

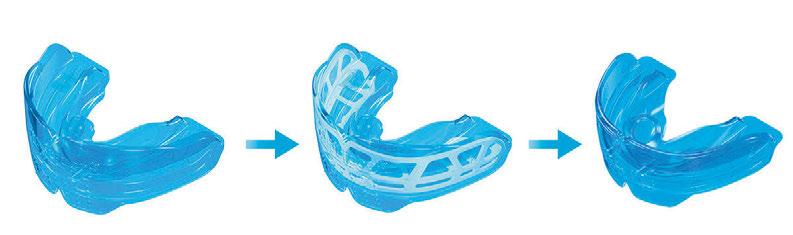
OrthoApnea NOA
A new, uniquely sophisticated mandibular advancement device clinically proven to treat obstructive sleep apnea and snoring.

The custom OrthoApnea NOA features two individual low-profile splints that hold the jaw in a controlled forward position to facilitate breathing and provide a more comfortable experience for the patient.



The flexible, controlled advancement allows for lateral jaw movement while preventing joint discomfort.
Indicated for:
> Patients with mild to moderate OSA
> Patients suffering from intolerance to other treatments
> Patients who snore during sleep
Mandibular advancement is defined by the doctor and performed in a progressive and controlled sequence through a series of lower splints.
greatlakesdentaltech.com

800.828.7626

Sharing is Caring
“If you have an apple and I have an apple and we exchange these apples, then you and I will still each have one apple. But if you have an idea and I have an idea and we exchange these ideas, then each of us will have two ideas.” – George
How many events in your life each day involve helping others understand something new to them? How many times does someone else provide a new thought you’ve not considered before? Read any good books lately? What happened then – you probably told someone else about it.
Readers of DSP, I’d wager, live every day filled with opportunities like these, because we are the curious, generous type. At the most basic level, we sit knee to knee with strangers, soon to become patients, and help them teach us something new – what is it about them that drove them to seek us out? Our expertise flows back to them, and we both have grown in the process. If they don’t have the courage, circumstances, and need to tell us their story, no treatment is possible. If we lack the ability to match deep knowledge with their highest perceived benefit, positive actions won’t be forthcoming.
On the plane today heading to a conference to meet a group of eager learners, I spent time catching up on several sleep journals. So many articles presenting ideas that energized researchers into doing what I could never do: patiently assembling data into useful stories. Editors and reviewers finding needles in haystacks of submitted articles. Curious clinicians supporting the whole effort with dues, subscriptions, and, in some cases, patronage of advertisers. We all have our role to play, our ante into the pot that gives us all a way to add value in meaningful ways.
Bernard ShawOutside of our field, we can’t wait to tell our friends about a new movie, bottle of wine, or fine vinyl record we discovered lately – these actions are part of the human condition, knitting together communities. We hope others find as much value as we did from a book, podcast, or TED talk. Keeping it to ourselves feels disrespectful. How does this help our community get healthier? Imagine if none of these exchanges took place. A common comment when journals are mentioned in my circle of friends goes along the lines of ‘if I only had time….’ Vast knowledge was hidden in the stack of journals I brought onto the plane. I read today about myofunctional therapy – a PubMed chart in the article showed a hockey-stick graph about the number of published essays in the past few years. No clinician can keep up with them all – and that’s just one small bit of our profession!
Steve Carstensen, DDS Diplomate, American Board of Dental Sleep Medicine
No one clinician. But we’re used to sharing, aren’t we? What if we formed a small group of friends and committed to studying one segment of shared interest every quarter? We could agree on who would do what and hold each other accountable for bringing discovered knowledge to all of us. Share the expertise in a small group and everyone benefits.
Start small. Be intentional about one idea to share with someone else every day, and one thing you learned. Then two, then three, then, try to keep up.
Do you like what you are reading in DSP? Do you have ideas you want to share about what works in your practice? As Chief Dental Editor, I am happy to consider essays from any reader! Contact me at stevec@medmarkmedia.com.
Cover Story
Turbinates to Tonsils –Lasers for Airway Therapy
by Dr. Harvey ShiffmanShine a light as your airway treatment choice.

20
BROOMS Screening
by Brittny SciarraMurphy, RDH, BS, MAS, COM, QOM, and Karese Laguerre, RDH, MAS
Who would benefit from OMT? Here’s a screener.
MEDICAL
Continuing Education
Why Every Dentist and Orthodontist Should Have an Orofacial Myofunctional Therapist on Their Team


 by Nicole Goldfarb, M.A., CCC-SLP, COM
by Nicole Goldfarb, M.A., CCC-SLP, COM
Solving problems with new thinking that’s actually been around 100 years.
2 CE CREDITS
Medical Insight
28
Insomnia Medications –Not All Are Created Equal by Colonel Scott Williams, MD, FAASM
A brief description of the types of medications to treat insomnia that may enhance OAT treatment adherence at the initiation of therapy.
30
Medical Insight
Atrial fibrillation and OSA
 by Alan D. Steljes, MD, FACC, FRCPC
by Alan D. Steljes, MD, FACC, FRCPC
OSA is associated with several cardiovascular disorders. Here’s a look at the connection to AFib.

Each drug-free treatment plan is tailored to address the individual patient’s symptoms, and includes the use of several tested technologies, including ultrasound, photobiomodulation, microcurrent, and muscle manipulation.






6 Publisher’s Perspective Human Trafficking: Staying Informed & Safe
by Lisa Moler, Founder/CEO, MedMarkMedia
12 Pediatrics The Missing Link in Pediatric Sleep Breathing Treatments
by Paulo Soares, DDS, MSD How they breathe is as important as whether they breathe.
18 Expert View The Vital Role of Dentists in Managing Orofacial Pain and Sleep Apnea
by Mayoor Patel, DDS, MS, D.ABDSM, and Terry Bennett, DMD, D.ABDSM Clinicians need to consider both, always.
24 Practice Management Three Things You Need for More Physician Referrals
byJon Nierman
Making community connections is the key to grow your practice.
26 Cardio-Sleep Corner Sleep Duration and Cardiovascular Disease Risk
by Lee A. Surkin, MD, FACC, FCCP, FASNC Learn about the effects of sleep deprivation and how sleep duration plays a role in increasing cardiovascular disease risk.
40 Product Debut Personalized, Precision, Oral Appliance Therapy
Don’t think all PDAC Herbsts are alike.
42 Inside the Lab A New Technique for Fabricating a MAD in the Edentulous CPAP-Resistant Patient
by Richard. B. Dunn, DDS, MS, D.ABDSM; Jessica Turner, CDA; and David Walton, CDT More people can be treated when clinicians master new skills.
46 Laser Focus Wake-up Call
by Dr. Anthony Bolamperti Looking for answers for your snoring patients?
49 Practice Management Analyzing the Influence of New 2024 Dental Codes for DSM Services
by Rose Nierman and Courtney Snow Does this mean the end of medical billing?
50 Product Profile Changing Standards in Dental Sleep Care
by Diane Robichaud, Panthera Dental co-founder, Dental Technician Patients and clinicians have no need to settle for less than the best.
52 Clinical Focus A Successful Case of Combination Therapy Using Myofunctional Therapy, an Aligner Sleep Appliance, and Clear Aligners
by Maria Sokolina, DDS, D.ABDSM OSA and orthodontic treatment at the same time.
56 Seek and Sleep DSP Word Search
Fall 2023
Publisher | Lisa Moler lmoler@medmarkmedia.com
Chief Dental Editor
Steve Carstensen, DDS, D.ABDSM stevec@medmarkmedia.com
Chief Medical Editor
Lee A. Surkin, MD, FACC, FCCP, FASNC drsurkin@n3sleep.com
Associate Editor | Lou Shuman, DMD, CAGS lou@medmarkmedia.com
Editorial Advisors
Steven Bender, DDS
Jagdeep Bijwadia, MD (Pulmonary, Sleep)
Kevin Boyd, DDS
Karen Parker Davidson, DHA, MSA, M.Ed., MSN, RN
Bertrand de Silva, MD, FCCP, D.ABSM
Kristie Gatto, MA, CCC-SLP, COM
Amalia Geller, MD (Neurology, Sleep)
William Hang, DDS, MSD
Steve Lamberg, DDS, D.ABDSM
Christopher Lettieri, MD (Pulmonary, Critical Care, Sleep)
Pat McBride, PhD, CCSH
Jyotsna Sahni, MD (Internal Medicine, Sleep)
Ed Sall, MD (ENT, Sleep)
Alan D. Steljes, MD (Cardiology, Sleep)
Laura Sheppard, CDT, TE
DeWitt Wilkerson, DMD
Scott Williams, MD (Psychiatry, Sleep)
Gy Yatros, DMD
National Account Manager Adrienne Good | agood@medmarkmedia.com
Sales Assistant & Client Services
Melissa Minnick | melissa@medmarkmedia.com
Creative Director/Production Manager

Amanda Culver | amanda@medmarkmedia.com
Marketing & Digital Strategy
Amzi Koury | amzi@medmarkmedia.com
eMedia Coordinator
Michelle Britzius | emedia@medmarkmedia.com
Social Media & PR Manager
April Gutierrez | medmarkmedia@medmarkmedia.com
Webmaster
Eileen Kane | webmaster@medmarkmedia.com
MedMark, LLC
15720 N. Greenway-Hayden Loop #9 Scottsdale, AZ 85260 Tel: (480) 621-8955 | Toll-free: (866) 579-9496 www.DentalSleepPractice.com
Subscription Rate: 1 year (4 issues) $149
©MedMark, LLC 2023. All rights reserved. The publisher’s written consent must be obtained before any part of this publication may be reproduced in any form whatsoever, including photocopies and information retrieval systems. While every care has been taken in the preparation of this magazine, the publisher cannot be held responsible for the accuracy of the information printed herein, or in any consequence arising from it. The views expressed herein are those of the author(s) and not necessarily the opinion of either Dental Sleep Practice magazine or the publisher.









Human Trafficking: Staying Informed & Safe
Recently, I saw a movie called “The Sound of Freedom,” the story of Tim Ballard, a federal agent who quits his job with the Department of Homeland Security to start his own independent team to rescue child trafficking victims. One of the movie’s executive producers is Tony Robbins. Anyone who knows my story realizes that Tony has been a mentor and inspiration to me. The movie was emotional and moving for me, watching (as Tony describes on his website), “the harrowing experiences faced by victims of human trafficking and the relentless dedication of those fighting to dismantle these dark criminal networks, which continue to enslave millions of children globally each year.
Lisa Moler Founder/CEO, MedMark Media
Human trafficking is not just a movie. The U.S. Department of Homeland Security (DHS) notes, “Every year, millions of men, women, and children are trafficked worldwide – including right here in the United States. It can happen in any community and victims can be any age, race, gender, or nationality.” Violence, manipulation, false promises of well-paying jobs, and even the promise of romantic relationships can lead to imprisonment of these innocent, frightened victims. DHS adds, “Language barriers, fear of their traffickers, and/or fear of law enforcement frequently keep victims from seeking help, making human trafficking a hidden crime.” What does this story of human trafficking have to do with dentistry? The movie started me thinking about the people, victims at risk, who may be hiding in plain sight. Dental professionals may not realize that patients who visit their offices may be impacted by this terrible crime. Because of signs and symptoms of human trafficking, dentists may be able to help a victim of human trafficking during the course of the dental visit. Several states mandate that dentists need a human trafficking continuing education course to renew their licenses. In these courses, dentists learn details such as:
• Work-settings that may employ trafficking victims.
• Physical and psychological clues that the patient may be being trafficked.
• Some key words that the victim or perpetrator may say to the dentist to avoid being identified as trafficking situation.
• Reasons why a victim may try to avoid being identified.
• Oral injuries that may be discovered during a dental exam that may indicate
a trafficking victim.
• Resources for intervention specialists in human trafficking.
• Steps a clinician can take if the patient is identified as a trafficking victim.
The DHS says that in helping these victims, the healthcare professional also needs to pay careful attention to the safety of themselves and their teams. They warn, “Do not attempt to confront a suspected trafficker directly or alert a victim to any suspicions. It is up to law enforcement to investigate suspected cases of human trafficking.”
Back to Dental Sleep Practice, in our Cover Story, Dr. Shiffman literally takes a laser focus on airway therapy and the benefits of using lasers for patients with sleep-breathing-related issues. In our CE, Certified Orofacial Myologist Nicole Goldfarb explains the advantages of adding an orofacial myofunctional therapist to the practice team. Dr. Lee Surkin delves into “Sleep Duration and Cardiovascular Disease Risk,” and in our Adjunctive Therapy column, Brittny Sciarra Murphy and Karese Laguerre discuss the “BROOMS” screener, a resource to identify oral dysfunction and screen for myofunctional airway issues.
In my Publisher’s Perspective column, I always share topics that are important to my growth not just as a publisher and entrepreneur, but also as a human being. Human trafficking is an outrageous and evil crime. Take a CE class on this topic to know warning signs and also to stay safe. Human trafficking “exists nationwide – in cities, suburbs, and rural towns – and possibly in your own community,” says DHS. Be aware, be smart, and be cautious – as you continue to be a vital and important part of helping patients to survive and thrive.
Eliminate Airborne Threats
Air Quality Guard is a Clean Air System Designed for the Unique Challenges of Dental Practices



Air quality is CRITICAL to your practice. Contaminants are everywhere: Pathogens, Pollutants, Viruses, Bacteria & Fungi all threaten our air quality and quality of care.
Benefits of Air Quality Guard:
• Arm and ceiling intakes capture aerosols at the source and move them away from occupants
• Contaminated air is filtered through a 3 layer system, removing greater than 99.99% of all contaminants
• Reduces the spread of COVID-19 and reduces sick leave
• Negative pressure airflow cycle ensures that contaminants are captured before they can circulate
• Quietly and efficiently filters & replaces up to 100% of air with pure, clean air
• Power ful enough to replace all the air in the room every 7 minutes*
LASERS Turbinates to Tonsils LASERS for Airway Therapy


Patients entering our practice are very likely to have some type of laser as part of their therapy. If they snore, have sleep apnea, have difficulty breathing through their nose, or even if they have enlarged tonsils, instead of “going under the knife” we shine a “light” on the problem. It was not always this way, however.
I’m originally from New York. I graduated from York College with a Bachelor of Science degree with honors in biology; York college is part of the CUNY (City University of New York) system. I attended dental school at Georgetown University School of Dentistry and graduated in 1984. In 1985, I completed a general practice residency program at Georgetown University Medical Center, with a focus on treating medically compromised patients.
After completing my residency program, I relocated to South Florida, and after a year as an associate, opened my first general dental practice in Broward County in 1986. After attending my first sleep course, I treated my first OSA patient in 2008 using a TAP appliance, and realized that I needed more education in the Sleep/airway area. I subsequently
attended training with several different wellknown providers to expand my knowledge base and the use of various types of appliances. Dental sleep became an important part of our practice and has been growing over the years. Seeing the effects of poor sleep quality on our adult and pediatric patients has really been eye opening, and has created in me an ongoing quest for knowledge in this area.
In 2005 after 20 years in a general, insurance-based practice, I relocated to Palm Beach County, Florida. I was searching for a way to reduce insurance dependency and make my patients’ dental experience less frightening and more comfortable. (Dental fear comes typically from the pain of injections and the sound of the drill.) I embraced dental lasers at that time, purchasing a soft tissue diode laser. After 6 months, I realized the limitations of that technology and purchased my first hard and soft tissue laser.
Unfortunately, the manufacturer went out of the dental market shortly after, and I no longer had support. After this expensive experience, my research led me to the Fotona laser company, in existence since the 1960s. I purchased my first Fotona laser in 2007, a

machine that is still in daily use. This longevity is a testament to its durability and design, and we have added new Fotona lasers as the technology has improved – ultimately our new Fotona Lightwalker AT 2023. The Fotona Lightwalker lasers are digital dual wavelength lasers with incredible control over the pulse modalities available.
Our dental practice is entirely laser focused, for sleep and airway, restorative (99% anesthesia free), periodontics, endodontics, surgery, TMD and facial pain, facial rejuvenation, lip plumping, and so much more. All of our patients get exposed to laser technology and its benefits. It has become their norm, and they rarely leave our practice because of this (and is a significant basis for referrals).
In 2011, I was exposed to the Nightlase™ procedure for snoring and sleep apnea by one of its early developers. Early NightLase™ used the Erbium:Yag portion of the Fotona laser only. It contains two laser wavelengths, Erbium:YAG and Neodymium:YAG, each affecting different tissues by their interaction with chromophores. Chromophores are molecules that absorb particular wavelengths of light. For Erbium:Yag, they are water and hydroxyapatite, and for Neodymium:YAG, blood and pigments. Subsequently, I have been responsible for the development of the U.S. training protocols and likewise developed and tested the advancements using both wavelengths and new pulse modalities as they have come available. Current NightLase C3℠ (circumferential) Protocol treats the three major areas of collapse/restriction in Sleep Disordered Breathing.
NightLase C3 was put into clinical use in 2018. It has multiple levels of mechanisms of action, very different from other laser applications for snoring with different laser wavelengths that are promoted by other companies. NightLase C3 has an affect on collagen, causing remodeling and tightening. It stimulates fibroblast cells to produce the proteins that are formed into new collagen through cellular signaling. The pulsing technology is called SMOOTHMODE™ – a burst of Erbium:YAG pulses each shorter than the “thermal relaxation time“ the time necessary for 63% of the heat to dissipate. Carefully controlled pulse duration allows for a deep heating without any ablation (removal) or damage to the tissue surface. This is very different from other wavelengths promoted for snoring reduction. Another result is improved fascial mobility
created by the Neodymium:YAG laser’s affect on hyaluronic acid liquidity/liquification, tongue fat reduction, and slimming using both wavelengths and SMOOTHMODE pulsing. Results include fat cell apoptosis, more airway space, and hyoid bone repositioning by treating the floor of the mouth. All these effects dilate the airway. Recent research has shown positive laser effects on neurotransmitters, muscle tone, and neuromuscular response in Sleep and airway.


