Dr Stephanie Giandzi Recent fellow












Dr Stephanie Giandzi Recent fellow






It is estimated that the screening program could reduce mortality rates by 20% and prevent more than 12,000 deaths in its first 10 years.
Andrea Downey | Managing Editor
Australia is a world leader on smoking cession, but lung cancer remains our leading cause of cancer death.
This is partly down to the late stage that most lung cancers are detected – often by the time symptoms present the disease has spread and it is too late for curative treatment.
Part of the solution to reducing deaths is catching the disease early. We already have successful screening programs in place for breast, bowel and cervical cancer and now, for the first time in decades, a lung cancer screening program will begin later this year.
It is estimated that the screening program could reduce mortality rates by 20% and prevent more than 12,000 deaths in its first 10 years.
While prevention is always better than a cure and efforts must still be made to tackle the causes of lung cancer, there is hope this screening program could see Australia become a world leader in lung cancer survival too.
And now a quick note from me, your new Managing Editor. Health journalism has been my passion for years. I have spent the last nine years living in the UK covering the NHS and health news for national publications, most recently a nurses’ magazine, and I feel privileged to be able to continue that work at Medical Forum
My door is always open for ideas, collaborations and general chat about the goings on in the local health sector, so please don’t hesitate to get in touch.
I am excited to be continuing to deliver the news and features you want to read in these pivotal times for the industry.
SYNDICATION AND REPRODUCTION Contributors should be aware the publisher asserts the right to syndicate material appearing in Medical Forum on the mforum.com.au website. Contributors who wish to reproduce any material as it appears in Medical Forum must contact the publisher for copyright permission.
DISCLAIMER Medical Forum is published by Medforum Pty Ltd (Publisher) as an independent publication for health professionals in Western Australia. Neither the Publisher nor its personnel are medical practitioners, and do not give medical advice, treatment, cures or diagnoses. Nothing in Medical Forum is intended to be medical advice or a substitute for consulting a medical practitioner. You should seek immediate medical attention if you believe you may be suffering from a medical condition. The support of all advertisers, sponsors and contributors is welcome. To the maximum extent permitted by law, neither the Publisher nor any of its personnel will have any liability for the information or advice contained in Medical Forum. The statements or opinions expressed in the magazine reflect the views of the authors and do not represent the opinions, views or policies of Medical Forum or the Publisher. Readers should independently verify information or advice. Publication of an advertisement or clinical column does not imply endorsement by the Publisher or its contributors for the promoted product, service or treatment.
Advertisers are responsible for ensuring that advertisements comply with Commonwealth, State and Territory laws. It is the responsibility of the advertiser to ensure that advertisements comply with the Competition and Consumer Act 2010 (Cth) as amended. All advertisements are accepted for publication on the condition that the advertiser indemnifies the Publisher and its personnel against all actions, suits, claims, loss or damages resulting from anything published on behalf of the advertiser.
EDITORIAL POLICY This publication protects and maintains its editorial independence from all sponsors or advertisers. Medical Forum has no professional involvement with advertisers other than as publisher of promotional material. Medical Forum cannot and does not endorse any products.


20 Close-up: Dr Amira Allahham
Kids’ ‘inside eyes’ putting sight at risk
52 Fangs on the Farm
Wine review: Fermoy Estate
Dr Craig Drummond 55 Guitar duos’ ascendant messages

Our bumper Summer Series of comps for the ballet and movies have been winners with readers. We have extended the chance to win a dozen bottles of Fermoy’s delicious wine so check out what our Master of Wine Dr Craig Drummond has to say on P54.
We are also giving readers a chance for an armchair ride to France with tickets up for grabs to the annual Alliance Francais French Film Festival. The details are on P53. Enter our competitions by using the QR code or go to www.mforum.com.au and hit the competitions tab.
PUBLISHERS
Alice Miles – Director Fonda Grapsas – Director Tony Jones – Director tonyj@mforum.com.au
EDITORIAL TEAM
Managing Editor
Andrea Downey 0437 909 904 andrea@mforum.com.au
Production Editor Jan Hallam 08 9203 5222 jan@mforum.com.au
Clinical Editor
Dr Joe Kosterich 0417 998 697 joe@mforum.com.au
Graphic Design Ryan Minchin ryan@mforum.com.au
ADVERTISING
Advertising Manager
Bryan Pettit 0439 866 336 bryan@mforum.com.au
Classifieds Manager
Paul Riessen 08 9203 5222 paul@mforum.com.au
Clinical Services Directory
Alice Miles 08 9203 5222 alice@mforum.com.au
CONTACT MEDICAL FORUM
Suite 3/8 Howlett Street, North Perth WA 6006
Phone: 08 9203 5222 Fax: 08 6154 6488 Email: info@mforum.com.au www.mforum.com.au
















Carers have called on the next State government to better support the thousands of unpaid carers in WA.
In the lead up to the March State election, Carers WA has launched its Carers Count campaign outlining five key priorities that matter most to unpaid carers.
The charity said there are over 3 million carers in Australia, including more than 320,000 in Western Australia.
The campaign calls for:
• A new WA Carers Strategy to build on the work already undertaken as part of the National Carer Strategy
• Establishment of a Carer Card in WA to ensure carers are included in the ongoing health and medical needs of the person they are caring for
• Annual funding to address the significant impact on employment, income, study and superannuation
• Annual funding to continue Carers WA support for young carers and regional carers
• Establishment of an easy service navigation program to support carers in understanding health and other services.
Chief Executive of Carers WA Richard Newman said caring was a significant form of unpaid work and integral to our aged, disability, health, mental health and palliative care systems.
Cancer research in WA has been given a $3 million boost from the Western Australian Future Health Research and Innovation (FHRI) Fund to support the work of Cancer Council WA.
Cancer Council WA chief executive Ashley Reid said the additional funding would enable the organisation to offer up to $4.34 million annually and address critical gaps that currently exist for WA cancer researchers.
“Together with the $2.52 million awarded to us by the FHRI Fund earlier this year, this new pool of funding will allow us to support the growth of cancer research in WA, including addressing a significant gap in support for mid-career cancer researchers,” he said.
“This new funding will ensure these researchers are supported to stay in research, contribute to life-saving discoveries, and advance cancer care and prevention.”

“Everyone likely knows at least one of, or is one of, the 320,000 people who are in an unpaid carer role in WA,” he said.
“To ensure carers count at the 2025 WA election, Carers WA is asking political candidates, current members of parliament and all major parties how they plan to support carers and what are their election commitments.
“Carers WA urges, not only carers, but the wider community across WA, to share their endorsement of what matters to them, with their local member of parliament, to ensure the needs of carers are prioritised.”
New research opportunities made possible by the funding include:
• A mid-career fellowship awarded annually for the next three years
• A mid-career investigator grant awarded annually for three years
• Clinical capacity-building grants to enable clinicians to incorporate research into their practice
• Undergraduate annual stipends to support Aboriginal students pursuing cancer research.
Mr Reid added the clinical capacitybuilding grants and Aboriginal student stipends would address other critical needs in WA’s cancer research landscape.
“We know the importance of strengthening the bridge between clinical practice and research, and these grants will empower clinicians to take an active role in advancing cancer care,” he said. “At the same time, supporting Aboriginal students to enter the field will help ensure our research reflects and meets the needs of WA’s diverse population.”
An injection that targets specific symptoms could be game-changing for the millions of people living with asthma and COPD – the first new treatment in 50 years.
Research from the UK, supported by researchers in WA, have found a drug already available, Benralizamab, can be repurposed in emergency settings to reduce the need for further treatment or hospitalisation.
Benralizamab is a monoclonal antibody which targets specific white blood cells called eosinophils to reduce lung inflammation. The drug could be used to treat eosinophilic exacerbations which cause symptoms including wheezing, coughing and chest tightness due to high amounts of eosinophils.
These exacerbations make up to 30% of COPD flare-ups and almost 50% of asthma flare-ups, and they
continued on Page 6

The highly anticipated updated Australian Cervical Screening Program Guidelines, which will take effect in April 2025, are now available by Cancer Council Australia and are detailed on the Clinipath Pathology website.
This update is a continued development of the guidelines since the introduction of the renewed cervical screening test
The scope of the revision was determined by previous advice from the Cervical Screening Expert Panel (CEP) which identified areas requiring further review and clarification
The revision also includes cases where new evidence has emerged or existing evidence has changed involving both clinician collect and self-collect results

By Dr Adeline Tan BMedSci (Hons) MBBS (Hons) FRCPA
Adeline is the lead histopathologist and cytopathologist for gynaepathology services at Clinipath Pathology in Perth WA, and holds an honorary Senior Clinical Lectuer position at the University of Western Australia. Additionally, she is on the expert panel for the Royal College of Pathologists of Australasia (RCPA) Structured Reporting for carcinomas of the cervix, the pathology convener and committee member of the Australian Society for Colposcopy and Cervical Pathology (ASCCP) and is a dedicated gynaepathologist in both aspects of clinical practice and academia.
The Guidelines Working Party overseeing these updates followed a rigorous process to incorporate emerging evidence, including expert feedback and practical user insights via public consultation
These guidelines have been endorsed by the Royal Australian College of General Practitioners (RACGP), the Royal Australian and New Zealand College of Obstetricians and Gynaecologists (RANZCOG), the Royal College of Pathologists of Australasia (RCPA), the Australian Society for Colposcopy and Cervical Pathology (ASCCP) and the Australian Society of Gynaecologic Oncologists (ASGO)
With the latest evidence now incorporated, these updated guidelines ensure the cervical screening program remains relevant and effective in achieving Australia’s goal of eliminating cervical cancer by 2035
Primary care-relevant changes
A new chapter consolidates screening content for primary care
Individuals with HPV detected on self-collected samples (not 16/18) who do not return for 9 months can be offered follow-up self-testing
Patients with immune-deficiency have been separated into highly suppressive conditions (3-yearly testing) and moderately increased risk (5-yearly testing) categories
“Test of cure” after completely excised HSIL (CIN 2/3) has changed, recommending annual HPV tests (instead of co-tests) until two consecutive negative tests are obtained
Follow-up after completely excised AIS will be extended to 3yearly testing after five consecutive negative results, with return to normal screening (according to patient’s age) after 25 years post treatment
Post-hysterectomy testing has been simplified to annual testing until two consecutive negative tests
Colposcopy-relevant changes
Colposcopists now have guidelines for managing HPV (16/18) detection without visible lesions, including the possibility of endocervical curettage if appropriate
There is an option to defer re-referral for HPV (16/18) detected with negative LBC if follow-up testing remains HPV-positive
Clarifications have been made regarding the diagnostic excision of the transformation zone
Loop electrosurgical excision procedure (LEEP) is now recommended over cone biopsy due to lower postsurgical complications, although both procedures have similar effectiveness
For further information on the upcoming changes to the screening program, visit our website at clinipathpathology.com.au
Our pathologists are based locally, to support you locally 310 Selby Street North, Osborne Park WA 6017
P (08) 9371 4200 | E info@clinipath net
clinipathpathology com au

continued from Page 4
can become more frequent as the disease progresses, leading to irreversible lung damage in some cases.
However, treatment for this type of asthma has not changed much over 50 years, with steroids still dominating treatment.
Steroids such as prednisolone can reduce inflammation in the lungs but have severe side-effects such as diabetes and osteoporosis. Furthermore, many patients fail treatment and need repeated courses of steroids, rehospitalisation or die within 90 days.
Researchers taking part in the ABRA trial have now found that a single dose of Benralizamab can be more effective when injected at the point of exacerbation compared to steroid tablets.
Respiratory physician and researcher Dr Sanjay Ramakrishnan, and member of Respiratory Care WA’s Clinical Advisory Group, is the first author and worked on the trial during his time at the University of Oxford.
continued on Page 8
Director of the Perron Institute
Professor Steve Wilton has been elected to the Australian Academy of Health and Medical Sciences. Professor Wilton is also Deputy Director of Murdoch University’s Personalised Medicine Centre.
WA has lost one of its pioneers in palliative care, Dr Douglas Bridge.
Dr Bridge died in December at the end of a 17-year journey with Parkinson’s Disease. He was an internationally acclaimed Professor of Palliative Care, and a respected mentor and trusted colleague for many in WA.
Dr Bridge lectured at WA medical schools and delivered sessions at international conferences in Bangladesh, Taiwan, China, and New Zealand, sharing his vision for quality palliative care on a global stage.
He operated in positions of clinical leadership in palliative care departments across WA. In recognition of his contributions, he was awarded the Australian Medical Association (WA)’s Hippocrates Award in 2018 and the Royal Australasian College of Physicians’ College Medal in 2020.

AMAWA President Dr Michael Page paid tribute to Dr Bridge’s profound dedication to education and advocacy.
“His legacy is one of compassion, dedication, and an unwavering commitment to improving the care of patients that continues to influence and inspire future generations of doctors,” he said.
Dr Bridge was also a life member of Palliative Care WA.

Executive Director of The Kids Research Institute
Australia Professor Jonathan Carapetis has been appointed to the Council of the National Health and Medical Research Institute.

Palliative care researcher Professor Samar Aoun was awarded the 2024 Motor Neurone Disease Association of WA President’s Cup. Professor Aoun is the Perron Institute Research Chair in Palliative Care at UWA and has served on the MNDAWA board for 12 years.
Devlyn Australia have been named as the preferred contractor for the $152 million redevelopment of Peel Health Campus.
Dr Moira Clay is the new Deputy Director of the Harry Perkins Institute of Medical Research.

Australian National University Medical School Professor of Obstetrics and Gynaecology Steve Robson is the new Chief Medical Officer of Avant Mutual. Professor Robson succeeds Dr Michael Wright who was recently appointed President of the RACGP.



“COPD is the third leading cause of death worldwide but treatment for the condition is stuck in the 20th century,” he said. “We need to provide these patients with lifesaving options before their time runs out.
“The ABRA trial was only possible with collaboration between the NHS and universities and shows how this close relationship can innovate healthcare and improve people’s lives.”
A Curtin University study has challenged the perception that heavy social media use has a significant impact on mental health, finding little to no relationship between the two.
Not only does the research indicate the amount of time spent on social media has a negligible effect on mental health indicators such as depression, anxiety and stress — the result isn’t always negative, either. Study lead and PhD candidate Chloe Jones said it was important to stress the findings do not suggest social media use is harmless or has no impact on mental health, however the relationship between the two likely has many complex layers.
“For example, a connection to a supportive online community could be a lifeline for people living in isolation, but hours of scrolling Instagram influencers could be really unhelpful if you have body image concerns,” Ms Jones said.
While most previous studies on social media use have relied on selfreported estimates from participants, researchers from the Curtin School of Population Health collected mobile phone data from more than 400 people ranging from 17-53 years old to accurately measure how much time they spent on social media a week.
The team then compared the usage data against the participants’ levels of depression, anxiety, stress and attentional control.
They found social media use was very weakly associated with anxiety and not associated with depression or stress.
It was also found to have a weak positive association with attentional control, suggesting increased social
West Australian doctors have come together to share ideas and strategies to address the challenges of the State’s GP workforce shortages.
More than 60 GPs and key stakeholders came together to share insights and strategies at the WA Primary Health Alliance’s recent GP workforce planning and prioritisation summit.

