On the management side, staffing issues have resulted in higher costs for overtime pay, retention bonuses, and hiring incentives, and not every health care institution is in a competitive posi-
tion to meet those financial challenges.
“Several factors, including volatile patient volumes, ballooning labor costs, and the ending of pandemic relief funding have squeezed hospitals,” Raymond said. “Days of cash on hand at not-for-profit hospital systems are trending downward as the sector recalibrates after last year’s higher-than-normal balances. For some, it requires tough choices to be made.”
“The prime directive from this landscape is leaders have to unearth every nook and cranny where there’s potential to lower operating expenses, and find any sources of revenue we can to get back on solid financial footing, while also looking for tools to alleviate the burden on staff,” she said.
“The hard truth of the revenue cycle is that no one ever touches everything,” Raymond said. “There isn’t enough time or staffing resources. What happens? Queues get deprioritized, denials aren’t appealed, accounts receivable gets increasingly aged, payments are delayed, and write-offs go up.”
Software automation offers the potential to address RCM issues while also freeing up staffers to address those projects for which their discretion, expertise and understanding is most required. In those instances where onsite staff (or budgets) aren’t available to manage some of those functions, health systems may consider outsourcing those roles to staff outside of the company. Sometimes, that strategy can lower costs or plug holes in the short term, but Raymond believes that after a while, RCM outsourcing can complicate in-house processes by being either more expensive or less responsive to change.
“Getting it right matters when you fully outsource revenue cycle operations,” Raymond said. “There’s a lot of expertise, context and operational knowledge that gets lost. This creates inefficiencies, so ultimately, the exercise can cause more pain than it solves. If you keep things in-house, and
layer on automation, all the savings trickle back to you.”
Getting to the root of RCM issues isn’t only meaningful for the financial health of a practice environment, but it can also affect whether its clients return to the same provider in the future. Sara Nofziger-Drew, client relations director for HealthPro Medical Billing of Lima, Ohio, said that when patients are confronted by surprise medical bills, or don’t understand for what they’re being billed, not only are they frustrated, but their confusion can make more work for the call center or billing environment, which can also impede the revenue cycle. At worst, it can turn a patient away from considering a given provider, hospital or practice group entirely.
“Whether the billing is sourced internally to the organization or outsourced, that process is vital to patient care, because that is often what people connect with at the end of their experience,” Nofziger-Drew said. “Patients are looking to see where they can be serviced the best. They are checking reviews, they are seeing what’s out there, and when a patient doesn’t have a positive ending experience, they’re going to look elsewhere.”
To alleviate those risks, NofzigerDrew said providers should work to
understand how much of an impact they can have on patient experience at the end of the appointment. Then, it becomes incumbent upon that billing department to ensure that patient has a positive experience through proper workflow, which can be compromised by a lack of oversight, potentially setting the patient up for a fight with their insurance provider, or the clinical office, or the billing department, or someone else.
“RCM is often the last interaction the patient has with anyone relating to their care,” Nofziger-Drew said. “If the patient has a great experience with their provider, but then billing doesn’t perform their duties well, it leaves a poor taste with the patient, and many times a patient will not come back to the same provider. Often patients and even providers don’t understand all of the steps involved to ensuring a service is billed appropriately and timely to the insurance company and subsequently to the patient if there is a balance owing.
“Failing to provide that generates frustration for the patient and extra calls to the call center,” she said. “When a patient has questions, the call center has to be knowledgeable about the process so they can help them resolve the problem.”
Even Nofziger-Drew, who has decades of experience in medical billing, confesses to having been frustrated when asked to help out friends and families with their challenging medical billing issues.
“Society in any area doesn’t do a good job of educating patients about every type of bill because of the way the health care system works,” she said. “Hospitals are dealing with challenges as well, so it’s hard to advocate and staff a person or people to educate patients. I have to sometimes jump through hoops to get my own bills paid, and that’s with my understanding of the system. How can we bring everything together symbiotically to provide the best care a patient can have?” •
These more intelligent AI and machine learning solutions that leverage humansin-the-loop, and can adapt to changes in real time with little to no maintenance, will be the future of revenue cycle automation.”
- AMY RAYMOND










In our previous Director’s Cut column “An Imaging Leader’s Role in Cybersecurity,” we discussed why you as an imaging leader should pause to consider this topic as well as alerted you of some ways your employees can cause cyber breaches. This article is a continuation of helping you to be cyber-ready!

