EFFORTNEEDEDTOCREATESTANDARDIZED HTMTITLESACROSSTHEINDUSTRY













The Insulation tester, Leak Tester Tester and Cable Continuity Tester are easy-to-use devices for verifying the functionality of equipment for safety



Detect & locate defects such as pinholes, cracks and bare spots in the jacket or coating of laparoscopic and bi-polar electrosurgical instruments
Test the functionality of automated & handheld endoscope leakage testers with healthmark’s new Leak Tester Tester.
Test the quality of monopolar and bipolar cords with this user-friendly, durable device. A green light notifies the user that the cable passed testing.
For more of Healthmark’s intelligent solutions for instrument care and infection control, visit HMARK.COM
RSTI is committed to improving the quality of diagnostic imaging service and helping students advance their careers through knowledge, education and hands-on, technical learning.

“Having completed Phase I: Principles to Servicing Diagnostic X-Ray Systems at RSTI was a large factor in getting selected for my current position with Mayo Clinic in the Medical Imaging Department.”
“RSTI teaches you how to work on a modality, not single machines…learning the theory then the process of how the machine works and how to service it gives you a good foundation and makes you ready for any model.”

COMPLETE SUPPORT PARTNERFOR OUR SERVICE CUSTOMER:


• Hands-On, Technical Training
• Imaging Parts Inventory – Tested and Ready to Ship!
• Service Support – Tube Installs, PMs, etc.
• Technical Support – Access to 174+ years of Instructor Technical Expertise
• Equipment Options – Including Mobiles













P.12 SPOTLIGHT
p.12 Department of the Month: The Keck Medicine of USC Biomedical Engineering Department
p.14 Company Showcase: CBET
p.18 Professional of the Month: Brian Inphouva, CBET, CHTM
p.20 Company Showcase: The Intermed Group
p.23 Next Gen: Paul Rasche
p.24 Shifting Gears: The Ultimate Escape; Free Falling to Earth
p.28 Company Showcase: Bird Technologies
P.30 INDUSTRY UPDATES
p.30 MD Expo Recap
p.32 News & Notes
p.38 Welcome to TechNation
p.41 AAMI
p.42 ECRI
p.44 Ribbon Cutting: CompliaMED
P.46 THE BENCH
p.46 Biomed 101
p.49 Tools of the Trade
p.51 Webinar Wednesday
P.52 FEATURE ARTICLES
p.52 Roundtable: Training and Education

p.58 Corporate Profile: Elite Biomedical Solutions
p.62 All Aboard: Effort Needed to Create Standardized HTM Titles Across the Industry

P.66 EXPERT ADVICE
p.66 [Sponsored Content] Avante Health Solutions
p.69 Career Center
62 52
p.70 [Sponsored Content] NVRT Labs
p.72 Right to Repair
p.74 [Sponsored Content] Innovatus Imaging
p.76 The Future
p.78 [Sponsored Content] Block Imaging
p.80 [Sponsored Content] Renew Biomedical
PUBLISHER John M. Krieg
VICE PRESIDENT Kristin Leavoy
VICE PRESIDENT Jayme McKelvey OF SALES
EDITORIAL John Wallace
CONTRIBUTORS
Roger Bowles
K. Richard Douglas
Jim Fedele
Joie Marhefka
Manny Roman
Connor Walsh
David Witt
Steven J. Yelton
ACCOUNT
EXECUTIVES
ART DEPARTMENT
Megan Cabot
Emily Hise
Karlee Gower
Taylor Hayes
Kameryn Johnson
DIGITAL SERVICES

Cindy Galindo
Kennedy Krieg
Haley Wells
EVENTS Kristin Leavoy
WEBINARS
HTMJOBS.COM

ACCOUNTING
CIRCULATION
Linda Hasluem
Kristen Register
Sydney Krieg
Diane Costea
Joanna Manjarrez
Rob Bundick, Director HTM & Biomedical Engineering, ProHealth Care
Carol Davis-Smith, CCE, FACCE, AAMIF, Owner/ President of Carol Davis-Smith & Associates, LLC
Jim Fedele, CBET, Senior Director of Clinical Engineering, UPMC
Bryant Hawkins Sr., Site Manager, Children’s Hospital of New Orleans
Benjamin Scoggin, MBA, MMCi, Director, Clinical Engineering | Biomedical Operations, Equipment Distribution, Clinical IT, DHTS, Duke Health Technology Solutions
Allison Woollford, Biomedical Equipment Specialist at Duke University Health System

The Keck School of Medicine of the University of Southern California (USC) was established in 1885. In 1999, USC received a gift of $110 million from the W.M. Keck Foundation. That gift prompted the school to rename itself in honor of the generous gift.
That is how Keck Medicine of the University of Southern California’s medical enterprise got its name also.
Keck Medicine is comprised of the USC Norris Cancer Hospital, USC Verdugo Hills Hospital, USC Arcadia Hospital and more than 100 unique clinics in Los Angeles, Orange, Kern, Tulare and Ventura counties.
The health system’s biomedical engineering department manages the many medical devices spread across the facilities that serve patients in southern California.
“Keck is a 400-bed acute care hospital, Norris Cancer Center is a 100-bed cancer center, and we have over 70 clinics throughout the Los Angeles and Orange country,” says Jesus “Jesse” Lopez, director of operations of the biomedical engineering department.
He says that Keck and Norris are equipped with state-ofthe-art medical equipment, including diagnostic imaging equipment, patient monitoring systems and surgical equipment.
“Our biomedical engineering department is responsible for maintaining and servicing this equipment to ensure that patients receive the best possible care,” he adds.
In addition to Lopez, the department staff includes USC Biomed Administrator Sandra Paredes; Keck Biomed Supervisor Rene Pulido; Keck Biomed Techs Adrian Banuelos, Anthony Contreras, Ericka Contreras, Gabriel Luque, Michael Velarde, Nelson Figueroa and Fernando Ruezga.
Other members of the department include Norris Cancer Center Biomed Supervisor Derik Davoudian and Norris Biomed Techs Chris Su and Christ Khodaverdy. There is also Ambulatory Services Biomed Supervisor Rot Tutam and
Ambulatory Biomed Techs Victor Azurdia and Jerson Alvarez.
The team members work closely with their colleagues in IT to harden the surface of their networks from external threats.
“Our biomedical engineering team works closely with our IT department to ensure that all medical devices and systems are secure and fully integrated into our network. We regularly conduct risk assessments and vulnerability testing to identify potential weaknesses in our systems and address them proactively,” Lopez says.
He says that the department has implemented a variety of technical controls, including firewalls, intrusion detection and prevention systems, and multi-factor authentication to help protect their systems and data from external threats. Lopez says that they also conduct regular penetration testing to identify potential vulnerabilities in their systems and address them proactively.
“Overall, our biomedical engineering department supports almost 19,000 pieces of equipment in a 500-bed environment and several outpatient clinics and medical offices,” he adds.
The team members also participate in various continuing education and training programs to ensure that they are up to date with the latest advances in medical technology and equipment management.
Working in conjunction with clinical staff, administrators, manufacturers and vendors, the biomed team has participated in several special projects aimed at improving patient care and health care operations.
“One notable project that our department was involved in was the upgrading of our electronic health record (EHR) system. Our team worked closely with the IT department and health care providers to ensure that the new system was properly integrated with our medical equipment and that all data was accurately captured and stored,” Lopez says.
He says that the project required extensive planning and coordination, as well as training and support for staff members throughout the organization.
“The successful upgrade of the EHR system has led to
more efficient documentation and communication of patient data, which has improved patient care and outcomes,” Lopez says.
He says that the department has also participated in several research studies and quality improvement initiatives aimed at improving patient care and outcomes.
“These projects have included the development of new protocols for equipment maintenance, the implementation of new technology and the evaluation of new medical devices,” Lopez says.
“We are committed to staying at the forefront of healthcare technology management and contributing to the advancement of the field,” Lopez adds.
In the area of problem-solving the biomed team has developed a prioritization protocol with input from clinicians.
“We have developed a system for prioritizing maintenance and repairs based on the urgency of the issue and the impact on patient care. Our team works closely with clinical staff to understand the needs of each department and to ensure that equipment is maintained and repaired in a timely manner to minimize downtime and ensure that patients have access to the equipment they need. We also utilize data analytics and performance metrics to identify trends and issues before they become major problems, allowing us to proactively address issues and prevent downtime,” Lopez says.
He says that the team is highly skilled in troubleshooting and
resolving issues with medical equipment quickly and efficiently.
“We understand that downtime can have a significant impact on patient care and outcomes, and we work diligently to resolve issues as quickly as possible to minimize disruption and ensure that patients receive the care they need. We are also constantly seeking new ways to improve our processes and procedures to reduce downtime and improve efficiency,” Lopez says.
Team members are active in the HTM community outside of work.
“As the director of our biomedical engineering department, I am proud to say that our team is actively involved in several professional association activities aimed at advancing the field of healthcare technology management and improving patient care,” Lopez says.
“Here at USC, we are involved in the California Medical Instrumentation Association (CMIA) which is dedicated to the promotion, education and information exchange of the state’s clinical biomedical engineering community,” he adds.
Working for one of the leading research and health care providers in the country requires an equally competent team of HTM professionals. The biomedical engineering team at Keck prove that they are up to the task.

“We are committed to staying at the forefront of healthcare technology management and contributing to the advancement of the field.”

The College of Biomedical Equipment Technology (CBET) was formed to address the growing demand for skilled biomedical equipment technicians.
“Since our founding, demand for skilled technicians has only grown, exacerbated by the effects of the ‘silver tsunami,’ the pandemic and other factors. Additionally, the health care industry is facing a skills gap, driven largely by rapidly advancing technologies and limited access to quality education and training,” said Richard L. “Monty” Gonzales, Ed.D., President, College of Biomedical Equipment Technology (CBET).
“Our success in addressing these issues can be attributed to the relationships of trust we have formed with HTM leaders across the country. By working closely with medical device manufacturers, independent service providers, hospitals and other health care organizations to design our programs, we can ensure students receive training and develop the necessary skills that meet evolving employment needs,” he added. “The most important measure of our success continues to be our ability to educate, train and place students with respected health care organizations across the country and internationally. In 2022, we provided education and training to more than 600 students, the overwhelming majority of whom are working in the healthcare technology management (HTM) industry today.”
TechNation found out more about CBET with a question-and-answer session with Gonzales.
GONZALES: One of the main advantages of being a college that offers its programs via interactive distance learning is the
flexibility it offers. Online classes can be completed from anywhere with an Internet connection, allowing students to work on their own schedule. This is particularly beneficial for students who have work, family or other obligations that make attending traditional classes difficult. In addition, online courses often offer a wider range of options and can be significantly more affordable than on-campus classes. Flexibility and affordability are too often barriers to meeting applicant needs, and being an online college allows us to bring down those barriers.
CBET is also an accredited college, which means that all our operations, programs, online educational delivery and hybrid offerings are subject to rigorous peer and accreditor review and independently held to the highest benchmarks for completion and placement.
Perhaps the most important advantage we possess is the relationship we have with the health care community. The unique relationship with the industry we serve enables our team to constantly improve the education and training our students receive consistent with real-time and evolving industry needs. Our relationship with industry also enables our career services team to better support graduates seeking employment or advanced career opportunities.
GONZALES: The biggest challenge we face, and a recurring theme in our conversations with our industry colleagues, is related to our goal of maintaining curriculum and programs aligned with industry demands. There are the “steady state” challenges, the day-to-day work of ensuring regulatory compliance and accreditation to maintain standards consistent with Department of Education guidelines. And there are the other challenges, like those driven by accelerated rates of change associated with technology, or simply aligning programs and content with the trends and needs of the health care sector. Our goal – to keep no light between us and those that we serve – has served us well in addressing this challenge.
Q: CAN YOU EXPLAIN CBET’S CORE COMPETENCIES?
GONZALES: The College of Biomedical Equipment Technology (CBET) is an accredited educational institution offering Biomedical, Healthcare Information Systems Management (HISM), Imaging, Cybersecurity, and other technically oriented courses and programs. Our core competencies revolve around the types of education and training we deliver and the instructional team responsible for delivering them.
In addition to our accredited certificate and degree programs, we work directly with health care organizations to design customized education and training to assess and address skills gaps. We don’t believe in “cookie cutter” solutions or a “one-size-fits-all” approach. We have discovered that flexibility and working with health care organizations in an iterative manner to customize high value targeted training is extremely beneficial.
A third unique competency we possess is our ability to develop customized XR training content. Several years ago, we began exploring paths into the XR development arena and made a commitment to establish an organic capability to develop XR content to improve the quality and expand the delivery options of education and training. We believe that the future of HTM education and training is going to be closely linked to this sort of technology and are committed to its full development and adoption.
Q: WHAT OFFERS ARE YOU MOST EXCITED ABOUT RIGHT NOW?
GONZALES: The college is thrilled to announce the unveiling of a new degree program, Healthcare Information Systems Management. This program was designed to meet the growing need for health care professionals who possess a unique combination of skills in Medical Device Integration (MDI), Cybersecurity, Information Technology, and Healthcare Technology Management. The program will prepare students to manage the complex information systems used in health care organizations, with a particular focus on cybersecurity and medical device integration.
The program concept was conceived from a years-long collaboration with the HTM team at Sodexo, and the development of a Biomedical and Imaging Information Systems (BIIS) training course designed to up-skill their technicians to better address cybersecurity risks in the health care organizations they serve. The collaboration, led by Tyler Chaney and Christopher Faulkner at Sodexo, and John Schmidt, from the College of Biomedical Equipment Technology, has proven an incredibly effective model for conceiving, developing, and delivering relevant and valuable training.
GONZALES: The College of Biomedical Equipment Technology (CBET) is in San Antonio, Texas, a few miles away from the Department of Defense Medical Education and Training Campus (METC) and epicenter of the military biomedical training program at Fort Sam Houston. Suffice it to say, the fact that we are in San Antonio is not by accident. As a majority
Veteran owned and operated company, there were too many obvious advantages to locating in San Antonio.
Additionally, through a partnership with 626, we have been able to establish a state-of-the-art imaging training facility just outside of Atlanta, Georgia. The 15,000-square-foot imaging training center enables us to provide hands-on training for students in the imaging technology program. The center includes classrooms, labs and simulation rooms that allow students to obtain hands-on experience in maintaining, operating, troubleshooting and diagnosing imaging equipment. The imaging training center is staffed by experienced instructors who are experts in imaging technology and are dedicated to providing students with the highest level of training and education.
As a college that provides much of its education and training online to a national student population, we have also invested heavily in a quality learning management system and other software infrastructure to ensure quality interaction between faculty and students, as well as students and their peers, and students and all of the career, academic and other services we provide to ensure their success. Our commitment to the development of XR training content and incorporation of this into curricula is a truly exciting opportunity to expand the value and delivery of online training.
GONZALES: In the near future, CBET plans to expand its offerings in several key areas. One area of focus is expanding accreditation and compliance training by introducing approved Certified Healthcare Operations Professional (CHOP) certification preparation courses. Working in concert with DNV, the college will be offering individual and group sessions designed to better equip technicians and managers with the skill necessary to address health care accreditation and compliance demands.
Another interesting area of expansion is our initiative to develop a new program for dental repair technicians. For the past year we have been working with representatives from Dental Whale, an ISO specializing in dental equipment repair, and Dexis, a leading provider of dental imaging equipment, to design a certificate program addressing the specific needs of the dental industry.
Lastly, we have been working with the widely regarded Al Gresch over the past year to develop a leadership training series. The series, which I hope will present much like the popular Master Class Series you see advertised, is intended to serve as a series of professional development seminars focusing on topics of critical importance that are under-addressed in formal education. Topics like “Lean Concepts and Performance Measures: Instruments to Optimize Performance and Customer Satisfaction” and “CMMS Use and Application: Keys to Demonstrating and Building Your Value” will be included in the series. We are excited to see where these seminars take us next.
For more information, visit cbet.edu.
























































leasanton, California sits east of the San Francisco Bay in Alameda County in northern California. It is northeast of the city of San Jose. Pleasanton is headquarters to several major corporations. It is also the location for Stanford Health Care Tri-Valley.
Stanford Health Care Tri-Valley is a part of Stanford Medicine and has locations in the cities of Dublin, Pleasanton and Livermore, California.
The health system’s biomedical engineering department includes Assistant Manager of Biomed and IT Brian Inphouva, CBET, CHTM.
Like many successful members of the HTM community, Inphouva got his start in the military.
“Before separating from the military in 2013, I found an article talking about the trajectory and demand for more HTM professionals. It was the perfect field for me to translate my aviation electronics experience into, given that I acquire the supplemental education and certifications,” he says.
Inphouva attended the military’s Aviation Electronics Intermediate Level Training and Calibration school, which provided the foundation for his technology/electronics knowledge.
“From there, I attended DeVry’s Biomedical Engineering Technology program in Fremont, California, where we topped it off with a six-month internship to really witness the day-today of HTM operations,” he says.
Inphouva worked his way up from starting out as an intern to a lead biomed, supervisor and into his current position as an assistant manager. His area of specialty is managing service contracts.
It is managing service contracts that Inphouva says can present some challenges. He says that managing every specialty device’s service contract in the hospital can be daunting at first.
“But, with the strategic approach of consolidating with a multi-year master service agreement, has helped reduce the itemization of each task and eased the hassle of adding devices in the future. Tracking these contracts via Smartsheets has been a tremendous hack for me. I am able to create intake forms for vendor quotes, track the life cycle of a contract from beginning to end and create rollup spreads for my leadership to see firsthand live the data they need, i.e., aggregates, number of contracts, lapses in service and savings,” Inphouva says.
Although he has an experienced team of HTM professionals, there are times when putting everyone’s head together can help with problem-solving.
“My team is a pretty veteran team with five-plus years of experience now, especially at our extension of Stanford. And seldom do they request for any technical assistance. I also respect their knack as natural problem solvers and love to encourage empowerment at the front lines. Most of the time nowadays, the team is educating me on technical issues and resolutions for our newest and updated medical systems,” Inphouva says.
He recalls one day, the team was tasked with assisting the cath lab, along with collaborating with many other vendors, to set up the room for different EP configurations.
“Two of our most technical biomeds were assisting the cath team for almost four hours, running mock setups for upcoming cases. They did great! They even drew a diagram and explained how the room was configured for the rest of our team,” Inphouva explains.
He says that midway through the day, they ran into an
issue where they were unable to get the video on the boom monitor even though they were able to bridge the connection with adapters.
“I hadn’t stepped out of the office all day, and due to the high visibility of this mock setup for the upcoming EP case, I decided to scrub up and peek my head into the room to see if I could be of any assistance of my team. After getting fully briefed, and seeing with my own eyes the adapters used, I can see that we were going from digital to analog, and if anyone has ever had experience with audio/video, that would not be possible without some kind of converter. Luckily, we had ordered five of these and had them stored in the shop from a few years back,” Inphouva says.
He says that once the DVI to VGA converter was installed, they were able to get a clean and crisp live feed from the source.
“Thinking I was out of my element for some time, I was glad I could still be of some technical use to my team and still tell them about a scenario I encountered years ago. Which just proves that a biomed’s experience will always be an accumulation of problem-solving scenarios along with the decisions and steps to remediate those issues. Thus, the importance of sharing our wealth of knowledge amongst colleagues and peers,” Inphouva adds.
When not on the job, Inphouva enjoys fitness activities.
“I occasionally go snowboarding when there are good deals, partake in the bowling summer league, pickup basketball at the local 24 Hour Fitness and ride my road bike in the really tight suits,” he jokes.
“I have an amazing wife that has blessed us with two wonderful children,” he adds.
Many people from Southeast Asia, who left to escape communism, have worked hard and discovered success in the U.S. Inphouva’s parents were among those immigrants.
“I am second generation Asian-American, born to Laotian refugees who arrived during the Vietnam war,” he says.
Inphouva says that one of the things he likes best about work is the people.
“I honestly care and look out for their well-being. I need to know that I did my best to make sure you are loving what you do, feel safe and are always supported, even outside of the workplace. Whatever I can do in my power to make work worth looking forward to everyday, will always pay itself back ten-fold,” he says.
Some of that life-view may have come out of Inphouva’s background. He is a U.S. Navy veteran who served a five-year term overseas on the USS George Washington at the time homebased in Yokosuka, Japan.
It is an attitude that helped him earn the attention of others to be nominated as a professional of the month.
FAVORITE BOOK: “Think and Grow Rich” by Napoleon Hill
FAVORITE MOVIE: “Harold and Kumar go to White Castle”
HIDDEN TALENT:
I am the chef at home.
FAVORITE FOOD:
Malaysian Nasi Goreng, fried rice with chicken satay and peanut sauce.
WHAT’S ON MY BENCH?
A cup of coffee, water flask, photos of my family, desk heater and a box of Costco size protein bars.
FAVORITE PART OF BEING A BIOMED?
The relief in the eyes of clinical staff when biomed saves the day.

