Dr Stephanie Giandzi Recent fellow










Dr Stephanie Giandzi Recent fellow






There will always be a balancing act between protecting the public from unsafe practice and protecting practices from unsafe bureaucracy.
It was always going to ruffle a few feathers – telling older doctors they need a health check to make sure they are still up to the job.
No matter how mandatory health checks for doctors aged over 70 are framed – even referring to practitioners as ‘late-career’ rather than ‘older’ – the proposal was set to be labelled by some as ageist and discriminatory.
Aphra and the Medical Board of Australia have produced a lot of data suggesting that older doctors with declining cognition are riskier and attract more notifications than their younger peers.
But critics say the devil is in the detail. That includes how many complaints are due to age-related health-impairment as opposed to other factors, and how many turn out to be unsubstantiated or even vexatious.
The RACGP and the AMA have voiced serious concerns that mandated health checks for older doctors could constitute agebased discrimination.
They argue that threatening 7000 doctors with compulsory health checks is counterproductive at a time when many of them are hankering to leave the red tape behind and retire from an already depleted workforce. The health checks could be the final straw.
Others maintain that a doctor who is safely working beyond the age of 70 has nothing to fear.
There will always be a balancing act between protecting the public from unsafe practice and protecting practices from unsafe bureaucracy.
“First, do no harm” – seen as the first rule of medicine – applies to both doctors and those who regulate them.
SYNDICATION AND REPRODUCTION Contributors should be aware the publisher asserts the right to syndicate material appearing in Medical Forum on the mforum.com.au website. Contributors who wish to reproduce any material as it appears in Medical Forum must contact the publisher for copyright permission.
DISCLAIMER Medical Forum is published by Medforum Pty Ltd (Publisher) as an independent publication for health professionals in Western Australia. Neither the Publisher nor its personnel are medical practitioners, and do not give medical advice, treatment, cures or diagnoses. Nothing in Medical Forum is intended to be medical advice or a substitute for consulting a medical practitioner. You should seek immediate medical attention if you believe you may be suffering from a medical condition. The support of all advertisers, sponsors and contributors is welcome. To the maximum extent permitted by law, neither the Publisher nor any of its personnel will have any liability for the information or advice contained in Medical Forum. The statements or opinions expressed in the magazine reflect the views of the authors and do not represent the opinions, views or policies of Medical Forum or the Publisher. Readers should independently verify information or advice. Publication of an advertisement or clinical column does not imply endorsement by the Publisher or its contributors for the promoted product, service or treatment.
Advertisers are responsible for ensuring that advertisements comply with Commonwealth, State and Territory laws. It is the responsibility of the advertiser to ensure that advertisements comply with the Competition and Consumer Act 2010 (Cth) as amended. All advertisements are accepted for publication on the condition that the advertiser indemnifies the Publisher and its personnel against all actions, suits, claims, loss or damages resulting from anything published on behalf of the advertiser.
EDITORIAL POLICY This publication protects and maintains its editorial independence from all sponsors or advertisers. Medical Forum has no professional involvement with advertisers other than as publisher of promotional material. Medical Forum cannot and does not endorse any products.



10 Is the clocking ticking on older doctors?
New mpox strain arrives in WA
Going local in fight for clean air
48 Exploring rest and movement
Wine review: Marq


This month we have a great selection from Marq Wines for our doctors dozen competition. Dr Louis Papaelias had reviewed them on page 51 and you can enter by using the QR code on this page or at www.mforum.com.au
We also have lots of movie tickets making their way to winners who are off to see the British Film Festival or Saturday Night this month.
PUBLISHERS
Alice Miles – Director Fonda Grapsas – Director Tony Jones – Director tonyj@mforum.com.au
EDITORIAL TEAM
Editor
Cathy O'Leary 08 9203 5222 editor@mforum.com.au
Production Editor Jan Hallam 08 9203 5222 jan@mforum.com.au
Clinical Editor
Dr Joe Kosterich 0417 998 697 joe@mforum.com.au
Graphic Design Ryan Minchin ryan@mforum.com.au
ADVERTISING
Advertising Manager
Bryan Pettit 0439 866 336 bryan@mforum.com.au
Classifieds Sales Ross Bulman 0428 759 076 ross@mforum.com.au
Clinical Services Directory
Alice Miles 08 9203 5222 alice@mforum.com.au
CONTACT MEDICAL FORUM
Suite 3/8 Howlett Street, North Perth WA 6006
Phone: 08 9203 5222 Fax: 08 6154 6488 Email: info@mforum.com.au www.mforum.com.au















Britta Regli-von Ungern-Sternberg has won the Frank Fenner Prize for Life Scientist of the Year in the 2024 Prime Minister’s Prizes for Science.
The consultant anaesthetist at Perth Children’s Hospital and UWA Chair of Paediatric Anaesthesia was recognised for her life-changing research into reducing risks associated with anaesthesia for children and to make surgery and recovery safer.
About a quarter of a million children have surgery involving anaesthesia each year in Australia, with one in seven suffering breathing problems during surgery.
Professor Regli-von Ungern-Sternberg found associations between family history, modifications in anaesthesia management and respiratory problems. This allowed children at high-risk of breathing problems to be identified during their pre-anaesthesia assessment and have their anaesthesia better managed.
She also helped advance doctors’ understanding and management of paediatric anaesthesia, including choosing the best method of anaesthesia and airway device for each patient.
After a winter of moderate to high levels of respiratory bugs, Australians are now breathing a little easier, according to the national influenza surveillance.
FluTracking, which is based on weekly surveying of more than 68,000 people around the country, collected two million surveys over winter.
The data shows that influenza, COVID-19 and RSV were all circulating, leading to moderate-tohigh levels of respiratory illness in the community.
But since then, they have all have been trending down and are currently sitting at low levels.
“Analysis of FluTracking data suggests all symptoms approximately follow the same seasonal pattern, with the most reported symptoms consistently being runny nose and cough from 2022 to 2024,” its summary said.
“The timing of respiratory illness peaks within each year appears to vary over the last three years. Respiratory illness activity peaked

Her work has now been incorporated into international guidelines and has changed how anaesthesia for children is performed worldwide.
“We know that the experiences we have as a child in healthcare, and particularly surgery, can shape not only the now but also the future and long-term health as an adult,” she said.
“If a child needs a vital operation, my aim is for this surgery to be as safe and comfortable as possible.
“I started out as the only female paramedic in my town in Germany and I’m now one of a small number of female academics in my specialty.
“I feel very passionate about mentoring people from all walks of life and all genders and giving them opportunities in our field. and hope it will encourage more people to become interested in the specialty.”
in the middle of July for 2022, while activity for the last two years has peaked notably earlier, in the last week of May/first week of June.
“In the last five years the greatest percentage of participants experiencing at least one annual episode of fever and cough, or runny nose and sore throat, was observed in 2022, 43% and 33%, respectively.
“Since then, there has been a gradual year-on-year decrease in the percentage of participants experiencing these symptom combinations.”
Despite this, participants in 2024 were more likely to experience a respiratory illness compared to 2020 and 2021, particularly for fever and cough. This pattern reflects the resurgence of multiple respiratory viruses in 2022 in addition to COVID-19.
Head gets in the way of recovery
Muscle activation in people suffering from hip osteoarthritis might be a case of mind over matter, according to new Edith Cowan University research.
ECU post-doctoral research fellow
Dr Myles Murphy investigated muscle function in people with hip osteoarthritis and found that these patients were unable to activate their muscles as efficiently.
“Previous research has established that the degree to which joints degenerate is not directly related to the amount of pain a person with arthritis will experience. In fact, the stronger your muscles are, the more protected your joint is, and the less pain you will experience,” he said.
“Our research has shown that people with hip osteoarthritis were unable to activate their muscles as efficiently, irrespective of strength.”
Dr Murphy and his team studied the brain function of people with hip arthritis, finding that the mind played an enormous part in this equation.
“Basically, people with hip arthritis are unable to activate their muscles properly because the brain is actively putting on the brake to stop them from using the muscle. We don’t know why that is, yet.
Following the implementation of the National Cervical Screening Program (NCSP) renewal in December 2017, the recommended upper age to be eligible for screening increased from 69 years to 74 years.
Professor Yee Leung explains
Why was the change to exit at age 74 introduced?
Modelling, using the NCSP renewal pathway of partial genotyping human papillomavirus (HPV) screen with reflex liquid-based cytology (LBC), predicted an overall 24% reduction in cervical cancer cases and a 29% reduction in cervical cancer mortality in the vaccinated population.
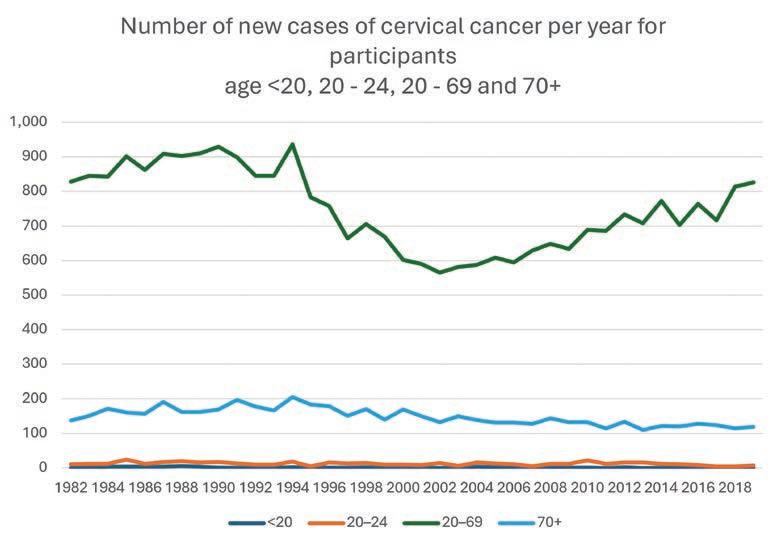
From 1982 to 2019 the number of new cervical cancer cases annually has reduced to approximately 100 cases in the 70+ age cohort. Screening this cohort would detect additional cases of cervical cancer that would otherwise present at a late stage.
The average life expectancy of a young septuagenarian (aged 70–74) woman in Australia today is approximately 18 years. The increase in age to exit the screening program to 74 years was based on modelling that accounted for the increasing life expectancy of the young septuagenarian. Exit testing with HPV subtyping and reflex LBC was therefore recommended between the ages of 70–74 on the basis that the benefits of screening outweighed the risks.
Are the young septuagenarians participating in the NCSP?
Progression towards five-year participation from 2018 to 2022 is 34.9% for participants aged 70–74. This compares to the 79.5% five-year participation in those aged 25–29. Coverage was also lowest at 38.9% for the aged 70–74 cohort who have a HPV or LBC test for any reason in 2018–2022. The aged 70–74 cohort are clearly not being screened.

What are the screening results for the young septuagenarian?
In 2022, the majority of primary screening test results in participants aged 70–74 was low risk (crude rate 94.3%), the remainder being intermediate risk (2.6%) and higher risk (2.2%) compared to results of all participants aged 25–74 at 89.4%, 7.5% and 2.3% respectively. For those with an intermediate result, 5.6% will be higher risk at first followup, comparable to 4.9% for eligible participants in the program.
The number of new cervical cancer
cases in those aged 70+ constitute approximately 12% of all cases, indicating that from a screening program perspective, this cohort should not be ignored.
Are septuagenarians at higher risk of high-grade abnormalities compared to the younger cohorts?
In 2022, there were 4.7 per 1000 participants screened aged 70–74 with high-grade abnormality detected compared to 14.2 per 1000 participants screened aged 25–74. Farnsworth et al confirmed previous studies that reported participants with
high-risk HPV (HR HPV) and negative LBC, the risk of a biopsy proven high-grade abnormality decreased with increasing age of the participant. However, if the LBC reported a highgrade squamous intraepithelial lesion (HSIL), the risk of a biopsy proven high-grade abnormality was not affected by the age of the participant.
Are there risks in screening the young septuagenarian?
Expect up to 5.3% of this cohort will be HR HPV positive. The challenge for the clinician is knowing how to discuss the significance of an intermediate or higher risk screening result in the young septuagenarian. Important considerations include:
1. A discussion on what a positive HR HPV screening test means. There is emerging understanding about immune regulation in the older person and the concept of immune latency. The host immune surveillance following a prior infection may result in the HPV DNA expressed at levels too low to be detected rather than clearance. Over time, as the host immune system becomes less efficient, the HPV DNA levels become detectable again. Currently there are insufficient data in the National Cancer Screening Register (NCSR) or published literature to further risk stratify the aged 70+ with an exit screen reporting a HR HPV,
negative cytology and normal colposcopy.
2. The relevance of the past screening history to risk stratify. A participant with a known negative screening history is at lower risk of a high-grade abnormality compared to the never-screened, underscreened or participant with a previous high-grade abnormality.
3. The importance of the LBC result to risk stratify. When the LBC result is negative, the risk of a high-grade abnormality is low.
4. Colposcopy is often challenging as the entire transformation zone (TZ) critical for a comprehensive colposcopic assessment is often not visible (Type 3 TZ). A negative LBC result is associated with a lower risk of a high-grade abnormality and treatment is not recommended on the basis of a persistent HR HPV and negative LBC.
5. The purpose of the NCSP is to prevent cervical cancer. A low participation rate results in later stage disease at diagnosis. Later stage disease is more complex to treat and associated with a higher morbidity and mortality rate. What can you do?
The availability of self-collection has made opportunistic screening more accessible for this cohort. In the first quarter of 2024, 37.7% of all screening tests in participants aged 70–74 was

self-collected. This is the highest uptake in any age group.
The young septuagenarian attending the exit screening test who has an HR HPV any type should be referred directly for a colposcopy (Rec 6.23). Early data from the NCSR indicates those with a HPV 16/18 result, 65.6% will attend for a colposcopy within three months and 87.5% within six months of the test result.
It would be beneficial to pretreat this age cohort with vaginal oestrogen (unless otherwise contra-indicated) prior to colposcopic examination.
The young septuagenarian and those aged 70+ constitute approximately 12% of all new cervical cancer cases annually. The benefits of screening this age cohort outweigh the inconvenience of finding a HR HPV with a negative LBC. Data are maturing on how to further risk stratify these participants found to have persistent HR HPV and negative LBC on their exit screening test.
Take the opportunity to offer a clinician or self-collect Cervical Screening Test (CST) to the next never-screened or under-screened young septuagenarian you see.
References available on request
Wome n a ged 25- 74 s hould have re gula r fiv e- yea rly ce r vica l sc ree ning tes t s , eve n if the y are no lo nge r se xually ac tive or h av e e xper ie nce d me no pause .

Specialist GP Dr Ramya Raman has been awarded Advocate of the Year 2024 by the AMA WA in recognition of her work promoting general practice.
Professor of Indigenous Genomics at The Kids Research Institute

Australia Professor Alex Brown has become a Fellow of the Australian Academy of Technological Sciences and Engineering.
Dr Pam Laird, senior clinician research fellow at The Kids and paediatric respiratory physiotherapist at PCH, was joint winner of the Early Career Scientist of the Year at the 2024 Premier’s Science Awards.
Rural doctor and educator Associate Professor Andrew Kirke has been inducted as a life member of Rural Health West.

ECU’s Australian Indigenous HealthInfoNet will for the first time in its three-decade history have an Aboriginal person at its helm. New director Professor Bep Uink is also the first female in the role.
The Aboriginal or Torres Strait Islander category winner in the 2024 Australian Mental Health Prize is Broome-based Aboriginal researcher Professor Juli Coffin
The Perron Institute has appointed Professorial Fellow Erin Godecke as its Professor of Stroke Recovery and Rehabilitation.
Telstra’s Championing Health state winner in its Best of Business Awards is Perth Scoliosis Clinic, while its Accelerating Women category winner is Menopause Friendly Australia
continued from Page 4
“But the brain seems to really be hampering the progress of rehabilitation and the muscles to protect the joint.
“We suspect that it is a short-term, protective response gone wrong. Unlike a rolled ankle or a hurt knee, chronic pain like osteoarthritis tends to hang around for a long time. Instead of being a protective response in the short term, the brain’s protective response becomes a problematic and maladaptive response in the long term.”
Dr Murphy is looking at novel ways to overcome this automatic muscle inhibition to effectively rehabilitate patients.
In the meantime, those living with hip osteoarthritis have been urged to continue strength training and to work with a qualified physiotherapist or exercise physiologist.
Fasting and exercise during chemo?
ECU researchers are investigating the impact of dietary restriction and exercise on women having
Home care provider Silverchain has partnered with the National Ageing Research Institute to develop a guide on the use of digital technologies in aged care.
Recently launched in Melbourne, the Framework for Enabling Technology Supported Aged Care at Home is aimed at helping in-home aged care providers as they plan and deliver technology-supported services.
It provides a practical step-by-step guide on how best to implement technologies in everyday service delivery and was devised specifically for the Australian context following using funding from the Aged Care Research and Industry Innovation Australia grants program.
NARI Director of Clinical Gerontology, Associate Professor Frances Batchelor, said that while new health-related technologies were developing rapidly across various sectors, in-home aged care providers were still in the early stages of adopting these.
“With older Australians living independently at home for longer, the need for technology-supported in-home models of care has increased,” Professor Batchelor said.

