
by Erin Elliott, DDS, DASBA









by Erin Elliott, DDS, DASBA







Asthe years go by, we accumulate birthday experiences that stick in the mind. The more years, the more memories we stash away.
My birthday this year will be one of those forever events. A band from England hosted a gathering for me and 40,000 of my friends. Mick Jagger somehow forgot to sing the birthday song, but he more than made up for it with Satisfaction, Wild Horses, and hits he’s been singing for nearly every year of my life.
A comment he made: ‘The first time the Rolling Stones played Vancouver was 59 years ago.’ I try to wrap my head around the value he and the band have brought to the world and the persistence it requires to keep putting out the message, over and over, for 62 years now. It takes commitment to believe your song is what the world needs. It takes an enormous belief in oneself to think that your message is important enough. It means listening to the supporters and learning from the naysayers, not letting either of them distract from what must be done.
You probably have not been a dentist, physician, dental hygienist, speech language pathologist, physical therapist or other health care provider for over 60 years. Your career may not last as long as a singer in a rock and roll band, but it still requires persistence and a belief that your message is important enough to keep pushing it out there, despite the supporters and detractors tempting you to take a different path.
What can fuel this fire? Dr. Pankey talked about the rewards that come to a dentist when four pillars of health are balanced. As he studied human behavior,
his mentor shared teachings from Aristotle that ensuring a balance of work, play, love, and worship resulted in rewards. I’ve always understood these concepts in the most helpfully vague ways – there are as many definitions for each term as there are people who need to learn them. Think about the times you felt most rewarded –complimented, paid, thanked, hugged –whichever was the reward that made you feel your best. As you relive that wonderful experience, explore the balance – was part of it from work you did, as in helping someone breathe better? Did you enjoy the teamwork that made that happen – could that be play? How about being willing to give up other attractive options to dedicate yourself to learning – isn’t that love? If you’ve put a lot of energy and focus into being part of the big profession of medicine, consider the spiritual value of that commitment.
Before going to the concert, I watched a video of how Mick Jagger prepares for the show – the workout he puts himself through at 80 years old to look strikingly like the showman I first saw 41 years ago in Dallas. No one does that work without loving it. The look on his face was serious, but the attitude was playful. The dedication is hundred percent.
If you approach each day in clinic with the whole package I saw on stage last week, you’ll impact your patients like Mick did 40,000 of us. The rewards will come, and they will be enough.
Do you like what you are reading in DSP? Do you have ideas you want to share about what works in your practice? As Chief Dental Editor, I am happy to consider essays from any reader! Contact me at stevec@medmarkmedia.com.

Steve Carstensen, DDS Diplomate, American Board of Dental Sleep Medicine
Cover Story
Don’t Give Up Before the Plane Takes Off: A Journey into Dental Sleep Medicine by Erin Elliott, DDS, DASBA
If it’s been done, it’s possible for you – the right tools help.


Continuing Education
Primary Care Dentistry, Airway, Inflammation, and Life Essentials by Steve Carstensen, DDS, and Pat Mc Bride, PhD, CCSH
Dentists clearly have a role in overall health.
2 CE CREDITS


Medical Insight The Case of the Sleepy Tourist by Alan D. Steljes, MD, FACC, FRCPC
How to shift the timing of our internal clock to beat jet lag.

Medical Insight The Importance of Research by Colonel Scott Williams, MD, FAASM
It is essential to remind the scientific and lay community of the benefits of Mandibular Advancement Therapy.

Physician’s Perspective Polypharmacy Impacts Home Sleep Test Results in OSA Patients Receiving Oral Appliance Therapy by Drs. Preetam Schramm, et al. Prescriptions can change results of your therapy.





Overnight oximetry reporting available when used with Nonin nVision® data management software Compact design wears like a watch, with large display screen and enhanced sensor connector


Long battery life operates for 44 hours on two AAA batteries
6 Publisher’s Perspective “By Changing Nothing, Nothing Changes.” by Lisa Moler, Founder/CEO, MedMark Media
12 Clinician Spotlight Genesis by Tom Colquitt, DDS
Serendipitous music opportunity provides health benefits.
16 Technology & Innovation
Building an Airway Center: A Journey of Systems and Tools by Dr.
Keith Gressell
Details matter, and simplify the care.
20 Expert View
The Dentist May Hold the Key to Unlocking Scoliosis by Mike Cantrell, MPT, AIAFellow
Did you know the dentist can help PT’s with scoliosis patients, and a lot more.
24 Cardio-Sleep Corner The Inner Workings of Our Circadian Rhythm by Lee A. Surkin, MD, FACC, FCCP, FASNC, FAASM
Our circadian rhythm determines sleep and wake times.
38 Product Spotlight Breakthrough: HealthyStart® Introduces new Innovative FasTrack System
Read about this major advancement in treating sleep disordered breathing.
40 Inside the Lab
Welcome to our Technician Series – Lessons from the Bench! by Laura Sheppard, BS, CDT, TE Lessons from the bench.
47 Communications Corner “The Best Decision I Ever Made” by Kalli Hale, DDS, MPH, D.ABDSM
Looking into what comes first turned treatment around.
50 Product Spotlight DynaFlex Herbst and Dorsal Devices Enhanced Patient Compliance
Spend your time on patient care, not on the appliance.
52 Practice Management Medical Billing for Dental Sleep Medicine – Getting Your Ducks in a Row by Rose Nierman
The right codes and the right time mean the right outcome.
54 Product Spotlight Sleep Dentistry Simplified – Sleepifi DENTAL
Automating the process can lower barriers to health.
56 Sleep Humor The Lighter Side of Sleep Apnea...
Fall 2024
Publisher | Lisa Moler lmoler@medmarkmedia.com
Chief Dental Editor
Steve Carstensen, DDS, D.ABDSM stevec@medmarkmedia.com
Chief Medical Editor
Lee A. Surkin, MD, FACC, FCCP, FASNC drsurkin@n3sleep.com
Associate Editor | Lou Shuman, DMD, CAGS lou@medmarkmedia.com
Editorial Advisors
Jamila Battle, MD (Family/Sleep/Addiction)
Steven Bender, DDS
Jagdeep Bijwadia, MD (Pulmonary, Sleep)
Kevin Boyd, DDS
Saim Choudhry, DO (Internal Medicine, Sleep)
Alison Kole, MD, MPH, FCCP, FAASM (Sleep, Pulmonary, Critical Care)
Karen Parker Davidson, DHA, MSA, M.Ed., MSN, RN
Bertrand de Silva, MD, FCCP, D.ABSM
Daniel Gartenberg, PhD (Behavioral Sleep)
Kristie Gatto, MA, CCC-SLP, COM
Amalia Geller, MD (Neurology, Sleep)
William Hang, DDS, MSD
Steve Lamberg, DDS, D.ABDSM
Christopher Lettieri, MD (Pulmonary, Critical Care, Sleep)
Pat McBride, PhD, CCSH
Jyotsna Sahni, MD (Internal Medicine, Sleep)
Ed Sall, MD (ENT, Sleep)
Alan D. Steljes, MD (Cardiology, Sleep)
Laura Sheppard, CDT, TE
DeWitt Wilkerson, DMD
Scott Williams, MD (Psychiatry, Sleep)
Gy Yatros, DMD

National Account Manager
Adrienne Good | agood@medmarkmedia.com
Sales Assistant & Client Services
Melissa Minnick | melissa@medmarkmedia.com
Creative Director/Production Manager
Amanda Culver | amanda@medmarkmedia.com
Marketing & Digital Strategy
Amzi Koury | amzi@medmarkmedia.com
eMedia Coordinator
Michelle Britzius | emedia@medmarkmedia.com
Social Media
Felicia Vaughn | felicia@medmarkmedia.com
Website Support
Eileen Kane | webmaster@medmarkmedia.com
MedMark, LLC 15720 N. Greenway-Hayden Loop #9 Scottsdale, AZ 85260 Tel: (480) 621-8955 | Toll-free: (866) 579-9496
www.DentalSleepPractice.com

• Offer FDA-cleared therapeutic procedures that provide pain relief and rehabilitate force imbalances for new and existing patients
• Provide medically necessary dentistry using tested technologies including ultrasound, photobiomodulation, microcurrent, and muscle manipulation.
• Precisely diagnose and deliver state-of-the-art treatment for chronic migraines and headaches, tinnitus, and other neck/jaw/face pain
• Address an individ ual patient’s symptoms with a drug-free, needle-free treatment plan that has a 95%-100% clinical success rate
• Receive clinical training along with ongoing implementation assistance
• Add a revenue stream to your practice, increasing your non-doctor revenue
• See nearly 389% ROI and only 30 minutes of doctor chair time per case.



Lisa Moler Founder/CEO, MedMark Media
Change is hard – some days it feels like fate is not satisfied with any stable situation that makes us comfortable and secure. Sure, no one can dispute the serenity of “business as usual” in the midst of ever-changing world issues, politics, and everyday craziness. Instead of losing sleep or stomach lining over change, let’s consider the positive aspects of being open to expanding our comfort zones, living in the moment, and having a mindset of “faith over fear.” As the title quote from Tony Robbins suggests, you have to build up some momentum in order to actually get somewhere. Let’s hear from some successful and inspirational people on how change can bring positive movement to our lives.
Neurologist and psychologist Viktor E. Frankl said, “When we are no longer able to change a situation, we are challenged to change ourselves.” Some people just need a bigger push to get moving. Taking the easy route and sticking with “the familiar” is only possible until the stress of the known outweighs the fear of the unknown. So, sticking with only the activities or mindsets that are within your safety zone, will eventually leave you watching others who have the ambition and confidence to move forward. You don’t want to look around in a few years and see your friends and peers busy and fulfilled with new possibilities that can change your community or your world. There is a lot of competition out there, and being a pioneer or game changer may be a challenge at first, but will head off the future frustration of a stagnating life.
Actress Sarah Parish noted, “Living with fear stops us from taking risks, and if you don’t go out on the branch, you’re never going to get the best fruit.” Overcoming fear of making the wrong decision or failing can feel daunting. But, there are a lot of ways to build your confidence, such as talking to friends, mentors, experts, attending conferences, reading MedMark publications, and listening to those who bring you inspiration. There will be learning
curves and maybe even some speed bumps, but most times, innovation will lead to new and exciting ways to grow.
Our fall issue is filled with innovation and information to create productive change in your practices. In our Cover Story, Dr. Erin Elliott talks about dental sleep medicine and some of the technologies that allow her to screen patients properly, treatment plan effectively, and enhance patient outcomes. Our CE, by Dr. Steve Carstensen and Pat Mc Bride, offers ways the primary care dentist can take the time to know the unique patients in their chair and apply that knowledge to facilitate improved whole-health choices. Trending topics in medicine are a focus in this issue –articles cover circadian rhythms, preventing jet lag, raising awareness of the value of mandibular advancement therapy, and how a physical therapist and sleep dentist dynamic duo co-treated a patient’s scoliosis.
World famous performer Robin Williams said, “No matter what people tell you, words and ideas can change the world.” Don’t leave your success to chance. Change your ideas into action. Innovation will create a happier you, family, and work life. When you embrace change, the benefits will spread throughout your world! To your best success.

by Erin Elliott, DDS, DASBA

From an early age, I was certain my future lay in medicine. I had my sights set on being a trauma surgeon, but when I thought more about work-life-balance, dentistry emerged as a natural choice, influenced by my father, who was also a dentist.
Creighton University School of Dentistry opened my eyes to the breadth of what dentistry entailed by offering substantial hands-on experience, allowing me to perform a variety of treatments and specialty work, but at the time, no sleep medicine. When I first started practicing, my perception of dentistry was conventional – I was a “drill and fill” dentist, handling routine dental care and referring out more complex cases. My perspective changed dramatically in 2008 at the Idaho State Dental Convention. I attended a session where a sleep physician spoke in the morning and a dentist specializing in sleep and TMJ disorders presented in the afternoon. This was a revelation. I love to sleep, always go to bed early, and am always the first to leave a party. I was fascinated by the potential to merge my personal love of sleeping with my professional life. Despite the early state of the field at the time and the skepticism it faced, I decided to delve into dental sleep medicine.
Implementing dental sleep medicine into my practice was not without challenges. Initially, I struggled to integrate my team into this new focus, mistakenly trying to handle everything on my own. Our practice consultant even doubted the viability of incorporating sleep medicine. I wasn’t always sure this plane would take off, but I was determined. Initially, medical insurance denials were a significant hurdle. When dentists encounter such rejections, it can be discouraging,
leading some to prematurely conclude that dental sleep medicine is not feasible. My approach was relentless – I refused to give up and was committed to finding solutions. Navigating the complexities of medical billing has become much easier, not just because our practice knows more, but insurance companies are understanding the benefits, too.
Patient denial is still a hurdle. Many patients tend to dismiss the severity of their condition, sometimes putting up defensive walls. In such cases, I learned to plant a seed of awareness and move on, understanding that persistence and patience are key.
One of my earliest and most impactful cases was my own father. He exhibited numer ous signs of sleep apnea – snoring, bruxism, a retrognathic profile, acid reflux, and a sensitive gag reflex – but never thought much about it. The results of a sleep test were alarming; he had moderate to severe sleep apnea, with his heart working excessively hard during what should have been restful sleep. An oral appliance had an immediate and profound effect. His snoring ceased, his heart rate stabilized, and my mother’s insomnia improved as a result. Witnessing such a transformative impact on my own family reinforced my commitment to dental sleep medicine.
My journey into Solea® Sleep (an application on the Solea® All-Tissue Laser by Convergent Dental) began out of necessity. I was encountering patients with severely compromised airways who, despite using dental appliances, continued to snore. Traditional treatments like surgery were not


ideal due to their low success rates, high costs, and painful recoveries. I knew we needed a non-invasive solution to effectively address these issues. Solea Sleep stood out for its ability to tighten and shrink airway tissue, reducing snoring by making the tissue healthier and less collapsible. As a general dentist, I was also drawn to Solea’s versatility for both hard and soft tissue applications. Solea is known for reliably anesthesia-free, pain-free restorations that enables more same-day, multi-quadrant dentistry. And unlike diode lasers, which often char and smell unpleasant, Solea offers a virtually blood-free, cleaner, more effective solution for soft tissue. This was particularly appealing for procedures like crown lengthening and subgingival work, which we

Erin Elliott, DDS, DASBA, left Southern California for Western New York to play collegiate soccer at Houghton College, where she graduated summa cum laude. After graduating from Creighton University School of Dental Medicine in the top five of her class, she began her general dentistry career in North Idaho. Dr. Elliott has a special interest in dental sleep medicine, which comprises a large part of her practice. She has lectured extensively on this topic and loves to help general dentists extend this lifesaving service to their patients. She is an active member of the Idaho State Dental Association, the American Academy of Sleep Medicine, American Academy of Dental Sleep Medicine, and is the past president and a diplomate of the American Sleep and Breathing Academy. In addition to speaking to study clubs and at dental meetings, Dr. Elliott teaches a two-day sleep apnea course at 3D Dentists in Raleigh, North Carolina, with Tarun Agarwal, DDS, as well as privately coaches practices about sleep medicine.
perform frequently in our busy practice. Solea is also ideal for releasing tethered oral tissues.
My previous attempts at tongue tie releases with a diode laser had been unsatisfactory. The Solea training we received from Anthony Bolamperti, DDS, a former Creighton University instructor of mine, revolutionized our approach to these procedures. The results were immediate and impressive, with minimal bleeding and quicker healing, significantly benefiting our pediatric and adult patients and their airway health.