The InterMed Group is a dynamic provider of comprehensive healthcare technology management (HTM) services covering a broad range of client needs. InterMed’s deep-rooted partnership philosophy drives all its offerings, helping to ensure everything it does moves clients closer to achieving their goals.
The most encompassing of their offerings is their HTM services. InterMed acts as the client’s “one-stop shop” for their medical devices –whether that is filling in the gaps for the health care facility’s existing program or implementing a new one. They always bring the best to the client’s devices ranging from the linear accelerators, MRIs and CTs through anesthesia, dialysis, and respiratory therapy, to the patient monitors, infusion pumps and beds and everything in between.
Expanding on this, InterMed also provides field service-based contracts on medical equipment. Roughly 50% of its technical team members are specialized in diagnostic imaging where it provides service contracts for specific devices in hospitals, imaging centers and veterinary hospitals. In service and support of their cli -

ents InterMed team members abide by the “Sundown Rule” – they address every challenge or customer service concern by sundown each day, so their clients know their response and when to expect a resolution.
To add value, InterMed is also able to offer new and pre-owned equipment to clients. InterMed provides clients with capital planning reports, through its Technology Planning Solutions (TPS) offering, along with assessments of existing equipment to identify capital replacements that will best benefit the client. InterMed then also provides the clients with options to consider if they choose to move forward with a replacement.
Many years ago, InterMed established the JumpTeams program as it saw the demand for temporary, highly skilled technical talent. Whether a facility is trying to fill in for vacation time, adding skills for a recall or supplementing staff until a full-time technician is hired, the InterMed JumpTeams can provide partners with qualified staff.
There is not a day that goes by without the industry hearing about another health care cyber security attack. The FDA has even issued a warning that health care is being targeted. In addition to their other offerings, InterMed has solutions to create and implement cybersecurity plans for clients, no matter their size or current status in security – a plan that
“Every organization has its own mission, and its employees thrive when there is alignment. InterMed is about making health care better and about helping our partners achieve their goals.
If you are passionate about health care, it’s a perfect place to grow.”
– Larry Hertzler, COO of InterMed
encompasses the life cycle of all medical devices, from procurement onward.


The industry has been facing a shortage of qualified technical talent for many years, with a large population approaching retirement age and a shortage of new technicians joining the workforce. However, due to the pandemic, those highly experienced technicians of retirement age chose to retire. Now, post-pandemic, InterMed has an increased focus on addressing staffing challenges, and continues to successfully recruit and maintain the most qualified individuals as part of the InterMed team. InterMed’s internal philosophy of constant and never-ending improvement is really highlighted by its training,
where each employee has a hand in creating their annual training plan, while also educating all employees to be the best at what they do.


At The InterMed Group, the team knows the industry will continue to evolve, so InterMed will continue to create solutions for tomorrow’s challenges. That is why their goal is to be the number one independent service organization in the healthcare technology management services industry – bringing the best to as many health care providers as they can, so their partners can focus on what’s important – the patients and their families.
For more information, visit intermed1.com.













Paul Rasche has an associate degree in applied science and is currently a biomed technician at Pioneer Biomedical.

TechNation recently learned more about this up-and-coming HTM professional.
Q: WHERE DID YOU GROW UP?
A: Belle, Missouri
Q: WHERE DID YOU RECEIVE YOUR HTM TRAINING/EDUCATION?

A: State Technical College of Missouri
Q: HOW DID YOU FIRST DISCOVER HTM?
A: I first discovered HTM from a roommate explaining what he was going to school for.
Q: WHY DID YOU CHOOSE TO GET INTO THIS FIELD?
A: I chose this field because a roommate going to school for biomedical engineering told me what he would be doing as a biomed tech. As someone who enjoyed taking electronics apart, I was immediately interested.
Q: WHAT DO YOU LIKE MOST ABOUT YOUR POSITION?
A: What I like most is that every day is different.
Q: WHAT INTERESTS YOU THE MOST ABOUT HTM?
A: What interests me the most is that it allows me to work behind the scenes in the medical field. I love
playing a role in helping patients without actually being right in front of them.
Q: WHAT HAS BEEN YOUR GREATEST ACCOMPLISHMENT IN YOUR FIELD THUS FAR?
A: My greatest accomplishment thus far, a year in this field, would be gaining the knowledge to troubleshoot and repair complex medical devices.
Q: WHAT GOALS DO YOU HAVE FOR YOURSELF IN THE NEXT 5 YEARS?
A: My goals in the next five years would be expanding my knowledge on different medical devices, acquiring AAMI certifications and figuring out which part of biomed I am most passionate about.
FAVORITE HOBBY: Soccer
FAVORITE SHOW OR MOVIE: “The Vikings”
FAVORITE MEAL:
A fat ribeye steak with roasted Brussel sprouts and truffle fries.
WHAT WOULD YOUR SUPERPOWER BE?
I would want Flash’s super powers.
1 THING ON YOUR BUCKET LIST: Visit the gladiator colosseum in Rome.
SOMETHING YOUR CO-WORKERS DON’T KNOW ABOUT YOU:
I’ve competed in a bodybuilding competition.
Jumping out of a plane may be on some people’s bucket list, but it is likely on many other “no-way in the world” lists as well. It takes a special personality with an adventurous and unconventional spirit to strap on a parachute and step out of a plane at 5,000 feet.
One biomed and business owner has dared to take that leap.
Curtis R. Shaw, owner and operations manager of Innovatrix Biomedical LLC in Colorado, has strapped on a parachute many times and stepped out of a plane.
“I have always been a fan of extreme sports; skydiving was just something I didn’t think ‘normal’ people got into. When I was really young, my friends and I were into skateboarding, snowboarding, bikes, etcetera, and we always tried to push the edge. As we got older, we got more into building fast cars, racing motorcycles, street luge; really anything that made me feel ‘alive.’ When a friend of mine called me to go do a tandem with them, I didn’t even have to think about it. ‘Yes, send me the time and place,’ ” Shaw says.
He says that when they got to the dropzone (DZ) that day, the group of six was down to a group of three.
“We were on a wind hold – winds gusting too much to be safe for landing – and we spent about four hours waiting to go. During those four hours, I talked to everyone; the owner of the DZ, the DZ staff, the packers, the tandem instructors, the students taking their AFF (a class to get your skydiving license), and even just other tandem students that were there that day,” Shaw says.
He says that he has always been interested in gear/ mechanics and how things work, and in his spare time, before skydiving, he built a lot of engines for cars, diesels and rotary engine vehicles.
“I spent a lot of those four hours at the DZ asking
about the gear and how it all worked. Before we went up to do our tandem, I was enrolled in a class the next day at Skydive Ricks in Petersburgh, Ohio. I knew before ever having gone that these people were more than just skydivers, they were a family. I was hooked already,” Shaw says.
It was that experience that started Shaw on his skydiving adventure, along with graduating to more advanced techniques and maneuvers. After a large number of jumps, Shaw moved into Canopy Relative Work (CRW), a more intricate version of skydiving, compared with the more common “free fall,” and which requires additional training and safety procedures.
While the more common singular, free fall skydive comes with instructions to avoid other parachutes and separate from others, CRW is all about bringing the skydivers together in the sky with a much more prolonged period of free fall. Shaw says the difference can vary by as much as 50 seconds compared to 13-15 minutes.
“CRW comes with a whole other set of emergency procedures and a whole other unique set of gear. The reserve we use is the same as normal skydiving, the main parachutes we use are specifically designed to be used for CRW and are not that good for much else. They land differently than any other parachute I’ve ever used, they open very abruptly — sometimes it hurts — but they do stay pressurized well and are great for CRW. We, like most skydivers, carry hook knives (like a seatbelt cutter knife) but we have several of them. The joke is: ‘Why does the CRW dog (what they call us) have five hook knives?’ ‘Because they didn’t have room for six.’ We use open face helmets, like you’d see someone skateboarding wear so our ears aren’t covered and we can hear each other yelling,” Shaw explains.
He says that some parachute containers, the back-
pack worn that contains the main/reserve parachutes, are better for CRW than others.
“Oftentimes, we have a lot of lines on us and we want a ‘rig’ – the whole parachute container/reserve/main – all together, that doesn’t have very many snag points on it,” Shaw says.

He says that CRW only represents about two percent of skydivers and that those who practice the sport have become like family.

When his feet are planted on the ground, Shaw is focused on the biomed business he started in 2020.
“I formed Innovatrix Biomedical LLC in January 2020, but didn’t tell anyone for about a year. December 3, 2021, was when I put in my two-week notice and four days later, I had my first meeting with the CNO and plant ops director of another, larger critical access hospital in Colorado. They asked me for a proposal; all I had was a blank Word document. I spent the next four days writing my own contract and paid my lawyer thousands to get it proofread/corrected over the weekend. A few days after that, we had an agreement and now this is the third year I’ve been there,” Shaw says.
He says that since that time, his company now works in three different states, has hired an employee and paid for his CABT certification through AAMI.
“We have full-service contracts with two critical access hospitals in Colorado, work for some local health care offices, seven nursing homes across Colorado, a lot of urgent care clinics in Wyoming and we add more every day,” Shaw says.
He says that it is his mission for his company to be the best healthcare technology management company in Colorado and surrounding states; maybe even the entire U.S. and beyond.
“All the goals I’ve set for five years, I’ve exceeded in less than three. My competitiveness as a skydiver translates very well to owning a business. A lot of skydivers are also coincidently business owners, too,” Shaw says.
He finds many parallels between the challenges of skydiving and the work of biomeds and running a business.
“If I can be calm entangled in one of my friend’s parachutes, falling towards the ground at a rate of speed high enough to kill me on impact, I can be calm when OR equipment breaks with a patient in the room. It takes a special breed of person to take that chance and possibly fail; for me I’d rather fail than regret. As of now, I have no regrets in life and my only fear is to ‘peak,’” Shaw adds.




LIVE:
JUNE 14 | Healthmark


Save the date for this live webinar. Participation is eligible for 1 CE credit from the ACI.
JUNE 21 | RLDatix
Save the date for this live webinar. Participation is eligible for 1 CE credit from the ACI.
JUNE 28 | Phoenix Data
Save the date for this live webinar. Participation is eligible for 1 CE credit from the ACI.
PODCASTS:
sponsored by MMS “Continuing Your Education as a Biomed”


All webinars and podcast are eligible for 1 CE credit from the ACI.

ON-DEMAND:
sponsored by RTI Group “The Importance of Traceability in X-ray QA and Testing Performance”

sponsored by Cynerio “5 Ways HTM Teams Are Leading Healthcare Cybersecurity”
sponsored by Claroty “The Contractual Cure for Cybersecurity Pain: The Power of Medical Device Negotiations”

Bird Technologies is a global provider of radio frequency measurement and management solutions. The company was founded in 1942 as Bird Electronic Corporation by J. Raymond Bird in Cleveland, Ohio. He was a pioneer in the field of radio frequency (RF) power measurements, and his innovative work laid the foundation for the company’s success.
In the 1940s, RF power measurements were in their infancy, and there was a lack of accurate and reliable instrumentation available. Bird recognized this need and began to develop a new type of power meter that was more accurate, reliable and versatile than any existing instrument.
One of Bird’s first products was the Model 43 Wattmeter, which was introduced in 1952. The Model 43 was the world’s first portable, dual-range RF wattmeter and became the de facto standard worldwide. Still used today, the instrument helps engineers and technicians measure forward and reflected RF power in a coaxial transmission line.
Bird continued to innovate in the field of RF power measurement, developing new instruments and techniques that helped to establish the company as a leading provider of high-quality RF measurement solutions.

Today, Bird continues to innovate and develop new products and technologies that help customers manage, calibrate and optimize their RF systems, test, measure, monitor and invent on a broader and deeper scale. Its newest products have been developed with ingenuity, precision and simplicity in mind to meet the emerging challenges for a wide range of industries, including medical.
Bird Technologies Director of Strategic Development Katie Wright recently shared more information about the company.
WRIGHT: Unlike competing products, Bird has built our reputation on impeccable accuracy and simplicity for making RF power measurements. Radio frequency (RF) power measurements can be challenging to make because RF signals are complex and have many different parameters that need to be accurately measured. RF signals can be affected by a variety of factors such as interference, reflections and other environmental factors, which can make accurate power measurements more difficult.
Thru-line radio frequency (RF) power meters offer several advantages, including:
• Accuracy: Thru-line RF power meters provide highly accurate measurements of RF power, allowing for precise power measurement in an MRI system.
• High power handling capacity: Thru-line RF power meters are capable of measuring high power levels without being damaged or affecting the performance of the RF MRI system. This is especially important when measuring MRI pulse signals.
• Wide frequency range: Thru-line RF power meters can measure RF power across a wide frequency range, making them suitable for use in many different types of RF systems.
• Low insertion loss: Thru-line RF power meters have very low insertion loss, which means that they do not significantly impact the performance of the RF system they are measuring.
• Low VSWR: Thru-line RF power meters have a low voltage standing wave ratio (VSWR), which means that they do not introduce significant reflections into the RF system they are measuring.
YEAR?
WRIGHT: Bird designs and manufactures our products in the United States. This was a significant advantage during COVID as our business was deemed essential to remain open to
produce products for mission-critical markets such as medical, public safety and semiconductor. The challenges, however, surrounded the ability to receive raw material. Being a small company, Bird was able to be extremely flexible and pivot with our manufacturing by prioritizing critical products, rethinking logistics and diversifying suppliers.
Q: WHAT IS ON THE HORIZON FOR YOUR COMPANY?
Q:
WRIGHT: Bird’s core competence is the ability to measure in-line, continuous or pulsed, RF energy with precision and simplicity. Bird is able to calibrate the MRI RF power to ensure the best diagnostic image without causing harm to the patient.
Bird’s solution would benefit MRI equipment that does not have the calibration procedure built into the unit. We have an easy-to-read display that will plug into the directional power sensor through a USB cable and our sensor that uses an element with a frequency range of 10MHz to 130MHz and load with peak power of 37kW and pulse width, max. of 10ms. This kit also is carefully calibrated at our factory to support the accuracy for MRI calibration.
• Simple and quick way to measure pulse power during MRI testing and calibration.
• Does not require a technician to use an oscilloscope.
• The sensor package is calibrated using the same pulse amplifiers used for the MRI machine.
• RF power and all the additional sources of uncertainty are eliminated.
WRIGHT: Data harnessing in RF products will make possible actionable insights that can inform decision-making and drive better performance outcomes. One example of how data harnessing in RF MRI sensors can lead to actionable insights is in the area of predictive maintenance. By collecting data from sensors embedded in RF products, it is possible to monitor performance and detect potential issues before they become major problems. This can help companies schedule maintenance activities proactively, reducing downtime and saving money on repairs.
Q: CAN YOU TELL TECHNATION READERS MORE ABOUT YOUR ON-SITE TEST EQUIPMENT FOR MRI CALIBRATION?
WRIGHT: RF power plays an important role in the medical industry that requires high precision RF power measurement. Most major manufacturers of magnetic resonance imaging (MRI) machines purchase Bird equipment for the research and development and field calibration of their MRIs.
Bird’s new MRI test kit provides a complete set of equipment to carry out precise and independent measurements of RF power encountered. It also determines if the equipment is not in the appropriate exposure limits during device or pulse sequencing test.

Our goal is to provide companies with an easier way to test MRI safety for RF exposure levels and to make independent RF power measurements to test the accuracy of the specific absorption rate over the range of operating conditions encountered in MRI.
Q:
WRIGHT: We are excited to expand our RF power measurement capabilities into the medical market, capitalizing on years of RF experience and our portable test equipment products. Bird’s new MRI kit is specially designed for MRI testing that directly samples and measures the RF power during MRI calibration. It is perfect for MRI equipment resellers, MRI and imaging service providers, field service managers and engineers.
These kits are deployed to hospitals all over the globe where technicians will disconnect the RF cabling connected to the MRI machine and use our test kit to determine the power output. Technologists, radiologists and facility staff all work hard to ensure MRI safety for every patient they treat and rely on service technicians, MRI providers and maintenance teams to have the proper test equipment to make sure their MR equipment is calibrated and safe.
For more information. visit birdrf.com
Record-breaking attendance, top notch educational offerings, signature networking events and a jammed exhibit hall marked the 2023 MD Expo in Houston, Texas. The final numbers from the healthcare technology management (HTM) conference included 659 attendees and 359 exhibit personnel for a total of 1,018 individuals not including MD Expo staff. The conference was strongly supported by HTMA-TX and HTMA-NTX.
“The 2023 MD Expo Houston is one from which all others will be measured! Every attendance record was broken, including booths, class sizes, etc., the list goes on and on,” MD Publishing President John Krieg said. “For the first time in our 20-plus year history, we had over 1,000 total attendance, and almost 700 attendees.

The HTMA-TX and HTMA-NTX societies were instrumental in getting the word out to the local community, and the national exposure the TechNation brand brought just added to the show’s huge success.”
“We are already looking at 2027 dates to return to the Houston area,” he added.
MD Publishing Vice President Kristin Leavoy, CMP, echoed Krieg’s excitement.
“Having helped organize and plan every MD Expo



since our inception in 2002, I can honestly say this MD Expo was one of the best. Not only was it the highest attendance, but the energy amongst everyone there was upbeat and positive,” Leavoy said. “Everyone was so glad to be together!”
“We anticipated this being a home run show so we started planning from day one and put the tools in place to ensure that we could hold this event with minimal hiccups. It was one of the smoothest shows we’ve ever planned,” she added. “From the moment the attendees walked up to registration to when we bid farewell at the Disco Rodeo!”
- John Krieg, MD Publishing PresidentLeavoy applauded everyone involved with the conference.
“The MD Publishing team onsite and behind the scenes truly puts their all into making every event a success. It’s not just a business event for us, it’s bringing together our friends and colleagues,” she said.
“The 2023 MD Expo Houston is one from which all others will be measured! Every attendance record was broken, including booths, class sizes, etc., the list goes on and on.”
“It’s practically a family reunion we hold twice a year!”
Health-ISAC Inc. Vice President of Medical Device Security Phil Englert said he always enjoys the networking opportunities at MD Expo.
“I get to spend more quality time with attendees and learn so much from those conversations,” he said.
“This is where you go to meet with and learn from peers,” is what Englert said he would tell anyone considering attendance at a future MD Expo.
Garrett Seeley, who presented at MD Expo Houston, said three words that describe the conference are, “vital, informative, fun.”
He added that his favorite part of the conference is catching up with friends and meeting new peers.
“It still has to be the interaction with people from the field. It is really what makes any tradeshow valuable. MD Expo provides a great opportunity to connect to other technicians and vendors,” Seeley said.


