






























































There
are concerns that rates of COPD could further escalate as we see the fallout from rising use of vapes, particularly in young people.
No one likes breathing in smoky air in the bush fire season or battling a bad pollen season, but it is especially tough for anyone with asthma.
Adding an extra later to the complexity of managing asthma is that the very thing that people rely on – inhalers – have their own environmental impact.
So, it is not surprising that the country’s peak asthma support group has released new information for GPs on ways to help reduce the carbon footprint of some traditional inhalers.
The National Asthma Council argues that every bit counts, and greener inhalers can actually help patients too.
It certainly is a changing world. This month we look at why Asthma WA, which turned 60 this year, recently opted for a name change to Respiratory Care WA.
It says it reflects the increasing demand to support patients with chronic obstructive pulmonary disease – the smoking-related condition we used to call emphysema – and their GPs.
There are concerns that rates of COPD could further escalate as we see the fallout from rising use of vapes, particularly in young people.
A dramatic fall in smokers in recent years was hailed as one of Australia’s greatest public health success stories, but cigarettes have been replaced with something that is far from innocuous.
Under latest Government reforms to curb vaping, from next month access to therapeutic vapes for those aged 18 and over will be via pharmacies without a doctor’s prescription. Only time will tell how all the changes ultimately affect use.
SYNDICATION AND REPRODUCTION Contributors should be aware the publisher asserts the right to syndicate material appearing in Medical Forum on the mforum.com.au website. Contributors who wish to reproduce any material as it appears in Medical Forum must contact the publisher for copyright permission.
DISCLAIMER Medical Forum is published by Medforum Pty Ltd (Publisher) as an independent publication for health professionals in Western Australia. Neither the Publisher nor its personnel are medical practitioners, and do not give medical advice, treatment, cures or diagnoses. Nothing in Medical Forum is intended to be medical advice or a substitute for consulting a medical practitioner. You should seek immediate medical attention if you believe you may be suffering from a medical condition. The support of all advertisers, sponsors and contributors is welcome. To the maximum extent permitted by law, neither the Publisher nor any of its personnel will have any liability for the information or advice contained in Medical Forum. The statements or opinions expressed in the magazine reflect the views of the authors and do not represent the opinions, views or policies of Medical Forum or the Publisher. Readers should independently verify information or advice. Publication of an advertisement or clinical column does not imply endorsement by the Publisher or its contributors for the promoted product, service or treatment.
Advertisers are responsible for ensuring that advertisements comply with Commonwealth, State and Territory laws. It is the responsibility of the advertiser to ensure that advertisements comply with the Competition and Consumer Act 2010 (Cth) as amended. All advertisements are accepted for publication on the condition that the advertiser indemnifies the Publisher and its personnel against all actions, suits, claims, loss or damages resulting from anything published on behalf of the advertiser.
EDITORIAL POLICY This publication protects and maintains its editorial independence from all sponsors or advertisers. Medical Forum has no professional involvement with advertisers other than as publisher of promotional material. Medical Forum cannot and does not endorse any products.





This month we have more tickets up for grabs, with five double passes to the 2024 ST ALi Italian Film Festival which returns to Perth from October 3 to 27, with more details on page 50.
To enter, use the QR code on this page or go to www.mforum.com.au and hit the competitions tab.
PUBLISHERS
Fonda Grapsas – Director Tony Jones – Director tonyj@mforum.com.au
EDITORIAL TEAM
Editor
Cathy O'Leary 08 9203 5222
editor@mforum.com.au
Production Editor
Jan Hallam 08 9203 5222 jan@mforum.com.au
Journalist Eric Martin 08 9203 5222 eric@mforum.com.au
Clinical Editor
Dr Joe Kosterich 0417 998 697 joe@mforum.com.au
Graphic Design
Ryan Minchin ryan@mforum.com.au
ADVERTISING
Advertising Manager
Bryan Pettit 0439 866 336 bryan@mforum.com.au
Classifieds Sales
Ross Bulman 0428 759 076 ross@mforum.com.au
Clinical Services Directory
Alice Miles 08 9203 5222 alice@mforum.com.au
CONTACT MEDICAL FORUM
Suite 3/8 Howlett Street, North Perth WA 6006
Phone: 08 9203 5222 Fax: 08 6154 6488 Email: info@mforum.com.au www.mforum.com.au













The RACGP’s expert committee on practice technology and management has been exploring the benefits and pitfalls on the emerging technology of artificial intelligence clinical scribes.
These AI scribes are proliferating in the software marketplace, with one brand already embedded into one of Australia’s biggest practice programs, Best Practice, but as chair of the committee, Victorian GP Dr Rob Hosking says, it’s still early days and more products will emerge.
To try and get ahead of the game (or at least keep abreast) the committee has drawn up guidelines to help those GPs who want to safely explore the benefits and avoid those pitfalls.
The AI scribes are marketed as a tool to reduce the burden of notetaking during a consultation, which can add value for both patient and doctor, with a handsoff keyboard and eyes-on-patient approach allowing for a better personal connection and more valuable conversations.
But it takes a bit of getting used to, says Dr Hosking, and not every doctor or patient will want to even try.
He told Medical Forum his own experiences had been positive, and he hadn’t had any patients decline his invitation to have the AI scribe listen in, but each consultation must start by a patient consenting to the digital recording of the visit.
He said that the transcripts always needed reviewing because the scribe interpreted the conversation, and it was not infallible – it made mistakes by filtering out pertinent information, mishearing and incorrectly categorising data. GPs were liable for the errors.
Nor was it diagnostic (though he added this would probably come and would create its own set of issues).
However, what he has found is that his consult notes were
Research and treatment of childhood cancer had a massive boost with the Stan Perron Charitable Foundation’s $135.5 million investment over the next decade to a multi-partner collaboration building on the work being done by Perth Children’s Hospital and Telethon Kids Institute.
The Perth Children’s Hospital Foundation (PCHF) will also make a multimillion-dollar contribution over the next five years with an option to extend and the University of Western Australia will add up to $9 million to help find effective treatments for children impacted by cancer.
Child and Adolescent Health Service Chief Executive Valerie Jovanovic

more detailed and nuanced, and he had saved time in the process.
Privacy and data security are, of course, some of the greatest concerns with use of any AI product and there are warning lights throughout the RACGP guidelines.
They state that the “software vendor offering the AI scribe should provide assurances about how the data is encrypted, stored, and destroyed. General practices should also have their own policies and procedures for managing information security to help prevent data breaches, such as enabling multifactor authentication on AI scribes and other applications.”
GPs also need to know how the vendor might use collected data for its own purposes to train new AI models and there might be on-sell of data to a third party. The college recommends GPs considering using or purchasing an AI scribe to carefully review the terms and conditions of the user agreement to determine if it is appropriate and acceptable before launching it.
Dr Hosking added that while the Office of the Australian Information Commissioner had given the AI products on the market the green light, it has yet to provide documentation that they adhered to Australian privacy principles.
“That would be reassuring,” he said. www.racgp.org.au/running-a-practice/technology/ business-technology/artificial-intelligence-ai-scribes
said investing in childhood cancer research and care was important, with 1240 Australian children diagnosed with cancer each year and it continuing to be the leading cause of death by disease for children.
“This field is moving rapidly with precision medicine, genomics and other science advances. The donation will not only benefit WA children, it will also allow our PCH clinicians and Telethon Kids researchers to contribute to these advances and lead the field in their areas of expertise,” she said.
The RACGP is advising people who want to stop taking antidepressants
to see their GP for support, after it endorsed the Maudsley Deprescribing Guidelines for use in Australia.
It also reiterated the call for higher Medicare rebates for patients who need longer consultations which were often essential for mental health care.
Outgoing president Dr Nicole Higgins said GPs knew how hard it could be for people who want to stop using antidepressants.
“GPs are increasingly reporting mental health in their most common reasons for a patient visit – from 61% in 2022 to 72%





“In the future, every CT will be a photon-counting CT”
Prof. Gabriel Krestin
Erasmus Medical Center Rotterdam, Netherlands
“This will redefine our clinical decision-making right from scan one.”
Prof. Dr. med. Thomas Kröncke University Hospital Augsburg, Germany

“PCD-CT is so exciting because it provides information that existing CT detectors – the types that we’ve used for over 50 years – previously just couldn’t capture.”
Dr. Cynthia McCollough Mayo Clinic CT Clinical Innovation Center. USA
In March 2024 ChestRad introduced Photon Counting CT to Western Australia. But best not to listen to us. Find out what the experts have to say.

Medical clinicians featured heavily in this year’s Premier’s Science Week awards.
Professor Markus Schlaich’s work at RPH and UWA on hypertension was recognised with the Scientist of the Year award, which he shared with Curtin University’s Professor Sharon Parker.
Respiratory researcher
Dr Pamela Laird at Telethon Kids Institute and Perth Children’s Hospital shared the Early Career award with chemist and engineer Dr Neil Robinson.
Sydney GP and health economist
Dr Michael Wright will take over the presidency of the Royal Australian College of GPs (RACGP) at the annual conference in November in Perth.

Australia’s largest provider of private cancer care services, Icon Cancer Centre, has appointed Colin La Galia as its WA State Manager.
Dr Marcus Tan has been appointed as an Advisory Council Member at the Western Australian Future Health Research and Innovation Fund.
Nobel Laureate, medical pathologist Emeritus Professor (John) Robin Warren AC , has died in Perth at the age of 87.
continued from Page 4
in 2023, according to our Health of the Nation report,” she said.
“Antidepressants generally are a helpful and effective treatment option for many people, but they are not generally advised for use longer than six to 12 months.
“But while some people can come off these drugs relatively easily, others have side effects severe enough they keep taking a medication they want to stop. And people have no way of knowing what their experience will be like until they stop.”
Artificial intelligence is being used in a program developed by researchers from Edith Cowan University to train frontline healthcare workers in de-escalating aggression in patients.
“Barry” is an AI computer-based model that allows clinicians and students to verbally interact with him in a hospital setting. Users have an actual conversation with Barry, and he responds in real time and each interaction is entirely unique, even if users provide the same wording more than once.
The training simulation incorporates emotive facial animations that align with real-time verbal responses, and Barry’s anger levels will either escalate or de-escalate based on the empathy displayed from the user.
Barry’s responses are based on prompting from the development team, outlining the gender, race and age of the user undertaking the training, which can be customised to suit different user profiles.
workplaces, he said. Exposing learners to human simulations that were also safe was resource intensive and problematic to implement at scale, particularly in rural and remote areas.
Barry is in its first phase of development, the second will incorporate motion capture to create animated body movements that could include situations where Barry turns physically violent.
New research compared the number of athletes in each Olympic discipline to the number of reported injuries, determining the sports with the highest risk factors and BMX has emerged as the most dangerous, with a 34.38% injury rate, while table tennis and handball were more injury-prone than equestrian and trampoline.
Taekwondo follows closely, with nearly 30% of athletes suffering injuries.
Football is the most dangerous team sport, with over 27% of its 1508 competitors experiencing injuries. Handball is the second most dangerous team endeavour, trailing by nearly 10%, with an average of 17.98% injured athletes.
Boxing had the second-highest number of injured athletes at the Tokyo Olympics, indicating a growing risk.
The International Olympic Committee (IOC) implemented a multi-sport injury surveillance system for the first time at the 2008 Beijing Olympic Games and this data was collected from the British Journal of Sports Medicine. It takes into account all Summer Games between Beijing 2008 and Tokyo 2020.

Medical students Shoshanna Scott from WA and Tamyka Bell were named 2024 President's Prize winners at ACRRM’s annual conference in Darwin.
ECU Senior Lecturer Dr Brennen Mills said exposure to aggression and violence was an unfortunate reality for frontline healthcare staff and these incidents could have long-lasting impacts on them.
Health Departments provide deescalation and safety training to staff to prepare them to manage aggressive incidents but access to training can prove difficult within busy
The London 2012 Olympics had the highest overall injury rate, with 12.8% of athletes reporting injuries.
For the record, the safest Olympic sport is canoeing/ kayaking, with an average injury rate of just 2.23%, which narrows down to 1.2% in canoe slalom.
COVID may be coming routine, but it is nonetheless damaging. The Lancet reports that a large study in the UK reveals that it is leaving a
In February, Medical Forum spoke with Associate Professor Anthony Kicic about the power of phages in an increasingly antibiotic-resistant world and how WA was powering ahead in research and development of a local capacity to produce them.
That hard work has paid off with the opening of Phage WA, the state’s first phage manufacturing facility based at the Centre for Advanced Therapies at Royal Perth Hospital.
Phage WA is the result of the collaborative efforts of the Wal-yan Respiratory Research Centre—a partnership between the Telethon Kids Institute, Perth Children’s Hospital Foundation and Perth Children’s Hospital.
Funding has come from the Federal Government, the WA Government, Conquer Cystic Fibrosis, Cystic Fibrosis WA, Perpetual’s Impact Philanthropy Program, the Rothwell Family Foundation, the Stan Perron Charitable Foundation, and Therapeutic Innovation Australia.
Its mission was to pioneer treatment solutions for children, particularly those with cystic fibrosis, facing antimicrobial-resistant lung infections, which has expanded to therapies that could help treat lung, skin and ear infections as well as bacterial infections such as golden staph.
A/Prof Kicic, who is Scientific Lead of Phage WA and a researcher at the Wal-yan Centre and the Curtin School of Population Health, said the manufacturing facility's opening was the next key step in bringing patients closer to faster and more effective phage treatments.

