






















AI-powered scribes that capture consultations in real-time are already in use. Elsewhere, there is promising work underway using AI as a tool for diagnostic support in rural and remote areas.
Andrea Downey | Managing Editor
Have you used Google Maps to plan your fastest route, asked Siri to find a healthy recipe for dinner, or asked Alexa to play your favourite songs?
Most of us use it every day, whether we realise it or not, but when artificial intelligence gets mentioned in healthcare it causes a few nerves.
There are understandably very real concerns about using AI in the medical sector. You are handling sensitive patient data, and the expertise and compassion of a doctor can never be replaced by a machine.
Yet technology offers a way to ease the administrative burden on doctors and improve access to care. AI-powered scribes that capture consultations in real-time are already in use.
Elsewhere, there is promising work underway using AI as a tool for diagnostic support in rural and remote areas.
Like it or not, technology is having a tangible impact on healthcare and doctors need to be at the forefront of shaping what that looks like rather than reacting after the train has left the station.
While I appreciate the benefits AI has to offer, I can also sympathise with doctors’ concerns about the impact it will have in medicine.
I have seen the use of AI play out quite disastrously in the media and will shout from the rooftops that it will never replace a trained journalist.
Do I use AI? Yes, I find it very useful for scanning lengthy government reports and transcribing interviews.
Will I use it for writing and editing? Never.
SYNDICATION AND REPRODUCTION Contributors should be aware the publisher asserts the right to syndicate material appearing in Medical Forum on the mforum.com.au website. Contributors who wish to reproduce any material as it appears in Medical Forum must contact the publisher for copyright permission.
DISCLAIMER Medical Forum is published by Medforum Pty Ltd (Publisher) as an independent publication for health professionals in Western Australia. Neither the Publisher nor its personnel are medical practitioners, and do not give medical advice, treatment, cures or diagnoses. Nothing in Medical Forum is intended to be medical advice or a substitute for consulting a medical practitioner. You should seek immediate medical attention if you believe you may be suffering from a medical condition. The support of all advertisers, sponsors and contributors is welcome. To the maximum extent permitted by law, neither the Publisher nor any of its personnel will have any liability for the information or advice contained in Medical Forum. The statements or opinions expressed in the magazine reflect the views of the authors and do not represent the opinions, views or policies of Medical Forum or the Publisher. Readers should independently verify information or advice. Publication of an advertisement or clinical column does not imply endorsement by the Publisher or its contributors for the promoted product, service or treatment.
Advertisers are responsible for ensuring that advertisements comply with Commonwealth, State and Territory laws. It is the responsibility of the advertiser to ensure that advertisements comply with the Competition and Consumer Act 2010 (Cth) as amended. All advertisements are accepted for publication on the condition that the advertiser indemnifies the Publisher and its personnel against all actions, suits, claims, loss or damages resulting from anything published on behalf of the advertiser.
EDITORIAL POLICY This publication protects and maintains its editorial independence from all sponsors or advertisers. Medical Forum has no professional involvement with advertisers other than as publisher of promotional material. Medical Forum cannot and does not endorse any products.

FEATURES
10 Q&A with Dr Kiran Puttappa
14 AI – making healthcare smarter
20 Close-up: Dr Jacinta Vu



26 Setting the standard on pain management
LIFESTYLE
50 What’s up, Doc? Meet the voice behind the Looney Tunes
52 Car review: A different kind of turbocharge
54 French Film Festival

Our recent competitions have seen Medical Forum readers enjoy a trip to the movies, a night out at the ballet and a well-deserved glass of Fermoy’s delicious wine.
This month we’re giving you the chance to win more movie tickets with double passes to the new Looney Tunes film The Day The Earth Blew Up, more details on page 51.
Or if you’re looking for a bit more rev in your engine, check out what our car reviewer
Dr Mike Civil has to say about the new iX1 BMW electric vehicle on page 52.
Enter our competitions by using the QR code or go to www.mforum.com.au and hit the competitions tab.
PUBLISHERS
Alice Miles – Director Fonda Grapsas – Director Tony Jones – Director tonyj@mforum.com.au
EDITORIAL TEAM
Managing Editor
Andrea Downey 0437 909 904 andrea@mforum.com.au
Production Editor
Jan Hallam 08 9203 5222 jan@mforum.com.au
Clinical Editor
Dr Joe Kosterich 0417 998 697 joe@mforum.com.au
Graphic Design Ryan Minchin ryan@mforum.com.au
ADVERTISING
Advertising Manager
Bryan Pettit 0439 866 336 bryan@mforum.com.au
Classifieds Manager
Paul Riessen 08 9203 5222 paul@mforum.com.au
Clinical Services Directory
Alice Miles 08 9203 5222 alice@mforum.com.au
CONTACT MEDICAL FORUM
Suite 3/8 Howlett Street, North Perth WA 6006
Phone: 08 9203 5222 Fax: 08 6154 6488 Email: info@mforum.com.au www.mforum.com.au















Two million bone transplants are performed globally each year, but research published in BMC Medicine found even though biomaterials science, tissue engineering and regenerative medicine has taken enormous leaps in the creation of new medical innovations, uptake into clinical practice is lagging.
Researchers asked 337 surgeons and 99 scientists for their opinions on medical innovations. Scientists were more optimistic than surgeons regarding the future replacement of autologous bone grafts with advanced biomaterials or tissue-engineered products.
Professor Dietmar Hutmacher, Director of the Centre of Regenerative Medicine and Director of the Max Planck Queensland Centre for the Materials Science of Extracellular Matrices at QUT, said the surge in scientific knowledge over the past 20 years has not been matched by an increase in clinical implementation that directly benefits patient care.
“Simultaneously, they [scientists] expressed the need for a more significant focus on clinical relevance
One in three West Australian toddlers is iron deficient, according to new research from the ORIGINS study.
Head of Paediatrics at Joondalup Health Campus Dr Jamie Tan said the findings were concerning, adding that low iron was potentially detrimental at a critical stage of life and development.
“If an adult has low iron, we know they can experience things like fatigue, headache and shortness of breath,” Dr Tan said.
“In children, the symptoms are the same but are exacerbated by the fact they are occurring at a developmentally significant time in their lives.
“Children as young as 12 months may present with symptoms like poor sleep, lethargy and grumpiness during the day and becoming what we commonly call a fussy eater.”
ORIGINS is the largest longitudinal birth study of its kind in Australia, using data from 10,000 babies born at Joondalup Health Campus and conducted in partnership with The Kids Research Institute Australia.
Work is now underway to find out

in preclinical studies and regulatory clarity around 3D-printed bone scaffolds,” he said.
“All the participants agreed that witnessing the technology in action was deemed most influential in adopting new bone regeneration methods in a surgical setting.”
QUT author Dr Stephen Whyte said the study's outcomes highlighted the urgent need for interdisciplinary collaboration between surgeons and scientists.
He added that aligning clinical needs, research outcomes and regulatory framework was critical for showing efficacy and efficiency in bone defect treatment.
why iron deficiency is so prevalent among toddlers and to help find solutions.
One area of focus is the possible links between iron deficiency and childhood anxiety and neurodevelopmental conditions, including ADHD.
“That means looking at nutrition and how parents can improve small things on a day-to-day basis that don’t cost a lot of money, but may have a big impact,” Dr Tan said.
An Australian first biobank to support research into gene therapies that could permanently cure certain types of hearing loss will be based in WA.
The Aussie Ear Bank is expected to be operational by the end of 2025 at the QEII Medical Centre in Nedlands.
The biobank, run by Ear Science Institute Australia, will store tissue related to genetic-associated hearing loss with the goal of advancing personalised care and new treatments, including a cure for genetic hearing loss.
Ear Science founder and WA surgeon
Professor Marcus Atlas said traditional causes of hearing loss, noise and age, were not the complete picture.
“The emerging research around the world and particularly at Ear Science is that genetics is the big new factor in middle age and older people’s hearing loss,” he said.
“This is not what we thought before and it is a game-changing finding because it (hearing loss) is potentially treatable.”
Ear Science and collaborators will work to address the many causes of genetic-associated hearing loss and hold clinical trials in WA, nationally and internationally.
Head of implant innovation Dr Christo Bester said pioneering gene therapy offered hope for restoring hearing in patients with genetic hearing loss.
“Our breakthrough therapeutics are only possible through a unique collaboration within our biobank, which connects clinicians and community members with cutting-edge diagnostic tools and genetic analysis to pinpoint viable treatments.”
The Photon Counting CT machine at ChestRad requires ten times less radiation dose for lung cancer screening
1 Heismann, B Photon counting CT versus energy-integrating CT: A comparative evaluation Med Physics Dec 2024
Finding - Siemens Naeotom Alpha PCCT ten times more dose efficient for LCS than Siemens Definition Force
2 American Association of Physicists in Medicine Lung Cancer Screening CT Protocols V 6 0 November 2023 Siemens Definition Force four times more dose efficient for LCS than the next best CT machine
Finding -


Professor Catherine Elliott is the new CEO of Rural Health West. She joins following her tenure as Deputy Executive Director and Director of Research at The Kids Research Institute Australia.
Professor Rebecca Anglin has been appointed Dean of the National School of Medicine at the University of Notre Dame Australia. She is currently Dean of the Global MD Program at UWA.
Nominations open for the 2025 Jeannie Ferris Award: Honouring champions of equitable cancer care. The deadline for submissions is 5pm (AEST) Friday, 11 April.
The State Government has confirmed construction on the new Women and Babies Hospital will begin this year.

Ahpra has appointed Justin Untersteiner as its new chief executive. He joins in April and was most recently COO at the Australian Financial Complaints Authority.
Mental Health Australia Board has appointed Dr Peggy Brown as its new Chair. Dr Brown was Commissioner for the Royal Commission into Defence and Veteran Suicide.
Perron Institute and UWA’s Dr Stuart Hodgetts has been awarded $1m from the NHMRC to further his research on red and near-infrared light therapy for spinal cord repair using implanted devices.
Bunbury resident Lynda Whitton has been awarded the 2024 John Studdy Award, MS Australia’s highest honour. Lynda was President of the MSWA Bunbury Outreach Group for 20 years and served as a MS Australia National Advocate for 13 years.
continued from Page 4
Australia’s medical colleges have launched an unprecedented expansion of specialist training in regional, rural, and remote areas, according to the Council of Presidents of Medical Colleges.
The RACGP has filled all rural training positions for 2025, with new data showing 585 GPs will begin rural specialist training in 2025, part of a broader intake of 1,506 junior doctors into specialist programs – a 20% increase from last year.
The Australian and New Zealand College of Anaesthetists has awarded 343 rural generalist certificates as part of its regional workforce strategy.
Meanwhile, the Australian College of Rural and Remote Medicine has reported that 80% of their graduates now practice in rural areas, and other colleges, including those for ophthalmologists and medical administrators, now mandate rural placements lasting six to 12 months.
Associate Professor Sanjay Jeganathan, Chair of the CPMC said regional and rural communities
deserve the same access to care as those who reside in cities.
“We're building lasting change by training specialists who understand regional communities and are more likely to stay long-term,” he said.
“We're seeing real results from our colleges' commitment to rural training.”
Federal Government estimates suggest Australia could face a shortage of 5,000 doctors by 2030.
The CPMC said while overseastrained specialists help fill immediate gaps, medical colleges are prioritising sustainable solutions through local training programs.
The first clinical consensus for managing multiple sclerosis in Australia and New Zealand has been released.
The consensus aims to help health professionals navigate the everchanging treatment landscape and new therapies.
Published in the Medical Journal of Australia, it encompasses pre-
A Perth medtech company that developed a device to help doctors draw blood in patients afraid of needles is set to expand into the US market.
VeinTech is aimed at addressing ‘needlephobia’ in patients and helping doctors avoid needle stick misses by identifying the most suitable veins for cannulation.
The company was awarded a $1.74m Federal Government grant 12 months ago to prepare the device to be marketed and commercialised. It also received a $500,000 grant in 2022 from the WA Government’s Future Health Research and Innovation Fund.

The device uses ultrasound-based technology to guide the clinician to deeper, hard-to-locate veins via a screen display.
VeinTech co-founder Nikhilesh Bappoo said despite being one of the most common procedures in healthcare settings, the failure rate for first-go IV insertion was 40%.
“High failure rates, plus the growing fear of needles during the COVID pandemic have seen a trend toward overall healthcare avoidance,” he said. “In some cases, this can be hugely problematic both for the individual and the health system which feels the impacts in the long-term.”
High failure rates for cannulation are reflected around the globe, and VeinTech has now partnered with the New England Medical Innovation Center as it prepares to enter the US market.
Automate all of your clinical documentation.
Lyrebird listens to your conversations with patients, writes down what’s said, and creates all the notes and paperwork you need.
Lyrebird Health strikes the right balance between efficiency, security and patient-centered care. I highly recommend it to fellow practitioners.
– DR SEAN STEVENS
Chair Digital Health and Innovation Specific Interest Group Royal Australian College of General Practitioners, Owner @ Grove Medical
Partnering with the best We’re dedicated to delivering seamless integrations that enhance your practice’s efficiency and elevate the capabilities of your software.



A leading neurologist and palliative care researcher were among the more than 70 West Australians who received Australia Day Honours.