The summit provided the opportunity for GPs across WA’s regional, rural and remote areas to collaborate, network and share ideas to strengthen the GP registrar workforce in country regions.
Chief executive of the alliance Learne Durrington said with the State facing GP shortages, particularly in remote and regional areas, it was important to get workforce strategies right.
“The State is not producing enough GP trainees to maintain current service levels, let alone meet future demand and we are seeing challenges in recruiting and retaining GPs to rural and remote areas,” she said.
“The GP workforce in WA is ageing, with a changing gender balance and an increasing trend towards part-time work. The shortage of vocationally registered GPs has also had significant implications for WA's GP training capacity.”
Ms Durrington added the summit provided a valuable platform for networking.
“There are great examples of innovative models of supervision and shared pathways being used across the State,” she said.
“These conversations highlighted the importance of collaboration and need for innovative solutions to ensure a robust and sustainable GP workforce now and into the future.”
media use was linked with slightly better performance in maintaining attention.
“If we are going to make wellinformed decisions in this space, it needs to be based on quality data and our research demonstrates when you objectively measure time spent on social media, the effects are tiny or non-existent,” Ms Jones said.
Eleven researchers at The Kids Research Institute Australia have been awarded funding in the Stan Perron Charitable Foundation’s latest round of grants to support healthrelated research.
Among the research supported are novel solutions for autism mental healthcare, a vaccine platform to optimise immunisation practice, improvements to the health and
wellbeing of young trans kids, and investigations into early genetic diagnosis to improve WA children’s life trajectory.
The Kids executive director Professor Jonathan Carapetis said the support of the foundation across three decades has been transformational to child health research.
“From chronic childhood diseases through to precision health, the Stan Perron Charitable Foundation has been there with us in an aligned commitment to see every child live their healthiest and happiest life possible,” Professor Carapetis said.
“The Kids is deeply grateful for the foundation’s continued commitment to support West Australian research and for the trust in our capacity to deliver health outcomes for our kids.”
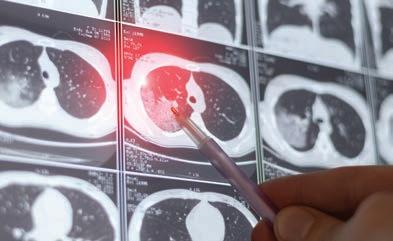
The Photon Counting CT machine at ChestRad requires ten times less radiation dose for lung cancer screening
1 Heismann, B Photon counting CT versus energy-integrating CT: A comparative evaluation Med Physics Dec 2024 Finding - Siemens Naeotom Alpha PCCT ten times more dose efficient for LCS than Siemens Definition Force 2 American Association of Physicists in Medicine Lung Cancer Screening CT Protocols V 6 0 November 2023 Siemens Definition Force four times more dose efficient for LCS than the next best CT machine
Finding -

Cancer experts are trying to change the narrative on the unwanted side effects from prostate cancer treatment.

By Cathy O’Leary
It was once the inevitable collateral damage from prostate cancer treatment – the lifechanging side effects that were considered the price that men had to pay to beat the disease.
Incontinence and erectile dysfunction (ED) have often been the unwanted legacy of radical surgery and radiation treatment, associated with poor rates of recovery.
For some men, their quality of life has suffered so much it has made them question their decision to go ahead with aggressive treatment and left them mentally scarred with severe depression and damaged relationships.
And while medical science has found new solutions that have changed the trajectory of postcancer treatment symptoms, many men – and even doctors – are unaware of what can be done now to restore sexual function in men.
That includes innovative rehabilitative techniques and penile implants, as well as a new technique which has been used in Melbourne to restore erectile function by removing sural nerves from the patient’s leg and grafting them for use in the penis.
“ED is also a common complication of prostate cancer and its treatment, and for some men, it can take up to two years or longer post-treatment to regain sexual function. ”
25-75% of men who undergo prostate cancer surgery.
PCFA is running an awareness campaign to encourage men to seek help before and after their cancer treatment, and to challenge the view that nothing can change the trajectory of ED.

Recent research commissioned by the Prostate Cancer Foundation Australia (PCFA) revealed that erectile dysfunction severely compromises the mental wellbeing of one in three men aged 40 and over.
It affects 10% of West Australian men in that age group at least once a month, and 22% at least once a week.
While there are a range of contributing factors to erectile difficulties, including diabetes, heart and blood vessel disorders, hypertension and high cholesterol, ED is a well-recognised side effect of prostate cancer treatment.
Urological Society of Australia and New Zealand president and Melbourne-based Professor Helen O'Connell is among those backing the campaign, arguing that an underlying medical condition is often the root cause of ED, with symptoms often presenting as the first sign of metabolic diseases, cardiovascular disease, high blood pressure, or high cholesterol, while stress can also be a risk factor.
“ED is also a common complication of prostate cancer and its treatment, and for some men, it can take up to two years or longer post-treatment to regain sexual function,” she said.

It is also difficult to get a full picture of the prevalence of ED in men post-prostate cancer treatment, partly because some men do not report symptoms or seek help, but it is estimated to affect between
According to PCFA’s head of research, Professor Jeff Dunn, one in five men are likely to be diagnosed with prostate cancer in their lifetime.
“Erectile dysfunction is one of the more common potential side-effects of prostate cancer treatment, and helping men and their partners adjust to common, physical sideeffects of treatment, including ED, is crucial because it can significantly affect quality of life,” he said.
“In fact, most men report their quality of life to be severely or moderately affected by ED following prostate cancer treatment.”
Dr David Sofield , a reconstructive urological surgeon at St John of God Subiaco Hospital and founding principal of Perth Reconstructive Urology, said 58% of Australian men who have experienced ED describe the condition as frustrating, while a third claim it is ‘depressing’.
“ED can lead to shame, frustration and compromised mental health, including depression, and it can influence a man’s view of himself as complete or whole,” he said.
“The new research reveals 65% of West Australian men who have experienced ED feel the condition robs them of intimacy with their partner, 39% reported it strains their relationship, while 58% reported it reduces relationship satisfaction with their partner.
“This does not, however, need to be the case, as there are many effective treatment options available to men living with ED, but timely treatment is crucial because the longer the condition continues, the more complicated it can be to treat.”
Dr Sofield told Medical Forum that there has not been major progress over the years in preserving erectile function after prostate cancer treatment – be it radiation or surgery.
Both had very high rates of causing erectile dysfunction, and to a lesser extent incontinence.
on Page 12
continued from Page 11
“The reason we probably haven’t made as much progress as we would want is that the average man having a prostatectomy is aged 65 and, if you assessed them, about 60% would already have some sign of ED, so their capacity for recovery is probably less,” Dr Sofield said.
“If I operated on a 45-year-old guy, most will be fine, but if it’s a 70-year-old guy, only a relatively small number are going to recover their function.”
Dr Sofield said on top of the age-related contributor, in the last 10 years there had been increased obesity, diabetes and heart problems – all of which are increased risk factors for ED.
“That’s also why our results don’t look like we’re improving much, because the background risk factors have increased pretty dramatically,” he said.
“But one of the things which has improved is with men who used to be the ideal surgical candidates to preserve all their erectile nerves –
the people who had small amounts of low-risk cancer – we no longer operate on them, so we preserve function in those guys really well now.
“The people we operate on now – those with more advanced and aggressive disease – aren’t such great candidates for trying to save their erections because their cancer is relatively advanced, so if you try to save those nerves you may well increase the risk of leaving the cancer behind.
“That paradigm has shifted quite a bit – the people who would have done really well surgically in the past, a lot of them now don’t even have surgery, so they do even better.
“The men who have often had pretty radical treatment and might be a bit older, they’re relatively more difficult to treat for their ED.”
However, Dr Sofield said there were now good treatments available to restore sexual health, with multidisciplinary rehab programs for men after surgery, using nonsurgical treatment.

“I refer people to these programs, which see men pre-operatively and plan ahead, and within weeks of surgery they can be on a penile rehab program,” he said.
“And at the end of that process, if conservative options fail, one to two years after surgery, then they might come back and we look at the last option, which is a surgical implant.
“The uptake of those is increasing but is still relatively low because a lot of men and their partners are willing to go so far, but for some of them that’s a step too far and they decide if that’s what it’s going to take, they’ll probably just let it go.
“These men live a long time after treatment, so there’s a long time to live with those quality-of-life impacts, and while I still do prostate cancer surgery, my reconstructive practice is my main area of interest, and the ED and incontinence. It’s important to make men aware of the options.”
While some men were just grateful that they no longer had cancer, for other men that was not enough, and they were not prepared to accept erectile problems as their lot in life.
Perth-based Ken Bezant went down the path of a penile implant, after almost giving up on the prospect of having any semblance of his sexual function restored.
The 70-year-old father, grandfather and business owner was diagnosed with ED following prostate cancer surgery in September 2013 when he was aged 59.
“When I learned I would never regain sexual function, I was shattered. I thought my life was over and was very concerned about my future,” he said.
“The biggest challenge of living with ED was mental. Despite surviving prostate cancer, developing ED following prostate cancer treatment was totally devastating.”
Ken spent three years trialling a plethora of treatment options, each of which offered him only short-term relief.
“I went through a long process following the prostate cancer surgery to regain my sexual function but sadly it didn’t come back to a normal function,” he told Medical Forum
Dr Sofield said some GPs were surprisingly unaware of the options now available.
“Even some urologists can be reticent – I’m not sure if it’s unwillingness or lack of taking these issues all that seriously – but there’s only a minority of other urologists in WA who will refer to our reconstructive service for incontinence or ED, leaving people to fight their way through other avenues,” he said.
“It might be an underappreciation of how those problems impact on men, but the treatment of incontinence is absolutely lifechanging and you can correct it in almost everybody.
letting these guys know that they’re not going to be 18 again,” he said. “It’s a lot better than having nothing, and does give back control and spontaneity, and it’s reliable and predictable, but it is a bit mechanical.
“Having said that, a penile implant for the right man, or the right couple with the right expectation and motivation, is actually a great procedure.”

“The treatments for incontinence have much higher satisfaction rates because the problem is more impactful to begin with, and the procedures we have are simpler and more effective.”
Dr Sofield said penile implants were good but were not the same as natural erectile function and had limitations.
“A lot of my work is managing expectations around that and
A Perth expert in prostate cancer rehabilitation, nurse practitioner and sexologist Melissa Hadley Barrett , was recently an Australian peer reviewer for new international guidelines for sexual health after prostate cancer.
The founder of the Restorative Health Clinic said some men had such bad experiences post-treatment that they almost wished they had never been told their diagnosis.
“What’s happened is that the surgeons and radiologists have got so good at curing prostate cancer but the quality of life after is often very bad,” she said.
“The thing that really worries me is that I don’t want it to deter people
As each treatment attempt failed, Ken’s frustration and desperation began to spiral. In 2016, he visited a urological specialist for further advice.
“Eventually, four years after my prostate cancer surgery, I found an ED treatment option that worked for me and it changed my life completely,” Ken said.

“Erectile dysfunction can be mentally very challenging, it changes your entire life, it changes the way you feel and your relationship with your partner. I’ve been extremely lucky with my prostate cancer journey in that I’ve had a strong, beautiful partner to help me through the process.”
Given his experience of living with prostate cancer and ED, Ken founded the not-for-profit, WA-based association PCaHELP to support men and their families during and after treatment.
“What I was told was ‘wait and see’ and I went through a penile rehab program but most of the things didn’t work well for me, and the urologist had told me it could take up to two years. We eventually got to three, and he said if it’s not working now, it’s never going to, and that was devastating when he said that to me.
“The biggest challenge of living with ED was mental. Despite surviving prostate cancer, developing ED following prostate cancer treatment was totally devastating.”
from getting checked.
“Radiology and surgery are so good now – the research says 3060% will have a full recovery – but research is always at least five years behind, so we’re seeing at least a 70% recovery to their pre-op or pre-radiation function.”
Melissa started out as a remote area nurse and midwife, before becoming a nurse practitioner in a primary care practice with a GP and then deciding to study sexology
continued on Page 14
“I was lucky because at the support group I was running we always had guest speakers talking about this issue, so I thought why not follow up these guys and do a bit more research, which worked out well for me.
“Sadly, we haven’t concentrated enough on the mental aspects of ED.
“What I had was the last resort and it gave me back function, which was absolutely brilliant, but a lot of guys continue to suffer in silence, and that’s the worst thing they can do. We get the same thing with incontinence, I’ve had guys come back 10 years later with severe incontinence and they haven’t done anything about it, and yet they could fix it so easily.
“It’s still part of our mission to make our group known, and GPs have been hard to reach, and a lot of the work we do is with prostate cancer specialist nurses because they have our brochures and will refer people to us.
“I encourage any man experiencing ED to seek help, from your GP, your friends, and talk to anyone who you think can help you through the process because there are many brilliant doctors and treatment options out there.”
continued from Page 13
and specialise in sexual health rehabilitation.
“One couple I helped, the man told me, ‘what’s the point of holding my wife’s hand when it just feels like window-shopping and I can’t follow through’, so sorting it out for them literally saved their marriage,” Melissa said.
“I started my business in 2016 just doing clinics in a couple of urologists’ rooms and before long we ended up with a clinic in every single one of them.
“I also started a podcast called The Penis Project, because men didn’t want to talk about it. One in three men aged over 50 – even if they’ve never had prostate cancer – get erectile dysfunction, but they don’t tell their mates.
“Some couples will say to me after getting help that their sex life is better now than it was before the man’s treatment, and part of that is because as we older we get a little bit slack with our sex life and we don’t pay enough attention to our partners, and then suddenly you get threatened with losing it.
“I feel like so much work has been done in this space to increase people’s longevity, but we really need to worry about their quality of life too, and people think as you get older you don’t want sex anymore.”
Melissa said erectile dysfunction often had a profound effect on men’s mental health and selfesteem.
“The women I see will often say they don’t care if they never have sex again, and they think they’re being nice to their partner, but what the man hears is ‘she’s glad it’s all over and we don’t have to do it anymore’.
“But when you speak to the woman on her own, what she really means is ‘I would rather you be alive, but if we could still have sex, I would prefer that’ but they don’t want to put pressure on the man.
Tailoring antidepressant use based on how people metabolise medicines is the goal of new pilot study in WA aimed at improving mental health outcomes for young adults.
The GENE-YD pilot trial will involve pharmacogenetic testing (PGx), a personalised medicine approach that examines how a person’s genetic makeup affects how they respond to certain medications. This information can help doctors choose the most effective treatment options.
The study, based at WA’s Perron Institute, aims to recruit up to 60 participants aged 16-24 years who live with depression or anxiety and are planning to start antidepressant therapy, or who are prescribed antidepressants and are looking to change medication.
Data collected will enable assessment of the benefits of genetic testing from the perspectives of both patients and doctors. This includes monitoring medication side effects and overall health outcomes compared to conventional treatment outcomes.
Chief investigators are Associate Professor Jennifer Rodger (Perron Institute and UWA), Professor Anthony Akkari (Perron Institute and Murdoch University) and Professor Sean Hood (UWA). Also involved are Curtin University, PathWest, and Drs Svetlana Baltic and Suzannah Lindsey-Temple from WA biotechnology company, Gene S.