From our last column, hopefully you have worked alongside your IT/security team and helped develop or been presented with an insider threat risk assessment. In tandem with a tailored risk matrix, you’re now aware of organization-crippling insider threat risks. As an imaging leader, it falls on you to help do something about it. How in the world do you even begin to deal with insider threats?
The first step, after identification, is to begin planning. Shocking right? You need to develop preemptive countermeasures. Too often, we get stuck in identification mode and wait for IT to pick up the pieces. However, as an imaging leader you need to be proactive on these countermeasures.
Enhance employee access control, expedite cybersecurity training, double down on information protection and compartmentalization, bolster your data security, have maintenance staff and procedures in place, and start using legitimately secure technology are all countermeasures you can put in place.
Some of you have already exceeded these preliminary phases of insider threat management. In that case, you can finally start preparing your strategies to mitigate the impact of insider threats when they inevitably happen. Here is a five-phase process you can use.
Insider threat mitigation isn’t as easy as inserting your response plan into a gaping hole caused by a threat. Instead, each security breach requires careful consideration. This process, known as the “respond” phase, is phase four of the five insider threat mitigation phases.
Upon detecting an insider threat, prepared organizations traverse the following “responding” phases:
• Response planning: Preceding any intervention, teams must assess the situation to ensure the threat is understood. Engage as many people as needed to evaluate the threat.
• Response communication: Sometimes overlooked, your department’s communication plan is often the most influential factor when assessing the long-term stability of your response team. Stakeholders, department heads and teams, necessary C-suite executives, and consumers are all privy to pertinent security information. Your team’s documentation needs to be meticulously reviewed and organized by those who use it the most.
• Analysis: As a leader, you’re hardwired to respond to stimuli. It’s tempting to want to immediately deploy the cybersecurity strategies that you’ve been working on for so long. However, working around insider threats takes a single mistake for a malicious user to cover their tracks. Spend the time to do a deep dive analysis. Give teams time to asses and investigate the incident. Incident reports can be generated within hours if all the training and preparation serve their purpose.
• Mitigation: The mitigation strategies
are only one piece of the puzzle, like the “execution” phase of similar project management methodologies. Without the other phases, mitigating insider threats is merely a band-aid solution to your organization’s gaping wound.
• Improvements: Finally, once your hard-working team helps dismantle and eliminate the insider threat, it’s not time to staple the papers. Every incident is an opportunity.
Weaved into the following “recovery” phase, the “improvements” sub-phase outlines the practices you and your team need to undergo to evaluate your performance, reflect on the situation, and prepare for the next time it happens.
Like a post-game interview or post-match review, teams will often dive deep into the analytics and data collected to systematically identify as many faults and weaknesses as possible, developing new risk matrices, response plans, and mitigation strategies for new threats they may find.
Now, you’re familiar with the overarching mission behind mitigating insider threats. While there are countless examples, and how you decide to respond depends on your organization’s team and resources, amongst dozens of other factors, here are some example courses of actions deriving from threats your institution may face:
• Risk: Employee’s limited knowledge of risks involved, unawareness of cybersecurity practices, or inexperience preventing insider attacks
When faced with a risk like this, consider what consultants and resources your institution may provide to rectify the risk of limited education and training. For example, you can pioneer a learning program for new and existing employees to understand your organization’s cybersecurity risks better.
When developing strategies, ensure you denote continued analysis and mitigation steps, like setting S.M.A.R.T. goals. You must ensure everything you’re doing is sustainable.
In this example, you may schedule annual, quarterly or monthly risk training alongside contracting with education and consulting firms.
• Risk: Systemic cyber risk arising from team inexperience with significant cyber events, threat uncertainty, dissemination concerns, the lack of cohesive data about events, and unknowns around the longterm impacts of cyber breaches
As one of the most intimidating cyber threats within institutions, especially in younger and smaller organizations, you mustn’t let a lack of experience cloud your IT team’s ability to defend patient data.
Contrary to the employee-centric risk above, this
risk and its associated vulnerabilities stem from fragile infrastructure, new policies and unweathered data. Many security-conscious organizations contract consultation check-ups, audits, performance reviews, and simulated attacks from cybersecurity providers to help ensure their patient data is safe.
For long-term success, running continuous experiments and stress tests on your system helps ensure that you consistently fight and, if not, are aware of operational risks. Surprise simulated incidents, long-term consultation, performance contracts as well as scheduled, spontaneous and periodic training programs contribute to a reliable cybersecurity force.
• Risk: Employees misuse, tamper or rig hardware
A glaringly obvious risk when considering insider threats is the risk of employees or stakeholders misusing security hardware to capitalize on that vulnerability later.
You may elect to invest in more reliable, rigid utilities and weekly coordinate maintenance of all critical security devices to prevent people from becoming complacent. You could also create a digital accountability system to track who used specific devices and when filtering out routine from unauthorized or suspicious device usage.
• Risk: Quickly stacking unforeseen costs of threat mitigation and maintenance
Suppose you or your organization isn’t in the financial position to fund large-scale cybersecurity operations. In that case, the pressure often falls on leaders to find something to put towards security. If you’re planning long-term or have a hand in building departments, allocating a cut of the quarterly or annual budget to cybersecurity can drastically help fund a small-scale operation.
Consistent and scheduled financial/budget analyses, budgeting, and expenditure reviews are also great ways to identify where and how your organization can contribute to cybersecurity expenses. Companies may also turn to managed service providers (MSPs) to provide subscription cybersecurity services to reduce costs and significantly increase the return on investment.
These strategies may not be directly applicable to your organization or department. Still, they contextualize the responsibility you have as a leader to contribute to developing your insider threat mitigation strategies. The Ponemon Institute found that 90% of health care institutions are targeted yearly, each incident chasing a different invaluable asset from your organization.
Some malicious actors seek money or equipment. Some may test themselves to see how long they can leave your hospital without power. And some insiders may want to get revenge on their co-workers by ruining their patients’ lives.
You may not know why insiders do what they do, but you should know you don’t want to wait to find out. •


















