






Avant offers a range of products and services designed fordoctors:

• Medical indemnity
• Health insurance

• Life insurance advice
• Lending
• Legal advice
• Practice solutions
By your side
everbefore.
















Avant offers a range of products and services designed fordoctors:

• Medical indemnity
• Health insurance

• Life insurance advice
• Lending
• Legal advice
• Practice solutions
By your side
everbefore.








We live in a world that has changed and now accepts far more diversity than might have been anticipated in the setting of the early 2000s when surrogacy laws were first drawn up.
While the will of many seems to support change, it has been a long and frustrating road for West Australians waiting for a modern-day reboot of our surrogacy laws.
Despite several government-commissioned reviews and reports, it looks like the chance of having a family will not be found giftwrapped under the Christmas tree for some people.
As we approach the end the year, this month’s Fertility and Sexual Health edition explores the pressing need for contemporary surrogacy laws in WA that would allow gay people and single men to access the path to parenthood.
We live in a world that has changed and now accepts far more diversity than might have been anticipated in the setting of the early 2000s when surrogacy laws were first drawn up.
WA remains the only state or territory where surrogacy is illegal for gay couples and single men – with access limited to single women or opposite sex couples where the woman cannot conceive due to medical reasons.
A bill to widen eligibility made its way through State Parliament in 2019 but failed to proceed through the Upper House and is still languishing.
Even Health Minister Amber-Jade Sanderson concedes the current laws are discriminatory and out of step, while fertility clinics say their hands are tied and they have people who are desperate and running out of time.
Let’s hope the slow wheels of government get some traction in 2025.
Merry Christmas to all our readers, and we look forward to reconnecting after a safe and happy Christmas and New Year break.
SYNDICATION AND REPRODUCTION Contributors should be aware the publisher asserts the right to syndicate material appearing in Medical Forum on the mforum.com.au website. Contributors who wish to reproduce any material as it appears in Medical Forum must contact the publisher for copyright permission.
DISCLAIMER Medical Forum is published by Medforum Pty Ltd (Publisher) as an independent publication for health professionals in Western Australia. Neither the Publisher nor its personnel are medical practitioners, and do not give medical advice, treatment, cures or diagnoses. Nothing in Medical Forum is intended to be medical advice or a substitute for consulting a medical practitioner. You should seek immediate medical attention if you believe you may be suffering from a medical condition. The support of all advertisers, sponsors and contributors is welcome. To the maximum extent permitted by law, neither the Publisher nor any of its personnel will have any liability for the information or advice contained in Medical Forum. The statements or opinions expressed in the magazine reflect the views of the authors and do not represent the opinions, views or policies of Medical Forum or the Publisher. Readers should independently verify information or advice. Publication of an advertisement or clinical column does not imply endorsement by the Publisher or its contributors for the promoted product, service or treatment.
Advertisers are responsible for ensuring that advertisements comply with Commonwealth, State and Territory laws. It is the responsibility of the advertiser to ensure that advertisements comply with the Competition and Consumer Act 2010 (Cth) as amended. All advertisements are accepted for publication on the condition that the advertiser indemnifies the Publisher and its personnel against all actions, suits, claims, loss or damages resulting from anything published on behalf of the advertiser.
EDITORIAL POLICY This publication protects and maintains its editorial independence from all sponsors or advertisers. Medical Forum has no professional involvement with advertisers other than as publisher of promotional material. Medical Forum cannot and does not endorse any products.





Dr Michael Leung is the lucky winner of our October doctors dozen from Sandalford, and there is still time to enter our doctors dozen competition featuring wine from Marq, which was reviewed in our last edition.
This month, we have 12 double movies tickets courtesy of Sony Pictures to the drama The Room Next Door which opens in cinemas on Boxing Day.
There is also a special giveaway of five hampers from Mondo Nougat – read the story of this WA family-run business on page 52.
To enter use the QR code or go to www.mforum.com.au and hit the competitions tab.
PUBLISHERS
Alice Miles – Director Fonda Grapsas – Director Tony Jones – Director tonyj@mforum.com.au
EDITORIAL TEAM
Editor
Cathy O'Leary 08 9203 5222
editor@mforum.com.au
Production Editor
Jan Hallam 08 9203 5222 jan@mforum.com.au
Clinical Editor
Dr Joe Kosterich 0417 998 697 joe@mforum.com.au
Graphic Design Ryan Minchin ryan@mforum.com.au
ADVERTISING
Advertising & Classifieds Manager
Bryan Pettit 0439 866 336 bryan@mforum.com.au
Clinical Services Directory
Alice Miles 08 9203 5222 alice@mforum.com.au
CONTACT MEDICAL FORUM
Suite 3/8 Howlett Street, North Perth WA 6006
Phone: 08 9203 5222 Fax: 08 6154 6488
Email: info@mforum.com.au www.mforum.com.au















A complex five-year experiment which cracked the code of a genetic mystery has paved the way for faster and more accurate diagnoses of rare and unknown diseases affecting children.
Scientists at The Kids Research Institute Australia, together with the Undiagnosed Diseases Program and Perth Children’s Hospital, used medical expertise, laboratory tests and computational biology to uncover cellular characteristics which pinpointed the cause of an undiagnosed disease that has puzzled doctors since 10-year-old Northam girl Charlotte Patterson was born.
The researchers then scoured literature and data from around the world to find other patients with similar traits to match the findings to the condition, which they now believe affects less than 10 people globally.
The findings were delivered to Chalotte’s family by doctors from the Undiagnosed Disease Program at PCH.
The Kids’ Precision Health Program Head and computational biologist, Dr Timo Lassmann, said discovering the characteristics of the variant gene which caused Charlotte’s disease was like finding a needle in a haystack.
“Charlotte’s case was extremely complicated and challenging because of the unique characteristics of the variant,” Dr Lassmann said.
“Now, as a result of this work, we will be able to apply the process we used to other cases to diagnose unknown diseases more quickly.”
The WA-based Lions Hearing Clinics have moved into NSW, with four new hearing clinics opening.
Ear Science Institute Australia currently operates 16 Lions clinics in WA and is the only clinic network in Australia owned and operated by an ear and hearing medical research institute.
All proceeds from Lions Hearing Clinic solutions go to Ear Science to fund research into ear and hearing disorders.
A rural and remote general practitioner in WA is among the winners of one-off awards to mark the 40th anniversary of Medicare. Among the nine individual winners were five GPs, including Dr Lorraine

In her short life, Charlotte has been diagnosed with cerebral palsy, seizure disorder, a heart defect, intellectual disability and many physical abnormalities that until now, have been unexplained. She has had 64 surgeries, takes 16 different medications daily and requires a feeding tube.
After a complicated process of assessing the genetic variant in the laboratory, researchers discovered the variant was changing the basic machinery in cells responsible for the gene and protein expression and altering the way the neural cells were developing.
They created a model of Charlotte’s disease in the laboratory so they could not only determine what was causing her symptoms, but also investigate how they could modify cell pathways to improve outcomes for Charlotte.
UDP lead Dr Gareth Baynam said families with a child with an undiagnosed disease were forced to live in ‘limbo land’ where their world was filled with uncertainty.
“We can now unequivocally say that Charlotte is going to have a long life. She is not going to go backwards, there is a path forward.”
Anderson, the medical director at Kimberley Aboriginal Medical Services where she oversees eight primary health clinics.
Dr Anderson was the first Aboriginal person to be appointed to a national health technology advisory committee and has been recognised for her leadership in delivering healthcare to Indigenous communities.
Nine people and 11 primary healthcare teams were named “champions” of the national patient insurance system.
Perth’s Homeless Healthcare Medical Respite Centre was recognised as a first-of-its-kind service that gives people experiencing homelessness somewhere to recover after leaving hospital and assistance in managing planned medical procedures.
The multidisciplinary team consists of GPs, nurses, nurse practitioners
and other social services, and provides everything from wound management to alcohol and other drug detox.
Pramana Medical Centre in Gosnells was awarded for its wraparound care, which includes weekly home visit clinics. The team of nurses, GPs and social workers provide culturally sensitive and trauma-informed care to patients from vulnerable communities who may not have engaged with health services for some time.
A Perth GP and researcher has cautioned against suggestions that intrauterine devices (IUDs) cause breast cancer, saying a recent study only showed an association.
Low coverage of prevention, testing, and treatment services for STIs during the pandemic has fuelled a resurgence of these infections globally. Over 1 million new sexually transmitted infections are acquired worldwide every day, with the majority being asymptomatic. This surge in cases highlights the ongoing importance of stringent measures in the prevention, testing, and treatment of STIs.
The three years from 2020 to 2022 saw a drop in STI notifications in Australia compared to 2019, reflecting the impact of the pandemic (see Table 1). However, in 2023, there was a resurgence of STIs, with notifications significantly higher than in 2019, especially for syphilis < 2 years duration (an 9% increase), gonococcal infection (a 16% increase), and congenital syphilis (a 400% increase; 4 each in VIC, WA, and NSW, and 5 in QLD).
Chlamydia
This is the most commonly reported communicable disease in Australia and those under age 30 are most at risk.
Symptoms: 85-90% of individuals have no symptoms. If present, symptoms may include dysuria, penile urethral and vaginal discharge, testicular and pelvic pain, intermenstrual and postcoital bleeding, pain during sex, and anorectal symptoms.
Testing recommendations: Urethral swabs, first-pass urine (FPU), and vaginal/endocervical swabs. Note: Vaginal/endocervical swabs are more sensitive than FPU samples in female patients. Additionally, an anorectal swab for patients with anorectal symptoms and all MSM, along with pharyngeal swab for MSM. Due to the risk of coinfections, STI guidelines recommend that gonorrhoea testing should accompany chlamydia testing. Testing for re-infection is recommended at three
By Dr Sudha Pottumarthy-Boddu MBBS FRCPA D(ABMM)

Dr Sudha Pottumarthy-Boddu has a distinguished career in microbiology with extensive experience in the US New Zealand and Australia. Sudha is a Diplomate of the American Board of Medical Microbiology, and a member of both the Antimicrobial Stewardship Committees and Infection Prevention and Control Committees at multiple St John of God hospitals in WA.
months. Consider testing for other STIs if not undertaken at first presentation.
Gonorrhoea
The bacterium Neisseria gonorrhoeae causes a disease spectrum similar to that of chlamydia.
Symptoms: Up to 70% of women with genital gonococcal infection are asymptomatic, while approximately 80% of men present with mostly mild symptoms. Symptoms may include dysuria, penile urethral and vaginal discharge, conjunctivitis (purulent, sight-threatening), and dyspareunia with cervicitis. Anorectal symptoms may include discharge, irritation, painful defecation, disturbed bowel function.
Testing recommendations: Urethral swabs, first-pass urine (FPU), and vaginal/endocervical swabs. Note: Vaginal/endocervical swabs are more sensitive than FPU samples in female patients. Additionally, for MSM, collect anorectal and pharyngeal swabs, even if patient is asymptomatic at these sites. Collect an additional penile urethral swab for culture if discharge is present or before antibiotics. If patient has symptoms, collect a clinician-collected endocervical swab. Swabs should be collected for culture to enable resistance testing prior to treatment Due to the risk of co-infections, STI guidelines recommend that chlamydia testing should accompany gonorrhoea
testing. Test of cure should be performed two weeks after completion of treatment. As re-infection is common, it is recommended that patients are tested again at three months.
Syphilis
In 2023, there was a 9% increase in cases of Syphilis < 2 years of duration in Australia. This increase is of concern, as a baby can contract congenital syphilis through transplacental transmission. The transmission rate is highest (60-90%) during untreated primary and secondary syphilis.
Symptoms: Often called the ‘Great Imitator’, syphilis can mimic many other conditions. Consider syphilis testing in all patients with unexplained symptoms.
Primary syphilis (on average three weeks post-infection): The presence of one or multiple genital, anal, or oral ulcers that occur at the site of entry.
Secondary syphilis (> six weeks postinfection): May include fever, malaise, headache, lymphadenopathy.
Look for a generalised rash involving the trunk. However, it may just affect the palms and soles. A skin rash occurs in over 90% of cases.
Testing recommendations: Syphilis should be excluded in all sexually active patients presenting with a rash. If the patient presents with a genital lesion, a swab for syphilis PCR as well as serology is recommended. If there is a clinical suspicion of primary syphilis but serology is negative, ensure a PCR swab has been completed and repeat serology after two weeks following presumptive treatment. Repeat testing at three, six and 12 months (if necessary) post-treatment.
Testing during pregnancy: Offer routine syphilis testing at the first antenatal visit. Recommend follow-up testing at 28–32 weeks, dependent on local guidelines.
Infectious disease clinicians
Professor Chris Blyth and Professor Asha Bowen are new fellows of the Australian Academy of Health and Medical Sciences. They work at The Kids Research Institute Australia and Perth Children’s Hospital.
Edith Cowan University’s Professor of Exercise Medicine
Professor Rob Newton was also among the 31 new fellows to the academy.
Roberts Co and Webuild have been named as preferred contractors for WA’s new $1.8 billion Women and Babies Hospital to be built at the Fiona Stanley Hospital precinct.
Paediatric anaesthetist

Professor Britta Regli-von UngernSternberg and antibiotic resistance researcher and microbiologist Dr Kieran Mulroney were WA finalists in the 2025 Australian of the Year Awards.
Professors Fiona Wood, Asha Bowen and Britta Regli-von Ungern-Sternberg are on the State Government’s new expert committee to guide medical research.

Researcher Professor Bridianne O’Dea is leading a project to help Australian GPs better support their teenage patients facing long wait times for mental health treatment using smartphone apps and automated SMS chats.
Perkins Institute researchers
Associate Professor Elena De-Juan-Pardo and Associate Professor Abdul Rahman Ihdayhid won the Wesfarmers Wellbeing Platinum Award at the WA Innovators of the Year Awards for their 3D printed replacement heart valve.
continued from Page 4
Writing in The Conversation, Dr Brett Montgomery said a recent study had found a link between IUDs and breast cancer, and while the research was important, media reports of a large increase in risk may be causing unnecessary worry.
The study by Danish researchers used data from national health registries to look for links between hormonal IUD use and breast cancer.
They tracked nearly 80,000 people who started hormonal IUDs across two decades. They compared these people to an equal number of people born at the same time who did not use hormonal IUDs.
Dr Montgomery said after the researchers adjusted their results to account for many differences between the two groups (including education, age, number of children, and some other medicines and medical conditions), the numbers pointed towards a higher risk of breast cancer among people who used a hormonal IUD.
“However, there are many other important risk factors for breast cancer the authors seem not to have adjusted for, such as body weight, alcohol use, smoking and physical activity,” he said.
“If there were differences between the two groups in these things, then the study’s results may still be biased. This makes me quite uncertain about the results.
“Ultimately, we can’t say the IUDs caused the breast cancer – just that there’s an association or link.”
The Esus Centre – the first eating disorder day hospital of its kind in Australia – has just marked its first year of operation in Subiaco.
Esus is the first integrated eating disorder day hospital in the country with high and low intensity programs delivered by a multidisciplinary team under one roof.
continued on Page 8
Home care should be more of a priority in the health care model, according to the nation’s leading demographer and social commentator Bernard Salt
Speaking at the inaugural Silverchain Symposium held in Perth last month, Mr Salt said Australia needed to prioritise care at home as part of its overall health care model to deal with the country’s shifting demographics.
He said the focus on “bricks and mortar” hospitals was a 19th century health care model that was not fit-forpurpose for the shifting demographics that would be heavily impacted by the ageing baby boomer generation.