Our development of open-ended treatment planning in 2018 allows customized therapy for the variations that we see in severity of disease, response to therapy, and tissue anatomy/habits of our patients. We are also able to use the two laser wavelengths effectively for tongue- and lip-tie releases, which are common in airway disorders. The clinician can reduce nasal snoring caused by inflammation in the turbinates with the photobiomodulation effect of Neodymium:YAG. This wavelength has exceptional effect and penetration depth in these tissues. External nasal valve collapse, another cause of nasal snoring, is reduced non-surgically by stimulating collagen response in the nares. These multiple areas/tissues affected by the Fotona Twinlight Laser make it hugely different in its effect on Sleep Disordered Breathing versus other surgical and ablative laser-based modalities.

Dr. Harvey Shiffman is in general practice at the Boynton Laser Dental and Wellness Center in Boynton Beach, Florida. He is a graduate of Georgetown University School of Dentistry and completed a general practice residency at Georgetown University Medical Center, with an emphasis on treating medically compromised patients. Dr. Shiffman completed certification with the Academy of Laser Dentistry (ALD) in three types of Laser systems and has been awarded a Fellowship in the ALD. He is personally involved in the use and development of cutting-edge technology and has performed tens of thousands of laser dental procedures over the past 20 years. Dr. Shiffman was the developer of the NighLase C3/ Mouthlase/Liplase and Necklase procedures for laser facial rejuvenation and airway, starting in 2012. Most recently, Dr. Shiffman has developed the “Dr. Acula’s Facial, Neck and Hair Regrowth protocols using laser and PRF. Dr. Shiffman received his initial PRF training from Intraspin in 2014, and his injectable training with National Laser Institute. Dr. Shiffman was a contributing author to Dr. Miron’s textbook “PRF in facial Esthetics” in the laser and PRF chapter. Dr. Shiffman’s clinical practice involves the use of lasers and PRF in all aspects of dentisty and facial esthetics. Dr. Shiffman is an instructor for the Academy of Clinical Technology, a Masters status lecturer with the Laser & Health Academy. Dr. Shiffman is an adjunct professor in the Department of Prosthodontics at Nova Southeastern College of Dental Medicine.

Patients report significant improvements in nasal breathing 24 hours a day and improved nasal air flow during cardio-intensive athletics. This has led to the development of the Performlase℠ protocol to take advantage of this phenomenon, currently in development and testing.
In addition, we developed Tonsilase℠, a non-surgical twinlight laser protocol for disinfecting and shrinking inflamed tonsillar tissue and tonsillar crypts. This can be a stand alone or part of a comprehensive treatment plan addressing snoring and Sleep Disordered Breathing in children and adults. This nonsurgical modality, we feel, will significantly affect the need for antibiotics and surgical interventions in appropriate cases.
Because of the non-surgical, non-invasive nature of the NightLase C3 protocol, the results are not permanent and periodic maintenance is necessary. Some patients may need palatal expansion and will need to be evaluated as part of the screening protocols. For some patients, there may possibly be a need for myofunctional therapy in conjunction with NightLase C3.



I am most proud of the non-surgical advancements that I have developed in the laser assisted area of treating Sleep Disordered Breathing that do not negatively affect occlusion, create TMD issues, affect growth and development, cause permanent scarring nor loss of functional tissue, and are safe for both children and adults.
All of our patients are worked up and screened/tested as with any traditional Sleep
Disordered Breathing patients and retested after the base treatment is completed. Previous to the C3 protocol and open-ended treatment planning, we had a percentage of patients in co-therapy with CPAP, but at lower pressures and MADs with less titration. In the last 5 years with the C3 protocol, we have seen a significantly reduced need for co-therapy and can effectively get a high percentage of our patients into a healthy range of AHI comparable to CPAP or MAD.
One of the biggest challenges is the education of our patients and their acceptance of treatment. The general medical community also needs more education about Sleep Disordered Breathing and its effects on multiple organ systems. They can reinforce need for treatment and present treatment alternatives. Another challenge is finding Sleep Specialists that are not DME (durable medical equipment) providers and educating them so that our patients are presented with choices in their therapy.
My personal opinion is that dental and aesthetic lasers such as the Fotona Lightwalker are going to be a huge part of the future of dentistry. Their impact will grow exponentially over time, especially as our population ages and the demand for less invasive and alternative treatments increases.

This future I feel will include a true hard and soft tissue laser in every dental office, along with and benefitting from CBCT imaging, digital scanning, and milling. As dentists, we have a choice to practice exactly as we did upon graduation, or embrace amazing technologies with their abilities to improve outcomes with increased comfort for our patients.
As a laser and dental sleep educator and practicing dentist, my top tips to my students are to thoroughly educate your entire staff and involve them and their families in Sleep HealthCare; screen every patient in your practice, both new and old, regardless of age; and fully understand the effects of Sleep Disordered Breathing on all the organ systems of our body!
Education is king and any dentists that are interested in pursuing laser applications in Sleep and Airway, and all aspects of dentistry, should do their due diligence and research companies’ strengths and weaknesses. They can contact me directly or avail themselves of training programs from the Fotona laser company.
Grow Your Practice with Sleep Medicine and Laser Aesthetics

Available with the Dental Laser


Fotona’s NIGHT LASE ® therapy is a noninvasive, patient-friendly laser treatment for increasing the quality of a patient’s sleep. NIGHT LASE ® can reduce the effects of and decrease the amplitude of snoring by means of a gentle laser treatment of the mucosa tissue.
√ Non-invasive
√ Reduces the effects of snoring
√ Safe and patient-friendly
√ No consumables
We have been providing NightLase® therapy for snoring or sleepdisordered breathing, for our patients for the last 8 years. NightLase® has added another dimension to our practice, giving us the ability to treat patients who may have failed in the use of appliances or just refuse to use them. The added income stream is incredible.

To learn more about the versatile LightWalker Dental Laser, scan this QR code!

The Missing Link in Pediatric Sleep Breathing Treatments
 by Paulo Soares, DDS, MSD (Orthodontics and Dentofacial Orthopedics)
by Paulo Soares, DDS, MSD (Orthodontics and Dentofacial Orthopedics)
Introduction
It is hard to turn a corner these days without hearing about mouth breathing and its effects on overall health. Aided by an increased exposure in pop culture and practitioner knowledge, patient awareness and demand for treatment continues to grow at a rapid pace. In response to this demand, practitioners have concluded that early treatment and prevention is best, but they continue to search for the best ways to help their patients.
While physicians have traditionally treated breathing disorders, dentists and orthodontists are increasingly being called upon to assist in these efforts. Given the close relationship between the upper airway and the oral cavity, dentists play a crucial role in the treatment of breathing disorders,1 which have also been associated with dental conditions, such as caries and periodontal disease.2

Historical Background
Optimum breathing patterns involve the mouth being closed, lips sealed, tongue resting in the palate and gentle nasal breathing. In his 1907 textbook, the father of orthodontics Dr. Edward Angle stated, “Of all the various causes of malocclusion, mouth breathing is the most potent, constant and varied in its results.”3 Angle understood that mouth breathing changed the function of the oral muscles (collectively known as myofunctional disorders), which changed the forces imparted on the teeth and jaws, leading to malocclusion.
Mouth breathing creates dysfunctional forces on the craniofacial complexIn response to this idea, one of Angle’s students, Dr. Alfred Rogers, began implementing a series of oral exercises in the 1930’s to correct this phenomenon, which was the birth of myofunctional therapy in orthodontics.4 As orthodontics became more focused on mechanics over biology, new bracket technology and better ways of straightening teeth dominated the discourse over the 20th century.5
Discovery of Sleep Disordered Breathing in Children
Thanks to a series of discoveries in sleep medicine which occurred in the latter half of the 20th century, scientists began to understand that it is not just adults who suffer from Obstructive Sleep Apnea (OSA), but a new spectrum of breathing disorders called Sleep Disordered Breathing (SDB) became understood to affect children as well.
SDB includes (in order of severity) mouth breathing, snoring, Upper Airway Resistance Syndrome (UARS) and OSA6 and can affect patients from the first days of life. SDB is known to be linked to numerous mental and physical conditions in both children and adults. As with most medical conditions, prevention is better than cure, and this is what the father of sleep medicine Dr. Christian Guilleminault suggested when he advocated for early treatment and stated, “the only valid treatment goal is restoration of nasal breathing.”7
Integration of Dentistry, Orthodontics, and Myofunctional Therapy
The research has led us to understand that there is an interplay of nasal obstructions or restrictions (e.g., allergic rhinitis or adenotonsillar hypertrophy), poor craniofacial development and myofunctional disorders in the development of SDB, especially in non-obese patients. We also understand the cumulative damage imparted by SDB, which means the issue must be treated as soon as it is detected.8
The role of poor craniofacial development and myofunctional disorders in the development of SDB has led to the inclusion of dentistry, orthodontics, and myofunctional therapy in the treatment of breathing disor-
ders (in cooperation with otolaryngology). In fact, the World Dental Federation (FDI) published a policy statement in 2018 urging dentists to be actively involved in treatment, more specifically “prevention of late-onset forms” of SDB.9
Challenges in Current Treatments
Unfortunately, the treatments proposed to address these breathing disorders and the restoration of nasal breathing have caused dissipation of enthusiasm among practitioners and patients. Positive Airway Pressure (PAP) therapy can be used, but it has been found to have adverse effects on facial development, potentially worsening breathing disorders in the long term.10

Orthodontic techniques have also been proposed, but their outcomes are unpredictable, unstable and they may exacerbate myofunctional disorders.11 Surgical interventions are often a last resort due to their complexity, cost, and potential side effects, while research clearly shows that surgery is not the
Paulo Soares, DDS, MSD, is an orthodontist in Brazil. Dr. Soares graduated with his dental degree from the Universidade Federal de Sergipe, Brazil. He is a specialist in Orthodontics and Facial Orthopaedics with more than 15 years of experience in Myofunctional and Airway Orthodontics. Dr. Soares is a Myobrace Certified Provider and Educator. He is also a member of the Brazilian Dental Sleep Medicine Association (ABROS).

only answer.12,13 Parents and practitioners alike are also hesitant to explore surgical options unless absolutely necessary.
Resurgence of Myofunctional Therapy
In recent years, myofunctional therapy has experienced a resurgence as a non-invasive approach to correcting myofunctional disorders, improving SDB and promoting healthy craniofacial growth and development in patients. While the concept is sound, traditional myofunctional therapy suffers from issues of unpredictability, complexity, and lengthy treatment duration. This was the reason it originally fell out of favour, and unfortunately the resurgence has done very little in the way of redesign or updates to this excellent intervention.
Poor patient compliance combined with the lack of a globally recognized and standardized program have hindered its widespread success. To address these challenges, a structured, simple, and cost-effective rehabilitation protocol is necessary to meet the growing demand for treatment. Since our understanding of early treatment has improved, the need to apply this interven-
tion to very young children means that the need to correct these deficiencies is even greater. Even if the treatment is not applicable to 100% of patients, even a modest reduction in the disease burden would still be worthwhile.
The Myofunctional Orthodontic Appliance Protocol
One potential solution that shows promise is the implementation of a myofunctional orthodontic appliance protocol. This approach involves the use of prefabricated myofunctional appliances as part of a simple and structured treatment plan. These appliances serve multiple functions, including promoting nasal breathing, developing dental arches, establishing correct habits, and aligning teeth. By combining non-invasive and cost-effective treatment methods, these appliances provide a way to correct poor habits associated with mouth breathing while improving orthodontic outcomes. Collaboration with medical practitioners is also integrated into the treatment protocols when necessary. Published studies have shown some potential for this technique, and as the openness of the profession to this novel approach improves, more high-quality studies are expected to arise.14
Sequential Stages of Treatment
The myofunctional orthodontic appliance protocol typically consists of administering 3-4 appliances sequentially to progressively rehabilitate the patient. If we reflect on the cascade of events that cause these issues, we understand that mouth breathing precipitates poor oral habits, which alter the patient’s growth and development and finally result in malocclusion.
In response, myofunctional orthodontic appliances address the problem in the order in which it occurs. The initial stage concentrates on correcting breathing and myofunctional disorders, as these habits form the basis of treatment. The second stage focuses on developing dental arches while continuing to address breathing and myofunctional issues. The final stages aim to retain the arch form, align teeth, and assess the stability of habit correction. Each stage corrects a certain

If we reflect on the cascade of events that cause these issues, we understand that mouth breathing precipitates poor oral habits, which alter the patient’s growth and development and finally result in malocclusion.






























































breathing and myofunctional disorders.
problem and sets the foundation for the next condition to be corrected in the cascade.
Benefits of Myofunctional Orthodontic Treatment
The myofunctional orthodontic treatment protocol offers several advantages. The prefabricated nature of the appliances and their advanced features make treatment easy to learn and implement for practitioners. This allows for wider dissemination of the treatment to meet the demand for early intervention and prevention of mouth breathing and myofunctional disorders. Moreover, the simplicity and child-friendly approach of the protocols make it enjoyable for children to participate in habit correction. Accompanying digital and print resources further enhance the effectiveness of the treatment and improve compliance. Treatment delivery is a key part of the myofunctional orthodontic approach. Overall, the myofunctional orthodontic treatment protocol represents an exciting development in the fields of orthodontics,
1. Leibovitz et al. Pediatric sleep-disordered breathing: Role of the dentist. Quintessence Int. 2018;48(8): 639-645.
myofunctional therapy, and dental sleep medicine.
Conclusion
In conclusion, the treatment of pediatric sleep breathing disorders requires a comprehensive and proactive approach. The integration of dentistry, orthodontics, and myofunctional therapy has emerged as a vital part of addressing these issues. The myofunctional orthodontic appliance protocol offers a structured, simple, and cost-effective rehabilitation strategy that can be implemented on a large scale to meet the increasing demand for treatment. By focusing on early intervention and prevention, this protocol aims to restore nasal breathing, correct poor habits, and improve orthodontic outcomes in pediatric patients. While further research and refinement are needed, the myofunctional orthodontic approach holds great promise in bridging the gap in pediatric sleep breathing treatments and ensuring the long-term oral and overall health of children.
For more information on Myofunctional Orthodontics, visit www.myoresearch.com and start with the free online courses.
2. Ballikaya et al. Oral health status of children with mouth breathing due to adenotonsillar hypertrophy. Int J Pediatr Otorhinolaryngol. 2018 Oct;113:11-15.
3. Angle E.H. (1907) Treatment of malocclusion of the teeth: Angle’s System. S.S. White Manufacturing Co., Philadelphia.
4. Rogers A. Evolution, development, and application of myofunctional therapy in orthodontics. Am J Orthod Oral Surg. 1939 Jan;25(1): 1-19.
5. Ackerman J. Was the destiny of orthodontics written in the stars. Am J Orthod Dentofacial Orthop. 2015;147:290-2.
6. Bonuck et al. Sleep-Disordered Breathing in a Population-Based Cohort: Behavioral Outcomes at 4 and 7 Years. Pediatrics. 2012 Apr; 129(4): e857–e865.
7. Guilleminault et al. Sleep-Disordered Breathing, Orofacial Growth, and Prevention of Obstructive Sleep Apnea. Sleep Med Clin. 2019 Mar;14(1):13-20.
8. Alison et al. Recent advances in paediatric sleep disordered breathing. Breathe 2022 18: 220151.
9. World Dental Federation 2018. Dentistry and Sleep-Related Breathing Disorders. Viewed 14 June 2023. <https://www.fdiworlddental.org/dentistry-and-sleep-related-breathing-disorders>
10. Roberts et al. Midfacial and Dental Changes Associated with Nasal Positive Airway Pressure in Children with Obstructive Sleep Apnea and Craniofacial Conditions. J Clin Sleep Med. 2016 Apr 15; 12(4): 469–475.
11. Barbosa et al. Rapid maxillary expansion in pediatric patients with obstructive sleep apnea: an umbrella review. Braz. J. Otorhinolaryngol. 2023 Jun;89 (3): 494-502.
12. Huang et al. Treatment Outcomes of Adenotonsillectomy for Children with Obstructive Sleep Apnea: A Prospective Longitudinal Study. Sleep. 2014 Jan 37: 71-76.
13. Guilleminault et al. A prospective study on the surgical outcomes of children with sleep-disordered breathing. Sleep. 2004 Feb 1;27(1):95-100.
14. Ferreira FG. Novel Approaches for Class II Malocclusion Treatment using Myofunctional Orthodontics Therapy: A Systematic Review. Int J Dentistry Oral Sci. 2017. 4(7), 503-507.
The simplicity and child-friendly approach of the protocols make it enjoyable for children to participate in habit correction.
Success in Sleep Through the Power of Teamwork

