STEADYSTATE
How many times has each of us been thermometized in the past two and a half years? Hundreds, no doubt. Maybe you just walked half a mile from your parking spot in baking sunshine and heat, only to be

How many times has each of us been thermometized in the past two and a half years? Hundreds, no doubt. Maybe you just walked half a mile from your parking spot in baking sunshine and heat, only to be
Every picture tells a thousand words, goes the old saying, but the picture above might tell ten thousand. Ah, but which words are they?
Maybe you’re thinking the picture tells the sad tale of a philandering husband who has come home from a business trip or “working overtime,” only to be greeted by evidence that his secret escapades are no longer secret.

Fair enough. That’s an understandable con clusion, but it’s a little behind the times. There is a newer, happier version of this picture.
We could cheat cancer. We could cheat death from cancer. Already, cancer treatment has progressed to the point that it is often a chronic disease rather than an acute one. Kind of like

predictions about COVID’s future, cancer is in many cases something we live with — some times quite amicably — instead of something that kills us. Patients by the hundreds of thou sands are cheating cancers that would have spelled the end for our grandparents, and even our parents.
But there is more. Medical researchers are redefining what it means to cheat cancer out of another victim. The scientific evidence says that instead of battling cancer and hopefully winning, we don’t even have to get cancer in the first place. We can avoid it altogether.
How is this possible? Read on.
greeted by someone with a thermal scanner at the entrance to your destination, possibly your workplace. If you lit up the screen at 102° or 103° you were going to be sent home and quarantined for days. Not good! Instead, you were shocked when the digital thermometer showed 98.6°.
How is that possible?
The credit goes to a small portion of the brain called the hypo thalamus, which is basically our on-board thermostat
We’re going to focus on thermoregulation, but the body must regulate much more than its temperature. There are all kinds of gauges that are constantly checked by the hypothalamus to keep blood sugar levels, electrolytes, water and salt levels, excess flu id from kidneys, and more at levels right where they should be.

The most visible and easily noticed of all of these functions — known collectively as homeostasis, the creation and main tenance of stability and equilibrium — is temperature control. It’s amazing that the body maintains its core temperature within one or two degrees whether a person is literally digging a ditch in 100° weather or skiing in sub-zero conditions.
How does it do it? Read on.


Your 3 year-old daughter has to take liquid medication every day, and it tastes horrible. It’s getting more and more difficult to get her to take it and often leaves both of you in tears. You know how bad it is because you have tasted it yourself. What do you do?

A. Keep fighting with her and make her take it as pre scribed. She has to learn to do unpleasant things in life.
B. Ask her doctor if there is another form of this medicine or another medicine that might be easier for her to take.
C. Don’t make her take it. She is only 3 after all and there is no need to torture her every day.
D. Try to mix the medicine with something else that will mask the taste. Then give her a little reward when she takes it.
A. There are better ways to accomplish this. There might be different medications that will also work. You might be able to find something to mask the taste. You might be able to use small rewards to get her to take it.
B. This is what you should try first. You may be fighting this battle for no real reason.
C. This is the most wrong of the responses. She has been prescribed the medication for a medical reason. Not giving it to her may well amount to child abuse.
D. This could work, but check with the doctor first to see if there’s a different form of the medicine or if there is a reason not to mix it.
The entire concept known as closure isn’t necessarily a myth. It could be said that there’s good closure, and there’s bad closure.
Simply put, closure means experiencing something that marks a clear conclusion to a difficult life event. It’s relat ed to Gestalt psychology or therapy, which comes from a German word meaning form or shape, carrying the suggestion that a circle has been closed; loose ends have been resolved.
The problem with closure as it’s often portrayed and under stood by most of us is that it’s extremely elusive, if not impos sible to attain. Therein lies the bad closure.
What is good closure? If your family has even been the vic tim of a serious crime and the perpetrator is unknown and at



large, that is at best unsettling and at worst absolutely terrify ing. Perhaps someone has been assaulted or even murdered by an unknown assailant. Are they going to come back for more? Are other members of the fami ly going to be attacked?
Closure (good closure, that is) can come when police find and arrest the person they believe to be responsible. That is a clear relief. Or after a trial and conviction, family mem bers will sometimes tell report ers, we have closure now.
Another crime-related exam ple of good versus bad closure might come from a disappear ance. Death is assumed, but a body has not been found. When that happens and the family can bury their loved one, they will often say now they have closure.

And they may be right. An event — something like a funeral or a verdict — has provided a clear endpoint.
The mythical aspect of closure, however, makes itself known well after those clear and definitive moments. It happens when people continue to mourn and grieve, some times for the rest of their lives, over something for which they thought they had “closure.” It could be something like the aforementioned violent or deadly events, but it could just as easily be a break-up or a divorce.
Many psychologists and therapists try to steer their patients away from the concept of closure and instead in the direction of a healthy accep tance of what has happened, be it death, divorce, or some thing else.
It’s actually more healthful to remember the person no longer in your life, to honor their great qualities, what you loved about them and what you learned from them that you continue to apply every day. Instead of “living with loss,” the goal is “living with love,” as one therapist put it, “really allowing the memories of that person to fortify you. that they’re still with you in certain essential ways.”
We all like happy endings. But maybe we need to redefine what makes an ending happy
There are often reasonable alternatives for childhood prob lems. Always explore them before trying other things. Dr. Proefrock is a retired local clinical and forensic child psychologist.
+
Grovetown•706-869-8535


It’s about as easy for the body to maintain its thermal, chemical, and even physical balance as it is for this ele phant to balance his prodi gious weight on a hard ball. But no worries; it’s definietly up to the challenge.