“Our team has spent the past five years creating a large library of phage viruses and matching them with the various strains of bacteria that cause serious infections to find the best treatment to destroy them and clear infection,” he said.
“Last year, nationwide ethics approval for compassionate use of phages was granted, offering new hope to patients suffering from chronic, recurrent infections that no longer respond to antibiotic treatment.
“We were also successful in securing WA and federal government funding to initiate a manufacturing facility and a translational trial program for patients with antibiotic-resistant lung infections.
“While small-scale phage facilities exist in Sydney and Melbourne, they would not be able to meet national demands including WA patients within practical timelines. The establishment of a WA facility is a monumental step toward delivering faster phage treatments to patients in need not only here but also around Australia and overseas."
trail of diabetes in its wake, with a 15% increased incidence in England and kids progressing to type 1 diabetes at twice the rate of their uninfected peers in Germany.
The numbers suggest that doctors should at least consider diabetes in any post-COVID infection followup, according to the authors of both papers.
Drawing on records for over 16 million people in England since the start of the pandemic, researchers from the US and the UK have found severe COVID significantly increased the risk of diabetes – both type 1 and type 2 – but vaccination greatly reduced that risk.
Incidence of type 2 diabetes remained elevated by 30% more than a year after COVID diagnosis in unvaccinated people. Type 1 diabetes incidence was elevated during the year post-infection, but not beyond. The associations were higher for people who’d been hospitalised with COVID.
“Encouraging vaccination –which, in addition to reducing the immediate severity of COVID, reduces the immediate and longerterm risk of incident type 2 diabetes after COVID-19 – is essential,” the authors write.
Across the entire study, unvaccinated people who had COVID had almost nine times the risk of developing diabetes in the first four weeks compared with uninfected people. Risk remained elevated by 64% in the second year after infection, the study found.
Before vaccines were available, incidence of type 2 diabetes after COVID was over four times higher than for infected people in weeks one to four of infection, subsiding to 24% higher after that period. Patients who were vaccinated before infection had only a 66% higher risk in the first four weeks after COVID infection compared to the uninfected.
The Royal College of Pathologists is calling for more regular testing for sexually transmitted infections, amid a significant rise in cases across the country.
Data shows that a nearly 20% increase in gonorrhoea notifications from 2022 to 2023, with further increases expected in 2024. Syphilis rates have also surged, particularly congenital syphilis.
Despite this surge of infection, the RCPA says testing levels have not notably increased, including among older adults.
Spokesperson A/Prof Caitlin Keighley said that low testing levels meant that infections could go undiagnosed and untreated, leading to severe health complications and further transmission. This was particularly concerning for
continued from Page 9
pregnant women, where untreated STIs could result in congenital infections with severe outcomes. The rise in STI cases can be attributed to changing sexual practices such as reduced use of condoms across various demographics. The RCPA highlights the importance of regular STI testing for all sexually active individuals, regardless of age.
Researchers at the Peter Doherty Institute for Infection and Immunity have identified a gene that may help identify recovery rates of patients hospitalised with respiratory viral infections.
Researchers and clinicians have long grappled with the mystery of why some individuals succumb to severe infections while others recover unscathed.

In a study published in Cell, researchers discovered the critical role of a gene called OLAH in disease severity. Co-research lead Dr Brendon Chua said the first ‘aha’ moment occurred during the analysis of patients hospitalised with A(H7N9) influenza, where a consistent association between high expression levels of OLAH and fatal outcomes was detected. Conversely, patients who recovered exhibited very low OLAH expression throughout their hospital stay.
“Further investigation using animal models and cell cultures revealed that OLAH is pivotal in driving life-threatening inflammation associated with respiratory viruses,” he said. “What’s interesting is that we all have this gene, but its expression varies during the early phases of a respiratory infection, which is why some of us recover faster while others experience severe complications.”
The researchers found elevated levels of OLAH in patients severely infected with seasonal influenza

GPs can refer babies with peanut allergies to a treatment program under a world-first model, which will include two Perth hospitals sites.
Ten hospitals – including Perth Children’s Hospital and Fiona Stanley Hospital – will work with the National Allergy Centre of Excellence (NACE) to introduce a nation-wide peanut oral immunotherapy program.
Children will follow a carefully planned daily dosing schedule of peanut powder, taken at home, over two years.
It is the first time that oral immunotherapy will be offered in mainstream care outside a clinical trial setting.
Any baby under the age of 12 months, diagnosed with a peanut allergy and being cared for at one of the participating hospitals is eligible.
The NACE, hosted at Murdoch Children's Research Institute, will evaluate the program for both its effectiveness and safety with the hope of extending it to more centres, public and private hospitals and private allergy clinics across the country.
Dr Michael O’Sullivan, Allergist and Program Lead at PCH and FSH, encouraged families who suspected their baby had a peanut allergy to first visit their GP.
“Australian guidelines recommend infants are introduced to common allergens, such as peanut in the form of peanut butter, in the first year of life,” he said.
“If you think your baby has had an allergic reaction to peanut, avoid that food and talk to your GP, who may refer your child to an allergist at one of the participating hospitals.”
Peanut allergy affects 3% of 12-month-olds in Australia, and over two thirds of children with a peanut allergy remain allergic at the age of 10.
While on the program, children will be prescribed an Australasian Society of Clinical Immunology and Allergy action plan for anaphylaxis and adrenaline injector, and families receive a comprehensive education pack and have access to an allergist on-call.
virus, SARS-CoV-2, respiratory syncytial virus (RSV) and in children experiencing multisystem inflammatory syndrome, a condition associated with COVID-19, but not in mild cases.
Professor Katherine Kedzierska, head of the Human T cell Laboratory at the Doherty Institute who has been leading this research since 2013, said the potential of the finding was far-reaching.
“Imagine if your doctor could predict whether your respiratory infection will become lifethreatening or if you'll recover quickly? Our findings suggest that OLAH expression levels could be used as a tool in assessing patients’ prognosis, empowering clinicians with crucial insights for early risk assessment and personalised treatment strategies,” she said.
Dr Stephanie Giandzi Recent fellow


A new campaign to encourage GPs to make greener choices in asthma management is a win-win for patients and the planet.

By Cathy O’Leary
Perth GP Brett Montgomery admits he was worried when he first broached the subject of greener inhaler options with some of his asthma patients.
“I thought people might think I was weird and a bit of hippie – bringing up climate change and the environment in their consultation – but it’s gone OK,” he said.
Dr Montgomery does not need to be won over about a new resource to help GPs make greener asthma medicine choices, because he helped develop it.
The National Asthma Council Australia (NAC) recently released the information paper to guide GPs in choosing options that could reduce asthma symptoms, prevent severe exacerbations and at the same time improve the health of the environment.
It is the first statement from the group that outlines why prescribing pressurised metered-dose inhalers (pMDIs) have a much larger impact than other inhalers and provides practice points on how to minimise wastage while maintaining good asthma control.
Dr Montgomery, a member of the NAC’s guidelines committee, said good asthma control and greener inhaler choices could go hand in hand.
“Better asthma disease control often leads to less use of inhalers that contribute to greenhouse gas emissions and that’s good for patients and the planet,” he said. “This new information will help health professionals to understand how poorly controlled asthma contributes to a larger carbon footprint through inappropriate or unnecessary prescribing, dispensing and purchase of inhalers.”

According to the NAC, Australian studies have shown that high rates of poor asthma symptom control are associated with the under-use of inhaled corticosteroids (ICS) and over-reliance on short-acting beta2-agonists (SABAs).
Salbutamol delivered via pressurised metered-dose inhalers is by far the most common reliever medicine used in Australia, with more than five million prescribed inhalers dispensed every year, plus an estimated six million sold over the counter.
While all inhalers have an impact on the environment, pMDIs are much bigger players because they contain hydrofluorocarbon propellants, which are released during use and through leakage after disposal.
Annual Australian greenhouse gas emissions from SABA inhalers have been estimated to be equivalent to over 350,000 tonnes of carbon dioxide – as polluting as driving a petrol fuel car from Sydney to Perth more than 360,000 times.
On the other hand, dry powder inhalers and soft mist inhalers have a 100 to 200-fold lower carbon footprint than pMDIs.
The NAC, which publishes Australia’s major asthma guidelines, the Australian Asthma Handbook, is now partnering with other organisations to help reduce emissions from respiratory inhalers.
Dr Montgomery said the overuse of salbutamol pMDIs was the greatest concern.
He told Medical Forum that for some time other countries such as the UK had guidelines and journal articles that had been vocal on the environmental impact of respiratory inhalers, but Australia and some other countries were just catching up now.
“Some of the messaging is familiar about poor asthma control and the over-reliance on short-acting beta2agonists that largely just relax the muscles in the airways, when there are other medicines that can do better settling down inflammation, not just the temporary muscle relaxation effect,” he said.
“But the nice thing about talking about the topic of the environmental effects of asthma treatment is that they’re not in tension with each other.
“It’s not like we’re saying we should use less of the polluting inhalers, even though they’re not as good for asthma control – it’s not like that, and I occasionally get that pushback from people.”
Many people could get just as good asthma control with greener inhalers and might need less of their inhalers which meant less pollution.
“It’s a real win-win for patients
and the environment if we get this right,” Dr Montgomery said.
“In Sweden, something like 90% of inhalers are not pressurised metered-dose – they are the greener types – and Australia is a long way behind that, with the majority used here being of the metered-dose inhaler type, often containing salbutamol, and it’s available over the counter as well as on prescription.
“It's hard to believe this is an ongoing issue because many of us practitioners have spoken to our patients about this, but still when I see articles measuring the problem of poor asthma control, I keep being surprised by how bad it seems to be.”
Dr Montgomery said an article in the Medical Journal of Australia a few years ago revealed the results of a survey of people with asthma, randomly selected across the country rather than relying on data from general practice presentations. It found that about a quarter of Australians with asthma had both poor asthma control and had barely or never taken inhaled corticosteroids.
“We know that one in nine Australians have asthma, and every year about 400 people will die of asthma in this country, and people who have poor asthma control are surely over-represented among those people who die,” he said.
“Personally, I’ve change quite a few of my patients from traditional inhalers to greener ones and I anticipated more resistance than I received. One patient looked at me a bit sceptically, but I brought up an article published in the British Medical Journal – because then we didn’t have any Australian statement on it – and he could see
Minimise wastage by reducing inappropriate or unnecessary prescribing, dispensing and purchase of inhalers:
• Confirm the diagnosis of asthma to target treatment effectively.
• Choose the best inhaler for the individual and train them to use it correctly.
• Aim for good asthma control to reduce patients’ requirement for salbutamol doses via pMDIs.
it was legitimate so was happy to try this different puffer.
“Sometimes GPs think it will be harder than it is. It’s all about everyone doing their bit, and there is a slow process of normalising care of the environment, and that’s the spirit in which we’ve put out this statement.”
But Dr Montgomery stressed that it was not a ‘one size fits all’ model, nor was it about swapping everyone with asthma onto greener inhalers or apportioning blame. In the past he had defended the PBS listing of metered dose steroid inhalers for children, fighting for medicines that only came in metered doses, because they were entirely appropriate.
“I wrote an article a few years ago on this topic for a general audience and got a bit of blow back on social media, along the lines of ‘sure, fossil fuel companies are destroying our planet but let’s blame those people with asthma’ which certainly wasn’t my intent,” he said.
“This is not about blaming people with asthma for the state of our environment, and we know there are much bigger fish to fry, but it is an immense and urgent problem so every industry needs to look and see what they can do.”
The primary importance was always going to be choosing an appropriate device type for each patient, and the right device choice depended on many factors including age, dexterity, inspiratory ability and learning ability.
For many adolescents and adults, a dry powder inhaler, or soft mist inhaler, could be appropriate and
continued on Page 14

• Discourage excessive over-the-counter purchase of inhalers.
Think of the environment when prescribing – consider inhalers that contribute least to global warming, where suitable for the patient. If switching inhalers, train the person in correct inhaler technique.
Advise patients on safe disposal of used and unwanted inhalers.
continued from Page 13
avoid emitting the propellant gases of metered dose inhalers.
“It’s not about making people feel guilty, and for some people I’m not even going to bring up this issue in the conversation. If there’s a good reason for them to be on their medicine and it wouldn’t be wise for them to consider another option, then it’s not relevant to bring it up,” he said.
“If a pMDI is genuinely the safest choice for a patient, we should not make people feel guilty about using their inhaler, because this might make their disease control worse, which can be bad for people and the environment.
“And there are some people who are better served by the traditional metered-dose inhalers, particularly children under the age of six. We’re not suggesting there is anything wrong with using metered-dose inhalers in those kids when they’re needed and used with a spacer device.
“Some people have trouble inhaling quickly enough to manage the greener dry powder devices, because you need to be able to get air in quickly to sweep up the fine powder into your lungs. But an important point is that in asthma the main difficulty is breathing out, and most people with asthma can breathe in just fine.”
Dr Montgomery said that climate changes happening around the world would ultimately impact asthma.
Higher temperatures contributed to bushfire and smoke, and climate change seemed to be altering pollen seasons – lengthening and intensifying them – and that could be bad for some people’s asthma, as well as causing a lot of other bad health effects.
One of the ongoing challenges for doctors was managing patients with mild asthma, who often steered clear of preventive medications. But now combination therapies – including greener options – could help them.
“When I first started talking about this issue, I was thinking

the way forward was to a move to greener inhalers rather than the old-fashioned ones – and that it is still true – but what has become even more clear in recent years is the idea of using combination inhalers – steroids and long-acting beta2-agonists – in mild asthma, as needed,” he said.
“There are many people out there who are very symptom-driven when it comes to their use of asthma medicines, so when they feel tight, they’ll take their puffer and for the rest of the time they kind of forget about it – they’re not that good on prevention.
“All doctors have been able to do for them is keep trying to persuade them to take them regularly, but now we have medicines that act as relievers but have steroids mixed in with them, and if we can use more of those then it’s a way of reaching people who have poor asthma control.
“In people who struggle to remember to take a puffer regularly as a preventer, if they’re taking these combination medicines, they’re getting a bit of the steroids to settle down the inflammation each time they reach for some symptom relief, and the nice thing is we can do it in a green way because some of them come in the new inhalers.
“But it’s a slightly difficult culture change because when I was a junior doctor, I was taught that if you’re using steroids, you must use them
regularly – this was drummed into us – so this new way of using them purely as needed seems to be in defiance of what we were taught, yet there is good evidence for it.”
Dr Montgomery said that GPs could also make a greener choice, where appropriate, when starting people on an inhaler for the first time.
“The first step before prescribing is to try to be sure that the diagnosis is correct, as there is evidence that overdiagnosis of asthma is common. Ideally, diagnosis should be confirmed with spirometry or other lung function tests,” he said.
“Then, if there is no special reason to choose a pMDI, a good option could be choosing a less polluting choice, which in asthma is usually a dry powder inhaler. Teaching the patient how to use their new device is important whichever device is chosen.
“Sometimes changing inhalers can offer other advantages, such as eliminating the need to use a spacer and some patients who are appropriate for anti-inflammatory reliever therapy (using budesonideformoterol as their only inhaler) appreciate the simplicity of only using a single inhaler.”
Dr Montgomery said important work was being done in Australia in this space, primarily via the National Health and Climate Strategy, to improve respiratory health outcomes and reduce greenhouse gas emissions from respiratory inhalers.