Our practice has seen a surge in demand for these services, driven by increasing patient awareness about the benefits of nasal breathing and the impact of tongue ties on overall health. This shift is in stark contrast to the early days when discussions about tongue ties often met with indifference or outright shock that I would suggest such a thing, as there was not a lot of information available to the benefits and impact.
One of the most rewarding aspects of using Solea Sleep specifically is the lack of post-operative pain and complications. Unlike other surgical interventions, patients experience minimal discomfort and we avoid the usual barrage of post-op calls. This not only enhances patient satisfaction but also strengthens the bond we build with them throughout their treatment journey.
I had a patient whose airway tissue was damaged after years of snoring, resulting in persistent noise even with the appliance functioning at its maximum clinical efficacy for sleep apnea. His compromised tissue continued to vibrate until we deployed Solea Sleep: we tightened and stiffened the tissue in his soft palate which solved his snoring problem! The added benefit? He reported significantly improved breathing during the day as well.
Both Solea and Solea Sleep have integrated seamlessly into our practice, improving patient outcomes, and expanding our ability to address complex airway issues comprehensively.
Understanding that each patient is unique
is crucial. I focus on their individual stories and needs. While oral appliances can be highly effective, I recognize that a multifaceted approach is often necessary.
A critical step in our process is always conducting a sleep study before treatment. During exams, I look for anatomical signs and symptoms indicative of airway problems, such as a swollen uvula or excessive soft tissue. For patients with poor tissue quality, we combine Solea Sleep with dental appliances to provide a comprehensive solution. By setting realistic expectations, we ensure patients understand that while appliances can manage nighttime airway issues, Solea Sleep can be essential for long-term tissue health. Starting with simple, cost-effective solutions and gradually exploring other treatments ensures personalized care and better outcomes.
I actively engage with my community to spread awareness, leveraging personal connections with local physicians, trainers, nutritionists, and optometrists. My husband often remarks that he can tell the difference between my dental and sleep patients when we are out in our small community. Dental patients will usually greet me warmly, but sleep patients go a step further – they introduce me to their families exclaiming, “This woman saved my life!”
A patient’s sister died from sleep apnea, which had caused her heart to enlarge. Motivated by her sister’s death, she lost ninety-eight pounds and kept it off, but her CPAP machine was not effective. She turned to us and, with an appliance, finally felt rested and stopped snoring. This story underscores the importance of offering alternative treatments for those who struggle with traditional methods.
We often help overlooked patients who don’t fit the typical profile of sleep-disordered breathing, like women with chronic insomnia and fatigue, often dismissed as stress or anxiety. Many of these women are given night guards that do not help, or even if they had a sleep study, were told they only had mild issues. I passionately advocate that chronic insomnia in women should be considered sleep-disordered breathing until proven otherwise.
One such case involved my partner, Kelly Harness, DMD. Despite being a “young, fit female,” she had upper airway resistance, considered herself a light sleeper, and regularly woke up to use the bathroom. After learning
more about dental sleep medicine as I integrated it into the practice, she realized these were signs of deeper issues. She started using a ProSomnus EVO Select appliance with a discluding element for her clenching symptoms and now sleeps deeply, waking up refreshed and ready for the day.
Educating patients on how sleep issues affect more than just snoring – highlighting impacts on blood pressure, nocturnal bathroom visits, and overall health – helps them understand the urgency. The most fulfilling part of my job is witnessing the transformation when patients, initially skeptical or resistant, embrace the treatment and experience significant improvements in their quality of life.
In essence, my practice aims to provide individualized care, addressing the unique needs and concerns of each patient. Whether through appliances, Solea Sleep or other treatments, the goal is to help them achieve better health and well-being, making every effort and every story worth it.
When considering dental sleep medicine, start with your “why.” If your primary goal is financial gain, rethink your motivation. Adding sleep medicine is not like adding a dental procedure such as implants; it requires a longer commitment and a different mindset. Success in this field demands persistence, especially when it seems like progress is slow.
Focus on the impact you can have on patients’ lives. Hearing from just one patient that you have changed their life can be incredibly motivating. Over time, patient referrals will grow organically, and your practice will thrive without extensive marketing. Remember, dental sleep medicine is about offering comprehensive care that extends beyond just teeth.
One of the most valuable resources in building my sleep medicine practice has been my mentor, Dr. Kent Smith. He is double board-certified by the American Board of Dental Sleep Medicine and the American Sleep & Breathing Academy (where he previously served as president) and is widely considered to be a pioneer in the field of dental sleep medicine. His guidance and education have allowed me to follow and thrive in our shared passion for dental sleep medicine. Where pos-
sible, find yourself a mentor to learn from their experience and lean on for advice.
I also have a close-knit group of dental sleep medicine colleagues, and we convene annually to discuss best practices, case challenges, and emerging trends. This mastermind group, similar to a study club, provides vital support and shared knowledge.
Additionally, the American Academy of Sleep Medicine and the American Academy of Dental Sleep Medicine offer essential guidance on medical insurance and practice standards. Staying updated with new research, case studies, and ongoing mentorship has been crucial in maintaining a successful and informed practice.
This journey has been both challenging and rewarding. Integrating dental sleep medicine has allowed me to enhance my practice and provide comprehensive care that addresses both dental and overall health. It is a reminder that in the pursuit of excellence, staying open to new ideas and persistent in the face of obstacles can lead to transformative outcomes.
The path for dentists entering this field is now clearer, with better tools and more educated patients driving the demand for innovative treatments like Solea Sleep. My final message to dentists is threefold:


First, even if you do not want to treat patients or handle medical billing, at least screen for sleep breathing disorders and find a reliable referral partner. Do not leave these people without help!
Second, having the right technology is important for proper screening, effective treatment planning, and enhanced patient outcomes. Advanced tools like digital imaging, intraoral scanners, home sleep study machines, and Solea laser therapy streamline processes and improve quality of care.
Finally, remember that this journey requires patience – a long runway before the plane takes off. Do not give up too soon. The rewards, both personal and professional, are truly worth it.
by Tom Colquitt, DDS
The Pulmo-venture started as a joke. Perhaps a rant of sorts, but certainly a joke-song. The joke highlighting the ever confusing if not crushing world for our patients and the predicament we found ourselves in as their dental providers. Our patients with breathing disordered sleep and an AHI of less than 5 received no allowable treatment from the medical/health insurance providers, and these people were sick. Very sick.
Snorin’ heartburn pissin’ sweatin’ on my face
Couldn’t get to sleep last night.
Woke up feelin’ ‘zactly like I ran a race
Nothin’ seems is goin’ right.
I’m Back in The UARS, boy!
You know my life is a mess, boy!
Knowing our limitations in a medically based system, we dentists knew these people needed much more than a pat on the head and a tear sheet recommending melatonin and bedtime rules. We needed to address gaps in the dental- medical health system, educate others on what could be done, and get treatment options that could potentially save lives.
Back then, being blessed/cursed with a longstanding practice of ranting about things that troubled me, I wrote the song sharing the peril of a human being suffering from UARS in a medical system actively trying to erase that term. It captured the existential plight for our patients and the dance we “Airway Centered
Dentists” were stepping to, on a floor that was as uneven as it was slippery, given the scrutiny from our medical colleagues.
Set to the tune of the Beatles’ “Back in the USSR,” the song became an anthem of sorts. A public health crisis/acknowledgement of the gaps and breaks that left our patients in the dust.
Went to see my doc, said “What you gotta do…
Need to go and take this test
Sleep Doc he says “Fella, I cannot help you.” It is not OSA, it’s UARS.
I’m back in the UARS, my health insurance’s a mess, boy!
The song was also a bridge. A bridge to needed collaborators, both clinical and musical. Like any anthem, the song needed a band to promulgate the message. Much later, a murder of musical crows would fulfill that hope.
In the past 25 years I’ve learned more and have met more wonderful new people than in the first 30 years of my restorative practice. Keith Thornton, Mark Cruz, Barry Raphael, Bill Hang, Kevin Boyd, Scott Neish, Roger Price, Ted Belfor, Darin Ward, and so many other thought leaders. Colleagues. Mentors. Friends. Turns out some of them are also rather good closet musicians. Barry’s a bassist. Scott’s a guitarist. Darin sings and plays a mean blues harp. Between our dental airway machinations to change the world, we found ourselves conspiring to get together in Shreveport so we could record “UARS” in my music room.
Six years pass. There are lots of conferences, lots of talk, and the needle begins to move. But there is no music in Shreveport.



Rapid snoring relief for your patients and significant revenue growth for your practice.
Solea® Sleep is a simple, non-surgical treatment that tightens and stiffens collagen in the soft palate with low-level laser light.1
• Immediate relief with minimal discomfort
• Takes only minutes to administer
• High patient acceptance
The treatment is available through the Solea® All-Tissue Laser - the only 9.3-micron CO2 laser. This novel technology enables you to work on everything from enamel to dentin to gingiva to collagen, gliding through tissue using a variable-speed foot pedal. It’s fast, precise, and reliably anesthesia-free for cavity preps, and allows for many soft tissue surgeries to be blood-free and suture-free.2
Learn more at convergentdental.com/DSP

Then, Steve Lamberg happens.
An avid dental sleep clinician with the jovial gait of an impresario, Steve hosts an annual spring meeting on Long Island called PAANNY. For the event in May 2022, he asked me to give a talk. With James Nestor as Keynote, it feels like a culmination. Nestor has single-handedly landed our decades of clinical airway investigations on the proverbial layperson’s map with his book Breath; PAANNY promises and proved to be a come-to-the-river sort of meeting, and the launching pad of The Pulmonauts, the name we chose for our band, from Nestor’s book. Airway explorers. On a Mission.

“We choose to go to the Moon in this decade and do the other things, not because they are easy, but because they are hard.” – JFK
The call to step into airway dentistry has not been dissimilar.
We jumped at the chance to do “UARS” and other “airway message” songs with rewritten lyrics decrying mouth breathing and chronic fatigue. “Doctor, My Nose!” “Every Breath You Take!” “I’m Only Sleeping!”
But: no battle plan survives first contact with the enemy.
The band met two days before PAANNY in Barry’s garage in Clifton, New Jersey. With coffee-stained, pen-scrawled cheat sheets in hand, all five of us slogged away at the other reality of being in a rock band: unpacking and repacking heavy equipment. Our song list was equally demanding. Before we know it, the hours spent together felt like we’re not
In 1970, after graduating from Baylor College of Dentistry, Tom Colquitt, DDS, began practicing in Shreveport, LA where he still maintains a private practice. His practice has expanded beyond Dentistry and “Dental Sleep Medicine” into reinventing a new multidisciplinary medical model focused on detecting and correcting dysfunctional breathing in patients of all ages. Dr. Colquitt has been addressing and studying nocturnal sleeping/bruxism issues since the 1970s and treating nocturnal breathing issues with oral appliances since the 1990s. Additionally, he has been an adjunct professor in the Sleep Fellowship Program at LSUHSC medical school in Shreveport, LA since 2007. He is a former trustee of the Baylor College of Dentistry and a fellow in the American College of Dentists. Dr. Colquitt is past president of Baylor Century Club, Northwest Louisiana Dental Association, Ark-La-Tex Dental Congress, Southwest Academy of Restorative Dentistry, American Academy of Restorative Dentistry, and International Academy of Gnathology American Section.
in Barry’s garage, but in the Lion’s Den of the creative process. If you’ve ever tried to pull anything creative off with little time, you know the pressure that swells inside. Add that to my own condition of congestive heart failure and a burning desire to do something monumental, and you know where this story is going…
Fact is, I’ve been at this game before. The music game.
First on my own and then with my band, “Tom & The Cats.” The music was a calling that dental school in the 1960s didn’t quite return. I will never forget the first time I heard The Beatles. I Saw Her Standing There came over those radio waves like a siren cutting through the heat of the night. I bought four album copies the next day so my band could all learn it.
Cut to: Barry’s garage.
Nestor is a drummer, too. He agreed to join us in the name of airway exploration, and it became apparent we’re missing a key ingredient: time.
Time is required: it’s how a band gets to know each other, hear each other, trust each other. Our shared airway mission isn’t enough. The pressure in my chest mounted, knowing we were stepping on stage the following night. The smile of a tall red-haired woman is all I needed to get through this launch. I Saw Her Standing There. I met Samantha Weaver in line at the hotel. She threw her proverbial arms around me and enthusiastically shared that she is going to be singing with us on stage. Good move, Barry! She’ll go on to relish that first gig, but from my perspective, we crash like Hindenburg.
Even with a niche celebrity author and a touch of glam to lift the vocals, the reality of tech breakdowns made it near impossible to hear each other over the din of cocktail chatter. Starting songs is an adventure without a countdown! Nestor exited the stage early to get ready for his more important gig, The Keynote. Spinal Tap for Dentists isn’t his jam. It left us sans drummer and with a lot of improvisational vocals on the part of Darin and Sam, who thankfully were up for it. Remember my heart condition? I returned home dehydrated and filled with fluid in my lungs. Upon doctor’s orders, it took weeks to recover.
September 2022
Fall has arrived in Shreveport. The angle of the sun has softened its harsh glare. I’m tossing the ball for my dog, Bella, when I get a call.
Barry: Tom, you ready for this?
Me: Hell, no…
Barry: We’re doing it. Again.
Me: Pulmonauts? You gotta be *%#@ing me.
Barry: Nope. It’s happening. You in?
I think about it for a few days. Mostly about that missing ingredient we did not have before: time.
On subsequent zoom calls, Barry and the mighty Jen Kirkham work to sell their vision: a dinner-theatre style oeuvre performance for Collaboration Cures 2023 in Orlando, Florida. Never mind that the 10 of us all live in different parts of the country. Plus, we have new bandmates. Even with the luxury of time, how the hell are we going to pull this off? (Enter the Lion’s Den.)
What happens over the next twelve months is nothing short of a miracle.
We pull it off.
10 remote musicians who meet only twice in person requires more than time. Turns out that missing ingredient is collaboration.
As I get up on stage in front of the crowd of 500 in Orlando that following September, my
heart has other plans.
I’ve been holed up in my hotel room for two days, barely able to walk, talk, or eat. I’ve got a fever, and the blinds are drawn. Bandmates arrive at my door, fear in their eyes. They know my season could be coming to a close. The angle of the sun has shifted.
Dave McCarty – dear friend, MD, and our appointed band Mojo Coordinator – knows that if I can only get on stage for “UARS,” that will be enough.
My bandmates are now deeply bonded to the whole of our system. With one man down, each player beams energy into my soul, between glances, hugs, smiles, and the act of playing music together. This translates into me singing the hell out of “UARS,” tears streaming down my cheeks by the closing act, “This is Me.”
What I did not realize is that I wrote that anthem to save others. That song ended up saving me.




by Dr. Keith Gressell
When summarizing the development of your practice style and office operations, no quote is as succinct and precise as this one from James Clear: “You do not rise to the level of your goals; rather, you fall to the level of your systems.” I had lofty goals when I purchased my office and decided to convert it into my vision of an Airway Center. Initially, my systems did not match these lofty goals.
After a period of trial and error, I discovered many ways not to establish my Airway Center. I regrouped and focused on improving my systems and protocols, which revealed the steps necessary to create the Airway Center I envisioned. Two crucial tools emerged as essential in this process: a reliable and comprehensive home sleep test (HST) and extensive training in laser therapy for treating obstructive sleep apnea (OSA).
Traditionally, diagnosing OSA required overnight polysomnography tests conducted in sleep clinics. The Zmachine Synergy offers a convenient alternative to in-lab sleep studies, allowing patients to test in the comfort of their own homes. This device is patient-friendly and easy to use. General Sleep offers a streamlined, dentist-centered approach to obtaining an accurate diagnosis from a board-certified sleep specialist. The interpreted report includes treatment recom-
mendations and alternatives following best practices in sleep medicine. The Zmachine Synergy HST simplifies the diagnostic process, increasing patient compliance by reducing the steps they need to take.
The Zmachine device provides extensive information, combining FDA-cleared EEG-based sleep staging technology with a full complement of respiratory sensors and tri-axis body position monitoring. It is a 9 channel, Type II device that is also very affordable. The EEG is collected from the mastoids and is self-applied by the patient, making it easier on both the practice and staff.
From day one, my choice of laser was clear. The Lightwalker laser from Fotona is a dual-wavelength laser utilizing Er:YAG and Nd delivery systems at 2940nm and 1064nm, respectively. This laser system allows me to treat snoring and address soft palate collapsibility, a potential factor in OSA, using the Nightlase C3 protocols. This treatment naturally opens the airway, aiming to achieve the same results as wearing an oral appliance therapy (OAT) or continuous positive airway pressure (CPAP) device without the need for these devices or their potential side effects. While not a full replacement treatment yet, it is an excellent option for patients with tolerability or compliance issues and can be used as an adjunct treatment.
The Fotona Lightwalker laser, with its patient comfort and compliance benefits, is

Comparing apples and oranges? Comparing apples and oranges? It's important to use the same tool for titration It's important to use the same tool for titration as used for diagnosis. as used for diagnosis.
Autoscoring included - Great for titration.
Nationwide network of RPSGT and Sleep Physicians for scoring, interpretation and telemed services.
Extended battery life for multi-night studies. Easiest to use and most affordable Type 2 HST.