The project has been developed based on the qualitative results of the project’s first phase, which involved focus groups with youth and case study discussions among GPs.
“The use of pharmacogenomics in improving youth mental health outcomes offers hope where traditional treatment options often fall short,” Associate Professor Rodger said. “Many young people struggle to find effective mental health treatments, leading to prolonged suffering and decreased quality of life.
“By tailoring treatments to an individual's genetic profile, we hope to show that we can provide young people with personalised care more likely to be effective and less likely to cause adverse effects.”
The findings from this new study will help develop a larger clinical trial, aiming to show how genetic information about metabolism can help create effective, well-tolerated treatment plans for young people prescribed antidepressants for depression and anxiety.
Though not the only contributing factor, four out of five people are believed to carry genetic variations that may alter drug efficacy and safety, with some research estimating genetic factors to account for up to 95% of treatment response.
Funding for the study has come from the WA Government’s Future Health and Innovation Fund and from the philanthropic Sarich family.
“I feel like so much work has been done in this space to increase people’s longevity, but we really need to worry about their quality of life too, and people think as you get older you don’t want sex anymore.”
“It’s a really nuanced area and people need specialist knowledge. Having said that, GPs do an amazing job when their time is so limited.”
Melissa said the newer technique being practised in Melbourne using a sural nerve removed from the patient’s leg to restore erectile function was also showing very good results.
“A lot of guys come in after being referred by their urologist or their GP and they’ll say, ‘I had my prostate cancer taken out three years ago and I was talking to my mate at golf and he suggested I get help but I’m not sure if it’s too late’.
“I tell them it’s never too late, although you will get better results if you do rehab in the first six months after radiation or surgery.
“When I first became a nurse practitioner, there was some resistance from doctors, but now we get a lot of support from urologists and GPs for the rehab service.”
Her clinic recently launched an online men’s health platform in conjunction with LTR Pharma, which provides telehealth consultations and access to drug treatments, including the erectile dysfunction nasal spray Spontan, which can now be prescribed online to eligible patients through the TGA’s early access scheme.
“We’ve got really thorough protocols approved by the urologists, but every person is different, and you need a thorough health assessment because sometimes ED can be telling you that you have heart disease, so it’s a warning sign,” she said.
“Guys need to know there are lots of options, but whatever you decide, you have to do rehab, whether it’s a sural graft or an implant, you have to think about it along the lines that if you were getting a hip replacement you’d go to the gym and get the exercises from the physio, and you have to do the same for the penis.”
ED: For more information about the support group PCaHELP go to www.pcahelp.org
EOSedge is a precise, low dose imaging system that delivers full body images covering the full set of musculoskeletal and orthopaedic exams.
• Imaging complete in 20 seconds
• Full body images in standing position
• 24 hour report turnaround
• True 1:1 scale
Refer your patients now for lower dose imaging and better visualisation for diagnostic or surgical planning and post operative assessment.
• Low dose radiation
• Walk ins welcome
• All request forms accepted
• All scans are bulk billed


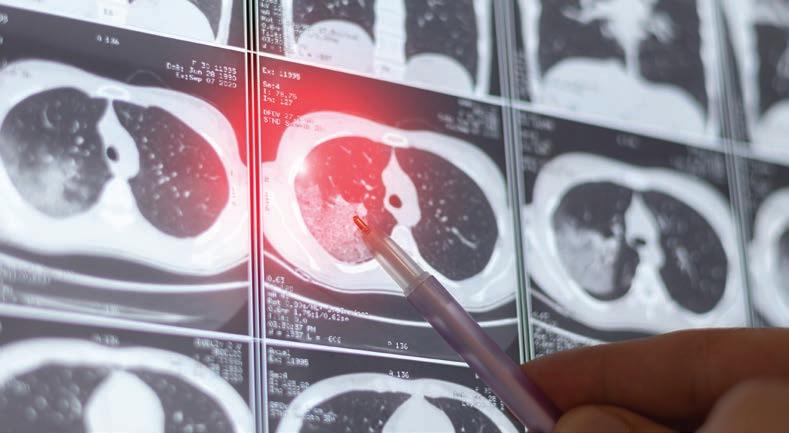
Lung cancer claims thousands of Australian lives every year, but a new targeted screening program could catch deadly cases earlier.
By Andrea Downey
It is Australia’s deadliest cancer with the vast majority of cases diagnosed too late for curative treatment, but a new screening program could turn that around.
The National Lung Cancer Screening Program comes into effect in July 2025, targeting people considered to be at high risk for lung cancer in the hope of detecting cases early, before they become incurable.
Lung cancer is the fifth most commonly diagnosed cancer in Australia, with about 15,100 cases diagnosed in 2024, according to the Australian Institute of Health and Welfare (AIHW). Yet it is the deadliest cancer of those most commonly diagnosed.
Just 26% of people survive past five years. Comparatively, the five-year survival rate of the second most deadly cancer, colorectal cancer, is 71%.
In WA, latest data suggests more than 1000 cases of lung cancer are diagnosed in the State every year, but many more cases could be going undiagnosed, or could be diagnosed at an earlier stage.
Consultant respiratory physician at Sir Charles Gairdner Hospital
Professor Fraser Brims said the screening program offered hope that more people could survive the disease.
“Most cases tend to present at a time where we can’t offer curative therapy because things are too advanced,” he said. “About 70-80% of the time we’re not able to offer either surgery, which is the gold standard, or more recently stereotactic radiotherapy.
could be as high as 60%, according to the Department of Health and Aged Care.
Through earlier diagnosis, it is estimated the proportion of advanced stage cancer will decrease from 53% to 11%.

Professor Brims, who is also Director of Early Years Clinical Skills at Curtin University Medical School, says the potential impact of the screening program is enormous.
“It is not overstating it to say it’s a game-changer, it has a huge potential impact,” he said. “It will take a cancer that has a 25% five-year survival rate and potentially turn that on its head, at least for these high-risk people to start off with.”
Health Organisation, Aboriginal Community Controlled Health Services and lung cancer screening program expert advisory groups –will be delivered to support care on country where appropriate.
Following an initial screening, people who have a low or moderate risk of lung cancer will be screened again in three or 12 months and may be referred to a specialist. High-risk patients will be referred to a specialist and linked with a multidisciplinary team.
WA Primary Health Alliance
Executive General Manager Primary Care Bernadette Kenny said the alliance would work with practices to support implementation of the program.
“GPs will be well placed to identify patients that will benefit from this program, being those at high risk with no symptoms,” she said.
“We know from mature screening programs that you can turn that virtually on its head to get 70% or so of cases at stage one and two.
“That’s the challenge, to really impact hard enough that you’re consistently able to capture lung cancer early and make an attempt at curative therapy.”
The screening program will use low-dose CT scans to look for lung cancer in eligible asymptomatic high-risk people. By screening more people before symptoms occur – usually when the disease is advanced – it is hoped more than 500 lives could be saved a year.
It will operate similarly to other early detection programs such as the national bowel cancer and cervical cancer screening programs.
Early-stage lung cancer can often be treated with surgery, but if the cancer has spread outside the lung, as is often the case in stage 3 and 4 cancer, more intensive treatment options may be needed.
Treatment for advanced lung cancer (stage 4) may only focus on slowing the growth of the cancer and improving quality of life, so there is a marked need to identify cases earlier.
Estimates suggest the proportion of cases identified at stage 1 without a screening program will increase by 16%, but with a screening program that number
Due to the cost of CT scans and the minor risks associated with them, including radiation exposure and false positives, the program will only target those considered to be at a high-risk for cancer.
To be eligible people must be asymptomatic, aged between 50 and 70 and have a history of smoking at least 30 pack-years and are still smoking, or have quit in the past 10 years.
A one pack-year is defined by smoking at least one pack of cigarettes per day for one year, or two packs a day for six months.
Eligible people will be called on to have a scan every two years while they participate in the program or until a lesion is found and needs to be treated.
Those with symptoms suggestive of lung cancer should not be referred to the screening program, instead their symptoms should continue to be investigated, according to Cancer Australia’s guide for lung cancer.
GPs, primary care and Aboriginal health services are expected to play an integral role in referral of eligible and at-risk patients to a radiology provider for a CT scan, which will then be reported into the National Cancer Screening Register.
For those in rural and remote areas, mobile screening services – co-designed with the National Aboriginal Community Controlled
Professor Brims encouraged GPs to be opportunistic if they have a high-risk patient who should be referred for screening. That could mean discussing screening during their next visit, or proactively sending letters to patients.
“The majority of people will be recruited through primary care and all practices will certainly be encouraged to have an organised process,” he said. “If they can search their databases for people within the right ages with a history of smoking and send out letters, that’s definitely to be encouraged.
“With appropriate advertising and communications, we would also hope that patients might see something in their local pharmacy or something on the back of a bus and say ‘Hey that’s me, I might be able to request getting screened’.”
Due to the high-risk nature of the people being screened – smoking causes more damage than just lung cancer – additional findings should be expected.
Professor Brims explained that the likelihood of finding nodules on the lungs was high in people who meet the screening criteria, but the severity of those would vary.
He likens it to melanoma and freckles – someone might be covered in freckles but that does not mean they are all melanomas.

Experience the future of electric mobility with the stunning BMW iX1 xDrive30 Money Magazines Best-Value Luxury Electric Car 2025 Winner.
This next-generation all-electric Sports Activity Vehicle (SAV) combines uncompromising performance, advanced technology, and the signature BMW driving dynamics you expect.
The iX1 features the latest generation of BMW’s iDrive infotainment system, with a large central display. Stay connected with wireless Apple CarPlay® and Android Auto™ integration, and keep your devices charged with wireless charging. Advanced driver assistance systems provide added safety and convenience on every journey
The iX1’s bold, aerodynamic exterior styling makes a striking statement, while the spacious, luxuriously appointed cabin surrounds you in premium materials and thoughtful details. Customize your iX1 with a range of wheel designs, exterior colors, and upholstery options to truly make it your own. Experience the future of electric mobility today. Visit Auto Classic to learn more.
Auto Classic 48 Burswood Road, Burswood WA 6100 Ph (08) 9311 7533. autoclassic.com.au. DL2271

continued from Page 17
This is where shared decision making has a role to play. Professor Brims said it will be a crucial part of the process to ensure patients understand screening and that their history means something is likely to show up.
“Maybe up to half of these people will have a nodule, but only one in 20 of those might be a lung cancer, or even lower perhaps,” he said.
“We know that about 95% of these nodules are not a cancer, so they are a nuisance, but we have to follow them through.
“If you target people who smoked a lot, then of course they’re going have conditions such as emphysema, or coronary artery calcification. These are not incidental findings, they are additional findings.
“It’s likely we’re going to find something on the scan, but if you can present that as a positive about early recognition, that’s good.”
Smoking is the leading cause of preventable disease burden in Australia, it is estimated that between 1960 and 2020, it killed more than 1.2 million people.
While Australia has been a worldleader on smoking cessation, the integration of smoking cessation tactics throughout the entire patient journey in the screening process will still play an important role.
Data from a new AIHW national preventive health monitoring dashboard show the prevalence of daily smoking among Australian adults has dropped from 13.8% in 2017-18 to 10.6% in 2022 – taking the country closer to the national target of 5% by 2030 as outlined in the National Preventive Health Strategy.
After stopping smoking, in 10 years the risk of lung cancer is half of that of someone who has continued to smoke.
But incidents of lung cancer have risen in recent years and are predicted to continue rising, partly due to the ageing population
and partly due to the legacy of smoking, highlighting a clear need for continued cessation efforts.
Cases are rising among women but falling among men. In 2000 there were 84 cases of lung cancer per 100,000 men, dropping to around 61 cases per 100,000 in 2024, according to the AIHW.
In contrast, women have seen an increase from 36 cases per 100,000 in 2000 to an estimated 52 cases per 100,000 in 2024.
The older a person gets the less likely they are to survive lung cancer. Five-year survival rates are around 94% for 20-24-year-olds but drop to just 36% for people aged between 40 and 79, and 9% for people aged 85 and over.
As is always the case in healthcare, prevention is better than a cure.
“Australia has, broadly speaking, led the world in terms of tobacco control and the next big step would be towards a tobacco free generation,” Professor Brims said. “That would be to effectively, over a generation, make cigarettes never available to our children. It would literally be life changing.”
But while tobacco use is the obvious risk factor for lung cancer, it is not a standalone factor. Environmental and genetic factors play a role as well.
Those with a family history of lung cancer are twice as likely to develop the disease and among Aboriginal and Torres Strait Islander people it is the most common cancer diagnosis.
A history of other lung conditions such as emphysema and chronic obstructive pulmonary disorder (COPD) also increases the risk.
“Tobacco exposure and age are the biggest drivers. So even though much of our population stopped smoking 20 or 30 years ago, the cumulative risk given their age continues to rise,” Professor Brims said.
“In terms of other risk factors, WA has a long, checkered history with asbestos, and we know that asbestos is a strong risk factor for lung cancer.
“Although here in WA air quality is pretty good, we also have to mention air pollution as a driver as well, certainly globally we’ve seen that.”
Vaping is also on health practitioners’ radars, but it is still too early to say if the habit is linked to lung cancer.
“The bottom line is, we’re going to have to wait and see,” Professor Brims adds. “There is lab-based data suggesting there are genetic changes going on in the airways of individuals who vape that would be consistent with early cancer changes.
“That strong epidemiological link is, to be frank, going to be another 20 years away, but we can’t wait that long just to see all of our kids get early lung cancers.”
Discovering and learning are the things that make Dr Amira Allahham’s life thrilling. With a number of discoveries already under her belt, the researcher is now looking at how burn injuries can change the brain.

By Ara Jansen
Learning is the biggest joy in Dr Amira Allahham’s life and she hopes that remains true for the rest of her years.
“It is true – learning is my biggest joy,” says Amira. “I don’t find as much joy anywhere else.”
The child of Palestinian refugees who migrated to New Zealand, Amira spent her first three years there before her family moved to Jordan.
She came to Perth in 2011 and began her studies at the University of WA. She has a Bachelor of Science (Hons), a PhD in biomedical science and is currently working in her first year as a post-doctorate researcher.
The 28-year-old is an adjunct research fellow at UWA and is currently undertaking research at the Fiona Wood Foundation, looking at the psychological and psychosocial effects burn injuries have on the brain.
“My grandfather really cared about education and made sure that his family were educated,” says Amira. “This was his ticket to a good life. He got his master’s degree very late in life. He gave that quest for knowledge to my mum. My other grandparents were teachers too.
“When I was in Year 12, I wasn’t sure what to do. I did love the arts and wanted to be a movie director, but my parents worried about that and told me it should be my hobby because as a career it didn’t offer a very stable future.”
A student counsellor at school had read about the field of neuroscience and suggested to Amira’s mum that her daughter might quench her thirst for knowledge this way. She started reading about it and was hooked.
“I’m glad I listened to them. I love discovery and finding new knowledge. I feel like with human biology and anatomy we have discovered so much but the brain is still so much of a mystery.”
Amira’s grandfather passed away in 2004, when she was still a child, but his influence was significant. He had a big library and told stories about how important knowledge was and how important it was to him. Her mum also passed on those stories.
As a Muslim, Amira balances her devotion to her religion with her quest for knowledge. The Quran


mentions the great importance –and indeed compulsory nature – of seeking knowledge in Islam from the cradle to the grave.
“Seeking knowledge is one of the principles – and there are so many things to discover. It says the work of a scholar is higher than the work of a worshipper. For me, the more I seek knowledge, the more I want to know and the more I know, the more I know I don’t know. The more I have, the more I am hungry for.
“The more I discover the more I see things playing in harmony and so much of it is perfect and symmetrical. That’s evidence to me
that it’s part of a bigger picture. That’s how I don’t find contradiction between science and my beliefs.”
Amira’s ongoing fascination and research work is in what kind of changes happen in the brain as a result of a burn injury – not necessarily a catastrophic injury –and why. It is a complex puzzle and just the kind she is keen to solve.
Her research was the first to identify the transcriptomic, metabolomic and lipidomic long-term alterations in the brain following burn injuries.
Additionally, it was the first to establish a link between these longterm physiological brain changes and a potential elevated risk of developing neurodegenerative diseases such as Alzheimer’s and Parkinson’s.
“That aspect of discovery is so exciting. I love that my work allows me to explore and discover things.
“At first, I wasn’t sure what I would do with a neuroscience degree. There were only jobs in research, and I didn’t know enough about it to know if it could be a career.
“I thought if research was my career path, I would be stuck in an office reading research papers all day –and that sounded really boring. I remember crying to my mum that I had made a bad choice.”
The Westin, East Perth | Saturday 7th June 2025
Please book a place for the conference at gpurologymasterclass.com.au or rsvp to events@perthurologyclinic.com.au Limited seats available

Supporting patients with specialised urological cancer treatments
Dr Shane La Bianca
Dr Andrew Tan
Dr Jeff Thavaseelan
Dr Trent Barrett
Dr Matt Brown
Dr Manmeet Saluja
Dr Alarick Picardo
Dr Steve McCombie
Dr Sarah O’Neill
With the largest partnership of Urologists in Western Australia, Perth Urology Clinic can manage all urological conditions, offering a wide range of treatment options. For urgent referrals or queries, use our GP Hotline on 1800 487 656 (Press 9). refer@perthurologyclinic.com.au
Healthlink: puclinic
Hollywood Clinic | Wexford Clinic
continued from Page 21
Luckily, a conversation with a lecturer led her to a project looking at the brain in burn injuries. She looked at mouse models and how their behaviour was impacted by a burn and potentially what long-term effects there might be. She discovered that certain gene expressions changed after a burn, which could ultimately cause changes in a person’s life.
The project revealed a path outside a dusty office and Amira has found a home in neuroscience that ticks all of her boxes.
“It made me incredibly happy to have made a discovery in science, it was a very proud moment. Being at the frontline of discovery is pretty special.
“I also found something with a practical aspect where I have been able to use my hands. Being able to suggest a path, try it out, wondering if it will work and having it work – that’s totally thrilling. Seeing an idea come to life from nothing to a discovery is completely fascinating. I often joke about it as being the addiction.”
Amira is currently studying the long-term effects of a burn injury on the brain, like whether a person’s future mental health and brain chemistry can be radically altered. If it is a negative change, could there be a way to halt or prevent it? Can something be done in the first 48 hours after the injury to help future potential issues?