The looming fallout from smoking and vaping has contributed to a name change for WA’s peak asthma group, as it widens the net to support people with other respiratory conditions.
Asthma WA, which turned 60 this year, is now known as Respiratory Care WA to reflect an expansion into chronic obstructive pulmonary disease, the degenerative respiratory condition that affects one in four Australians over the age of 65.
There are 40,000 people in WA with COPD, and an estimated 24,000 will die because of their condition this year. With COPD caused largely by smoking and vaping, Respiratory Care WA has warned it is seeing exponential increases in the rates of diagnosis and lung damage.
In its 60 years, the organisation has helped more than 300,000 West Australians with asthma or COPD, with increased demand for its services since COVID, including a 400% year-on-year growth in demand for its lung function testing.
But patient demand—particularly if vaping adds an extra wave of COPD cases – could test the limits of current services. Respiratory Care WA is the only free service in the State offering diagnosis through lung function testing, which is the only way for people to be correctly diagnosed.
Sir Charles Gairdner Hospital respiratory physician Clinical Professor John Blakey, an advisor to Respiratory Care WA, said lung function testing was essential in the diagnosis of asthma and COPD. It was highly valuable
By Cathy O’Leary

in assessing disease severity, progression and response to therapy.
“Unfortunately, our most common lung function test – spirometry – is infrequently undertaken,” he told Medical Forum. “The situation was worrying before COVID, and the number of tests done has dropped substantially since.”
Medicare data shows that in 199394, more than 300,000 of the tests were done in Australia but in recent years that had fallen to about 100,000 a year.

“This means many people treated for asthma or COPD have never had a formal diagnosis, and several studies have shown that about a third of people treated for these conditions don’t have them, and many more are treated for mild disease when it
is actually severe – or vice versa,” Professor Blakey said.
“In terms of how this affects outcomes, just imagine how poorly people with diabetes would do if we didn't measure their blood sugar, blood pressure or cholesterol.
“We always say asthma is both under and over-treated.”
Professor Blakey said the lung function testing that most people had – in terms of desktop spirometry – had not changed in 60 years, but the broader context had changed greatly.
“We now have many more helpful tests that we can do if the spirometry is better or worse than we expect from the symptom burden,” he said.
“These include newer desktop physiological tests like forced oscillometry technique (FOT) and Fraction of Exhaled Nitric Oxide (FeNO) that tell us things that spirometry doesn’t.
“We also have newer imaging techniques, with lower radiation doses and AI-assisted interpretation, and mixed techniques like PS-OCT and CPETCLE.”
Small, portable “home” spirometers could also be used to test or monitor people who could not routinely make it into clinic, and they had been shown to be robust and reliable.
“Knowing more about the type of problem that exists in an individual allows us to tailor therapy, and
we have a tremendous range of effective treatments available –inhaled, tablet, injection, devices or via allied health – that weren’t around 60 years ago,” he said.
“But we need to match the right treatment to the right patient. Doing this hugely reduces asthma exacerbations and the massive preventable harm people continue to accrue from the injudicious use of oral corticosteroids.”
While the number of people with COPD and bronchiectasis was smaller than the huge cohort of people with asthma, they were still more common than other ‘common’ diseases and were major causes of unscheduled healthcare use.
“Year on year, COPD climbs the rankings of causes of death – it’s third or fourth currently – and while there has been some nihilism around COPD, hopefully the message that the condition is not fully fixable but is certainly treatable is getting out there,” Professor Blakey said.
“More support for this population is essential, as we know that exacerbations of the condition lead
to a vicious cycle of deconditioning and vascular pathology. Early diagnosis is uncommon and a vital window for intervention is being missed.”
GPs urged to test
Respiratory Care WA is urging GPs to refer patients for a lung function test to confirm if they have asthma or COPD. Working with Respiratory Testing Services, it provides free lung function clinics, with the tests bulk billed.
Lung function testing involves a range of breathing tests that are completed while the patient is sitting in a chair, with the appointment usually taking about an hour. The results can help physicians diagnose and treat respiratory conditions.
Initial testing includes spirometry and FeNO, with additional testing available if the physician orders it or if it is indicated. All results are interpreted by a respiratory specialist before being sent to the referrer and GP.
Lung function testing is available for paediatric patients aged six years and over and adults, with
clinics in Joondalup, West Perth, Cockburn and Bunbury.
Respiratory Care WA also has respiratory health nurses and educators who can support people with asthma or COPD, while also encouraging them to keep in contact with their GP.
Their education covers:
• basic facts and symptoms of asthma and COPD
• how to recognise worsening respiratory health
• understanding prescribed medication and when to take it
• checking of device technique
It can also provide support in medication reviews, asthma or COPD care plans and selfmanagement of their condition and discussions regarding vaccinations.
Our treatment services include:
• Intensive Treatment Program (ITP) and a NEW Adolescent Intensive Treatment Program (AITP).
• Private Health Funded Day Programs including Schema Therapy, Teen DBT Skills, DBT Skills, RO-DBT, as well as Binge Eating Disorder (BED) and Post-bariatric surgery BED groups.
• Coordinated and collaborative individual and family outpatient treatment with Psychiatrists, Psychologists, Dietitians, Occupational Therapists, Physiotherapists and Specialist GPs.
For more information about our programs and services visit www.esuscentre.au
Esus Centre, 588 Hay Street Subiaco WA 6008 T 08 6255 9900 F 08 6255 9920
We are all hard-wired to react to outside stimuli. Deep in our brain, the amygdala makes sure of that. This pea-sized structure has us ready to stand and fight, or run and hide, depending on what life throws our way.

By David Andrew
In the past few weeks, we have seen world financial markets get the jitters on the expectation that the US could be headed for recession. If that’s not enough, we have the US presidential election, the slowdown in an increasingly belligerent China, and ongoing tensions in Eastern Europe and the Middle East. There’s a bit to worry about, right?
Globalisation suddenly looks less secure than it did. Trade protection is rising along with political tensions. In response, the US is onshoring manufacturing capability fuelled by some of the lowest energy prices in the world. We’re not writing the US economy off just yet. In fact, we could see a huge resurgence in US manufacturing capability.
With all this uncertainty, we are likely to see greater economic dislocation and market volatility rather than less. That’s likely to be uncomfortable.
So, how can you think about your financial security amid these fluctuations.
Risk is what you don’t see coming
First, let’s focus on risk. It’s important not to confuse uncertainty in the world, with risk. You see, we can plan for uncertainty, but it’s harder to plan for risk, because risk is what we don’t see coming.
The global financial crisis and the pandemic are great examples of real risks we didn’t see coming.
Conversely, global tensions and market uncertainty are predictable, we don’t know exactly what they’ll look like, but because we expect it, we can plan for it.
During the GFC and the pandemic, we learnt that the medical professionals who suffered most did so because of overspending and too much debt. The good news is that these issues can be resolved with good planning.
The other big cost during the GFC and pandemic was for those who sold down their investment portfolios in the expectation that there was much worse to come.
Here’s
Markets will be volatile, sometimes downright scary. If you panic during these periods, you’ll likely lose. Until a couple of weeks ago, we had had more than 350 consecutive trading days without a single market decline of two per cent or more.
Investors love these calm waters. It gives you confidence. But then the market did something it does often. It went down. A lot.
The financial press immediately went into fear reporting mode. One

headline from The Australian read, ‘ASX plunges: $100 billion wiped off stock market value.’
It’s hard to understand the drama when, typically, we get market pullbacks of at least 5% on average three times every year.
So, here’s the point. While it might feel prudent to exit the market during a volatile period, all successful investors know that short-term fluctuations are meaningless if you have a positive view of long-term expectations. Great investors use periods of volatility as opportunities to buy good long-term assets at cheaper prices.
The Millionaire Next Door is a timeless classic first published in 1996. It chronicles the factors that lead to financial success. It’s one of those books I've read countless times and each time I uncover a new gem.
The biggest financial challenge faced by many medical professionals is that being well-educated with a high-income does not automatically translate into financial independence. That’s a frustrating truth, but we have seen many cases where financial independence is elusive. There are many reasons getting in the way of financial success, and these include the embedded cost of

living in high status suburbs, the cost of funding a significant debt burden, providing economic life support for children, and a lack of time to focus on wealth accumulation.
Those who achieve financial independence either understand these challenges or find the answers they need to get on the right track. The good news is that financial independence is available to every medical professional. Even better, there’s a systematic way to achieve it.
In an increasingly uncertain world, having a clear plan for financial independence will give you an anchor point, a repeatable way to harness good habits to keep moving in the right direction.
Many years ago, we worked out that the appearance of affluence can be a thin veneer. It means you need to be careful who you admire and seek to emulate, and need to be mindful of who you look down on and wish to avoid becoming.
What we’ve discovered is that many medical professionals living affluent lifestyles consume almost all their income in funding their lifestyle. This reveals an uncomfortable truth. Financial independence for these individuals is virtually impossible.
Any assumption that the appearance of affluence equals sustainable, long-
term financial success is dangerous. Its important to run your own race, have your own plan, and celebrate your own success.
Remember, no one is as impressed with your possessions as you are.
Freedom of time is the biggest challenge facing medical professionals, and we meet very few who describe themselves as being in ‘lifestyle’ mode – the medical system just doesn’t seem to work that way. It’s more common to be pulled from pillar to post with the demands of a busy practice and family life.
Our research shows that truly prosperous families all seek three critical outcomes.
The first is a desire to make smart decisions with their money. This covers cashflow, tax, structuring and planning. Earning a big income and having little to show for it isn’t much of a prize and truly prosperous families understand this.
Next is a desire to ensure everyone they care about will be okay, no matter what. This covers financial security, education and opportunity, right down to helping children learn good money habits and avoiding parental economic dependency.
The final outcome is to live the best life possible. This includes finding the right balance between living
well today and securing financial independence for later. We describe this as a journey towards freedom of time, money, relationships and purpose.
Taking control of your financial future requires leadership and commitment and it begins with you. This leadership is important to protect your financial interests, achieve your goals and reinforce a positive money culture in your family.
As with every other aspect of your life, accepting personal accountability for managing your money increases the likelihood of a positive outcome. But taking control isn’t always easy or practical. That’s where having a family CFO (Chief Financial Officer) as the primary wealth manager for the family can be a huge advantage. A clear plan with help to implement and stay on track is a gamechanger.
The economy will always be uncertain and financial markets will be volatile and at times scary – you just need to factor this into your plans. The next 20 years will present economic challenges and opportunities that the purposeful will embrace and profit from.
If you have questions about our family CFO service, contact me personally at dandrew@capital-partners.com.au

Paul Davies has spent his working life in the air as a critical care paramedic. His mobile office is a helicopter and his job is to treat people and get them to a critical care facility.
By Ara Jansen
Paul Davies often wonders what happens to the people he delivers to the emergency departments after they’ve been transferred by RAC Rescue. Were they OK? Or did the worst happen?
Like any job, however, there are always those that stick in your mind, like the parents he rescued in a car crash. Months later at a party someone recognised him as that paramedic and the kids went out of their way to thank him for saving their parents.
Paul has spent almost two decades as a critical care paramedic working on the RAC Rescue helicopters. As part of a three-person team onboard for each mission, the helicopters are called to incidents within 200km of Perth and Bunbury. That can be everything from a road vehicle crash to lost hikers or a sailor needing to be airlifted off a tanker in turbulent seas.
Paul – known as Taffy – might be called on to hoist down into the ocean for a water rescue or down onto the side of a cliff to help an injured person back to safety. From a medical perspective, all of the medical decisions and actions in the field are his. An aircrew officer is trained to assist him if they are not working the hoist and other onboard rescue equipment, while the third crew member is the pilot.
As a kid born in Wales, Paul liked taking things apart – and at least in the early days, not being able to put them back together. He was fascinated in how things worked and he liked working with his hands.
In the late 1980s Paul took a backpacking holiday to Australia.
Three years later with 120kg of luggage, his then wife, a two-yearold and about $2000 in his pocket, the Davies family left the cold of Wales and migrated to Perth.
Getting in touch with some people he’d met while travelling, he made his way into a mine site job because he knew how to fix machines thanks to his previous work in large factories that made components and some studies in robotics.
Three years later, he saw an ambulance attending an accident and thought he “might give that a go”. He started training at St John

WA in 1994 and spent around a decade as an ambulance officer, working towards becoming a critical care paramedic. Eight months after the inception of the RAC Rescue helicopter, he became an airborne paramedic. Twenty years later, he’s their longestserving and part of an elite crew of 13 critical care paramedics. His job combines both being a paramedic and a rescue crew officer. The helicopters fit two patients, but usually only carry one. Paul is able to administer a wide range of drugs, put someone into
a medically induced coma and do everything he can to keep them alive until the helicopter can get to an emergency department.
His rescue bag carries about 10kg of drugs, dressings and gear such as syringes and tubes. The helicopter is equipped with various portable medical equipment such as a blood gas analyser, defibrillator and an ultrasound as well as equipment like night vision goggles.
“In a hospital you can have a whole team of people treating a patient but in an emergency situation like the ones we find ourselves in, it’s just me,” explains Paul. “I think I have seen just about any type of accident you can imagine.”
Like many professions who operate in high-stress situations, Paul suggests critical care paramedics are likely to have a bit of a black sense of humour to help get themselves through it.
“I think you have to be strong when you are on your own. You make those critical decisions and that’s the hardest thing. You have to take a stand.
“Each of us on the RAC Rescue helicopters has something we are in charge of, and we respect that
continued on Page 23









At Perth Radiological Clinic your chest imaging investigations are reported locally by WA’s largest team of fellowship trained accredited respiratory radiologists:
• Teaching hospital consultant radiologist appointments. Involved in multidisciplinary team meetings at FSH, MIHC, Mount Hospital, SCGH and JHC.
• RANZCR registered experts in occupational dust lung disease (RANZCR EODLD register).
• Expertise in all types of chest disease including malignancy, ILD, occupational lung diseases, lung cancer, vascular diseases and trauma.