“This laser system allows me to treat snoring and address soft palate collapsibility using the Nightlase C3 protocols.”

a valuable addition to a dentist’s toolset for treating airway restrictions. The procedure’s ease, coupled with no pain or downtime following treatment, made it the clear choice for me. I have seen other companies’ options for similar treatments and own some of those lasers. However, the Nightlase C3 protocol, as taught by Dr. Harvey Shiffman for Fotona, is the most patient-friendly and successful treatment for soft palate collapsibility in patients with snoring or OSA issues.
The combination of the Fotona laser and the General Sleep’s Zmachine Synergy home sleep testing device became the diagnostic and treatment cornerstones of my practice.

Dr. Keith Gressell grew up in Scranton, PA. After graduating from The University of Scranton in 2001 with a BS in Biology/Physics, he moved to Philadelphia to attend Temple University School of Dentistry where he graduated in 2005 with a DMD degree. He then joined the US Army as a Captain and was stationed in Landstuhl, Germany. After completing his service obligation in 2012, Dr. Gressell obtained his German Dental License (Zahnärztliche Approbation) and worked in private practice in Wiesbaden and Ramstein, Germany, which serviced military family members, US Consulate staff, and Expats alike. Dr. Gressell enjoys all aspects of General Dentistry, with a focus on Airway Management and Development. That “focus” incorporates an Overall Health approach and desire to discover and treat the SOURCE of a patient’s issues. In 2017, he moved to San Antonio, TX and worked in private practice with his wife, Jackie, for 2 years before eventually relocating to her hometown of Gig Harbor, WA in 2019. In January of 2021, Dr. Gressell was appointed as a Board Member with the Washington State Department of Health. He is the dentist member on the Board of Denturists. He is active on the lecturing circuit and is one of the keynote speakers at the Fotona Laser Symposium in October 2024. Dr. Gressell is a member of a number of multiple interdisciplinary societies. Additionally, Dr. Gressell is the inventor of Linguaguard – a dental suction device that is used to aid the dental assistant in suction and cheek/ tongue retraction with the use of only one hand.
This powerful and transformative combination benefited both my practice and my patients. It eliminated guesswork about whether patients would be tested in a timely manner and if they would follow through with the necessary steps. Each extra step you eliminate increases compliance rates exponentially.
One of the most critical uses of the Fotona laser and Zmachine device is in titration and post-treatment studies. Many colleagues rely on attended polysomnography for initial diagnostic studies and then use non-FDAapproved sleep tracking devices to determine treatment effectiveness. I prefer using the same HST for pre-, mid-, and post-treatment efficacy to provide consistent “apples to apples” comparisons. This approach also allows patients to see the clear, easy-to-read results themselves, which is invaluable for skeptical patients. Having a third-party diagnostician with no vested interest recommending the best treatment based on objective data ensures the best interest of the patient is maintained. This teamwork approach to therapy and treatment ensures top-notch care and personalized treatment, resulting in better breathing and better sleep for more patients.
The landscape of dental sleep medicine is constantly evolving. The most important advice I can give fellow dental sleep professionals is to continuously educate themselves on the most effective testing and treatment options available for OSA patients. My desire to maintain and enhance the services my dental sleep practice offers is a constant in my professional activities. I am always looking for ways to expand my knowledge base in the field of dental sleep medicine, from sleep testing tools to therapy options. This ongoing process involves analyzing, revising, and improving my processes and ensuring that checks and balances are in place. I hope that other dentists can gain insight from my experiences and use them as guideposts to achieve their goals of establishing a patient-centered dental sleep practice.
To learn more about General Sleep’s Zmachine Synergy, visit http://www.generalsleep. com/.
Restful I + Billing Intelligence is the only complete solution built to help dentists treat more sleep patients and get paid.
Restful I + Billing Intelligence is the only complete solution built to help dentists treat more sleep patients and get paid.

ALL-IN-ONE SOFTWARE
ALL-IN-ONE SOFTWARE
✓Follow required protocols
✓Follow required protocols
✓ Manage documents and tests
✓ Manage documents and tests
✓ Automate communications
✓ Automate communications
✓ Empower referrals
✓Guaranteed Credentialing
✓Guaranteed Credentialing
✓ Hands-on training
✓ Hands-on training
✓ Ongoing support
✓ Ongoing support
✓ Clea ringhou se & payor portal integration



by Mike Cantrell, MPT, AIAFellow
The dentist has incredible power to control body movement. As movement specialists we know of this power because we observe it on a near-daily basis in our practice. The key? Our practice is with two dentists – Dr. Alice Lam in Houston, Texas and Dr. Elizabeth Caughey in Atlanta, Georgia. We spend a great deal of time on Delta Airlines traveling from Central Georgia and Southern Utah to Houston, Texas. But the travel is worth it because of the power that you, the dentist, hold within your skill set. James Anderson, MPT, AIA Fellow, and I have spent over 20 years training physical therapists and dentists how to properly wield and control that power together, as a team. The idea is slowly taking hold. If you’re familiar with Harry Potter, then our academy is the Hogwarts of interdisciplinary practice.
It is nothing new for a PT to work with a dentist. PT’s have helped dentists with TMJ patients for years. But, neither PT’s nor dentists are aware that the dentist can help PT’s with scoliosis patients, and a lot more…
In Houston on a sunny morning, we had a 14 year old young lady (let’s call her Kim) enter the clinic with her parents. Mom and Dad are both dentists, and they had heard of the unique work we did with Dr. Lam. They hoped we could help their daughter. She was diagnosed with a significant 43 degree dextro-rotary thoracic scoliosis. She had been in physical therapy twice a week for about two years during which time she did a variety of exercises designed to control her curves or, hopefully, reduce them. She wore a Boston brace 23 hours per day as well. Unfortu-
nately, her curves were not reducing and, in fact, were increasing. She had a Risser score on entry into our clinic in the order of 2/5 so there was still some skeletal growth that could take place. A Risser score is determined by an X-ray of the pelvis and assessing iliac crest cartilage growth.
A low Risser score causes concern for an orthopedic surgeon who straightens spines using Harrington rods or similar, because there is potential for the curves to worsen as they grow. We, however, see a low Risser score as an opportunity to “bend the sapling” in the direction desired…conservatively. In other words, we see the low Risser score as potential for the curve to improve/reduce.
Interdisciplinary initial examination of the scoliosis patient is designed first to establish into which hemisphere the patient is attempting to shift her Center Of Mass (COM). This is done by using specific markers of determination in the pelvis (the lower extremities), the rib cage (upper extremities), and the head and neck (using the neck and occlusion). Accurate measurements of range of motion (ROM) of all of these areas give powerful indications regarding orientation of the body. Kim oriented her pelvis into the left hemisphere of her body while the rib cage and neck was in the right hemisphere. Was the orientation causing the scoliosis? Was the scoliosis causing the orientation?
The answer is yes! But there is more. There is a genetic marker for scoliosis. This was disclosed by Al-Othman AA et al. in the Asian Spine Journal in 2017. It was pointed out that at the allelic level, marker DS1034 was significantly associated with AIS (Adolescent Idiopathic Scoliosis) patients and their fathers. This allelic marker on chromosome 19p13.3 appears to be important in AIS etiology.5 Considering the possible genetic link for scoliosis, we should also consider that work to reduce scoliosis is always juxtaposed with this possible genetic predisposition.6 This is not to say that conservative reduction of curvature is impossible. It is to note that we are always working with an ongoing skeletal distortion that can progress as long as the child is growing and that there is a strong drive to do just that.
This is important for the physical therapist to know as this understanding can help us realize that the work we do with a child with scoliosis should be a body-generated
treatment plan that is globally diagnostic. It should also be monitored closely and carefully through to skeletal maturity.
It is also noteworthy to understand that there is an association with crossbite and various malocclusions and scoliosis.1,2,3,4 This information is crucial to both dentists and physical therapists. One can infer that the curve in the spine is potentially present into the cervical spine, the cranium, in the maxilla and subsequently in the occlusal scheme. All of this must be considered and addressed.
Kim’s exam showed that she had significant asymmetric limitations of range of motion that allowed us to categorize her body position (orientation of the COM), but it also showed tremendous limitations in cervical range of motion. There was almost no freedom of movement of the cervical spine. This sort of finding is problematic in a healthy adult but in a developing adolescent it is alarming. No 14 year-old young lady should have the stiff neck of a 75year-old! Kim did.But we also saw a possible reason for that stiffness. Kim was wearing braces.
Kim had been in braces for approximately 2 years before we saw her, and we learned that the orthodontic progress was going poorly. We had enough reason to believe that the orthodontist was up against a wall called a low Risser score. As long as there was a strong drive for the scoliosis to progress, the
“Orthodontics potentially holds a key for preventing increase of scoliosis.”

Mike Cantrell, MPT, AIA Fellow, is a physical therapist and is the cofounder of Applied Integration Academy® along with his partners James Anderson MPT, AIA Fellow, and Alice Lam, DDS. Mike pioneered the grassroots, onsite interdisciplinary application model that is at the heart of the Applied Integration Academy. He has over 35 years of medical practice experience developing course content for physical therapists, dentists, myofunctional therapists, and optometrists as well as for the strength and fitness community. His efforts in this realm have led to consultations with countless clients across the US, Europe, Asia, and Australia. He has quietly been consulting with professional athletes in the NBA, MLB, MLS, the NFL, FIFA, UEFA, and Australian Football. He also is a performance consultant for the US Navy seals. He has authored or co-authored countless scientific papers over the past 20 years clarifying issues regarding biomechanics, dentistry, and human movement. Mike and his wife, Tammi, live on 600 acres in central Georgia, have five grown children, and enjoy the outdoors and country living.
ortho was going to be challenging. We also surmised that as long as he continued to fight that battle, we would never be able to reduce the scoliosis. This led us to a small request.

That morning, we asked her parents if they were ok with pausing the orthodontia; at least until we could gain some control over the scoliotic spine. They were in agreement and by the afternoon the ortho wire was removed and Kim returned to the clinic for a reassessment. The evaluative findings were stunning. All of Kim’s findings revealed a nearly body-centric position of the center of mass. This was in all areas previously tested: pelvis, rib cage, and neck were all equilibrated. The neck had full ROM after removal of the orthodontia as did all her extremities. This is significant and allows us as movement specialists to begin a program designed to teach Kim how to move efficiently and without compromise to her airflow, from one hemisphere to the other.

Once the braces were removed, we initiated very specific breathing exercises designed to alter the position of the spine via the diaphragm. This is important as the rib cage is responsible for control of the spine and not the other way around. Additionally, the diaphragm is responsible for control of the rib cage’s position.10,11 Further, training of the functionality of the diaphragm enhances thoracic mobility.7,8,9 So, for Kim, a program designed to reduce spinal curvature had to involve control of the diaphragm to correct her airflow. Not to improve airway, but to normalize air-FLOW in body positions that reduce spinal curvature. The results of removal of ortho impacted her spinal curvature in a very dramatic way and this was seen on follow-up imaging studies.
90 days after removal of her orthodontia, Kim had a follow-up X-ray and new Cobb angle measurement taken. The scoliosis was reduced from 43 degrees to 26 degrees…in 90 days! (See Figures 1 and 2.)
The ramifications of Kim’s case are profound. First, we should consider the typical scoliosis patient: Females of middle-school age are the main cohort of individuals who
present with scoliosis. The typical screen for scoliosis occurs in middle school where the PT has school kids forward-bend to look for asymmetry of rib cage position. If there is a significant-enough asymmetry, the child is advised to have it investigated by their doctor. I submit that there needs to be a change in thought. Movement specialists should also be looking into the mouth of these kids and, if the child is in ortho, a discussion should also take place with the orthodontist.
It is unfortunately possible that orthodontia may be preventing improvement of scoliosis. Orthodontics also, potentially, holds a key for preventing increase of scoliosis provided we wait until scoliosis programs are completed (Risser scores at 4 or 5/5), or near completed. If ortho is applied at that point to correct the all-too-common cross-bite that is associated with scoliosis, we suspect that we could lock the spine in a more favorable position. This may be the wave of the future. That remains to be seen. This article is an effort to pull together the research and apply that research to a real-life human being in order to make it real for all of us.
1. Laskowska M, Olczak-Kowalczyk D, Zadurska M, et al. Evaluation of a relationship between malocclusion and idiopathic scoliosis in childrenand adolescents. Journal of Children’s Orthopaedics. 2019;13(6):600-606. doi:10.1302/1863-2548.13. 190100 (higher prevalence of malocclusion in kids who have scoliosis vs those who do not)
2. Saccucci M, Tettamanti L, Mummolo S, Saccomanno S, Saran S, Paskay LC, Giannotta N, Mastrapasqua RF, Pirino A, Scoppa F. Malocclusion and Scoliosis: Is There a Correlation? Journal of Personalized Medicine. 2023;13(8):1249. (crossbite and scoliosis)
3. Polimeni A, Festa F, Tecco S (2011) Scoliosis and dental occlusion: a review of the literature. Scoliosis. 6:15. Pmid: 21801357
4. Ohlendorf D, Seebach K, et al. The effects of a temporarily manipulated dental occlusion on the position of the spine: a comparison during standing and walking. Spine J. 2014 Oct 1; 14(10):2384-91.
5. Al-Othman AA, Sadat-Ali M, Amer AS, Al-Dakheel DA. Genetic Markers for Adolescent Idiopathic Scolios is on Chromosome 19p13.3 among Saudi Arabian Girls. Asian Spine J. 2017 Apr;11(2):167-173.
6. Wise CA, Gao X, Shoemaker S, Gordon D, Herring JA. Understanding genetic factors in idiopathic scoliosis, a complex disease of childhood. Curr Genomics. 2008 Mar;9(1):51-9.
7. Estenne M, Derom E, DeTroyer A. Neck and abdominal muscle activity in patients with severe thoracic scoliosis. Am J Respir Crit Care Med. 1998 Aug;158(2):452-7.
8. Reddy V, Sharma S, Cobanoglu A: What dictates the position of the diaphragm – the heart of the liver? J Thorac Cardiovasc Surg108:4,1994.
9. Hudson AL, Butler JE, et al. Role of the diaphragm in trunk rotation in humans. JN Physiol. Oct 2011;106(4):1622-28.
10. Mead J: Functional significance of the area of apposition of diaphragmt o rib cage. Am Rev Respir Dis 11:31, 1979.
11. Obayashi et al. Effects of respiratory-muscle exercise on spinal curvature. Journal of Sport Rehabilitation, 2012; 21:63-68.




BelunSleepPlatformisanAI-enabledFDA510(k)clearedsystemforOSAdiagnosis withsleepstages.It’susedforbothHSAT& MADtreatmentcalibrationfor multi-nighttestingandhasreusablecapability.