French physiologist Claude Bernard (1813-1878) is consid ered one of the first modern scientists to appreciate the body’s ability to maintain con stancy despite ever-changing external conditions, although knowledge of the concept dates back to ancient Greeks. It was American physiologist Walter Cannon (1871-1945), however, who coined the term homeostasis from Greek root words meaning “similar” and “standing still; not moving.”
The word is often mistaken to mean stagnant or unchanging, but Cannon purposely chose the Greek word for similar rather than the word for same (homo) to express the idea that internal conditions could and would vary — but in normal conditions all but imperceptibly, a degree or two at most.
To compare the brain’s tem perature regulator to a thermo stat is actually an insult to the
hypothalamus. All a thermostat does is detect an out-of-range temperature and turn heat or air on until a set tem perature is reached.
The hypo thalamus, by contrast, is monitor ing a bevy of systems 24/7/365 and employs a number of complex systems to respond. They include a sophisticated array of both chemical and physical adjust ments to constantly balance heat production against heat loss, automatically keeping us at the factory pre-set, 98.6°F.
The first tool in the arsenal of homeostasis most of us would think of is sweat, although in nicer parts of town it’s called perspiration. Sweat sometimes gets a bad rap, but without it we would be in very sore straits indeed. Its evaporation is a major force for cooling.
The hypothalamus also opens and closes little levers in our internal ductwork to
bring circulating blood clos er to the surface of the skin where it can also benefit from the cooling effect of evaporat ing sweat. Conversely, if it’s 10-below outside, the system will close off surface ducts and send our blood circulation deep, away from the cold, cruel world outside. Those strategies explain why we can be red as a beet on a hot summer day and practically cyanotic in bitter cold weather.
It’s all part of what the Greek physician and philos opher Alcmaeon of Croton called “a balance of oppo sites.” Comparing the body to a political system, he wrote “Health is the equality of rights...wet-dry, cold-hot, bitter-sweet; but single rule of either pair is deleterious.” True enough, inequality and im balances of power can lead to unrest in political systems and disease in the body. Around the same time Alcmaeon of Croton wrote his words, the concept of the four humors came to the fore, and their balance was said to be the key to health.

More recently, novelist Tom Robbins wrote words that could well apply to the body’s system of homeostasis: “A truly stable system expects the unexpected, is prepared to be disrupted, waits to be trans formed.”
It certainly can be, but it isn’t necessarily. Nearly everyone experiences heartburn from time to time. The condition has a number of names, and sometimes they help determine if what’s happening is serious or not. Other than heartburn, it’s sometimes called acid indigestion or acid reflux, as well as the ever-popular gastroesophageal reflux.
More and more, however, another descriptor is seen and heard, the abbreviation GERD. It could be said that GERD denotes an escalation. After all, GER is simply the aforemen tioned gastroesophageal reflux. GERD, on the other hand, is gastroesophageal reflux disease. That means something closer to serious and chronic, and it can lead to complications.
Considering that both GER and GERD involve stomach contents coming back up into the esophagus, there is a high likelihood of damage to the esophagus. After all, stomach contents contain stomach acid. It’s powerful stuff, and it’s called acid for a very good reason: it is acid. The stomach is designed to handle gastric juices just fine, but the esophagus, not so much.
So what can be done to prevent gastric reflux? An under standing of your personal heartburn triggers is useful. Avoid ing a problem is always a better option that treating one. Perhaps it’s certain foods, or maybe it’s an issue of quantity. Smaller meals often cut the chances of having reflux. Or it can be a time-of-day thing: some people find that nighttime heartburn doesn’t happen if they don’t eat within 3 or 4 hours of their bedtime.
In terms of treating existing heartburn, antacids like Tums and Rolaids are the simplest way to neutralize acid, and they often provide fast relief. But they aren’t a long-term fix.
The next step up are known as histamine blockers, products like Pepcid, Tagamet and Zantac. Available in prescription and OTC strengths, they generally offer 8 to 12 hours of relief, so they’re more preventive than a source of instant relief.
Anyone who feels the need for something beyond histamine blockers, or who would like to pop them like candy, should probably check in with their doctor. It’s always good to get an expert involved and get a nagging, chronic issue resolved.
AIKEN-AUGUSTA’S MOST SALUBRIOUS NEWSPAPERwww.AugustaRx.com

The Medical Examiner’s mission: to provide information on topics of health and wellness of interest to general readers, to offer information to assist readers in wisely choosing their healthcare providers, and to serve as a central source of salubrious news within every part of the Augusta medical community.

Direct editorial and advertising inquiries to: Daniel R. Pearson, Publisher & Editor E-mail: Dan@AugustaRx.com

AUGUSTA MEDiCAL EXAMINER P.O. Box 397, Augusta, GA 30903-0397 (706) 860-5455 www.AugustaRx.com • E-mail: Dan@AugustaRX.com


The next time you read or hear something about the tremendous progress made in treating cancer, think of this woman, Janet Rowley. There may be people reading this very article who are alive because of her, and the same might be said for people all over the world.
In a nutshell, her work established that cancer is a genetic disease. Not necessarily meaning that you inherit it from your parents or grandparents, but that abnormalities in specific genes can be the cause of specific cancers. Met by skepticism within the research community at first, her ongoing discoveries solidified her initial conclusions and changed the way cancers are treated.
Her early detractors might have reconsidered if they had known a little more about the object of their skepticism. She was not one to be trifled with. Born in New York City in 1925, her parents, both graduates of the University of Chicago, moved back to Chicago when Janet was 2. In 1940 she was granted a scholarship to study in an advance placement program at the University while she finished high school. Staying at UChicago (after having to wait 9 months to enroll because their quota for female students that semester - 3 - had already been reached) she earned a Bachelor of Philosophy degree in 1944, a Bachelor of Science degree in 1946, and a Doctor of Medicine degree in 1948. If you’re doing the math, at that point she was all of 23 years old. Janet Davidson became Janet Rowley the day after graduating from medical school when she married fellow medical student Donald Rowley; the couple went on to have four boys.
Her interests in the connection between chromosomes and cancer arose from a one year sabbatical at Oxford University in 1962. After spending a decade peering into microscopes, a second Oxford sabbatical led to her first big discovery, and it happened at home at the dining room table.

