The Concussion Riddle and the Breathing Brain™
by Cynthia Stein, PT, MEd, and Karen Parker Davidson, DHA, MSA, MEd, MSN, ARPN by Zhu Zhu, MD, PhD; Saniya Pervin, MBBS; and Daniel O. Lee, MD, FAAN, FAASM
by Zhu Zhu, MD, PhD; Saniya Pervin, MBBS; and Daniel O. Lee, MD, FAAN, FAASM



 by Zhu Zhu, MD, PhD; Saniya Pervin, MBBS; and Daniel O. Lee, MD, FAAN, FAASM
by Zhu Zhu, MD, PhD; Saniya Pervin, MBBS; and Daniel O. Lee, MD, FAAN, FAASM


Imaginethere’s no AHI. It’s easy if you try. No oxygen to measure, breathing is all you see. Imagine all the people, living for their health.
Huge apologies to Mr. Lennon. We must move away from what we know and allow ourselves to think more about the person than the numbers.
We learned to follow the numbers because in medicine it is often the best course – people’s symptoms are the result in disruptions to physiology that we can find in discrete biosignals. When blood sugar falls, people become pale, confused, and anxious.
Physicians observed people in hospitals with disturbed breathing and found a way to measure events that explained what they saw. When the airway closes, oxygen falls, people show characteristic signs; it’s easy to connect those dots and a whole segment of medicine formed around the results of the closing airway. Systemic consequences line up and doctors create therapies to recover health. In the part of sleep medicine that includes airway performance, treatment begins with resolving what can be measured – the airway blockages.
Dr. L. D. Pankey taught dentists to get to know their patients as part of the healthcare process. He said doctors couldn’t be as effective using what they know to help people until they and the patient understood how that treatment could benefit them. Drs. Hirshkowitz and Kryger wrote in Principles and Practices of Sleep Medicine in 2011 “High perceived benefit is the first, and perhaps the most important, step on the road to therapeutic acceptance and utilization.” Since patients can’t feel or measure their own AHI, they report to us their lifestyle problems – snoring, sleepiness, and other ways the poor sleep quality is affecting them. When our prescriptions match the patient’s perceived benefits, they apply the therapies we prescribe.

29 million Americans have sleep related breathing disorders. Since the founding of sleep medicine, the percentage of adults at risk that have been diagnosed, much less treated
successfully, has barely budged. Perhaps it is because we clinicians have focused too much on what we know – what we can measure and how our therapies address the numbers, instead of how we can provide our patients the benefits they can feel and observe. What they perceive as success. Sleepy patients use their CPAPs, snorers, their oral devices.
We know it’s success when our device ‘solves’ the medical problem by comparing pre-treatment tests with follow-up measurements, conveniently not thinking about the hours our therapy is not being used.
Steve Carstensen, DDS Diplomate, American Board of Dental Sleep MedicineMedicine is moving toward more a more ‘precise’ approach, taking into consideration more data, more expert labeling of the problem. Our field is incorporating endotypes, recognizing biochemical and biomechanical reasons why the airway functions poorly during sleep. More measurements, more data, more ways to address problems that don’t involve the patient’s perceptions. Soon, we’ll have pharmaceuticals to change the body’s response to carbon dioxide concentrations in the blood, reducing loop gain and/or raising the arousal threshold. Scientists and non-scientists have been training the body to manage CO2 for thousands of years using intentional breathing patterns. Which is the better way to address what we clinicians see?
Children breathing poorly suffer irreversible changes in brain development, with consequences no one will ever be able to measure. Recognizing and offering therapy to littles as early in life as possible is a benefit every caregiver can perceive. Fewer tests will be needed when clinicians spend more time getting to know the patient and offering treatments based in science but prescribed to meet what matters to them. It’s what we need to think about.
Cover Story
The Science Behind the Appliance

Learn about a big upgrade to a process used on every patient: bite registration.
Medical Insight
Narcolepsy
by Jyotsna Sahni, MDPatients with this rare neurologic disorder often have other sleep disorders such as OSA.


Restless Legs Syndrome


by Zhu Zhu, MD, PhD; Saniya Pervin, MBBS; and Daniel O. Lee, MD, FAAN, FAASM

Knowing about this sensorimotor neurological disorder can help you better treat your patients and communicate with their medical providers.
2 CE CREDITS
Medical Insight
The Very Real Relevance of Restless Legs Syndrome to Optimal Management of Many DSM Patients
by Daniel E. Taché, DMDThis highly prevalent sleep disorder can cause significant sleep fragmentation leading to sleep bruxism.
Adjunctive Therapy
The Concussion Riddle and the Breathing Brain™ by Cynthia Stein, PT, MEd, and Karen Parker Davidson, DHA, MSA, MEd, MSN, ARPN
Incomplete results might have a hidden reason.

The Academy of Clinical Sleep Disorders Disciplines is the only organization offering a fully online and on-demand certificate in Dental Sleep Medicine. Study the lectures and course materials at your own pace, then when you are ready, take the exam. The C.DSM certificate from ACSDD provides the necessary medical and dental knowledge to confidently approach physicians and seek insurance reimbursement.
The certificate is a prerequisite for ACSDD Fellow and Diplomate.
The Academy of Clinical Sleep Disorder Disciplines is the only organization offering a fully online and on-demand certificate in Dental Sleep Medicine. Study the lectures and course materials at your own pace, then when you are ready, take the exam. 12 modules present both the medical and dental science of sleep medicine providing a solid foundation for understanding clinical applications. Most dentists are able to complete the 13 CE program in 4-6 months.
The certificate is a prerequisite for ACSDD Fellow and Diplomate
16
Clinical Focus
There is No OSFA: How the Many Moving Parts of Sleep Apnea Demands Precision Medicine
by David E. McCarty, MD, FAASM You have the power to unlock mysteries – with profound results.
47 Military Matters
A Commemoration of Oral Health Services to Soldiers
by Dr. Francis Nasser, Jr. A special way to recognize the important role of military dentists.
48 Team Effort Rx for Boosting Actual Collaboration
by Steve Lamberg, DDS, D.ABDSM You can do this in your town.
50 Practice Management Schrödinger’s Dentist
by Ben Waldman Sales means more people get help.
52 Technology & Innovation
all functions.
42 Expert View How to Prevent a Snoring and Poor Sleep Public Health Crisis
by Howard Hindin, DDS The beginning of an open airway.
46 Product Spotlight Treating the Edentulous Patient with OSA Saying Yes to more patients.
The Preferred New Alternative Treatment for OSA
Explore a device that puts patientcentric medical care at the forefront.
54 Marketing How Much Should I Spend for a New OSA Patient?

by Ernie Cote, Bullseye Media, LLC
Focus on desired results and you will make good budget decisions.
56 Seek and Sleep DSP KnotWord
Spring 2023
Publisher | Lisa Moler lmoler@medmarkmedia.com
Chief Dental Editor
Steve Carstensen, DDS, D.ABDSM stevec@medmarkmedia.com
Chief Medical Editor
Lee A. Surkin, MD, FACC, FCCP, FASNC drsurkin@n3sleep.com
Associate Editor | Lou Shuman, DMD, CAGS lou@medmarkmedia.com
Editorial Advisors
Steven Bender, DDS
Jagdeep Bijwadia, MD (Pulmonary, Sleep)
Kevin Boyd, DDS
Karen Parker Davidson, DHA, MSA, M.Ed., MSN, RN
Kristie Gatto, MA, CCC-SLP, COM
Amalia Geller, MD (Neurology, Sleep)
William Hang, DDS, MSD
Steve Lamberg, DDS, D.ABDSM
Christopher Lettieri, MD (Pulmonary, Critical Care, Sleep)
Pat McBride, PhD, CCSH
Jyotsna Sahni, MD (Internal Medicine, Sleep)
Ed Sall, MD (ENT, Sleep)
Alan D. Steljes, MD (Cardiology, Sleep)
Laura Sheppard, CDT, TE
DeWitt Wilkerson, DMD
Scott Williams, MD (Psychiatry, Sleep)
Gy Yatros, DMD
National Account Manager

Adrienne Good | agood@medmarkmedia.com
Sales Assistant & Client Services
Melissa Minnick | melissa@medmarkmedia.com
Creative Director/Production Manager
Amanda Culver | amanda@medmarkmedia.com
Marketing & Digital Strategy
Amzi Koury | amzi@medmarkmedia.com
eMedia Coordinator
Michelle Britzius | emedia@medmarkmedia.com
Social Media & PR Manager
April Gutierrez | medmarkmedia@medmarkmedia.com
Webmaster
Eileen Kane | webmaster@medmarkmedia.com
MedMark, LLC
15720 N. Greenway-Hayden Loop #9 Scottsdale, AZ 85260
Tel: (480) 621-8955 | Toll-free: (866) 579-9496 www.DentalSleepPractice.com
Subscription Rate: 1 year (4 issues) $149
©MedMark, LLC 2023. All rights reserved. The publisher’s written consent must be obtained before any part of this publication may be reproduced in any form whatsoever, including photocopies and information retrieval systems. While every care has been taken in the preparation of this magazine, the publisher cannot be held responsible for the accuracy of the information printed herein, or in any consequence arising from it. The views expressed herein are those of the author(s) and not necessarily the opinion of either Dental Sleep Practice magazine or the publisher.




In my columns, I have always shared my thoughts on professional and personal success. I’ve shared MedMark Media’s triumphs, and in recent years searched with you for solutions to some very tough challenges. As always, I am so proud of MedMark Media’s publications and the team that has been the center of my life for so many years. With this column, I am thrilled to announce some amazing news. As of this writing, I just got notified that I am a 2023 Denobi Award nominee. This prestigious nomination is incredibly humbling and inspiring. The Denobi Awards recognize leaders in the dental industry worldwide – including, as the Denobi website notes, “clinicians, educators, brand leaders, students, administrative personnel, sales, advocates, speakers, and leading experts.” From the nominations, finalists include 10 individual winners, one dental team, and one individual that receives the esteemed Dr. Lou Shuman Denobi Pinnacle Achievement Award. Right now, as a nominee, I think back to the years when I ran MedMark out of my tiny condo. Step by step the company has grown into publishing of five magazines, many digital platforms, podcasts, webinars, and opportunities. Some have described me as a “go-getter,” but I like to define myself as a “goal-getter.”
Speaking of setting and reaching new goals, you all know that specialty dentistry is our focus and our passion. So some more good news is the debut this spring of our newest national publication, Pediatric Dental Practice US. Articles will focus on oral health from infancy through teens and offer pediatric dentists new insights on helping young patients. As we strive to inform and improve the practices of endodontists, implant specialists, orthodontists, and dental sleep medicine professionals, reaching clinicians that care for the youngest patients seems like a perfect fit into our coverage of dental care that spans a lifetime.
In this issue of Dental Sleep Practice, our Cover Story takes a look at bite registration, a key step that is often overlooked in the process of dental sleep medicine. Optimal Air, a patent-pending system for bite registration, developed specifically for dental sleep medicine from Nexus Dental Systems, is designed to be easy to use, provide an accurate measurement, and reduce pos-
sibilities for error. This issue’s CE explores Restless Legs Syndrome, offering a comprehensive view of its impacts, symptoms, and treatment, as well as common language that dentists can use with other medical providers. Our column on Adjunctive Therapy provides insight into the impacts of concussion and its connection to patients in the dental sleep practice.
I struggled over whether to announce the Denobi Award nomination in my column. That humble voice in my head didn’t want to seem boastful. But, I know that my team, friends, readers, and advertisers would want to share in my excitement of this recognition. This is not just about me. I always try to encourage you all to take some chances, believe in yourself, and as inspirational author Norman Vincent Peale advises have a “humble but reasonable confidence in your own powers.” I also try to emphasize my philosophy of “know your worth.” It sure is a fantastic feeling when others realize your worth too.
If you’re a dentist, you are taught to focus on smaller and smaller parts of human anatomy. From a big-picture overview of physiology, training is intensified to the oral cavity, then to the tooth, then to parts of the tooth. If you’re going to take the Airway Pledge and become part of the mission to raise awareness and educate the public (and yourself!) about the airway, you turn all that around and think back to the whole person.
DSP presents someone who has been leading the profession in raising curiosity about the entire body for over 50 years – most recently with the Foundation for Airway Health, the American Academy of Physiological Medicine and Dentistry, and soon Collaboration College. Dr. Howard Hindin – Howie to everyone – practices outside of New York City and influences healthcare around the globe.
DSP: Howie, tell us how you got started in this unique kind of dental practice.
HH: I started out wanting to be a history professor, but my family convinced me to consider a real career – and try dental school. I enjoyed my early dental practice, doing surgery, TMD, and cosmetic dentistry. Early in my practice, I spent 4 days at a workshop to learn a practice to help my pain patients achieve a deeper, alpha state of relaxation, so I could become a better TMJ dentist – that was
in 1972. I haven’t had a headache ever since, and I learned that we can be taught how to influence general health. Acupuncture training came next – that’s something I’ve used for my entire career. I’ve been part of working to ensure dentists and physicians can add innovative ways of therapy to their practice in an acceptable way without risking their license over it.

I studied nutrition because I wanted to help my patients control and reverse their diseases. I used to love to do periodontal surgery – really believed it helped my patients. After some training in nutrition, as an experiment, I treated the next 20 patients, half with surgery, half with nutritional counseling. While the surgery patients looked great right away, after six months, I couldn’t find the difference between the ones who took care of themselves after surgery and those who changed their nutritional habits. This isn’t a scientific study, of course, but being curious about what could be done helped me realize that what I’d been taught had its limits.
I believe the body wants to, and can, heal itself. If we can learn to recognize the obstacles to a higher level of function, then we can remove them. There are always ways to improve our general health. Early on, I studied with Mariano Rocabado, the famous physical therapist from Chile. He would hold a baby upside down to see if the child turned its head one way or another. He believed that would indi-

cate bad posture habits were forming and he would advise the parents on how to reset them. This story, and so many others, taught me to be constantly curious, to recognize and use the clues the body gives me to advise my patients on how to approach their health issues.
From my earliest days, I set out to make time to learn. I practiced three 12-hour days in clinics, so I could spend time in mentors’ offices – Harold Gelb, Brendan Stack, and others stoked my curiosity with their approaches to health. I’m thankful I never fell into the thinking that only one ‘camp’ was right, as so many did, and learned something from many dentists, physicians, acupuncture practitioners, and others along the way. I guess I was just too curious about everything to limit myself to one topic.
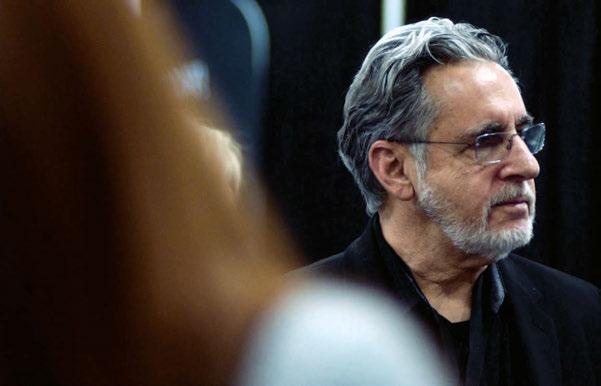

DSP: How would you advise today’s curious dentist to learn more, to follow a path like yours?
HH: First off, I don’t think there is a one path. Look for the crossroads, detours, and scenic side roads. If you do things that are interesting, more choices will present themselves, and you can build your skills by being open and curious about what comes your way. I’ve seen too many dentists align themselves with one guru or group or specialty, becoming comfortable and complacent, and make changing the way they think even more difficult. If you are a curious practitioner, there is always an “AHA!” moment that presents an opportunity to expand if you allow yourself to see it. Proper communication is a key, though. No one wants to feel like an idiot – and too often, a
lack of training creates a defensive posture. I think I’m pretty good at getting people to talk with one another; so, when I’ve encountered a dentist or a physician who has less training in airway health, I try to be careful how I talk about it to keep the conversation going. It is less important to impress someone with what I know than to find a way to open a clear path to learning.
One periodontist who was cotreating a patient warned me off expanding the arches. The patient had OSA and persistent periodontal disease, even with pretty good home care. I wanted to replace the oral device they were using with expansion, but the periodontist couldn’t see the connection between inflammation and OSA. The automatic, trained response was orthodontics with periodontitis is dangerous. However, if in fact OSA was a major contributor to the inflammation, nothing was going to solve it unless breathing was improved.
DSP: Out-of-the-norm practices sometimes present risks to dentists. Some are getting in trouble for stepping up to help patients with medical problems.
HH: Yes, when I started using acupuncture, nutrition, and things like posture evaluation, the FDA and state regulatory boards were paying attention to these things. I looked around my busy restorative practice, thought about my two little children, and kept things quiet for a while, not willing to risk all that. But I stayed curious. Some of us formed a group, called the Foundation for Advancement of Innovative Medicine (FAIM) to advocate for
patient and doctor rights to practice complementary medicine. We were getting practitioner, patient, and corporate support and doing a lot of good education. One of my proud achievements is we helped get a bill passed in the New York legislature protecting the right of licensed health-care providers to practice complementary medicine (outside the ‘norm’ at that time). The bill provided they couldn’t be prosecuted just because their practice was different. This was the first health-care bill ever passed in New York over the objection of the NY State Medical Society. I became President of FAIM – think I must have missed a meeting and got elected – and that’s what led me to always think about what else we can be doing to help our patients.
There is so much more we can and should be doing for our patients. I can usually get people with different perspectives to sit together and have a conversation, to work together on mutual goals. One big problem we all have is that narrow focus – as I said about dentists getting interested in smaller and smaller parts of the oral cavity. I like to turn the funnel around and expand into other areas. We as dentists need to expand our view and find colleagues in other practice disciplines to collaborate with and cotreat. With these colleagues, once we recognize all we have in common, like airway, we can find ways to provide more complete care for more optimal results. Together we turn our awareness from tiny parts to how the body works as a whole, seeing clues we’ve never seen before.
DSP: You have been an advocate for dentists to work with physical therapists.