Join DreamSleep – a nationwide network of dentists & physicians fighting sleep apnea. Our Whole Patient Program is a comprehensive plan that empowers dental practices with the knowledge, resources, and tools in order to provide patients with the highest standard of care for dental sleep medicine. The Whole Patient Program consists of four principles: Raise public awareness of Obstructive Sleep Apnea, DMSD, TMD, migraine and associated symptoms; train dentists to work with physicians and implement medical treatments; create screening and therapy programs for the industry; and connect patients with providers.
Through state of the art, individualized training and implementation processes, we help you seamlessly integrate these medical treatments into your dental practice to increase your patients’ quality of life and add a valuable revenue stream. Call 844.363.7533 today for details.
Comprehensive education you and your whole team: •Online, on-demand academic certification
•Individualized training programs
• In-office clinical training
•Team Coaching •Screening
The Vital Role of Dentists in Managing Orofacial Pain and Sleep Apnea
by Mayoor Patel, DDS, MS, D.ABDSM, and Terry Bennett, DMD, D.ABDSMAs dental professionals, we are well aware of the impact oral health has on our patients’ overall well-being. However, it is essential to recognize that oral health extends beyond the boundaries of a healthy smile. Growing research has shed light on the intricate relationship between pain and sleep, revealing a compelling connection that demands our attention in the realm of dentistry.
Chronic orofacial pain – such as temporomandibular joint disorder (TMD) and bruxism – can significantly disrupt sleep patterns, leading to reduced quality of life for our patients. On top of that, chronic pain conditions, such as TMD, can manifest as headaches, facial pain, and discomfort in the jaw joint and surrounding muscles.
Similarly, inadequate sleep has been associated with an increased risk of various oral health conditions. By integrating dental sleep medicine into our dental practices, we can identify and address sleep disorders that may be impacting our patients’ oral and overall health. Sleep apnea, for example, is a prevalent condition that can pose significant risk to systemic health.
By integrating pain management and sleep evaluation into our practices, we can provide comprehensive care that not only targets oral health but also
Mayoor Patel, DDS, MS, D.ABDSM, DABOP, DABCP, DABCDSM, DAIPM, RPSGT, FAAOP, FICCMO, FAACP, FAGD, FPFA, received his dental degree from the University of Tennessee in 1994 and then went on to complete a one-year residency in Advanced Education in General Dentistry. He also earned a Masters in Science from Tufts University in 2011. Dr. Patel served as an Adjunct Clinical Instructor at the Craniofacial Pain Center at Tufts Dental School from 2011-2014 and presently again. Dr. Patel has taken over 2,200 hours of postgraduate education courses in the areas of Sleep Medicine, Craniofacial Pain, Sleep Disorders, and Orthodontics. Since 2003, he has limited his practice, Craniofacial Pain & Dental Sleep Medicine Center of Georgia, to the treatment of TMJ Disorders, Headaches, Facial Pain, Sleep Apnea, and Snoring. Dr. Patel lectures nationally and internationally to the dental and medical communities.
Terry Bennett, DMD, DABCP, D.ABDSM, has had more than 40 years of experience in private dental practice. Dr. Bennett graduated from the University of Louisville School of Dentistry with his dental degree in 1977. For the past three decades, Dr. Bennett has limited his practice, The Tulsa Orofacial Pain & Sleep Disorders Clinic, to the conservative treatment of temporomandibular joint dysfunction (TMD) and sleep apnea. Dr. Bennett has been active in the American Academy of Craniofacial Pain having served on the board of directors for more than a decade. Dr. Bennett currently divides his time between his private practice and lecturing for dental schools and organizations across the country.
addresses the overall health and well-being of our patients. But expanding our practices to include craniofacial pain and dental sleep medicine services can also extend beyond improving our patients’ health and well-being. It can help us too.
Differentiate Your Practice
Incorporating the management of orofacial pain and sleep apnea into dental practices can help attract new patients and differentiate the practice from competitors. Many individuals suffering from these conditions may not be aware that dentists can play a significant role in their treatment. By offering these specialized services, dentists can expand their patient base and provide value-added services that set their practice apart.
It is important to note that dentists should pursue additional education, training, and certification in the management of orofacial pain and sleep apnea to ensure they have the expertise and skills to provide optimal care.
Less Impact on Medical Resources
Dentists who help manage patients’ orofacial pain and sleep apnea can also experience a host of other benefits. For one, you get to see patients experience an improvement in their pain. In turn, that can restore their well-being because they no longer have to suffer from pain or miss out on sleep. Additionally, there is less impact on medical resources for chronic pain sufferers. We know that those who suffer from chronic pain continue to seek out resources and relief through health care services. But with dentists screening and treating orofacial pain, there will be less use of medical resources such as seeing a doctor for medications that don’t work or multiple imaging tools.
Now is the time to take charge of your dental practice to offer further resources for patients with orofacial pain or sleep apnea. It will not only help your patients, but your practice too.
Want to learn more, please join our mini residency at Tufts: http://bit.ly/439e0Lm


BROOMS Screening
by Brittny Sciarra Murphy, RDH, BS, MAS, COM, QOM, and Karese Laguerre, RDH, MASIntroduction
Don’t ignore the elephant in the mouth. Well the elephant trunk that’s in the mouth. More commonly known as the tongue, this essential organ aids us in respiration, digestion, speech and swallowing. Yet very few acknowledge the essential influence this muscular hydrostat has on oropharyngeal space during respiration. Each muscle intertwines and relies on each other for alternate movements that enable the tongue to bend, twist, cup, hump, retract, etc.
Any change or dysfunction in these hydraulics encourages compensatory muscle function of the lips, cheeks, soft palate, and/or pharynx. Dental sleep medicine can use these hydraulics to their advantage with the assistance of myofunctional therapy. Imagine taming an elephant trunk with a bit of plastic. Numerous challenges present including but not limited to controlling each muscle, taming an anxious animal, and retention. Not unlike fitting and titrating an oral appliance within a mouth of dysfunction on a skeptical patient with a strong gag reflex.
The ability to identify oral dysfunction is vital to case success in a dental sleep practice. Dental schedules often leave little room for new processes. Easy to integrate, the B.R.O.O.M.S. screener is a quick resource for clinical use. Efficiently observe strong indicators during oral cancer screening and extraoral examination. Two or more noted in the first column requires referral for orofacial myofunctional assessment and evaluation.
Screening with BROOMS
Bruxism/Occlusal Wear

How often do patients come in with pain or tenderness in the masticatory muscles? How often do patients complain of tooth pain, but upon oral and radiographic evaluation, there are no significant findings? Have you considered the possibility of it being referred pain due to bruxism? Occlusal wear is a common finding in clinical practice. Our trained response is recommending a traditional night guard. While some of us still make this recommendation, we are here to argue that. We believe in an airway first model. It is critical to rule out airway obstruction or issue before recommending a night guard. Many airway focused dental providers no longer utilize traditional night guards in their armamentarium. According to sleep medicine specialist Jerald Simmons, MD and sleep
dental specialist Ronald Prehn, DDS, “when most patients exhibit obstructive respirations during sleep the mandible falls back bringing the back of the tongue with it. This triggers a series of events that in some people results in a reflexive attempt to open up the airway by increasing masseter tone. This brings the mandible forward and in many patients improves respirations. We postulate that nocturnal bruxism is a compensatory mechanism of the upper airway to help overcome upper airway obstruction by activation of the clenching muscles which results in bringing the mandible, and therefore the tongue, forward.”2
Myofunctional therapy can aid in the patency of the upper airway. According to Guimarães et al, 2018 “oropharyngeal exercises significantly reduce OSAS (obstructive sleep apnea syndrome) severity and symptoms and represent a promising treatment for moderate OSAS.”3 A clinical study conducted by Messina et al., 2017 documents the benefits of myofunctional therapy on bruxism. This study showed that myofunctional therapy can be “an effective therapeutic strategy in regard to the treatment of muscle facial pain and hypertonia of the chewing and swallowing muscles. All treated patients had a reduction of facial pain and reduced the number of bruxism episodes per hour, and in many cases such episode disappeared.”4 Another indication to look for intra-orally is the presence of maxillary or mandibular tori. According to research, tori are associated with presence of abnormal tooth wear due to the abnormal pressure on the teeth.5
Respiration
Have you ever considered your patient’s mode of breathing and how that can impact their dental health and overall health? This is something that can be easily done through simple observation. We welcome our patients from the waiting room. Prior to calling their name,
SomnoMed makes it EASY to Treat More OSA Patients More Effectively





























































As a SomnoMed preferred dentist you have exclusive access to our robust OAT patient pipeline through the restASSURED® patient diagnostic and treatment portal.






















Physicians in the SomnoMed Medical Initiative are using restASSURED® to easily screen, test and match patients with SomnoMed preferred dentists to treat their patients with oral appliance therapy. We also launched a direct-to-consumer campaign to funnel those at risk into a simple pathway to treatment through the restASSURED® portal. Patients prescribed OAT are sent to SomnoMed preferred dentists.
And, our partnership with Nexus assures optimal, predictable insurance participation for you, your patients, and their physicians.

Treat
SomnoMed + RestAssured + Nexus: It’s the perfect fit.




watch them in their natural state. Are they breathing through their nose or their mouth? You can even take time to observe this while they are sitting in the dental chair. Where is the primary movement of breathing coming from, their chest or their diaphragm? Are they breathing shallow? Is their breathing audible? Mouth breathing can negatively impact the development of the craniofacial respiratory complex, a term coined by Kevin Boyd, DDS. Mouth breathing can also impact the retention of orthodontic treatment. According to Zhao et al., 2021, mouth breathing affected facial skeletal development and malocclusion in children. “The mandible and maxilla rotated backward and downward, and the occlusal plane was steep. In addition, mouth breathing presented a tendency of labial inclination of the upper anterior teeth.”6
In 1907, Dr. Alfred Rogers published Malocclusion of the Teeth, where he recognized the influence of mouth breathing on oral rest posture and successful orthodontic treatment.7 Optimal oral rest posture includes the entire tongue resting in the roof of the mouth, lips closed, and dominant nasal breathing. This posture should be dominantly maintained during the day and night. Optimizing oral rest posture is the ulti-
Brittny Sciarra Murphy, RDH, BS, MAS™, COM®, QOM®, is a registered dental hygienist; myofunctional therapist; Buteyko Breathing educator; author; and key opinion leader in myofunctional therapy, sleep, and functional breathing. Brittny is the founder of CT Orofacial Myology and cofounder of MyoAir, both practices focus on preventing and treating the causes of orofacial myofunctional disorders, getting to the root of the problem instead of merely treating the symptoms. Brittny is an educator for Airway Health Solutions and Dental Sleep Toolbox. She is also the face behind the podcast, “I Spy with My Myo Eye.”

Karese Laguerre, RDH, MAS™, is a registered dental hygienist and myofunctional therapist. She founded The Myo Spot, a practice aimed at amplifying oral wellness to whole body wellness. Through tele-therapy, she helps clients of all ages overcome tongue ties, TMJ disorders, sleep apnea, grinding, anxiety, and various breathing and orofacial dysfunction. Passionate about education and self-help, she published Accomplished: How to Sleep Better, Eliminate Burnout and Execute Goals. When not working with clients globally, she spends time with her husband and four kids.

mate goal of a myofunctional therapy program, and therefore, should always be included in a patient’s treatment whose dominant mode of breathing is orally. As dental clinicians, we are aware of the harmful effects of mouth breathing on the progression of periodontal disease and increased caries risk. We must keep in mind the oral systemic connection, our mouth is the gateway to the rest of our body.

Orally Defensive
If you have ever reviewed your schedule for the day and begin dreading taking that full mouth series on the patient with a severe gag reflex, you are familiar with oral defensiveness. It is that familiar battle between your hands and their lips when the patient has so much tension in their orofacial muscles that it hinders visualization of their teeth as you fight to retract. What about the patient whose tongue is everywhere your instrument goes? I remember when I was practicing clinically, there were some patients I had to stand up for to get enough traction to pull down their lower lip and scale the mandibular anterior dentition. Why are these patients so orally defensive? What if we told you that a gag reflex can be a protective mechanism for one’s airway? Each situation depicted above can suggest symptoms of orofacial dysfunction and signal further investigation with a comprehensive orofacial myofunctional evaluation.
Lingual control and optimal lingual function play a crucial role in optimal craniofacial growth and development, mastication, swallowing, speaking, and keeping the upper airway open during sleep. Myofunctional therapy includes exercises to strengthen the tongue and orofacial muscles. Oropharyngeal exercises effectively modify tongue tone.8
Open Mouth Posture
Also in the waiting room breathing can be observed. Examine whether their mouth posture is open or closed by noting if their lips are together or apart. Continue observing throughout the entire recare appointment. Any time the patient is not actively talking, take silent note of how they are posturing their lips and tongue at rest. Additionally, dried or cracked lips may be observed. This is indicative of open mouth posture or a mouth breathing habit. Some patients may even apply chapstick while they are in your dental chair. Ask them if that’s a pretty common occurrence. Should you notice any asymmetries in their lips, be aware that a flaccid, inverted or rolled out, lower lip
can suggest an open mouth posture or mouth breathing habit as well.
What is the root cause of this open mouth posture? We should rule out airway obstruction. A myofunctional evaluation along with a CBCT or referral to an ENT is a good starting point. It is imperative to work collaboratively with an otolaryngologist, or ENT, to evaluate for nasal patency. Airway impatency can be due to allergies, enlarged tonsils and/or adenoids, nasal polyps, enlarged nasal turbinates, deviated septum, or tethered oral tissues. As a result of the open mouth posture, it is not unlikely to find low tongue posture, a reverse or tongue thrust swallowing pattern, and/or malocclusion.
Maxillary Transverse Width
We were created to have a full dentition, thirty-two teeth. This means there should be enough room for all teeth to erupt. How many patients a day do you see with a complete dentition, that is third molars included? More often, we see patients present with some form of dental crowding or malocclusion.
Measuring maxillary transverse width can be done with the simple use of a cotton roll. Dr. James A. McNamara gives us the range of 36 to 39mm indicating a maxillary arch that can accommodate a dentition without crowding or spacing.9 We are measuring from tooth #3 to #14 on the maxillary arch. First, take a cotton roll and measure it with your periodontal probe. Cotton rolls are generally about 36-37mm. Second, hold the cotton roll up between tooth #3 and #14. Is the cotton roll getting squished or is there ample space?
When I explain this to patients, I take out my skull that is color coded and I show them their maxilla. I then ask them what else does this bone make up? Typically, their answer will be the nose. I even ask this question to children. When discussing the importance of nasal breathing and sufficient transverse develop-
ADJUNCTIVEtherapy
ment, we must remember that the maxilla is the floor of the nose and the lateral walls of the nasal cavity. When the maxilla develops narrow, we typically see insufficient oropharyngeal space. When assessing craniofacial develop, or the lack of, we must not ignore tongue rest posture. Where the tongue rests matters. According to Dr. Ben Miraglia, “the tongue should fit in the roof of your mouth, like your car fits in your garage”. Often times we hear, “my tongue is just too big for my mouth.” There is a book written by Dr. Felix Laio, Six-Foot Tiger, Three-Foot Cage, that presents the mouth as too small for the tongue.
In utero, the tongue begins to shape the structure of our jaws and nasal airway. The tongue aids in the architecture of our jaw by pushing the palate laterally and anteriorly. It is the counterbalancing forces that allow our arches to reach their fullest potential and develop proper bone growth.
Strained Mentalis:
Patients with true lip incompetence will exhibit mentalis strain. Mentalis strain presents as dimpling over the mentalis muscle. An overdeveloped mentalis muscle may be the result of insufficient craniofacial development. You will see overactivation of the mentalis muscle present in patients with increased vertical growth. Those are your patients with gummy smiles. A retrognathic mandible or extreme overjet may also cause the mentalis to be strained due to the compensatory pattern to keep the lips closed.
Conclusion
We strongly encourage you to begin using the ‘BROOMS’ screener in your practice. It would be beneficial to not only your patients overall health and efficacy of their oral appliance therapy, but your practice growth and retention to stop ignoring the elephant in the mouth.
1. KIER, WILLIAM M., and KATHLEEN K. SMITH. “Tongues, Tentacles and Trunks: The Biomechanics of Movement in Muscular-Hydrostats.” Zoological Journal of the Linnean Society, vol. 83, no. 4, 1985, pp. 307–324., https://doi.org/10.1111/j.1096-3642.1985.tb01178.x. Accessed 2022.
2. Simmons J, Prehn R. Nocturnal Bruxism as a Protective Mechanism against Obstructive Breathing during Sleep. Accessed December 19, 2021. https://csma.clinic/Bruxism_Poster.pdf
3. Guimaraes KC, Drager LF, Genta PR, Marcondes BF, Lorenzi-Filho G. Effects of Oropharyngeal Exercises on Patients with Moderate Obstructive Sleep Apnea Syndrome. American Journal of respiratory and Critical Care Medicine. https://www.atsjournals.org/doi/10.1164/rccm.200806-981OC. Published February 19, 2009. Accessed December 19, 2021.
4. Messina, G., Martines, F., Thomas, E., Salvago, P., Menchini Fabris, G., Poli, L. and Iovane, A., 2021. Treatment of chronic pain associated with bruxism through Myofunctional therapy. [online] NCBI. Available at: <https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5656808/> [Accessed 19 December 2021].
5. Bertazzo-Silveira, E., Stuginski-Barbosa, J., Luís Porporatti, A. and Dick, B., 2017. Association between signs and symptoms of bruxism and presence of tori: a systematic review. [online] Research Gate. Available at: <https://www.researchgate.net/publication/313834203_ Association_between_signs_and_symptoms_of_bruxism_and_presence_of_tori_a_systematic_review> [Accessed 19 December 2021]
6. Zhao Z, Zheng L, Huang X, Li C, Liu J, Hu Y. Effects of mouth breathing on facial skeletal development in children: A systematic review and meta-analysis - BMC Oral Health. BioMed Central. https://bmcoralhealth.biomedcentral.com/articles/10.1186/s12903-021-01458-7. Published March 10, 2021. Accessed December 19, 2021.
7. Angle Orthod (1973) Effect of Mouth Breathing on Dental Occlusion 43 (2): 201–206.
8. Villa MP;Evangelisti M;Martella S;Barreto M;Del Pozzo M; Can myofunctional therapy increase tongue tone and reduce symptoms in children with sleep-disordered breathing? Sleep & breathing = Schlaf & Atmung. https://pubmed.ncbi.nlm.nih.gov/28315149/. Published March 18, 2017. Accessed December 19, 2021.
9. McNamara JA. Maxillary transverse deficiency. Am J Orthod Dentofac Orthop. 2000;117(5):567-570. http://www.dent.umich.edu/sites/default/files/departments/opd/160.pdf.
Oral defensiveness is the battle between your hands and their lips...
Three Things You Need for More Physician Referrals
by Jon NiermanHave you been eagerly offering your patients oral appliance therapy, only to be disheartened when their physicians are not on board? This is one of the most common frustrations among sleep dentists, but the good news is you can take steps to establish great physician partnerships.
Become a Trusted Authority
Becoming recognized as an authority in your field can lead to numerous benefits, such as increased credibility, opportunities, and personal fulfillment. However, becoming an authority in dental sleep medicine (DSM) is not something that happens overnight. It requires dedication, time, and energy. Nonetheless, several tips can help speed up the process, including:

• Pursue dental sleep medicine continuing education and credentialing through reputable organizations.
• Network with colleagues who specialize in airway-related fields. Having expert connections can provide invaluable knowledge and help raise your own status as a sleep practitioner.
• Create a separate brand for your DSM practice, complete with a new logo, tagline, business cards, and website.
• Develop educational content for your website, social media, and publications
As President of Nierman Practice Management, Jon Nierman specializes in the development of continuing education programs, software systems, and medical billing services to facilitate dental practice growth for medically necessary services. Jon’s mission is to remove the barriers and make it easier for dental practices to implement airway and orofacial pain treatment. Under Jon, Nierman Practice Management has provided over 5,000 hours of continuing education featuring an internationally renowned faculty. Jon is a graduate of the Georgia Institute of Technology, a brazilian jiu-jitsu brown belt, and a classical/jazz pianist.
to showcase your expertise and build your reputation.
• Enroll as a Medicare DME supplier. This allows you to bill Medicare for oral appliances for OSA. Pro tip: you can enroll in a way you don’t have to accept Medicare’s allowed amount as payment in full.
Identify & Communicate with Physicians

Collect a list of your sleep patients’ other healthcare providers during intake. You can easily accomplish this by using an online questionnaire form in your dental sleep software, such as DentalWriter Plus+.
Distribute narrative SOAP reports and progress reports to all doctors involved in the patient’s care including sleep physicians, primary care, ENT, and cardiologist, among others. By keeping all healthcare providers informed, including successful outcomes, you’ll establish yourself as a reliable and valuable resource in the field of DSM.
According to Steve Lamberg, DDS, sending narrative reports to physicians was his number one tool for practice growth. Dr. Steve Greenman concurs, highlighting that SOAP reports generated and shared from the questionnaire and examination have facilitated a co-referring database with 250 physicians. “Just today we got four new referrals and continue to get an influx of patients who need our help”, says Dr. Greenman.
Medical Billing Enhances Referrals
Dentists who bill medical insurance, including Medicare, are often the preferred choice for referring physicians. Ensure that they are aware you are well-equipped to handle medical insurance billing.
Do these three things, and over time you’ll see your dental sleep practice flourish with referrals.

Sleep Duration and Cardiovascular Disease Risk
by Lee A. Surkin, MD, FACC, FCCP, FASNC, FAASMWe are all aware of the fact that sleep is of great importance for our overall health and well-being. But, did you know that sleep and heart disease are closely connected? Probably not. Hence, if you want to learn more about the effects of sleep deprivation and how sleep duration plays a huge role in increasing cardiovascular disease risk, continue reading below.
Sleep Duration and Heart Health
According to studies (Laksono et al., 2022), poor sleep quality or short sleep duration is linked to increased cholesterol levels, high blood pressure, and atherosclerosis. Plus, chronic short sleep increases the risk of cardiovascular events. The effects of sleep deprivation also include weight gain, diabetes, inflammation, stroke, heart attack, and death.
Sleep Duration and Mortality
Researchers conducted a study on mortality data from almost 7,000 adults over nine years (Bradley, T. D., & Floras, J. S., 2009). The results showed that the mortality rate from ischemic heart disease, cancer, and

stroke was lower in those getting 7-8 hours of sleep each night. In addition, the death rate was higher by 1.7 times in men getting less than 6 or more than 9 hours of sleep per night. Subsequent studies have confirmed this data.
Sleep Duration and Cardiovascular Disease
A review of 15 separate studies (Nagai, M., Hoshide, S., & Kario, K., 2010) on the effects of sleep deprivation on cardiovascular events that included almost 475,000 participants with a follow-up done for 7 to 25 years showed that a little bit over 16,000 events occurred during this period. These cardiovascular events included 8,420 for total
cardiovascular disease, 4,169 for coronary heart disease, and 3,478 for stroke.
The analysis pointed out that those getting less than 5-6 hours of sleep per night were at a 48% higher risk of coronary heart disease-related mortality or developing the disease. Additionally, those getting 8-9, or more, hours of sleep were at a 38% higher risk.
When it comes to sleep duration and stroke, the review found that those not getting enough hours of sleep (<5-6 hours) were at a 15% higher risk of stroke. And those who overslept, i.e., slept for more than 8-9 hours had a 65% increased risk for stroke.
Sleep Duration and Coronary Artery Calcification
One of the main predictors of future coronary heart disease incidence is coronary artery calcification. A study of 500 participants with a follow-up done for five years found a strong connection between coronary artery calcification and reduced sleep duration (King et al., 2008). Furthermore, it showed that the risk of calcification may be reduced by a whopping 33% by simply increasing sleep duration by one more hour.
Sleep Duration and Hypertension
Last but not least, sleep duration and hypertension are also closely connected. One study tested the hypothesis that poor sleep increases the incidence of hypertension by conducting a longitudinal study of 4,800
participants (Gangwisch, J.E., et al., 2006). The results showed that a higher percentage of younger individuals who got less than 7 hours of sleep were diagnosed with hypertension in the follow-up period of 8-10 years. Conversely, a higher percentage of older individuals who got more than 9 hours of sleep each night got diagnosed with hypertension in the follow-up period.
The Bottom Line
Multiple studies show that people who get less than 6-7 hours or more than 9 hours of sleep per night are at a higher cardiovascular disease risk and even more prone to cardiovascular mortality. That said, ensure you get good-quality 7-9 hours of sleep at night for optimal heart health.
1. Laksono, S., Yanni, M., Iqbal, M., & Prawara, A. S. (2022, February 7). Abnormal sleep duration as predictor for cardiovascular diseases: A systematic review of prospective studies. Sleep disorders. Retrieved April 10, 2023, from https://www. ncbi.nlm.nih.gov/pmc/articles/PMC8844105/
2. Bradley, T. D., & Floras, J. S. (2009). Obstructive sleep apnoea and its cardiovascular consequences. Lancet (London, England), 373(9657), 82–93. https://doi.org/10.1016/S01406736(08)61622-0
3. Nagai, M., Hoshide, S., & Kario, K. (2010). Sleep duration as a risk factor for cardiovascular disease- a review of the recent literature. Current cardiology reviews, 6(1), 54–61. https://doi. org/10.2174/157340310790231635
4. Gangwisch, J.E., et al. (2006). Short Sleep Duration as a Risk Factor for Hypertension. Hypertension, 47, pp 833–839. https://doi.org/10.1161/01.HYP.0000217362.34748.e0
5. King, C. R., Knutson, K. L., Rathouz, P. J., Sidney, S., Liu, K., & Lauderdale, D. S. (2008, December 24). Short sleep duration and incident coronary artery calcification. JAMA. Retrieved April 21, 2023, from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2661105/
Lee A. Surkin, MD, is the Chief Medical Officer of Nexus Dental Systems. A private practitioner in cardiology, sleep medicine, and obesity medicine, he is one of a small group of physicians to be triple board certified in cardiology, sleep medicine, and nuclear cardiology. In 2009, he created Carolina Sleep – the only dedicated sleep medicine practice in eastern NC. Dr. Surkin has created a cardiovascular and sleep healthcare model that includes a multi-faceted diagnostic and treatment approach that is enhanced by a network of relationships with physicians, dentists, respiratory therapists, sleep technologists, and public officials who recognize the important role that sleep medicine has in our daily life. In 2012, Dr. Surkin founded the American Academy of Cardiovascular Sleep Medicine which is a not-for-profit academic organization dedicated to educating healthcare providers, supporting research, and increasing public awareness of the convergence between cardiovascular disease and sleep disorders. In 2014, Dr. Surkin created a new multi-specialty practice called Carolina Clinic for Health and Wellness which combines his specialties with primary care, gynecology, behavioral health and a medical spa. Dr. Surkin is married with three daughters and a golden retriever and resides in Greenville, NC.

Chronic
short sleep increases the risk of cardiovascular events.
Insomnia Medications –Not All Are Created Equal

 by Colonel Scott Williams, MD, FAASM
by Colonel Scott Williams, MD, FAASM
Insomnia and difficulty acclimating to oral appliance therapy (OAT) are two of the most significant barriers to initial adherence. Given that adherence is a big factor in selecting treatment for sleep disordered breathing, it is important for Dental Sleep Medicine (DSM) providers to be aware of the pharmacologic and behavioral treatments for insomnia. For CPAP (and likely OAT), the first few weeks of treatment are the most predictive of long-term success (Budhiraja 2007). While Cognitive Behavioral Treatment for Insomnia (CBT-I) is the first line treatment for chronic insomnia, medications are often helpful for short term treatment.
There are many different classes of sedative-hypnotic medications available to clinicians. The most widely prescribed medication for insomnia is the antidepressant trazodone despite lacking FDA approval for this indication (Wong 2020). Trazodone is a serotonin antagonist and re-uptake inhibitor (SARI) which has been available since the 1970s. Its profound antihistaminergic and anti-adrenergic effects can cause nextday somnolence as well as dizziness. Multiple organizations to include the American Academy of Sleep Medicine have suggested against the use of trazodone for insomnia (Sateia 2017, Martin 2020, Qaseem 2016).
Other off-label medications that have anti-histaminergic properties include tricyclic antidepressants, atypical antipsychotics, and the novel antidepressant mirtazapine. In addition to blocking the wake promoting neurotransmitter histamine, the GABA system has long been a target for sedation. One of the first classes of medications to enhance GABA were benzodiazepines (BZDs). Of the many available BZDs, only five are FDA approved for insomnia (estazolam, flurazepam, quazepam, temazepam and triazolam). These medications are still used frequently although they have a variety of side effects to include dependence, tolerance, and risk of falls especially in the elderly (Holbrook 2000). Because of these concerns, there was pressure to develop additional options. Non-BZD GABA-A agonists, known as “Z-drugs”, surged in popularity during the first two decades of the 21st century. Zaleplon, zolpidem and eszopiclone are highly effective in reducing sleep latency and depending on their half-life, have differential effects on wake after sleep onset. Eszopiclone has a longer duration of action than zolpidem (6-7 hours vs. 2.5-3 hours), and as a result the manufacturer of zolpidem has developed novel delivery mechanisms to extend its effects throughout the second half of the sleep period. Concerns about complex
sleep-related behaviors have gained significant attention in both scientific and lay press (FDA 2019, Carey 2019). While these medications remain effective and safe for the vast majority of patients, some clinicians and patients are hesitant to initiate even a brief course of treatment.
Melatonin is a regulatory hormone synthesized by the pineal gland in the absence of light. While melatonin is not in itself a sedative/hypnotic, it does enhance the release of sleep-promoting neurotransmitters and regulates the circadian rhythm. Melatonin is not regulated by the FDA and is considered a dietary supplement. Therefore, it is not approved for any indication and the potency of over-the-counter formulations can vary widely from the published label on the bottle (Cohen 2023, Erland 2017). Melatonin receptor agonists such as ramelteon are available and have shown some efficacy for sleep onset but do not appear helpful for sleep maintenance.
The newest class of insomnia medications are dual orexin receptor antagonists (DORAs). As opposed to GABA-ergic medications which enhance the sedative properties of this inhibitory neurotransmitter, DORAs block the wake-promoting effects of orexin. Like GABA agonists, the DORAs have different half-lives. The three currently available DORAs, suvorexant (12 hours), lemborexant (17-19 hours), and daridorexant (8 hours) may have differential potential for next-day somnolence as a function of the markedly different half-lives, though the data for this is scant at the moment. DORAs appear to have a gentler onset of action and some patients who are expecting an immediate soporific effect can be disappointed unless appropriate expectation management and counseling is given at the time of prescription.
For dental sleep practitioners, it is important to discuss the risk-benefit ratio of medications for insomnia with patients who are
being initiated on OAT. For most, the risk of untreated or under-treated OSA is far greater than the risk of a short course of sedative-hypnotic therapy. That being said, the type and duration of sedative medication to enhance OAT adherence is a topic that is vastly under-studied and an area ripe for exploration. In the absence of higher quality data, a standard practice of 2-3 weeks of an FDA-approved sedative with a medium-term (3-8 hour) half-life, is appropriate. As with all treatment decisions in DSM, a close working relationship between the dental clinic and the medical clinic is of paramount importance. A synchronized treatment paradigm for referrals, periodic follow-up and troubleshooting, is key to optimizing treatment outcomes.
1. Budhiraja R, Parthasarathy S, Drake CL, et al. Early CPAP use identifies subsequent adherence to CPAP therapy. Sleep 2007; 30(3):320-4.
2. Carey B. Drug agency calls for strong warning labels on popular sleep aids. The New York Times. April 30, 2019.
3. Cohen PA, Avula B, Wang, Y-H. Quantity of melatonin and CBD in melatonin gummies sold in the US. JAMA 2023; 329(16):1401-2.
4. Erland LA, Saxena PK. Melatonin natural health products and supplements: presence of serotonin and significant variability of melatonin content. J Clin Sleep Med. 2017; 13(2):275-81.
5. FDA drug safety communication: FDA adds black box warning for risk of serious injuries caused by sleepwalking with certain prescription insomnia medicines. 2019. www.fda.gov.
6. Holbrook AM, Crowther R, Lotter A, Cheng C, King D. Meta-analysis of benzodiazepine use in the treatment of insomnia. CMAJ 2000; 162, 225-33.
7. Martin JL, Mysliwiec V, Chowdhuri S, Ulmer CS. The Veterans Administration and Department of Defense clinical practice guidelines for the diagnosis and management of sleep disorders: what does this mean for the practice of sleep medicine? J Clin Sleep Med. 2020; 16(8):1377-81.
8. Qaseem A, Kansagara D, Forciea MA, Cooke M, Denberg T. Management of chronic insomnia disorder in adults: a clinical practice guideline from the American College of Physicians. Ann Intern Med. 2016; 165(2):125-33.
9. Sateia MJ, Buysse DJ, Krystal AD, Neubauer DN, Heald JL. Clinical practice guideline for the pharmacologic treatment of chronic insomnia in adults: an American Academy of Sleep Medicine clinical practice guideline. J Clin Sleep Med. 2017; 13(2):307-49.

10. Wong J, Murray Horwitz M, Bertisch SM, Herzig SJ, Buysse DJ, Toh S. Trends in dispensing of zolpidem and low-dose trazodone among commercially insured adults in the United States, 20112018. JAMA. 2020; 324(21):2211-3.
Colonel Scott Williams, MD, FAASM, is the director of the Center for Military Psychiatry and Neuroscience at the Walter Reed Army Institute of Research. Dr. Williams received his medical doctorate from the Uniformed Services University of the Health Sciences. He completed a dual residency in Internal Medicine and Psychiatry at the Walter Reed Army Medical Center with fellowship training in Sleep Disorders Medicine at the Walter Reed National Military Medical Center. He has served on numerous committees within the AASM and AADSM, and remains passionate about furthering the interdisciplinary nature of sleep medicine.

The type and duration of sedative medication to enhance OAT adherence is a topic that is vastly under-studied and an area ripe for exploration.
Atrial fibrillation and OSA
by Alan D. Steljes, MD, FACC, FRCPCObstructive sleep apnea (OSA) is associated with several cardiovascular disorders as diverse as coronary artery disease, congestive heart failure, atrial fibrillation and pulmonary hypertension. Untreated OSA may exacerbate cardiac disease, by imposing significant mechanical, metabolic, oxidative or hemodynamic stresses on the heart. The hope is that effective therapy of OSA may ameliorate the trajectory of the cardiovascular disease. The evidence is most compelling for atrial fibrillation.
What is Atrial Fibrillation?