Krieg said the MD Expo team is already preparing for a successful fall conference in Florida.
“The momentum from Houston is already in full swing as we are busy gearing up for a phenomenal MD Expo Orlando,” Krieg said. “We always have an incredible turnout when we return to Florida, and the FBS support always helps with our local and regional attendance. Our education and speaker line up is once again second to none, and we expect another memorable return to Florida!”
See the MD Expo Scrapbook on page 98.
For more information, visit MDExpoShow.com.


The Joint Commission has released its Sentinel Event Data 2022 Annual Review on serious adverse events from Jan. 1 through Dec. 31, 2022. A sentinel event is a patient safety event that results in death, permanent harm or severe temporary harm. Sentinel events are debilitating to both patients and health care providers involved in the event.
The Joint Commission reviewed 1,441 sentinel events in 2022. The most prevalent sentinel event types were:
• Falls (42%)
• Delay in treatment (6%)
• Unintended retention of foreign object (6%)
• Wrong surgery (6%)

• Suicide (5%)
Failures in communications, teamwork and consistently following polices were the leading causes for reported sentinel events. Most reported sentinel events occurred in a hospital (88%). Of all the sentinel events, 20% were associated with patient death, 44% with severe temporary harm and 13% with unexpected additional care/extended stay.
“COVID-19 continued to present challenges to healthcare organizations throughout 2022, and we saw the number of
sentinel events increase above pre-pandemic levels,” notes Haytham Kaafarani, MD, MPH, FACS, chief patient safety officer and medical director, The Joint Commission. “For each sentinel event, a Joint Commission patient safety specialist worked with the impacted health care organization to identify underlying causes and improvement strategies. Our goal is to help prevent these types of adverse events from occurring again.”
The majority of sentinel events (90%) were voluntarily self-reported to The Joint Commission by an accredited or certified health care organization. The remaining sentinel events were reported either by patients or their families, or employees of a health care organization.
Reporting of sentinel events to The Joint Commission is a voluntary process, and no conclusions should be drawn about the actual relative frequency of events or trends in events over time.
The full sentinel event data summary is available at: jointcommission.org/resources/sentinel-event/sentinel-event-data-summary
Paramount Bed has selected US Med-Equip (USME) to become the exclusive U.S. distributor of its medical equipment.
USME now offers thousands of hospitals and clinicians around the country Paramount’s beds, built stronger for a lifespan surpassing many others in the industry, according to a press release. The bed’s Japanese-engineered design helps accelerate early mobility and makes preventative maintenance and repairs simple and easy, the release adds.

“The portfolio of top-quality paramount equipment for sale includes the A6 Series Medical Surgical Bed and ALiUS Medical Surgical/ICU Bed, a sought-after low-height bed with an early mobilization tool. Both have a 562-pound capacity and include advanced patient features such as simple controls and buttons for ease-of-use, grip assists for patients to hold on to support mobility and help keep them safe, stable, and balanced when standing, and built-in USB ports to charge their phones,” the release states.
Other available mobility equipment for rent includes the Sittan Rehabilitation Table, which promotes early, upright ambulation by helping patients balance when sitting on the side of their bed, and Paramount’s walking aid, which comes with two sets of brakes for enhanced safety and an adjustable height to suit most patients. All overbed tables come with an auto or a manual-locking brake to reduce the risk of patient falls when they lean on them while getting out of the bed.
“We chose USME as our partner because of their proven record providing the best service to top clinicians and staff seeking
the best equipment for their patients,” Paramount Bed USA President Kazuya Takahashi said. “We are excited to work with a dedicated team working from more than 90 locations, USME has the best resources and processes to best serve hospital partners nationwide.”
US Med-Equip partners with thousands of hospitals across the nation for the rental, sale, service and asset management of medical equipment – diagnostic and clinical devices ranging from ventilators to therapeutic patient beds. In 2022, US Med-Equip acquired Freedom Medical, known for its beds and Page 1 therapeutic mattresses with WAVE technology, which helps protect patients’ skin from pressure injuries.
“We continue to align ourselves with the best partners in the industry to bolster support for hospital partners focused on their patients’ healing,” said US Med-Equip CEO Greg Salario. “As a leader in patient bed safety, quality and durability, we share with PARAMOUNT an unwavering commitment to helping health care heroes.”

On December 29, 2022, the bipartisan $1.7 trillion Omnibus Appropriations Act was signed into law. A measure in the new bill provides the FDA with the authority to require medical device manufacturers to take additional cybersecurity protection measures, such as the inclusion of a Software Bill of Materials (SBOM) with each device brought to market through future pre-market submissions.
As of March 22, 2023, what were once cybersecurity control guidelines are now enforceable requirements. Walt Szablowski, founder and executive chairman of Eracent, which has provided complete visibility into its large enterprise clients’ networks for over two decades, suggests, “These new cybersecurity regulations tend to have a cascade effect that may sneak up on some unsuspecting entities in and around the aggregate medical-industrial complex. The good news is that Eracent can help catch everyone up to speed and is offering free access to Eracent’s Supply Chain Risk Management application (SBOM Management Application) to hospitals, health care facilities and medical device software developers.”
It’s getting harder to underestimate the evil genius of the modern-day cybercriminal. The FBI has been sounding the alarm regarding the vulnerabilities of “unpatched” or outdated medical devices that run on legacy software and those with substandard security features. Medical devices, such as insulin pumps, defibrillators, mobile cardiac telemetry, pacemakers, and intrathecal pain pumps, can be appropriated by malicious hackers who could endanger a patient’s health by changing a monitor’s reading or administering a drug overdose. A skilled hacker can exploit unsecured devices, interfere with a medical facility’s operational
activity, and compromise data confidentiality and integrity.
An SBOM essentially contains a listing of items that make up the ingredients of a hardware/software device. It comes into play when tracking security vulnerabilities and updates for each software component. The SBOM is also used for the verification and management of software licenses. Szablowski elaborates, “An SBOM by itself is impotent and ineffective if it is not constantly scrutinized by an automated, proactive process with instant visibility and vigilance in mitigating and resolving any component-level security weaknesses across the life cycle of the hardware/software device. Eracent’s cutting-edge Intelligent Cybersecurity Platform (ICSP) Cyber Supply Chain Risk Management (C-SCRM) module is unique in that it provides an additional, critical level of protection to minimize software-based security risks.”
The ICSP C-SCRM recognizes obsolete components that can increase security risks; it offers up-to-the-minute protection by independently scanning the itemized details within the SBOM and matching each listed component to the most up-to-date vulnerability data using Eracent’s IT-Pedia IT Product Data Library – a single, authoritative source for essential data concerning millions of IT hardware and software products. Medical device software developers frequently utilize open-source software (OSS) to produce products faster to hasten their release into the market. OSS is pre-coded, real-world-tested, and often free to use. An astounding 92% of applications contain open-source software. Standard vulnerability analysis tools do not scan individual OSS components within applications.

MW Imaging Corp, a leading ultrasound parts, probes, systems and service provider, recently announced the achievement of ISO 13485:2016 recertification for its business operations based out of St. Charles, Missouri.
MW Imaging’s facility was audited by DEKRA Certification Inc., an accredited ANAB Certification body. They were presented with their certificate on March 21, 2023. The St. Charles facility repairs ultrasound probes, systems and equipment from all leading manufacturers. The company has implemented standardized in-house processes and testing methods that ensure a high quality of repairs for their products and services.
ISO 13485:2016 is the world’s most widely recognized medical device quality management standard, developed and published by the International Organization for Standardization (ISO) for medical device companies. It provides a framework to establish a rigorous quality management system that aligns with FDA regulatory requirements laid out in 21CFR, Part 820. It predominantly focuses on
mandatory regulatory requirements, compliance, evidence-based decision-making, risk management and accountability across all organizational processes. It ensures that medical devices placed on the market are safe and effective.
“The core values of MW Imaging have always been to achieve the highest standards in all that we do. This recertification is a direct result of the collective efforts of the MW Imaging team. Without the dedication of our employees, this achievement would have been impossible. These efforts have led to improved efficiency, productivity and most importantly customer satisfaction. We believe this certification demonstrates our dedication to quality, continuous improvement, patient safety and both employee and customer satisfaction.” said Amber Sportsman, vice president of operations/ quality manager.
MW Imaging has been certified since March 2020, and has been audited yearly for conformance to ISO 13485:2016 standards despite the challenges of the COVID-19 pandemic.
ReNew Biomedical recently celebrated Josh Weatherford and instructor Richard Woods. Josh Weatherford, ReNew’s shop manager, was recognized as the first-ever technician to complete a biomedical apprenticeship program in association with AAMI (Association for the Advancement of Medical Instrumentation) and the U.S. Department of Labor. As part of this two-year course, he achieved his CABT and CBET certifications under the instruction of Richard Woods.


AAMI Vice President of HTM Danielle McGeary presented Weatherford with his apprenticeship completion certificate from the Department of Labor. Also in attendance was Robert Burroughs, AAMI’s Chief Learning and Development Officer. As the first individual to recieve this recognition, Weatherford’s certification has been specially recorded in the Federal
Department of Labor Archives.
The ReNew Biomedical Training Academy was announced by Governor Bill Lee and Commissioner Bob Rolfe in October of 2020, and aims to train Certified Biomedical Equipment Technicians (CBET) in West Tennessee. With the growing need for medical equipment service, ReNew is comitting to revitalize the healthcare technology management and biomedical workforce to maintain, service and repair life-saving medical equipment around the country. The RBTA program is aimed at facing labor challenges head-on and creating local skilled jobs. The academy is set to create 43 new skilled jobs over its first five years. The ReNew Biomedical Training Academy, and newly refurbished facilities, officially launched in January of 2021.

Royal Philips and Northwell Health, the largest healthcare provider in the state of New York, announced that they have entered into a seven-year agreement to help the health system standardize patient monitoring, enhance patient care and improve patient outcomes while driving interoperability and data innovation. This will not only allow Northwell Health to lay the foundation for a future-proof, enterprise-wide platform, but the system will also allow them to support innovative technologies as they evolve and give them the flexibility to scale their patient monitoring systems quickly and efficiently.
Northwell Health has 83,000 employees at 21 hospitals, including flagship facilities North Shore University Hospital and Long Island Jewish Medical Center, 850 outpatient facilities and one of the largest residency programs in the U.S. with over 1,900 residents and fellows. All of this to help them address a service area of 12 million people, treating over two million patients a year, delivering over 30,000 babies, and treating more New Yorkers for cancer than any other care provider. Northwell Health is also pioneering research at the Feinstein Institutes, including national clinical trial sites for treating lupus, rheumatoid arthritis and paralysis.
“With the new system, we wanted something that could
leverage our existing IT infrastructure and allow Northwell to offer cybersecurity, while also building in redundancy with local availability,” said Phyllis McCready, vice president and chief procurement officer for Northwell Health. “The new Philips system gives us an enterprise-wide platform that centralizes our patient monitoring and allows us to see what is happening at each bedside. The innovative approach is extensible and allows us to give the communities we serve the very latest technology, while helping us to deliver a better patient and staff experience and better outcomes.”
“As forward-thinking health systems like Northwell Health take an enterprise-wide approach to healthcare IT, we can help take the guesswork out of the technology and help them to standardize their systems, with an open, interoperable architecture that can break down barriers to integration and simplify workflow for care providers,” said Jeff DiLullo, chief market leader of Philips North America. “Their new patient monitoring system can help minimize manual tasks, give staff a centralized view of patients, and harness the power of massive amounts of data by using AI to provide actionable clinical insights – all of which are helping them to deliver a better patient and staff experience, lower costs and contribute toward the goal of improving outcomes.”









































Tenacore provides immediate access to highquality, pre-owned medical equipment at a greatly reduced price. Typically, you can realize a savings of over 50% compared to new!
































• Ten-step process ensures that all equipment is tested and cosmetically like new



















































• Six to twelve-month warranty on all equipment provides peace of mind with your purchase














• Ongoing inventory allows immediate shipment on most orders

































Q: WHAT PRODUCT, SERVICE, OR SOLUTIONS DOES YOUR COMPANY PROVIDE TO THE INDUSTRY?
NVRT Labs is an XR development company singularly focused on the creation of XR content to train healthcare technology technicians and students on various medical device procedures and repairs. NVRT Labs provides customized content development services to healthcare organizations, medical device manufacturers, educational institutions, and independent service organizations looking to scale their service capabilities and streamline their training budgets.
Q: TELL US WHAT DIFFERENTIATES YOUR COMPANY FROM THE COMPETITION?
Each of NVRT Labs’ modules is designed to be a highly-interactive and immersive learning experience that places technicians in virtual environments with photorealistic 3D models to simulate real-world scenarios and develop real-life competencies. With a constantly growing catalogue ranging from general biomedical equipment procedures to extremely sophisticated radiology device installations and calibrations, NVRT Labs’ platform is the only XR content library created specifically for HTMs.
For more information, visit nvrtlabs.com.
Q: WHAT PRODUCT, SERVICE, OR SOLUTIONS DOES YOUR COMPANY PROVIDE TO THE INDUSTRY?

With over 80 years of experience, Bird provides highly accurate and elegantly simple, high power radio frequency (RF) measurements and calibration kits for MRI and RF ablation equipment.
Q: TELL US WHAT DIFFERENTIATES YOUR COMPANY FROM THE COMPETITION?

Bird has the unique ability to measure in-line, continuous or pulsed RF energy, with accuracy traceable to NIST. We provide peace of mind that the applied RF power will provide the best diagnostic image and/or accurate targeted RF therapy without causing harm to the patient.
For more information, visit birdrf.com.

Q: WHAT PRODUCT, SERVICE, OR SOLUTIONS DOES YOUR COMPANY PROVIDE TO THE INDUSTRY?



Cynch brings a digital revolution to MRO operations by automating the resource intensive maintenance and repair work order processes in the cloud. With automated MRO, our customers save time and eliminate rework using fully guided procedural instructions (checklists) and live reporting features. Cynch customers maximize up-time for manufacturing assets, medical devices, and aircraft using proactive maintenance schedules that increase overall profitability.
Q: TELL US WHAT DIFFERENTIATES YOUR COMPANY FROM THE COMPETITION?
 Alfredo Rey, Market Development
Alfredo Rey, Market Development

Cynch is a unified ERP platform offering Computerized Maintenance Management (CMMS) plus asset management, purchasing, inventory management, subcontracting and warranty claims. Customers can log-in to Cynch through their own website to manage their entire operation in one place. Technicians can see their work queue, follow a guided inspection and maintenance process, add notes, upload photos, add MRO inventory parts to the order, see asset specific user/repair manuals and so much more. Cynch also offers lightning fast filtering and searching of enormous asset catalogs by customer location, asset type, asset status, work order status, plus your custom requirements. Cynch has everything you need. Call 720-939-8467 or email Alfredo@Cynch.me to schedule your personalized demo.
For more information, visit cynch.me.
Your Ultrasound Partner
Your Ultrasound Partner
QUALITY, TESTED PARTS
QUALITY, TESTED PARTS
ULTRASOUND SERVICE TRAINING
ULTRASOUND SERVICE TRAINING
PROBE REPAIR WITH FREE LOANERS
PROBE REPAIR WITH FREE LOANERS


NEXT DAY RENTALS
NEXT DAY RENTALS
SERVICE ACROSS THE US
SERVICE ACROSS THE US
Mention this ad for 10% OFF your next part or repair.
Mention this ad for 10% OFF your next part or repair.
HAVING PROBLEMS WITH YOUR ULTRASOUND PROBE?
HAVING PROBLEMS WITH YOUR ULTRASOUND PROBE?


Scan the QR code and get an instant quote by using our free ultrasound probe evaluation tool.
Scan the QR code and get an instant quote by using our free ultrasound probe evaluation tool.
AAMI and the British Standards Institute (BSI) have jointly published guidance documents on performing risk management for machine learning (ML) or artificial intelligence (AI) incorporating medical devices.
AAMI Technical Information Report (TIR)34971:2023, Application of ISO 14971 to machine learning in artificial intelligence – Guide, derives from a 2022 AAMI consensus report (CR). The U.S. Food and Drug Administration recognized the CR as a guidance document “appropriate for meeting requirements for medical devices under the Federal Food, Drug, and Cosmetic Act.” Developed in collaboration with BSI, the CR was the first AI-related guidance to receive this level of recognition from the agency.
“The key difference about the TIR is that we’re doing it jointly with BSI,” said Hae Choe, principal director of standards at AAMI. “It is a dual-logo document. The documents are a little different because BSI doesn’t have technical information reports. They’re publishing theirs as a British Standard.”
Notably, the content of the TIR is substantively the same as the CR content, with only minor spelling and formatting differences between the U.S. and British versions. “The technical content is the same,” Choe said. But the TIR and Standard designations carry more weight – and the British Standard will extend the reach of the guidance.
To develop the CR and TIR, AAMI’s Artificial Intelligence Committee piggybacked on ISO 14971:2019, Medical Devices-Application of risk management to medical devices, and
the AAMI/ANSI/ISO 14971:2019, which is the U.S. adoption of the standard. This widely used standard details how manufacturers can implement the risk management process of assessing and mitigating potential risks to protect the health and safety of patients as well as data and system security.

Rather than reinvent the wheel, the AAMI Artificial Intelligence Committee applied the standard risk management process to the elevated or unique safety-related vulnerabilities and risks of AI- and ML-enabled medical devices, including:
• Data management
• Bias
• Data storage, security and privacy
• Overtrust
• Adaptive systems
“The risk management process is the same, but there are new ways to fail, different concerns and different risk controls to consider,” said Pat Baird, senior regulatory specialist at Philips and co-chair of the AAMI Artificial Intelligence Committee, in AAMI’s inaugural Medical Device Safety in Focus report, Artificial intelligence: The Trust Issue. “Recognize the fact that AI systems, data and clouds are going to change and that is outside your control. Plan for it. Don’t wait until something bad happens and then try to figure out what you’re going to do about that. Have the infrastructure and mechanisms in place.”
In the near future, AAMI and BSI are planning to propose TIR34971 as in international standard through International Organization for Standardization (ISO) Technical Committee (TC) 210, Quality management and corresponding general aspects for products with a health purpose including medical devices, and IEC (International Electrotechnical Commission) Subcommittee (SC) 62A/Common aspects of medical equipment, software and systems.
For more information, visit aami.org.
ecall management remains challenging for health care providers, as the number of hazard alerts involving medical devices, pharmaceuticals and other products continues to increase. From cybersecurity vulnerabilities involving complex medical technologies, to sterility issues with various consumables, to shortages across the industry, managing product recalls and corrections becomes more complex every year.
An analysis of 2022 data from the ECRI Alerts Workflow system, which facilitates efficient recall and technology risk management for medical equipment, supplies and pharmaceuticals, highlights the scale of the challenge that providers are facing:

In 2022, the number of ECRI medical device alerts and related recalls kept pace with the prior year; however, reports from providers point to a higher volume of impacted units and increased burden on the provider. The 2022 alerts breakdown as follows:
• 1,923 total medical device alerts – 62% of these were related to supplies, while the rest were related to capital equipment
• 636 alerts related to pharmaceuticals
• 546 alerts related to food products
As an indicator of risk, ECRI assigns a priority level to
each alert to help members prioritize. In 2022:
• 5% of device alerts were classified as “critical,” indicating the potential for serious injury or death
• 77% were classified as “high” priority,” indicating the potential for serious injury, temporary illness or harm
• 18% were classified as “normal priority,” based on regulatory or other risks that are unlikely to cause injury or illness
Medical device alerts classified as “critical” priority included a range of technologies, with specific types being represented multiple times:
• Several alerts related to cardiac circulatory assist units, which are used to improve blood circulation in patients with a debilitated heart
• Multiple alerts involved infusion pumps, which remain a common device affected by recalls and corrections
• As in previous years, issues involving continuous positive airway pressure and bi-level continuous positive airway pressure technologies continued to arise
• COVID tests continue to be a hot topic, as inaccurate or unapproved tests continue to cause issues for patients
In addition to the many alerts that require review and the diverse group of technologies affected, health care providers experienced several high-profile recalls that garnered much industry attention:
• Recalls involving Philips continuous positive-airway pressure devices and ventilators, stretching back to 2021, continued to be a big issue in 2022
• Contamination and resulting shortages of infant formula placed a large burden on providers and parents
• A production disruption of GE Healthcare Omnipaque (Iohexol) and Visipaque (Iodixanol) contrast media led to shortages and diagnostic imaging delays

With the large volume of recalls shown above and the complexities of recall management and supply chain sourcing, management of recalled medical devices, pharmaceuticals and food products remains a complex problem for health care providers. To ensure the safety of patients and staff, providers should have appropriate resources and technologies working seamlessly together for more effective and efficient recall management.
Some best practices are as follows:
• Ensure that recall notifications are being received and
distributed in a timely fashion.
• Confirm that recall information is properly communicated to all organizational stakeholders.
• Make sure that staff takes appropriate action to isolate affected products to help keep patients safe.
• Validate that proper information is communicated back to the manufacturer to close the recall loop. Track all recalls to closure and record actions taken for regulatory compliance and audit.
• Incorporate reporting and related dashboards to support quarterly updates and to confirm complete enterprise-wide recall compliance. ECRI can help you ensure the removal of harmful products before they reach the patient and reduce the time spent on recalls by 50% to 90%.
For information, visit ecri.org/solutions/alerts-workflow.

ompliaMED is highly specialized business and CMMS software engineered for the biomed service industry. It offers an end-to-end CRM, asset and inventory management system, with companion mobile inspection and work order apps.