“We’ve heard from in-home aged care providers that there are substantial barriers to introducing technology in the home environment, such as difficulties in encouraging uptake and embedding technology into service delivery processes.
“We joined with Silverchain to develop specific guidance for implementing digital tools in an effective, efficient and person-centred way. It also offers practical tips and a checklist of key considerations when developing a technology implementation plan.”

Silverchain Director of Research Discovery Dr Tanya Davison said that in-home aged care providers recognised the potential for digital technologies to improve outcomes for older people.
“The research we’ve done has shown that older people are increasingly using technologies in their lives and the in-home aged care workforce is ready to try innovative new approaches,” she said.
“But simply making technology available isn’t enough for success. We need to make sure the specific technologies selected and the ways we implement them are carefully designed. This includes consideration of the kinds of training and supports that are required.”
chemotherapy to treat breast cancer.
“We want to evaluate the effectiveness that exercise and a fasting-mimicking diet have on the immune system in patients who are undergoing chemotherapy, because we know that a part of the efficacy of chemotherapy relies on the immune system,” PhD student Ms Cristina Crespo Garcia said.
The clinical trial follows preclinical studies which showed that fasting and exercise promotes systemic changes that could help to restore immune system function by enhancing immune cells that attack tumours.
Dietary restriction and exercise training in mice had been shown to enhance the efficacy of chemotherapy. In human studies there was also emerging evidence that fasting and exercise could make the immune system more antitumoral.
It was widely established that anti-tumour immune responses contributed to the success of chemotherapy agents.
Social media is helping fill gaps in sex education and providing an essential connection point to health services for young adults, according to a Victorian study.
The report highlights the reasons young adults (aged 18-29) turn to digital technologies for sexual and reproductive health support. It found that social media is providing validation of young people’s personal experiences, particularly for those with chronic pain or identifying as LGBTQIA+, as well as providing sexual health education that may be missed at school or required post-graduation.
Swinburne’s Professor Kath Albury said there were lots of adult topics that school-based sex education did not cover, and social media platforms were filling these gaps with both information and peer support.
“These spaces are often dismissed as ‘misinformation’, but our participants valued them as sites of validation for lived experiences of sexual, reproductive and gender health,” she said.
TikTok is another source of validation, particularly for those experiencing symptoms of conditions such as endometriosis, or those seeking gender-affirming healthcare.
“This population group is aware that information available online can be inaccurate or catastrophised, but they want health providers to take their health concerns seriously during consultations – even when they mention TikTok,” she said.
A medical oncologist who grew up in regional WA has become the face of a new campaign from the Hospital Research Foundation Group to highlight its activities in the State.
Dr Tom Ferguson, who works at Fiona Stanley Hospital specialising in genitourinary and colorectal cancer management, received critical funding for clinical trials into treatment for men with advanced prostate cancer.
Last year, the Hospital Research Foundation Group merged with the Fremantle-based Spinnaker Health Research Foundation, which for 27 years had supported researchers and clinicians in the South Metropolitan region. The combined charity now funds work in more than 50 diseases and illnesses, with all funds donated in WA invested back into local research, hospitals and healthcare initiatives.
Dr Ferguson grew up on the family farm in Kojonup before attending boarding school in Perth and earning his medical degree from the University of WA.
Australia’s biggest charity ride, the MACA Cancer 200 Ride for Research, has raised more than $10 million this year for WA cancer research.
The record amount was raised by the event – in its 13th year –which was held in early October and as usual included dozens of doctors taking part.
The funds raised will go to Perth’s Harry Perkins Institute of Medical Research to support medical research into the hardest-to-treat cancers.

Almost 2000 riders set off from Optus Stadium on a 200km two-day ride to Mandurah and back over a weekend.
Perkins Institute CEO Professor Peter Leedman said vital new cancer research would be supported by the funds from the ride.
“The MACA Cancer 200 is the most successful charity bike ride in Australia, raising $64 million for research over the past 12 years,” he said. “Each year, corporate WA unites with the big-hearted WA community to ride with one purpose – to make cancer non-lethal and keep our families together for longer.”
He furthered his expertise with a two-year clinical research fellowship at the Royal Marsden Hospital in London before returning to Perth to work as a consultant medical oncologist.
At the FSH’s medical oncology department, his primary focus is conducting clinical trials, often in collaboration with research groups or pharmaceutical companies.
Thanks to a grant from the Hospital Research Foundation Group, Dr Ferguson and his team are now undertaking the LuCAPE clinical trial for prostate cancer.
The trial is looking at the safety and potential benefits of combining two existing treatments for men with advanced prostate cancer and ultimately aims to improve their quality of life and life expectancy.
“Conducting research such as the LuCAPE trial helps foster a culture and environment conducive to future research, innovation and breakthroughs, and supports our junior researchers coming through,” Dr Ferguson said.
His team has been busy recruiting for the trial, which is expected to run over three years, with early results possible by the end of this year.
By Cathy O’Leary
With submissions now closed on a controversial proposal for mandatory health checks on older doctors, some are calling for caution while others are claiming age discrimination.

By Cathy O’Leary
Few people would argue that patients need to be protected from ageing doctors who are seriously struggling in their cognitive ability but refuse to entertain the idea of calling it a day and retiring.
Doctors already have a reputation as reluctant patients with a propensity for corridor consultations, but add to the mix someone who is significantly impaired cognitively and it could be the final lightning rod.
The Australian Health Practitioner Regulatory Agency is now drawing a line in the sand as it responds to a spike in patient complaints about older practitioners – with the rate of health impairment-related notifications for doctors aged over 70 more than three times higher than for younger colleagues.
In Australia, judges and magistrates are required by law to retire between 65 and 72 years, depending on the state, while international commercial pilots cannot fly planes from the age of 65, but there is no mandatory retirement age for doctors.
And with the stakes high for medical professionals when it comes making errors, there is momentum to set the bar higher.
Through Ahpra, the Medical Board is proposing doctors aged over 70 undergo general health checks with their GP or another doctor every three years, and then every year from the age of 80 upwards.
It argues this will help to pick up early concerns and provide the chance to intervene before the public is at risk, particularly in cases where the doctor lacks the cognitive insight to know the risk is even there.
But apart from criticism of potential ageism and discrimination, one of the big concerns raised by doctors’ groups is that, if not done properly, mandatory checks could fuel an exodus of highly experienced practitioners who are already fed up with growing red tape.
In August, the board sought feedback on three options –maintaining the status quo, introducing a detailed ‘fitness to practise’ assessment, or having a general health check with a GP.
The consultation period closed on October 4, but the Medical Board has already pegged its money on the third option, arguing it would be the best for patient safety while keeping doctors in control of their careers as they age.
By its own reckoning, the second option of a detailed assessment would be a financial blow-out, potentially reaching almost $20 million a year in compliance costs.
Based on data from last year showing 6,975 doctors aged 70 years and over holding practising registration, with 5,940 of them aged 70-79 years and 1,035 aged 80 years, the cost would be between $4.52 million and $7.54m
Based on data from last year showing 6,975 doctors aged 70 years and over holding practising registration, with 5,940 of them aged 70-79 years and 1,035 aged 80 years, the cost would be between $4.52 million and $7.54m a year for a fitness to practise assessment without cognitive assessment.
a year for a fitness to practise assessment without cognitive assessment.
If cognitive assessments were included, costs would increase to between $8.14m and $18.09m, and on top of that, there would be about 9000 hours of late career doctors’ time, at a cost of $1.36m.
“It would be very costly for the late career doctor, and overall costs were likely to be unreasonable relative to the possible benefits to the community,” the board’s report concluded.
But the board also insists that keeping the status quo is not the solution, instead backing the option of requiring doctors aged 70 and older to undergo general health checks every three years, and yearly from the age of 80.
It said some doctors failed to recognise the limitations of their standards of care, particularly as their sustained attention, reaction time, visual learning and memory decreased markedly after the age of 75. Yet many were reluctant to retire.
Compounding this was concerns that older patients with a long-time family doctor were more likely to be trusting of the doctor and less likely to question their advice or treatment.
And despite the board’s code of conduct and advice from professional bodies, many doctors were not effectively managing their own health, and this did not appear to have improved since the start of the National Scheme in 2010.
The board said general health checks would cost significantly less than detailed health check option, with compliance ranging from $1.53m to $2.62m a year, and it was likely to be less than this because some doctors would be having a similar health check regardless of the board’s requirement.
“The major cost is likely to be social or emotional costs to some late-career doctors who may be offended and feel their professionalism is undermined if they are required to undergo mandatory regular health checks,” it said.
continued on Page 12
continued from Page 11
But Medical Board chair Dr Anne Tonkin argued the proposal was in line with public health screening measures, with early detection allowing early management and risk avoidance, and it did not mean doctors had to retire from the age of 70.

“We are looking for effective and practical ways to support late career doctors to stay in safe practice through health checks that will identify and enable doctors to address any risks that come from increasing age,” she said.
“General health checks will give individual doctors and their treating practitioners information to help them manage any health concerns early and re-equip doctors to practise past their 70th birthday.
“But doctors are often reluctant patients, and we are concerned they don’t always seek the care they need.”
The proposed general health checks would be like existing Medicare-funded general health checks provided by GPs for patients aged over 75.
Results would be confidential between doctor and their treating practitioner and would not be routinely provided to the Medical Board, which would only be informed if a treating practitioner made a mandatory report about a late career doctor who refused to manage the risk to patients.
What the data shows
Ahpra’s complaints shows a pattern of aged-related risk, with doctors aged over 70 more than 80% more likely to be the subject of a notification for any reason than those aged under 70.
The rate of notifications about late career doctors has almost doubled over the past eight years, rising from 36.2 notifications per 1000 practitioners aged 70 and older in 2015 to 69.5 complaints per 1000 in 2023.
Notifications for doctors aged 70 to 74 have jumped markedly,
rising more than 130% from 32 notifications per 1000 doctors in 2015 to more than 74 per 1000 in 2023. For those aged 80 and over, notifications have climbed by more than 180% per 1000 doctors between 2015 and 2023.
Many complaints are in relation to clinical care, communication, documenting records and reports and prescribing or supplying medicines.
While the same trend in cognitive decline could be said for ageing workers in any profession, the stakes are big for medical professionals, and many argue the bar needs to be set higher for them.
A recent American study found that although cognitive decline is less common among more highly educated people, about one in five physicians older than 70 may experience mild cognitive decline, and one in 15 may have cognitive impairment.
It warned that years of experience had to be weighed up against a possible decline in professional competency, including not staying up to date with the most recent guidelines and the rapid advances in medical science.
But critics say the mandatory health checks could discriminate against older, experienced doctors – and add to their exodus from the workforce.
Australia’s peak GP group has warned against it becoming another timewaster for busy doctors.
Asked by Medical Forum to comment on the proposals, the Royal Australian College of GPs initially showed cautious support, adding that while patient safety was essential, the proposed mandatory health check must focus on doctors’ wellbeing.
RACGP President Dr Nicole Higgins said any health check process needed to be
straightforward and focus on the health and wellbeing of doctors and not add to the administrative burdens placed on GPs.
“There must be a balance,” she said. “Even among doctors under 70, notifications to the medical regulator have drastically increased, growing by 63% since 2015.
“Sourcing and retaining GPs remains the biggest challenge for general practices. GPs have told us they’re experiencing more burnout. They’ve told us about the strain notifications can put on their mental health. Mandatory reporting and vexatious notifications add to that strain.
“Many GPs, who pushed up their working hours during the pandemic, are now thinking about retirement.”
But when the RACGP’s formal submission to the Medical Board was later released, it was more strident in its criticism, arguing there was no evidence that mandatory health checks would reduce patient harm or notifications.
It called for the status quo to remain, saying the board did not present any evidence that health checks would reduce notifications against late-career doctors.
“It is unclear if notifications received by Ahpra were specifically related to the physical or cognitive decline of the doctor, or the age of the doctor, and could be avoided with a mandatory health check based on the doctor’s age,” the college wrote.
Health checks would be another regulatory burden unnecessarily imposed on the general practice profession without evidence to support the effectiveness.
“GPs will retire early rather than face increased administration and red tape to practise,” it warned.

Other doctors’ groups have also made submissions to the board, with the Australian Medical Association confirming it had received significant feedback from

members, including concerns that mandatory health checks were a form of age discrimination.
It had strongly urged the board to seek and publish legal advice on whether mandatory health checks for doctors over a certain age to qualify for registration contravened the Age Discrimination Act 2004.
Unlike the RACGP, the AMA said it did not support retaining the status quo, nor fitness-to-practise assessments or any models of revalidation, but said the preferred option was still too complicated for late career doctors and treating practitioners.
“The board should refine its preferred model of health checks for late career doctors, so it is just a health check with one’s usual general practitioner,” the AMA said.
“This would demonstrate the purpose of the health check is to support the health and wellbeing of the doctor, not to penalise the doctor for their age.”
It cautioned that mandatory health checks for older doctors had the potential to become a
major disincentive to remain in the workforce, denying patients access to a doctor and younger doctors' access to an educator or mentor.
“The board must tread carefully in its communication with the medical community,” it said. “There is a delicate balance between enforcing compliance and inadvertently driving experienced physicians towards premature retirement.
“For some late career doctors, the health checks may be perceived as a coercive imposition.”
The AMA is also concerned about the financial implications of regular health checks at three-yearly and yearly intervals and supports the introduction of an MBS item for the assessments.
The Australian College of Rural and Remote Medicine said that while it was not unreasonable to require health checks, the effect of a doctor retiring in a regional town where the medical workforce was already thin on the ground was felt by the whole community.
The college said any health assessments should be able to be
undertaken in their entirety in the local practice, including having telehealth as an option.
A spokesperson for Aphra told Medical Forum that about 180 submissions were received by the cut-off date last month. Where consent had been given, the submissions would eventually be made publicly available.
The spokesperson foreshadowed that the review process would take “a considerable period of time” as the board considered each submission.
“If any proposal is to be taken to the stage of a standard, then a regulatory impact report will have to be done before the matter is taken to the Australian health ministers,” he said.
The State and federal ministers would ultimately make the decision about whether to go forward, and because of the amount of work still to be done there was no timeline on the process.

GPs are being urged to be aware of their patients’ work environment, particularly blue-collar workers such as welders and fabricators, as dangers on the job become more apparent.
By Eric Martin
While work-related ill health is not a new phenomenon, concern about the risks facing some professions is gaining momentum.
Australia’s workplace hazards have been under intense focus, with the recent ban imposed on the highly popular engineered stone benchtops due to its links to silicosis causing shockwaves through the construction industry.
Similarly, the recent news that welding, which employs about 60,00070,000 people nationally, causes black lung has seen welding worker vacancies increase by 80% in Western Australia in 2024.
According to Weld Australia, the number of welding trade workers in Australia dropped by 8% over just five years, and the completion rates of welding apprenticeships, including a Certificate III in Engineering (Fabrication Trade), have fallen by as much as 23% with a predicted shortfall of at least 70,000 welders by 2030.