“The baby boomer freight train is heading straight for us, and we will have to deal with an issue at a scale that humanity has never had to deal with previously – so many people in a stage of the life cycle where they need so much care,” Mr Salt said.
“We have to reorganise society in such a way that we can care for the needs of an older population. The two options we have would be ratchet up taxes to a stratospheric level or we can find innovative solutions, and providing care at home is one way to do that.
“The baby boomers are a generation that is not just going to sit around and wait to die. They will want to remain mobile and active, and they will want to contribute to society.
“They will make it clear how their care should be delivered, and the vast majority will want in-home care, and as a consequence, we will see the care sector redefined, re-imagined and repurposed by this generation.”
Mr Salt said that based on Australian Bureau of Statistics, the population of people aged 85 and over will grow to more than 2 million by 2071, with the year-on-year net growth peaking at 62,000 by 2032 as the baby boomer generation ages.



Part of its approach is its own homestyle kitchen in which patients have their meals cooked for them and where their families join them for dinner once a week.
Understanding how technology can be used to better deliver accessible healthcare to remote Indigenous communities across WA is the focus of new research between WA Country Health Service, the University of Sydney and the Digital Health Cooperative Research Centre.
Following a successful pilot of providing virtual emergency services in a community with about 700-800 residents, that community has now been accessing the services for over three years.
With the support of Aboriginal Medical Services, more communities are seeking access to these virtual emergency services.
WACHS represents one of the largest areas serving over 500,000 residents, 11% of whom identify as Aboriginal.
WACHS Executive Director Strategy and Change Melissa Vernon said virtual care could help address critical unmet health needs, reducing the burden of travel and improving healthcare equity for Aboriginal populations.
“It is also important that we understand the cost benefits of providing these services to ensure we are providing valuable and sustainable services.”
The project will see the University of Sydney undertake research to understand the economic costs, and service access benefits, of embedding the service into additional regional communities.
Researchers from Edith Cowan University have called for greater recognition of the needs of neurodivergent mothers during perinatal care.
For neurodivergent women, the inherent changes associated with this period, such as shifts in daily routines, poor sleep, hormonal fluctuations, sensory sensitivities and social communication difficulties, can exacerbate their vulnerability to mental health issues.
These challenges can lead to increased rates of antenatal and postnatal depression, anxiety and isolation, impacting their transition to parenthood.
ECU PhD student Jata Elliott said a 2023 study found that compared to neurotypical mothers, neurodivergent mothers are frequently diagnosed with postnatal depression, and ADHD increases the risk of depression and anxiety in the perinatal period.
“Research has also found that autistic individuals were significantly more likely to experience depressive episodes in pregnancy and postpartum compared to their nonautistic counterparts,” she said.
“This suggests a critical need for perinatal care systems to adapt and respond to these elevated risks.”
My open letter to the Minister for Health Mark Butler
Sadly, your recent comments in the media only magnify the perceptions among my graduating students that general practice is not for them.
The figure of an 11,000 shortage of GPs by 2030 is clearly an underestimate as we boomers retire and 1000 new GPs are required for every 100,000 new immigrants, despite the five new medical schools in mainland capitals graduating over 600 new doctors.
The gap fee of $50 is clearly having a huge impact, with over 50% of people saying they have delayed or avoided visiting a GP because of cost. I acknowledge bulk billing for pensioners and children under 16 and after hour GP clinics has helped, but the public just hears GPs are getting a bonus for bulk billing, yet I am charged $50.
The solution is elegant, simple, better for patients, better for GPs and cost neutral for the government – halve the time for a long consultation to 10-20 minutes and double the rebate.
Please don’t believe those that run corporate practices who are demanding you boost the bonus for bulk billing so they can see more patients in six minutes. This is the worst outcome for productivity and turns GPs into wage slaves for the corporates. No wonder we are leaving in droves to do other things like skin clinics.
Dr Colin Hughes
Former Chair RACGP WA and tutor at Curtin Medical School, Midland
Growth in community services, a rise in patient numbers and progress towards environmental targets have been listed as highlights for the year at St John of God Health Care.
In releasing its 2024 annual report, Group CEO Bryan Pyne acknowledged the difficulties facing the Australian private health care sector while anticipating a positive future.
“We’ve been navigating a challenging landscape of regulatory shifts, rising costs and fluctuating patient demand for several years but we are resolute in our commitment to deliver outstanding care and clinical excellence,” Mr Pyne said.

“We are pleased to have generated more than $2 billion in revenue, which reflects our resilience and reinforces our path toward sustainable success, but our margins remain challenging.
“We are responding to pressures on health care funding by leaning into change and aligning resources to streamline service delivery across the organisation.”
Mr Pyne said environmental sustainability remained a key focus for the group, with a target of net zero greenhouse gas emissions by 2050 and a minimum 50% cut by 2030.
WA has lost one of its most respected and 'generous of heart' cardiologists, Professor Peter Thompson.
He passed away at home surrounded by family on October 25, two months shy of his 83rd birthday as a result of complications from metastatic melanoma.
Prof Thompson was active in his research right up until his last illness, publishing work in October on the use of colchicine for secondary prevention of ischaemic stroke and atherosclerotic events.
He was most recently consultant cardiologist and head of the Heart Research Institute at Sir Charles Gairdner Hospital, and Clinical Professor of Medicine at UWA.
He also served as Laboratory Head of Cardiology Clinical Trials at the Harry Perkins Institute of Medical Research and was its deputy director until 2023.
Prof Thompson is survived by his wife of 57 years Jane, children James, Alexandrea and Angus and eight grandchildren.
Associate Professor Angus Thompson, also a cardiologist and based in Queensland, recalls that although his father was always busy, his first rule of politics was “be there.”
“He would tell me that you can’t change anything unless you are there to influence the decision- making,” he said. “Faxes followed by email made sharing of written information quicker, teleconferences reduced travel somewhat, and his pager soon gave way to the omniscient mobile phone.
“COVID introduced the ubiquitous video calls which continued to facilitate his research in the last four years, but the in-person touch never ended.”
Prof Thompson also adopted a second career as a winemaker, which led to the establishment of the successful Thompson Estate.
Perkins CEO Professor Peter Leedman said Prof Thompson would be remembered as a remarkable man.
“He was a pioneering cardiologist, brilliant researcher, passionate mentor and true friend to the Perkins, and he achieved so many things throughout his life,” Prof Leeman said.
“From establishing himself as one of Australia’s leading cardiologists to mentoring hundreds of clinicians and researchers to pioneering wine making in Margaret River, Peter embraced life, leadership and learning.
“Peter was a teacher, doctor, researcher and advocate. He was also a great friend to many including me. I feel truly privileged to have worked alongside him. I learnt so much from him.”
Prof Thompson graduated from medicine and did his postgraduate degree in medicine at UWA before training in cardiology at Royal Melbourne Hospital and the Brigham and Women’s Hospital and Harvard University in Boston.

In addition to his leadership roles at SCGH and UWA, Prof Thompson held roles including President of the Cardiac Society of Australia and New Zealand, Deputy President of Asian Pacific Society of Cardiology, President of the Australian Medical Association WA, chair of the Heart Attack Committee and Board Member of the National Heart Foundation, and Asian Region Editor for European Heart Journal
Prof Thompson had extensive experience in the training and mentoring of young cardiologists and clinical researchers. He sat on the editorial board of four cardiology journals and published extensively in peer-reviewed journals and authored over 270 research articles, reviews, book chapters and editorials.
Director-General of Health Dr Shirley Bowen said Prof Thompson was “a superb physician, a scholar and a gentleman in all his pursuits.”
“Dedicated to improving the lives of his patients, Prof Thompson has received numerous awards and accolades but was never one to look for praise,” she said.
Prof Thompson was appointed a Member of the Order of Australia in the Queen’s Birthday 1998 Honours List for services to medicine, particularly in the field of cardiology and coronary care.
ED: I have known Peter for decades and he helped me when I was a young ‘green’ health reporter trying to get my head around the intricacies of cardiovascular disease. He gave his time freely, wanting to help to better educate people about heart risks and prevention to save lives – and he did.

In an Australian-first, WA’s health system is offering inpatient and outpatient services for people suffering from gaming disorders or excessive digital use.
By Cathy O’Leary
It is an issue that doctors might inadvertently be dealing with on a regular basis with younger patients – teens who are anxious, depressed, not sleeping well and missing school.
Drill down to how they are spending their time, and the answer might be that they are sitting at home playing games or scrolling social media –morning, noon and night.
Gaming disorder and excessive internet use might not have been on the medical school curriculum for many doctors, but it is a fast-growing social phenomenon being fuelled by the omnipresent digital world.
While there are some global estimates of 3-4% of people suffering from gaming disorders, and rates of one in 10 people with excessive screen use, the figures are thought to be higher, with the problem sometimes camouflaged by other symptoms and co-morbidities.
But a team of clinicians in Perth is spearheading a new intervention and treatment approach – thought to be an Australian first, if not the world – by offering both an outpatient clinic as well as inpatient treatment.
Funded under the South Metropolitan Health Service, Fiona Stanley Hospital is the first public hospital to have a gaming disorder clinic, and from this month, GPs can also refer female patients aged 18 and over to five designated inpatient beds at Cockburn Health.
Cockburn will provide in-patient admissions for patients from both metropolitan and rural areas who need digital detox and other in-patient treatments. For males and female aged 16-18, in-patient admissions will be provided by the youth in-patient unit at FSH.
The gaming disorder clinic has been operating since 2022 as part of the FSH’s Addiction Prevention and Treatment Service.
Clinicians recognised the need for a specialist gaming disorder clinic during the COVID-19 pandemic when they saw a steep rise in gaming disorder and related
problems in adolescents and young adults presenting to the emergency department and the youth and adult mental health and medical wards.
When the clinic was piloted in 2021, it was believed to be the first in the world, as other international centres tended to have clinics as outpatient or detox camps rather than one within an acute hospital setting.

doctors were unaware of the service, but since then, it has treated more than 200 patients, almost threequarters of them male, with the majority aged 15 to 19, while some patients have been as young as seven while others are aged in their 50s.
Many have co-morbidities such as ADHD, autism, depression, anxiety and substance use issues.
Few patients were initially referred to the clinic by GPs because most

Demographics of 200-plus patients at FSH
Gender
• Three-quarters male –153 males, 50 females.
Age:
• Almost half aged 15-19 years
• A quarter aged 10-14 years
• Two children aged 5-9 years
• Eldest patient aged 59
Primary diagnosis in order of prevalence:
• Hazardous gaming
• Gaming disorder
• Hazardous internet use
• Hazardous social media use
Employment/education status:
• Half students
• 33% unemployed
• 18% employed
Co-morbidities in order of prevalence:
• ADHD
• Depression
• Anxiety disorder
• Autism spectrum disorder
• PTSD
• Others – bipolar, substance abuse, personality disorder, gender dysphoria, eating disorder.
School attendance among school-aged:
• 45% good attendance
• 29% non-attendance
• 26% limited attendance.
The clinic has been spearheaded by consultant psychiatrist and head of service Dr Daniela Vecchio, who is working to raise public awareness about gaming disorders, promote prevention and early intervention, and develop solutions.
She told Medical Forum it was not about being ‘anti-gaming’ but for some people this form of entertainment could turn into a harmful addiction.
“In Australia, the data shows that in school-aged children there is a prevalence of 2.8%, and in terms of problematic screen use it’s over 10%, particularly in teenagers, and we also think it’s the tip of iceberg and likely to be higher,” she said.
“The phenomenon is very much under recognised, and people present to the emergency department due to schizophrenia, depression or attempted suicide.
Dr Vecchio said many people could play games without it causing any problems but in others it was a persistent pattern of gaming despite negative consequences and involved loss of control and making it a priority over other activities.
“It’s where it’s causing impairment in their functions. In the clinic, we see very severe cases where patients become very reclusive, they don’t go to work or attend school, and they might act in an aggressive way when limits are placed on their gaming use.
“They’re often anxious, depressed and irritable, and their lifestyle is compromised, and they might have obesity and musculoskeletal problems.
continued from Page 11
“We had one patient who developed severe pressure ulcers, the bone could be seen, because of prolonged sitting while playing games.”
Dr Vecchio said that before the clinic opened, there were few resources to treat these disorders.
While progress had been made, the next step was to educate professionals in the health and school sectors, and to develop screening and prevention, but both required funding.
“We are the only outpatient clinic of its kind in Australia, so it is important that we have community-based services who can do screening in schools or do interventions in home because we have the phenomenon of school refusal,” she said.
Data showed that among a schoolaged cohort, only 45% attended school, and of those of working age, the majority did not work.
“This is very concerning, and shows we need to act early, but we also need to promote healthy gaming because we also don’t want to demonise gaming because it can be fun, and people can connect with each other,” Dr Vecchio said.
“The problem is that some individuals are vulnerable to develop gaming disorder addiction, and the games are designed to keep the user engaged, and others encourage online gambling so people can end up spending thousands of dollars which then makes them depressed.
“We’ve had patients who have attempted suicide in the context of this depression and loss of control, and like other addictions, there can be physical damage, such as to the prefrontal cortex, so their ability to plan and to regulate their emotions is affected.”
She said often gaming disorders did not happen in isolation, with the majority of FSH’s patients having ADHD, depression or social anxiety, so it was important in terms of interventions to treat the comorbidities and work with families.
Patients were encouraged to have a


digital detox, which could be done at home or in more severe cases carried out on the youth ward.
“We usually start by encouraging them not to have devices in their room at night, to give it to their families, and perhaps switch off the wifi,” Dr Vecchio said.
“We encourage them to have other activities, because the worst enemy for them is the boredom, so they need to replace gaming with social activities – or social prescribing – so family activities like cooking a meal together without devices around, and not just for the individual but for the whole family.
“There isn’t medication for this
disorder, so you need to make changes to the system.”
Dr Vecchio said the clinic staff were particularly concerned about school refusal in these children, because if they did not get an education that could affect their whole life, their work and relationships.
“We try to facilitate a return to school, and we work with the school – such as the principal and school psychologist,” she said. A learning centre at FSH could give students tutoring one-on-one before they started the return to school.
The hospital also offered a self-help group, facilitated by a doctor and a peer support worker, where they could come once a week to talk about their week and engage in fun activities such as playing board games using fantasy and strategies similar to those used in online gaming.
Dr Vecchio told Medical Forum the clinic was funded solely through the hospital but to be sustainable it needed to secure long-term funding.
“The demand is now very high, and the patient cases referred to us are often very complex, and while the trial has been successful, to treat the disorder you have to address many things like education, and that can be complicated,” she said.
“Children with conditions like ADHD are more vulnerable to the harms from gaming disorders and have to be assessed on a case-by-case basis.
“But we need to be doing more for prevention and early intervention such as screening before children become severely affected.
“For some, gaming is an escape from reality, and of course we’re in a digital world and nobody wants people to stop engaging in healthy activity, but not when it gets to the stage where they don’t sleep at night because they’re playing video games, or they stop looking after themselves – they don’t eat or shower – and they might become obese.
“There have been cases of children assaulting family members, and there is also a risk of radicalisation online – Australia has seen a few cases of this.”
Some people with gaming disorders also gambled, and this compounded their financial woes.
“In some cases, detox has to be done in a safer, more supported environment than home, and that’s
where we’re looking to use our five inpatient beds for gaming disorder at Cockburn Health – there has never been anything like this before,” she said.
“We believe this could be the first unit of its kind in the world – and it’s not just for gaming disorders, it might be excessive social media use. These cases will be a detox, but in a very supported way, treating any co-morbidities.”
The service also liaises with clinics in other countries such as Korea and Japan, where gaming disorder is very prevalent, and this was helping to further global research into gaming disorder.
Dr Vecchio said that as well as the need for funding and policies, other options that could be considered to combat the adverse effects from gaming included advertisements –supported by the multimillion-dollar gaming industry – warning on the harms or having taxes on games.
GP referrals welcome
In the meantime, she encouraged GPs to refer patients for outpatient treatment as well as inpatient care if needed.
The clinic is accepting referrals for patients with gaming disorder, hazardous gaming, problematic internet use, social media use disorder and allied conditions for assessment.
The criteria included patients who game excessively and experience functional impairments; are aged over 16 (although lower ages can be considered on a case-by-case basis); are not currently suicidal; and are being case-managed by a service or have already been referred and accepted.
Since October 14, the service has accepted referrals for females aged 18 and over for admission to Cockburn Health, with the beds due to open on December 2.
Referrals can be emailed to fsh.gamingdisorderclinic@ health.wa.gov.au