CompliaMED COO Chris Zulliger recently shared more information about the company.
Q: WHAT ARE SOME OF THE SERVICES AND PRODUCTS YOU OFFER? IS THERE A SPECIFIC OR NEW ONE YOU ARE EXCITED ABOUT RIGHT NOW?
ZULLIGER: CompliaMED has officially launched its computerized maintenance management system (CMMS) software. It is designed by biomed technicians and built specifically for the biomed service industry which enables any size company to capture and report test documentation from start to finish on an iPad and produce compliant reports all in one application. CompliaMED also integrates with QuickBooks Online for an all-in-one CRM, CMMS and financial solution for efficiently operating biomed service companies.
Q: HOW DOES YOUR COMPANY’S STAND OUT IN THE MEDICAL EQUIPMENT FIELD?
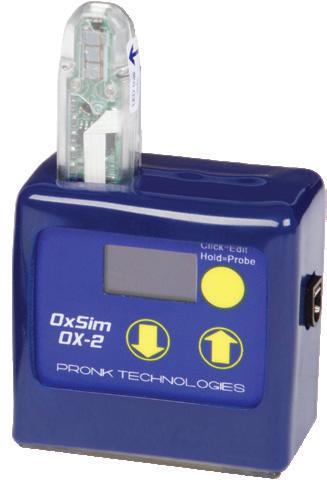
ZULLIGER: CompliaMED is a complete solution for operating a biomed service company. We know of no other all-in-one application for managing biomed service companies. Our mobile inspection and service order applications allow for offline operation. Freeing technicians from unstable cell service and slow Wi-Fi makes working remotely fast, reliable and accurate. Integration with Pronk Technologies testing and simulation devices produces traceable, compliant test and simulation results. We offer easily shared comprehensive inspection certificates and service reports.
Q: DO YOU HAVE ANY GOALS YOU WOULD LIKE TO ACHIEVE IN THE NEAR FUTURE?
ZULLIGER: Our goal is to provide technology to independent biomed service companies that will allow them to compete in an ever changing and competitive market.
Q: IS THERE ANYTHING ELSE YOU WOULD LIKE OUR READERS TO KNOW?
ZULLIGER: Biomed service companies can no longer merely provide a pass/fail sticker or report. Industry regulators are now requiring compliant and traceable results to meet long established standards. CompliaMED delivers these results.
For more information, visit compliamed.com.

The latest advancement in the health care sector is the use of drones to transport medical supplies and devices. Simulation models show that this new mode of transport could have huge cost advantages, with savings between 20 and 50 percent compared to traditional multi-tiered land transport systems. Due to their smaller size, drones also have the advantage of being able to access more remote areas and need less manpower to run them.
Drones are proving invaluable in remote communities that have poor access to health care and are geographically distant from major hospitals, such as southeast Asian countries and especially islands such as Indonesia. The current system of using helicopters to deliver medical equipment amongst islands is not cost-efficient and can lead to some of the most rural communities being forgotten, as there are no helicopter landing spots nearby.
Cargo drones are easier to land as they can be six times shorter in length than cargo helicopters. Fixed wing drones can also deliver medical supplies whilst airborne by dropping the load, which parachutes down into a three-meter-wide landing zone (an area 10 times smaller than a typical helicopter landing zone). Helicopters
cannot drop supplies whilst airborne due to the risks of the parachute getting caught in the rotor blades.
The large landing zone needed for helicopters can also be problematic in the event of a natural disaster, when terrain becomes inaccessible. For example, in 2017, Hurricane Ophelia and Storm Emma hit the Aran Islands in the Republic of Ireland within four months of each other, causing significant damage to roads and seaports. Therefore, it is no surprise that the Aran Islands have been participating in drone delivery trials, with the Wingcopter drone distributing insulin successfully.
Drones have also been used to dispatch automatic external defibrillators (AEDs) to people in need. Trials in Sweden (reported by The European Heart Journal ) proved successful and, in 63% of cases, the AEDs arrived by drone before an ambulance reached the scene. One AED delivery saved a 71-year-old man’s life, arriving three minutes after the alarm was first raised by a passer-by.
In addition to distributing medical supplies and devices to those in need, drones can be used to help health care professionals diagnose health problems more rapidly, through the delivery of urine or blood samples from homes to hospitals. For example, Neuron’s MediDrone project has seen them help the NHS with urinary tract infection (UTI) samples. The National Institute for Health Research cites UTIs as one of the most common infections but, to get antibiotics, a urine sample must be tested by the doctor. For those in remote communities or with other health problems, travelling to give a sample

could be a problem. Being able to give one from your home, and have a drone pick it up, speeds up the process of getting the diagnosis and prescription for medication.
The samples themselves may also be time and temperature sensitive, making prompt and efficient delivery essential, even between different buildings in the same hospital. If this is not done smoothly, it can massively increase the time patients wait in the hospital, which can lead to an increase in bed occupancy. Drones can help decrease the time it takes to get a sample, whilst maintaining the quality control needed.
Although there have been many successful pilot schemes, there are some challenges remaining before more widespread uptake of drones is feasible. One of the
to terms with this relatively new form of air transportation. Bill Wimberley, head of business at Wingcopter, suggests that drones will become more economically viable once their efficiency and battery-life increases. To ensure that the optimum battery is selected for a drone, drone manufacturers ought to consider customized solutions that take into consideration the weight that is being carried (and the power the engine will need) and the distance being travelled (and, therefore, the required runtime of the battery). This can vary massively: for example, urine samples are a considerably lighter payload than medical devices and drones that are transporting supplies from the mainland to a remote island will most likely be travelling a further distance than

Offering a one-stop-shop vendor-neutral platform where customers can purchase different models - up to 50% below the cost of new.
Established rental program that allows facilities long-term, short-term, and rent-to-own options.
One of the largest inventories of parts & accessories in the industry allows 5-10 years of support for all equipment sold.

Contract and non-contract services from CBET/CRES certified engineers that meet or exceed JCAHO requirements.
INFUSION DEVICE ANNUAL PREVENTATIVE MAINTENANCE
• MMS will deploy a team of technicians to your facility to complete Annual Periodic Maintenance on your Infusion Pumps




• Daily updates and final reports provided at completion of project
EQUIPMENT SALES
• All types of medical equipment- new or refubished
• All equipment is patient ready with warranty
• Rent-to-own options available!

The Mobile Table is designed to support lightweight laboratory equipment. Sizes from 38” and 48” wide, 24” and 30” deep and 30” standard height. It is constructed of 1” X 2”, 16-gauge rectangular tubing, with welded construction. It has four wheels with 250-pound capacity casters and two casters are

lockable. The work surface is chemical resistant, plastic laminate with matte finish, and black perimeter edge bumper. It has a powder-coated finish that resists chemicals.
For more information, visit www.hemcocorp.com.
SAKOMEDSAKOMEDSAKOMEDSAKOMEDSAKOMEDSAKOMEDSAKOMEDSAKO
MEDSAKOMEDSAKOMEDSAKOMEDSAKOMEDSAKOMEDSAKOMEDSAKOMEDSA
KOMEDSAKOMEDSAKOMEDSAKOMEDSAKOMEDSAKOMEDSAKOMEDSAKOMED
SAKOMEDSAKOMEDSAKOMEDSAKOMEDSAKOMEDSAKOMEDSAKOMEDSAKO
MEDSAKOMEDSAKOMEDSAKOMEDSAKOMEDSAKOMEDSAKOMEDSAKOMEDSA
KOMEDSAKOMEDSAKOMEDSAKOMEDSAKOMEDSAKOMEDSAKOMEDSAKOMED
SAKOMEDSAKOMEDSAKOMEDSAKOMEDSAKOMEDSAKOMEDSAKOMEDSAKO
MEDSAKOMEDSAKOMEDSAKOMEDSAKOMEDSAKOMEDSAKOMEDSAKOMEDSA
KOMEDSAKOMEDSAKOMEDSAKOMEDSAKOMEDSAKOMEDSAKOMEDSAKOMED
SAKOMEDSAKOMEDSAKOMEDSAKOMEDSAKOMEDSAKOMEDSAKOMEDSAKO
MEDSAKOMEDSAKOMEDSAKOMEDSAKOMEDSAKOMEDSAKOMEDSAKOMEDSA




KOMEDSAKOMEDSAKOMEDSAKOMEDSAKOMEDSAKOMEDSAKOMEDSAKOMED


SAKOMEDSAKOMEDSAKOMEDSAKOMEDSAKOMEDSAKOMEDSAKOMEDSAKO







MEDSAKOMEDSAKOMEDSAKOMEDSAKOMEDSAKOMEDSAKOMEDSAKOMEDS

AKOMEDSAKOMEDSAKOMEDSAKOMEDSAKOMEDSAKOMEDSAKOMEDSAKO







MEDSAKOMEDSAKOMEDSAKOMEDSAKOMEDSAKOMEDSAKOMEDSAKOMEDSA KOMEDSAKOMEDSAKOMEDSAKOMEDSAKOMEDSAKOMEDSAKOMEDSAKOMED SAKOMEDSAKOMEDSAKOMEDSAKOMEDSAKOMEDSAKOMEDSAKOMEDSAKO












sodexo.com

The webinar provided HTM professionals in attendance with actionable risk reduction actions for cybersecurity. Biomeds often find that this space is full of governance models, monitoring software and awareness, but does not give onsite technicians guidance on where to start and specific actions to take. Presenter Ryan Gonzalez, Director of HTM Cybersecurity at Sodexo, shared his top three cyber risk reductions. He was joined by Chad Holmes, Security Evangelist at Cynerio.
• “The two presenters gave very, very practical advice that can be employed by hospitals to lower their risk of malware.”
– Ethan Hertz, Clinical Engineer, Duke University Health System.
ordr.net

In this webinar, Ordr Head of Product Marketing Chris Westphal and Seth Feder, former health care professional and Gartner Analyst, outlined the role HTM and clinical engineering teams can play to protect against ransomware, including:
• Keeping an accurate medical device inventory.
• Monitoring for unknown devices on the network.
• Identifying medical devices with outdated operating system.
• Effectively prioritizing and managing device vulnerabilities.
bcgroupintl.com

Lucio Simoni, engineering manager at BC Group, demonstrated the use of the SA-2600 Electrical Safety Analyzer covering manual testing, auto-sequences and remote operation with myBC Mobile. Simoni has been with BC Group for 28 years and has been instrumental in the development of most of the BC Biomedical brand testers and analyzers.
• “I think it is important to keep up to date on test equipment options.”

– Shannon Dingus, manager, Indian Path
“Medical Right to Repair and Anticompetitive Behavior”
• “I’m concerned about equipment maintenance costs continuing upward because of poor vendor documentation. This has been going on for years and needs to be fixed. I can buy generic parts for my car, why not for medical devices?”
–
Frank Nickells, BMET, ProjectCURE volunteer• “The future is technology! With all the scammers and hackers in this world you can never be too careful with all these attacks. This webinar was just the perfect information we need in today’s health care technology.”
– James Hawkins, a biomedical technician at Kaiser Permanente.
nuvolo.com
• “Understanding your HTM workflows and strategic thinking about what your health system needs is critical to successful CMMS implementation.”
– Carol Davis-Smith, president, Carol Davis-Smith & Associates LLC.
June 2023 | TechNation 51
“Top
Reductions Your HTM Team Can Start Today”
“Manual Testing, Auto-Sequences, and Remote Operation of SA-2600 Electrical Safety Analyzer Using myBC Mobile”
Dustin Smith, senior advisory solution consultant at Nuvolo, and Arleen Thukral, VISN 2 healthcare technology manager at VA, discussed how high-reliability organizations “learn, inquire and improve” while supporting a culture of safety. This session discussed Nuvolo CMMS in VISN 2 VA New York/New Jersey Healthcare Network’s automated workflows to support a culture of safety. Use cases were shared of preventative maintenance workflows that allow constant communication between technician and stakeholders when medical devices are in use or closed as deferred could not locate. Another workflow includes a new incoming inspection process that includes a verification step to ensure proper naming and attributes of inventory and a request portal that includes incoming equipment support for non-hospital owned equipment. Quality assurance and checklist workflows were also discussed. A question-and-answer session provided additional insights.
This month, TechNation contacted several healthcare technology management (HTM) professionals and asked them to share their thoughts and insights regarding training and education. Participants in the roundtable article are College of Biomedical Equipment Technology’s Dr. Richard “Monty” Gonzales; Innovatus Imaging Director of Commercial Operations and Business Analytics Ted Lucidi, CBET; Maull Biomedical Training LLC Owner Stephen Maull; RSTI Training Registrar Anna Morrison; and Elite Biomedical Solutions CBET/BMET II Jake Walters.
technologies in the health care sector. Second, ensure that the program is accredited by a recognized organization or institution. Third, consider the quality and expertise of the faculty, as well as the availability of industry connections and networking opportunities. Finally, consider the program’s cost and duration, as well as its potential for career advancement and job placement. By considering these factors, you can ensure that you receive the best education and training in the healthcare technology management industry.
GONZALES: When seeking education and training, it is important to consider several key factors. First, look for programs that offer practical industry-specific education and training consistent with current and emerging
LUCIDI: The questions that need to be answered are 1) “What does the training, on a specific device, enable the technician to do? 2) Are there any limitations? and 3) Are there any additional costs required after the training?” You don’t want to find out, post-purchase, and more so post-training, that there is a periodic subscription fee to enable access to diagnostics or technical documentation. HTM directors need to be integral to the capital purchasing process. HTM can serve as a control to prevent those in supply chain from focusing on price versus overall cost. Ideally, the cost of technical training, access to diagnostic tools and technical documentation

would be integrated into the final cost of new capital equipment. After all, the sales price of the device itself might be relatively small compared to that of the overall support costs throughout the device’s life cycle.
MAULL: Will this training satisfy our needs. Some training is big picture overall view of a topic (like introductory training) while some training is very detailed when it comes to maintenance or repair procedures. Make sure you know exactly what knowledge this training will provide.
MORRISON: There are three vital things to look for when seeking training:
• Depth of instruction
• Utilization of hands-on learning methods
• Reputation of training provider Training providers should utilize proven techniques in adult learning concepts. RSTI adheres to the VARK Adult Learning Methodology which employs Visual, Auditory, Reading/Writing and Kinesiology learning techniques. In other words, adults learn by seeing, hearing, reading/writing and hands-on experience. RSTI places utmost importance on lab exercises to reinforce the concepts learned in the classroom.
WALTERS: Speaking from personal experience, one of the most important things to seek out when training is needed is a program that has both a knowledgeable instructor and quality course material. It can be difficult to find training with both, but it is important to leave training with the confidence that you can go out into the field and put your new knowledge to use.
Q: HOW OFTEN SHOULD BIOMEDS UPDATE THEIR TRAINING ON SPECIFIC TYPES OF MEDICAL EQUIPMENT?
GONZALES: Technicians should update their training on specific types of medical devices regularly. The frequency of updates may vary depending on the complexity and criticality of the devices, changes in regulations, cybersecurity concerns or other factors. For high-risk devices, more frequent updates may be necessary to ensure patient safety and compliance with regulations. Continuing education and training is particularly important when we consider the impact of rapidly advancing technologies, software and cybersecurity concerns, and other evolving factors.
LUCIDI: Never stop learning! Tech advancements are occurring at a much more rapid pace than they did just 5 to 10 years ago. Although the fundamental function of a device may not change, the manners in which technology is applied to a device does. Volunteer for every training opportunity and continually invest in yourself. Remaining status quo is the most effective means of obsoleting yourself.
MAULL: In most cases never! Be very leary of any company that wants to charge you to “update” your training or tries to push regular “refresher” courses on you every year. Did they or did they not teach you everything you needed when you first attended. I assume if you attended the training, you are using the knowledge they gave you, so why do you need to attend again? What, because you slightly altered one of the procedures you taught me last year you want to charge me again? Sorry, but that should be free info to attendees of prior training sessions. If they don’t give you everything you need during the initial training session (manuals, handouts, software, etc) then I would think twice before attending that training.
MORRISON: Training should be valid for the life of the equipment, but as equipment evolves and new revisions are released, additional updated training may be required.
WALTERS: Things can change very rapidly in the health care industry, and it is important to stay up to date on as much as you can. How often a technician should update their training can vary based on their role at their facility, but I would say a good rule of thumb would be to seek out additional training at least on a yearly basis. Subscribing to various newsletters and literature such as TechNation is a great way to stay informed.
GONZALES: Certifications such as those offered by AAMI, COMP TIA, HIMSS and others are a crucial component of career development. Not only do they verify that individuals possess the necessary knowledge and skills to perform their jobs effectively, ensuring that medical equipment is appropriately maintained and functioning correctly, but they also serve as a quality indicator for the organizations they serve. One other thing to consider is that certifications demonstrate a commitment to ongoing education and professional development. Employers often prefer to hire certified professionals as it provides assurance that they have met industry standards and are competent in their roles. At the College of Biomedical Equipment Technology, we work very closely with our industry partners, we have found that certification can lead to career advancement opportunities and higher salaries. Overall, certifications can play a vital role in ensuring patient safety and improving the quality of healthcare technology management services.
LUCIDI: Until more employers require certification as a condition of employment, the importance of certification will be merely personal. In the industry’s current state, at best, possessing certification may provide a candidate an advantage over one who is not certified. Personally, I view certification as a commitment to oneself and to the HTM industry. To that end, I value certifications. When considering
choosing between two individuals with similar experience, interpersonal skills and personal recommendations, the certified individual would be my choice.
MAULL: That really depends on the eye of the beholder. Some hospitals/companies value certifications much more than others. There are plenty of very fine BMETs who don’t have any certifications; however, most upwardly aspirational BMETs know if they want a raise or a promotion, they will most likely have to show some growth in their career field, and that is most easily done by receiving certifications.
MORRISON: Certifications and certificates of completion are becoming more required by the health care provider. They bring validity to the engineers’ qualifications to work on specific systems. RSTI supports industry certifications by working with organizations like AAMI/ACI and ASRT to offer CEUs on relevant courses and by providing a preparatory class for the CRES exam.
WALTERS: I believe obtaining a certification such as a CBET is both important for your career and personal growth. While you are able to be employed and be successful in your career without a certification, it does help you stand out from other technicians who may not have one. Earning continuing education units to maintain your license can also be helpful for a BMET’s growth.