Circadian rhythm is the biological clock that regulates the body’s sleep-wake cycle over a 24-hour time period. The part of the brain that responds to light and natural light exposure is also responsible for regulating circadian rhythm. So, alertness is at the highest level during the day and declines as the night approaches.
But, what’s the importance of circadian rhythm? Continue reading below to find out the answer.
Let’s begin with the basics and learn how the circadian rhythm works. In short, two main processes control the circadian rhythm including the internal biological clock system and external surroundings, such as natural light exposure.
Each of the body’s biological clocks is regulated by the master clock which is a group of about 20,000 nerve cells forming the suprachiasmatic nucleus, or SCN. The SCN is located in the hypothalamus in the brain and uses daylight and other cues to signal alertness and sleepiness. What’s more, the SCN also regulates melatonin production, also known as the sleep hormone.
In addition to controlling sleep, the SCN also plays a huge role in metabolism and hormone production. It synchronizes local clocks, found in the liver, lungs, muscles, and connective tissues, with the master clock through a complex process of alterations in body temperature and hormone secretion. Then, as soon as the master clock sends signals to trigger specific body functions, the biological clock sets the circadian rhythm in motion. The biological clock produces daily circadian rhythms, tracks their timing, and manages other seasonal and yearly cycles. At the same time, the biological clock coordinates with the master clock to keep the circadian rhythm in sync with the surrounding environment, including:
• Daily changes in light
• Humidity
• Temperature
• Activity levels
• Meal times

Moving on to circadian rhythm and sleep, the circadian rhythm determines sleep and wake times by detecting light signals. During natural light exposure at daytime, light enters the eye and travels to the SCN which triggers alertness and wakefulness. But, when the sun sets, the master clock triggers melatonin production by the pineal gland which promotes drowsiness and sleepiness.
Other factors that contribute to the sleep-wake cycle include:
• Seasons
• Daylight saving time
• Sleep deprivation
• The length of time of being awake
• Work Schedules
The importance of circadian rhythm doesn’t end with sleep. Indeed, the impact of circadian rhythm on health is quite remarkable. The circadian rhythm is crucial for the proper function of key bodily processes and affects energy and fitness levels. A healthy circadian rhythm is associated with a strong metabolism, reduced stress levels, as well as longevity.
On the other hand, irregular circadian rhythms have been connected to chronic health issues such as depression, obesity, and sleep disorders. Namely, the body’s internal clock can affect over thirty medical conditions, including the following:
• Heart disease
• High blood pressure
• Diabetes
• High glucose levels
• Cognitive decline
• Bipolar disorder
Finally, let’s go through several circadian rhythm disorders:
Delayed Sleep Phase Syndrome (DSPS)
– This circadian rhythm disorder is characterized by a feeling of tiredness later in the night meaning that the person goes to sleep at least two hours past a reasonable bedtime and also wakes later than social norms.
Advanced Sleep Phase Syndrome (ASPS)
– Contrary to DSPS, this disorder makes people feel tired earlier at night meaning that the person with ASPS goes to bed at least two hours before a reasonable bedtime and tends to wake earlier than social norms.
Non-24-Hour Sleep-Wake Syndrome –
People with this disorder have a circadian rhythm that’s out of sync resulting in sleep cycles slightly longer than 24 hours, leading to later daily sleep and wake times which tends to work itself around the clock. This disorder is typically associated in individuals who are blind and do not have the typical light cues.
Shift-Work Sleep Disorder (SWSD) –
This disorder is a result of a conflict between the circadian rhythm and the work schedule which runs counter to the internal body clock, resulting in insomnia, excessive daytime sleepiness, and other health issues.
In conclusion, circadian rhythm serves as the intricate orchestration of the body’s inter-
nal clocks, governed by the master clock in the suprachiasmatic nucleus. This complex system not only regulates the sleep-wake cycle but also plays a vital role in metabolism, hormone production, and overall health. The synchronization of circadian rhythms with environmental factors such as light, temperature, and activity levels is crucial for optimal functioning.
The profound impact of circadian rhythm on health is evident, with a well-maintained rhythm associated with enhanced metabolism, reduced stress, and longevity. Conversely, irregular circadian rhythms have been linked to various chronic health issues, including depression, obesity, and sleep disorders, affecting over thirty medical conditions such as heart disease, diabetes, and cognitive decline.
Furthermore, circadian rhythm disorders, such as Delayed Sleep Phase Syndrome (DSPS), Advanced Sleep Phase Syndrome (ASPS), Non-24-Hour Sleep-Wake Syndrome, and Shift-Work Sleep Disorder (SWSD), highlight the vulnerability of this system to disruptions. Understanding and maintaining a healthy circadian rhythm prove essential not only for a good night’s sleep but also for overall well-being and the prevention of potential health complications.

Read Dr. Surkin’s latest research article published in the Journal of the American Heart Association... Irregular circadian rhythms have been linked to various chronic health issues, including depression, obesity, and sleep disorders, affecting over thirty medical conditions such as heart disease, diabetes, and cognitive decline.

A. Surkin, MD, is the Chief Medical Officer of Nexus Dental Systems. A private practitioner in cardiology, sleep medicine, and obesity medicine, he is one of a small group of physicians to be triple board certified in cardiology, sleep medicine, and nuclear cardiology. In 2009, he created Carolina Sleep – the only dedicated sleep medicine practice in eastern NC. Dr. Surkin has created a cardiovascular and sleep healthcare model that includes a multi-faceted diagnostic and treatment approach that is enhanced by a network of relationships with physicians, dentists, respiratory therapists, sleep technologists, and public officials who recognize the important role that sleep medicine has in our daily life. In 2012, Dr. Surkin founded the American Academy of Cardiovascular Sleep Medicine which is a not-for-profit academic organization dedicated to educating healthcare providers, supporting research, and increasing public awareness of the convergence between cardiovascular disease and sleep disorders. In 2014, Dr. Surkin created a new multi-specialty practice called Carolina Clinic for Health and Wellness which combines his specialties with primary care, gynecology, behavioral health and a medical spa. Dr. Surkin is married with three daughters and a golden retriever and resides in Greenville, NC.

by Alan D. Steljes, MD, FACC, FRCPC
Imagine this: You have been planning for a much needed vacation. Your trip will take you to Europe for a week. You have packed the schedule with an ambitious program in your enthusiasm to “see all the sights.“ You are aware of the time change, so you booked an overnight flight, reasoning that you can sleep on the plane and be ready for adventures on arrival.
En route from Chicago to London, you managed to eke out about four hours of sleep on the 8 hour flight. All is going according to plan.
On arrival, it is 10 a.m. local time, and you are excited to see your first destination, the Tower of London. After standing in line
for four hours, you are understandably tired. You enjoy a nice dinner, then look forward to going to bed at 10 p.m. local time. This is great, you think. I will be on local time within the first day. Easy!
Much to your chagrin, you lie awake for hours, unable to sleep. You get only about 4 hours of sleep that first night, before you have to get up in the morning for a scheduled tour. You feel excessively tired during the day and feel like you may nod off at any time. The second night is only a little better. Your normally robust appetite is now poor despite some enticing food options. You’ve had some bowel issues. You find yourself dragging to keep up with your busy schedule. You do feel significantly better after about a week (just as you are getting ready to return to the US.) Obviously, this is jet lag. This syndrome is associated with complaints of insomnia or excessive daytime sleepiness accompanied by a reduction in total sleep time. There is impairment of daytime function and general malaise. Somatic complaints are common

after the first or second day (poor appetite, inappropriate timing of defecation, excessive urination.)
The degree of dysfunction depends on various factors including the number of time zones crossed, the direction of travel (westward travel is better tolerated), sleep loss during travel, availability of daylight at the destination, and one’s ability to tolerate circadian misalignment.
What is the problem? Your internal clock is out of synch with the local time. We say that your internal circadian rhythms are phase delayed with respect to the local time zone. The 10 p.m. bedtime in London is only 4 p.m. for you. Your brain is not at all prepared to sleep.
In EASTWARD TRAVEL, people have difficulty falling asleep and staying asleep because they are trying to sleep at a time when the circadian alerting signal is high. Adaptation requires a phase advance i.e. falling asleep at an earlier time with respect to your internal clock. London is 6 hours ahead of Chicago. You need to phase advance your bedtime by 6 hours. Your body will eventually adapt to the new time zone, without any change in routine. However, it typically adjusts by only half an hour a day when traveling eastward.
The process should start at home, beginning 3 days prior to your flight. Try to go to bed one hour earlier each night and get up earlier each day. Exposure to bright light in the morning is helpful to consolidate your shift in bedtime. Adding melatonin 0.5 mg or 3 mg prior to the usual bedtime may have additional benefit.
Consider scheduling travel to arrive at your destination at least 2 days before any important events, (for example a speech or a wedding) to give your body some time to adjust.
An overnight flight is helpful, by matching the flight time to your normal sleep schedule. Optimize your sleep time as much as possible. Noise cancelling headphones or eyeshades may help. Your physician may prescribe a sleeping pill. Regardless, you will still lose sleep time on a typical 6-8 hour long transatlantic flight.
After arrival, we can speed up the adaptation process, but we will have to use our knowledge of those circadian processes which induce sleepiness at bedtime and
Noon 6 p.m.
The upper and lower timelines show the simultaneous times in Chicago and London respectively. The times in London are 6 hours ahead of Chicago. The open rectangle between the timelines shows the typical bedtime of our traveler which is from 10 p.m. to 6 a.m. Chicago time. The green arrowhead shows the CBTmin at 4 a.m. Eastern. We want to phase advance this patient by 6 hours, the direction indicated by the arrow. Administering melatonin early in the evening may “pull” the CBTmin to the left. Exposure to light before the CBTmin will “push” the CBTmin to the right i.e. the wrong direction. Exposure to light from 11 a.m. to 2 p.m. London time is ideal to push the CBTmin to the left i.e. phase advance.
promote alertness during the day. Melatonin secretion and core body temperature are the most relevant for bedtime sleepiness. We fall asleep with rising melatonin blood levels and falling core body temperature.
The timing of these processes are governed by our internal clock, our master pacemaker, which is the suprachiasmatic nucleus (SCN) located in the anterior hypothalamus. The SCN has cells which cycle independently with a time period which is close to 24 hours. The SCN must be “entrained” to local time by external clues, the most powerful of which is exposure to daylight.
We can shift the timing of our internal clock by the strategic use of light and melatonin. The rule is that melatonin “pulls” while light “pushes.” This is best visualized by referring to Figure 1.

Alan D. Steljes, MD, FACC, FRCPC was trained as an interventional cardiologist. Since fellowship, he has obtained additional certification in nuclear cardiology, echocardiography, CT coronary angiography and finally sleep medicine. In 2010, he opened a two bed sleep lab, recognizing the heart-sleep apnea interaction. The initial 2 beds have been scaled up to 12 beds since associating with the Nevada Heart & Vascular Center. He has since retired from the cardiology practice but continues to oversee the sleep program. He remains passionate about spreading the word about sleep disordered breathing and the heart. He currently shares his time between Las Vegas, NV and Mount Pleasant, SC.


We can shift the timing of our internal clock by the strategic use of light and melatonin. The rule is that melatonin “pulls” while light “pushes.”
The evening rise in melatonin secretion and the minimum core body temperature (CBTmin) are two useful markers of the position of an individual’s circadian rhythm with respect to the local time of day. The CBTmin occurs 2 to 3 hours before our natural awakening.
After your arrival in London, you should have avoided exposure to light before 10 a.m., by wearing sunglasses or staying indoors. Exposure to light prior to CBTmin, will reset your clock in the wrong direction. Ideally, you want to expose yourself to sunlight between 11 a.m. to 2 p.m. Light exposure after the CBTmin will “push” the CBTmin in the desired direction. Avoid evening light as you are approaching your new bedtime.
Melatonin at your new bedtime is an option to “pull” the CBTmin earlier i.e. phase advance.
In WESTWARD TRAVEL, people may experience sleepiness prior to bedtime which may make falling asleep easier, but they may have difficulty maintaining sleep for as long as desired since the internal circadian alerting signal will be rising during the sleep period. Adaptation requires a phase delay. That is the individual will go to bed later than customary. Westward travel is typically better tolerated, since it is easier to stay up later at night than to get up earlier in the morning. Adaptation to western travel is also quicker i.e. about one hour a day.
Pre-flight adjustment may not be necessary. However, phase delaying could be tried before travel begins (go to bed later, get up later) using evening bright light for 1 to 3 hours. Daytime flights are preferred. Light should be avoided in the morning in the new destination (if it occurs soon after CBTmin) to prevent phase advance. Exposure to light in the evening (if before CBTmin) may be helpful (phase delay). See Figure 2.
Melatonin use for westward travel can be counterproductive if not timed carefully. For example, melatonin at bedtime in the destination, if taken before CBTmin, induces phase shift in the wrong direction (phase advance). Taking melatonin on awakening is the correct time for phase delay but may make the individual sleepy during the day. If melatonin is used, it is recommended that a small dose (to avoid prolonged sleepiness) be taken during the last half of the night.
After eastward flights, very early light (inappropriate phase delay) should be avoided. On westward flights, light at dusk (inappropriate phase advance) should be avoided for 2 to 3 days. Thereafter, light at the usual times may help with adaptation.
Some physicians recommend attempts at phase delay even if the direction of travel is eastward when more than eight time zones are crossed.
It does get complicated. There are websites which will customize a schedule for you including wake times, bed times, caffeine, and melatonin.
Finally, these common-sense steps will help you adjust and avoid jet lag symptoms.
• You should follow the sleep and waking routines of your destination when you arrive.
• Hypnotic sleeping pills at bedtime may help with sleep but do not necessarily help with alertness the next day. Even if you get adequate sleep, decreased circadian alertness will occur at the time of CBTmin
• Take meals on the local schedule. Eat small meals to avoid stomach aches or other problems.
• Avoid alcohol as it disrupts sleep.
• Use caffeine and exercise strategically; these may help you stay alert throughout the day, but you should avoid these after noon.
• Drink plenty of water.
• If you are sleepy during the day, take short naps, no more than 15-20 minutes, to help you feel better during the day, yet still sleep at night.
Good luck on your travels.

• Whole-Team Training
• Ongoing Coaching
• Streamlined Protocols
• Precision Bite Technology
• Patient Ed ucation
• In-Network Medical Billing

by Colonel Scott Williams, MD, FAASM
When one considers treatment of sleep disordered breathing, the first therapeutic modality that likely comes to mind is positive airway pressure (PAP). In fact, some clinicians think that it is the only option available to patients. In order to increase the awareness of mandibular advancement therapy (MAT), high quality research is critical. A quick PubMed search with common key words (mandibular advancement device, oral appliance, etc.) shows that just over 3,000 articles have been written about MAT, compared with almost 12,000 for CPAP. Broadening the search term to “positive airway pressure,” the number jumps to over 20,000. The dental/orthodontic literature base is robust, however. A search for “oral appliance” yielded almost 50,000 results, but when general orthodontic/prosthodontic articles are excluded, only about 1,500 articles remain. For the most recent American Academy of Sleep Medicine Clinical Practice Guideline regarding MAT, only 377 citations met criteria for inclusion.1
This research disparity has important ramifications, especially considering the rapid dissemination of information via media that would have been considered unimaginable even just a few decades ago. Whereas historically, research articles were relegated to medical libraries and read only by those who had institutional access, nowadays results are shared over social media platforms, traditional and digital news outlets, and “go viral” very easily. What follows are a few examples of simple yet impactful research that many dental sleep practices are able to (and should) replicate.
First, its helpful to highlight the need to change perceptions regarding the patient population that might benefit from MAT. Most feel that MAT is contraindicated in severe OSA but there is some emerging data showing that some patients can be adequately treated, and that device design may play an important role in relative effectiveness.2 PAP manufacturers have long been experimenting with a variety of design improvements to in-

clude auto-adjusting algorithms, transient expiratory pressure decrements, and adjustable humidification. Mask technology is also constantly evolving, and with each new iteration there is usually published literature showing a benefit. Very few published data compare the relative advantages of newer mandibular advancement device (MAD) technologies, so the study by Vanderveken and colleagues should serve as a template for future work. It is crucial for independent groups to validate initial industry-funded trials, however, to increase the confidence of the findings.
Second, it is essential to remind the scientific and lay community of the benefits of MAT, specifically the cardiovascular impact. While it has been known for more than 20 years that MAT can decrease blood pressure,3,4 CPAP has consistently been thought of as superior to MAT. A recent study by Thant and colleagues underscored the important difference between efficacy and effectiveness.5 In Thant’s study, MAT therapy was non-inferior to CPAP (and actually showed a marginally greater reduction in BP), likely mediated by greater use of MAT vs. CPAP. In this study, 74.7% of patients used the MAD more than 6 hours per night, compared with 56.5% of patients in the CPAP group. The importance of reporting nights of full usage, not just nights with greater than 4 hours use, is critical for OSA trials. A concerning number of CPAP trials have fallen short of reversing the many physiologic changes seen with sleep disordered breathing. It’s not because CPAP doesn’t work, its because there is a dose-response curve, and this is where MAT can show superior outcomes...if it is studied. Finally, much more research is needed in the area of stepped care or combination therapy. Surprisingly little data exists in this area, and where it does, the data quality is variable. That said, the outcomes are usually very good. Aishah and colleagues conducted a very nice study looking at mandibular advancement in combination with positional therapy, pharmacotherapy, and other modalities.6 Other studies have looked at the role of alternating between CPAP and MAT to mitigate jaw discomfort and to provide options for patients who travel frequently. However, these trials are typically small, sometimes underpowered, and have inconsistent outcomes.
In my clinic, I often see patients who are new to me and are struggling with CPAP.