Atrial fibrillation (also known as AFib) is an irregular, usually rapid, heart rhythm. It arises from the upper chambers of the heart, the atria. AFib is the most common persistent heart rhythm disorder in adults and appears to be increasing in frequency.
What Are the Potential Complications of Atrial Fibrillation?
For patients whose heart function is already compromised in some way, the ad-
dition of AFib lessens the heart’s efficiency leading to symptoms of fatigue or shortness of breath.
AFib is also associated with an elevated risk of stroke. When the heart is out of rhythm, there is a tendency to form blood clots within the heart. If the clots stay in the heart, it is not usually a problem. However, if the clots break loose from the heart, it flows in a straight line to the brain where the clot blocks off a blood vessel, causing a stroke. You’ve seen the many ads on TV for blood thinners to prevent strokes in AFib patients. It is important to note that some patients have no symptoms at all, but are still at risk for stroke.
What Are the Treatment Options for Patients with Atrial Fibrillation?
Most patients require antiplatelet or anticoagulant therapy to reduce the risk of stroke. Medications may be prescribed to slow the rapid heart rate, or to restore and maintain normal heart rhythm.
Symptomatic patients, who have failed on medication, may require cardioversion, an

electrical shock therapy designed to restore normal heart rhythm. Ablation is an invasive therapy designed to restore and maintain a normal heart rhythm.
Is Atrial Fibrillation Associated with Obstructive Sleep Apnea (OSA)?
About half of patients with AFib, also have OSA which appears to be relevant to the progression of AFib, since treatment with CPAP significantly reduces the risk of relapse following either cardioversion or ablation therapy.
How Does OSA Contribute to Atrial Fibrillation?
OSA causes structural and electrical re-modelling of the atria, distorting the electrophysiological mechanisms that maintain normal rhythm. CPAP reverses this re-modelling process over time.
The American Heart Association recommends that all patients with AFib should be screened for OSA which, when identified, should be treated. “Continuous positive airway pressure should be offered to patients with severe OSA, whereas oral appliances can be considered for those with mild to moderate OSA or for continuous positive airway pressure–intolerant patients. Follow-up sleep testing should be performed to assess the effectiveness of treatment.”1
Does Oral Appliance Therapy (OAT) Benefit Treatment of Atrial Fibrillation?

We are all familiar with the benefits of OAT in improving patients’ symptoms by relieving upper airway obstruction thereby reducing the cycle of recurrent hypoxia. It is not difficult to imagine that this would benefit the heart.
However, OAT is a technology which is still in its youth. Data supporting oral appliance specifically for atrial fibrillation is currently lacking. I am aware of one prospective study, sponsored by Texas A&M. However, the results have not yet been reported.
Is the Cost of PAP or OAT Justified?
Complications of AFib are costly. Patients with AFib incur approximately $28,000 additional health care costs annually, when compared to similar people without AFib.2
The costs of CPAP or OAT are small in comparison to costs of treating hospitalizations for AFib. Even small reductions in relapse rates are likely to reduce health care costs.
How Can Dentists Work with Cardiologists?

Sleep medicine spans multiple specialties and requires a multidisciplinary approach. Cardiologists in general are willing to screen their patients for sleep apnea. However, most cardiologists are not comfortable with hands on management of OSA. They are open to relationships with sleep medicine practitioners, including dentists, to manage and monitor their apnea patients.
1. Obstructive Sleep Apnea and Cardiovascular Disease: A Scientific Statement from the American Heart Association. Yerem Yeghiazarians, Hani Jneid, Jeremy R. Tietjens, Susan Redline et al Circulation. 2021;144:e56–e67. DOI: 10.1161/ CIR.0000000000000988
2. Deshmukh A, Iglesias M, Khanna R, Beaulieu T. Healthcare utilization and costs associated with a diagnosis of incident atrial fibrillation. Heart Rhythm O2. 2022 Aug 4;3(5):577-586. doi: 10.1016/j.hroo.2022.07.010. PMID: 36340482; PMCID: PMC9626881.
Alan D. Steljes, MD, FACC, FRCPC was trained as an interventional cardiologist. Since fellowship, he has obtained additional certification in nuclear cardiology, echocardiography, CT coronary angiography and finally sleep medicine. In 2010, he opened a two bed sleep lab, recognizing the heart-sleep apnea interaction. The initial 2 beds have been scaled up to 12 beds since associating with the Nevada Heart & Vascular Center. He has since retired from the cardiology practice but continues to oversee the sleep program. He remains passionate about spreading the word about sleep disordered breathing and the heart. He currently shares his time between Las Vegas, NV and Mount Pleasant, SC.
“About half of patients with AFib, also have OSA which appears to be relevant to the progression of AFib, since treatment with CPAP significantly reduces the risk of relapse following either cardioversion or ablation therapy.”
Why Every Dentist and Orthodontist Should Have an Orofacial Myofunctional Therapist on Their Team

Educational Aims
This self-instructional course for dentists aims to help the reader understand more about the connection and the value of having an orofacial myofunctional therapist on the treatment team for most patients of nearly all ages. Oral-systemic connections are becoming common knowledge in Dentistry. The links are rapidly expanding beyond nutrition, medications, and microbiome to include movement and body work, including physical therapy and orofacial myology. There is a long history of therapy that is only now gaining widespread recognition as a key element in wholebody wellness, including oral health.
Expected Outcomes
Dental Sleep Practice subscribers can answer the CE questions online at https://dentalsleeppractice.com/continuing-education/ to earn 2 hours of CE from reading the article. Correctly answering the questions will demonstrate the reader can:
1. Define the role orofacial myofunctional therapy (OMT) can play in their practice and lead their team to present this to patients.
2. Discuss how OMT can be helpful at many age levels of patients for specific indications.
3. Back up clinical observations with research supporting potential therapies.
by Nicole Goldfarb, M.A., CCC-SLP, COM®As knowledge about the etiology of sleep-disordered breathing (SDB) has expanded over the recent years, it is imperative to recognize that a team approach to intervention is paramount to the success of any treatment plan. In accordance with this multidisciplinary approach, an orofacial myofunctional therapist may be a key player on your dental team. Working directly with an orofacial myofunctional therapist may be one of the most effective ways to comprehensively treat your dental sleep patients. This article will explore the relationship between orofacial myology and dentistry and how these specialties can work together to better benefit patients of nearly any age. The team of the dental specialist and the orofacial myofunctional therapist can play a joint role in not only resolving malocclusion, but more importantly identifying red flags for soft tissue dysfunction, airway issues, and SDB.
It is now recognized that dental specialists have a responsibility to screen their patients of any age for sleep-related breathing disorders and to assist in treating or referring out for treatment for this condition. In addition, it is important to emphasize that over the past century, empirical and clinical data has shown that orofacial myofunctional therapy (OMT) goes beyond the benefits to the dental structures and into other disciplines like sleep medicine as well. Therefore, this crucial collaboration between the dental specialist and the orofacial myofunctional therapist cannot be overstated. Let’s look at what OMT is and how an orofacial myofunctional therapist can help your patients.
What is Orofacial Myofunctional Therapy?

OMT is a treatment program to resolve oral muscular dysfunction in order to establish correct oral rest posture and functioning of the oral facial system. OMT identifies and treats dysfunction of the oral facial muscles across the 5 domains of:
1. Oral rest posture
2. Chewing and swallowing of food
3. Swallowing of liquids
4. Sucking and swallowing of saliva
5. Speech (if the therapist is a Speech-Language Pathologist (SLP))
OMT can further be defined as “therapeutic exercise-based techniques, based on the principles of motor learning and neuroplasti-
city, to stabilize, tone, strengthen, or improve the range of motion of the skeletal muscles of the face and neck used to treat a range of orofacial myofunctional disorders.”1 Research and clinical evidence proves that OMT plays a crucial role in the identification and treatment of a variety of oral dysfunctions, and remediation of such soft tissue dysfunction can help prevent or assist in the treatment of the related sequelae of issues including dental malocclusion, oral health problems, feeding issues, speech disorders, postural issues, upper airway problems, sleep-disordered breathing, and the health and quality of life impacts of such problems.
Figures 1A and 1B: Adolescent with anterior open bite: Orthognathic surgery unnecessary post-myofunctional therapy. A. Pre-myofunctional therapy: The bite only touched on the back molars, yet the patient had already gone through full braces. The original orthodontist recommended orthognathic surgery to close the bite. The patient was referred for a second opinion. The second orthodontist recognized the tongue thrust and referred the patient for myofunctional therapy but made no guarantees that the patient would not need jaw surgery. B. Post-myofunctional therapy: After 2.5 years of braces and myofunctional therapy, the orthodontist gave the patient the good news that jaw surgery would not be necessary. The myofunctional therapy allowed the orthodontist to close the bite once the tongue pressure was removed from between the teeth.
Nicole Goldfarb, M.A., CCC-SLP, COM, founded the San Diego Center For Speech & Myofunctional Therapy 20 years ago, and shas been practicing Speech-Language Pathology since 2003 and Orofacial Myofunctional Therapy since 2008. Nicole holds the distinction of being one of only a few Certified Orofacial Myologists® in all of San Diego County that also has a master’s degree in Speech-Language Pathology, an unparalleled combination of degrees which allows her to provide the most advanced and comprehensive treatment, as most patients with speech issues also have myofunctional issues. Nicole worked as a Speech-Language Pathologist in a school district for 7 years, servicing thousands of children with speech and orofacial disorders. She has a special passion and interest in sleep-disordered breathing (SDB) and diagnosing restricted frenums as they relate to myofunctional disorders. Nicole has presented internationally on myofunctional therapy as it relates to SDB in both children and adults. She is currently on the Child Airway Initiative Task Force (CAST), a national team of doctors, dentists, and orthodontists developing a universal screening tool for all dentists to use to screen patients for SDB as per the 10/2017 American Dental Association proposal that all dentists should screen all patients for SDB. Nicole is the host and developer of the audio and video podcast for Airway Circle Radio titled “Airway Answers: Expanding Your Breath of Knowledge”. Nicole is also a Breathe Institute Ambassador, a Talk Tools® Education Partner, author of the myofunctional therapy chapter in an upcoming medical textbook, and she is currently on the faculty for ASAP (Airway, Sleep, and Pediatrics Pathway) and the Sleep Education Consortium. Nicole’s life-long quest is to help in the early identification and treatment of SDB.

History of Orofacial Myofunctional Therapy
Orofacial myofunctional therapy is not a new profession, to say the least, emerging in the early 1900s as a response from the orthodontic field to restore normal muscle function to remove unintentional pressure on the dental structures. OMT was initially developed by orthodontists as a means of improving orthodontic outcomes and preventing orthodontic relapse. As early as the late
1800s, Edward Angle, DDS, first recognized that mouth breathing and poor resting posture of the tongue can play a primary role in hindering orthodontic outcomes. In the early 1900s, Alfred Rogers, DDS, further advanced the field by acknowledging the role of soft tissue dysfunction on the oral skeletal system, and he developed exercises for the orofacial musculature.2 Rogers was an orthodontist born in 1873, and he was the President of the American Association of Orthodontists (AAO), the American Academy of Dental Sciences, and was also instrumental in forming the American Board of Orthodontics. Rogers was one of the first to develop a treatment program targeting orofacial muscular exercises which was indicated to stimulate desirable growth in the maxillofacial region, and he called this therapy “Myofunctional Therapy in Orthodontics.”3
teeth in OMT, the occlusion was able to normalize. The orthodontist feels the patient does not need braces.

As early as 1918, Rogers wrote articles and presented papers on this concept, including presenting at the annual meeting of the AAO in which he relayed the effects of the orofacial musculature and highlighted the foundation of OMT as a means of improving orthodontic outcomes, orthodontic stability, achieving facial balance and better growth and development of the oral structures. Rogers stressed that orthodontists must not focus solely on straightening teeth, but rather must attend to the role of the function of the oral facial muscles as having an impact on the skeletal system. Rogers asserted that alterations in functional activity of the oral cavity can cause malocclusion. The work of Alfred Rogers, DDS, over 100 years ago lay the foundation for OMT and the concept that muscular functioning has an impact on oral facial growth, development, and overall whole-body health. As the field of OMT advanced, over 50 years ago in 1972 the International Association of Orofacial Myology (IAOM) was developed, which is the first international organization to train and certify SLPs and dental hygienists in OMT.4
Figures 4A and 4B: Unilateral open bite developed later in life. A. This patient’s unilateral open bite was due to a change in muscle function, as after a left root canal the patient began to only chew on the right side. This chewing pattern changed the muscle balance as the patient continually spread the right side of the tongue to push food onto the teeth. There was no orthodontic progress, and the patient was referred for orofacial myofunctional therapy. B. OMT restored muscle development, resting tongue posture, correct chewing function, and correct swallowing. In 5 months, the patient was debanded.

Orofacial myofunctional therapy is a specialty area on top of an individual’s already established licensure as an SLP, dental hygienist, physical therapist, or occupational therapist. Although some individuals choose to focus their clinic work solely within OMT, this practice cannot be separated or isolated from their primary licensure which regulates
 Figure 3A and 3B: A. Pre-myofunctional therapy: Anterior open bite caused of soft tissue dysfunction including incorrect lingual rest posture and tongue thrust. B. Post-myofunctional therapy: 4 years after the start of myofunctional therapy with no orthodontic treatment, and the open bite closed. By taking the tongue pressure off of the
Figures 2A and 2B: Open bite corrected with myofunctional therapy. A. Pre-myofunctional therapy: This patient was in braces for 3 years with no success at closing the open bite. B. Post-myofunctional therapy: After 5 months of myofunctional therapy to address the mouth breathing and tongue thrust, the open bite closed.
A.
B.
A.
B.
A.
Figure 3A and 3B: A. Pre-myofunctional therapy: Anterior open bite caused of soft tissue dysfunction including incorrect lingual rest posture and tongue thrust. B. Post-myofunctional therapy: 4 years after the start of myofunctional therapy with no orthodontic treatment, and the open bite closed. By taking the tongue pressure off of the
Figures 2A and 2B: Open bite corrected with myofunctional therapy. A. Pre-myofunctional therapy: This patient was in braces for 3 years with no success at closing the open bite. B. Post-myofunctional therapy: After 5 months of myofunctional therapy to address the mouth breathing and tongue thrust, the open bite closed.
A.
B.
A.
B.
A.
their practice of OMT. You can therefore view OMT as a “modality” of treatment.
The importance of OMT cannot be overstated in the comprehensive treatment of orthodontic patients as well as playing a key role in the in the prevention of serious developmental problems within the orofacial respiratory complex. We begin with what defines correct oral rest posture before truly grasping the significance of OMT for the dental specialist.

What is Correct Oral Rest Posture?
Correct oral rest posture entails the following components: the lips closed/sealed at rest, the entire tongue gently suctioned to the palate (front, middle, and back of the tongue, with the sides of the tongue resting within the dental arch), and the teeth slightly apart with appropriate dental freeway space. This correct vertical alignment of the arches combined with a lips-closed posture will help maintain correct tongue posture. When the lips open or even slightly part, the tongue will likely lose suction from the palate and will drop within the oral cavity. Moreover, the tongue has enough weight to drop the mandible and cause the lips to open. This bidirectional relationship of lip and tongue posture cannot be overemphasized. This correct posture produces better relaxation of the facial and perioral muscles and promotes nose breathing, which is proven to be the healthiest way for humans to breathe. In addition, correct oral rest posture will assist in better dental and facial development, as the tongue and lips are natural growth supports for proper arch development.
What is an Orofacial Myofunctional Disorder (OMD)?
Given that we know what correct rest posture of the oral facial structural complex entails, we must seek to understand why a deviation in such patterning may exist. An OMD encompasses any of the following, often in combination:
1. Any deviation in correct oral rest posture of the lips, tongue, and/or jaw
2. A thrusting of the tongue during chewing and swallowing or speech
3. Noxious or parafunctional oral habits such as digit sucking, tongue sucking, cheek biting, nail biting, lip licking,
Figures 5A and 5B: Adolescent with anterior open bite: Orthognathic surgery unnecessary post-myofunctional therapy. A. Pre-myofunctional therapy: If mouth breathing is left untreated until the patient is skeletally mature, the only remaining way to correct the jaw discrepancy may be with orthognathic surgery. This patient was healthy and breathing through his nose until age 3 when he went to preschool. His colds and breathing issues did not clear until he was 7 years old. By then, he had a mouth breathing habit. Now at 17, he is in braces for the third time and being prepared for surgery to align his jaws. There are a number of myofunctional problems including lip incompetence, low forward tongue posture, and tongue thrust contributing to his severe open bite. B. Post-myofunctional therapy: His therapy included correcting his mouth breathing by strengthening the lips, exercising and training the tongue to rest sucked up on the palate, and retraining his swallowing patterns for saliva, food, and drinks. He was an excellent compliant patient which is necessary for successful therapy. After 7 months of myofunctional therapy, his bite corrected without surgery because of the myofuctional therapy. The oral surgeon cancelled the surgery, and he had a successful orthodontic result because: 1) the mouth breathing was corrected; 2) the tongue thrust was corrected.
prolonged pacifier use, or bruxism, to name a few
An orofacial myofunctional therapist identifies and evaluates the causes of OMDs to determine the best treatment plan of such habits and soft tissue dysfunction. A key understanding in the myofunctional therapy evaluation process is not complete unless it identifies all the factors that are capable of causing or contributing to the OMD, which may include problems in the medical system, dental system, or the myofunctional system.
Orofacial myofunctional therapists refer patients to ENT doctors, allergy doctors, and airway focused dentists or orthodontists to assist in the comprehensive treatment plan to resolve such dysfunction and the sequelae of effects that such soft tissue problems can trigger. There are many cases where the medical
Figure 6A-6D: A-B. Pre-myofunctional therapy: This 9-year-old was treated by the orthodontist for 3 years with a Bead Roller and two tongue guards. There was no progress in closing the open bite. It is evident in the Pre-Myofunctional Therapy photos that there is an anterior open bite accompanied by low tongue tone when the patient is asked to engage in lingual palatal suction. C-D. Post-myofunctional therapy: After 10 months of OMT and no orthodontic treatment, increased oral muscle tone is obvious when the patient is engaged in lingual palatal suction, and the open bite was resolved simply by treating the OMD thereby removing the tongue pressure from the teeth and establishing correct oral rest posture and functioning.