Professor Graeme Hankey AO received the Officer of the Order of Australia for “distinguished service to medicine as a neurologist and stroke physician”, and Professor Samar Aoun AM was appointed a Member of the Order of Australia for her “significant service to community health through palliative care and aged care research”.
Professor Hankey, Perron Institute Chair in Stroke Research at the University of Western Australia, has been involved in epidemiological studies and clinical trials of treatment strategies for acute stroke and stroke prevention.
He said the honour was a tribute to the help and support he had received from teachers, colleagues, students, patients, and loved ones in his endeavours to be an effective clinical neurologist, researcher and teacher.
“Helping patients and families negotiate and minimise the impact of their illness helps to inspire, teach, train and mentor the next generation of doctors, nurses, allied health professionals and clinician scientists,” he said.
Professor Aoun, Perron Institute Research Chair in Palliative Care at UWA, said the honour was a great vehicle to keep spreading the message of “compassion in life and death”.
“Thanks to the many colleagues who were part of this journey and who shared and supported this vision,

whether in palliative care, compassionate communities, aged care and MND care,” she said.
“In palliative care, it is important to have the community as an equal partner with clinicians in delivering that care, so it is more sustainable and affordable.”
The pair received their honours alongside former WA Deputy Premier and GP Dr Kim Hames AM, who was appointed a Member of the Order of Australia for his “significant service to the Parliament of Western Australia, to medicine, and to the community”.
Mr Hames, who was WA’s Minister for Health from 20082016, said: “You do a lot of things in government and in work and don’t expect to get any recognition for it, but when you do…I’m really grateful and very happy.”
Read more about the WA medical professionals who received honours at: mforum.com.au/Australia-day-honours

MF: You have had a successful career as a GP – you founded GP West, and you are now president of AIMA-WA. How did you get to where you are now?
KP: I came here from the UK for one year, my plan was to go back, but I never went back. I liked it here, the culture, the medical system and, of course, the weather. The weather here is similar to where I grew up in India, so in that way everything was perfect.
Being a GP is a good lifestyle and has flexibility. In the hospital I was a cardio registrar and a neuro registrar, so whole nights I could be on call, and the next morning.
But primary care is close to the heart. You feel very close to your patients and that’s very important, it’s not only the flexibility for my personal life but from a patient perspective you become part of their family in a way.
I have around 20 GP clinics now. Okley is my first medical centre, it’s close to my heart and that’s the reason why I still work there. My second is Ellenbrook and was started in 2014. The reason I started it was because I had a few doctors
Dr Kiran Puttappa was appointed President of the Australian Indian Medical Association (WA) in August last year. After completing his medical training in India, Dr Puttappa worked in various hospitals in the UK before moving to Australia and settling in Perth in 2004.
After initially training in Psychiatry in India and the UK, Dr Puttappa undertook his physician training while he was a registrar at Sir Charles Gairdner Hospital. He completed his training in 2010 and opened his first general practice, Okley Medical Centre, in 2011.
Now, 14 years later, Dr Puttappa is the chief executive and founder of GP West with 20 medical centres across Perth. He is also a WA council member of the Royal Australian College of GPs.
Medical Forum spoke with Dr Puttappa about his aspirations for AIMA-WA and his experience as an internationally trained doctor.
approach me looking for a job, but we did not have any spots.
I had got to understand the art of running a business, so, I thought, why not open a second? And then a second became a third, a third a fourth and so on.
MF: You have been in Perth 20 years now, how has the medical system changed in that time and what are some of the challenges you’ve faced along the way?
KP: General practice is becoming tougher and tougher every day. There is the rising cost, doctor shortages and, of course, Medicare rebates are not enough.
General practice is a specialty just like any other, but if you compare the Medicare rebates with non-GP specialists and to us, there’s a significant difference.
General practices are shutting down recently, they cannot survive. If you have one GP or two GPs in a practice you need to have a practice manager, you need a nurse, you need to pay the rent…how can you afford to run the business?
COVID dramatically changed general practice. Up until then we
had never heard of teleconsultations, but they started during COVID and are still ongoing. There are a lot of private platforms now for telehealth consultations that are non-Medicare. It’s good for the patients but at the same time I would say it’s making things more fragmented.
Coupled with the bureaucracy of the pharmacy prescribing and all of those things, the care of the patient is getting fragmented. It impacts quality of care, that’s where we are at the moment.
MF: What do you hope to achieve in your two years as president of AIMA-WA and how does the association support international medical graduates (IMGs)?
KP: We are the strongest Indian medical association here in WA. We have around 650 doctors registered in Perth and the outer metro area.
We run a lot of health awareness programs, we support medical students and have an IMG support group so they have someone to help them to settle into the Australian medical system more effectively and easily.
It’s not just Indian doctors – we work with any IMG. Any doctor can join

our organisation as long as they believe in the constitution of AIMAWA – we have a lot of British GPs who are members of AIMA-WA.
We also do a lot of charity programs. During COVID we raised $150,000 and donated it to the Red Cross, Destiny Rescue, Perth Children’s Hospital and a number of other organisations. We have a big gala event every year and the funds raised go to charities.
During my time as president, I would really like AIMA-WA to be involved in advocacy and government decision making in health, we want to be a main stakeholder just like the AMA.
We have experienced doctors starting from consultants right through to head of departments and directors of training, and they could use the expertise of the association on policy changes. If you can get the medical profession involved [in decision making] then it will reach the public and culturally diverse communities more effectively.
At the end of the day, when the government makes a decision about health it has to be realistic, and it should reach all patients in the right way. If patient care is considered in policy making, then that’s good for the community.
MF: India is one of our biggest sources of OTDs and we are expecting to see more international doctors working in Australia through the Australian Health Practitioner Regulation Agency’s new expedited pathway. What is it like moving here as an OTD?
KP: Any doctor coming to a country like Australia needs to be well supported, irrespective of which country they are coming from. If they feel like they’ve been left alone
and are not part of the system, they cannot work effectively.
They may have the skills, but if they’re not supported it will be difficult for any practitioner coming from overseas to deliver quality care. They may end up leaving [the profession] depending on their personal circumstances.
That’s when they seek help from professional organisations like AIMA-WA to see if we can help them out.
MF: Are there any challenges that OTDs face working in WA?
KP: The Distribution Priority Area (DPA) is hampering our efforts to recruit more GPs. We may have GPs wanting to come to WA, but we only have very limited places where they can work.
I could have a GP call me tomorrow and say they want to work at Okley Medical, but I can’t take them because it’s not a priority area. They can only work in a DPA location for 10 years. It’s a big commitment for an international medical graduate.
MF: Do OTDs experience much racism and discrimination when they move here?
KP: Personally, I haven’t had any racist experiences in my medical career, whether that was in the hospital systems or as a GP. There are instances that happen all over the world, but Australia is a great system and colleagues have been supportive.
The international medical graduates who have come here and settled are quite happy. But we do get phone calls about it at AIMA-WA, that’s why we have the IMG support group. We also run a program for
medical students to support them during their training.
If IMGs decide to come to Australia, they are definitely more than welcome.
MF: A recent Federal Government supply-and-demand study suggested GP shortages in Australia will increase from 800 in 2024 to 2600 by 2028 and 8600 by 2048. To help plug gaps we have increasing numbers of OTDs in the system, but this has been a point of contention and concerns have been raised about international graduates taking limited training spots from ‘homegrown’ doctors. What is your response to these concerns?
KP: The government should be looking into promoting local doctors as a priority. They need to provide more funding for education, more funding for primary care and they need to make primary care attractive.
Good funding for general practice, so GPs can provide quality care, is hugely important. The more money that’s put into primary care, you’re actually saving money.
But, of course, we need to look to international medical graduates. There should be a correct selection process and good support systems in place. If IMGs are coming in and are seen on par with the local trainees, they apply for jobs and are treated equally, that’s fair. But if one is treated inferiorly or superiorly then that’s not correct.
MF: Concerns have also been raised about Australia’s impact on international medical systems through overseas recruitment, do you share the same concerns?
KP: I agree with that, but it also comes down to the doctor’s personal choice.
Every country needs to improve their health system so they can keep their homegrown doctors in their own country. I don’t want the same thing to happen to Australia where the homegrown doctors start moving to different countries because they’re not well supported. If you don’t look after the IMGs as well, then they may choose to go to different countries, so the

continued from Page 11
Australian healthcare system will definitely be affected.
In the UK, even though the NHS is fully aware a lot of UK doctors are moving to Australia, they haven’t taken effective steps to keep their homegrown doctors.
MF: What advice do you have for GPs looking to set up their own medical centre?
KP: Do your due diligence well before you set it up, because at the end of the day you don’t want to be shutting down your practice one or two years later.
Look at who you need to hire. Allied health is so important and without a practice manager you can’t run a practice.
My first practice was a bit difficult. I had to learn the art of running a business. Now I’ve got a very good team who can set them up and run

As a new GP, setting up a clinic in the current situation is very tough. But if you can do your due diligence and provide a good

ED: At the 2024 AIMA-WA gala dinner the State Government announced that 150 trainee doctors from India would arrive to work in WA under a new program starting in January 2025. Neither the AIMA-WA or AMA(WA) were consulted on the program. AMA(WA) has raised concerns about the lack of detail on where the doctors would be working and how they would be supported in the system.
A State Government spokesperson said from January 2025, Indian trained medical graduates, who have successfully completed the AMC1 examination are now able to apply to work in WA Health.
“As with all recruitment pools, offers of employment are subject to public sector standards and are a highly competitive process,” they said.
“Future opportunities to support up to 150 Indian trained medical graduates, with relevant clinical experience, is expected to be finalised in early 2025. The AMA and AIMA-WA will be consulted once finalised.”






Some experts say doctors who think artificial intelligence is a fad about robots that will bypass the healthcare system risk being left behind and doing unnecessary work.

Cathy O’Leary reports
As little as a decade ago, there was scepticism that artificial intelligence could – and would – play a significant role in healthcare.
After all, how could machines do the job of healthcare staff in examining, diagnosing and treating patients?
Even though monitoring equipment has long been used in medical care, from ECGs to blood glucose monitors, there has been firm resistance to artificial intelligence, considered by many as a bridge too far amid concerns about safety and privacy as well as fears that machines will replace people.
And among those most wary have been doctors, for whom AI raises specific legal, professional and ethical challenges.
At the Royal Australian College of General Practitioners’ annual conference held in Perth late last year, a keynote speaker told the 1600 GP delegates that the risk was not losing their jobs to machines but rather being left behind.
Dr Jordan Nguyen, a world-renowned PhD biomedical and AI engineer, said that with two brothers who were specialist GPs he appreciated first-hand that many doctors were cautious about AI but often it was because they did not understand it.
“It’s not that GPs are going to be replaced by robots and AI –GPs will be replaced by GPs who use AI.”
– Dr Jordan Nguyen PhD
applications of AI included automating administrative tasks, clinical decision support, enhanced patient triage, efficient e-health records management, predictive analysis for patient risk stratification, medical imaging assistance and virtual health help for patients.
He said there were many forms of AI, including digital 'twins' which were digital representations of the patient – a more sophisticated version of someone’s social media profile.

“You can then connect your data to the data of millions of people, which can then give you insights into your health that might not be obvious, such as predisposition to diabetes even though there is no family history,” he said.
“This is an application of machine-learning, and they’re now doing work to apply it to the human body, even to editing genes of living people.
important thing not to just go ‘all in’ when it comes to AI,” he said.
“That’s why it is important to show doctors practical applications, because as soon as you can see it in the real world you can go ‘OK now I can see how it can be used’ rather than talking about the actual technology itself, which a lot of the time sounds scarier than it is.
“My brothers are both GPs and even with them there is some resistance when I talk to them, and while they’re identical twins, one is quite open to technology, while the other says ‘I’m too busy to have to understand any of this’ so it’s easier not to engage.
“My message is that this powerful technology can actually make your job easier, but I also realise that it’s about small steps, and it’s the stuff people are increasingly going to hear about, like easier transcription.
“It’s best to start small with something you’re comfortable with that will help you in your day-today role.”
Other speakers stressed that the benefits of AI were often dependent on the quality of the information and data underpinning it.
More GPs were starting to adopt medical AI scribe software –artificial intelligence programs that capture consultations in real-time by recording in the background and generating detailed notes ready to go into a patient’s medical record – going far beyond basic transcription.
“There are a lot of areas where AI will have an impact on general practice, and you’re going to hear about AI a lot more,” he said.
“It’s not that GPs are going to be replaced by robots and AI – so that’s not where the job losses are going to be – it’s more that GPs will be replaced by GPs who use AI.”
As the founder and chief executive of Psykinetic, a social business creating technologies to help people in the disability and aged care sectors, Dr Nguyen has helped develop, among other things, a mind-controlled wheelchair and an instrument to allow people to perform live music using eye movements.
“What it could mean is that some time down the track you’re able to say to your patients there is a very simple procedure if you’re going to have a child – it’s been deemed completely safe – and we can make sure your unborn child is never going to get cancer.”

Dr Nguyen told Medical Forum that resistance to the use of artificial intelligence within the medical profession was often because doctors had limited knowledge of its real-life applications and had concerns about patient privacy.
Professor Richard Hobbs , from the University of Oxford, said AI and digital health were going to transform the approach to a more accurate and personalised approach to medicine.
“But there are huge obvious risks and concerns that patients and practices have, and it’s very important that clinicians direct how this transformation of medicine is going to occur,” Prof Hobbs said.
“AI is a syndrome, it’s like heart failure – there are multiple ways to it, and multiple methodologies to the outputs – it’s not a single mechanism.”
Dr Nguyen told the RACGP conference that potential health continued on Page 17
“I understand those concerns completely, and it’s a very
Your health, in full view

At PRC, your referrals for musculoskeletal (MSK) investigations and pain injection procedures are locally reported and managed by the largest team of MSK and Spinal radiology experts in Perth.
Our elite MSK and Spinal radiology teams specialise in providing expert imaging and pain injection services across the board, expediting treatment pathways with precise diagnostic insights. We offer MRI appointments in the evenings and on weekends for your patients’ convenience.
Stay tuned for the opening of our new clinics: Alkimos opening July 2025 and Bunbury coming in 2026.
Doctor Priority Line For urgent bookings and enquiries 9599 3929
continued from Page 15
Big-ticket items include machinelearning, language processing and robotics.
“Part of the solution will be more automated management of health, such as AI-driven scripts, where the doctor’s and the patient’s speech is picked up, and this results in an automated clinical record, which is a start because it will save you time, and although you still need to check the entry at least it’s a draft for you.
“But once we get into the total language models, you will be able to end up with automated coding systems, and eventually we’ll have systems which will have been tested enough to be reliable, and then it will be easier for the clinician.
“The dynamic of the consultation will change because you will be able to focus more on the consultation, and you can record the bits that you want, and you can get consent at the same time.”
Meanwhile, many industry groups have stepped up to become more proactive in the AI space, including the Australian Medical Association which has developed policies around the use of automated decision making (ADM) and large language models (LLMs) in healthcare.
In its submission to the Select Committee on Adopting Artificial Intelligence last June, the AMA said AI could improve the efficiency and quality of healthcare but also created risks for patients and the medical profession, including bias, discrimination and errors.
“Risks include a potential overautomation of decision making, poorly defined measures of accountability, transparency and liability, adverse outcomes for groups with diverse needs and misuse of patient information,” the AMA submission said.
“AI must never compromise medical practitioners’ clinical independence decisions and professional autonomy. To avoid machine error or over-reliance on AI technology, decisions relating to patient care must always be made

“AI is a syndrome, it’s like heart failure – there are multiple ways to it,”
– Prof Richard Hobbs
by a human, and this decision must be a clinically sound, meaningful decision, not merely a tick-box exercise.”
The AMA argues there is a grey area over who is responsible for errors in diagnosis and treatment related to the use of AI products, including compensation for patients who have been misdiagnosed or treated incorrectly.
It wants the Federal Government to address Australia’s poorly defined civil and criminal liability rules in relation to cases of damages caused by artificial intelligence systems.
In Western Australia, the use of AI continues to expand in leaps and bounds, from remote primary care locations to hospital emergency departments.
WA-developed wearable biobands are showing promise in improving patient monitoring care and safety and reducing reliance on manual vital sign checks and in-ward equipment.
In a recent trial, 35 intensive care patients at a Perth tertiary hospital who were transitioning to a general
ward were fitted with AI wearable bands which captured their health data, giving nurses and doctors real-time monitoring while they could attend to other cases, and avoid the need to wake up patients for monitoring.
The biobands were developed by WA medtech company Medivitals using funding from the State Government’s Future Health Research and Innovation Seed Fund.
The technology has already been successfully trialled in a hospitalin-the-home program, allowing remote monitoring of patients and avoiding unnecessary hospital admissions, with the results due to be published soon.
Its developers say it has strong potential in hospital emergency department waiting rooms, enabling real-time monitoring of patients waiting for care and identifying signs of deterioration so that high-risk patients can be prioritised.
Professor Warren Harding, cofounder of Medivitals, said the
continued on Page 18
continued from Page 17
bioband used software which could be customised to the needs of individual patients, while AI assistance could provide alerts to clinicians about abnormal vital signs.
“The device ensures that highrisk patients are identified and prioritised even before they reach a hospital bed, and this predictive approach addresses critical challenges such as bed capacity overcrowding and staff shortages,” he said.
Prof Harding, who was recently appointed to the board of the Australian Digital Health Agency, said the technology could be applied in residential aged care and hospital-in-the-home care, allowing patients to avoid hospital while vital signs such as heart rate, oxygen saturation, temperature, blood pressure and respiratory rate were monitored remotely.
Professor Yogesan Kanagasingam, Medivitals cofounder and Chair of Digital Health and Telemedicine at the University of Notre Dame’s School of Medicine, said the technology also ensured data security and patient privacy.