Proposed changes to WA’s onerous surrogacy laws could finally be passed in 2025, a long-overdue option for thousands of people seeking to have a family.
By Suzanne Harrison
Pushing a pram into a suburban café on a Saturday afternoon, Jamie* is like any other doting new father – exhausted and yet over the moon to finally be able to hold his own baby.
But Jamie’s journey to fatherhood has been a little different from most. For the past decade or so, the now 42-year-old had been hoping to have a child, but as a single gay man, the video producer discovered a few years ago that he would not be able to legally access domestic surrogacy in Western Australia, even if it was of an altruistic nature.
In fact, commercial surrogacy – where the surrogate is compensated for more than their expenses, with no other payment provided or personal profit made – is punishable by law throughout Australia.
In WA, it is permitted altruistically only for cis gendered couples or single women where the woman is unable to conceive due to medical reasons. In New South Wales, Queensland, South Australia, Tasmania, and Victoria, altruistic surrogacy is legal for same sex couples.
The Federal Government also says that if Australians engage in commercial surrogacy, they are usually not recognised as legal parents in Australia and the surrogate remains the legal parent of the child.
The concern is that in some countries, commercial surrogacy can lead to risks of exploitation of surrogates, babies and commissioning parents. In the US, where commercial surrogacy is legal and a common location for Australians to access, the cost is prohibitively high for many people.
While in 2020, the Medicare Benefits Review Taskforce recommended removing the restrictions, Medicare is still not accessible for surrogacy.
People like Jamie are not deterred. He did everything in his power to realise his dream of having a baby without breaking the law or dealing with disreputable agencies. The process was agonising, but with the right advice, he made it work.

report was published as part of this review and as a result a Ministerial Expert Panel was convened in May 2022 to ensure new legislation reflected social trends and medical and scientific advances for the accessible and safe use of ART and surrogacy.

And he argues that if someone wants to have a baby, they will find a way.
According to a report from Monash University, 213 Australian babies were born through international surrogacy in the financial year from 2021-2022, a reality the WA government has acknowledged via a review that is soon expected to lead to a relaxation of WA’s laws.
In a recent statement from the WA Health Department, it said the government was committed to supporting more people to start a family or expand their family with help from assisted reproductive technology (ART) and surrogacy “that is safe and ethically sound for all”.
Associate Professor Sonia Allan completed an independent review in 2019 (the Allan Review) into the existing state laws. A two-part
It was chaired by Perthbased independent fertility expert Professor Roger Hart , and its work was completed two years ago – in December 2022 –and its final report with recommendations was provided to WA Health Minister Amber-Jade Sanderson.
Its review of the state's surrogacy and human reproductive technology laws found them to be outdated and discriminatory.
Ms Sanderson has said the State Government was committed to supporting people who wanted to start or grow their family with assisted reproductive technology laws that were inclusive and safe.
She told the ABC the Government was “absolutely committed to this legislation” and would “introduce a Bill as soon as possible”.
However, with few sitting days left this year, a Bill to Parliament slated for the end of 2024 is now reported to be unlikely.
For Professor Hart, who is National Medical Director of City Fertility, the changes cannot come soon enough. The pathway to surrogacy needs to be streamlined, he says, and the WA laws are “onerous”.
“Certainly, the inequity of a single man, or a homosexual male couple, being unable to access surrogacy needs to be addressed,” Professor Hart said.
The process needs to be less burdensome, while ensuring the health and the rights of the child born from the arrangement are paramount. Support for those seeking surrogacy is a major step, he adds, as is access to Medicare.
“Other than a male couple seeking surrogacy, most others seeking a surrogacy arrangement will have had a very distressing and often painful journey to reach the point that they need surrogacy to realise their desire for a family,” he said.
For example, a surrogate would be required for any woman who was born without a uterus or undergone a hysterectomy due to cancer or obstetric haemorrhage, or had undergone multiple rounds of unsuccessful IVF treatment, or had a medical condition which would make carrying a pregnancy life threatening for her or her baby.
“We need to recognise that fact and try to ensure the process is supportive of those involved in an arrangement that has been less complicated to negotiate, while ensuring that due process is followed.”
Professor Hart believes that individuals and couples seeking surrogacy should be able to access Medicare, which to date, “unfortunately, they are excluded from.”
For intended parents, there is an increasing flow of information amid the groundswell of support for both opposite sex and same sex men and couples seeking a relaxation of the state’s laws.

Sam Everingham, founder of Growing Families Australia, recently hosted the annual Surrogacy and Donor Seminar in Perth.
New clinic Murdoch Square opening January 2025

Perth Radiological Clinic offers a comprehensive range of women’s imaging services including:
• Obstetric ultrasound including first trimester screening and cervical length assessment
• Gynaecological ultrasound imaging
• Pelvic MRI and pelvic floor ultrasound
• Endometriosis MRI
• Five breast imaging clinics across the metropolitan area (North, South, East and Central) for ultimate patient convenience
• All breast imaging modalities and breast biopsies performed including—
- Breast implant volumetric assessment, using low dose CT
- Digital mammography
- 3D mammography (tomosynthesis)
- Breast MRI.
Doctor Priority Line for urgent bookings and enquiries 9599 3929
continued from Page 15
“We always have great interest in our Perth seminars on this topic because there is so little that WA professionals can offer in this area,” says Mr Everingham, a prominent figure in the surrogacy and family building community and a father to two daughters born via international surrogacy.
“We have been running seminars in Perth since 2015. Often the Department of Health (WA) writes to warn us about complying with WA legislation.”
Mr Everingham’s hope is that the WA Government acts promptly on its long-awaited promise to allow male singles and couples to access domestic surrogacy and has been lobbying for years via Surrogacy Australia and The All Kids Are Equal campaign.
He adds that neither WA lawyers nor medical professionals are allowed to advise on surrogacy arrangements, and with the ongoing ban on gay men accessing surrogacy locally, “we see an alarming reliance on unfiltered online advertising of questionable programs and program in unregulated environments by WA citizens with apparently no awareness of the risk”.
Jamie’s story of overseas surrogacy has a happy ending. He’s now busy with his happy and healthy sevenmonth-old son, relieved to have him home after proceeding with commercial surrogacy in Argentina.
But as Professor Hart has explained, the experience of travelling overseas to find a surrogate is hugely emotionally and financially stressful for someone like Jamie, not to mention a legal minefield that he was very careful to avoid.
For him, that meant finding a recommended country in terms of providing the correct birth certificate, and one he could afford. The US was too expensive, so Argentina ended up being his final choice.
Initially, it was a smooth process, thanks to the help of prominent Queensland-based surrogacy advocate Stephen Page. The

passionate family and fertility lawyer has just released a new guide called When, not if: Surrogacy for Australians
Mr Page put Jamie in touch with an Argentinian lawyer who introduced him to a reputable agency. Jamie visited Argentina, met the local lawyer and chose an anonymous egg donor alongside a surrogate to carry the embryo.
There was a slight hiccup – he had to make another lightning trip back to Argentina when the laws changed, forcing him to sign papers in person rather than via technological means.
Then, after the birth of his son, the relatively quick process of about 18 months was turned on its head.
While still in Argentina and awaiting an Australian birth certificate to then apply for an Australian passport, a staunchly Catholic judge announced a crackdown on commercial surrogacy in the country, stalling the certificate. At the time, Jamie and other intended parents had no idea if they would ever be able to take their children home.
What should have been two months at a push ended up being 16 traumatic weeks for Jamie, forcing him to rent an Airbnb, taking care of a new baby, hoping for the best and still trying to run
his Perth-based business. It was only after the efforts of a group of surrogacy lawyers acting for the parents who banded together to sue the judge.
“It was people power,” says Jamie. “When the judge went on a leave of absence, the Australian government stepped in and released a citizenship by descent (document) and they allowed this to be enough for a passport.
“But the entire time I was there, I thought I’d be in Argentina until the baby was 18.”
Now happily home and getting used to life as a single dad – with the help of his parents and friends –he’s managing to work and still care for his little one, but the twists and turns with his surrogacy experience are still very fresh.
“They need to make it fair here, for men and for women,” says Jamie. “I’d like commercial surrogacy – if they make it legal – to be regulated in a way that’s good for the kids and the parents.”
* Jamie is unnamed for privacy reasons. ED: The inaugural Australian Surrogacy and Donor Awards were recently held in Sydney, recognising the contributions of individuals and organisations. The Community Person of the Year was Paul Hadfield-Jia from WA.

Many of WA’s top neurologists are backing a locally led push to ban a farm chemical that some believe could be linked to Parkinson’s disease.
By Cathy O’Leary
Perth neurologist David Blacker does not know whether his diagnosis of Parkinson’s disease is linked to a common herbicide, but he believes it is not worth taking the risk.
Dr Blacker – along with many of his colleagues – is calling on the country’s chemical regulator to ban the controversial weedkiller paraquat, which grain growers say is vital to crop production and food supply.
Parkinson's is a progressive brain disorder that affects the nervous system, but symptoms generally develop over years and can affect movement, sleep, mental health and cognitive function. It is believed that more than 150,000 Australians have Parkinson’s, and it is thought to be the fastest growing neurological disorder in the world.

According to the World Health Organization, there is no known cause of the disease but exposure to pesticides may increase the risk.
Dr Blacker suspects his diagnosis of early onset Parkinson's disease in 2018 could be partly linked to his exposure to agricultural chemicals while growing up in the Wheatbelt, where he played and worked in areas that had been sprayed with herbicides.
A neurologist specialising in stroke for more than 20 years, his diagnosis forced him to retire from clinical work last year, although he still works in medical research at Perth’s Perron Institute and in Parkinson’s disease advocacy.
First concerns
Dr Blacker says that while people joke about doctors’ poor handwriting, it was seeing how his own writing had deteriorated over years – as well as watching the movements of Parkinson’s patients in the clinic – that led to his concerns that something was amiss and his subsequent diagnosis.
His submission is one of 168 made to the Australian Pesticides and Veterinary Medicines Authority (APVMA), which is reviewing the use of paraquat and the related chemical diquat.
While the authority has proposed some limits on the use of the chemicals, it rejects the view that they are unsafe and says, “the overwhelming weight of evidence is that paraquat does not induce neurotoxicity.”
The APVMA says it is working its way through the submissions, as well as reviewing the science and data, but a final decision is not expected until midway next year.
While grain industry and farming bodies have weighed heavily into the debate, arguing restrictions on the use of paraquat in cropping systems will hurt agriculture, 29 of the submissions have been from doctors and health organisations, with many calling for a ban.
Dr Blacker wrote a private submission but ended up with a strong quorum of doctors who co-signed it, with 41 West Australian colleagues, including 32 neurologists, eight movement disorders specialists and 11 professors.
The submission reads like the who’s who of WA neurology, with Professors Graeme Hankey, Bill Carroll, Frank Mastaglia and Peter Silbert among the signatories.
The Australian and New Zealand Association of Neurologists and the Movement Disorders Society of Australia and New Zealand have also made submissions supporting a ban, with the ANZAN describing Australia as an "outlier."
MDSANZ president Carolyn
Sue is a world-renowned expert in movement disorders. In a submission to the regulator, she described the paraquat situation as a critical public health issue.
"The evidence supporting this connection is compelling and warrants immediate action to protect public health," she wrote. "The health risks associated with this herbicide far outweigh any potential benefits, and alternatives are available that do not pose such severe threats to human health."
Parkinson’s Australia, which has an online petition calling for paraquat to be banned, argues that 70 countries have banned its use due to its severe health risks, including strong links to Parkinson’s disease. The group maintains paraquat poses a serious health risk to farmers, agricultural workers and the public.
Dr Blacker says the doctors who have called for the ban are not activists, but rather medical experts, including global leaders in Parkinson’s disease.
“It started out with me doing my submission as an individual and grabbing support from other neurologists and then organisations, and by the end I had over 40 signatures – and there’s not that many neurologists and neuroscientists, so I’ve ended up with about 90% of the practising adult neurologists,” Dr Blacker told Medical Forum
“I said what I thought was wrong with the assessment by the APVMA, which had conclusions including that the overwhelming weight of evidence was that there wasn’t any neurotoxicity and the link to Parkinson’s was not proven.
“I took objection to that because over the last few years there has been accumulating evidence that that’s not the case. The incidence of Parkinson’s disease worldwide is escalating quite rapidly over the past decade, and the leading experts in the world believe it’s probably linked to a number of factors including air pollution, exposure to toxins and exposure to herbicides specifically.
“The thing that stands out about paraquat is that biologically it causes damage to the brain, like Parkinson’s disease.”
Dr Blacker said in his submission that it was not just an agricultural
problem – it was also a health problem, as well as an environmental problem. And there were emerging epidemiological studies that had shown that exposure to paraquat did increase the risk of Parkinson’s.
“This is always a tricky business because previous research has relied on looking backwards at people’s previous history, say 20 or 30 years when it’s a bit hard to know what you were exposed to, so that’s been one of the criticisms,” he said.
“But more recently, in February this year, a group from California published a much more objectively based paper where they’ve had excellent records on which counties have used paraquat.
“They have a really good idea of the dose of it, and they lined it up with maps of where people lived and worked, and where paraquat was used, to see if there were any linkages, and if you lived less than 500 metres from a paraquat field, your risk was increased. But that wasn’t mentioned in the APVMA report.”
Farmers’ groups have accused campaigners against paraquat of scaremongering and argue there is no established causal link.
But Dr Blacker and some leading figures in this field have come down very hard on this, arguing there is a strong link.
“An association doesn’t always mean causation, but this is being played on,” he said. “My core argument is that the data is accumulating, and the scenario of requiring us to prove that something is doing harm before we do anything about it is completely different to what I do as a medical researcher.
“If we’re developing a drug, we have to prove it’s safe before we can expose people to it, so the approach with paraquat is completely illogical.
“And the fact of the matter is that more than 67 other countries have been able to make the change, and the fact that there are alternatives there, it’s just asbestos all over again.”