HH: Breathing is a whole-body function. All practitioners influence the airway for good or bad, whether they know it not. We’ve been watching our patients stand and walk in the clinic for a long time and noticed that changing jaw position and changing breathing makes a difference. As we’ve learned more about breathing, diaphragm function, and how it interacts with posture, what has become obvious is the way people stand and walk shows the compromises they’ve had to make over many years because they don’t breathe well. As breathing improves, they don’t have to work to compensate as much;
those long-established physical compromises are best treated by physical therapy. At the same time, people seeking PT who don’t breathe well may not respond to treatment – just like the periodontist’s patient I talked about. When I found a few physical therapists through my studies with Rocabado, Ron Hruska, Gregg Johnson, and others, I not only had answers I never had before, but partners in care. There is now a rapidly growing group of physical therapists in the AAPMD
DSP: What’s next?
HH: Every dentist, actually every healthcare practitioner, should take the Airway Pledge: go to the Foundation for Airway Health website, AirwayHealth.org, and follow the prompts. When we all choose to ask our patients about how they breathe, we’ll be moving them in the direction of health. In case anyone needs an incentive, my web managers told me over 1,000 people a month are looking to connect with an airway practitioner through our website. Taking the Airway Pledge, which costs nothing, is the way to get on the list.
A long-held vision of mine is Collaboration College. Today, if health-care providers want to learn about airway, they must go here and there to find information. I want there to be one place they can get everything they need. Clinical, scientific, communications, different specialties, even finance courses will be available to help every provider find answers to their clinic needs. It’s coming soon from the American Academy of Physiological Medicine and Dentistry, aapmd.org.
Over the past 20 years, there has been a dramatic rise in awareness of and interest in dental sleep medicine. In response, there have been major advances in home sleep testing, pulse oximetry, 3D scanning, 3D printing, and an array of different and specialized appliances have been developed. Yet, there have been relatively few advances in one key step in the process: bite registration.
Bite registration is one of the most important elements in successful Oral Appliance Therapy. Accurate measurements are key to fabricating a comfortable and effective device for treating OSA. The ideal starting position for treatment is a perfect balance between comfort and effect. Getting this right can make a big difference with patient compliance and ultimately the success of treatment. If the device is set too far forward and is uncomfortable, the patient may abandon treatment. Too many return visits for titration can lead to patient frustration, and even abandoning treatment. Accurate bite registration can prevent both scenarios: patients can experience treatment benefits on the first night, with little discomfort adjusting to the device. Positive initial experiences increase patient buy-in, ultimately leading to better treatment outcomes.
Despite the crucial role bite registration plays in dental sleep medicine, there are still
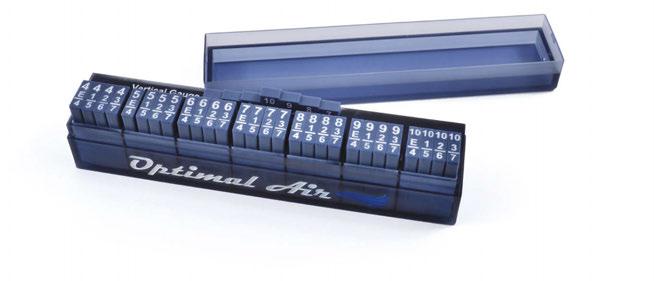
only a handful of alternatives on the market, each with their limitations.
There are several issues that in various ways can apply to all the currently available options:
As the science of dental sleep medicine has advanced, there is growing acceptance that many patients benefit from a combination of horizontal protrusion and vertical rotation of the mandible. Many bite registration systems are horizontal only, or with limited vertical positions.
Bite registration should not take very long. Some options select a random starting point, waiting until the patient returns for titration to fine-tune the mandibular position. This delay in finding an ideal point of efficacy can lead to patient frustration and even abandoning treatment.
The variation in bite registration systems can lead to inaccurate measurements in several ways. Some devices require very specific positioning to get an accurate reading. Some are manufactured using inherently variable methods. We tested one popular system and
found that some of the gauges can be off by as much as 300 microns, which seems small but can be a huge difference when titrating an oral appliance.
Some bite registration systems are overly complicated, with pieces that need to be flipped or reversed to step through all the sizes. Some require calculations to determine the final measurement, or specialized training like phonetic bite set methods. Some methods are so complicated that dentists don’t trust their assistants to take the registration correctly, resulting in more chairside time for each case. Complicated methods result in longer time in the chair and measurement mistakes, leading to more titration visits.
Not all bite registration systems play nicely with 3D scanners, which are increasingly replacing impressions. 3D scans are more accurate, and for 3D printed appliances, allow an entirely digital workflow. But not all materials and shapes are ideal for taking 3D scans of a patient’s start position. Shiny, reflective surfaces can interfere with the sensors, producing inaccurate scans. Bulky or obstructive devices can prevent the scanner from “seeing” enough teeth.
Meet Stan Jones, a 26-year veteran of dental sleep medicine and inventor of Optimal Air, a patent-pending system for bite registration developed specifically for dental sleep medicine from Nexus Dental Systems. Stan got his start as a dental assistant back in the 90s just as dental sleep medicine was starting
Stan Jones brings over 25 years of experience with coaching dentists and their teams in Dental Sleep Medicine, from the early days, and has watched it evolve. He has extensive knowledge and hands-on experience in the implementation and practical application of Dental Sleep Medicine. He has studied the mechanics of oral sleep appliances, and understands that every appliance needs to be customized for one patient. He is a certified dental assistant and a dental lab tech for over 30 years, and the lead trainer and coach for Nexus Dental Systems. Stan looks forward to meeting you and working together to streamline and optimize your sleep practice.

to gain wider acceptance. “I went to a day seminar on the topic with [his dentist], and that was the first time that I heard the words ‘dental sleep medicine’ used together,” Stan recalls. The following week Stan got a sleep test and was diagnosed with Obstructive Sleep Apnea. His physician offered a CPAP, but after attending the seminar, he decided to try oral appliance therapy first.
At the time, only a few appliances were available. Stan studied the different types carefully and being a lab technician, took his own impressions and fabricated his first device out of wire and acrylic. Within 3 months, his blood pressure was down, he had lost weight, and his AHI went from 28 to 7. This began a decades-long journey into the world of dental sleep medicine. Over the years since, Stan has worked with dentists of all experience levels to integrate Sleep Medicine into their practices as a coach. He has
developed and refined protocols for each stage of sleep medicine in the dental practice – laser focused on making the process seamless for the team and reducing opportunities for errors.
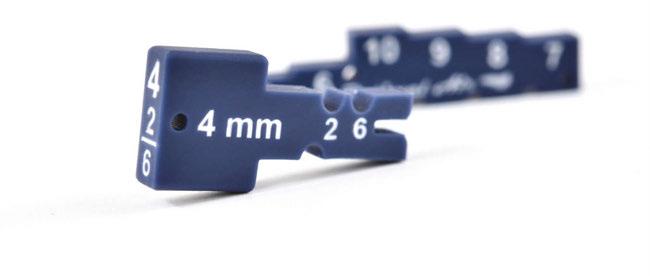
“For many years, I used horizontal bite systems to set the bite for oral sleep appliances, but after studying the upper and lower airway and TMJ, I began to consider the possibility that horizontal and vertical offset might be the secret to optimal jaw position.” At the time, there were several systems on the market that incorporated horizontal and vertical advancement, and Stan tried them all. He received positive feedback from patients, and dentists were getting good therapeutic results, but he felt the available systems were complicated and difficult to use compared to a horizontal-only method like a George Gauge™.
Optimal Air has integrated well into my dental sleep workflow. There’s honestly so much to love about this product, especially for those familiar with Airway Metrics. The vertical gauge is much easier to use, more precise, and allows for patient buy-in as they can feel and hear their snoring soften chairside. The Horizontal keys have notches that sit better on patients’ incisors, which seems to improve the stabilization of the mandible in protrusion. The abundance of keys really helps us to dial in an accurate starting position and feel more confident about it. The large handle on the Horizontal keys, easy to read labeling, and very organized arrangement are advantages that make this system easy on myself and the team.
– Dr. Marc Newman, Newman Dental Sleep Medicine, Carmel, IN
Over the years, Stan had used all the various techniques to set a bite, searching for each patient’s optimal starting position. No method was exact, and devices always had to be titrated for optimal performance. Some patients quit therapy because oral appliance therapy was not comfortable at the starting position of the device. Each method of measurement came with its own learning curve. There could be significant differences in measurements based on how the device was held and read. Some systems involved flipping measurement blocks and doing calculations to determine jaw position. It was easy to write down the wrong number. That just didn’t fit with Stan’s philosophy of keeping things seamless, simple, and reducing the opportunity for error.
Stan knew there could be a better way. It needed to measure vertical and horizontal displacement. It needed to get the measurement right, before the appliance was made. It needed to be simple enough that the results would be the same no matter who took the measurements. After years of development and field testing, he partnered with Nexus Dental Systems to bring Optimal Air to practices across the country in 2023. “We’re always looking for smart solutions that improve everyday processes in dental practices. Optimal Air is exactly that. It’s a big upgrade to a process used on every patient - at the end of the year it’s a big difference for the practice,” says Brett Brocki, one of the founders of Nexus Dental Systems.
Every element of Optimal Air is designed to make the system easier to use, provide an accurate measurement and reduce possibilities for error.
Optimal Air comes with a 7-level vertical gauge, in 1mm increments. This allows accurate vertical measurements within 1mm to be taken prior to the fabrication of the appliance.
Stan paid special attention to the shape of the horizontal keys. Other systems use double-sided keys, with different measurements on each side. This makes it hard to know what size was in the patient’s mouth and makes it hard to hold the key. Optimal Air keys are one sided, with the measurements written on each side, and with a large key shape on the other side. This makes the keys easy to hold, and easy to see what size is in the patient’s mouth, no matter where you are. Optimal air also features a safety system: a small hole in each key, allowing dental floss or wire to be threaded through, which prevents keys from falling on the ground or worse, into the patient’s mouth.
Optimal Air is proudly made the USA, 3D printed in house to an accuracy of under 50 microns of the indicated size. The bite notches on the horizontal keys are deep and oval shaped, making for a more secure fit on the tooth compared to systems with shallower or more rounded notches. Less wobble and play in the notch makes for a more accurate and reproducible bite registration.
The Optimal Air process is designed top to bottom to be easy to understand and fast to administer. First the clinician uses the vertical gauge to determine optimal vertical displacement, then tests each of the 4 horizontal keys for the corresponding vertical size. The keys are tested in order from left to right, with no flipping, no calculations, and only one set of numbers visible on all sides. This makes it easy for the clinician to record the correct measurements every time – spending as little as 2 minutes taking the bite.
I have been using Optimal Air for the better part of a year now. What I most value is that I am able to find a very therapeutic bite right out of the gate. I have had multiple experiences where my mandibular advancement appliances required zero titrations, which saves on chair time but also helps the patients feel confident in their treatment and my clinical skills. I love that I have the ability to control both vertical and horizontal possession independently with great precision and to demonstrate a desired outcome to my patients. The key system is easy to use. As part of the process of using Optimal Air, it also allows you to control for and evaluate upper/nasal airway restrictions that may affect treatment while assuring that you have the conversation with a patient who may benefit from nasal expanders or additional upper airway interventions. Optimal Air has helped make me a better clinician for my patients.
 – Adam Milmont, DDS, Hilltop Family Dental, Casper, WY
– Adam Milmont, DDS, Hilltop Family Dental, Casper, WY
Optimal Air is an ideal system for 3Dscanning. The selected horizontal key is compact and does not interfere or block any teeth. The keys are printed with a non-reflective surface, so the light from the scanner or ambient light from the room does not cause errors due to reflections.
While there have been no definitive studies on Optimal Air yet, field testing has shown incredible potential. Dentists are reporting fewer titration visits are required to get optimal results, reducing the cost of treating each case. Some patients require no titration at all. Most patients are experiencing positive results the first night of treatment with appliances made using Optimal Air: their snoring stops, their AHI drops, and they feel better. For more information on Optimal Air, visit optimalairsleep.com or nexusdentalsystems.com.
Sleep Apnea. Say those words to a group of physicians or dentists, and then wait a minute. After you’ve let the words sink in, ask the most gregarious person in the room for a definition.
Chances are, you’ll get a response akin to: “That’s a condition where soft tissues of the back of the throat collapse during sleep, leading to snoring, disturbed sleep, daytime tiredness, and cardiovascular consequences.”
Then everybody in the room will nod, because it sounds like a good explanation. Somebody might even clap, because the phraseology was so good. Your gregarious friend will blush.
Not to be a killjoy, but good as it sounds, this explanation also happens to be wrong. Well, not wrong, exactly. Incomplete may be a better word. And this is where all the trouble starts.
Your gregarious friend appears crestfallen.
Truth be told, the entity commonly known as Sleep Apnea has many “moving parts,” variably present in each individual, making the granular presentation of each case as variable as a fingerprint. Each person experiences Sleep Apnea differently, because the disease is different in every iteration.
Think about that.
Some individuals with this label can’t stay awake. Some can’t sleep at all. Some are heavy. Some are thin. Some have ruinous, catastrophic symptoms. Others don’t notice it. Some snore like a chainsaw. Some are completely silent. Some will die young if they don’t get treatment. Others will die old, of something else, and will never know they had it.
At the end of the day, the label can mean so many things, it flutters at risk of being meaningless.

To say Sleep Apnea is conceptually “complicated” is an understatement, kind of like saying Jesus is “famous.” McKeown et al do a wonderful job of picking apart this complexity in a recent review, a worthy read for anyone interested in this subject. The basic idea is that a floppy airway is just one piece of a larger puzzle, a revelation that helps to explain why a singularly anatomic treatment strategy (like CPAP or oral appliance therapy) doesn’t always work.
Let’s explore that.
In the jargon of the field, a “floppy” airway that’s easy to collapse is said to have a high pharyngeal critical closing pressure, usually designated as a “high Pcrit.“ Anatom-
Mini-Residency
2023 - 2024
Tufts University School of Dental Medicine’s Dental Sleep Medicine Mini-Residency is a 6-month program where participants engage with the material through live lectures from world-renowned experts in the field, workshops, and self-study. The live portions of this program are split into three 3-day modules and two half-day intermodules:
Module I: Live-Streamed Online
September 28 - 30, 2023
Intermodule 1: Live-Streamed Online
December 2, 2023

Module II: On Campus
January 18 - 20, 2024
Intermodule II: Live-Streamed Online
March 2, 2024
Module III: On Campus
April 11 - 13, 2024
Registration open! Space is limited. dental.tufts.edu/CE

ic treatment strategies like positive airway pressure therapy and standard mandibular advancement devices tackle this component. When they work well, everyone goes back to your gregarious friend to tell him that he was right after all.
When they don’t work, though, we’ve got some more head-scratching to do. In these cases, it’s helpful to know that there are three other “moving parts” in this complex machine, namely: arousal threshold, loop gain, and upper airway recruitment.
Let’s take a tour.
A person is said to have a low arousal threshold when they’re easy to wake up from sleep. Mild shifts in CO2, mild discomforts
associated with increased upper airway resistance and snoring vibrations will wake these folks up. These are the sleep-apnea-insomniacs, with autonomic overdrive, trending towards daytime anxiety and panic symptoms.
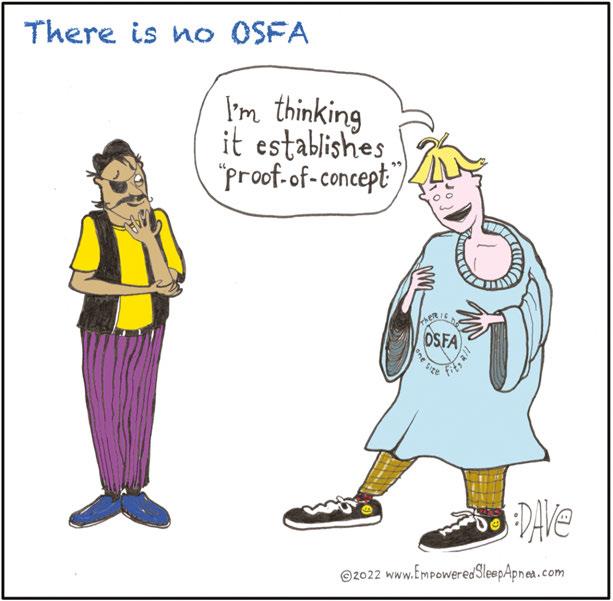
On the other hand, other individuals have a very HIGH arousal threshold, meaning they continue sleeping even when struggling to breathe against a closed airway. This can lead to much deeper oxygen desaturations, which drives more end-organ damage.
The arousal threshold is like a volume knob, and it can fluctuate over time. Things like pain, chronic mouth-breathing and psychological trauma can lower it, while some medications and chronic exposure to intermittent hypoxia can make it higher.
The concept of “loop gain” is an engineering term that describes the “twitchiness” of a self-correcting system. How aggressively does the system respond, when a parameter gets out of whack?
Let’s look at an example. If your home furnace has a high loop gain, as soon as the temperature drops below the desired setpoint, the furnace fires up so aggressively that it overshoots the goal, and makes the house sweltering hot, before it shuts off. It won’t come back on again until the house is too cold. Over and over it goes, too-cold alternating with too-hot, never achieving stability.
If control of breathing is like a thermostat, then the CO2 level is the “temperature” that the brain is trying to control. When a breathing pause occurs, CO2 level will rise, and trigger a corrective response: recovery breathing with an arousal from sleep. Those with a high loop gain tend to overdo it, taking several gigantic breaths, driving CO2 down low enough that the respiratory drive is temporarily erased.