The perceived attributes of innovation in medical imaging that AI can assist with are taking a long time to arrive. It has been labeled the trough of disillusionment on the maturity scale.
Consumer innovations such as the cellular phone and the VCR required only a few years to reach widespread adoption in the United States. Other new ideas – such as using the metric system or seat belts in cars – required decades to reach complete use. The characteristics of innovations, as perceived by individuals, help to explain the different rates of adoption.
Radiologist and radiology administrators have yet to appreciate the relative advantages that imaging AI offers. It has not proven itself better than the current workflow that it is trying to supersede.

The degree of relative advantage may be measured in economic terms, but social prestige factors, convenience and satisfaction are also important. It does not matter, so much, whether an innovation has a great ideal of “objective” advantage. What does matter is whether an individual perceives the innovation as advantageous. The greater the perceived relative advantage of an innovation the more rapidly its rate of adoption will be.
Imaging AI has a compatibility issue. It is an innovation that was framed as a replacement solution for radiologist and that conflicts with existing values, past experiences and the needs of the potential adopters. An idea that is incompatible with the values and norms of a social system will not be adopted as rapidly as innovations that are compatible.
The adoption of an incompatible innovation often requires the prior adoption of a new value system, which is a relatively slow process.
The complexity of imaging AI is perceived as difficult to understand and use. Some innovations are
readily comprehended by most members of a society while others are more complicated and thus are adopted more slowly.
The trialability of imaging AI and the degree to which an innovation may be experimented with on a limited basis are factors. There is not an easy way to try an imaging AI solution. Some models are glass-like in deployment and fail unless supported by perfect non-real-world conditions.
The last issue is observability. Is it measurable? What is the degree of confidence that we have in the outcome it is providing?
When do we know that drift in results has occurred? What tools do we have to fix the AI when it has drifted? What does good look like? What does better look like?
Trust is the issue. To build trust more transparency and education need to occur. The solutions need to be wider in application and scope.
I spoke with renowned radiologist Dr. Curtis Langlotz, professor of radiology and biomedical informatics at Stanford University School of Medicine. We were discussing the killer application for medical imaging AI. The thing that will be the critical mass that launches it forward. He said, “I want a resident in a box.” Someone to pre read my exams. My solution was the power of the negative exam. A pre read by AI that lowers the priority of a normal exam and places an exam with a finding at the top of the worklist. The normal can be batch read later. The one in a thousand spontaneous pneumothorax is placed at the top of the worklist. The needle in the haystack is found by a super powerful magnate.
The future of AI in imaging is being built today, but it will look much different in 5 years. •


































































































































































