This Christmas, we extend our gratitude to the doctors, nurses, and all those who tirelessly support Western Australia’s health care community. Your dedication helps to bring healing and hope, and we thank you for the light you bring to those in need. May the spirit of the season shine brightly through each of you.


www.sjog.org.au
continued from Page 19
Dr Blacker said he was surprised by the reactions from leaders of the farming community to any change affecting their crop yield rather than being concerned about the safety of their members.
“There is also a perception being portrayed that the farmers are all against it but that is absolutely not the case, and one very senior farmer in the Wheatbelt has been speaking out saying this pesticide must be banned.”
The leading farm peak body, the National Farmers’ Federation, said in its submission that paraquat and diquat are widely used in Australian agriculture, supporting the production of grains, cotton, horticulture, sugarcane, rice, wine and various pastures.
The herbicides were critical to minimum and no-tillage farming practices, allowing farmers to better manage glyphosate resistance in a variety of weeds. They were also commonly used to get crops ready for harvest.
“Farmers rely on essential chemical products, including paraquat and diquat, to maintain yields and farm sustainably in an increasingly changing, challenging and volatile climate. The chemicals provide cost-effective protection against crop yield losses across Australia,” the NFF wrote.
“The APVMA proposes to remove a number of current uses at rates of application that pose an unacceptable risk to the environment, as determined on the data available at this time. The proposed regulatory decisions will have a significant and adverse impact on the agricultural sector, rendering the use of the chemicals impractical or ineffective in many circumstances.”
The NFF said Australian farmers were extremely concerned about the impact of the proposed decisions on their ability to farm sustainably and productively.
“Misinformation, particularly when linked to technical assessments undertaken as a component of APVMA reviews, is not in the interests of the Authority, the

agricultural sector or the general public,” it said.
Syngenta, the company that first manufactured paraquat, also maintains that the chemical does not cause Parkinson's disease and is safe to use if the label is followed.
And grain-growing organisations have called for the APVMA not to rush its review of diquat and paraquat. Grain Producers Australia said no deadlines should be put on the review by the Federal Government.
APVMA chief executive Scott Hansen said the regulator had received submissions from across industry, community, medical and public health sectors.
“We recognise that there is heightened interest in paraquat, both from those who rely on it as a key tool in farm management, as well as those who have concerns of a possible link between paraquat and Parkinson’s disease,” Mr Hansen said.
“The APVMA is committed to completing a rigorous scientific assessment and will take the necessary time to consider all the evidence provided to us during the public consultation. We expect to publish a final regulatory decision on paraquat in mid-2025.
“However, we take human health risks seriously and should new evidence emerge out of this consultation process that shows an imminent risk to human health, then we have the power to take quick action.”
In his submission, Dr Blacker and his colleagues called on the APVMA to take that swift action.
“Even if there are doubts about the weight of current evidence regarding causation, to continue to allow use of paraquat while safer options exist, continues to risk exposing more and more people to an increased risk of developing Parkinson’s disease,” Dr Blacker wrote.
“I find this to be illogical and unethical. I encourage further research to obtain as much knowledge as possible but believe this should not delay acting now.”
Dr Blacker told Medical Forum there would be costs associated with a ban on paraquat, but it had to be borne against the health costs.
“I would hope they will listen to the medical experts, and it gets some traction,” he said.
What is paraquat:
• Paraquat and the related diquat, are fast-acting, non-selective herbicides that kill most plants on contact
• Farmers' groups say it is an important tool for managing weeds and farming sustainability
• It is banned in 70 countries – and the number is growing – due to its toxicity but is still widely used in Australia
• Critics argue there is growing scientific evidence linking paraquat to the development of Parkinson's disease.
Over his 45-year career, Dr Lewis (Lew) Marshall evolved from general practice to become a specialist sexual health physician.

By David Rossbach
Early on in his career, Lew spent time in the remote northwest of Western Australia before landing at Fremantle Hospital, where he eventually became Head of Sexual Health Services. Until recently, he was an Associate Professor at both the University of Notre Dame and the University of WA.
Reflecting on his financial journey, Lew highlighted that “as medical professionals, we’re trained to care for others but often struggle to care for our own futures.” Lew’s transition from a busy medical professional to a fulfilling retirement offers valuable insights for doctors at any stage of their career.
The procrastination trap Lew’s early financial habits were not ideal. “I’m a great procrastinator,” he admitted. "If money was coming in, there wasn’t an issue.”
But eventually, work stops and so does the money. He acknowledged that working in a well-paid profession added to his
procrastination: “You get comfortable and feel you can put aside planning for the future, hoping it will all work out.”
This mindset often causes doctors to delay seeking the help they need, even when they have concerns.

Lew and his wife Kate also had children later in life. “It did concern me. I thought, how long will I have to work? How much money will I have? Will I be able to support my family? Because we all want to do things for our kids, don’t we?”
The work demands on doctors can lead to personal finances being a distant afterthought. “If you’re on call or operating and you always have to be available, and you have to look after your family, there isn’t a lot of spare time to do your own financial planning.”
Despite his concerns, Lew found
it challenging to act. "It was just in the too-hard basket. We’ve always been late doing our tax returns. It’s those things where you ask yourself, surely my time is better spent doing other things.”
Lew’s breakthrough came when retirement became a real prospect. “We should have done it earlier…my advice would be to go early and get things sorted.”
Leaning on the professionals
In 2018, at 63, Lew sought professional financial advice. Until then, he had managed the family finances in an ad hoc way. “There was so much more we should have been doing. I felt I’d wasted a lot of opportunities.”
“We were able to get completely organised and reduce our tax using the right strategy. We ended up with a clear pathway and confidence that we could retire comfortably.”


"My advice is to get these things sorted sooner rather than later because as doctors, we're all very aware of how tenuous our hold on life can be. And if something happens, we need to make sure that what we've got in place will sustain our family."
“I really didn’t know what I was going to do when I gave up work. I mean, I’m 70 now, so I’ve worked
until I was 70.” His gradual transition from full-time to progressively fewer days was key to his successful transition.
“I couldn’t imagine retiring cold turkey – working full time one week and dropping everything the next.” His transition removed the shock of completely altering his daily routine. It allowed him to develop new interests to fill his time when his professional commitments ended.
Lew’s hobbies now include travel, tennis, French lessons, a men’s book club, and gardening.
Intentionality is crucial when setting yourself up for the next stage of life. “It’s not just about what you do with your time but also who you will be spending it with.” Relationships play a crucial role in a successful retirement, so it’s important to invest in the people that matter most to you.
Lew’s story highlights the importance of seeking professional financial advice early. For medical professionals with demanding careers, a trusted adviser can help navigate the complexities of financial planning. Lew’s experience shows that it is never too late to start, but the earlier one begins, the better the outcomes.
If you would like to have a conversation with someone to start your financial planning journey, please reach out.

ADHD is easy to treat, but hard to treat well, according to experts. Now a new guide for clinicians aims to make it easier to optimise care.
It affects one in 20 Australians, yet diagnosis and prescribing for attention deficit hyperactivity disorder varies across the country, with patients often having to see multiple medical professionals before finding a treatment plan that works for them.
This process alone can cause stress, anxiety and disengagement from care among people who may already struggle to put their health first.
But now a new ADHD prescribing guide aims to improve diagnosis and access to ADHD care by empowering medical professionals, with a practical guide for the safe and responsible use of medications and holistic treatments.
By Andrea Downey
It is a response to the Australian Evidence-Based Clinical Practice Guideline for ADHD, published two years ago, and covers topics such as diagnosis, assessment, medication choice, dosing, monitoring, adverse effects, switching, stopping, and specific populations.

AADPA board president Professor David Coghill said it was intended to complement, not replace, the clinical judgment and expertise of healthcare professionals who prescribe or manage ADHD medications.
“We knew that prescribing of stimulant medications and nonstimulant ones was very variable. There’s still room for an individual clinician’s variation on a theme, but at least the theme is more standardised.”
Dr Paterson, who is also chair of the ADHD WA professional advisory board, said there is often a “misunderstanding” that if one of the stimulant treatments for ADHD –methylphenidate, dexamphetamine or lisdexamphetamine – does not work, then the other would not either.
The guide, developed by the Australian ADHD Professionals Association (AADPA) – an advisory group of cross-disciplinary health professionals including pharmacists, clinicians, academics, researchers and people with ADHD – provides the most up-to-date set of protocols and advice for diagnosis and treatment.
Contributing author Dr Roger Paterson, a Nedlands-based child and adolescent psychiatrist with a special interest in ADHD, said the guide aims to standardise the quality of prescribing for patients without stifling individualised care.
“Our principal has always been that bad practice anywhere is a threat to good practice everywhere,” he told Medical Forum

Yet in compiling the guide the authors found it did not matter which medication a prescriber started with, as long as they were flexible to change the medication if one was not working. They also found some patients responded better to short-acting medication, whereas others had better results with longacting medication.
Trial and error
“ADHD is easy to treat but hard to treat well, Dr Paterson said.
“What that means is the clinician has to be very active initially when choosing medication, with a process of trial and error and titration of dosage to reach what is called the optimal dose.
“The danger of not doing that is you get sub-optimal treatment.”
AADPA director, pharmacist and co-lead author Kate Tognarini also emphasises the importance of clinicians feeling confident in prescribing to help patients reach their full potential.
“When a person suspects they, or a family member, might have ADHD they are at the start of what can be a confusing and at times overwhelming journey,” she said. “This guide is another piece of the puzzle to allow health professionals to support them in the best way possible.
The guide also has advice on prescribing non-stimulant medication for those who have had an adverse reaction to stimulants, or in circumstances such as parents opting not to treat young children with stimulants.

While the primary focus of this guide is medication, AADPA encourages a holistic approach to the management of ADHD using a mix of non-pharmacological methods including psychoeducation, cognitive therapy and ADHD coaching.
Any interventions should balance, focusing on an individual’s strengths and include components of education about ADHD, as well as environmental and behavioural modifications, AADPA recommends.
strategies a lot easier.
“Medications target the core symptoms of ADHD – things like planning and organisation – the holistic or non-pharmacological strategies are things like working with a counsellor or coach to put strategies in place so that the medication is then working a lot better,” she said.
A person’s lived experience of ADHD is vital in helping doctors understand their patients. To support this understanding, the guide includes examples of lived experience.
Perth-based contributing author and appointed director on the AADPA board Lou Brown shared her own experiences of ADHD in the guide. She said her diagnosis at the age of 47, after her son was also diagnosed, changed her life.
“The titration of the dose is really important. A lot of professionals will start stimulants or non-stimulants, and they don’t really titrate it to a dose that’s working optimally, we often are happy with any improvement.
“Getting to that perfect dose with the least side effects – that will translate to more optimised care when dealing with medication. Of course, there are all the nonpharmacological therapies that go hand-in-hand but at least this is a start.”
“When the doctors do their diagnostic assessment, their number one treatment before they talk about medication is psychoeducation,” Dr Paterson said.
“You’ve got to explain to the patient what they’ve got and how it’s best treated, and that’s usually a combination of medication and non-medication treatments such as counselling or coaching.”
Ms Tognarini, who was diagnosed with ADHD at the age of 47, said that pills do not teach skills, though they make the implementation of
It is advised that when switching from one formulation of methylphenidate to another, the prescriber matches the immediate release dose across the different formulations.
There is no way to calculate a dose equivalence between dexamphetamine and lisdexamphetamine. This means that it is not possible to predict the dose of one based on response to the other.
For people who require higher doses for optimal treatment, guidelines often overlook the potential for conflict between adhering to a maximum dose and the principle of establishing the optimal dose by titration.
Clinicians who are experienced in dose titration may feel confident in choosing to continue dose titration into a higher dose range than is officially sanctioned, particularly when the alternatives may be suboptimal treatment.
“When I first took medication, it was like I could pause, stop and think for the first time,” she told Medical Forum
“I said to my partner ‘What is this? It’s like this space to think where I could consider my options and make a decision’. It had never been there before.
“But I actually didn’t know what to do in that situation because I had never learned, I had never been able to stop and think and have the ability to regulate my attention.”
After her son’s diagnosis, she

On behalf of the Doctors and staff at SKG Radiology, we thank you for your continued support throughout the year and wish you and your family a safe and happy festive season.

continued from Page 25
became so anxious about his future due to her own negative experiences that she found it difficult to leave the house. Without holistic interventions, her experience today would be very different.
“I went to counselling to help accept that, and I did a coaching course. I also have some really good friends who I could speak to and ask, ‘What would you do in this situation?’ or ‘Could you explain this to me?’.”
Ms Brown, who is now an ADHD coach, said she often hears from people who have different experiences of prescribing.
“There can be expectations that medication takes all symptoms away and makes everything feel like normal but someone who has ADHD is likely to never be neurotypical, and that’s OK,” she said.
“Medication is just one support strategy that you can use to work out how to live successfully with ADHD.
‘If someone is just given medication and all those other things aren’t addressed you can feel like a failure because you’re taking your medication but you’re not perfect.”
Put into practice
So, what can doctors and prescribers take away from the guide?
Firstly, the treatment of ADHD is never a one-size-fits-all approach, every patient is unique, and treatment needs to reflect their own lived experiences and areas they feel treatment can enhance their life.
Dr Paterson said that initially it was going to help specialists – the psychiatrists and paediatricians who are doing most of the diagnostic assessments and early titrations because they do not get a lot of training in ADHD when they are registrars.
“It’s going to be useful for them to flick through particular topics of interest, starting with medication and titration and then how to deal with certain situations, side effects, unusual developments,” he said.
“But it’s also going to be very useful to GPs who are going to be very new to co-prescribing, because more and
Examples of non-medication interventions:
• Lifestyle changes
Lifestyle factors include diet, exercise or activity levels, and sleep patterns. Lifestyle changes have the potential to improve day-to-day functioning for people with ADHD.
• Education about ADHD (psychoeducation)
This ensures people diagnosed with ADHD are told what their diagnosis means, common difficulties arising from ADHD, common strengths, increased health risks associated with ADHD such as anxiety, depression and substance misuse, and possible impacts on relationships, school and the workplace.
• Parent-family training
This aims to help parents meet the additional needs of children and adolescents diagnosed with ADHD and may look at the effects of the diagnosis on the child and the whole family.
• Cognitive Behavioural Interventions
This is a broad range of approaches that use cognitive or behavioural interventions to minimise the day-to-day impacts of ADHD. This usually includes environmental modifications, behavioural modifications, and psychological adjustment and cognitive restructuring. Environmental modifications involve adjusting home, school, work or social settings to maximise success.
Behavioural modifications may include strategies to help compensate for cognitive difficulties and improve social communication, while psychological adjustment can help people develop skills such as problem solving and managing stress.
Source: Australian Evidence-Based Clinical Practice Guideline for ADHD Factsheet
more the specialists are stabilising the patients then asking the GP to get involved to a certain level.”
Ms Tognarini hopes the guide will have far-reaching benefits for patients.
“One is to get more prescribers confident in prescribing in this area and hopefully that will improve access Australia-wide,” she said.
“Hopefully more GPs will be comfortable getting into this area and working in co-share arrangements with psychiatrists or paediatricians to manage all of the medication questions that can come up.”
But while it will be a useful resource for the pharmacological and nonpharmacological treatment of ADHD, Ms Brown emphasised the importance of compassion in care.
“The language used around medication and ADHD can empower or it can crush,” she said.
“Treat people with compassion,
empathy and understanding and do not look at them as a group of symptoms that need to be addressed or removed.
“You can have doctors who will give you medication and all they’re focusing on is assessing your symptoms, but you need a holistic approach, it also needs to be about what the person with the condition wants to achieve.”
AADPA hopes that the guide will serve as a first step toward national prescribing standards for ADHD medications and improve the quality and consistency of care for people with ADHD and their families.
It eventually plans to translate the guide into a smaller patient resource.
Find the guide here: aadpa.com.au/product/adhdmedication-prescribing-guide/