“It is essential to remind the scientific and lay community of the benefits of MAT, specifically the cardiovascular impact.”
Almost without fail they have not been offered a mandibular advancement device and most are unaware that it is an option. In fact, more patients are aware of hypoglossal nerve stimulation than MAT. It is imperative for the Dental Sleep Medicine community to increase the pace of research in order to more fully demonstrate the benefits of this treatment option.
1. Ramar K, Dorr LC, Katz S, et al. Clinical practice guideline for the treatment of obstructive sleep apnea and snoring with oral appliance therapy: an update for 2015. J Clin Sleep Med, 11(7), 773-827, 2015.
2. Vanderveken OM, Van Daele M, Verbraecken J, Braem MJ, Dieltjens M. Comparative analysis of two custom-made mandibular advancement devices with varied designs for treating moderate to severe obstructive sleep apnea. Sleep Med, 117:95-98, 2024.
3. Gotsopoulos H, Kelly JJ, Cistulli PA. Oral appliance therapy reduces blood pressure in obstructive sleep apnea: a randomized, controlled trial. Sleep 27(5):934-41, 2004.
4. Bhushan A, Tripathi A, Gupta A, Tripathi S. The effects of an oral appliance in obstructive sleep apnea patients with prehypertension. J Dent Sleep Med, 2(2):37-43, 2015.
5. Thant AT, Shih EC, et al. Mandibular advancement vs CPAP for blood pressure reduction in patients with obstructive sleep apnea. J Am Coll Cardiol, S:0735-1097(24)00906-9, 2024.
6. Aishah A, Tong BKY, Osman AM, et al. Stepwise add-on and endotype-informed targeted combination therapy to treat obstructive sleep apnea: A proof-of-concept study. Ann Am Thorac Soc, 20(9):1316-25, 2023.

Colonel Scott Williams, MD, FAASM, is the director of the Center for Military Psychiatry and Neuroscience at the Walter Reed Army Institute of Research. Dr. Williams received his medical doctorate from the Uniformed Services University of the Health Sciences. He completed a dual residency in Internal Medicine and Psychiatry at the Walter Reed Army Medical Center with fellowship training in Sleep Disorders Medicine at the Walter Reed National Military Medical Center. He has served on numerous committees within the AASM and AADSM, and remains passionate about furthering the interdisciplinary nature of sleep medicine.


by Steve Carstensen, DDS, and Pat Mc Bride, PhD, CCSH
Dentistry can, and must, be more than surgical and preventive services limited to the oral cavity. In service of improving healthspans, dentistry has an open opportunity to engage people suffering from any number of chronic conditions and facilitate better choices that might mitigate challenges to homeostasis. The American Heart Association recently added Sleep to its list of essential health concerns. This essay points out a common link among the 8 essentials. This self-instructional course for dentists offers ways the primary care dentist can suggest changes during ongoing dental-health relationships between the dental team and interested patients.
Dental Sleep Practice subscribers can answer the CE questions online at https://dentalsleeppractice.com/continuing-education/ to earn 2 hours of CE from reading the article. Correctly answering the questions will demonstrate the reader can:
1. Understand the link between systemic inflammation and life’s essential health measures.
2. Discuss patient health history in unexpected ways, leading to more engaging conversations with patients
3. See clear pathways to improve knowledge around whole-person health
Within medicine, Dentists have the sole responsibility for preventive and restorative care of the hard tissue in the body that can’t repair itself. The teeth, which are supported by surrounding tissues, cannot and should never be treated as isolated units. There is a strong connection between whole-body health and oral health. So, this begs the question of how far away from the teeth, how deep into the supporting structures, and how connected must the body system(s) be, to fall outside the dentist’s consideration and care?
The American Heart Association (AHA) recently added Sleep to its healthy lifestyle meme, creating “Life’s Essential 8™”. This essay will look at the common connections between each of these essentials and show how the Primary Care Dentist (PCD) contributes to whole-body health, improve communications and co-collaboration with patients while providing customary dental care.
The “Essential 8” are aimed at improving cardiovascular health and lowering the risk of
heart disease, stroke, and avoiding the negative quality-of-life impact any of these events cause.
Life’s Essential 8 are divided into two categories, Health Behaviors and Health Factors:1
1. Healthy Behaviors
a. Eat Better
b. Be More Active
c. Quit Tobacco
d. Get Healthy Sleep
2. Healthy Factors
a. Manage Weight
b. Control Cholesterol
c. Manage Blood Sugar
d. Manage Blood Pressure
Dentists and their teams are in prime position to not only inquire about eating habits, but to advise and educate on nutrition and the effects of poor nutrition on the whole body. Most patients expect to be asked about sugar intake, as the the causal link between excess sugar and cavities discovered by Pierre Fauchard in the late 17th century is common knowledge. Overall US obesity rates continue to escalate. The Food and Action Center’s June 2024 publication notes that 42.4% of US adults and 19.3% of children are obese (BMI>30).2 With most of our population being overweight or obese, normalizing BMI via mindful discussions including the increased risks and adverse system consequences of obesity such as diabetes, heart disease and sleep disordered breathing (OSA) must be included in the primary care dental setting. This is where dentists and their teams can add their professional voice to discussions of food choices. By expanding the conversation away from one which simply focuses on the adverse effects of sugar on teeth, to include information on how the whole body is impacted by eating highly processed foods. Illustrating the benefits of whole foods and how easily small changes in dietary choices can provide huge health benefits, the PCD can offer small (inoffensive) examples of good choices without feeling the need to become a nutritionist or offend people who are sensitive about weight.
A paper published in the journal Nutrients3 noted that almonds are shown to benefit cardiovascular health by decreasing systemic inflammation and affecting gut microbiome to increase beneficial biome populations
and promote more efficient digestion. Nutrients such as vitamin E, fiber, and antioxidants which are concentrated in almond skins, aid the body to improve glycemic response in patients with type 2 diabetes (T2DM). Lower cholesterol and endothelial functional improvements have also been found with daily almond consumption. Since raw almonds are not cariogenic, the PCD can offer “real world” suggestions patients can easily relate to when making decisions regarding snack choices with solid nutritional benefits for whole-body health.
Who doesn’t know that moving is better than sitting? Our patients need no reminder of the benefits of aerobic and strength exercise. If providers are observant, commenting on the Smart watch, Fitbit or any other wearables the patient has and if they use the fitness apps reveals much about their behav-

Steve Carstensen, DDS, has treated sleep apnea and snoring in Bellevue, WA since 1998. He’s the Consultant to the ADA for sleep related breathing disorders and heads the ADA’s Children’s Airway Initiative. He trained at UCLA’s Mini-Residency in Dental Sleep Medicine and is a Diplomate of the American Board of Dental Sleep Medicine. He lectures internationally, directs sleep education at Airway Technologies and the Pankey Institute, and is a guest lecturer at Spear Education, Louisiana State Dental School, and University of the Pacific, in addition to advising several other sleep-related manufacturers. In 2014 he helped found Dental Sleep Practice magazine and currently serves as Chief Dental Editor. In 2019, Quintessence published A Clinician’s Handbook for Dental Sleep Medicine, written with a co-author. The AADSM awarded him the 2023 Distinguished Service Award.

Pat Mc Bride, PhD, CCSH, has spent her entire career as a full time clinician, educator, and author in the fields of dentistry, respiratory medicine, and dental sleep medicine. Her extensive experience in clinical, laboratory, research, and educational arenas has led to the development of interdisciplinary care model delivery systems used in collaboration by physicians and dentists around the globe. Pat has a unique ability to intervene in the interstices of global systems, developing protocols which can be translated across demographics and cultures into improved clinical outcomes. In addition to teaching and writing, Pat continues to work hands on in the craniofacial surgical space as Clinical Director for Movahed OMS in St. Louis, MO and Walnut Creek, CA. Serving the underserved and marginalized patient remains a passion and priority for her. She sits on numerous Boards such as the AAPMD and National Institute of Health Sleep Disorders Research Advisory Board (SDRAB). She is also the Executive Director for The Foundation for Airway Health.
iors. For example, the PCD can link a better night’s sleep to having enough energy to take a walk, which for many people can be a starting point for a change in leisure habits from negative to positive for health. Simply inquiring if a patient “counts their steps” or fills their activity rings on their wearable improves patient provider communications, promotes trust, and illustrates the PCD’s genuine care and concern for the patient and their daily lives. In Frontiers in Physiology, Guo, et.al, wrote about the link between exercise and inflammatory markers in obese and overweight populations.4 Their analysis of 22 studies including 1,135 subjects showed aerobic exercise reduces CRP (C-reactive protein) and IL6 levels (Interleukin 6), two markers of inflammation that affect the whole physiology. Strength training, which includes the use of weights, also reduces CRP, so a mix of activity (aerobic + strength training) will help people who list inflammation-linked chronic health conditions as part of their medical history and life challenges.
Stopping smoking may be the single most important health change possible for your patients who struggle with the noxious addiction. The science behind nicotine addiction is clear, yet many people still do not realize cigarettes are as hard to quit as cocaine or heroin. It’s unimaginable that any smoker considers smoking a health benefit, but which motivator will prove to be the right one to facilitate smoking cessation is unique to each person. No one wants to age prematurely, so citing a study that shows smokers produce an enzyme that accelerates telomere shortening and induction of inflammation may help them see a way to decide to quit.5