Patient data was securely stored at the hospital or locally within Australia, ensuring compliance with privacy regulations, and by avoiding external servers and thirdparty cloud providers, the system minimised cyber risks.
Prof Kanagasingam, who is on the board of directors at the IndoAsia Digital Health Centre for Innovation and Commercialisation, told Medical Forum there had been good feedback from patients and clinicians involved in the ICU hospital trial.
“The doctors think it’s very cool
There is no one-size-fits-all approach to vascular surgery. My team and I address patients’ individual needs with the most appropriate and best comprehensive management option.
– DR NISHATH ALTAF | Vascular & Endovascular Surgeon
because the bioband technology is just providing the information but then the clinician still makes the decisions,” he said.
“Hospital-in-the home is also one of the major areas of interest for this technology, because there is only a limited number of beds in hospital, and this is a way to allow patients to stay at home and for doctors and nurses to manage them.
“And the ED use is potentially very exciting, as it can alert clinicians if the patient’s condition changes, so it allows doctors and nurses to focus on what they’re doing.”
Prof Kanagasingam said there were other AI projects well underway in WA, including a system of techniques to grade and diagnose eye diseases such as diabetic retinopathy, glaucoma, aged-

Dr Altaf alongside his colleagues – diagnostic sonographer Simon and clinical nurse Mel – provides a comprehensive diagnostic and therapeutic service of arterial and venous diseases including:
Abdominal aortic aneursyms
Carotid artery disease
Peripheral artery disease
Leg ulcers & diabetic foot disease
Varicose vein diagnosis & treatment
Renal access
Dr Altaf consults at Hollywood Medical Centre, SJOG Midland Private Hospital, SJOG Carine Specialist Centre and public appointments at RPH and SJOG Midland Public Hospital. Operates out of SJOG Midland Public and Private, Hollywood Hospital and SJOG Subiaco.
Appointments are coordinated through practice manager Michelle Burrell and her team.

Hollywood Medical Centre
Level 2 Suite 45/85 Monash Ave, Nedlands WA 6009 Phone: 6244 6215 | Fax: 6315 6423 | Healthlink ID: drnaltaf
draltaf.com.au

related macular degeneration and cataracts. It is the first AI system for eye diseases to receive regulatory approval in Australia, and the technology is now licensed to international company TeleMedC and used in Singapore, Europe, the Middle East and India.
Prof Kanagasingam said one of the most interesting recent trials involved bringing AI-based eye screening to two remote Aboriginal communities located near Fitzroy Crossing.
The partnership between the University of Notre Dame’s School of Medicine and the Foundation for Indigenous Sustainable Health secured $1.3 million in funding from the Australia-India Strategic Research Fund.
“We were the first to implement AI-based eye screening in such remote Aboriginal communities using Starlink satellite technology,” he said.
“The results were eye-opening – approximately 20% of those
screened required urgent referrals to an eye doctor due to severe disease and remarkably many of them had never seen an eye doctor before.
“We are also working with one of the world’s largest eye service providers, the Aravind Eye Institute in India, which sees over 8.5 million people a year.
“We are deploying our AI system from WA into rural and remote locations in South India where they train women from villages to screen local people and then use AI to grade and refer those who need treatment and surgery – this has been a very successful project.”
Meanwhile, the State Government has recently accelerated funding for a range of other AI research projects, including a personalised health platform known as Orva to help patients better understand their health; an AI-based initiative that can predict sepsis in emergency departments; and the use of AI data in diabetes care plans.

1 2 3 4 5 6


They say if you want something done, give it to a busy person. Oral medicine specialist Dr Jacinta Vu enthusiastically loves all three parts of her busy life: family, a practice and life-changing pro bono work.
By Ara Jansen
It is hard to comprehend how much your smile means for your confidence, until your mouth is a mess and you’re too embarrassed to grin.
Recently named the 2025 WA Local Hero in the Australian of the Year Awards, Dr Jacinta Vu has been honoured for her dedication to pro bono work, giving smiles back to other women.
Since 2020 she has been a director of Healing Smiles, a free dental treatment program for survivors of domestic violence, which was created in 2018 by the Women in Dentistry Society, a group supporting female dental practitioners in WA. All the female volunteers within the program have donated their skills, time, materials and, until recently, surgery space.
Healing Smiles received $1 million in funding, which finishes this year. With that funding the group has built and recently opened a dedicated dental clinic for trauma and aftercare work within the newly opened Ruah Centre for Woman and Children.
“Not only does the work give women a nice smile but it does amazing things for their confidence, self-worth and dignity,” says Jacinta. Healing Smiles has treated more than 500 women so far and Jacinta hopes the new surgery is able to increase the number of women they can help. About 50 dentists, specialists and dental assistants are part of the program.
According to Jacinta, the dental aspect of domestic violence is under reported, if reported at all. In such cases, the care needed can vary from broken or knocked out teeth through to basic dental care.
“We’ve had patients who had been under coercive control and not always able to leave the house to visit a dentist or buy a toothbrush. Or they lose care for themselves and might not brush their teeth, or they are self-medicating or being forced to take substances which impact their teeth.
“It becomes so much more than that, because generally a lot of people are fearful of the dentist. You lie back in a chair with two strange people in the room getting really close to you and you can’t control what goes on. That’s hard for most people, let alone people who have been traumatised.
“Add in the sexual abuse element and it can be even more challenging. Or something like the noise of a drill or latex in their mouth might trigger them.
“There are patients who can’t look at us because they are so embarrassed about their mouth.”
For those reasons and others, that’s why the Healing Smiles team are all women. The important qualities they provide alongside dental care are compassion, empathy and being able to listen.
“To be able to look after these women survivors and see their journey and how the treatment has changed their lives is amazing. There’s something cathartic and healing about it for them.”
Jacinta is an oral medicine specialist and co-owner of the Centre for Oral Medicine and Facial Pain in Como. She did her dental degree at UWA and specialist oral medicine training at the University of Sydney.
Born in the UK to a Sri Lankan father and Malaysian mother, Jacinta and her family migrated to

Australia when she was eight and moved to Perth from Sydney about 18 months later.
As a registered nurse, Jacinta’s mother shared with her the kinds of sacrifices she saw the doctors and other medical professionals around her making.
“That was one of the reasons I wasn’t sure if medicine was for me,” she says. “I went to a dentistry information session and thought it was pretty cool. Working with my hands in that way appealed to me.
“It also put you in contact with people and seemed to have regular hours. Plus, after uni I didn’t have to do another 10 years to specialise. Instead, I started with the first year of a science degree, then moved into dentistry and after four years started my dental career.”
At 22, Jacinta was posted to Exmouth and got a crash course in being away from home and learning to look after herself, with no family close by. She was also one of the few non-Caucasian people living in town.
“It was a steep learning curve, both personally and professionally. Getting used to living alone and not having someone to come home and talk to or hug was really hard. I was the only dentist for 400km, so it was sink or swim.
“I did have a lot of telephone support. It was 2002, before email. Notes were still handwritten. I had to teach myself how to do certain things, and not be too scared to take things on, but at the same
time, not be too gung ho. Generally, I am on the more cautious side. People were grateful I was there to help.
“I think you can learn something from everyone you meet. It doesn’t matter who they are or how old they are, there’s something they can teach you or you can learn from them.
“Being in Exmouth was a defining moment in my life. I still have moments when I realise that I have done a lot of stuff, not just survived situations but thrived in challenging situations, both personally and professionally.”
Back in Perth she worked in the public system with Dental Health Services and at a private clinic. Both places helped her grow and refine her skills, while a management role as Head of Unit taught her leadership skills at a young age.
She met her husband, dentist Dr Chuong Vu, when they worked at the same clinic for about six months and married in 2007. He works at a clinic in South Perth.
By 28, Jacinta was wondering what steps to take next, not being a person to sit back and let life run her. She and Chuong decided to sit their Royal Australasian College of Dental Surgeons primary examinations. Babies could wait a while.
Fertility
Freezing
Genetic
Surrogacy
Fertility Counselling


continued from Page 21
Someone suggested Jacinta specialise and, being a person who likes to engage her brain, she decided on oral medicine.
“I wrote down all the dental speciality options and when I got to oral medicine I thought, it uses the basic sciences I love, and you have to use your brain to put all the pieces of a medical puzzle together. It felt like the right kind of place for me,” she said.
“I applied and doing the interview was like a dream date. This is what I’m supposed to do. This is my calling. I resigned from my Head of Unit position and went to Sydney for four years to complete my postgraduate training in oral medicine.”
More than a decade on, Jacinta still loves her work with that same passion. She enjoys puzzling out issues around facial pain, autoimmune diseases affecting the face and jaw, non-healing ulcers and the many other issues which affect the head, face, mouth and neck.
She’s part of a small group of professionals in Australia –around 40 – who work in this not particularly well-known specialty.
In 2022, Jacinta and her business partner Dr Alissa Jacobs, stepped out on their own and opened the Centre for Oral Medicine and Facial Pain.
She is also a consultant oral medicine specialist at Perth Children’s Hospital and an honorary research fellow at UWA, as well as teaching and lecturing over the years.
After finishing her specialist studies in Sydney, it was time to have kids. Jacinta decided if she was going to do it, they were going to be close together. She had one son and three daughters in three and a half years. They are now nine, seven and six-year-old identical twins.
“My kids were all born on a Thursday on the 13th of the month and exactly 20 months apart. Not by design at all, but I believe that things happen for a reason in my life,” she said.
She hopes that closeness in age

will make them lifelong friends and allies for each other.
“I like that they are growing up together and generally play pretty well together and get on most of the time.”
The whole family can now ride a bike, so they’ve started going out on rides. They like to swim and have started playing more board games. Piano lessons are also afoot, with all four children and Jacinta taking lessons.
Jacinta enjoyed playing when she was younger, and at the very least she hopes it gives them a grounding in music and a love for it.
Jacinta has a brother and her husband is the eldest of six. Her parents and aunt still live together in Perth and Jacinta is determined to instil and nurture a strong inperson connection between her children and their grandparents, other relatives and network of friends.
Her parents and aunt are highly involved in the children’s lives, and she wants to keep it that way. They live with the Vus on and off during the week to help with pick-ups and drop-off. Chuong usually takes care of school lunches, and everyone pitches in with household duties.
“I have a fantastic family network that supports me and gives me time and space to engage my brain, heart and soul professionally and on different projects,” she said.
In keeping with always having something sizable on the go, Jacinta is currently designing a multi-generational home for her family, taking great care to create welcoming communal areas, space for the kids to run around, a massive kitchen which allows for three to four people to be moving through it at a time, and enough private, quiet space.
“I want a dedicated area for my parents and aunt if they want to be alone as well as personal space for each of us. There will be nine of us living together.”
When it comes to time on her own, Jacinta exercises to keep fit and clear her head and always has a book on the go. A Kindle is one of the best investments she’s ever made.
Although her life is certainly busy, Jacinta feels fulfilled.
“I find when things are happening for me, when life is going in a good direction, things seem to happen easily. When things are hard, I know I need to seek out and find a different path. That has been true for most of my life.”
ED: Information on referrals and eligibility to Healing Smiles, see www.healingsmiles.com.au Sponsors and support are also welcome.
Did medical school ever teach you how to build wealth? Probably not.
By David Rossbach

You spent years learning anatomy, histology and biology to become skilled clinicians, but most likely never received a single lesson on how to invest, save, or escape a pay check to pay check cycle. Medical school taught you to diagnose diseases, not compound interest.
This education gap leaves many doctors playing catch-up with wealth creation and establishing financial security, despite their earning potential.
Money isn't just numbers. It's personal. Your financial choices, especially about saving and investing, are shaped by your emotions and experiences. Understanding these influences helps us make better decisions and avoid mistakes. For doctors, after years of study and hard work, a secure financial future should be inevitable, but that’s not always how it turns out.
Your financial DNA
We all have a unique relationship with money. It starts with where and when you were born. Someone who grew up during a stock market boom might see investing
as an opportunity. Those who lived through economic hardship might view it as risky. These early experiences shape our attitudes towards saving, spending and investing.
We also inherit money attitudes from our families. If your parents were cautious, you might be too. If they took risks, you could see that as normal. These patterns often feel logical, even if they're not always rational.
Financial success isn't just about knowledge. It's about behaviour. You could know everything about money and still make poor choices if emotions take over. Fear, greed and overconfidence often lead people astray.
Overconfidence
Doctors, while experts in their field, can have the tendency to overestimate their expertise in financial markets. This leads to excessive trading, underestimating risk and poor outcomes. This shows up particularly when investing in med or biotech stocks, where
doctors tend to go ‘all-in’ on one company or idea in the hope of big returns.
To counter this, invest based on your specific goals and objectives. Review your investment performance regularly and compare it to benchmarks. Diversify your portfolio to spread risk. And if you don’t have the time or inclination to do any of this, then seek guidance from financial professionals.
We hate losing money more than we enjoy gaining it. In fact, studies show that losses are felt roughly twice as intensely as gains of the same magnitude. This can make us cling to bad investments for far too long or be overly conservative. Doctors used to high-stakes environments might avoid all risks. But this can mean missing out on potential gains. Balance is key.
To mitigate this, focus on your portfolio's overall performance. Measure performance against your goals, not just the highest return. Consider the opportunity cost of holding onto underperforming investments.
Financial success isn't just about knowledge. It's about behaviour.

Humans tend to follow the crowd. If everyone's investing (or selling) a particular stock, it creates a sense of urgency. For example, the recent launch of DeepSeek's R1 AI model in January 2025 led to a significant shift in market sentiment, causing a mass short selling of Nvidia stock, and a drop by 17% in one day, the equivalent of $590 billion dollars. So, following the crowd isn't always wise. Independent, informed decisions are crucial.
Develop a well-thought-out investment plan based on your goals and risk tolerance. Stick to it. Avoid decisions based on market hype.
We often give more weight to recent events when making investment decisions. This leads to short-term thinking. If the stock market's been doing well, you might assume it'll continue and invest more aggressively. If it's been underperforming, you might delay or sell. This 'buy high – sell low' strategy diminishes wealth.
Take a long-term view of your
investments. Base decisions on comprehensive analysis and historical data, not short-term trends.
Familiarity bias
This is the tendency to invest in what you know, like property. Doctors might prefer investing in healthcare companies, potentially missing out on other profitable sectors.
Educate yourself about different asset classes and industries. Diversify your investments across sectors and geographies.
As a doctor, your expertise is in medicine, but understanding and mitigating investor biases is essential for achieving your financial goals. Recognise these biases and implement strategies to counteract them. This will help you make more rational, informed investment decisions. Seek advice from financial professionals and maintain a diversified portfolio.
There's a difference between being rich and being wealthy. Being rich is
about having money now — high income, flashy possessions, visible success. Wealth is quieter. It's about having options, freedom, and security.
True wealth allows you to live life on your terms. You can choose how you spend your time and who you spend it with. This is often more valuable than any material possession.
In 2019, our founder, David Andrew, wrote the book, Wealth with Purpose: A commonsense guide to wealth, investing and an inspiring life. If you’d like a free copy mailed to you, email me at drossbach@capital-partners.com.au with your contact details.
It costs the Australian economy billions of dollars every year, but what is the true cost of chronic pain for the millions of people living with it and are health practitioners equipped to manage it?