Coformulated tenofovir and emtricitabine (TDF/FTC) has been proven to be effective as preexposure prophylaxis (PrEP) for HIV. When taken as prescribed, PrEP can reduce the risk of sexually transmitted HIV by up to 99%.
Who can prescribe PrEP?
PrEP is listed on the Pharmaceutical Benefits Scheme as an s85 medication. This allows any medical practitioner or endorsed nurse practitioner to prescribe PrEP to eligible clients. According to data from the Pharmaceutical Benefits Scheme, 47,172 Australians were dispensed PrEP in the April-June quarter of 2024.
What are the barriers to PrEP prescription?
Research suggests that there are still gaps in Australian health professionals’ PrEP knowledge and confidence. For instance, a qualitative study of health professionals found that barriers to PrEP prescription included lack of familiarity with the clinical guidelines, a perceived lack of patient demand, and a perception that PrEP is a specialist medicine.
Similarly, an online cross-sectional survey of 407 GPs found that less than half felt confident prescribing PrEP, with the main barriers being ‘difficulty identifying clients who require PrEP/relying on clients to ask
for PrEP’ (76%, 310/407) and ‘lack of knowledge about PrEP’ (70%, 286/407).
Who should be considered for PrEP?
Anyone at risk of HIV acquisition should be considered for PrEP.
Indicators of behavioural suitability include:
• Casual receptive condomless intercourse with any men who have sex with other men (MSM).
• Rectal or vaginal gonorrhoea, chlamydia or infectious syphilis in a person who is not exclusively heterosexual.
• Methamphetamine use.
• Condomless intercourse with a regular HIV+ partner who is not on treatment and/or has a detectable viral load.
• A person in a HIV serodiscordant heterosexual relationship who is planning natural conception in the next 3 months.
• Shared injecting equipment with an HIV+ individual or with MSM of unknown HIV status.
Low rates of PrEP use have been reported among overseas-born gay/ bisexual MSM and gay/bisexual MSM who consider themselves to be at low risk of HIV acquisition because they are in mostly monogamous relationships. It is important to ensure that these groups are considered for PrEP suitability to avoid the emergence of HIV disparities.
What support is available for health professionals interested in prescribing PrEP?
• ASHM (previously the Australasian Society for HIV, Viral Hepatitis and Sexual Health Medicine) has published PrEP Guidelines to assist health professionals. These are available at prepguidelines.com.au. The guidelines are accompanied by a two-page, step-by-step decision-making tool for clinicians (scan the QR code on the accompanying page).
• ASHM also offers a free 40-60 minute introduction to PrEP prescribing online learning module: ashm.org. au/lms/introduction-to-prepprescribing/
• While all medical practitioners and endorsed nurse practitioners can prescribe PrEP, you can refer your patients to another health professional if you feel you are not yet ready. WA Health maintains a list of ‘PreP confident’ prescribers here: https://www. health.wa.gov.au/Articles/N_R/ PrEP-Prescribers (or scan the QR code on the accompanying page).
• If your patients want to know more about PrEP, you can refer them to www.waac.com.au/prep/
Sponsored by WAAC with support from the WA Department of Health

Fertility
Freezing
Genetic
Surrogacy
Fertility Counselling


exercise' in everyday activities

from falls, says
As our population continues to age and the preference for home-based care grows, we are faced with the situation where availability of care is decreasing while the need for it is increasing.
We know that older people are particularly vulnerable to falls at home and, tragically, those who do fall, often have a life expectancy of just 12 months thereafter. But falls don’t have to be an inevitable part of ageing.
The key to staying strong, active, and independent in our own homes lies in the simple, everyday movements we have all been practising for decades.
It’s a simple approach that shifts the focus from clinical, formal exercises to functional movements that mimic daily activities, such as reaching for a cupboard, moving a chair, lifting the kettle, watering the garden or walking across a room.
These familiar actions form the foundation of our exercise program, enabling seniors to maintain their mobility, balance, and strength in ways that feel natural and attainable.
By focusing on movements they already know, seniors gain confidence in their ability to remain self-sufficient and reduce their reliance on outside assistance. The program's success is built on the understanding that maintaining strength and functionality doesn’t always require complicated routines or gym equipment.
It can be as simple as harnessing the power of movement they’ve engaged in throughout their lives. It’s not only more accessible but also a more sustainable approach, helping to reduce the risk of falls, promote physical wellness, and preserve dignity as older adults age at home.
The reasoning behind this exercise program is not just preventative care but it demonstrates to seniors that maintaining an active lifestyle

is key to their long-term health and independence. In a world where ageing is often associated with decline, home-care exercise programs can reassure them that staying strong and active is well within their reach.
When someone can bend down to pick up laundry or reach for a cup on the top shelf, it’s not just about completing a task, it’s about having the freedom to live safely and comfortably in their own home.
These are movements we all do instinctively, yet as we age, they become more challenging, and even risky. Most falls are preventable with the right awareness, education, and exercise.
With one in four people aged 65 and over experiencing at least one fall a year, the falls prevention and balance training program has improved outcomes for people living at home so they avoid the need to enter a nursing home or a hospital admission.
When older people lose their confidence about doing household tasks, they become more reliant on other people to care for them and slowly lose their independence.
For many seniors, losing the ability to perform everyday tasks can feel like losing a piece of themselves but by focusing on these functional movements, home-care exercise programs offer practical skills with personal benefits.
There’s satisfaction knowing
someone’s gone from a high falls risk to a moderate falls risk and they’re less likely to fall over, break their hip, end up in a nursing home or die.
The program was named ‘Instinct’ because it combines the functional tasks people perform in their own home with evidence-based physiotherapy practise.
A decline of balance and increased fall risk can be retrained through everyday activities:
• Strengthen stability – balanced based tasks such as bending, reaching, or walking can unknowingly affect balance but physiotherapy exercises can help strengthen stability
• Continue with everyday activities – as people age, their centre of gravity becomes less stable but repetition of natural movements in daily routines can help rebuild coordination and reduce fall risks.
• Improving balance issues –balance can be addressed, retrained and improved by performing regular, instinctive movements in the home environment
• Practising home-based exercises – by continuing to perform daily activities, seniors can improve and rebuild their strength and stability.
• Wearing supportive footwear – well-fitted and comfortable footwear will provide ease of walking and greater support and balance than slippers or socks.
The link between mental illness and dementia is not well-known but the implications are alarming, according to neurodegenerative diseases expert
Professor Matthew Kiernan.
There is a perfect storm brewing, largely unnoticed, in the 21st century: the convergence of two high prevalence, high impact and growing groups of brain conditions – mental illness and dementia.
While previously these conditions were studied in silos, recent medical research has uncovered a growing body of evidence revealing strong links between the two. It is still uncertain exactly what is cause and what is effect, but what is known is that we are losing our minds at an unprecedented rate and scale. And not just in Australia. Neuroscience has taught us that
above all else, it is the health of our brains that will determine our trajectory through life and particularly as we age. Currently, one in five Australians suffers from a mental health disorder during their lifetime, ranging from depression and anxiety, through to psychotic illness such as schizophrenia, or bipolar disorder.
According to the Australian Institute of Health and Welfare, for every 1000 Australians, one in 15 is affected by a form of cognitive impairment, with Alzheimer’s disease and vascular dementia representing the most common causes.

The latest WHO statistics indicate that globally, more than 970 million people live with a mental health disorder and 55 million have dementia: 60% of the latter live in middle to low-income countries.
The Western Pacific region, which comprises 37 countries including Australia, houses the largest and fastest-growing ageing population in the world, which will account for more than 50% of global dementia cases by 2050.
Our growing understanding of the interconnectedness of mental health and dementia presents an opportunity to channel this perfect storm and explore novel approaches to prevention,


Our warmest Christmas greetings, best wishes of health, happiness & work life balance for 2025 to all our referring doctors, allied health professionals, colleagues and their families. Thank you for entrusting us to be part of the health and wellbeing of our mutual patients. Best of true health
Marek Garbowski & Perth Vascular Clinic Team
Perth Vascular Clinic is WA’s leading vascular solutions centre. With state of the art management & treatment of conditions affecting vascular health we also offer minimally invasive vascular investigations and treatment.

Dr Marek Garbowski | Vascular & Endovascular Surgeon All enquiries & appointments bookings Phone: 6116 4955 | Email: reception@perthvascularclinic.com.au
Visit our comprehensive website www.perthvascularclinic.com.au
risk reduction, early diagnosis, treatment and care to benefit not just Australia, nor the Western Pacific, but more globally.
Families share conditions that affect the brain and the mind. For instance, conditions such as bipolar disease, schizophrenia and autism are more common in the families of people diagnosed with dementia. In turn, that may suggest that psychiatric therapies such as lithium may be useful to treat dementia. And conversely, monoclonal antibody therapies for dementia which treat inflammation in the brain may yet be successfully introduced for psychosis.
In September this year, Neuroscience Research Australia and The Lancet Regional Health Western Pacific launched a dementia series – global reviews of the best scientific and clinical evidence to provide a roadmap for the region.
For example, depression and hearing loss have now been added to the list of modifiable risk factors for dementia. Other key risks previously identified include hypertension, obesity,

tobacco use, alcohol intake and physical inactivity. The Lancet Commission asserts today that 45% of dementia cases (an increase on prior estimates) could be delayed or reduced if modifiable risk factors were addressed.
Meanwhile, the Productivity Commission calculated that the direct economic costs of mental illness range up to $70 billion per year in expenditure and reduced economic productivity. Separately, Dementia Australia estimated the total economic cost of dementia as $15 billion per annum.
If we worked to address both health issues in tandem, we may potentially solve an annual $85 billion problem.
As one of the few high-income countries in the Western Pacific, Australia is well placed to step up and adopt a leadership position to reduce the rate and scale of mind loss. The National Dementia Plan can help guide similar initiatives across the Western Pacific, to collectively address the burden of depression and dementia in a fashion that is culturally appropriate and engages local communities. A key priority relates to prevention, and to education: as a region, we must develop education programs to target modifiable disease risk factors, with a specific focus on depression. Allied to education is a need to accelerate diagnostic capacity, while further integrating models of care for both depression and dementia, tailored to the diverse cultural and ethnic groups in the region and expanding supportive services for carers.
continued on Page 35

Thank you for your support this year, and all the best for 2025.
Warm regards,
Dr Shane Kelly Ramsay Health Care State Manager (WA)
Ovulation Induction & Ovulation Tracking (OI/OT)
Intrauterine Insemination (IUI)
Our Fertility Specialists in WA

Dr Gayatri Borude
MBBS, MD, DNB, FRANZCOG, FACOG, FMAS
Clinical Director (WA), Fertility Specialist, Obstetrician & Gynaecologist
In Vitro Fertilisation (IVF)
Intracytoplasmic Sperm Injection (ICSI)

Frozen Embryo Transfer (FET)
Donor Program Egg Freezing

Dr Mahalakshmi Ragunath
MBBS, DGO, MRCOG, MSc, FRCOG, FRANZCOG
Fertility Specialist, Obstetrician & Gynaecologist
Perth 9 Perilya Road, Craigie WA

Dr Shanthi Srinivasan
MBBS, MD, DNB, FNB(Rep Medicine), FRANZCOG
Fertility Specialist, Obstetrician & Gynaecologist
The number of Australians having strokes is the highest it has been in more than two decades, with a new national report projecting this figure will get worse if immediate action is not taken.
In 2023, there were 45,785 Australians who experienced a stroke – this equates to one stroke every 11 minutes.
As a result, a neuroprotective drug that protects the brain and buys patients extra critical time while they are waiting to receive care to remove the stroke-causing clot is revolutionary.
The neuroprotective drug ARG007 (which was developed by WA scientists), targets ischaemic strokes, which accounted for 81.2% of firstever strokes and 84.8% of recurrent strokes in Australia in 2023.
The Stroke Foundation’s Economic Impact of Stroke Report further indicated that total strokes which occurred in Australia last year –34,793 – were first-ever strokes and this numbers has surged from the 27,428 new strokes estimated in the 2020 Deloitte Report.
This increase underscores the urgent need for effective treatments and interventions as the incidence of ischaemic strokes is projected to rise to 55,000 annually by 2050, due to population growth and ageing, meaning one person every 10
minutes will be suffering a stroke in Australia.
Key findings from the report include:
• Mortality rates: Around 11.4% of first-ever ischaemic strokes resulted in death within 28 days, and the mortality rate for recurrent strokes was 14%. These figures highlight the need for timely and effective treatment options.
• Demographics: Notably, 25% of first-ever ischaemic strokes occurred in individuals under 65, while the likelihood of a fatal stroke increased significantly with age, reaching 24% for those over 85 years.
• Regional disparities: Australians living in regional areas face a 17% higher likelihood of experiencing a stroke and often encounter barriers to receiving standard treatments.
The economic implications are staggering, with short-term costs for ischaemic strokes estimated at $1.43 billion, with an average cost per person of $36,611 for first-ever incidences.
Lifetime costs of ischaemic strokes exceeded $13.6 billion, including healthcare, productivity losses, and informal care, equating to approximately $325,231 per person.
We want to shift the thinking around ischaemic stroke treatment
continued from Page 33
of the total global health research output.

and ARG-007 represents a step forward in potentially reducing mortality rates, improving health outcomes and alleviating some of the economic impact of stroke highlighted in the report.
Its ability to be administered alongside current standard of care to ischaemic stroke patients presenting to metropolitan hospital emergency departments is already proving possible in a nation-wide Phase 2 clinical trial.
Through this trial we will determine how well ARG-007 works to reduce brain injury in patients who have suffered a stroke and are receiving clot removal (endovascular thrombectomy) treatments.
The trial, being conducted at 10 hospitals across Australia, aims to determine the safety and preliminary efficacy of ARG-007 in patients, with results expected in 2025.
It is hoped that ARG-007 will eventually be administered by first responders and stocked in ambulances around the world.
ED: Dr Liz Dallimore is a neuroscientist, and CEO and managing director of Argenica Therapeutics which is developing new therapeutics to reduce brain tissue death after stroke and other types of brain injury and neurodegenerative diseases.
through dementia and mental illness.
ED: Professor Matthew Kiernan is CEO at Neuroscience Research Australian (NeuRA) Losing our minds
To achieve these goals, we must close existing research gaps by focusing on the diverse populations within our region. In the face of this need, we must address an imbalance whereby dementia research accounts for less than 3%
In a new take on the old African proverb “It takes a village to raise a child”, investment in multi-sectoral, collaborative consortia will be required – at both national and international levels – to reduce the cognitive impairments induced
Science has opened the door for us: now we must support global approaches so that we may collectively walk through it together, but always guided by people with lived experience and their carers.
Bulk-billed for three cycles
No out-of-pocket expenses for Medicare-eligible patients at Genea monitoring centres.
Easy online referrals
Simple referral process with full nursing support for your patients.
Ovulation reports sent directly to your practice
Receive detailed ovulation reports with hormonal status and cycle insights for informed fertility assessment and management.

Discover Genea’s ovulation tracking service
Scan the QR code to learn more and to download a referral pack.
Genea Perth
Level 2, 190 Cambridge Street, Wembley WA 6014
Genea Mandurah 29-31 Sholl Street, Mandurah WA 6210
Men and teenage boys are resorting to the dangerous use of anabolic steroids to buff up to match images on social media, body image experts have warned.
A new review study in Psychology of Men & Masculinities journal found that exposure to social media posts depicting ideal muscular male bodies was directly linked to a negative body image and greater odds of resorting to anabolic-androgenic steroid use.
“The ideal male body in Western society is simultaneously very lean and very muscular, with a V-shaped figure and emphasis on large arms, shoulders and chest,” said senior author Associate Professor Ivanka Prichard from Flinders University’s College of Nursing and Health Sciences.
“While previous research in this space has predominantly focused on women, recent evidence suggests that men also experience the negative effects of social media on their body image and are also engaging in risky behaviours to address their body image,” she said.
“There is pressure on men and adolescent boys to not only meet this appearance ideal but to also be physically strong, as this is intrinsically linked to masculinity.”
Data from six electronic databases was used to compile the review with studies looking at either general social media use, appearance-related social media behaviours, or exposure to social media content.

Among bodybuilding enthusiasts, the term ‘natty’, short for natural, symbolises a commitment to achieving fitness goals without the aid of synthetic substances such as steroids.