She would take micrographic images of the chromosomes of leukemia patients home to examine, meticulously cutting out pairs of chromosomes and carefully lining them up on the table, ordering her kids not to sneeze.
At that table she became the first scientist to discover that “translocation” was the cause of leukemia and other cancers, thereby proving that cancer is genetic. Specifically, she noted in a patient with acute myeloid leukemia (AML) that a portion of chromosome 21 had broken off and moved to chromosome 8 — and a piece from 8 had moved to 21. Once she noticed this “translocation,” she found it in other AML patients. Then she found a similar translocation between chromosomes 9 and 22 in patients with chronic myelogenous leukemia (CML). Because of these gene transfers, cell growth regulators were out of position and unable to do their jobs, resulting in uncontrolled cell growth. About 5 years later she and her colleagues discovered a third translocation as the cause of yet another form of leukemia. By 1990, more than 70 translocations had been identified and linked to various cancers.
Her discoveries led to the development of effective therapies to counteract the abnormal results stemming from various translocations.
Dr. Rowley died at home in 2013 at age 88 from complications of ovarian cancer.
I am enjoying these cooler days of fall. It is so much easier to get out even if it’s only down the driveway to my mailbox and back. I’m noticing too that the drier air means less huffing and puffing from the exertion. I know that for many, these are laughable statements because you can manage a five-mile run with little challenge to your body. But good health is not a competition! It’s a more solitary me-and-myself set of accomplishments, no matter how long it takes, or how slight the accomplishments might be.
A mere year ago I couldn’t get out of bed, or into it without help. I couldn’t put any weight on my right leg. A broken hip had resulted in a plate holding my hip bone together, and a titanium rod down the length of my femur. The prognosis was grim. They said things to me like you’ll never walk again, you’ll be in a nursing home for the rest of your life, there’s no way you can go home and live independently. I took it all in and some part of me said, you’re all a bunch of stupid morons and you are absolutely, positively out of your minds if you think you’re going to make an invalid out of me!
That all makes walking out to my mailbox at the end of the driveway of my own home where I am living very independently, thank you, so much sweeter! But it is time for me to turn up the heat a bit on my achievement record. Beating the odds has been great, but it’s not enough. What more do I want to accomplish? What is still left for me to achieve? Next year at this time what do I want to be able to do?
Well, there’s driving. If I can walk out to the end of the driveway, I could also walk to a car and get in it. That would expand my universe a lot. It would mean I could drive myself to get a haircut. I could go to
restaurants with pick up at the curb options and cut my costs almost in half from ordering through Door Dash. I could go for a ride on a nice day to see whatever fall colors exist in Georgia. I could order groceries and pick them up myself and again save a substantial amount of money. So many options are out of reach for someone needing others to do things for them. It would be fun to be able to drive to the Y and get into the pool for folks with handicaps and exercise there. With Christmas not all that far off, I’d enjoy being able to go for a drive to see the lights and other decorations. But there are other things I could do that don’t involve driving.

My neighbor asked me this week if I’m getting up and around, even at home. I must confess that I could and probably should challenge myself to get up more often and move around the house more. Why haven’t I done more? Fear of falling has really limited me from doing things I want to do. It is really aggravating to realize that I’m limiting myself from enjoying my life more. But I know how to challenge myself to do more. It’s been a few weeks now since I prayed every time I stood up and used my walker to go out to the mailbox. The move from being terrified to feeling competent is a slow one. And a big part of the battle to improve my health is to recognize when I have surmounted an insurmountable barrier and it’s time to face another obstacle and win the challenge of bypassing that one too.
For the time being it might mean putting on my mask and seeing if I can walk a bit past the end of my driveway, just a bit, not a mile. A couple driveways down would be great. Even at my age, I can always work toward a goal of better health.
Editor’s note: This installment of A Patient’s Perspective appeared in a previous edition of the Medical Examiner.
The best way to support the Medical Examiner is by supporting our advertisers!
When I first started writing this column almost three years ago now, I had counted on having lots of stories to tell about dealing with both my own health issues of middle age and the issues of taking care of aging parents, especially my father who had been diagnosed with Alzheimer’s. I must admit that I had hoped it would be mostly the latter. And I had expected to have both my parents for at least several more years, but as my regular readers know, I lost my father on Labor Day week end in 2021, a little over a year ago. Then, my mother moved out on her own earlier this year, so I wondered what I would write about.
up on Friday. I was nonchalant and ex plained that I hadn’t come on Friday because of the storm but would try to get by that day or the next as I was quite busy with work. Matt seemed uncomfortable about any delay, so I pressed him by saying something to the effect, that low potassium isn’t an emergen cy. He then corrected me and said that it was high potassium and that if the reading was accurate, I had dangerous levels and it could mean something serious that I would need to get treatment for right away.
Dad helped me out with over two years of stories from things that had happened before they moved in with us and things that happened while they lived with us that I shared during and after his life, but as those have been drying out, I was really concerned that there wouldn’t be anything to write about. Fortunately or unfortunately, that hasn’t been a problem, as most of you are aware. Since my father’s passing, I’ve had three surgeries, was mostly dead for a short while, and got my first ambulance ride, in the back anyway. I rode in the front once when my mom was in one. That said, we’ve been slowly getting things fixed in regard to my health and I thought that there was only sunshine on the horizon. Then a routine blood test result threw me for a loop a cou ple of weeks ago.
On my way out of town for a business trip, I stopped at my doctor’s office for a rou tine checkup, including them drawing some blood to check on all of my vital functions. That was on Tuesday afternoon. A couple of days later, I got a call from the nurse who works for my doctor saying that they were concerned about one of the blood test results and needed me to come back to make sure there wasn’t a mistake. I asked what it was, and they said something about my potassi um level. That didn’t sound too worrisome to me and I explained that I wouldn’t be back in town until Friday, but that I would come in for another blood test as soon as I got back. The nurse, Matt, hesitated but I guess he just figured there was nothing we could do until I was back, so he agreed.
I didn’t think too much of it and when I was telling my wife about it on the phone later, I mistakenly said it was low potassium, when in actuality it was high potassium. She did some research and so did I, and the issue didn’t seem too scary. Friday was the day when hurricane/tropical storm Ian was terrorizing Georgia and South Carolina, so I decided I’d just wait until Monday to go back for the additional test. We had not made an appointment for my tests anyway. They said to just show up when I could.
On Monday morning, fairly early, Matt called again, concerned that I had not shown
I said that I had a meeting in about 30 minutes and may be could come after that, but something about what Matt said or how he said it, made me offer to come right away if he thought I should and, much to my surprise and concern, he did prefer me to come right away. So, I made my work apologies about missing the meeting and headed straight for the doctor.
It was quick and easy, as all they needed this time was a single vile of my blood, so I sat in a chair as their vampiric specialist skillfully sucked my blood out into a lit tle vile while I carefully looked the other way and then I was quickly on my way back home. This is where things get a little frustrating. They had pushed me pretty hard to get back as soon as possible, but the so-called emergency blood test took parts of three days to get any results back. In the meantime, imagine me reading every horror story about what high potassium can mean for the body, like kidney failure for exam ple, and worrying about it for days. Finally I got the good news: the second test came back normal. Of course, while I waited to find out, I had every symptom I read about for the earlier, worst-case-scenario diagnosis based on that incorrect test result. It was sort of like the placebo effect in reverse. I was told I might have an issue and on cue I start ed exhibiting the symptoms as if I did.
Even before the results, I was doing my best to be optimistic, but I was expecting for the worst. I was planning on joining a monthly audiobook club, so I’d have some thing to listen to during dialysis treatments.
I looked at some puzzle books to have some thing to do besides browsing the web.
Of course, I was relieved that I wasn’t about to lose my kidneys, but the worry certainly didn’t do me any good. I usually don’t worry too much, but it seems like get ting older is changing that. Next time, I am not going to let it bother me until a bad test result or diagnosis is confirmed by a second test or second opinion. Why grow more gray hairs worrying until we are sure about our diagnosis?
J.B. Collum is a local novelist, hu morist and columnist who wants to be Mark Twain when he grows up. He may be reached at johnbcollum@gmail.com