Not only does Amira want to continue making discoveries, she also wants to share the results and benefits with as many people as possible. An eventual goal of hers is to open a school as a way of passing on a love for knowledge, holistic education and learning.
She also sees it as a way of bringing people together and recognising all aspects of a human alongside creating an ethical life with integrity and an appreciation of all cultures.

Amira is the eldest child with two younger brothers and is close to her family. On Saturdays she teaches Islamic studies to local kids and says it brings her great joy.
When she has down time, she loves playing video games and reads widely. Subjects on her bookshelf include theology, philosophy, religion and history. To extend her understanding of the area, Amira also attained a graduate certificate in education.
She has also begun reading the Bible to compare it to the Quran and is generally interested in the similarities of stories and messages in various holy books.
“They remind me we have more similarities than differences. I think science will lead me to education. Islam encourages us to ask questions. God challenges you to question the Quran and see if you can find errors. I take that literally. I’m always exploring and it’s making me more grounded in religion, and coming back with answers from science helps solidify the essence of who we are as humans.”

It is often thought that too much screen time is damaging children’s eyes, but not spending enough time outdoors could be posing a bigger risk.
By Andrea Downey

Researchers from the Lions Eye Institute in Perth have been looking at the causes of myopia and found the amount of time people spend outdoors correlates to their likelihood of the condition.
While the reason for this is not explicitly known, it is thought to be linked to the amount of bright, natural light the eye is exposed to.
Myopia is caused when the eyeball grows too long from front to back, affecting the eye’s focusing ability. People with myopia can see objects that are near but have difficulty seeing objects in the distance.
Research suggests eyes that are not exposed to much bright, natural light in formative years – so in younger children and teenagers – tended to grow too long.

Professor David Mackey and his colleague Dr Samantha Lee from the Lions Eye Institute have conducted studies on myopia, as well as comparing other research, to better understand why cases are increasing.
Professor Mackey warned that we were in the midst of a global myopia epidemic, with environmental factors such as more time spent indoors partly to blame.
effect. So, we think that doing near work and reading books are doing the damage, exacerbated by children and adults spending less time outdoors in daylight and more time indoors for work or education.
“Our recommendation to Australian families is simple: increase the amount of time your kids spend outside, aiming for two hours a day, but follow SunSmart guidelines.”
While parents have an important role to play in making sure kids spend enough time outside, so too do GPs, optometrists and ophthalmologists.
Often the family GP might be the first to notice a child is having issues with their vision as they are the first point of contact for routine check-ups or any health concerns parents might have, says Professor Mackey.

“In many cities in China, more than 90% of university students are living with myopia. Currently about six million Australians – or more than 20% of us – have myopia and we’re heading for 50% by 2050,” he said.
In one recent study, Professor Mackey and Dr Lee looked at the impact of screen time and when myopia develops. What was interesting was that looking at TV screens was not found to be having an impact, but reading books was.
“We found that about 14% of young adults developed myopia between the ages of 20 and 28 years. We also found that looking at small screens didn’t seem to have an effect, neither did watching TV,” Prof Mackey said.
“However, near work on larger computer screens did have an
“The risk factors to look for if a child is becoming short-sighted are if their parents are both myopic, that puts your risk up a fair bit,” he said. “Or children who are struggling with school or any other educational problem, it is worthwhile having an eye check because occasionally we pick up problems in younger children.
“It’s usually when a child is complaining they can’t see the blackboard. You can sit them a bit closer, but then if they are still struggling then you go and get an eye check.”
Dr Lee adds that GPs should ask parents about their child’s vision during routine check-ups and refer to an optometrist if any concerns are raised.
“A lot of people only realise they have myopia when they go for their driver’s license because when you’re a kid and everything is blurry you just think that’s how the world is,” she said.
“It’s something parents could be more aware of – asking their child if they can see street signs that are far away, and if they can’t, maybe it’s time to get their eyes checked.”
Professor Mackey and Dr Lee have identified a simple test that can
guide which children should be treated for myopia early.
Similar to height and weight measurements taken during childhood, they suggest routinely measuring children’s axial length – the length of each eye, from the front of the cornea to the back of the eye.
“We need to identify children with severe myopia earlier in life so we can intervene and avoid a lifetime of challenging eye disease leading to blindness,” Professor Mackey said.
“Some children will just have longer eyes, but if the axial length increases faster over time, that’s a good predictor of future myopia.
“Preschool and primary school children at greatest risk will need interventions, which include increased time outdoors, lowconcentration atropine drops, peripheral defocus lenses and possibly other treatments being investigated.”
They suggest all ophthalmologists and optometrists working with kids should use the test and hope that in the future it will be globally adopted as a routine preschool screening test.
In Western Australia, there is currently no routine screening test for myopia or other visual impairments, but the picture varies across Australia. In New South Wales, for example, they have the StEPS program which offers all four-year-old children free vision screening before they start school.
Dr Lee said a national approach to eyesight screening, such as the StEPS program, would help to identify cases of myopia earlier, but in the absence of a screening program, the onus falls to GPs and other health professionals to check a child’s vision and refer if issues arise.
Cases of myopia are increasing worldwide. The World Health Organization predicts myopia will affect 52% of the world’s population by 2025.
While genetic factors are at play, studies have shown the near work we do – like studying and working on a computer – are also a risk factor because they hinder time spent outdoors.
Providing PET/CT, MRI, CT and interventional radiology expertise for oncology patients.
Our expert oncology team is involved in private and public multidisciplinary meetings across all facets of oncology imaging. We also provide imaging support for clinical trials in Oncology /Haematology at our Murdoch Square clinic.

PET/CT now available at convenient locations, with PRC Murdoch Square now open.




continued from Page 25
Studies have found cases to be higher in countries including China, Japan, Korea and Singapore, where intensive education is often undertaken from a young age, but increasingly places like Australia and Europe are seeing more cases.
“People have been blaming screens for myopia since televisions came around and then it was computers, then laptops and more recently smartphones and personal electronic devices,” Professor Mackey said.
“However, the myopia epidemic in Asia happened back in the 1980s before most of these devices came about and it was actually the near work they were doing, so reading books and holding things close.”
He said the amount of time kids spent inside during their school years, alongside the intensity with which they study, both impacted the eye’s development.
“All of it interacts with the amount of time spent outdoors,” he said.
But he adds it is not to say that children need to study less or stay away from screens, it just needs to be countered with time outside like reading a book on the veranda or walking to school.
One study compared the prevalence of myopia among children aged six and seven of Chinese ethnicity in Sydney and Singapore.
Children living in Sydney had a significantly lower prevalence (3.3%) of myopia compared with those in Singapore (29.1%). The children in Sydney read more books per week and did more total nearwork activity but spent about 10 hours more outside each week than children in Singapore.
Researchers concluded that the lower prevalence of myopia in Sydney was associated with increased hours of outdoor activities.
Slip, slop, slap
Using the Busselton Healthy Ageing Study, Professor Mackey and Dr Lee’s research has also shown those who have had skin cancer are half as likely to have myopia.

They are now looking at the practicality of spending more time outside in a country where skin cancer is also a major risk.
“We already know that spending time outdoors does slow down the onset of myopia, but what we want to do with this research is see how feasible it is in Australia where we have the problem of melanoma and skin cancer,” Dr Lee said.
“What we are encouraging people to do is spend time outdoors in the early mornings before 10am and later in the afternoon after 4pm when the UV index is below three.
“That way they get the benefit of the bright outdoor sunlight without the strong UV levels.”
Even when the UV is at its lowest, it is still important to take sun precautions like suncream, a hat and sunglasses.
Dr Lee adds that getting outside is the cheapest thing parents can do to help prevent myopia. Once myopia has begun, it cannot be reversed and if left unchecked can require expensive treatments.
For some this may mean the inconvenience of glasses, but in more severe cases it could mean special lenses, corrective contacts that are worn at night, or atropine
eyedrops. Risks also may include retinal detachment, glaucoma, myopic maculopathy and even vision loss.
According to Global Burden of Disease uncorrected distance refractive error, which occurs when the eye is misshapen such as in cases of myopia, is the third largest cause of blindness.
Prof Mackey’s message is clear: health professionals and parents need to be aware that cases of myopia are increasing and if left unchecked will cause lasting damage.
“What they are seeing now in China where there are so many young people with myopia, there is a huge rise in vision loss from myopic maculopathy,” he said.
“It’s not just a cosmetic inconvenience issue, it is that the rates of irreversible blindness will go up if we don’t control the myopia epidemic.”

Voluntary Assisted Dying has been legal in WA since 2021. But in light of reviews of the practice, how successful has it been – and is there room for improvement?
By Suzanne Harrison
True to form, Gabrielle, an 84-year-old former social worker, had the last laugh when she chose to end her life with VAD.
“You’re blocking the view”, she said to a nephew, as a large group of loved ones stood with arms linked around her bed. Gabrielle wanted one last look at the beautiful trees outside her French doors – and her friends and family were standing in the way.
“Everyone in the house roared with laughter, including the doctor,” says her son, Brendan, one of four children Gabrielle brought up largely on her own.
Brendan says he is comforted that one of the last things his mother heard is the sound of laughter, in her own home, surrounded by those most important to her.
“On her final day, she was at peace and happy,” says Brendan. “I felt we had no right to question her decision. If that’s what she wanted, she had the right to access it.”
After a transient ischaemic attack in her 70s, the active, headstrong Gabrielle noticed things were not right, particularly with coordination, which was unusual for the avid table tennis player.
Over time, her symptoms were diagnosed as the degenerative effects of motor neurone disease (MND), among a 'grab-bag' of other health issues.
She had lost the power of speech and one day knew that choking on her food was inevitable, Brendan explains.
Gabrielle’s own father had suffered a stroke and spent five years in a vegetative state, something Brendan says his mother – in one of her last written notes – said “I’m not going there”.
Gabrielle is one of hundreds of people who have chosen to die by VAD in Western Australia since the Voluntary Assisted Dying Act 2019 came into law in 2021.
As of June 2024, all States and the Australian Capital Territory have passed legislation creating an assisted suicide and euthanasia scheme for eligible individuals.
According to the only national voluntary assisted dying charity, Go Gentle, 190 West Australians ended their life through VAD within the first year of the law coming into
effect, a greater-than-expected number.
The numbers have continued to grow, with recent figures from the WA Department of Health showing 738 patients have died following administration of a VAD substance since July 2021. The vast majority were cancer-related and in palliative care, with an age range from 32 to 100.
As it stands now, an adult must meet the following criteria to be eligible for VAD:
• Make three separate requests
• Be assessed by two doctors
• Have a medical condition that is expected to cause death within 6-12 months
• Undergoing suffering that cannot be relieved in a tolerable manner
• Have the mental capacity to make the decision
• Be an Australian citizen or permanent resident who has been a resident in Western Australia for at least 12 months.
A person can withdraw their request for VAD at any time, even after they have had an assessment or made a request in writing, and as per the current ‘no carriage laws’, Go Gentle says people must raise the topic of VAD with their GP themselves.
While the Act itself does not require amendment, the review suggests that improving policy and operational processes, as well as education, training and information materials, will increase both compliance with the Act and levels of access and support for eligible people and VAD-assisted dying providers.
“Processes provided under the Act are generally operating well in supporting all those involved in providing and accessing voluntary assisted dying,” the department said in a statement.
“The panel has, however, made 10 recommendations centred on increasing compliance with the Act and improving access and support for eligible people and voluntary assisted dying providers.”
These include the development of a targeted strategy to improve community and health practitioners’ knowledge of assisted dying.

Yet the number of practitioners who have completed the WAapproved training has grown at a more conservative rate.
The WA Voluntary Assisted Dying Board confirmed a total of 114 medical and nurse practitioners have completed the WA approved training – 103 medical practitioners and 11 nurse practitioners – since the Act came into play.
The figure stands at just over double the number of practitioners who had completed the WA approved training in March 2022, seven months after right-to-die laws came into effect.
In 2023-24, 13 medical practitioners and four nurse practitioners completed the training.
Late last year the WA Department of Health released a statutory review of the Act, finding that awareness of VAD was “not consistently high across the State”.
Dr Linda Swan, chief executive of Go Gentle, says that while there has been sufficient time to show that there is demand, positive family and patient interactions, and a satisfactory legal framework, the processes and medical involvement in VAD are a work in progress.
What can be done better?
“There are obstacles,” says Dr Swan. “Despite the laws in all states and the ACT, there is still a need to update and improve.
“We do have a focus on trying to highlight where there are unintentional regulations – the most concerning one is the gag laws.”
By this, Dr Swan means that doctors are not permitted to raise the concept of VAD to potential patients, it can only be discussed if the patient asks them first.
However, this rule does not exist in WA. As it stands at the time of print, this is only enforced in Victoria and South Australia.
“The second one – and this affects WA – is a federal law prohibiting the use of a carriage service [telephone, email, videoconference]
Icon Cancer Centre provides state-of-the-art cancer care across more than 40 centres nationwide, including dedicated locations in Midland and Rockingham.
Advanced radiation oncology technology
• Stereotactic radiation therapy, including HyperArc® for brain cancer
• Tattoo-less radiation therapy
• Deep Inspiration Breath Hold (DIBH) for breast cancer
• Brachytherapy
Integrated day oncology & haematology
Our specialist team
Radiation Oncologists






Dr Eve Tiong – State Lead Radiation Oncology
Breast, prostate, lung, gastrointestinal, skin cancers, palliative radiation therapy and brachytherapy
Dr Nicholas Bucknell
Colorectal, gastrointestinal, lung, skin, spine (CNS) cancers and stereotactic radiation therapy
Dr Rainer Fröhling
Breast, gastrointestinal, lung, prostate and skin cancers
Dr Stephen Kennedy
Lung, brain and spine (CNS), genitourinary, skin cancers and lymphoma
Dr Saad Maqsood
Breast, prostate, skin, lung and gastrointestinal cancers
Dr Mandy Taylor
Breast, brain cancers and sarcoma

Specialist nursing support
• Prostate and bowel care nurses
• Nurse practitioner (palliative and supportive care)
Comprehensive allied health services
• Exercise physiology
• Dietetics
• Psychology
No wait list access
Medical Oncologists






A/Prof Sayed Ali Colorectal, lung, prostate cancers and melanoma
A/Prof Tim Clay
Breast, lung and prostate cancers
Dr Siao Hoon
Breast, lung, prostate and gastrointestinal cancers
Dr Yasir Khan
Thoracic, breast, gastrointestinal, genitourinary cancers and melanoma
Dr Sanjana Kondola
Gastrointestinal, urological, breast cancers and palliative care
Dr Raj Tota
Colorectal, genitourinary, gastrointestinal, lung, urological cancers and melanoma
Clinical Haematologists