Ten major radiology organizations have collaborated to form the Radiology Health Equity Coalition to positively impact health care equity in the radiology arena and beyond. While disparities and inequities in health care have been evident for many years, the COVID-19 pandemic has magnified the disproportionate numbers of people of color and rural residents in the U.S. affected by barriers to care.
The Coalition, convened by the American College of Radiology, includes the American Board of Radiology, American College of Radiology, American Medical Association Section Council on Radiology, Association of University Radiologists, National Medical Association Section on Radiology and Radiation Oncology, Radiological Society of North America, Society of Chairs of Academic Radiology Departments, Society of Interventional Radiologists, Society of Nuclear Medicine and Molecular Imaging and American Association of Physicists in Medicine, with specialty and state radiology organizations already joining the initiative (radhealthequity. org/About-Us).
I am impressed by this website and the resources that this group has delivered thus far. On the site you will find a resource tab with articles and webinars that speak directly to how radiology is uniquely geared to addressing many opportunities of health equity. In radiology operations, we must communicate and educate our patients about the care we are to deliver. This requires radiology professionals to engage and build trust to have a high-quality output. These are the same attributes required to reduce health care disparities seen in health care today. In one particular webinar on the site, Dr. John Williams, surgical oncologist, spoke directly to radiology professionals about the disparities that exist in cancer screenings (cervical, breast, colorectal)
between demographics. In his presentation, he stated that the barriers to reduce these disparities are:
• Lack of awareness or understanding
• Lack of provider recommendations
• Logistical challenges
• Fear and stigma
• Cost
Coincidentally, these are the exact day-today issues that are faced in radiology operations. Whether it is explaining the importance of screening mammography to a patient or trying to get administration to approve a capital request, radiology overcomes barriers. Now, more than ever, I feel that my background in radiology operations has prepared me for the job responsibilities that I have currently. As the vice president of community health equity, I seek out leaders in the marginalize communities of Birmingham, Alabama, and collaborate with them. Whether it is a religious leader, community agency leader or local government official; my objective is to raise awareness and offer solutions.
Williams’s presentation offered solutions to the five barriers mentioned above. All which he included in a report he delivered to President Joe Biden as a member of the president’s cancer committee.
• Improve and align communication
• Facilitate equitable access
• Strengthen workforce collaborations
• Create effective healthcare IT
I am asking you as an imaging leader to join me in the war against health care disparities. If you are an imaging leader, you already have the tools to reduce these barriers because of your work performance in radiology. Consider speaking with your quality committee, health equity officer and/or chief diversity officer about utilizing your skill set to help them accomplish your organization’s goals for health equity. •
Verlon E. Salley is the vice president of community health equity at UAB Health System.