cause of the dysfunction must be resolved before the muscles are rehabilitated in OMT, and this may include certain cases of adenoid or tonsillar hypertrophy or other pathology impacting nasal patency. The OMT acts as a team player in initiating such referrals and in gauging when myofunctional therapy can be initiated. Timing of myofunctional therapy is also influenced by whether a malocclusion is too significant and needs to be addressed prior to the OMT. In some cases, OMT should be initiated before or during orthodontic treatment, whereas in other cases therapy is best to wait until after appliances are removed. Communication between the orofacial myofunctional therapist, ENT doctor, dentist, and orthodontist is crucial to outcome success.
What are the Impacts of OMDs?
tongue thrust, low and forward lingual rest posture. B. Post-myofunctional therapy: His bite closed substantially after OMT, and this photograph is pre orthodontic treatment.
Figures 8A and 8B: A. Pre-myofunctional therapy: This 8-year-old had an open bite and an array of OMDs including tongue thrust, poor oral rest posture, and speech issues. B. Post-myofunctional therapy: His open bite closed after OMT, and this photograph is pre orthodontic treatment.
This foundational understanding of OMDs and what defines normal resting posture of the orofacial structural complex leads to a discussion of the negative health and developmental impacts when an OMD is present. Not only does soft tissue dysfunction contribute to dental malocclusion, but it is also important to understand the multitude of changes in the orofacial respiratory complex and entire body system that can occur when malocclusion is present. If there are alterations in the airway which interfere with normal nasal breathing, then facial growth and function may proceed along a different path, with the potential to change the skeletal growth not only of the entire face, but also head/neck posture, whole-body posture, breathing patterns, and sleep quality. Physical therapists have referred to the tongue as “the rudder to the spine” and understand that correct tongue posture helps with wholebody posture via connections of the tongue to the oral pharyngeal airway, down the hyoid bone, through the deep frontal fascial plane. When jaw growth is not ideal, the nasal and pharyngeal airway can become negatively impacted. When the airway is impacted, the head and neck can compensate in a “forward head posture” to help open the airway to facilitate better breathing. Moreover, any reduction in the airway size from the tip of the nose down the throat including factors such as nasal obstruction, narrow palate, retruded jaws, open mouth posture, low tongue posture, or any hypotonia of the
 Figures 7A and 7B: A. Pre-myofunctional therapy: This 13-year-old thumb sucker developed an open bite from this noxious oral habit and poor tongue rest posture and functioning. His OMDs included mouth breathing, lip incompetence,
A.
C.
B.
D.
A.
A.
B.
Figures 7A and 7B: A. Pre-myofunctional therapy: This 13-year-old thumb sucker developed an open bite from this noxious oral habit and poor tongue rest posture and functioning. His OMDs included mouth breathing, lip incompetence,
A.
C.
B.
D.
A.
A.
B.
orofacial complex can affect the quality of sleep in individuals of any age, from infancy through adults, leading to SDB and the end stage disease of obstructive sleep apnea (OSA). OMDs should be recognized early and must not be ignored once red flags are identified, which can often easily be recognized in the dental or orthodontic office.
Research on OMT
Research shows that OMT is effective in helping to prevent orthodontic relapse, facilitating correct growth of the orofacial complex, assisting with correction of orthodontic problems during orthodontic treatment, and has a significant role in not only helping to treat but also helping to prevent SDB and OSA. Studies show that OMT:
1. Significantly improves the outcome SDB post adenotonsillectomy
2. Combined with rapid palatal expansion (RPE) leads to better treatment outcomes among patients with SDB than with RPE alone
3. Can be the necessary factor in preventing the relapse of SDB in patients who have undergone RPE and lingual frenectomy
4. May actually prevent much SDB in the young population
5. Can decrease the severity of OSA, promotes improved oxygen saturation during sleep, and can improve sleep quality and life quality
6. Improves CPAP compliance
7. Can be an adjunct to hypoglossal nerve stimulation treatment for OSA

8. Can assist in preventing orthodontic relapse in most orthodontic cases
9. Can improve oral health in patients, including decreasing the risk of periodontal disease

Early Intervention
It is not surprising that the earlier an OMD is identified, the chances of a further sequelae of related issues is mitigated. Myofunctional disorders are progressive and if left untreated they will typically worsen over time. Therefore, early identification of such soft tissue dysfunction is paramount in the treatment process. Typically, it is an SLP with specialized training in feeding therapy and oral sensory motor therapy that has the skills and expertise to treat children younger than
the age of 4. Often there are foundational feeding and oral motor skills that need to be addressed in the early intervention (infancy through 3-year-old age group) before a standard OMT program would ever be considered. After age 4, most children then have the cognitive ability to imitate, self-monitor, understand the goals, and therefore participate in an OMT program. In many cases even 4+ year old children need regular feeding and oral sensory motor therapy by an SLP in addition to OMT. It is never too early to seek an OMT assessment by a trained professional, whether it be a specially trained SLP for the birth through 3-year-old age range or an SLP or dental hygienist specially trained OMT for patients aged 4-years-old and above. Often multiple therapists including IBCLC, PT, OT are on the team for such patients who have multiple whole-body issues. Signs of dysfunction are often there before symptoms are present, and it is best to refer out for an assessment as early as issues are noticed.
It is Never Too Early, and It is Never Too Late
Just as “it is never too early to learn normal oral function,”5 it is never too late
to remediate problems in the oral muscular system. Currently, the youngest patient in our office with oral sensory/feeding dysfunction is 12-months-old, and our oldest patient with oral muscular dysfunction contributing to his OSA is 84-years-old. It is also important to understand that many cases of untreated OMDs may have begun in childhood and developed into end stage sleep apnea in adulthood as the oral muscular system, facial structure, and airway never properly developed due to these initial muscular problems. Although early treatment and prevention is of utmost importance, there is always an opportunity to help a person suffering from an OMD, as this can truly impact the quality of that person’s life.
How an Orofacial Myofunctional Therapist Can Help You

Given this detailed description of OMT, it is obvious that dentists and orthodontists should team up with orofacial myofunctional therapists in the assessment and treatment of their patients. According to the ADA Policy Statement in 10/2017, all dentists should screen patients for sleep-related breathing disorders, and an OMD is a clinical marker to look for.6,7 It is important for dental specialists to be able to identify markers for OMDs which include red flags such as nar-
row palates, crowded teeth, malocclusion, dental wear or tori from bruxism, scalloped tongue, open mouth breathing, low tongue posture, tongue thrust, tongue tie, mentalis strain / lip incompetence, large tonsils, noxious oral habits, and even speech issues such as a lisp can be easily identified by the dental specialist and can trigger a referral to the orofacial myofunctional therapist in the team approach. Once we know something, we must not ignore it, and I am hopeful that this knowledge of our intermixed disciplines will help to bridge the connection between dental specialists and orofacial myofunctional therapists to better help our patients achieve the best care and quality of life possible.
1. D’Onofrio L. (2019, November 22). Publication trends and levels of evidence in orofacial myofunctional therapy literature. [Presentation]. ASHA 2019: Orlando, FL, United States.
2. Rogers, A. P. (1939). Evolution, development, and application of myofunctional therapy in orthodontics. American Journal of Orthodontics and Oral Surgery, 25(1), 1-19.
3. Rogers, A. P. (1918). Exercises for the Development of the Muscles of the Face, with a View to Increasing Their Functional Activity. The Dental Cosmos, LX(59), 857-924.
4. Mills CS. International Association of Orofacial Myology History: origin - background - contributors. Int J Orofacial Myology. 2011 Nov;37:5-25. PMID: 22774699.
5. Direct quote from D’Onofrio L, “It is never too early to learn normal oral function.”
6. D’Onofrio L. Oral dysfunction as a cause of malocclusion. Orthod Craniofac Res. 2019;22:43-48.
7. ADA Policy Statement: The Role of Dentistry in the Treatment of Sleep Related Breathing Disorders. Adopt ed 2017
Correct oral rest posture assists in facial development, supporting natural arch development.
Continuing Education Test
AGD Code: 180
Date Published: August 10, 2023 Course Expires: August 10, 2026
Legal disclaimer: Course expires 3 years after publication date. The CE provider uses reasonable care in selecting and providing accurate content. The CE provider, however, does not independently verify the content or materials. Any opinions expressed in the materials are those of the author and not the CE provider. The instructional materials are intended to supplement, but are not a substitute for, the knowledge, skills, expertise and judgement of a trained healthcare professional.
CE CREDITS
Each article is equivalent to two CE credits. Available only to paid subscribers. Free subscriptions do not qualify for the CE credits. Subscribe and receive up to 8 CE credits for only $149 by visiting https://dentalsleeppractice.com/subscribe/.
n To receive credit: Go online to dentalsleeppractice.com/continuing-education/, click on the article, then click on the take quiz button, and enter your test answers
To provide feedback on this article and CE, email us at education@medmarkmedia.com.
Why Every Dentist and Orthodontist Should Have an Orofacial Myofunctional Therapist on Their Team by Nicole Goldfarb, M.A., CCC-SLP, COM®
1. The age limit for reasonable expectations of OMT success is ________.
a. 3 - younger than that it's best to just wait
b. 12 - after puberty, muscle pattern memory is difficult to change
c. 60 - a lifetime of bad habits means learning new tricks is a waste of time
d. 110 - before that, OMT may be helpful at any age, appropriate to the individual's needs
2. An orofacial myofunctional disorder (OMD) ___________.
a. Represents a deviation from rest posture and/or function of the orofacial structural complex.
b. Is an observable phenomenon such as an involuntary tic.
c. Typically resolves on its own as a patient ages.
d. Must be treated by a trained orofacial myofunctional therapist before any surgery.
3. Correct oral rest posture means ____________.
a. The head must be centered over the shoulders and pelvic floor.
b. The tongue must be in contact with the lingual of the maxillary incisors.
c. Lips closed, entire tongue suctioned to the palate, and teeth slightly apart.
d. With teeth in maximum intercuspation, the condyles are centered in the glenoid fossae.
4. An Orofacial Myofunctional Therapist is ____________.
a. A recognized subspecialty of dental hygiene.
b. A licensed provider in many, but not all, states.
c. Capable of additional training to become a fully recognized Physical Therapist.
d. A person with specialized training in orofacial myofunctional therapy and is only a modality of treatment, not a separate stand-alone profession.
5. In the late 1800s ____________.
a. Orthodontists established the proper tongue position for successful tooth alignment.
b. Edward Angle, the ‘Father of Orthodontics,’ recognized mouth breathing as a hindrance to orthodontic success.
c. Protocols of orthodontic therapy included specific tongue exercises.
d. Tooth alignment was thought to be genetically defined and unchangeable.
6. OMT is a therapy best initiated ____________.
a. Before orthodontic treatment
b. During orthodontic treatment
c. After orthodontic treatment
d. This is determined on a case-by-case basis with the OMT and the orthodontic provider, depending on the patient’s appliances and individual treatment plan.
7. Domains of OMT include ____________.
a. Chewing and swallowing, oral rest posture, and spine alignment
b. Speech therapy, Singer training, and vocalization improvement
c. Breathing coaching, swallowing of liquids, and saliva control
d. Chewing and swallowing of food, saliva control, and oral rest posture
8. According to Dr. Alfred Rogers, ____________.
a. Alterations in functional activity can cause malocclusion.
b. Dental hygienists should never provide OMT.
c. Organizations such as the AAO were out of touch and unimportant.
d. Dr. Angle’s classification system led to unhelpful treatment protocols.
9. Research on OMT has established ____________.
a. That OSA in adults can be eliminated with OMT
b. OMT as a helpful adjunct in nearly every treatment for sleep-related breathing disorders.
c. Dental hygienists as the leading providers of OMT.
d. The potential for preventing tooth crowding and the need for orthodontics.
10. Orofacial myofunctional disorders ____________.
a. Are rare and usually associated with neurological diseases.
b. Are not covered by the ADA’s 2017 Policy Statement for Dentist’s Role in Sleep Related Breathing Disorders
c. May be recognized by noticing one of many red flags during dental exams.
d. Are always associated with poor speech issues such as a lisp.
Personalized, Precision, Oral Appliance Therapy
Personalized medicine tailors medical diagnostics and treatments to a patient’s unique characteristics, needs, and responses. Dentists excel at providing personalized precision care to address individual needs and desires.
With sleep study data and clini cal insights, dentists identify targeted therapies for Obstructive Sleep Apnea (OSA), addressing specific obstructions and dental considerations driving the disease.
DynaFlex, a renowned leader in dental technology and solutions, has recently acquired Respire, the company behind the innovative Respire Pink AT, a groundbreaking oral appliance therapy for OSA. This strategic move by DynaFlex showcases their commitment to investing in cutting-edge technologies and being at the forefront of personalized, precision healthcare.
When looking to improve on this leadingedge design, David Walton, former CEO of Respire, notes the desire to continuously enhance the treatment for the benefit of the patient, emphasizing that “data-driven success and patient acceptance are paramount for OAT to become the leading therapy for OSA.”
Appliance selection remains our most powerful resource to ensure desired outcomes. In the last few years, the Respire Pink AT (Advanced Titration) Herbst has become one of the most effective appliances applicable for many patients due to several key innovations. The titration mechanism advances up to 7mm using a simple and continuous turning mechanism. The adjustment key has a user-friendly handle and patented technology ensures the screw does not turn back on itself during use. The measuring scale on the arm allows both the patient and the dentist to closely monitor jaw position.
The Respire Pink AT Micro has been meticulously refined to elevate patient comfort. We have been able to maintain all the current AT features, while creating one of
the smallest PDAC approved hinges on the market. By reducing the length of the hinge by ~24% this prevents irritation of the commissures of the lip while the patient’s mandible is being advanced. This dedication to patient-centric design sets a new standard for oral appliance therapy.

Flexibility has been further expanded with the addition of an anterior fixing element, accommodating up to 4mm of further advancement (total potential advancement 8mm). Renowned Sleep Specialist Dr. Barry Chase notes, “this is rarely needed but it is great to have the option,” demonstrating the appliance’s versatility in catering to individual patient needs.
Knowing your options for appliance selection can provide you with the opportunity to deliver precision therapy for your sleep apnea patients. By partnering with an oral appliance manufacturer like DynaFlex, dentists have multiple options for OAT devices. This ensures that each patient receives tailored treatment according to their unique needs and preferences, ultimately fulfilling the vision of personalized medicine.
The acquisition of Respire by DynaFlex marks a pivotal moment in the field of personalized, precision OAT for Obstructive Sleep Apnea. With the Respire Pink AT Micro and DynaFlex’s steadfast commitment to innovation and investment in advanced technologies, dentists can anticipate achieving even better outcomes and providing improved patient experiences, reinforcing oral appliance therapy as a leading treatment option for OSA.




A New Technique for Fabricating a Mandibular Advancement Device in the Edentulous CPAP-Resistant Patient

 by Richard. B. Dunn, DDS, MS, D.ABDSM; Jessica Turner, CDA; and David Walton, CDT
by Richard. B. Dunn, DDS, MS, D.ABDSM; Jessica Turner, CDA; and David Walton, CDT
Obstructive Sleep Apnea (OSA) is a major medical problem throughout the world. It has been estimated to affect 15-30% of male adults and 5-15% of female adults.1,2 In a more recent publication, it is estimated that 50% of men and 23% of women aged 45-85 years have moderate to severe OSA, defined as 15 or more breathing disturbances per hour of sleep.3 Furthermore, the estimated prevalence of OSA has increased by 14% to 55% over the past two decades.4 The prevalence of OSA is therefore significant and increasing with greater obesity and aging of populations.5 Moreover, according to the American Dental Association more than 36 million Americans are edentulous. This article presents a technique to address OSA in this patient population using oral appliance therapy.
OSA is a disorder characterized by recurrent, transient narrowing (hypopnea) and collapse (apnea) of the upper airway during sleep. These breathing disturbances cause frequent oxygen desaturations (nocturnal hypoxemia) and sleep fragmentation with recurrent arousals from sleep. When left untreated there is an extensive list of symptoms as well as adverse health consequences of daytime sleepiness, decreased concentration, fatigue, irritability, and memory loss,6 reduced quality of life,7 increased risk of motor vehicle accidents,8 cardiovascular disease,9,10 metabolic disorders,11 cognitive impairment,12 depression13 and cancer.14 In addition, studies have shown that patients suffering from edentulism are more likely to develop OSA. Edentulism leads to a decrease in size and tone of the pharyngeal musculature and reduction of the retropharyngeal and posterior airway space.15,16 Studies have inferred that pharyngeal expansion can be accomplished with a Mandibular Advancement Device (MAD) and the increased volume was most
pronounced in the velopharynx region.17 A great challenge faced by dental sleep medicine (DSM) clinicians is to provide effective and comfortable treatment with MAD therapy for edentulous patients. DSM providers are seeing more of these patients referred by physicians due to the increased number of people with OSA and non-compliance or inability of patients to use CPAP. Lack of teeth and anchorage for the MAD can be very challenging. Some qualified dentists will not treat these patients for a variety of reasons including reduced retention and comfort of the MAD and difficulty in obtaining accurate protrusive and bite records. However, for many of these patients, dental sleep clinicians may be their last chance to have their OSA treated. An excellent option for the edentulous patient is the use of implants to help anchor the MAD but patients may not be able to afford them or are not good candidates due to lack of bone or other medical conditions. Some clinicians prefer to make the MAD to fit over the existing denture(s). Impression techniques are relatively simple and the dentures can be used to establish the bite relationships, vertical dimension, and horizontal range of protrusion. This combination may not be successful due to the increased thickness, bulk, crowding, and vertical opening it creates which can be counter-productive to the treatment of the underlying OSA. The patient is essentially wearing four oral prosthesis (upper and lower dentures, along with upper and lower oral sleep devices) which is likely to decrease tongue space perhaps worsening, not improving, OSA. If the MAD is to be made to fit the edentulous ridge without the denture, it is difficult to accurately record the vertical dimension and protrusion of the appliance and communicate this to the lab correctly and effectively. Use of occlusal wax rims can be extremely challenging to set
the correct incisal edge position and midline alignment to determine the protrusive start position. If the wax rim doesn’t accurately replicate the incisal edge of the denture, the dentist could take a protrusive bite at 3mm (for example) but could actually be advancing them much more, or much less, than the wax rim is showing. This could lead to unnecessary side effects and/or not increasing the pharyngeal space in the airway, rendering the oral sleep device ineffective.