Dr Sung Kai Chiu
Myelodysplasia, myeloproliferative neoplasms, lymphoma, multiple myeloma, haemostasis and thrombosis
Dr Colleen May
Leukaemia, lymphoma, multiple myeloma, myeloproliferative neoplasms and stem cell transplantation
Referrals
Specialists and GPs can refer patients via IconDoctorApp.com or Healthlink: Midland: iconmidl | Rockingham: iconrock

continued from Page 29
to discuss, counsel, promote or instruct on VAD. This is crazy and outdated, especially for those living in regional areas,” Dr Swan said.
But the most common concern from those working in VAD is the general lack of awareness, both from inside and outside the medical community.
“When we get down to what could be done better, there’s a lack of awareness among clinicians, among the general public, that this is a viable end of life option.” She added that there had been cases where there was “what I would describe as institutional obstruction by clinicians”.
“If you have a personal objection, that’s fine, but it’s not fine to deny that person access by dismissing it or not referring them to someone who can help them,” she said. “It’s not about the practitioner it’s about the person (patient).”
People like Dr Swan are well versed in the positives of voluntary assisted dying. Families have told her that watching a loved one choose that option is “a bizarre thing, but beautiful”. Among some of the Go Gentle testimonies are “we left nothing unsaid” and “he wanted his suffering to end”.
For VAD practitioner Dr Bhawani O’Brien, easing the suffering of those with terminal illness is something she sees as a privilege.
“When a patient’s life is so limited and their suffering is undeniable and all that palliative care can do is ease that suffering, they say to me: ‘I don’t want to be gaga in my last five days’.”
The Mt Lawley GP says the recent review was well thought out, but “there’s always room for improvement”. And she believes that a couple of those improvements could be enacted sooner rather than later.
“I hope people in the medical community and the Voluntary Assisted Dying Board pay notice to the recommendations. Every patient I go to, the family says, ‘I didn’t know this existed’.”
Dr Bhawani is keen to raise awareness and generate discussion

on VAD, recalling that the last time she visited a medical school to talk on the subject she had tremendous interest from junior doctors.
“We’re not doing enough publicly and that’s a big priority,” she said. “I’ve had patients nearly miss out on a VAD option, yet they’d spoken to their oncologist eight or nine times.
“Patients get delays. They ask their specialist, and their first request has been ignored. There are many conscientious objectors in the medical community, but they still have an obligation to refer these people.”
In its 2023-24 annual report, the WA Voluntary Assisted Dying Board stated it was “disappointed by feedback received this year that requests for voluntary assisted dying have been brushed aside or ignored when made to a medical practitioner in a consultation”.
“We are aware that some people have experienced a delay in access, and some have been prevented from accessing their lawful choice for voluntary assisted dying under the Act as a result.
“Improving the information about voluntary assisted dying available to the community and to health professionals is an ongoing focus of the Board. Practical steps are being pursued to achieve this goal.”
Dr Bhawani was the practitioner at Gabrielle’s death, and Brendan describes her as a “rock star”.
“Bu (as she is known) is the authority on this,” says Brendan. “The process was thorough. She
said: ‘this is how it will go’. And the process does get repeated throughout.”
Brendan says that once Gabrielle made the decision and got sign off, she had health tests every three months. At the last one, she was told her deterioration meant she had less than 12 months left.
“There was a huge grin and a double thumbs up,” he says. “So, you couldn’t question that.”
Brendan now realises that in the final months of his mother’s life living with the illness, she was mostly “cantankerous”, but as soon as she was granted access to VAD, her mood changed.
“She was happy,” he says. “And on the day, we got to give her a hug, and most people don’t get that.”
Dr Swan said this has also been her experience.
“The interesting thing is, when we hear from people who are dying and are potentially facing death, they get enormous relief from knowing voluntary assisted dying is approved,” she says.
At present, a person’s mental capacity to choose assisted dying is at the heart of this law, meaning dementia patients without viable decision-making abilities and no other illness are not eligible.
Dr Swan says there may be a possible pathway to this changing, “but it would take years and a lot more research to be done”.
Currently, the most common diseases that have resulted in people seeking assisted dying are cancers, motor neurone, and heart disease.
“It’s here and it’s working well. It’s rewarding for those involved and there is support for those who want to get involved,” Dr Swan adds.
How often should women check their breasts? What is the correct technique? These are the common questions asked of doctors, says breast surgeon Associate Professor Sanjay Warrier
Research and statistics clearly show that the health outcomes of women diagnosed with breast cancer are better if the disease is detected earlier before symptoms even appear.
This is a key factor to encourage women to undertake regular scans and self-examinations at home.
For women who are menstruating, I suggest undertaking an exam about a week to 10 days after each menstrual cycle starts, as this is when the breasts are least tender and lumpy.
For women no longer menstruating, the key is routine. Pick a day such
as the first day of each month and remind yourself to do it.
Regardless of life stage, it is important for women to know their breasts. Check in the mirror to note their shape and colour and undertake a self-examination in the same way each month to become familiar with them and be better placed to detect any changes in the breast or on the skin and nipples. Common reasons for colour change include general ageing and/or pregnancy. However, one of the more overlooked reasons for changes in nipple colour is associated with the presence of breast cancer. It's especially abnormal if it's occurring

in only one nipple and not evenly on both breasts.
Any changes should be checked by a health professional as soon as possible.
A woman's risk of developing breast cancer increases with age. Over 75% of breast cancers fall into the 50 to 74 years age group. Regular breast screens are the best way to find cancer early.
Women aged 40 and over and who do not have any breast symptoms are entitled to a free mammogram every two years through BreastScreen.
BreastScreen Australia is the
Our purpose is to design cancer care experiences

In WA, we have 8 metro and regional centres dedicated to offering fast access to care, delivered utilising evidence-based treatment techniques.
*GenesisCare data held on file Scan here to learn more or visit: genesiscare.com
national breast screening program and actively invites women aged 50-74 to have a free two-yearly mammogram. Women aged 40-49 and those aged over 74 are also eligible to receive a free mammogram but do not receive an invitation.
Some risk factors may increase the need for annual screening and additional forms of screening. Some risk factors can’t be changed, and these include:
• a family history of breast or ovarian cancer
• inherited genetic factors
• medical history, such as previous radiation therapy for another type of cancer
• reproductive history, such as starting menstruation very young, reaching menopause late, or not having a baby
• getting older; and
• having dense breasts.
Other considerations
Hormonal changes during menopause can affect breast tissue, so it is important that women continue regular checks and
discuss any changes with health professionals.
Regardless of age, if they notice any unusual changes during their self-exam, such as lumps, thickening, discharge or changes in skin texture, they need to contact their healthcare provider promptly.
A healthy diet undoubtedly improves wellbeing and combined with regular exercise, women will not only feel better but lower their risk of breast cancer as an increase in body fat can also mean that their body is storing extra oestrogen, which can stimulate tumour growth. If breast cancer runs in the family, the risk of developing breast cancer may be higher. However, this research is dependent on so-called ‘breast cancer genes’ (BRCA1 or BRCA2).
Most breast cancer diagnoses have no known family history of the disease. Even if their family does not have a history of breast cancer, it is important they flag with their GP any other cancers that have affected the family, including prostate cancer, pancreatic cancer, colon cancer, ovarian cancer or
melanoma. This counts for both sides of their family.
It is globally accepted that smoking causes lung cancer, but it also increases the risk of developing other cancers as well. Studies have shown that people who have smoked for 10 years or more were at least 16% more likely to develop breast cancer than non-smokers.
Women should also be encouraged to exercise regularly. Just 30 minutes of exercise five days a week can dramatically cut their breast cancer risk. Regular exercise not only helps to keep weight in check but can also lower oestrogen levels and boost the immune system, which helps to prevent abnormal cells from growing and spreading in the body.
ED: Associate Professor Warrier is a Sydney breast health and breast cancer surgeon. He is a past president and current committee member of Breast Surgeons of Australia and New Zealand. His views are his own, not BreastSurgANZ.

You and a partner are invited to afternoon tea and discussion organised by Dr Carolyn Graham and Dr David Blacker

When Sunday 23rd February at 2:30pm Venue 6 Strathcona St, West Perth
RSVP Carolyn Graham 0476 760 698
With Avant Practice Insurance, you’re covered for the actions of staff and claims made against the practice. And for eligible practices, we include complimentary Cyber Insurance to protect your practice against cyber extortion, privacy liabilities and damage to digital assets.


More
than 70,000 West Australians have COPD, but half are unaware they have it, writes respiratory physician Dr Sanjay Ramakrishnan.
Chronic obstructive pulmonary disease is the number one cause of preventable hospitalisations in WA and a change is needed not only in how we approach education, but in how we activate, mobilise and direct the community towards lung function testing for correct diagnosis.
COPD affects about one in four West Australians over the age of 65. It is estimated that about half of people living with COPD are unaware they have the disease, and in my experience many sufferers only seek help once their daily lives are significantly impacted, which can be during later stages of the condition.
A lack of general awareness and knowledge, coupled with an acceptance of reduced baseline health, can mean critical delays in diagnoses and treatment.
An estimated $831.6 million was spent on treatment and management of COPD in 2020-21, which represents 0.6% of overall health system expenditure. Disease burden is greatest in remote and regional populations and in lower socioeconomic areas, potentially adding to barriers to accessing treatment.
Indigenous Australians are 5.4 times more likely to be affected, highlighting a critical need for targeted population-based interventions. Whether mild, moderate or severe, a COPD diagnosis diminishes quality of life, most acutely when paired with comorbidities.
Following the release of Australia's first COPD Clinical Care Standards, the 22nd World COPD Day launched a call to action for the general community, ‘Know Your Lung Function’.
With the welcome establishment of the standards comes a set of 10 simple goals that any service helping people with COPD needs


to meet. Are they tested and diagnosed? Is their treatment enough? Are they being seen quickly enough?
These standards also speak to the importance of lung function testing, a set of gold standard diagnostic tools and markers that can help identify COPD often before quality of life is significantly impacted. It allows people to kick-start proactive management, preventing further deterioration.
These tests involve traditional spirometry, but may also include gas exchange, lung volume tests, exercise tests and others.
While many patients view a COPD diagnosis as a slow but terminal progression, it is critical that we impart the message that severe and frequent exacerbations are not inevitable and that research and new trials into the use of drugs like monoclonal antibodies continue, with constant improvements to the way we are treating the disease.
It is positive to see LFTs offered as a fully bulk billed service by Respiratory Care WA, where I am a member of the Clinical Advisory Group.
This is a crucial step in helping to break down barriers to early diagnosis.
My research has included focus on understanding and mitigating COPD flare-ups as well as ensuring existing management methods are being adequately utilised. Collaborating with global experts, at the University of Oxford, King’s College London and University of Sherbrooke, Canada, I have seen how proactive care can help people regain control over their lives.
Early symptoms of COPD are often put down to ageing or a sedentary lifestyle, and sufferers are found to dismiss breathlessness or fatigue as “just part of getting older”.
This misconception, among other reasons, can stop them from seeking help until the disease has significantly progressed. But here is where we must reassure our patients; understanding what is happening in their lungs is the first step toward breathing easier—both literally and figuratively.
ED: Dr Sanjay Ramakrishnan is a clinical advisor at Respiratory Care WA.

More needs to be done to help the forgotten people living with younger-onset dementia, according to occupational therapist Naomi Moylan.
When most people think of dementia, they imagine elderly individuals in their seventies or eighties. Yet an increasing number of people in their 50s – and sometimes even younger – are living with younger-onset dementia (YOD).
While this may reflect a rise in cases, it’s also likely due to greater awareness and improved diagnostic tools. Estimates suggest that over 28,650 Australians currently live with younger onset dementia, a number projected to grow to more than 42,400 by 2058.
Dementia in younger adults often goes unrecognised due to the broad spectrum of symptoms it presents. Unlike traditional forms
of dementia, which typically exhibit as memory loss, younger-onset dementia can manifest in a range of ways: changes in personality, difficulties with problem-solving or struggles in performing familiar tasks.
For individuals in their 50s, these symptoms are sometimes mistaken for stress, depression, or even midlife crisis. Such misattributions often delay diagnosis until the disease has progressed significantly, leaving the person living with younger-onset dementia and their family with fewer options for effective intervention.
This is why routine cognitive assessments should be a priority whenever behavioural changes
arise in patients over 50, allowing for earlier support and a better quality of life.
Occupational Therapy (OT) can have a transformative impact on the lives of people living with dementia. However, as OTs working with younger-onset dementia clients, we often see patients only after significant deterioration. By the time they receive a diagnosis and seek OT support, many have had to leave their jobs, their personal relationships are strained, and their daily lives are markedly disrupted.
Despite these challenges, OT interventions can bring meaningful improvements to quality of life,


helping people adapt to their environment and routines that support independence and safety. Recognition of younger-onset dementia as a distinct medical and social issue is gaining traction. Supported independent living homes are specifically designed for people living with younger-onset dementia.
These forms of accommodation address the unique needs of younger adults with dementia, which differ significantly from those of older residents in traditional aged care facilities. Key features include a garden space to encourage engagement with the outdoors, as people living with younger-onset dementia can be more mobile and require large spaces to walk around.
Dementia enabling design features help to create a home for five people where they are enabled to engage in everyday activities such as cooking, doing laundry and engaging in meaningful activities.
At Perth’s currently only supported independent living home run by the Brightwater Care Group, the home
coordinator is an OT and there is a multidisciplinary YOD allied health team so people can access therapeutic interventions designed to preserve and support functional abilities.
While these developments are a step forward, as a nation, we have a long way to go. A recent study from Dementia Australia revealed that more than half of the population believes there is inadequate support for the 421,000 people living with dementia.
The field still struggles with many unknowns surrounding the causes, progression, and treatment of this devastating condition, which complicates the development of comprehensive care plans.
While there is no cure, OT remains one of the most effective interventions for maintaining quality of life, fostering independence, and adapting to the challenges of dementia.
With no one-size-fits-all solution, OT provides individualised strategies that allow people living with YOD to continue engaging with their communities, stay

Saturday, March 29th 9am-5pm The University Club of Western




connected with family and friends, and retain a sense of purpose and dignity.
Early diagnosis and support, combined with targeted interventions could provide a significant improvement in the quality of life for people with younger-onset dementia and help alleviate the toll on their families and loved ones.
By embracing cognitive screening and increased awareness, we can better serve this often overlooked cohort. Ensuring that people with younger-onset dementia receive timely support is critical to their wellbeing and underscores our commitment to compassionate, holistic care.
ED: Naomi Moylan is an OT specialised in working with people with YOD and is project coordinator with Brightwater in Perth.


Advert removed in compliance with Medicines Australia's Code of Conduct and the Therapeutic Goods Administration's Therapeutic Goods Act.
https://medicinesaustralia.com.au/code-of-conduct/about-the-code/ https://www.tga.gov.au/legislation-legislative-instruments

Medical practice prides itself on being evidence based. Yet as practising doctors we are obligated by time constraints to assume that the basis of the evidence is sound.
This
Mark Twain quote may be more apt than ever –
“It ain't what you don't know that gets you into trouble. It's what you know for sure that just ain't so”. I have been reflecting on this after discovering something I, and I suspect most doctors, was unaware of.
The ‘father’ of modern international scientific, technical and medical (STM) publishing was the late media tycoon Robert Maxwell long before he became (in)famous for a variety of reasons.
Before to WWII, most STM books and journals were produced by learned societies for their members. After the war, publishers saw commercial opportunities and in 1951 Maxwell bought Pergamon which in 1991 was sold to Elsevier.
As Maxwell’s empire grew, Permagon remained the jewel in the crown. Over 40 years it published 7000 monographs and launched 700 journals. Maxwell liked to name them beginning with “International Journal of…”. Medical journals were and remain to this day a highly profitable business. This is largely driven by demand for reprints of papers published.
Does Maxwell’s involvement matter? I don’t know. Obviously, publishing must be profitable because if not, the publication ceases to exist. However the increasing number of medical journals necessarily needs an increasing number of papers. Could quantity reign over quality? Could papers be more likely to be published if reprint demand is higher?
Medical practice prides itself on being evidence based. Yet as practising doctors we are obligated by time constraints to assume that the basis of the evidence is sound. It likely is. But there are increasing murmurings that papers on certain topics face censorship not because of any scientific reason but because of politics.
One step before this is getting funding for research. This also has become increasingly political. We don’t know what we don’t know or what we are not allowed to research.
Perhaps this reached its zenith when Scientific American’s editor was forced to resign after calling Trump voters (the 77+ million, not Trump himself) the “meanest, dumbest most bigoted group”. She is absolutely entitled to her opinion, but had to clarify that it didn’t reflect the position of Scientific American. Would a Trump voter have any confidence in being published in that magazine?
We advance through medicine largely by bowing to those above us and not asking difficult questions. We need to be more questioning. What if what we know for sure, ain’t so?
By Dr Steve McCombie, Urologist, Murdoch
Haematuria is a highly concerning symptom for urological malignancy, with 26% of patients with visible haematuria and 6% of patients with non-visible haematuria having cancer identified – most being bladder cancers.
The absence of risk factors for bladder cancer should not deter or delay full and prompt investigation – 8% of under 45-year-olds, 18% of non-smokers, and 20% of females with visible haematuria have an underlying malignancy. Women, unfortunately, suffer worse outcomes from bladder cancer once diagnosed, partly due to under-investigation and delayed referral.
Investigations for haematuria should include an MSU, upper tract imaging (CTIVU or renal ultrasound) and cystoscopy (most sensitive investigation for bladder cancer). Once identified, transurethral resection of the bladder tumour informs the urologist of the grade and T-stage of the cancer. Over 90% of bladder cancers are urothelial cancers (transitional cell carcinomas), however, rarer variant pathologies do occur.
Patients with non-muscle-invasive bladder cancer (NMIBC) require close cystoscopic surveillance after initial resection because bladder cancer has a high risk of recurrence (return of non-muscleinvasive disease) and progression (subsequent increase in grade or stage).
Patients with higher risk disease may also undergo intravesical drug instillations to reduce these risks, with either chemotherapeutic agents or Bacillus CalmetteGuérin (BCG). BCG consists of live attenuated mycobacterium bovis, which stimulates an antigenmediated immune response that is very effective in destroying bladder cancer cells.