However, even within these communities, social media's pervasive influence can contribute to a heightened pressure to conform to unrealistic body ideals, particularly those characterised by a lean and muscular physique.
to a negative body image and thoughts of using anabolicandrogenic steroids.
“It was clear that appearancerelated social media use is related to a more negative body image and greater odds of anabolicandrogenic steroid use in men,” they said.
“We need to consider the implications of media consumption on men’s health and selfperception, so we can develop a more supportive environment where body image concerns can be addressed constructively.”
The review looked specifically at males and broadened the outcomes to include the appearance-altering behaviours of physical activity and anabolicandrogenic steroid use to explore the relationships between social media and body image.
Lead author Nepheli Beos from the College of Psychology, Education and Social Work said that time spent on social media platforms, engaging in online appearancerelated behaviours, and being exposed to appearance-related social media content were linked
Advert removed in compliance with Medicines Australia's Code of Conduct and the Therapeutic Goods Administration's Therapeutic Goods Act.
https://medicinesaustralia.com.au/code-of-conduct/about-the-code/ https://www.tga.gov.au/legislation-legislative-instruments

Second opinions are vital and questioning should never have been shut down. Doctors should offer advice to policy makers but we are too narrow in thinking to be the sole voice.
How has 2024 disappeared at record speed? All ideas welcome. It is also hard to believe that it is five years since the COVID-19 pandemic began.
Those constantly berating doctors to “self-reflect” seem reluctant to apply the same standards to themselves. The report into Australia’s COVID response is a credit to its authors who managed to highlight what was done right and wrong, despite the limited terms of reference which excluded the actions of state governments.
It found that Australia fixated on case numbers and lost sight of the broader mental-health impacts of lockdowns and school closures. “Increased social isolation, stress, anxiety, uncertainty, loss of control, disruption to daily routines and concerns for the wellbeing of family and loved ones created the conditions for either the onset of mental-ill health or deterioration of existing conditions,” the authors said.
“School closures and remote learning also led to increased engagement with social media, triggering weight and ‘body checking’ behaviours among some young people.”
Research also suggested that lockdown-induced “lifestyle disruptions” caused changes in brain biology in children and young people, with a greater impact on females.
These effects could last decades. Are we listening?
Chris Uhlman writing in The Australian had some self-reflection points for consideration.
“Doctors were indispensable and underlined why you should always seek a second opinion. As a class, they should never again be the sole voice in a crisis. The real Long COVID is the tail of iatrogenic harm left by the lockdowns they championed”. Ouch.
Uhlman is right. Second opinions are vital and questioning should never have been shut down. Doctors should offer advice to policy makers but we are too narrow in thinking to be the sole voice. Leadership requires listening to multiple inputs and preparedness to take risks that doctors are not equipped for.
My sense is that on the ground, we get it. In officialdom, I am not so sure.
Thank you to readers for your support in 2024. May you all get some rest and spend time with friends and family. I wish you all a very Merry Christmas and a Happy and prosperous 2025.
By Dr Preethi Nagubandi, Gynaecologist, Murdoch
Preconception care is a critical component of reproductive care that can significantly influence maternal pregnancy outcomes and have a lifelong impact on a child’s health. Appropriate care can reduce the risks of gestational diabetes, hypertension, preterm birth, impaired fetal growth, poor birth outcomes and congenital anomalies.
Both underweight and overweight women are at increased risk of adverse pregnancy outcomes. Overweight or obese women should be encouraged to lose 5-10% of their body weight before conception as this reduces rates of fetal abnormalities, miscarriage, preeclampsia, gestational diabetes, preterm delivery, macrosomia and stillbirth.
This may require referral to a dietitian, education regarding a healthy and balanced diet with supplementation for any identified nutritional deficiencies, guidance on exercise and in some cases referral for bariatric surgery.
Educate women regarding the limiting of caffeine consumption to < 300 mg/day (2-3 cups a day) as this increases the risk of fetal growth restriction and the cessation of smoking, alcohol and illicit drug use as applicable.
Male partners also require counselling as obesity, smoking, excessive alcohol consumption, illicit drug use and poor diet may affect their fertility and influence pregnancy outcomes.
Folic acid supplementation is vital in preventing neural tube defects. A Cochrane review demonstrated a 72% reduction in defects compared to no intervention, placebo or supplements without folic acid.
A dose of 400-500 mcg is recommended for at least one month prior to conception and continued for the first 12 weeks of pregnancy. A higher dose of 5mg is recommended for women with pre-pregnancy diabetes mellitus, a previous affected child or family
history of neural tube defects, a BMI over 30 or those using antiepileptic medications.
Also recommended is 150 mcg of iodine for all pregnant and breastfeeding women to aid with the development of the fetal brain and central nervous system.
Chronic conditions (e.g. diabetes, hypertension, thyroid disorders, epilepsy, renal disease, autoimmune conditions and cardiac conditions) should be optimised before conception. Achieving optimal glycaemic control in diabetes reduces the risk of congenital malformations, miscarriage, preterm birth and birth weight abnormalities.
Women may require specialist input or input from maternal-fetal medicine specialists. They may also require contraception while being treated.
Mental health status should also be assessed and managed, as appropriate, before pregnancy.
Women should also be screened for domestic violence as this is associated with poor antenatal attendance and poor obstetric outcomes.
Review medications, over the counter preparations and vitamins as they may carry teratogenic potential and need to be ceased or changed before conception.
Review the woman and her partner’s ethnic background and family history as this may raise concerns for inheritable genetic disorders. Referral for genetic counselling may be needed.
All couples considering pregnancy should be offered reproductive carrier screening for conditions such as cystic fibrosis, spinal muscular atrophy and fragile X syndrome. Carrier rates are 1:25, 1:40 and 1:250 respectively.
The woman is tested (blood test)

Preconception health greatly influences pregnancy outcomes and the child’s health lifelong
Simple interventions including folic acid and iodine supplementation greatly impact fetal development
Reproductive screening should be offered to all couples and a Medicare rebate is now available.
first and if positive, the partner is tested. Testing prior to pregnancy allows for genetic counselling and increased reproductive options including in vitro fertilisation with preimplantation genetic diagnosis, in vitro fertilisation with donor oocytes or sperm, or adoption.
A general examination should be performed including blood pressure, auscultation of heart sounds and where relevant, a breast examination and cervical screening.
Vaccination status should be reviewed. Advise immunisation for hepatitis B, rubella and varicella for women not immune. Women should not conceive for at least 28 days after receiving live, attenuated vaccines.
Women should also be screened regarding their risk of exposure to toxins or radiation in the home, workplace or during other activities and advised to avoid travelling to areas with high rates of infection while trying to conceive.
– References available on request
Author competing interests – nil
Advert removed in compliance with Medicines Australia's Code of Conduct and the Therapeutic Goods Administration's Therapeutic Goods Act.
https://medicinesaustralia.com.au/code-of-conduct/about-the-code/ https://www.tga.gov.au/legislation-legislative-instruments
By Dr Arpita Ghosh, Gynaecologist & Fertility specialist, Hollywood
A woman’s chance of having a baby decreases with age –accelerating after 35. Oocyte cryopreservation (egg freezing) has established itself as a viable option for women wanting to preserve their fertility for medical reasons (e.g. prior to cancer treatment) or for personal considerations.
Modern reproductive technology utilises a rapid method for efficiently freezing eggs using a process called ‘vitrification’. This has challenges, risks and costs. These need to be discussed so women can make an informed choice.
freezing process
The woman is screened for infectious diseases including HIV, hepatitis B and C. She is then given a course of fertility drugs to stimulate her ovaries and the size and development of follicles is tracked with serial ultrasound examinations and hormone levels. When mature, the eggs within the follicles are retrieved using an ultrasound-guided procedure under sedation. The number of eggs retrieved per stimulation cycle can vary (depending on ovarian reserve, technique of operator etc) and this determines how many cycles is deemed necessary to retrieve the optimal number of eggs. The eggs are then frozen and stored at the fertility clinic.
Biologically, eggs can be stored indefinitely, and when the woman is ready to become pregnant, the eggs can be thawed and fertilised with her partner’s or donor’s sperm. If healthy embryos develop, one will be transferred to her uterus and any remaining embryos can be frozen for later use.
What are the success rates of egg freezing?
In IVF treatment, the chance of a live birth is similar for frozen and ‘fresh’ eggs. The two most important factors determining the chance of having a baby from frozen eggs are age when the
Fertility preservation is a viable option, with a 70-80% chance of having a baby from frozen eggs for a woman freezing eggs before age 35
The optimal number of eggs to be collected for freezing increases with age, needing multiple stimulation cycles, with implications on overall costs
Return of user to use the eggs is low, opening important ethical and legal considerations including ownership, discarding, or donating the oocytes if unused.
eggs are frozen and the number of stored eggs.
The number and quality of the eggs that develop when the ovaries are stimulated decline with age while chromosomal abnormalities increase. At every step of the process there is a risk that some will be lost. Of the transferred embryos, only some will result in a pregnancy, and some pregnancies miscarry.
Currently there is a 70-80% chance of having a baby from frozen eggs in a woman who froze her eggs below age 35, with success declining with increasing age.
Current data indicates that a woman under 35 years when freezing eggs needs to store 10 eggs for a successful pregnancy. This increases to 20 at age 38 and as many as 35 at age 40. Although there is no current evidence to support exact number of eggs required to be frozen at any particular age, in practice, the aim is to freeze at least 15-20 eggs for optimal chance of success. The number of cycles needed to get to this number will depend on age and ovarian reserve.
A small proportion of women can have an excessive response to the fertility drugs that are used to stimulate the ovaries. In rare cases, this causes ovarian

hyperstimulation syndrome (OHSS), a potentially serious condition. Bleeding and infection are very rare surgical complications of the egg retrieval procedure.
Egg freezing technology is still at a nascent stage and the long-term health of babies born from a frozen egg is unknown. However, although safety data remains preliminary, the fact that the babies are born healthy with no apparent health issues is reassuring.
In general, a Medicare rebate is only available for egg freezing for medical, not personal reasons. Costs may be considerable and provided up front. More than one stimulation cycle is usually required with final costs depending on the number of cycles needed.
Frozen eggs are stored in liquid nitrogen tanks at minus 196 degrees Celsius incurring an ongoing storage cost This can be substantial if stored for several years, especially given the fact that return of user is low (10-12% in Australia). There will also be costs involved eventually when using the eggs to conceive.
Women need to know the chances of successfully having a baby from frozen eggs, considering age and other factors and how many eggs will need to be stored as this impacts cost. Women should be counselled that they may not need to use the frozen eggs, and that pregnancy is not guaranteed. Ethical and legal considerations, including issues surrounding delayed parenthood, ownership, and status of stored oocytes; and eventual discarding or donating the oocyte if not used should be discussed.
Robust education and counselling about the procedure’s efficacy, risks, limitations and potential outcome and thorough informed consent are imperative before making this important choice.
Author competing interests – nil
By Dr Grace Phua, GP, & Dr Sarah Smith KEMH GP Liaison
Gonorrhoea and chlamydia are on the rise and, in WA, notifications have surpassed pre-pandemic levels. Syphilis has re-emerged as a threat: in 2023, the highest number of congenital syphilis cases were reported Australiawide since 1995.
STI testing is an important part of preventative healthcare. Early detection and treatment can prevent complications of disease and onward transmission. Primary care clinicians are encouraged to test often, treat according to guidelines, undertake contact tracing and educate their patient community about safer sexual behaviours.
While STIs continue to spread, doctors may feel hesitant to broach the topic of testing, especially when patients have come with an unrelated complaint. A small study conducted in Perth in 2013 indicated that patients would not be embarrassed if GPs initiated discussion about sexual health even if this was unrelated to the presenting complaint.
Interviews with a small number of young women in Victoria indicated that they found routine STI testing acceptable, especially where it is offered based on age demographic.
In WA, opportunistic STI screening is recommended for all sexually active people 40 years or younger. Screening for syphilis at multiple points in pregnancy is now also a part of routine testing in WA. These approaches normalise testing, do not stigmatise those who are tested and


STIs are on the rise, particularly gonorrhoea and syphilis
Offer STI testing widely
Syphilis serology should be included in all STI tests.
are less likely to miss detection in people not known to have risk factors for infection.
Risk groups that should also be offered opportunistic STI screening include:
• People who have recently changed sexual partner or are known to have casual partners
• Men who have sex with men
• People from a high prevalence country, or have a sexual partner from a high prevalence country
• Aboriginal people
• People experiencing homelessness
• People who use methamphetamine and/or inject drugs (7).
STI tests should include syphilis serology. Over the past decade, cases of infectious syphilis have been increasing in Western Australia and Australia. These trends mirror that in other developed countries around the world. Consequently, syphilis
serology should now be included as part of all STI testing.
Furthermore, if a patient presents with genital lesions, the lesions should also be swabbed for syphilis PCR.
For up-to-date recommendations on STI treatment, the Silver Book and STI Management Guidelines are important resources to bookmark. Note that syphilis is treated with intramuscular benzathine benzylpenicillin, which is not routinely stocked at community pharmacies. You can order a supply through the Doctor’s Bag and have it stocked in the practice fridge to facilitate prompt treatment.
An important aspect of management is the initiation of contact tracing to address re-infection risk and mitigate onward transmission. Notifying contacts can be done anonymously using website-based portals, and your local sexual health unit can also assist.
STIs are on the rise. So, let’s talk about testing. What are some conversation openers you could use in your practice?
– References available on request ED: Dr Phua is a part of the Boorloo Public Health Unit (formally known as the Communicable Disease Control)
By Dr Sean Copson, Gynaecologist and Fertility Specialist, West Perth
Endometriosis is a common condition which affects one in seven females and those assigned female at birth. It is a complex condition that affects fertility through inflammatory pathways, impacting ovarian, peritoneal, tubal, and endometrial function. This disruption can hinder folliculogenesis, fertilisation and implantation, potentially leading to infertility.
Endometriosis can be surgically staged as Stage I-IV, and these stages correlate directly with fertility outcomes. In advanced stages (III and IV), endometriosis may cause significant anatomical distortions and adhesions, further complicating oocyte release, folliculogenesis, sperm motility, myometrial contractions, fertilisation and embryo transport.
Treatment approaches
While medical or hormonal therapies are often prescribed for pain management, they do not enhance fertility outcomes in cases of endometriosis-associated infertility. These therapies are therefore not recommended as a treatment for infertility itself. However, they can
Key messages
Endometriosis disrupts fertility through inflammation and anatomical changes
Surgery and ART provide fertility options based on endometriosis severity
Personalised treatment and preservation aid family planning with endometriosis.
be useful post-surgery to alleviate pain and reduce recurrence of endometriosis without affecting future pregnancy rates.
Surgical intervention can improve spontaneous pregnancy rates depending on the stage and extent of endometriosis. For patients with endometriosis-associated infertility, surgical options may be beneficial, particularly for those looking to avoid assisted reproductive technology (ART) such as IVF.
Stage I/II endometriosis:
Laparoscopic surgery for early-stage endometriosis has been shown to enhance spontaneous conception rates in patients with infertility.