PRC Specialist Chest Radiologist, Dr Stephen Melsom saysIf diagnosed early, particularly before symptoms develop, the progression of chest disease can be slowed
Dr Priority Line 9599 3929 perthradclinic.com.au
continued from Page 21
in each other. You have to be part of the team and have to be able to speak up. If you don’t, someone can die.
“Equally, I don’t think you could do the job without having that sense of humour or the ability to let off steam.”
As with most emergency medicinerelated jobs, it’s one of great thrills, rush and excitement in equal measure with a heart pounding and stomach drop in the other direction. He likens the work to a duck that looks calm on the surface but is paddling like mad under the water.
“There is a lot of downtime, but then you have these periods of intense energy and activity. And they can last for quite a while. When you are on your way to a job, you never quite know what you might find. You might need to be hoisted down 50 metres because the trees are too dense to land or you can’t land close to the people you need to help.
“It’s probably one of the best jobs in the world. Some days, coming back from a job, you fly across the ocean and you see dolphins or sharks – on a nice day, it’s a pretty special vantage point of Perth.”
That downtime, however, isn’t spent sitting around watching television. There’s a constant regime of re-qualifications, currencies and checks, some of which happen weekly, some monthly and some once a year. Then there’s the training, like a recent trip to a New South Wales facility which simulates wild weather during rescues, simulated rescues or helicopter hoist training at night, which in the middle of winter isn’t a lot of fun.
Plus, originally being a Welshman, Paul reckons he is not supposed to be predisposed to loving the ocean. He has a diving ticket but didn’t learn to swim until he was 18 after almost drowning as a young kid.
As part of the job, Paul also has to keep up his own fitness. At 60, he says that’s a lot harder than it was in his 40s, but he keeps on top of it with a regular schedule that includes swimming and walking


with a weighted backpack. From a mental health perspective, Paul says recognising and helping this type of stress has come a long way in 20 years and there’s so much more recognition and help available if an incident affects you.
A dad to four kids and grandad to three, Paul is indulging his love of fixing things and hating to throw anything out by renovating his house and helping fix things at his kids’ homes. When he’s not working, he also likes to go fourwheel driving with his mates and walking along the Bibbulmun Track.
His love for travel usually sends him hiking up mountains, such as Mount Kilimanjaro or the Inca Trail, followed by a good relax. Next on the list, he’s thinking the Kokoda Trail and a trip to Venezuela’s Angel Falls, the world’s tallest waterfall. Located in an isolated jungle the 1000m waterfall requires you sleep on rocky ledges while climbing it.
ED: The RAC Rescue helicopters are funded by the State Government, managed by the Department of Fire and Emergency Services (DFES) and sponsored by RAC.
Vaping changes have been made but there is still no clear pathway ahead for GP, pharmacist or consumer.
Eric Martin reports
As of 1 June 2024, it became illegal for any business other than a pharmacy to sell vapes or vaping products in Australia, irrespective if the vape contained nicotine or not.
The move has been hailed by GP and specialists’ groups as a step in the right direction, however it has put GPs in an even more pivotal role in smoking cessation.
Dr Ramyan Raman, the Chair of RACGP WA, said that from a clinician’s perspective, while the vaping restrictions were supported, one of the most surprising aspects was the decision to redesignate vapes as a pharmacy supplied product.
“GPs have been on the frontline of smoking cessation for a long time in Australia, it's part and parcel of preventative health. We know that patients will need to have a conversation with their pharmacist about their options whenever they purchase vaping products, and the system will need monitoring to ensure there is genuine compliance at the point of purchase,” Dr Raman said.
THC and vitamin E acetate, although around one in eight cases in the largest study to date were from reported use of nicotine-only products. Their environmental impacts include waste, fires and indoor airborne particulate matter, which, in turn, are likely to have adverse health impacts, the extent of which cannot be determined,” the report said.
Overall, it concluded that nicotine was highly addictive and there was clear evidence of ‘widespread use and addiction, particularly among youth,’ around the world.

One of the key factors touted by the ‘vape-to-quit’ campaign has been the relative success of New Zealand in using the electronic devices to lower traditional tobacco consumption. The much-cited 2022 study by Burrowes et al. found that vaping showed good potential as a medium for quitting.
“Based on our data the use of e-cigarettes in a “vape to quit” strategy is attractive to smokers, based on the high uptake of their selected use as a smoking cessation aid (75%),” Professor Burrowes’ team concluded. “In total, 16% of those in the follow up “vape to quit” cohort were both smokefree and vape free.”

“We are especially interested in what that means for the prescription process and GPs. We have a responsibility to support this primarily because vaping can cause quite serious respiratory damage, even if we are still not particularly clear about the full long-term impact of vaping.”
The National Centre for Epidemiology and Population Health compiled a report for the Australian Department of Health that was foundational in the department’s approach to the issue and the subsequent ministerial decision.
They reported that the prevalence of dependence symptoms ranged from 23-46% among exclusive e-cigarette users in 15 studies. Among exclusive e-cigarette users, 46.1% reported use 30 minutes after waking, 46.2% reported strong cravings, 46.2% reported the need to use and 22.8% reported withdrawal symptoms when abstaining.
“There is conclusive evidence that e-cigarettes cause acute lung injury, largely linked to e-liquids containing
However, Dr Raman noted that because there were pros and cons with each of the options available for cessation, it depended on the actual patient, their specific needs, and the GP’s expertise in selecting the most tolerable product in those circumstances – starting with nicotine replacement, using gum or lozenges, then followed by medicines such as Champix.
“When those medications were initially released, there was a lot of interest and uptake in terms of how they would work. For example, Champix was very popular with patients and at that time, it was determined to be the first and best treatment,” she said.
“But importantly, that discussion involved a counselling process with the patient. There was a consultation explaining what the side effects were, examining where they were in their motivational change cycle, and looking at their past medical

continued from Page 24
history and current medications to ensure there were not going to be any adverse interactions.
“Everything has side effects, and the original system was not perfect, but at the same time, with GPs now required to issue prescriptions for a nicotine-replacement device, we are potentially being asked to favour an option that is definitely not first-line in terms of smoking cessation.
“There are a lot of misconceptions in the community about the effectiveness of vaping as a nicotine replacement therapy, but that's not the case at all – it’s not first line or even second or third line, for that matter.”
Australian research conducted by the department found that there was insufficient evidence regarding the exacerbations of respiratory disease or changes in respiratory symptoms, lung function and other respiratory measures, to justify recommending vapes.
“There is limited or insufficient evidence that use of ENDS (electronic nicotine delivery systems) in non-smokers leads to acute reductions in lung function and other respiratory measures. Among smokers, there is moderate evidence that use of ENDS increases heart rate, systolic blood pressure, diastolic blood pressure and arterial stiffness acutely after use,” the report said.
“There is strong evidence that e-cigarettes increase the uptake of combustible smoking in nonsmokers, particularly youth, and limited evidence that freebase nicotine e-cigarettes are efficacious in the clinical setting as an aid to smoking cessation. There is limited evidence that ex-smokers who use e-cigarettes have around double the likelihood of relapse to resuming smoking than ex-smokers who do not use e-cigarettes.”
“As such, we don't want these things to make their way into the hands of young patients - we need
that close monitoring and while there's still questions that remain,” Dr Raman said.
“And that's not to undermine the role of the pharmacist in any way at all, but rather highlight the need for clarification around that process. How is that conversation going to be had? And what is that monitoring and compliance process?
“We don't want pharmacies to become like the new corner store, and they don’t want that either, going by the comments that they have made. It is a real concern for pharmacists as well.”
However, one of the biggest challenges facing GPs is potentially locating a pharmacist willing to stock vaping products as nicotine replacement services, especially after the amendment to the legislation pushed by the Greens and Nationals, allowing people 18 years or over with no prescription to purchase – effective as of 1 October 2024.





Medical Forum spoke with the WA Pharmacy Guild last month, when changes were announced and the guild’s policy and media officer, Mr Alan Hill, said that the decision to stock vaping products would be up to individual pharmacists.
“As was the case prior to that date, nicotine vapes are available from community pharmacies. However, only to patients who have a valid prescription. However, individual pharmacies have the discretion on stocking and supplying vaping products, early feedback from pharmacies is that post 1 October, many may or may not,” Mr Hill said.
“While it is too early to effectively measure any increase in demand at a sector-wide level, patients providing a valid prescription should be aware of the possibility that their preferred community pharmacy will have to order in the stock, which may take 24-48 hours.
“The WA Branch is yet to be advised of how this legislation will be implemented in community
pharmacies. However, currently, there is no guidance or protocol for pharmacists regarding their requirements for patient consultation to establish a clinical need for a nicotine containing vape, or the regulatory compliance of these instances.
“Vaping products have not been approved by the Therapeutic Goods Administration (TGA) and no nicotine-containing vape is listed on the Australian Register of Therapeutic Goods.”
Similarly, as far as Dr Raman was aware, there had been no guidance from the government or the health department in terms of what devices, mechanisms or processes was going to be recommended by GPs.
A pharmacist, who stocked vaporising products, told Medical Forum that the product they stocked was not compatible with any of the pre-existing vaporiser products that patients already owned.
“I'm a practising GP. We would know if something came through
than 30,000 patients annually*
Our purpose is to design cancer care experiences that deliver the best possible life outcomes close to home.
In WA, we have 8 metro and regional centres dedicated to offering fast access to care, delivered utilising evidence-based treatment techniques.
*GenesisCare data held on file
for the patients in our clinic that specified this is what we need to give them,” Dr Raman said.
“We are now in a position where there's a lot of information out there for patients, readily available on multiple platforms, but the reliability of this information can be questionable – especially on social media platforms. Just in my population of patients, there's a lot of myths about the use of nicotine containing e-cigarettes.”
Whatever the outcome of the ongoing political and medical discussion around vaping, the article in the Medical Journal of Australia in December by Dr Samantha Howe from Melbourne’s School of Population and Global Health holds true:
“The COVID pandemic saw each jurisdiction charting a different course to manage the pandemic. Some policies and jurisdictions were more successful than others. Sharing the lessons of what worked and did not work, and why, is an important part of transferring policy success that will be a key part of preparing for current and future public health challenges.”

Scan here to learn more or visit: genesiscare.com
CAHS development services team have produced a series of podcasts to help parents and their GPs navigate the science and the support around child development issues.

By Eric Martin
Children can be challenging patients at the best of times, and often the most complicated part of the consultation is explaining the various treatment pathways and options to parents, especially if a neurological or developmental issue is suspected.
So, the Child and Adolescent Health Services (CAHS) has come up with a digital solution in the form of Kids Health Matters, the new podcast series to help GPs and parents keep abreast of topical medical issues that impact children and the local services available to support families.
According to the CAHS Child Development Service’s Paediatric Head, Dr Brad Jongeling, the eight-episode series, hosted by professional broadcaster and mother of two, Ms Dani Shuey, Coordinator of Nursing, Ms Danielle Engelbrecht, and Dr Adelaide Withers, Respiratory Consultant, represents a new approach to providing accessible information.
“I think it's been needed in our service for some time. When parents see a clinician or they approach their telehealth support, they'll be better equipped and more knowledgeable, which is always helpful when supporting your child,” Dr Jongeling said.
“Similarly, GPs have got such a broad range of responsibility across adult and paediatric needs. Keeping up to date can be a challenge and knowing what services are available and how to access them isn't always easy.
“This series provides an avenue for greater, up-to-date knowledge about these processes, such as how to support language and development and the early signs of developmental challenges.”
The podcast has already attracted more than 5000 listeners.
“It's a good way of getting a message across and introducing potentially complex topics. The combination of Dani as the broadcaster and Danielle as the nurse meant there is an ability to cross the clinical and parent threshold - we're all parents, but we're parents as clinicians,” Dr Jongeling said.
“Having a parent who is not a doctor ask those questions and relate it back to her own journey, with her own children, makes it

more applicable. It also enables those questions to be asked that we might not think of as a clinician, because you already know how the hospital and health service works.”
“As a parent myself, I've been in those situations where you're just so anxious for your child, that you don’t always hear fully or completely understand what your doctor is telling you. And there's no fault with that,” Ms Engelbrecht confirmed.
“But by the time they get to see their nurse, they have calmed enough that the nurse has the time and opportunity to use lay language to explain what the diagnosis means for their child, and the next steps from there. And that's why nurses and doctors work in partnership so well.”
“A thing I love about this podcast is that our specialist doctors and nurses now have the opportunity to explain their work and what services are available in a way that our listeners can really take the time to digest and understand. The podcast showcases the expertise we have at CAHS, but also shows how well our services work in partnership as a multidisciplinary team, with our doctors, nurses and allied health practitioners.”
The team pointed out that when people thought about CAHS, they often focused on Perth Children’s Hospital (PCH) often overlooking the resources provided for families in the community.
“The acute care that is provided at PCH is second to none, but so too is the preventative care and the post-discharge care such as the supports that Child and Adolescent Community Health (CACH) and Child and Adolescent Mental Health Service deliver,” Ms Engelbrecht said. “Our service structure is quite different and unique to WA, particularly around how our child and community health programs are run and the support that they provide to new mothers and new families, and our Child Development Services.
“Many families aren't aware of our services and that's where there is an important link with their GP. They see their GP when they're concerned about developmental milestones or other issues around their child. Just being able to ask a GP what community supports are available or how to get a referral to CAMHS for example, to access services is invaluable. Being able to hear about things like that in our podcast, to know what's available for families who are really struggling, are important.
“The more families know about our services, the better they can request and seek the support that they need. Similarly, when listening to our podcast, parents know that it's factual, evidencebased information, and they can feel empowered to manage health matters for their children.”
continued from Page 29
Dr Jongeling explained that much of the podcast content was about early intervention and that wasn’t just about seeing someone in the child development service.
“It's about being part of a parenting group; it's taking a child to a toy library; it's being involved with play groups; it's exposing them to outdoor play. All of those are factors which a podcast series like this can both promote and highlight,” he said.
“While you might also be on a journey to a comprehensive assessment, there's a whole lot more that can be done to support children in the early intervention phase than specific therapies for a specific diagnosis.
“There is a proliferation of online disinformation or, unfortunately, incorrect information, and parents are struggling to find an accurate resource that they can trust. In these days of social media, it's essential for parents to have a resource that they know is medically approved. And this is something that the health service can provide – an evidence-based introduction to topics that parents can go to as their first step in exploring issues.”
Presenter and regular guest on the podcast is sleep and respiratory paediatrician Dr Adelaide Withers. She highlighted this misinformation in the community about what was considered normal for sleep, including whether children should be using medication to help them sleep.
“So, we focus in the podcast on what was developmentally normal for kids and when there might be a medical problem causing sleep issues. And we've stressed that GPs and child health nurses are the first port of call in that instance, and that they would be able to direct parents appropriately if it might be something like sleep apnoea, or whether they need to see a sleep specialist,” Dr Withers said.
“That was a great episode because we gave people information about what to be concerned about, some simple strategies and when they should seek more advice.
“One of the biggest misconceptions is ‘my child should have perfect sleep’ and ‘everyone else is judging me because my child doesn't have good sleep.’ It can cause a huge amount of anxiety for parents because there's a wide range of what's developmentally normal.
“Some kids just need less sleep than others. They are unsettled
Creating tiny, laboratory-grown human organs is becoming one of the latest frontiers in the search for new personalised medical treatments.
Known as organoids, miniature human organs grown in laboratories using a patient’s own cells allow researchers to learn about diseases and test new treatments more accurately than ever before.
A new Curtin University-led project is looking to enhance this breakthrough’s real-world impact and could see Australia become a global leader in this space.
Researchers plan to use cutting edge technology to make organoid
research more effective and efficient, with the creation of the Western Australian Organoid Innovation Hub (WAOIH) using more than $500,000 from the WA Government’s Future Health Research and Innovation Fund Enabling Scheme.
The hub will be based at the Curtin Health Innovation Research Institute and use advanced technology to take images of the organoids, with the team using machine learning for quick and accurate image analysis.
The FHRI grant will see upgrades to equipment, which study lead Dr Ben Dwyer said would allow the hub to capitalise on the
and wake up a lot each night. It doesn't necessarily mean there's something wrong with that child, or there's something wrong with your parenting. Sometimes, it can be a sign that there might be something else going on.
“However, parents can be quite scared about sharing this information with their friends because they're worried about being judged.
“The podcast highlights the huge range of strategies to improve sleep. Which one works depending on that child’s developmental stage, abilities and the family needs because for some people, a child waking up six times a night is not actually a problem for them, while others are expecting their six-month-old baby to sleep for 14 hours – and that's not going to happen.
“We also focus on support for the parents themselves. If your child is not sleeping well, you're going to be exhausted and sleep deprived. We encourage parents to see their GP – just for them – because we know that's got huge impacts on the rest of the family as well.”
Co-host Danielle Engelbrecht said some thought had been put into designing the podcast series to include topics that could be
growing momentum surrounding organoid research and significantly enhance the current liver cancer organoid program’s capabilities.
“Organoids can mimic real human organs better than traditional cell cultures, so they’re excellent models for studying human biology and disease,” Dr Dwyer said.