The welding research, a joint project by Curtin’s School of Population Health and the University of Sydney, found that 76% of participants exposed to welding fume inhaled a high level of toxins, as well as being exposed to other carcinogenic metals – most commonly hexavalent chromium and nickel.
Study lead Dr Renee Carey, who was previously involved in a landmark study outlining the dangers of working with engineered stone, said the study of 634 workers and employers showed that many Australian welders could be at risk of developing serious health problems.
“Welding fume exposure has been associated with various adverse health effects, including cancer, respiratory disease, neurological disorders and reproductive effects,” she noted.
While the findings are alarming, the general estimate is that it will likely take 5-10 years for the findings to impact policy, resulting in the type of workplace inspections conducted in factories and on construction sites by WorkSafe WA. But even then, current inspection figures show that this messaging could take even longer to bring about meaningful change in workplaces.
For example, WorkSafe WA has already carried out 29 investigations under its silica verification project in 2024, resulting in 145 notices being issued across the State.
The project found a “continuing level of non-compliance by a large portion of the engineered stone industry” with ongoing concerns including the uncontrolled use of power tools on engineered stone, workers either not being provided with or fit-tested for respirators, workers refusing to wear respirators, poor housekeeping and the inadequate treatment of recycled process water.
WorkSafe WA even found workers with diagnosed or suspected silicosis continuing to work in the industry against medical advice. And significantly, the silicosis story has only deepened, with cases of autoimmune disease now being reported in engineered stone benchtop workers.
Dr Karen WalkerBone, Professor of Occupational Rheumatology and Director of the Monash Centre for Occupational and Environmental Health, has been spearheading this research in Australia and explained that occupational exposures to respirable crystalline silica (RCS) have been implicated in systemic lupus erythematosus (SLE), systemic sclerosis (SSc), rheumatoid arthritis (RA) and antinuclear cytoplasmic antibody (ANCA)-associated vasculitis.
“Although having detectable autoantibodies is not diagnostic of an autoimmune disease, their presence in certain rheumatic diseases, such as SLE and RA, has been shown to predate clinical features often by many years,” she said.
“The body is only designed to recognise bacterial and viral pathogens but will still do its best to eliminate any foreign body, be it fungus or even ingested plastic. The particles that we call respirable crystalline silica are so tiny they get to the very bottom of the airways, into the alveoli and on to the bloodstream.
“And they when they get that far, nothing removes them, the body's incapable of clearing that particle. They are so toxic that they kill the body’s first line of defence, the macrophages, leaving both the dead cells and the original particles behind after that first, failed attempt at removal.
“That causes local inflammation in the lungs, or silicosis, but it seems to be the persistence of a foreign body close to a rich blood supply that is precipitating the development of autoantibodies.
“The body continually tries to repair the resulting local tissue damage, eventually exhausting the repair mechanisms and causing an overwhelming state of inflammation and the beginnings of an immunological cascade. And once that cascade is initiated, it's very hard to switch off again.”
Professor Walker-Bone said that in a study of 133 people with SLE, 78% already had detectable antinuclear antibodies (ANAs) 3.3 years before the onset of symptoms prompting
her exploration of the association between autoantibodies, RCS exposure and silicosis diagnosis by quantifying the prevalence of ANAs, extractable nuclear antigens (ENAs), rheumatoid factor (RF) and other autoantibodies – the fundamental tools in the screening and diagnosis of autoimmune disease.
“The first case reports were written about in the 1950s, which is still recent in medical science terms, when patients were diagnosed with silicosis from coal mining and then developed rheumatoid arthritis,” she said
“Rheumatoid factor was the first ever autoantibody we discovered, and while we knew that there was some overlap in coal miners, it was a very different source of exposure, and not such a huge exposure over such a short time as we've had in this industry.”
Professor Walker-Bone said the ability to conduct the latest research in RCS autoimmunity was due to WorkSafe Victoria’s funding of a free screening program for all the workers in Victoria’s stone benchtop industry.
“This is the first time that anyone has had such a large group of patients who've all had massive exposure over a relatively short time, and then been able to measure their autoantibodies,” she explained.
“We screened about 900 or so initially, but they weren't all sent to hospital during that first stage – they were screened by occupational health physicians and then referred to the hospital if necessary. But eventually, so many of them needed to come to hospital that we now do all the screening there, and we've seen about 1300 in total between June 2019 to August 2023.”
WorkSafe Victoria has committed another two years of funding with a possibility of two more beyond that.
“As such, we're seeing new workers if they've not yet had the opportunity to get tested, as well as bringing back some workers that were seen in the occupational health clinics who were thought to be low risk,” she said.
“With the new data available, we have been recalling them to ensure
Discover unparalleled cardiac imaging excellence with our specialised team of cardiac reporting experts and dedicated radiographers, united in delivering superior medical imaging and exceptional patient care.

Equipped with cutting-edge GE Revolution CT machines, we offer the pinnacle of cardiac CT scanning technology.
• Remarkably low radiation doses • Complete CT coronary angiograms in a single heartbeat • Suitable for patients with arrhythmic and high heart rates • Exceptional image quality.
Services include: MRI Cardiac • MPS • CTCA • CT Calcium Score.
Doctor Priority Line for urgent bookings and enquiries
and
continued from Page 15
they really are as low risk as we first thought, as well as following up all people we think have evidence of silicosis and/or autoantibody formation.”
RCS exposure was categorised according to the duration of work in the stone benchtop industry and the highest dry processing exposure reported, though in the end, nearly all workers fell into the ‘medium’ and ‘high’ exposure groups.
Almost half (43.7%) had very high levels of exposure to RCS and nearly one-quarter of workers with diagnostic information (253 workers, 24.3%) were diagnosed with silicosis at assessment.
“The only workers with very low exposure were literally confined to the office. They didn't go anywhere near the factories or the manufacturing process,” Professor Walker-Bone explained.
“But anybody who went anywhere near the environment – if they were cleaning it after the guys had finished work, or if they were doing any work in there, even if they didn't do it directly – they had such a high level of bystander exposure that it was as good as if they were doing the work.
“The silica dust is so fine that it just gets everywhere. We've got some amazing photographs of workers. It looks like they've been playing in the snow – they are covered in the dust and you can't get away from it. Even when you've washed it all down and it dries, there's still some visible residue.”
In those workers without clinically diagnosed autoimmune disease the prevalence of detectable ANAs was 24.6%, ENAs 4.6% and RF 2.6%, and those with high levels of industrial RCS exposure were more likely to have detectable ANAs. Likewise, detectable autoantibodies were found in significantly higher proportions among those diagnosed with silicosis.
“The prevalence of detectable ANAs in this cohort was also much higher than that expected in the general adult male population. For example, among those aged 40-49 years in the US National Health
and Nutrition Examination Survey, the prevalence of ANAs was <6%, whereas in our cohort, the prevalence was 24.6%,” Professor Walker-Bone said.
“One of the most interesting results to emerge from the study was the almost exact correlation between the number of individuals who contracted silicosis and the number who developed an autoimmune disease – almost 25%.
“So, if you have silicosis, you're more likely to have an autoimmune disease. But the Venn diagram isn't a precise match. There are people who've got one or the other and not both, it’s incredibly strange.”
Despite the insidious nature of airborne hazards, the worst offenders for workplace injuries in WA, and the ones most likely to result in a presentation to a GP, were muscular injuries. Specifically, manual handling accounted for 41% of all work-years lost.
According to the RACGP’s latest Health of the Nation report, musculoskeletal injuries accounted for 37% of GPs’ consultation time.
College guide
The college’s online resources include a detailed article on returning to work after an injury by Dr Peter Fenner, which highlights the importance of documenting any work-related injury properly, noting that the relevant workers’ compensation authority or insurer usually required notification of an injured worker within 48 hours of the injury occurring, using their specific paperwork.
He also stressed that some injuries may initially appear minor while the muscles were still warm.
“However, on cooling down after work, or even the next morning, muscle spasms can greatly restrict movement, causing pain at rest that is aggravated by even the smallest of movements,” Dr Fenner advised.
“It is essential that at the first consultation a detailed history of the mechanism of the injury, as well as any exacerbating or contributing factors, is taken and carefully documented. This should be followed by careful examination of the patient and formulation of a
diagnosis based on the history and the physical examination.”
Dr Fenner warned that imaging could be misleading and should not be used to diagnose workplace injuries in general practice, especially imaging of the spine due to the many variants in a ‘normal’ skeleton.
“An exception to this rule is an early MRI for severe unstable knee injuries, which may assist in assessing the need for early orthopaedic intervention. Workers’ compensation funds may pay for MRI in this setting to facilitate faster specialist assessment and treatment, as this speeds recovery and subsequent return to work,” he said.
The RACGP’s guide includes a quick table for GPs to ensure they document all the essential factors correctly during the initial diagnosis, such as the mechanism of injury, previous injuries, the level of pain and any radiation, paraesthesia, other complaints or symptoms, and any current medications or medical problems that may impact recovery –including mental health issues.
Importantly for GPs, according to WorkSafe WA the mental health impact of witnessing a traumatic event resulted in six months lost time from work – outlasting the physiological effects of injuries. This was backed up by current data from the Health of the Nation Report, which revealed that in 2024, 71% of GPs were reporting psychological issues in their top three reasons (and often the most common cause) for patient presentations.
“It is essential that GPs access support and advice from mental health specialists, such as psychiatrists, on the management of patients with mental health issues, and the assessment and treatment of mental illness is informed by a holistic, wholeof-person approach,” the report highlighted.
“Unlike many other public and private health care settings, general practice does not draw a distinction between mind and body systems.”
Five years ago, John Ryan was a young financial executive with a big life ahead of him, until a diagnosis rocked the ground under his, his wife’s and his children’s feet. When life became shockingly uncertain, sound planning had taken money worries out of the equation. This is his story.

G“Hey Ravi, how did the bloods look?”
“For a 37-year-old Caucasian male, there is no reason your iron should be this low. Did the blood in your stool clear up?”
“Nah, not really.”
“The chances are one in a million, but I’ll send you for a colonoscopy just to be safe.”
With that referral letter, my GP, Ravi, saved my life. The diagnosis was metastatic colon cancer, the bowel lesion was too big even for the colonoscopy to get past! There was also cancer well entrenched in the liver as well as different locations around the body within lymph nodes.
My personal team of life-saving angels (Dr Tom Van Hagen, Prof Cameron Platell and Prof Luc Delriviere) got to work and are the only reason I am still here today.
Luc said to me early on, “this is going to be a marathon, not a sprint, John”. I’m so glad he said that as I was trying to find a quick fix. But as you know, the quick fix doesn’t exist, and to get anywhere near a fix is not guaranteed.
I had walked out of the office on a Thursday to prepare for a colonoscopy on Friday and didn’t
return to the office for a year.
Phase one, the mountain climbing stage of the marathon.
That 12 months was filled with three surgeries, six months of chemotherapy, and a lot of sleep. At the end of it all, I was declared cancer-free and began my path to being normal again.
Phase two of the marathon began.
Throughout my interactions with various medical professionals, I realised that by the time I received my diagnosis, the opportunity to organise my financial affairs had largely slipped away. At that critical juncture, spending time with my children and wife took precedence over perfecting anything on the financial front.
After my diagnosis, I could no longer apply for more insurance, nor would I have had the mental bandwidth to plan for my family’s financial security in my absence.
Reflecting on this, I am profoundly grateful for having done much of the work earlier in my career. Knowing that my financial affairs were mostly in order provided immense relief, allowing me to focus on what was most important – time with family and doing anything to assist recovery before the next round of treatment. It becomes an all-consuming pattern.

Was my financial safety net perfect? Definitely not. I hadn’t stayed on top of what would be needed financially if something happened to me. I did this for other people every single day – just not myself!
Fortunately, having somewhat of a financial safety net was enough to circumvent any financial burden on my family during our most vulnerable moments. It granted me a sense of liberation and peace so I could focus on me.
So, having gone through this, what should be done before the unforeseen occurs?

1. Simplify your financial complexity
Let’s start by approaching your financial affairs with the same precision and thoroughness you apply in your medical practice and clean up any loose ends.
This might involve tracking down old super funds or unclaimed money, consolidating high-interest loans into lower-interest facilities, or selling speculative share portfolios that have been sitting in the bottom drawer, hoping they will “come good one day.”
Streamlining your finances and addressing them with the same diligence you apply to patient care, will significantly ease the burden on those who will manage your affairs in your absence, as well as provide peace of mind for you and your loved ones.
2. Secure your legacy
Studies routinely show that at least 50% of people haven’t prepared a will, and instead, leave it up to a formula set by the State government to determine the division of their assets. This makes it a more complicated and expensive process for your family to navigate, and for many doctors, not proactively structuring your estate results in the loss of multi-generational tax savings that are available.
It may also increase the probability of your estate being challenged, particularly in blended family situations.
Thinking through all the issues, having open conversations and clearly documenting your intentions will ensure that one of the last memories you leave for your family isn’t a negative one.
3. Eliminate financial worry
It’s true that insurance is a topic that most of us love to hate. What’s also true is that when it does pay out, the impact for a family who is navigating a terminal illness diagnosis is lifechanging. For example, I had a trauma payment deposited into my bank account within two weeks of diagnosis. That is ‘breathe easy’ money.
One of the first things I was asked by one of the supporting clinical nurses was whether I had income protection insurance. She gave a sigh of relief when I said yes. Work was just not physically possible during the acute phases of treatment.
Having the right team of advisers working alongside you can help you and your family navigate one of the most challenging times they will face.
While you will never be replaced,
having someone you can trust to outsource the responsibility and oversight of managing your financial affairs, before or after a health event occurs, allows you to focus on the things that are most important to you.
It is not lost on me how lucky I am, and I must attribute some of that luck to having the headspace to focus 100% on the amazing healing capabilities of the body. You cannot do that if you have financial tasks or worry creeping in.
My final encouragement for you? Take control of your financial future today.
Simplify your financial complexity, secure your legacy, eliminate financial worry, and enable financial continuity. By doing so, you not only protect your loved ones but also grant yourself the freedom to focus on life’s most important moments.
Coming from a place of integrity, please don't wait. Start planning now to ensure peace of mind for you and your family.
John Ryan is a Senior Wealth Adviser at Capital Partners Private Wealth. You can contact John at jryan@capital-partners.com.au

A doctor with a hugely civic heart, Dr Anh Nguyen is in the process of retiring from medicine but still has a lot of work to do with his beloved Vietnamese community.
By Ara Jansen
When Dr Anh Nguyen started practising medicine in Perth, he was one of only two Vietnamese doctors in the city.
At 31 years of age, he’d arrived here via boat with his wife and five brothers, after successfully starting a medical career in Vietnam.
Anh had been one of 2500 hopeful students wanting to become a doctor in Saigon and was one of the 200 chosen, starting medical studies around the Fall of Saigon in 1975.
While other Vietnamese doctors had preceded him into Perth, they’d not passed the qualifying exams to allow them to work in Australia. Anh didn’t want to follow them and take up another profession, so he went to Adelaide and did seven more years of training.
“While many things about medicine don’t change, there were things I had never learnt before like psychology, biochemical science, ethics and genetics,” he says. “Some of what I had learned was definitely outdated. Learning about genetic engineering was beautiful.
“I knew some English but spent a year learning and after that year the teacher said I had enough language to go into medicine. Those seven years seemed to pass in a blink of an eye. It was also a bit like military training. When I was an intern, I often had to work 72 hours straight with no sleep at all.”
Growing up, Anh was determined to be a doctor. He’s the third generation in his extended family to be a doctor, which includes a brother practising in Queensland and another doctor practising overseas among his 11 siblings, who are scattered all over the world.
Anh has a daughter and a son, born soon after his arrival in Australia.
“My wife Yung was a paediatrician, but when we arrived here, she said one doctor in the family was enough because otherwise there would be no time for family. She said she’d look after the kids and keep us safe, which is what she has done.”
Anh received his Australian medical qualifications when he was 38. After graduation, the Nguyens moved to Perth.
In 1990 – a decade after arriving in Australia – he set up Bulwer Medical Centre in Palmerston Street and, in the beginning, most of his patients were Vietnamese. He was one of only two Vietnamese doctors in Perth in a community of about 15,000. The other doctor was a friend who moved from Sydney.
He started solo in this practice, eventually bringing on another doctor to work Wednesdays and weekends. Over the years, the practice continued to grow and now comprises GPs as well as allied health providers who speak more than half a dozen languages between them apart from English. Two years ago, Anh sold the practice and has been slowly transitioning out of medicine, working five half days a week.
“When one of the family came to me and they trusted me, then the whole family came. First it was Vietnamese families and then Chinese, Japanese, Italian, Thai and other migrant families. I think they felt comfortable expressing what they felt with someone who had similar experiences.”
While Anh adopted Australia as his new home, he has always been determined to make sure his ties


to Vietnam are not forgotten. He laughingly reveals he refuses to answer texts in English from his children as a way to keep their Vietnamese language skills sharp.
“It’s very effective!” There’s also five grandchildren and he’s working hard to make sure they also learn Vietnamese.
Anh is president of the WA Chapter of the Vietnamese Community in Australia and has been for 14 years. It is a not-for-profit organisation celebrating Vietnamese culture, language and traditions and provides support for Vietnamese living in WA.
“I broke the record. I was only going to stay for one or two terms. I’ll have to retire soon – and we’re
nurturing a lot of our young people to take over.”
A member of the Ministerial Multicultural Advisory Council for the Office Of Multicultural Interests, he’s also a coordinator of the Vietnamese Community School of WA, convener of the Vietnamese radio program on 6EBA, a board member of Girrawheen Senior High School and a member of the City of Wanneroo’s Multicultural Advisory Group.
Anh was a vital part of the installation of the Vietnamese Boat People Monument of Gratitude