GONZALES: Healthcare technology managers are the unsung heroes in health care facilities. HTM professionals are involved in everything throughout the medical device life cycle, ensuring equipment is used efficiently, effectively and safely. HTMs are responsible for implementing preventive maintenance programs, which reduce the likelihood of equipment failure and the need for costly repairs. They also ensure that equipment is used optimally – reducing
downtime and maximizing the lifespan of equipment. One additional consideration for health care organizations seeking to increase cost savings is the role that HTM professionals play in evaluating the cost-effectiveness of equipment purchases. I have had countless conversations with HTM professionals discussing their involvement in the capital committee discussions in health care organizations – we probably do not discuss this factor often enough.
LUCIDI: Could you imagine if the OEM had to be called for, not just every device failure, but for every user problem and every user concern? The entire HTM industry exists to combat the ever-increasing cost associated with and the lack of availability and response time that would exist if OEMs were the sole option for support. To this end, the value that HTM professionals provide to health care facilities is virtually priceless. More so, the investment in continued HTM training provides increased cost savings through reduced reliance on OEM service. Investing in employee training also informs team members that they are valued. In turn, this leads to greater job satisfaction, quicker advancement and, ultimately, lower employee turnover.
MAULL: You can remove equipment from costly service contracts; or maybe just downgrade the contract to a first-look contract. The ability to service equipment in-house vs. waiting for the contractor to show up also can dramatically decrease downtime, which also has obvious financial benefits.

MORRISON: A single, properly trained engineer can significantly reduce or effectively eliminate costly OEM contracts on multiple pieces of the same equipment within the health care provider’s network.

WALTERS: A trained technician can lead to cost savings in a number of ways. They can save money by performing repairs in-house, rather than outsourcing the repair at a higher cost and turn-around time. A BMET that is better trained can also move through
 Stephen Maull Maull Biomedical Training LLC Owner
Ted Lucidi Innovatus Imaging Director of Commercial Operations and Business Analytics
Anna Morrison RSTI Training Registar
Richard “Monty” Gonzales College of Biomedical Equipment Technology Presdident
Jake Walters Elite Biomedical Solutions CBET/BMET
Stephen Maull Maull Biomedical Training LLC Owner
Ted Lucidi Innovatus Imaging Director of Commercial Operations and Business Analytics
Anna Morrison RSTI Training Registar
Richard “Monty” Gonzales College of Biomedical Equipment Technology Presdident
Jake Walters Elite Biomedical Solutions CBET/BMET
repairs/tasks more quickly since they are familiar with what they are working on. Cross-training coworkers can improve cost savings even further.
GONZALES: MD Expo, the AAMI eXchange, AORN and other health care conferences play an important role in the professionalization of the HTM industry. Access to valuable technical training on specific medical equipment, updates on the latest technologies and trends in the industry, and information on regulatory and compliance issues, are just a few of the benefits. Conferences also offer opportunities for professional development, such as leadership training and professional skills workshops. One of the most important aspects, however, is the ability to network with peers and mentors in the industry.
LUCIDI: In my opinion, the content provided through training sessions, at conferences such as MD Expo, exceeds that which is provided by OEMs. OEM training seems to focus on content and tools that the design engineers want customers to use. Education provided by independent service organizations often focuses on actually servicing the device. Content typically includes tips and tools to address common failures found in the field and troubleshooting by not relying on diagnostics.
MORRISON: Conferences like MD Expo, ICE and AAMI eXchange offer valuable educational tracks designed to introduce attendees to various topics related to HTM, biomed and diagnostic imaging. While this educational programming provides solid fundamental information or a good basis of understanding, attendees should not expect these sessions to be a replacement for in-depth, comprehensive, hands-on training. They should explore additional training opportunities that deliver the level of instruction needed to be a successful service engineer or manager.
WALTERS: Conferences offer a wide variety of training topics and have opportunities for most everyone regardless of your role in the health care industry. Whether you need technical training, managerial training, network systems training or even want to discuss what the future of the health care industry looks like, there is something for everyone at these types of conferences.
GONZALES: In answering this question I consider the advice I gave my son. First, ask yourself, what is the return on investment? Are you pursuing an education and training aligned with your career path or are you pursuing education for the sake of obtaining a degree. Secondly, focus on quality. In education, like health care, accreditation implies higher standards and commitment to quality outcomes. Accreditation ensures that education and training programs meet industry standards and provide high-quality instruction. This ensures that professionals have the necessary knowledge and skills to perform their job duties effectively and safely. This leads me to my last point, technicians should understand the outcomes and expected professional advancement opportunities related to their education and training.
LUCIDI: Seek out partners that provide free training opportunities, whether at conferences, in-person at your facility, or via webinars (live or recorded). Recorded webinars are a great option, but viewers do not have the option of interacting with the educator or asking questions. The Innovatus team has in-the-can content but is also able to design and deliver custom training sessions relative to ultrasound technology. Whether in-person or virtual, sessions are always no-charge.
MORRISON: The landscape of training has changed and there are many more online options available. RSTI has incorporated some eLearning classes in response to this trend. While this can be a valuable solution for some instructional theory, there is no substitute for hands-on, practical learning. RSTI would implore prospective students to ask themselves if they are just looking to check a box to meet a requirement or if they really want the comprehensive training that will give them the confidence and competence to effectively service imaging equipment throughout their career.
WALTERS: There are countless opportunities out there if one feels like they should need additional training, all you have to do is look. It can be something as simple as an informative article that takes minutes to read, attending a virtual seminar or all the way up to traveling for a multipleday technical training course. Always have your eyes and ears open, and keep in mind that there is always something new to learn out in the health care space.






We have a passion for patients and patient safety.”
Jeff Smith’s words as CEO and co-founder of Elite Biomedical Solutions and Elite Precision Plastics are equal parts corporate mission, personal mantra and family motto.
The driver of the family business – about 20 percent of Elite’s 50 employees are Smith family members – has always been a greater purpose. As one of the country’s first manufacturers of high caliber, U.S.-made third-party replacement parts for infusion pumps and telemetry units, Elite is transforming the medical equipment industry to make a difference in health care.
When Jeff and his nephew, Nate Smith, co-founder and Chief Revenue Officer, established Elite Biomedical Solutions in 2012 in Cincinnati, Ohio, only one other company made new replacement parts for infusion pumps to provide savings. Hospitals had to buy used equipment
and harvest the parts themselves or purchase parts from original equipment manufacturers (OEMs) at a higher cost.
Elite saw a need and forged a niche by manufacturing OEM-quality replacement parts, combining the OEM’s focus on engineering with the innovation and flexibility of a biomedical start-up. Elite stands out by focusing on better quality, accountability and unmatched integrity. Every Elite new replacement or re-certified part – crafted and tested by Elite – must pass the rigorous FDA CFR 21: Part 820 (cGMP) and International Organization for Standardization (ISO 13485:2016 and ISO 9001:2015) certification processes. The industry doesn’t require it, and few competitors bother with it, but Elite doesn’t cut corners. Passing the highest industry standards ensures optimal reliability and patient safety.
By treating customers as part of the family, Elite has grown its revenue to over $20 million annually and has a client list of over 1,500 hospitals and a slew of national awards. From 2017 to 2021, INC. 5000 magazine named Elite as one of the Fastest-Growing Private Companies in America and they are a four-time Manny Award winner for Top Growth

in Manufacturing. But profits or accolades are not the top priority, they are a by-product of the Smiths’ commitment to helping patients and creating a better industry.
In addition to their core business and as a result of the pandemic, they founded Elite Precision Plastics (EPP), which contract manufactures custom plastic medical products and disposables, to address ongoing supply-chain issues. EPP continues to grow quickly due to the large need for onshoring manufacturing. Recently, Elite was approached by one of their larger independent service organizations to begin training the ISO’s newly hired biomedical technicians. Thus, Elite started an AAMI-certified program that provides training on both OEM and Elite products. They are currently in the process of creating a national networking group of biomedical technicians. With many biomedical technicians about to retire and fewer people entering the profession, Elite saw this as an opportunity to train these unsung heroes of hospitals who are responsible for maintaining aging, critical equipment.
Though only 11 years old, the seeds of Elite were sown during summers in the late 1970s when Jeff worked for his dad’s heating and air conditioning business in Bryan, Ohio. He watched his dad, a former salesman, focus on people, not profits. And he saw the pride his hometown had for manufacturing. Though only a community of 10,000, Bryan was home to the Etch A Sketch, Dum-Dum suckers, and played a key role in supporting Detroit’s automanufacturing.
Those summers sparked his dream to someday own a company with the same values shared by his father, and his hometown. After studying finance at Ohios Miami University, he chose to go into health care. “There are plenty of other widgets I could sell, but I wanted to sell something that I believed in,” Jeff says.
He started his career in sales for original equipment manufacturers (OEMs).
“When I started, the OEM sold the best product in the marketplace,” he explains. “Unfortunately, we kept getting bought by other companies focused on improving profit and cutting engineering costs.”
He watched much of the manufacturing move overseas. But the turning point was when the president of the board of a
large hospital system, demanded accountability over the OEM’s product quality and the company’s position was to deflect, Jeff knew what he had to do.
For two months, he worked nearly round-the-clock securing rental pumps until the product he sold was fixed and ready for patient care. But Jeff was done with OEMs. For the next 11 years, he was COO of a start-up that repaired, rented and sold infusion pumps. It was then, that he tapped his oldest nephew Nate as a sales representative, who eventually became vice president of sales.
“Nate and I were running everything and knew we wanted to build it into something that was what the OEMs used to be, but we didn’t have the fiscal responsibility and the ownership,” Jeff says. “Nate and I controlled all sales and operations and successfully grew that business.”
Other Smith family members joined Jeff and Nate, including Jeff’s daughters, Alex Heileman, Elite’s COO, and later Madison Trejo, now Elite’s Chief Vision Officer. In addition, they recruited and hired Nate’s two brothers, Travis Smith, and Tyler Smith, for sales.
“We were very successful but unfortunately the owner ended up having to declare personal financial bankruptcy in 2012 and the company ceased all operations.” Jeff explains. This left the Smith family without jobs and in search of potentially new careers.
Jeff and Nate saw their chance to make high-quality, American-made replacement parts. They bought the manufacturing end of the business and opened Elite Biomedical Solutions with a team of eight (also known as “The Elite 8”). Along with family members, they recruited key employees from the former company to join them in June 2012. Nate and his brothers plus Sarah Noggle focused upon sales. While Jeff, Alex, Jeff Diesel and Jeremy focused on operations. “We center ourselves on our commitment to patient safety, our customers, our employees and our community,” says Nate.
It’s an approach that earned a solid reputation for dependability and savings. “We use a fair pricing structure that offers an average of 30 percent annual savings for our customers,” Nate explains.
The secret sauce is in the process. Every Elite part begins with the product development team – biomedical engineers, process engineers, plastics engineers, quality engineers, biomedical equipment technicians and leadership team – taking an OEM part and reverse engineering how to improve it. FDA requires form, fit and function restrictions that can’t change, but

other variables are examined, tested and explored to extend the life of the part. They analyze competitors’ products and compare them to their own product lines. Frequently resulting in products that outperforms the competition.
When patients’ health is on the line, validation, verification and documentation matters. Elite performs the highest level of testing to ensure the highest level of product quality. “We have to test for every possible scenario,” Jeff explains.
The lifespan of an average infusion pump is seven to 10 years, with a 20 percent failure rate after the first couple of years. “Most hospitals are changing out a fleet to parts once, if not twice,” says Nate. “Parts can degrade due to the level of cleaning agents utilized and the amount of wear and tear they endure. This is why it is critical not to utilize cheaper resins to manufacture the part.”
Madison Trejo adds, “We’re creating parts that can save or prolong a device’s useful life. The same devices that are utilized on hospital patients. You can’t mess that up.”
“Our goal is to have a competitive advantage and ensure that those companies follow the same rules to ensure patient safety,” Nate explains. “If you’re going to do this, you need to do it the right way.”
Elite is one of the first third-party companies to earn true ISO certification, registered and recognized by the U.S. government. And it remains one of the only companies to withstand three FDA audits to date.
Quality control is just as critical at the manufacturing and assembly stages. At Elite, employees are empowered with authority to stop the process if something doesn’t meet the quality standards. Such safety scrutiny hardly slows down Elite’s production. The company’s Cincinnati plant handles thousands of pieces per month and main -
tains several months of inventory to meet any backorder issues that an OEM might have.
Jeff and Nate knew the difference they wanted to make with Elite, but they never envisioned that a global pandemic would change health care. Thanks to their healthy inventory, they could pivot in early 2020. “We were able to facilitate the needs of hospitals right off the bat by putting pumps on hospital shelves,” COO Alex says.
Deemed an essential company, Elite worked hard to ensure that infusion pumps would not be part of the same supply woes as the other supply shortages. They increased their technical support to fix IV pumps and rented pumps to assist in helping their customers.


Early on during the pandemic, the company researched manufacturing syringes, which were being sold to other countries for the highest profit and creating a shortage in the U.S. during the pandemic. After several months of investigating the feasibility for Elite, instead the exercise inspired a new product – a collection container for the pharmaceutical and biotech companies in Cincinnati – and launched Elite Precision Plastics. Creating a new contract manufacturing business that customized biomedical products is a new way to further the Elite culture of making an impact.
With new medical products developed by Elite Precision, Elite is poised to enhance its presence in the medical marketplace. Each innovation and opportunity to help keep patients safe is anchored by the Smith family values, which are at the very heart of Elite.
“We put patient safety first, always,” Madison reflects.
For more information, visit elitebiomedicalsolutions.com.
When patients’ health is on the line, validation, verification and documentation matters. Elite performs the highest level of testing to ensure the highest level of product quality.





here are organizations that develop and publish standards adopted by entire industries. These standards create guidelines that ensure consistency, specifications and characteristics in products, processes and materials.
AAMI covered healthcare technology management (HTM) career progression in its “Career Planning Handbook,” illustrating a leadership progression path, a technician progression path and a clinical engineer career path. The guide delves into the accrued skills and experience garnered at each level.
Nomenclature has crept into many facets of life, and the HTM profession, through a meeting of minds, evolved into a more accurately defined profession with the introduction of healthcare technology management as a more apt descriptor.
While many biomed departments have embraced this updated description, the descriptions for positions within an HTM department have lagged, with no standardized nomenclature. An industrywide standardization of titles is not required, however the articulation of titles, roles and responsibilities, along with remuneration, is an important topic.
Leadership within HTM organizations have been focused on determining the titles and salaries of their HTM staff based on capabilities, responsibilities, roles and focus. The efforts of leadership have been determined more on getting these things right within their organizations instead of an effort to align titles and roles across the entire profession.
Perry Kirwan is vice president of technology management at Banner Health in Phoenix, Arizona.
Kirwan says he doesn’t see much disparity in the titling of general biomedical technicians and imaging service engineers. He says that the titling of the roles that go beyond these two areas, such as roles in cybersecurity, medical equipment planning, application management, technology specialists, database/CMMS administrators, might be the exception.
He says that while the titling of the biomed and imaging positions seems mostly consistent, it is defining what each position means and what is expected in terms of capabilities of those who hold a particular title, that may present some disparities.
“The other issue is salary range within those positions and continuing to find a way to calibrate those in such a manner that it reflects the talent and skills that it takes to be an HTM professional at any level. What I’d like to see is work to try and standardize what the requirements are between the levels because you should expect a BMET I, II, III, etcetera, to be of a certain caliber anywhere you go throughout the country,” Kirwan says.
This is why having some consistency within a biomed department with position titles, expectations and responsibilities can help with defining those positions more clearly and finding candidates who are the best fit for the position.
“I determined job titles for my program by my experience as an HTM professional through the years. One of the biggest influences on my job description structure was the disparity I saw with technicians who had medical imaging system experience versus ‘biomeds.’ The imaging engineers acted like prima donnas. They looked down upon the ‘biomed’ and the lack of teamwork and respect was palpable. This was troublesome to me, and I vowed to work to make the playing field more suitable to teamwork,” says Christopher G. Nowak, CBET, CHP, CSCS, senior director of healthcare technology management at Universal Health Services (UHS) in King of Prussia, Pennsylvania.
Nowak says that when he developed the job titles for the HTM program, he wanted to recognize the strengths of the skill sets that each employee brought to the table and what could be contributed to make the patient experience exceptional, i.e., little, if any downtime to medical devices.
“This meant that the value that an experienced imaging systems technologist brought was equivalent to the value an experienced clinical laboratory technician brought. HTM professionals who brought an IT skill set were equally compensated based on their experience, competency, and value they brought to the program. I did not want the technician working on the nuclear camera performing a PM, to not touch the physiological gating monitor sitting in the corner because that device is a ‘biomedical’ device and beneath me to also perform the PM on that device. That inefficiency drives me crazy. I sought to streamline the role responsibilities to gain efficiencies,” Nowak says.
Applying critical thinking to the process of determining job roles and compensation led one biomed director to categorize those in the biomed department into two general groups. Further delineation was then applied to these roles to determine both the team member’s focus and skills.
“When I first started in biomed at Stanford in 2007, there were only six job roles; three management and three tech roles. We had a director, assistant director, manager, lead biomed tech, certified biomed tech and biomed tech. Things didn’t make much sense, considering the work was so broad and there were varying degrees of responsibilities that overlapped most roles,” says Michael Kozuma, BSM, CBET, director of biomedical engineering/technology and digital solutions at Stanford Health Care and School of Medicine in Palo Alto, California.
He says that over the years, more job titles were added to the pool and more confusion commenced.
“When I started the journey of job title alignment a couple years ago, I was bound to the organization’s job title library. As I navigated what made the most sense without creating tsunami for the bureaucratic system most of us are boxed into. Into the first year of the process, it made sense to ‘tweak’ job roles and compensation, and I was pleasantly supported by HR, Compensation and IT (TDS) leadership,” Kozuma says.
He says that during this process, they determined there are two types of employees; project-focused and
“The general rule is all operational employees should have 10 percent of their work time available for ‘projects.’ We carved the two types of employees into different buckets within project types and operational support. The ‘end’ result is as follows: Assistant Biomed – 90 percent operations; Biomed – 90 percent operations; Certified Biomed – 90 percent operations; Lead Biomed – 50/50 percent operations/ projects; Biomed Systems Engineer – 25/75 percent operations/projects; Senior Biomed Systems Engineer – 25/75 percent operations/projects; Lead Biomed Systems Engineer – 25/75 percent operations/projects; and Biomed Applications Manager – 90/10 percent projects/operations,” Kozuma says.
He says that the assistant manager, manager, senior manager, director and administrator director are all at the needs of the department.
Differences in the terms used across the biomed field have precluded the standardization of roles and descriptions. There will need to be a large-scale effort to create real standardization.
“A lot of the issue with job titles has been self-imposed by the industry as the field developed. Much of this started with the variation in the industry and department names. We have everything to include medical equipment repair, medical equipment service, clinical engineering, biomedical engineering, medical engineering, clinical technology, medical instrumentation, clinical equipment maintenance and now healthcare technology management. Because of this, the job descriptions have varied across the industry and they continue to evolve,” says Mike Busdicker, MBA, CHTM, AAMIF, FACHE, senior director of healthcare technology management at Intermountain Healthcare in Salt Lake City, Utah.
He says that another factor in the wide variation of job descriptions includes different duties and responsibilities across the industry.
“We have caregivers working for manufacturers, independent service organizations, academic institutions, stand-alone hospitals, health care systems, and other service providers. This has resulted in the creation of multiple job descriptions to cover things like field service, depot repair, biomedical equipment, imaging equipment, dialysis systems and sterilizers,” Busdicker says.
He says that over the years, many of these titles and job descriptions have been adopted and utilized by organizations across the industry.
“It would be great if we could get these standardized and everyone using the same terminology and titles. Some of the issue is the resistance, or reluctance, to change and the desire to stay with the current terminology,” Busdicker adds.
Nowak says that he suspects the reasons why job titles are not standardized relate to the difference in leadership in the career field.
“Some leaders have not evolved as the technology has evolved. Some leaders have not recognized the changes to the fiscal pressures, i.e., the need to drive efficiency. Having an

“I determined job titles for my program by my experience as an HTM professional through the years. One of the biggest influences on my job description structure was the disparity I saw with technicians who had medical imaging system experience versus ‘biomeds.’ ”
- Christopher Nowak
‘imaging engineer’ sitting at a computer reading a newspaper or watching a video movie while the ‘biomed’ team is killing themselves trying to complete the infusion pump planned maintenance cannot happen in 2023,” he says.