Better sleep is why we are in the conversation, yes? How sleep relates to overall health is the subject of thousands of scientific papers, popular books and professional tomes. It’s why we started this magazine. Which bit of data is useful for the patient in your chair depends on your depth of knowledge and how you can apply it in a meaningful and mindful way. The value of healthy sleep has long been known yet this behavior was only added to the Essentials list in 2022. Welcome, I say! Sleep deprivation, whether it be from a lifestyle decision or a health concern interrupting normal physiology, is a major contributor to development and progression of various chronic inflammatory diseases.6 Considering that the quality of our health at any age is a result of accumulated physiologic challenges throughout all body systems, the soonest in life we can manage improvements in sleep quantity and quality will generate the best opportunity for optimum health span. The PCD is uniquely situated to partner with patients in their journey to better sleep by illustrating how simple changes to and in quality and quantity can exponentially improve overall health status and daytime functioning.
Simple suggestions to improve sleep can include the following:
• Stick to a sleep schedule. Waking at the same time every day is key.
• Gets some kind of exercise every day.
• Go outside.
• Avoid caffeine and nicotine.
• Do not take naps in the afternoon.
• Avoid large meals and alcohol before bed.
• Limit and turn off electronics at least 1 hour before bed.
• Create a cool, quiet, and dark sleep environment.
in 2022.
The value of healthy sleep has long been known yet this behavior was only added to the Essentials list
Dr. Robert Lustig, in a recent American Dental Association sponsored wellness program, Dentistry’s Role in Complete Health, pointed out the microbiology connections between obesity, caries, mitochondrial dysfunction, and T2DM. He pointed out differences in body fat deposits – some obese people are at lower risk of nonalcoholic fatty liver disease (NAFLD, an expression of chronic inflammation), while some thin
people show no visible fat deposits but are sick with poor liver function. Managing weight is not just about how one looks, but how each body deals with energy balance. A non-inflammatory diet supports proper mitochondrial function, the baseline of our metabolism. Reduction in population NAFLD will lower the rate of T2DM and improve community health and decrease health care costs. In summary, fructose is very bad for health – watch your food labels. Ultraprocessed foods (look for many ingredients on the label) are always inflammatory.
It’s pretty safe to say your patients know that high cholesterol is bad for their heart. Perhaps some understand that there is LDL (bad) and HDL (good) versions of cholesterol. The PCD has no time to get into the nuances of why that statement might be an incomplete presentation of a complex subject, but we are finding details that can help every health care professional provide important information useful to interested patients. We know that cholesterol is most dangerous in small-particle form, called Remnant Cholesterol, which targets organ damage through inflammatory pathways.7 Increasingly, PCD are exploring blood tests to uncover hsCRP (High-sensitivity C-reactive protein) as a marker for refractory periodontal disease. High levels of hsCRP are also associated with increased remnant cholesterol; while the PCD and dental hygienist discuss controlling oral disease, they can add value to needed changes by linking the effort to whole body health. Helping patients understand the link between hsCRP, poor oral health and periodontal disease is essential to this collaborative discussion.
Glucose is necessary for our mitochondria; getting it from the digestive tract to inside the cells is a function of insulin. Uncontrolled blood sugar signals insulin resistance and decreasing ability to manage energy metabolism. This leads to a host of physiological problems, the most evident being obesity and T2DM. In turn, obesity increases chronic inflammation which leads to further insulin resistance. People who already have T2DM understand blood sugar very well; however, most people with unstable blood sugar may
only feel symptoms easily confused with other sources, like hunger, fatigue, or anxiety. Careful review of patient intake or updated medical history is essential as many patients, especially those without health insurance, who do not have PCP’s or go to a physician unless they have an emergent situation. As you discuss general health issues, an inquiry about fasting blood sugar tests reveals your patient’s awareness of their individual health status and can improve discussions connecting overall systems issues to oral health. A history of Metformin prescriptions can be another clue, however, it is essential that the PCD be knowledgeable regarding current trends in “off label” Metformin use in medically managed weight loss for non-diabetic patients. Metabolic syndrome, a collection of sugar metabolism dysfunctions, also produces neuropathological issues like Alzheimer’s disease by affecting adenosine receptor signals in the brain, producing changes that no one wants to live with.8 Helping your patients understand that insulin resistance can lead to brain damage and loss of quality and quantity of life may help motivate them to improve diet choices.
Less salt, right? Lower stress? What else is there, any patient may ask when queried about a high blood pressure reading during a routine PCD preventive visit. “Traffic was terrible, Doc” they might say. Hypertension falls in the category of disease that would be better if there were some symptoms to raise awareness in those who suffer from this challenge to health. They call hypertension a silent killer for good reason. Would it surprise you that research is showing a major contributor to chronic hypertension is gut microbiome dysbiosis?9 There is an enormous curiosity in physiology research around the role our digestive tract symbiotic microorganisms play in our overall health. Causative connections are being uncovered about contributions the gut microbiome and the immune system make to exacerbate hypertension and cardiovascular disease, and to mitigate them. When proinflammatory diets are the choice, high blood pressure can be an uninvited guest. The PCD, while discussing hypertension, can explore what the patient understands about how pre- and probiotics
A primary care dentist engages the patient about why a tooth needed repair in the first place
can help establish gut microbiome health and promote symptom relief easily felt by long-suffering patients. While these supplements are not proven with randomized controlled trials and individual responses vary widely, they are low risk to trial and often show remarkable effectiveness in a wide spectrum of patients.
Inflammation is a body’s generalized response to a stressor. When we can control the stressors, we allow a response towards homeostasis, our best condition for health. As part of primary care, the dental team who takes the time to learn, to communicate, and to support lifestyle choices towards health in our patient population will become increasingly important in the mission of improving healthspans. If you look back at the American Heart Association’s “Life’s Essential 8” you will find a common link to systemic inflammation. A dentist’s surgical repair of a decayed tooth is a necessary health service. A primary care dentist who engages the patient in an ‘upstream’ discussion of why that decayed tooth needed repair in the first place will be a better co-discovery partner during that person’s health span. Patients who wish to sleep and breathe better at night or have been diagnosed with OSA might request a mandibular advancement device from the PCD, or a positive air pressure system provided through their PCP or Sleep Medicine MD. Providing these non-invasive therapies manages symptoms in the short term; the discussion of the upstream ‘why’ can lead to patients making changes in their overall health, which could provide resolution of those issues. Dentists are trained to see the underdeveloped craniofacial respiratory complex; it’s time now for primary care dentists to see underlying phys-
1. https://www.heart.org/en/healthy-living/healthy-lifestyle/lifes-essential-8
2. https://frac.org/hunger-obesity
iologic challenges related to inflammation and point to different health paths that relieve downstream suffering for their patients.
Looking for education beyond traditional restorative dental lectures and workshops is the key. There are meetings and online conferences focusing on whole-person wellness sponsored by such groups as American Academy of Physiologic Medicine and Dentistry (AAPMD.org) and American Academy of Oral Systemic Health (AAOSH.org), two non-profits dedicated to enhancing health, mostly by training dental teams, with enthusiastic participation of dental hygienists, physicians, physical therapists, speech language pathologists, and functional medicine practitioners. Websites such as the American Heart Association and TED talks supply inexhaustible amounts of useful information much of which is in “small bites” so the PCD can learn new concepts easily and quickly. Reading books by Robert Lustig, MD, Nathan Bryan, PhD, Susan Maples, DDS, Peter Attia, MD, Robert F. Barkley, DDS, and Alan Alda, among (many) others will raise the level of knowledge, awareness and exponentially improve PCD communication skills to turn complicated concepts into accessible and useful information to share. When the caring Primary Care Dentist knows their work and takes the time to know the unique individual presenting in front of them, then applies that knowledge in a way that is meaningful to that person, they can facilitate improved health choices made by the fortunate people they are privileged to serve.
3. Singar S, Kadyan S, Patoine C, Park G, Arjmandi B, Nagpal R. The Effects of Almond Consumption on Cardiovascular Health and Gut Microbiome: A Comprehensive Review. Nutrients. 2024 Jun 20;16(12):1964. doi: 10.3390/nu16121964. PMID: 38931317.
4. Guo Y, Qian H, Xin X, Liu Q. Effects of different exercise modalities on inflammatory markers in the obese and overweight populations: unraveling the mystery of exercise and inflammation. Front Physiol. 2024 Jun 12;15:1405094. doi: 10.3389/fphys.2024.1405094. PMID: 38933362; PMCID: PMC11199780.
5. Deb S, Berei J, Miliavski E, Khan MJ, Broder TJ, Akurugo TA, Lund C, Fleming SE, Hillwig R, Ross J, Puri N. The Effects of Smoking on Telomere Length, Induction of Oncogenic Stress, and Chronic Inflammatory Responses Leading to Aging. Cells. 2024 May 21;13(11):884. doi: 10.3390/cells13110884. PMID: 38891017; PMCID: PMC11172003.
6. Visallini TS, Parameswari RP. Retrospective Case Study on the Evaluation of Inflammatory Markers, Macrophage Inhibitory Protein-1α and Interferon-γ in Sleep Deprivation Condition. J Pharm Bioallied Sci. 2024 Apr;16(Suppl 2):S1326-S1329. doi: 10.4103/jpbs.jpbs_607_23. Epub 2024 Apr 16. PMID: 38882737; PMCID: PMC11174169.
7. Yuan Y, Hu X, Zhang S, Wang W, Yu B, Zhou Y, Ou Y, Dong H. Remnant cholesterol, preinflammatory state and chronic kidney disease: association and mediation analyses. Ren Fail. 2024 Dec;46(2):2361094. doi: 10.1080/0886022X.2024.2361094. Epub 2024 Jun 10. PMID: 38856016; PMCID: PMC11168229.
8. Jang MH, Song J. Adenosine and adenosine receptors in metabolic imbalance-related neurological issues. Biomed Pharmacother. 2024 Jun 18;177:116996. doi: 10.1016/j.biopha.2024.116996. Epub ahead of print. PMID: 38897158.
9. Dinakis E, O’Donnell JA, Marques FZ. The gut-immune axis during hypertension and cardiovascular diseases. Acta Physiol (Oxf). 2024 Jun 20:e14193. doi: 10.1111/apha.14193. Epub ahead of print. PMID: 38899764.
10. Dinakis E, O’Donnell JA, Marques FZ. The gut-immune axis during hypertension and cardiovascular diseases. Acta Physiol (Oxf). 2024 Jun 20:e14193. doi: 10.1111/apha.14193. Epub ahead of print. PMID: 38899764.
AGD Code: 730
Date Published: August 9, 2024 Course Expires: August 9, 2027
Legal disclaimer: Course expires 3 years after publication date. The CE provider uses reasonable care in selecting and providing accurate content. The CE provider, however, does not independently verify the content or materials. Any opinions expressed in the materials are those of the author and not the CE provider. The instructional materials are intended to supplement, but are not a substitute for, the knowledge, skills, expertise and judgement of a trained healthcare professional.
Each article is equivalent to two CE credits. Available only to paid subscribers. Free subscriptions do not qualify for the CE credits. Subscribe and receive up to 8 CE credits for only $149 by visiting https://dentalsleeppractice.com/subscribe/.
n To receive credit: Go online to dentalsleeppractice.com/continuing-education/, click on the article, then click on the take quiz button, and enter your test answers
To provide feedback on this article and CE, email us at education@medmarkmedia.com.
by Steve Carstensen, DDS, and Pat Mc Bride, PhD, CCSH
1. The American Heart Association improved its “Life’s Simple 7” to include sleep and renamed the meme __________.
a. “Useful 8”
b. “8 Health Lessons”
c. “Life’s Essential 8”
d. “Eight is Enough”
2. A link between hypertension and inflammation is based on understanding ___________.
a. Total sodium intake
b. That tight feeling one gets in the gut when stress is overwhelming
c. High blood pressure creates inflammation in every body system
d. Gut microbiome directly affects inflammation, leading to hypertension
3. People understand weight control is important to health; what is one link?
a. Losing weight eliminates obstructive sleep apnea
b. Accumulation of fat in the liver inhibits mitochondrial function
c. Quality of life is directly related to body mass index
d. Weight management is mostly related to amount of fat in the diet
4. Smoking decreases healthspan in many ways including ________.
a. Driving away people who would otherwise be friendly
b. Exposure to bad weather as smokers are forced outside
c. Increasing air pollution from discarded lit cigarettes igniting fires
d. Enhancing a telomere-destroying enzyme, prematurely aging DNA
5. Fasting blood sugar is a key biomarker that is important because ____________.
a. Insulin production and levels of resistance, influenced by inflammation, leads to many physiologic problems
b. Choosing between eggs or doughnuts for breakfast is not always easy
c. It is easy to judge based on symptoms
d. Dental offices can easily use blood samples to determine sugar levels
6. The most dangerous cholesterol in our systems is ___________.
a. High density lipoprotein
b. Low density lipoprotein
c. Remnant cholesterol
d. Statin-resistant cholesterol
7. Better food choices lead to less inflammation by ____________.
a. Whole foods are easier to process by our gut microbiome
b. Providing nutrients not found in ultraprocessed foods
c. Producing fewer harmful digestive by-products
d. All of these and so much more
8. Increasing the level of daily aerobic and strength training _______.
a. Forces a loss of critical screentime
b. May result in debilitating injury and should be avoided
c. Decreases inflammatory cytokines like CRP and IL6
d. Takes too much time and is a poor use of limited resources
9. The right amount of sleep improves health by __________.
a. Decreasing the risk of cardiovascular disease
b. Overall improves inflammation when sleep is restful
c. Requires an open airway to achieve homeostatic sleep
d. Increases quality of life (and all the other answers above, too)
10. Education for dentists interested in becoming Primary Care Dentists
__________.
a. Should focus on increasing knowledge of dental materials
b. Can mostly be found at traditional dental conferences
c. Grows from a close relationship with local primary care physicians
d. Is supported by the American Dental Association and other non-profit organizations of forward-thinking professionals enthusiastic to welcome another interested dentist to the journey
The FasTrack system represents a major advancement in treating Sleep Disordered Breathing (SDB) through the HealthyStart Pulsator device. It eliminates the need for daytime exercises, requiring only a 5-minute session before sleep and nighttime wear. Additionally, the system includes a customized adjunct device, designed specifically for each patient, to enhance the treatment’s effectiveness. Both devices are key components of HealthyStart’s comprehensive 5-Prong System, known as FasTrack.
HealthyStart’s FasTrack addresses SDB with a five-prong approach:
1. Comprehensive Patient Evaluation: This involves a thorough assessment of breathing, orthodontic, and sleep issues to identify the root causes of SDB.
2. Built-In Myofunctional Therapy: This therapy, activated by swallowing, operates throughout the night to improve oral function and airway health.
3. 5-Minute Pulsator Compliance Device: This innovation simplifies therapy by removing the need for daytime exercises, making it easier for patients to comply with the treatment.
4. Customized Adjuncts: Tailored specifically for each patient, these adjuncts are designed to provide appropriate expansion and distalization based on individual needs.
5. Significant Growth and Development: Research indicates that HealthyStart patients experience 54% more growth and development compared to control groups, demonstrating the system’s effectiveness.
HealthyStart by OrthoTain, a pioneer in orthodontic devices, has been addressing orthodontic conditions for over 57 years. With over 5 million successful cases, they have extensive research and a deep understanding of the breathing and sleep issues affecting many patients. The recent introduction of the Pulsator and customized adjuncts aims to resolve previous treatment challenges and enhance patient success.
• Difference from Traditional Orthodontic Treatment: The FasTrack system evaluates all related issues, including habitual problems, growth deficiencies, and orthodontic conditions linked to SDB.
• Comparison with RPE: While a Rapid Palatal Expander (RPE) can improve nasal breathing, it doesn’t address tongue posture and swallowing habits. Unlike HealthyStart’s FasTrack Adjuncts used with the HealthyStart devices to provide comprehensive expansion, distalization, and internal myofunctional therapy and never compromises tongue placement.

• Arch Width Expansion: Generic standards like a minimum 40 mm arch width can be misleading. HealthyStart emphasizes customized assessments to avoid complications such as teeth being pushed outside the cortical bone and potential gum and bone recession.
• Types of Expansion: Understanding sagittal versus transverse expansion and distalization is crucial. HealthyStart provides digital and live courses to educate providers on these concepts.
• Eliminating Exercise Stress: By integrating myofunctional therapy with the Pulsator, the system reduces the need for additional exercises, minimizing stress for children and parents.
HealthyStart will launch a $1 million educational marketing campaign in September to raise SDB awareness, which affects 40 million children in the US. The campaign aims to boost public interest, increase office inquiries, and elevate provider requests. Current providers have received training, and new doctors can register for a digital course on October 28th, with a special offer of $500 off and a free FasTrack treatment for one patient. HealthyStart continues to lead the industry with innovative technology to enhance treatment for sleep and breathing issues. Their mission is to ensure no child is left behind, and their investment in education is designed to improve health outcomes and treatment efficacy for children affected by SDB.


by Laura Sheppard BS, CDT, TE
I’m Laura Sheppard, CDT, TE, and I’ve had the pleasure of helping doctors learn about and practice Dental Sleep Medicine for over 30 years. This series will help you to understand the technical side of laboratory challenges and appliance design, as I shine a light on obstacles that your patient’s dentition, bite or function may present, and provide various design, material or manufacturing remedies.
Understanding oral appliances and their design is key to building practice success in DSM. As we know, dentists dedicate their lives to the minutia. They are often immersed in the details of occlusion and alignment. As a certified technician, I also know the importance of a balanced, functional oral environment and the beauty of a dynamic smile. When it comes to Dental Sleep Medicine, it’s important to keep things in perspective during appliance treatment. We recently lost a great friend, teacher, and founding father of DSM, Dr. Alan Lowe, Professor and Chair of Orthodontics at the University of British Columbia. I remember in the early 00’s, there was quite a stir over Dr. Lowe’s presentation of his published studies concluding that ‘all sleep appliances move teeth!’ Many of us still laugh when we recall his response to those who were shocked and disturbed by this revelation. His simple retort to the audience was “Get over it!”

Applied forces (such as repositioning the mandible) against a resisting musculature can stimulate response in adaptable systems, such as the periodontal ligament complex. Tooth movement can be mitigated by good design, whether an appliance is digitally or manually manufactured.
Perspective: The most important take away is that dentists transitioning to dental sleep medicine develop a whole new understanding that supersedes issues of minor tooth movement. They realize that they have the opportunity to save lives!
Find a lab that is experienced with various dental sleep appliances and cares about your success. One that understands the treatment as well as the appliances, and one that questions everything. An experienced lab can often anticipate and try to prevent difficulties that may occur based on alignment, draw or function. The most successful doctors welcome calls that ask for verification of a bite or the protrusive midline, or calls about model anomalies. An experienced lab might also question appliance type or design concerns, because no one wins if there are future unwanted side effects in fit or function. And while some doctors and staff assume no communication equals competence, sometimes a lab is ‘conditioned’ to ignore these red flags which only diminishes treatment success. Most of these issues can be mitigated by a doctor and a qualified lab that work together as a communicative team.
Distorted Models or Incomplete Scans are the #1 reason cases don’t fit.
• Most common is impression material distortion caused by not being fully cured before removal (follow the instructions and add some buffer time!) or if the material is a low cost or low performance variety.
• For a well-fitting appliance designed to prevent tooth movement, make sure your impression or scan always includes the distal of the terminal molars and at least 2mm of tissue all around.
• Scan issues are most common around the terminal molars. Keep the areas being scanned completely dry.
• Clean up! Saliva, blood, and any debris in the scan area will reflect and interfere with the scanner’s reading.
• Please re-scan if your scan suffers from any of the problems in Figure 2.
Fill Tool: If scans are missing data or appear fuzzy, use the fill tool to capture missing data. Press and hold on the screen and select fill. Use caution with this, however. You can try to fill too much, and it becomes too much data for scanners to read.
Bite Registrations are the next point of concern.
• Understand the correct use and positioning of your chosen bite gauge.
• Confirm the amount of opening required for the appliance you are considering. Make sure your bite gauge reflects this opening. Most appliances require 4-5mm clearance between the U/L incisal edges.
• Some require only 3mm of clearance – but realize that this means ‘global flat plane’ clearance at the thinnest point.
• Verify and document where midline positions are. Observe where your patient’s dental midline is in:
1. Closed position – deviation may be functional (dentally-guided)
2. Protrusive position (is it repeatable?)
Determine your patient’s protrusive midline by having them translate a few times for you to recognize a constant. Note where the lower dental midline is compared to the upper dental midline, for both positions, and record this on the Lab Rx and in the patient’s chart. Documenting this is very important. First, it’s difficult to visually determine if a patient has incorrectly





Laura Sheppard BS, CDT, TE, is a practicing 40 year board-certified dental laboratory technician with her AAS in Dental Technology and BS in Education for Allied Health. Named to the ‘Top 25 Women in Dentistry’ roster by Dental Products Report, Laura has been nationally recognized and published as an expert and educator in the development and implementation of Dental Sleep Medicine and Quality Systems since 1993. As the design collaborator for DSG APM Positioner™ and DSG Remed-eze™, inventor for DSG Relaxer™, and co-inventor of MicrO2™ aka ProSomnus® AI, Laura’s expertise and contributions in dental sleep device invention, design, manufacturing, and regulatory compliance has been utilized to the success of many of today’s advanced sleep devices.