By Suzanne Harrison
Mandy has been living with chronic pain for about a decade and takes around six different medications every night, as well as requiring regular IV drips.
The 59-year-old Perth-based mother of five, suffers from debilitating rheumatoid arthritis and migraines. The former keen netballer and golfer does not want to take the prescribed pain medication, but without it she could not function.
It all started in her 40s with pain in her feet and ankles, then she had trouble walking. After an initial lupus diagnosis Mandy was prescribed steroids but, two years on, sought further advice on whether to continue. Then she was told the pain was caused was fibromyalgia, but was later tested for and diagnosed with rheumatoid arthritis.
“I was annoyed by [those initial wrong diagnoses]. How could two of them [physicians] get it wrong?
“Before this, I’d not had any pain like that,” she says. “Now I can’t even play golf, because I can’t hold the club.”
To counteract that, Mandy has been motivated to keep moving with regular gym sessions, but she really misses playing golf.
“No one understands it until they have experienced it themselves,” she adds. Mandy’s story is far from unusual in Australia and around the world.
According to the Australian Institute of Health and Welfare (AIHW), chronic pain is a condition characterised by persistent pain experienced on most days of the week, and affects one in five Australians aged 45 and over.
Curtin University has estimated chronic pain costs the Australian economy $139 billion every year.
AIWH says chronic pain can result from injury, surgery, musculoskeletal conditions such as arthritis, or other medical conditions like cancer, endometriosis or migraines. In some cases, there may be no apparent physical cause.
Analysis in an AIHW report from 2020 shows that compared with people without pain, people with chronic pain are more likely to:
• be female and older
• have long-term conditions
• stay longer in hospital
• report limitations to daily activities
It is considered chronic if the pain lasts beyond normal healing time after injury or illness – generally three to six months – and the pain experienced can be anything from mild to severe.
The defining characteristic of chronic pain is that it is ongoing and experienced on most days of the week.
This is true for Mandy and millions of other Australians. According to the AIHW analysis, GPs are seeing more people with chronic pain, with patient interactions increasing by 67% over 10 years.
Thankfully, in the years since a 2010 Federal Government pain strategy meeting with specialists including Perth-based Dr Roger Goucke – an Associate Professor at UWA and a former head of pain management at Sir Charles Gairdner Hospital – a lot has been done to move towards standardised treatment and physician and specialist education.
of that, the question was asked ‘how do we educate people?’ as it’s well known in med schools that pain management is not well taught.”
Considering that about 20% of the world’s population lives with chronic pain, this had to change.
The original Action Plan was spearheaded by Painaustralia (PA), the national peak body working to improve the quality of life of people living with pain.
In a 2021 report, The Cost of Pain in Australia, PA and the Department of Health found that more than 68% of people living with chronic pain were of working age.
Without action it found the prevalence of chronic pain will increase to 5.23 million Australians (16.9%) by 2050.
By 2032, it is projected that the number of cases of arthritis and other musculoskeletal conditions will increase by 43% to 8.7 million.
Osteoarthritis is projected to affect three million people, up from 1.9 million in the same timeframe, back problems are predicted to affect 3.8 million people, up from 2.9 million, and osteoporosis cases are set to increase to 1.2 million people from 0.8 million.
“Yet many people living with pain cannot get access to best practice pain management, often due to cost, location or low awareness of treatment options, and medication is playing an increasing role,” the PA report states.
To implement the Action Plan, PA consulted widely with consumers, clinicians, allied health practitioners, key health groups, researchers and the medical community to understand what people think the key priorities should be.

“Since then, a whole lot of positive things have happened, but it is slow,” says Dr Goucke.
“The National Strategic Action Plan for Pain Management came out after a lot of lobbying and, as part
As a result, Australia was the first country to have a National Strategic Action Plan for Pain Management
Since then, all Australian states have adopted recommendations.
The Action Plan, PA says, has been a catalyst for major change in the way pain – especially chronic pain – is understood and managed in Australia and the provision of pain services.
Highlights include:
• Statewide pain plans are in place in Western Australia, Queensland, New South Wales, and South Australia while Tasmania and the Australian Capital Territory are advanced in their planning with a focus on developing community-based services
• A total of 14 new regional pain clinics have been established across the eastern states
• Dedicated paediatric pain clinics have been established at Perth Children’s Hospital in Perth and Lady Cilento Children’s Hospital in Brisbane, and regional paediatric service capacity has been increased at John Hunter Children’s Hospital in Newcastle
• A range of new chronic pain education and training opportunities have been developed for health professionals
• More education for people living with pain, including award-winning online portals PainHEALTH and painbytes.
Meanwhile – through its Faculty of Pain Management (FPM) –the Australian and New Zealand College of Anaesthetists (ANZCA) is leading a project to develop Australian standards for health practitioner pain management education.
ANZCA says the overarching aim of the National Strategy for Health Practitioner Pain Management Education is that health practitioners receive high quality, evidence-based, contextually relevant and timely education throughout their career to support the delivery of best-practice care.
“The development of a set of standards governing health practitioner pain management education will assist in ensuring the consistency, relevance, appropriateness and overall quality of the education provided,” a spokesperson says.
“A set of well-developed and accepted national standards for health practitioner pain management education will aim to inform policy, education, and practice to improve the care of Australians living with pain.”
Advert removed in compliance with Medicines Australia's Code of Conduct and the Therapeutic Goods Administration's Therapeutic Goods Act.
https://medicinesaustralia.com.au/code-of-conduct/about-the-code/ https://www.tga.gov.au/legislation-legislative-instruments
continued from Page 27
It is intended that a nationally consistent set of standards for health practitioner pain management education be developed that will:
• Be relevant across multiple health practitioner disciplines and levels of education
• Be underpinned by the values and principles of the National Strategy for Health Practitioner Pain Management Education
• Set the minimum level of quality
• Provide guidance in the development and delivery of pain management education
• Be inclusive of the needs of priority populations.
The final standards are set to go to government in October 2025.
As part of developing the standards, one of five in-person and three online, national stakeholder consultation workshops was held in Perth in August last year.
Twenty-two people took part, with attendees including pain physicians, academics, allied health professionals, people with lived experience of pain, peak body representatives, nursing staff, and health professional educators.
Dr Gouke, who attended, said the workshop was a way for stakeholders to collaborate and consult.
“There was amazing consensus, more about the communication than the content,” he says.
“This involved how do we have good relationships with people and make sure the doctor is on the same page? How can we put the patient at the centre, and if we can’t find a cause, how can we help?”
ANZCA says a governance advisory group, consisting of a range of relevant stakeholders, was established in the early stages of the project to provide advice and guidance to the FPM project team.
RACGP Pain Management Chair Dr Adele Stewart told Medical Forum that GPs are in great need of improved knowledge and skills in pain management.

“There is certainly quite a lot in the literature confirming that many GPs struggle in managing people’s pain,” says Dr Stewart.
“For example, an article in ‘Australian Family Physician on GP Pain Management’ states ‘The literature shows that GPs have low satisfaction in treating patients with chronic pain and only 34% of primary care physicians felt comfortable in managing these patients.”
ANZCA’s spokesperson adds: “It would be great if GPs are aware of the National Strategy for Health Practitioner Pain Management Education and take the opportunity to be engaged in any stakeholder consultation activities.”
While this standardised approach to care and education has been a while in the making, pain medicine has been recognised as a separate specialty since 2005 in Australia and 2012 in New Zealand, and the two countries are considered pioneers in the field.
Another step in the right direction is a 2022 national blueprint to help health professionals support the many Australians living with chronic pain, developed here in Perth.
Published in the international pain journal PAIN, the ‘Listen to me, learn from me’ framework was co-developed by a national team of Curtin University-led researchers working in partnership with Australian people living with chronic pain, carers and health professionals.

With funding support from a fouryear Commonwealth grant, the framework
is a blueprint for the development of Australian interdisciplinary pain training programs.
Lead researcher Professor Helen Slater, from the Curtin School of School of Allied Health, says chronic pain was often debilitating for the Australians living with the condition, and with significant implications for the health system and economy.
“Living with chronic pain means lives are often put on hold. You can’t see pain, but it can derail people’s lives,” Professor Slater says.
“People with chronic pain are not consistently supported with high quality person-centred care in Australia, and it’s a similar situation across the world.”
Dr Salter’s team has utilised the resulting framework to establish an open training platform.
“This has now been established,” says Dr Slater. “And in mid-2025, that open training platform will be launched to any and all health professionals around Australia.”
In a nutshell, ANZCA and people including Dr Slater have worked to develop a clear way forward for pain management education for health practitioners.
Dr Slater and her team have formed an education program, while ANZCA has developed the upcoming, Australia-wide educational standards for training and pain management for all medical professionals.
For people like Mandy, finding such care, medication and ongoing support is vital. While she would much prefer to be medication free, Mandy says “I would fall to the ground” without them.
A new clinical definition of obesity is a step in the right direction, writes WA lead for the RACGP obesity special interest group Dr Mark Mellor.
Obesity is globally prevalent, affecting one in eight people in the world in 2022. In Australia, around two-third of adults and one-fifth of children have overweight or obesity.
The prevalence of obesity has risen over the decades, so much so that the World Health Organisation (WHO) classifies it as a ‘global epidemic’.
The WHO first recognised obesity as a disease in 1948. It was defined as ‘an abnormal or excessive fat accumulation that presents a risk to health’. This simple definition, based on phenotype and health risk, has persisted for decades but is recognised as insufficient for describing the chronic systemic illness that some people with obesity experience.
Historically, our understanding of obesity has been mired by moral viewpoints, with assumptions made about its cause, like eating too much or exercising too little. This leads to weight bias and stigma, like people with obesity are lazy and lack motivation.
Unfortunately, these erroneous beliefs remain prevalent in society, political and healthcare settings. Obesity certainly is not a lifestyle choice. When viewed through a clinical lens, genetic/epigenetic, environmental, nutritional, psychological and metabolic factors are all implicated.
The dichotomy of obesity as a risk factor for disease has been the focus of many previous discussions. On the one hand, classifying all obesity as a disease risks overdiagnosis and overmedicalisation. On the other hand, classifying obesity as a risk factor for disease only diminishes the negative health effects that obesity causes.
Reconciling this dichotomy has been challenging because a robust clinical diagnosis for obesity has


been lacking and its aetiology and pathophysiology incompletely understood.
The WHO definition does not describe the causes of excess adiposity and ignores how it might progress to severe organ dysfunction and chronic illness. Further, body mass index (BMI), the most common metric used to diagnose obesity, falls short for measuring its complex and heterogenous nature. BMI is not a direct measure of adiposity, does not determine body fat distribution nor define when excess adiposity is a health issue.
Taking these issues into account, in 2022 The Lancet Diabetes and Endocrinology Commission sought to address the lack of an accurate definition of obesity and formulate a comprehensive approach to diagnosis. The commission comprised 58 international experts from various medical specialties
and people of lived experience for balanced representation. It published its findings in January 2025.
The Lancet commission’s new definition of obesity is simply ‘a state of excess adiposity (body fat)’ preferably measured directly, for example using dual energy x-ray absorptiometry or bioimpedance, or indirectly using anthropometric measures of central adiposity like waist circumference, waist-to-hip ratio or waist-to-height ratio.
BMI should not be relied upon as the sole measure to diagnose obesity, although those with a very high BMI (over 40 kg/m2) can be assumed to have excess adiposity.
The Lancet commission also sets out two new obesity categories: pre-clinical obesity and clinical obesity.
Pre-clinical obesity defines a state of excess adiposity with preserved
tissue and organ function. People with pre-clinical obesity are not limited in their activities because of obesity but do have a higher risk of developing clinical obesity and several other non-communicable diseases such as diabetes, cardiovascular disease and some cancers.
Clinical obesity is a state of excess adiposity with reduced tissue or organ function. People with clinical obesity have a chronic disease due to obesity alone. They may have various symptoms and signs directly related to obesity such as breathlessness, hip or knee pain, various metabolic abnormalities, and dysfunction related to abnormalities in other organ systems.
The commission sets out 18 adult and 13 child and adolescent diagnostic criteria for clinical obesity. These are conditions associated with tissue, organ or body dysfunction caused by obesity, such as raised arterial blood pressure and venous thromboembolism.
This pivotal undertaking marks a change in conceptualisation
of obesity from a BMI-based classification to a model underpinned by body fat measurement and the presence or absence of tissue or organ dysfunction and/or reduced functional capacity.
Importantly, the model considers that some conditions are causally related to obesity (same aetiopathogenesis) and not co-morbidities (different aetiopathogenesis).
Of course, there are other frameworks for defining and diagnosing obesity – the European Association for the Study of Obesity (EASO) and Edmonton Obesity Staging System (EOSS) frameworks, to name but a few. These models are highly regarded and agree that BMI is insufficient for diagnosing obesity.
The Lancet commission report is also not without criticism. What constitutes ‘excess adiposity’ is debated and the list of criteria meeting the definition of clinical obesity might be difficult to implement in real-world clinical practice – psychosocial drivers and complications of obesity are not
included, and no comment is made on the causative factors for obesity (albeit this was outside of the commission’s scope).
Nevertheless, the model paves a way for clinicians, policymakers, and health authorities to target treatment to those with the negative health effects of obesity and its associated chronic illness.
Further work is needed to address criticisms, and in time, the model may adapt to reflect changes in thinking and understanding as we learn more about obesity as a disease.
It is a much-needed step in the right direction that combats weight bias and stigma, promotes empathy and understanding of those living with obesity, and frames obesity as a disease to support treatment prioritisation.
ED: Dr Mellor is the lead clinician at the Perth Weight Clinic.
EOSedge is a precise, low dose imaging system that delivers full body images covering the full set of musculoskeletal and orthopaedic exams.
• Imaging complete in 20 seconds
• Full body images in standing position
• 24 hour report turnaround
• True 1:1 scale
Refer your patients now for lower dose imaging and better visualisation for diagnostic or surgical planning and post operative assessment.
• Low dose radiation
• Walk ins welcome
• All request forms accepted
• All scans are bulk billed

The Westin, East Perth | Saturday 7th June 2025
Please book a place for the conference at gpurologymasterclass.com.au or rsvp to events@perthurologyclinic.com.au
Limited seats available

Supporting patients with specialised urological cancer treatments
Dr Shane La Bianca
Dr Andrew Tan
Dr Jeff Thavaseelan
Dr Trent Barrett
Dr Matt Brown
Dr Manmeet Saluja
Dr Alarick Picardo
Dr Steve McCombie
Dr Sarah O’Neill
With the largest partnership of Urologists in Western Australia, Perth Urology Clinic can manage all urological conditions, offering a wide range of treatment options. For urgent referrals or queries, use our GP Hotline on 1800 487 656 (Press 9). refer@perthurologyclinic.com.au
Healthlink: puclinic
Hollywood Clinic | Wexford Clinic