Ovarian endometriomas:
Laparoscopic excision of ovarian endometriomas, including cyst wall stripping, sclerotherapy, or plasma ablation, is effective in increasing spontaneous conception rates. Simple drainage of endometriomas is not advised due to a 100% recurrence rate. If attempting conception is not desired immediately following surgery, hormonal therapy may help prevent recurrence.
Deep infiltrating endometriosis (DIE): No substantial evidence supports laparoscopic treatment of DIE to improve fertility, though surgery may be beneficial for symptomatic individuals desiring pregnancy.
For those weighing natural conception post-surgery versus ART, clinicians and patients should collaborate on decisions using the Endometriosis Fertility Index (EFI), which predicts non-ART pregnancy rates after surgery.
Medically assisted reproduction provides additional pathways to pregnancy for those with endometriosis-related infertility,


particularly when spontaneous conception is unlikely.
Intrauterine insemination (IUI): For patients with Stage I/II endometriosis, IUI combined with ovarian stimulation shows improved pregnancy rates over expectant management. However, the efficacy of IUI in more advanced stages (III/IV) is unclear.
In vitro fertilisation (IVF): IVF is often the preferred option for patients with a low EFI score postsurgery, those with impaired tubal function, or those facing male factor infertility. ART does not increase the risk of endometriosis recurrence, though symptoms may intensify during treatment.
During IVF, oocyte retrieval can be performed with an endometrioma present. Prophylactic antibiotics are sometimes administered to minimise
the risk of infection, which remains low.
Pre-ART hormonal treatment using GnRH analogues has not been clearly shown to improve live birth rates, though it may be beneficial for pain management or reducing endometrioma recurrence when ART is delayed. Likewise, hormonal suppression via combined contraceptive or progesterone-only pills does not enhance live birth rates in ART.
Surgical treatment may serve as an adjunct to ART in certain cases, particularly for pain relief or improved access to follicles prior to oocyte retrieval.
Stage I/II endometriosis: Routine surgery is not recommended for patients planning ART as it does not enhance ART pregnancy outcomes.
Ovarian endometriomas: Surgery should be avoided for endometriomas smaller than 4cm to preserve ovarian reserve. However, it may be offered for pain management or improved accessibility to follicles during oocyte aspiration.
Deep Infiltrating Endometriosis (DIE): Surgical intervention prior to ART should be based on pain severity and patient preference, as current evidence does not indicate reproductive outcome improvement, however studies are limited.
Fertility preservation options, such as oocyte freezing, should be considered in patients with ovarian endometriomas due to the potential impact on ovarian reserve. Recurrence of endometriomas that may necessitate repeat surgery could further compromise fertility, making fertility preservation a strategic consideration and one that should be discussed in detail with the patient to ensure they are aware of the pros and cons.
The treatment of endometriosisassociated infertility requires a tailored approach that balances surgical options, assisted reproductive techniques, and preservation strategies. Collaborative decision-making using tools like the Endometriosis Fertility Index allows clinicians and patients to consider all options in a way that best addresses both fertility and quality of life.
Author competing interests – nil

Peripheral vascular disease (PVD) refers to a range of symptoms usually resulting from atherosclerosis of arteries. In Australia it is estimated that 10% of patients in the primary care setting suffer from PVD and 20% of all patients over the age of 75 have arterial disease.
Progression from asymptomatic PVD lesions is low with some studies quoting an estimated 5% progressing to symptoms at five years to 21% symptomatic at one year.
Most patients with claudication have stable symptoms at five years (70-80%), while 10-20% develop worsening claudication and 5-10% develop critical limb ischemia (CLI).
The outcomes for patients with CLI remain poor with mortality rates of 25% and amputation rates of up to 30% at one year.
There is also a significant overlap with coronary and cerebrovascular disease, where the mortality rates in patients with PVD are between 13% and 50% at five years. There has traditionally been an underdiagnosis and undertreatment of cardiovascular disease in this group of patients.
The aims of management include decreasing the risk of cardiovascular morbidity and mortality, reducing claudication symptoms, improving quality of life and preventing disability. It includes lifestyle changes, medical therapy and select surgical management in patients with lifestyle limiting claudication and CLI.
Smoking Cessation: 50% of PVD is due to tobacco consumption.
Perth’s comprehensive vascular and vein treatment destination, with fully accredited integrated vascular ultrasound.


Smoking cessation doubles fiveyear survival improves claudication distance and reduces the risk of postoperative complications.
Antiplatelet agents: These reduce cardiovascular morbidity and mortality in patients with PVD.
Blood pressure control: Hypertension is associated with progression of atherosclerosis and increases rates of cardiovascular mortality.
Lipid lowering agents: Statins reduce major cardiovascular events and major limb adverse events in patients with PVD.
Glycaemic control: Good glycaemic control in patients with diabetes improves the long-term prognosis.
Exercise prescription: An exercise program can reduce symptoms of
All surgeons at Perth Reconstructive Urology – Dr James Chen, Dr David Sofield and Dr Mikhail Lozinskiy – have dual expertise in prostate cancer surgery and management of post-prostatectomy incontinence & erectile dysfunction. No matter where patients are on their journey, we are here to help.
We accept referral for all forms of urological conditions and offer rapid access for new patients and direct access cystoscopy with GP referral.

All surgeons consult at 4 Antony St, Palmyra 6157
Dr James Chen: reception@drjameschen.com.au
Dr David Sofield: reception@sofield.com.au
Dr Mikhail Lozinskiy: info@southwesturology.com.au
Dr James Chen also consults at SJOG Subiaco Sessional Suite at Level 2, 2 McCourt Street, West Leederville 6007
Phone number: (08)6363 5688 Fax: (08)9339 1832
Peripheral vascular disease is common
Most patients can be managed conservatively
There are revascularisation options for those with more severe disease.
claudication and increase walking distance. The recent 2024 European Vascular and Endovascular Surgery guidelines ‘recommend at least 150300 minutes a week of moderate intensity or 75-150 minutes of vigorous exercise a week to reduce all cause cardiovascular morbidity and mortality’.
Revascularisation is indicated in patients with severe lifestyle limiting claudication (IC) or critical limb ischaemia. Asymptomatic PVD patients do not need treatment, unless the aim of the intervention is to preserve patency of a procedure which has previously been performed (e.g. for in-stent stenosis).
Revascularisation decisions
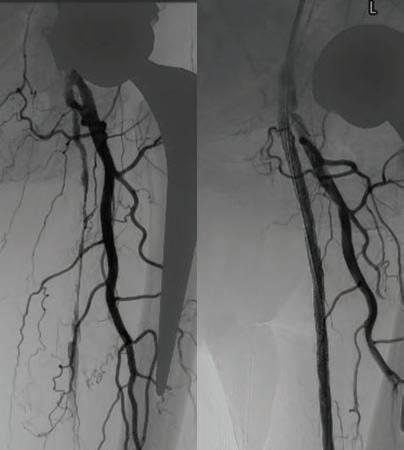
in patients with IC should be individualised as the majority treated conservatively have benign outcomes. Studies show that an early revascularisation procedure for IC increases the rate of subsequent reintervention, development of CLI and in some case limb loss. This is worse in patients who continue smoking.
The choice of surgical intervention depends on numerous factors including the patient’s age,
Heel pain is a frequent problem that presents to the general practitioner. Plantar fasciitis is the most common cause of under the heel pain. Most patients will improve with non-operative treatment but not all.
Surgery is a very effective form of treatment for this condition in patients with long standing refractory symptoms.
Before being considered for surgery patients should undergo at least six months of non-operative treatment that includes the following (in the appropriate order):
• Rest, avoidance of activity
• NSAIDs, stretching exercise program
• Orthotics: off the shelf or custom
• Cortisone injection (one only)
• Shockwave therapy

Surgery can be open or endoscopic. The principle part of the procedure is release of the plantar fascia near its origin on the heel. Historically only the medial half was released but recent literature supports more complete release.
comorbidity and the location and extent of arterial disease. Generally, endovascular surgery is used to treat shorter narrowing or occlusions and those in vessels below the knee. Multiple endovascular surgical techniques are now available to improve patency and go alongside angioplasty techniques such as drug-eluting balloons, stenting, atherectomy and lithotripsy to the vessel walls.
Endovascular techniques allow for treatment of large vessels through small incisions in the skin. Although not without risk, this technique can be done under local anaesthetic and sedation as a day case or overnight stay, reducing some of the risk from larger surgeries.
Open surgery, in the form of a bypass or endarterectomy, uses patients’ veins or prosthetic grafts to reconstitute blood flow. These operations are generally reserved for patients who can tolerate a bigger procedure under general anaesthetic and have longer and multiple level disease that may not be suitable for endovascular surgery.
By Mr Peter Ammon
continued on Page 48

Open surgery is performed through a 3cm incision in the proximal arch and allows not just plantar fascia release but also decompression of the tarsal tunnel and Baxters nerve which is often implicated in heel pain.
Endoscopic plantar fascia release is indicated for those without nerve compression symptoms and is done through a much smaller incision using a camera assisted cutting device much like a carpal tunnel release.
Both open and endoscopic releases are performed as day cases and require approximately two weeks on crutches. Recovery is slightly quicker for endoscopic patients as you would expect. Patients can expect an 8090% chance of a good result from surgery. Complications are rare.


St John of God Medical Centre
Suite 10, 100 Murdoch Drive, Murdoch WA 6150
Telephone: (08) 6332 6300 Facsimile: (08) 6332 6301
www.murdochorthopaedic.com.au
By Dr Dan Marshall, Orthopaedic Surgeon, Murdoch
Previously I have written about causes and investigations for foot pain Once the underlying cause of foot pain is diagnosed, the appropriate treatment plan can be developed. The mainstay of most foot pathologies is non-operative measures.
Reducing or modifying activities that exacerbate the pain is often the first step in managing foot pain. Rest allows tissues to heal, reducing inflammation and preventing further damage.
Applying ice to the painful area can help reduce inflammation and numb the pain. Heat therapy, on the other hand, can help relax muscles and improve blood flow. Alternating between ice and heat therapy can provide relief for certain conditions such as plantar fasciitis and tendonitis.
Nonsteroidal anti-inflammatory drugs (NSAIDs) can help alleviate pain and reduce inflammation. Along with regular paracetamol, these medications are particularly useful for managing mild to moderate pain caused by conditions such as arthritis, tendonitis or minor injuries.
Orthotics, such as shoe inserts or custom-made orthotics, can provide support, improve foot alignment and relieve pressure on certain areas of the foot. They can be beneficial for conditions such as mild pes planus,


mild cavus, plantar fasciitis and metatarsalgia. Commonly we see patients that have spent thousands of dollars on orthotics that have never worked. If they haven’t worked for the patient, they likely never will, so refer them to see an orthopaedic foot and ankle surgeon.
Physiotherapy involves exercises and stretches designed to improve strength, flexibility and range of motion in the foot and ankle. A physiotherapist can help develop a personalised treatment plan to address specific issues such as plantar fasciitis, Achilles tendonitis or stress fractures.
For persistent pain, corticosteroid injections may help reduce inflammation and provide temporary relief for conditions such as arthritis or bursitis. However, they are generally not a long-term solution and should be used with caution due
continued from Page 47
Both endovascular and open surgery rely on patients adhering to best medical therapy as described above as well as complying with a surveillance program of stents and bypasses allowing early intervention on any stenosis that may occur. There is an immediate risk of post procedural restenosis and re-
thrombosis of peripheral arteries which persists despite single antiplatelet and statin therapy. Recent trials have demonstrated that low-dose rivaroxaban with aspirin reduces the risk of acute limb ischaemia, major amputation, MI, ischaemic stroke and cardiovascular death in post-operative patients.
Ongoing smoking postrevascularisation increases the risk
to potential side effects and damage to tendons and fascia.
I would caution the prescribing of corticosteroid injections for conditions such as plantar fasciitis and Achilles tendinopathy. For diagnostic purposes of a patient with generalised foot pain, an image guided injection of local anaesthetic may be recommended to an area of interest and potential surgical target.
Surgery is the last resort when other treatments have failed to provide pain relief. Surgical options vary depending on the cause of foot pain. Recovery from foot surgery can also differ, so the decision to undergo surgery should be made in consultation with an orthopaedic foot and ankle surgeon.
Preventing foot pain is often easier than treating it. Here are some
of graft/stent failure threefold as well as delaying wound healing post revascularisation.
– References on request
Author competing interests – nil
Treatment follows accurate diagnosis and is mainly nonoperative
Prevention is easier than cure and there are a number of approaches
Surgical review/intervention may be needed in severe or persistent pain.
practical tips for your patients to help maintain foot health and prevent pain:
Choosing the appropriate shoes is crucial for preventing foot pain. Good shoes provide adequate arch support, cushioning, a rocker-type bottom and a proper fit. Avoid high heels and shoes with narrow toe boxes, as they can contribute to conditions like bunions and neuromas. Replace worn-out shoes regularly to ensure optimal support.
Excess body weight puts additional stress on the feet. Maintaining a healthy weight through a balanced diet and regular exercise can help reduce this excessive load and prevent conditions such as plantar
fasciitis and arthritis. This is one of the most significant modifiable conditions that drastically improve foot pain.
If your patients have chronic medical conditions such as diabetes, arthritis or peripheral vascular disease, work closely with them to manage these conditions effectively.
Incorporate foot stretches, calf stretches and lower limb strengthening exercises into a daily routine to improve flexibility, support, and balance. Exercises such as toe curls, calf raises and ankle rotations can help maintain foot health and prevent injuries.
Proper foot hygiene including washing and drying feet thoroughly, can prevent fungal infections such as athlete's foot, which can cause discomfort and pain. Regularly trimming of toenails can also help prevent painful conditions such as ingrown toenails. This is especially important for the neuropathic feet and patients with diabetes.
When a patient is starting a new exercise regimen or increasing physical activity, urge them to do it gradually to allow the lower limb muscles and feet to adjust.
Avoid sudden increases in intensity or duration, as these can lead to overuse injuries such as stress fractures and tendonitis.
Regularly inspect the feet for signs of injury, swelling, redness or deformities. Early detection of foot problems can prevent deterioration, which is particularly important for individuals with diabetes or neuropathy who may not feel pain or notice injuries.
While many cases of foot pain can be managed with self-care measures, some situations require specialist attention. Referral may be indicated if your patients experience severe pain that does not improve with rest or over-the-counter pain relievers, persistent swelling in the foot, difficulty walking or bearing weight on the affected foot or pain that is affecting their quality of life and activities of daily living
Associated symptoms such as fever, wounds, acute onset of pain and swelling that may indicate an infection or septic joint, requires referral to an emergency department with orthopaedic cover.
Author competing interests – nil