It’s a new year, and lots of things are changing. However, if managers and leaders want their workplace to do well, at least one unchanging principle should be kept in mind.
To start, remember that management and leadership responsibilities require a different level of thinking from those working on the front line. For people who wear multiple hats, it’s easy to get into “production” mode. What I mean is we know production is important, so sometimes managers and even leaders step into doing what is needed to generate the products or services your organization provides. That may seem honorable, but if you’re in a management or leadership role, your core job responsibilities should not take a back seat to that. Not only does being a manager or leader require different levels of thinking, those roles also require a different set of skills.
Intangible skills, such as emotional intelligence, are important for everyone, but especially for managers and leaders. Research from more than 200 companies worldwide shows that in middle management and senior technical positions, two-thirds of the difference between being an average performer and a top performer is strong emotional intelligence (EQ).
That number goes even higher for senior management and leadership positions, where four-fifths of the difference between average and top performers is EQ.
Looking at it another way, managers and leaders with lower levels of emotional intelligence are less likely to be top performers. That’s because practicing emotional intelligence – especially at the managerial and leadership levels – helps everyone throughout the organization stay engaged and productive. Therefore, it makes sense that exercising EQ is important if managers and leaders want things to run smoothly.
Multiple definitions of emotional intelligence (EQ)
exist. Some are too long and therefore not useful because nobody is going to remember them. Other definitions emphasize controlling the emotions of others, which I don’t think is healthy and therefore do not recommend. In an effort to make emotional intelligence both practical and easily understandable, many years ago I created a straightforward definition that serves as a handy guide for learning and using EQ. Here it is: Emotional Intelligence is the ability to perceive and assess one’s own and others’ emotions, desires and tendencies, and then make the best decision for all concerned to move forward.
Let’s break that down. First is the ability to perceive and assess.
1. Perceiving is noticing something. Observing it. Hearing it. Sensing it.
2. Assessing means evaluating what you perceived. It’s understanding what you observed.
OK, so when it comes to EQ, what are we supposed to perceive and assess? Our own and other people’s emotions, desires and tendencies. Let’s expound on that, because to be good at EQ, we must understand these things about ourselves as well as the people with whom we are interacting. However, as we break these down, let’s do it in reverse.
For tendencies, think behavioral tendencies and cognitive tendencies. To understand behavioral tendencies I like the DISC model. DISC assessments measure our preferred behavioral approach – our tendencies – in four areas.
• How we approach problems
• How we influence others
• Our preferred daily pace
• How we deal with rules and procedures
The DISC acronym helps us remember our tendencies in these four areas: Dominant (in the face of problems), Influencing (other people), Steady (in preferred pace), and Conscientious (with regard to rules and procedures). We can’t put people in a box, but a fundamental understanding of EQ means knowing that
each of us has predictable tendencies in these four behavioral areas.
For cognitive tendencies, I like to use the Myers-Briggs Type Indicator, or MBTI. This assessment identifies our tendencies in four cognitive areas:
• How one gets re-energized


• How one tends to perceive information
• How one prefers to process that information
• How one prefers to make decisions and live life
In both the behavioral and cognitive tendencies, we must remember not to put people in boxes, because people can and will adapt their behavioral and cognitive styles to fit different situations. Think about it. Most people don’t behave the same way while attending a football game as they would if attending a black tie event.
Accordingly, when I say perceive and assess ourselves and others, it’s an “in the moment” thing. People’s behavioral and cognitive styles can change depending on the situation.
Practicing good EQ means we must also perceive and assess our own and other people’s emotions and desires. Again, let’s look at these in reverse.
When it comes to understanding our desires, we’re really just answering the question, “What do I want?” Another way to ask it is, “What am I trying to achieve?” When it comes to perceiving and assessing others, this includes asking, “What does the other person want?”
Once we have answers to these questions, we can direct our thinking on how we can best move forward.
The last thing to perceive and assess is our own and the other person’s emotional status. Are we energized? Tired? Curious? Defensive? Angry? Fearful? Interested? Getting an idea of where we are emotionally – and also where the other person is – also helps us choose how to interact.

The last part of my EQ definition is deciding how to move forward in a way that’s best for everyone involved. Some EQ definitions I’ve seen advocate that our decision for moving forward should be based only on our own benefit. I disagree. I am a strong advocate for win-win thinking, because if we use emotional intelligence only for our own benefit, it won’t be long before others view us as selfish manipulators, not team players. Not exactly intelligent.
As you can probably ascertain, I believe practicing good emotional intelligence requires becoming a student of behavioral and cognitive styles. Once that knowledge is combined with a healthy dose of empathy – a desire to understand another’s situation and/or feelings – we help take our organizations to higher levels of productivity and effectiveness. •
Daniel Bobinski, who has a doctorate in theology, is a best-selling author and a popular speaker at conferences and retreats. For more than 30 years he’s been working with teams and individuals (1:1 coaching) to help them achieve excellence. He was also teaching Emotional Intelligence since before it was a thing. Reach him by email at DanielBobinski@protonmail.com or 208-375-7606.