Treatment protocols vary, but one published example is the ‘Fremantle protocol’ that consists of an induction phase (weekly instillations for six weeks) followed by a maintenance phase (monthly instillations for 10 months).
Advances in the management of NMIBC that have been incorporated into current clinical practice in Western Australia to varying degrees include improved modalities for bladder tumour detection (narrow-band imaging, blue light cystoscopy), utilisation of immediate post-operative intravesical chemotherapy, and combination intravesical chemotherapy regimens for BCG-refractory disease (e.g. gemcitabine-docetaxel).
Treatment options for NMIBC are likely to expand significantly over the coming years with the outcomes from trials examining
combination treatments, vaccine therapies, novel agents, and alternative modalities for delivery of treatment eagerly awaited.
Patients with muscle-invasive bladder cancer (MIBC) usually undergo further staging with either CT or FDG PET. Their treatment options include radical cystectomy (+/- neo-adjuvant or adjuvant chemotherapy), chemoradiation, or radiotherapy. Radical cystectomy preceded by neo-adjuvant chemotherapy is generally considered to offer the best chance of cure, however, various patient and disease factors may affect individual suitability or fitness for this.
If undergoing radical cystectomy, then a concurrent bilateral pelvic lymph node dissection is commonly
Patients with visible haematuria have a high risk of underlying urological malignancy. Even if they do not have risk factors for bladder cancer, further investigation is generally warranted with an MSU, upper tract imaging, and cystoscopy
Non-muscle-invasive bladder cancer is usually managed with cystoscopic surveillance and intravesical BCG or chemotherapy for higher risk tumours, while options for muscle-invasive bladder cancer include radical cystectomy (+/- neo-adjuvant or adjuvant chemotherapy), chemoradiation, or radiotherapy
Recent treatment advances include combination intravesical chemotherapy for BCG-refractory disease, robotic cystectomy, and adjuvant immunotherapy for high-risk patients.
performed, as well as urinary diversion usually with either an ileal conduit or neo-bladder.
Constructing a neo-bladder involves fashioning approximately 60cm of ileum into a bladdershaped reservoir, with reimplantation of the ureters and anastomosis of the urethra onto this. While a neo-bladder avoids the need for a stoma, it does not function like a normal bladder and may not be suitable for most patients.
Robotic cystectomy appears to deliver equivalent oncologic and perioperative outcomes to open cystectomy, with the robotic approach conferring advantages regarding blood loss, recovery, and potentially wound complications and venous thromboembolism.
Robotic cystectomy is now being offered in WA, through both the public and private sector, although some patients may not be considered suitable for this approach.
Another recent advance in the management of patients with MIBC in Australia is the ability for high-risk patients to access adjuvant immunotherapy funded through the PBS following neoadjuvant chemotherapy and radical cystectomy. Future directions for the treatment of MIBC may include combination systemic treatments, use of antibody-drug conjugates, and the use of novel investigations such as circulating tumour DNA to help identify patients suitable for bladder preservation.
Patients with metastatic bladder cancer have historically had limited treatment options, however, some patients are now able to access several lines of therapy including chemotherapy, immunotherapy, antibody-drug conjugates, and combinations thereof, resulting in improved survival.
Author competing interests – nil





Dermatologist supervised total body photography and sequential digital dermoscopic imaging for high risk patients with multiple naevi and melanoma.
Urgent Lesion Clinic for suspected melanoma diagnoses or any urgent lesion (private health insurance rebates apply in our day procedure centre).
Personalised melanoma risk assessment to determine surveillance intervals and educate patients on risk factors.
Confocal microscopy for diagnosis and pre-surgical mapping of lentigo maligna (in situ melanoma) at complex and cosmetically sensitive sites (Dr Collgros).
Management of cutaneous toxicities related to medical oncology treatments (A/Prof Caccetta).

A/Prof Tony Caccetta MBBS (Hons) FACD
Dermatologist

By Dr Reza Feizerfan, Pain Specialist, Nedlands/Murdoch
Cancer pain is a multidimensional phenomenon. The source of pain may be from cancer progression itself, from associated treatments, or from non-cancer related pain generators for example arthritis or radicular pain. Regardless of the reason, pain can significantly impact on patients’ quality of life, cause psychological distress, and lead to functional limitations.
While pharmacological approaches generally are the first line of treatment in cancer pain management, interventional techniques are a valuable tool to help reduce pain and improve dignity and quality of life.
Indications for interventional techniques
Refractory pain: When pain persists despite optimal pharmacological treatment.
Intolerance to medications: When systemic analgesics cause intolerable or uncontrolled side effects.
Decline in quality of life: While pain killers may produce an effective pain control, they may lead to cognitive bluntness, reduced ability to interact with the loved ones or increased need for support and care which may not be desirable.
Common pain interventions
Neurolytic Blocks are procedures where alcohol or phenol is used to abolish nerve function. Coeliac Plexus Block is used for upper abdominal malignancies such as pancreatic cancer. Superior Hypogastric Plexus Block for gynaecological and pelvic organ cancer. Lumbar sympathectomies for lower limb ischaemia. Intrathecal neurolysis for rectal and pelvic cancer.
Intrathecal Drug Delivery Systems are one of the most effective techniques to control wider spread pain from cancer. A catheter is inserted inside the thecal space, at the desired level of the spinal cord, to cover the dermatomes responsible for the painful area.
A connected pump delivers a range of medications, usually local
Key messages
Interventional pain techniques can be very useful in managing cancer pain
Cancer patients may have noncancer related pain which can respond to injections
Interventional pain techniques can help reducing polypharmacy, their side effects and improve quality of life in cancer patients.
anaesthetics (LA), opioids (morphine, hydromorphone) with or without adjuncts (clonidine). LA blocks pain signal propagation, opioids work on central nervous system mu receptors and clonidine helps with desensitisation. The combined effect can produce significant pain reduction, allowing to reduce, even to stop most of the systemic analgesia. This technique requires access to a trained nursing team in the community and generally is offered in terminal stages of cancer.
Neuro-ablation (Pulsed or Thermal radiofrequency denervation, Cryoablation,) uses a variety of techniques to modulate neural tissue activity or ablate/denervate nerves to prevent pain signal propagation. As an example, in metastatic rib lesions, cryo-ablation of subcostal nerves can reduce pain. Pulsed rhizotomy of peripheral nerves can reduce neuropathic pain secondary from radiotherapy.
I recently utilised thermal rhizotomy effectively to address pain from a metastatic lesion in the spinous process. I have combined thermal and pulsed rhizotomy in a case with localised shoulder cancer, preventing recurrent hospitalisations for pain management.
Hence, this technique can be utilised in number of different scenarios depending on the location of the lesion, the cause of the pain and the nerve supply.
Vertebroplasty – Metastatic vertebral body fractures unresponsive to analgesia can respond very well

by injecting bone cement into the fractured vertebral body.
Epidural injection, nerve root sleeve injection and dorsal root ganglion pulsed rhizotomy aim to deposit medications around the neural tissue to diminish localised inflammation or to modulate their function. Examples would be nerve irritation from cancer tissue compressing spinal nerves or neuritis from chemo or radiotherapy.
Peripheral nerve block and regional catheter is most commonly used for a neck of femur fracture or a paravertebral catheter for rib fractures. This is generally a shortterm measure to control the pain while the patient is awaiting definite treatment.
Spinal Cord Stimulation (SCS) is an advanced technique for managing neuropathic pain. It works by delivering electrical impulses to the dorsal column of the spinal cord providing pain modulation. Its efficacy has been established in chronic pain and its role is emerging in cancer pain, though the data is limited.
Cervical cordotomy – a thermal neuro-ablation of lateral spinothalamic tract at the level of C1/2 of the spinal cord would abolish the pain arising from contralateral body. It is generally used for chest wall pain such as mesothelioma.
While the above examples are modalities to help cancer-related pain, it is important to note that cancer patients may present with non-cancer related pain.
For example, knee arthritis, facet joint disease or sacroiliac arthralgia. Considering that the majority of cancer patients would be already on some form of analgesia for their cancer treatment, interventional pain technique can play an important role to help with their non-cancer related pain generators.
Author competing interests – nil
By Dr Greg Ong, Endocrinologist, Diabetes WA & Fiona Stanley Hospital
As another new year begins, we can reflect on the ingenuity of the past. Early in the 19th century, Royal Artillery surgeon John Rollo first used the term ‘diabetes mellitus’ to describe the excessive production of sweet urine by a “large corpulent person”.
Rollo differed from his peers, deducing that the problem arose from metabolism and not urination. He proposed appetite suppression with nauseating substances and a regulated low-carb diet “of animal food principally”. Sound familiar?
Rollo’s early methods are surpassed by the global collective wisdom of generations of clinicians, scientists and entrepreneurs. The 1920s provided insulin and metformin, while the 1940s brought sulfonylureas. Since 1990, many other drug classes have been commercialised.
Management guidelines grow fatter as more therapies and expanding research change best practice. Summary flowcharts still channel nostalgia for ‘stepwise’ management plans, but struggle to succinctly describe myriad options for numerous situations. Some basic concepts will help navigate this confusing landscape.
What is the overall treatment objective?
Is the objective of a professional football club to win matches? If a
Glycaemic control alone is inadequate for cardiovascular protection if attempted after years of hyperglycaemia
Prioritise SGLT2i or GLP1RA in certain T2DM cohorts for improved longevity, reduced hospitalization, and protection from cardiovascular and renal disease regardless of glucose effects
For advice, call the Diabetes Connect hotline for GPs on 9436 6270.
mediocre team has packed stadia and huge profits every season, it might risk ruin by buying better, but expensive players. Winning titles may lead to success, but not always. Diabetes is defined by high blood sugar, so we dutifully treat glucose. However, the main objective is really to maximise length of life free from amputation, heart disease, dialysis and blindness. Lowering glucose may achieve this, but not always.
Rigorously adhering to stringent targets (e.g. HbA1c <7%) delays microvascular complications. If applied early from diagnosis and for as long as possible, macrovascular disease and mortality is also delayed. These benefits persist even if there is less diligent
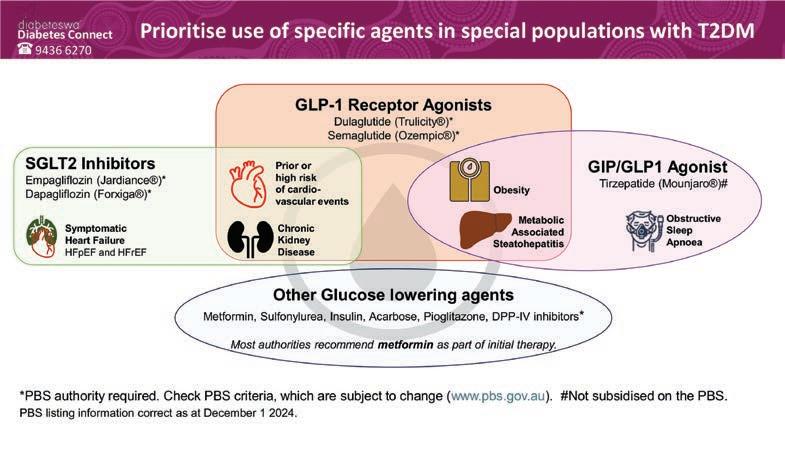

control later. However, there is a narrow window of opportunity, as stringent glucose control becomes insufficient for preventing death, MI and stroke in patients with chronically suboptimal levels.
Rollo frequently observed treatment failure due to “the careless and faulty application of [his methods] by most physicians” and “rebellion of patients”. Avoid procrastination and hit targets by intensifying therapy. Metformin is usually recommended as firstline. After that, it’s your choice. I am often asked if sulfonylureas are “bad”, or if early use of insulin should be avoided. All agents should be on the table, chosen for the clinical context, and always subject to review.
New potent incretin agents such as the weekly GLP-1 receptor agonists (GLP1RA) and twin GIP/ GLP1 agonist tirzepatide enable the realistic possibility of diabetic utopia: normoglycaemia (HbA1c <5.7%) without hypoglycaemia. We are clearly not helpless for want of effective options.
However, throwing more medications at the problem won’t work if intolerance provokes noncompliance. Always consider the positive or negative impacts of proposed treatments on girth, gut, hypos, sanity and bank accounts. Allied health review for diabetes education and lifestyle modification will improve patient buy-in. Also, weight loss by any method (especially >15% below baseline) can achieve prolonged normoglycaemia without glucose lowering agents. However, a rebound in weight will see the return of elevated blood glucose.
GLP1RAs and SGLT2 inhibitors (SGLT2i) have outsized value for those with high cardiovascular risk, symptomatic heart failure and nephropathy. The cardiovascular and kidney preserving benefits are unrelated to lowering glucose. In contrast, other classes of diabetes
By A/Prof Tee Lim, Radiation Oncologist
Prostate cancer remains one of the most common malignancies affecting men, particularly those over 50 years of age. While it typically progresses slowly, allowing for prolonged disease management, early detection and timely intervention are key to improving clinical outcomes.
The asymptomatic nature of earlystage prostate cancer highlights the importance of routine screening and awareness of potential symptoms, such as lower urinary tract symptoms, haematuria, erectile dysfunction, or pelvic and lower back pain. These symptoms often overlap with benign conditions like benign prostate hyperplasia or prostatitis, necessitating careful differential diagnosis through appropriate clinical investigations.
The prostate specific antigen (PSA) test remains a cornerstone for initial prostate cancer screening, despite its limitations in specificity. Elevated PSA levels warrant further investigation, which may include multiparametric prostate MRI scan and/or a prostate biopsy, to confirm malignancy.
Advanced imaging modalities, such as PSMA PET scans, are invaluable for staging, providing crucial information about extracapsular extension or potential metastatic spread.
Early diagnosis of prostate cancer significantly improves the chances of successful treatment. Early-stage localised prostate cancer, typically confined to the gland, offers an opportunity for curative interventions,
Advanced Treatments Offer Options: Techniques such as stereotactic provide effective, less invasive alternatives to surgery.
Research Drives Progress: Clinical trials, such as ASTuTE, offer opportunities for patients to access new technologies.
such as radical prostatectomy or radiation therapy (RT).
In contrast, advanced-stage disease, requires a multidisciplinary and multimodality treatment approach that incorporates androgen deprivation therapy (ADT), systemic therapies, palliative RT, and palliative care. Understanding the disease's variable progression – ranging from slow-growing to more aggressive forms – is critical for developing personalised management strategies.
Treatment modalities
For localised prostate cancer, treatment options such as surgery and radiation therapy offer comparable cancer control outcomes, necessitating patientcentred discussions about potential side effects, recovery, quality of life, and potential salvage treatment options for local recurrent disease.
Advances in radiation therapy, including technologies such as volumetric modulated arc therapy (VMAT) and stereotactic ablative
medications only lower glucose as their sole therapeutic benefit –except for pioglitazone which has an unfavourable side-effect profile. The special roles for GLP1RA and SGLT2i have been acknowledged in major guidelines since 2018. Yet, uptake has been glacial in those with the greatest need.
In patients with specific comorbidities, a glucocentric
strategy must be supplanted by an organ protecting strategy. We need to change paradigms – SGLT2i and GLP1RA are actually agents for longevity and preventing cardiorenal disability, with a bonus of glucose lowering.
Potent incretin agents also improve obesity, sleep apnoea and metabolic fatty liver disease. Therefore, if patients have a