The brain of people with hip osteoarthritis is driving motor control differently and may be contributing to their pain intensity, writes physiotherapist Molly Coventry
Hip osteoarthritis is a debilitating chronic condition that affects one in 11 Australians.
People with hip osteoarthritis typically experience high levels of pain and impairments to daily function, which both contribute to poorer quality of life. Despite many interventions available to manage hip osteoarthritis, the overall burden continues to grow.
To better understand muscle function in people with the condition, we studied the brain function of people with hip osteoarthritis compared to those without hip osteoarthritis, finding that the mind played a part in this equation.
During the course of our research, we identified changes in both motor cortex processing and maximal muscle activation capacity in people with hip osteoarthritis.
The central nervous system, consisting of the brain and spinal cord, controls and coordinates our body’s movement. The primary motor cortex of the brain sends signals to muscles via the spinal cord and motor neurons.
However, in the presence of pain, particularly chronic pain, these processes can be altered. This can result in a reduced ability to activate muscles, which is problematic as strong muscle activation provides support and stability to joints.
This ability to maximally activate our muscles is quantified using a technique called voluntary activation. It assesses the proportion of muscle fibres activated by the brain to drive strong muscle contractions.
Our research demonstrated voluntary activation of the leg muscles is impaired in individuals with hip osteoarthritis. This finding is comparable to what has been


shown in knee osteoarthritis and following anterior cruciate ligament reconstruction.
However, the research also demonstrated higher hip-related pain intensity was associated with a poorer ability to activate the leg muscles.
This finding suggests local pain inhibition is not a factor as we assessed the quadriceps at the knee, not hip, so all testing was pain free.
We suspect that pain may interfere with the ability to perform strong muscle contractions in areas outside of the affected joint. This is clinically important as it suggests individuals with higher levels of pain are more likely to have poor muscle activation irrespective of pain region.
In the primary motor cortex of the brain, we have facilitatory and inhibitory pathways that work to increase or decrease overall neural drive to muscles. These can be thought of as the accelerator and brake of the brain.
This research demonstrated that greater inhibition was associated with less maximal voluntary activation. Additionally, we found greater levels of facilitation were associated with greater hip-related pain intensity.
Overall, the findings suggest people with hip osteoarthritis have differences in the intracortical networks within the brain.
These changes within the brain are linked to a poorer ability to activate the leg muscles and produce strong contractions, which means the muscles have a lesser ability to support joint health.
Research investigating interventions which can modulate motor cortex function and improve voluntary activation during rehabilitation is currently being undertaken in an effort to improve outcomes for those with hip osteoarthritis.
ED: Molly Coventry is a PhD candidate in Nutrition and Health Innovation Research Institute at Edith Cowan University.
Help is needed to address rising rates of perinatal depression and anxiety, writes the head of a national support group, Arabella Gibson.
Pregnancy and parenthood represent a unique period in an individual’s life, but alongside the joy and excitement, new and complex emotions can also arise.
At Gidget Foundation Australia, we have witnessed the growing need for support amid rising rates of perinatal depression and anxiety. More than 3500 clients accessed our specialist perinatal face-to-face or telehealth counselling during the 2024 financial year – up from 1,625 in FY 2021. This marks an increase of 214% over the past three years alone.
Loneliness is also a significant risk factor for women developing perinatal depression, the stigma surrounding the condition
leading to further isolation. Our recent survey revealed that two-thirds (67%) of Australian parents with children under five reported that they lack a strong community support network to help them navigate the challenges of parenthood. Parents from disadvantaged or marginalised communities faced additional burdens, with existing inequalities and social isolation intensifying their experiences of perinatal depression and loneliness.
As CEO, I have seen first-hand the challenges faced by mothers and fathers who struggle to seek support or simply don’t know what support is available. It is crucial parents receive consistent,
Heel pain is a frequent problem that presents to the general practitioner. Plantar fasciitis is the most common cause of under the heel pain. Most patients will improve with non-operative treatment but not all.
Surgery is a very effective form of treatment for this condition in patients with long standing refractory symptoms.
Before being considered for surgery patients should undergo at least six months of non-operative treatment that includes the following (in the appropriate order):
• Rest, avoidance of activity
• NSAIDs, stretching exercise program
• Orthotics: off the shelf or custom
• Cortisone injection (one only)
• Shockwave therapy

Surgery can be open or endoscopic. The principle part of the procedure is release of the plantar fascia near its origin on the heel. Historically only the medial half was released but recent literature supports more complete release.

trusted support and validation from healthcare professionals, peer support from those with lived experience of perinatal depression, and non-judgmental emotional and practical support from their families.
Raising awareness of PNDA is critical, but fortunately there are numerous specialist organisations in Australia who are working to address it. Initiatives like Perinatal Mental Health Week play a vital role in offering information, referral pathways, and reducing the stigma surrounding perinatal mental health. To further support parents in need, over 55 organisations have come together to present the Perinatal Mental Health Support
By Mr Peter Ammon

Open surgery is performed through a 3cm incision in the proximal arch and allows not just plantar fascia release but also decompression of the tarsal tunnel and Baxters nerve which is often implicated in heel pain.
Endoscopic plantar fascia release is indicated for those without nerve compression symptoms and is done through a much smaller incision using a camera assisted cutting device much like a carpal tunnel release.
Both open and endoscopic releases are performed as day cases and require approximately two weeks on crutches. Recovery is slightly quicker for endoscopic patients as you would expect. Patients can expect an 8090% chance of a good result from surgery. Complications are rare.


St John of God Medical Centre
Suite 10, 100 Murdoch Drive, Murdoch WA 6150
Telephone: (08) 6332 6300 Facsimile: (08) 6332 6301 www.murdochorthopaedic.com.au
Each year in Australia, an estimated 100,000 parents will experience perinatal depression and anxiety. Our foundation has delivered over 90,000 appointments to potential, expectant and new parents since our inception.
or call 1300 851 758. We also encourage more organisations and healthcare professionals to collaborate in raising awareness and providing timely support to parents in need at all times of the year.
Finder this year – a valuable resource designed to connect parents with essential support and services during this challenging period.
Each year in Australia, an estimated 100,000 parents will experience perinatal depression and anxiety. It has been highlighted that the perinatal support services we provide contribute an estimated $108.9 million in benefits to clients and the broader community annually, offsetting 12% of the estimated $877 million cost of PNDA, which stems from presenteeism, absenteeism, and increased workforce exit.



Our foundation has delivered over 90,000 appointments to potential, expectant and new parents since our inception. As the leading national provider of perinatal mental health services, we offer up to 10 bulk-billed face-to-face or telehealth psychological treatment sessions per calendar year with an experienced perinatal clinician, alongside our group programs and our online virtual peer led support groups.
If you, or a parent you know, is struggling, support is available. For more information and to find the right resources, visit www.gidgetfoundation.org.au
As the national leading provider of perinatal mental health services, we offer year-long, free, specialist perinatal mental health psychological services, via face-to-face and telehealth; and invest in retention, engagement, and development of more than 175 clinicians through a training, mentoring and supervision workforce development program.
ED: Arabella Gibson is CEO of Gidget Foundation Australia, a not-for-profit that supports the emotional wellbeing of potential, expectant and new parents. Gidget was the nickname of a young mother who took her own life while experiencing postnatal depression. Her family and friends created the foundation to try to prevent it happening again.
We are delighted to announce the expansion of our services at St John of God Murdoch Hospital

Dr. Helen Ballal and Dr. Lee Jackson are joining Dr. Wen Chan Yeow in delivering state of the art breast surgery.
Our well-established unit is dedicated to providing exceptional, patient-focused care through a compassionate and evidence-based approach. We coordinate the entire patient journey with a multidisciplinary team of highly regarded and qualified specialists and a broad range of allied health professionals.
Our comprehensive services include:
Management of malignant and benign breast conditions
Level 1,2 and 3 oncoplastic breast resections
Breast reconstruction
Breast reduction and mastopexy
Assessment and care for individuals with high-risk family histories or lesions
Healthlink EDI: perthsbc | drwcyeow (Dr Yeow only)
Appointment bookings: Phone 9382 4622 | Fax 9382 4611
With regular consulting and theatre sessions at SJOG Murdoch, we ensure that patients are treated in an extremely timely manner.
We are pleased to inform you that Dr. Lee Jackson will also continue to offer consultations in Joondalup.
At Perth Specialist Breast Care, we are committed to guiding you and your patients through every step of the journey with expertise, care, and compassion.
For referrals and appointments, please contact us today.
Murdoch St John of God Medical Clinic Suite 37, Level 1, 100 Murdoch Drive
Genesis Care,
House, 57 Shenton Ave
Advert removed in compliance with Medicines Australia's Code of Conduct and the Therapeutic Goods Administration's Therapeutic Goods Act.
https://medicinesaustralia.com.au/code-of-conduct/about-the-code/ https://www.tga.gov.au/legislation-legislative-instruments

The health system is not immune to wasteful spending. The default position is always more funding is needed, never where we can make savings.
Individuals, families, contractors and businesses all have to work to a budget of some form. If money gets tight expenditure must be reviewed and wasteful spending cut. Equally, as consumers, we expect value for the dollars that we spend.
Government, of course, is different. If money is needed it either raises taxes or prints it. What never happens is a review of how the money is spent and how much is being wasted.
There is simply no imperative to do so and there seems to be no accountability as the finances of government departments are often opaque.
The health system is not immune to wasteful spending. The default position is always more funding is needed, never where we can make savings or where money is being wasted.
Many years ago, there were estimates that one dollar in every three nominally spent on health was spent on administration and bureaucracy. It is almost certainly higher now.
But before health dollars can be redirected, we need to know where they are currently going.
In the US, the National Institutes of Health put out data showing that in 2023 $US9 billion out of $35 billion (25.7%) in research grant money was used for administrative purposes. Some research institutions used 69% for administration. How are we doing in Australia? We need to know. How much money could be freed up to provide actual services if waste was reduced?
For reasons I have never understood, efficiency is not valued in medicine. If I cannot deal with issues more efficiently than 10 years ago, there is something wrong with me. And yes, that comes with experience that cannot be taught but is gained each day. Technology also helps.
Meanwhile in 2023, 26.6% of GPs were aged over 60. With Ahpra seeking to introduce mandatory health assessments for doctors at 70, we will have to become more efficient. But maybe, with better allocation of dollars, we could train and have more doctors.


By Dr Michael Collin, Paediatric Surgeon, Subiaco & Joondalup
There are a number of lesions that occur at, or near, the umbilicus during childhood, especially during infancy. Their natural history and management are dependent on clinical diagnosis.
Persistent paediatric umbilical hernias are caused by the failure of the umbilical cicatrix to scar down and close through early childhood, leaving a defect in the abdominal musculature that allows intraabdominal contents to protrude through the defect into a sac under the umbilicus.
The normal natural history of the umbilicus after delivery involves the Wharton’s jelly surrounding the vessels becoming scarified and the navel formed by the remnant umbilical cord stump.
Beneath the umbilicus, the cicatrix is formed as the small umbilical ring closes and scars down. This process can continue to occur through the first few years of life.
While all babies are born with the umbilical defect, at least 20% will persist clinically through the first year of life, some even getting

Most babies are born with a small umbilical defect that closes in 98% of cases in the first few years, even if it appears to get larger in the first few months
Lesions that are unlikely to resolve include supraumbilical or epigastric defects or remnant embryological structures, persistent polyps and cysts
While the risk of complications from these lesions is small, they can be symptomatic and require formal surgical management.
larger initially. Although 98% will resolve by 3-4 years of age.
Umbilical hernias that persist beyond this period could be considered for repair. Complications are exceptionally rare, with entrapped omental or pre-peritoneal fat much more common than bowel incarceration.
Umbilical hernias may be symptomatic, most commonly with pain, and may also cause issues in adulthood. Families may


elect to observe uncomplicated, asymptomatic umbilical hernias. Repair, if offered, usually involves an infraumbilical incision and primary closure of the defect. Unlike adults, use of mesh in the paediatric population is exceptionally rare.
While an umbilical hernia is most likely to resolve, a supraumbilical hernia is unlikely to do so. Unlike umbilical hernias, which have a concentric swelling of the umbilicus, a supraumbilical hernia can be identified by the bulge creating a more prominent infraumbilical crease with a flattened appearance superiorly (see Figure 2).
To achieve a good cosmetic result, an infraumbilical incision and separation of the cicatrix to access the hernia, with subsequent umbilicoplasty (reconstruction) is preferred.
Epigastric hernias are defects in the linea alba (midline fascia between the recti) that occur in the line between the xiphisternum and the umbilicus. They are often small


and most commonly contain preperitoneal fat from the falciform ligament.
They may be symptomatic even if small. Repair is achieved easily through a small incision over the defect.
A common differential is divarication of the rectus musculature, which occurs with a laxity of the linea alba that causes swelling all the way from the xiphisternum through to the
umbilicus, with the muscle edges visible laterally to the bulge.
There is no actual defect in the linea alba and as the child grows the bulge/divarication should become less pronounced or resolve completely. There is no role for surgical correction of divarication.
Small umbilical granulomas or polyps can form as a result of granulation tissue forming in the umbilicus after Wharton’s jelly fails
to completely scarify. In a general practice setting, a small flat granuloma can be safely managed with cauterisation with silver nitrate sticks, with or without paraffin around the lesion on the normal skin to protect it.
A more polypoid lesion, especially with a narrow base, can be managed with a simple suture ligation. Place a suture tie with double throw or slip knot at the base of the lesion and tighten to ensnare and strangulate the polyp. The lesion should become ischemic and auto-amputate within a week. A failure of outpatient-based management may require surgical excision.
The differential for these granulomas includes lesions related to a persistent vitello intestinal duct or urachus, or a distinct remnant of these. These structures are embryological remnants of the foetal yolk sac and allantois.
Beware of a cherry red appearance of mucosa, discharge from the umbilicus – especially if chyme/ faeculant or urinary in nature – or any clearly patent lumen. A true remnant of these structures will require formal surgical excision.
A cystic lesion within the umbilicus and covered with skin may be a simple epidermoid cyst, although these will also likely benefit from formal excision.
Author competing interests- nil
Results of a recently published WA preclinical study could help clinicians make better informed decisions on the use of noninvasive brain stimulation to treat symptoms in depression and some other neurological disorders.
In shedding light on what noninvasive brain stimulation does to the brain and where changes occur, the research assists in understanding which conditions are most likely to respond well to this form of therapy and which protocols to use.
The study was authored by Perron Institute and UWA PhD candidate
Rebecca Ong and neuroscientist Dr Alex Tang and published in Science Advances
Repetitive transcranial magnetic stimulation (rTMS) is commonly used to study the human brain and as a treatment for a wide range of neurological disorders.
But the neural circuits and molecular mechanisms affected by this form of therapy have been unclear.
“Our preclinical study found that the effect of magnetic brain stimulation is far reaching, affecting multiple neural plasticity mechanisms at and beyond the site of stimulation,” Rebecca Ong said.
“Many more neurological processes were affected than previously thought, and the changes which occurred were specific to individual brain areas and even down to individual brain circuits.”
Dr Tang added: “By mapping what rTMS is changing in the brain and in which neural circuits, we now have a much better idea of how to apply and interpret effects of rTMS.
“The knowledge gained could assist in a more optimised and targeted use of rTMS to manipulate neural circuits in clinical and non-clinical populations.”
By A/Prof Chris Jones, Orthopaedic Surgeon, Mt Lawley & Murdoch
Arthritis is a significant health concern in Australia, affecting over 2.5 million people and accounting for more than $20 billion annually in healthcare costs.
Among the most common forms of arthritis are hip and knee osteoarthritis (OA), conditions that severely impair mobility and quality of life. As life expectancy increases, so does the burden of these conditions with a projected 370% increase in joint replacements by 2030.
Osteoarthritis is a degenerative joint disease caused primarily by ‘wear and tear’. Common symptoms include pain, stiffness and reduced function.
Hip and knee OA are the most prevalent forms, particularly among individuals aged over 70. While mild to moderate cases can often

be managed conservatively, severe OA typically necessitates surgical intervention.
GPs play a pivotal role in identifying OA early. A thorough patient history should explore pain characteristics, for example nocturnal hip pain or knee stiffness, functional limitations and mechanical symptoms such as locking or clicking.
Physical examination is equally critical. Key tests include an assessment of range of motion, the valgus/varus stress test for knee stability and the FABER test for hip flexibility.
X-rays are first-line imaging for both hip and knee OA (Fig. 1). Findings include joint space narrowing, osteophytes, and subchondral sclerosis.