Wow, what a crazy few years we have had. The roller coaster of current events and market swings has been un precedented. It will be interesting to see what the history books say about 2020 through 2022. No doubt, it will be the years of COVID-19, stock market bust-boom-bust cy cles, and high inflation. As the dust settles, one of the best things you can do as a family is to take an inventory of your financial situation and reflect on the changes. Then come up with a list of actions you can consider taking to improve your financial situation.
That process is actually what financial planners help people with. Consider engaging a financial planner to help you with this process. Often times, we hear that the rea son people never do financial planning is that they do not know what the financial planning process is or covers. The good news is that the CFP Board has established standards that all Certified Financial Planner™ profession als are expected to follow. These standards outline what financial planning is and covers. The CFP board defines financial planning as “the process of determining wheth er and how an individual can meet life goals through the proper management of financial resources.” Plans are customized to the areas of importance for your family.
The following subject areas are typically included in financial plans: financial statement preparation and anal ysis, insurance planning and risk management, employee benefits planning, investment planning, income tax plan ning, retirement planning and estate planning.
Once you identify the subject areas for your plan, a Certified Financial Planner™ can help you work through the planning process. The steps in the planning process are also outlined by the CFP Board. It involves six steps:
1. Establishing/defining the client-planner relationship
2. Gathering client data including goals
3. Analyzing and evaluating the client’s current finan cial status
4. Developing and presenting recommendations and/or alternatives
5. Implementing the recommendations
6. Monitoring the recommendations
The hardest steps are often five and six, but a good financial planner will check in with you on a regular basis to make sure you stay on track. The planning process is ongoing and life events can change the original plan. When that happens, it is important to re-visit the steps in the planning process and update your plan.
This ongoing planning process is the reason most families look to form a long-term relationship with their financial planner. A good planner will clearly explain how they’re paid and why their help is worth the cost to you.
Almost anyone can call themselves a financial planner, so be sure to do your homework and make sure they know what they’re talking about. A good starting place is look ing for a Certified Financial Planner™ that is held to the CFP Board code of ethics & standards of conduct found on www.cfp.net.
by Clayton Quamme, a Certified Financial Planner (CFP®) with AP Wealth Management, LLC (www.apwealth.com).
AP Wealth is a financial planning and investment advisory firm with offices in Augusta, GA.

Back in 80s and 90s, our schools began focusing less on the 3 Rs and more on how student feel about themselves. Medical prac titioners became more cog nizant of mental disorders.
College psychology majors expanded. Pharmaceutical companies developed new pills for everything. Most of them worked. Categories of mental disorders blos somed. Group therapy ses sions became as common as fleas on a junkyard dog.
In all my years of school, not once did a teacher ask me how I felt about something. We dealt with facts and skills. Algebra, geometry, physics, Amer
ican literature, speaking before groups, essay writ ing, arguments and logic, oral debates, home bud gets, checkbook balancing, how to change oil in a car or tractor, marksmanship.
(Yes, we brought guns to school and knew how to use them and had shooting contests. Nobody killed anyone.) I learned wood working. I still have a walnut bowl I turned on a wood lathe. It is functional after half a century, collect ing dust, loose change, and car keys.
Not once did we have to declare our pronouns. I did not know I had a choice.
No one got stressed out over the highly volatile sexual orientation deci sions encountered today. Back then, men were men. Women were women. And men protected women. We were settled with the roles determined by DNA. I have a friend whose grand daughter is a “non-binary
virgin” … whatever that is. Certainly, it is beyond my pay grade. And of course, the 14-year-old child has green hair and is on multi ple anti-depression medica tions. But she is improving. And pretty. Just got a job as a hostess at McDonald’s. It turns out hamburgers do not care about hair color or the state of her hymen. The job has demolished some of her depression and she has a savings account
In my time, men worked hard and saved money, provided for their families, raised children, and had value in the form of prop erty, money, and family values left over for the next generation. It was expected.

Over the years, the Dark Path of Despair has gotten steadily more foot traffic. Financial Pressures and Mental Illness hold hands as they lead us there. Inflation has chewed away at family stability. Depres sion and assorted mental

illnesses abound therein. People’s sense of personal worth decreased. Various studies show that 15-20% of our population is mental ly challenged in some way. That is scary.
Family values are system atically degraded. Rapid ly. Net worth dwindles. Divorce is commonplace. Illegal drug use blossoms. Jails fill up. News headlines scream of late-night shoot ings. Road rage is common.