This article will explain a new way to eliminate errors and construct an effective MAD for the treatment of the patient’s OSA. Clinical cases and photos will demonstrate this process.
Methods
The cases demonstrate the construction of a MAD in an edentulous maxilla with teeth present in the mandible. The patient is wearing a full upper denture (FUD) which is retentive. Examination reveals adequate bone and alveolar ridge to support the maxillary component of the MAD. Impressions are taken of the mandible, edentulous maxilla and the existing FUD in the mouth. The impression of the edentulous maxilla should include all borders and extensions of the FUD for maximum retention of the OA (see Figure 1). The maxillary component of the MAD will be fabricated to fit directly over the edentulous maxilla (see Figures 2A, 2B, and 2C). Therefore, this needs to be a very accurate impression to ensure excellent fit, retention and comfort for the patient. With the patient wearing their FUD, records for the MAD can be obtained by standard techniques using a George Gauge to choose the starting position and desired vertical dimension of the appliance and record the maximum range of motion from most retruded to maximum protrusive positions. This eliminates the guess work previously described in obtaining an accurate protrusive position. After obtaining the protrusive bite records the impressions are poured up with good quality stone and trimmed when set. A suck down over the stone model of the FUD with 060-gauge material is done and carefully trimmed to fit accurately over the edentulous model with full extension to the borders. The suck down can then be held in place on the edentulous model with sticky wax or any other techniques preferred (see Figures 3A and 3B). This gauge material is used to obtain good
definition of the FUD without being too thick to alter vertical dimension and to be sturdy enough to not distort by flexing when mounting. The edentulous model with attached suck down is then placed into the George Gauge bite and sent to the lab which will then place the opposing model in the bite and mount the case on a semi-adjustable articulator (see Figures 4A and 4B). When the mounting is set in the articulator the suck down can be removed from the maxillary model. The starting protrusive position, midlines and vertical opening of the appliance have now been accurately provided to the laboratory and construction of the appliance can begin. Figures 5A, 5B, and 5C demonstrate the MAD appliance intraorally. It’s important to note that there is often a misunderstanding between the clinician and the laboratory around transferring the dimensions of the denture to the sleep device. Unfortunately, it is not possible to take an impression of the denture and an impression of the oral cavity and lay one model over the top of the other.

Richard B. Dunn, DDS, MS. D.ABDSM, went to Franklin & Marshall College, received a MS from Roswell Park Memorial Cancer Institute in Head & Neck Cancer, and his dental degree from NYU College of Dentistry. He was nominated for Fellowship in The American College of Dentists and the Pierre Fauchard Academy. He is a Diplomate of The American Board of Dental Sleep Medicine and serves as a Director of the ABDSM and is on the Executive Committee. Dr. Dunn has been practicing Dental Sleep Medicine for over 13 years and practices in a team approach with physicians, dentists, and dental sleep labs. He is the owner of Chemung Family Dental in Elmira, New York.

Jessica Turner is a Certified Dental Assistant in NYS and has assisted Dr. Dunn for the past 10 years in overseeing the Sleep Department at Chemung Family Dental. She is extremely focused on the sleep patients and their care and has dedicated herself to continuing education and clinical experience in Dental Sleep Medicine.

Originally from the UK, David Walton graduated from the Royal College of Surgeons as a Clinical Technician treating patients for dentures before moving to New York where he co-founded Respire in 2010. Over the last 13 years, David has spearheaded the growth of Respire to become one of the leading oral sleep devices in the industry and recently led the company through a successful acquisition with Dynaflex where he continues to support future innovation.

It is also possible to make a MAD for a fully edentulous patient (Figure 4C) using the same process of using a suck down transfer record. However due to the lack of retention in the mandible, implants would be needed to attach the mandibular component of the Oral Appliance to gain adequate retention.





If the patient has implants present or if implants are to be placed, impressions are taken through standard techniques that will record the position of the implants to the lab. The use of 4 or more implants would be ideal for retention of the MAD but 2 would be the minimum. Communicate with the dental sleep lab about your intention to connect the sleep appliance component to the implants, type of attachments that will be used, and how much relief on the underside of the appliance you desire at each implant site. This will save chair time at the insertion appointment. The technique to connect the mandibular component of the MAD to the implants is similar to that used for an implant retained overdenture. The same procedures can be used if there are implants in the maxilla.
A common question asked is what fees should be charged for these procedures. This obviously needs to be determined by each clinician. The author chooses to not make additional charges for a MAD for an edentulous maxilla. Delegating some of the extra tasks to team members can mitigate the extra
costs. Attaching a component of the MAD to implants can be a time consuming process so a fair fee needs to reflect time spent as well as components and materials needed. Our experience has been that patients are accepting of these additional fees when explained prior to treatment. This discussion should include the improved effectiveness, retention, and comfort of the sleep appliance with implant support.
After a combined 24 years working in dental sleep medicine, the authors believe this technique has great value when treating edentulous patients with OSA. We have had repeated clinical successes while reducing some of the clinical and production challenges previously encountered.
1. YoungT, Palta M, Dempsey J, Peppard PE, Nicio FJ, Hia KM (2009) Burden of sleep apnea:rationale, design and major findings of the Wisconsin Sleep Cohort Study, WMJ 108(5): 246-249.
2. Peppani PF, Young T, Barnet JH, Palta M, Hagen FW, Hla KM. (2013) Increased prevalence of sleep-disordered breathing in adults. Am J Epidemiol 177(9):1006-1014
3. Lai V, Carberry J, Eckert D. Sleep Apnea Phenotyping: Implications for Dental Sleep Medicine. J Dental Sleep Med (2019): 6(2)
4. Peppard PE, Young T, Barnet JH, Palta M, Hagen EW, Hia KM. Increased prevalence of sleep-disordered breathing in adults. Am J Epidemiol 2013; 177(9): 1006-1014.
5. Nieto FJ, Peppard PE, Young T, Finn L, Hla KM, Farre R. Sleep-disordered breathing and cancer mortality: Results from the Wisconsin sleep cohort study. Am J Respir Crit Care Med 2012; 186: 190-194
6. Adult Obstructive Sleep Apnea Task Force of the American Academy of Sleep. Clinical Guideline for the Evaluation, Management and Long-term Care of Obstructive Sleep Apnea in Adults. J Clin Sleep Med. 2009: 5(3) 263-276.
7. Lacasse Y, Godbout C, Serios F. Health -related quality of life in obstructive sleep apnea. Eur Resp J. 2002; 19(3):499-503.
8. Ellen RI, MarshallSC, Palayew M, Molnar FJ, Wilson KG, ManSon-Hing M. Systemic review of motor vehicle crash risk in persons with sleep apnea. J Clin Sleep Med. 2006;2(02): 193-200.
9. Hla KM, Young T, Hagen EW, et al. Coronary Heart Disease Incidence in Sleep Disordered Breathing; The Wisconsin Sleep Cohort Study. Sleep 2015;38(5):677-684.
10. Rodine S, Yenokyan G, Gottlieb DJ, et al. Obstructive sleep apnea-hypopnea and incident stroke. The Sleep Heart health Study.. Am J Resp Crit Care Med. 2010;182(2):269-277.
11. Aurora RN, Punjabi NM. Obstructive sleep apnoae and type 2 diabetes mellitus: a bidirectional association. Lancet Resp Med, 2013;1(4):329-338.
12. Osorio RS, Gumb T, Pirraglia E, et al. Sleep-disordered breathing advances cognitive decline in the elderly. Neurlology. 2015;84(19):1964-1971.
13. BaHammam AS, Kendzerska T, Gupya R, et al. Comorbid depression in obstructive sleep apnea: an underrecognized association. Sleep Breath. 2016;20(2):447-456.
14. Marshall NS, Wong KK, Phillips CL, Liu PY, Knuiman MW, Grunstein RR. Is sleep apnea an independent risk factor for prevalent and incident diabetes in the Bussolton Health Study? J Clin Sleep Med. 2009;5(1):15-20.
15. Bucca C, Carossa S, Piuetti S, Gai V, Rolla G, Preti G. (1999). Edentulism and worsening of obstructive sleep apnea. Lancet. 353(9147): 121-122.
16. Bucca C, Cicolin A, Brussino L, Arionti A, Graziano A, Erovigni F, Pera P, Gai V, Mutani R, Preti G, Rolla G, Carrosa S (2006) Tooth loss and obstructive sleep apnea. Respir Res 7:8.


17. Tripathi A, Gupta A, Sarkar S, Tripathi S, Gupta N. (2015) Changes in upper airway volume in edentulous obstructive sleep apnea patients treated with modified mandibular advancement device. J of Prosthodontics: 1-7.

Sapphire is uniquely positioned “Expand North American sales and

Sapphire is uniquely positioned to impact the dental strategic “Expand North American sales and leverage the marketing organization

Holdings
pillars. organization to drive adoption of a national turnkey brand”


OSA public awareness activities: website, social media, brochures, posters, videos, events and most importantly the B to C products
Complete turn on approach to Sleep implementation, ongoing coaching & support and new sales of equipment, software and services
Unique therapeutic framework for Chronic Headache, Migraine, TMD, Tinnitus, Vertigo, Pain Head, Neck, and Face

OSA public awareness media, brochures, importantly the Complete turn-key, implementation, new sales of equipment, Unique therapeutic Headache, Migraine, Head, Neck, and
501C3 Non-Profit Fully accredited, online, ondemand Dental Sleep Medicine credentialing. The only one of its kind in the world.



Medmark LLC is proud to be the leading interactive marketing and multi-platform advertising company focused on the niche specialties of dentistry. We are creating a healthier America through knowledge, due diligence, and experience, by empowering dental professionals with high quality clinical information in clear and concise language and showcasing innovative technologies.

The Future of Sleep Medicine Starts Here

www.nexusdentalsystems.com
 Nexus Bill
Nexus Airway
Nexus Bill
Nexus Airway
Wake-up Call
Improving Patient Sleep and Dental Practice Outcomes with Laser Dentistry
 by Dr. Anthony Bolamperti
by Dr. Anthony Bolamperti
Snoring is a fact of life for nearly half of men and close to 30% of women, and the impact of this disorder ranges from mild annoyance to significant sleep disruptions that can contribute to heart disease, kidney disease, high blood pressure, diabetes, stroke, obesity, and depression. Snoring is also the third-leading cause of divorce in the United States, and I have heard from plenty of patients who sleep in a different room from their spouse just to get a good night’s sleep. But even if those middle-of-the-night rumblings don’t cause tensions with your partner, they prevent the body from getting needed rejuvenation, causing sleep deficiency that has been linked to a higher chance of injury for adults and teens.
However you look at it, snoring reduces quality of life, and given its prevalence, chances are there are plenty of patients in your own waiting room who would benefit from learning about the value-added services you can provide to help alleviate snoring for them, their partner, or family members.
Dentists have a long history of helping patients sleep better, but our contributions have historically focused on creating oral appliances for use at night. While appliances can be effective, that effectiveness is heavily dependent on patient compliance. Dentists who establish an open line of communication about broader patient needs, such as snoring, have an opportunity to understand and influence patient compliance with the use of oral appliances, but they can also create opportunities to identify a potential connection between snoring and more
serious health conditions, such as sleep apnea. Providing this level of attention to the overall needs of patients can solidify your doctor-patient relationships and create new revenue streams, particularly if you have adopted laser dentistry into your practice. Laser dentistry presents a tremendous opportunity for dentists to deliver an alternative to invasive surgical procedures that have been used to treat snoring, such as UPPP (uvulopalatopharyngoplasty), or to support and complement traditional snoring therapies to deliver more long-lasting relief with minimal discomfort.
I have been performing such procedures using the Solea® All-Tissue Laser and Solea Sleep from Convergent Dental. The 9.3-micron laser makes it easy to quickly relieve snoring for “palatal” or mouth snorers, which account for 80% of snorers overall. In as little as 15 minutes per treatment, Solea Sleep tightens the collagen fibers of the soft palate, reducing or eliminating the vibrations that cause snoring. Similar treatments are possible with other lasers, but at these varied wavelengths, absorption depth is either too shallow to effectively target collagen, meaning additional treatments are necessary, or too deep, which results in needlessly heating tissues in the soft palate.
While we have seen great success at our practice treating snoring with Solea Sleep, laser treatment is not a perfect fit for every type of snorer. For example, patients who have a high body mass index or other lifestyle factors such as consumption of alcohol or caffeine might not see the desired result from laser treatment, especially if pa-
Rapid snoring relief for your patients and significant revenue growth for your practice.
Solea® Sleep is a simple, non-surgical treatment that tightens and stiffens collagen in the soft palate with low-level laser light.*
• Virtually no patient discomfort
• Long lasting, life changing results
• High patient acceptance
The treatment is available through the Solea® All-Tissue Laser - the only 9.3-micron CO2 laser. This novel technology enables you to work on everything from enamel to dentin to gingiva to collagen to bone, gliding through tissue using a variable-speed foot pedal. It’s fast, precise, and reliably anesthesia-free for cavity preps, and blood-free, pain-free, and suture-free for most soft tissue treatments.

SOLEA® ELEVATES SLEEP


tients continue those behaviors post-treatment. To ensure that patients understand the connection between such factors and their treatment success, I recommend taking the time to screen and educate patients prior to treatment, setting realistic expectations so patients can make the best decision for their situation.
3 Ways Laser Dentistry Can Improve Your Practice

Treating snoring with laser dentistry has several potential benefits for patients and dentists, but following are three practice-changing outcomes that I have experienced from using the Solea laser to treat snoring for our patients.
1. Fast treatment won’t disrupt patients’ lives. Treatment with Solea Sleep takes about half as long as I experienced with an erbium laser, and patients can get back to their day with little to no discomfort. Minor irritation from the procedure – patients have compared it to the feeling of drinking a very hot cup of coffee – usually abates within 24 hours, compared to two to four weeks of discomfort following surgical procedures. In some cases, patients report dramatic snoring reduction and easier breathing the night after their procedure. This is good news for patients and it allows you to add new services to your practice without disrupting existing workflows and procedures.
2. Long-lasting relief increases patient satisfaction. Palate stiffness typically increases significantly after treatment with Solea Sleep, and the procedure offers most patients (and their partners) long-lasting snoring relief with little to no discomfort. I have seen such gratitude
from patients, who in some cases report getting a good night’s sleep for the first time in years following treatment. I’ve also heard from patients who say they are sleeping and even dreaming more vividly. As someone who pursued this career to make a difference in my patients’ lives, that is incredibly rewarding.
3. In-house treatment capitalizes on doctor-patient trust. While sleep dentistry is not new to the industry, treatment to reduce snoring has typically required a referral to a sleep specialist or surgeon. Using Solea Sleep has allowed our practice to retain more business by conducting this simple procedure in-house. I have performed more than 200 procedures with Solea Sleep, and I currently do three or four snoring consultations every week despite no longer advertising the procedure. Most of these patients are new to my practice, and while some return to their own dentist for ongoing care, I have retained many as patients. At the same time, I have seen increased patient satisfaction and referrals from satisfied patients without disrupting any other activities.
Just the fact that I can have conversations about snoring with my patients – and offer them real solutions – has allowed me to identify new patients for whom I can provide a better night’s sleep. In addition, the Solea laser allows me to provide services like correcting tongue ties to improve breathing, another significant cause of snoring, rather than referring those procedures out to a specialist. This has allowed me to take my practice to levels I couldn’t have imagined.
As dentists, we all go to great lengths to build rapport and trust with our patients. Expanding into laser-based sleep dentistry offers the opportunity to solidify patient relationships by providing additional services that improve a patient’s – and in some cases, a family’s – quality of life and overall health. My experience with laser dentistry in general and Solea Sleep in particular has allowed me to become more than a general dentist and offer services that change patients’ lives for the better. That’s good for patients, and it’s good for business.
Expanding intolaser-
based sleep dentistryoffers
the opportunity to solidify patient relationships by providing additional services that improve a patient’s – and in some cases, a family’s – quality of life and overall health.
Analyzing the Influence of New 2024 Dental Codes for DSM Services


 by Rose Nierman and Courtney Snow
by Rose Nierman and Courtney Snow
The 2024 CDT codes have been released, and they have introduced some noteworthy additions that have captured considerable attention. As experts in medical coding for dental practices here at Nierman Practice Management, you might wonder why we are discussing new dental codes. Well, thank you for recognizing our expertise! The reason behind our focus on dental codes is the recent inclusion of additional CDT codes specifically associated with Dental Sleep Medicine (DSM). These new codes, effective starting January 1, 2024, complement the three CDT codes introduced in 2022.
We understand you’re likely curious about what DSM services these CDT codes represent. In 2022, the three codes that were introduced represent the oral appliance itself, adjustments, and repair (D9947-D9949). Building on this, the five additional codes for 2024 encompass a reline service for the appliance, morning repositioning appliances, titration visits, home sleep tests, and screening for sleep-disordered breathing (D9953-D9957).
The introduction of the initial codes in 2022, along with the latest additions in 2024, has sparked numerous inquiries within the Dental Sleep Medicine (DSM) community. Questions have arisen, such as: Should we be alarmed by the inclusion of these new dental codes? Does this signify a shift towards dental insurance covering Oral Appliance Therapy (OAT) for Obstructive Sleep Apnea (OSA) instead of medical insurance? Will medical insurers start mandating that services be billed to dental insurance first?
We hold the view that the introduction of these new CDT codes will not have a detrimental effect on medical reimbursement for OAT for OSA. Despite concerns expressed regarding potential claim delays by dental and medical insurers, we approach this situation with a different perspective. It is crucial to remember that the diagnosis determines whether a service is classified as medical or dental and which benefit plan or insurance will cover it. Mere inclusion of a code in either coding system does not indicate coverage; it serves solely as a representation of a service. A pertinent example is a panoramic x-ray, which has a specific code in both medical and dental coding systems. However, whether it is covered by medical or dental insurance is determined by the purpose of the x-ray for the patient. For instance, if the panoramic x-ray is taken for OAT for OSA or to assess Temporomandibular Joint Disorder, many medical insurers provide coverage. Conversely, if the panoramic x-ray is conducted as part of a routine dental visit, it would not be covered by medical insurance.
Although we acknowledge that the introduction of these dental codes related to Dental Sleep Medicine (DSM) may potentially cause confusion regarding coverage, we firmly believe that the medical diagnosis of OSA and the fact that custom oral sleep appliances are prescribed by physicians and classified as Durable Medical Equipment (DME) will ensure their continued coverage by medical insurance.
For clarification, a full listing of codes, or guidance on establishing medical necessity for oral appliance therapy, we aim to help dental practices succeed.
Rose Nierman is the CEO of Nierman Practice Management (NPM) and creator of the DentalWriter Plus+ software. For over 30 years, Rose has taught dental practices successful & ethical medical billing through the iconic Successful Medical Insurance in Dentistry seminars.Changing Standards in Dental Sleep Care
by Diane Robichaud, Panthera Dental co-founder, Dental TechnicianChange is constant. New designs, materials, and manufacturing methods are shaking things up for oral appliance therapy. Comfort, outcomes, and durability have improved. Let’s explore Panthera Sleep’s contribution to this transformation.
Design Philosophy
Oral Appliance (OA) design philosophy must come first before considerations of materials and manufacturing methods.