Nerissa Ferrie Medico-legal adviser
Am I obliged to provide a treating doctor report?
Musculoskeletal injuries are high on the list of requests for treating doctor reports - which can come from a variety of sources including patients, their lawyers, insurers and employers.
Consent Format for the report
Unless compelled by law, consent should be obtained from the patient (or their parent/guardian) before any personal health information is released. It is recommended that consent is obtained prior to the report being prepared.
A medico-legal report will usually include:
• Your credentials, including professional address, qualifications, experience and position at the time you were involved in the patient’s care
• The requesting party’s name, the date of the request, the purpose of the report, and the date of the authority
• The patient’s name and date of birth
• Medical facts in chronological order: – presentation (history and symptoms) – examination findings – investigations – provisional diagnosis – treatment/management – current condition – prognosis
• Your response to any specific questions
• Your clinical opinion (where appropriate)
• Your signature and the date the report was completed.
If you have no independent recollection of your management of the patient, the information in the report will be based solely on what’s recorded in the medical records (e.g. ‘I have no independent recollection of my involvement in the patient’s care. According to the medical records…’). If the report refers to a colleague’s notes, this should also be clear (e.g. Dr Smith’s notes indicate…’).
Irrelevant information shouldn’t be included; but clinically relevant information must not be omitted. If the patient only consents to certain parts of the relevant information being released, then you should consider whether this is a withdrawal of consent and advise the requesting party that consent has been withdrawn. Gratuitous comments about third parties should also be avoided.
• Allocate time to review requests and prepare reports.
• Your practice may have clear policies around requests for reports, including a minimum timeframe for a report (e.g. 14 days), a schedule of fees, and a requirement for pre-payment prior to the release of the report.
• If you are unsure about fees, you can use your normal hourly rate. Statutory bodies may have a prescribed fee schedule which may be provided with the direction or order.
• Before commencing work on a report, consider the amount of work involved and provide a cost estimate so the fee can be agreed before you start drafting the report.
• You should decline to respond to questions which are outside of your scope of practice or your area of expertise.
• Refer to the medical records, and don’t rely on your memory, or information provided by the requesting party.
• Address the report to the requesting party, and not “to whom it may concern”. If you don’t have a specific addressee, you can address the report to the patient.
• your signature and the date the report was completed.
If you have no independent recollection of your management of the patient, the information in the report will be based solely on what’s recorded in the medical records and if the report refers to a colleague’s notes, this should also be clear. Irrelevant information shouldn’t be included; but clinically relevant information must not be omitted. If the patient only consents to certain parts of the relevant information being released, then you should consider whether this is a withdrawal of consent and advise the requesting party that consent has been withdrawn. Gratuitous comments about third parties should also be avoided.
Professional Obligations
The Medical Board of Australia provides clear expectations for treating doctors who are providing medico-legal reports under section 10.9 of Good medical practice: a code of conduct for doctors in Australia.1
Legal obligations
It is important to be aware that any opinions expressed in a medicolegal report may be publicly tested and challenged in court. The weight given to the opinion will generally depend on the expertise and experience of the author.
Tips and traps
• Ensure that you are legally compelled or have the patient’s permission to provide a report.
• Prepare your report within a reasonable time frame – if necessary, discuss this with the requesting party.
• Always refer to your medical records when preparing the report.
• Remember that you may be cross-examined on your report – only write what you would be prepared to give evidence to in court.
• Do not alter your report at the request of your patient or a third party – if you receive additional information, or you need to correct an error, provide a supplementary report.
• Explain medical terms and concepts in plain English and avoid using legal terminology.
• Differentiate fact(s) from opinion(s) and avoid using emotive language.
• Do not act as an advocate for your patient or be tempted to deliberately omit any relevant information.
If the request is unclear, or you have any specific concerns about the request or the report, contact our Medico-legal Advisory Services team for advice.
1 https://www.medicalboard.gov.au/Codes-Guidelines-Policies/Code-of-conduct.aspx
continued from Page 21
project and the Long Tan Peace Park in Koondoola. In 2003, he was awarded a Centenary Medal and in June was awarded an OAM at the King’s Birthday honours for services to the Vietnamese community of Western Australia.
“I’m lucky my wife has good community spirit,” Anh says in answer to how he has juggled being a doctor and civic leader for so long. “She coordinates the Vietnamese language school on the weekends. She also wrote seven levels of teaching Vietnamese in the phonetic way. This way you can learn the language in two years instead of four.
“We do this work for our community. I don’t feel it’s a burden. We need to preserve our culture and language. If we lose it, we lose everything. Learning a new language is not just learning a language, it’s learning a whole culture. A whole world is in there.
Our community is multicultural and we need to integrate into Australian culture but also not forget the other one.
“Over the last 14 years the group and our community profile has been elevated. We have lots of strong connections in the wider community, our students excel at school and we have become successful in so many areas of our lives.”
Perhaps though, Anh’s most notable piece of legacy was using all the valuable connections he has made over the years, particularly political ones, to secure a piece of land adjacent to Girrawheen Senior High School for the association to finally build themselves a cultural and community home.
The Vietnamese community has been settled in WA for almost 50 years and despite being highly active and one of the largest culturally and linguistically diverse groups in the State, they have never had a centre of their own to meet,
celebrate and preserve Vietnamese culture and traditions.
“The younger generation integrates very quickly. If they don’t have a strong centre, like the one we are building, they won’t have a place to come to where they can also learn what it’s like to be Vietnamese.”
While Anh spearheaded the acquisition of the land – bought by the group freehold for $1 from the State – he has now left the construction of the $5 million centre to younger professionals in the association to coordinate architecture, project management and other aspects of the build.
In early October, the City of Wanneroo approved the building permit for the centre and there was a sod turning to celebrate. Practical completion is expected in September 2025 – just in time for the 50th anniversary celebrations of Vietnamese migrants settling in Western Australia.





A summit in Perth this month will explore the challenges of palliative care and neurodegenerative disease, explains Palliative Care WA CEO Lenka Psar-McCabe.
Quality palliative care enables people with life-limiting illnesses or conditions, and those important to them, to be supported to live, die and grieve well.
But for people living with neurodegenerative diseases and other neurological conditions, accessing palliative care can often present additional barriers.
The nature of neurodegenerative diseases is that they present and progress with significant clinical variation. People living with these illnesses and conditions can live for many years while developing cumulative physical and cognitive disabilities. They often must deal with a decreasing quality of life before reaching the end-of-life stage of their condition.
The appropriate time to provide palliative care can be a challenge due to the longer and varying time-course of neurodegenerative conditions and difficulties in
determining when the person is approaching the end-of-life stage. The diversity of symptoms including cognitive, behavioural and communication problems can also be a challenge for palliative care.
The role of general practice can be especially challenging. Holding the responsibility to find answers for clinical questions can be hard. Differential diagnosis between disorders can be difficult, especially in the early stages and with atypical variants. Guiding the patient and their loved ones adds additional complexities for the management of their long-term care.
Recognition of the nuances of palliative care for those with neurodegenerative illnesses and conditions and the goal of improving quality of life, symptom control, end-of-life care, and support for the person, their family and carers at all stages, has prompted Palliative Care WA to explore in detail the intersection
between palliative care and neurodegenerative conditions in our upcoming 2024 Palliative Care Summit on November 21 at the Pan Pacific hotel.
The summit aims to:
• Provide an opportunity for clinicians, service providers and the community to interact with political and service leaders to discuss priorities for quality palliative care in WA, with an emphasis on neurodegenerative diseases
• Present international, national and local evidence and experience to inform the delivery of quality palliative care in WA
• Embed the voice of lived experience, particularly those with experience of neurodegenerative diseases
• Champion the role of carers, families, aged care providers and community, including the compassionate community approach

• Provide an opportunity for attendees to be engaged in personal reflections and conversations about death, dying, grief and loss.
The program includes keynote addresses from Professor Hsien Seow, Canada Research Chair in Palliative Care and Health System Innovation and Professor in the Department of Oncology, McMaster University, Ontario, Canada, and Professor Susan Kurrle, Curran Professor in Health Care of Older People, Faculty of Medicine and Health at the University of Sydney.
Professor Seow will present on the ‘Evolution of the Waiting Room Revolution: How to improve care for neurodegenerative conditions and other illnesses’. He will also present workshops on how to apply the seven keys that help patients, families and providers to be both hopeful and prepared when facing serious illness.
Professor Kurrle will discuss ‘Improving care near end of life for people with neurodegenerative disease’ and will present workshops on improving enjoyment and quality of life in older patients.
Other experts presenting at the summit include:
• Dr Nathalie Huitema –Psychologist and sexologist specialising in the intersection of sexuality, ageing and consent, who will be joining online from the USA to discuss ‘Empowering choice: Nurturing sexual agency and consent amidst cognitive impairment in palliative care and neurodegenerative diseases’.
• Professor Samar Aoun – Perron Institute Research Chair in Palliative Care, University of Western Australia; Chair, Compassionate Communities Australia, PCWA Board Member, who will speak about ‘Reframing palliative care for neurodegenerative conditions using the example of Motor Neurone Disease’.
• Lenni Duffield – CEO Huntington’s Australia will present on ‘Good news, You’re worth Million$’.
• Professor Alan Harvey –Emeritus Professor and Senior Honorary Research Fellow in the School of Human Sciences and Conservatorium of Music at UWA, will discuss ‘The lifetime
Heel pain is a frequent problem that presents to the general practitioner. Plantar fasciitis is the most common cause of under the heel pain. Most patients will improve with non-operative treatment but not all.
Surgery is a very effective form of treatment for this condition in patients with long standing refractory symptoms.
Before being considered for surgery patients should undergo at least six months of non-operative treatment that includes the following (in the appropriate order):
• Rest, avoidance of activity
• NSAIDs, stretching exercise program
• Orthotics: off the shelf or custom
• Cortisone injection (one only)
• Shockwave therapy

Surgery can be open or endoscopic. The principle part of the procedure is release of the plantar fascia near its origin on the heel. Historically only the medial half was released but recent literature supports more complete release.
benefits of music on mental and physical health’.
• Andrew Allsop – Director Clinical Operations, Palliative Care, Silverchain WA and Bernadette Nowak – Clinical Nurse Manager, Bethesda Health Care will discuss the ‘Challenges when providing specialist care for people with Dementia’.
A panel discussion will cover the realities of caring for a person living with a neurodegenerative condition and will include Vicki Barry (care partner and young onset dementia advocate); Janet Wagland (General Manager Disability, Brightwater) and Richard Newman (CEO, Carers WA).
The WA Health Department and Bethesda Health Care are the main sponsors of the free inperson and online event for health professionals, service providers and health consumers.
Details are at https://palliativecarewa.asn. au/event/2024-palliative-caresummit/

Open surgery is performed through a 3cm incision in the proximal arch and allows not just plantar fascia release but also decompression of the tarsal tunnel and Baxters nerve which is often implicated in heel pain.
Endoscopic plantar fascia release is indicated for those without nerve compression symptoms and is done through a much smaller incision using a camera assisted cutting device much like a carpal tunnel release.
Both open and endoscopic releases are performed as day cases and require approximately two weeks on crutches. Recovery is slightly quicker for endoscopic patients as you would expect. Patients can expect an 8090% chance of a good result from surgery. Complications are rare.


St John of God Medical Centre
Suite 10, 100 Murdoch Drive, Murdoch WA 6150
Telephone: (08) 6332 6300 Facsimile: (08) 6332 6301
www.murdochorthopaedic.com.au
Monkey pox has mutated – even its name – and is creating new challenges for public health watchdogs.
Eric Martin reports
Only two years ago, monkey pox was a medical curiosity for Australian doctors, but fast-forward to 2024 and WA Health is asking GPs and people at risk of contracting the virus to be vigilant after two locally acquired cases were reported in WA.
While the local cases – which are still being investigated – are the milder Clade 2 strain of mpox and not connected to the more severe Clade 1b strain that is spreading in Western Africa, experts strongly recommend that those at risk still be vaccinated against the previous strain, as Australian cases are expected to surpass previous years.
More than 17,000 cases and 5037 deaths have been detected in the Democratic Republic of Congo and the recent change in transmission dynamics in Africa have alarmed global health officials. Less than 24 hours after the World Health Organization declared the new strain of mpox virus and a global public health emergency, the first case in Europe was confirmed in Sweden.
Mpox can be spread through skinto-skin contact, including during sex, and contact with contaminated items such as bedding and towels, with a lower risk of infection from breathing in droplets from coughs and sneezes.
Symptoms usually start within five days to three weeks of exposure to the virus and can include a rash that can look like bumps, pimples or sores, which later develop into fluid-filled lesions, pustules or ulcers. Some people also exhibit fever, headaches, muscle aches, backache or enlarged lymph glands.
WA Health’s Communicable Disease Control Director, Dr Paul Armstrong said people with the Clade 2 strain usually experienced a milder illness which could last for two to four weeks. He urged high-risk groups in the community to be alert for symptoms and seek testing promptly.
with men and through higher risk activities such as casual sex and multiple partners,” Dr Armstrong said.
“The numbers seen in Australia in 2024 have all been Clade 2b. Only a few people experience more severe illness, and many cases are resolved without specific treatment. This is the same pattern we saw in 2022 with the global spread of mpox at that time.

“Mpox infections have been increasing in Australia over the past few months – particularly among sexually active men who have sex
“What has been challenging this year is the ability to identify sexual partners of mpox cases easily as many people may not know the contact details of their partners, which is why we are encouraging people at risk to exchange those details with each other so they can be contacted if someone is later identified to have mpox.
“The change in behaviours in men who have sex with men, as well as the roll out of the mpox vaccine helped control the 2022 outbreak.
If people have any symptoms suggestive of mpox – even if they are mild and they have had the mpox vaccine – they should contact their GP or sexual health service for an appointment.
“And importantly, wear a mask, call ahead and cover up any rashes, bumps or pimple-like sores.”
Dr Armstrong said some of the most effective ways to prevent the spread of mpox were to avoid sex if there were any signs of sores or blisters, limiting sexual partners, and keeping contact details of new partners to help with contact tracing if needed.
“Condoms offer some protection, but only protect the area of skin covered as sores can be on and around other parts of the genitals and body,” he said.
“Now that we are seeing locally acquired cases of mpox in WA, it’s important to raise awareness of this virus and encourage people at risk to get vaccinated. Vaccination plays an important role in reducing the severity of illness and preventing spread among those at highest risk of contracting mpox, which is important to protect people who may be vulnerable to severe infections.”
The JYNNEOS® mpox vaccine is free for those considered to be at higher risk including sexually active men who have sex with men (cis and trans) and their sexual partners, as well as sex workers and their sexual partners.
Two doses at least 28 days apart are required for optimal protection, though at this stage, given the emergence of the new strain, the mpox vaccine is not being considered as a travel vaccination for people travelling to Africa unless they are otherwise eligible.
Dr Armstrong explained that while the Clade 2b virus, like all viruses, constantly mutated during replication and spread, it had not mutated to the point where it had significantly changed its transmissibility or ability to cause significant disease.
“We know this is the case as we can see genomic differences in the cases detected in Australia in 2024,” he said.