“We currently use organoids in the context of liver cancer to better

isolating for families.
“Families can feel incredibly isolated,” Ms Engelbrecht said.
“I know that feeling as I also have a child with developmental issues. But if your child or young person has a diagnosis of anxiety, depression, ADHD or ASD, it is so important to know that you're not alone as a family and your child's not alone.
“There are plenty of people out there who have experienced these issues as well and they do live
functional, happy, well-supported lives. But it's knowing how to get that early intervention. How to get that support and realising that you don't have to feel embarrassed about this diagnosis or that you're experiencing this issue.
“We wanted the podcast series to be wide reaching and we were very careful in the subject matter we selected because we wanted there to be something for everyone. There is a great range of topics and I think every parent will find value in
listening to the series,” Dr Withers explained.
“But at its heart, it's about being extremely clear where to get help.
“We see lots of children at CAHS who have chronic medical conditions. And it has a significant impact, not only on a child, but on that child’s family. It has a huge flow on impact, and support is needed and there are services available to help everybody.”
Dr Jongeling said CAHS now had an online referral form for the Child Development Service via the CAHS website and was creating more resources.
“In addition to these resources, the Kids Health Matters podcast is a great start for GPs and families,” he said. “GPs are well placed to know the family and provide that referral to allied health supports, in addition to giving advice around behavioural and educational strategies, which remain essential, even well before a diagnosis is considered.
“They have a great knowledge of neurotypical development and where there's variation, and the need for support for families –including when they might direct them towards a service such as ours.”
understand disease mechanisms to develop new treatments, and also for large scale screening experiments to repurpose approved compounds for use in cancer treatment.
“Because they’re made from a patient’s own cells, organoids can also be used to determine which treatments are most likely to be effective or may result in side effects for that specific patient, paving the way for personalised medicine.”
Dr Dwyer said since establishing a liver cancer platform, there was significant demand to apply this emerging technology and expertise to a broader range of diseases and cancers.
“Being able to automate our imaging and liquid handling equipment will allow the WAOIH
to work faster and conduct more experiments at once, and this will allow us to broaden our scope of research,” he said.
“Collaborating with the National Drug Discovery Centre in Melbourne and the Human Organoid Innovation Hub in Calgary, Canada, also offers access to national screening programs and partnerships with global experts, which will enhance the international impact of WAOIH’s work developing new treatments.”
Other partners include the Cancer Research Trust, Perkins Cancer Biobank, Australian Centre for RNA Therapeutics in Cancer, Cell and Tissue Therapies WA and the WA Data Science Innovation Hub based at Curtin.
The WAOIH evolved from the patient-derived organoid drug screening platform of the Liver Cancer Collaborative established in 2021, which expanded thanks to previous funding from the Ian Potter Foundation, Minderoo Foundation, Charlies Foundation, McCusker Foundation and WA Health Department.
Dr Dwyer said these latest developments would help position WA as a leader in innovative drug discovery.
“This will create a state-of-the-art pipeline to provide personalised, precision medicine to patients across the world,” he said.
There is a new weapon in the battle against the flu, writes molecular virology expert Vinod Balasubramaniam.
Clinical trials of an mRNA vaccine for influenza have begun, and researchers expect broadly positive outcomes in the battle against the widespread illness that kills up to 650,000 people around the world each year.
A staggering 99% of deaths in children under five years of age in developing countries are due to influenza-related infections, according to the World Health Organization.
The current crop of influenza vaccines has limitations in effectively combating the billion cases of seasonal influenza each year as they provide immunity against only one specific existing strain or mutation. The propensity of flu viruses to mutate into new strains means vaccines must be continuously monitored and reformulated each year.
But a universal influenza vaccine using mRNA technology, which was used with success during the COVID pandemic, has the potential to provide broader and longerlasting immunity against diverse influenza strains.
The technology allows for rapid development and deployment and offers versatility in targeting multiple regions of the influenza virus.
New or mutated influenza variants are always a threat, particularly those originating from animal sources. Pandemics such as the Spanish flu of 1918, which killed 50 million people, and recent outbreaks of the viruses underscore the persistent threat posed by influenza. It also underscores the urgent need for a universal influenza vaccine capable of safeguarding against all subtypes of the virus.
In recent years, lipid nanoparticle (LNP) encapsulated nucleosidemodified mRNA (‘mRNALNP’) vaccines have emerged as a potent tool in combating influenza and other infectious diseases.
These vaccines use mRNA created in a laboratory to teach cells how to make a protein, or even just a piece of a protein, that triggers an immune response inside our bodies.
The limited efficacy of current vaccines can be attributed to their focus on only generating strain specific antibodies against the influenza virus hemagglutinin (HA). This is a protein within the virus which causes infection.
To broaden protective immunity, novel vaccine strategies aim to elicit responses against more proteins. One promising avenue involves triggering T-cell responses.
T-cell-mediated immunity not only eliminates infected cells but also correlates with improved outcomes in individuals affected by influenza. Animal studies have demonstrated the protective role of T-cells against various influenza virus strains.
These vaccines, exemplified by the successful development and global deployment of mRNALNP-based COVID-19 vaccines, elicit robust T-cell and antibody responses. These vaccines also offer the advantage of rapid production and adaptation to target emerging viral variants.
While several mRNA-LNP influenza vaccines are in development, most prioritise stimulating antibody responses and under-exploit the potential of T-cell immunity.
The development of a universal influenza mRNA vaccine requires careful consideration of several pivotal factors to optimise its effectiveness and suitability. Initially, the vaccine should target regions within the influenza virus responsible for viral replication but are less susceptible to mutation. By concentrating on these regions, the vaccine can elicit broad and enduring immune responses, offering protection against an array of virus strains. Encapsulating

nucleoside-modified mRNA within lipid nanoparticles has emerged as a promising strategy to bolster vaccine effectiveness.
These LNPs shield the mRNA from degradation and facilitate its delivery to target cells, where it can be translated into viral proteins, triggering the body’s immune responses. Additionally, optimising the mRNA sequence can boost protein reaction, ensuring robust and persistent immune responses post-vaccination.
Another crucial aspect of designing a universal influenza mRNA vaccine is incorporating adjuvants or ‘agents’ to amplify vaccine efficacy. Integrating adjuvants into the vaccine formulation improves vaccine efficacy, especially in individuals with compromised immune systems.
The design of a universal influenza mRNA vaccine should prioritise triggering T-cell responses, enhancing mRNA delivery and expression, incorporating adjuvants to boost efficacy and addressing practical considerations for global distribution.
By tackling these critical aspects, a universal influenza mRNA vaccine holds the potential to revolutionise influenza prevention and control efforts, offering comprehensive and enduring protection against seasonal and pandemic influenza strains.
Ongoing advancements in mRNA technology, such as improved delivery systems and stabilisation methods, further enhance the prospects of creating a universal influenza vaccine that ticks all the boxes.
The US National Institute of Allergy and Infectious Diseases has started enrolling volunteers at Duke University in North Carolina to test its experimental mRNA-LNP vaccine against seasonal influenza,
It is frustrating when a patient has to repeat their medical history over and over again. Digital health expert Mark Woodland explains.
Imagine a patient going to their medical appointment and the doctor already knows their medical history.
Better still, patients do not have to waste the 15-minute appointment repeating the details of their previous physiotherapy or speech therapy session because the clinical notes are digitally logged and on file.
We shouldn’t have to imagine. Our medical histories – therapy sessions, test results, treatment plans and progress, insurances and clinical notes – should be stored in a centralised, secure electronic health record system accessed by providers, practitioners and carers. If our medical histories were properly stored, we could avoid duplicate tests and redundant treatment plans, and avoid the embarrassment of repeatedly explaining our medical condition. It would also spare us the frustration of having to justify our NDIS plan.
A recent Productivity Commission report revealed that better integration of digital technology into healthcare could save more than $5 billion a year and ease pressures on the entire system. It also revealed that despite a $2 billion investment in the My Health Record system, patient data is still fragmented.
My Health and the many other bitsy electronic patient record platforms have resulted in fraud, inefficiencies and gaps in care.
continued from Page 32
one of several universal influenza vaccine candidates now in the pipeline. Another clinical trial has begun at the institute’s Clinical Centre in Maryland.
Despite their promise, challenges remain in effectively delivering
It’s clear that healthcare records are not up to date, they are not genuinely integrated and healthcare providers are not actually using them. The whole point of health records is to physically trace a patient’s health journey so that informed and realtime clinical decisions can be made about treatment.
One of the biggest pain points, especially for people with a longterm or chronic illness, is that they need to explain and justify their illness at every appointment. It’s demoralising and a waste of time. Without clinical notes, the lack of data just perpetuates the sloppy cycle of duplicated treatments, ineffective routines, no results and in the case of the NDIS, failing to meet its intended purpose.
Integrated digital medical records is a big fraud reduction for the NDIS and aged care and it also offers checks and balances for caregivers and family members so that they know how a person is doing.
When payments are tied directly to logged clinical notes, there's a natural incentive for health providers to ensure currency, accuracy and completeness in their clinical documentation.
This payment model aligns with the shift towards value-based care, where reimbursement is tied to the quality and outcomes of services and care rather than the volume of services provided.

The benefits of improving electronic medical record keeping system is a game-changer that will bring power and control back into the hands of those who need it.
• Patient control – give patients the power to actively participate in their own care. With platforms’ AI-driven voice command, patients directly input details about their health without the need for typing or navigating complex interfaces.
• Better use of appointment time – reviewing and gathering a patient's health status before an appointment reduces time wasted gathering and reviewing patient information during the appointment so there’s a focus on a patient's current status for future health.
• Continuity of care – especially in scenarios where patients receive treatment from multiple providers or transition between healthcare settings.
• Reduce fraud, waste and cost inefficiencies – once clinical notes are entered into the system, it creates a verifiable trail of care, and users can track their budgets and insurances. It ensures services rendered are accurately documented and align with billing claims.
ED: Mark Woodland is co-founder and CEO of digital health platform Kismet.
mRNA molecules into a vaccine due to their inherent instability. Overcoming these challenges is essential for the successful development of universal mRNA vaccines for influenza.
This aside, the advancements in mRNA vaccine technology have paved the way for innovative approaches to crystallising
universal influenza vaccination, offering hope for broad protection against this ever-changing virus.
ED: Dr Vinod Balasubramaniam is Associate Professor (Molecular Virology) at the Jeffrey Cheah School of Medicine and Health Sciences at Monash University Malaysia.
Originally published under Creative Commons by 360info.
Advert removed in compliance with Medicines Australia's Code of Conduct and the Therapeutic Goods Administration's Therapeutic Goods Act.
https://medicinesaustralia.com.au/code-of-conduct/about-the-code/ https://www.tga.gov.au/legislation-legislative-instruments

In early August, IV drip bag stores had been almost completely depleted in Australian hospitals with IV fluid supplies hitting crisis levels. … there is nothing inherently complicated in putting saline or dextrose into plastic bags with an outlet tube. None of the core components are rare or in short supply … Manufacturing standards matter but this is not building a spaceship.
According to The Australian, glucose 5% bags, Hartmann’s solution bags, sodium chloride 0.9% bags, and water for injection bags were most affected. Health departments called on doctors in hospitals to ration IV fluids. (Yes, Minister stuff!) Options included using the smallest volume of IV fluid appropriate, limiting IV fluid administration in day surgery, minimising fasting in surgical patients to reduce the need for fluid replacement and giving medicines by alternative methods.
Allegedly some hospitals had almost no supplies of IV drip bags. What? IV fluids are an absolute bedrock of hospital care.
The TGA blamed a global shortage. Yet New Zealand apparently has no problems, nor does the US! The Federal Government formed a “response group”. The health minister was silent.
Call me a simple soul but there is nothing inherently complicated in putting saline or dextrose into plastic bags with an outlet tube. None of the core components are rare or in short supply. Manufacturing standards matter but this is not building a spaceship.
The question arises – how could this have happened? The response group may produce a report in 18 months or so.
Meanwhile, my questions are firstly, have we learned nothing from the pandemic response? Have we not learned about supply chains, inventory and reliance on imports. My suspicion is we import these bags, despite producing here to supply New Zealand. Can we not produce for local needs? If not, why? Guesses welcome.
Secondly, why was this not foreseen? It has apparently been coming for 18 months. Are we running a “just in time” system? Perhaps the “response team” should have been established 12 months ago.
Thirdly, why are all the highly paid health bureaucrats and health ministers asleep at the wheel? This is supposedly a first world country. Why do systems not exist to ensure that products as essential and basic as IV drip bags do not run out?
This is absolutely not good enough and is 100% on government.


By Dr Conor Murray, Radiologist, Nedlands
You may not be interested in lung nodules, but lung nodules are interested in you.
In May 2025, an Australian National Lung Cancer Screening Program (NLCSP) will commence and will uncover thousands of prevalent lung nodules in West Australian patients, each requiring consideration and appropriate management.
Up to 10 subsequent rounds of biennial screening with potential additional interval scans will generate further though smaller waves of incident nodules thereafter.
Lung nodules are very common on chest CT scans in smokers and non-smokers. Thirty-nine per cent of smokers screened for lung cancer at Royal Perth Hospital in 2009 had lung nodules, though in a high-risk population screened at Sir Charles Gairdner Hospital between 2010 and 2020 only 9% had nodules of sufficient concern to warrant further investigation (1.4% were cancer) – this data is consistent with the international experience that almost all lung nodules are benign.
A lung nodule is defined as a rounded or irregularly bordered discrete opacity on chest X-ray or CT less than 30mm in diameter (those larger than 30mm are designated “masses”).
One of the most mentioned lung nodules in the radiology report is, paradoxically, not a nodule. This is the erroneously termed peri-fissural

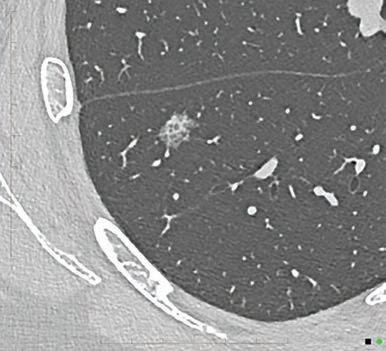
nodule (PFN), sometimes known as a juxta-pleural nodule.
A PFN is not a nodule in that it is not round or irregular, it is instead faceted and polygonal when considered in three dimensions and appears pyramidal or lentiform in two dimensions. PFNs are normal pulmonary lymph tissue, and their characteristic shape is dictated by the tension of the surrounding interstitium as they are only firm enough to ‘peel’ the interstitium back and not bulge or invade it in the way a true lung lesion would.
Lung nodules are analogous to calcifications on mammography, being very common with radiologists trained to recognise the difference between benign and malignant features. From a radiological perspective, the most prognostic features of lung nodules are their size, density and growth velocity.
The larger the nodule the more likely it is to be malignant.