Mental health is a major and growing problem.
You have all heard that a financial recession is when your neighbor loses his job. A depression (financial and mental) is when you lose your job.
The question reoccurs: Why is there such a strong undercurrent of depression and mentally derangement? No one knows all the an swers, but the instability of our financial foundations and institutions certainly isn’t helping. As our bank account shrinks, our chanc es of mental depress ex pands. Inflation forces you to decide what you want
versus what you need.
Higher taxes, higher in flation, higher food prices, higher gas prices, all make our lives more unstable. Mental illness is potentiat ed by uncertainty. Physical illnesses are sometimes unavoidable. Mental stress makes them worse. They are symbiotic. Together, they may limit life expec tancy.
Frederick Douglass, the famed Civil War era orator and debater of Abe Lincoln, said: “A man’s rights rest in three boxes. The bal lot-box, the jury-box, and the cartridge-box.” I believe him, but I prefer to avoid the cartridge box and the jury box and rely upon the ballot box. And you should, too.
Remember those words come November when you encounter the ballot box. Our mental health and the future of our country rests with your voting booth decision.
Make your decision on policies. Don’t be a person ality voter. Nor a one-issue voter.






 Registered Dietitian Nutritionist, Chef Coach, Author Follow Kim on Facebook: facebook.com/eatingwellwithkimb VANILLA PUDDING TOPPED CLEMENTINE FRUIT SALAD
Registered Dietitian Nutritionist, Chef Coach, Author Follow Kim on Facebook: facebook.com/eatingwellwithkimb VANILLA PUDDING TOPPED CLEMENTINE FRUIT SALAD
This delightful fruit salad makes a refreshing dessert any time of the year.

• 2 (3.5 ounce) containers of fat free vanilla pudding
2 Tbs. orange marmalade
3 Clementine oranges
1 cup grapes
3 bananas
3 Tbs. orange juice
1/2 cup of blueberries
Slice the bananas and toss light ly with the orange juice. Drain the remaining juice from the bananas and place it in a medium bowl. Add the pudding and marmalade to the juice and stir to combine, set aside.
Peel the Clementines and slice each section in half. Combine the bananas, oranges, grapes in a bowl.
Divide the fruit equally into 8 dessert cups and top with pudding mixture.
Yield: 8 servings

Nutrition Breakdown: Calories 90, Fat 0g, Cholesterol 0mg, Sodium 40mg, Carbohydrate 24g, Fiber 2g, Protein 2g.
Percent Daily Value: 2% Vitamin A, 4% Calcium, 30% Vitamin C, 0% Iron
Carbohydrate Choice: 1 ½ Carbo hydrates
Diabetes Exchange Value: 1 Fruit, ½ Other Carbohydrate



“It’s true, he killed him self!” And how many times have you heard the response, “Oh no! I sure didn’t see that one coming!”
What is often left out of these conversations is the fact that alcohol is in the blood of around one-third of all who attempt and com plete a suicidal gesture!
And why is that? It is speculated that alcohol serves several functions for a person who has decided to end his/her life. First, it
helps a person to get the courage to follow through with the thought of dying at one’s own hand, then it helps numb fears, then helps anesthetize the pain of dying, and at times alcohol is chosen as the method of suicide itself by drinking to death via alcohol poisoning (about .50% blood alcohol content) as a way to stop breathing without inflicting the physical pain of cutting wrists or risking a gunshot wound.
In other words, one’s sound judgment becomes im paired which causes inhibi tions to decrease and suicide is then seen as an option to continue living with whatev er pain he/she is feeling at the time. And interestingly, heavy intoxication lends one to choose a more sure meth od of ending life, like using a gun, than suicide without the assistance of alcohol.

Medical experts also feel that heavy intoxication may promote self-inflicted injuries by increasing impulsivity and promoting depressive thoughts and feelings of hopelessness (go to nih.gov and SAMHSA.gov, like I did, to find excellent articles on this subject).

And all of this is not to even venture into the facts of drug overdose deaths, whether intentional or not.
Truly, alcohol and drug abuse is one of the most neglected public health issues of this and every other year and un fortunately, treatment for it is one of the least-funded med ical conditions in our coun try. Nobody really wants to bring it out in the open and COVID has a much more interesting topic these days anyway — at least for the past two and a hald years.
A popular saying about suicide among self help groups is “Suicide is a per manent solution to a tempo rary problem.” And there is probably no other group that expresses the level of un derstanding and forgiveness towards the one who has suffered so intensely as the one who prematurely ended life itself.


Sadly, the family members of one who has taken his/her own life have a more difficult time dealing with the death than if the death was caused by natural causes. They are left with questions and be wilderment, often taking part of the blame themselves for not seeing the signs of sui cide and wondering if they could’ve done something to prevent it. All death is not created equal. What is not understand is that for most people, most of the time, sui cide is not an act of immedi ate impulse. More often than
not the person has decided to end his/her own life at some time in the future and is just waiting for the oppor tune time. It is usually not done in the very depths of despair, either, but often after some signs of improvement is experienced.
Looking at suicide pre vention, the best antidote is to live a really good life… right now. When the founder of Alcoholics Anonymous spoke to audiences about recovery from alcoholism, he rarely if ever mentioned the word alcohol! His theme was about what self-help groups know as restoration to sanity, insanity being known as “do ing the same thing over and over expecting different and better results.”
If you or someone you know and love is not living the good life, do call 988, the National Suicide Prevention Hotline, and confidentially talk to someone who cares before someone says of your friend — or even you — “He did what?!!!”


3626 Walton Way Extension (Walton’s Corner)
706.736.1099
706.736.4401

Postseason baseball is, perhaps surprisingly, an apt moment to think about cancer.
If you’re a baseball fan, one of the most poignant moments of any season is the “Stand Up to Cancer” feature of the All Star Game.
An entire stadium’s worth of people, 50,000 or more, along with all the players and coach es, stand up as one, each hold ing a sign bearing the name of someone they know (or knew) who has had cancer. Virtually every last person has someone they’re standing up for.

It is a graphic annual demonstration of what a dev astating scourge cancer truly is.

But medical researchers say nearly half of all cancers are preventable. Those cases, specifically a little more than 44% of all cancers, would save almost 4.5 million lives if they could be avoided.
That’s the good news. The bad news is that we’re not talking primarily about medical interventions. The prevention is largely on an
individual level. In other words, behavioral factors are the key to making huge progress in the fight against cancer. That means we have to do the work, not our doctors. We can’t smoke a pack a day and be heavy drinkers and be a hundred pounds overweight and expect our doctor to give us a magical pill to undo all our bad habits.