Ultrasound is useful for diagnosing gluteal tendinopathy or bursitis. CT/MRI are reserved for detecting labral tears or subtle OA changes, however MRI and/or CT are rarely indicated for GP referral.
While hip OA is a common cause of groin pain, other conditions may mimic its presentation, including:
• Femoroacetabular impingement: characterised by 'pistol grip' thigh pain
• Stress fractures: consider in patients with sudden onset pain, especially athletes or those with osteoporosis
• Referred pain: lumbar spine pathology often manifests as hip or knee pain.
When in doubt, advanced imaging or specialist referral is warranted.
Knee OA often coexists with other pathologies including meniscal tears, ligament injuries, for example ACL or PCL tears, and patellar tendinopathy.
Differentiating between these conditions requires a combination of history, examination, and imaging.
General practitioners are the first point of contact for patients considering joint replacement. It’s crucial to identify candidates

As the prevalence of hip and knee arthritis grows stay informed about advancements in diagnosis, management, and surgical options
Early intervention and clear communication can significantly improve quality of life for patients with OA
Robotic-assisted surgery is a promising development, offering precision and potentially better patient outcomes.
early, particularly those with persistent pain unresponsive to conservative measures, functional limitations affecting daily activities, or structural changes evident on imaging.
Reassure patients that outcomes are overwhelmingly positive, with over 90% of total joint replacements lasting more than 20 years.
For mild to moderate OA, nonsurgical options can provide substantial relief.
These include:
• Lifestyle modifications: encourage weight loss and low-impact activities
• Medications: NSAIDs, paracetamol and COX-2 inhibitors remain mainstays
• Injections: corticosteroids and viscosupplementation are useful adjuncts.
When conservative measures fail, referral for surgery should be considered (Fig. 2). Options include:
• Total joint replacement: the gold standard for advanced OA
• Partial knee replacement: suitable for unicompartmental arthritis, offering faster recovery and better range of motion
• Hip resurfacing: ideal for younger, active males under 65 years.
Robotic-assisted and technology enabled surgery is revolutionising total and partial knee replacements (Fig. 3).
These systems allow for enhanced preoperative planning using 3D imaging, precise bone resection and implant placement, and
improved alignment which correlates with reduced wear and longer implant life.
Studies reveal that roboticassisted knee replacements reduce postoperative pain and accelerate recovery compared to conventional techniques. Similarly, technology assisted hip replacements have been shown to have improved accuracy and precision of component placement with fewer outliers in terms of leg length discrepancy. Furthermore, technology enabled surgery may lower the risk of complications, contributing to better overall patient satisfaction.
As the prevalence of hip and knee arthritis grows, GPs must stay informed about advancements in diagnosis, management, and surgical options. Robotic-assisted surgery is a promising development, offering precision and potentially better patient outcomes.
Early intervention and clear communication can significantly improve quality of life for patients with OA.
Author competing interests – consultant for J+J Medtech, Enovis, MatOrtho, NavBit.




By Prof Krish Ragunath, Gastroenterologist, Hollywood, RPH & Curtin
Heartburn is a common symptom and about one in five Australians suffer from it. However, not many will be aware that it can cause oesophageal cancer.
Chronic heartburn resulting in reflux of acid and gastric contents leads to the condition called Barrett’s oesophagus (BO).
Australian surgeon Norman Barrett, working in London in the 1950s, first described this condition as a congenitally short oesophagus when he observed gastric type columnar epithelium in the distal oesophagus.
Subsequent research has recognised this as an acquired condition due to chronic gastrooesophageal reflux wherein the distal oesophageal squamous epithelium is replaced by the pre-malignant metaplastic columnar epithelium with intestinal metaplasia.
About 10-15% patients with reflux symptoms undergoing endoscopy get diagnosed with BO and predisposed to adenocarcinoma which is the predominant type of oesophageal cancer in the Western population. Whereas squamous cell carcinoma is more common in the Asian population.
Globally there is an increasing incidence of oesophageal adenocarcinoma (OAC) in the Western world. Barrett’s oesophagus is the only identifiable pre-malignant condition that could account for the increasing incidence of OAC.
It is estimated that 1,742 Australians were diagnosed with oesophageal cancer in 2023 and 1419 died of it. The majority of these cancers were OAC. The overall five-year survival rate is only about 23% making this a killer disease. It is more common in men, with males more than twice as likely as females to be diagnosed with the disease and die from it.
Regular surveillance endoscopy is recommended by national societies including the Australian Cancer Council to monitor and

Key messages
Heartburn is a common symptom that should not be ignored due to its association with oesophageal cancer.
Screen with endoscopy for BO in those with persistent heartburn requiring long-term acid reduction therapy
Screening followed by regular surveillance is the most effective way to combat OAC.
detect dysplasia and early cancer. Surveillance detected cancers are usually at early stage and potentially curable by modern endoscopic treatments or minimally invasive surgery.
While endoscopy is increasingly being performed nationally, with corresponding increase in the diagnosis of Barrett’s oesophagus, the incidence of OAC has not fallen. Less than 10% of patients diagnosed with OAC have a preexisting diagnosis of BO.
It is evident that patients at risk of developing OAC are not diagnosed with BO to undergo regular surveillance. This could partly be explained by the fact that up to 40% of patients with BO do not have ongoing heartburn symptoms

and thus go undiagnosed in the community.
The public awareness to seek prompt medical attention is lacking as well with easy access to overthe-counter antacids to ease heartburn symptoms. Proton pump inhibitors (PPI) effectively cure reflux and heartburn symptoms. It is important that patients with persistent heartburns and reflux symptoms requiring long-term treatment with PPI undergo endoscopy to screen for BO.
The annual incidence of OAC arising from BO is quite small, around 0.1-0.5%. However, the development of low or highgrade dysplasia increases the risk and are currently managed by endoscopic treatments. There is an urgent need to identify risk stratification tools and biomarkers that can identify patients at risk of cancer progression and an effective screening test to identify asymptomatic or minimally symptomatic individuals.
Screening followed by surveillance is the most effective approach to address the increasing incidence of OAC. Currently there are no costeffective proven screening tests in routine clinical practice. However, there are several non-endoscopic approaches to screening that are being researched.
Cytosponge is one such tool that looks promising and multiple studies have been conducted in the UK. Other options include exhaled volatile compounds, oral microbiome alterations and blood-based biomarkers, which are in early phase studies. Artificial intelligence-based risk stratification tools are also under development to identify BO individuals at higher risk of progression to OAC.
Author competing interests – nil
By Dr Reshad Mirnour, Specialist Pain Medicine Physician, Ardross
Pain is a prevalent and significant concern in cancer patients, warranting careful attention and management. Pain can happen at any stage of the disease and like any other pain condition, a sociopsycho-biomedical approach needs to be considered.
A multidisciplinary setting is often necessary, involving the patient’s general practitioner, pain specialist, palliative care physician, radiation oncologist, surgeon and allied health.
In patients with cancer, pain may arise directly from the disease itself, such as the mass effect of a tumour, or indirectly as a consequence of cancer, for example pathological fractures, or its treatment, such as chemotherapy-induced peripheral neuropathy.
Perhaps the first step of pain assessment in cancer is to determine the prognosis which can significantly influence the management. Cancer is a lifechanging diagnosis, and therefore, psychological and environmental pain contributors should be carefully explored and managed as well as any biomedical factors.
Addressing patients' immediate and long-term psychological, social and existential needs is a crucial part of holistic pain management.
Pharmacotherapy should include multimodal analgesia including opioids, non-opioid analgesics and anti-neuropathic agents. Although opioids are no longer recommended for chronic non-cancer pain, they are one of the most frequently used medications in cancer pain as well as the most effective ones.
Morphine, an old opioid, and codeine are two medications that are recommended in the WHO guideline for cancer pain treatment (the WHO analgesics ladder). However, there are many other opioids with different mechanisms and routes of administration which include oral, rectal, sublingual, transdermal and injectables (e.g., intravenous, or subcutaneous) and intrathecal.
Holistic care is key: Cancer pain needs a multidisciplinary approach addressing medical, psychosocial and existential factors
Opioids need caution: Effective for cancer pain but require careful use in long-term survivors
Multiple pharmacological and non-pharmacological options are available to improve quality of life and possibly cancer survival.
The oral route is the most common method of delivering opioids to cancer patients as it is less invasive and, therefore the most preferable. The transdermal route is suitable particularly for longer-term pain relief and in situations when the use of oral medication is not possible.
The new generation of opioids such as tapentadol and buprenorphine are considered safer options than conventional opioids, particularly with a longer survival when the opioids are considered for a longer period. However, caution should be practised when opioids are prescribed in patients with cured cancer as the ongoing chronic pain may no longer be considered ‘cancer pain’. In such cases, or when long-term remission is expected, an appropriate weaning plan is necessary
Apart from the quality of life, pain and related stress can promote the progression of cancer. Based on the current evidence, 19 out of 20 patients treated with opioids for their cancer pain, report their moderate to severe pain is reduced to mild or no pain. Interestingly, only one in 10 people treated with these medications, have to change or stop them due to side effects.
The side effects include nausea, vomiting, opioid-induced ventilatory impairment, cognitive impairment, opioid-induced hyperalgesia, constipation, drowsiness, itching, tolerance, dependency and addiction. Although opioids are the most effective cancer pain

medications, neuropathic pain is usually resistant to opioids and other medicines are often prescribed for its management.
There is a general concern about the effect of opioids on the progression of cancer. This is a controversial subject and while some animal studies show opioids can enhance the progression of cancer, others show an improved overall survival following treatment with opioids, probably due to improved compliance with cancer treatment and better quality of life. Generally, we need more research in this area to have a better understanding of the role of opioids on cancer outcomes.
There are non-analgesic medications that can be used as part of pain management in cancer patients. Monoclonal antibodies have been used to treat bone pain from cancer metastasis and currently denosumab is PBS-subsidised for such indications in breast cancer.
In terms of non-pharmacological options, pain procedures can provide excellent pain relief while minimising the side effects of opioids. Examples are coeliac plexus block or ablation, sympathetic ablation, intrathecal pumps, and peripheral nerve blocks. Moreover, radiotherapy can be an effective non-pharmacological strategy for bone pain.
In summary, cancer pain is a manageable issue that needs early intervention to improve patients' quality of life and compliance with cancer treatment. Multiple pharmacological and non-pharmacological strategies are available to manage this undertreated condition. The use of opioids in cancer survivors should be assessed in the same manner as in patients with chronic non-cancer pain.
Author competing interests – nil
By Mr Bradley Roberts, Perron Institute & UWA, and Professor Sean Hood, Perron Institute, UWA and SCGH
Researchers at the Perron Institute for Neurological and Translational Science have recently launched the GENE-YD study, an innovative trial exploring the benefits of pharmacogenetic testing to optimise antidepressant pharmacotherapy in young Western Australians.
This pilot randomised controlled trial aims to explore the feasibility for a larger trial in WA to improve treatment outcomes through personalising patients’ antidepressant prescriptions, helping young people achieve symptom relief faster with fewer medication-related side effects.
Major Depressive Disorder (MDD) is among the leading causes of disability in Australian youth, with a rising number of young people seeking treatment and support for their mental health each year.
Antidepressants are often a first-line treatment for those suffering from moderate to severe depression, and with the prevalence of MDD rising so too are prescription and consumption rates of antidepressant
medications. Between 2015 and 2019, antidepressant use increased by 16% in Australians aged 1024 years – a rate likely to have climbed further since the COVID-19 pandemic.
GPs are at the coalface of MDD treatment with over 85% of antidepressant medications prescribed in primary care settings. These medications are often prescribed using a clinical trial-anderror approach, with adjustments based on patient initial response or side effect presentation.
This process can be particularly challenging for young people, who may become discouraged by unsuccessful attempts to find the right medication, often choosing to cease treatment without informing their mental healthcare professionals, friends, or family.
The traditional antidepressant prescription model has been associated with a reduction in antidepressant treatment response by up to 20% come the second drug trial and up to 32% come the third and fourth.


Furthermore, the likelihood for symptom remission drops to 14% when patients start their third antidepressant drug trial, with side effects presentation more likely with each subsequent medication.
Given these limitations, new methods of prescription are required to ensure all young people exploring antidepressant medication are given the best chance for a therapeutic outcome. Pharmacogenetics, or PGx, is the study and application of how common genetic variance may influence the way in which we metabolise and respond to drugs. By understanding the variance in key genetic markers, clinicians may be better informed on medications and doses best suited to individual patients, potentially shortening the time to symptom relief and reducing the need for multiple drug trials.
PGx testing requires the collection of a DNA sample, often via a simple cheek swab, to identify and characterise genetic markers associated with drug metabolism. For antidepressants, drug-

Key messages
A new WA trial is investigating the utility of genetic testing to improve treatment outcomes in youth depression
Genetic markers for drug metabolism are being evaluated to optimise antidepressant pharmacotherapy and provide more personalised care
The GENE-YD study is actively recruiting people aged 16-24 years with a history of MDD who are seeking antidepressant treatment.
metabolising enzymes such as CYP2D6 and CYP2C19 play critical roles in how individuals process medications.
Simply put, an upregulation of these genes may result in metabolising drugs quickly, reducing antidepressant efficacy. Alternatively, metabolising drugs slowly due to a downregulation of these genes may result in increased risk of drug toxicity and medication-related side effect presentation. PGx testing reveals
these insights prior to treatment commencement, guiding informed prescription decisions.
In the Perron Institute GENEYD study, WA researchers are taking a pre-emptive approach to PGx-informed care, investigating how proactive PGx testing in the early stages of mental healthcare impacts antidepressant response and treatment outcomes in young people with MDD.
The GENE-YD study is actively recruiting up to 80 participants aged 16-24 years who have been diagnosed with MDD and are considering either starting or adjusting their antidepressant prescription.
Participants in the study will undergo a PGx test to identify specific genetic markers linked to antidepressant response. This will allow the research team to provide participants’ GPs with an antidepressant treatment guide, written by psychiatrist and GENEYD Chief Investigator, Professor Sean Hood.
The goal of the GENE-YD study is to improve the efficacy of

antidepressant pharmacotherapy for young people suffering MDD. By using PGx screening to identify optimal treatment plans, we hope to increase the likelihood of achieving symptom relief with the first prescribed medication. This trial also aims to assess the utility of PGx in reducing medication-related side effects, improving medication adherence and quality of life. As the GENEYD study is a pilot trial, results and participant feedback will help to inform a larger RCT to further explore the use of PGx in youth psychiatric primary care.
ED: For more information, email the Perron Institute PGx research team on PGx@perron.uwa.edu.au or visit www.perroninstitute.org/clinics/ clinical-trials/youth-mental-healthgene-yd-project
Author competing interests – the authors are involved in the study.