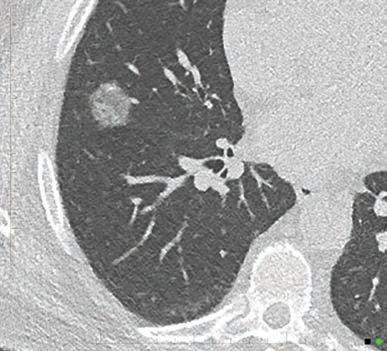
The density characteristics on CT affects the probability of malignancy as the density pattern reflects the histological differences between lesions.
The least suspicious nodules overall are solid nodules – most often uniform soft tissue density (though may contain calcium and rarely fat) and completely replace normal lung. This is because almost all the benign lesions (including granulomas, PFNs and hamartomas) are histologically confluent which translates to their uninterrupted density on CT.
The most suspicious are part solid nodules, that is those that are part ground glass and part soft tissue density (with the ground glass portion evoking a pre-invasive component and the solid portion an invasive component). Less commonly, the non-soft tissue component is an air-cyst density with the air cysts due to destruction of basement membranes with secondary conglomeration of air sacs by the cicatrising effect of invasive malignancy.
Of intermediate suspicion are the non-solid nodules which are of a pure hazy or ‘ground glass’ density. These nodules are the most specific and are usually indicative of atypical adenomatous hyperplasia (a pre-cursor to early invasive adenocarcinoma) or focal interstitial fibrosis. Their hazy appearance is
Lung nodules are very common and the great majority are benign. Nodules larger than 6mm, with short doubling times or with part-solid density are of greatest concern
The Australian National Lung Cancer Screening Program commences in 2025 and will uncover prevalent lung nodules in thousands of people. Doctors will be supported by the National Cancer Screening Registry and education from representative colleges.
The risk of malignancy per nodule in the initial round will be determined by the PanCan model and in subsequent rounds LungRADS.
due to fine intermixing of dense (lesion) and non-dense (normal lung) components.
Nodule growth is expressed by volume doubling time (VDT). The VDT of a nodule is the number of days required for a nodule to double its volume. A longer VDT indicates a more benign lesion, whilst a short VDT suggests a higher histological grade.
According to most studies a volume doubling time less than 500 days represents a high likelihood of malignancy and the longer the VDT the less concerning the lesion.
The NLCSP will use a risk prediction model for the initial round of screening (the Pan-Canadian Early Detection of Lung Cancer (PanCan) risk model). This calculates the probability of lung cancer on a continuous scale.
PanCan incorporates patient characteristics (age, sex, presence of emphysema and family history of lung cancer) and nodule characteristics (size, type, location, number of nodules, and signs of spiculation). A nodule risk index of less than 1.5% is regarded as benign, 1.5% to 5% low risk, 6% to 30% moderate risk and greater than 30% high risk of malignancy.
The PanCan result will determine if a patient requires further testing immediately and guide the schedule for subsequent screening rounds.
For the subsequent rounds, LungRADS will be used as the reporting template. This was developed to

standardise the reporting and management of lung nodules.
Lung-RADS models cancer risk on three nodule characteristics – size, density and growth.
The Lung-RADS category 1 means negative (no nodule), 2 means benign, 3 means probably benign, 4A means suspicious (with 5% to 15% probability of clinically active cancer in the next year), 4B means very suspicious (with greater than 15% probability of cancer in the next year), and 4X means very suspicious (not otherwise specified).
For a deep dive into the rationale for the adoption of these lung nodule management models we refer you to Medicare Service Advisory Committees March-April 2022 Public Summary Document.
The Australian National Cancer Screening Register (NCSR) will support the NLCSP by:
• maintaining a national database of lung screening records
• reminding participants when they are due or overdue for lung screening and when they need to take action after a scan
• providing participant lung screening reports to
o assist radiologists in reporting LDCT scans
o support healthcare providers in recommending follow-up investigations
• enabling participants to access their lung cancer screening information in the register, including updating their participation
• monitoring of the effectiveness, quality and safety of lung cancer screening to improve delivery of the NLCSP.
Minimising overdiagnosis is critical to the success of any screening program. The risk of overdiagnosis requires careful consideration before embarking on invasive investigations. The most common lung cancer is an early invasive adenocarcinoma, and these lesions are typically indolent, therefore elderly patients with multiple co-morbidities may not live long enough to suffer from these lesions.
Author competing interests – nil
By Dr Nick Fitzpatrick, ENT Surgeon, Nedlands
The terms unified airway or united airway describes the concept that inflammation affects upper and lower airways by similar mechanisms and diseases exhibit similar anatomical, histological and immunological features.
Unified airway pathophysiology may manifest as rhinitis, rhinosinusitis and nasal polyposis in the upper airway and asthma or bronchial inflammation in the lower airways.
The airway is an area of multidisciplinary crossover and multiple specialists may be involved (GPs, ENT surgeons, respiratory physicians and allergists). Each has their own clinical priorities and approach.
The clinical importance of the unified airway concept is that these conditions should not be investigated and treated as isolated entities, rather the diagnosis of lower airway inflammation should prompt workup of the upper airway, and vice versa. Several clinical studies demonstrate a bi-directional naso-bronchial
The unified airway concept highlights that inflammation affects the upper and lower airways by similar mechanisms
A multidisciplinary, patient-focused approach comprehensively managing both upper and lower airway pathology together generally leads to improved overall outcomes across the entire airway Sinus and nasal surgery play an important role in managing combined airway disease.
relationship, where nasal stimulation can induce bronchial inflammation and lower airway provocation results in sinonasal inflammation.
The epidemiology also supports an interconnected airway model, 20-25% of patients with chronic rhinosinusitis (CRS) have asthma and 10% of asthmatics have CRS. In patients who have CRS with


nasal polyps, rates of asthma are even higher (40-60%), which is associated with more severe asthma and poorer lung function (lower FEV, steeper FEV vs. age) –the equivalent of smoking a pack of cigarettes per day.
The coexistence of allergic rhinitis (AR) and asthma is higher still, 1538% of AR patients have asthma and 80-100% of asthmatics meet diagnostic criteria for AR.
A range of other diseases are associated with the underlying inflammatory pattern (predominately eosinophilic, IgE mediated) and would benefit from review by an otolaryngologist as their diagnosis may be more challenging. These include allergic fungal rhinosinusitis, central compartment atopic disease, nonallergic rhinitis with eosinophilia syndrome and aspirin-exacerbated respiratory disease.
Granulomatous conditions such as sarcoidosis and granulomatosis with polyangiitis also cause concomitant upper and lower airway pathology based on their underlying inflammatory mechanisms.
The cornerstone of management in unified airway conditions addresses the underlying inflammation through topical and systemic medication, exposure minimisation and optimisation of comorbidities. Surgery plays an important role in the upper airway.
Topical corticosteroids play a central role in unified airway disease, targeting the underlying inflammatory cascade. Asthma treatment is underpinned by longacting beta agonists and inhaled corticosteroids. Steroid nasal sprays and rinses/douches are used to deliver medication to the nasal cavity and sinuses respectively in all sinonasal diseases (usually in mometasone or fluticasone).
These second-generation intranasal corticosteroids are safe for longterm use without treatment breaks
as their systemic bioavailability is less than 1%. Patients are often concerned about long-term topical steroid side effects, particularly when using inhaled steroids for asthma as well, so taking time to allay these fears may pay long-term dividends.
Evidence suggests that only 20% of patients use their topical medication correctly. Adequate education and reinforcement of delivery technique and regular usage are essential.
Oral corticosteroids are commonly employed for acute flares of disease and when there is symptomatic progression despite optimised topical medication. They act in part by downregulating eosinophils and associated interleukins (IL-4, IL-5 etc).
Ideal dosage and duration are unclear and may range from five days to three weeks, but there is a growing body of evidence that they should be used with more caution and cumulative lifetime exposure of as little as one gram
increases the risk of adverse events, such as type 2 diabetes. When a patient is prescribed two or more courses of oral corticosteroids within 12 months, alternatives such as surgery or biologics should be strongly considered.
Biologics are a group of monoclonal antibody medications targeting part of the (type 2) inflammation seen in rhinitis, sinusitis with polyps and severe asthma. While four agents have been licensed for many years in Australia for use in severe asthma, only last year was one (Mepolizumab) TGA approved for use in chronic sinusitis with nasal polyps, significantly improving the treatment options for severe/refractory nasal polyps. Omalizumab has been shown to significantly improve nasal scores in allergic rhinitis when used to treat asthma, although no biologics are currently licensed for AR alone.
Nasal and sinus surgery are sometimes overlooked in management of the unified airway, despite being a vital part of the management of allergic rhinitis and chronic rhinosinusitis. They both
Heel pain is a frequent problem that presents to the general practitioner. Plantar fasciitis is the most common cause of under the heel pain. Most patients will improve with non-operative treatment but not all.
Surgery is a very effective form of treatment for this condition in patients with long standing refractory symptoms.
Before being considered for surgery patients should undergo at least six months of non-operative treatment that includes the following (in the appropriate order):
• Rest, avoidance of activity
• NSAIDs, stretching exercise program
• Orthotics: off the shelf or custom
• Cortisone injection (one only)
• Shockwave therapy

Surgery can be open or endoscopic. The principle part of the procedure is release of the plantar fascia near its origin on the heel. Historically only the medial half was released but recent literature supports more complete release.
reduce validated nasal symptom scores and improve quality of life scores. They act to enlarge the nasal airway, resulting in less obstruction and better topical delivery of medication.
Allergic rhinitis often benefits from turbinate reduction and CRS from endoscopic sinus surgery (ESS), both of which have been shown to improve asthma control.
In CRS patients without asthma, a study found that early ESS may decrease inflammatory burden and mitigate risk of developing asthma by a factor of 10. In CRS patients with comorbid asthma, ESS has been proven to improve clinical asthma outcomes measures (decreased asthma exacerbations, hospitalisations, and medication usage) and asthma control.
Author competing interests – nil

Open surgery is performed through a 3cm incision in the proximal arch and allows not just plantar fascia release but also decompression of the tarsal tunnel and Baxters nerve which is often implicated in heel pain.
Endoscopic plantar fascia release is indicated for those without nerve compression symptoms and is done through a much smaller incision using a camera assisted cutting device much like a carpal tunnel release.
Both open and endoscopic releases are performed as day cases and require approximately two weeks on crutches. Recovery is slightly quicker for endoscopic patients as you would expect. Patients can expect an 8090% chance of a good result from surgery. Complications are rare.


St John of God Medical Centre
Suite 10, 100 Murdoch Drive, Murdoch WA 6150 Telephone: (08) 6332 6300 Facsimile: (08) 6332 6301 www.murdochorthopaedic.com.au
By Associate Professor Tee Sin Lim, Radiation Oncologist
Prostate cancer is the most commonly diagnosed male malignancy, with over 25,500 cases estimated in Australia in 2023. Although frequently slowgrowing and often manageable with effective treatments, prostate cancer remains the leading cause of cancer-related disability worldwide.
This high incidence of disability primarily results from the adverse outcomes linked to both over- and under-treatment. The majority of prostate cancers are diagnosed with local disease and the management for cure can either be surgery or radiotherapy, sometimes in combination with androgen deprivation therapy (ADT).
Understanding ADT in prostate cancer treatment is important. Short-term ADT (4-6 months) has been shown to improve disease outcomes when added to radiation therapy for patients with intermediate risk localised prostate cancer.
However, ADT is associated with several risks, including weight gain, decreased bone mineral density, decreased insulin sensitivity, and a worsening lipid profile. These

complications can negatively impact patients' quality of life and can be a significant burden on healthcare systems.
Potential adverse effects of ADT include acute myocardial infarctions, fractures and the necessity for medications to manage glucose tolerance, blood pressure and cholesterol levels, as well as to mitigate ADT side effects such as hot flashes.
The challenge lies in identifying