Those three factors (smok ing, heavy alcohol use and a high body mass index) aren’t used randomly: they are the ones most commonly linked to
cancer risk as enumerated in the recent study published in The Lancet.
The conclusion that many cancer cases are preventable isn’t exactly earthshaking news. What is unusual about the Lancet study is the breadth and scope of the research, measuring extensive data from 204 countries. Data was com piled about 23 types of cancer and 34 risk factors which encompassed environmental, occupational, behavioral and metabolic factors. Additional ly, information was evaluated
by age group, gender, loca tion and year to get an even sharper picture of exactly what affected who, and when and where it did so.
With such a wealth of infor mation, the study was able to highlight what is perhaps the fullest and clearest picture of cancer risk factors to date. As one example, lung cancer is just one of 18 cancers linked to smoking.
Researchers involved in the study took great pains to point out that “behavioral” factors being paramount in so many cancer cases might lead some to inaccurate conclusions.
The takeaway might be a moralistic view that people with cancer are getting what they deserve. It’s their own fault. They have no one to blame but themselves. “If we could just get people to have the willpower to do the right thing we could almost cut cancer in half.”
That is miles away from the conclusion reached by study authors. The problems are far deeper and more complex. They are systemic and societal.
If that sounds enabling, con sider the way the world has changed in the past century. Historically, only the wealthy were overweight and could
live a life of indolence and inactivity. The vast majority of people worked long hours at physically demanding jobs. They burned off the calories they ate (many of which came from their own gardens).
Today, at least in developed lands, most people work sed entary jobs, and food prepared by others is often chosen for speed and convenience rather than nutrition. By definition it often is high in salt, a pre servative humans have been using for centuries.
In other parts of the world, poverty is rampant, presenting a host of obstacles to salubri ous living that are beyond the control of any individual or community.
As one of the authors of the study we’re discussing noted, no one is immune from cancer, including people who avoid tobacco and alcohol abuse and have a low BMI.
But the more we know about cancer, the better we can avoid it — or succeed in defeating it if it happens.
And the more we know, the more likely it is that we’ll come home from a visit to an oncologist, or even a stay on a cancer floor in a hospital, and be greeted by a banner like the one on our front page.

irbags are a pretty amazing invention, both in terms of what they do and how blin dingly fast they do it.
They are comprised of a complex system that starts with sophisticated crash sensors that decide whether seat belts offer sufficient protection, and if not, which airbags to deploy.
The deployment itself happens in less than the blink of an eye: 1/20th of a second, give or take a few milliseconds.
In other words, an airbag inflates so rapid ly that its speed as it expands can be as high as 200 mph. It has to be that fast so that it’s sitting there waiting for you to slam into it from the force of the crash a split second earlier.
Airbags might look like pillows, but they are anything but soft and fluffy. Very few things feel soft and fluffy when they hit us at 200 mph. But it’s far better to hit an airbag than a steering wheel, a dashboard, or a windshield.
Safety enhancements provided by airbags, required equipment on US vehicles since 1999, have saved more than 50,000 lives as of 2017, according to the National Highway Traffic Safe ty Administration (NHTSA).
At the same time, airbags have caused inju ries, even deaths. According to NHTSA, more
than 290 deaths were caused by airbag inflation between 1990 (when airbags were optional equipment) and 2008. 90% of the deaths were in older vehicles, and more than 80% of those killed were un belted or improperly restrained.
First generation airbags deployed with greater force than today’s versions, and today’s advanced airbags even modify their deployment pattern if weight sensors detect a small driver or passenger, or a child safety seat.
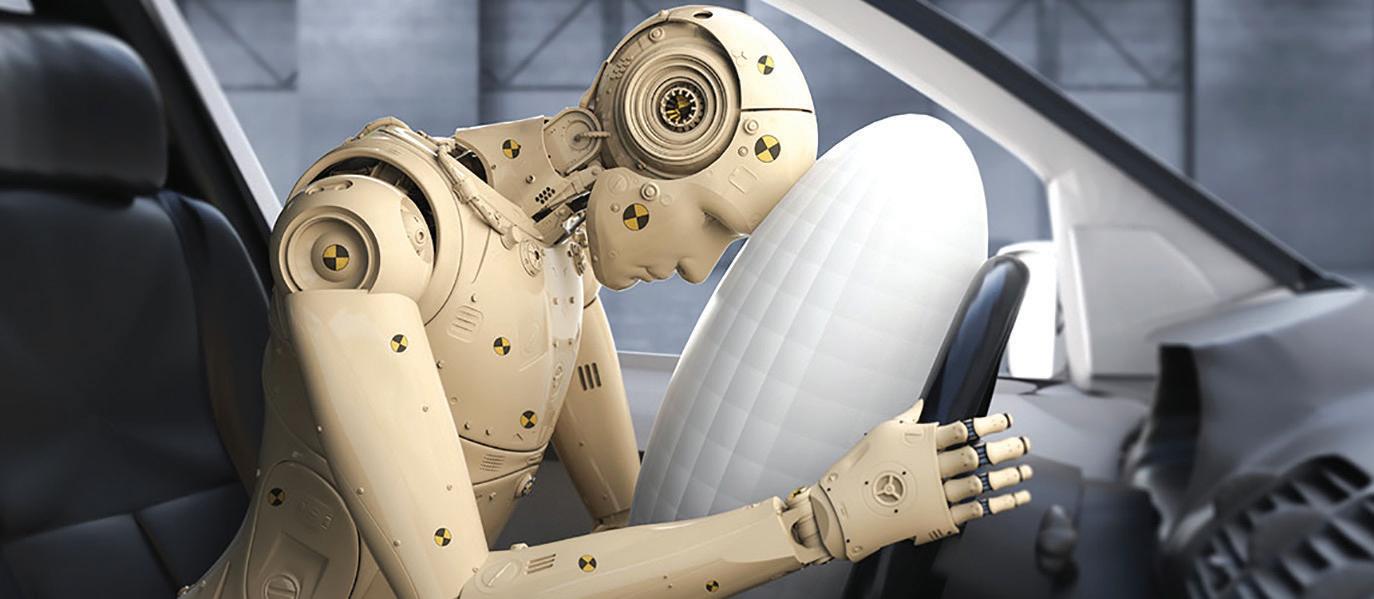
Even so, airbags are known as a supplemen tal restraint system. That means they need to work along with seatbelts for maximum safety and effectiveness.
Because of their super-fast deployment, sitting very close to the steering wheel (which contains an airbag in most vehicles) is also dangerous. 10 inches is the minimum safe distance (including for pregnant drivers).
These are the same reasons kids under 13 are supposed to sit in the back seat and wear seat belts and/or be safely restrained in a car seat of the appropriate size and design for the child’s age and weight.
Airbags are not reusable, so if yours have deployed, they need to be replaced as part of the repairs made. +
The world’s most salubrious mugs, created for us by the artists at Augusta’s Tire City Potters, are here! Win a chance to get one by entering our celebrated Mystery Word Contest!