He says that everyone is on the same team and helping one another achieve the goals of the department is tantamount to the success of providing patients and the clinical staff, who directly treat the patients, with a great experience.
Determining both titles and compensation can help more clearly define roles while providing some transparency regarding expectations and rewards for contributions.
Kozuma says that compensation is a challenge to overcome and that there is still work to be done.
“We restructured the pay scale to align with job roles, duties, responsibilities, and difficulty, alongside individual qualifications such as education and experience. It was far too common with the old biomed structure, for someone with similar qualifications to get compensated lower than another employee a grade or two, sometimes several grades below,” he says.
Nowak says that he has five technical positions in the career ladder.
The entry-level role is MST (medical systems technologist), then there is the MSET I (medical systems engineering technologist 1), MSET II (medical systems engineering technologist 2), MSET III (medical systems engineering technologist 3) and the Senior MSET (senior medical systems engineering technologist).
“There are no ‘imaging engineer’ titles because the compensation plan for the role’s rewards experience, competency and the value proposition that is delivered by the technician. As an example, the person with an imaging service skill set, but with little competency since they may be inexperienced, i.e. cannot change an X-ray tube and perform required calibrations, is compensated similarly to the biomedical
professional who might not be able to work on clinical lab gear or perform anesthesia system planned maintenance,” he says.
“I have witnessed that since developing and deploying this strategy of job descriptions, the teamwork among the technical staff is very effective. No longer is there an us-versus-them attitude among the team,” Nowak adds.
When a biomed is applying for a job, the disparities in job titles and responsibilities across health care systems may result in expectations or assumptions that are incorrect.
“Absolutely, at times job titles may not accurately reflect the overall duties, responsibilities and span of control of the position. For example, health care systems across the country vary in size and the job titles within healthcare technology management are not always consistent. Leadership positions can range from vice president of CE to HTM manager. This disparity can cause a difference in pay along with several other implied job duties, responsibilities and educational requirements within the industry,” Busdicker says.
Kozuma agrees and says that these assumptions are common.
“We often have experienced biomeds apply for senior or lead roles because they are used to the ‘time in service’ mentality. Just because you did a biomed job elsewhere, doesn’t qualify you by default to be in an elevated role. In addition, the senior biomed systems engineer is a biomed that manages multiple systems and can handle the project aspect in a project manager capacity. Lead biomeds must be able to flow between operations and projects. A biomed with 10 years of bench work experience will most likely not be the right fit for these roles,” he says.
Nowak says that the technical skill set, the clinical skill set and the personality must mature as the technician grows in the career field.
“Fixing a medical device is only one aspect of the total repair process. ‘Fixing’ the clinical or technical (lab tech, rad tech, respiratory therapist) professional who uses the medical device must take place and that requires a mature personality. The ability of the technician to communicate and provide the clinician or technical professional with the confidence that the medical device is repaired and ready for service is critical to the success of patient care. If I have a 20-year technician who all they do to contribute to the team is fix infusion pumps, then that person does not qualify for a senior level technologist. Time in service is not the arbiter of position or compensation,” he says.
While few leaders in HTM expect a national standard anytime soon regarding titles, skill sets and expectations; most are focused on a well-defined structure within their own departments to make clear what a particular title entails along with expectations and compensation.
Within the efforts to ascertain that HTM is a true profession by any measure, the precise defining of a position is a key ingredient.
“We had a director, assistant director, manager, lead biomed tech, certified biomed tech and biomed tech. Things didn’t make much sense, considering the work was so broad and there were varying degrees of responsibilities that overlapped most roles.”
- Michael Kozuma
The Philips iE33 and iU22 have been a significant part of my life for the past 13 years. When I started working on A cart iU22’s and iE33’s back in 2010, I knew absolutely nothing about the machine. This machine has been a big part of my third-party multivendor ultrasound service work life and career ever since. I have worked on over 200 of these machines over the years and have helped troubleshoot 200 more over the phone. On many occasions, I have had sonographers ask me if I am or was a sonographer because of how familiar I am with the system. I know everything about these machines, from settings, applications, networking, error codes, and error logs, I know it all and I cannot imagine my career without them. Sometimes I feel like I know these machines better than I know myself.
Over the years I’ve replaced every possible circuit board, bezel and cable. I’ve replaced Firewire cables to molex cables, video cards to SPD boards, and front casters to the bicycle cable that controlled the rear swivel on A/B/C/D carts. I know this machine just as well as I know my #1 Philips Wiha screwdriver. There have been many long nights wondering if I should’ve ordered a host instead of a SIP or a channel board instead of a NAIM, and there have been many channel board and video card “swappy roos.” I can’t count on my fingers and toes how many times I’ve told a sonographer to plug a qwerty keyboard into a USB port behind the DVD drive until I am able to show up and replace the keyboard cable and cable guide. The iU/iE has a deeper meaning than just an ultrasound machine to me. It has been with me from day one and has been a big part of my ultrasound life ever since. I know other machines very well, but I know this one the best. I’m great on the Epiq/Affinity, CX50, Sparq, and I know all GE products very well. I’m good with the Samsung/Medison and I can handle Siemens products well, but this machine is my guy. I believe that if you can maintain A/B/C cart iU22’s and iE33’s, especially if they go mobile, you can take care of any ultrasound machine.
New ultrasound technologies really excite me as an ultrasound field service engineer and these technological advancements are the main reason why I love what I do so much. With that being said, I recognize that this machine should not stick around forever. Just like the ultrasound machines that came before it (HP Sonos 5500, ATL HDI 5000, etc), there is a day where the passing of the torch must happen to make way for the latest and greatest technological advancements.
The A/B/C carts were deemed EOL (End of Life) by Philips on December 31, 2021. Avante and I still support these machines in a limited capacity. The D/E/F/G/R carts were also deemed EOL by Philips on December 31, 2022, and we’ll continue to support these as well. I love these machines and still believe that they serve a useful purpose in the field. I will happily and willingly continue to work on these machines until there are no longer parts available to support them. And when that day comes, I might shed an inaudible, high frequency, 5 MHz, ultrasound tear and I will pour out a bottle of Transeptic Cleaning Solution Spray in its memory. LONG LIVE THE iE33/iU22!
“Avante Health Solutions is committed to empowering the biomed community with outstanding training programs. We offer comprehensive hands-on ultrasound and diagnostic imaging training courses and capabilities that are designed to provide health care professionals with the skills and knowledge necessary to operate and maintain imaging equipment,” Avante Marketing Communications Manager Carissa Diaz said. “By providing cost-effective, hands-on and practical training, engineers are immediately able to impact the bottom line of day-to-day operations.”
For more information about Avante’s training capabilities visit these links:

• Ultrasound Training: avantehs.com/ultrasound/training
• Diagnostic Imaging Training: avantehs.com/imaging/training
Lyle Cmerek is a Senior Field Engineer servicing Texas, with over 13 years of experience as an ultrasound field service engineer.
























t’s a situation that happens frequently: The company you work for is hiring and a good friend is asking for a recommendation — but you don’t have any experience working with him in a professional capacity. How should you respond?
The first step is to assess the friend based on competencies you can judge. That includes considering if the friend’s previous experience and education makes them a good potential match for the job, says career coach Jeroen De Koninck, founder of the career coaching platform Preppally.
Erny Peibst, founder and CEO of Inside Bodybuilding, echoes that advice.
“Since you have intimate knowledge of your job, and knowledge about what it’s like to be friends with this person, you can extrapolate what working with them would feel like,” Peibst says.
“Is this friend reliable? If you’re meeting up for a party or event, do they show up on time? Do they fulfill their responsibilities and obligations? Would you enjoy working with them?” The answer to those questions, he says, “can help you decide whether they’re worth mentioning to your boss or HR team.”
If it ends up you don’t want to offer a recommendation, don’t.
“If you feel like they won’t be a good fit or are unsure, tell them to go through the regular application process and you’ll see what you can do to pass your name along to the powers that be,” suggests Jonathan Marshall, owner at New Jersey-based The Law Offices of Jonathan F. Marshall.
If you think the friend is a good candidate, proceed with a recommendation, says De Koninck, who notes that employee referral programs often allow employees to indicate whether a referral is a “network” or a
“professional” connection. Even if there isn’t a formal process for indicating that information, “it’s best practice to include this [somewhere] within your referral itself,” he stresses. “This will create credibility: You have assessed the person to your best knowledge and within the best interest of the company.”
“If you feel comfortable, there’s nothing wrong with gently passing along the name of your friend to someone in your company,” Marshall adds. “You don’t have to sing their praises, but there’s nothing wrong with just passing it along with a short note.”
Then, it’s up to the recruiter and hiring manager.
“They will have the necessary information to evaluate your judgment and understand you act out of interest for all parties involved,” De Koninck adds. “You have informed the company the candidate is a network connection and hence you are limited in your assessment.”
“Don’t do anything you aren’t comfortable with, but also understand that you aren’t responsible for the final decision if you do pass along someone’s name for a recommendation,” concludes Marshall, who notes he never blames anyone for a referral that doesn’t pan out successfully.
“I will always go through my own process of interviewing, and the final decision will be on me. I don’t think it’s fair to blame someone who recommended a friend, because hiring managers and company leaders are the ones who always get the chance to make the final decision.”
Kathleen Furore is a Chicago-based writer and editor who has covered personal finance and other business-related topics for a variety of trade and consumer publications. You can email her your career questions at kfurore@yahoo.com.

ur industry is constantly evolving. It goes without saying that medical device service is a fast-paced and dynamic field full of both challenges and opportunities. With much of the industry struggling with limited resources and an aging workforce, there’s an abundance of knowledge and skill gaps that desperately need to be filled.
With that being the case, as an industry we are always on the lookout for new strategies to give us an edge. Whether it’s GPS device tracking platforms, new workflow automation apps, or a number of new AI productivity tools, techs in our industry are fairly good at adopting new technologies – as long as they promise to help us manage our workloads. So, what’s the next wave? Could the next technology that is showing great promise be extended reality? We feel that with its immersive and interactive nature, VR has the potential to completely revolutionize and democratize the way BMETs, and all health care professionals, are trained. Let’s explore the potential of VR and XR technologies in the biomedical equipment industry and how they can improve the quality of training, support and patient care.
Let’s start with a 30,000-foot view. Virtual reality (VR) training and emerging technologies have been making a significant impact on various industries. With VR success stories coming out of everything from welding and automotive to clinical training programs,
the data is showing that virtual scenarios significantly increase both speed to competency and retention. And according to a study coming out of UCLA, VR simulations drastically improve performance of surgeons. In the study, 20 surgeons were to perform a procedure to repair a fractured tibia. The results showed that the surgeons who simulated the procedure in VR before the real procedure were six times less likely to make a mistake during the procedure and they completed the procedure an average of 20% faster.
The biomedical equipment technician sector is no exception to the rule. We are already seeing adoption of these technologies provide a more engaging learning experience compared to traditional training methods. At the 2022 AAMI eXchange, nine BMET students (no prior experience) participated in a proof-of-concept virtual reality training on a contrast injector PM procedure. The training was put on by the Imaging Academy and Maull Biomedical. After spending 20-30 minutes in a virtual simulation, all nine students were able to successfully perform a full PM procedure on a live device in less than two hours.
Essentially, VR improves performance by providing a more immersive and interactive training experience for medical device technicians, making it easier for learners to understand and manage complex medical equipment faster. By keeping learners interested and invested in the training process, VR and XR can lead to better retention of information and better performance in the field. Most of us agree that in this industry, the best way to learn is by doing. VR training provides that opportunity anytime, anywhere.
One of the main benefits of VR training is simply that it provides a realistic and safe environment for
technicians to learn how to service and manage medical devices. VR simulations can simulate a variety of scenarios and medical equipment malfunctions, which can help technicians become more prepared for real-life situations. By using VR technology, BMETs can practice their skills and troubleshoot potential issues without the risk of damaging real medical equipment or putting patients at risk.
VR technology can also help reduce training costs for medical device service and management companies. Traditional training methods can be costly, as they require travel expenses, equipment logistics and instructor fees. However, VR training can be accessed remotely, which can reduce travel expenses and eliminate the need for physical training equipment. Additionally, once the VR simulations have been created, they can be reused indefinitely.



Emerging technologies such as augmented reality (AR) and mixed reality (MR) can also provide valuable benefits to medical device service and management companies. AR technology can overlay digital information onto real-world objects, which can help technicians identify and troubleshoot problems in real-time. AR technology can be used to provide step-by-step
instructions for equipment maintenance or repair. MR technology can combine the benefits of VR and AR, allowing technicians to interact with virtual objects in the real world. This can be particularly useful for complex medical equipment that requires a high level of precision and accuracy. We believe that while VR shines for initial controlled environment training, AR and MR really show a strong utility in the real-time field repair applications.
In conclusion, we at NVRT Labs, believe that VR/ XR training and emerging technologies have the potential to become the next technology megatrend in our industry. It may only be a matter of time before every device sold has an accompanying XR training module. It could be a very good thing for the whole industry if one day there’s an XR headset in every biomed toolbox in the country.
When we don’t have access to the repair materials we need to fix our devices, we don’t truly own them. A manufacturer’s decision to stop providing software support can turn our software-enabled devices into unusable hunks of junk – ‘bricks’ of plastic with nowhere to go but the scrap heap.
Sonos provided a notable example of bricking. In 2020, it announced that customers would have to put their smart speakers into irreversible “Recycle Mode” to take advantage of a discount on a new product. Sure, the discount is nice, but why ruin a perfectly good speaker in the process?
Sonos ended up reversing this policy after significant blowback, but that hasn’t prevented other companies from temporarily or permanently bricking smart homes, toasters or tractors by ending software support or withholding repair software and materials needed to put the devices back into use.
Unfortunately, some medical devices are doomed to be another brick in the wall of electronic waste. Let’s look at two examples.
Stryker’s Sterizone VP4 Sterilizers are used to sterilize flexible endiscopes, cameras and – during the pandemic – respirators or even N95 masks. Effective cleaning of such reusable products is critical to the safety of patients and staff alike. VP4s can cost roughly $100,000 and require a service contract of up to $120,000 per year, one biomed told me, but no service training was available to him or his team.
That high cost was one reason that this biomed (who asked to remain anonymous for fear of retribution) was so frustrated when he received a letter from Stryker announcing that they would no longer support the device. The letter states:
“In November 2022, a business decision, not related to the safety or efficacy of the product, was made to suspend the sale and manufacture of VP4 capital equipment. Maintaining parts and service on the VP4 has become increasingly complex and challenging. After careful consideration, we will no longer offer service and disposables sales effective December 31, 2023.”
It’s one thing to make a business decision to stop manufacturing a given product. The Right to Repair movement is not about forcing companies to continue making devices that are no longer profitable.
Even ending service support for devices – provided the materials needed to physically and digitally repair them are publicly available – can be defensible. But when manufacturers monopolize service, they have the power to condemn owners’ products to an early grave. They have the power to force the owner to buy new products before their old one is obsolescent.
That fact was plaguing the biomed who sent me Stryker’s letter. “For the $20k Stryker birthing bed I just bought, they have to know that I’m wondering if a Stryker executive is going to decide tomorrow to no longer supply parts and accessories?”
“THEY SENT ME BACK A BRICK THAT WOULD NEVER TURN ON AGAIN”
Manufacturers sometimes go beyond just ending service support of a product. They physically destroy it.
That’s what happened to a biomed who sent his story to YouTuber and Right to Repair advocate Louis Rossman. This biomed was having trouble with his Eitan Sapphire epidural pump, which is used to manage patients’ pain by injecting an anesthetic or steroid into an area around their spinal nerves.
In this case, the biomed said one of his hospital’s pumps was giving false occlusion alarms, essentially reporting a blockage in flow when there was none. The biomed started troubleshooting: “I tried changing tubing set, making sure we have brand name OEM tubing; adjusting the occlusion sensitivity … I even contacted their clinical support team to make sure that the nurse was using the pump properly per Eitan instructions,” he explained in his video account. “None of this worked.”
Eitan doesn’t sell all replacement and repair parts, the biomed said. So, he turned to a measure of last resort – sending the device back to the manufacturer for repair. He explains, as Right to Repair advocates often argue, in-house service “not only reduces the cost of repair to the hospital but it reduces downtime,” meaning the device can be back in use providing patients with the care they need more quickly.
Because the pump was one year outside of Eitan’s serviceable lifespan of seven years and the problem required more than a simple screen or case replacement, Eitan technically would not support the service. The biomed said that the company had him send it in anyways.




What he got back was shocking. The manufacturer slapped an “out of order” sticker on the front of the pump. “They cut the connection going to the battery. They nicked the wires going to the motor. They shoved a flathead screwdriver through the ribbon cable. And, to top it off … they cut the screen cable,” the biomed explained. “They absolutely demolished this pump. It will never turn on again.”
If you took your car into the dealership and the mechanic noticed your tire tread is low, you wouldn’t expect them to return your car with slashed tires. You’d be furious. That’s essentially what happened with this epidural pump.
The biomed says the manufacturer told him that they did this for his liability. It’s hard to argue with Rossmann’s description of this behavior as gaslighting. “We’re not toddlers. We don’t need choices of liability being made for us by some company,” the biomed said. “We’re all adults here. We can deal with our own issues.”

Without access to comprehensive repair materials, manufactur ers retain immense amounts of control over the devices you buy and own. In health care, that means your devices can be bricked – or even destroyed – because of a business decision or corporate policy.