Central apnea: it’s nice to make your acquaintance!
The thing about loop gain: it’s fluid over a lifetime, but, as a general rule, it increases with age, and it’s higher with mouth-breathers. Cardiovascular disease, by virtue of introducing a longer circulation time, also contributes to increasing loop gain. For example, if a person has atrial fibrillation, the pump function of the heart is simply less efficient. It takes longer for blood to get around the block. In our thermostat analogy, this would be akin to having the temperature sensor a
long way away from the furnace. The delay in message delivery about the status of the system makes for a loping, periodic response, rather than stability.
The final element to consider is upper airway recruitment. This refers to the concept that the upper airway has a resting motor tone that changes between the sleeping state and the waking state. Whereas the concept of high Pcrit imagines a flaccidity to the upper airway (implying a status of “always floppy”), the concept of upper airway recruitment acknowledges that the many muscles comprising the upper airway may be differentially recruited during sleep.
In other words, the muscles aren’t floppy all the time. In fact, these muscles can be retrained, using a strategy called Breathing Retraining Exercises (BRE). The amazing thing? BRE also moves the needle in the right direction for the other “moving parts” of Sleep Apnea, too.
The main point of all of this? There is no One Size Fits All solution to the beast we call Sleep Apnea.
Fortunately, McKeown et al offer a more functional paradigm for Sleep Apnea management called Precision Medicine. Practically, this means deconstructing the functioning phenotypes of disease active in an individual patient, whilst simultaneously providing the right coaching to help that person understand what they might gain from a given treatment, and what they might be missing out on. There is no OSFA. The complexity of Sleep Apnea demands that we can no longer dedicate ourselves to caring for a “label.” We owe it to our patients to care for them, as individuals. That’s the human thing to do. That’s a statement even our gregarious friend would probably agree with.
Recommended Reading:
McKeown P, O’Connor-Reina C, Plaza G. Breathing Re-Education and Phenotypes of Sleep Apnea: A Review. J. Clin Med. 2021, 10,471.
https://doi.org/10.3390/jcm10030471
ANNOUNCING the
launch of a new YouTube series: Nexus Connexus. This series will embody our Nexus Dental Systems’ vision and mission to inspire others to take action and be informed.


We are all extensions of this great cause and your efforts can benefit so many!
WATCH NOW
https://www.youtube.com/ @NexusDentalSystems

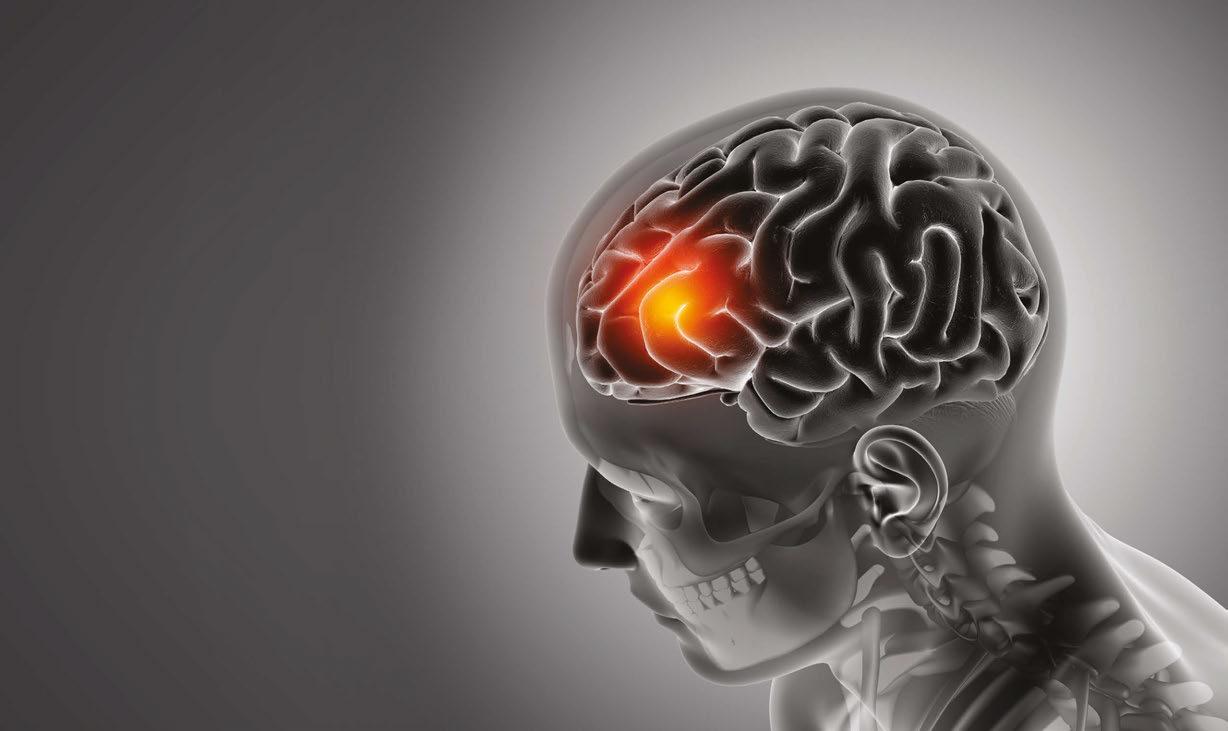
If you are a sports connoisseur and watch the news often, the numerous injuries resulting in a concussion are overwhelming and may catch your attention. More than 3 million concussions occur annually with approximately 1.7 million concussions among kids where nearly 20% are sports related, more often in girls than boys.1 Based on the prevalence statistics, concussive care is finding its way into many medical, dental, and ancillary practices such as chiropractic and physical therapy. Many clinicians may not have recognized the connection to breathing, especially in the dental chair.2 The common denominator among these specialties and the injury is the breathing brain. How does the practitioner address this type of injury in their practice, and how is it identified? Major concerns in recent years are the longitudinal effect of concussion on health, such as vestibular changes, the development of chronic traumatic encephalopathy (CTE), and sleep apnea.3
A concussion impacts the “breathing brain” by a potential disruption in coordination between the brain and lungs because the brain cannot function as it did prior to the injury. The result is breathing disturbances with symptoms of fatigue, dizziness, and shortness of breath. Furthermore, breathing problems
may be misidentified as sleep disordered breathing problems (SDBP), headaches, daytime fatigue, or exercise intolerance. The respiratory issues from post-concussion syndrome (PCS) may linger for months or years after the initial injury before diagnosis. A thorough history in the dentist’s office with a patient suspected as having SDBP should include concussion.
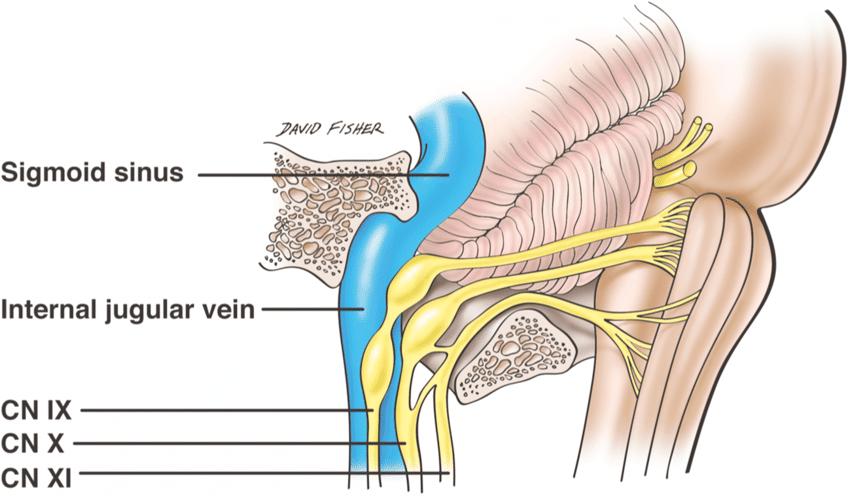
When there is any form of blunt trauma to the head, the bones of the skull become jammed. These bones fit together like a puzzle. The sphenoid and occipital bone articulate with each other to form the sphenobasilar joint. The temporal bone articulates with the occipital bone to form the jugular foramen. This foramen is where the glossopharyngeal nerve (IX), the vagus nerve (X), spinal accessory nerve (XI), and jugular vein exit from the brainstem (Figure 1). Because trauma shifts these bones, it affects nervous and vascular transmission. The vagus nerve is a part of the autonomic nervous system (ANS). This nerve is the major sensory pathway from the lungs to the brain. It controls pulmonary function and it regulates respiration, including normal breathing and respiratory defense mechanisms, and also provides sensory feedback from the lungs to the brain. This is why breathing has to
• Durable, biocompatible, and medical grade nylon
• Efficient manufacturing process resulting in a high value, affordable quality product

Available at apexsleep.com & serenasleep.com
• A temporary, 30 day, semi-custom, oral sleep appliance




• Chair-side fabrication in less than 10 minutes using heat-to-fit trays
• FDA Cleared
Available at be-innovations.com
9 different strap lengths allow for advancement of the mandible in 1 mm increments
ema-sleep.com
be measured and addressed in treating Post Concussion Syndrome.

As part of the care plan, predictive models in symptom recovery using artificial intelligence (AI) have been discussed and researched. Newer modalities for assessment and treatment should be considered in making clinical predictions and separated from the potential misdiagnoses mentioned above.4 The role of physical therapy (PT) is outlined in concussive care that further accentuates the collaborative relationship with dentistry beyond the posture and positional aspects of SDBP.5
Oleski et al. (2002) examined motility of the cranium on x-rays post cranial vault manipulation. The findings showed 91.6% of patients had documented cranial bone movement differences in measurement at 3 or more sites on the radiographs.6 This type of manipulation connects to Nasal Release Technique (NRT). NRT, developed by Dr. J. R. Stober of Portland, OR in the 1930s, has many other names, such as nasal specific technique, cranial facial release, endonasal technique, and neurocranial restructuring. The procedure is one aspect of concussion care and is done by inserting a finger cot attached to a blood pressure bulb into the 3 nasal meatuses. The balloon is quickly inflated and deflated which is said to adjust the bones of the skull. NRT is commonly used by physical therapists and chiropractors to mobilize the bones of the skull after concussion, for sinus problems, and treating headaches. Dentists use it prior to oral expansion therapies. Mystery and skepticism surround the efficacy of NRT and the impact of breathing in the post concussive patient because this has never been researched. In the first of its kind study, an analysis of data from transnasal pressure changes, nasal flow limitations, and vestibular changes in 9 concussion patients was conducted to find a correlation between the measurement variables and NRT.
Cynthia Stein, PT, MEd, is a physical therapist and tireless educator. She served as a commissioned officer in the US Navy as a staff physical therapist at Annapolis Naval Hospital and later as chief physical therapist at Philadelphia Naval Hospital. She owned and operated Squirrel Hill Physical Therapy for 30 years in Pittsburgh,Pa. During this time, she attended extensive training on methods for treating concussion that included standard vestibular rehab and alternative methods. As the founder of Conquer Concussion, she has taken her expertise on the road and long distant learning platforms teaching her proprietary Nasal Release Technique around the world to numerous medical and dental providers over the past 8 years. She graduated from the University of Pittsburgh with a B.S. in Physical Therapy and Temple University with a Masters in Education.
Karen Parker Davidson, DHA, MSA, MEd, MSN, ARPN, for over two decades has held many positions in the medical device industry in the ENT and Sleep markets, in addition to thirty years of clinical experience to include service as a Critical Care Nurse and Flight Nurse in the US Air Force Reserves. Dr. Davidson is adjunct faculty at Liberty University and Central Michigan University, founder of FACT Healthcare Consulting Group, and creator of the patent pending DAFNE Score System to guide and educate healthcare providers the values of objective nasal function and treatment options and improvements based on the readings. She is published in medical journals discussing airway disorders, a coauthor of “The Power of the Tongue In the Beginning, We Were All Tongue Tie” and “Sleep Apnea and Pregnancy: The Female Response to Sleep Breathing Disorders”, a contributing author to “Growing Into Breathing Problems: The Quest for Collaborative Life Time Solutions” and “Health Informatics and Patient Safety in Times of Crisis”, and the author of an upcoming book for release this year, “Breathe Through Your Nose, Don’t Pay Through It: The Impact the Healthcare Industry has on Nasal Function and How We Breathe”.

Each participant had three measurements done pre and post NRT: transnasal pressure changes/nasal resistance with 4-phase rhinomanometry (GM Instruments, Ltd.), nasal patency and flow limitations measured and Peak Nasal Inspiratory Flow (PNIF) meter (GM Instruments, Ltd.), and vestibular changes measured with eye tracking technology (RightEye, LLC). The mean age was 36.9 with 45% male, 21.5% female. The results found 8 of the 9 patients, or 88%, had a 55% decrease in inspiratory mean resistance (1.27-0.57 Pa/cm3/s) and a 26% decrease in expiratory mean resistance (0.98-0.72 ro Pa/ cm3/s). and a 24% increase in inspiratory flow (102- 126 L/min). Seventy-five percent of the cohort had vestibular changes. Patient #7, who had an increase in transnasal pressure changes was identified as having a histamine reaction to latex. The results provide preliminary evidence that NRT can increase nasal flow and decrease nasal resistance. In postnasal release testing, Martha Cortes, DDS, also found a correlation between sleep apnea and transnasal pressure changes in the concussion patient with 4-phase rhinomanometry, in addition to the vestibular chang-
es seen in patients with OSA. The study is in peer review for publication.
Based on the study outcomes, it is recommended that airway dentists ask patients if they have a history of concussions or concussive events if they suspect them of breathing disorders or OSA.
Acknowledgments: We wish to thank Martha Cortes, DDS, and Jennifer Hobson DPT, MTC, CFC, CMTPT, OMT of the Hobson Institute for their valuable contributions to the study.
1. Kosoy J, Feinstein R. Evaluation and Management of Concussion in Young Athletes. Curr Probl Pediatr Adolesc Health Care. 2018;48(5-6):139-150.
2. Jackson WT, Starling AJ. Concussion Evaluation and Management. Med Clin North Am. 2019;103(2):251-261.
3. Santos A, Walsh H, Anssari N, Ferreira I, Tartaglia MC. Post-Concussion Syndrome and Sleep Apnea: A Retrospective Study. J Clin Med. 2020;9(3):691.
4. Fleck DE, Ernest N, Asch R, et al. Predicting Post-Concussion Symptom Recovery in Adolescents Using a Novel Artificial Intelligence. J Neurotrauma. 2021;38(7):830-836.
5. Concussive Events: Using the Evidence to Guide Physical Therapist Practice. J Orthop Sports Phys Ther. 2020;50(4):176-177.
6. Oleski SL, Smith GH, Crow WT. Radiographic evidence of cranial bone mobility. Cranio. 2002;20(1):34-38.
7. Lower Cranial Nerve Syndromes: A Review - Scientific Figure on ResearchGate. Available from: https://www.researchgate. net/figure/Anterolateral-view-of-the-contents-of-the-right-jugular-foramen_fig1_342773452 [accessed 3 Jan, 2023]
LEARN about the lastest techniques and technology from industry leaders with our free live and archived educational webinars. Our online seminars are a convenient way to access great information and upskill. Check out our most recent webinars:
• Elevate Your Dental Sleep Practice: Keys to Success with hosts Dr. Jeff Rodgers and Dr. Tiffani Stratton
• Medical Billing Credentialing with host Stan Jones, CDA, DLT
• An Orthodontic Approach to Sleep Medicine with host Dr. Michael Ellis
Narcolepsy is a rare neurologic disorder that is characterized by excessive daytime sleepiness. “Sleep” attacks, overwhelming episodes of sleepiness, may occur. The Epworth sleepiness scale score is a validated test that is frequently used to determine sleepiness. Scores vary from 0–24 and are based on likelihood of being sleepy in eight different clinical scenarios. Scores greater than 10 are considered excessive daytime sleepiness and most patients with narcolepsy show a severe amount of sleepiness with scores greater than 18.
Narcolepsy occurs in one per 2,000 people. Its age of onset varies from early childhood to the fifth decade with a peak around the second decade. The delay from symptom onset to diagnosis is typically very long, about 10-12 years. It occurs slightly more in men than women.