Garden City Specialist Centre 537 Marmion Street, Booragoon WA 6154

Surgeons House 162 Cambridge Street, West Leederville WA 6007

Mandurah – 360 Health 10/3 Dower Street, Mandurah WA 6210


By Professor Belinda Beck, Griffith University
Osteoporosis is a significant global health challenge leading to an increased risk of fragility fractures, loss of independence, and reduced quality of life.
While pharmacological interventions can play an important role in managing osteoporosis, exercise offers a vital non-pharmacological strategy that provides additional benefits such as improved balance, functional capacity and overall health.
An evidence-based exercise program specifically designed to combat osteoporosis by enhancing bone density and reducing fracture risk is the new gold-standard of treatment.
This treatment is grounded in research, including the LIFTMOR (Lifting Intervention for Training Muscle and Osteoporosis Rehabilitation) and MEDEX-OP (Medication and Exercise for Osteoporosis) trials, conducted at Griffith University and The Bone Clinic.
These studies demonstrated that postmenopausal women and older men with low bone mass could safely perform high-intensity resistance and impact training (HiRIT), resulting in significant improvements in bone mineral density (BMD), muscle strength and functional performance.
These findings challenged the long-standing misconception that individuals with osteoporosis should avoid high-impact or heavy-load exercises.
Bone tissue responds to mechanical stress through a process called mechanotransduction, wherein the cells within the bone sense strain and initiate remodelling to adapt to the load. However, not all forms of exercise stimulate bone growth effectively.
Bone loading requires clinically supervised exercises that involve:
• Exercises performed with heavy weights to stimulate the skeletal system
A new program can improve bone health and reduce fractures in osteoporosis
The program emphasises highintensity resistance and impact training under expert supervision It is proven to offer a safe, effective strategy for people to take an active role in managing osteoporosis.
• Impact loading – activities that create ground reaction forces sufficient to elicit bone adaptation These principles are central to the design of any beneficial program, ensuring optimal bone health outcomes while maintaining participant safety.
Program delivery must be under the supervision of accredited exercise physiologists, physiotherapists, or other appropriately trained and accredited exercise medicine professionals to ensure safety and efficacy.
Participants undergo an initial assessment to determine their baseline bone health, functional capacity, and risk factors. Based on these findings, they then initiate the exercise program according to their individual capacity keeping the following principles in mind:
• Progressive overload: gradually increasing the resistance or intensity of exercises to continue stimulating bone and muscle adaptation
• Proper technique: emphasising correct form/movement pattern to minimise injury risk while maximising load on the skeleton
• Targeted exercises: prioritising weight-bearing activities that load the hip, spine, and other critical fracture sites
• Injury prevention: incorporating balance and functional training to reduce the likelihood of falls, which are a major contributor to osteoporotic fractures.

The benefits of an exercise program extend beyond improved BMD. Participants often report enhanced physical strength, better posture and increased confidence in performing daily activities.
The program also addresses comorbidities associated with osteoporosis, such as sarcopenia (age-related muscle loss), and contributes to overall functional independence.
A common misconception is that individuals with osteoporosis should avoid high-intensity or high-impact exercises due to fracture risk. However, research has demonstrated that when appropriately prescribed and supervised, these exercises are not only safe but also necessary for bone health.
The program bridges the gap between evidence and practice, empowering individuals with osteoporosis, or those at risk of developing it, to take an active role in managing their condition.
Healthcare practitioners play a crucial role. Referring patients to accredited exercise professionals and educating them about the benefits of bone-loading exercises are essential steps.
Furthermore, a program needs to align with current clinical position statements that recommend exercise as a first-line treatment for osteoporosis prevention and management.
Empowering patients with the tools and knowledge to enhance their skeletal strength, offers a pathway to healthier ageing and improved quality of life. Exercise programs have the potential to significantly reduce the societal and economic burden of osteoporosis.
Author competing interests – Creator ONERO Program, owner and Director of The Bone Clinic.
By Dr Vanitha Budhavaram, Breast Surgeon, Joondalup & Midland
Breast cancer is often thought of as a disease associated with older women, however, recent studies indicate an increased incidence in women younger than 40.
Early onset of breast cancer poses unique challenges in terms of detection, treatment, psycho-social impact and long-term outcomes. This trend reflects a growing global concern, as the prognosis in these women is poorer when compared to their older counterparts.
In Australia, one in 10 women with a breast cancer diagnosis are under the age of 40.
The cause of breast cancer in young women is attributed to hormonal, environmental and lifestyle factors. A significant number of breast cancers in young women are linked to genetic mutations like BRCA1 and BRCA2 genes.
Women with these mutations have a high lifetime risk of developing second breast cancer and ovarian cancer. Family history, risk stratification and genetic counselling is important to devise treatment strategies for these women.
Younger women often present with advanced disease as detection of breast cancer is delayed. Often the lumps are overlooked or attributed to a benign lesion. Misinterpretation of symptoms or lack of awareness contributes to delayed diagnosis, especially in pregnant and lactating women.
Younger women fall outside the routine surveillance programs. Further complicating the scenario, conventional imaging may obscure findings due to dense breasts.
Contrast mammogram and/or MRI Breast are required in addition to conventional imaging for diagnosis and staging. Breast lumps in any age group should be subjected to triple testing which includes clinical examination, imaging and biopsy.
Discordant lesions present a diagnostic challenge leading to missed malignancies. When imaging findings do not correlate
Key messages
Breast cancer in women younger than 40 is on the rise
Triple assessment is mandatory for investigation of breast lump in any age group
Early detection leads to better outcomes.
with pathology results, it is important to revisit the diagnosis in a multidisciplinary team, perform additional investigations and surgical excision biopsy.
Younger women with breast cancer require specialised care and personalised treatment plans. They are likely to have aggressive sub types of breast cancer such as HER2 amplified or triple negative breast cancer.
They are also more likely to have chemotherapy which can adversely affect fertility. Collaboration with fertility specialists for egg harvest and preservation is imperative before commencement of treatment.
Recommended treatment may include double mastectomy in patients with genetic predisposition. This can affect body image, sexual life, breast feeding and timing for future conception.
Diagnosis of breast cancer at a younger age significantly impacts mental health, relationships and career plans. They are also at risk of long-term side effects of treatment such as early menopause, osteoporosis, cardiovascular disease and second cancers.
Management strategies for breast cancer in younger women require a tailored approach, multidisciplinary care, long term survivorship strategies and support. Advanced imaging, genetic testing and tumour genomic profiling are required for treatment planning.
Surgical management depends on tumour breast ratio, genetic results and patient preference. Breast conserving surgery requires adjuvant

radiotherapy to achieve an optimal oncological outcome.
Several techniques such as level 1 or level 2 oncoplastic procedures using volume displacement and replacement techniques, therapeutic mammoplasty, and partial breast reconstruction using local perforator flaps can be used to achieve safe oncological outcomes with good cosmesis.
Neoadjuvant therapies have helped in shrinking the size of tumours to enable breast conservation in a certain sub-set of patients.
Patients preferring mastectomy or those not suitable for breast conserving procedures can have immediate or delayed reconstruction using autologous free flap reconstruction or implant reconstruction. Alternatively, some patients prefer to “go flat”.
De-escalation strategies in breast and axillary surgery have shown improved outcomes with the concept of “less is more”. These strategies reduce the intensity of the treatment without compromising its effectiveness. Targeted axillary dissection is used in eligible patients with axillary nodal disease to assess response to neoadjuvant treatment, thereby reducing lymphoedema rates in young women.
Breast cancer in younger women presents a unique set of challenges that require a multidisciplinary and personalised approach. Diagnostic delays, biological aggressive tumours and genetic factors coupled with psycho-social and reproductive implications of the disease contribute to challenges in treatment.
Advances in imaging, surgery, targeted therapy, radiation techniques, lymphoedema interventions and supportive care have helped improve outcomes. GPs, multidisciplinary collaboration and allied health support are essential in providing the comprehensive care these young women deserve.
Author competing interests – nil
By Dr David Lim, General & Breast Surgeon, Mt Lawley
Breast cancer remains a challenging diagnosis, transforming many aspects of patients’ lives beyond physical health.
Breast cancer was mentioned in the first known surgical text, known as the Edwin Smith Papyrus (named after the American that acquired it in 1862). This Egyptian document dated circa 1600 BCE described 48 cases of various pathologies and how to deal with them in a practical and rational way.
Case 39 in this text described a swelling in the breast as: “the disease was cool to touch, bulging and spread all over the breast”. This was deemed incurable.
Hippocrates, a forerunner in separating medicine from religion, coined the term ‘karkinos’ which eventually led to ‘carcinoma’. He also misguidedly propagated the humoral theory that diseases arose from an imbalance of four ‘humors’ within the body (blood, phlegm, black bile and yellow bile). Cancer was thought to be an excess of black bile.
Galen, another figure of equal fame in antiquity, also supported humoral theory. In surgical treatment of the disease, he discouraged cautery to remove excess black bile through bleeding.
Horrific surgical practices were utilised over the years by surgeons in futile efforts to treat breast cancer, with instruments devised to extirpate the breast in a rapid and efficient manner, of utmost importance in the era before anaesthesia.
The 19th century witnessed the birth of anaesthesia (Seishu Hanoaka in 1804 and William Morton in 1846). Joseph Lister in the 1860s pioneered antiseptic surgery, applying the research of Louis Pasteur.
Countless advancements and brave innovations were made in


surgery. Many individuals made contributions that were no less significant than those mentioned here.
Despite this optimism, mortality of breast cancer remained high and the prognosis from breast cancer was grim.
“Most of us have heard our teachers in surgery admit that they have never cured a case of cancer of the breast,” - William Halsted.
William Halsted is considered the father of modern surgery and is one of the founders of the Johns Hopkins medical school. His contributions include the “Tenets of Halsted” to be used in surgery – this includes gentle handling of tissues, meticulous haemostasis, preservation of blood supply,
strict aseptic technique, minimum tension on tissues, accurate tissue apposition and obliteration of dead space. All the above are still principles adhered to.
He published his landmark paper in 1894 on the outcomes of 50 patients with breast cancer that he treated with a radical mastectomy. This operation excised the entire breast, regional lymphatics and pectoralis muscles. Although mutilating and morbid, Halsted’s paper reported significantly improved recurrence rates compared to contemporaries.
For many who had surgery alone, long-term cancer-free survival remained elusive, but radical mastectomy became the gold standard for many decades, disseminated by Halsted’s disciples near and far.
Breast cancer surgery has evolved over centuries
Today there are many surgical options
Treatments continue to be refined and improved.
The development of chemotherapy, radiotherapy, breast imaging, gene testing, screening, hormone therapy, targeted therapies and breast awareness drastically changed the face of breast cancer outcomes in the latter half of the 20th century.
During this time, surgeons revisited their practices. Large RCTs demonstrated equivalent survival rates with lumpectomy and radiotherapy. Although not suitable for every patient, breast conservation became possible without compromising cancer treatment outcomes.
Donald Morton, in 1992, developed a technique for sentinel node
biopsy in melanoma treatment. This was evaluated in breast cancer, eventually replacing axillary clearance in staging the axilla in clinically node-negative patients.
Breast cancer surgery and the development of oncoplasty as a subspecialist craft group was born in the 21st century.
Today, there is a huge array of oncoplastic techniques that facilitate breast conservation. Where not possible, reconstruction with implants or autologous techniques are available for suitable patients that desire it.
Neoadjuvant systemic treatment (NAST), including recent breakthroughs in targeted and immunotherapies, has further allowed refinement of surgical options. Downstaging of the primary tumour facilitates breast conservation.
In some settings, positive lymph nodes may no longer mandate axillary clearance after NAST, as other methods, such as targeted axillary dissection (TAD), can
be used to evaluate treatment response in the axilla.
Today, within a multidisciplinary team, surgery remains indispensable in breast cancer treatment. However, patients would tell you that it is only part of an arduous and intrepid journey.
It is impossible to overstate the vital role played by breast nurses, support and advocacy groups, physiotherapists, social workers, psychologists, occupational therapists, genetic counsellors, community nurses and, of course, family and friends.
We are a far cry from the bygone days of desperate and mutilating surgery, but there is no doubt that breast cancer surgery will continue to achieve more for our patients as it evolves in its role and techniques.
Author competing interests – nil





Meet Eric Bauza, the iconic voice from some of the Looney Tunes most-loved characters –Bugs Bunny, Daffy Duck and Porky Pig.
By Ara Jansen
If Eric Bauza did his class work, he was allowed to get on the school PA and tell a joke or do an impression.
Ever the class clown, he became that guy who got on the mic at assemblies, rallies and before sports events showing off his impressions of late-night television characters or the likes of Ace Ventura, Forrest Gump and the cartoon characters he loves so much.
It paved the way for an eventual career as an award-winning voice artist – and these days voicing some of the screen’s most well-known and loved characters Bugs Bunny, Daffy Duck, Porky Pig, Tweety and Marvin the Martian.
“My family were relieved when they found out I wasn’t crazy and all these voices would lead to a paycheck and a career,” laughs Eric as he delivers the last part in one of his famous voices.
“They know how important it is to me and how much it affects my life. I would still be a big fan of all these characters even if I wasn’t part of this heritage.”
However, they are still not thrilled with his fashion sense – a constant parade of cartoon T-shirts, honouring the characters he loves.
“It has been an amazing career so far, both in the opportunities I have had and the people I have met and worked with. I just can’t help but want to share that.”