A recent study in England found that walking just under 10,000 steps a day reduces a person’s risk of developing dementia by 50 percent. Pick up the pace to a “brisk” walk (over 40 steps per minute), and that risk goes down even further. Perhaps most strikingly, the authors found that even a low number of daily steps was associated with a reduced risk of dementia.
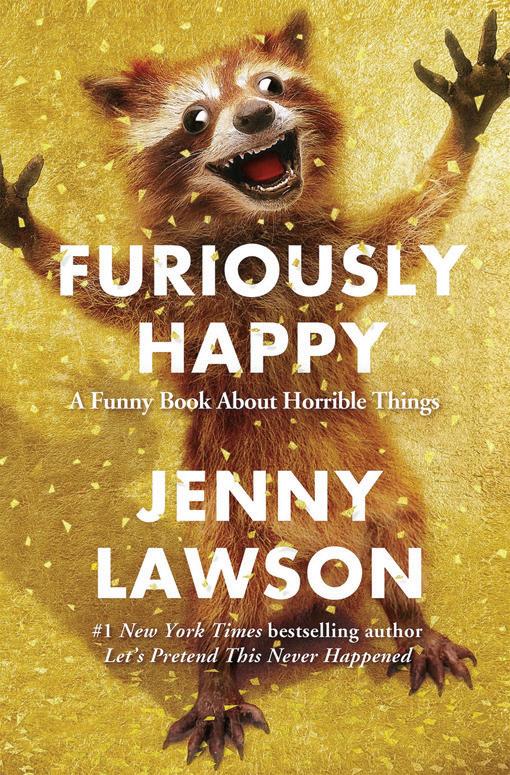
If you noticed the subtitle of this book (“A Funny Book About Horrible Things”) you already understand the contras ts painted by this author.
The walking study is the latest finding in a long line of research that links exercise to our brain health. In fact, some authors have suggested that through a brainhealthy lifestyle, an individual may reduce their lifetime risk by 70 percent. I’ve found that the health interven tions that benefit the brain [are] the most impactful. Get physically active. Mentally stimulated. Socially connected. Lower your blood pressure, your cholesterol, and your blood sugar.
You don’t have to be a brain expert to know that healthy habits lead to healthy living. But it’s nice when a brain expert offers quantifiable reminders. So, here are a few:
Walk. Cardiovascular health has been linked to better brain health. Improving your cardio fitness does not need to be strenuous or difficult. It can be as easy as walking for 30 minutes a day. Check your pulse rate at the end of your walks and track it over a month. See the number fall? That’s a good indication that your heart (and your brain) are benefitting from your efforts.
Eat well. Reducing your sugar, blood pressure, and cho lesterol not only improves heart health but brain health, as well. That’s because high blood sugar levels and high blood pressure cause blood vessels in the brain to affect thinking and memory.
See your doctor. Many physicians are equipped with re sources for our aging population – especially for cognition and brain health. Your primary care physician can pro vide tools and education to guide patients with baseline assessments and screenings. This means your doctor is better informed than ever to help you identify early signs of cognitive decline – and direct you to the help you might need.
Forgetting a name from time to time or misplacing your keys does not mean you are on the road to Alzheimer’s disease. As we get older, it is natural for our brains to get a little slower (if also a little wiser). However, should your cognitive problems get worse over time or interfere with your day-to-day life, it might be time to see a specialist.
Several neurological diseases cause a progressive decline in memory, thinking, reasoning, personality, or behavior. Alzheimer’s, Parkinson’s disease, Lewy body disease, and others all fall under the umbrella term “de mentia.” If you’re over the age of 65, you are at increased risk of developing dementia. In fact, it is estimated that 50 percent of people have changes in the brain that could lead to dementia. That is why taking steps to lower your risk is so important.


Nine thousand eight hundred and twenty-six of them, to be exact.
Ritter is a psychiatristJenny Lawson, you see, is writing about depression and mental illness. If you would like to read a depressing book about depression, this is not the book for you. In fact, if you’d like to read a G-rated book about depression, keep moving right along. Jenny has what some people might call a potty mouth. She has words, and she’s not afraid to use them. But no one can accuse her of not getting her point across.
And it’s a rather important point, since millions of Americans have to deal with chronic depression, severe anxiety, and various mental disorders that range from merely annoying to crippling and life-altering.
It probably tells you all you need to know about Jenny Lawson and this book that her readings are a lot like stand-up comedy. But that doesn’t mean she trivializes
this important subject; it just means she isn’t wallowing in despair or living her life curled up in the fetal position in her closet. Depression is giving her a battle, and she’s fighting right back. And making a lot of fair points for all of us, even people who aren’t battling depression.
Example: have you ever told someone in the throes of depression to “just cheer up” (or words to that effect)? As defined by this book, you have said the equivalent of telling someone who just had their legs amputated to “just walk it off.”
Have you ever told someone who is depressed that they just have “a case of the Mondays”? If so, you’ll get a reminder that mental illnesses are borne of issues a lot more complex than what day of the week it is. Even so, no one should expect to read this book for scientifically-based clinical insights. It might even be slightly comparable to this newspaper: hopefully informative and insightful, but perhaps leaning more in the direction of general knowledge than doctorate level data. And in the case of this book, throw in an almost prescriptionlevel dose of humor and entertainment.
Add it all up, and without discounting the importance of therapy and medication, it offers a light-hearted cheering section for anyone determined to be, despite their depression, furiously happy.
+

Furiously Happy: A Funny Book About Horrible Things by Jenny Lawson; 352 pages, published by Flatiron Books

“My energies will be devoted to your defense, not television commercials.”