In addition to excessive daytime sleepiness, it has several other symptoms associated. These include sleep paralysis which is an inability move that occurs upon awakening from sleep or upon falling asleep. It can last a few seconds to a few minutes. Understandably, it can be frightening.
Sleep paralysis is also often seen in association with hypnagogic or hypnopompic hallucinations. These are vivid dream-like hallucinations that occur upon falling asleep or awakening from sleep, respectively. They
are sometimes frightening, have a surreal quality, and can either be very vivid and detailed or sometimes just consist of shadowy figures or shapes.
Cataplexy is an abrupt and reversible decrease or loss of muscle tone, frequently provoked by strong emotion such as laughter, anger, or surprise. Consciousness remains intact and it can also last for a few seconds to several minutes. There is no sensory component to cataplexy. Its presence distinguishes type one from type two narcolepsy. It is the last symptom typically to evolve in this disorder.
Disturbed nocturnal sleep is also present in 50% of patients with narcolepsy. While they usually have no trouble falling asleep, they often have restless sleep that is highly fragmented and often complain of insomnia. They also typically have early onset dreams. The average adult falls into their dreams after about 90 minutes of sleep onset. Narcoleptics can experience dreams within seconds to minutes of falling asleep. In addition, they experience an increased amount of REM throughout the night. The average adult has about 20-25% of dreaming during the night; a narcoleptic patient can have 30% or more dreaming.
Patients with narcolepsy also tend to have a higher incidence of other sleep disorders such as obstructive sleep apnea (estimates are as high as 50% of patients with narco-

lepsy have OSA), restless leg syndrome, periodic movements of sleep, and REM behavior disorder. Their increased cardiovascular risks are especially concerning. The incidence of myocardial infarction and cardiac arrest is 1.6 x higher than the average population. Hypertension is increased by 1.3 x, whereas heart failure is up by a whopping 2.6 x. Stroke is increased by 2.5 x. There are also increased rates of obesity, depression, and ADHD.
The pathophysiology of patients with narcolepsy and cataplexy, type one, is low hypocretin-1 levels in the central nervous system. Hypocretin (also called Orexin) is the neurotransmitter that promotes wakefulness, helps maintain motor control and inhibits REM sleep. It stabilizes the sleep-wake state.
There is also a genetic predisposition to narcolepsy with cataplexy and occurs much more commonly in people with HLA – DQB1*0602. Genetics alone, however, are not sufficient for the development of narcolepsy. Often other environmental factors are also involved. There is an increase evidence of the role of winter associated infections, specifically an increase in antistreptolysin O (ASO) antibodies, a marker of infection with Streptococcus pyogenes. Interestingly, increased ASO was also found in narcolepsy patients who developed the disorder after vaccination against H1N1. This suggests an autoimmune component.
Diagnosis is made based on the clinical scenario of excessive daytime sleepiness,

How Sleepy Are You?
How likely are you to doze off or fall asleep in the following situations? You should rate your chances of dozing off, not just feeling tired. Even if you have not done some of these things recently try to determine how they would have affected you. For each situation, decide whether or not you would have:
· No chance of dozing =0
· Slight chance of dozing =1
· Moderate chance of dozing =2
· High chance of dozing =3
Write down the number corresponding to your choice in the right hand column. Total your score below.
Situation
Sitting and reading ·
Watching TV ·
Sitting inactive in a public place (e.g., a theater or a meeting) ·
As a passenger in a car for an hour without a break ·
Lying down to rest in the afternoon when circumstances permit ·
Sitting and talking to someone ·
Sitting quietly after a lunch without alcohol ·
In a car, while stopped for a few minutes in traffic ·
Analyze Your Score
0-7: It is unlikely that you are abnormally sleepy.
8-9: You have an average amount of daytime sleepiness.
Chance of Dozing
Total Score =
10-15: You may be excessively sleepy depending on the situation. You may want to consider seeking medical attention.
16-24: You are excessively sleepy and should consider seeking medical attention.
sleep paralysis, hypnagogic/hypnopompic hallucinations, cataplexy, and disrupted nighttime sleep along with formal testing. First, ruling out other etiologies such as insufficient sleep syndrome, obstructive sleep apnea, hypothyroidism, depression, sedating medications, etc. should be done. If there no other reasons for these symptoms, then
Dr. Sahni has been in medical practice for 22 years. The first 11 years of her career she was an internist at Canyon Ranch Health resort. Since then, she has practiced sleep medicine exclusively. She opened her own practice, Swan Sleep Medicine, four years ago. When asked why she chose sleep medicine, she often jokes that she could not commit to a single organ. Fortunately, sleep medicine is a combination of pulmonology, cardiology, neurology, and psychiatry. Never boring, sleep medicine requires a multi-disciplinary approach to diagnosis and treatment. To that end, she has been certified in holistic medicine, nutrition, and Ayuvedic medicine as well as Sleep medicine. In general, sleep medicine is a happy field of medicine. When people are sleeping well, they feel more rested, of course, but also have better mood, sharper memories, lower heart risk, and stronger immunity. Dr. Sahni asks that you forgive the pun, but when sleep is improved, it’s like night and day! She evaluates patients in her office as well as administers home sleep tests to look for sleep apnea and insomnia studies to look at brain waves while sleeping. She treats a wide variety of adult sleep disorders. She is taking new patients.

an overnight polysomnogram should be performed to observe sleep. The polysomnogram should be normal and the patient should sleep at least six hours. The following day, an MSLT (Multiple Sleep Latency Test) should also be performed. This is a daytime sleep study where the patient is given four or five 20-minute nap opportunities. If they fall asleep in 8 minutes or less, this is considered hypersomnolence. It is an abnormally short amount of time to fall asleep. If during their nap opportunities they display two or more sleep onset REM periods (SOREMP), this is positive for narcolepsy. A urine drug screen may be obtained to rule out the influence of substances that could affect sleepiness.
Treatment involves good sleep hygiene with a regular wake and bed times, adequate
sleep opportunity, scheduled naps (naps are restorative in patients with narcolepsy, at least for a short while) and medications. Medications will be chosen based on the patient’s severity and symptomatology. They could include alerting agents/stimulants, anti-depressant medications such as selective serotonin uptake inhibitors (SSRIs) or serotonin and norepinephrine reuptake inhibitors (SRNIs) and sodium oxybate.
Narcolepsy is generally considered a chronic and irreversible lifelong disorder. Awareness, early detection and aggressive treatment can greatly improve quality of life at home and at work.
www.
READ the latest industry news and business

WATCH DocTalk Dental video interviews with KOLs
LEARN through live and archived webinars
RECEIVE news and event updates in your inbox by registering for our eNewsletter

CONNECT with us on social media
Sapphire is uniquely positioned “Expand North American sales and

Sapphire is uniquely positioned to impact the dental strategic “Expand North American sales and leverage the marketing organization

pillars. organization to drive adoption of a national turnkey brand”


OSA public awareness activities: website, social media, brochures, posters, videos, events and most importantly the B to C products
Complete turn on approach to Sleep implementation, ongoing coaching & support and new sales of equipment, software and services
Unique therapeutic framework for Chronic Headache, Migraine, TMD, Tinnitus, Vertigo, Pain Head, Neck, and Face
OSA public awareness media, brochures, importantly the Complete turn-key, implementation, new sales of equipment, Unique therapeutic Headache, Migraine, Head, Neck, and
501C3 Non-Profit Fully accredited, online, ondemand Dental Sleep Medicine credentialing. The only one of its kind in the world.



Medmark LLC is proud to be the leading interactive marketing and multi-platform advertising company focused on the niche specialties of dentistry. We are creating a healthier America through knowledge, due diligence, and experience, by empowering dental professionals with high quality clinical information in clear and concise language and showcasing innovative technologies.


www.nexusdentalsystems.com
 Nexus Bill
Nexus Airway
Nexus Bill
Nexus Airway
 by Daniel E. Taché, DMD
by Daniel E. Taché, DMD
In 2015, the American Academy of Sleep Medicine endorsed the use Oral Airway Therapy (OAT) devices for the treatment of mild Obstructive Sleep Apnea (OSA) because evidence showed a sufficient level of efficacy.1 More recently, MAD therapy has shown “impressive amelioration of symptoms” with and satisfactory efficacy in the majority of patients provided with MADs who were diagnosed with moderate OSA.2
of perceived benefits (residual fatigue).5,6,7 Furthermore, many of these patients reported that they will awaken with significant symptoms suggestive of sleep bruxism (SB).
The prevalence of RLS in patients reporting disturbed sleep and pain from sleep bruxism is between 14% 19%
Since 2015, commensurate with the favorable treatment outcomes with OAT therapy, there has been a significant increase in the number of dentists who are offering MAD therapy as an alternative to CPAP therapy, for the patients who present with appropriate structural phenotypes for an adequate response to repositioning of the mandible for control of OSA.
Historically, it was believed that SB was most often occurred shortly after respiratory-related events during sleep such as that in OSA or patients diagnosed with UARS. Furthermore, it was hypothesized that SB, characterized by rhythmic masticatory muscle activities (RMMAs) contributed to the restoration of a compromised upper airway during consequent to respiratory events. However, current evidence suggests that SB is more of a non-specific orofacial activity that is associated with numerous factors leading to sleep fragmentation but not solely respiratory events per se.8
and
Adherence with OAT was, until recently, mostly limited to self-reported data. Based on this self-reported data, OAT adherence showed a wide range of adherence (4-76%).3 More recent objective evaluation showed adherence to OAT was 83% for the first year but declined to 62-64% after 4 or more years.4
The most common, self-reported reasons for discontinuing the OAT treatment are significant side-effects (e.g., jaw pain, headache and/or bite changes) and/or a substantial lack

Restless Legs Syndrome (RLS), is a highly prevalent sleep disorder which can cause significant sleep fragmentation leading to SB. RLS affects 5-10% of the general population who meet the standard diagnostic criteria for RLS.9 The prevalence of RLS in patients reporting disturbed sleep and pain from SB, is much higher ranging between 14% and 19%.
RLS suffers who reported discussing their symptoms with a healthcare provider more often received an erroneous diagnosis for their RLS symptoms such as: poor circulation
(18.3%), arthritis (14.3%), back/spinal injury or problem (12.7%), varicose veins (7.5%) depression and anxiety (6.3%), and trapped nerve (5.6%). Typically, only 6.2% were given the correct diagnosis of RLS.10
The identification of the DSM patient with RLS is relatively simple but it all begins with the DSM clinician having a heightened awareness of the enormous prevalence of this significant affliction. The diagnosis of RLS is relatively simple because identifying RLS sufferers does not require a sleep study, it is a clinical diagnosis.
Clinical Pearl #1
Because RLS has such a high prevalence and can so degrade the quality of life of our patients, assume every DSM patient has RLS until he/she indicates that they are not so afflicted. Simply add the 4 questions below to your DSM intake/history forms.
Clinical Pearl #2
All DSM patients whose respiratory indices are normalized from OAT but despite an excellent response continue to have signs and symptoms of sleep-related bruxism and/ or have persistent excessive daytime sleepiness, should be suspect of having RLS until your clinical interview of those patients, i.e., asking if he/she reports symptoms of RLS listed below:
Do you have an urge to move your legs due to uncomfortable sensations such as itching, cramping, tingling?
Do you have an urge to move your legs when you’re resting or inactive?
Do you have an urge to move your legs that is relieved by moving your legs or stretching them
Do you have an urge to move your legs that worsens during the evening or at night?
Clinical Pearl #3
RLS is a very heritable condition and affects many members of the same family including children who may report “growing pains”.
Clinical Pearl #4
Most RLS patients have had this condition for their entire life and many will just dismiss

it as a variant of their “normal” sleep. Be Persistent. Let them know that sleep bruxism & orofacial pain upon awakening and/or persistent fatigue are in fact, not “normal” and that treatment is typically quite simple and does not require a sleep study.
If you choose not to treat RLS but persist to help establish a diagnosis of RLS and refer such patients to a qualified clinician for treatment, you have done much for your patient. Because of such efforts, it may enable your patient(s) to remain compliant with OAT while also potentially experiencing enhanced health and markedly increased quality of life.
1. Li, D. K. (2022). Sleep bruxism is highly prevalent in adults with obstructive sleep apnea: a large-scale polysomnographic study. Journal of Clinical Sleep Medicine, pp.jcsm-10348.
2. Balasubramaniam, R. P. (2014). Sleep medicine education at dental schools in Australia and New Zealand. J Dent Sleep Med, 1(1), pp.9-16.
3. Hoffstein, V. (2007). Review of oral appliances for treatment of sleep-disordered breathing. Sleep and Breathing, 11(1), pp.1-22.
4. Walker-Engstrom ML, T. A. (2002). 4-year follow-up of treatment with dental appliance or uvulopalatopharyngoplasty in patientswith obstructive sleep apnea: a randomized study. Chest, 121(3), pp:739–746.
5. Ramar, K. D. (2015). Clinical practice guideline for the treatment of obstructive sleep apnea and snoring with oral appliance therapy: an update for 2015: an American Academy of Dental Sleep Medicine clinical practice guideline. Journal of clinical sleep medicine, 11(7), pp.7.
6. Tallamraju, H. N. (2021). Factors influencing adherence to oral appliance therapy in adults with obstructive sleep apnea: a systematic review and meta-analysis. Journal of Clinical Sleep Medicine, 17(7), pp.14851498.
7. Izci, B. M. (2005). Clinical audit of subjects with snoring & sleep apnoea/hypopnoea syndrome fitted with mandibular repositioning splint. Respiratory medicine. 99(3), pp.337-346.
8. Kuang, B. L. (2022). Associations between sleep bruxism and other sleep-related disorders in adults: A systematic review. Sleep Medicine. (89), pp.31-47.
9. Lavigne, G. a. (1994). Restless legs syndrome and sleep bruxism: prevalence and association among Canadians. Sleep, 17(8), pp.739-743.
10. Allen RP, W. A. (2005). Restless Legs Syndrome Prevalence and Impact: REST General Population Study. Arch Intern Med., 165(11), pp:1286–1292.
11. Attali, V. C. (2016). Predictors of long-term effectiveness to mandibular repositioning device treatment in obstructive sleep apnea patients after 1000 days. Sleep medicine (27), pp.107-114.

12. Buyse B, N. P. ( 2023, 1). Short-term positive effects of a mandibular advancement device in a selected phenotype of patients with moderate obstructive sleep apnea: a prospective study. J Clin Sleep Med, 19(1), pp. 5–16.
Daniel E. Taché, DMD is a graduate of Tufts University School of Dental Medicine and completed an advanced General Dentistry Residency program with the Veterans Administration in Houston, TX, where he first practiced TMD/Pain therapy before relocating to Wisconsin. Dr. Taché attended an 18-month training program for the diagnosis and treatment of Myofascial Pain Dysfunction (MPD). Between 2008-2010 he conducted research on the relationship between Fibromyalgia and sleep disorders. He is a staff member of the TMJ & Orofacial Pain Treatment Centers, based in Milwaukee, and his practice of dentistry in Wisconsin is limited to TMD/Orofacial and Dental Sleep Medicine. In 2009, Dr. Taché was elected for a 3-year term as President of the Wisconsin Sleep Society. He currently serves on the Board of Directors. Dr. Taché is married to Kathy, his wife of 30 years, and has four children.
Restless legs syndrome (RLS) is a common sensorimotor neurological disorder characterized by an irresistible urge to move the limbs. The uncomfortable feelings are typically described as “creeping, tingling, pulling, crawling or painful” sensations deep inside the limbs. Of note, symptoms can involve other parts of the body as well, particularly among those with a longer course of the disease.1 Other features of RLS include worsening of symptoms at night or with inactivity and development of complete or partial relief with movement.2,3
This self-instructional course for dentists aims to define the sensorimotor neurological disorder called Restless Legs Syndrome (RLS); offer a comprehensive view of its impacts, symptoms, and treatment; and provide common language that dentists can use with other medical providers.
Dental Sleep Practice subscribers can answer the CE questions online at https://dentalsleeppractice.com/continuing-education/ to earn 2 hours of CE from reading the article. Correctly answering the questions will demonstrate the reader can:
• Identify symptoms of Restless Legs Syndrome.