Manufacturers might argue that they’re doing this for your safety, your liability. These products are incredibly complex, they say.
The biomed with the pump problem put it best: “With new technology comes new technicians. We will always be able to fix our stuff – unless companies stop imposing these artificial repair restrictions. It’s absolutely nonsense.”










e’re often asked, “How did you get in the business of repairing ultrasound probes and MRI coils?” It’s actually a very interesting story. To keep it simple … as a former manufacturer of MRI coils and current FDA registered manufacturer of ultrasound probes, Innovatus Imaging has the in-house engineering talent, proprietary fixturing and instruments, and expertise to fully understand the technology we repair. Innovatus is both an original equipment manufacturer (OEM), and an independent service organization (ISO). It’s quite unique in the HTM industry. Let’s look at ultrasound probes as an example.
Innovatus maintains two facilities dedicated to ultrasound probes: An FDA-registered Center of Excellence for Design and Manufacturing in Denver, Colorado, and a Center of Excellence for Ultrasound Repair in Tulsa, Oklahoma, which together combine to address the entire life cycle of ultrasound probes … design, engineering, manufacturing and, finally, providing repair solutions that meet OEM form, fit

and function as well as safety and efficacy.
Like any medical device, an ultrasound probe begins its design life cycle as a series of user needs, intended uses, requirements (or design inputs) and ultimately ends as a finished medical device. There is a tremendous amount of effort, years of planning and continual testing that occurs in-between. Some of the major requirements include electrical, mechanical, acoustic and chemical verifications and validations. Other seemingly minor requirements might be the color of the probe housing, its shape and the degree of protection from fluid and dust intrusion (IPX-rating).
Our Denver facility manufactures ultrasound probes from concept to production and must follow FDA regulations every step of the way. Every device manufacturer needs to prove that they are manufacturing a safe and effective product. Two important questions that need to be answered by every device manufacturer are:
• “Does the output equal the input (or design specifications)?”, or “Did I make the product correctly?”
• Just as important is answering the question, “Does the product meet the user’s needs and intended uses?”, or “Did I make the correct product?”


Many of the same FDA current Good Manufacturing Practices (cGMPs) and philosophies are transferred and implemented when we engineer solutions for your products in our repair centers. The goal in our repair operations is to return a product, whether a probe or a coil, to OEM form, fit and function and not alter safety, performance or intended use. Because Innovatus is a manufacturer, we have all the necessary instruments, knowledge, training and processes to ensure this outcome. We’re also able to design and manufacture proprietary test and repair fixtures based on the design of the various OEM makes and models.
Let’s look at a common failure on an ultrasound probe, intermittent or broken wiring in the system cable. There are several solutions available to independent service providers and one that is definitely not. OEMs of ultrasound probes will not sell components to ISOs.
Solution 1: There are one-size-fits-all cable replacement solutions available in the aftermarket space, but there are many electrical parameters to consider (characteristic impedance, DC resistance, capacitance, shielding) and physical characteristics (length, diameter, color) which differ for almost every probe model.
Solution 2: Re-termination involves cutting-back a cable past the point of damage and then re-terminating it to the probe. Although this practice is widely used in the repair industry, cutting-back too much of a cable, or splicing individual micro-coaxial wires, can alter the electrical properties of the OEMs design, ultimately affecting performance.
Solution 3: Harvesting used cables to replace the cable on your probe. There is a risk to re-using an already worn, potentially over-flexed cable. The repair provider is betting that his solution will outlast his warranty period.
Solution 4: Fabrication of a replacement cable. Using sophisticated instruments, Innovatus benchmarks new OEM cables (by probe model) to determine their specifications and then designs to those specifications. The cables are then stress tested using customized “torture” devices as well as undergoing electrical and acoustic verification. In fact, we currently manufacture over 90 different
wiring harnesses and cables to ensure performance consistent with OEM design.
Replacing plastics and lenses may seem simple until you research the hundreds of OEM recommended cleaners and disinfectants for the hundreds of probe models we restore. All materials used by Innovatus must not only be compatible with recommended cleaners and disinfectants but also ISO 10993 compliant (biocompatible).
Once our Design and Manufacturing Center completes and approves a material or process, it then transfers to our ISO 13485:2016 registered Ultrasound Repair Center to be implemented into our probe repair processes. This is a continuous, evergreen, process as new devices enter the market, as each model will have different characteristics and unique designs which we have to engineer.
As mentioned above, our single goal is to restore safety, performance and OEM design intent to the products that your clinical teams use every day – not just getting it working again … and do so at a highly competitive price. There are no short-cuts taken to save costs, yet Innovatus provides OEM quality at ISO pricing. We encourage potential clients to perform a true apples-to-apples comparison between providers. You’ll find that, for the same level of and approach to repair, Innovatus actually provides greater longevity and long-term value to your facilities.
As an OEM, we understand the entire life cycle of the products we support. After more than 180,000 probe repairs and 40,000 MRI coil repairs, we understand not only how they fail but how to restore them to provide many additional years of patient care. Learn more at innovatusimaging.com.
Ted Lucidi, CBET, is the director of commercial operations and business analytics at Innovatus Imaging.
“The goal in our repair operations is to return a product, whether a probe or a coil, to OEM form, fit and function and not alter safety, performance or intended use.”
t’s summer – the time of year when our biomedical engineering technology students at Penn State New Kensington typically are completing their internships and preparing for graduation. Of course, this means that they are also looking for their first jobs in the field. Therefore, I thought it would be a good time to share some tips for job searching, as they could be helpful not only to students and recent graduates looking for their first position but also to anyone looking for a new opportunity.
When looking for a new opportunity, I’ve heard people say that “who you know is as important as what you know,” and I believe that there is some truth in that. Classmates, previous coworkers and even people that you’ve met at a conference could help when looking for that perfect position. I’d also recommend checking in with your alma mater. I often have contacts who reach out to me with opportunities, not only entry level, but also for more experienced professionals, and I’d be happy to share these with alumni. Our campus job board also lists these positions, and I would think that other schools have similar resources.
I’ve had several recent graduates use LinkedIn to find positions. LinkedIn can be a great way to make connections that could lead to opportunities. I’d recommend creating a professional looking LinkedIn profile and keeping it up to date. That way, a prospective employer might find you. If you are looking to work in a certain city or for a certain company, a LinkedIn search can help you to connect with people who work there. HTMjobs.com is another great free resource for people looking for a healthcare technology management job.
Everyone has their own preferred style for resumes. Rather than focusing on that, I’d suggest looking at the job posting when writing a resume. That way, you can include key words in your resume and focus on required skills. My preference is to show where you have applied skills in jobs or activities on your resume rather than just listing the skills. I’d also recommend thinking of examples you could give during an interview for
each skill mentioned on your resume. Finally, advice that I always give my students is to make sure to check the email and voicemail for the number on their resumes on a regular basis.
I always recommend writing a cover letter, especially if the job posting asks for one. A cover letter offers the opportunity to explain how you are a good fit for the position. My first piece of advice on cover letters is to focus on what you can contribute to the company rather than what the company can do for you. My second piece of advice is to write it in your own, normal words rather than using fancy words and canned statements that don’t sound genuine. Finally, make sure that the letter is addressed to the correct employer (if you are applying to multiple companies).
I’d suggest having a list of professional references available when going to an interview. I’d also recommend asking people if they are willing to be a reference before giving their contact information to a perspective employer. One of my pet peeves is getting a call or email asking me to provide a reference for someone when I wasn’t even aware that they were looking for a job.
I believe that the best way to be successful in an interview is to be prepared. I’d recommend taking some time before the interview to learn about the company for which you will be interviewing as well as the position. Another good way to prepare is to practice answering typical interview questions. There are many lists available online. I’d also suggest thinking of some questions to ask, as that is a good way to show interest in the position. After the interview, it is a good idea to follow up with a thank you note or email.
While this is certainly not an exhaustive guide to getting a job, I hope that it provides a few tips and things to think about when applying for a first job or a new position. Finally, I want to congratulate all of the 2023 graduates and wish them luck in their job search and new careers!
Joie Marhefka, Biomedical Engineering Technology Faculty at Penn State New Kensington.


reventative maintenance and backups can help ensure your Hologic Dimensions or 3D Dimensions system stays up and running. In this article, we will explore how you can create AWS backups, where to properly store them, and WHY you should store them.
Backups are one of the most important things to have for your AWS system for a few reasons. First, backups ensure you have the latest information on your system. Second, you’re not waiting on the OEM to assist in gathering this information for you.
While Hologic backups are not automatic, there are options to save your own backups to keep handy. Below we will discover how to create backups, your backup options, how to gather important files, and how to save those files.
There are a couple of ways to create a backup in system tools.
• Step One: Log in to the application as a service. Then we will click Admin System Tools
• Step Two: Once in System Tools go to Troubleshooting
Troubleshooting Backups Create a Backup
You will then be given five options before you
create your backup. Click the corresponding box next to the backup option you would like.
Here is an explanation of what each option includes:
1. Licenses – As is stated this will get all your licensing.
2. UsersDB – The tech logins and any other user on the system login page
3. MainDB – Patient database
4. ConfigDB – All settings within System Tools. IE. Site name, DICOM, CPT codes
5. RejectFiles – Reject repeat files
The system will default to Licenses, UsersDB, and ConfigDB. In PM cases, these options will be sufficient. A time when you would want to select all would be if you were replacing a computer that same day. As the patient database and reject repeat files change as the system is used.
After you have created your System Tools backup, we can move on to gathering important files. Note: You will need to know your detector serial number to achieve this.
• Step one: Navigate to the About screen in the application.
• Step two: Login to your system
• Step three: Locate the gantry icon on the bottom right of the screen Click the icon Then click About.
• Step four: In the About screen, you will find your
detector serial number in the Detector section.
Once you have your detector serial number, you can start saving your files.
Create a folder on the desktop. Pro tip: I normally name the folder Backups with the current date. Next, copy and paste these files into your Backups folder on the desktop.
• C:\Licensing – Here you will find your license file. Depending on the software version this will be either a. HOLX or. XML file.
• C:\Gemini\Data\m35 – Here you will find your detector files. the files you are: (detector SN).map, (detector SN).dlc, (detector SN).llc, (detector SN). cfg. IE. YM837654.map, YM837654.dlc, ect.
• C:\Caltool_xfer – Here you will find your node calibration data. These will be .txt files. I recommend you pull all of them.
• C:\Backups\manual – Here you will find the System Tools backup we created earlier. These will be .zip files and you will pull all of them.
• C:\Gemini\data\HVL – Here you will find your HVL. You will only need to pull the Subsystem.tubeoutput.xml file.
• The last thing you will want to copy is your IP configuration info for the PC. I found that using a command prompt to make the ipconfig info into a text file is the best way. To do this open a command prompt and change the directory to the desktop. Then run the following command. “ipconfig /all >> IP.txt”
Once you have all the files to the desktop, be sure
to load onto a new external USB drive to be easily found by yourself or the next engineer who will work on the system.
And there you have it! You now have everything you need to restore the system in case of a crash. Be sure you pull the backups folder off the system to access them later in case of a crash.
As with any mechanical device, computers are prone to wear and tear, which can lead to malfunctions, data loss, and system crashes. To avoid such situations, it is important to prioritize preventive maintenance and regular backups.
“By taking these steps, users can ensure that the system’s computers remain in good working condition and that their important files and documents are always safe and secure.”
If you are looking for more preventative maintenance tips for Mammography or additional modalities, visit the Block Imaging Learning Center: info.blockimaging.com.

Be sure to check out my most recent blog on Preventative Maintenance for Hologic Dimensions & 3D Dimensions!
Brad Lee is a field service engineer at Block Imaging. He co-manages their Texas team, while also performing maintenance on multiple modalities.

t ReNew Biomedical, we recognize that your equipment is your lifeline as an EMS agency or first responder. You rely on it in emergencies to save lives and provide the best possible care to your patients. But what happens when that equipment isn’t calibrated right or hasn’t been maintained properly? The consequences can be disastrous, leading to delayed response times, misdiagnoses or even death.
As a medical equipment maintenance, calibration and repair services provider, our team at ReNew Biomedical is dedicated to ensuring optimal performance for your medical equipment. Regular medical equipment maintenance ensures reliability, functionality and safety, ultimately saving more lives while also easing your budget. Let’s examine the importance of regular equipment maintenance for pre-hospital response and how it benefits EMS agencies, paramedics and patients.

It’s no surprise that regular maintenance helps ensure your equipment is always ready for use. EMS and first responders rely on defibrillators, infusion pumps, ventilators, stretchers and other equipment to help save lives. Your equipment must work as fast as you do, with extreme accuracy and dependability. Calibration errors can lead to disaster. Additionally, mistreated equipment is more prone to error or malfunctions, which, at best, wastes precious time and, at worst, can have life-threatening consequences.
Regular maintenance also helps keep EMS agencies cost-efficient. Well-maintained equipment lasts longer, requires fewer repairs and is less likely to break down. This service reduces the need for repairs and delays the need to
purchase replacement equipment. Additionally, regular maintenance and calibration can detect minor problems before they become significant, meaning you lower your long-term cost of ownership.
Furthermore, regular maintenance can save time for EMS agencies and first responders. Every second counts in an emergency and any delay caused by malfunctioning equipment can be catastrophic. By ensuring that equipment is always in good working order, EMS agencies and first responders can reduce the time spent troubleshooting equipment and focus on delivering patient care.
For example, a defibrillator is vital for restoring normal heart rhythm in patients experiencing cardiac arrest. If a defibrillator is not regularly maintained and calibrated, it may cause delays or deliver inaccurate information. Regular maintenance can help detect faulty batteries, worn electrodes and malfunctioning leads, which you can address before they cause a serious problem.
Another example are EMS stretchers, a key part of patient safety. Over time, stretchers can become worn and damaged, leading to an increased risk of injury for the patient or EMS provider. Regular maintenance and refurbishing can help address issues such as worn belts, faulty brakes and broken motors, ensuring the stretcher is always in good working order.
Regular maintenance ensures your patient’s and staff’s safety and well-being. At ReNew Biomedical, we understand the importance of routine maintenance and offer industry-leading service contracts and comprehensive preventative maintenance plans to help you keep your equipment in top shape. Contact us today to learn more about how we can help you save the lives of life-saving equipment.
Jake Beals is a Content Strategist with ReNew Biomedical.
Diag nos t ic Solut ion s i s a c u s tome r se r v ice ba se d pa r t s pr ov ide r t hat s pe c ia l i ze s i n a l l i mag i ng mod a l it ie s a nd manufacturers. Created to offer hos pita l s a nd I SO’s a cos t ef fe c t i ve a nd t i me sav i ng solut ion for or de r i ng i mag i ng r e place me nt pa r t s , e qu ipme nt move s , u lt r a sou nd pr obe r e pa i r a nd on-site se r v ice.





Contac t u s today, we a re conf ident you w i l l see u s a s T H E Pa r t s Solut ion!


hat do medical device security, inventory management and equipment recalls all have in common? They are only as good as their most up-to-date information. This affects the accuracy, thoroughness and itemized information recorded in your computerized maintenance management system (CMMS). No matter how “secure” your network is, there is always a possibility for cybersecurity threats. These threats can come in many forms such as zero-day attacks, ever evolving vulnerabilities and the risk of ransomware/viruses.
The introduction of vulnerabilities and recalls on your networked, and non-networked medical devices, introduces risk to the integrity of your medical devices and, most importantly, the security and safety (both physical and information security) of your patients. How quickly and accurately are you going to be able to identify and take action to implement a remediation to protect patient information and well-being? The answer to this question truly depends on your inventory, the information your management system collects and the frequency at which the information is updated.
A : The top three reasons are safety, security and service. CMMS is a software management solution that maintains a computer database of all networked and non-networked
medical device inventory. Being able to quickly populate all devices of a specific metric from your inventory is very important to ensure all affected devices are known when a recall or security threat presents itself. For instance, knowing the exact location of a medical device that has been recalled can save your department time and help to remediate the issue faster and with more confidence that you’ve remediated the correct device. The last thing you want when a recall/security threat is posted, is to miss devices and enable that device to be a risk to patients and staff. CMMS allows in-depth monitoring and analysis of devices on the network and can potentially be used to point out the vulnerabilities before a security breach can occur. As HTM professionals, one of our biggest responsibilities is servicing equipment by performing preventative and corrective maintenance to keep our patients and end-users safe. CMMS can store data on work performed to increase management on the maintenance of devices as well as aid in troubleshooting efforts. With the growing amount of networked medical equipment, it is very important to have data on the medical devices on your network so that the highest level of security is applied.
The metrics that should be included into your CMMS vary and can be tailored to your role/position in your department (manager/technician/engineer) to view the information that is most useful to your needs. While the metrics used to have the best representation of the managed systems can differ depending on the management needs and values, foundational metrics are used to get a quick understanding of the device. Additional metrics create a more thorough understanding of the system as well as protect it, these metrics add value to the CMMS. The foundational metrics may be things like the medical device’s hostname, physical location, IP/ MAC address, manufacturer, model and serial number.
hospital are correctly evaluated, protected and




























































































Living in a time of ever evolving, advancing and extensive data gathering that a CMMS can provide us with, the main purpose of the CMMS is to visualize and gain a better understanding of our overall medical system environment. But don’t be fooled, even though a CMMS can provide us with the impression of data being well managed, without continuous monitoring by HTM professionals, management software and communication between staff and departments, you can’t be certain that your inventory is up to date. In the end, you can only ensure the safety of patients and their information by being on top of your medical device inventory.


Today’s health care industry faces multiple challenges – looming clinician shortage, technological advances and cybersecurity threats, to name a few. Enter HIMSS with a solution: continuing education for information technology professionals and clinicians alike.
Dubbed the “HIMSS Center for Professional Excellence,” the immersive program offers HIMSS’ expansive global network of experts, thought leaders, resources, publications and other assets. It is geared to shore up a pipeline of workforce in healthcare IT – executives, clinicians and staff.
HIMSS is renowned for its many continuing education programs for credentials and licensures. The longtime proponent of digital healthcare brings heft, knowledge and innovation to the marketplace with its latest offering.
HIMSS executives announced the program’s launch the week of April 17 in Chicago at the 2023 HIMSS Global Health Conference & Exhibition, widely considered the global standard of substantive healthcare strategy and innovation.
“Our plan is to build a wave of digital health-conscious workforce. HIMSS provides highly relevant, timely and impactful education and experience for the
ever-changing demands in the digital health ecosystem,” said HIMSS Chief Products Officer Reid Oakes.
“It makes perfect sense that HIMSS takes the helm to educate all levels across the enterprise,” Reid added. “Through HIMSS’ Maturity Models, we’ve enabled hospitals to validate their digital health maturity; by creating the HIMSS Center of Professional Excellence, we fortify this evolution by providing a learning environment that enables changemakers to prepare for the future of health care, today.”
The HIMSS Center’s first offering is slated for late summer 2023, a 9-month program for aspiring chief information officers. The academic program is comprised of thought leadership, team-based learning, case-study analysis, webinars, book reviews, community service and other formats. Included is a 2-1/2 day in-person class in Torey Pines, San Diego. Future programs offer immersive experiences for other critical stakeholders in the digital health ecosystem.
“We are very excited about all that the HIMSS Center for Professional Excellence has to offer,” said HIMSS Vice President, Professional Development JoAnn Klinedinst. “We’ve designed this offering so that health information and technology professionals have access to tools and resources to keep them equipped throughout their professional life.”
For more information, visit himss.org/global-conference.