 CROSSWORD
EXAMINER CROSSWORD
CROSSWORD
EXAMINER CROSSWORD




A miniature pony walks in a doctors office. “What seems to be the problem?” asks the doctor. “I’m not sure doc,” the pony says, “but I think it’s laryngitis.” After a brief exam the doctor says “You seem to be just fine. You’re just a little hoarse.”
Moe: Why do people say “break a leg” before an audition?
Joe: Because they want to end up in a cast.
George Sink walks into a bar and starts chatting with a lady whose charm is not just her beauty; she also has a foreign accent, which adds to her exotic allure. “I’m from Germany,” she tells George in answer to his in quiry. Things seem to be going rather well, so George asks if he can have her phone number.
“Nein, nein, nein, nein, nein, nein, nein,” she tells him.
Moe: The post office is hiring.
Joe: If service at my house is any indication, they need all the help they can get.
Moe: Wonder what their problem is?
Joe: For one thing, they can’t keep women on the payroll.
Moe: I did not know that. Why?
Joe: Because they don’t want to work in a mail-dominated workplace.
Moe: This economy is supposedly so great, but no matter what I do I can’t find a job.
Joe: Why don’t you apply at Search & Res cue?
Moe: Why them?
Joe: They’re always looking for people.
Moe: Burglars are getting so clever these days.
Joe: What makes you say that?
Moe: Last night my wife woke me up in the middle of the night and whispered, “Darling! There’s a burglar downstairs!!”
So I go down, check every room and don’t find anyone. Then I suddenly realize I don’t have a wife, and when I went back upstairs my wallet, TV and computer were gone.
Moe: How many pushups can Chuck Norris do?
Joe: All of them.
Moe: How many divorced men does it take to change a lighbulb?
Joe: Nobody knows. They never get the house
Moe: I told my doctor I’m a compulsive liar.
Joe: And?
Joe: He didn’t believe me.
Moe: What is a rorschach test?

Joe: Why don’t you just Google it?
Moe: I tried that, but all I got were pictures of me and my wife arguing.
+


Staring at my phone all day has certainly had no Effect on ME!
try as they might,
stare at their
all day.


I truly believe my teenage son is the most stubborn human being on the planet. The other day I told him he would argue black is white and white is black. You know what he said? “I would not!” It doesn’t matter how quick or simple the chore or favor I ask him to do might be, he refuses. I can beg and plead until I’m blue in the face and nothing will make him budge once his mind is made up. What can I do?
This is an extremely important issue, one I am very glad you raised.
A bluish, grayish or purplish tinge to the skin is often most noticeable initially in lips and nailbeds, and while it can be a striking symptom in light-skinned people, it can be easy to miss in dark-skinned people.
What causes cyanosis? Its presence means that oxygen is not being delivered to that area, either at all or in dangerously low quantities. Oxygen is what gives blood its red color, and by extension what gives our skin a pink or reddish tinge. Arteries carry our oxygenated blood, and we’ve all seen our veins just beneath the skin’s surface, clearly blue because they’re carrying oxygen-depleted blood back to the lungs for a fresh supply.
All of that is normal. What isn’t normal is for other parts of the body to turn blue. The cause might be a breathing issue like severe COPD or an airway obstruction, congestive heart failure or some other serious circulatory issue, or (in places not named Augusta GA), hypothermia.
Whatever the cause, it is not something to wonder or guess about, or patiently observe to see if it goes away. Or Google. It is something to get immediate treatment for. Immediate as in call 9-1-1. It’s a great time to apply the “better safe than sorry” rule. Sometimes people think, “I could drive myself to the hospital by the time an ambulance gets here.” Maybe that’s true and maybe it isn’t, but a private vehicle can’t run red lights and most likely doesn’t have an onboard oxygen delivery system and trained medical people carefully attending to the passenger. An ambulance always offers the advantage of treatment beginning well before arrival at the emergency department.
I hope this answers your question.
Do you have a question for The Advice Doctor about life, love, personal relationships, career, raising children, or any other important topic? Send it to News@AugustaRx.com. Replies will be provided only in the Examiner.
Medical Examiner, PO Box 397, Augusta GA 30903- 0397




Dr. Eric Sherrell, DACM, LAC Augusta Acupuncture Clinic 4141 Columbia Road 706-888-0707 www.AcuClinicGA.com
Evans Chiropractic Health Center Dr. William M. Rice 108 SRP Drive, Suite A 706-860-4001 www.evanschiro.net
Resolution Counseling Professionals

3633 Wheeler Rd, Suite 365 Augusta 30909 706-432-6866 www.visitrcp.com

Jason H. Lee, DMD 116 Davis Road Augusta 30907 706-860-4048
Georgia Dermatology & Skin Cancer Center 2283 Wrightsboro Rd. (at Johns Road) Augusta 30904 706-733-3373 www.GaDerm.com


Karen L. Carter, MD 1303 D’Antignac St, Suite 2100 Augusta 30901 706-396-0600 www.augustadevelopmentalspecialists.com
Steppingstones to Recovery 2610 Commons Blvd. Augusta 30909 706-733-1935



Everyday Elder Care LLC Certified


WOODY MERRY www.woodymerry.com Long-Term Care Planning I CAN HELP! (706) 733-3190 • 733-5525 (fax)
Parks Pharmacy 437 Georgia Ave. N. Augusta 29841 803-279-7450 www.parkspharmacy.com
Zena Home Care Personal Care|Skilled Nursing|Companion 706-426-5967 www.zenahomecare.com



Chaudhary,
Rd,
Floss ‘em or lose ‘em!
Steven L. Wilson, DMD Family Dentistry 4059 Columbia Road Martinez 30907 706-863-9445