Dr Shane La Bianca
Dr Andrew Tan
Dr Jeff Thavaseelan
Dr Trent Barrett
Dr Matt Brown
Dr Manmeet Saluja
Dr Alarick Picardo
Dr Steve McCombie
Dr Sarah O’Neill
With the largest partnership of Urologists in Western Australia, Perth Urology Clinic can manage all urological conditions, offering a wide range of treatment options. For urgent referrals or queries, use our GP Hotline on 1800 487 656 (Press 9). refer@perthurologyclinic.com.au
Healthlink: puclinic Hollywood Clinic | Wexford Clinic
continued from Page 27
“What has happened recently in Central and West Africa, with the emergence of Clade 1b, is the mutation of Clade 1 that has created a new strain or lineage of the disease. The genomic analyses show that it is distinctly divergent from previously circulating strains in the Democratic Republic of Congo.”
He suggested that those interested should read the recently published article in Nature Medicine, ‘Sustained human outbreak of a new MPXV clade I lineage in eastern Democratic Republic of Congo.’
“We know that clade 1b has also been seen in groups other than men who have sex with men in Central and West Africa, such as children and women, but we don’t yet know if this will be the case if it spreads and sustains transmission outside Africa.
“The current vaccines are thought to be effective against all strains of mpox and were vaccines initially developed against smallpox. Smallpox and monkeypox viruses belong to the same family – the orthopoxvirus family – so the smallpox vaccine also protects against mpox.
“At the moment, we don’t know fully understand if the vaccines will be as effective against the Clade 1b strain, as it was against the strain we are seeing in Australia – the Clade 2b strain though studies have reported that the vaccine is as high as 80% (one dose) or 88% (2 dose) effective at preventing the disease in at-risk people.”
Currently, the vaccine is only considered necessary for those at higher risk due to sexual activity, and Dr Armstrong noted it was unlikely that Australia would extend the provision for people working in primary healthcare settings.
“While healthcare workers who work in clinics or practices with a high throughput of patients with sexual health complaints may be eligible for the vaccine, it is not currently recommended for most healthcare workers,” he said.
“There have not been many secondary cases in healthcare workers anywhere in the world, so

the risk in healthcare settings has been deemed low. Additionally, appropriate infection prevention and control measures including personal protective equipment will protect healthcare workers from mpox.
“However, ultimately that would depend on the epidemiology of mpox.”
While there are no specific comorbidities or genetic predispositions that make certain people more susceptible to mpox infection than others, Dr Armstrong pointed out that those most at risk of severe disease included immunocompromised people, especially those living with poorly controlled HIV infection.
“In the context of spread outside of men who have sex with men, children and pregnant women may also be at greater risk of severe mpox disease – and we know this is the case with Clade 1 mpox infections in children in Central and West Africa,” Dr Armstrong said.
“This does not necessarily mean that they are engaging in sexual activity, as the most likely course of transmission in these contexts are through contact with sores and contaminated clothing or bedding.
“Mpox is still predominately seen in the men who have sex with men cohort so Australian GPs should consider relevant screening for those presenting with clinically compatible symptoms such as a rash or pox-like lesion.
“Patients may also present with proctitis, and a travel history should be taken if mpox is suspected to help ascertain the risk of Clade 1 or 2I infection.”
WA Health has developed a one-page guide for GPs to help assessment, testing and diagnosis, and infection prevention control recommendations and notification requirements. It can be found at www.health.wa.gov.au/~/media/ Corp/Documents/Health-for/ Infectious-disease/Monkeypox/ Monkeypox-quick-guide-forclinicians.pdf.
“The Department continues to monitor the situation closely, both nationally and internationally, and will provide additional advice to GPs if the situation changes,” Dr Armstrong said.
“Specifically, the Communicable Disease Control Directorate releases clinician alerts which provide important updates on communicable disease risks. GPs can subscribe to the disease alert mailing list and receive key updates to their inbox, and other resources include the Australian Society for HIV, Viral Hepatitis and Sexual Health Medicine (ASHM) decision making in mpox quick reference tool – found on ASHM’s webpage, as well as the STI guidelines.”

Advocating for better air quality is a grassroots action which doctors and their patients can readily embrace, and it will have tangible health benefits.
Eric Martin
reports
The latest Doctors for the Environment Australia report, Fossil Fuels are a Health Hazard, was a timely reminder for doctors that they are the ones who will be dealing with the emerging impacts a changing climate.
One of the most immediate concerns highlighted was the growing impact of air pollution on the development of chronic disease and escalating deaths in populations around the world.
The State of Global Air Report 2024 found that “8.1 million people died in 2021 from air pollution, with 58% of these deaths due to particulate matter measuring less than 2.5 micrometres (PM2.5), making air pollution the second largest risk factor for death after high blood pressure, followed by smoking.”
In Australia, traffic-related air pollution from burning fossil fuels causes 11,105 premature deaths per year, which is 8.7 times more than national road toll (1266) and more than 6.3 times the number of alcohol-induced deaths (1742). Yet subsidies to fossil fuel producers totalled $14.5 billion in 2023–24, an increase of 31% on the $11.1 billion recorded in 2022–23.
Perth GP and local representative of Doctors for the Environment Dr George Crisp said that despite the clear science backing a reduction in the amount of fossil fuel investments, there were 124 new fossil fuel projects listed by the Federal Government in 2023, 10 more than at the end of 2021.
“If all the listed projects proceed, they are projected to contribute over 4.8 billion tonnes of emissions by 2030. For context, the global carbon budget to give us a 2 in 3 chance of limiting warming to 1.5°C is 92 billion tonnes. These Australian projects alone would consume over 5% of the global budget by 2030,” he said.
According to the report, this estimate does not include significant proposed gas fields such as the Beetaloo Basin with its estimated lifetime emissions of up to 3.2 billion tonnes, or the Burrup Hub gas project, which has estimated lifetime emissions of 6.1 billion tonnes. These two gas fields alone would account for 10% of the global carbon budget for limiting global heating to 1.5°C.
Associate Professor Alex Larcombe, the head of Respiratory Environmental Health at The Kids’ Institute, said that for every 1000 tonnes of carbon burned, one human being died prematurely. The implication of this was the Bettaloo and Burrup projects would be responsible for 3.2 million and 6.1 million premature deaths, respectively.
Associate Professor Larcombe highlighted that the impacts of pollution would be exacerbated by an ageing population and noted that for the first time in decades the life expectancy in many countries had gone down.
“A component of that would have to be exposure to all sorts of new pollutants that were absent years ago. Despite better healthcare and increased knowledge, more disease is going to manifest in older people
and the WHO states that 99% of the planet breathes air that exceeds safety guidelines,” he said.
“And unlike climate change, it is beyond doubt that air pollution is causing large scale health effects across the Australian population in terms of asthma, heart disease, lung cancer, and premature births, which involve a whole range of significant illnesses that affect people's lives profoundly.”
Both doctors agreed that Perth’s air quality was good but that was not the case for all of Australia or for most of the world, especially in developing countries where air pollution from a range of sources had significant health impacts.
“Much of what we are exposed to is anthropogenic particulate matter, which in Australia, like the report says, comes from primarily burning fossil fuels and many of these pollutants are carcinogenic. For example, diesel combustion, which is used a lot in Australia, is a class one carcinogen on numerous scales,” A/Prof Larcombe said.
“It is known to cause cancer in humans and everything in between. The particulate matter is carbonbased particles with a lot of other nasty stuff absorbed onto them.
“Even if the combustion process is super-efficient and it does output relatively pure carbon (which it never does), that carbon itself is toxic. The particulate matter, regardless of whether it has absorbed other chemicals or polyaromatics, is harmful in and of itself, and the health effects go all the way from minor, irritation from short-term, low-level exposure that everyone would have experienced.
“But over time, if the exposure dose is high enough, it can lead to serious health issues. And there is not a huge amount of information on what the real range of that damage is because the human population is so varied. What might be mildly harmful to a worker, or a healthy adult would be different for a child, an older person, or someone with cardiovascular disease – demographics that are more at risk.”
Dr Crisp said that a lot was known about air pollution from research over the decades.
“And thanks to the countless epidemiological studies, we also know that these impacts have been
massively underestimated and occur even at relatively low levels of exposure,” he said.
“Separating out the individual pollutants such as particulates, oxides of nitrogen and volatile organics is extraordinarily complex, as are the pathways by which these pollutants cause disease. For example, both oxides of nitrogen and particulates occur in combination, and both have significant impacts. In fact, it is oxides of nitrogen that are the biggest drivers of asthma rather than particulates.
“While the nitrogen dioxide in our cities is produced by motor vehicles, it is produced in the home is by the burning of gas. We also know that households with gas cookers have much higher rates of childhood asthma, and 12% of all childhood asthma episodes in Australia are the result of a gas cooker.
“If you're a GP and you have a family that comes in with a child with asthma and you're talking to them about managing it, it's highly likely they will be asked if anyone in the house smokes, or if they have pets, but I suspect that very rarely does someone say, ‘do you cook with gas’?”
A recent expert statement by Melbourne Climate Futures recommended that Australian estimates of death and illness attributed to vehicle emissions should be updated to incorporate NO2 impacts as well as those of PM2.5.
“One of the most crucial factors is the interaction between the original waste, the process used for combustion, and the size of the particulate matter produced,” A/ Prof Larcombe explained. “Not only are smaller particles breathed in more readily, but they also stay suspended in the atmosphere for longer, making them more likely to be inhaled.
“A PM gradient does not mean that they are all produced at that size, rather, it includes everything up to that size including nano-sized particles and that hampers efforts to estimate the level of damage caused.
continued from Page 31
“The issue is further complicated by changes in the atmosphere as well. Once the exhaust leaves the vehicle and enters the atmosphere, the particles change and aggregate. They interact with the UV light from the sun and change, producing potentially worse volatiles.
“But the general trend is the smaller they are, the more harmful – for a range of reasons. We have our own built-in defence mechanisms with mucus in our noses and throats that trap the bigger particles, and we effectively swallow those most of the time and they pass through and don’t cause too much trouble.
“But smaller particles can bypass that mucus, penetrate the lungs, and enter circulation in the bloodstream. And concerningly, they can cross the blood-brain barrier and cause neurological disease.
“There are now established links between these types of exposures and diseases such as Alzheimer's, for example, as well as all sorts of cardiovascular issues as well as exacerbating existing disease and impairing immunity.
While your body is working overtime to compensate for the particulate matter, your ability to fight off other exposures to viral or bacterial pathogens is significantly compromised. There is a lot of evidence accumulating that diesel exhaust and others promote the development of asthma if it was not already there.”
He said that the cells and macrophages in our lungs were designed to recognise a virus or bacteria and attack that. When they see a carbonaceous particle from combusting fossil fuel, they will also try their best to clean it up too.
“Macrophage means big eater and while this tactic works reasonably well in the short-term, as they keep trying to devour these particles over time, they become overwhelmed and die. All the carbonaceous particles that they have previously consumed are rereleased into your body, triggering an ongoing inflammatory process,” he said.
Dr Crisp said that many local

councils already had noise pollution zones indicated next to main roads for real estate buyers to consider, but there was no equivalent demarcation that showed the amount of air pollution people living in the vicinity would be exposed to.
“Why is that? We know that living within 50m of a main road has significant effects for your health and the proximity is important. So, why do we not say something about living near those areas? More importantly, why are we still building childcare centres and schools next to main roads when we know that they are the most vulnerable populations? There is a big disconnect here,” he said.
“There is an extraordinarily strong correlation between proximity to major roads and your levels of exposure to vehicular pollution, just like there is a correlation between how close you are to a coal fired power plant – it is a wellestablished link,” A/Prof Larcombe added.
“Which is why it is so concerning that so many childcare centres are built on major roads – these levels of exposure exacerbate underlying asthma. Don’t build our daycare centres next major roads, because moving away even a couple of hundred metres makes an enormous difference in terms of health.”
Dr Crisp said GPs had an important role to play as leaders within the local community when it came to sharing information and spearheading action.
“Just like we have done for smoking cessation, immunisations, and a host of changing areas of medicine and health beyond the consulting room. Our voice is important because we are informed about the medical science and because we can bridge the gap between information and the actions that we need to take to improve our health, both individually and collectively,” he said.
“GPs are on the ground. They can see and monitor the impacts in their local clinic, and we can change outcomes. There is a wonderful opportunity here for improving our patient’s health through air pollution literacy and advising our patients and communities about local impacts.”
Falls remain the leading cause of injury deaths and hospitalisations in WA, and some marked increases have experts worried.
WA has seen more than a 50% increase in the number of fallsrelated deaths over four years, according to the latest annual study into the personal and community toll from falls-related injuries.
The Injury Matters report shows a marked increase in the number of hospital bed days occupied by people admitted after a fall, as well as thousands of clinical incidents where patients have suffered a fall while being cared for in the WA health system.
It warns of an ongoing burden on the WA community because of falls, with someone dying every 17 hours in 2021, and in 2022 someone admitted to hospital every 16 minutes and someone attending an emergency department every 12 minutes.
In 2021, falls accounted for 35% of all injury deaths and in 2022 falls made up 24% of injury hospitalisations and 13% of emergency department attendances.
“In isolation these figures are concerning, however previous WA Falls Reports demonstrate the growing incidence of falls in WA and the alarming impact that this is having on our community and the healthcare system,” the report said.
“For example, there has been a 43% increase in the number of hospital bed days occupied due to a falls incident from 2018 to 2022, and a 53% increase in the number of falls fatalities from 2017 to 2021 is other significant reason for concern.”
Some sections of the community are over-represented, with older adults having the highest rate of falls fatalities, hospitalisations

and ED attendances, and males outnumbering females in the stats. But not all falls are in the elderly, with childhood and workplace falls contributing to the numbers.
Aboriginal people account for 5% of all falls hospitalisations despite representing 3% of the population, and Kimberley residents have highest rate of falls hospitalisations compared to other areas of WA, for the fifth consecutive year.
Injury Matters chief executive
Sandy Lukjanowski said the report provided insight into the considerable burden that fallsrelated injuries imposed on the WA community and healthcare system.
“It is forecasted that by 2036, approximately one in five Western Australians will be aged 65 years and over,” she said. “Given the high incidence of falls among our older adult population, it is therefore likely that the burden of falls will continue to increase.
“The good news is that the majority of falls are preventable, and therefore it is imperative that we upscale our
preventative efforts today in order to reduce future burden.”
Ms Lukjanowski said at present WA lacked dedicated injury prevention or falls prevention strategies, so the impending release of the National Injury Prevention Strategy and updated Australian Falls Prevention Guidelines was keenly awaited.
Among the report’s recommendations is a call for improved integration of acute care services and prevention programs, because many people sought acute treatment following a fall.
“Referral pathways within the health system must be enhanced urgently to ensure high-risk people are referred for follow-up assessments and support to prevent subsequent falls,” the report said.
“Barriers such as unclear pathways, limitations on referring clinicians and clinical capacity prohibit the referral of patients to specialised fall programs.”
It called for clinical guidelines and referral pathways so that all health professionals could refer patients to other health professionals for assessment, support for post-fall recovery and the transition to community-based maintenance programs.
“An important touch point that could be leveraged to identify and support people at risk of falls are emergency medical service (EMS) clinicians,” the report said.
“When assisting a person who has experienced a fall, the EMS clinicians’ objectives are to
Kids need nature – risks and all – argues the head of Nature Play WA Dr Kelsie Prabawa-Sear
Almost weekly, I see research articles highlighting the benefits of nature and unstructured play for children. But despite the mounting research, it appears there is a significant gap between what the research is telling us about child development and wellbeing and what we are doing as a society.
A recent article in the Journal of Pediatrics outlined the causal relationship between a lack of independent play and declining mental health in children and youth. It wasn’t a suggested link or observed correlation, it was an identified cause.
The authors noted that a lack of independent play is not the sole cause, but possibly a major cause in children’s declining mental health. They suggest that our current societal concern for children’s immediate safety has overwhelmed our historical understanding that children need increasing amounts of independent activity (and access to risk) as they grow, to develop the character traits they need for good mental health.
Put simply, poor mental health is a much bigger risk to our kids than letting them ride their bike around the neighbourhood or play at the park without a parent supervising. As a society, we need to balance our often-disproportionate concern for safety with the needs of our kids for independent, unsupervised, moderately risky activity. To really help our kids, we need to be willing to do this both within our education
and care systems and in our kids’ free time.
Kids need time to play where adults are not involved, not directing them, and not supervising, where they decide what they do and how they do it.
The importance of this autonomy is beautifully conveyed in a study of childhood play from Switzerland in the early 1990s. The study found that children who were allowed to play freely in the neighbourhood, on average, spent twice as much time outdoors, were much more active while outdoors, had more than twice as many friends, and had better motor and social skills than those denied such play.
Interestingly, children who were regularly taken to the park by their parents did not achieve the same positive results, due to leaving the park before they wanted to (children will stay longer if given the chance), their friends not being there to take part in collaborative play, having their play monitored (so they played in less challenging and risky ways), and lack of diverse play opportunities that neighbourhood play allowed (like bringing tools and equipment from home for loose parts play.
We find ourselves in the situation where most West Australian kids are growing up with a lack of opportunity to play in neighbourhoods unsupervised and have absolutely no opportunity to play unsupervised at school, daycare, or afterschool care. Most