 BY PHIL ENGLERT
BY PHIL ENGLERT
e althcare technology is evolving at a furious pace and the benefits for clinical care re nothing short of amazing. From wearable glucose monitoring systems to water vapor cancer ablation and many other technologies, todays’ patient care technologies are less invasive and provide better outcomes with lower risks.
Increasingly, medical devices are interfaced with the outside world to either take in treatment plans or report out physiological parameters such as blood glucose levels, heart rate, oxygen levels and others. Interoperability – the ability to interact with different devoices, applications or products to exchange data and instructions in a coordinated way – is the great enabler of technology but is not without risks. Each communication boundary presents a risk for the data and the instructions that cross them. Cyber actors can cause medical device failures in several ways.
Cyber actors can exploit vulnerabilities in medical devices or the software and networks that support them. These vulnerabilities may allow cyber actors to gain unauthorized access, steal sensitive information or cause damage to the devices or systems. Stolen data is commonly ransomed and may invoke regulatory penalties. Threat actors can launch denial of service (DoS) attacks against medical devices or networks. These attacks overload the devices or networks with traffic, causing them to fail or become inaccessible. Patients and caregivers are more reliant than ever on health care systems to interact with each other. System outages are not only frustrating but may result in delayed treatment.
Cyber actors can distribute malware or viruses that infect medical devices and cause them to fail or become compromised. These attacks may result in the theft of sensitive data, the destruction of critical systems, or the disruption of business operations. Cyber actors may use social engineering techniques to trick users into revealing sensitive information or clicking on malicious links, which can result in medical device failures or compromise. Cyber actors may physically tamper with or damage medical devices to cause failures or compromise their security. Access to medical devices varies greatly within health care settings and should be considered during risk assessments and deployment. Devices may be found in access-controlled spaces and actively monitored or they may be found stored in hallways or other public spaces. Employees or other insiders with access to medical devices or systems may intentionally or unintentionally cause failures by misconfiguring devices or systems, stealing data or introducing malware.
Cyber actors have several methods and tools they use to gain access to medical devices. In the patient care environment, cyberactivity can have disastrous outcomes. Cyber is another mode of failure which needs to be considered in maintenance operations planning. Healthcare technology management (HTM) staff are playing a growing role in the management of cyber threats in the patient care environment. They are uniquely qualified to understand the technology, the patient care environments and the clinical workflows. To prevent these types of attacks, it is important for biomedical technicians (HTM staff) to play a larger role to implement strong security measures, such as regular software updates, network security controls, access controls and user education and training. Additionally, organizations should regularly monitor medical devices and
networks for signs of suspicious activity and have incident response plans in place to quickly respond to and mitigate any attacks.
Cyber maintenance activities should be added to maintenance routines and performed regularly to ensure the security of medical devices. Keep medical devices up to date with the latest software releases, including firmware and security patches, to ensure they are protected against known vulnerabilities. Not all medical devices are supported the same way so working with the manufacturer to learn release schedules and delivery methods is essential for HTM to manage these processes efficiently. Wherever possible, use strong and unique passwords for medical devices, and change them regularly. Avoid using default passwords, which are commonly known within the HTM service community. Work with your network architecture team to secure the network that the medical devices are connected to with firewalls, intrusion detection and prevention systems, and other security measures to prevent unauthorized access. Employ encryption techniques for data transmitted between medical device and the cloud or other systems to prevent interception and theft.

Move patient data off medical devices and into data centers where it can be better monitored and protected when it is no longer needed on the device. Educate users on the need for and best practices for medical device security, such as not clicking on suspicious links and avoid using the public guest Wi-Fi network with medical devices. Implement strong authentication mechanisms to prevent unauthorized access to medical devices, such as two-factor authentication. Work with clinicians to find the best balance of security controls and workflows. Extend the HTM mantra of
“trust but verify” for patient safety to medical device security. Regularly inspect the configuration settings of devices. Monitor medical device communications with passive monitoring tools. Test the more robust medical devices for vulnerabilities and weaknesses using tools like vulnerability scanners. Regularly back up important data and configurations to prevent data loss in case of an attack or system failure.
Cyber-attacks can impact medical devices in many ways. Cyber actors who only access and steal data may be very hard to detect. Cyber actors can also make the data unavailable through encryption, rendering the device inoperable and impacting patient care. In some cases, this delay may cause patients to lose trust in the health care system or the delay may prolong diagnosis and treatment. In the worst-case scenario, cyber actors may be able to alter the delivery of therapy causing direct physical harm. Cyber is a way for the medical device to not function as expected or even at all. Cyber is just another failure mode. HTM staff are responsible for keeping medical devices available and functioning correctly. By getting involved in the management and maintenance of cyber controls and regularly performing these maintenance activities, HTM staff can help their organization mitigate the risk of cyber-attacks on medical devices and ensure the security and reliability of healthcare technology systems.

e ople can be confused by the TCP/IP because it is a number system. The meaning of numbers are not as clear as words explaining them. However, math is the language of machines and therefore networks. It is essential for a technician to understand these numbers.
In TCP/IP, an IP address is used to identify a machine and identify a network. That may seem odd, but it is like something people use daily: a phone number. Think of a phone as a way to communicate over a network. Phone numbers identify a group of people with an area code and an individual with a local phone number. In this way, phones follow the main goals of any network. All networks identify a group of devices and then identify the individual device in that group. Computers, phones and medical devices follow this pattern even if they do not use TCP/IP to do it. Consider a phone as an example of a network.
In the phone system, the area code is a three-digit number in parenthesis before a seven-digit local number. Similarly, IP addresses, or just IPs, are divided into four groups of three digits from 000 to 255 i.e., 255.255.255.255. This is because each group is an 8-bit number, and the largest number is 1111 1111 or 255 in decimal form. If this is not clear, please review binary math and hexadecimal math. This article will reference, but not focus on data conversions.
This article will consider the numbers pertaining to Local Area Networks, or LANs. It will focus on the IP version 4 addressing model, or IPv4, when discussing IP addresses. IPs are structured in what is called an Octet and there are four of them. The octets explain where a network, a subnet and a host number are in an IP. However, it does not do this alone. There is a subnet number that accompanies an IP address. This subnet
tells a computer how to make sense of the IP. An IP by itself will not make sense to the computer, nor does a subnet by itself. They must be used together.
Consider the graphic above: An IP address 192.168.000.001 with a subnet 255.255.255.000. This is a common IP address and subnet. Notice how the subnet number changed from 255 to 0 at the third to fourth octet. That means that the change from network to host occurs in the last octet of the IP address. The subnet tells that the first three octets are the network part of the IP, and the last octet is the unique host number part of the IP. The rule is this: The network part must match for two devices to be networked, and the host number must be different from all other host numbers. If these conditions are met, the devices will communicate. This must be exact, or the network will not function. That is just like the phone system, a phone can be in the same area code, but cannot use the exact same number as another phone. The IPs follow the same pattern.
In an IP address of 192.168.0.1 with a subnet of 255.255.255.0, the network address is 192.168.0.XXX, where XXX is the individual host number of a device. The total number of individuals in this network about 250 unique hosts. That is plenty of devices for a home

or a clinic, but not nearly enough for a full hospital. Therefore, bigger networks change the subnet for more hosts. Changing the Subnet to 255.255.0.0 moves the network and host part of the IP. It is no longer at the last octet, but now is between the second and third octets. The first and second octets are now the network portion of the IP, and the last two octets are now the host portion. Our available numbers expand to 250 times 250, or over 64,000 different unique host numbers.


In this way, IPs are expandable. If more IPs are needed, just change a number in the first two octets for a separate network. In this way, IP addresses are also scalable. This is how hospitals can have several different networks connected to the same switches. The devices listen for their networks and communicate only to the other hosts in their network. This is called network segmentation and is one of the most essential concepts of TCP/IP.
It is important to note that these IP numbers are not compatible with the Internet without a router. LAN IPs do not appear on the Internet. A router understands its internal LAN IP numbers and knows how to switch packets between networks. Routers know if a packet’s destination is inside the LAN or over the Internet (a Wide Area Network or WAN). An example of an Internet number would be 1.1.1.1, which is a server over the Internet that we can use in troubleshooting. Most LAN would not use a host number like this one. If this is seen, a router transfers the related packets to an Internet service provider for Internet access. For a device using the Internet, two more settings must be used; they are the Gateway and the Domain Naming Service or DNS. A gateway is just what it sounds like, an exit to leave a network. A gateway IP is the number a device must use on its LAN to communicate on another network. A DNS is a server that converts a webpage name to an IP. Think of it like the phonebook for the Internet. Typing 142.251.45.46 in a web browser may lead to a Google website, but it is easier to remember to type Google.com in the browser. The DNS server makes the connection between webpage names, called Uniform Resource Locators or URLs, and the web IP addresses. In this way, people use the Internet referring to a webpage by name. Keep in mind that it is still just a set of IP numbers in the background.
In this way, medical devices use IPs to connect with other devices and bring the hospital together into one network. In concept, all networks accomplish the same tasks of identifying groups of devices and identifying each device as a unique number in that network. The settings required for TCP/IP to work on a LAN are its IP address and Subnet. Optionally, a Gateway and a DNS can bring Internet connectivity. The wonderful thing about TCP/IP is that anything using it uses the same settings. Therefore, understanding it will help a technician work on many devices. Following this information will help a technician gain more familiarity on networking and increase their value to the field. Networking is, after all, the future of HTM.






























2. Exhibitor personnel at Fresnius Kabi discussing the products they showcased at the HIMSS 2023 conference.


The 2023 HIMSS Global Health Conference & Exhibition was held April 17-21 in Chicago. It is the most influential health information technology event of the year. More than 40,000 professionals from throughout the global health ecosystem met to build relationships during lively networking events, learn from experts in hot topic education sessions and discover innovative health tech products to solve their greatest challenges. For more information, himss.org
4. Megan Cabot interviewed Chad Holmes from Cynerio and discussed their upcoming Webinar Wednesday, as well as what you would find if you stopped by their booth.


5 Healthcare Information & Management Systems Society (HIMSS) fosters collaboration, learning, and growth for health tech entrepreneurs.

6 The Sodexo Healthcare team was on hand to answer any questions about their innovative healthcare support services solutions.

7 With over 40,000 attendees and two exhibit halls, HIMMS was buzzing with excitement.



Show us what Ben Calibrating has been up to! Follow MedWrench on Facebook at facebook.com/medwrench & on LinkedIn at linkedin.com/company/medwrench
Step 1: Like the MedWrench Facebook or LinkedIn company page. Step 2: Post your picture of Ben C. to Facebook or LinkedIn & tag MedWrench in your photo. Step 3: Post a funny caption with your picture. Step 4: Use #BenC







SPONSORED BY:
 Mic check 1, 2... mic check 1, 2...
At the recent MD Expo in Houston, TX.
Ben C. at the theater watching Matilda, the musical.
Ben C. at the River Walk in San Antonio
Grabbing a spin ride at CycleBar in Franklin, TN
Mic check 1, 2... mic check 1, 2...
At the recent MD Expo in Houston, TX.
Ben C. at the theater watching Matilda, the musical.
Ben C. at the River Walk in San Antonio
Grabbing a spin ride at CycleBar in Franklin, TN




More than 1,000 HTM professionals from throughout the United States descended on Houston for MD Expo. The signature conference delivered a packed exhibit hall, outstanding educational sessions, entertaining networking opportunities and more.




For more information, visit mdexposhow.com.

1. MD Expo Houston exceeded expectations with more than 1,000 HTM professionals in attendance.

2 Door Prize Bingo was a hit with attendees in search of great door prizes.
3 The photo booth at the Disco Rodeo proved to be a popular place to create a memento.
4 Top-flight educational sessions provided ACIapproved credit.
5 Panel discussions were a hit.
6 Attendee Jason Chaffin was among the winners at the door prize raffle.

7 Attendees and exhibitors were in awe of the packed exhibit hall.

8 The Disco Rodeo was the perfect ending to a successful event.

9 Keynote speaker Billy Riggs exploded the debilitating myths that render workers ineffective.
10 MD Expo was the place to be in the spring of 2023.

11 MD Publishing’s Haley Wells takes a professional headshot photo for Edwin Saunders at the Career Center.

“HEMS One” by EQ2 is designed specifically for hospitals and offers more than a typical CMMS...




• Requires no third party platform, yet integrates with numerous other applications


• Reporting: hundreds of reports included plus EQ2 can provide custom reports plus you can create your own

• Fully automatic Dispatch Board that can be configured to meet your hospital’s assignment policies for multi-level escalation based on response time, location, type of problem, shift hours, etc. Location can be as precise as room, floor, building, campus, city level, etc.



Booth 1050
Years
We’d love to feature you, your colleague or the entire department in one of TechNation’s monthly features!
Think of a Biomed/CE Department deserving of recognition. Scan the QR code or email editor@mdpublishing.com.
We will contact you for additional information if your nomination is accepted!
trainingoptionsavailabletothedepartment’stechnicians. Inaddition managingequipmentattheeighthospitals, thelargebiomedteamalsoservesmorethan20orthopedic andsportsmedicinelocationsofferingphysicalandoccupationaltherapyacrosstheGreaterHoustonarea. PhysicianTheyarealsoresponsibleforequipmentattheSpecialty Groupwith848physiciansat191locationsandthe PrimaryCareGroupwith169physiciansat42locations. ThehospitalisaffiliatedwithWeillCornellMedicine, NewYork-PresbyterianHospitalandtheTexasAnnual Conference theUnitedMethodistChurch.TheHoustonMethodistAcademicInstitute,which researchand educationinstitute,hasafaculty 742,with2,110credentialedresearchers.BIGTEAM,BIGPROJECTS ThechallengestoaddressCOVID-19surgestaxedthe resourcesofhealthcarefacilitiesacrossthenation,but requiredinnovationon grandscaleforthebiomedteamat HoustonMethodist.“AttheonsetoftheCOVID-19pandemic,therewas glaringneedtoreduceexposure patientswithinthe hospitalforourRTdepartment.Thankfully,ourHamiltonG5 ventilatorshave detachableinteractionpanel. askedto haveventsinsidetheCOVIDroomandplacetheinteraction paneloutsidetominimizeexposureforthe therapist go insidetheroom.Theinteractionpanelwasattachedto tableoutsidethepatientroomandwehadtodothisfor 90-100G5patientrooms,”Smithsays. Hesaysthattogetherwiththe medicaldeviceintegrationteam,theysuccessfullyopenedavirtualICU(vICU).“We had keyroletoplayinensuringthepatientphysiological monitorswerecapableofbeingusedinthisnew,innovative setting,”Smithsays.TheteamtackledmanyotherprojectsrelatedtothevICUtomeettheneeds patientsandvisitorsduringthe pandemic.AnotherprojectwascenteredaroundAlarispump interoperabilityandtyingthemtopatientrecords. “Pharmacy,nursing,biomed,multiple groups,andthe

Hoperatingbeds,HoustonMethodistincludes27,947employees,withmanyworkinginbiomed.The85-memberbiomedicalengineeringdepartment ledbySystemDirector AnthonyMaroulis.Othermembersofleadershipinclude CampusDirectorofClinicalEngineeringMarcBateman, ManagersofClinicalEngineeringTerresaEverhart,Javier Ruiz,MiguelMezaandCoreaunJacksonandProgram CoordinatorsBrandonHightandNathanStathos.Theteam’s clinicalengineersincludeZachSmith,CristianDelgado, BailynPiecewiczandHaniKhalil.Thedepartmentalso consistsoftwoadministrationassistants,fivebiomed equipmenttechleads,23biomedequipmenttechIIs,23 biomedequipmenttechIIIs, biomedequipmenttechIs,biomedradiologyserviceengineersand dataentry specialist.Batemansaysthatthebiomedteamservicesmorethan 91,000medicaldevicesin-housethankstotheexceptional
was helpinghimcrew someseattimehereand there on some faster bikes and rode for some teams inDivision4,thenstartedracingsome bracketsandgrudgeracesinthelate’90s,”Barronsays. motorcycleIn2010,hewasintroducedtotheprostock classby mutualacquaintanceoftheUnderdahlRacingfamily. “When approachedthem theFallNationals Texas,andaskedwhat wouldtake transitiontoprostockmotorcycle,GregUnderdahltoldmehe neededtosee couldhandle bikeofthatmagni-
tude justholding throttlewideopenand 660releasingtheclutch;thenprogressedto330feet, feetandprogressinginto quarter-mile(1,320 feet)passin couple testsessions,”Barronsays. Underdahl then told Barron that he felt comfort-
PROOF APPROVED CLIENT SIGN–OFF AD SIZE NOTES


PLEASE CONFIRM THAT THE FOLLOWING ARE CORRECT MEDICAL DEALER TECHNATION ORTODAY BUYERS GUIDE OTHER
• NIHON KOHDEN •
SPACELABS • DRAGER • SCOTTCARE NIHON KOHDEN • DATASCOPE GE • PHILIPS

BEDSIDE & CENTRAL MONITORING • MODULES TELEMETRY FLAT PANELS













PUBLICATION MONTH J F M A M J J A S O N D
SPACELABS • DRAGER • SCOTTCARE DATASCOPE • GE • PHILIPS WWW.SWBIOMED.COM • 800.880.7231





RECORDERS • ACCESSORIES • FREE TECHNICAL SUPPORT FREE REPAIR EVALUATIONS

“We Put The ACE In Spacelabs!”
BLEED 11” TRIM 10.75” SAFETY 10.25” FULL PAGE
ber kidwatchingtheCharlieBrownandPeanuts WorldserieswhereSnoopyoftendreamedoffightingthe War acepilot,BaronManfredVonRichthofen,aka,TheRedBaron. stillhavemanyofmygrandma’strophiesfromdragracingwhenshecompeted Ft.thePowderPuffWomen’sDragRacingSeriesin wasWorthinthelate1960sandearly1970sbefore Barronborn,”Barronsays.saysthathetriestoattendeventscloseto “We Put The ACE In Spacelabs!”
THE SEARCH IS OVER. WE WILL REPAIR YOUR SPACELABS EQUIPMENT. June 2023 | TechNation 101


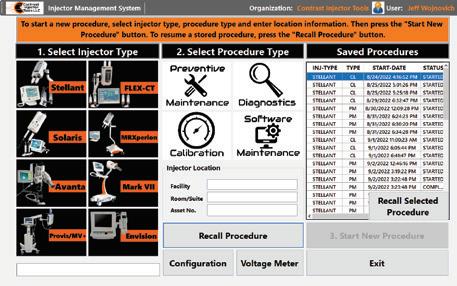



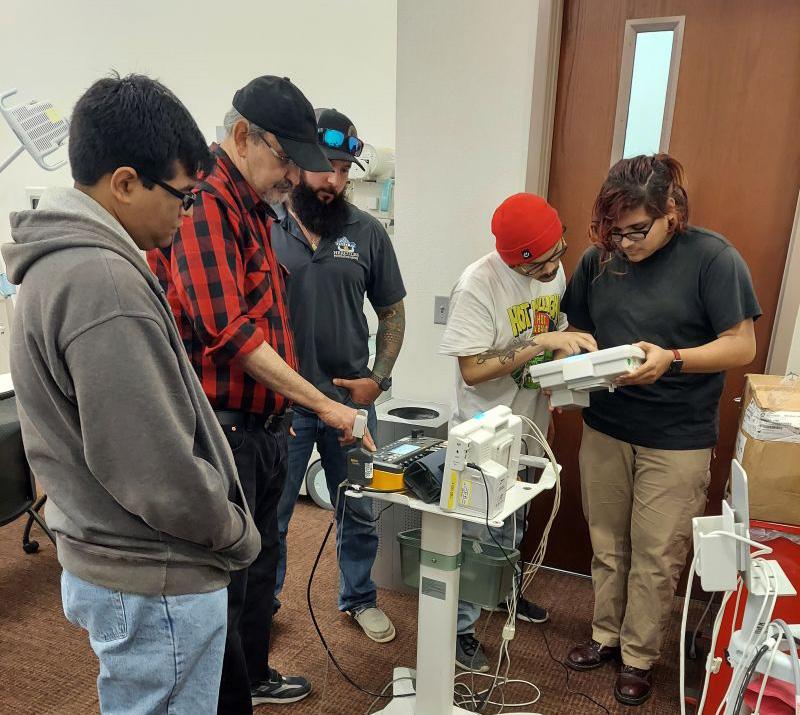


J oin us as we celebrate the TechNation community. You - each and every reader, Webinar Wednesday attendee, HTM Jobs user and MD Expo attendee - are the most important part of the TechNation community. Share a photo of yourself, a colleague or the entire biomed team on social media and tag it with #IamTechNation. Then, check each issue of the magazine to see yourself and all of the men and women that are TechNation.