shifted when taking or scanning a repositioning bite. It’s great to be able to check this before you send the patient home. Second, without recording this in the patient’s chart or on the Rx, it’s hard to answer a midline question when the lab calls to question the bite.
An incorrect shift can often be confused with and accepted as the protrusive-translation position. Without this verification, a ‘connected’ sleep appliance will keep the patient incorrectly shifted all night, every night.
• Manual Repositioning Bites require a stable material. A heavy-body or rapidly-setting PVS bite registration material is best. Not wax or cotton rolls! Also, ensure your bite registration material captures the entire arch length to prevent models from rocking during articulation.
• Scanned Repositioning Bites require any gauge that allows for a stable anterior index, and you only need to scan one side of the arches.
You can also scan a manual bite. Before
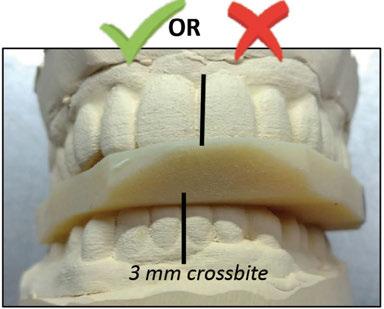
6: Note: Labs should not alter nor be asked to alter a protrusive bite for desired correction, this will introduce condylar misalignment.
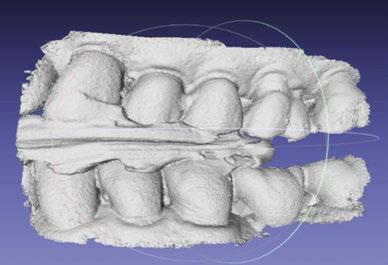
scanning a manual bite, cut away bite material to expose facial cusp tips for visibility.
Final Tip: Currently Used Appliances can also be helpful to the lab. To a seasoned wearer, a new appliance can be difficult getting used to. And, without known parameters, a lab technician will use ‘standard art’ to manufacture. An easy way to replicate the old appliance is to send your patient’s current appliance to the lab with the case. Request that the appliance be returned as soon as relations are captured. The lab can note and replicate the bite position, the mechanism position, the splints’ borders and contours, tongue space, etc. Even if prescribing a different type of appliance, the lab can try to glean as many ‘known factors’ as possible.
Future installments of this column will include help on Appliance Selection, Designs and Retention Challenges, Clasps & Adjustments, Bite Configurations & Other Design Tips, Design Overload & Liabilities, Benefits & Limitations of Materials, Edentulous Appliances, CAD/CAM, and Regulations.






by Drs. Preetam Schramm, Jason Hui, Pollyana Moura, Zohre German, Ju Ying Lin, William Stenberg, Emet Schneiderman
Background
The prevalence of Sleep Disordered Breathing (SDB) is well described and documented. Awareness of the disorder, its negative impact on health, and the financial burden it creates is growing globally. When SDB is viewed as a multisystem physiological disorder characterized by abnormal breathing during sleep that is often associated with repetitive upper-airway collapse, it is important to recognize that certain medications and the number of medications may have a direct impact on oral appliance therapy effectiveness. In mild forms, the SDB subtype, obstructive sleep apnea (OSA) manifests as snoring. Snoring is the most common form of SDB with about 37 million habitual snorers in the US population, almost 10%. More severe forms present as apneas, defined as an absence of breathing occurring for ≥10 seconds or hypopneas – shallow breathing associated with a 30% decrease in airflow for ≥10 seconds.1 Apneas and hypopneas are considered brain and cardiovascular stressors that are time-linked with blood oxygen desaturation (hypoxia), electroencephalogram arousals, hypercapnia, and increases in blood pressure, heart (tachycardia) and respiratory rate (tachypnea).
OSA involves several biological systems.3 Patients with OSA often present clinically with some or all of the following symptoms: daytime sleepiness, complaints of loud snoring, dry mouth on awakening, sexual dysfunction, forgetfulness and a concerned bedpartner. Frequently neglected during anamnesis for OSA are side effects from various medications addressing OSA-related symptoms and how they impact upper airway collapse during sleep. The research team led by Dr. Emet Schneiderman at Texas A&M University College of Dentistry (TAMUCOD) in Dallas, TX investigated this observation in a controlled trial in subjects randomly assigned to oral appliance only or oral appliance plus mouth shield. The results from their investi-
gations suggest various medications and their number are highly relevant to dental sleep clinicians who provide upper airway management with oral appliance therapy.
A recent publication from the team presented novel information on the influence of polypharmacy on respiratory dynamics during sleep among mild to severe OSAmouth breathing patients receiving either oral appliance only or oral appliance plus mouth shield.9 The myTAP oral appliance (AMI, Dallas TX) that comes with a mouth shield was used in this study (Figure 1). The study results showed persistent apneas, hypopneas, snoring and mouth breathing occurred among medication users of commonly prescribed medications after 8-weeks of using either oral appliance intervention. The list of medications used among study participants are listed in Table 1. At 4-weeks, among non-medicated subjects, those using oral appliance plus mouth shield had significantly less oxygen desaturations compared with oral appliance only users. At 8-weeks of using either oral appliance intervention, the respiratory event index (REI; #apnea + hypopnea events/hour) was significantly higher in medication users (17.8 [9.7 – 25.7] events/h) compared with non-users (6.4[3.1 – 7.9] events/h, p = .027). While both medication and non-medication users showed reduction in the REI, the percent REI, mouth breathing and snoring reduction was significantly greater among non-medication users. Anti-depressants and opioids/opiates users of either intervention, had lower mean and minimum oxygen saturation percentages compared with non-medication users.

To ascertain if the above study’s observations were consistent, a retrospective analysis of a previous TAMUCOD study whose subjects alternatively used two different types of oral appliances,8 found that the REI was significantly lower in non-medicated compared with medicated subjects who were using 2 or 3 different medications. Negative correlations were found between the numbers of medications (1 – 3) and the mean and minimum oxygen saturation with oral appliance therapy (unpublished data).

Challenges remain to present this polypharmacy information, identified by dental sleep clinicians conducting airway management to medical physicians prescribing these medications. Interdisciplinary approaches need to focus on communication with the
Preetam Schramm, PhD, is a psychologist and sleep scientist in the Department of Biomedical Sciences at Texas A&M University College of Dentistry in Dallas, Texas.
Jason Hui, DDS, is a general dentist and specialist in Dental Sleep Medicine in the Department of Comprehensive Dentistry at Texas A&M University College of Dentistry in Dallas, Texas.
Pollyana Moura, DDS, PhD, is an orthodontist and oral radiologist in the Department of Craniofacial and Pediatric Plastic Surgery, Dell Children’s Medical Group in Austin, TX.
Zohre German, MS, is the clinical research coordinator in the Department of Biomedical Sciences at Texas A&M University College of Dentistry in Dallas, Texas.
JuYing Lin, DDS, MS, is a periodontist in the Department of Biomedical Sciences at Texas A&M University College of Dentistry in Dallas, Texas.
William Stenberg, DDS, MS, PhD, is a periodontist and evolutionary biologist in the Department of Biomedical Sciences at Texas A&M University College of Dentistry in Dallas, Texas.
Emet Schneiderman, PhD, is an anatomist and the director of the Sleep Research Program in the Department of Biomedical Sciences at Texas A&M University College of Dentistry in Dallas, Texas.
patient’s respiratory-sleep health as the primary focus. The use of Home Sleep Testing to generate an apnea hypopnea index (AHI), a now very familiar parameter, could be utilized by dental sleep clinicians to determine oral appliance treatment efficacy. The AHI metric can be used as a biomarker of sleep respiration ‘responsiveness’ relative to oral appliance effectiveness. Oral appliance advancement measures collected at 4-week intervals in association with AHI can provide clinically useful information in support of optimal advancement (i.e., AHI <5 events/h)
Table 1: List of prescribed medications taken by participants in the clinical trial on OAT with and without mouth shield9 and their impact on the
or persistent residual AHI (>5 events/h) with polypharmacy.
Bupropion; Venlafaxine 2SNRI
Escitalopram 1SSRI
Methylphenidate
Zolpidem (+Benzodiazepine – OA+) 11Sedatives and hypnotics; ‘Z drugs’; Non-benzodiazepine; (GABA receptor agonist)
Non-significant increase in AHI; significant SaO2 desaturation increase with 20mg
Propranolol 1 β1-blocker Lower AHI in CHF patients 10
Trazodone 1SARI
Non-significant AHI increase in NREM sleep stages 2 and 3, but reduced AHI in Stage 1 7
Sertraline 11SSRI Increases AHI in depression 6
Fluticasone 21 Trifluorinated glucocorticoid (intranasal) Decreased AHI in children 2
Tamsulosin 1 α1-blocker; Anti-muscarinic Increases AHI (on CPAP) 5
Abbreviations: AHI, apnea hypopnea index; SNRI, serotonin norepinephrine reuptake inhibitor, SSRI, selective serotonin reuptake inhibitor; GABA, gamma-aminobutyric acid; SARI, serotonin antagonist reuptake inhibitor; CHF, congestive heart failure; CPAP, continuous positive airway pressure; OSA, obstructive sleep apnea; OA+, oral appliance plus mouth shield, OA, oral appliance only.
Awareness of the number of medications and polypharmacy’s detrimental impact on the AHI and assessment of oral appliance efficacy under pharmacological conditions is the next logical phase to enhance our understanding of upper airway management, biomarkers, SDB phenotypes and comorbidities as well as assessment of oral appliance treatment efficacy. Tracking the pathophysiology along a continuum to determine biomarkers, oral appliance incremental advancement and symptom changes from baseline to clinical improvement is a reasonable approach. The use of temporary oral appliances fitted chairside such as the myTAP might provide the cost effective and testing solution to determine the effect on sleep quality. Furthermore, titration measures of oral appliances may provide thresholds to create categories that facilitate communication and clinical decision-making in patients with a history of snoring, mouth breathing and OSA.
1. Berry, R.B., Budhiraja,R., Gottlieb,D.J., Gozal,D., Iber,C., Kapur,V.K.,et al. (2012). Rules for scoring respiratory events in sleep: update of the 2007 AASM manual for the scoring of sleep and associated events. Deliberations of the sleep apnea definitions task force of the American academy of sleep medicine. J Clin Sleep Medicine. 8:597-619.
2. Brouillette RT, Manoukian JJ, Ducharme FM, Oudjhane K, Earle LG, Ladan S, Morielli A. (2001) Efficacy of fluticasone nasal spray for pediatric obstructive sleep apnea. J Pediatr. 138(6):838-44.
3. Lyons MM, Bhatt NY, Pack AI, Magalang UJ. (2020). Global burden of sleep-disordered breathing and its implications. Respirology. 25(7):690-702.
4. Mickelson SA, Lian T, Rosenthal L. (1999) Thyroid testing and thyroid hormone replacement in patients with sleep disordered breathing. 78(10):768-71, 774-5.
5. Moran M. (2016) Reversible exacerbation of obstructive sleep apnea by α1-adrenergic blockade with tamsulosin: A case report. Respir Med Case Rep. 14;19:181-186.
6. Robillard R, Saad M, Ray RB, Bujaki B, Douglass, Lee EK, et al. (2016) Selective serotonin reuptake inhibitor use is associated with worse sleep-related breathing disturbances in individuals with depressive disorders and sleep complaints: a retrospective study. J Clin Sleep Med. 17(3):505–513.
7. Smales ET, Edwards BA, Deyoung PN, McSharry DG, Wellman A, Velasquez A, et al. (2015) Trazodone Effects on Obstructive Sleep Apnea and Non-REM Arousal Threshold. Ann Am Thorac Soc. 12(5):758-64.
8. Schneiderman E, Schramm P, Hui J, Wilson PD, Moura P, German Z, et al. (2021) Randomized Trial of 2 Self-Titrated Oral Appliances for Airway Management. J Dent Res. Feb;100(2):155-162.
9. Schramm, P., Schneiderman, E., Hui, J., German, Z., Stenberg, W. and Lin, J.Y. (2024) Obstructive Sleep Apnea Mouth Breathing Phenotype Response to Combination Oral Appliance Therapy. Frontiers in Sleep, 3, p.1272726.
10. Tamura A, Kawano Y, Naono S, Kotoku M, Kadota J. (2007) Relationship between beta-blocker treatment and the severity of central sleep apnea in chronic heart failure. Chest. 131(1):130-5.
by Kalli Hale, DDS, MPH, D.ABDSM, D. ABSB
There are few times in life that a decision you make completely disrupts your path. As a new dentist the idea of working in dental sleep medicine was so far off my radar it may have well not existed. As my journey in studying obstructive sleep apnea began, my plan was to focus on adults. I never planned to treat children and knew nothing about pediatric sleep related breathing disorders (SRBDs) – but all of that changed when I heard an extraordinary educator speak of this “fringe” aspect of healthcare known as pediatric sleep dentistry.

In 2019, I discovered that what I had been taught in dental school regarding pediatric snoring, bruxism, and tethered-oral-tissues was entirely wrong. Imagine my astonishment learning that a child’s inability to breathe well through their nose could be the root cause for their crowded teeth? I have some regrets in my early career, but the biggest was telling a parent their child’s snoring was normal and they would “grow out of it”. Little did I know that the snoring child would turn into a snoring adult…
The Best Decision I Ever Made? Foundation First, Teeth Second
I never thought I would be able to help children suffering from ailments such as ADHD, bedwetting, snoring, bruxism, mouth breathing, etc. by learning airway dentistry. I’m “just a dentist” clouded my thoughts many times as I’ve shared in previous articles, but little did I know there was no profession more qualified to treat these children by making sure their jaw growth/development was on track. I had no training in pediatric expansion, nor understood that the way our orthodontics was done in our early years would affect the way we breathed as an adult. The association between crowded teeth and SRBDs is the missing link for dentists and parents. I feel such guilt for the number of children I saw with major crowding that I recommended “waiting until the baby teeth fell out,” when I should have asked some very basic sleep questions. Our children deserve the best – imagine how you will change generations of kids by improving their breathing and sleep quality, which will affect every aspect of how they grow! It is heartbreaking that so many children are put on psychotropic medications for ADHD when there is a 50% chance they are in fact just tired.13 Given there is evidence that patients’ apnea hypopnea index (AHI) improves after dental arch expansion, and
The cure rate for OSA after tonsillectomy hovers around
5
1%
the correlation between underdeveloped jaws and ADHD, we must sleep test children suspected of ADHD!9,12 The long-term consequences of medicating children for ADHD are not well understood and there are published variations in the adherence of the clinical guidelines for managing this condition across the globe.10,11 We have to do better, and we can start by insisting on a sleep study for these kids.
Another regret? Ignoring pediatric bruxism. One of the most common parasomnias in children is sleep bruxism!1 The evidence for this has been published supporting the correlation between sleep bruxism and OSA.2 Although most of these studies were conducted in adult patients,2 sleep bruxism has been reported to be more common in children than in adults.3 The watch and wait methods taught in dental schools have little merit given the lack of evidence of spontaneous resolution, and the vast evidence in its correlation to OSA.4 The dental community needs to reevaluate their approach to bruxism in children. Because bruxism is associated with OSA, a first-line question in the medical history intake form should be whether parents have noticed teeth grinding in their child, so that the child can be properly screened and referred to an airway dentist.18,33
What about big tonsils, is removal the “cure” for pediatric OSA? While tonsillectomy is the most common surgery performed in children, with sleep-disordered breathing being the most frequent indication for