children do not walk or ride to school with friends.
Not only is this impacting on their play opportunities, it is also limiting their opportunities to engage in risk and to learn from it. How does a child who does not ride their bike around the neighbourhood learn to navigate a road crossing, the danger of hitting the front brakes too hard, or the impact of going from footpath to sand at speed? How do they learn not to accelerate into corners, or that tyres slide in the wet? We know they need to practise and experience such things to acquire the relevant skills. And we want them learning on bikes as kids and not in cars as young adults.
Kids also need to experience and overcome challenges to build up their resilience toolkit. Challenges like conflict resolution when playing games or recovering from gazed knees are child-sized versions of falling out with friends as a teen or recovering from injury as an adult. Without experiencing the kid-sized versions, how will they know that they can cope with the bigger versions?
While the lack of unsupervised play and lack of exposure to risk is a very concerning trend, the solution is simple and free. We just need to convince the adults to let the kids play.
ED: Dr Kelsie Prabawa-Sear is the CEO of Nature Play WA, a not-for-profit organisation supporting the mental and physical health of WA children by connecting them to nature and community through outdoor play.
provide interventions to alleviate their symptoms, prevent further deterioration and, when necessary, transport the patient to a hospital.”
Research showed that high-risk groups including older adults were more likely to sustain a secondary fall that required emergency medical attention within 30 days of their initial fall. But with the right
pathways in place, EMS clinicians could refer patients to services for follow-up assessments and support to prevent subsequent falls.
Families are at the heart of a new early warning system for sick kids, explains Professor Fenella Gill from Curtin University School of Nursing and Perth Children’s Hospital.
Curtin University research has led to the recent development and implementation of an important paediatric early warning system across WA.
The ESCALATION system is now in place in all WA hospitals that care for children as well as the prehospital emergency services run by St John Ambulance and the Royal Flying Doctor Service.
This system marks a significant advancement in the early recognition of clinical deterioration in children, with a key feature being its strong emphasis on family involvement.
Our team of researchers developed the system as a standardised evidence-based approach to facilitate early recognition and response to paediatric clinical deterioration for acutely unwell patients in the WA Health context.
The key features include integrated family involvement, sepsis recognition, a structured communication framework and escalation pathways tailored to suit the different operational contexts across all facilities.
The goal of the research, published in Pediatric Research, was to ensure ESCALATION’s feasibility and acceptability across different hospital settings while accounting for varying levels of resources. Throughout the process, we examined key implementation concepts, including context and mechanisms of impact, from the perspectives of all users.
Our data sources ranged from interviews and audits with families to focus groups with nursing and medical staff. We also reviewed the use of the observation and response (PARROT) charts and tracked escalations of care within hospitals including patient transfers to Perth Children’s Hospital.
This approach created and sustained the collaborative environment for refining and implementing the system.
Continuous stakeholder engagement throughout the refinement process identified the need for a sepsis escalation pathway.
This meant that when the ESCALATION system was fully implemented in 2022, an integrated paediatric sepsis clinical support tool was included, coinciding with the release of the Sepsis Clinical Care Standard for Australian health services to use sepsis pathways to support early recognition of sepsis and escalate care when required. As a result, WA paediatric healthcare was ahead of the national Sepsis Clinical Care Standard requirements.
Optimising staff preparation was essential to ensuring the successful implementation of the system because early warning scoring represented a significant practice and behaviour change for many intended users.
A key component of successfully reaching agreement to adopt the standardised system across WA healthcare was supporting change through adequate preparation and education for staff.
Our team developed and tested an online e-learning education package to train staff on using the system, including calculating early warning scores, recording on an age specific PARROT chart and following the escalation pathways.
We knew there were system features requiring new behaviours for some health professionals such as involving a child’s family in detecting early signs that can indicate clinical deterioration. It was important that we clearly explained how to elicit family concern or worry and that we

demonstrated desired behaviours by using clinical simulation.
Our e-learning package was a useful way to both raise awareness about signs of sepsis and demonstrate how to escalate care. A completion rate of 80% by health professionals supported implementation success at every site.
Looking ahead, my ongoing research program, Safer Care for Children in Hospital, focuses on the long-term sustainability of the system in the WA Country Health Service. This work is key to empowering parents, including Aboriginal families and people from culturally and linguistically diverse backgrounds to feel safe and confident to raise their concerns if they recognise their child’s condition is getting worse in hospital.
Working in partnership with St John WA, the research team is measuring effectiveness of the system to predict patient clinical deterioration and outcomes throughout the patient journey from prehospital care to hospital discharge.
For more information visit www.ESCALATION.com.au
ED: The Safer Care for Children in Hospital research program is supported by funding from WA Future Health and Medical Research Fund and Stan Perron Charitable Foundation.
References available on request.






Add into this mix that millennial doctors will not accept the crazy hours of prior generations. Then add changing disease patterns reflective of the ageing demographics.
Data can be revealing and staggering. In the US, rates of autism have risen from one in 10,000 in the early 1960s to one in 36 nationally and one in 22 in California.
Notwithstanding current thinking that three into two can be anything it wants, reality has a way of biting. Three does not go into two.
As reported last month by Medical Forum, almost a fifth of WA’s medical specialists are due to reach retirement age in the next 10 years, while many senior doctors are working less hours in the public system. According to Ahpra there were 15,019 registered doctors in WA on June 30. Of these, 1882 (12.5%), had either limited or provisional registration or were non-practising.
Estimates put the average age of doctors in Australia in their mid-50s. This will likely rise with more people entering medicine as mature age students and taking longer to enter their chosen field.
Add into this mix that Millennial doctors will not accept the crazy hours of prior generations. Then add changing disease patterns reflective of the ageing demographics.
The cherry on the cake is Ahpra’s stated intention to effectively force doctors to retire at age 70. Before you all scream, they are not stopping doctors working but will make doing so a demeaning and expensive option. This could knock out up to 10% off the national workforce.
More demand – less capacity! Three into two?
What is the plan to attempt to make doctor numbers approach what the community expects? Health Minister Sanderson said it was important to build and retain a health workforce that would have the capacity and capability to provide quality care and support across the State.
This is a bland statement of the obvious with zero indication of how it is to be achieved.
The Federal Health Minister through Ahpra is trying to make it easier to bring in international medical graduates. So far there is little to suggest that this is keeping up with current, let alone future, demand. Post-COVID, Australia is not as appealing to would-be migrant doctors who are spoiled for choice with the number of countries facing the same issues we are.
We have both State and federal elections in the first half of 2025. Will any realistic plans be announced? Or will three just have to identify as going into two?


By E/Prof Johan Rosman, Nephrologist & Hypertension Specialist, Hollywood & Curtin Medical School
Hypertension as a modifiable risk factor remains the leading cause of death globally, accounting in 2020 for 1.4 billion deaths that year. This number is increasing despite the major efforts of international organisations, improved training of healthcare professionals and patient awareness campaigns.
Major global associations such as the International Society of Hypertension, the American Society of Hypertension and the European Society for Hypertension have special working groups monitoring the global burden of hypertension and its end-organ damages and deploy major initiatives to mitigate these and come up with guidelines.
As so often with guidelines, there is no worldwide consensus about the treatment of hypertension because of different reasons for hypertension in different parts of the world, the ability to screen for secondary causes and the availability of certain medications.
Regretfully, the guidelines are often generic, focus on common comorbidities, and give little specifics about how to treat hypertension in the elderly, who are an often difficult-to-treat subgroup.
Hypertension in the elderly comes with unique challenges that cannot be compared to younger age groups, and hence requires a very different approach to the treatment.
Systolic blood pressure continuously rises with age, partly as a physiological principle (lack of cerebral blood flow autoregulation, requiring higher systolic blood pressure), but also ageing consequences such as arterial stiffness.
In general, after the age of 55, the diastolic blood pressure declines, thus increasing pulse pressure. Whereas the guidelines have dictated for many years low blood pressures for all ages, awareness has grown that the elderly require a higher blood pressure to maintain


sufficient brain and other vital organ perfusion.
At the same time, this is a precarious balance, as these patients obviously are also more at risk for stroke. In ageing people, the risk of cardiovascular events and mortality remains directly related to the systolic pressure but is inversely related to the diastolic blood pressure.
The question remains, what is an acceptable blood pressure for an individual over 60 years of age?
Whereas for younger patients this has quite firmly been established at 115-125/75-80, for the elderly there
is not such a rule. At an older age, too many co-factors come into play that have their own influences on cardiovascular and cerebrovascular health (ischaemic heart disease, diabetes, hyperlipaemia, heart failure, etc).
The SHEP (Systolic Hypertension in the Elderly) Trial, and the STOP (Swedish Trial in Old Patients with Hypertension), showed a significant reduction in cardiovascular events if the blood pressure was maintained below 145/90, resp 143/78.
Studies in the elderly over 80 years of age, where typically clinicians become reluctant to treat elevated blood pressure, showed benefits if
Hypertension has equally deleterious effects in the elderly as in young patients, although there is a difference in the weight of systolic versus diastolic pressures
For physiological reasons, a slightly higher blood pressure in the elderly should be accepted
The choice of anti-hypertensive medication in the elderly differs from the guideline-proposed drugs for younger generations.
blood pressure could be targeted at 142/78. There was a negative effect on the results with a diastolic pressure below 60 mmHg. These studies were not controlled for secondary effects of treatment (such as falls) due to a too-
significant drop in blood pressure and the consequences of such trauma, especially since this group is frequently using anticoagulants.
For this reason, it is highly recommended not to rely on office blood pressures alone but do at least once a 24-hour ambulatory blood pressure measurement study.
Another factor that is stressed in literature is the concept of ‘frailty’, be it as general condition or secondary to another disease such as Parkinson’s where higher blood pressures will need to be tolerated to prevent the patient from falling and the blood pressure reduction would do more harm than good.
The question what drug to use in the elderly is not consistently answered in the literature. Whereas in younger generations an ACE inhibitor or Angiotensin Receptor Blocker, if needed, followed by a
Dihydropyridine and potentially after that hydrochlorthiazide is considered, in the elderly, especially those with frailty, a thiazide diuretic may be the first choice, followed by a non-dihydropyridine calcium antagonist, and only then an ACE inhibitor or Angiotensin Receptor Blocker.
Beta blockers should, given their profound effect on the heart rhythm, be kept for compelling indications. It needs to be said, that no hard data is available to back this up, and again, studies give conflicting results in the elderly.
Author competing interests – nil
Better medication management is needed for older hospital patients, which could in turn reduce their stay and lower their risk of death, according to a new Australian study.
Research by Flinders University and the Flinders Medical Centre, published in The Journal of the American Medical Directors Association, found that one in 10 older people experienced adverse drug reactions to medications while in hospital.
Researcher Dr Joshua Inglis said that as the population aged, patients had more chronic medical conditions and were taking more medications so it was increasingly important to prevent harm from the drugs.
The study looked at more than 700 patients aged 65 and older admitted to Flinders Medical Centre over three years and found that 72 of them had experienced an unwanted reaction to their medications, and they were associated with longer stays and a higher risk of death.
The findings have prompted calls for hospitals to take further steps to prevent medication-related harm.
The medicines most associated

with adverse drug reactions include those used to treat high blood pressure and other cardiac conditions, strong painkillers such as oxycodone, and antibiotics such as penicillin.
Side effects included kidney and liver injuries, low blood pressure, sedation, nausea and vomiting, diarrhoea and bleeding.
Dr Inglis said that, currently, doctors review each patient’s medications during their hospital stay, but multidisciplinary teams could take a hospital-wide approach to managing specific high-risk medications classes.
“Stewardship programs have
been successfully developed for antibiotics and shown to improve patient outcomes and the concept can also be applied to other highrisk medications such as opioids, anticoagulants and psychotropics,” he said.
“To our knowledge, this is the first study to find an association between experiencing an adverse drug reaction in hospital and serious consequences for patients.
“Importantly, it highlights the need for healthcare organisations to develop stewardship programs that prevent ADRs from occurring in the first place.”
Dermatology Specialist Group (DSG) announces that Dr Clare Tait is ceasing private Dermatology practice in January 2025. She will continue to provide outreach services to the Kimberley region through WACHS.

Dermatology Specialist Group in Ardross will continue to accept new and review referrals as usual.
To ensure continuity of care for Dr Tait’s patients, Dr Janet Kim is returning to DSG from interstate. All current patients can receive first class dermatology care from Dr Kim, or any of the other consultant dermatologists at DSG:








Dr Clare Tait extends her heartfelt thanks to all referring doctors for their support over the years and wishes all colleagues and their families the very best for the future.

5 Almondbury Rd, Ardross, WA 6153
Phone: (08) 9314 9900 Fax: (08) 9314 9988
Email: admin@dermatologists.com.au
Healthlink: quikchan dsgderm.com.au
By Mrs Gordana Petkovska, Nurse Practitioner
A palliative approach to care can be employed in managing complex chronic wounds that fail to heal despite optimal treatment. Palliation being the comprehensive care provided to individuals with life-limiting diseases or incurable advanced chronic conditions that focuses on relieving symptom burden and improving a patient's quality of life rather than curative treatments.
Healing as a goal of wound care may not be feasible when medical interventions are ineffective, or when the patient is unable to physically tolerate wound therapies.
Non-healing wounds include malignant lesions, though they are more often wounds associated with conditions such as advanced peripheral vascular disease, diabetes, musculoskeletal disease and neuropathic disorders.
Examples of such wounds may be gangrenous foot ulcers where amputation is declined, arterial leg ulcers with failed revascularisation attempts and sacral pressure injuries in patients with motor neurone disease on continuous positive air pressure therapy where positioning is limited.
Patients presenting with these types of chronic palliative wounds may not necessarily be at the end of life, but it is imperative to recognise that these wounds significantly impact their life expectancy, activities of daily living and quality of life.
Conversely, patients in palliative care can develop wounds as a natural consequence of disease progression, often due to comorbidities and complex symptoms such as malnutrition, dehydration, immobility and incontinence heightening susceptibility to skin injury.
A 2019 review of the Silverchain Community Specialist Palliative Care Service found pressure injuries and skin tears were the most common wound. A percentage of the superficial skin injuries were found to heal in this palliative population contrary to general consensus, while
Key messages
Not all wounds are able to be healed
A holistic assessment of the patient determines the goal of care and management plan
A multidisciplinary, patient centred, palliative approach should be adopted for unhealable wounds.
the deeper wounds typically did not. It is important to recognise that just because a patient is for palliation does not mean that their wounds are not healable.
A comprehensive assessment is fundamental and encompasses the wound, the individual, and the physical and psychosocial healing environment.
The wound presentation guides the clinician in choosing products to manage exudate and malodour, support the need for debridement, provide antimicrobial treatments and, if possible, facilitate healing. Determining the underlying wound aetiology can prevent further injury to the wound and potentially optimise wound interventions and outcomes.
Management of underlying comorbid conditions and addressing functional and nutritional deficits reduce the impact of systemic confounders on healing, and further guides targeted therapies.
The person’s environment, support systems, and personal desires and goals of care are also crucial considerations that shape the wound management plan. Access to resources, equipment, assistive devices, and formal or informal caregiver support can substantially affect outcomes.
At assessment, if most of the patient’s intrinsic and extrinsic factors can be identified and addressed, the wound may be responsive to standard evidence-based wound care interventions even if the patient is palliated.

An example is a skin tear on the arm of an end-stage heart failure patient that is treated with appropriate cleansing, silicone dressing, and protective strategies that allow for healing.
However, suppose the same patient subsequently develops a venous leg ulcer that precludes the use of compression therapy due to its impact on cardiac function. In that case, it presents significant obstacles to wound healing and may not be achievable as a goal. Wound palliation for the leg ulcer may become the best approach, while healing remains the goal for the skin tear.
Rather than focusing solely on the wound, the clinician must adopt a holistic approach to align the wound management plan with the patient's anticipated clinical trajectory, values and care goals determining if healing is unachievable.
Careful consideration of the patient’s prognosis, their quality of life and treatment preferences are essential particularly if the patient is transitioning to a palliative care approach. Strategies that focus on symptom control and addressing quality of life issues instead of wound closure predominate.
Informing patients of the risks and benefits of potential treatment options is crucial, however the practitioner needs to ensure they do not overburden or offer unreasonable hope. All healthcare providers, the patient and their significant others must discuss and agree on the palliative plan of care to avoid conflict and confusion. Open, honest and empathetic communication with the patient and their family is essential to ensure shared understanding and agreement on the care approach.
– References available on request
Author competing interests – nil
ED: The author is a nurse practitioner with Silverchain.
By Prof Camile S. Farah, Oral Medicine & Maxillofacial Pathology,
Ageing is a complex process reflecting changes that occur over the lifespan. Life expectancy has increased remarkably during the latter half of the last century. The number of persons aged 60 or above will rise from 962 million globally in 2017 to 2.1 billion in 2050 and 3.1 billion in 2100.
Recognising the manifestations of age changes in the oral and dental tissues can help clinicians distinguish healthy ageing changes from pathological conditions, even though the incidence and prevalence of several oral disorders and conditions, such as oral lichen planus, oral ulceration, oral potentially malignant disorders, and oral cancer, frequently increase with age.
Increasing evidence supports that osteoporosis contributes to the loss of teeth via loss of alveolar bone and potentially basal bone. It can be difficult to distinguish ageing changes from those of osteoarthritis. The use of bisphosphonates to treat osteoporosis has been found to increase the incidence of osteonecrosis of the jaw in some cases. This relationship has been established in different populations throughout the world.
With ageing, an individual may lose some or all of their teeth. Teeth become worn, and muscles of mastication may be subject to atrophy. These changes lead to impairments in oral function, particularly speech and mastication.
Physical maturity is reached in the early 20s, and subsequently human facial soft tissues begin to undergo changes not as a consequence of growth but due to the onset of ‘ageing’, which involves a gradual decrease in skin elasticity, reduction in subcutaneous fatty tissue volumes, increase in muscle tone, and the effects of gravity.
These factors lead to an increase in skin folds ‘wrinkles’, usually perpendicular to facial muscle fibre direction, and a decrease in overall