At Panthera, the design philosophy is about reducing forces on teeth and joints, mitigating risks of side effects, and maximizing patient comfort. Every OA decision originates from this philosophy, starting with selecting the proper retention and titration systems, designing the appropriate bands and plateaus, and carefully measuring the biomechanical impacts of even the smallest change.
The vision is to create the best appliance for each patient. Therefore, we set out to build an industrial platform able to execute this vision at scale without any of the traditional manufacturing constraints.
The Dynamic Duo: 3D Printing and Medical Grade Nylon


Nylon has shown tremendous benefits in the medical device industry. Its mechanical properties allow it to be flexible or rigid as needed, for accurate matching to the most complex dentition and undercut retention while being less bulky, stronger, and more durable than traditional materials. Combining this versatility with industrial 3D printing allows us to create any object of any shape and is one of the two keys to creating truly patient-matched appliances aligned with our design philosophy.
The Software that Powers the Dynamic Duo
The second key is Panthera’s proprietary software, which is purpose-built in-house for the manufacturing of OA. It allows the freedom to execute any design on the CAD side, and for precision, consistency, and speed at an industrial scale on the CAM side. These innovations make the Panthera difference notable.

Blending Design, Manufacturing, and Materials = Quality
Panthera has decades of know-how in the dental world, and is an Industry 4.0 pioneer, combining innovations such as robotics, AI, automation, and 3D printing. Yet quality must always align with innovation, and Panthera’s leadership has engaged the organization with a quality culture from the ground up. Achieving and maintaining over the years the ISO 13485 certification as a medical device manufacturer is evidence of the highest standards for quality management.
The Panthera Whys!
Panthera’s first “why” is the patient. Patients viewing the first-time fit of their OA as comfortable will improve adherence, treatment experience, and satisfaction. Because the patient and their experience matter, design philosophies and manufacturing choices must allow for a no-compromise “Care that Fits” mindset.
Panthera’s second “why” are the providers. Physicians will appreciate the time to treatment, durability, and improvement in adherence. For the dental provider, it is the timeliness, first-time fit rates, and reduced risk of side effects that will minimize problem appointments and, at the end of the day improve profitability. In summary, the blend of design, 3D printing, material, and knowhow results in a perfect combination of technology and quality, dedicated to patient care.

A Successful Case of Combination Therapy Using Myofunctional Therapy, an Aligner Sleep Appliance, and Clear Aligners



 by Maria Sokolina, DDS, D.ABDSM
by Maria Sokolina, DDS, D.ABDSM

Alot of obstructive sleep apnea (OSA) patients have misaligned, crowded teeth that impinge on the tongue space, forcing the tongue into the airway. An Aligner Sleep Appliance in combination with Clear Aligners can address the misalignment of the teeth and achieve restorative goals after orthodontic therapy. Patients can use the ASA with modified clear aligners during restorative treatment as well.
An Aligner Sleep Appliance in combination with Clear Aligners can be a useful solution for practitioners who are preparing their patients for orthognathic surgery to correct OSA. Most patients who seek orthognathic surgery have misaligned teeth and are also seeking surgery because they could not tolerate CPAP therapy.


Abstract
Patients that present with obstructive sleep apnea (OSA) often have co-existing dental conditions including bruxism and dental
malocclusions1-3 (Figures 1-5). Comprehensive treatment for these patients requires customized plans that take into account individual anatomy, medical history, lifestyle, and preferences. This report details one such case in which we were able to significantly improve a patient’s sleep and breathing quality with a combination of oral appliance, clear aligners therapy, myofunctional therapy, and home remedies to relieve nasal congestion.
Introduction
An estimated 2-4% of middle-aged Americans meet the diagnostic criteria for obstructive sleep apnea (OSA), with up to a quarter of men between 30 and 49 years of age potentially experiencing sleep-disordered breathing.4 The gold standard treatment for OSA is continuous positive airway pressure (CPAP) therapy, but adherence to CPAP therapy is low.5 Mandibular advancement devices (MAD) are a common alternative for patients who do not want to use or do not tolerate

CPAP therapy. These devices increase space in the airway by repositioning the lower jaw forward to create more room for the tongue. However, the majority of patients with OSA have dental pathologies, including dental problems such as dental malocclusion, teeth crowding, and loss of tooth structure due to bruxism.1-3 These coexisting conditions can complicate the treatment of OSA, even as treatment of them can decrease the severity of OSA.6 Traditionally, the treatment of dental malocclusion requires the use of CPAP therapy while the patient is undergoing Clear Aligner treatment. This can pose a significant obstacle, as Clear Aligner treatment typically takes 19-24 months.
Here, we describe a case where a patient presented with OSA and CPAP intolerance, as well as bruxism and dental malocclusion. Comprehensive treatment required a multi-disciplinary approach including oral appliances, orthodontic treatment, myofunctional therapy and nasal saline irrigation.
Report of Case
A 60-year-old male was referred to our practice due to CPAP intolerance. His chief complaints were dry mouth, air in the stomach, and dry eyes from the CPAP machine. Patient used nasal pillows and a full face mask during his 3 years of CPAP therapy. The patient has a history of high blood pressure, nasal congestion and chronic sinus infections and moderate OSA. Patient complained of a dry mouth in the morning with or without a CPAP machine. He was informed by his bed partner that he kept his mouth open during his sleep and for that reason he kept a glass of water next to his bed during the night.
Oral examination revealed upper and lower dental crowding and bruxism. The results of the initial polysomnography are presented in Table 1. Upon consultation, the patient expressed the desire to correct the malocclusion and address the loss of tooth structure due to bruxism.
While we were discussing treatment options, I mentioned that surgery could be a viable choice to eliminate my patient’s OSA, once they have fully recovered from the procedure. However, he ultimately decided to prioritize addressing his aesthetic concerns.
The patient was offered two treatment options. The first plan included using a dorsal oral appliance to protrude the lower jaw and
Table 1: Polysomnography Results Before and After Treatment
tongue forward, which would help increase the size of the airway’s lateral dimension. That solution only addresses breathing problems while leaving the underlying dental pathology intact.
The alternative plan was a more comprehensive approach. It included: (1) a referral to a myofunctional therapist to improve tone and function of the tongue, promote nasal breathing, create lip competency (2) clear aligner therapy (Invisalign) in combination with the Aligner Sleep Appliance® (ASA; SleepArchiTx, Newport Beach, CA). Clear aligner therapy would help correct crowding and expand the dental arches, while the ASA would assist in both dental arch expansion and protruding the lower jaw and tongue forward, ultimately increasing the size of the airway’s lateral dimension, (3) Restorations of loss tooth structure due to bruxism with
As a founder and CEO of Harmony Dental Arts, Dr. Maria Sokolina is very passionate about making the world a more beautiful and more healthy place with sound sleep and healthful breathing. Dr. Sokolina emigrated from Russia with her first medical degree, and later received her DDS degree from New York University College of Dentistry. Upon graduation, Dr. Sokolina pursued specialized skills in different areas of dentistry such as implants, cosmetic dentistry, full mouth rehabilitation, and orthodontics. As part of her practice, Dr. Sokolina became an active explorer of the world of Dental Sleep Medicine, trying to find a cure for sleep apnea with dental appliances and myofunctional therapy. Dr. Sokolina is a lecturer and Diplomat of American Academy of Dental Sleep Medicine. Dr. Sokolina is a Board member of the American Academy of Dental Sleep Medicine as well as TEDx. Dr. Sokolina spends much of her professional time trying to spread knowledge with lectures about “Sleep, Breath and Wellness” among the general population as well as in the medical community. She may be contacted through her website at https://www.harmonydentalarts.com/.
Disclaimer: Dr. Sokolina has no financial involvement with SleepArchitx nor with Invisalign.

Zirconia veneers. The patient chose the alternative treatment plan as prescribed.



The goals of the myofunctional therapy sessions were to train the patient to: (1) create direct contact between the tongue and palate; (2) be able to hold his tongue in a flat position on the palate; (3) move his tongue independently from his lower jaw, (4) keep lips together during day and night; and (5) promote nose breathing during day and night.
For the oral appliances, the patient was instructed to wear custom clear aligners 20-22 hours a day and the ASA every night on top of the clear aligners. Treatment for clear aligners and ASA started at the same time (Figures 6-7). Patient had prescribed 20 aligners for the upper arch and 22 aligners for the lower arch. In addition to the protrusion mechanism, ASA has a 5 mm expansion screw to accommodate the expansion with clear aligners. He had a positioner made to use over the clear aligners to reposition his jaw in the morning and was instructed on the hygienic maintenance of all oral devices (Figures 8-10). The patient changed clear aligners every 10 days and monitored the amount of time he was wearing the clear aligners during the day with the TrayMinder Invisalign Tracker app.
The patient received additional home remedy suggestions to prepare him for successful adaptation to ASA therapy. First, the importance of nasal breathing was discussed. Second, the patient was advised to rinse his nose with saline in the morning and evening using the NeilMed sinus rinse squeeze bottle system. Third, the patient was instructed to use tape over the mouth to promote nasal breathing at night. Finally, the patient was asked to use the SnoreLab app on his phone to record his breathing sounds during sleep before and during the course of treatment.
The patient reported rinsing his nose with saline before going to sleep significantly

helped with nasal congestion at night. However, he reported anxiety over taping his lips at night. It was recommended that he begin by taping his lips for 5 minutes during the day to promote nasal breathing and increasing the duration over time.
The patient adapted easily to the combination clear aligner and ASA therapy. After the original insertion, he reported immediate side effects of increased salivation and slight discomfort of dentition, which were addressed in a follow-up phone call. Patient had his ASA advanced 4 mm horizontally and 2 mm transverse during the first 3 months. The patient got through 17 out of 20 clear aligners before the aligners stopped tracking his teeth according to clear aligner therapy standards. The ASA reached a maximum expansion of 5 mm and became less stable due to the full opening of the screw. Therefore, new refinement aligners and a new ASA were ordered after 6 months of treatment. Patient received 22 upper aligners, 18 lower aligners and started the refinement stage with a new ASA appliance. During the treatment plan financial presentation, we discussed the possibility of refining the treatment with clear aligners and ordering a new version of the Aligner Sleep Appliance (ASA) to continue with the expansion of the arches. We explained to the patient that creating space between the anterior teeth would require minimal preparation for Zirconia veneers. This required a new ASA with a new expansion screw to accommodate the existing expansion and achieve an additional 5 millimeters.
The patient filled out the Epworth Sleepiness and Fatigue Scales at each appointment,8,9 and reported that his snoring was significantly reduced. Tiredness and sleepiness improved. On the SnoreLab app, the patient’s Snore Score, based on the average volume and duration of snoring, decreased from 50

at baseline to 30 after 1 month, 19 after 2 months, 10 after 3 months, and 2-4 after 4 months. After 1 year of combined aligner and ASA treatment, a follow-up sleep study was performed by the patient’s sleep physician. As shown in Table 1, multiple measures of OSA severity were improved by the treatment, including the number of apneas, hypopneas, and respiratory effort-related arousals, as well as oxygen saturation. The patient underwent a repeated sleep study with both the Aligner Sleep Appliance (ASA) and clear aligners in place. Upon the completion of active aligner therapy at 14 months, the patient had his teeth restored with Zirconia veneers – from #5 to #12 and from #22 to #27 (Figures 11-13).
After the patient completed their orthodontic and restorative treatment, the retention of the ASA with clear aligners was not optimal. We presented two treatment options: the first was to proceed with the ASA and clear aligners as they were, and the second was to use a new appliance, the Respire Blue, which had better retention and could be worn without the clear aligners. He planned to wear his clear aligner retainers for 2 hours during the day, and ordered a Respire Blue oral appliance (Whole You Dental Laboratory, Brooklyn, USA) with the same settings as the ASA for night wear. The patient was placed on a recall schedule according to standards of the American Academy of Dental Sleep Medicine (every 6 months for the first year and once a year after). 7 He was advised to see his sleep doctor every year for sleep evaluation.

Discussion
The case presented here is a notable example of a complex patient presentation requiring a multi-disciplinary approach. Our patient needed simultaneous treatment for OSA and a dental malocclusion. Clear aligners were paired with a new generation oral appliance, the ASA, to simultaneously correct the malocclusion and alleviate pre-existing OSA. As a result, the patient’s OSA significantly improved (see Table 1) with both
the apnea-hypopnea index (AHI) and supine AHI decreasing from moderate/severe levels to clinically minimal. Our hope is that this report will help guide other practitioners in how dental interventions can be customized and combined with myofunctional therapy and nasal irrigation to treat patients with complex dental sleep conditions.
Combining oral appliance therapy with orthodontic and restorative treatment can be a controversial approach, but an Aligner Sleep Appliance in combination with clear aligners can address the misalignment of the teeth, achieve restorative goals, and provide a solution for OSA patients who have crowded, misaligned teeth that impinge on tongue space and force the tongue into the airway. The use of the ASA with modified clear aligners during restorative treatment can be an effective approach.





It also has the potential to offer a useful solution for practitioners who are preparing their patients for orthognathic surgery to correct OSA. Most patients who seek orthognathic surgery have misaligned teeth and have not been able to tolerate CPAP therapy.
Conclusion
In the future, when you encounter a patient with OSA who is also interested in straightening their teeth, you don’t have to inform them that using CPAP is the only way to maintain proper breathing during clear aligner treatment.
3.
sleep apnea and comorbidities: a dangerous liaison. Multidiscip Respir Med. 2019;14(1):8. doi:10.1186/s40248-019-0172-9
4. Young T, Palta M, Dempsey J, Skatrud J, Weber S, Badr S. The Occurrence of Sleep-Disordered Breathing among Middle-Aged Adults. N Engl J Med. 1993;328(17):1230-1235. doi:10.1056/NEJM199304293281704
5. Weaver TE, Grunstein RR. Adherence to Continuous Positive Airway Pressure Therapy: The Challenge to Effective Treatment. Proceedings of the American Thoracic Society. 2008;5(2):173-178. doi:10.1513/pats.200708119MG
6. Ataii, Payam. Performing Orthodontics While Treating OSA. Inside Dentistry. 2019;15(2). Accessed April 21, 2022. https://www.aegisdentalnetwork.com/id/2019/02/performing-orthodontics-while-treating-osa
7. Ramar K, Dort LC, Katz SG, et al. Clinical Practice Guideline for the Treatment of Obstructive Sleep Apnea and Snoring with Oral Appliance Therapy: An Update for 2015: An American Academy of Sleep Medicine and American Academy of Dental Sleep Medicine Clinical Practice Guideline. Journal of Clinical Sleep Medicine. 2015;11(07):773-827. doi:10.5664/jcsm.4858
Word Search

Dental Sleep Education That Fits Your Schedule
Dental Sleep Education that fits your schedule

The Academy of Clinical Sleep Disorders Disciplines is the only organization offering a fully online and on-demand certificate in Dental Sleep Medicine. Study the lectures and course materials at your own pace, then when you are ready, take the exam. The C.DSM certificate from ACSDD provides the necessary medical and dental knowledge to confidently approach physicians and seek insurance reimbursement.
The certificate is a prerequisite for ACSDD Fellow and Diplomate.
The Academy of Clinical Sleep Disorder Disciplines is the only organization offering a fully online and on-demand certificate in Dental Sleep Medicine. Study the lectures and course materials at your own pace, then when you are ready, take the exam. 12 modules present both the medical and dental science of sleep medicine providing a solid foundation for understanding clinical applications. Most dentists are able to complete the 13 CE program in 4-6 months.
The certificate is a prerequisite for ACSDD Fellow and Diplomate