body radiotherapy (SABR), allow for highly precise tumour targeting and while minimising damage to adjacent healthy tissues. Recent evidence demonstrates that SABR (e.g. 5-fraction regimens), offer excellent cancer control rates exceeding 95% at five years for early-stage disease. This approach also reduces treatment durations, improving patient convenience without compromising outcomes.
Supportive technologies such as absorbable rectal spacers further reduce radiation exposure to critical structures. These innovations make radiation therapy a viable, noninvasive alternative to surgery, often offering reduced recovery times and preserving functional outcomes.
Clinical trials play a vital role in advancing prostate cancer management, offering patients access to emerging and novel therapies and technologies. The ASTuTE clinical trial, currently recruiting intermediate-risk patients in Western Australia, is an excellent example of innovation in action.
This trial is evaluating the use of an artificial intelligence biomarker test to determine the need for ADT alongside radiation therapy. By stratifying patients based on tumour biology, the test aims to optimise treatment decisions, enhance prognostic accuracy, and potentially reduce ADT-related side effects for suitable patients.
– References available on request
relevant comorbidity, add or switch to SGLT2i or GLP1RA even if glycaemic goals are met with other agents. And don’t forget the lipids and blood pressure.
Author competing interests – Author has received educational grants or honoraria from Eli Lilly, Novo Nordisk and Astra Zeneca.
By Dr Shahriar Raj Zaman, Plastic, Reconstructive Surgeon, Mt Lawley & Murdoch
Skin cancer remains one of the most prevalent malignancies in Australia, with effective treatment occasionally requiring a multidisciplinary approach.
Among the treatment options, reconstructive surgery plays a pivotal role in restoring both function and appearance after excision of cancerous lesions.
Skin cancer treatments such as wide local excisions, often leave significant defects, particularly when tumours are located in cosmetically or functionally sensitive areas such as the face, neck, or hands. Reconstructive surgery bridges the gap between successful oncological treatment and the restoration of the patient’s quality of life, with the aim to strike a balance between form and function.
Beyond aesthetics, reconstructive procedures aim to maintain functionality, minimise scarring, and prevent complications such as contractures or impaired mobility.
Reconstructive surgery in skin cancer follows several core principles (owing to the modern day father of plastic surgery Sir Harold Gillies) to ensure optimal outcomes:
• Oncological safety: Reconstruction is planned only after achieving clear margins to prevent recurrence.
• Minimal morbidity: Techniques prioritise minimising donor site morbidity, especially in complex reconstructions.
• Functional preservation: Surgeons focus on restoring functionality, particularly in areas like the eyelids, lips or nose.
• Aesthetic outcome: Reconstructive efforts aim to blend scars into natural lines and contours for a harmonious appearance.
A variety of reconstructive techniques are available,




ranging from simple to complex (now known as the so-called reconstructive elevator). The choice depends on the size and location of the defect, patient-specific factors, and surgeon expertise.
• Primary closure: For small defects, direct suturing of the wound edges can provide excellent results with minimal
disruption to surrounding tissues.
• Skin grafting: This technique is suitable for larger defects where primary closure is not possible. Split-thickness or full-thickness grafts are harvested from donor sites and transplanted to the affected area. While effective, grafts may have a less natural appearance compared to local flaps.
Reconstructive surgery is integral to comprehensive skin cancer treatment
It restores what cancer takes away—function, form, and confidence
As techniques evolve, the synergy between oncological treatment and reconstruction continues to offer hope and healing to patients, reaffirming the critical role of this specialty in modern medicine.
• Local flaps: Local tissue is repositioned to cover the defect, ensuring a better colour and texture match. Common examples include rotational, advancement, and transposition flaps. Local flaps are often used for facial reconstructions.
• Free tissue transfer (free flaps): For extensive or deep defects, tissue is transferred along with its vascular supply from a distant site. This technique demands microsurgical expertise and is ideal for complex reconstructions
requiring robust vascularisation.
• Composite reconstruction: Combining techniques, such as a flap with a graft, is sometimes necessary for intricate defects involving multiple tissue layers.
The field of reconstructive surgery has benefited from technological and procedural innovations. For example, bioengineered scaffolds and dermal matrices facilitate tissue regeneration and provide good integration in certain complex reconstructions. Similarly, advancements in surgical planning, including the use of 3D imaging and virtual simulation, allow for more precise and tailored approaches for the complex microsurgical reconstructions.
Despite advancements, reconstructive surgery faces several challenges. Achieving oncological safety while minimising reconstruction-associated complications can be difficult, especially in high-risk patients with comorbidities. Managing patient expectations regarding aesthetic outcomes and recovery timelines
Heel pain is a frequent problem that presents to the general practitioner. Plantar fasciitis is the most common cause of under the heel pain. Most patients will improve with non-operative treatment but not all.
Surgery is a very effective form of treatment for this condition in patients with long standing refractory symptoms.
Before being considered for surgery patients should undergo at least six months of non-operative treatment that includes the following (in the appropriate order):
• Rest, avoidance of activity
• NSAIDs, stretching exercise program
• Orthotics: off the shelf or custom
• Cortisone injection (one only)
• Shockwave therapy

Surgery can be open or endoscopic. The principle part of the procedure is release of the plantar fascia near its origin on the heel. Historically only the medial half was released but recent literature supports more complete release.
is another critical aspect of the reconstructive process.
A practical case example illustrates the importance of reconstructive techniques: An elderly patient underwent a wide local excision of a biopsy proven squamous cell carcinoma on the right pre-auricular region (Figure 1). Post-excision, the defect was approximately 5x7cm in size requiring reconstruction (Figure 2). A large cervicofacial flap was utilised to reconstruct the defect and is shown here at only three weeks post-surgery (Figure 3).
The success of reconstructive surgery in skin cancer is measured not only in oncological terms but also in the patient’s satisfaction with their functional and cosmetic outcomes. Early intervention and tailored reconstructive plans significantly improve long-term results, ensuring patients regain confidence and normalcy in their lives.
Author competing interest – nil

Open surgery is performed through a 3cm incision in the proximal arch and allows not just plantar fascia release but also decompression of the tarsal tunnel and Baxters nerve which is often implicated in heel pain.
Endoscopic plantar fascia release is indicated for those without nerve compression symptoms and is done through a much smaller incision using a camera assisted cutting device much like a carpal tunnel release.
Both open and endoscopic releases are performed as day cases and require approximately two weeks on crutches. Recovery is slightly quicker for endoscopic patients as you would expect. Patients can expect an 8090% chance of a good result from surgery. Complications are rare.


St John of God Medical Centre Suite 10, 100 Murdoch Drive, Murdoch WA 6150
Telephone: (08) 6332 6300 Facsimile: (08) 6332 6301
www.murdochorthopaedic.com.au Murdoch Orthopaedic
By Dr Santanu Baruah, Obstetrician & Gynaecologist, South Perth
Endometriosis is a common yet often misunderstood gynaecological condition affecting millions of women globally, particularly during their reproductive years. It is a leading cause of chronic pelvic pain and, significantly, infertility.
Endometriosis occurs when tissue similar to the endometrium grows outside the uterus, often on the ovaries, fallopian tubes, and the pelvic peritoneum. It causes inflammation, scar tissue formation (adhesions), and sometimes cysts, particularly on the ovaries (known as endometriomas or ‘chocolate cysts’).
According to estimates, 30-50% of women with endometriosis struggle with infertility, making it one of the most common causes of reproductive challenges The exact mechanism by which endometriosis impairs fertility is unknown.
One of the most direct ways it can lead to infertility is through the distortion of the pelvic anatomy. Adhesions and scar tissue can form between the reproductive organs. This can block the fallopian tubes, preventing the egg and sperm from meeting, or impairing the movement of the embryo towards the uterus. Endometriomas on the ovaries can also affect ovulation, either by damaging ovarian tissue or causing the release of poorquality eggs.
Women with endometriosis, experiencing infertility have several treatment options
Early diagnosis and a tailored treatment plan are critical for improving reproductive outcomes
With the right approach, many women with endometriosis can successfully conceive and build the families they desire.
Endometriosis is associated with chronic inflammation in the pelvic cavity, which can have several negative effects on fertility. Elevated levels of pro-inflammatory cytokines and immune cells can impair sperm motility and function, making it more difficult for sperm to reach and fertilise the egg. Inflammation may interfere with normal embryo implantation in the uterine lining.
Hormonal dysregulation is another significant factor in the infertility associated with endometriosis. The condition is associated with elevated levels of oestrogen and reduced levels of progesterone. Oestrogen stimulates the growth of endometriotic lesions, while a relative lack of progesterone may impair the ability of the endometrium to support implantation and early pregnancy. These hormonal imbalances may also contribute to irregular ovulation or poor-quality eggs.
Women with advanced stages of endometriosis (Stage III and IV) may experience a decline in their ovarian reserve – an estimate of the number and quality of a woman’s remaining eggs. This decline is partly due to the damaging effects of endometriomas on ovarian tissue. Studies have shown that the ovarian environment in women with endometriosis may also impair egg quality, leading to lower rates of successful fertilisation and embryo development.

Diagnosis is often delayed due to the variable nature of its symptoms. While pelvic pain and painful periods are hallmark symptoms, some women may have mild or no symptoms, making it difficult to identify the condition without a thorough evaluation. A definitive diagnosis of endometriosis often requires a laparoscopy, a minimally invasive surgical procedure that allows a surgeon to directly visualise and biopsy the endometrial lesions.
Women with endometriosis have several infertility treatment options depending on the severity of the disease and the individual’s reproductive goals.
Laparoscopic surgery is often considered for women with endometriosis who are trying to conceive. During surgery, the endometriosis surgeon can remove or destroy endometrial lesions, adhesions, and cysts, potentially improving fertility outcomes.
Research suggests that removing endometriomas and other lesions can restore a more normal pelvic anatomy, enhance ovarian function, and increase the chances of natural conception. About 60% of couples with stage I and II endometriosis may conceive naturally within six months provided there is no other associated factors for infertility. However, stage III and IV endometriosis cases are often referred for assisted reproduction.
For women who struggle to conceive with endometriosis, assisted reproductive technologies (ART) such as in vitro fertilisation (IVF) may be recommended. IVF bypasses many of the anatomical barriers and inflammation-related issues seen in endometriosis.
For instance, IVF allows eggs to be retrieved directly from the ovaries, fertilised in the laboratory, and transferred into the uterus,
By Malina Kelly, Pelvic Health Physiotherapist, Guildford
Common prostate conditions such as benign prostatic hyperplasia (BPH) or prostate cancer can cause pelvic symptoms such as voiding dysfunction, nighttime and daytime frequency of urination, urinary urgency and urinary incontinence (UI).
Despite the importance of the prostate and the prevalence of prostate symptoms, many men are unaware of the anatomy of their pelvis and do not know how they can improve their pelvic health to conservatively manage pelvic symptoms secondary to prostate changes.
In 2022, an estimated 24,217 men were diagnosed with prostate cancer in Australia. Prostate cancer has a five-year survival rate of 96%. It is an age-related condition and men with a male primary relative with prostate cancer have an increased risk of diagnosis.
Treatment of prostate cancer, including radical prostatectomy (RP), radiation therapy and hormone therapy can have both short-term and long-term side effects. Side effects of prostate cancer treatment significantly impact the physical, mental and emotional health of men and their families.
Common RP side effects include UI and erectile dysfunction (ED). Over 90% of men will experience UI following RP. Approximately 5-10% of these men will have UI that will persist beyond 12 months postoperatively. ED persists beyond two
Key messages
Prostate cancer treatment impacts a man’s quality of life
Pelvic health physiotherapy can improve outcomes after surgery.
years in approximately 40% of men.
Radiation therapy has an increased risk of bowel dysfunction in the short term, and though side effects of UI and ED are less common in the short term they can occur up to 1-2 years following radiation treatment. Side effects of hormone therapy can include fatigue, sexual dysfunction, weight gain and mood changes.
Active surveillance is an option that is given to some men who have a low-grade, localised prostate cancer diagnosis. This involves monitoring changes in the prostate but not having active cancer treatment. These men avoid the side effects of treatments and may potentially be able to avoid treatment long term.
Pelvic health physiotherapists have an important role to play in supporting men on their prostate cancer journey. This includes education on the anatomy of the pelvis, the role of the prostate and the pelvic floor muscles (PFM) and the side effects of chosen treatments. This can also include helping men undergoing active surveillance to be proactive in their pelvic health.
Pelvic health physiotherapists provide individual PFM assessment
circumventing any blockages in the fallopian tubes. Studies show that IVF success rates in women with endometriosis are lower than in women without the condition, but it remains one of the most effective fertility treatments.
Egg freezing is an option for women with endometriosis who wish to protect their future fertility. It is important to assess ovarian
reserve (AMH level) for patients with endometriosis as it can be a potential guide for those wishing to protect fertility.
Hormonal treatments such as oral contraceptives, gonadotropinreleasing hormone (GnRH) agonists and antagonists, and progestins can effectively manage the symptoms of endometriosis but are generally not used as a fertility treatment. These

and training using a variety of biofeedback techniques including real-time ultrasound and manual feedback. Studies have shown better outcomes for men post RP if they have done pre-operative PFM training.
Physiotherapy education includes fluid optimisation, bladder retraining strategies and bowel education. Physiotherapy management also includes support and advice for ED and continence products. Pelvic health physiotherapists can prescribe strength exercises, advise on physical activity and provide lifestyle advice to help men to improve their overall health.
Pelvic health physiotherapists have a significant role in supporting men with prostate issues. The combination of postgraduate expertise and time spent with patients, allows physiotherapists to effectively support men to process their diagnosis, treatment and symptoms. Through ongoing care and problemsolving physiotherapists help men to connect to their bodies, improve their pelvic health and optimise their outcomes. A prostate cancer diagnosis is often the first-time a man has focused on pelvic health. This may also be the first time a man has seriously considered improving his health. Pelvic health physiotherapists are vital in supporting men as they navigate this journey.
Author competing interests – nil
therapies suppress ovulation and reduce the production of oestrogen, helping to shrink or suppress endometrial lesions. However, since they also prevent pregnancy, they are typically reserved for women who are not actively trying to conceive.
Author competing interests – nil
By Dr Amit Saha, Paediatric Gastroenterologist, Hollywood
Fussy eating is common in childhood, and a frequent cause for stress in parents. It can start as early as two months with the disappearance of the sucking reflex. Data suggests introducing solid, lumpy food no earlier than from six months onwards, or children are more likely to develop fussy eating habits.
Babies six to 12 months are usually open to eating anything that is offered, and fussy eating usually starts just after turning one and peaks at around 20 months of age, mainly with the introduction of food that leaves a bitter aftertaste, such as vegetables.
However, it is important to persist and keep offering them nonsweet and non-fat food in this crucial developmental window, to prevent future fussy eating. Tongue protrusion may be a problem in babies refusing food, but this is considered a normal initial physiological reaction to solids and can be overcome with persistence. Thus many parents may think their child is fussy, when, they are showing normal, age-appropriate behaviours.
The first consideration is growth: it is imperative to do an accurate anthropometry and establish their percentiles both for height and weight. The next thing to consider is nutrition, and good growth may not necessarily mean good nutrition.
Review of grazing habits and beverage consumption through a typical day is important, and aim to reduce all sugar containing drinks, including fruit juices, especially at least 30 minutes prior to mealtimes. Go through different food groups which can have specific nutritional value, such as milk/dairy providing the calcium requirements of the body, meat being a good source of zinc and iron.
Specific vitamin deficiencies, for example vitamin A, C or B12, arising from a restrictive diet, can give rise to distinct conditions.
If either growth or nutrition seem to


be affected, further investigations may be warranted.
Pattern recognition is paramount, always suspect eosinophilic esophagitis (EoE) in a child with atopy, food allergies and frequent vomiting.
However, children may present with a wide range of symptoms and signs including reflux, regurgitation, coughing, food refusal, poor sleep and vomiting in the younger child; to abdominal pain, swallowing difficulties, retrosternal pain, drinking excessive water at mealtimes and food bolus obstruction in the older child.
Peripheral blood eosinophilia and/ or raised total IgE level may be seen but not universal. Children with a past history of cow’s milk protein allergy and autistic children are more prone to having EoE. A high index of suspicion and prompt referral for a gastroscopy with biopsies can lead to an early diagnosis and effective, tailored management in these children.
Paediatric feeding disorder (PFD) is defined as impaired oral intake that is not age-appropriate, and is associated with medical, nutritional, feeding skill, and/or psychosocial dysfunction. If suspected, an early referral to a specialist and subsequent involvement of a multidisciplinary team is warranted.
Evaluation by a speech therapist, possibly with a videofluoroscopy may be appropriate. A dietician must be involved if malnutrition is suspected, and high calorie supplementation is deemed necessary. Psychosocial impact on feeding may be significant and should be appropriately assessed by professionals. A paediatric gastroenterologist must be involved to determine the need for bloods, imaging, endoscopy for example, and these children often need longterm monitoring and follow up at a multidisciplinary feeding clinic.
In primary care, the focus should be on evaluation and interventions, rather than investigations. After initial evaluation of growth and nutrition, and as long as EoE or PFD is not suspected, there are several strategies that can implemented, mainly with a view to promote appetite and increase the range of food groups offered in the diet and supplementing vitamins and minerals to ward off any nutritional deficiencies.
Interventions include increasing the gap between mealtimes to
Evaluating growth and nutrition is the first step in assessing children with fussy eating; good growth may not mean good nutrition
Most children do not need investigations in primary care. Commonsense behavioural interventions are the cornerstone of management in the community
A low index of suspicion and early referral is warranted in suspected eosinophilic esophagitis and/or paediatric feeding disorder.
stimulate appetite, cutting down on fruit juices and other beverages between meals, encouraging cereals with fortified vitamins, minerals, and iron, administering multivitamins (tablets rather than gummies as gummies have little iron or zinc) and calcium fortified orange juice in children who refuse milk and dairy products.
Cyproheptadine is used as an appetite stimulant with good success but should always be used in conjunction with other strategies. Food logs are not recommended as

this has been shown to cause more parental anxiety. Dietary recall is more pragmatic. A high calorie supplement in these children is not recommended as it may further promote fussy eating. Bribery may also be an effective strategy, as long as the incentive is not another food group, for example dessert for eating some vegetables, as studies have shown this may make matters worse.
Commonsense behavioural interventions to successfully expand the variety of food groups in the diet and nutritional supplementation remain the cornerstone of managing this common but challenging issue.
Author competing interests – nil