• Realize the features that differentiate this condition from other similar conditions.
• Realize the association of RLS with other cardio-cerebral vascular diseases.
• Consider the benefits and risks of non-pharmacological management of RLS.
• Recognize the benefits and risks of certain forms of pharmacotherapy for RLS.
The prevalence of moderate to severe RLS symptoms, occurring at least twice a week, is about 1.5% to 2.7%.4,5 The symptoms of RLS often result in reduced quality of life and cause significant distress and impairment in social, occupational, educational or other important areas of daily function by the sheer impact on sleep, energy/vitality, cognition, or mood. For many patients, RLS can lead to depression and even increased risk of suicide.6,7 In one case control study, the odds ratio of having a lifetime suicidal ideation or behavior was much higher in those individuals with RLS even after adjusting for underlying depression and other confounders.6
Diagnosis of RLS is based on key clinical features in addition to differentiation from other similar conditions, and specification of clinical course and clinical significance of RLS according to the 2012 revised diagnostic criteria:2
1. An urge to move the legs often, but not always, accompanied by or felt to be caused by an uncomfortable and unpleasant sensations in the legs.
2. The urge to move or any accompanying unpleasant sensations begin or worsen during periods of rest or inactivity such as lying down or sitting.
3. The urge is partially or totally relieved by movement, such as walking or stretching, at least as long as the activity continues.
4. The urge often occurs or are worse in the evening or at night than during the daytime.
5. The occurrence of the above features cannot be solely accounted for as symptoms primary to another medical or a behavioral condition (e.g., myalgia, venous stasis, leg edema, arthritis, leg cramps, positional discomfort, habitual foot tapping).
A. Chronic-persistent RLS Symptoms defined by occurring at least twice a week on average for the past year when not treated.
B. Intermittent RLS Symptoms occur less than twice a week on average for the past year when not treated.
Recent studies suggest the association of RLS and cardio-cerebral vascular diseases. A Canadian study, enrolled 30,097 participants, found that higher carotid intima-media thickness in patients with RLS, suggesting RLS is associated with atherosclerosis.3 Factors correlated with higher atherosclerotic
risk include a chronic diagnosis of RLS over 3 years duration with frequent symptoms.8 Underlying mechanisms were thought to be due to a nocturnal increase in cardiac sympathetic surge and blood pressure. However, other studies showed conflicting results. A cross-sectional study among 22,786 participants of the US Physicians Health Studies I and II used age- and multivariable-adjusted logistic regression models to evaluate the association of cardiovascular disease, vascular risk factors, and RLS. The study reported an increase in the prevalence of stroke but decreased prevalence of myocardial infarction in patients with RLS.9 Women’s Health Study of 30,262 participants with similar design; however, demonstrated no association between prevalent cardiovascular disease (including major cardiovascular disease, myocardial infarction, and stroke) and RLS prevalence.10 The complex association of cardiovascular disease and RLS was thought to be confounded by the presence of comorbid conditions such as hypertension and other vascular risk factors such as obstructive sleep apnea, etc.11 A retrospective cohort study within Kaiser Permanente Northern California (KPNC), including 7,621 primary RLS and 4,507 secondary RLS patients, found
Zhu Zhu, MD, PhD, conducted clinical research on stroke at the University of California Irvine and published work on substance abuse and stroke in young patients before joining the University of Kentucky. Her clinical and research interests include stroke and neurocritical care. Dr. Zhu is a member of the American Heart Association/American Stroke Association and the American Academy of Neurology. She recieved her MD from Shanghai Medical College, Fudan University, Shanghai, China followed by her PhD in Neuroscience from the Department of Neurology, Huashan Hospital, State Key Laboratory of Medical Neurobiology, Fudan University.
Saniya Pervin, MBBS, graduated from Kasturba Medical College, Manipal, India. Dr. Pervin's clinical and research interests include Vascular Neurology, Behavioral and Cognitive Neurology, Epilepsy, and Neuromuscular disorders.
Daniel O. Lee, MD, FAAN, FAASM, received his Neurology training at the Washington University Barnes-Jewish-Children Hospital in St. Louis, MO. Additionally, Dr. Lee completed his training in Sleep Medicine at The Stanford University School of Sleep Medicine in Palo Alto, California. He authored the first paper on the treatment of Restless Legs Syndrome with Ropinirole and the first Alpha 2 Delta Ligands treatment. Dr. Lee has published extensively in peer-reviewed journals and served on the National Scientific Advisory Board of RLS research. His recent publication in the Journal of Clinical Sleep Medicine led to the FDA mandating label changes for all the Dopamine Agonists in the treatment of RLS in November 2019. He has received numerous teaching awards including the AOA Medical Honor Society Faculty Teaching Award and has presented at various national and international conferences including the International Conference on Translational Research in Beijing, China and the International Congress of Parkinson Disease and Movement Disorders in Paris, France. He is the recipient of the 2020 Kentucky Senate Commendation for his accomplishments. He is serving as the Medical Director at the Kentucky Neuroscience Institute and has served as the President of the Kentucky Sleep Society. He is also the Chief of Staff at the Frankfort Medical Center.
primary Restless Legs Syndrome (RLS) was associated with a slight increased risk of hypertension but not associated with new-onset cardiovascular disease or coronary artery disease. In contrast, secondary RLS was associated with an increased risk of CVD, CAD, and hypertension.12 In summary, there isn’t enough data to confirm this complex association between cardiovascular disease and RLS. Further clinical trials that investigate the beneficial effect of RLS treatment on progression of cardiovascular disease may provide further insight for this complex relationship.
Treatment discussion for RLS should include the consideration of non-pharmacological approach and pharmacotherapy, and this must be individualized and closely monitored by the provider due to variability with periods of exacerbation and remission.
Nonpharmacologic therapies may obviate the need for medications in mild cases of RLS and may even allow a reduction in dosage in patients with moderate or severe disease in some cases. Determine the patient’s iron status and replace iron as indicated. Consider the role of current medications in causing or exacerbating the underlying restless legs such as antidepressants, neuroleptic agents, dopamine-blocking antiemetics such as metoclopramide, or sedating antihistamines (including those found in nonprescription medications) may be contributing
and whether discontinuation is possible without causing the patient harm.13 Recommend mental alerting activities, such as video games or crossword puzzles, which have been reported to be beneficial. Consider a trial of abstinence from caffeine and alcohol. Consider the possibility of other concomitant sleep disorders, most importantly obstructive sleep apnea.
Concurrent sleep disorders, sleep fragmentation, or insufficient sleep may exacerbate RLS. Clinicians should especially inquire about symptoms suggestive of obstructive sleep apnea and pursue appropriate testing as indicated; in some cases, sleep apnea treatment results in improvements in RLS, eliminating the need for medications. Patients with RLS may have other causes of insomnia, including underlying anxiety and depression, and these may need further psychological intervention.
A randomized controlled trial showed that aerobic and resistance exercise significantly reduced RLS symptom severity. The exercise and control groups did not differ significantly in either the total RLS severity total score or the 8-point rating at baseline. However, severity scores on the RLS Rating Scale for the control group decreased less than 8% over 6 weeks, whereas the exercise group severity scores dropped by 39% during the same time period. Scores for both groups remained relatively stable from six to twelve weeks, with symptom improvement from baseline only evident for the exercise group.14

Pooled data from two randomized, double-blind, prospective clinical trials were analyzed to determine if vibratory stimulation can safely treat patients with moderately severe Restless Legs Syndrome as compared to shams device. Patients that were randomized to the vibrating pads had significantly better outcomes than did patients randomized to the sham pads, after adjustment for multiplicity, on examination of IRLS scale and MOS-II scale, which is a validated medical outcome study scale (P <=0.03).15
Evidence suggests that RLS is associated with low intracerebral iron stores due to as yet unclear defects in iron homeostatic mechanisms and downregulation of striatal dopamine receptors.
An evidence-based consensus paper16 recommended that all RLS patients with se-
A randomized controlled trial showed that aerobic and resistance exercise significantly reduced RLS symptom severity.
rum ferritin concentration of 75 mg/L or less and transferrin saturation below 45% should receive a trial of oral iron therapy.
A cause for iron deficiency should also be pursued in those with serum iron levels below the lower limit of normal. Iron should not be prescribed empirically because it may result in iron overload, especially in patients with previously unsuspected hemochromatosis. Follow-up ferritin determinations are needed, initially after 3 months and then every 3 to 6 months until the serum ferritin level is greater than 100 mg/L. Intravenous administration of iron should be first-line iron therapy if moderate to severe chronic persistent or refractory RLS is present.
Intravenous iron therapy is also recommended if oral iron cannot be adequately absorbed because of disorders of the gastrointestinal system or bariatric surgery or if oral iron is not tolerated, and RLS symptoms do not improve despite an adequate (3-month) trial of oral intake of iron.
The majority of the class I well-designed clinical trials for intravenous iron therapy in RLS used ferric carboxymaltose, the clinical response to treatment is rarely immediate and may be delayed for 4 to 6 weeks or longer. Other intravenous iron preparations that can be considered are low-molecular-weight iron dextran and ferumoxytol, both as single infusions. Although low-molecular-weight iron dextran has a lower risk of life-threatening allergic reactions (estimated at 1 per 300,000 uses) compared with the older high-molecular weight iron dextran, a test dose (25 mg) should be given first. Pretreatment with diphenhydramine is unnecessary and may exacerbate restless legs. If there has been an adequate response to an intravenous iron infusion but symptoms recur, repeated infusions can be given in at least 12-week intervals as long as serum ferritin concentration is below 300 mg/L and transferrin saturation is less than 45%.13
Carbidopa/levodopa, 25 mg/100 mg (1/21 tablet), can be used for RLS that occurs intermittently in the evening, at bedtime, or on waking during the night or for RLS associated with specific activities, such as airplane or lengthy car rides or theater attendance.
Problems with levodopa treatment include augmentation and rebound. Aug-
mentation (drug-induced worsening of RLS) may occur in up to 70% of patients taking levodopa daily, and the risk increases with daily doses of 200 mg or more. As a result, levodopa should be prescribed only for intermittent use, such as 3 or fewer times a week, although a lower risk of augmentation with such use has not been firmly established. Rebound, the recurrence of RLS in the early morning, occurs in 20% to 35% of patients taking levodopa.
Low-potency opioids – Intermittent use of low-potency opioids usually before bed can be effective. Doses of 30 to 90 mg of codeine, in combined preparations with acetaminophen, or 50 to 100 mg of tramadol can be taken before bed or during the night. Constipation or nausea may occur. Tramadol can rarely induce seizures and is the only nondopaminergic drug associated occasionally with the development of augmentation.
Benzodiazepines – Intermittent use of benzodiazepines or benzodiazepine receptor agonists before sleep may be considered such as temazepam, zolpidem, zaleplon, or eszopiclone, especially if the patient has another cause of poor sleep efficiency in addition to RLS, such as insomnia associated with psychophysiological factors.13
Pharmacotherapy: Chronic Persistent RLS
Alpha2-delta ligand – Treatment should start with an alpha2-delta ligand (gabapentin, pregabalin, or gabapentin enacarbil) unless patient factors suggest that a non-ergot dopamine agonist (pramipexole, ropinirole, or rotigotine patch) would be safer.
A 12-week, multicenter, double-blind, placebo-controlled study that compared the efficacy and tolerability of gabapentin enacarbil with placebo in subjects with moderate-to-severe primary restless legs syndrome showed that gabapentin enacarbil significantly improved mean IRLS total score at Week 12 LOCF (baseline: 23.2; Week 12: 10.2) compared with placebo (baseline: 23.8; Week 12: 14.0). The study also showed that gabapentin enarcarbil significantly improved sleep outcomes when compared to placebo.17
Factors for considering a dopamine agonist, instead of alpha 2 delta ligands, as initial treatment include obesity and its complications, past or present moderate or severe depression, gait instability, disorders causing
respiratory failure, and previous history of substance use disorder.
A double-blind, randomized, 12-week, multinational study compared the efficacy and safety of ropinirole and placebo in RLS, showed that improvements were significantly greater for ropinirole than placebo for change in IRLS score at week 12 with adjusted treatment difference of -2.5 (P = 0.0197).18
Dopamine agonists – When dopamine agonists are considered, nonergot agents like pramipexole, ropinirole, rotigotine patch should be prescribed because ergot agonists such as cabergoline and pergolide are associated with cardiac valvular fibrosis and other fibrotic reactions. Doses used are lower than approved for treatment of Parkinson disease because higher doses are associated with increased risk of augmentation. A second common adverse effect of long-term dopamine agonist use is impulse control disorder, with rate of occurrence estimated to be between 6% and 17%.19
Iron stores should be rechecked. If the serum ferritin level is less than 100 mg/L and symptoms are severe, intravenous iron therapy should be considered. Other exacerbating factors should be sought. These include the use of medications that can worsen restless legs; change in lifestyle, such as more sedentary behavior or shift work; and other causes of sleep disturbance, such as sleep apnea or chronic insufficient sleep. Consider combination therapy with drugs of different classes, taking into account the augmentation from dopamine agonists. Consider adding a second agent when trying to reduce the dose of the initial Dopamine agonist drug. Second agents may include an alpha2-delta ligand or a longer acting dopamine agonist and vice versa, a benzodiazepine (if RLS is present mainly at night with resulting insomnia), or a low- or high-potency opioid. Consider substituting an opioid such as oxycodone, hydrocodone, morphine, or methadone. In particular, consider low-dose methadone for severe refractory RLS resistant to other treatments.13, 20
syndrome/Willis-Ekbom disease diagnostic criteria: updated International Restless Legs Syndrome Study Group (IRLSSG) consensus criteria--history, rationale, description, and significance. Sleep Med 2014; 15:860-873.
3. Zolfaghari S, Dasgupta K, Postuma RB. Restless Leg Syndrome and Objectively-Measured Atherosclerosis in the Canadian Longitudinal Study on Aging. Mov Disord. 2020 Dec;35(12):23142318. doi: 10.1002/mds.28326. Epub 2020 Oct 12. PMID: 33044035.
4. Allen RP, Bharmal M, Calloway M. Prevalence and disease burden of primary restless legs syndrome: results of a general population survey in the United States. Mov Disord. 2011;26(1):11420.
5. Allen RP, Stillman P, Myers AJ. Physician-diagnosed restless legs syndrome in a large sample of primary medical care patients in western Europe: Prevalence and characteristics. Sleep Med. 2010;11(1):31-7.
6. Para KS, Chow CA, Nalamada K, Kakade VM, Chilakamarri P, Louis ED, et al. Suicidal thought and behavior in individuals with restless legs syndrome. Sleep Med. 2019; 54:1-7.
7. Zhuang S, Na M, Winkelman JW, Ba D, Liu C-F, Liu G, et al. Association of Restless Legs Syndrome with Risk of Suicide and Self-harm. JAMA Network Open. 2019;2(8): e199966-e.
8. Li Y, Walters AS, Chiuve SE, Rimm EB, Winkelman JW, Gao X. Prospective study of restless legs syndrome and coronary heart disease among women. Circulation 2012; 126:1689-1694.
9. Winter AC, Berger K, Glynn RJ, et al. Vascular risk factors, cardiovascular disease, and restless legs syndrome in men. Am J Med 2013; 126:228-235, 235 e221-222.
10. Winter AC, Schurks M, Glynn RJ, et al. Vascular risk factors, cardiovascular disease, and restless legs syndrome in women. Am J Med 2013; 126:220-227, 227 e221-222.
11. Ferini-Strambi L, Walters AS, Sica D. The relationship among restless legs syndrome (Willis-Ekbom Disease), hypertension, cardiovascular disease, and cerebrovascular disease. J Neurol 2014; 261:1051-1068.
12. Stephen K Van Den Eeden , Kathleen B Albers, et al Risk of Cardiovascular Disease Associated with a Restless Legs Syndrome Diagnosis in a Retrospective Cohort Study from Kaiser Permanente Northern California Sleep 2015 Jul 1;38(7):1009-15
13. Silber MH, Buchfuhrer MJ, Earley CJ, Koo BB, Manconi M, Winkelman JW, et al. The Management of Restless Legs Syndrome: An Updated Algorithm. Mayo Clinic Proceedings. 2021;96(7):1921-37.
14. Aukerman MM, Aukerman D, Bayard M, Tudiver F, Thorp L, Bailey B. Exercise and restless legs syndrome: a randomized controlled trial. J Am Board Fam Med. 2006;19(5):487-93.
15. Burbank F BM, Kopjar B, Segawa C. Sleep improvement for restless legs syndrome patients. Part I: pooled analysis of two prospective, double-blind, sham-controlled, multi-center, randomized clinical studies of the effects of vibrating pads on RLS symptoms. Research and Reviews in Parkinsonism. 2013;2013; 3:1-10.
16. Allen RP, Picchietti DL, Auerbach M, Cho YW, Connor JR, Earley CJ, et al. Evidence-based and consensus clinical practice guidelines for the iron treatment of restless legs syndrome/Willis-Ekbom disease in adults and children: an IRLSSG task force report. Sleep Med. 2018; 41:27-44.
17. Lee DO, Ziman RB, Perkins AT, Poceta JS, Walters AS, Barrett RW. A randomized, double-blind, placebo-controlled study to assess the efficacy and tolerability of gabapentin enacarbil in subjects with restless legs syndrome. J Clin Sleep Med. 2011;7(3):282-92.
18. Walters AS, Ondo WG, Dreykluft T, Grunstein R, Lee DO, Sethi K. Ropinirole is effective in the treatment of restless legs syndrome. TREAT RLS 2: a 12-week, double-blind, randomized, parallel-group, placebo-controlled study. Mov Disord. 2004;19(12):1414-23.
19. Hankin C, Lee DO, et al Increased Risk for New-Onset Psychiatric Adverse Events in Patients with Newly Diagnosed Primary Restless Legs Syndrome Who Initiate Treatment with Dopamine Agonists: A Large-Scale Retrospective Claims Matched-Cohort Analysis. J Clin Sleep Med. 2019; 15(09)
20. Lee DO, McClees A and Lee T Experts detail their strategies for RLS patients, including non-pharmacological and pharmacological treatments, as well as how to prevent and manage augmentation. Sleep Review 2016, Feb 29
AGD Code: 150
Date Published: February 20, 2023 Course Expires: February 20, 2026
Legal disclaimer: Course expires 3 years after publication date. The CE provider uses reasonable care in selecting and providing accurate content. The CE provider, however, does not independently verify the content or materials. Any opinions expressed in the materials are those of the author and not the CE provider. The instructional materials are intended to supplement, but are not a substitute for, the knowledge, skills, expertise and judgement of a trained healthcare professional.
Each article is equivalent to two CE credits. Available only to paid subscribers. Free subscriptions do not qualify for the CE credits. Subscribe and receive up to 8 CE credits for only $149 by visiting https://dentalsleeppractice.com/subscribe/.
n To receive credit: Go online to dentalsleeppractice.com/continuing-education/, click on the article, then click on the take quiz button, and enter your test answers
To provide feedback on this article and CE, email us at education@medmarkmedia.com.
1. Which of the following features are NOT consistent with typical symptoms of RLS:
a. Tingling of feet and legs worsening during nights
b. Creeping and crawling sensation of legs
c. Urge to move legs due to sensory discomfort; can involve other parts of body with longer course of the disease
d. Tingling, numbness of hands with neck worse during the days
2. Which of the following is FALSE regarding the 2012 revised diagnostic criteria for RLS:
a. An urge to move the legs always accompanied by, or felt to be caused by, uncomfortable and unpleasant sensations in the legs only
b. The urge to move the legs and any accompanying unpleasant sensations begin or worsen during periods of rest or inactivity such as lying down or sitting.
c. The urge to move the legs and any accompanying unpleasant sensations are partially or totally relieved by movement
d. The symptoms of RLS cause significant distress or impairment in social, occupational, educational or other important areas of functioning by their impact on sleep, energy/vitality, daily activities, behavior, cognition, or mood.
3. Which of the following description is correct about chronic-persistent RLS and intermittent RLS:
a. Chronic-persistent RLS Symptoms occurring at least twice a week on average for the past year when not treated. Intermittent RLS Symptoms occurring less than twice a week on average for the past year when not treated.
b. Chronic-persistent RLS Symptoms occurring at least once a week on average for the past year when not treated. Intermittent RLS Symptoms occurring less than once a month on average for the past year when not treated.
c. Chronic-persistent RLS Symptoms occurring at least once a week on average for the past 6 months when not treated. Intermittent RLS Symptoms occurring less than once a week on average for the past 6 months when not treated.
d. Chronic-persistent RLS Symptoms occurring at least twice a month on average for the past 6 months when not treated. Intermittent RLS Symptoms occurring less than twice a week on average for the past 6 months when not treated.
4. Which statement is INCORRECT regarding the mechanisms of association between RLS and cardiovascular disease:
a. Nocturnal increase in cardiac sympathetic activity and blood pressure in RLS patients
b. Con-founded by presence of comorbid conditions such as hypertension and other vascular risk factors
c. Risk of cardiovascular disease increases in RLS patients with longer course but infrequent symptoms
d. The association of RLS with cardiovascular disease may be driven by the fact that RLS causes poor sleep quality or quantity and the latter factors are independent risk factors for cardiovascular outcomes
5. What non-pharmacological intervention has been shown to reduce RLS severity?
a. Increasing caffeine intake
b. Sleep deprivation
c. Aerobic and resistance exercise
d. High fat diet
6. Which of the following electrolytes abnormality should be considered in RLS patients?
a. Magnesium
b. Iron
c. Zinc
d. Selenium
7. Treatment of intermittent RLS involves which of the following medications?
a. Metoclopramide
b. Carbidopa/Levodopa
c. Diphenhydramine
d. Escitalopram
8. What is the first line treatment for chronic persistent RLS?
a. Pramipexole
b. Ropinirole
c. Alpha 2 Delta Ligands
d. Rotigotine
9. What is an important adverse effect to be considered while using dopamine agonists?
a. Hyperglycemia
b. Weight gain
c. Depression
d. Impulse control disorder
10. What is an important adverse effect of levodopa therapy in RLS?
a. Augmentation
b. Hyponatremia
c. Weight gain
d. Seizures
Obstructive Sleep Apnea (OSA) is an intermittent collapse of the tongue into the uniquely at-risk human pharynx during sleep that disrupts breathing and contributes to numerous morbid long-term health consequences. OSA has been found amenable to treatment by dental prostheses that reposition the anatomic parts of the head, neck and pharynx. By initially registering a specific stable multidimensional mandibular interarch relationship in the mouth, an intraoral mechanical stent fabricated as close as possible to a position of optimal pharyngeal dilation serves to prevent collapse of the tongue and preserve patency in the upper airway.
There are few scientific correlates for simultaneous jaw comfort and pharyngeal airway size. Numerous techniques have been developed and are being used in clinical
D.ABDSMdental sleep practice to register the specific mandibular interarch relationship of optimal airway dilation, however many of them are incompatible with anatomic function. The first paper in this series1 discussed ”slant” in terms of differences between anterior and posterior stabilization devices. This second in the series discusses the effect of condylar asymmetry on interarch jaw registration devices. This article will discuss the interarch jaw registration devices that mechanically direct mandibular movement in a midline sagittal plane and expect to achieve optimal airway dilation and stenting.
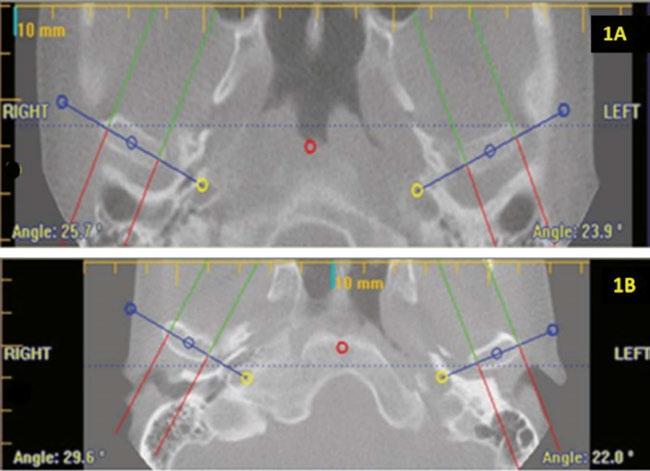
Human beings as a species may be considered bilaterally symmetrical. The reality is they are quite asymmetrical. Dentists doing craniofacial evaluations carefully note higher eye, higher ear, larger nostril and higher shoulder. Faces are universally asymmetric. A study by Moses, et. al.2 demonstrated that 95% of all human condyles are asymmetric relative to a sagittal plane, defined by the contact between teeth numbers 8 and 9 and the middle of the anterior border of foramen magnum. Moses’ study also demonstrated that anterior condylar protrusion at the level of the maxillary incisors is asymmetric by 5-5.5 millimeters. Intercondylar asymmetry is the normal state in human beings.
According to Sicher and DuBrul,3 the translatory component of joint movement is completely dependent on the shape of the articular eminence. This means that all movements of condyles with their discs must follow the curved surfaces of the articular eminentia. Normal human jaw movement functions smoothly on asymmetric curves and with asymmetric neuromuscular movement. Within human biologic systems,
joints never move in a straight line, either vertically, antero-posteriorly or laterally. The temporomandibular joints from the closed mouth position to the open position rotate forward and simultaneously glide along the articular disc and eminentia of the temporal bones out of the glenoid fossa. This is an anterior and downward movement guided by the neuromusculature, restricted by the rigid nature of the bony architecture, the hardness of the articular disc and the asymmetry of the condyles and limited by fibrous capsules. It is not a simple unidirectional pull-forward mechanism (Figure 2).
The mandible is the only bone with free-moving bilateral joints in the body. Smooth mandibular movement requires simultaneous complex neuromuscular coordination of both sides. The mandible of humans is not a simple hinge like other animals but has an extended range of motion and function, such as facilitating speech and separating food from airflow to prevent aspiration.
Normal interarch jaw position varies depending on the biological function being carried out, such as mastication, breathing, swallowing, incising, speaking, and screaming. Each different biological function utilizes different combinations of muscle activity and different muscle pressures. Each person has a unique combination of facial features and facial muscle alignment.
Pharyngeal airway dilation and stenting is accomplished by the complex inter-reaction between at least seven neurological/anatomic factors:
1. Create optimal space for the tongue in the mouth