the patient population that will benefit most from ADT treatment intensification when combined with radiotherapy.
The ArteraAI prostate test represents an advancement in the management of prostate cancer. Developed using a multi-modal AI (MMAI) deep learning architecture, this test leverages both clinical and imaging data. It comprises two AI models: a prognostic model that estimates the risk of distant metastasis and prostate cancerspecific mortality, and a hormone therapy benefit model that provides a binary result on the likelihood of benefit from short-term ADT after radiation.
The AI models were trained and validated using data from five phase III randomised controlled trials (NRG/RTOG 9202, 9408, 9413, 9910, and 0126), involving a total of 5654 patients and a dataset of 16,204 histopathology slides. The test uses clinical variables such as combined Gleason score, primary and secondary Gleason scores, clinical T-stage, baseline PSA, and age.
It employs two distinct machine learning pipelines: one for
Researchers will investigate whether anti-gout medication colchicine and/or non-enteric coated aspirin can lower the instances of cardiovascular events in people with type 2 diabetes who have no clinically evident cardiovascular disease (CVD).
The team, led by John Curtin Distinguished Professor Christopher Reid from the Curtin School of Population Health, will use a $2.84 million Medical Research Future Fund 2023 International Clinical Trial Collaborations grant to conduct a long-term trial,
COLCOT-T2D, to test the drugs’ effectiveness and safety. The trial is a collaboration with Dr Jean-Claude Tardif from the Montreal Heart Institute, Canada.
A large portion of the 1000 trial participants will come from regional and rural Australia, which Professor Reid said was important because people in these areas faced significant health challenges compared to city dwellers.
“The further a person lives from a metropolitan centre, the greater their risk of hospitalisation and death from CVD,” Professor
Reid said. “Despite this, there is evidence that CVD medications and interventions are prescribed less frequently in rural and remote areas compared with metropolitan areas.
“It’s clear patients in these regions would benefit significantly from a low cost, easily accessible treatment to lower the burden of disease.”
The study will explore the benefits of the powerful anti-inflammatory gout medication, colchicine for people with Type 2 diabetes.
Much prostate cancer disability is related to adverse treatment outcomes from over or under treatment
The ArteraAI prostate test represents an advancement in management of prostate cancer
The ASTuTE trial is recruiting in Australia-wide including WA.
pathological image analysis and another for the combined clinical and image data analysis. The AI systems independently generate MMAI scores for distant metastasis and prostate cancer-specific mortality.
The ArteraAI prostate test is endorsed by the National Comprehensive Cancer Network (NCCN) guidelines for prostate cancer. This biomarker test has the potential to change staging and prognostication in prostate cancer. Utilising this test could allow lowerrisk patients to be treated with radiotherapy alone, avoiding the toxicities associated with combined radiotherapy and ADT.
Conversely, it can also select patients who would benefit from treatment intensification, thereby improving outcomes related to distant metastasis and prostate cancer-specific mortality. This would suggest improvements in health and economic outcomes and help standardise management decisions among clinicians.
The ASTuTE clinical trial is a research study collecting de-identified health information, treatment recommendations and decisions to assess the clinical utility of the ArteraAI prostate test in managing short-course ADT for intermediaterisk prostate cancer. The study will enrol 800 participants across NSW, VIC, SA, QLD and WA.
The research will investigate how the ArteraAI prostate test affects doctors’ treatments recommendations, and what the outcomes for patients are five years after having the test.
To be eligible, patients must meet the following guidelines:
• Adult males over 18 years of age
• Intermediate-risk, localised
Prompt bookings with timely and successful outcomes, focusing on patient needs and care
Inguinal and femoral hernias
– laparoscopic and open
Ventral hernia
Rectus diastasis
Cholecystectomy
There were 32,000 groin hernia repairs performed in Australia in 2023
adenocarcinoma of the prostate according to NCCN risk stratification
• Absence of high-risk and very high-risk group features
• Presence of one or more intermediate-risk factors:
o Clinical stage cT2b-cT2c based on digital rectal exam
o Grade Group 2 or 3 (Gleason Score 7 {3+4} or 7 {4+3})
o PSA 10-20 ng/mL
The ArteraAI prostate test is a promising tool in the landscape of prostate cancer treatment. Its ability to refine patient stratification and optimise treatment plans could significantly improve patient outcomes and reduce the burden of ADT-related toxicities. As the ASTuTE trial progresses, it’s realworld utility and impact will become clearer.
– References available on request
Author competiting interests – nil
Laparoscopic approach preferred for most patients
– Results as good as for open surgery with a more comfortable recovery and faster return to physical activity
– Allows both sides to be repaired and easily extended to femoral hernia repair

Most ventral hernias are performed as day case procedures
Minimally invasive rectus diastasis repairs
No gap treatment for HBF patients, minimal out of pocket costs for other funds
Telehealth consultations offered
30-40% of men and about 5% of women develop inguinal hernia in their lifetime
With indirect inguinal and femoral hernias, there is a relatively high risk of occult contralateral hernia discovery, and the need for repair is on a case-by-case basis

55 Hampden Rd, Nedlands
Email: admin@westernsurgical.com.au
Phone: 6424 8596 HL: Cocperth westernsurgical.com.au




By Dr Scott Claxton, Respiratory Physician, Joondalup
Chronic breathlessness is a major symptom of lung and cardiac diseases and may also be a significant symptom in cancer and other non-cardiorespiratory chronic disease. In severe or latestage cardiac and respiratory disease, it is often a disabling symptom.
The experience of breathlessness can vary between patients even though they may have the same apparent severity of disease.
In the patient with severe or latestage lung disease (e.g. COPD or ILD) or heart failure, the severity of breathlessness can have a massive impact on quality of life. The approach and management of this symptom in these patients can be challenging. Usually by this point, disease-specific treatment has been maximised but the symptom of breathlessness remains or progresses.
A first step in the management is for the patient, and also the doctor, to acknowledge that this is going to be a persisting and likely progressive symptom. Understanding that, management will be to ease the symptom rather than resolve it, which allows everyone to focus on what is realistic. In this situation, management of severe breathlessness is about easing the symptom, improving quality of life and perhaps the patient’s level of function.
The feeling of dyspnoea arises from a complex interplay between the physiological requirement for ventilation and the cortical responses of the individual to the work of breathing. The breathing control centre in the medulla receives inputs from the airways, respiratory muscles, the lung parenchyma, the chest wall and the central and peripheral chemoreceptors. It then sends outputs to the respiratory system to drive ventilation.
Unique to the respiratory system is a corollary discharge from the medulla to the cortex giving a

Chronic breathlessness has many causes and is very disabling Management is focused on improving symptoms and not cure Exercise and pulmonary rehabilitation programs still offer value in even severe cases.
conscious component to this otherwise automatic response. This allows conscious control of breathing but also means there is a conscious sensation of breathing.
It is this cortical component that can lead to the feeling of dyspnoea and the emotional response that has an impact on the person. Severe dyspnoea in an otherwise well person who has undertaken a significant physical effort will have a different emotional overlay to a patient with severe lung disease who is breathless walking around their house.
The management of this aspect of breathlessness is starting to receive some attention from research groups and is already being looked at in the management of chronic pain.
The practical management of chronic breathlessness is challenging – it does not resolve it. The approach is more about easing the feeling and trying to improve quality of life. As mentioned, disease-specific management is important and has usually already been optimised. The management

of chronic breathlessness can be divided in to pharmacological and non-pharmacological strategies which can be applied regardless of the aetiology.
Low-dose opiates have been investigated the most in the management of breathlessness. The recent withdrawal from the Australian market of liquid morphine has caused some challenges. Low-dose sustainedrelease morphine (Kapanol 10mg) does provide some benefit by reducing the baseline level of breathlessness. Short-acting agents are useful either as pre-treatment before an activity (e.g. showering) and/or post-activity to manage symptoms. The risk of respiratory depression with this use is low. However, constipation is a common side effect.
Benzodiazepines, especially those with anxiolytic properties, have shown minimal benefit and may be more harmful due to sedation, but they may have a role in the patient with higher levels of anxiety driving breathlessness.
Even in the patient with very severe lung disease, exercise and pulmonary rehabilitation programs still offer value. The degree and duration of exercise may be limited, but maintaining physical condition helps with breathlessness management. Pursed-lipped breathing can help with exercise as well.
Improved lung emptying reduces the degree of dynamic hyperinflation. Recovering from exertion with a posture that supports the shoulders (e.g. tripod) can help ease breathlessness. This allows the accessory muscles of respiration to function more effectively.
Oxygen therapy can improve exercise capacity and reduced breathlessness in some patients. Often severe lung disease is associated with exertional hypoxia, but this is not necessarily the cause
By Dr Chloe Ayres, Gynaecological Oncologist, WAGCS*
Gestational trophoblastic disease (GTD) is an uncommon group of conditions associated with pregnancy and defined by abnormal trophoblastic proliferation. Arising from an abnormal placenta, it occurs in about 1:1000 pregnancies in Australia but wide variations exist in the reported incidence due to ethnic variations, issues with data capture and a lack of registries.
GTD typically presents in the first trimester with irregular vaginal bleeding and can be suspected on ultrasound but confirmation requires histopathological evaluation of the products of conception and ancillary testing. Most molar pregnancies resolve without treatment after uterine evacuation (D&C), but occasionally the disease persists and progresses into cancer requiring chemotherapy or further surgical intervention.
Histologically, there is a spectrum of disease from premalignant partial (PHM) and complete hydatiform moles (CHM) to malignant conditions of invasive mole, choriocarcinoma, placental site trophoblastic tumour (PSTT) and epithelioid trophoblastic tumour (ETT), collectively known as gestational trophoblastic neoplasia (GTN)
More recently the GTD spectrum has been expanded to include atypical placental site nodules (APSN) as 10-15% may coexist with or develop into PSTT/ETT.


Each have unique management depending on fertility wishes.
All cases are made complex by the need for intense monitoring with the hCG tumour assay, potential for malignancy and the occurrence of disease in young patients where future pregnancy is often desired.
In low risk GTN requiring single agent chemotherapy, overall survival approaches 100% and even in high risk GTN treated with multimodal chemotherapy and sometimes surgery for excision of resistant foci of disease and radiotherapy for brain metastases, survival rate is approximately 90%.
Rare diseases such as GTD should have centralised care through state or national-based registries and services. This allows for expert pathology review, clear
surveillance pathways, the removal of inconsistent treatment decisions and, most importantly, improved patient survival and patient reported outcomes.
The Western Australian Trophoblastic Centre (WATC) is a state-wide service established in January 2023 by Western Australian Gynaecologic Cancer Service and allows centralised and specialised care to both new and existing, public and private patients with trophoblastic disease.
There is a registry only option for clinicians who wish to continue to manage and follow-up their own patients but can re-refer if escalation of care is required. The service provides full medical, nursing, psychological care and support.
continued from Page 43
of the breathlessness. In some patients, the benefit may come from the sensation of airflow in the upper airway.
WAGCS Survivorship Team
A similar response can be elicited with a handheld fan. This can provide some relief to the feeling
of dyspnoea. In some preliminary work from a Japanese group, inhalation of menthol can induce a cooling sensation in the airways which can reduce some of the more unpleasant feelings associated with breathlessness.
Breathlessness in the patient with chronic severe disease is
a distressing and challenging symptom. Some strategies for management do exist, but there is a need for further work in this area.
Author competing interests – nil
Centralised care is crucial to the management of rare diseases such as GTD
Management of GTD by expert centres results in better patient survival and patent reported outcomes
Long-term psychological support and management of patient anxiety is critical.
The dedicated GTD nurse is pivotal to the service in the provision of support through diagnosis, monitoring, treatment and beyond. There is a weekly multidisciplinary case conference where all patients on hCG monitoring and chemotherapy are discussed, and once weekly afternoon multidisciplinary clinic.
Psychological support is an integral component of the service. These patients are not only coping with pregnancy loss and its associated grief, but anxiety around fear of recurrence and potential cancer, chemotherapy and loss of future fertility and not surprisingly often
require more psychological support in their subsequent pregnancy.
There is a specific second daily clinic for intramuscular methotrexate administration for low-risk GTN including on Saturdays. Logistically methotrexate works well as it avoids the fortnightly day admission for intravenous Actinomycin D with a medical oncologist but patients are given the choice of regimen given both are equally effective.
The WATC has been well supported nationally (QTC and Victorian HyMol) and internationally (Charring Cross and Sheffield) since inception by established trophoblastic centres.
So far, WATC has received approximately 200 new and existing referrals for patients aged 17-53 years (median 31 years). The histology of the referrals includes:
• 108 PHM of which two were ectopic in the fallopian tube or caesarean scar. Two had recurrent partial moles after hCG normalisation. Approximately 25% of partial moles were subsequently non-molar chromosomally abnormal miscarriages on FISH and could be discharged from WATC care
• 72 CHM (two with coexistent viable twin)
• Four APSN
• One new choriocarcinoma, five pre-existing
• One pre-existing ETT and one pre-existing PSTT 10% of referrals are for registry only and the remainder for WATC care.
Nine patients required a hysterectomy (6 CHM, 2 APSN, 1 GTN). All had completed childbearing; 14 patients developed low risk GTN (all complete moles) and required single agent chemotherapy for which approximately 30% had to change to Actinomycin D (consistent with known methotrexate resistance). Two patients required multi-agent EMACO chemotherapy for high risk GTN (one complete mole and one choriocarcinoma). The complete mole had a subsequent hysterectomy on completion of chemotherapy for persistent disease and is now in remission. The choriocarcinoma returned overseas for treatment. For further information contact watc@health.wa.gov.au
ED: *WA Gynaecologic Cancer Service
Author competing interests – nil

By A/Prof Davinder Hans, Psychiatrist, Nedlands
Approximately one in six individuals in Western countries use antidepressants. The increasing prevalence of antidepressant use does not align with the incidence rates of mood and anxiety disorders. This rise is primarily attributed to prolonged usage durations.
In the United States, the average duration of antidepressant use exceeds five years. Surveys conducted among long-term antidepressant users in the United Kingdom, the Netherlands and Australia reveal that 30-50% of these individuals may lack a clear evidence-based indication for continued use and might consider discontinuing treatment.
There is concern that one reason for the continued use of antidepressants is the difficulty individuals experience when attempting to discontinue them. These challenges, potentially linked to withdrawal symptoms, are often misdiagnosed as a relapse of the underlying condition.
Several reasons to consider deprescribing antidepressants include the lack of ongoing benefit from the medication, completion of the treatment course, uncertainty regarding the relapse prevention properties of antidepressants, patient preference, preference for alternative treatments and the impact of adverse effects, tolerability and quality of life.
After completing a treatment course and achieving symptom remission, patients with major depressive disorder typically continue antidepressants for an additional 4-9 months, as recommended by the APA and NICE. This duration varies with different illnesses. For instance, patients with PTSD or OCD require longer-term antidepressant therapy. Surveys indicate that approximately 50% of patients exceed the recommended duration of treatment.
There is uncertainty about the relapse prevention properties of
Key messages
Withdrawal symptoms often misdiagnosed as relapse hinder discontinuation
Many patients exceed recommended antidepressant treatment duration
Gradual tapering may reduce relapse and withdrawal symptoms.
antidepressants. Discontinuation studies, such as the ANTLER study (2021), struggle to differentiate between withdrawal symptoms and illness relapse. Gradual tapering of antidepressants over six months, instead of the conventional two months, has shown benefits, suggesting minimal to no excess relapse compared to continued use.
The notion that depression is directly linked to low serotonin levels, previously known as the monoamine hypothesis, lacks robust evidence. This outdated belief might cause patients to be reluctant to discontinue antidepressants even when they are no longer needed, despite increasing adverse effects.
Antidepressants can cause side effects such as drowsiness, restlessness, excessive sweating, dry mouth, gastrointestinal issues, weight gain, and emotional blunting. Emotional blunting is acknowledged as a dosedependent side effect but can also result from the underlying condition. Long-term use of antidepressants is increasingly associated with more significant weight gain than short-term clinical trials suggest.
Sexual side effects, including reduced desire, diminished sexual sensation, and difficulty achieving orgasm, affect 25% to 80% of patients. Post-SSRI sexual dysfunction (PSSD), recognised by the European Medicines Agency, indicates that these side effects can persist after discontinuing the medication in some patients.