Recognising the manifestations of age changes in the oral and dental tissues can help clinicians distinguish healthy ageing changes from pathological conditions
The incidence and prevalence of oral lichen planus, oral ulceration, oral potentially malignant disorders, and oral cancer increase with ageing
Taste and smell sensitivities often decline with ageing and may be associated with a reduction of appetite as the food becomes tasteless.
facial volume. Facial soft tissue thickness varies between different regions of the face, generally being thinnest over the tip and bridge of the nose and infraorbital rim and thickest over the lips, chin, cheek, and lower jaw.
The oral cavity has unique structures to perform functions necessary for life (e.g. speech, respiration, mastication, taste, digestion, and deglutition). Anatomical changes may impact these functions. Changes to the
oral mucosa with ageing are often unrecognisable. However, ageing makes the mucosa more susceptible to local trauma and oral diseases. Age-related hyposalivation may alter the clinical appearance of oral mucosa substantially.
Neurological impairment increases with advanced age. Taste and smell sensitivities often decline with ageing and may be associated with reduced appetite as the food becomes tasteless. This decline is thought to be due to apoptosis of cells in the taste buds of the oral cavity.
This may affect nutritional status, as individuals may add abundant seasoning (particularly salt or sugar that have potential harmful effects), or they may prefer very hot foods, which may burn the gingiva or palatal mucosae.
Also, there are groups of elderly with certain disorders affecting their ability to taste either as a response to the prolonged use of medications or to the course of the disease itself. Examples of these disorders include mouth, nose, or sinus infections, gingivitis and periodontitis, cancer, and chronic kidney or liver disease. Medications to manage hypertension (e.g. ACE inhibitors), hypercholesterolemia (e.g. statins),
By Prof Peter Drummond, Centre for Healthy Ageing, Murdoch University
Pain is common in Alzheimer's disease and in its preclinical stages including subjective cognitive decline and mild cognitive impairment, but what underlies this association is unclear.
In a novel study at Murdoch University, supported by the Alzheimer's Association-USA, a research team is investigating whether degeneration of a small but powerful centre in the brainstem, the locus coeruleus, might explain this connection.
The locus coeruleus is a tiny bilateral cluster of noradrenergic neurons in the upper pons. Among other functions, these neurons regulate attention, arousal and sleep-wake cycles. They also regulate sensory inputs including sight and sound by helping to filter out background activity, thus optimising signal strength.
They use this capacity to control the flow of nociceptive traffic (which signals pain) downstream in the spinal cord and upstream in the thalamus and prefrontal cortex.
Crucially, neurodegeneration in the locus coeruleus starts decades before the onset of memory complaints in people who later
Key messages
Pain is common in dementia
Reduced ability to control pain could be an early warning sign
New research is looking at this connection.
develop Alzheimer's disease. Once it reaches a tipping point, this neurodegeneration disrupts attention and arousal, thereby seriously impacting learning and memory.
Long before this, it could also impact the capacity to control pain. If so, it might be possible to detect early signs of neurodegeneration in the locus coeruleus, a step toward Alzheimer’s disease, by assessing physiological and behavioural responses to pain.
The locus coeruleus provides a bridge between arousal centres in the brain and sympathetic nervous system output which, among other physiological effects, drives pupillary dilatation. This link is so strong that reactivity of the pupils is increasingly being used in physiological studies to track activity in the locus coeruleus.
In the Murdoch University study, pupillary dilatation to a sudden
and depression may also affect the sense of taste.
The functions of saliva include lubricating and maintaining the integrity of the oral mucous membrane, soft tissue repair, balancing pH buffering, maintenance of ecological equilibrium, maintenance of tooth integrity, and physical and immunological protection.
Although salivary flow is said to diminish as an age-related process, salivary production in healthy
elderly patients remains stable. Gender and weight can influence salivary flow as these factors are correlated with the size of salivary glands.
Males and overweight healthy people have larger major glands and subsequently have higher salivary flow. Gender-related salivary flow variations become more obvious with ageing and beyond the age of 55. It is important to note that hormonal changes in postmenopausal females reduce unstimulated salivary flow remarkably. However, controversy surrounds the impact of menopause

loud noise and to painful stimuli (a weak electric shock and painfully cold water) is being used to assess the functional integrity of the locus coeruleus in people with subtle or more obvious signs of memory impairment.
The hope is that pupillary responses of this nature can be used as a screening tool for early signs of neurodegeneration in the locus coeruleus (a possible precursor of Alzheimer's disease neuropathology) in the future.
The research team is now seeking volunteers aged between 60 and 85 years with memory difficulties or other signs of mild cognitive impairment to participate in this study which will involve one or two assessment sessions in our lab. If you know of anyone who might be interested in participating, or who would like to know more about the study, please ask them to email p.drummond@murdoch.edu.au or phone 08 9360 2415. The research has been approved by the human research ethics committee at Murdoch University.
Author competing interests – the author is leading the research quoted.
on saliva production. Interestingly, the use of hormone replacement therapy in postmenopausal females is said to result in recovery of salivary flow.
– References available on request
Author competing interests – the author is co-author and co-editor of Contemporary Oral Medicine: A Comprehensive Approach to Clinical Practice published by Springer from which excerpts are cited in this article and referenced.
By Dr Hendrick Tan, Radiation Oncologist, Murdoch
Radiation therapy is an important component of cancer treatment, where a multi-disciplinary approach is the standard of care. Modern computer technology in treatment planning, coupled with continuous innovation and in the improvement in the knowledge of the radiobiology of cancer, has led to the development of new radiation therapy techniques.
Over the past 30 years, we have moved from two-dimensional to three-dimensional radiation therapy with the development of inverse computational algorithms allowing the planning of precise, complex radiation delivery patterns.
Modern techniques such as imageguided intensity-modulated radiation therapy (IGRT) and stereotactic ablative radiation therapy (SABR) have been implemented, which demonstrate improved shaping of the radiation dose to the target and away from surrounding healthy organs, allowing for radiation dose escalation to tumours with decreased toxicities.
Globally, we are witnessing the implementation of the latest revolution in radiation therapy, the magnetic resonance imaging linear accelerator (MR Linac), a technology that has integrated a diagnostic quality 1.5T MRI scanner with the treatment delivery linear accelerator. The MR Linac can provide real-time images during treatment without increased radiation exposure to deliver what is referred to as online MR-guided adaptive radiation therapy (MRgRT).
Benefits and clinical indications
MRgRT represents a paradigm shift in radiation therapy. With enhanced visualisation of internal organs using the excellent soft tissue delineation on the MRI and the ability to monitor anatomical structures, position and physiological motions during treatment delivery, we can safely escalate the radiation dose and reduce margins during treatment planning.


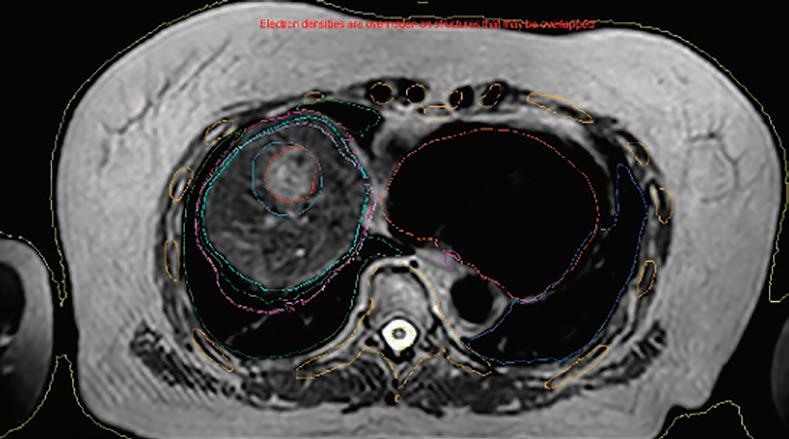
Readily available imaging at every treatment session allows for adaptive radiation therapy by which the dose delivered at each session can be evaluated and optimised on the go, taking into account daily variations in patient position and internal organ physiological motions to mitigate toxicities.
The versatility of the MR Linac makes it possible to help treat numerous tumour sites where the soft tissue contrast using MRgRT
will allow safe high-precision treatment with optimal sparing of surrounding healthy organs.
Most experienced centres and the European Society for Radiotherapy and Oncology (ESTRO) have recommended clinical application to prostate cancer, brain tumours, pancreatic cancer, liver cancer and pelvic lymph nodes. Moving intraabdominal or pelvis targets would specifically benefit from the MRgRT motion management approach
MR Linac offers real-time tumour tracking and delivery, allowing clinicians to target tumours more precisely
The integration of MRI with a linear accelerator provides superior soft-tissue imaging to aid accurate delineation of the tumour and surrounding healthy organs
While MR Linac is a promising technology, high capital cost and complexity limit widespread adoption. Ongoing research and advancements will likely improve future accessibility.
due to the deep-seated nature, the difficulty of placing fiducials markers and the tendency for variable deformation between treatment sessions.
Another noteworthy advantage of the MR Linac is ‘radiomics’, which is the application of quantitative imaging analysis to predict tumour response or resistance based on functional, structural, or physiological MR imaging data in addition to anatomical images obtained by the MRI. Radiomics can be integrated with traditional clinical data to establish tumours that will respond to treatment and assist with decision-making to identify tumours that would benefit from radiation dose escalation.
There are four MR Linacs in Australia, the latest of which is in Murdoch, Western Australia. It is integral to provide specific training and credentials for staff to ensure the safe and effective utilisation of the MR Linac, and all centres have a rigorous training and credentialing process in place.
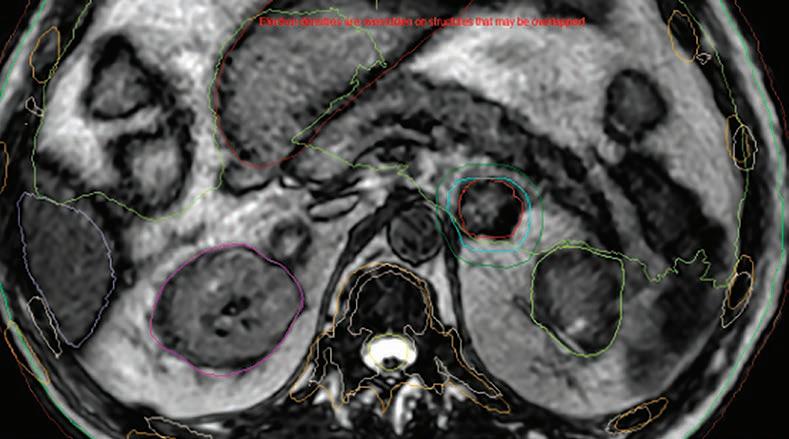
Despite the superior imaging quality of the MR Linac, the visualisation of targets may be affected by breathing-induced motion artefacts. To address this, a compression belt is recommended to reduce breathing artefacts when treating targets in the upper abdomen.
Furthermore, larger tumours may pose a challenge to treatment due to the limited field of view in the superior-inferior direction on the MR Linac. By nature of MRgRT being fully adaptive, the treatment times are longer, hence, compliance and comfort could be a potential issue for a subset of patients.
Treatment contra-indications include patients with MRIincompatible implanted materials or claustrophobia.
Finally, higher capital costs, resources, and the complexity of the treatment have constrained the widespread adoption of this technology.
While MR Linac offers a promising solution to high-precision treatment with more outcome data now being published, the long-term outcomes of MRgRT remain unclear. To produce real-world evidence, prospective registries have been established, such as MOMENTUM, a multi-institutional, international registry collecting clinical, technical, and patient-reported outcome data. These will pave the way to ongoing evidence-based development of MRgRT to confirm the most suitable treatment sites and techniques to enhance toxicity reductions.
Ultimately, the MR Linac has unveiled a transformative shift in the radiation therapy treatment paradigm. It presents opportunities for greater personalisation of treatment and holds the potential to revolutionise the field of radiation oncology in the coming decades, inspiring hope for improved patient outcomes.
– References available on request
Author competing interests – nil
Good nutrition is essential for healthy ageing, yet older adults face multiple significant challenges in achieving adequate dietary intake. Screening and monitoring are important.
Addressing nutritional issues requires a comprehensive, person-centered approach including social and psychological interventions aimed at improving access to and quality of food.
Prioritising nutrition in older adults can improve health outcomes, reduce healthcare costs and enhance the well-being of ageing populations.
Physical barriers can be tackled via dental care and dietary modification. Encouraging exercise can aid appetite,
Social support and meal assistance are also helpful. Encourage participation in communal meal programs (e.g. senior centers, Meals on Wheels) to improve social interaction and increase meal enjoyment.
Mealtime assistance and caregiver support, education and training are helpful strategies. Home meal delivery services such as Meals on Wheels can be engaged to ensure access to good quality balanced meals, especially for elderly individuals with mobility issues or limited access to grocery shopping. Review medications that interfere with appetite or nutrient absorption or cause side effects (nausea, dry mouth, or reduced appetite). Tailor diets to manage chronic conditions such as diabetes, heart disease, or gastrointestinal issues, while ensuring that nutritional needs are met.
For individuals with cognitive impairment, offer simple, familiar foods and assist with mealtime reminders. Treat any associated mental health issue (e.g. depression).
A multidisciplinary approach makes a big difference. Collaborate with dietitians, speech therapists, occupational therapists and geriatricians as needed. Home visits by community nurses or dietitians for assessment of dietary intake and addressing meal preparation barriers.
Ongoing follow up and monitoring includes setting follow-up appointments to assess the patient's progress, monitor weight, and adjust interventions, as necessary. If there is no improvement, consider more comprehensive interventions in collaboration with a specialist. By integrating regular assessment, early intervention, and a collaborative approach, general practitioners can effectively manage malnutrition in elderly patients, improving both their quality of life and health outcomes and reduce the burden and cost of care.
• Imaging complete in 20 seconds
• Full body images in standing position
• 24 hour report turnaround
• True 1:1 scale
Refer your patients now for lower dose imaging and better visualisation for diagnostic or surgical planning and post operative assessment.
• Low dose radiation
• Walk ins welcome
• All request forms accepted
• All scans are bulk billed


A Perth dancer’s illness forced her to adopt a whole new attitude toward movement while finding a way back to what she loves.
By Ara Jansen
Daisy Sanders loves to dance. When she had to stop dancing because of chronic fatigue, she used the artform as her recovery tool.
On the way, the 34-year-old dancer, multidisciplinary and community artist created a work called A Resting Mess, which explores energy and fatigue on a personal and planetary level.
Hailing from a family which loved and participated in the arts, Daisy excelled academically and surprised everyone when she chose to pursue dance, moving from Canberra to Perth to study at WAAPA. She studied ballet but it wasn’t quite right as she was missing the social interaction and community connection.
About eight years ago, Daisy was struggling with anxiety and depression. After a surgery for endometriosis this progressed into severe chronic fatigue syndrome. These combined conditions meant that Daisy couldn’t work, couldn’t walk for more than a few minutes and found it hard to even get out of bed.
“I remember at one moment it became really clear that I had to dance again,” says Daisy. “I needed to go back to dance, but not to ballet, because it needed to be physical and creative. I wanted to dance and connect with people and have the energy for that. My greatest fear is that I would never dance again.”