2. Advance the tongue anteriorly
3. Advance the mandible anteriorly
4. Stretch the mylohyoid muscle
5. Lower the mandibular position

6. Advance the hyoid bone anteriorly
7. Change the alignment of the masticatory muscles
No one factor acting independently can accomplish unidirectional movement. All seven factors working in synchrony never causes unidirectional movement. Jaw movement to create an open airway is always multidimensional.
Since condylar movement rarely, if ever, occurs in a straight midline linear plane, interarch jaw registration devices that mechanically restrict protrusive movement to a midline cranial plane do not have a sound anatomic or scientific basis.
Allen J. Moses, DDS, DABCP, D.ABDSM, was in private dental practice for 48 years in Chicago Illinois and assistant professor at Rush University Medical School in the Department of Sleep Disorders and Research for 13 years. He holds three US Patents for intraoral sleep devices and a Patent Pending for a shim system for registering the posterior interarch jaw relationship for intraoral sleep appliances. He was a member of the United States Food and Drug Administration Dental Products Panel for 10 years, has authored a book on temporomandibular disorders and over 30 scientific papers on TMDs and sleep dentistry. He was book review editor

Protrusive or pull-forward interarch jaw positioners not only introduce an effect on the positions of the temporomandibular joints that is not desirable for patients having TMD problems, but they also misdirect protrusive movement as often as 95% of the time. This can carry over to the custom intraoral mechanical stent. Anterior push or pull mechanisms and appliance material in the palate can restrict proper tongue positioning and/or lip closure. Lateral adjustment mechanisms by either screw, strap or tube all direct jaw movement in a straight linear trajectory.
There is little or no substantiating scientific literature:
• That optimal airway dilation occurs
at a position arbitrarily determined as upper midline over lower midline
• On how far forward to protrude the mandible to establish optimal posterior airway dilation
• On how much vertical component is necessary in the interarch jaw registration to establish optimal posterior airway dilation
• On what combination of vertical and protrusive components is necessary or indicated scientifically to establish optimal posterior airway dilation for an oral sleep appliance.
Many dentists may fail to recognize that the jaw becomes trapped in an anatomy-required deflection coupled with a rigid-position pull-forward registration device and take a bite record in a forced position. Given that the milled and printed MADs out there are similarly constraining in jaw movement, clinicians should think multidirectionally about what they are affecting with their interarch jaw registration device and choice of MAD.
Purely mechanical adjustment devices such as screws, tubes, straps, hinges, rubber bands and springs bring about unidirectional structural changes that are a mere guess at achieving optimal posterior oral airway stenting, and they are capable of bringing about deleterious changes and pain.
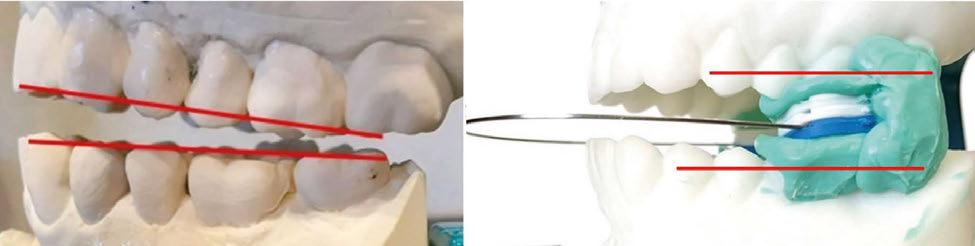
X-Slant™, a new disposable posterior/molar stabilization system makes it possible for a dental sleep clinician to factor the parameters of vertical, lateral, protrusive and slant into the design process for effective oral sleep appliances. Posterior/molar stabilization makes


Join DreamSleep – a nationwide network of dentists & physicians fighting sleep apnea. Our Whole Patient Program is a comprehensive plan that empowers dental practices with the knowledge, resources, and tools in order to provide patients with the highest standard of care for dental sleep medicine. The Whole Patient Program consists of four principles: Raise public awareness of Obstructive Sleep Apnea, DMSD, TMD, migraine and associated symptoms; train dentists to work with physicians and implement medical treatments; create screening and therapy programs for the industry; and connect patients with providers.
Through state of the art, individualized training and implementation processes, we help you seamlessly integrate these medical treatments into your dental practice to increase your patients’ quality of life and add a valuable revenue stream. Call 844.363.7533 today for details.
Comprehensive education you and your whole team: •Online, on-demand academic certification
•Individualized training programs
• In-office clinical training
•Team Coaching •Screening
possible the capture of multidimensional movement, eliminates slant by aligning the dental arches parallel to each other and enables normal shift to be registered.
X-Slant™ is comprised of the following parts: stackable shims and a shim coupler. The shims, are essentially square-shaped discs about 15 mm per side, having curved corners for patient comfort. The molar shim system is comprised of square-shaped, rigid plastic stackable shims of either 1.5 mm or 2.0mm thickness and having two alignment pegs on one side and two matching apertures on the other side. Said pegs and apertures allow the shims to be stacked in a stable, accurate, vertical, friction-fit manner. The essentially smooth underside of the shims also has a slot to receive a rectangular arch-wire that connects two sets of stacked shims for bilateral positioning inside the mouth.
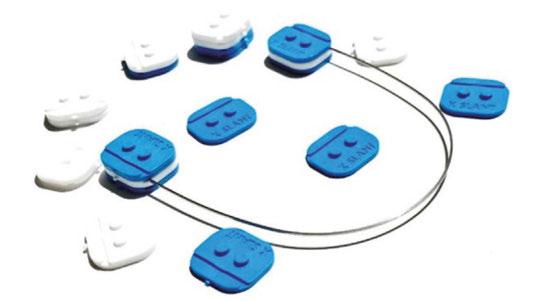
The patient closes on shim sets of varying heights placed bilaterally in the molar area until the clinician feels the proper vertical dimension is established. The intent of this paper is not how a clinician should arrive at the optimal vertical dimension. Consideration of the seven neurologic / anatomic factors mentioned earlier, as well as selection of lateral and protrusive dimensions are based on clinical judgment. Bite registration putty is then placed on the peg upside of both shim stacks, which is then placed in mouth. Patient is instructed to close in a comfortable bite until set. Patient is then instructed to slide along lower shim surfaces to where clinician determines is the best protrusive and comfortable lateral position and then instructed to hold that position for the clinician to scan the bite.
Bite registration putty can be added if stone or printed models are used.
There are few scientific correlates for simultaneous jaw comfort and pharyngeal airway size. There are scientific correlates for establishing the jaw position for an intraoral appliance. Establishing the initial position to dilate and stent the airway during sleep is possible based on embracing anatomic characteristics. Two factors of biologic movement have been introduced for consideration: slant and shift. Establishing the optimal position to dilate and stent the airway during sleep is not based on unidirectional movement of hard tissue components. The position of optimal pharyngeal airway dilation and stenting is best arrived at by posterior stabilization to establish a position of parallel upper and lower dental arches.
Humans have asymmetric translatory jaw movement, and the intracondylar asymmetry of human beings averages 5 degrees. Shift, as smooth multidimensional functioning over asymmetric curved systems is normal and healthy. However, within human biologic systems jaw joints never move naturally in a straight linear plane. Unidirectional mechanical adjustment devices are based on illogical, biologically flawed perceptions of jaw movement. Bite registration devices that mechanically direct protrusive movement to a midline cranial plane also do not have a sound anatomic or scientific basis.
Conclusion
Slant happens in oral sleep devices. It is bad. It can be eliminated.