The 2022 NICE guidelines on deprescribing recommend regular reviews for individuals taking antidepressants, focusing on the ongoing need for the medication, adverse effects, benefits and patient preferences. Addressing potentially erroneous beliefs about antidepressants, such as the misconception of a chemical imbalance or serotonin deficiency, is also crucial.
Patients often report that withdrawal symptoms from antidepressants are underrecognised or minimised by clinicians, likely due to official guidelines downplaying the frequency and severity of these symptoms. As a result, many patients seek help outside the medical system, including private online groups.
Clinicians should carefully consider withdrawal as an important differential diagnosis when antidepressant doses are reduced or missed, as withdrawal symptoms are frequently misdiagnosed as a relapse.
In summary, considerations for antidepressant deprescribing should begin with regular reviews of ongoing prescriptions at least every six months, particularly if adverse effects are present or the patient is pregnant or planning pregnancy. These reviews should include mood monitoring, sideeffect assessment, addressing perpetuating factors, and exploring patient preferences.
In the next part of this series, I will discuss specific clinical aspects of antidepressant withdrawal, including duration, severity, influencing factors, and management strategies.
Author competing interests – nil

For the second time, the Indian Ocean Craft Triennial brings craftspeople and their work from the ocean’s rim to Perth. Expect the gloriously unexpected and expand your definition of craft.
By Ara Jansen
While you might consider craft to be nice objects that you can look at or maybe even use, the Indian Ocean Craft Triennial proves there’s so much more going on.
From the traditional to found objects, rescued and recycled materials, the artists who make these works build on traditional skills and mediums and expand them into a modern context.
The second IOTA has been happening across a major international exhibition at six galleries, a conference and more than 70 exhibitions and events around WA. John Curtin Gallery, Fremantle Arts Centre, the Holmes à Court Gallery @ No 10, Bunbury Regional Art Gallery and Rockingham Arts Centre are all holding major exhibitions until the end of September or October. Added to that are exhibitions hosted all over the State across IOTA’s three months.
Carola Akindele-Obe and Jude van der Merwe are the event’s founders and co-curators. Both have a love for the work behind the craft made by these artists and artisans.

“It’s a mix of craft techniques and contemporary expression,” says Carola. “I love the way the makers are so ingenious, they are problem solvers and adapt and work with the materials they have or find to make objects for decoration and beauty, for self-expression or for shelter or use. Often, they are works of beauty but behind them there are tragic and difficult stories.”
A scarf made by Trish Little was finished earlier this year, not long before her death. The meme mat was a tactile response to a selfportrait. The black piece with the red word “me” intwined in it is completed and ends with a blank space. In contrast, India’s Ankon Mitra contributes a large installation of folded paper, as origami meets lines of code while local Emma Buswell documents and comments on women’s labour in large-scale knitted tapestries inspired by Greek mythology.
“Most, if not all, of this work is


hand-made by these artists and in some cases, it takes years of training and practice to perfect. In many cases this work is also a collegiate practice. Many of these artists work with artisan groups which provide an economic injection and direction, rather than giving inspiration to the work.”
The triennial’s theme, Codes in Parallel, speaks to how craft communicates on many levels and celebrates old and new stories. The events illustrate the innovative role that craft plays in practice and how craft is integral to community cohesion, environmental impact and socio-economic improvement.
“Because we are on the edge of the Indian Ocean and are of a colonised history, the craft heritage of the other countries is much more embedded in society and community. First Nations Australians have been crafting objects for daily life for millennia.
For all these groups aspects such as language, trade and even dye

colours have become enmeshed in craft and culture.
“Craft is a link to many other things. For many groups it’s a way to hand on stories and culture and hang onto a sense of identity. Many of the pieces are about reclaiming culture or making comments about sustainability, a circular economy, repurposing, over consumption and a conscious use of materials.”
Western Australia is well represented among artisans from India, Indonesia, Iran, Malaysia, First Nations Australians and Australians of the IOR diaspora.
All the work shares the commonality of a human need to use our hands, to experience a sense of the tactile and the need to connect. It also shares a resourcefulness and the energy of the mind-body connection.
For Carola, the cultural exchange aspect of the triennial is hugely important. The works provide an avenue for audiences to learn about the represented cultures and the stories embedded within. Secondly, the conference and gathering in Perth is the opportunity for the artists to meet others with different skills, to share knowledge and ways of working and is an important driver of inspiration and innovation.
ED: The Indian Ocean Craft Triennial 2024 (IOTA24) runs in WA until the end of October in a series of exhibitions, talks, demonstrations and interactive opportunities. For program details and artist information: https://indianoceancrafttriennial.com

A love for the coastal environment and the peace it brings continue to influence artist Trish Waters. You’ll get to peek inside her studio this month as part of the Margaret River Region Open Studios.
By Ara Jansen
Given her last name, it may come as no surprise that the beach and the ocean are special places for artist Trish Waters. An endless curiosity and love for patterns which come from both the sand and sea as well as natural elements feature prominently in her work.
A lifelong artist, Trish paints but also draws, creates ceramics, dyes silk, makes wire sculptures and rope baskets. You can probably put her diversity of skills down to being a secondary art teacher.
Based in Dunsborough, Trish is part of the Margaret River Region Open Studios which this year features 144 artists who you can meet in their creative spaces. As part of Australia’s largest open studio event, from September 7-22, there’s free access to the studios of artists and craftspeople of all types, whether it’s milliners and painters, glassmakers and potters.
Trish loves the colours and patterns of nature, which effortlessly find their way into her work. The ocean is solace, and she spends much of her free time by the sea, sailing on it, swimming in it and watching the light play on water.
Growing up across from the beach in Sorrento, she spent endless hours playing by the water. When she got her first set of Textas, Trish drew all over the walls of her house. They were soon replaced by bath crayons, and she continued her drawing. Art accompanied her from then on and Trish eventually became a high school art teacher. Even when she wasn’t always making her own art, she was helping inspire students with theirs and encouraging them to use it to help their mental health.
“I have a really wide variety of things I like to do,” says Trish. “Sometimes I find it hard to decide what to focus on, and what I’m exploring changes all the time.
“At the moment I’m exploring different ways to create movement in paint using repeated textures and contrasting colours. People say you can’t do something in terms of materials and then I just have to try it and find a way. There’s a curiosity and a bit of bloody-mindedness that makes me want to take on challenges.”
While studying teaching at Edith Cowan University three decades ago, she did a cultural exchange to study textiles in Indonesia. A love for South East Asia continues to this day, which has included recent trips to Singapore and Sri Lanka.
Every five years she takes a year off and goes travelling. What she sees, hears, feels, touches and tastes remain a big inspiration for her, whether it’s the famous galleries of Europe, making her way from Istanbul to London over six months or a posting to the Cocos Keeling Islands which taught her about winds and the patterns they make.
“Going to the beach is great for my mental health. A lot of my time in summer is spent at the beach, watching the water. I take a lot of photographs and obsess with how the ripples make the water look. My next challenge is to play with light through water. Just watching that blisses me out and I hope that people who see my art get that feeling from it.”
Meet all the artists and plan your studio visits, go to www.mrropenstudios.com.au
While you’re in the area, check out Bloom Festival from 21 September to 20 October and the Southern Art & Craft Trail from 21 September to 6 October.


The 2024 ST ALi Italian Film Festival returns to Perth from October 3 to 27, with the best new Italian movies and classic gems.
Screening at Palace Cinemas Raine Square, Luna Leederville, Luna on SX Fremantle and Windsor Cinema Nedlands, this year’s diverse program includes the playful comedy Marcello Mio, led by acting royalty and real-life mother-daughter duo Chiara Mastroianni and Catherine Deneuve.
Other highlights include the winner of the 2024 Sydney International Film Festival’s coveted Sydney Film Prize There’s Still Tomorrow, which follows a woman living in post-war Rome with her family who dares to break with tradition. It was the highest-grossing film in Italy last year.
Medical Forum readers have the chance to win one of five double passes, valid for any film screening at Palace Cinemas Raine Square (excluding special events).
To enter, use the QR code on this page or go to mforum.com.au and hit the competitions tab.

Suite 39, HOLLYWOOD
MEDICAL CENTRE, Nedlands
•Furnished, generously proportioned Consulting room available for specialists.
•Currently available Tuesdays and Wednesdays on sessional basis.
•Half day or full day, depending on requirements.
•On second floor of the exclusive Hollywood Medical Centre.
•Corner suite with exceptional views, reception, waiting area and kitchenette.
•Onsite on Hollywood Private Hospital, with Cafe and all other amenities
•Dedicated undercover car bay available for parking
•Easy patient parking in multi-storey car park
•Admin/Secretarial support requirements can be discussed
A unique opportunity to have a prestigious practice location long term!
For more details or to view, contact Amit on 0451824144 or Email Admin@dramitsaha.com.au


Medical & Consulting • Offices
56B Mornington Parkway, Ellenbrook, WA 6069
Price information
Lease: $25,000 excluding GST p.a.
Key property information
Floor area: 80 m2
Outgoings: $10,100 p.a.
Specialised Medical Unit
•Rare Medically Zoned Unit
•Previous Dental Use
•Available Immediately
Tilt Commercial is pleased to present this dedicated medical suite for lease in the rapidly expanding area of Ellenbrook. As one of only two units on site, this facility is not to be missed.
• 80 m2 medical unit
• Independent rear parking for staff
• Fit-out included if required
• Previously used for dentistry
• Adjoining orthodontist
• Part of the Mornington Medical strip
• Front parking and entry for clients
• Rear parking and entry for staff
• Available for immediate occupation
For further details, please contact Adam Yeo from Tilt Commercial, 0410 483 121

Treendale Medical Group
– GP Positions
•DPA Area’s and MMM5 Available
•FSP GP’s are welcome to apply
•Busy & well established
Medical Group with 4 Location in the South West of WA
•Full time & Part Time GP Positions in Treendale & Harvey
•Fully computerized and accredited modern practice with nursing and admin support
•Well supported with large team of experienced GP’s
•Situated in the beautiful South West Region surrounded by coast and forest and close to tourist areas in the south of WA
•Only 1 ½ hrs from Perth
•Family friendly working hours and no on call or hospital cover required
•65 – 70% of billings depending on experience
Please forward CV and enquiries to Kylie Wilson kyliew@harveymed.com.au
Contact Ross, classifieds@mforum.com.au or phone 9203 5222 to place your classified advert

Central City Medical Centre
Full time or Part-time VR GP
Private doctor-owned medical centre, providing excellent medical services to our patients for 35 years.
We offer:
•Excellent earning potential as a private billing Medical Centre
•Experienced administrationmanagement team
•Convenient proximity to the CBD
•Hourly retainer for the first few months while you settle in and build your own patient base
•Full-time doctors have exclusive use of their own room and part-time doctors would share with another part-time doctor.
Contact the Practice Manager, Claire Stocks, on 0422 511 906 or claires@ccmc.net.au

Earn 100% of Billings for the First 3 Months!
Join our well-established, accredited mixed-billing clinic in Burswood and earn 100% of billings for the first 3 months (75% thereafter).
Perfect for new VR GPs looking to establish themselves, with full-time/ part-time options.
Work alongside 3 experienced GPs in a fully computerized clinic with on-site pathology and RN support.
Please contact Dr Ang on 9472 9306 or Email: info@thewalkingp.com.au

for VR GP - F/time or P/time
Full Private List available now from retiring GPs
FRACGP essential
Up to 70% private billings
Unique opportunity to join our family orientated practice in one of Perth’s fastest-growing suburbs.
Enjoy working for a doctor-owned, non-corporate, well supported, and accredited practice.
Please contact the Practice Manager on 6165 2444 or email: reception@comogp.com.au








67 HA / 167 AC
LYNTONVALE is a rural lifestyle property located just 3km east of the Waroona townsite. Perched high on the Darling Scarp, it offers breathtaking panoramic views of the coastal plain and Peel Inlet. The landscape is undulating, and parkland cleared, featuring remnant stands of Marri, Wandoo, and Jarrah trees. A brook and a perennial creek run through the property, complemented by a substantial dam. The area is a haven for bird enthusiasts, with abundant white- and red-tailed forest cockatoos, magpies, robin red-breasts, and blue wrens. The property also includes a well-established orchard with citrus, olive, stone-fruit, and mulberry trees, all irrigated by water from the adjacent dam.
John Garland
M: 0418 923 347
E: johng@garlandintl.com.au www.garlandinternational.com.au
Nick Wallace
M: 0409 295 914
E: nick@bellcourtpg.com.au www.bellcourtproperty.com.au

Description: Sonic HealthPlus is Australia’s leading provider of occupational healthcare and general medical services. Backed by Sonic Healthcare, Sonic HealthPlus is a truly national company with wholly owned clinics operating in metropolitan, regional and remote locations across the country.
We have an extensive array of medical and allied health practitioners and specialists who understand the importance of protecting the health and wellbeing of families and workforce.
We currently have job opportunities at the following Sonic HealthPlus clinics.
SHP Mandurah - This beautiful city is known for its stunning beaches, scenic foreshores, estuaries, and rivers. With an array of cafes, bars, and restaurants, combined with its serene waterways and laidback atmosphere. SHP Mandurah offers a mix of occupational health and general practice. Candidates with 19AB restrictions are encouraged to apply.
SHP Hay Street Perth – Our Hay Street clinic is in the middle of Perth’s CBD with easy access to Perth’s finest shops, restaurants and bars. Hay Street offers general practice and travel medicine.
SHP Joondalup Drive Medical Centre - Located just a short drive from Perth, Joondalup offers a welcoming community, excellent schools, and a range of recreational activities. The centre offers general practice.
SHP Bunbury - Located just two hours south of Perth, Bunbury offers a perfect mix of vibrant city life and serene coastal living. The centre offers occupational medicine and does not provide any general practice service and will suit a non VR GP.
SHP Karratha - Situated in the heart of the Pilbara region, Karratha offers stunning landscapes, from red desert plains to lush bushland. Accommodation support is available. The centre offers general practice and occupational medicine.
With over 50 years’ experience in the industry, SHP is a Continuing Medical Education (CME) approved provider, giving our doctors and staff opportunities to broaden their knowledge and to advance regular training and development.
Benefits
High billing capacity
Private billing clinic services
A friendly and focused multi-disciplinary team
Support from operations, administration, property and IT teams
General Medicine
Men’s & Women’s health
Occupational health assessments
Acute injury treatment and management
Skin screening
Chronic Disease Management
Immunisations
Full Registration with AHPRA
Postgraduate training in general practice
Eligibility to access Medicare
A caring and quality driven commitment to providing general practitioner health services. FRACGP or ACCRM preferred. To Apply
Contact Sandy McNab – Business Development WA on 0419 917 010 or email Sandy.McNab@ipn.com.au for more information

We respect your time is precious. Humphrey Homes’ integrated model of architecture, building and interior design ensures you realise your vision with unrivalled efficiency, construction quality and budget control. To learn how our approach makes the process seamless and enjoyable, contact Dean Humphrey for an informal chat