Kalli Hale, DDS, MPH, D.ABDSM, D.ABSB, is passionate about how our teeth affect our systemic health – the link between chronic jaw infections, periodontal disease, and subsequent heart problems. Her training in obstructive sleep apnea has transformed both her personal and professional career. Dr. Hale is a Clinical Advocate for VIVOS Therapeutics and works with dentists around the country to develop clinical protocols for the treatment of mild to moderate obstructive sleep apnea and sleep-disordered breathing. Her work in pediatric expansion and sleep-disordered breathing catapulted her speaking career and she lives by the slogan “we have to stop getting it wrong, for our kids.” She is faculty for the Dental Success Network, a key-opinion leader for Candid, and the Chief Dental Officer for Toothpillow. She travels monthly across the U.S. and abroad to teach dentists about Obstructive Sleep Apnea. Learn more about her sleep mentorship program at https://sleepwelljourney.com/.
this procedure,5 the cure rate for OSA after tonsillectomy hovers around 51%.5,6 Many children with OSA are not helped by clearing the “breathing straw” through removal of the tonsils and adenoids, often because underdeveloped dental arches and a weak tongue that continues to fall back/obstruct the airway are the true cause of their apneas. Furthermore, adenotonsillectomy can be associated with numerous risks and sequelae, including severe postoperative pain, bleeding, dehydration, complications of general anesthesia, and potential long-term adverse effects.5,7 Luckily, thanks to work from Dr. Audrey Yoon, we now have evidence that maxillary expansion shrinks the tonsil/adenoid tissue statistically significantly!14
When I learned about the guided growth appliances for children, my initial reaction was hesitation. Would they wear it? Could this habit-corrector monoblock appliance really do all the things I had seen in lectures? How can you get a 3-year-old child to wear something removable? If this is the first time you are reading about a pediatric nighttime oral appliance, I implore you to learn more. The craniofacial and dental changes that over 1,000 of my own personal patients have achieved deserves to put it on the map. When a child is actively growing, especially between the ages of 3-9 years old, these appliances are gold. If you can reestablish nasal breathing, improve tongue posture, and let that tongue do its job (i.e., expand the palate), you will change the trajectory of a child’s growth and development. While my own hesitation from self-inflicted bias delayed my offering this treatment to thousands of children, DON’T LET IT BE YOUR EXCUSE. Our own biases and misconceptions about the efficacy of these nighttime appliances have serious consequences for our pediatric patients.
As my journey progressed, I was also empowered to learn about myofunctional therapy. I now have oral myofunctional therapists (OMT’s) in all my practices as it has proven to be a critical component in the progress of my pediatric and adult sleep cases. Tongue
posture should be evaluated in patients with mouth-breathing. In an individual with appropriate tongue posture, the tongue can sit at the roof of the mouth; correct tongue posture helps ensure proper palate development, promoting palatal expansion naturally in children. Among patients who are chronic mouth-breathers, the tongue posture tends to be low and arch development is compromised.8
Pediatric sleep medicine is currently plagued by the inefficiencies caused by long wait times for PSG studies, while patients’ parents or caregivers frequently are given little to no information on treatment options for OSA other than CPAP therapy and surgery. Dental arch expansion, frenectomy, myofunctional therapy, and even simple interventions such as nasal hygiene are not commonly discussed with patients’ parents. Children with sleep-disordered breathing suffer not only from the complications and long-term effects of OSA, but from comorbidities linked to OSA such as ADHD and enuresis, which can be easily mitigated by proper airway management. The use of simple dental appliances for arch expansion and other noninvasive and nonpharmacologic interventions that promote proper oxygenation while preserving important lymphatic tissues can be life-changing for these children. The dental community needs to reevaluate their mindset and approach to pediatric OSA. It is the responsibility of orthodontists, general dentists, and pediatric dentists to examine the new research surrounding maxillary expansion and interceptive orthodontics to treat OSA and sleep-disordered breathing, so that the current epidemic of sleep disorders can be prevented for generations to come.
To avoid being misunderstood, please note I am not implying every patient is a candidate for a simple, removable, habit corrector appliance. My practice is full of fixed expander treatments, complex appliances, and clear aligners. The decision you must make as to which appliance to use will be your biggest challenge when you start. But rest assured you will not find a more powerful, minimally invasive tool, like the guided growth appliances for your little patients. It is my hope that this information motivates you
to pick a tool to learn about, so you can save more children.
A special thanks to those who have helped me become the airway dentist I am today: Drs. Jay & Tracy Elliott, Dr. Kyle Hale, Dr. Ben Miraglia, Mrs. RaeAnn Byrnes, and my teams at New Teeth Dental & ToothPillow.
1. Laberge L, Tremblay RE, Vitaro F, Montplaisir J. Development of parasomnias from childhood to early adolescence. Pediatrics. 2000;106(1 Pt 1):67-74.
2. Martynowicz H, Gac P, Brzecka A, et al. The relationship between sleep bruxism and obstructive sleep apnea based on polysomnographic findings. J Clin Med. 2019;8(10):1653.
3. Bulanda S, Ilczuk-Rypuła D, Nitecka-Buchta A, Nowak Z, Baron S, Postek-Stefańska L. Sleep bruxism in children: etiology, diagnosis, and treatment - a literature review. Int J Environ Res Public Health. 2021;18(18):9544.
4. Khoury S, Rouleau GA, Rompré PH, Mayer P, Montplaisir JY, Lavigne GJ. A significant increase in breathing amplitude precedes sleep bruxism. Chest. 2008 Aug;134(2):332-337. doi: 10.1378/chest.08-0115. Epub 2008 May 19. PMID: 18490400.
5. Schneuer FJ, Bell KJ, Dalton C, Elshaug A, Nassar N. Adenotonsillectomy and adenoidectomy in children: the impact of timing of surgery and post-operative outcomes. J Paediatr Child Health.
6. Hairston TK, Links AR, Harris V, et al. Evaluation of parental perspectives and concerns about pediatric tonsillectomy in social media. JAMA Otolaryngol Head Neck Surg. 2019;145(1):45-52.
7. Uwiera TC. Considerations in surgical management of pediatric obstructive sleep apnea: tonsillectomy and beyond. Children (Basel). 2021;8(11):944.
8. Chen W, Mou H, Qian Y, Qian L. Evaluation of the position and morphology of tongue and hyoid bone in skeletal Class II malocclusion based on cone beam computed tomography. BMC Oral Health. 2021;21(1):475. Published 2021 Sep 27.
9. Martos-Cobo E, Mayoral-Sanz P, Expósito-Delgado AJ, Durán-Cantolla J. Effect of rapid maxillary expansion on the apnoea-hypopnoea index during sleep in children. Systematic review. J Clin Exp Dent. 2022 Sep 1;14(9):e769-e775. doi: 10.4317/jced.59750. PMID: 36158770; PMCID: PMC9498642.
10. Ellis LA, Blakely B, Hazell P, Woolfenden S, Hiscock H, Sarkozy V, Gould B, Hibbert PD, Arnolda G, Ting HP, Wiles LK, Molloy CJ, Churruca K, Warwick M, Braithwaite J; CareTrack Kids Investigative Team. Guideline adherence in the management of attention deficit hyperactivity disorder in children: An audit of selected medical records in three Australian states. PLoS One. 2021 Feb 8;16(2):e0245916. doi: 10.1371/journal. pone.0245916. PMID: 33556083; PMCID: PMC7869992.
11. Wolraich ML, Hagan JF Jr, Allan C, Chan E, Davison D, Earls M, Evans SW, Flinn SK, Froehlich T, Frost J, Holbrook JR, Lehmann CU, Lessin HR, Okechukwu K, Pierce KL, Winner JD, Zurhellen W; SUBCOMMITTEE ON CHILDREN AND ADOLESCENTS WITH ATTENTION-DEFICIT/HYPERACTIVE DISORDER. Clinical Practice Guideline for the Diagnosis, Evaluation, and Treatment of Attention-Deficit/Hyperactivity Disorder in Children and Adolescents. Pediatrics. 2019 Oct;144(4):e20192528. doi: 10.1542/peds.2019-2528. Erratum in: Pediatrics. 2020 Mar;145(3): PMID: 31570648; PMCID: PMC7067282.
12. https://doi.org/10.1177/108705472412323
13. Moore M, Bonuck K. Comorbid symptoms of sleep-disordered breathing and behavioral sleep problems from 18-57 months of age: a population-based study. Behav Sleep Med. 2013;11(3):222-30. doi: 10.1080/15402002.2012.666219. Epub 2012 Dec 3. PMID: 23205586.
14. Yoon A, Abdelwahab M, Bockow R, Vakili A, Lovell K, Chang I, Ganguly R, Liu SY, Kushida C, Hong C. Impact of rapid palatal expansion on the size of adenoids and tonsils in children. Sleep Med. 2022 Apr;92:96-102. doi: 10.1016/j.sleep.2022.02.011. Epub 2022 Feb 19. PMID: 35390750; PMCID: PMC9213408.
The dental community needs to reevaluate their mindset and approach to pediatric OSA.
Sleep apnea, a pervasive and potentially dangerous condition, demands innovative solutions for effective management. DynaFlex, a privately held leader in the manufacturing of sleep apnea devices, stands at the forefront of such innovations with its precision-milled Herbst and Dorsal devices. These devices, coupled with the remarkable Accu-Fit liner, provide a groundbreaking approach to sleep apnea therapy, ensuring unparalleled comfort and efficacy for patients.
Precision milling, the process by which DynaFlex crafts its Herbst and Dorsal devices, is a game-changer in the realm of sleep apnea treatments. Unlike traditional fabrication methods, precision milling allows for the creation of devices that are exceptionally accurate in their design and fit. This accuracy translates directly into increased effectiveness in keeping the airway open during sleep, thus mitigating the disruptive breathing patterns characteristic of sleep apnea.
The Herbst device (Figure 1), known for its robust and adjustable structure, offers a reliable solution for many patients. Its design allows for the gradual advancement of the mandible, promoting better airflow and reducing apnea events. Similarly, the DynaFlex Dorsal device (Figure 2), which utilizes fins to prevent the jaw from falling back during sleep, is an excellent option for those seeking a less bulky alternative. Both devices, when milled with precision, provide tailored solutions that cater to the unique anatomical needs of each patient.


What sets DynaFlex apart from other manufacturers, however, is the integration of the Accu-Fit liner. This innovative feature guarantees a perfect fit on the first try, every time. The Accu-Fit liner is designed to be highly adaptable, ensuring that dental professionals can easily verify its proper placement and fit. This readability is crucial in ensuring that the devices function optimally, as even minor deviations in fit can significantly impact their efficacy.
The guaranteed fit provided by Accu-Fit also translates into enhanced patient compliance. One of the most significant challenges in sleep apnea treatment is ensuring that patients consistently use their prescribed devices. Ill-fitting or uncomfortable devices often lead to poor adherence, which diminishes treatment effectiveness. By offering a liner that ensures comfort and precision, DynaFlex addresses this challenge head-on, promoting better outcomes for patients.
The precision and reliability of DynaFlex devices reduce the need for frequent adjustments and replacements, ultimately saving time and resources for both patients and healthcare providers. The durability and resilience of these devices, thanks to advanced milling techniques and high-quality materials, further underscore their value in long-term treatment plans.
In conclusion, the DynaFlex precision-milled Herbst and Dorsal sleep apnea devices, enhanced by the Accu-Fit liner, represent a significant advancement in the management of sleep apnea. These devices offer a blend of precision, comfort, and reliability that sets a new standard in the field. By ensuring a guaranteed fit and promoting better patient compliance, DynaFlex not only improves the quality of life for those suffering from sleep apnea but also demonstrates a commitment to excellence and innovation in medical device manufacturing. For patients and practitioners alike, the benefits of these state-of-the-art devices are both immediate and profound, paving the way for healthier, more restful nights.
3-Year





The Accu-Fit™ liner guarantees a perfect fit
first time, every time. The delivery is simple and only takes seconds. There’s no adjustment of acrylic or clasp with this method.
The Accu-Fit™ material is completely re-adaptable and stable for several years.
A device does not become obsolete after a patient has had any type of dental restoration, sparing you and your patients the expense of frequent replacements.
by Rose Nierman, Nierman Practice Management
Medical billing doesn’t have to be complicated. Dental sleep medicine practitioners can build a successful practice by ensuring they submit accurate codes and documentation to payers. With the right systems and support in place, medical billing for oral appliances becomes more straightforward. At Nierman Practice Management, we are dedicated to educating dental offices, keeping them informed of the latest changes in medical billing practices. Staying informed helps you navigate medical billing and achieve quicker reimbursement.

separately obtained medical history
3. Conducting a medically appropriate examination and/or evaluation
Code 2023 “total time ... spent on the date of the encounter”
2024 “total time on the date of the encounter” that “must be met or exceeded”
99202 15-29 15
9920330-4430
9920445-5945
9920560-7460
9921310-1910
9921320-2920
99214 30-39 30
9921540-5440
One update is that Current Procedural Terminology (CPT®) 2024 removed the time ranges from office visit codes (Evaluation & Management (E/M codes). CPT replaced them with a single total time amount. This time “must be met or exceeded” according to the new descriptors. This change refers to both the new and established visit codes. For example, 99203 had a time range of 30-44 minutes. Now, the provider must meet or exceed 30 minutes of total service time to bill this code by time.
Determining office visit time now extends beyond face-to-face interactions. When selecting your code level, include:
1. Preparation for the patient (e.g., reviewing tests)
2. Obtaining and/or reviewing
A pioneer of medical billing in dentistry, Rose Nierman is the CEO of Nierman Practice Management (NPM) and creator of DentalWriter Plus Software. For more than 30 years, Rose has taught dental practices successful and ethical medical billing through the iconic Successful Medical Insurance in Dentistry seminars. Contact NPM at 1-800-879-6468 or at Coding@dentalwriter.com.
4. Counseling and educating the patient, family, or caregiver
5. Ordering medications, tests, or procedures
6. Entering relevant data into software
Legislative efforts are gearing up on preauthorization. Currently, a bill in Congress mandates 72 hours for an urgent preauthorization request and 7 calendar days for standard requests, optimistically reducing future timeframes for payer decisions when all the needed documentation is in place. Many states have recently set stronger directives for preauthorization. For updates about state mandates, visit your state insurance commissioner’s website or contact us at Nierman Practice Management.
To streamline the Dental Sleep Medicine process and help your practice thrive, consider adopting these practices: implement a web-based system for patient registration and history-taking, verify benefits allowing you to establish financial responsibility for oral appliances and send progress reports to coordinating physicians. This will help to simplify the process and maintain effective written communications with physicians to position your practice as the go-to sleep dentist in your area.



































Practicing Dental Sleep Medicine can be both rewarding and profitable….but it’s not always been easy…until now!
“Sleepifi has played a crucial role in expanding our dental sleep medicine practice while allowing us to maintain focus on our general dentistry services.”
– Ashley Spooner, DDS, D.ABDSM
VirtuOx, the nation’s largest sleep diagnostics provider is proud to introduce Sleepifi DENTAL, its innovative software platform that enables dentists to easily manage every process of the dental sleep medicine workflow, from screening and diagnosis to treatment and documentation preparation for billing.
1. Identify a patient who may have sleep apnea using the electronic sleep screening questionnaire.
2. Send your patient home with a multiuse NightOwl testing device, provided to you at no cost.
3. Schedule a telemedicine consultation with a sleep physician, who will order a home sleep apnea test. Easily track the status of the appointment and testing within the Sleepifi software.
4. After the patient completes their test, the sleep physician will interpret the



results and, if medically necessary, will prescribe an oral appliance. Prescriptions, physician notes, and the test report are all attached to the patient record.
5. Save your staff time by creating an auto-titration schedule. Sleepifi will text and email your patient when it’s time to repeat tests to titrate the oral appliance and measure efficacy. You’ll be notified when test results and patient subjective questionnaires are available for review.
6. Get paid with one-click preparation of all supporting documentation required to submit your insurance claim.
“You can count on Sleepifi to improve patient and staff experiences throughout the entire patient journey,” says Jon Fedele, a founder at VirtuOx. “Hundreds of dental practices are already leveraging the power of Sleepifi to increase revenue, save time, and improve patient outcomes, and you can too.”
Integrations with oral appliance manufacturers, billing companies, and EHR systems are next on the product roadmap.
Interested in learning more? Contact us at sales@sleepifi.com or (855) 472-8776.
“Sleepifi
has done an amazing job listening to their customers by providing an amazing product to simplify patient management while providing an easy to use system.” – Darren Ramsey, DDS













12 modules cover both the medical and dental science of sleep medicine. Dentists who complete the coursework and pass the exam are qualified to submit cases for board review to achieve Diplomate status. The certificate is a prerequisite for ACSDD Fellow and Diplomate