Shift happens normally. It is okay. It should be facilitated in oral sleep devices. Anterior Stabilization Systems cause slant, restrict normal anatomic shift and can cause pain.
Available now is a new posterior stabilization system for interarch jaw registration that both eliminates slant and facilitates normal shift.
1. Moses AJ, Interarch Jaw Registration Devices for Oral Sleep Appliances: Consequences of Anterior vs Posterior Stabilization, Dental Sleep Practice, Winter 2022, p.32 - 36
2. Moses AJ, Bonato RA, Pacini P, Consideration of Intracondylar Angles in Determining Maxillo-Mandibular Relationship for Intraoral Sleep Appliances, Sleep Diagnosis and Therapy Vol 7 (3) p. 41 – 49, 2012
3. Sicher’s Oral Anatomy by DuBrul. CV Mosby, Philadelphia 7ed, 1980, p184
Dental Sleep Practice magazine is the sleep apnea publication for dentists –encompassing everything they need to know to properly treat this condition.
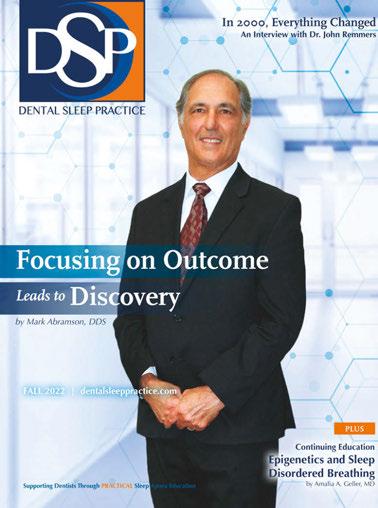
SUBSCRIBERS BENEFIT FROM:
s 4 fantastic issues per year
s 8 continuing education credits each year

s Clinical articles enhanced by high quality photography
s Practice management advice on how to make dental sleep more profitable
s Analysis of the latest groundbreaking developments in dental sleep
s Real-life profiles of successful dental sleep practices
s Technology reviews of the latest products
o 1 year print & digital subscription for $149
o 1 year digital only subscription for $79


 by Howard Hindin, DDS
by Howard Hindin, DDS
All of us who have joined me down the sleep / airway rabbit hole, continue to feed our passion and motivation with the successes we have, the people we help and the lives we change. Yet, as you will see, still only a small percentage of sufferers are recognized and treated. We have been preaching for years that more data is needed to move the needle of awareness. The Mute 2022 Annual Global Sleep & Snoring Report provides a wealth of information about how extensive this problem is and the work needed to be done.
The Mute Report is a study of 6,000 adults in the United Kingdom, the United States, and Australia. The report found that 96% of people believe quality sleep is very or somewhat important to their overall wellbeing, but only 64% are happy with the quality of their sleep.1 The problem? 51% say their own snoring; and 50% say someone else’s snoring.2
It’s not surprising that all that nocturnal noise has serious consequences, most notably sleep deprivation. According to the study, which was commissioned by nasal dilator brand Mute and conducted by One Poll, 42% of people say they wake up so tired that their everyday life is negatively affected, causing them to have trouble concentrating, to become argumentative, and even to nap at work.3 More than half admit that snoring is causing problems in their relationships.4
That last statistic is understandable considering that snoring impacts the snorer as well as their partner, primarily in regard to sleep deprivation. A full 50% of survey respondents accused their partner of snoring, 44% said their partner’s snoring was worse than their own, and 25% said it is the most annoying thing their partner does.5 While wrestling with sleep here in the U.S., 39% of snorers’ partners kicked, nudged or elbowed their noisy loved one; 23% slept in another room.6
Whether due to snoring, stress or anxiety, the majority of adults in the study are not achieving the coveted – and medically recommended – seven or eight hours of sleep per night. In the U.S., just 32% of adults achieve that idyllic number. Aussies and Brits fare somewhat better with 42% and 47% enjoying the suggested amount of sleep respectively.7

Taking the survey as a whole, a troubling trend emerges: a vicious cycle of widespread snoring leading to sleep deprivation leading to stress that ultimately has a physiological and psychological impact on individuals, partners, friends, families, co-workers, and communities. And nearly 122 million adults in the U.S. alone are caught in this cycle.8 Does this constitute a public health crisis? Perhaps it should.
It is well noted that insufficient sleep can lead to an increased risk of developing a number of chronic illnesses, such as cardiovascular disease, depression, obesity, and type 2 diabetes.9 Further, there is direct evidence linking obstructive sleep apnea to these diseases. In fact, it is estimated that between 40 – 60% of patients with cardiovascular disease also have obstructive sleep apnea.10
It is also well documented that sleep apnea and snoring are nearly always the result of a partially blocked airway due to structural or physiological condition of the mouth, jaw, nasal passages, tongue, or throat.11 In this sense, sleep apnea and snoring are symptoms of an Airway-Centered Disorder, a problem that impacts breathing 24 hours a day – not just but primarily during sleep – and that itself can lead to chronic health issues along with developmental, educational, and performance issues.12
By understanding and accepting that breathing disorders, airway disorders, snoring, sleep apnea, sleep disruption, and chronic illness are interrelated, the medical community can work together to apply functional medicine best practices to not only quiet the droning din but to positively impact the underlying disorder(s) causing it. Working together, sleep physicians, sleep dentists, ENTs, neurologists, pulmonologists, speech pathologists, and others have the ability to not only treat the symptoms of sleep apnea and snoring but to genuinely improve life quality through better breathing and better sleep.
Back to the Mute survey, the data shows that 22% of adults just here in the U.S. have
Dr. Howard Hindin is co-founder and chairman of the Foundation for Airway Health and the current president of the Academcy for Physiological Medicine and Dentistry. Dr. Hindin has more than 50 years of practice experience and is a pioneer in the relationship between dental issues and wholebody health.

talked to their doctor in an effort to improve their sleep.13 The survey didn’t dive deeper into the types of doctors consulted or the results of those discussions, but with an estimated eight million CPAP (Continuous Positive Airway Pressure) machines sold in the U.S. annually, there’s a good chance those doctors are sleep specialists.
While seeing a sleep specialist is a logical first step in a patient’s journey to get better sleep, this should not be the only step, because, while CPAP machines are often a good solution, they are not always the only solution. This is where the functional medicine approach to patient care can make a significant difference. Working together with medical professionals with different specialties and subspecialities, a sleep doctor might refer a patient to a speech pathologist for myofunctional therapy, an orthodontist for possible mouth expansion, or a sleep dentist for a fitted mouthpiece. And vice-versa.
If the end goal is to improve breathing, any and all specialists might be consulted to address the myriad of issues that could be at play causing snoring, sleep apnea, poor sleep, and the implications of each. The more information a patient has, the better decision they can make. The better the decision they make, the better sleep they get. The better sleep they get, the less argumentative, forgetful and tired they are. At the end of the day, it is collaboration by the right team of practitioners for each patient that will achieve optimal results. And with optimal results, the vicious cycle comes to an end, one patient –and their loved one – at a time.
1. Mute 2022 Annual Global Sleep & Snoring Report. 6, 7
2. Mute 2022 Annual Global Sleep & Snoring Report. 10
3. Mute 2022 Annual Global Sleep & Snoring Report. 8
4. Mute 2022 Annual Global Sleep & Snoring Report. 11
5. Mute 2022 Annual Global Sleep & Snoring Report. 10, 11, 13
6. Mute 2022 Annual Global Sleep & Snoring Report. 15

7. Mute 2022 Annual Global Sleep & Snoring Report. 6
8. Mute 2022 Annual Global Sleep & Snoring Report. 6
9. CDC. Sleep and Chronic Disease. www.cdc.gov/sleep/about_ sleep/chronic_disease. 2018

10. AHA Journals. Obstructive Sleep Apnea in Cardiovascular Disease. www.ahajournals.com. 2018
11. Foundation for Airway Health. www.airwayhealth.org.
12. Foundation for Airway Health. www.airwayhealth.org.
13. Mute 2022 Annual Global Sleep & Snoring Report. 15
Each drug-free treatment plan is tailored to address the individual patient’s symptoms, and includes the use of several tested technologies, including ultrasound, photobiomodulation, microcurrent, and muscle manipulation.






denture is in good condition and fits snug over the ridges, especially on the mandible. This will be crucial when needing to move the sleep device further forward over time.
Typically, you have 3 options when it comes to treating an edentulous patient with an oral device for sleep apnea.
1. Making the device over the dentures and treating it like a normal case
2. Making a tongue retaining device (TRD)
3. Making the device over the ridges with implant support on the mandible Let’s dig into which option would work best for your patient. To determine the best option for your edentulous patient you need to have a thorough exam and review in your consultation. It’s always best to have some “show and tell” when reviewing the options. This allows the patient to fully comprehend what exactly each option would look like. During the consult the most important question to ask is, “do you wear your dentures at night?”. If the answer is yes, then you could keep things simple and make a well-fitting device over their current dentures. For this option, you want to make sure the current
If the patient does not wear their dentures at night, we need to explore the other two options – Implant supported device, or a tongue retaining device. For the patients with no implant support and are sleeping without their dentures, the immediate option would be a tongue retaining device. A tongue retaining device has proven to have good results in treating sleep apnea; however, the compliance rate of TRDs is very low. I strongly encourage you to at least have a picture to show the patient how the device works before you go down this treatment path. Their bed partner may prefer the snoring over a lollipop tongue sticking out at them all night. Try to talk your patient into getting implants on the lower for a more comfortable and successful treatment outcome.
The third and final option, is making a sleep device over implants. This is the best option for your edentulous patients; it guarantees maximum space for the tongue, and secure anchorage for the sleep device. At minimum, the patient will need 4 mini-implants or two regular implants on the mandible to secure the sleep device. You’ll need to send wax rims, or a duplicated denture for mounting at the lab. If you’re using a firstclass lab, like DynaFlex, you can send the female locator attachments with the case and we will imbed them into the sleep device for you, or if you prefer you can pick them up chairside.
Don’t be fearful of the unknown; where there is a will there is a way! DynaFlex is your trusted partner in dental sleep medicine; we are here to help. Give us a call today so your sleep patients can start achieving the rest they deserve.

When you run into your first edentulous patient that needs to be treated for sleep apnea it can seem overwhelming. Don’t fret, there are options for a successful outcome for these patients!
“Treating my edentulous patients with an oral sleep device used to be a challenge and working with the DynaFlex team has eliminated my frustration and worries. The DynaFlex team assists me to ensure a successful treatment outcome even on the most difficult cases.”
– Thomas M. Gotsis, DDS
Edentulous Dorsal appliance
The Association of Army Dentistry (AAD) dedicated the Army Dentistry Monument on Friday, March 24, 2023, in a ceremony at the U.S. Army Medical Department (AMEDD) Museum in San Antonio, Texas. According to Dr Ronald Lambert (COL USA DC ret, Past President of the AAD), “The monument is a lasting tribute to all the soldiers, civilians, and spouses who have served and continue to serve in the Army Dental Care System in support of the U.S. Army and its military mission. The monument recognizes and honors the selfless contributions made by the diverse members of the Army Dental Care System and its key supporting components in the overall mission of Army Medicine.”
Founded in March 1911, the Army Dental Corps has a long and distinguished history of providing global dental services to soldiers and ensuring the readiness of the nation’s fighting forces. Even before 1911, the Army contracted dental surgeons to provide dental care to soldiers deployed to the new territories of a growing nation. The tradition of providing oral health services to soldiers wherever they are assigned continues to this day.
During World War II, more than 18,000 dentists served in uniform. It was during this time that the role of Army Dentistry expanded to include not only all levels of dental services, but also non-dental support and leadership. In the battle of Saipan in the Pacific, a Dental Corps Officer, Captain Ben Salomon, took command of the battalion aid station on the island. During an ensuing and desperate attack by enemy forces, CPT Salomon, also a skilled infantry soldier, heroically fought and defended the battalion aid station. He lost his life in the battle, but his gallantry and sacrifice did not go unrecorded. He was awarded the Medal of Honor posthumously, the only Army dentist to ever
receive the nation’s highest military award. The image of Dr. Ben Salomon was used in the design of the dental officer sculptured in the monument.
Army Dentistry was firmly established as a permanent and essential element in preserving the readiness and fitness of the fighting force. During the conflicts in Korea and Vietnam, Army Dentistry continued to provide direct support to soldiers in the field of operations.
The Persian Gulf War brought the largest expansion of Reserve Dental Support in Army Dentistry. Over 220 reserve dental officers and 320 reserve enlisted soldiers were called up to support the mission. Overall, 121 dental officers served in the theater. The expanded use of reserve forces continued throughout the later conflicts in Iraq and Afghanistan.
Today the Army Dental Care System is a highly trained and integrated team of military officers, non-commissioned officers (NCO), enlisted soldiers, and government service (GS) civilians. The Army Dental Corps has 970 dentists in uniform and is augmented with 455 GS and contracted civilian dentists. There are 1,225 NCOs and enlisted soldiers and 2,300 civilians providing clinical and administrative support. All services and specialties of the dental profession are provided to the nation’s service members. In addition, Army Dentistry is a leader in the postgraduate education and specialty training of young dentists, and the advanced training of enlisted soldiers and civilians. The mission of the Army requires that Army Dentistry be prepared to support soldiers wherever they are deployed. Colonel Tom Goksel, DDS, MD, says, “The Army Dental Corps is the leader in expeditionary dentistry and sustainment of force readiness … the mission is to have a ready Dental Corps capable of delivering global dental services in order to sustain the readiness of the total military force.”
The Association of Army Dentistry is proud to keep the legacy of the Army Dental Corps alive and preserve its rich history, in order to inspire those who choose to serve and support the nation’s military men and women. The Army Dentistry Monument Dedication commemorates this unique contribution to the U.S. Army and the nation.


Would you go to a party that opens doors for your practice? We all know the importance of working together with all the specialties in the medical field. If the patient has a nasal obstruction, they are referred to the otolaryngologist. If they have some indication of compromised lung function, it’s an easy referral to the pulmonologist. It’s off to the cardiologist if the patient’s blood pressure is high despite using multiple medications to control it. There are over 100 conditions that we can pick up during our airway evaluation which require a referral to a dental or medical colleague. Maybe the patient needs to be expanded or they have a tongue tie or large tori pushing their tongue into the airway, or their TMJs are on fire. Maybe they failed a trial of CPAP and/or they can’t wear an oral appliance. I could go on, but there’s nothing new here, right?
The real question is, how does one navigate this seemingly unbreachable hierarchy of health care providers? Mailing out referral cards or stopping by offices never achieved the desired results.
So…in 2017 I decided to throw a big meeting to attract many of the “players” we need to connect with. A big “geographically relevant” airway party seemed to be the answer. We decided to invite a well-known keynote speaker to help seduce the many professionals out of their silos. A little food and drink and a national speaker helped to melt the ice here on Long Island. The Pediatric and Adult Airway Network of New York launched, and we called it “PAANNY”.


After 5 years of this “regional style” meeting I can tell you that I highly recommend it. Last year we had 175 attendees and featured James Nestor, author of Breath, as the keynote. This year we have scheduled Uche Odiotu DMD who is a dentist and wellness coach doing the keynote after a morning of MDs giving 10 min Ted Talks in most of the specialties of medicine. This is a how to get everyone into a room together.
I’ve heard of offices having a series of small dinner parties with one person from each specialty and that just seemed to exclude more people that it included. On the other hand, large national organizations “set

the table” with a wide variety of health care specialists which is excellent for learning about connect ing the dots but when the rubber hits the road they tend to fail miserably at providing a local network of people to work with. We have all heard the clarion call for collaboration so many times I’m sure it has become just as annoying as a honking car alarm horn. What is the action that fosters an environment where the connections between specialties can take root?
I recommend that you make a local event like PAANNY in your own hood and invite everyone. On Long Island we have over 400 ENTs and although only a handful attend the yearly event, they are all invited.

I’m happy to help and give suggestions if you decide this path is for you. The first step is to form a board to brainstorm – a few creative minds are always better than one. Discuss a name for your group and possible speakers. Divvy up responsibilities so everyone feels important, and you don’t end up doing everything. Decide on a few catchy marketing phrases, create a flyer, and possibly a website. Having a few sponsors on board will help prime the pump, allow you to hire a professional if you need one, and so you’ll be able to advertise. Don’t overlook practice resources – it’s amazing how many ‘graphic artists’ there are lurking in some team member’s family!
I promise you it will be a fun filled journey and you’ll get to meet many people that you never would have had the opportunity to connect with. If you want to see how this works join us on May 5th, 2023, on Long Island. Registration information is available at PAANNY.org. I encourage you to offer dis-

counts if offices come with their entire staff. An orthodontic office from the east end of Long Island rented a bus and they brought 15 people! After the event over 60 people hung out in the bar and many friendships were spawned. Once a year is adequate to start this community of like-minded airway advocates, or as we like to call ourselves, Pulmonauts.
Think this sounds like you can’t do it? Nelson Mandela said, “It always seems impossible until it’s done.” I’ve done it, so it’s not impossible for you, either. All you really need to do is “copy and paste”.
Dr. Steve Lamberg has been practicing comprehensive restorative dentistry in Northport, NY for 40 years. Always passionate about sleep and wellness, he became a Diplomate of the American Board of Dental Sleep Medicine in 2011 and has served on their board review faculty. He holds several patents, and is the inventor of the Lamberg SleepWell Appliance, which is FDA-cleared for the treatment of OSA. Dr. Lamberg also launched and serves as the director of the Pediatric and Adult Airway Network of New York (PAANNY), to provide a local platform where dentists, physicians, orofacial myologists, and other related professionals learn and collaborate on treatment patients of all ages. Additionally, Dr. Lamberg serves as a Scientific Advisor at the Kois Center in Seattle. His recently published book for the general public, “Treat the Cause…Treat the Airway” correlates many common medical conditions to airway and sleep and is available on Amazon.