The 45-year-old Filipino Canadian now lives in LA. He hails from the Toronto district of Scarborough and shares his birth town with the likes of actors Eric McCormack and Mike Myers, filmmaker and Elton John’s husband David Furnish and musicians The Barenaked Ladies and The Weeknd, amidst a long list of famous types.
A two-time Children and Family Emmy winner, Eric owns a long list of television, film and commercial credits dating back 20 years, including Marvin the Martian for Nike’s Air Jordans.
He’s also the voice star of the new big screen animated sci-fi comedy adventure Looney Tunes: The Day the Earth Blew Up which opens this month.
The world is facing an alien invasion. The only hope is a stuttering duck and his porcine best friend. Somehow cartoon characters Porky Pig and Daffy Duck are just the animals to foil the plot and save everyone from a mysterious new bubble-gum flavour and the villain who wants to take over the world.
In the movie Eric voices best friends Porky Pig and Daffy Duck, Candi Milo voices Petunia Pig and the alien is Ally McBeal actor Peter MacNicol. Porky and Daffy are a highly energetic odd couple, constantly talking, yelling and panicking while trying to save the world.
“The energy is a big part of these performances no matter how subtle or extreme they are. It’s a balance and each character is as hard to do as the other.”
He says it was a challenge doing both Porky and Daffy as they talk to each other, dialogue whipping quickly between them.
What’s also challenging is that all these years later, Eric is also
responsible for sometimes speaking new or modern words for the characters for the first time; ones that that weren’t in their vocabularies decades ago or when Mel Blanc was originally voicing them.
The movie has taken four years to complete and has kept the 2D legacy hallmarks of a Looney Tunes cartoon.
“It’s almost like an indie film, that people are going to discover when they see it. It’s not that common anymore and that’s good. It’s like a renaissance,” Eric says.
Being back on the big screen this year is like a return to when Looney
Tunes cartoons were shown in cinemas from the 1940s to 1970s, but instead the main feature.
“I think people can use a good laugh right now, thanks to the state of things and life in general. It’s nice to be able to turn your brain off and laugh along with other people and with loved ones,” Eric says.
“It’s a great honour to have had the opportunity to voice these characters. It’s like stepping into my first day of school all the time. I never feel stale, which is a great thing.”
While he might be the voice of some of the world’s most famous cartoons, not everyone is convinced. Eric says his young son’s friends think he only does a fair impression and do not actually believe he’s the real deal.
“Ba-deep, ba-deep, that’s all folks!”
Looney Tunes: The Day the Earth Blew Up opens in cinemas March 27.

Beep, beep! Win tickets to Looney Tunes: The Day The Earth Blew Up
Want to see the new Looney Tunes movie?
We’ve got five double passes to Looney Tunes: The Day The Earth Blew Up to give away.
The tickets will be valid across all major cinema chains including Hoyts, Event and Reading.
To enter, use the QR code on this page or go to mforum.com.au and hit the competitions tab.

The iX1 BMW EV drives effortlessly and will get you from A to B smoothly, writes Dr Mike Civil.
As I drove my 2018 Series 76 Landcruiser to the BMW dealer, I realised I was going to be driving a car at the other end of the tech spectrum.
The iX1 BMW is a fully electric vehicle. It was not my first test of a BMW EV, but somehow the contrast seemed greater today.
My dinosaur ‘Troopie’ is from a very different era and style with five gears, three pedals, diff locks and it’s a polluting diesel V8. The iX1, on the other hand, is bang up to date – and it shows.
I wandered around the show room and was struck by how cars just seem to be getting bigger. It doesn’t make much sense to me, when we are trying to have less environmental impact.

Fortunately, the iX1 was svelte and trim. It is the base model, so only a two-wheel drive, there’s no electric adjustment for the seats, but there is a metallic choice of white paint.
Don’t get disheartened by the term ‘base model’ – being a modern BMW it comes with all the expected electronic accompaniments. There’s a clear display for the driver showing speed and range, and then a centrally mounted display for any comfort setting you want in the car, like media centre or navigation. It’s all push button or touch screen.
My first test came when the friendly staff member handed over the keys and left me to it. Would I be able to figure out how to get things into motion without an embarrassing “hold on a minute…”?
It is an important test, to assess how intuitive the car is. Fortunately, the Beemer passed first time.
After a brief check on the dash, all is clear and I’m good to drive. The car effortlessly glides away with no sound whatsoever. I know I should expect that, particularly at slow speeds, but it is still a little unnerving. I am so last century.
The driving position is excellent, there’s great visibility, the cabin is comfortable, aircon is efficient, it’s all so effortless.
Just one kilometre down the road and the most I have had to do is make sure that the car and I are pointed in the right direction. In Troopie I would have likely been through all available gears with both feet and hands involved.
After negotiating my way out of the city, I head towards the Perth


Hills with more effortless gliding. The drive quality is excellent, like smooth silk. The acceleration is brisk and with no fuss.
There are three driver modes to choose from: Efficiency, Sport and Leisure. Efficiency seems to only add a couple of kilometres to the range, but this was a limited test today. As usual, Sport is more fun, but Leisure is a good balance.
The range today was around 320km, and presumably that was a full charge. There is a 4-wheel drive version with greater performance but less range.
I won’t need anywhere near that 300km mark today, but needless to say, the Beemer comes with various charging cables to avoid getting stranded. I’m sure that ‘range anxiety’ issues will get better as I get used to using electric vehicles, but despite the inability to consider things logically it is still an issue. A mindset thing most certainly, but real all the same.
So, all in all, it is a typically well made, efficient, electric BMW that will get five people comfortably, efficiently and quietly to their destination. The car does not yell “I’m an EV”, it is primarily a BMW that just happens to be electric. So, what’s not too like?
Perhaps, if you enjoy driving for driving, you may be less inclined to go for an EV. The effortlessness of the whole experience felt like a small disappointment to me. I drive because I enjoy it, it is all very tactile for someone like me. I like feeling the car change gear and hearing it talk to me.
It’s not just about exhaust notes, there are other sensory messages like smells and changing temperatures that don’t exist on an EV. Buying an EV is a big decision, they are not cheap, so, for me, they do need that elusive character.
But, at the end of the day, EVs like this excellent Beemer get you from A to B really well.

Perth welcomes back the much-loved Alliance Française French Film Festival and this year’s films offer a bit of everything from a classic re-imagined and French box office hits, to family flicks and compelling dramas.
What do the Netflix hits Emily in Paris and mystery series Lupin, last year’s Paris Olympics and the recent win of a Grammy for French metal band Gojira for their opening ceremony performance have in common?
They have all sparked an increased interest in France and all things French, whether it’s beautiful scenery, a tourism boost, music, food, language lessons or Emily and Mindy’s endlessly chic wardrobes paraded in iconic locations.
Alliance Française de Perth general manager Thomas Feldstein hopes that regard and curiosity translates into a new audience coming to this year’s Alliance Française French Film Festival.
“The festival is a great way for us to reach a different audience,” Thomas said.
“It enables us to go wider than just our students. I love being able to meet up with new people and discuss the films.”
He adds that one of the joys of his job is to be able to see and discuss each year’s movies.
“It’s amazing to see how French
By Ara Jansen
cinema is so beloved by Australian audiences. Every year I have been struck and amazed by this. I meet so many people who don’t speak French but just love the culture or want to enjoy the scenery on the big screen. It’s so heartwarming.”
Because of his job with the Alliance, it has been 13 years since Thomas left France. While he has visited, he says the festival comforts the part of him that misses home. Thomas’ fouryear term in Perth is up later this year and he and his family will be landing in the Loire Valley, the first time his kids will be living in France.
Each year the festival reminds us that French cinema loves a good story. Whether it’s the biopics of Monsieur Aznavour or The Divine Sarah Bernhardt, the reimagining of the Dumas classic The Count of Monte Cristo or the very real drama of a young courier waiting for his all-important and life-changing residency interview in The Story of Souleymane
“The festival movies cover a lot of topics, many of them universal but there are many which are also uniquely French, or things French cinema likes to explore.”
There are 42 films to see this year including Cannes highlights, screen sirens, impossibly true stories and France’s biggest box office hits.
They also love a good classic. The Count of Monte Cristo, based on the 1844 novel, is the 11th retelling and it includes two miniseries and countless other movies based on or around the story. This thrilling new adaptation sold 10 million tickets in France.
That contrasts with the tasty, heartwarming and fun for all, All Stirred Up! (Tous Toques) as Victor, a French chef, has the contents of his car confiscated at the Quebec/ US border by an unyielding customs officer. The officer must then enlist Victor’s help for her daughter to win a cooking competition, despite barely being able to cook.
The Alliance Française French Film Festival runs from 13 March – 16 April in Perth at Palace Raine Square, Luna Outdoor, Luna on SX, Luna Leederville and Windsor Cinema. Selected films will also be screened in Bunbury from 10-13 April.
This page intentionally left blank


Consult rooms available for sessional rental – suitable for specialists or allied health
4 strategic locations in Nedlands, Bentley, Mandurah and Geraldton
•Nedlands – Hollywood Specialist Centre, suite 23, 95 Monash Ave
•Bentley – unit 3, 10 Mills St
•Mandurah – unit 7, 21 Sholl St
•Geraldton – 9 Urch St, Beresford
For more info, contact practicemanager@apollocardiology.com.au or 6166 3737 Website link https://apollocardiology.com.au
Hollywood Medical Centre Suite 36, First Floor, 85 Monash Avenue, Nedlands
87sq m – fully fitted, large reception, 2 consulting, 2 treatment & 2 store rooms.
Contact: Irene 0409 688 339
MARGARET RIVER – GNARABUP (DPA/MM4)
VR General Practitioner
– Full-time or Part-time
We’re looking for a VR GP to join our growing practice overlooking the ocean in idyllic Gnarabup.
Flexible working options are available to suit a new lifestyle Down South by the beach.
Vitality GP has been part of the community since 2022. Our fully accredited practice comes with onsite podiatrist, physiotherapy and nursing support, a friendly team, and brand-new, well-appointed facilities.
Please email resume to alison@vitalitygp.com.au
Contact: Dr Alison Lyons 9757 1022 www.vitalitygp.com.au

Doctor Opportunity at The Woods Medical Centre
We are looking for an enthusiastic and experienced GP to join our growing team.
The Ideal Candidate:
Strong General Practice Skills:
•Proven experience in providing highquality patient care across a diverse range of medical conditions
•Excellent clinical skills and a commitment to preventative healthcare
•Experience in managing chronic diseases effectively
•A keen interest in skin cancer management preferred but not essential. We offer a unique opportunity to combine comprehensive general practice duties with an opportunity to develop skin cancer screening and procedures for that candidate with skin cancer management interest.
Team Player and Communicator:
•Ability to collaborate effectively with a supportive team of healthcare professionals.
•Excellent interpersonal and communication skills to build rapport with patients.
Essential Requirements:
•FRACGP qualification
•Vocational Registered
•AHPRA registration.
What We Offer:
•Supportive and friendly work environment with a focus on work-life balance
•Nursing support
•No weekends or afterhours work
•Modern facilities and equipment
•Best Practice software
•Mentorship and training opportunities should you wish to develop skin cancer management skills
•Opportunity to work alongside experienced practitioners in a collaborative setting
•A location that is not far from the beach.
For more information or a confidential chat, please contact our Practice Manager at 0478 021 910 or email practicemanager@thewoodsmedical.com.au

Silver Sands General Practice
Exciting Opportunity for a Full-Time or Part-Time VR General Practitioner in Mandurah!
Are you a passionate and dedicated
VR General Practitioner looking for a rewarding opportunity in a familyfriendly environment? Look no further!
Silver Sands General Practice is one of the longest standing medical centres in Mandurah, and we are actively seeking a talented GP to join our dynamic team on a contract basis.
Our practice is committed to providing high-quality, patient-centred care to individuals and families. Our team is supportive, collaborative and dedicated to creating a positive work environment.
Requirements:
•MBBS
•Current general / specialist registration with the Australian Health Practitioner Regulation Agency (AHPRA)
•FRACGP or FACRRM qualifications or active enrolment with the training program
•Medical Indemnity Insurance
•Commitment to providing high quality patient care
•ABN as an independent GP Benefits:
•Competitive remuneration package at 70% of billings (30% service fee)
•Supportive and collaborative team environment
•Flexible working hours. Ideally 4-5 days per week +/- nursing home visits if desired
•Mixed billing
•Replacing outgoing GP with full books
•Large existing patient base with great billing potential and rewarding continuity of care
To apply, please submit your resume and cover letter to office@silversandsgp.com.au

MOUNT
General Practitioner
$200 – $300 per hour
6-7 sessions available.
Excellent working environment, with modern facilities.
Quality nursing staff and an onsite non dispensing pharmacist.
Adjacent to the practice we have a pharmacy, and allied services, consisting of audiology, pathology, physiotherapy, podiatry, dental, and cardiology.
Visit our website: www.thirdavenuesurgery.com.au
If interested contact Practice

Palin St Family Practice is a small privately owned GP located in Palmyra which has been continuously operating since 1923.
We are looking for a VR doctor and provide a supportive administrative and nursing team in a fully accredited practice.
Our patient base is well established, and you would have an immediate patient list on commencement.
For further information
please contact Jackie our Practice Manager on 0403 343 401 or via email office@psfp.com.au

Earn 100% of Billings for the First 3 Months!
Join our well-established, accredited mixed-billing clinic in Burswood and earn 100% of billings for the first 3 months (75% thereafter).
Perfect for new VR GPs looking to establish themselves, with full-time/part-time options.
Work alongside 3 experienced GPs in a fully computerised clinic with on-site pathology and RN support.
Please contact Dr Ang on 9472 9306 or Email: info@thewalkingp.com.au

GP Opportunity at South Lake Family Practice.
We are looking for an enthusiastic VR GP to join our team.
Full time / Part time VR GP. Flexible hours. 75% and minimum guarantee for first 3 months. Onsite pathology & Allied Health. Day and after hours shifts available. Ability to do Women’s health and procedures preferred.
For further information please contact p.manager@southlakefamilypractice.com.au ph: 08 9417 1009
Contact Paul, paul@mforum.com.au or phone 9203 5222 to place your classified advert
Manager Rachael Hadlow via email: rhadlow@3rdave.com.au
paul@mforum.com.au (08) 9203 5222
www.mforum.com.au

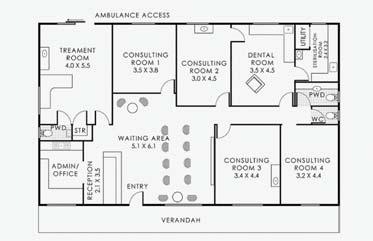




Joondalup Campus is seeking expressions of interest from vocationally registered general practitioners
WHAT WE OFFER
15% service fee
Mixed billing
Free, reserved parking
Full time registered nurse and practice management support
Exceptional administrative support team.
The ECU Health Service assists students, staff and the university community with their health care needs. The primary function of the service is to provide students with psychosocial and physical health support, so that they may achieve an optimal academic performance for the duration of their studies.
In providing comprehensive patient healthcare, our medical practitioners will consider and respect patients’ rights, identity, body diversity, beliefs, language, religious and cultural backgrounds.
WHERE WE ARE
Located within the Wellbeing Precinct on the ECU Joondalup Campus, our AGPAL accredited student psychological services, with a coffee shop and free parking close by.
Availability for four to six GP sessions per week
We are open Monday to Friday, 8.30am – 4.30pm
No weekends or after-hours necessary.
Applications are now open from candidates who have either Permanent Residency or Australian citizenship, unrestricted Medical Board of Australia registration and no Provider Number restrictions. For more information , please contact Laura Harnett –Practice Manager on practicemanager@ecu.edu.au or 08 6304 5618



25 is a “Fini” built for purpose Medical Centre comprising a large waiting room, office space, 2 consulting rooms, minor theatre with change rooms, kitchen, and laundry facilities. 11 car bays.
25 Mills St. was built with the intention of expanding on to 23 Mills Street.
Contact Dr Tony Taylor – 0418 945 047 or thuff.t@bigpond.com for brochure of Plans and further information.

