By Dr Reza Feizerfan, Pain Specialist, Nedlands/Murdoch
The Australian Institute of Health and Welfare (AIHW) has quoted the prevalence of chronic pain to be 20% between the ages of 65-74, increasing to 24% in those 85 and over. With an aging population, managing chronic pain in older adults has become an increasingly important area of healthcare, albeit with its challenges.
Assessing pain, a subjective experience, can be particularly challenging in older adult patients. They may struggle to describe the pain accurately or pinpoint its exact location, and often find it difficult to distinguish between different types of pain, such as musculoskeletal and neuropathic.
Some may underreport their discomfort, either because they believe pain is an inevitable part of ageing, don't want to be seen as a burden, or worry it may signal a more serious condition.
Communication about their symptoms may be further complicated by cognitive impairments such as dementia or the side effects of medications. This makes it essential to use modified pain assessment tools such as PAINAD or PACSLAC, and to account for sensory impairments such as vision or hearing loss, which can also hinder effective communication.
It’s important to allocate additional time to gather collateral information from healthcare providers, family members or medical records. In many cases, functional assessments can provide valuable insights. Observing patients' body language and movement while they perform activities that mimic their daily routine, combined with targeted physical examinations, can offer a more comprehensive understanding of their pain.
Comorbidities and polypharmacy
It is estimated that 28% of older adults have three or more chronic conditions, which complicates


pain management in this population. Chronic conditions such as diabetes, osteoarthritis, osteoporosis, cancer, and the aftereffects of surgeries or injuries can each contribute to distinct types of pain.
For example, diabetes may lead to peripheral neuropathic pain, while an acute exacerbation of chronic obstructive pulmonary disease (COPD) with persistent coughing can cause rib cage pain. Similarly, vitamin D deficiency may result in widespread musculoskeletal discomfort.
The presence of multiple comorbidities often leads to an extensive list of medications, further complicating the choice of analgesics due to potential drug interactions and side effects. In some cases, the medications themselves can cause or exacerbate pain.
For instance, statins are known to cause myofascial pain, and certain osteoporosis treatments can result in long bone pain. These factors make it crucial to carefully consider both the patient's overall medical condition and the potential
Pain assessment can be complex and challenging in older adults
Effective pain management begins with a thorough assessment, aimed at identifying all potential biomedical sources of pain
Consideration should be given to assess social and psychological factors that may influence pain perception and impact.
effects of their medications when managing pain.
Assessing, investigating and managing acute and chronic pain can be very different to each other. It is worth noting that the majority of acute exacerbations of chronic pain resolve without a major intervention. However, distinguishing between acute and chronic pain can be challenging in the older age group.
It is often the case that potential
pain generators in this age group are multifactorial. For example, a mechanical fall causing muscular pain, leading to a period of reduced activity and rest which further complicating muscle deconditioning and musculoskeletal pain.
Inactivity worsens their underlying lumbar spine arthritis, and the presentation may become complex. Or in the case of a chronic lower back pain where potential pain generator can be from multiple sources, each necessitating a different approach and treatment.
In some cases, what appears to be an acute pain episode may actually be a manifestation of poorly managed chronic pain.
It is crucial to recognise the influence of psychological and social factors on pain in older adults. Depression, anxiety, social isolation and the fear of becoming dependent can significantly affect how this population experience and report pain. Pain-related functional decline often leads to reduced
social interactions, increasing the risk of depression, while untreated depression can, in turn, intensify the perception of pain.
Older patients may also be hesitant to seek help or medical care, often due to limited social support, a desire not to burden their families, or concerns about appearing dependent and potentially losing their independence. These dynamics highlight the need for a multidisciplinary approach to pain management.
Involving general practitioners, allied health professionals, and other specialists is essential to the provision of comprehensive care that addresses both the physical and psychosocial aspects of pain in this age group.
– References available on request
Author Competing interests - nil


Mondo Nougat might be celebrating 25 years in the Swan Valley next year, but the simplicity of great ingredients, an old traditional recipe and family remain at the heart of this local company.
By Ara Jansen
As a young boy, Andrea Romeo always knew Christmas was around the corner when the nougat appeared. Coming from an Italian family, it was traditionally what his family made as the festive season neared.
“My dad Alfonso and his brothers had a patisserie, and everyone would be wrapping the pieces by hand,” remembers Andrea. “We would stand around this big table and it was all hands on deck.”
After migrating to Perth from Italy when he was seven, Andrea’s parents opened a patisserie in Midland in the 1990s. The store was next door to Mondo Meats, owned by Andrea’s uncle Vince Garreffa, so they became Mondo Patisserie. In 1999 they moved to Morley, but eventually ran out of room, which is how Mondo Nougat (choosing the English world over the Italian, torrone) finally settled in the Swan Valley.
Next year, in 2025, Mondo celebrates 25 years at that location.
By the late 1990s, Mondo’s customers started asking for nougat after Christmas, which led to the traditional honey-based sweet being made year-round – and the start of a sweet empire.
“We’ve been able to share an experience with people that’s true to our roots and family traditions,” says Andrea proudly.
The eldest of this generation of Romeo brothers, Andrea is Mondo’s general manager and his two brothers are also directors as well as helming the café –Marco is a barista and Simone a pastry chef.
The two-hectare Swan Valey property gives Mondo space to manufacture as well as a way to welcome visitors to watch nougat being made, for tastings and to enjoy the café, which serves cakes and pastries also using traditional family recipes.
Andrea is adamant that the group uses as many local ingredients as it can – honey is sourced five minutes down the road, macadamias come from a grower in Baldivis and hopefully within three years, WAgrown almonds will be available to them.
“That’s something we are committed to – we start sourcing locally and then go nationally. We’re a local business and we want to support other local businesses.”
All three Romeo brother grew up in the business and Andrea says he never considered doing anything else. When it came time to start looking at careers, he looked around the business for skills it needed and chose marketing and commercial law.
Two of his favourite jobs are designing Mondo’s packaging and product development. That means experimenting and discovering what interesting tastes he can bring to a basic nougat. Whether it’s using bush food, finding pandan or something interesting in an Indian grocery store, Andrea is always thinking of how he can combine ingredients to make a delicious new nougat.
The latest flavour has been granola bites, in partnership with Meredin’s Merre Granola.
“I love being able to collaborate with other local companies. The great thing about it is we can

Win a hamper of WA-made nougat
Mondo Nougat has been making some of Australia’s most-awarded nougat using the finest local ingredients at its factory, café and retail outlet in the Swan Valley since 2005. Mondo Nougat was originally produced only at Christmas, as a sideline to the Romeo family’s patisserie business that dates back to 1989, but demand for the traditional honey-based nougat saw production become year-round in 1997.
Medical Forum readers have the chance to enjoy a taste of la dolce vita just in time for the festive season, with the chance to win one of five All Star Hampers. Each hamper comprises a 500g Assorted Original Nougat Bites, a 225g All Star Selection Gift Pack, and a 150g Bambino Gift Tin, packaged inside a stylish and practical Mondo Nougat cooler bag.
To enter, use the QR code on this page or go to mforum.com.au and hit the competitions tab.
experiment with small batches. We can make 80kg and see what happens. I get so much joy out of this.”
A basic nougat is made from egg, honey and sugar. Mondo has 17 regular different flavours. While his favourites tend to change fairly often, Andrea is rather dedicated to roast hazelnut nougat and a classically traditional lemon.

Andrea estimates over the years they have tried about 100 different nougat combinations and flavours. Some only stay for a little while but others have endured and remain favourites. Around Christmas these include soft nougat flavours almond and honey, cranberry and almond, salted caramel and coffee. Other favourites include pistachio nuts, cherries and chocolate covered hard nougat.
“I’d love to think we have played a part in bringing nougat to Australia and to the world, as people have taken our product home. If more people can experience nougat for the first time and it’s a good experience, then that’s good for nougat. It’s one of the oldest confections in the world and we want to continue to grow its popularity.”

Danny McCubbin’s dream cheap house in Sicily led to a social enterprise project which has brought new life to a town in bad shape.
By Ara Jansen
When Danny McCubbin decided to buy a home for one euro in a dying town in Italy, he couldn’t have dreamed what would come from it.
Originally from the Gold Coast, Danny had been living in the UK and working with celebrity chef Jamie Oliver in his Fifteen restaurant and as culture manager for many years.
Danny decided it was time for a change, so he took up the one-euro home offer with the idea that he would turn it into a community space. Through a series of twists and turns he made it to Italy in 2020, landing in Mussomeli, a remote town in the middle of Sicily, population 10,000. He didn’t know a soul, couldn’t speak the language and had no job.
He went up to the attic of the house he had bought and discovered boxes of cooking equipment, beautiful wooden chopping blocks and handsewn shopping bags. People started stopping by to ask him who he was and what he was doing – and they were so kind in offering help.
Danny walked everywhere and got to know the town. As a connector and natural social enterprise builder, often using food as his vehicle, it wasn’t long before Danny’s brain was whirring with ideas.
Once again, through a series of twists and good turns, Danny found a kitchen space to rent and started his new social enterprise: The Good Kitchen. It started as a meals-onwheels for anyone who needed it in the economically depleted town and offered meals for the elderly or those who were alone. They received donated fresh food and dry goods from local supermarkets. People young and old began to volunteer. With a lot of work, it became a hub for local activities. Kids cooking classes started with kids from a local orphanage, which drew the local nonnas out of their homes to pass on traditional recipes and forge new inter-generational relationships.
Saturday is English lessons. Sunday is a long table lunch stretching out into the square and welcoming anyone to join the meal, even tourists passing through. The kitchen sends meals to five Ukrainian refugee families who speak no Italian and have little. Danny also welcomed a young man to do six months community service to work in the kitchen who proved to be one of his best volunteers.
Danny started documenting the journey on a blog, which five years on led to his first book, The Good Kitchen – Love and connection through food. The book is a mix of Danny’s journey plus vegetarian recipes which they serve in the kitchen, using simple, everyday
ingredients. There are also recipes if you find yourself needing to cook for a large group of people and information on how to swap out ingredients if you don’t have everything. Danny’s celery leaf pesto is a favourite, made when getting creative.
Danny turns 60 this month and has now moved out of town to a new home. The property has olive trees on it and Danny has been making his own oil. A local friend brings his goat herd around to mow the grass and the goat milk goes to his sister to make cheese, which Danny buys. A gloriously simple circular economy, which Danny loves.
He continues to donate his time to The Good Kitchen three days a week and is all monies from the book go to the kitchen. Danny’s goal is to make sure the enterprise is sustainable for many years to come and create work opportunities for locals.


Ingrid (Julianne Moore) and Martha (Tilda Swinton) were close friends in their youth, when they worked together at the same magazine. Ingrid went on to become an autofiction novelist while Martha became a war reporter. Eventually, they were separated by the circumstances of life. After years of being out of touch, they meet again in an extreme but strangely sweet situation.
Based on the novel What Are you Going Through by Sigrid Nunez, The Room Next Door opens in cinemas on Boxing Day.
Courtesy of Sony Pictures, we have 12 double in-season passes to give away.
To enter, use the QR code on this page or go to mforum.com.au and hit the competitions tab.
This page intentionally left blank


NEDLANDS
Rare Large Medical Suite on Hollywood Campus
•Huge 96sqm* medical suite
•Generous waiting and reception area
•2 huge consulting rooms
•Fully Fitted & Furnished Suite
•1 car bay on title
•Ready for occupation
•Central location within the specialist centre
•Modern fit out
•Exclusive basement storage area
Asking Price $984,000+ GST
Asking Rent $450/sqm + Outgoings
+ GST
Luke Randazzo 0417 181 309 lrandazzo@brwa.com.au
Rob Selid 0412 198 294 rselid@brwa.com.au

WEMBLEY
2 rooms available for lease
Consulting room 15m2
Consult/treatment room 23m2
(has sink, can be sub-divided)
Within Suite 2, 178 Cambridge Street, Ground floor
Undercover car bays available for staff parking
Opposite St John of God Hospital Subiaco
Radiology and pathology in same building
Physiotherapy available on site
Great patient parking
600m walk from Subiaco train station
Sessional basis considered
Specific fit-out requirements to be discussed
Admin support requirements can be discussed
·Suite facilities include new reception/ waiting room, kitchenette/break room, treatment rooms
For more details or to view, contact Johan on 6166 3751 or jm@thebonejoint.com.au
Hollywood Medical Centre Suite 36, First Floor, 85 Monash Avenue, Nedlands
87sq m – fully fitted, large reception, 2 consulting, 2 treatment & 2 store rooms.
Contact: Irene 0409 688 339

Unlock the potential of this exceptional property.
Dr’s Surgery consists of:
•Large reception area
•2 x large waiting areas
•Staff room with kitchenette
•Large lockable records room
• Female/male/disabled toilets
•5 x Doctors Rooms
(potential 2 extra rooms from Pathology)
•Treatment room
Pathology configuration
•Separate entrance
•Small waiting room
•Reception room
•3 x consulting room (2 rooms could be Doctors Rooms)
•1 x toilet
Ample parking with approx. 40 car bays.
Asking price: $95,000 + GST + Outgoings
Contact Chantelle Mammoliti at Growth
Realty on 0413 138 847 or chantelle@growthrealty.com.au


NEDLANDS / BENTLEY / MANDURAH / GERALDTON
Consult rooms available for sessional rental – suitable for specialists or allied health
4 strategic locations in Nedlands, Bentley, Mandurah and Geraldton
•Nedlands – Hollywood Specialist Centre, suite 23, 95 Monash Ave
•Bentley – unit 3, 10 Mills St
•Mandurah – unit 7, 21 Sholl St
•Geraldton – 9 Urch St, Beresford
For more info, contact practicemanager@apollocardiology.com.au or 6166 3737
Website link https://apollocardiology.com.au

Lot 3 / 140 Mounts Bay Road, PERTH Mount Medical Centre - RARE OPPORTUNITY
MMJ Real Estate (WA) are pleased to present to market this rare opportunity to buy this 76sqm medical consulting suite located on the third floor within the Mount Medical Centre.
Key Features:
•Strata area of 76sqm
•Fully fitted with reception, meeting room and main consulting room
•Small storage area
•Kitchenette
•Corner position with good natural light
•Views towards Kings Park
•2 secure undercover car parking bays
This unit is situated within a prime location adjacent to the Mount Private Hospital one of Western Australia’s leading private providers of Cardiology and Cardiac Surgery.
For more details or to inspect contact Tom Prout on 0434 746 259 or tom.prout@mmj.com.au

Medical Rooms Available for Specialists and Allied Health
Lakes Shopping Centre, Shop 2, 620 Northlake Rd, South Lake WA 6164
•Available for ALL Specialists and allied health professionals. Opportunity to become a part of the GP clinic / support.
•Consulting rooms, reception/waiting area, kitchen/breakout area, store records room, and other zones.
•These consulting suites are situated on the ground floor of the medical practice.
•Pathology on site (Clinipath)
•Room Sizes:
– Room 3: 3.5 x 3.4 meters = 12 Sq m
– Room 4: 4 x 3.2 meters = 12.8 Sq m
– Room 5: 4 x 3.2 meters = 12.8 Sq m
•Rent hourly and full time available.
•Rent negotiable.
For Further details and enquiries please contact p.manager@southlakefamilypractice.com.au or 08 9417 1009

Queens Road Surgery is a busy GP owned general practice located in Mount Pleasant.
We are looking for a VR GP to join our well established practice.
We offer a supportive team based culture, experienced administrative staff and quality full time nursing support.
Queens Road Surgery is a fully equipped accredited practice.
For a confidential discussion please contact our Practice Manager Narelle 0412 113 584 or narelle@queensroadsurgery.com.au

Doctor Opportunity at The Woods Medical Centre
Join our dynamic team at The Woods Medical Centre!
We are seeking a passionate and experienced GP to join our growing practice. The ideal candidate will have a strong interest in skin cancer management and be skilled in performing skin procedures.
Key Responsibilities:
•Provide comprehensive general practice services
•Perform skin cancer checks and biopsies
•Conduct minor surgical procedures
•Manage chronic diseases effectively
•Collaborate with a supportive team of healthcare professionals
Essential Requirements:
•FRACGP qualification
•Vocational Registered
•AHPRA registration
•Proven experience in skin cancer management and minor procedures
•Strong interpersonal and communication skills
•Ability to work independently and as part of a team
What we offer:
•Competitive remuneration package
•Supportive and friendly work environment
•Modern facilities and equipment
•Mentorship to develop skin cancer management skills
•Opportunity to work alongside experienced practitioners
•Ongoing professional development opportunities
Contact Bryan, classifieds@mforum.com.au or phone 9203 5222 to place your classified advert
Mature-aged Male Australian born & Australian Trained G.P. seeking full time work in Perth inner city Eastern suburbs. Strengths include holistic care, computer literacy, and attention to detail. Sees 4 patients per hour. English and Yugoslav speaking. Email gp@qld.red
If you are a dedicated and enthusiastic GP who is passionate about providing high-quality patient care, we encourage you to apply.
For more information or a confidential chat, please call 0478 021 910 or email practicemanager@thewoodsmedical.com.au for more information.







At Humphrey Homes, we design and build every home to award-winning standards. And often, like this City Beach residence, they take home actual awards too. The judge we really care about however, is you. We want you to be delighted, from concept to completion. By integrating architecture, interior design and construction, we make the process stress-free and seamless; our model ensures you achieve your vision on time and on budget. To bring your forever home to life, contact Dean Humphrey for an informal chat


