I promise you it will be a fun filled journey and you’ll get to meet many people.
If I’ve heard it once, I’ve heard it a hundred times from my dentist friends and clients: “I don’t sell dentistry,” or the more emphatic “I hate selling dentistry.”
Doctors, so this line of thinking goes, are demeaned by having to stoop so low as to have to “sell” treatment to a patient.
It seems that in the evolution of modern dentistry, the art and skill of selling is akin to the coccyx, a vestigial tail that hints of our simian, knuckle-dragging past.
Allow me to make the case that selling is not only an essential skill for a dentist, but that dentists who don’t know how or won’t engage in selling sleep and airway treatments are, in fact, harming their patients.
To illustrate the point, let’s stroll down memory lane to Physics 101.
You may remember that Schrödinger’s cat is a thought experiment in quantum mechanics in which a cat is placed in a sealed box with a radioactive substance that has a 50% chance of decaying and releasing poison. According to the principles of quantum mechanics, until the box is opened, and the cat’s fate is observed, the cat is both alive and dead at the same time.

But let’s imagine a similar scenario involving a dentist who is an accomplished clinician. This dentist has fantastic passion for their patients, has built a successful practice with thousands of patients, is an accomplished manager, has excellent communications skills, and loves to help afflict-
ed patients choose their best treatment plan, but is simultaneously the same dentist who avoids “selling dentistry.” Let’s call this person Schrödinger’s dentist.
Schrödinger’s dentist is in a sealed box with a patient diagnosed with moderate Obstructive Sleep Apnea. In this moment, Schrödinger’s dentist is simultaneously a skilled salesperson who knows exactly how to persuade the customer to accept treatment, and someone who doesn’t know the first thing about selling and is unable to convince the customer to move forward because they fear being called a ‘salesperson.’
This is, perhaps, where the parallel with Schrödinger’s cat experiment breaks down a bit because it’s not the fate of Schrödinger’s dentist that we are concerned with.
In this example, until the dentist makes or doesn’t make the sale, we can’t know the fate of the patient. Will they accept treatment and be healed or not choose treatment and have their condition deteriorate?
In this example of quantum entanglement, the fate of the patient rests with the selling skills of Schrödinger’s dentist.
So too does the health of your patients.
Sleep apnea is one of the few areas of dentistry that left untreated has an extraordinarily high mortality rate. Obstructive Sleep Apnea is a grave condition that can lead to a range of health problems including cardiovascular disease, hypertension, and stroke, even death. Early and continued intervention is highly responsive.
Sales is the penultimate step in the healing process.
You can read a patient’s chart, listen to their chief complaints, analyze their posture and anatomical symmetry. You can measure respiratory flow and volume using rhinomanometry and pharyngometry. You can measure minimum cross-sectional areas and inter-molar distances on a cone beam. You can prescribe sleep tests at home or in an overnight sleep facility. Armed with a diagnosis of Obstructive Sleep Apnea, you could recommend palatal expansion, myofunctional therapy, or even CPAP therapy.
But if you do not understand the rudiments of successful selling, you will not be able to allow the patient to accept the treatment that you know they so desperately need to heal and live their lives free of this terrible disease.
If the patient does not accept treatment, all your efforts and the efforts of your team and your colleagues will be for naught.
Ultimately, with too many of these treatment acceptance failures, you may become discouraged. Consciously or unconsciously, you may begin to shift your time and efforts away from treating sleep and airways and toward other “safer” areas of your practice.
Conversely, doctors who see the importance of selling and consider it an integral and valuable part of patient health, will spend time and resources gaining and maintaining selling skills so that they can increase the number of patients who will be seen, diagnosed, and healed by their practice.
It is far beyond the scope of this article to properly address the question of how a clinician can be a better salesman, but I think it’s important to address the subject of what selling is not.
Selling is not negotiation.
Selling is not manipulation.
Selling is not deception.
People who use these tactics to get you to do what they want are not selling, they are pushing.
If you don’t like “selling” because you don’t want to negotiate, manipulate, and deceive, then I don’t blame you. Neither would I.
Properly understood, selling is an act of mutual discovery of problems and solutions. In dentistry, the clinician is the chief detec-
tive, and the patient is often the scene of the crime.
While the rest of the dental office team is involved in the selling process, the primary players in this process are the patient and the doctor.
Especially in the Sleep Medicine world, the patients are coming to see you. They may like your team members and enjoy their company, but it is your expertise that has brought them to your chair.
It is you from whom they want to hear their symptoms.
It is you from whom they want to hear answers to their questions.
It is you by whom they want to be reassured.
It is you by whom they want to make and explain the treatment plan.
It is you who they are trusting to heal them.
This last step – the healing of patients – is our calling as an industry.
It is your calling as a clinician. You’re healing people and saving lives. But only if they let you.
Don’t let your fear of selling keep them from health!
Ben Waldman serves as a sales manager and lecturer for i-CAT and DEXIS. He has spoken to thousands of dentists around the world on clinical and commercial areas in dentistry but is a specialist in Sleep & Airway Disorders, how it’s diagnosed, treated, and reimbursed in the dental arena. Ben has been in dental imaging for over 20 years teaching dentists about both 2D and cone beam technology. He currently serves on the Board of Directors for the American Academy of Physiological Medicine and Dentistry (AAPMD). Prior to his career in dentistry, Mr. Waldman served in the Reagan White House as Associate Director of Presidential Personnel and as the Associate Director of Office of Public Liaison. He and his wife Rebecca have four grown children and live in Northern Virginia with their neurotic dachshund.

The healing of patients is our calling as an industry. It is your calling as a clinician. You’re healing people and saving lives. But only if they let you.

You’ve probably noticed that the healthcare system in the United States is expensive, dysfunctional, and often provides poor outcomes when serving its population. Yes, there are many reasons as to why this is the case, but one reason is the inadequate handling of treatment for chronic conditions.
A chronic disease is one that a patient must live with almost all their life, or at least for a very long time. Most people think of diabetes, heart disease, or depression when speaking of chronic conditions. One of the least thought about conditions, but one that affects a huge share of the adult population, is obstructive sleep apnea (OSA). Untreated OSA can exacerbate comorbidities like COPD, obesity, heart disease, depression, and many more. One of the most common symptoms of OSA is excessive daytime sleepiness, which causes poor work performance, diminishes social life, and leads to vehicular accidents at work or on the road.
For decades, the main treatment for OSA patients has been Continuous Positive Air Pressure, or CPAP: a pump that continuously
pushes air into patient’s airways, ensuring the obstruction is removed and the airway stays open. It works quite well if patients can tolerate it. For many patients, that is a very big IF. The bulky mask and noise, the cumbersome maintenance, being required to plug it into a wall socket, the dryness of mouth and throat, pain and discomfort from pressure of the mask on your face, the bloating…these are all complaints of CPAP users that make the overall experience miserable. Yet, to get their OSA and comorbidities under control, they must adhere to this treatment.
At Somnics, we believe there is a better way to approach the treatment of this chronic condition. Our engineers have designed and manufactured a small, light-weight device that is quiet, and battery operated. We designed this device with the patient’s comfort and lifestyle in mind. Our aim with this type of treatment is to make patients love it and use it night after night. We call it iNAP: intermittent Negative Air Pressure.
If a patient can breathe through his/her nose, iNAP is efficient in reducing the rate of apneas and hypopneas per hour. For those
that question their ability to breathe nasally, we have developed a coaching program with tools and tips to get the patient on the right track to breathing nasally again. iNAP has been proven in many clinical trials to effectively treat OSA as shown in the table at right. The FDA granted us a clearance in May 2020 (Class II device) to treat all severities of OSA.
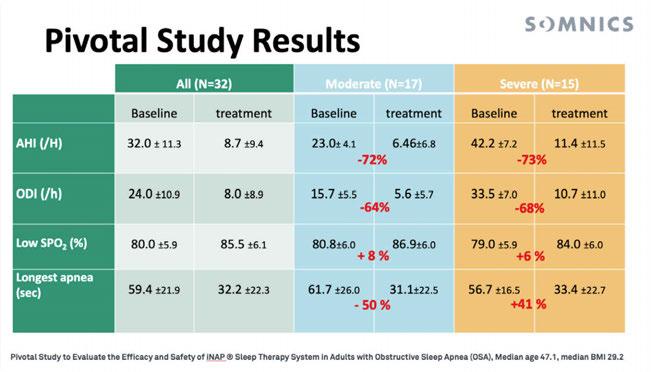
This is the dawn of a new era for sleep apnea treatment. A time of patient-centric medical care that understands that a chronic condition is best treated when the patient is motivated and willing to receive the treatment that is being offered.
Unlike CPAP, iNAP is a static pressure device. This means that the device has a small pump that will create negative pressure in the patient’s mouth. All the unsupported tissues, like the tongue or soft palate, will be pulled forward and upward to minimize the volume of the oral cavity in response to this low pressure. Once the target pressure is reached, the pump goes into an idle mode and the device is silent. Any leakage, or loss of negative pressure, is detected by a sensor, which triggers the pump to restart until the target pressure is reached again. Our goal is to have patients at the target pressure for more than 80% of the time. This means that 80% of the time the device is idle, it doesn’t need any energy from the battery, and therefore the Li-Ion battery of the device (like the one in your cell phone) can last for up to 6 nights without the need to recharge.
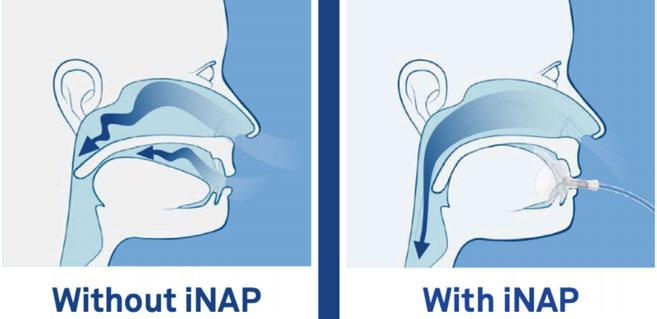
Our vision is to make an OSA diagnosis a non-event for the patient’s life, with little to no negative consequences for their lifestyles. Even better, this little device will get them back on track to a life full of energy, recovering from debilitating conditions, full of fun adventures, and free from annoying side effects.
• Need to go on a camping trip? Check!
• Bed partner is very sensitive to noise? Check!
• Don’t want the throat and mouth dryness? Check!
• Don’t want the bloating and stomach cramps? Check, Check!
As with any chronic condition, the symptoms and severity of OSA can evolve over time, meaning the treatment needs to adapt to stay efficient. iNAP allows for this flexibility through our companion app. Patients can
download the app on their phone to both follow the treatment progress and (soon) to allow remote tuning of the device’s pressure by their physician.
iNAP has rapidly gained users since its commercial introduction in January 2021. We have close to 1,000 patients in the US and distribution in almost every state. The patient experience as a user is more comfortable, and we have made the experience of getting the device and being trained how to use it properly a user friendly one. Now our system allows the patient to receive the device at home within 7-10 days from the time we receive their Rx from their physician!
In an effort to constantly improve the patient experience, we are eager to talk to as many providers and patients as possible to collect their feedback on the iNAP experience. We appreciate the opportunity to answer your questions and address your concerns. Our goal is to free as many patients as possible from the cumbersome hassles of living with OSA. If you have any question about iNAP, you’ll find many answers here: https://somnics.zendesk.com/hc/en-us.
Igave a keynote at the North American Dental Sleep Medicine Symposium (NADSM) last year and had the picture below on the screen.
Then I said, “If you build it…” and the audience echoed back enthusiastically, “they will come!”
I replied, “For your general practice, that was true. For DSM practice, not so fast. For baseball players to trudge through cornfields to find a ballpark, they gotta know what baseball is!
If they don’t, I don’t care what Kevin Costner does; ain’t no way they’re risking heat stroke and field mice to find a magical field.”
The point is, if you build a Field of Dental Dreams, they will indeed come. Dentistry is familiar.
However, if you build a Field of OSA Dreams, don’t expect to sell out your first game. You’ll probably have to invest in educating them, first.
Case in point: A year ago I was diagnosed with sleep apnea. My PCP referred me to a Sleep doctor where I expected to learn about

The Patient "Yep"
I have a clear need:
The Patient
I have a clear need:
• "It;s time for a cleaning""
• "Ouch. My tooth hurts" 4
I know where to go:
• "Can you recommend a good dentist?"
• "Hey, Siri. Best dentist in town?" 4
I understand the treatment:
• "Ah, OK. A filling? That makes sense."
• "An aligner? Oh, like Invisalign?" 4
Insurance coverage is clear:
• "A cleaning is covered every 6 months"
• "Yes, I've met my deductible" 4
• "My wife says I snore a lot. I bought her earplugs."
• "I'm tired all of the time. Guess I need Ambien." ?
I know where to go:
• "I guess I need to see my PCP?"
• "Or a Sleep Doctor?"
I understand the treatment:
• "An Oral Appliance? Like a talking refrigerator?"
• "I thought sleep apnea was treated with a CPAP."
Insurance coverage is clear:
• "I need to be a CPAP fail? Like get an F or something?"
• "You can 'order' a sleep test, but someone else reads it?"
CPAPs and oral appliance therapy (OAT) (which of course, I would not know about if I were not in the industry). Shocker, he never mentioned an oral device. I had to ask – scratch that – I had to practically demand OAT information. And I don’t think my experience is unique.
Let’s compare the marketing challenge of attracting new general patients (drills and fills) vs. new sleep patients (see Figures 1 and 2 on next page).
I’m not out to be a Debbie Downer here, folks. Besides, the readers of DSP already know this reality, right?
Maybe. At the NADSM I surveyed attendees on what they charge for an oral appliance. The answers ranged from $2,000$6,000, while they responded that their average cost for that appliance is well-under $1,000.
Then I asked them what they would be willing to spend on advertising to get a new OSA patient (not someone to come in for an eval, but someone to buy OAT from them). Over 60% said ‘under $100’.
That’s .015% up to 5% of revenue for a new patient, depending on what they charge.
For perspective, the average B2C company allocates 6% to 12% of total revenue annually on marketing. That’s for ‘older companies’ (over 5 years old with a recognized brand).
For younger companies (1-5 years old, no recognized brand), it’s 12%-20%.
(Hint: “An Oral Appliance? Like a talking refrigerator?”)
So what does all that math mean? You gotta spend more than $100 per new DSM patient. Typically, a lot more!
How much more? That depends on the answers to three questions:
1. The number of OAT you currently sell per month
2. The number of OAT you want to sell per month
3. How fast do you want to get there? (6 months? 1 year? 5 years?)
Using data from thousands of DSM ad buys across the country, The DSM Growth Calculator will tabulate what you need to spend, depending how many OAT you want to sell and how fast. Email the answers to the three questions to growthcalculator@ bullseyemediallc.com and the results will be emailed to you.
When it comes to luring the ghost of Shoeless Joe Jackson to a baseball field in Iowa, I have no clue – no insight. But I can tell you with certainty that if you build a Field of OSA Dreams, they will come. You just may have to educate, and advertise, a little more than anticipated.
Arrange the letters in each section, so every word is valid (across and down).
For the solution, visit www.dentalsleeppractice.com.




Air quality is CRITICAL to your practice. Contaminants are everywhere: Pathogens, Pollutants, Viruses, Bacteria & Fungi all threaten our air quality and quality of care.
Benefits of Air Quality Guard:
• Arm and ceiling intakes capture aerosols at the source and move them away from occupants
• Contaminated air is filtered through a 3 layer system, removing greater than 99.99% of all contaminants
• Reduces the spread of COVID-19 and reduces sick leave
• Negative pressure airflow cycle ensures that contaminants are captured before they can circulate
• Quietly and efficiently filters & replaces up to 100% of air with pure, clean air
• Power ful enough to replace all the air in the room every 7 minutes*
Introducing, ProSomnus EVO [PH], FDA cleared and Medicare E0486 verified. EVO [PH] is the only dual arm advancement device with innovative materials, manufacturing robotics and artificial intelligence designed to provide a better experience for all patients. Incorporating the ProSomnus precision OAT platform, EVO [PH] offers the best comfort, first-time-fit and reliability for a Herbst-style advancement mechanism providing 7.0mm total titration. EVO [PH] comes with a Best in Class, 3+2 Year Warranty.
✔ 100%(1) of Providers experienced first-time-fit, just like EVO

✔ 100%(1) of Providers would prescribe and recommend
✔ 90%(1) of Providers had no adjustments
✔ 94%(1) of Patients reported a smaller, more natural and comfortable device


✔ 51% More flexible for greater ease of use
✔ Anatomical splint design


✔ Visual laser markings on splint for advancement confirmation


STRONGER NEW!
✔ Highest medical grade class VI, biocompatible material
✔ 60% Stronger torquing arms, designed for the greatest durability

✔ 74% Greater robustness
✔ 9X Greater impact toughness
✔ 51% More flexible for greater ease of use
✔ 70% Less volume than traditional, dorsal style devices