Consulting at:
Garden City Specialist Centre 537 Marmion Street, Booragoon WA 6154
Surgeons House 162 Cambridge Street, West Leederville WA 6007
Mandurah – 360 Health 10/3 Dower Street, Mandurah WA 6210
Office Phone: (08) 9332 0066 | Mobile Phone: 0401809255 | Email: reception@oswa.com.au





After a series of medical episodes with her son, Kate Mitchell created a video to educate regional kids and their families about snake bite first aid.
By Ara Jansen
Passionate about creating positive change in rural and regional Australia, Kate Mitchell came up with a short animation to educate regional kids on how to respond to a snake bite.
With a team of animators and video makers, the mum, teacher and sheep farmer from the Great Southern region created Fangs on the Farm. In it you’ll meet Darcy Dingo, Gracie Gecko and Harry Hopperoo and their travelling first aid Help HQ which helps a local survive a medical emergency.
Mum-of-three Kate was inspired to create the freely available 10-minute video after having to perform CPR on her then 16-month-old and youngest son Darcy who had a tonic-clonic (grand mal) seizure at their Narrikup farm, five hours from Perth.
Darcy had three seizures in one month and the last one could have been fatal. He is now four and has not had a seizure for almost 18 months.
Spending all those hours in hospital away from home in Perth, much of it during COVID, meant friends and family could not visit. With everyone wrapped up tight in PPE, there weren’t many hugs or much contact to go around.
Understandably Kate found it very isolating, but the upside was it gave her time to think.
A number of ideas came from those long hours by Darcy’s bedside, including a website called The Darcy Effect, home to the Hospital Bags initiative, which can be delivered to regional and rural hospitals when a family finds themselves unexpectedly in hospital. The bag is filled with functional and fun items, including toothbrushes and kids’ books.
The website is also linked to a paediatric health information hub, with a pilot currently being run in the Great Southern region in conjunction with Perth Kids Hub to help rural and regional families access services to support their child’s development.
The other idea which came from her time spent in hospital was the creation of a video for young children – and the odd adult or

grandparent who needs a reminder – about how to deal with a snake bite when you’re not close to a hospital. It was a year in the making to finish Fangs on the Farm
“I feel like kids in rural areas need resources which relate directly to them and their lives and situations,” says Kate, who self-funded the project. “That’s why we created Darcy Dingo, Gracie Gecko and Harry Hopperoo. Kids need something to relate to and they are clever, if you give them information, they can use it.
“We thought a snake bite was a simple and direct one to use first. We were able to give simple and clear directions for what you need to do.”
Kate has also put together a series of supporting resources for teachers about medical emergencies and how to deal with them.
With her teaching background, she has made sure they can be used as part of the primary school syllabus, spanning across a number of subjects.
Fangs on the Farm premiered late last year to 100 family and friends at Perth Zoo and is free to view on YouTube.
The feedback has been so positive, Kate is looking to find sponsorship or funding for a series of video adventures for the trio of animal rescuers about other medical emergencies faced by kids in rural and remote areas.
You can find the video by searching ‘Fangs on the Farm’ on youtube.com

The Alliance Française French Film Festival, Australia’s largest national film festival and the biggest celebration of French cinema outside of France, is back next month.
The festival returns to Perth for five weeks from 13 March-16 April and regionally in Bunbury from 10-13 April. From outstanding biopics honouring and bringing new life to the journeys of legendary figures in French culture, exhilarating stories, music-driven dramas and l’amour in all its forms, there’s truly something for all to enjoy.
The full festival line-up will be released, and tickets go on sale, Wednesday, 5 February. Courtesy of Alliance Française we have five double passes to give away.
To enter, use the QR code on this page or go to mforum.com.au and hit the competitions tab.
It is indeed a pleasure to again review the wines of this great Margaret River producer. Since my first article in 2012, they have continued to climb the quality ladder. Located in the Wilyabrup sub-region of Margaret River, in what one might call the ‘dress circle’, they certainly compare with famous neighbours in terms of quality production. The vineyard was established in 1985 and has 27ha of vines with plantings of the mainstream regional varieties – Semillon, Sauvignon Blanc, Chardonnay, Cabernet Sauvignon, Merlot and Shiraz.
Winemaking has been under the direction of the vastly experienced Jeremy Hodgson since 2015, and wines are marketed under several quality levels, the mainstay being the Fermoy Collection (or Estate Range), with Estate Reserve wines the pinnacle of quality and only produced from selected parcels of the best fruit.

Fermoy Margaret River 2024
Semillon Sauvignon Blanc (RRP $30)
A great expression of this popular regional blend. The season was warm and dry, resulting in an early vintage, with fruit of good quality. It was one of those nice years when the Marri blossom kept the birds from the vines. This wine is vibrant and enticing, with the 63% Semillon giving dominant aromas of fresh herbs and guava and the Sav Blanc adding citrus notes, pungency and spices. Palate weight is excellent by way of fermentation and maturation in oak. A nice wine, displaying the synergy of these two varieties in the classic Margaret River style.
Fermoy Margaret River 2020
Wilyabrup Cabernet Merlot (RRP $30)
Needs to breathe off a little in glass to dissipate some ullage characters, but quickly freshens up. A 50% Cab Sav, 40% Merlot, 10% Shiraz blend. Displays aromas of dark berries, dried herbs and cardamon, with a distinct savoury edge, which leads to a supple smooth mouthfeel, a mid-weight, mid-length wine with a fruity finish. Tannins are softened by the Merlot. Oak is evident but not central to the style. Flavours of mulberry, redcurrant and black olive, with a touch of spice. A good everyday wine and should drink well up to five more years.
Fermoy Estate Margaret River Wilyabrup 2018 Cabernet Sauvignon (RRP $55)
Great to taste a wine again from that classic 2018 vintage. The wine is still youthful at six years, with deep garnet/red colour, the meniscus only slightly softening. The nose displays some beautiful development. The slow ingress of oxygen is evident, resulting in a wonderfully complex, integrated mix of superb fruit and oak. It has the Margaret River cassis foremost, backed up by silky black olive, sage and supported by cedary oak. This wine is drinking nicely now. Complex, integrated and complete, but has the structural elements to go another 8-10 years.
Fermoy Margaret River 2023 Reserve Chardonnay (RRP $80)
This wine is from the top Reserve range, a classic MR Chardonnay and certainly my wine of the tasting. Has a luminescent mid-gold colour, attractive in the glass. The nose is rich, ripe and inviting. Shows hazelnut characters, and wonderful toasty oak. The fruit is intense, succulent and mouthfilling, and displays white peach, grapefruit, cashew and oatmeal. All the winemaking techniques come into play here –quality oak, creamy malo-lactic fermentation, lees stirring – all giving to an intense, balanced, complex and lingering wine. I love this wine now, but it will reward with a few years cellaring.



Two classical musicians have commissioned four new works by female composers to bring something different to Fringe World this year.
Presenting a classical music show for this year’s Fringe World came with a twofold mission from its creators.
While percussionist Paul Tanner and guitarist Jonathan Fitzgerald wanted to draw a new audience into their musical world and hopefully find some new converts, they also had a bigger plan.
Ascendent Messages at Callaway Auditorium on 8 February is an immersive concert featuring new works for classical guitar, percussion and electronics. What’s special is that the evening will be the world premiere of four works by award-winning female Australian composers Maria Grenfell, Alice Humphries, Kate Milligan and Kathy Potter.
“Fringe dips into and attracts a totally different audience and we hope to draw in some of those people,” says Jonathan, who is also a lecturer and the chair of strings and guitar at UWA. “What better way to show off four fantastic composers in a way that’s accessible to people who might have otherwise never seen a classical concert.”
Each piece ranges from 10 to 15 minutes in length, making it a perfect classical tasting plate for those who
By Ara Jansen
are unfamiliar with the genre but curious to dip their toes in.
Paul, the principal percussionist of the Perth Symphony Orchestra and a frequent performer with the West Australian Symphony Orchestra, has collaborated musically with Jonathan in the past, but this time they wanted to do a bigger, more substantial work.
Ascendent Messages is the name of Alice Humphries’ piece and the pair felt it served well as a collective name for the first performances.
When Jonathan and Paul took part in a collaboration between the UWA percussion and guitar students in 2023, it became clear that the number of new works by female composers was very low.
“In this canon and in a number of others, female composers are under-represented and this genre is particularly affected,” says Jonathan. “We thought what better way to take a positive step to rectify this than by commissioning a series of new works.”
The four composers – three who hail from Perth and one from Tasmania – had no brief and total artistic freedom while writing for percussion and guitar. Jonathan says they were familiar with the
composers’ previous works and knew each of the pieces would be very different. Apart from the instruments they are performed on, the pieces share nothing in common thematically or stylistically.
Expect a diverse program on the night. For example, Promenade by Maria Grenfell explores the idea of instruments moving along together at several different speeds, while Kate Milligan’s Red Earth Mine is a soundscape for the iron ore industry, including an archival recording of a mining blast, while reflecting on mining’s impact on the landscape.
Across the four pieces, Jonathan says the work is a mix of solid playing and some challenging sections which will definitely make him sweat a little.
“Part of the goal of commissioning new work is so that other people can play them in the future as well.”
The pair also plan to record the works later in the year.
Ascendent Messages is at Callaway Auditorium at UWA on 8 February at 7pm. Tickets from www.fringeworld.com.au
This page intentionally left blank


Consult rooms available for sessional rental – suitable for specialists or allied health
4 strategic locations in Nedlands, Bentley, Mandurah and Geraldton
•Nedlands – Hollywood Specialist Centre, suite 23, 95 Monash Ave
•Bentley – unit 3, 10 Mills St
•Mandurah – unit 7, 21 Sholl St
•Geraldton – 9 Urch St, Beresford
For more info, contact practicemanager@apollocardiology.com.au or 6166 3737
Website link https://apollocardiology.com.au

Medical Rooms Available for Specialists and Allied Health
Lakes Shopping Centre, Shop 2, 620 Northlake Rd, South Lake WA 6164
•Available for ALL Specialists and allied health professionals. Opportunity to become a part of the GP clinic / support.
•Consulting rooms, reception/waiting area, kitchen/breakout area, store records room, and other zones.
•These consulting suites are situated on the ground floor of the medical practice.
•Pathology on site (Clinipath)
•Room Sizes:
– Room 3: 3.5 x 3.4 meters = 12 Sq m
– Room 4: 4 x 3.2 meters = 12.8 Sq m
– Room 5: 4 x 3.2 meters = 12.8 Sq m
•Rent hourly and full time available.
•Rent negotiable.
For Further details and enquiries please contact p.manager@southlakefamilypractice.com.au or 08 9417 1009
Hollywood Medical Centre Suite 36, First Floor, 85 Monash Avenue, Nedlands
87sq m – fully fitted, large reception, 2 consulting, 2 treatment & 2 store rooms.
Contact: Irene 0409 688 339

Doctor Opportunity at The Woods Medical Centre
We are looking for an enthusiastic and experienced GP to join our growing team.
The Ideal Candidate:
Strong General Practice Skills:
•Proven experience in providing highquality patient care across a diverse range of medical conditions
•Excellent clinical skills and a commitment to preventative healthcare
•Experience in managing chronic diseases effectively
•A keen interest in skin cancer management preferred but not essential. We offer a unique opportunity to combine comprehensive general practice duties with an opportunity to develop skin cancer screening and procedures for that candidate with skin cancer management interest.
Team Player and Communicator:
•Ability to collaborate effectively with a supportive team of healthcare professionals.
•Excellent interpersonal and communication skills to build rapport with patients.
Essential Requirements:
•FRACGP qualification
•Vocational Registered
•AHPRA registration.
What We Offer:
•Supportive and friendly work environment with a focus on work-life balance
•Nursing support
•No weekends or afterhours work
•Modern facilities and equipment
•Best Practice software
•Mentorship and training opportunities should you wish to develop skin cancer management skills
•Opportunity to work alongside experienced practitioners in a collaborative setting
•A location that is not far from the beach.
For more information or a confidential chat, please contact our Practice Manager at 0478 021 910 or email practicemanager@thewoodsmedical.com.au

Palin St Family Practice is a small privately owned GP located in Palmyra which has been continuously operating since 1923.
We are looking for a VR doctor and provide a supportive administrative and nursing team in a fully accredited practice.
Our patient base is well established, and you would have an immediate patient list on commencement.
For further information
please contact Jackie our Practice Manager on 0403 343 401 or via email office@psfp.com.au

BURSWOOD
Earn 100% of Billings for the First 3 Months!
Join our well-established, accredited mixed-billing clinic in Burswood and earn 100% of billings for the first 3 months (75% thereafter).
Perfect for new VR GPs looking to establish themselves, with full-time/part-time options.
Work alongside 3 experienced GPs in a fully computerised clinic with on-site pathology and RN support.
Please contact Dr Ang on 9472 9306 or Email: info@thewalkingp.com.au



Joondalup Campus is seeking expressions of interest from vocationally registered general practitioners
WHAT WE OFFER
15% service fee
Mixed billing
Free, reserved parking
Full time registered nurse and practice management support
Exceptional administrative support team.
The ECU Health Service assists students, staff and the university community with their health care needs. The primary function of the service is to provide students with psychosocial and physical health support, so that they may achieve an optimal academic performance for the duration of their studies.
In providing comprehensive patient healthcare, our medical practitioners will consider and respect patients’ rights, identity, body diversity, beliefs, language, religious and cultural backgrounds.
WHERE WE ARE
Located within the Wellbeing Precinct on the ECU Joondalup Campus, our AGPAL accredited student psychological services, with a coffee shop and free parking close by.
Availability for four to six GP sessions per week
We are open Monday to Friday, 8.30am – 4.30pm
No weekends or after-hours necessary.
Applications are now open from candidates who have either Permanent Residency or Australian citizenship, unrestricted Medical Board of Australia registration and no Provider Number restrictions. For more information , please contact Laura Harnett –Practice Manager on practicemanager@ecu.edu.au or 08 6304 5618



25 is a “Fini” built for purpose Medical Centre comprising a large waiting room, office space, 2 consulting rooms, minor theatre with change rooms, kitchen, and laundry facilities. 11 car bays.
25 Mills St. was built with the intention of expanding on to 23 Mills Street.
Contact Dr Tony Taylor – 0418 945 047 or thuff.t@bigpond.com for brochure of Plans and further information.

“We chose Humphrey Homes because of their reputation for designing and building to an exceptional standard, in a seamless and integrated journey. Even with that knowledge, they have far exceeded our expectations. We would build with them again tomorrow.”
- Erin and Andrew, Cottesloe
Designing and building a home should be one of life’s great experiences. By integrating architecture, interior design and construction, Humphrey Homes makes the process seamless, efficient, stress-free, and most of all, enjoyable. For an architect-designed home that is perfectly you, built to Humphrey Homes’ award-winning quality, contact Dean Humphrey for an informal chat