Iam about to disturb most of you with this month’s column. I will provide my opinion on the task of filling an open position in a department. As a position becomes available, the manager must make many decisions. These decisions will impact the department and the organization for a considerable length of time.
The availability of an opening provides an opportunity to revisit the job description to ensure that departmental and organizational goals and objectives are accurately addressed. The job description should have well-defined criteria for qualified applicants including education, training and experience. It might also be beneficial to list people and relationships skills that are required or desired. Once we have the job and candidate descriptions well-defined, the decision becomes the dreaded internal or external dilemma. Do we promote from within or hire from outside?
I will explore a non-all-inclusive list of issues inherent in promoting from within first. Internal promotion is good for morale they say. It offers a career path and provides hope for advancement. A long time ago, a mentor told me that when you consider promoting from within, you need to figure out who will quit and whether that will be acceptable. I add, who will stay and disengage, whether passively or actively. Without the support of the team, failure is nearly guaranteed.
Will you settle for a nearly fully qualified internal candidate for the sake of the internal promotion? How will you fill the opening left behind by the promotion? Will you wind up now with two new people who will need special attention as they acclimate to their new positions? Will there be a need to provide additional training? A benefit of internal promotion may be that the promoted individual should already be fully aware of the goals and objectives of the department and the organization.
Hiring externally can be a long recruiting process of advertising, interviewing, evaluating, selecting, offering and not coming to an agreement, then repeat. An outsider may cost more. He may also disengage some team members. Others may leave the newly unknown future “Boss.” The individual will

need time to acclimate to the goals and objectives and may need additional training. He may also bring some bad habits and undesired baggage with him. His people and relationships skills may be unknown or only hearsay. He may bring a fresh and new perspective that could prove beneficial. He may possess skills unavailable internally.
As you may have surmised from the above, I don’t know which is the better way. I strongly believe that the right move is situational. Here is what I think I know: Communication is key.
Continually communicating with your reports is key to minimizing the effects of a new “Boss.” Having a well-defined set of goals and objectives for each report. Continually evaluating and adjusting these during scheduled one-on-ones will allow for discussions of opportunities and evaluation of the report’s needs, desires and personal objectives. Short of a sudden promotion opportunity, the one-on-ones should provide the manager the opportunity to have honest and direct discussions regarding enhancement of requisite skills.
I personally would post the promotion opportunity with the job description and the required and desired skills for the department and the organization to have the opportunity to formally apply. I would also recruit externally. This would be a time-bound process at the end of which, I would evaluate the situation for any fully qualified candidates. If no fully qualified candidates exist, I would conduct a quick evaluation of what “fully qualified” means and act accordingly. This is where I end the discussion since your own individual circumstances will determine how you will proceed.
We all work under organizational constraints and objectives that may force our decision in one direction or another. HR may decide who the “qualified” candidates are or whether they are internal or external. In any case, the person will report to you and work within your department’s culture, make sure you make the final decision. Although you don’t have to like someone to work with them, it is important that there is mutual respect. Make sure that you and your team can hit the respect button. •
Manny Roman, CRES, is association business operations manager at Association of Medical Service Providers.













626 Holdings p. 2
InterMed Group p. 23
Advanced Health Education Center p. 13

Banner Imaging p. 13


International X-Ray Brokers p. 42 Isikel p. 48

MW Imaging Corp. p. 46
KEI Medical Imaging p. 40


PM Imaging Management p. 42
Ray-Pac p. 52
®
CM Parts Plus p. 45 Engineering Services p. 3 HTMJobs.com p. 30


ICE Webinars p. 36

Innovatus Imaging p. 9

RSTI p. 51

KMG p. 25
Maull Biomedical p. 46

Medical Imaging Solutions p. 5




Technical Prospects p. 4
Metropolis International p. 42

TriImaging Solutions p. 18 W7 Global, LLC. p. 40

We understand that your future depends on quality education in a rapidly growing technological field. Our program offerings are designed to provide you with the skills and expertise needed for servicing today’s imaging modalities.
With one of the largest inventories in the industry, if we don’t have the part or device you’re looking for, we can help you source it from a variety of trusted partners around the globe.
We have engineers and installers on-board to make your purchase a priority. Whether it’s a full installation or de-installation, or technical troubleshooting, RSTI eXchange is Engineered for Life™



Our certified techs know our catalog and equipment like the backs of their hands. You’ll always get expert advice from the friendly and capable RSTI eXchange team.
Visit rsti-exchange.com for more information.