Starting by rolling out of bed, onto the floor and doing some gentle movements, Daisy gradually added more movement as she could manage it, experimenting with dance to heal. She was forced to be very patient and listen to her body.
Over a number of years, Daisy eventually recovered full health and once more found her home in dance. The journey helped her develop a way of leading other artists to dance, build community, create and perform that is profoundly caring and joyful.
Among other professional activities, over the past eight years Daisy created the dance and theatre piece titled A Resting Mess. While it seems counterintuitive for a dancer or actor, Daisy uses something she calls deep rest to facilitate her own dancing and the work she created.
“Dancing became my healing tool. Rest has come to underpin my dancing. That will be eternal for me and it’s now my way of working. When I rest deeply my life force comes back to me,” she says.
For her recovery, Daisy gathered a team of health professionals around her – doctors, allied and alternative health practitioners –changed her diet, gave up alcohol and had an adaptive daily routine around getting up, sleeping and incrementally increasing activity.
She developed the somatic practice of listening closely to her body and utilised techniques such as Alexander and Feldenkreis to survey her internal landscape.
“Even more than before, I learnt to listen to the nuances of my body. What does it need in every moment? I listened closely and honoured my body, inviting myself into movement while being tender with myself. This radical regard for the body is where A Resting Mess came from.”
She went back to WAAPA, completing an honours degree at her own pace, which included going to dance classes and lying down on the floor whenever she needed to. Daisy became quite well-known for this, but her actions allowed her to rest and recover, resisting the
urge to overdo it and calming her nervous system.
She also schooled her body to engage in deep rest for short bursts, which has become one of the cornerstones of her dance style and teaching. It values humour, the health of the body, acceptance that energy changes and listening to the body to cultivate both resting deeply and activating energy and vitality when needed.
“I listen to my body and dance with the way my energy changes. I’m interested in being really in-tune with different levels of energy, both physical and otherwise. For example, how you can change the feeling in the space between the performers and an audience. How you can create not only the movement but the tone, the atmosphere; it’s like electricity or a social charge or something else.”
A Resting Mess has been staged locally, interstate and internationally in development forms. This year it enjoyed a full-scale premiere in Fremantle – a unique project including a free community space for rest and reflection alongside wild and warm-hearted performances exploring personal and planetary fatigue. How can deep rest help us come together, care for each other and face the world’s mess, it asks.
Like her own recovery, the piece has high energy moments and more restful ones, which Daisy hopes affects the audience in the same way.
“I have a saying: rest is a feeling, not an action. When emotions bubble up and there’s waves of rage or enthusiasm, you have the freedom to be and express that fully. My real understanding of rest is about presence, about having an attuned sensitivity to what the body needs, combined with permission to express and feel, so that everything can pass through the body. It’s about surrendering to it all and then coming back to equilibrium.
“When I was sick, I did a lot of meditation, another way to access detailed body awareness. My work has these combined aspects of meditation, expressive feeling and movement that constantly changes in energy. These qualities assist my health but also translate to supporting other artists and the audience to become present, rest deeply, feel and reflect.”
Sheridan Adams landed her first major role as a lead in Wicked. She’s making the role of Elphaba her own.
When Sheridan Adams auditioned for an ensemble spot in the stage musical Wicked, she never expected to come away with the leading role.
“My audition was quite spectacular in how it turned out,” laughs Sheridan, who landed the part of Elphaba, the green Wicked Witch of the West, in the hugely popular musical.
“I applied online and sent through a video of me singing. I was auditioning for the ensemble, but I prepared for a few parts. A number of things happened, and I ended up singing Defying Gravity, which is Elphaba’s big song. I did more auditions and thought I was in line for a stand-by role until they told me I had the part of Elphaba. It was the best experience of my life!”
Elphaba is Sheridan’s first major role and a dream come true. It’s also something the Melbourne singer thought she’d have to work up to. By the time Wicked arrives in Perth in December, she will have been playing the part for well over a year.
It’s a big load for a young singer and actress as Elphaba is on stage for most of the show.
By Ara Jansen
“There’s time when it’s just me on the stage and no one else to rely on,” she says. “Plus, it has been running for 20 years and there have been phenomenal women playing her around the world. I’ve been their fans and now I’m playing the role.
“I’ve come to find so much joy in playing Elphaba. I love that I keep discovering things about her and building them into the performance. I feel really comfortable with her now and I’m having so much fun growing along with the part.”
Sheridan discovered musical theatre in her early teens and fell in love with Wicked after hearing it for the first time and seeing Jemma Rix play the part remains an inspiration.
She says, of course, you want to make a part your own. You also want to stay true to yourself and somehow honour the people who have played the part before you.
“I wanted to follow my instincts and truths and didn’t want to be disingenuous in how I played her. I’ve also got creative freedom to add in pieces of me. That’s why I think each Elphaba can be so different.”
As part of her preparation, Sheridan listened to lots of podcasts of other
actresses talking about how and why they played Elphaba the way they did, and what to expect on and off stage.
“I’m discovering so much about my voice through this part and how to keep it healthy. I get nine to 10 hours’ sleep, I’m careful with what I eat and drink, plus I drink lots of water. I’ve cut things like alcohol and strong spices out. I also have to be careful how I socialise.
“I like to hike when I can. I have a strict warm-up routine for my voice and make sure to rest and relax and work my back and release tension in my body. Elphaba’s costume and props are heavy and I wear heels every night. There’s not a lot of dancing but she’s very physical.”
While Sheridan has never accidentally left the theatre in full green make-up, she says despite best efforts, she’ll always find a spot of green somewhere. She reckons that’s a small price to pay for the biggest and best role of her life to date.
Wicked tickets are on sale now for shows from 15 December to 26 January at Crown Theatre. Tickets from Wickedthemusical.com.au
Mark Warren is a champion of the lesser known varieties in Margaret River. Varieties such as Gamay, Vermentino, Fiano, Grenache and Tempranillo have all found their way to his Yallingup winery.
With degrees in science and wine science coupled with years of teaching wine science and advanced sensory at Curtin University’s branch in Margaret River, he is well equipped to explore many paths that others may not choose to follow. After starting his career at Lamonts in the Swan Valley, he moved south where he has been the winemaker at Happs for the past 22 years. In addition. he makes wine under his own Marq label as well as finding the time to consult with many other small wineries. He is responsible for producing 60-70 different wines a year.
This month’s tasting was most enjoyable. All the wines were beautifully made, each highlighting the best sensory characters of the variety in the glass. All are eminently drinkable right now.

2024 Marq Vermentino (12.9% ABV, rrp $28)
This popular Sardinian variety is given four days of skins contact to bring out texture and flavour. Stainless steel fermentation and early bottling capture the fresh aromatics of flowers, tropical fruit and fine talc. Palate is clean, dry, mouthfilling and a touch savoury. A very appetising alternative to the semillon, sauvignon blanc style.
2023 Marq Epiq Chardonnay (12.8% ABV, rrp $55)
From the cooler part of Margaret River around the village of Witchcliffe, the best of the chardonnay harvest is wild yeast fermented in new oak (50%) then left on lees for 10 months prior to bottling. A very refined bouquet of peach, grapefruit and a touch of spicy oak. very crisp and clean in the mouth. Powerful yet tight with the promise of opening more with time. This is classic premium Margaret River chardonnay.
2023 Marq Serious Rose (13.1% ABV, rrp $28)
From Grenache grown in southern Margaret River, early picking with two-hour skin contact, then five months’ lees maturation in old barrels. Vibrant pale salmon pink in colour. Heady fragrance of berries and flowers. Palate has texture with soft tannins and clean well-rounded dry finish. Indeed, a serious rose.

2023 Marq Lo-fi Shiraz (13.7% ABV rrp $30)
The most interesting wine of the tasting. Premium shiraz fruit made ‘au naturel’ with no chemicals. A tribute to good viticulture. Only a touch of sulphites at fermentation. This wine has seen no oak, having matured in large concrete eggs and bottled unfiltered. Pure berry fruit spicy shiraz with lovely mouthfeel, soft gentle tannins and a clean long finish. You could call this a Syrah style. A very successful collaboration with Marq and Old Bridge Cellars. Definitely worth seeking out.
2022 Epiq Malbec (14.01% alcohol, rrp $55,)
The best parcels of Malbec from a single Wilyabrup vineyard are fermented to dryness on skins for 15 days before receiving 18 months maturation in 1-year-old oak. This wine has an exuberant aroma of rich ripe red and blue berries and violets leading to an intense fruity sweetness in the mouth. The flavours linger long and seductively. Oak is hardly evident. such is the power of the malbec fruit. A real cracker!


Support services group Avivo is celebrating the vital and often unseen work their people do through three unique public art installations.
Support workers are often unsung heroes. In an effort to celebrate them, reveal them in a different light and recruit new employees, community services organisation Avivo partnered with Perth agency Block Branding to create The Support Project.
It’s a series of three life-sized sculptural installations, which are called monuments, each with two intersecting metal plates, one bearing the cut-out silhouette of an Avivo support worker and the other their supported customer. The intersection of these two people symbolises the mutual respect, interconnectedness and interdependence of the relationship.
A series of short video documentaries capture the personal stories behind the artworks. This has allowed Avivo to share the stories on social media and reach a wider audience and create a deeper connection through the stories.
“We were looking to create a branddriven campaign that reflects our values,” says Avivo communication and engagement lead, Natalie Green. “Support work is a job which is not highly paid, it’s emotionally taxing and the people that do it, love it.
“We wanted to make a statement about support workers and about
Ara Jansen reports
the value of the relationship between them and their customers. Those relationships make a unique and quality contribution to the fabric of our community.”
Avivo CEO Kate Fulton said support work was often misunderstood in the community and The Support Project was a way of showing the public how important it was and how it could make a difference to the lives of both parties.
“I hope our monuments spark conversations about the role itself and the enormous benefits this work can bring,” she said.
Avivo has just under 1000 support workers around WA working with about 3000 people and families. One of the relationships highlighted in the installations is between support worker Paul and his customer Kenny.
“Kenny hugs everyone and has a beautiful warmth about him,” says Natalie. “He likes to go to his local Subway for lunch. Watching him interact with people there is gorgeous and seeing how Paul helps him connect with the people behind the counter is special. Paul supports him with such care and respect.
“In that way, good support workers are invaluable in communities and building communities and making
sure that people are accepted. Paul and Kenny have worked together for nine years, so that relationship is pretty special – that’s a lot of time and love.”
Natalie says the project is also a reminder about inclusion and championing diversity, while redefining the notion of heroes. This is especially true for support workers, who for the most go about their business quietly and without fanfare.
“We’ve been able to put The Support Project in front of a diverse audience and that has started a lot of conversations. The project has been very well received and it’s something different for the sector.
“We want it to reach people who might not have considered support work but through this project see what satisfying work it can be and what the benefits are. One of the key things is seeing how reciprocal these relationships are. As a human, the value you get from support work is tremendous. This is heart work.”
The Support Project has been seen in Kings Park, Crown Towers and Fremantle’s Walyalup Civic Centre. Avivo is planning more appearances across metro sites and in the regions. To find out where they go next: www.avivo.org.au/the-supportproject/the-monuments


Rare Large Medical Suite on Hollywood Campus
•Huge 96sqm* medical suite
•Generous waiting and reception area
•2 huge consulting rooms
•Fully Fitted & Furnished Suite
•1 car bay on title
•Ready for occupation
•Central location within the specialist centre
•Modern fit out
•Exclusive basement storage area
Asking Price $984,000+ GST
Asking Rent $450/sqm + Outgoings + GST
Luke Randazzo 0417 181 309 lrandazzo@brwa.com.au
Rob Selid 0412 198 294 rselid@brwa.com.au

Lot 3 / 140 Mounts Bay Road, PERTH Mount Medical Centre - RARE OPPORTUNITY
MMJ Real Estate (WA) are pleased to present to market this rare opportunity to buy this 76sqm medical consulting suite located on the third floor within the Mount Medical Centre.
Key Features:
•Strata area of 76sqm
•Fully fitted with reception, meeting room and main consulting room
•Small storage area
•Kitchenette
•Corner position with good natural light
•Views towards Kings Park
•2 secure undercover car parking bays
This unit is situated within a prime location adjacent to the Mount Private Hospital one of Western Australia’s leading private providers of Cardiology and Cardiac Surgery.
For more details or to inspect contact Tom Prout on 0434 746 259 or tom.prout@mmj.com.au


Medical & Consulting
• Offices
56B Mornington Parkway, Ellenbrook, WA 6069
Price information
Lease: $25,000 excluding GST p.a.
Key property information
Floor area: 80 m2
Outgoings: $10,100 p.a.
Specialised Medical Unit
•Rare Medically Zoned Unit
•Previous Dental Use
•Available Immediately
Tilt Commercial is pleased to present this dedicated medical suite for lease in the rapidly expanding area of Ellenbrook. As one of only two units on site, this facility is not to be missed.
• 80 m2 medical unit
• Independent rear parking for staff
• Fit-out included if required
• Previously used for dentistry
• Adjoining orthodontist
• Part of the Mornington Medical strip
• Front parking and entry for clients
• Rear parking and entry for staff
• Available for immediate occupation
For further details, please contact
Adam Yeo from Tilt Commercial, 0410 483 121

WEMBLEY
2 rooms available for lease
Consulting room 15m2
Consult/treatment room 23m2
(has sink, can be sub-divided)
Within Suite 2, 178 Cambridge Street, Ground floor
Undercover car bays available for staff parking
Opposite St John of God Hospital Subiaco
Radiology and pathology in same building
Physiotherapy available on site
Great patient parking
600m walk from Subiaco train station
Sessional basis considered
Specific fit-out requirements to be discussed
Admin support requirements can be discussed
·Suite facilities include new reception/ waiting room, kitchenette/break room, treatment rooms
For more details or to view, contact Johan on 6166 3751 or jm@thebonejoint.com.au

SOUTH LAKE
Medical Rooms Available for Specialists and Allied Health
Lakes Shopping Centre, Shop 2, 620 Northlake Rd, South Lake WA 6164
•Available for ALL Specialists and allied health professionals. Opportunity to become a part of the GP clinic / support.
•Consulting rooms, reception/waiting area, kitchen/breakout area, store records room, and other zones.
•These consulting suites are situated on the ground floor of the medical practice.
•Pathology on site (Clinipath)
•Room Sizes:
– Room 3: 3.5 x 3.4 meters = 12 Sq m
– Room 4: 4 x 3.2 meters = 12.8 Sq m
– Room 5: 4 x 3.2 meters = 12.8 Sq m
•Rent hourly and full time available.
•Rent negotiable.
For Further details and enquiries please contact p.manager@southlakefamilypractice.com.au or 08 9417 1009

Earn 100% of Billings for the First 3 Months!
Join our well-established, accredited mixed-billing clinic in Burswood and earn 100% of billings for the first 3 months (75% thereafter).
Perfect for new VR GPs looking to establish themselves, with full-time/ part-time options.
Work alongside 3 experienced GPs in a fully computerized clinic with on-site pathology and RN support.
Please contact Dr Ang on 9472 9306 or Email: info@thewalkingp.com.au

Central City Medical Centre
Full time or Part-time VR GP
Private doctor-owned medical centre, providing excellent medical services to our patients for 35 years.
We offer:
•Excellent earning potential as a private billing Medical Centre
•Experienced administrationmanagement team
•Convenient proximity to the CBD
•Hourly retainer for the first few months while you settle in and build your own patient base
•Full-time doctors have exclusive use of their own room and part-time doctors would share with another part-time doctor.
Contact the Practice Manager, Claire Stocks, on 0422 511 906 or claires@ccmc.net.au

Queens Road Surgery is a busy GP owned general practice located in Mount Pleasant.
We are looking for a VR GP to join our well established practice.
We offer a supportive team based culture, experienced administrative staff and quality full time nursing support.
Queens Road Surgery is a fully equipped accredited practice.
For a confidential discussion please contact our Practice Manager Narelle 0412 113 584 or narelle@queensroadsurgery.com.au
Contact Ross, classifieds@mforum.com.au or phone 9203 5222 to place your classified advert
State of the art new building in Murdoch Square precinct
Well appointed with dedicated reception area Sessional or permanent lease available


Contact Ross, classifieds@mforum.com.au or phone 9203 5222 to place your classified advert
Contact Michelle Cooper – Practice Manager 08 6183 1945 or admin@perthpain.com.au

KALGOORLIE – The RFDS WA Strategy
2024 – 2028 strives to make a positive difference to the health and well-being of people living and working in regional WA.
One of the focus areas will be to expand Primary Health Care services for a bigger community impact, with an initiative to establish an inaugural RFDS GP Clinic in Kalgoorlie, partnered with the Kalgoorlie Campus of the Curtin Goldfields University Department of Rural Health. We are looking for a Clinical Lead General Practitioner, who will provide clinical leadership for the RFDS General Practice Clinic supporting the delivery of high-quality care to patients and the community.
Please contact Lauren.Dawe@rfdswa.com.auau

rfdswa.com.au



Phone: 0432 895 542
Apply Now and Join a Rapidly Growing Team!!!

The M Clinic is seeking a GP to join our dedicated Perth team to help manage positive STIs and BBVs as well as prescribe PrEP to eligible persons. Training will be included.
LOCATION Perth, WA RATE 70% of billings, with additional incentives available for the right candidate OUR VALUES Compassion, Inclusion, Respect, Integrity, and Collaboration
ABOUT US M Clinic is Perth’s only sexual health clinic specifically for gay, bi, trans, gender diverse and non-binary people, and for anyone who identifies as a man who has sex with other men.
The successful candidate will:
Hold full registration with AHPRA and have the necessary permissions to prescribe and practice in Australia. Bring a non-judgmental approach to care, ensuring a respectful and inclusive experience for all clients. Provide care to a diverse client base, focusing on the needs of vulnerable populations.

Work in a supportive environment with on-site pathology services and nursing support. Enjoy a flexible working arrangement with a 70% share of billings and the potential for further incentives. Be passionate about making a positive difference to members of the LGBTIQA+ community through compassionate and quality medical care.
Sharmila Radha Krishnan